Abstract
Background
Congenital syphilis incidence has more than tripled in recent years, in parallel with the resurgence of syphilis among reproductive-aged women. An understanding of risk factors associated with maternal syphilis infection can guide prevention of congenital syphilis through prenatal diagnosis and treatment. We aimed to describe factors associated with maternal syphilis and congenital syphilis at a public medical center in Chicago, Illinois.
Methods
Maternal syphilis diagnoses were identified using a database for local health department reporting. Medical records were reviewed for infant congenital syphilis diagnoses, sociodemographic information, medical history, and other behavioral factors. Maternal characteristics associated with congenital syphilis were assessed using logistic regression.
Results
Of 106 maternal syphilis diagnoses between 2014 and 2018, 76 (72%) had a known pregnancy outcome; of these, 8 (11%) delivered an infant with congenital syphilis. Women with psychiatric illness and noninjection substance use each had a >5-fold increased odds of having an infant with congenital syphilis. Cases with congenital syphilis were more likely to have late or scant prenatal care and initiated treatment nearly 3 months later in pregnancy. None were human immunodeficiency virus positive or reported incarceration, intravenous substance use, sex work, or having sex with men who have sex with men.
Conclusions
Maternal psychiatric illness and substance use may have complicated prenatal care and delayed syphilis treatment, describing a population in need of public health intervention. Women experiencing such barriers to care may benefit from closer follow-up after a prenatal syphilis diagnosis to prevent congenital transmission.
Keywords: congenital syphilis, maternal-child health, sexually transmitted infections, STI, syphilis, TORCH infections
Understanding congenital syphilis risk factors helps identify women experiencing barriers to care. Our medical record review suggests that maternal psychiatric illness and substance use complicated prenatal care and delayed syphilis treatment, describing a population in need of public health intervention.
There has been a major resurgence of syphilis in the United States (US), including among reproductive-aged women, for whom primary and secondary syphilis rates more than tripled from 2011 to 2018 [1–4]. Coinciding with this rise in syphilis among women, congenital syphilis has increased from 8.4 per 100 000 live births in 2012 to 33.1 in 2018 [1–5]. Although much less common than syphilis in adults, untreated congenital syphilis causes more deaths with 78 stillbirths and 16 infant deaths in 2018, and a case-fatality rate of 6.5% [4, 6]. Furthermore, congenital syphilis disproportionately impacts minority women and their families. In 2018, 39.1% of mothers of infants with congenital syphilis in the US were non-Hispanic Black and 31.5% were Hispanic [7]. In Chicago, congenital syphilis incidence has ranged from 10 to 24 cases per year since 2009 [8–10]. Incidence peaked in 2015 followed by a decrease to 11 or 12 cases per year after 2 congenital syphilis media campaigns [11].
Fortunately, early prenatal screening and treatment is highly effective for preventing congenital syphilis. Timely treatment with penicillin during pregnancy reduces the risk of congenital syphilis by 97%, stillbirth by 82%, and neonatal mortality by 80% [1]. The American Academy of Pediatrics (AAP) and American College of Obstetrics and Gynecology (ACOG) advise universal syphilis screening at the first prenatal visit in the first trimester and rescreening at the third trimester and delivery in high-risk populations [12, 13]. While Illinois and 12 other states mandate universal screening at the first trimester and again at either the third trimester or delivery, 31 states mandate universal screening only once during pregnancy and 6 states have no mandate for universal screening [14]. While some states require targeted prenatal syphilis screening in situations where women are considered “high risk,” this population is rarely defined in the laws and is largely left to providers’ interpretation.
The US Preventive Services Task Force includes those living with human immunodeficiency virus (HIV), with a history of incarceration or commercial sex work, or residing in communities with a high syphilis prevalence as some specific high-risk groups [15]. Meanwhile, recent studies have attempted to further characterize and describe risk factors associated with the more recent surge in congenital syphilis and syphilis in reproductive-aged women. A large national study conducted in 2018 found that (1) lack of adequate maternal treatment despite timely diagnoses and (2) lack of timely prenatal care were the most commonly missed opportunities for congenital syphilis prevention [7]. However, in a review of 9883 reported syphilis cases in pregnant women nationwide between 2012 and 2016, nearly half of the women did not report any of the queried risk factors during case investigations, suggesting that screening methods that rely solely on behavioral risk factors would miss a large proportion of pregnant women with syphilis [16].
A deeper understanding of factors associated with the resurgence of maternal syphilis infection and subsequent congenital syphilis can help guide clinical and public health interventions to target populations at highest risk. In this retrospective cohort study, we aimed to describe characteristics of pregnant women with syphilis and risk of congenital transmission in an urban public medical center.
