Posttraumatic stress disorder (PTSD) is one of the most common mental illnesses experienced by US military veterans, with prevalence estimates among previously deployed veterans ranging from 12-23% (Dursa et al., 2014; Fulton et al., 2015; Marmar et al., 2015). The U.S. Department of Veterans Affairs (VA) is tasked with providing mental health services to men and women veterans who develop PTSD as a result of their military service. In fiscal year (FY) 2017, approximately 11% (n=650,000) of the nearly six million veterans enrolled in VA health care carried a diagnosis of PTSD (Harpaz-Rotem & Hoff, 2018). Among those veterans in VA with PTSD diagnoses in FY 2017, nearly 608,000 (93%) received some mental health services (Harpaz-Rotem & Hoff, 2018).
Numerous studies have observed that prevalence rates of PTSD among veterans who are of minority race or ethnicity are significantly higher than that of non-Latinx White (NLW) veterans (Dohrenwend et al., 2008; Dursa et al., 2014; Koo et al., 2015, 2016; Smith et al., 2016; Trivedi et al., 2015). Racial and ethnic minority veterans who suffer from PTSD are also more likely to experience a severe course of illness than NLW veterans (Kaczkurkin et al., 2016; Sripada et al., 2017). Although these disparities in PTSD prevalence and severity are likely multidetermined, factors resulting from direct and indirect effects of military service are partially contributory (Dohrenwend, Turner, Turse, Lewis-Fernandez, & Yager, 2008b; Foynes, Smith, & Shipherd, 2015; Loo, Singh, Scurfield, & Kilauano, 1998; Loo, Lim, Koff, Morton, & Kiang, 2007; Muralidharan, Austern, Hack, & Vogt, 2016).
This greater illness burden born by some racial and ethnic minority groups of veterans may be compounded by difficulties within the health care system. Minority veterans are more likely to experience barriers to accessing VA mental health services, to not feel welcome in VA facilities, and to have worse health care experiences for those services that are accessed (National Academies of Sciences, Engineering, and Medicine, 2018). Among racial and ethnic minority veterans with PTSD, several disparities in mental health services have been observed, including non-clinical variation in the types of mental health treatments received, the treatment settings in which mental health services were delivered, and the likelihood of receiving a minimally adequate trial of treatment (Hebenstreit, Madden, Koo, & Maguen, 2015; Koo et al., 2015; Rosen et al., 2019; Spoont et al., 2015; Spoont, Sayer, Kehle-Forbes, Meis, & Nelson, 2017). For example, Latinx veterans with PTSD are less likely than NLWs to receive any psychotherapy or, if they do, are less likely to receive individual psychotherapy (vs. group therapy), and less likely to receive a guideline recommended evidence-based psychotherapy (Rosen et al., 2019; Spoont et al., 2017; The Management of Posttraumatic Stress Disorder Work Group, 2017). African American veterans who receive psychotherapy are also less likely than NLWs to receive individual rather than group therapy, are more likely to prematurely discontinue pharmacotherapy, less likely to receive a minimally adequate trial of mental health treatment, and more likely to require emergency/urgent care services (Hebenstreit et al., 2015; Koo et al., 2015; Spoont et al., 2015; Spoont et al., 2017).
Determining if these observed inequities in mental health treatment exacerbate pre-treatment differences in PTSD severity and prevalence (i.e., cause an even greater disparity in mental illness burden) is critical if we are to improve the health and well-being of racial and ethnic minority veterans with PTSD. To evaluate whether disparities exist in clinical outcomes across racial and ethnic groups of veterans seen in VA, we conducted a planned secondary analysis of patient-reported outcomes from a prospective cohort study of veterans with PTSD. We evaluated two sets of outcomes. First, we examined symptom change and functioning/quality of life outcomes among those veterans with PTSD who initiated any treatment. If treatments and services provided met the clinical needs of all veterans equally, then we would expect that rates of significant benefit (controlling for baseline illness severity) would be comparable across racial/ethnic groups. That is, if all groups of veterans showed relatively similar improvements, then variations in services likely correspond to differences in patient needs (i.e., they are equitable)(Smedley et al., 2003). However, if treatments and services provided addressed the clinical needs of NLW veterans more often than those of racial or ethnic minority veterans (i.e., services received were not equitable), then we would expect relatively greater rates of improvement among NLW veterans. Such preferential improvement among NLW veterans would further exacerbate pre-treatment disparities.
Because factors contributing to racial and ethnic disparities in mental health treatment may occur at any point along the continuum of care -- from referrals to assessments and treatment planning to treatment engagement, and so on (Alegría et al., 2016; Kugelmass, 2016; Marx et al., 2017; Merino et al., 2018; Penner et al., 2013) -- we also examined clinical outcomes for the whole system of care beginning at the point of case identification until the end of the sampling period six-months later independent of whether veterans initiated any treatment. If racial and ethnic minority veterans were more or less likely to receive treatment (for any reason), then this second analysis would allow us to evaluate variations in outcomes due to differences in treatment access or availability.
METHODS:
Study overview:
This is a planned secondary analysis of variations in outcomes across racial and ethnic groups using an observational prospective cohort study of veterans who had been diagnosed with PTSD (n=7,645). Sampled were veterans who were diagnosed with PTSD by a primary care or mental health provider in any VA facility during the recruitment period. To evaluate health care outcomes, we wanted to specifically identify those veterans with PTSD who might begin a new episode of mental health care for PTSD (due to new diagnosis or recurrence) or an exacerbation of PTSD. Therefore, we excluded from the surveyed population those who had been diagnosed with any mental health disorder, had any mental health related appointments (except for substance use disorders or SUD; (Kimerling et al., 2006), or who had received either antidepressants or antipsychotics in the prior year. We did not exclude SUD diagnoses since PTSD may be more difficult to identify in that clinical context. Eligible patients were identified by abstraction of demographic, diagnostic, and VA health care utilization data from the National Patient Care Database (NPCD) and outpatient prescriptions from the Decision Support System (DSS) National Pharmacy Extract database. Data on outpatient encounters are uploaded daily to the NPCD from all VA facilities and made accessible every two weeks; we identified veterans within 1 to 14 days of the appointment in which PTSD was diagnosed. Veterans were sent a baseline questionnaire soon after they received a PTSD diagnosis and a second, follow-up survey 6 months post-diagnosis. Data were collected between 6/2008 and 3/2010. The study was approved by the local VA Institutional Review Board.
Sample:
Methods for sample ascertainment and collection of the survey dataset are described in detail elsewhere (Spoont, 2015; Spoont, Sayer et al., 2017). Briefly, a weighted stratified random sample was drawn from all veterans diagnosed with PTSD (International Classification of Disease 9 or ICD9 code 309.81) during an outpatient visit at any VA facility nationwide. Given high rates of mental health comorbidity and chronicity of PTSD among veterans (Marmar et al., 2015; Pietrzak et al., 2011; Santiago et al., 2013), patients were not excluded if they had prior mental health diagnoses (including PTSD) before the year prior to the index appointment in which PTSD was diagnosed. In other words, a history of mental health problems or treatments was not an exclusion; however, treatment in the year immediately prior to the index PTSD diagnostic appointment was. This balanced our need to follow Veterans prospectively once PTSD was identified as a current problem (operationalized as the diagnosis of record for a given appointment) and still retain ecological validity. Sampling was stratified by race, ethnicity and gender; specific proportions were determined from previous work, with women and racial and ethnic minorities oversampled to allow for group comparisons (Spoont, 2015; Spoont, Sayer et al., 2017). Self-reported racial or ethnic identities that were relatively uncommon among survey respondents (i.e., n <70) and veterans diagnosed with PTSD in clinics other than a mental health or primary care clinic were excluded from the analyses because such small groups would limit our statistical power to detect effects. We also excluded veterans who had moderate to severe cognitive impairments, schizophrenic spectrum disorders, who died during the study sampling period, or who had no available mailing address. Lastly, because our focus was patient-reported outcomes, we restricted our dataset to those subjects who responded to both the post-diagnostic baseline and the 6-month follow-up surveys (n=5,070; see Figure 1).
