Abstract
Background:
Despite the considerable public health burden of rotator cuff tears, there is no consensus on risk factors associated with symptomatic rotator cuff tears. In this study, a large data source was used to identify factors associated with symptomatic rotator cuff tears. We defined cases of rotator cuff tears as those verified by imaging or operative reports and controls as symptomatic shoulders without rotator cuff tears as verified by imaging or operative reports.
Methods:
We performed a case-control study of patients with and without symptomatic rotator cuff tears by use of the Vanderbilt University Medical Center de-identified electronic medical record system, the Synthetic Derivative, with records on >2.5 million patients from 1998 to 2017. Cases and controls were confirmed by individual chart review and review of imaging and/or operative notes. A final set of 11 variables were analyzed as potential risk factors for cuff tears: age, sex, body mass index (BMI), race, smoking history, hypertension, depression/anxiety, dyslipidemia, carpal tunnel syndrome, overhead activity, and affected side. Multivariable logistic regression was used to estimate the association between predictor variables and the risk of having a rotator cuff tear.
Results:
A total of 2738 patients were selected from the Synthetic Derivative, which included 1731 patients with rotator cuff tears and 1007 patients without rotator cuff tears. Compared with individuals without tears, those with rotator cuff tears were more likely to be older (odds ratio [OR], 2.44; 95% confidence interval [CI], 2.12–2.89), to have a higher BMI (OR, 1.45; 95% CI, 1.24–1.69), to be of male sex (OR, 1.56; 95% CI, 1.32–1.85), and to have carpal tunnel syndrome (OR, 1.41; 95% CI, 1.03–1.93). Patients with rotator cuff tears were less likely to have left shoulder symptoms (OR, 0.68; 95% CI, 0.57–0.82) and to have depression/anxiety (OR, 0.77; 95% CI, 0.62–0.95) compared with the control group, which had symptomatic shoulder pain without rotator cuff tears.
Conclusions:
In a large imaging and operative report–verified case-control study, we identified advancing age, male sex, higher BMI, and diagnosis of carpal tunnel syndrome as risk factors significantly associated with an increased risk of rotator cuff tears. Left shoulder symptoms and depression/anxiety were less likely to be associated with rotator cuff tears compared with symptomatic shoulders without rotator cuff tears. Contrary to some prior reports in the literature, smoking was not associated with rotator cuff tears.
Level of evidence:
Level III; Retrospective Case-Control Design; Prognosis Study
Keywords: Rotator cuff, risk factors, body mass index, case control, depression, smoking
Rotator cuff tears are a common cause of shoulder pain, with a lifetime incidence between 25% and 40% in the United States.41,43 An estimated 272,148 rotator cuff repairs are performed annually in the United States,23 and the rates of these procedures have been increasing over time.3,24,43 Despite their considerable public health burden, data on the risk factors associated with symptomatic rotator cuff tears are sparse. Several studies have investigated risk factors for both symptomatic and asymptomatic rotator cuff tears in variable study populations.1,19,20,22,30,40,46 However, recruitment of a large study population with rotator cuff tears has been difficult from a logistical and financial perspective, and some of these studies have had smaller sample sizes. Nevertheless, a recent UK-based study did explore risk factors for surgery in patients with rotator cuff tears in a population cohort of 2156 patients.47
An improved understanding of the etiology of rotator cuff tears can help to identify at-risk individuals and improve future treatment options. Age, sex, ethnicity, body mass index (BMI), smoking history, and family history have all been proposed as risk factors.14,18,27,39,44 We hypothesized that age and overhead activity would be the risk factors most likely to be associated with the presence of a rotator cuff tear given that rotator cuff tears are thought to be an age-related degenerative process. Thus, we performed a case-control study of 2738 patients to identify risk factors associated with the likelihood of a symptomatic rotator cuff tear by using an electronic medical record (EMR) repository of >2.5 million patients. We defined cases as patients with symptomatic rotator cuff tears verified by imaging or operative reports and controls as patients with shoulder symptoms without tears by imaging or operative reports.
Materials and methods
Patient population
Patients were selected from a de-identified version of an EMR depository, the Synthetic Derivative (SD), with records on >2.5 million patients at Vanderbilt University Medical Center (Nashville, TN, USA) from 1998 to 2017.36 In brief, the SD was designed to provide researchers and administrators a secure and reliable method to query clinical data. The SD can be considered a de-identified, reorganized mirror of clinical data collected at Vanderbilt University Medical Center including, but not limited to, laboratory data, provider order entry, provider and nursing documentation, and various other ancillary data including radiology data.15
Patient selection
With the assistance of a bioinformatics programmer and using an algorithm previously described,17 we extracted a sample of 2738 total patients with shoulder symptoms. Of these patients, 1731 were identified to have rotator cuff tears (cases) and 1007 patients were found to be without rotator cuff tears (controls). All of these cases and controls were individuals aged between 40 and 75 years. Individual chart reviews were performed to determine whether patients had rotator cuff tears.