METHODS
Study Design, Setting, and Participants
We conducted a retrospective cohort study of all pregnant women diagnosed with intrapartum syphilis at the University of Illinois Health and Hospital System (UIHealth) from December 2014 to December 2018. UIHealth is a public academic medical center that serves a medically underserved patient population with a high syphilis prevalence. It provides a broad range of services for pregnant women, including family medicine and obstetrics/gynecology outpatient practices, a federally qualified health center, inpatient antepartum unit, obstetric emergency room, and a high-risk labor and delivery unit. UIHealth providers screen all pregnant women for syphilis at the first prenatal visit and the third trimester in accordance with Illinois law (410 ILCS 320/1). UIHealth laboratories use the reverse-sequence screening approach, which includes a treponemal enzyme immunoassay/chemiluminescence immunoassay (EIA/CIA), followed by a nontreponemal rapid plasma reagin (RPR) test if the EIA/CIA is positive. Discordant results are confirmed by an additional Treponema pallidum antigen test. Pregnant women who initiate prenatal care at an outside clinic may undergo first trimester screening using the traditional screening approach, which involves an initial nontreponemal test followed by, if positive, a confirmatory treponemal test.
We included all women with an intrapartum syphilis diagnosis during the study period; this information was obtained from a database used for reporting syphilis diagnoses to the Chicago Department of Public Health. We excluded women with an unknown pregnancy or congenital syphilis outcome. Medical records of the women and their infants were reviewed for maternal syphilis testing, diagnosis, and treatment; and congenital syphilis diagnosis in the newborn (newborns are not discharged from the hospital without determination of maternal syphilis serology). In addition, we abstracted data on prenatal course and pregnancy outcomes; sociodemographic information; medical history, including psychiatric diagnoses (Diagnostic and Statistical Manual of Mental Disorders, 5th edition diagnosis, or receiving medication or counseling for a mental illness); and other sociodemographic factors.
Definitions
Women with a history of completely treated syphilis who had serologic test results (ie, RPR) with low, stable titers of 1:4 or less 1 year or more after treatment were defined as being serofast. For our analysis, maternal treatment was considered to be indicated in patients who had new infections, those with previous incompletely treated infections, or those who were not serofast from a previously treated infection. However, providers were able to use their own clinical discretion for ordering tests and treatments that may or may not have aligned with AAP and ACOG guidelines. Late prenatal care was defined as having the first prenatal care visit in the second trimester or later. Scant prenatal care was determined by the patient’s provider and their documentation in the medical record.
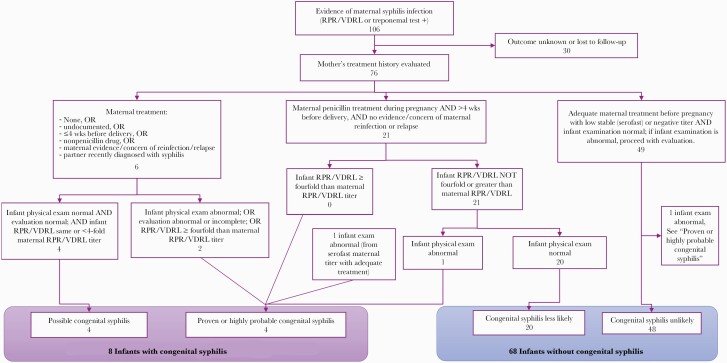
For congenital syphilis diagnoses, we used the 2018 AAP Red Book Diagnostic Algorithm for Infants Born to Mothers With Reactive Syphilis Serologic Tests to categorize infants as having highly probable, possible, less likely, or unlikely congenital syphilis (Figure 1) [17]. For analyses, we defined the “with congenital syphilis” group as women who delivered infants diagnosed with highly probable or possible congenital syphilis; and the “without congenital syphilis” group as women with infants diagnosed with less likely or unlikely congenital syphilis. These groupings were based on the significant difference in clinical management between infants born with highly probable or possible congenital syphilis (10 days of parenteral antibiotics and further evaluation recommended) and those with less likely or unlikely congenital syphilis (single-dose or optional antibiotics and further evaluation not recommended).
Figure 1.
Maternal syphilis and infant congenital syphilis diagnoses, based on the American Academy of Pediatrics Red Book diagnostic approach for congenital syphilis. Abbreviations: RPR, rapid plasma reagin; VDRL, Venereal Disease Research Laboratory (nontreponemal) test.
Statistical Analysis
We assessed sociodemographic and clinical characteristics of women with an intrapartum syphilis diagnosis and compared characteristics of those whose infants had a diagnosis of congenital syphilis to those without congenital syphilis using Fisher exact or Wilcoxon rank-sum tests, as appropriate. We performed logistic regression analyses to assess maternal factors associated with congenital syphilis. Due to the small number of congenital syphilis cases documented, we did not perform multivariable logistic regression analyses.
Patient Consent Statement
This study was approved by the University of Illinois at Chicago Institutional Review Board. The requirement for informed consent was waived as the study involved retrospective review of medical records.
RESULTS
Characteristics of Women With Intrapartum Syphilis
From December 2014 through December 2018, 106 pregnant women tested positive for syphilis. Of these, 30 (28%) were excluded due to an unknown pregnancy or congenital syphilis outcome. Among the 30 excluded cases, 18 (60%) were completely lost to follow-up and 4 (13%) had abortions. Seven (23%) had live birth deliveries at outside hospitals, but information regarding the delivery and infant congenital syphilis outcomes were unavailable. There was 1 (3%) report of fetal demise at >33 weeks of gestational age (GA) (possibly at term); this delivery occurred at an outside hospital and no information about congenital syphilis infant evaluation was available. There were no reported miscarriages.