Figure 1.
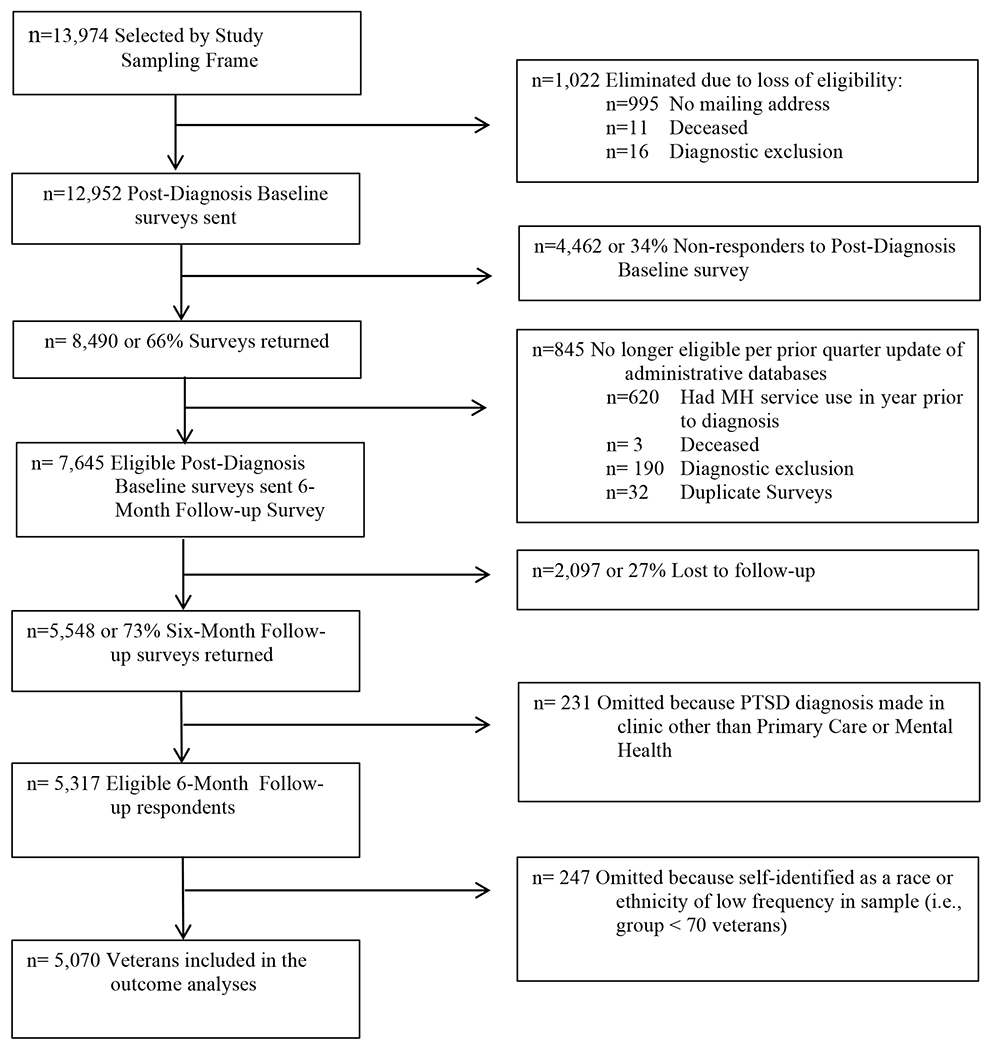
Sampling and Response Diagram.
MH=mental health
Survey procedure:
For both the baseline and 6-month follow-up surveys, we used Dillman’s approach to multiple mailings (Dillman, 1991). First, an introductory letter was mailed, followed 2 days later by a packet containing an informed consent letter, a survey, $10 cash payment, and a postage-paid return envelope. Ten days later, non-respondents were sent a 2nd letter/survey/envelope packet. Non-respondents to the 2nd packet were sent a 3rd packet 10 days later via Federal Express. The $10 incentive was included only with the first mailing. Follow-up surveys and a new $10 incentive were sent 6 months after the PTSD diagnostic appointment only to respondents of the baseline survey. The same mailing procedures were followed as for the baseline survey except that no additional introductory letter was sent.
Model Predictors and Data Sources:
Predictors of treatment outcomes in the analytic models included demographic information (age, race/ethnicity, gender) and treatment need (baseline measures of PTSD symptom severity and measures of physical and mental health quality of life). Administrative indicators of race/ethnicity, age, and gender were abstracted from VA NCPD and DSS databases. PTSD symptom severity, physical and mental health quality of life were assessed on both the baseline and 6-month follow-up surveys. Administrative race and ethnicity were used for sampling stratification; however, only self-reported race and ethnicity assessed on the baseline survey was used in analytic models.
Treatment Need:
We defined Treatment need as the baseline survey assessments of symptom severity and health-related quality of life measures. PTSD symptom severity, physical and mental health quality of life were measured in both the baseline and 6-month follow-up surveys. PTSD symptom severity was assessed by the PTSD Checklist-Military version, for which scores can range from 17 to 85 with higher scores indicating greater symptom severity (PCL-M; sample α=0.94) (Blanchard et al., 1996; McDonald & Calhoun, 2010; Weathers, 1993). In the baseline survey, veterans were asked to indicate their trauma for which they filled out the PCL-M symptom measure (combat, unwanted sexual experiences, physical attack, natural disaster, serious accident, unexpected or violent death, “other” with write-in option). Health related quality of life was assessed by the Mental Health Quality of Life score (MHQoL) and the Physical Health Quality of Life score (PHQoL) of the veterans Rand 12-item Health Survey (VR-12) (Goldberg et al., 2014; Jones et al., 2001). Scores for PHQoL and MHQoL range from 0 to 100, and are standardized to the general veteran population with a mean of 50; higher scores indicate better quality of life (sample α=0.88 PHQoL, α=0.86 MHQoL) (Jones et al., 2001; Kazis et al., 2006).
Race and ethnicity:
As in previous work (Spoont, 2015; Spoont, Sayer et al., 2017) race/ethnicity was assessed by survey checklist allowing for multiple endorsements: White, African American, Native American/Native Alaskan, Asian American, Hispanic or Latinx, Native Hawaiian, and Pacific Islander. Most veterans identified only a single race or ethnicity, but a significant portion of Latinx and Native American Veterans also endorsed White. We included these veterans in the Latinx and Native American groups respectively. Although we acknowledge that differences exist among Hawaiians, Pacific Islanders, and Asian Americans, given their small individual sample sizes we chose to combine these veterans into a single group rather than omit them from the analyses. This left us with five racial/ethnic groups for our analyses: NLW, Latinx, African American, Native American, and Asian/Hawaiian/Pacific Islander (A/H/PI).
Treatment initiation:
To address our first research question as to whether there are differences in outcomes among those who initiated treatment, we defined treatment initiation as completion of at least one therapy appointment or receipt of one prescription. Specifically, treatment initiation included completion of any individual or group psychotherapy appointments with a mental health clinician, or receipt of any medication prescription in one of the two drug classes recommended by VA/DoD clinical practice guidelines for PTSD [i.e. selective serotonin reuptake inhibitors (SSRI) and serotonin-norepinephrine reuptake inhibitors (SNRI)] (The Management of Posttraumatic Stress Disorder Work Group, 2017) during the 6-month follow-up period. Psychotherapy appointments were identified using Current Procedural Terminology (CPT) codes and provider identifiers in VA databases uploaded from providers’ encounter forms. Appointment and pharmacy information were from abstracted NCPD and DSS databases respectively. Veterans were considered treatment initiators if they completed at least one psychotherapy appointment or received one prescription during the 6-month follow-up period.
