Abstract
In many types of cancer, microRNAs (miRs) are aberrantly expressed. The aim of this study was to explore the prognostic impact of miR-17-5p and miR-20a-5p in colon cancer. Tumor tissue from 452 stage I-III colon cancer patients was retrospectively collected and tissue microarrays constructed. miR-17-5p and miR-20a-5p expression was evaluated by in situ hybridization and analyzed using digital pathology. Cell line experiments, using HT-29 and CACO-2, were performed to assess the effect of miR-17-5p and miR-20a-5p over expression on viability, invasion and migration. In multivariate analyses, high miR-17-5p expression in tumor (HR = 0.43, CI 0.26–0.71, p < 0.001) and high expression of miR-20a-5p in tumor (HR = 0.60, CI 0.37–0.97, p = 0.037) and stroma (HR = 0.63, CI 0.42–0.95, p = 0.027) remained independent predictors of improved disease-specific survival. In cell lines, over expression of both miRs resulted in mitigated migration without any significant effect on viability or invasion. In conclusion, in stage I-III colon cancer, high expression of both miR-17-5p and miR-20a-5p are independent predictors of favorable prognosis.
Subject terms: Cancer, Gastrointestinal cancer, Tumour biomarkers
Introduction
Colon cancer is the 4th most and 5th most common cause of cancer and cancer related deaths, respectively1. In 2020, it is estimated that 1 150 000 patients experienced a de novo colon cancer and that 575 000 succumbed to their disease. Despite improved diagnostics and treatment, and decreasing incidence, the mortality of colon cancer remains high. To further tailor the treatment of these patients, the development of novel prognostic and predictive biomarkers is important2,3.
MicroRNAs (miRs or miRNAs) are short, non-coding RNAs, approximately 22 nucleotides long. They regulate gene expression at the post-transcriptional level. An estimated 30% of human genes are regulated by miRs4. miRs influence diverse biological mechanisms including apoptosis, growth, differentiation and proliferation5. In cancer, miRs act as both oncogenes and tumor suppressors6. The miR-17 ~ 92 cluster, located at chromosomal locus 13q31.3, comprises six tandem stem-loop hairpin structures that yield six mature miRs (miR-17, miR-18a, miR-19a, miR-19b, miR-20a and miR-92a)7. There are two miR-17 ~ 92 cluster paralogs in mammals: miR-106b ~ 25 located on chromosome 7 and miR-106a ~ 363 located on the X-chromosome, comprising an additional 6 and 3 mature miRs. Collectively, these 15 mature miRs are grouped into four families, namely the miR-17, miR-18, miR-19 and miR-928. The polycistronic structure of miR cluster genes differs from most protein coding genes, as multiple miRs can be produced within a single pri-miR transcript. Each of these can act independently9. miR-17 ~ 92 is predominantly related to cell cycle regulation. In normal development it is involved in lung and heart maturation and hematopoiesis, where it promotes cell proliferation and survival10. The cluster was first discovered in 2005, when it was found to act with c-MYC to promote tumorigenesis in B-cell lymphomas11. Over expression of the miR-17 ~ 92 cluster has been observed in multiple tumor types including hematological malignancies (B-cell lymphomas) and solid tumors (breast, lung, CRC, pancreas and prostate)11,12.
The miR-17 family comprise miRs 17 and 20a in the miR-17 ~ 92 cluster, 106a and 20b in the miR-106a ~ 363 cluster and 106b and 93 in the miR-106b ~ 25 cluster8. Hence, miR-17 and miR-20a are the only members of the miR-17 family situated in the miR-17 ~ 92 cluster. Of interest, the expression level of mature miRs belonging to the same cluster are not equivalent13. An early discovery was that c-MYC activates expression of the miR-17 ~ 92 cluster by binding directly to its locus on chromosome 13. c-MYC also targets transcription factor E2F1, promoting cell cycle progression. E2F1 is negatively regulated by both miR-17 and miR-20a. Thus, on one side c-MYC activates members of the E2F family of transcription factors, and on the other side limits their translation14. Subsequent studies identified that miR-17-5p and miR-20a-5p expression is suppressed by p53 and NKX3.1, stimulated by MXI1 and STAT, and that their expression suppress known regulators of cell death, cell cycle regulation, hypoxia, angiogenesis, and proliferation15. In gastrointestinal cancers (gastric, CRC and HCC), miR-17 has been related to increased cell proliferation, migration and invasion and reduced overall survival16. In contrast, miR-17 was shown to act as a tumor suppressor in breast-, cervical- and prostate cancer17–19. miR-20a regulates cell proliferation and cancer progression, and is dysregulated in both solid and hematopoietic cancers15. miR-20a was related to poor survival in lung- and gastric cancer, among others20,21. Whereas in oral squamous cell carcinoma and hepatocellular carcinoma, miR-20a acted as a tumor suppressor22,23.