Case definition
Patients with magnetic resonance imaging (MRI) or operative reports documenting rotator cuff tendon tears or a surgical history of rotator cuff repair were classified as having rotator cuff tears (cases). Both partial- and full-thickness tears were included as rotator cuff tears. Patients with distinct documentation of MRI or operative findings of rotator cuff tears in the physician notes, despite a lack of formal MRI or operative reports, were also classified as having rotator cuff tears.
Control definition
A control was defined as a patient without a partial- or full-thickness rotator cuff tear. A patient who presented with shoulder pain but was documented to have an intact rotator cuff by MRI and/or operative report was defined as a patient without a rotator cuff tear and, thus, a control patient. Other pathologies may have been the underlying etiology for these patients’ shoulder pain, but all control patients had intact rotator cuff tendons. Imaging or operative documentation of an intact cuff is essential to classify a patient as having a normal rotator cuff because imaging data show that 40%−65% of individuals aged ≥ 50 years without shoulder symptoms have rotator cuff tears.17
Risk factor selection
Initially, 34 variables were selected a priori as potential risk factors of interest based on expert opinion and previously published peer-reviewed data.1,20,22,25,30,38,40,41,46 Risk factors were determined by keyword queries and data extraction from structured fields within the SD de-identified EMR database. The presence or absence of these risk factor variables in cases and controls was then identified in the SD de-identified electronic record by a bioinformatics programmer. Data extraction from the SD was performed in a systematic manner with guidance from our clinical experts via data from structured fields in the EMR by using keyword queries and International Classification of Diseases, Clinical Modification (ninth revision and tenth revision) codes. Risk factors were categorized as demographic characteristics (age, sex, race, ethnicity), physical factors (height, weight), social factors (tobacco use, alcohol use, occupation, marital status, education level), presence of medical comorbidities (hypertension, hyperlipidemia, diabetes, rheumatoid arthritis, depression, anxiety, arthritis), laboratory values (C-reactive protein level, high-density lipid level, low-density lipid level), and shoulder-related factors (duration of symptoms, history of overhead activity, dominant shoulder, contralateral shoulder problems, history of adhesive capsulitis, shoulder osteoarthritis, history of fluoroquinolone use).
Statistical analysis
Redundancy analysis was conducted and variables with R2 > 0.9 were removed to avoid collinearity. Hierarchical clustering using the Spearman correlation metric was estimated to assess whether a set of variables provide similar information. From the initial 34 variables selected a priori, redundancy and clustering analysis was used to eliminate variables providing similar information. A final set of 11 variables were analyzed as potential risk factors for cuff tears. Differences in these risk factors between the case and control groups were tested by the Pearson test for categorical variables and the Wilcoxon rank sum test for continuous variables. These variables comprised age, sex, BMI, race, smoking history (currently or formerly), hypertension, depression/anxiety, dyslipidemia, carpal tunnel syndrome, overhead activity, and affected side (left or right). To adjust for missing data, 20 imputation data sets were analyzed using predictive mean matching. Estimates of standard errors among these data sets were calculated using Rubin’s rules.37 Logistic regression was used to estimate the association between predictor variables and the probability of a rotator cuff tear. All analyses were conducted using R, version 3.4.1.32
Results
Of the 2738 patients included from the SD, 1731 had rotator cuff tears and 1007 did not have rotator cuff tears (Table I). As compared with patients without rotator cuff tears, those with rotator cuff tears were older (mean age ± standard deviation, 64 ± 8 years vs. 59 ± 9 years), had a greater BMI (mean BMI ± standard deviation, 31 ± 7 kg/m2 vs. 29 ± 7 kg/m2), and were more likely to be male patients (n = 929 [54%] vs. n = 432 [43%]) (P < .001).
Table I.
Baseline characteristics of patients with and without rotator cuff tears selected from Synthetic Derivative cohort from 1998 to 2017 (N = 2738)
| Characteristic | Rotator cuff tear group (n = 1731) | Control group (n = 1007) |
|---|---|---|
| Age, yr* | 64 ± 8 | 59 ± 9 |
| BMI, kg/m2* | 31 ± 7 | 29 ± 7 |
| Sex* | ||
| Male | 929 (54) | 432 (43) |
| Female | 802 (46) | 575 (57) |
| Race | ||
| Black | 196 (12) | 104 (11) |
| White | 1455 (87) | 864 (88) |
| Other | 30 (2) | 16 (2) |
| Smoking history* | ||
| Current smoker | 148 (11) | 108 (13) |
| Former smoker | 261 (19) | 128 (16) |
| Never smoker | 946 (70) | 571 (71) |
| Hypertension* | 875 (50) | 462 (46) |
| Depression/anxiety* | 974 (56) | 628 (62) |
| Dyslipidemia* | 565 (33) | 270 (27) |
| Carpal tunnel syndrome* | 168 (10) | 70 (7) |
| Overhead activity and/or sport* | 133 (8) | 107 (11) |
| Affected side* | ||
| Left | 605 (41) | 430 (48) |
| Right | 883 (59) | 472 (52) |
BMI, body mass index.