Study Outcomes:
Change scores in PCL-M and MHQoL from baseline to the 6-month follow-up surveys served as study outcomes. For both the PCL-M and MHQoL measures, we determined medium effect sizes corresponding to 50% of the baseline sample distribution standard deviations. A medium effect size, or .5 SD units, corresponds to what is considered the Minimally Important Difference (MID) in multiple areas of medicine, including PTSD treatment outcomes (Le et al., 2013; Schnurr & Lunney, 2016; Shiner et al., 2011; Stefanovics et al., 2018). Improvements in scores by .50 SD or larger are considered reliable improvements and worsening of scores by .50 SD or more are considered reliable declines. In our sample, .50 SD units equaled 7.49 points on the PCL-M. We therefore used this medium effect size threshold to define a three-level ordinal outcome measure of change in PCL-M: improvement by at least 7.49 points, no significant change, or worsening by at least 7.49 points. Similarly, we constructed a three-level ordinal outcome measure for change in MHQOL: improvement by at least 5.85 points, no significant change, or worsening by at least 5.85 points. We used these MID criteria to determine what proportion of veterans evidenced reliable improvement or worsening or no change in PTSD symptom severity (PCL-M) and/or MHQoL (Norman et al., 2003; Schnurr & Lunney, 2016; Shiner et al., 2011; Stefanovics et al., 2018).
ANALYSES:
We implemented a series of descriptive and multinomial logistic regression analyses using the following structure:
Outcomes:
3 categories each (improved, no change, worsened); Categories represented change scores in PCL-M or MHQoL from Baseline to 6-month follow-up. For each outcome, we examined medium effect changes of .5 SD units and large effect changes of .7 SD units to define improvement or worsening.
Treatment need and demographic covariates:
Baseline PCL-M, VR-12 MHQoL and PHQoL; age, and gender
Independent variable:
race/ethnicity (NLW, Latinx, African American, Native American, Asian/Hawaiian/Pacific Islander)
Analyses occurred in several steps. First, we descriptively examined differences across racial and ethnic groups in baseline and follow-up PTSD symptoms and MHQoL and change in these measures. Bonferroni corrections were used for group comparisons to assess significance of results. We then fit multinomial logistic regression models using race/ethnicity and the demographic and treatment need covariates as fixed effects to estimate adjusted rates of improvement, worsening or no significant change for both outcome measures.
To determine if outcome rates differed for minority racial and ethnic groups relative to NLWs, we compared adjusted odds ratios for improvement vs. no change and for worsening vs. no change between each minority racial/ethnic group and NLWs among those veterans who initiated any treatment in the six-month follow-up period (n=2,992) using Wald tests. Then, to determine if our estimates were affected by treatment receipt, we re-ran all models using a non-restricted sample that included all Veterans that met our inclusion criteria (i.e., both treatment initiators and non-initiators) (n=5,070).
Sensitivity Analyses:
We conducted two sensitivity analyses to examine the robustness of our findings. First, although our definition of MID in PTSD symptoms (i.e., PCL-M score differences) is an accepted indicator of reliable change (Le et al., 2013; Norman et al., 2003; Stefanovics et al., 2018), it falls mid-range in estimates of what has been assumed to be “reliable change” used in treatment trials (e.g., see Stefanovics, Rosenheck, Jones, Huang, & Krystal, 2018), and below the commonly used PCL-M change metric of 10-points (NCPTSD, 2012). To determine if the pattern of our findings would still be present if we used a more stringent change criterion, we constructed new PCL-M and MHQoL outcome measures using a large effect size threshold (i.e., change of at least .7 SD units/10.58 points on PCL-M) to define significant worsening or improvement, and then re-ran our models in both the treatment initiator and in the full unrestricted samples. The large effect threshold for the MHQoL score was 8.19 points.
To evaluate potential biases introduced by stratified sampling, incomplete responses to survey items, and variable rates of survey nonresponse, for our second set of sensitivity analyses we used sampling weights, multiple imputation, and survey response propensity score adjustments and re-ran our analytic models. Markov Chain Monte Carlo multiple imputation was used to address potential bias due to missing PTSD symptom, MHQoL or PHQoL survey items. Ten different imputed values were constructed for each missing item, creating ten complete imputed data sets. Age, gender, race and ethnicity were not imputed.
To address potential survey nonresponse bias, a propensity model was developed for responses to baseline and follow-up surveys using all available administrative data as predictors. The sample was then stratified by both the original survey sampling strata and the estimated survey response propensity vector. Within each stratum, the original sample design weights for those subjects responding to both surveys were adjusted by multiplying the weights by the ratio of the number of stratum members to the number of stratum respondents. Observations weighted by these adjusted survey inclusion probabilities were then used in analyses of the outcome measures. These weighted analyses were implemented for each of the imputed datasets and results were aggregated using standard methods for multiple imputation.
Using this approach, we estimated population-based rates of improvement, worsening or no significant change for both outcome measures. We used weighted multinomial logistic regression models to estimate demographic and treatment need adjusted population-based differences in these rates across racial and ethnic groups. As in the observed data models, we then examined the model estimated odds ratios comparing the differences of improvement vs. no change and worsening vs. no change between each racial and ethnic minority group relative to NHWs for both outcomes. Standard errors and confidence intervals for model estimates were constructed using bootstrapping methods.
In these population based weighted models, some propensity strata included very few veterans from some racial/ethnic subpopulations. These sparse strata greatly increased the estimated standard errors, thereby limiting our statistical power to for subgroup comparisons. Consequently, results from these adjusted analyses were used to identify potential response biases and to confirm/refute findings by comparing the direction and magnitude of the point estimates with those derived from the observed data analyses. Of note, the overall population change estimates were not impacted by the statistical limitations in the subpopulation comparisons and so we present them alongside the overall observed rates of change.
Post hoc analyses:
To better understand seemingly inconsistent and ambiguous aspects of our results, we conducted additional 3-way contingency table analyses to explore relationships between veteran race and ethnicity and the associations: a) between outcome measures, and b) between outcomes and treatment initiation.
RESULTS
Of the n=5,070 veterans in the sample who responded to both surveys (Figure 1), n=4,338 (86%) were men, n=732 (14%) were women, and fifty-nine percent (n=2,992) had initiated some mental health treatment in the 6-month follow-up period. Mean baseline treatment need variables were in the clinically significant range in PTSD symptomatology and mental and physical health-related functional impairments. PTSD severity was slightly higher and MHQoL slightly lower among those who initiated some treatment (Table 1). All racial and ethnic minority veterans except those who were A/H/PI had significantly more severe PTSD symptomatology than NLW veterans at both the baseline assessment (F=27.98, df=4, 5,019, p<0.001) and at the 6-month follow-up (F=27.08, df=4, 4,770, p<0.001). Bonferroni-corrected post hoc tests for all comparisons except those that included A/H/PI veterans were significant (all p<0.001). Similarly, NLW’s had better MHQoL than African American and Latinx veterans at baseline (F=6.98, df=4, 5,045, p<0.001; ) and at 6-month follow-up (F=6.19, df=4, 5,042, p<0.001). Bonferroni-corrected post hoc tests for those comparisons p<0.001.
Table 1.
Sample Characteristics
| Treatment Initiators a | Total Sample | |
|---|---|---|
| Characteristics | n (%) b | n (%) |
|
| ||
| Men | 2,500 (84) | 4,338 (86) |
| Women | 492 (17) | 732 (14) |
| Race/Ethnicity | ||
| Latinx/Hispanic | 617 (21) | 1,003 (20) |
| Native American | 269 (9) | 496 (10) |
| African American | 645 (22) | 1,010 (20) |
| Asian/Hawaiian/Pacific Islander | 141 (5) | 254 (5) |
| Non-Latinx White | 1,320 (44) | 2,307 (46) |
| Treatment Initiators | 2,992 (59) | |
| No Treatment Initiation | 2,078 (41) | |
| M (SD) | M (SD) | |
|
|
||
| Age | 51.7 (15.2) | 53.9 (15.3) |
| PTSD Checklist (PCL-M) c | 60.3 (13.4) | 57.4 (15.0) |
| VR-12 MHQoL | 31.4 (11.0) | 33.7 (11.8) |
| VR-12 PHQoL | 36.2 (11.1) | 36.0 (11.1) |
For demographic information and PHQoL, Total Sample =5,070 and Treatment Initiator sample=2,992. Because of missing items, values for MHQoL n=2,985; PCL n=2,967.