Previous studies in gastrointestinal cancers reported that both miR-17 and miR-20a frequently are over expressed and that miR-17 was associated with an unfavorable prognosis16,24. However, to our knowledge these studies included patients with advanced disease, combined separate entities such as colon and rectal adenocarcinoma and did not distinguish between expression in tumor epithelial cells and tumor stroma. Therefore, we explore the prognostic impact of miR-17-5p and miR-20a-5p expression in tissue from colon cancer patients treated with curative intent. We supplement our results with functional experiments in select early-stage colon cancer cell lines. And hypothesize that these miRs are clinically relevant biomarkers in localized colon cancer.
Results
Patient characteristics
The patient characteristics have previously been reported25. Briefly, 452 patients were included in the study. There was a minor female predominance (53.8% vs 46.2%), and the median age at surgery was 74 years (range 30–94). Seventy-two (15.9%), 219 (48.5%) and 161 (35.6%) patients were diagnosed with pTNM stage I-III, respectively. Median follow-up of survivors was 173 months. At the end of follow-up, 119 patients had recurrent disease and 313 patients were dead, either due to colon cancer (108) or other causes (205).
Expression of miR-17-5p and miR-20a-5p and their correlations
miR-17-5p and miR-20a-5p were mostly expressed in tumor epithelial cells and to a varying degree in stromal cells including spindle shaped cells (likely fibroblasts, endothelial cells and vascular smooth muscle cells) and immune cells (Fig. 1).
Figure 1.
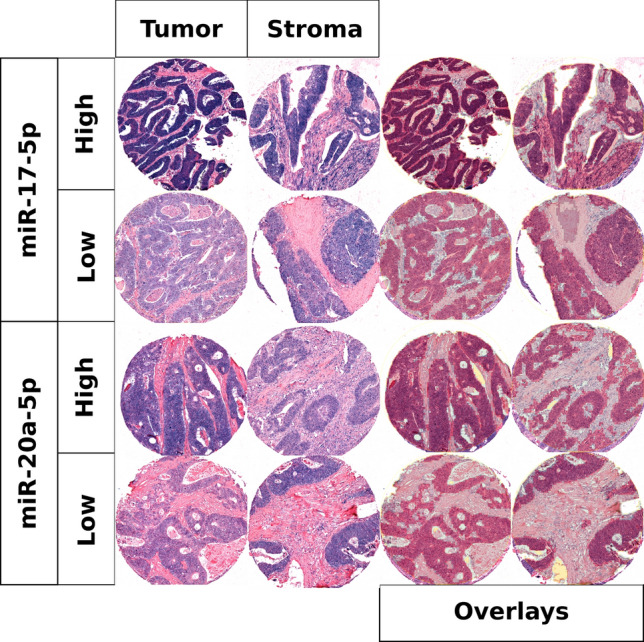
High and low scores for miR-17-5p and miR-20a-5p in tumor and stroma with and without overlays.
Correlations between miRs and clinicopathological variables are presented in Table 1. High expression of both miR-17-5p and miR-20a-5p in tumor tissue was associated with well and moderately differentiated tumors. In addition, miR-20a-5p in tumor was associated with cancers of the right colon. Between-miR correlations were as follows: miR-17-5p in tumor was correlated with mir-17-5p in stroma (r = 0.27), miR-20a-5p in tumor (r = 0.52) and stroma (r = 0.17); miR-17-5p in stroma was correlated to miR-20a-5p in tumor (r = 0.16) and stroma (r = 0.37); miR-20a-5p in tumor was correlated with miR-20a-5p in stroma (r = 0.65).