Data are presented as mean ± standard deviation or number (percentage).
Statistically significant difference at P ≤ .05.
For ease of clinical interpretation, we have presented the odds ratios (ORs) comparing the 75th percentile with the 25th percentile for continuous variables (Fig. 1). In the multivariable logistic regression model, advancing age (OR, 2.44 for 75th percentile of age [69 years] vs. 25th percentile of age [56 years]; 95% confidence interval [CI], 2.13–2.80), higher BMI (OR, 1.45 for 75th percentile of BMI [34 kg/m2] vs. 25th percentile of BMI [25 kg/m2]; 95% CI, 1.24–1.69), male sex (OR, 1.56; 95% CI, 1.32–1.85), and diagnosis of carpal tunnel syndrome (OR, 1.41; 95% CI, 1.03–1.93) were associated with higher odds of having rotator cuff tears.
Figure 1.
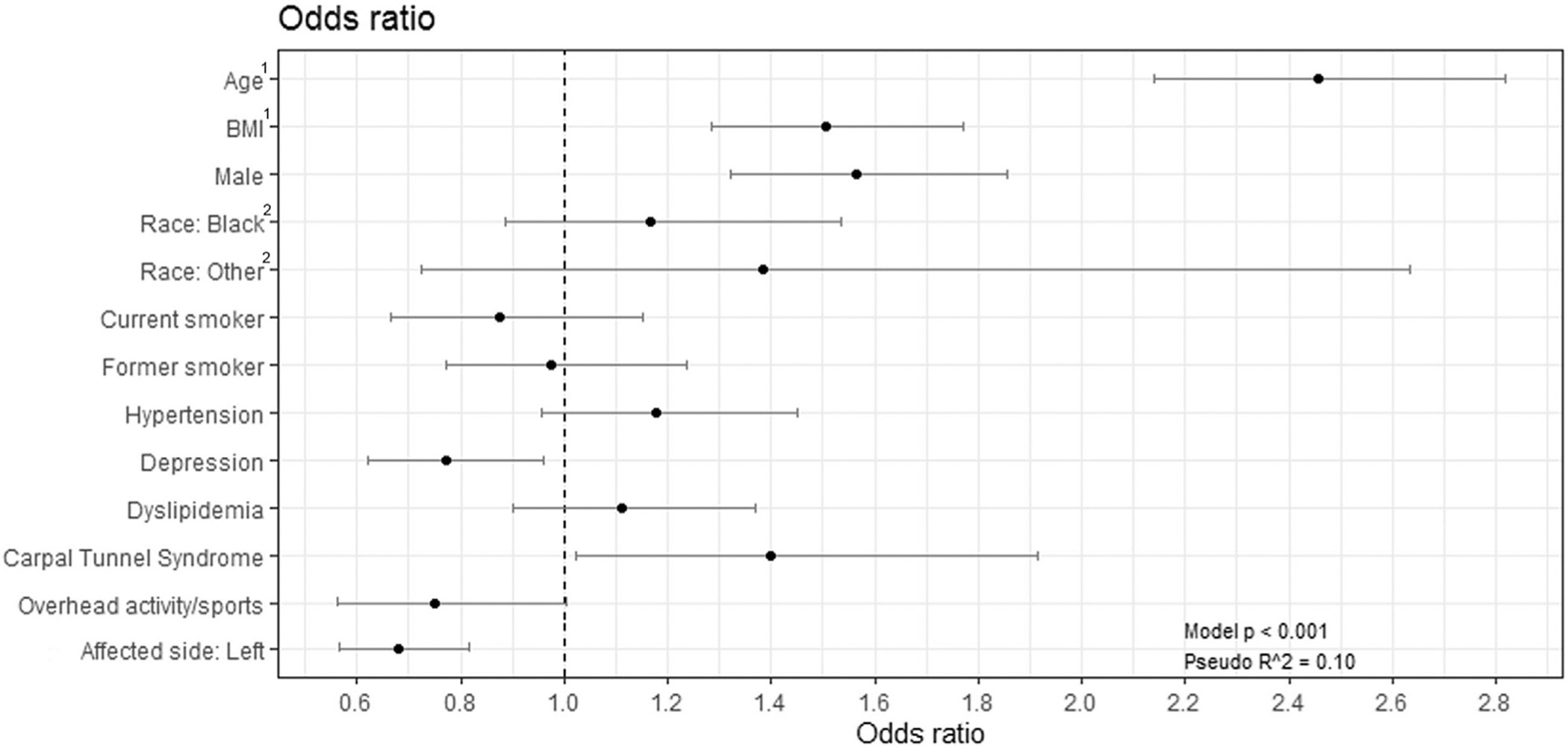
Risk factors associated with degenerative, symptomatic rotator cuff tears in a cohort of patients selected from the Synthetic Derivative database (N = 2738). Bars represent 95% confidence intervals. 1Odds ratios for age and body mass index (BMI) comparing 75th percentile with 25th percentile. 2Odds ratios for race comparing black race and other race with white race.