Percentiles for categorical variables are represented as whole numbers and may not add to 100 due to rounding.
PCL-M scores can range from 17 to 85, with higher scores indicating greater symptom severity. VR-12 MHQoL and VR-12 PHQoL scores can range from 0 to 100 with a mean of 50, with higher scores indicating better quality of life.
Rates of reliably significant change (MID criterion) in both the treatment and the total sample in the 6-month period after veterans received a PTSD diagnosis showed that a little more than 1 in 4 veterans evidenced significant improvement in PTSD symptoms and MHQoL (Table 2). Using a large effect criterion, rates in both samples reduced to about 1 in 5. Population adjusted rates were comparable to observed rates, suggesting that these results were not due to sampling or responses biases.
Table 2.
Observed and Adjusted Rates of Clinically Significant Change in Outcomes 6-months after Veterans were Diagnosed with PTSD
| Unadjusted Observed Sample Ratesb | Adjusted Population Rates c | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Improved | No Change | Worsened | Improved | No Change | Worsened | ||||
| Treatment Initiators | % | % | % | % | 95% CI | % | 95% CI | % | 95% CI |
|
|
|||||||||
| PCL Medium Effect Rates | 27.5 | 56.0 | 16.4 | 27.3 | [25.3, 28.9] | 59.3 | [57.3, 61.3] | 13.3 | [12.0, 14.8] |
| PCL Large Effect Rates | 19.1 | 70.8 | 10.0 | 18.2 | [16.4, 19.7] | 74.9 | [73.1, 76.6] | 6.9 | [5.8, 8.0] |
| MHQoL Medium Effect Rates | 29.8 | 46.7 | 23.5 | 26.4 | [24.4, 28.3] | 51.4 | [49.4, 53.3] | 22.2 | [20.3, 24.1] |
| MHQoL Large Effect Rates | 22.1 | 61.2 | 16.8 | 18.0 | [16.0,19.6] | 66.8 | [64.8, 68.9] | 15.1 | [13.4, 16.9] |
|
| |||||||||
| Total Sample | |||||||||
| PCL Medium Effect Rates a | 26.7 | 57.3 | 16.0 | 27.2 | [25.2, 28.8] | 58.9 | [56.9, 60.9] | 13.9 | [12.5, 15.4] |
| PCL Large Effect Rates | 18.0 | 72.4 | 9.6 | 18.1 | [16.3, 19.6] | 74.2 | [72.3, 76.0] | 7.7 | [6.4, 8.9] |
| MHQoL Medium Effect Rates | 28.6 | 46.8 | 24.7 | 26.4 | [24.5, 28.3] | 51.3 | [49.3, 53.3] | 22.2 | [20.4, 24.2] |
| MHQoL Large Effect Rates | 20.7 | 61.4 | 17.8 | 18.0 | [16.0,19.6] | 66.7 | [64.7, 68.7] | 15.3 | [13.5, 17.0] |
PCL: Medium Effect Size is 0.5 SD units or ± 7.49 points; Large Effect Size is 0.7 SD units or ± 10.58 points; MHQoL Medium Effect Size is 0.5 SD units or ± 5.85 points; Large Effect Size is 0.7 SD units or ± 8.19 points.
Because of missing items, Treatment Initiator Sample n=2,817 for PCL outcomes and n=2,978 for MHQoL outcomes; Total Sample n=4,739 for PCL outcomes and n=5,028 for MHQoL outcomes
Adjusted population rates were derived from models that included baseline PCL-M, VR-12 MHQoL, VR-12 PHQoL, gender, age, and race/ethnicity as covariates, used multiple imputation and propensity scores to address item and survey non-response respectively, and adjusted for stratified sampling via sampling weights. Treatment Initiators n=2,992; Total Sample n=5,070.
As observed by others (Maguen et al., 2014; Sripada et al., 2017), we found racial and ethnic disparities in clinical outcomes. Among treatment initiators, both Latinx and African American veterans were less likely than NLWs to evidence reliably significant improvement in PTSD symptoms (PCL scores; see Table 3). This disparity was also observed in the total sample for Latinx veterans; for African American veterans, the lower odds of improvement relative to NLWs were no longer significant, but the odds of significant worsening were.
Table 3.
Odds Ratios of Clinically Significant Improvement or Worsening vs. No Change Comparisons of Racial/Ethnic Minority Veteran Groups Relative to non-Latino Whites in PTSD Symptoms
| Treatment Initiators c | Total Sample | |||||||
|---|---|---|---|---|---|---|---|---|
| Improve | Worsen | Improve | Worsen | |||||
| PCL MID Change a | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|
|
|
|||||||
| Latinx | 0.66** | [0.52, 0.84] | 0.99 | [0.74, 1.34] | 0.77** | [0.64, 0.94] | 0.99 | [0.78, 1.25] |
| Native American | 0.91 | [0.65, 1.26] | 1.29 | [0.87, 1.91] | 1.01 | [0.79, 1.28] | 1.15 | [0.85, 1.54] |
| African American | 0.75* | [0.59, 0.94] | 1.22 | [0.92, 1.63] | 0.87 | [0.72, 1.05] | 1.28* | [1.02, 1.59] |
| Asian/Hawaiian/Pacific Islander | 0.92 | [0.61, 1.39] | 0.95 | [0.55, 1.66] | 1.04 | [0.76, 1.42] | 1.01 | [0.67, 1.51] |
| Non-Latinx White b | ||||||||
| Reference Group | ||||||||
MID (Minimally Important Difference) is a Medium effect size change in 0.5 SD units, or 7.49 points.
Non-Latino Whites are the reference group for comparisons of significant improvement or worsening vs. no significant change.
Models included age, gender, race/ethnicity and baseline PCL, MHQoL and PHQoL scores. Because of missing items, Total Sample n=4,739, Treatment initiator sample n=2,817.
p<0.05
p<0.01
In contrast to outcomes for PTSD symptoms, outcomes for MHQoL were better among Asian/Hawaiian/Pacific Islander and African American veterans relative to NLWs in the sample of treatment initiators (Table 4). In the total sample, the relatively greater rates of improvement among Asian/Hawaiian/Pacific Islander veterans disappeared but those of African American veterans remained; outcomes among Native American veterans were now significantly greater than those for NLWs.
Table 4.
Odds Ratios of Clinically Significant Improvement or Worsening vs. No Change Comparisons of Racial/Ethnic Minority Veteran Groups Relative to non-Latinx Whites in VR-12 MHQoL Scores
| Treatment Initiators c | Total Sample | |||||||
|---|---|---|---|---|---|---|---|---|
| Improve | Worsen | Improve | Worsen | |||||
| MHQoL MID Change a | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|
|
|
|||||||
| Latinx | 1.03 | [0.81, 1.30] | 1.11 | [0.85, 1.44] | 1.15 | [0.95, 1.39] | 1.04 | [0.85, 1.27] |
| Native American | 1.07 | [0.78, 1.48] | 1.01 | [0.77, 1.57] | 1.31* | [1.03, 1.67] | 1.04 | [0.80, 1.35] |
| African American | 1.27* | [1.01, 1.60] | 1.14 | [0.88, 1.46] | 1.24* | [1.03, 1.49] | 1.01 | [0.83, 1.22] |
| Asian/Hawaiian/Pacific Islander | 1.79** | [1.18, 2.72] | 1.33 | [0.83, 1.66] | 1.33 | [0.97, 1.83] | 1.04 | [0.74, 1.46] |
| Non-Latinx White b | ||||||||
| Reference Group | ||||||||
MID (Minimally Important Difference) is a Medium effect size change in 0.5 SD units.
Non-Latinx Whites are the reference group for comparisons of significant improvement or worsening vs. no significant change.
Models included age, gender, race/ethnicity and baseline PCL, MHQoL and PHQoL scores. Because of missing items, Total Sample n=5,028, Treatment Initiation Sample n=2,978 outcomes.
p<0.05
p<0.01
Sensitivity Analyses:
The differences observed in outcome rates across racial and ethnic subgroups of veterans with PTSD were similar to those observed in PCL and MHQoL scores when a large effect criterion was used (Online Table 1), suggesting that the findings were not due to the threshold used. Population adjusted outcome rates across racial and ethnic subgroups for both PCL and MHQoL outcomes (Online Table 2) were also comparable to those seen in the observed models. Both sensitivity analyses demonstrate that the observed group differences in the primary analyses are unlikely to be due to the stringency of our outcome criteria, sampling stratification, or response biases.