Of the 76 women included, 18 (24%) were diagnosed in December 2014 and 2015, 29 (38%) in 2016, 11 (14%) in 2017, and 18 (24%) in 2018. As outlined in Figure 1, there were 8 women (11%) in which congenital syphilis was either highly probable or possible (with congenital syphilis group) and 68 (89%) in which congenital syphilis was either less likely or unlikely (without congenital syphilis group). There were no stillborn deliveries. None of the women presented with symptoms of syphilis.
Median age at delivery was 26 years (interquartile range [IQR], 24–32 years); 68 women (89%) were Black, 4 (5%) were Hispanic, 3 (4%) were foreign born, 8 (11%) were experiencing homelessness, and 67 (88%) had public or no medical insurance (Table 1). Forty-four (61%) had late or scant prenatal care, and the median GA at initiation of prenatal care was 11.2 weeks (IQR, 6.4–25.9 weeks). Ten (13%) had a history of psychiatric illness, 15 (20%) reported any substance use, 1 (1%) reported intravenous drug use (IVDU), 3 (4%) had HIV, and 22 (29%) were diagnosed with a recent sexually transmitted infection (STI) other than HIV or syphilis. Three (4%) reported having female sex partners and none reported having partners known to be men who have sex with men (MSM).
Table 1.
Maternal Characteristics
| Characteristic | Total (N = 76) |
Highly Probable or Possible Congenital Syphilis (n = 8) | Less Likely or Unlikely Congenital Syphilis (n = 68) | P Value |
|---|---|---|---|---|
| Obstetric information | ||||
| Median age at delivery, y (IQR) | 26 (24–32) | 24 (23–27) | 27 (24–32) | .29 |
| Median gravida (IQR) | 4 (3–5) | 4 (3–4) | 4 (2–5) | .85 |
| Median parity (IQR) | 1.5 (1–3) | 2 (1–3) | 1 (1–3) | .47 |
| Median GA at birth, wk (IQR) | 39.00 (37.29–39.57) | 39.07 (37.32–39.71) | 39.00 (37.29–39.46) | .72 |
| Late or scant prenatal carea | 44 (61) | 6 (75) | 38 (56) | .46 |
| Median GA at initiation of prenatal care, wk (IQR) | 11.21 (6.43–15.86) | 15.21 (12.18–16.46) | 10.43 (6.43–15.86) | .38 |
| Race and ethnicity | ||||
| Black | 68 (89) | 7 (88) | 61 (90) | .61 |
| White | 4 (5) | 1 (13) | 3 (4) | |
| Other or unknown race | 3 (4) | 0 (0) | 3 (4) | |
| Hispanic or Latina | 4 (5) | 1 (13) | 3 (4) | .20 |
| Residence and place of birth | ||||
| Chicago resident | 71 (93) | 8 (100) | 63 (93) | .99 |
| Residing in Chicago Community Area with a high EHIb | 51 (72) | 6 (75) | 45 (71) | .99 |
| Homelessness within past 12 moc | 8 (11) | 2 (25) | 6 (9) | .20 |
| Foreign born | 3 (4) | 0 (0) | 3 (4) | .99 |
| Health insurance | ||||
| Private | 9 (12) | 0 (0) | 9 (13) | .63 |
| Public/Medicaid | 61 (88) | 8 (100) | 53 (78) | |
| None | 6 (8) | 0 (0) | 6 (9) | |
| Social, behavioral, and clinical characteristics | ||||
| Psychiatric illness within past 12 moc | 10 (13) | 3 (38) | 7 (10) | .07 |
| Substance use within past 12 moc | 15 (20) | 4 (50) | 11 (16) | .04 |
| Intravenous/injection drug use within past 12 moc | 1 (1) | 0 (0) | 1 (1) | .99 |
| HIV | 3 (4) | 0 (0) | 3 (4) | .99 |
| STI diagnosis other than syphilis or HIV within past 12 moc | 22 (29) | 1 (13) | 21 (31) | .43 |
| Anonymous sex within past 12 moc | 1 (1) | 1 (13) | 0 (0) | .11 |
| Positive intimate partner violence screening within past 12 moc | 10 (13) | 1 (13) | 9 (13) | .99 |
| Incarceration within past 12 moc | 2 (3) | 0 (0) | 2 (3) | .99 |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: EHI, Economic Hardship Index; GA, gestational age; HIV, human immunodeficiency virus; IQR, interquartile range; STI, sexually transmitted infection.
Late prenatal care was defined as having the first prenatal healthcare visit in the second trimester or later. Scant prenatal care was determined by the patient’s provider as was documented in the patient’s medical record.
A high EHI was defined as being in the top fourth or fifth quintiles of all Chicago Community Areas [18].
Recent risk factor, defined as occurring within approximately 12 months of when pregnancy began.