Risk factors protective against the presence of a rotator cuff tear were left-sided symptoms (OR, 0.68; 95% CI, 0.57–0.82) and depression/anxiety (OR, 0.77; 95% CI, 0.62–0.95) (Table II). Smoking, race, hypertension, dyslipidemia, and overhead activity were not significantly associated with the diagnosis of rotator cuff tears. Overall, the variable with the greatest relative contribution to our multivariable logistic regression model was age, followed by sex, BMI, and affected side (P < .001; Fig. 2).
Table II.
ORs of patient characteristics associated with rotator cuff tears
| Risk factor | OR | 95% CI | |
|---|---|---|---|
| Lower | Upper | ||
| Age (75th percentile [69 yr] vs. 25th percentile [56 yr]) | 2.44 | 2.13 | 2.80 |
| Sex (male vs. female) | 1.56 | 1.32 | 1.85 |
| BMI (75th percentile [34 kg/m2] vs. 25th percentile [25 kg/m2]) | 1.45 | 1.24 | 1.69 |
| Race | |||
| Black vs. white | 1.21 | 0.93 | 1.59 |
| Other vs. white | 1.45 | 0.76 | 2.76 |
| Smoking | |||
| Current vs. never | 0.85 | 0.65 | 1.12 |
| Former vs. never | 0.97 | 0.76 | 1.25 |
| Hypertension | 1.19 | 0.96 | 1.46 |
| Depression | 0.77 | 0.62 | 0.95 |
| Dyslipidemia | 1.12 | 0.91 | 1.38 |
| Carpal tunnel syndrome | 1.41 | 1.03 | 1.93 |
| Overhead activity | 0.75 | 0.56 | 1.00 |
| Affected shoulder (left vs. right) | 0.68 | 0.57 | 0.82 |
OR, odds ratio; BMI, body mass index; CI, confidence interval.
Figure 2.
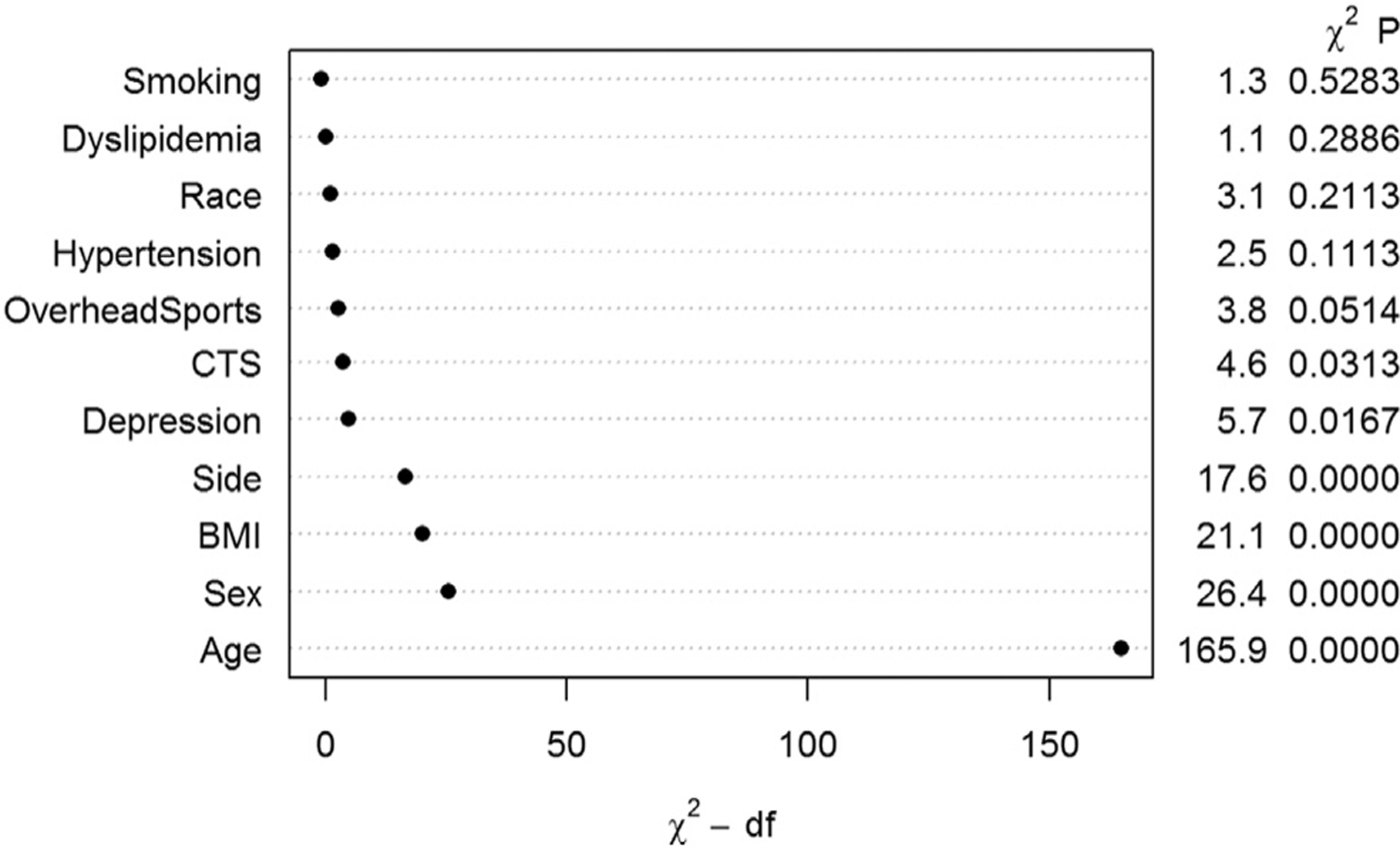
Relative contribution to multivariable logistic regression model of selected risk factors to probability of rotator cuff tear, in ascending order. CTS, carpal tunnel syndrome; BMI, body mass index.
Discussion
This case-control study compared patients with and without rotator cuff tears to determine variables associated with an increased likelihood of rotator cuff tears. Overall, increasing age, male sex, a higher BMI, and a diagnosis of carpal tunnel syndrome were significantly associated with an increased likelihood of rotator cuff tears. A diagnosis of depression/anxiety and left-sided symptoms were significantly associated with a decreased likelihood of rotator cuff tears. Contrary to some previous reports,4,7 smoking was not associated with the presence of a rotator cuff tear.
Prior literature has identified that advancing age is an independent risk factor for degenerative rotator cuff tears.5,22,39–41,46 The prevalence of rotator cuff tears is estimated to be as high as 80% after the age of 80 years.28 Advanced patient age has a strong association with diminished tendon healing rates and further progression of disease.6,29,31,33 Thus, the association of aging with rotator cuff tears is likely due to a degenerative process.