Post hoc analyses:
Although the simple correlation between baseline PCL and MHQoL scores was high (r= −0.70, n=5,014, p<0.001), the correlation between continuous outcome change scores in those measures was significant but more modest (r= −0.46, n=4,727, p<0.001). This suggests that the domains captured by these measures include both overlapping and unique aspects of recovery. Given that changes in PCL and MHQoL scores were moderately correlated, it was surprising that improvement rate differences for African American veterans relative to NLWs appeared to be in the opposite direction for the two outcomes (Tables 3 and 4). To better understand these discrepant findings, we examined associations between race/ethnicity and the two outcome measures using 3-way contingency tables. For those veterans’ whose PTSD symptoms worsened or were unchanged, MHQoL score distributions were similar for African Americans and NLWs. However, among veterans whose PTSD symptoms showed large effect size improvements, African Americans were more likely than NLWs to experience concomitant improvements in MHQoL (African Americans: 64% improvement in MHQoL vs. 28% unchanged; NLWs: 53% improved MHQoL vs. 38% unchanged; comparison of proportions, p<0.05). Rates among Native American veterans showed a similar pattern of correlated improvements (58% improved vs. 39% unchanged, p=ns), but the rate difference fell midway between the two other groups.
To determine if treatment initiation rate differences impacted our results, we used 3-way contingency tables to explore associations between outcome measures and treatment initiation rates across racial/ethnic groups. Treatment initiation (vs. non-initiation) was only associated with greater improvement rates in MHQoL among NLWs and Asian/Hawaiian/Pacific Islanders; the magnitude of this effect was significantly greater for A/H/PI veterans than for NLWs (A/H/PI veterans: 37% treatment initiators improved in MHQoL vs. 23% non-initiators, X2=7.42, df=2, p<0.05; NLWs: 29% treatment initiators improved vs. 24% non-initiators, X2=8.93, df=2, p<0.02). The relatively greater improvement rate among A/H/PI veterans relative to NLWs among treatment initiators is also reflected in the odds ratios for A/H/PI veterans in improvement vs. no change comparisons in Table 4. In contrast to change in MHQoL, treatment initiation was associated with improvement in PTSD symptoms only among NLW veterans (30% initiators improved vs. 23% non-initiators; X2=15.84, df=2, p<0.001). This mirrors the greater disparity observed in the Latinx and African American odds ratios in Table 3 in the treatment initiator sample relative to the odds ratios seen in the total sample.
DISCUSSION
Among veterans who had no mental health care in the prior year, six-months after being diagnosed with PTSD only 1 in 4 veterans experienced significant improvements in PTSD symptoms and MHQoL. These modest rates of improvement indicate that many veterans continued to suffer from PTSD and its sequalae well after the condition or an acute exacerbation had been identified. Reasons for this limited rate of improvement were not the focus of this paper, but insufficient treatment, treatment with non-efficacious interventions, or other provider or system factors might be contributory.
Controlling for initial treatment need (i.e., baseline PTSD symptom severity, MHQoL and PHQoL), we found that rates of PTSD symptom improvement or worsening (vs. no significant change) 6-months after receipt of a PTSD diagnosis varied depending on veteran race/ethnicity. Both Latinx and African American veterans were less likely than NLWs to show significant improvement, and African Americans were more likely than NLWs to show significant worsening. These findings are consistent with other national reports of relatively worse outcomes among Latinx and/or African American veterans with PTSD (Maguen et al., 2014; Sripada et al., 2017, 2019, 2020). Although these data do not allow us to determine reasons for these outcome disparities, they were observed in both the treatment initiation sample and the total sample (initiators and non-initiators). This suggests that differential access to treatment or differences in treatment initiation rates were not major drivers of racial/ethnic differential outcomes. However, because disparities in PTSD outcomes were greater in the sub-sample that had initiated treatment, engagement with the treatment system may actually widen pre-treatment disparities in PTSD severity observed for African American and Latinx veterans by selectively improving outcomes for NLWs. Our post hoc finding that NLWs were the only group to be more likely to improve in PTSD symptoms if they initiated treatment suggests that this may be the case.
Several studies have identified mental health treatment disparities for African American and Latinx veterans relative to NLWs. For example, African American and Latinx veterans with PTSD are more likely than NLWs to receive group rather than individual psychotherapy, and group therapy is less likely to be effective (Imel et al., 2013; Mott et al., 2014; Resick et al., 2017; Sloan et al., 2012). Latinx veterans are less likely to get psychotherapy or, if they do, are less likely to receive an evidence based psychotherapy (Rosen et al., 2018; Spoont et al., 2017). On the other hand, among veterans who initiate prolonged exposure therapy for PTSD, African Americans are more likely than NLWs to complete the treatment (Maguen et al., 2019). Although such treatment-related disparities may contribute to these findings, it is likely complex and non-treatment factors may also impact treatment outcomes. For example, African American and/or Latinx veterans are more likely to delay treatment initiation (Holder et al., 2019), to experience deployment-related social stressors (Muralidharan et al., 2016), to experience discrimination (Sibrava et al., 20190117), and to have low income (Chen et al., 2019) -- any of these factors may contribute to worse outcomes. Whether these or other variations in mental health treatment engagement, treatment delivery, or in non-health care system factors (e.g., social determinants of health such as income) (Duran & Pérez-Stable, 2019) underlie the disparities in the observed outcomes cannot be discerned from these data. Future studies will need to disaggregate the complex interactions between veteran level factors, social determinants, and treatment system factors.
That MHQoL outcomes across racial and ethnic groups partially differed in direction from those of PTSD symptom changes was surprising given the moderately high correlation across outcomes noted here and by others (Schnurr & Lunney, 2016; Shiner et al., 2011). In our post-hoc analyses, we found that the greater improvement among African American veterans relative to NLWs was limited to those whose PTSD symptoms showed a significant large effect improvement, suggesting that the lower (i.e., worse) initial MHQoL in those African American veterans was directly associated with the severity of their PTSD. A similar, but attenuated pattern was noted among Native Americans. These findings speak to the deleterious impact PTSD has on the lives of many veterans and the critical importance of providing appropriate and effective treatments. Most importantly, those who experienced improvement in PTSD symptomatology also experienced improved MHQoL.
Asian, Hawaiian, and Pacific Islander veterans had better MHQoL outcomes only in the treatment initiator group, suggesting that improving their mental health treatment access and/or uptake may improve health outcomes even further for many of these veterans. Because of small sample sizes, we were not able to explore in this study whether the benefit from treatment initiation was equally true for Asian Americans, Native Hawaiians, and Pacific Islanders. Veterans in these three groups differ from each other in many ways, including rates of PTSD, socioeconomic factors, geography, and beliefs about treatments (Spoont et al., 2015; Tsai & Kong, 2012; Whealin et al., 2015, 2013) -- any of which may drive group differences in treatment receipt and/or clinical outcomes. More granular studies with larger samples are needed to determine if outcomes differ among these subgroups as well.
VHA has undergone a number of transformations since these data were collected (2009-2010), such as a national roll-out of evidence based treatments for PTSD (Eftekhari et al., 2013; Karlin & Cross, 2014) and expansion of the mental health provider workforce (Rosenheck & Fontana, 2007). Veterans engaged in treatment at facilities embracing the evidence based treatment initiative have witnessed more significant average improvements than those found in this study (Sripada et al., 2017), suggesting that increased dissemination or and engagement in more efficacious treatments will likely increase overall improvement rates.