Syphilis History and Treatment
Fifty-seven (75%) women had a history of a prior syphilis diagnosis and 52 (68%) were serofast on initial testing (Table 2). Twenty-six (34%) women were not serofast (ie, treatment was indicated). Three (4%) had evidence of reinfection during pregnancy, of whom 2 were initially serofast. A total of 32 (42%) were treated for syphilis during pregnancy, including 23 (88%) of the 26 women who were not serofast. Of all the women treated during pregnancy, 19 (42%) completed treatment at least 4 weeks prior to delivery, and median GA at syphilis treatment initiation was 26.9 weeks (IQR, 13.6–35.9 weeks). Among the 23 nonserofast women treated during pregnancy, 18 (78%) completed treatment at least 4 weeks prior to delivery and median GA at treatment initiation was 21.6 weeks (IQR, 10.89–27.93 weeks).
Table 2.
Syphilis Diagnosis and Treatment Among All Pregnant Women Diagnosed With Syphilis and Nonserofast Pregnant Women for Whom Treatment Was Indicated
| Characteristic | Total | Highly Probable or Possible Congenital Syphilis | Less Likely or Unlikely Congenital Syphilis | P Value |
|---|---|---|---|---|
| Full cohort | N = 76 | n = 8 | n = 68 | |
| Prior syphilis diagnosis | 57/76 (75) | 3/8 (38) | 54/68 (79) | .02 |
| Initial test results serofasta | 52/76 (68) | 2/8 (25) | 50/68 (74) | .01 |
| Evidence of reinfection during pregnancyb | 3/76 (4) | 1/8 (13) | 2/68 (3) | .29 |
| Treated for syphilis at any point during pregnancy | 32/76 (42) | 6/8 (75) | 26/68 (38) | .06 |
| Completed treatment ≥ 4 wk before delivery | 19/32 (59) | 0/6 (0) | 19/26 (73) | .002 |
| Median GA at syphilis treatment initiation, wk (IQR)c | 26.86 (13.57–35.93) | 29.86 (19.89–37.57) | 26.14 (12.71–34.89) | .32 |
| Median time from positive syphilis test to treatment initiation, wk (IQR)c | 1.86 (1.25–4.14) | 2.71 (1.00–6.89) | 1.86 (1.32–3.86) | .91 |
| Nonserofast women | n = 26 (34%) | n = 6 (75%) | n = 20 (29%) | |
| Initial test results serofast with later evidence of reinfectionc | 2/26 (8) | 0/6 (0) | 2/20 (10) | .99 |
| Treated for syphilis at any point during pregnancy | 23/26 (88) | 5/6 (83) | 18/20 (90) | .99 |
| Completed treatment ≥4 wk before delivery | 18/23 (78) | 0/5 (0) | 18/18 (100) | <.001 |
| Median GA at syphilis treatment initiation, wk (IQR) | 21.64 (10.89–27.93) | 27.29 (17.43–32.43) | 16.07 (9.79–26.29) | .13 |
| Median time from positive syphilis test to treatment initiation, wk (IQR) | 2.14 (1.57–4.57) | 3.57 (1.86–8.00) | 2.00 (1.46–3.86) | .50 |
Data are presented as no./No. (%) unless otherwise indicated.
Abbreviations: GA, gestational age; IQR, interquartile range.
Serofast is defined as having serologic test results (ie, rapid plasma reagin [RPR]) that are indicative of a previously treated syphilis infection with low, stable titers of 1:4 or less, 1 year or more after treatment.
Evidence of new infection during pregnancy was defined as a ≥4-fold increase in RPR titer after completing treatment for an initial infection. The 2 cases without congenital syphilis were initially serofast and later found to have reinfection; they were successfully treated for their reinfections >4 weeks from delivery with normal infant evaluations. The 1 case with congenital syphilis was initially diagnosed and treated with decreasing titers earlier in pregnancy (ie, not initially negative or serofast), then diagnosed with a reinfection at delivery).
Four women diagnosed at delivery excluded.
Congenital Syphilis Diagnoses
A total of 8 (11%) infants were diagnosed with highly probable or possible congenital syphilis. Descriptions of each case are displayed in Table 3, which includes diagnostic information, maternal treatment, prenatal care history, infant outcome, and maternal psychiatric and substance use histories.
Table 3.