Prior studies have reported conflicting results on the association of male sex with rotator cuff tears. Several studies of smaller, single-site cohorts have shown an equivocal association of sex with rotator cuff tears.1,20,30,46 However, in our analysis, male sex was the second most strongly associated risk factor with the presence of a rotator cuff tear. A potential explanation for this relationship is shoulder overuse and physical labor among male individuals.34 Moreover, the protective effect of estrogen on tendon structure and mechanical properties has been reported in several studies.9,11,12,21
Our findings also correspond to recently reported literature on the association between an increasing BMI and the diagnosis of rotator cuff tears.1,20,30,35,44 The exact mechanism for this relationship is still unclear. The shoulder is not a weight-bearing joint, and thus, it would be unexpected for an increased BMI to contribute to the mechanism of injury for a rotator cuff tear. However, BMI may be a surrogate for obesity and other metabolic syndrome diseases such as diabetes, hypertension, and hyperlipidemia that affect the microvascular supply to the rotator cuff tendons, particularly near the footprint of the supraspinatus.10,26 Increased adiposity may also have a deleterious effect on tendon health through promotion of proinflammatory cytokines and oxidative stress.2,16,35
We found an increasing likelihood of rotator cuff tears with the presence of a previous diagnosis of carpal tunnel syndrome. An association between carpal tunnel syndrome and rotator cuff tears was also found in a study of Latino manual workers by Cartwright et al.8 Rather than a direct association between carpal tunnel syndrome and rotator cuff tears, this finding may be a result of the relationship of repetitive upper-extremity activity increasing the risk of overuse injuries such as carpal tunnel syndrome and rotator cuff tears. Our findings also indicate a predilection for right-shoulder involvement in patients with rotator cuff tears. Given that the prevalence of right-handedness is about 90% in the general population,42 our observation of rotator cuff tears occurring in the dominant shoulder is in line with the idea of shoulder overuse that may lead to tears in the cuff. This finding is supported by prior studies.30,38,46
The diagnosis of depression/anxiety was associated with a decreased likelihood of degenerative rotator cuff tears. However, in the literature, poor mental health has been associated with worse patient-reported shoulder pain and an increased risk of rotator cuff tears.13,25,45 Our results are likely contrary to those in the prior literature owing to the subset of the patient population presenting with shoulder pain in which MRI is warranted (controls in our study). This patient population may be more likely to have chronic, undifferentiated or nonspecific shoulder symptoms and thus an increased prevalence of depression/anxiety. Finally, smoking has been previously associated with rotator cuff tears.4,7 However, smoking was not associated with rotator cuff tears in our study. Clinicians may need to consider this new evidence in their practice because surgeons may be more hesitant to operate on patients who are current smokers.