There were several limitations in this study. First, although we had a relatively large sample, it is possible that our models are not generalizable to the population of veterans with PTSD in VA. Although we attempted to statistically extrapolate to the broader population of veterans, subgroup comparisons were hampered by sparse representation in select strata. Despite this limitation, our findings for the observed and adjusted models are very similar, indicating that they appear to be robust to the effects of response bias. To be included in the study, all participants had to have been diagnosed with PTSD by a primary care or mental health provider. However, we do not know for certain if all veterans in the study actually had PTSD or how many veterans in the sample would have been excluded if PTSD were more rigorously assessed. It is possible that our findings might differ if those who did not meet full PTSD criteria were removed from the sample. Our use of a 6-month follow-up period may have also impacted our findings. Not all veterans had finished, and some may not have even started, treatment by that endpoint. Improvements may still have occurred for such veterans. It is possible that population outcome rates and group differences in those rates might be different if a longer follow-up timeframe had been used. Finally, these data were collected just at the beginning of the national roll-out of evidence based treatments for PTSD within the VA health care system (Eftekhari et al., 2013; Karlin & Cross, 2014). It may be that the racial and ethnic disparities we observed are no longer present given greater availability of more efficacious, manualized evidence-based treatments. However, because less than half of veterans receive one of these evidence based treatments and that some minority groups may be less likely to receive them than NLWs, improved overall outcomes or reduced disparities in those outcomes are far from certain (Cook et al., 2014; Rosen et al., 2018; Steenkamp et al., 2015). If racial and ethnic minority veterans are less likely to receive an evidence based treatment or are less likely to complete one, the nationwide dissemination may inadvertently further exacerbate racial and ethnic disparities in outcomes by selectively improving those of NLWs to a greater extent.
To better understand drivers of racial and ethnic disparities in outcomes among veterans with PTSD, it will be important to examine specific processes of care as well as potential contributions of social determinants of health on treatment behavior. Detailed knowledge of veterans’ resources, social support networks, mental health service accessibility, treatments offered, treatments received, and quality of care would be needed. More frequent assessments would help to disentangle the impact of specific factors on clinical outcomes.
Given numerous changes across the VA health care system since these data were ascertained, it will also be important to determine if racial and ethnic disparities in mental health treatment outcomes have been exacerbated or ameliorated by these changes and to identify specific current drivers of outcome disparities. These data may be viewed as a baseline against which future system-wide interventions to improve outcomes or diminish disparities can be evaluated.
Supplementary Material
Acknowledgments
This work was funded by the Department of Veterans Affairs Health Services Research and Development grant (IAC-06-266) awarded to the first author. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
A portion of this work was presented as a poster at the 33rd Annual Meeting of the International Society for Traumatic Stress Studies, November 9-11, 2017, Chicago, Illinois.
Contributor Information
Michele Spoont, National Center for PTSD, Pacific Islands Division, Center for Care Delivery and Outcomes Research, a VA HSR&D Center of Innovation, Minneapolis VA Healthcare System, One Veterans Drive 152/ Bldg 9, Minneapolis, MN 55417, Departments of Medicine and Psychiatry, University of Minnesota, Minneapolis, MN.
David Nelson, Center for Care Delivery and Outcomes Research, a VA HSR&D Center of Innovation, Minneapolis VA Healthcare System, One Veterans Drive 152/ Bldg 9, Minneapolis, MN 55417, Departments of Medicine and Biostatistics, University of Minnesota, Minneapolis, MN.
Shannon Kehle-Forbes, National Center for PTSD, Women’s Health Division, Center for Care Delivery and Outcomes Research, a VA HSR&D Center of Innovation, Minneapolis VA Healthcare System, Department of Medicine, University of Minnesota, Minneapolis, MN.
Laura Meis, Center for Care Delivery and Outcomes Research, a VA HSR&D Center of Innovation, Minneapolis VA Healthcare System, Department of Medicine, University of Minnesota, Minneapolis, MN.
Maureen Murdoch, Center for Care Delivery and Outcomes Research, a VA HSR&D Center of Innovation, Minneapolis VA Healthcare System, Department of Medicine, University of Minnesota, Minneapolis, MN.
Craig Rosen, National Center for PTSD, Disssemination and Training Division, VA Palo Alto Health Care System, 795 Willow Road, Menlo Park, CA 94025, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine.
Nina Sayer, Center for Care Delivery and Outcomes Research, a VA HSR&D Center of Innovation, Minneapolis VA Healthcare System, Departments of Medicine and Psychiatry.
REFERENCES
- Alegría M, Alvarez K, Ishikawa RZ, DiMarzio K, & McPeck S (2016). Removing Obstacles To Eliminating Racial And Ethnic Disparities In Behavioral Health Care. Health Affairs., 35(6), 991–999. 10.1377/hlthaff.2016.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- Chen R, Kessler RC, Sadikova E, NeMoyer A, Sampson NA, Alvarez K, Vilsaint CL, Green JG, McLaughlin KA, Jackson JS, Alegría M, & Williams DR (2019). Racial and ethnic differences in individual-level and area-based socioeconomic status and 12-month DSM-IV mental disorders. Journal of Psychiatric Research, S002239561930531X. 10.1016/j.jpsychires.2019.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook JM, Dinnen S, Simiola V, Thompson R, & Schnurr PP (2014). VA residential provider perceptions of dissuading factors to the use of two evidence-based PTSD treatments. Professional Psychology: Research and Practice, 45(2), 136–142. 10.1037/a0036183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillman DA (1991). The Design and Administration of Mail Surveys. Annual Review of Sociology, 17, 225–249. [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Lewis-Fernandez R, & Yager TJ (2008). War-Related Post-Traumatic Stress Disorder in Black, Hispanic, and Majority White Vietnam Veterans: The Roles of Exposure and Vulnerability. Journal of Traumatic Stress, 21(2), 133–141. 10.1002/jts.20327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duran DG, & Pérez-Stable EJ (2019). Novel Approaches to Advance Minority Health and Health Disparities Research. American Journal of Public Health, 109(S1), S8–S10. 10.2105/AJPH.2018.304931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dursa EK, Reinhard MJ, Barth SK, & Schneiderman AI (2014). Prevalence of a Positive Screen for PTSD Among OEF/OIF and OEF/OIF-Era Veterans in a Large Population-Based Cohort. Journal of Traumatic Stress, 27(5), 542–549. 10.1002/jts.21956 [DOI] [PubMed] [Google Scholar]
- Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, & Karlin BE (2013). Effectiveness of National Implementation of Prolonged Exposure Therapy in Veterans Affairs Care. JAMA Psychiatry, 70(9), 949–955. 10.1001/jamapsychiatry.2013.36 [DOI] [PubMed] [Google Scholar]