Descriptions of Congenital Syphilis Cases
| Case | Diagnosis | Maternal Syphilis Labs and History | Maternal Syphilis Treatment | Late or Scant Prenatal Care | Infant GA | Infant Syphilis Labs | Infant Symptoms and Additional Evaluation | Maternal Psychiatric History | Maternal Substance Use |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Highly probable congenital syphilis | - EIA reactive, RPR 1:16; tested at 20 wk + 2 d GA - EIA reactive, RPR 1:16; tested at 34 wk + 6 d GA - RPR reactive; tested at delivery - Two prior treated syphilis infections, most recent infection was <1 y from first prenatal test |
Not treated because patient completed syphilis treatment within the past year with decreasing RPR titers | Scant and late prenatal care, first visit at 20 wk + 2 d GA | Late preterm, 35 wk + 2 d GA | RPR ≤4-fold maternal titer, treponemal test not obtained | - Long bone radiographs abnormal with metaphyseal lucent bands - Normal physical exam, CBC, CSF analysis |
Adjustment disorder | Marijuana |
| 2 | Highly probable congenital syphilis | - RPR 1:2, treponemal test not obtained; tested at 12 wk + 5 d GA - EIA reactive; RPR 1:2; tested at 28 wk + 2 d GA - Prior treated syphilis infection >1 y from first prenatal test - Serofast |
Not treated | Adequate, first visit at 6 wk + 2 d GA | Term, 38 wk + 0 d GA | Treponemal test reactive, RPR ≤4-fold maternal titer |
- Thrombocytopenia and leukopenia
- Hypoglycemia - CSF abnormal with pleocytosis (>25 WBCs/mL) and elevated protein (>150 mg/dL); VDRL NR - Normal physical exam, LFTs |
None | None |
| 3 | Highly probable congenital syphilis | - Diagnosed at outside clinic at 14 wk + 1 d GA (unknown test type or titer) - EIA reactive, RPR 1:16; tested at delivery - No prior syphilis diagnosis or treatment |
Inadequately treated; received 2 of 3 doses with second dose <4 weeks before delivery | Late prenatal care, first visit at 14 wk + 1 d GA | Term, 39 wk + 5 d GA | RPR ≤4-fold maternal titer, treponemal test not obtained |
- Leukopenia
- CSF abnormal with pleocytosis (>25 WBCs/mL); VDRL NR - Normal physical exam |
None | None |
| 4 | Highly probable congenital syphilis | - Diagnosed initially at outside hospital, but date unknown and results not confirmed - EIA reactive, RPR 1:32; tested at 31 wk + 5 d GA - RPR 1:16; tested at delivery - No prior syphilis diagnosis or treatment |
Completed treatment (3 penicillin doses) > 4 wk before delivery | Scant and late prenatal care, first visit at 15 wk + 2 d GA | Term, 38 wk + 4 d GA | Treponemal test reactive, RPR ≤4-fold maternal titer | - CSF abnormal with pleocytosis (>25 WBCs/mL), elevated protein (>150 mg/dL); VDRL NR - Normal physical exam, CBC, long bone radiographs |
Bipolar I disorder with active SI and psychiatric hospitalization during pregnancy | Marijuana |
| 5 | Possible congenital syphilis | - EIA reactive, RPR NR; tested at 31 wk + 2 d GA - EIA positive, RPR NR; tested at delivery - No prior syphilis diagnosis or treatment |
Received treatment at delivery (<4 wk before delivery) | Late prenatal care, first visit at 15 wk + 1 d GA | Term, 39 wk + 4 d GA | Treponemal test reactive, RPR not obtained | Normal physical exam, long bone radiographs, CBC | None | None |
| 6 | Possible congenital syphilis | - RPR NR, treponemal test not obtained; tested at 17 wk + 1 d GA - EIA reactive, RPR NR (tested at delivery) - Test results consistent with serofast serology, but prior syphilis infection only partially treated (1 of 3 penicillin doses received) |
Received treatment at delivery (<4 wk before delivery) | Late prenatal care, first visit at 19 wk + 1 d GA | Term, 39 wk + 5 d GA | Treponemal test reactive, RPR ≤4-fold maternal titer | Normal physical exam, long bone radiographs, CBC. CSF obtained, but inadequate sample for testing | None | Marijuana |
| 7 | Possible congenital syphilis | - EIA reactive, RPR NR; tested at 6 wk + 6 d GA - EIA reactive, RPR NR; tested at 22 wk + 2 d - No prior syphilis diagnosis or treatment |
Inadequately treated; received 2 of 3 penicillin doses | Adequate, first visit at 4 wk + 6 d GA | Preterm, 33 wk + 1 d GA | Treponemal test reactive, RPR ≤4-fold maternal titer | Normal physical exam, long bone radiographs, CBC, LFT, CSF analysis | Bipolar II disorder, major depressive episode with SI | Methamphetamine (ecstasy), marijuana, alcohol use during pregnancy |
| 8 | Possible congenital syphilis | - EIA reactive, RPR 1:32; tested at 15 wk + 4 d GA - RPR 1:4; tested at 32 wk + 3 d GA - EIA reactive, RPR 1:16; tested at delivery (4-fold increase in RPR titer indicating reinfection) - No prior syphilis diagnosis or treatment |
Completed treatment for initial diagnosis (3 penicillin doses) >4 wk before delivery. Not treated for reinfection diagnosed at delivery | Late prenatal care, first visit at 15 wk + 4 d GA | Term, 41 wk + 0 d GA | Treponemal test reactive, RPR ≤4-fold maternal titer | Normal physical exam, CBC, CSF analysis. CSF VDRL unable to be performed in lab | None | None |
Bolded terms indicate key information that determined how cases were determined when the 2018 American Academy of Pediatrics Red Book Diagnostic Algorithm for Infants Born to Mothers with Reactive Syphilis Serologic Tests was applied. Significant associations for psychiatric and substance use history are also bolded.
Abbreviations: CBC, complete blood count; CSF, cerebrospinal fluid; EIA, enzyme immunoassay; GA, gestational age; LFT, liver function test; NR, nonreactive; RPR, rapid plasma reagin; SI, suicidal ideation; VDRL, Venereal Disease Research Laboratory (nontreponemal) test; WBCs, white blood cells.