The limitations of our study include a control group that may not be directly comparable to the general population because it consists of a selected group of patients who underwent shoulder MRI indicated by a symptomatic shoulder. Recruiting a random set of controls from the community and offering a research shoulder MRI scan were not feasible in our study. Although we had a large sample size and assessed several risk factors, selection bias may play a role in explaining some of our findings as we have done so for associations between rotator cuff tears and depression, as well as rheumatic disorders. Furthermore, residual confounding for factors such as smoking status and reverse causality for factors such as BMI may explain some of our findings in part. Our reported findings should best be interpreted as hypotheses and associations worthy of further investigation in longitudinal settings rather than as definitive causal associations. However, regardless of causality, these associations may be used to characterize frequently reported comorbidities in individuals with rotator cuff tears for surgical consideration.
Conclusion
Identifying factors associated with rotator cuff tears is critical in diagnostic prediction, disease prevention, and understanding the pathophysiology of disease. In a large imaging and operative report–verified case-control study, we identified increasing age, male sex, higher BMI, carpal tunnel syndrome, and dominant-shoulder involvement as risk factors significantly associated with rotator cuff tears. Contrary to some prior reports in the literature, smoking was not associated with rotator cuff tears. Conclusions from this large electronic health record study should be limited to associations rather than definitive causal inferences related to rotator cuff tears, particularly given that the control group was a selected group of patients who underwent shoulder MRI indicated by a symptomatic shoulder.
Disclaimer
The research reported in this manuscript was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (NIH) under award no. R01AR074989 and Clinical and Translational Sciences Award no. UL1TR000445 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the NIH.
Gregory D. Ayers receives all of his funding from NIH or National Cancer Institute grants; 10% of his effort is funded through the Center for Quantitative Sciences at Vanderbilt University Medical Center, which has a contractual agreement with a principal investigator who has a funding arrangement with Incyte. Dr. Ayers is a journal editor for the Journal of Shoulder and Elbow Surgery and receives a stipend for his reviews. All the other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was not required for this retrospective study.
References
- 1.Abate M, Di Carlo L, Salini V, Schiavone C. Risk factors associated to bilateral rotator cuff tears. Orthop Traumatol Surg Res 2017;103:841–5. 10.1016/j.otsr.2017.03.027 [DOI] [PubMed] [Google Scholar]
- 2.Abate M, Schiavone C, Salini V, Andia I. Occurrence of tendon pathologies in metabolic disorders. Rheumatology (Oxford) 2013;52: 599–608. 10.1093/rheumatology/kes395 [DOI] [PubMed] [Google Scholar]
- 3.Austin DC, Torchia MT, Lurie JD, Jevsevar DS, Bell J-E. Identifying regional characteristics influencing variation in the utilization of rotator cuff repair in the United States. J Shoulder Elbow Surg 2019;28: 1568–77. 10.1016/j.jse.2018.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baumgarten KM, Gerlach D, Galatz LM, Teefey SA, Middleton WD, Ditsios K, et al. Cigarette smoking increases the risk for rotator cuff tears. Clin Orthop Relat Res 2010;468:1534–41. 10.1007/s11999-009-0781-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berbig R, Weishaupt D, Prim J, Shahin O. Primary anterior shoulder dislocation and rotator cuff tears. J Shoulder Elbow Surg 1999;8:220–5. [DOI] [PubMed] [Google Scholar]
- 6.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 2005;87:1229–40. 10.2106/JBJS.D.02035 [DOI] [PubMed] [Google Scholar]
- 7.Carbone S, Gumina S, Arceri V, Campagna V, Fagnani C, Postacchini F. The impact of preoperative smoking habit on rotator cuff tear: cigarette smoking influences rotator cuff tear sizes. J Shoulder Elbow Surg 2012;21:56–60. 10.1016/j.jse.2011.01.039 [DOI] [PubMed] [Google Scholar]