Table 1.
Dichotomized miR-17-5p and miR-20a-5p in tumor and stroma and their distribution over and correlation with clinicopathological variables (chi-square and Fisher’s exact tests).
| miR-17-5p in tumor | miR-17-5p in stroma | miR-20a-5p in tumor | miR-20a-5p in stroma | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | High | p | Low | High | p | Low | High | p | Low | High | p | |
| Age | 0.115 | 0.947 | 0.742 | 0.472 | ||||||||
| ≤ 65 | 80 | 27 | 26 | 83 | 76 | 31 | 27 | 80 | ||||
| > 65 | 213 | 110 | 83 | 252 | 244 | 89 | 72 | 266 | ||||
| Gender | 0.547 | 1.000 | 0.930 | 0.665 | ||||||||
| Female | 154 | 77 | 59 | 181 | 170 | 65 | 51 | 189 | ||||
| Male | 139 | 60 | 50 | 154 | 150 | 55 | 48 | 157 | ||||
| Weight_loss | 0.027 | 0.818 | 0.055 | 0.507 | ||||||||
| < 10% | 151 | 81 | 62 | 180 | 172 | 71 | 52 | 194 | ||||
| ≥ 10% | 70 | 19 | 22 | 71 | 73 | 16 | 23 | 68 | ||||
| ECOG_status | 0.827 | 0.093 | 0.526 | 0.066 | ||||||||
| 0 | 150 | 76 | 47 | 185 | 163 | 68 | 45 | 188 | ||||
| 1 | 100 | 41 | 45 | 102 | 106 | 38 | 42 | 104 | ||||
| 2 | 35 | 16 | 14 | 39 | 42 | 11 | 9 | 45 | ||||
| 3 | 6 | 2 | 3 | 5 | 7 | 1 | 3 | 5 | ||||
| Site | 0.101 | 0.133 | 0.023 | 0.150 | ||||||||
| Sigmoid | 158 | 58 | 48 | 177 | 165 | 56 | 40 | 183 | ||||
| Transversum | 42 | 20 | 16 | 49 | 53 | 11 | 17 | 48 | ||||
| Left | 12 | 6 | 3 | 16 | 16 | 5 | 7 | 14 | ||||
| Right | 79 | 52 | 42 | 90 | 83 | 48 | 34 | 99 | ||||
| pStage | 0.085 | 0.006 | 0.306 | 0.165 | ||||||||
| 1 | 42 | 28 | 10 | 61 | 45 | 24 | 10 | 60 | ||||
| 2 | 139 | 70 | 48 | 168 | 160 | 57 | 49 | 170 | ||||
| 3 | 112 | 39 | 51 | 106 | 115 | 39 | 40 | 116 | ||||
| Hist_grade | 0.015 | 0.463 | 0.026 | 0.722 | ||||||||
| Well | 22 | 13 | 10 | 26 | 20 | 14 | 6 | 29 | ||||
| Moderate | 203 | 111 | 81 | 240 | 230 | 93 | 74 | 251 | ||||
| Poor | 59 | 12 | 14 | 61 | 61 | 12 | 15 | 59 | ||||
| Undifferentiated | 3 | 1 | 0 | 4 | 3 | 0 | 1 | 2 | ||||
| Vasc + | 0.281 | 0.323 | 0.131 | 0.066 | ||||||||
| No | 128 | 60 | 49 | 146 | 149 | 45 | 43 | 152 | ||||
| Yes | 14 | 3 | 7 | 11 | 17 | 1 | 8 | 10 | ||||
| Resection margins | 0.234 | 0.255 | 0.571 | 0.609 | ||||||||
| 0 mm | 25 | 4 | 12 | 19 | 24 | 5 | 6 | 25 | ||||
| < 1 mm | 31 | 10 | 9 | 33 | 31 | 11 | 9 | 33 | ||||
| 1-2 mm | 22 | 11 | 6 | 29 | 22 | 13 | 4 | 31 | ||||
| 2-10 mm | 76 | 38 | 28 | 89 | 82 | 35 | 26 | 91 | ||||
| 10-50 mm | 94 | 52 | 34 | 117 | 111 | 38 | 39 | 113 | ||||
| > 50 mm | 30 | 15 | 15 | 31 | 33 | 13 | 11 | 35 | ||||
ECOG, Eastern cooperative oncology group, pStage, pathological stage, Hist_grade, histological grade, Vasc + , vascular infiltration.