The strengths of associations between maternal characteristics and congenital syphilis are shown in Table 4. History of psychiatric illness (odds ratio [OR], 5.23 [95% confidence interval {CI}, 1.02–26.72]) and any recent substance use (OR, 5.18 [95% CI, 1.12–23.90]) were each associated with a >5-fold increased odds of congenital syphilis. All women with substance use who delivered infants with congenital syphilis reported using marijuana; 1 also reported using ecstasy; and none reported IVDU. None of the women used marijuana for medical purposes, which is legal in Illinois. Maternal characteristics of HIV coinfection, sex with partners who are MSM or have IVDU, incarceration, foreign born, and having sex for drugs or money were not associated with congenital syphilis. A prior syphilis diagnosis was associated with a lower odds of congenital syphilis (OR, 0.10 [95% CI, .02–.50]).
Table 4.
Associations Between Maternal Characteristics and Congenital Syphilis
| Characteristic | Odds Ratio (95% CI) |
|---|---|
| Late or scant prenatal care | 2.37 (.45–12.59) |
| Black race | 0.80 (.09–7.52) |
| Hispanic or Latina ethnicity | 3.10 (.28–33.91) |
| Chicago residents who lived in Community Areas with high EHIs | 1.20 (.22–6.51) |
| Homelessness within past 12 mo | 3.44 (.57–20.97) |
| Prior syphilis diagnosis | 0.10 (.02–.50) |
| Psychiatric illness within past 12 mo | 5.23 (1.02–26.72) |
| Substance use within past 12 mo | 5.18 (1.12–23.90) |
| Recent STI other than syphilis or HIV within past 12 mo | 0.32 (.04–2.77) |
| Positive intimate partner violence screening within past 12 mo | 0.94 (.10–8.53) |
Abbreviations: CI, confidence interval; EHI, Economic Hardship Index; HIV, human immunodeficiency virus; STI, sexually transmitted infection.
Late or scant prenatal care was associated with a >2-fold increased odds of congenital syphilis (OR, 2.37 [95% CI, .45–12.59]). On average, prenatal care for those delivering infants with congenital syphilis began in the second trimester at 15.21 weeks GA, more than a month later in pregnancy and in a subsequent trimester than those without congenital syphilis (median, 10.43 weeks GA). Additionally, syphilis treatment was initiated an average of 11.22 weeks later for nonserofast women who delivered infants with congenital syphilis compared to nonserofast women who did not deliver an infant with congenital syphilis (median, 27.29 vs 16.07 weeks GA, P = .13). Treatment was also delayed an additional 1.57 weeks in those with congenital syphilis than those without after receiving a positive syphilis test (median, 2.00 vs 3.57 weeks, P = .50). Overall, 6 (75%) of the women who delivered infants with congenital syphilis did not receive adequate syphilis treatment.
DISCUSSION
In this retrospective cohort study, we found that treatment was initiated for nonserofast women almost 3 months later in pregnancy among women who delivered infants with congenital syphilis compared to those who did not, suggesting that delayed or limited healthcare access may substantially contribute to the incidence of congenital syphilis in Chicago. While receiving treatment later in pregnancy may be due to late prenatal care, time between diagnosis and treatment was also longer in women who delivered infants with congenital syphilis compared to the women who delivered infants without congenital syphilis. Specific reasons for delayed or lack of treatment were not consistently documented, but common barriers included difficulties contacting patients (ie, disconnected phone numbers), arranging transportation to clinics, and family planning (ie, unexpected pregnancies).
Women with syphilis in our study were likely to report various social determinants of health (SDOH), such as homelessness or having either Medicaid (public health insurance) or no health insurance. Similar associations between congenital syphilis and lack of access due to SDOH have been documented elsewhere [1, 19–22]. In New York City, 30.9% of mothers of infants with congenital syphilis between 2010 and 2016 did not receive prenatal care until 45 days or less from delivery, with 76.2% of these women citing obstacles to accessing care such as lack of healthcare coverage, substance use, recent arrival in the US, unstable housing, and mental health disorders [21]. Mothers also did not receive any prenatal care in more than a third of Indiana’s congenital syphilis cases between 2014 and 2016, with the majority of the women experiencing social vulnerabilities such as homelessness, substance use, and incarceration [19].
Notably, there were higher odds of having psychiatric illness among women who delivered infants with congenital syphilis compared to those who did not in our cohort. Psychiatric illness may complicate care in several ways that lead to delayed syphilis diagnosis and treatment. In some situations, it may act as a barrier to obtaining primary and prenatal care or, in cases of mania, lead to high-risk sexual activity such as anonymous or unprotected sex. Therefore, psychiatric illness may be a risk factor that both increases chances of syphilis infection and decreases access to treatment. For clinical implications, this association may help identify an emerging group of high-risk women for whom more social and material support may be required for timely prenatal syphilis screening and treatment. In states where prenatal screening is not universally mandated, providers could consider including mental illness to their risk stratification when evaluating whom to screen and rescreen more than others.