- 8.Cartwright MS, Yeboah S, Walker FO, Rosenbaum DA, Newman JC, Arcury TA, et al. Examining the association between musculoskeletal injuries and carpal tunnel syndrome in manual laborers. Muscle Nerve 2016;54:31–5. 10.1002/mus.24982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cauley JA. Estrogen and bone health in men and women. Steroids 2015;99:11–5. 10.1016/j.steroids.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 10.Chansky HA, Iannotti JP. The vascularity of the rotator cuff. Clin Sports Med 1991;10:807–22. [PubMed] [Google Scholar]
- 11.Chidi-Ogbolu N, Baar K. Effect of estrogen on musculoskeletal performance and injury risk. Front Physiol 2018;9:1834. 10.3389/fphys.2018.01834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cook JL, Bass SL, Black JE. Hormone therapy is associated with smaller Achilles tendon diameter in active post-menopausal women. Scand J Med Sci Sports 2007;17:128–32. 10.1111/j.1600-0838.2006.00543.x [DOI] [PubMed] [Google Scholar]
- 13.Coronado RA, Seitz AL, Pelote E, Archer KR, Jain NB. Are psychosocial factors associated with patient-reported outcome measures in patients with rotator cuff tears? A systematic review. Clin Orthop Relat Res 2018;476:810–29. 10.1007/s11999.0000000000000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dabija DI, Gao C, Edwards TL, Kuhn JE, Jain NB. Genetic and familial predisposition to rotator cuff disease: a systematic review. J Shoulder Elbow Surg 2017;26:1103–12. 10.1016/j.jse.2016.11.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Danciu I, Cowan JD, Basford M, Wang X, Saip A, Osgood S, et al. Secondary use of clinical data: the Vanderbilt approach. J Biomed Inform 2014;52:28–35. 10.1016/j.jbi.2014.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gaida JE, Cook JL, Bass SL. Adiposity and tendinopathy. Disabil Rehabil 2008;30:1555–62. 10.1080/09638280701786864 [DOI] [PubMed] [Google Scholar]
- 17.Gao C, Fan R, Ayers GD, Giri A, Harris K, Atreya R, et al. Development and validation of an electronic medical record algorithm to identify phenotypes of rotator cuff tear. PM R 2020;12:1099–105. 10.1002/pmrj.12367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grusky AZ, Song A, Kim P, Ayers GD, Higgins LD, Kuhn JE, et al. Factors associated with symptomatic rotator cuff tears: the Rotator Cuff Outcomes Workgroup cohort study. Am J Phys Med Rehabil 2021;100:331–6. 10.1097/PHM.0000000000001684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gumina S, Arceri V, Carbone S, Albino P, Passaretti D, Campagna V, et al. The association between arterial hypertension and rotator cuff tear: the influence on rotator cuff tear sizes. J Shoulder Elbow Surg 2013;22:229–32. 10.1016/j.jse.2012.05.023 [DOI] [PubMed] [Google Scholar]
- 20.Gumina S, Candela V, Passaretti D, Latino G, Venditto T, Mariani L, et al. The association between body fat and rotator cuff tear: the influence on rotator cuff tear sizes. J Shoulder Elbow Surg 2014;23: 1669–74. 10.1016/j.jse.2014.03.016 [DOI] [PubMed] [Google Scholar]
- 21.Hansen M, Kjaer M. Sex hormones and tendon. Adv Exp Med Biol 2016;920:139–49. 10.1007/978-3-319-33943-6_13 [DOI] [PubMed] [Google Scholar]
- 22.Harvie P, Ostlere SJ, Teh J, McNally EG, Clipsham K, Burston BJ, et al. Genetic influences in the aetiology of tears of the rotator cuff. Sibling risk of a full-thickness tear. J Bone Joint Surg Br 2004;86:696–700. 10.1302/0301-620x.86b5.14747 [DOI] [PubMed] [Google Scholar]
- 23.Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord 2014;15:4. 10.1186/1471-2474-15-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jain NB, Peterson E, Ayers GD, Song A, Kuhn JE. US geographical variation in rates of shoulder and knee arthroscopy and association with orthopedist density. JAMA Netw Open 2019;2:e1917315. 10.1001/jamanetworkopen.2019.17315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuo L-T, Chen H-M, Yu P-A, Chen C-L, Hsu W-H, Tsai Y-H, et al. Depression increases the risk of rotator cuff tear and rotator cuff repair surgery: a nationwide population-based study. PLoS One 2019;14: e0225778. 10.1371/journal.pone.0225778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lohr JF, Uhthoff HK. The microvascular pattern of the supraspinatus tendon. Clin Orthop Relat Res 1990:35–8. [PubMed] [Google Scholar]