- Foynes MM, Smith BN, & Shipherd JC (2015). Associations Between Race-based and Sex-based Discrimination, Health, and Functioning: A Longitudinal Study of Marines. Medical Care, 53, S128–S135. 10.1097/MLR.0000000000000300 [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, Elbogen E, & Beckham JC (2015). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders, 31, 98–107. 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Goldberg J, Magruder KM, Forsberg CW, Kazis LE, Üstün TB, Friedman MJ, Litz BT, Vaccarino V, Heagerty PJ, Gleason TC, Huang GD, & Smith NL (2014). The association of PTSD with physical and mental health functioning and disability (VA Cooperative Study #569: The course and consequences of posttraumatic stress disorder in Vietnam-era Veteran twins). Quality of Life Research, 23(5), 1579–1591. 10.1007/s11136-013-0585-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpaz-Rotem I, & Hoff R (2018). FY2017 Overview of PTSD Patient Population Data Sheet (Annual (FY 2014-present)). VA Office of Mental Health and Suicide Prevention (10NC5): Northeast Program Evaluation Center. https://vaww.visn1.portal.va.gov/connecticut/nepec/ptsdreports/PTSD%20Annual%20Review%20Reports/FY%202017/PTSD%20FY17%20Supplemental%20fact%20sheet.pdf [Google Scholar]
- Hebenstreit CL, Madden E, Koo KH, & Maguen S (2015). Minimally adequate mental health care and latent classes of PTSD symptoms in female Iraq and Afghanistan veterans. Psychiatry Research, 230(1), 90–95. 10.1016/j.psychres.2015.08.028 [DOI] [PubMed] [Google Scholar]
- Holder N, Shiner B, Li Y, Madden E, Neylan TC, Seal KH, Lujan C, Patterson OV, DuVall SL, & Maguen S (2019). Timing of evidence-based psychotherapy for posttraumatic stress disorder initiation among Iraq and Afghanistan war veterans in the Veterans Health Administration. Psychological Trauma: Theory, Research, Practice, and Policy. 10.1037/tra0000496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imel ZE, Laska K, Jakupcak M, & Simpson TL (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81(3), 394–404. 10.1037/a0031474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones D, Kazis L, Lee A, Rogers W, Skinner K, Cassar L, Wilson N, & Hendricks A (2001). Health Status Assessments Using the Veterans SF-12 and SF-36: Methods for Evaluating Outcomes in the Veterans Health Administration: Journal of Ambulatory Care Management, 24(3), 68–86. 10.1097/00004479-200107000-00011 [DOI] [PubMed] [Google Scholar]
- Kaczkurkin AN, Asnaani A, Hall-Clark B, Peterson AL, Yarvis JS, & Foa EB (2016). Ethnic and racial differences in clinically relevant symptoms in active duty military personnel with posttraumatic stress disorder. Journal of Anxiety Disorders, 43, 90–98. 10.1016/j.janxdis.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Karlin BE, & Cross G (2014). From the laboratory to the therapy room: National dissemination and implementation of evidence-based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. American Psychologist, 69(1), 19–33. 10.1037/a0033888 [DOI] [PubMed] [Google Scholar]
- Kazis LE, Miller DR, Skinner KM, Lee A, Ren XS, Clark JA, Rogers WH, Iii AS, Selim A, Linzer M, Payne SMC, Mansell D, & Fincke BG (2006). Applications of Methodologies of the Veterans Health Study in the VA Healthcare System: Conclusions and Summary. Journal of Ambulatory Care Management, 29(2), 182–188. 10.1097/00004479-200604000-00011 [DOI] [PubMed] [Google Scholar]
- Kimerling R, Trafton JA, & Nguyen B (2006). Validation of a brief screen for Post-Traumatic Stress Disorder with substance use disorder patients. Addictive Behaviors, 31(11), 2074–2079. 10.1016/j.addbeh.2006.02.008 [DOI] [PubMed] [Google Scholar]
- Koo KH, Hebenstreit CL, Madden E, & Maguen S (2016). PTSD detection and symptom presentation: Racial/ethnic differences by gender among veterans with PTSD returning from Iraq and Afghanistan. Journal of Affective Disorders, 189, 10–16. 10.1016/j.jad.2015.08.038 [DOI] [PubMed] [Google Scholar]
- Koo KH, Madden E, & Maguen S (2015). Race-Ethnicity and Gender Differences in VA Health Care Service Utilization Among U.S. Veterans of Recent Conflicts. Psychiatric Services, 66(5), 507–513. 10.1176/appi.ps.201300498 [DOI] [PubMed] [Google Scholar]
- Kugelmass H (2016). “Sorry, I’m Not Accepting New Patients”: An Audit Study of Access to Mental Health Care. Journal of Health and Social Behavior, 57(2), 168–183. 10.1177/0022146516647098 [DOI] [PubMed] [Google Scholar]
- Le QA, Doctor JN, Zoellner LA, & Feeny NC (2013). Minimal clinically important differences for the EQ-5D and QWB-SA in Post-traumatic Stress Disorder (PTSD): Results from a Doubly Randomized Preference Trial (DRPT). Health and Quality of Life Outcomes, 11, 59–59. PMC. 10.1186/1477-7525-11-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loo CM, Singh K, Scurfield R, & Kilauano B (1998). Race-related stress among Asian American veterans: A model to enhance diagnosis and treatment. Cultural Diversity and Mental Health, 4(2), 75–90. [PubMed] [Google Scholar]
- Loo Chalsa M., Lim BR, Koff G, Morton RK, & Kiang PNC (2007). Ethnic-Related Stressors in the War Zone: Case Studies of Asian American Vietnam Veterans. Military Medicine, 172(9), 968–971. 10.7205/MILMED.172.9.968 [DOI] [PubMed] [Google Scholar]
- Maguen S, Li Y, Madden E, Seal KH, Neylan TC, Patterson OV, DuVall SL, Lujan C, & Shiner B (2019). Factors associated with completing evidence-based psychotherapy for PTSD among veterans in a national healthcare system. Psychiatry Research, 274, 112–128. 10.1016/j.psychres.2019.02.027 [DOI] [PubMed] [Google Scholar]
- Maguen S, Madden E, Neylan TC, Cohen BE, Bertenthal D, & Seal KH (2014). Timing of Mental Health Treatment and PTSD Symptom Improvement Among Iraq and Afghanistan Veterans. Psychiatric Services, 65(12), 1414–1419. 10.1176/appi.ps.201300453 [DOI] [PubMed] [Google Scholar]
- Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, Corry N, Williams CS, Ho C-L, Horesh D, Karstoft K-I, Shalev A, & Kulka RA (2015). Course of Posttraumatic Stress Disorder 40 Years After the Vietnam War: Findings From the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry, 72(9), 875–881. 10.1001/jamapsychiatry.2015.0803 [DOI] [PubMed] [Google Scholar]
- Marx BP, Engel-Rebitzer E, Bovin MJ, Parker-Guilbert KS, Moshier S, Barretto K, Szafranski D, Gallagher MW, Holowka DW, Rosen RC, & Keane TM (2017). The influence of veteran race and psychometric testing on veterans affairs posttraumatic stress disorder (PTSD) disability exam outcomes. Psychological Assessment, 29(6), 710–719. 10.1037/pas0000378 [DOI] [PubMed] [Google Scholar]
- McDonald SD, & Calhoun PS (2010). The diagnostic accuracy of the PTSD Checklist: A critical review. Clinical Psychology Review, 30(8), 976–987. 10.1016/j.cpr.2010.06.012 [DOI] [PubMed] [Google Scholar]
- Merino Y, Adams L, & Hall WJ (2018). Implicit Bias and Mental Health Professionals: Priorities and Directions for Research. Psychiatric Services, 69(6), 723–725. 10.1176/appi.ps.201700294 [DOI] [PubMed] [Google Scholar]
- Mott JM, Barrera TL, Hernandez C, Graham DP, & Teng EJ (2014). Rates and Predictors of Referral for Individual Psychotherapy, Group Psychotherapy, and Medications among Iraq and Afghanistan Veterans with PTSD. The Journal of Behavioral Health Services & Research, 41(2), 99–109. 10.1007/s11414-013-9352-0 [DOI] [PubMed] [Google Scholar]
- Muralidharan A, Austern D, Hack S, & Vogt D (2016). Deployment Experiences, Social Support, and Mental Health: Comparison of Black, White, and Hispanic U.S. Veterans Deployed to Afghanistan and Iraq. Journal of Traumatic Stress, 29(3), 273–278. 10.1002/jts.22104 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2018). Evaluation of the Department of Veterans Affairs Mental Health Services. National Academies Press. 10.17226/24915 [DOI] [PubMed] [Google Scholar]