Although substance use was frequently reported among mothers of infants with congenital syphilis, all but 1 of the cases with substance use reported using marijuana only and none reported IVDU, which has been more often associated with syphilis [20, 21, 23]. Recreational marijuana use was illegal during all years included in this study but became legal in Illinois in 2020. Our findings could therefore be explained by marijuana use becoming less stigmatizing in the years leading up to legalization; additionally, the prevalence of self-reported past-month marijuana use across the US more than doubled (3.4% to 7.1%) among pregnant women during the years of this study [24, 25]. Although some studies have linked overall substance use to riskier sex behaviors and syphilis infection, the association between marijuana specifically and STIs or condom use is less clear [26–28]. Therefore, we theorize that the association between noninjection substance use and congenital syphilis in our cohort is more related to difficulty accessing care and comorbidity with psychiatric illness rather than risky sex behaviors.
Public health interventions can also curb congenital syphilis cases by connecting women to primary or prenatal care. More support could be provided for STI and pregnancy testing services in settings where high rates of psychiatric illness, substance use, and other healthcare barriers overlap among reproductive-aged women. Some examples of such settings may include addiction clinics, mental health centers, jails or prisons, and women’s domestic violence and homeless shelters. Although not commonly utilized in the US, syphilis point-of-care tests in higher-risk populations could also be a valuable strategy to decrease the amount of time between testing and treatment and help initiate treatment earlier in pregnancy [29, 30].
Interestingly, there was a lack of established risk factors in this cohort. Psychiatric illness and substance use outnumbered several historical risk factors for congenital syphilis, including IVDU, sex work, incarceration, HIV coinfection, and sex with others known to be MSM or inject drugs [1, 15, 16, 19–21, 23]. However, many of these risk factors may be less frequently asked about by providers during clinical encounters; in addition, many patients may be reluctant to endorse behavioral risk factors due to stigma or fear of repercussions such as losing custody of her children. In other cases, women may not be aware of a partner’s high-risk activities, such as sex with MSM.
There are several limitations to this study. First, the small number of syphilis and congenital syphilis cases makes identification of factors associated with congenital syphilis risk challenging. Larger studies to further investigate the associations with congenital syphilis, including maternal psychiatric illness and substance use, are needed. State or local health departments could consider adding mental health questions to syphilis case investigations to assess whether psychiatric illness is associated with maternal syphilis diagnoses over larger geographical areas.
Second, 28% of the women with syphilis were excluded from our analysis due to having unknown pregnancy or congenital syphilis outcomes. Documented reasons for loss to follow-up when available varied widely, including providers unable to contact patients, transfer of care or delivery at a different hospital, miscarriage, and abortion. Of the women excluded, 8 were known to have delivered at another hospital (with 1 fetal demise); however, no information about congenital syphilis was available.
Third, our study population was taken from a single medical center and may not be generalizable. However, Chicago has a high syphilis prevalence with universal mandated screening of all pregnant women, making it representative of other urban areas in the US with high syphilis burden and medically vulnerable communities.
Finally, the design of this study involved retrospective review of electronic medical records, and no standardized screening tools or questionnaires were used. As a result, all outcomes and other social factors may not have been captured in this study. In addition, providers were able to make patient care decisions at their discretion that did not necessarily align with evidence-based guidelines.
Importantly, our comprehensive cohort study covers a 4-year period and includes all maternal syphilis diagnoses at a large medical center. We conducted a thorough medical record review to assess as many sociodemographic, clinical, and behavioral risk factors as were available.
CONCLUSIONS
This study helps to characterize pregnant women with syphilis and risk of congenital syphilis in the US. Psychiatric illness and noninjection substance use may create barriers to care and increase risk of congenital syphilis, and pregnant women with these risk factors may benefit from additional resources and closer follow-up after a prenatal syphilis diagnosis to prevent congenital transmission. Public health interventions tailored to reach those at highest risk of syphilis transmission—including those with psychiatric illness, substance use, and other healthcare barriers—are key to reducing congenital syphilis burden.
Notes
Acknowledgments. We thank the infection control department at University of Illinois Health and Hospital System for assistance in obtaining the syphilis cases used in this study.
Financial support. This work was supported by the Infectious Diseases Society of America Foundation through the Grants for Emerging Researchers/Clinicians Mentorship Program, which provides grants to medical students to support longitudinal, mentored clinical learning and research projects in infectious diseases.