- 27.Maher A, Leigh W, Brick M, Young S, Millar J, Walker C, et al. Gender, ethnicity and smoking affect pain and function in patients with rotator cuff tears. ANZ J Surg 2017;87:704–8. 10.1111/ans.13921 [DOI] [PubMed] [Google Scholar]
- 28.Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br 1995;77:296–8. [PubMed] [Google Scholar]
- 29.Oh JH, Kim SH, Kang JY, Oh CH, Gong HS. Effect of age on functional and structural outcome after rotator cuff repair. Am J Sports Med 2010;38:672–8. 10.1177/0363546509352460 [DOI] [PubMed] [Google Scholar]
- 30.Park HB, Gwark J-Y, Im J-H, Jung J, Na J-B, Yoon CH. Factors associated with atraumatic posterosuperior rotator cuff tears. J Bone Joint Surg Am 2018;100:1397–405. 10.2106/JBJS.16.01592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park JS, Park HJ, Kim SH, Oh JH. Prognostic factors affecting rotator cuff healing after arthroscopic repair in small to medium-sized tears. Am J Sports Med 2015;43:2386–92. 10.1177/0363546515594449 [DOI] [PubMed] [Google Scholar]
- 32.R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 33.Rashid MS, Cooper C, Cook J, Cooper D, Dakin SG, Snelling S, et al. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop 2017;88:606–11. 10.1080/17453674.2017.1370844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Razmjou H, Davis AM, Jaglal SB, Holtby R, Richards RR. Cross-sectional analysis of baseline differences of candidates for rotator cuff surgery: a sex and gender perspective. BMC Musculoskelet Disord 2009;10:26. 10.1186/1471-2474-10-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rechardt M, Shiri R, Karppinen J, Jula A, Heliövaara M, Viikari-Juntura E. Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis: a population-based study. BMC Musculoskelet Disord 2010;11:165. 10.1186/1471-2474-11-165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roden DM, Pulley JM, Basford MA, Bernard GR, Clayton EW, Balser JR, et al. Development of a large-scale de-identified DNA biobank to enable personalized medicine. Clin Pharmacol Ther 2008; 84:362–9. 10.1038/clpt.2008.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons; 1987. [Google Scholar]
- 38.Sayampanathan AA, Andrew THC. Systematic review on risk factors of rotator cuff tears. J Orthop Surg (Hong Kong) 2017;25: 2309499016684318. 10.1177/2309499016684318 [DOI] [PubMed] [Google Scholar]
- 39.Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med 2012;31:589–604. 10.1016/j.csm.2012.07.001 [DOI] [PubMed] [Google Scholar]
- 40.Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg 1999;8: 296–9. [DOI] [PubMed] [Google Scholar]
- 41.Teunis T, Lubberts B, Reilly BT, Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg 2014;23:1913–21. 10.1016/j.jse.2014.08.001 [DOI] [PubMed] [Google Scholar]
- 42.Turner BS. Left handedness. BMJ 1993;307:1577–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Varkey DT, Patterson BM, Creighton RA, Spang JT, Kamath GV. Initial medical management of rotator cuff tears: a demographic analysis of surgical and nonsurgical treatment in the United States Medicare population. J Shoulder Elbow Surg 2016;25:e378–85. 10.1016/j.jse.2016.05.001 [DOI] [PubMed] [Google Scholar]
- 44.Wendelboe AM, Hegmann KT, Gren LH, Alder SC, White GL, Lyon JL. Associations between body-mass index and surgery for rotator cuff tendinitis. J Bone Joint Surg Am 2004;86:743–7. 10.2106/00004623-200404000-00011 [DOI] [PubMed] [Google Scholar]
- 45.Wylie JD, Suter T, Potter MQ, Granger EK, Tashjian RZ. Mental health has a stronger association with patient-reported shoulder pain and function than tear size in patients with full-thickness rotator cuff tears. J Bone Joint Surg Am 2016;98:251–6. 10.2106/JBJS.O.00444 [DOI] [PubMed] [Google Scholar]
- 46.Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116–20. 10.1016/j.jse.2009.04.006 [DOI] [PubMed] [Google Scholar]
- 47.Yanik EL, Colditz GA, Wright RW, Saccone NL, Evanoff BA, Jain NB, et al. Risk factors for surgery due to rotator cuff disease in a population-based cohort. Bone Joint J 2020;102-B:352–9. 10.1302/0301-620X.102B3.BJJ-2019-0875.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]