- NCPTSD. (2012). Using the PTSD Checklist (PCL). Department of Veterans Affairs, National Center for PTSD. https://www.ptsd.va.gov/professional/assessment/documents/PCL_handoutDSM4.pdf [Google Scholar]
- Norman GR, Sloan JA, & Wyrwich KW (2003). Interpretation of Changes in Health- related Quality of Life: The Remarkable Universality of Half a Standard Deviation. Medical Care, 41(5), 582–592. 10.1097/01.MLR.0000062554.74615.4C [DOI] [PubMed] [Google Scholar]
- Penner LA, Hagiwara N, Eggly S, Gaertner SL, Albrecht TL, & Dovidio JF (2013). Racial healthcare disparities: A social psychological analysis. European Review of Social Psychology, 24(1), 70–122. 10.1080/10463283.2013.840973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Wachen JS, Dondanville KA, Pruiksma KE, Yarvis JS, Peterson AL, Mintz J, and the STRONG STAR Consortium, Borah EV, Brundige A, Hembree EA, Litz BT, Roache JD, & Young-McCaughan S (2017). Effect of Group vs Individual Cognitive Processing Therapy in Active-Duty Military Seeking Treatment for Posttraumatic Stress Disorder: A Randomized Clinical Trial. JAMA Psychiatry, 74(1), 28. 10.1001/jamapsychiatry.2016.2729 [DOI] [PubMed] [Google Scholar]
- Rosen CS, Bernardy NC, Chard KM, Clothier B, Cook JM, Crowley J, Eftekhari A, Kehle-Forbes SM, Mohr DC, Noorbaloochi S, Orazem RJ, Ruzek JI, Schnurr PP, Smith BN, & Sayer NA (2018). Which Patients Initiate Cognitive Processing Therapy and Prolonged Exposure in Department of Veterans Affairs PTSD Clinics? Journal of Anxiety Disorders. 10.1016/j.janxdis.2018.11.003 [DOI] [PubMed] [Google Scholar]
- Rosenheck RA, & Fontana AF (2007). Recent Trends In VA Treatment Of Post- Traumatic Stress Disorder And Other IVIentai Disorders. Health Affairs, 26(6), 1720–1727. 10.1377/hlthaff.26.6.1720 [DOI] [PubMed] [Google Scholar]
- Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, Friedman MJ, & Fullerton CS (2013). A Systematic Review of PTSD Prevalence and Trajectories in DSM-5 Defined Trauma Exposed Populations: Intentional and Non- Intentional Traumatic Events. PLoS ONE, 8(4), e59236. 10.1371/journal.pone.0059236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, & Lunney CA (2016). SYMPTOM BENCHMARKS OF IMPROVED QUALITY OF LIFE IN PTSD: Research Article: Symptom Change and Quality of Life in PTSD. Depression and Anxiety, 33(3), 247–255. 10.1002/da.22477 [DOI] [PubMed] [Google Scholar]
- Shiner B, Watts BV, Pomerantz A, Young-Xu Y, & Schnurr PP (2011). Sensitivity of the SF-36 to PTSD symptom change in veterans. Journal of Traumatic Stress, 24(1), 111–115. 10.1002/jts.20613 [DOI] [PubMed] [Google Scholar]
- Sibrava NJ, Bjornsson AS, Pérez Benítez ACI, Moitra E, Weisberg RB, & Keller MB (20190117). Posttraumatic stress disorder in African American and Latinx adults: Clinical course and the role of racial and ethnic discrimination. American Psychologist, 74(1), 101. 10.1037/amp0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan DM, Bovin MJ, & Schnurr PP (2012). Review of group treatment for PTSD. The Journal of Rehabilitation Research and Development, 49(5), 689. 10.1682/JRRD.2011.07.0123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, & Alan R (Eds.). (2003). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (p. 12875). National Academies Press. 10.17226/12875 [DOI] [PubMed] [Google Scholar]
- Smith SM, Goldstein RB, & Grant BF (2016). The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Journal of Psychiatric Research, 82, 16–22. 10.1016/j.jpsychires.2016.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoont M, Nelson DB, Murdoch M, Sayer NA, Nugent S, Rector T, & Westermeyer J (2015). Are There Racial/Ethnic Disparities in VA PTSD Treatment Retention? Depression and Anxiety, 32(6), 415–425. 10.1002/da.22295 [DOI] [PubMed] [Google Scholar]
- Spoont MR, Sayer NA, Kehle-Forbes SM, Meis LA, & Nelson DB (2017). A Prospective Study of Racial and Ethnic Variation in VA Psychotherapy Services for PTSD. Psychiatric Services, 68(3), 231–237. 10.1176/appi.ps.201600086 [DOI] [PubMed] [Google Scholar]
- Spoont MR, Hodges J, Murdoch M, & Nugent S (2009). Race and ethnicity as factors in mental health service use among veterans with PTSD. Journal of Traumatic Stress, n/a-n/a. 10.1002/jts.20470 [DOI] [PubMed] [Google Scholar]
- Spoont MR, Sayer NA, Kehle-Forbes SM, Meis LA, & Nelson DB (2017). A Prospective Study of Racial and Ethnic Variation in VA Psychotherapy Services for PTSD. Psychiatric Services, 68(3), 231–237. 10.1176/appi.ps.201600086 [DOI] [PubMed] [Google Scholar]
- Sripada RK, Blow FC, Rauch SAM, Ganoczy D, Hoff R, Harpaz-Rotem I, & Bohnert KM (2019). Examining the nonresponse phenomenon: Factors associated with treatment response in a national sample of veterans undergoing residential PTSD treatment. Journal of Anxiety Disorders, 63, 18–25. 10.1016/j.janxdis.2019.02.001 [DOI] [PubMed] [Google Scholar]
- Sripada RK, Pfeiffer PN, Rampton J, Ganoczy D, Rauch SAM, Polusny MA, & Bohnert KM (2017). Predictors of PTSD Symptom Change Among Outpatients in the U.S. Department of Veterans Affairs Health Care System: Predictors of PTSD Symptom Change. Journal of Traumatic Stress, 30(1), 45–53. 10.1002/jts.22156 [DOI] [PubMed] [Google Scholar]
- Sripada RK, Ready DJ, Ganoczy D, Astin MC, & Rauch SAM (2020). When to Change the Treatment Plan: An Analysis of Diminishing Returns in VA Patients Undergoing Prolonged Exposure and Cognitive Processing Therapy. Behavior Therapy, 51(1), 85–98. 10.1016/j.beth.2019.05.003 [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, & Marmar CR (2015). Psychotherapy for Military-Related PTSD: A Review of Randomized Clinical Trials. JAMA, 314(5), 489–500. 10.1001/jama.2015.8370 [DOI] [PubMed] [Google Scholar]
- Stefanovics EA, Rosenheck RA, Jones KM, Huang G, & Krystal JH (2018). Minimal Clinically Important Differences (MCID) in Assessing Outcomes of Post-Traumatic Stress Disorder. Psychiatric Quarterly, 89(1), 141–155. 10.1007/s11126-017-9522-y [DOI] [PubMed] [Google Scholar]
- The Management of Posttraumatic Stress Disorder Work Group. (2017). VA/DOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder.
- Trivedi RB, Post EP, Sun EL, Pomerantz A, Saxon AJ, Piette JD, Maynard C, Amow B, Curtis I, Fihn SD, & Nelson K (2015). Prevalence, Comorbidity, and Prognosis of Mental Health Among US Veterans. American Journal of Public Health, 705(12), 2564–2569. 10.2105/AJPH.2015.302836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J, & Kong G (2012). Mental health of Asian American and Pacific Islander military veterans: Brief review of an understudied group. Military Medicine, 777(11), 1438–1444. [DOI] [PubMed] [Google Scholar]
- Weathers FW (1993, January). International Society for Traumatic Stress Studies. http://scholar.google.com/scholar_url?url=https://www.researchgate.net/profile/Frank_Weathers/publication/313709159_PTSD_Checklist_Reliability_validity_and_diagnostic_utility/links/58a5e38f92851cf0e39f24bl/PTSD-Checklist-Reliability-validity-and-diagnosticutility&hl=en&sa=X&scisig=AAGBfm3k34_vVN_W2AlL2MHgKZtLbopSEg&nossl=l&oi=scholarr [Google Scholar]
- Whealin JM, Nelson D, Stotzer R, Guerrero A, Carpenter M, & Pietrzak RH (2015). Risk and resilience factors associated with posttraumatic stress in ethno-racially diverse National Guard members in Hawai’i. Psychiatry Research, 227(2–3), 270–277. 10.1016/j.psychres.2015.02.023 [DOI] [PubMed] [Google Scholar]
- Whealin JM, Stotzer R, Nelson D, Li F, Liu-Tom H-TT, & Pietrzak RH (2013). Evaluating PTSD prevalence and resilience factors in a predominantly Asian American and Pacific Islander sample of Iraq and Afghanistan Veterans. Journal of Affective Disorders, 150(3), 1062–1068. 10.1016/j.jad.2013.05.044 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