Potential conflicts of interest. All authors: No potential conflicts of interest.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
REFERENCES
- 1. Adhikari EH. Syphilis in pregnancy. Obstet Gynecol 2020; 135:1121–35. [DOI] [PubMed] [Google Scholar]
- 2. Bowen V, Su J, Torrone E, Kidd S, Weinstock H.. Increase in incidence of congenital syphilis—United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2015; 64:1241–5. [DOI] [PubMed] [Google Scholar]
- 3. Torrone EA, Miller WC.. Congenital and heterosexual syphilis: still part of the problem. Sex Transm Dis 2018; 45(9S Suppl 1):S20–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. US Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2018. Atlanta, GA: US Department of Health and Human Services; 2019. [Google Scholar]
- 5. Galvis AE, Arrieta A.. Congenital syphilis: a U.S. perspective. Children (Basel) 2020; 7:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cooper JM, Sanchez PJ.. Congenital syphilis. Semin Perinatol 2018; 42:176–84. [DOI] [PubMed] [Google Scholar]
- 7. Kimball A, Torrone E, Miele K, et al. Missed opportunities for prevention of congenital syphilis—United States, 2018. MMWR Morb Mortal Wkly Rep 2020; 69:661–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chicago Department of Public Health. HIV/STI Surveillance Report 2013. Chicago, IL: City of Chicago; 2013. [Google Scholar]
- 9. Chicago Department of Public Health. HIV/STI Surveillance Report 2016. Chicago, IL: City of Chicago; 2016. [Google Scholar]
- 10. Chicago Department of Public Health. HIV/STI Surveillance Report 2019. Chicago, IL: City of Chicago; 2019. [Google Scholar]
- 11. Tabidze I; Chicago Department of Public Health HIV/STI Bureau. Update on Congenital Syphilis Elimination Efforts [presentation slides]. Chicago, IL: National Coalition of STD Directors; 2017. [Google Scholar]
- 12. American Academy of Pediatrics (AAP) Committee on Fetus and Newborn/American College of Obstetricians and Gynecologists Committee on Obstetric Practice. Guidelines for Perinatal Care . 8th ed. Itasca, IL: AAP; 2017. [Google Scholar]
- 13. US Centers for Disease Control and Prevention. Sexually transmitted disease treatment guidelines 2015. MMWR Recomm Rep 2015; 64:34–49. [PMC free article] [PubMed] [Google Scholar]
- 14. Warren HP, Cramer R, Kidd S, Leichliter JS.. State requirements for prenatal syphilis screening in the United States, 2016. Matern Child Health J 2018; 22:1227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Curry SJ, Krist AH, et al. US Preventive Services Task Force. Screening for syphilis infection in pregnant women: US Preventive Services Task Force reaffirmation recommendation statement. JAMA 2018; 320:911–7. [DOI] [PubMed] [Google Scholar]
- 16. Trivedi S, Williams C, Torrone E, Kidd S.. National trends and reported risk factors among pregnant women with syphilis in the United States, 2012–2016. Obstet Gynecol 2019; 133:27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. American Academy of Pediatrics (AAP) Committee on Infectious Diseases. Red Book (2018): Report of the Committee on Infectious Diseases. 31st ed. Itasca, IL: AAP; 2018. [Google Scholar]
- 18. Wilson M, Tailor A, Linares A.. Chicago Community Area Economic Hardship Index (2017). Chicago, IL: Great Cities Institute, University of Illinois at Chicago; 2019. [Google Scholar]
- 19. DiOrio D, Kroeger K, Ross A.. Social vulnerability in congenital syphilis case mothers: qualitative assessment of cases in Indiana, 2014 to 2016. Sex Transm Dis 2018; 45:447–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Peterman TA, Cha S.. Context-appropriate interventions to prevent syphilis: a narrative review. Sex Transm Dis 2018; 45(9S Suppl 1):S65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Slutsker JS, Hennessy RR, Schillinger JA.. Factors contributing to congenital syphilis cases—New York City, 2010–2016. MMWR Morb Mortal Wkly Rep 2018; 67:1088–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whitham M, Bandy S, Eppes C, Rac M.. Maternal characteristics of congenital syphilis. Obstet Gynecol 2018; 131:101S. [Google Scholar]
- 23. Schmidt R, Carson PJ, Jansen RJ.. Resurgence of syphilis in the United States: an assessment of contributing factors. Infect Dis 2019; 12:1178633719883282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ewing AC, Schauer GL, Grant-Lenzy AM, Njai R, Coy KC, Ko JY.. Current marijuana use among women of reproductive age. Drug Alcohol Depend 2020; 214:108161. [DOI] [PubMed] [Google Scholar]
- 25. Substance Abuse and Mental Health Services Administration (SAMHSA). 2018 National Survey of Drug Use and Health: Women [presentation slides]. Rockville, MD: SAMHSA; 2019. [Google Scholar]
- 26. Gorbach PM, Javanbakht M, Shover CL, et al. Associations between cannabis use, sexual behavior, and sexually transmitted infections/human immunodeficiency virus in a cohort of young men who have sex with men. Sex Transm Dis 2019; 46:105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Patel EU, White JL, Gaydos CA, et al. Marijuana use, sexual behaviors, and prevalent sexually transmitted infections among sexually experienced males and females in the United States: findings from the National Health and Nutrition Examination Surveys. Sex Transm Dis 2020; 47:672–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tucker JS, Shih RA, Pedersen ER, et al. Associations of alcohol and marijuana use with condom use among young adults: the moderating role of partner type. J Sex Res 2019; 56:957–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Adamson PC, Loeffelholz MJ, Klausner JD.. Point-of-care testing for sexually transmitted infections: a review of recent developments. Arch Pathol Lab Med 2020; 144:1344–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sanchez L, Harris T, Duford A, Duran N.. Recognizing and limiting syphilis to prevent congenital syphilis. JAAPA 2020; 33:44–7. [DOI] [PubMed] [Google Scholar]