Statistically significant values in bold.
Cell line experiments
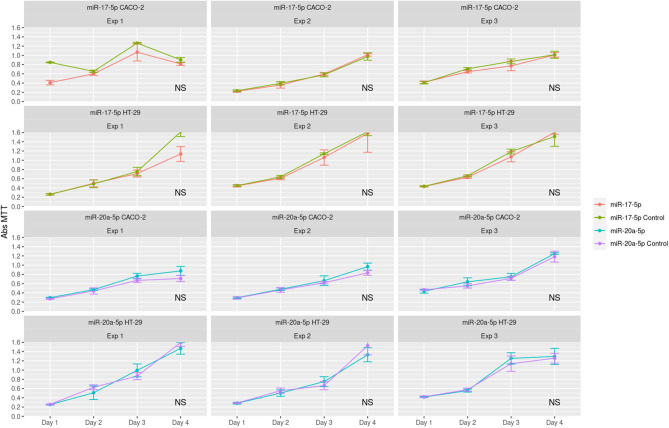
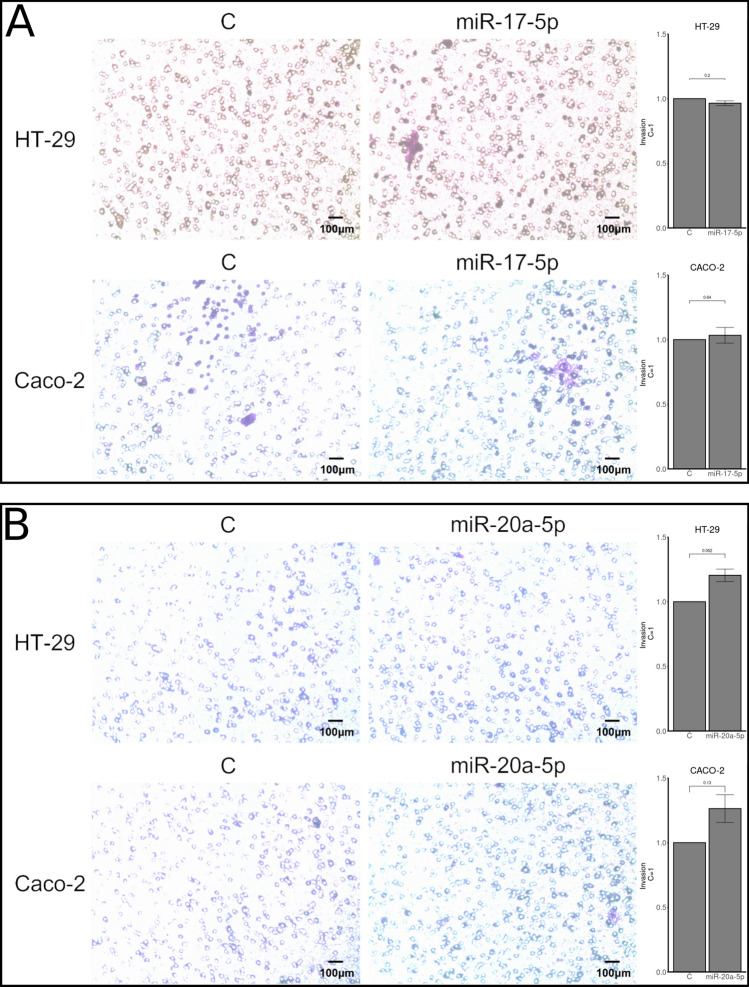
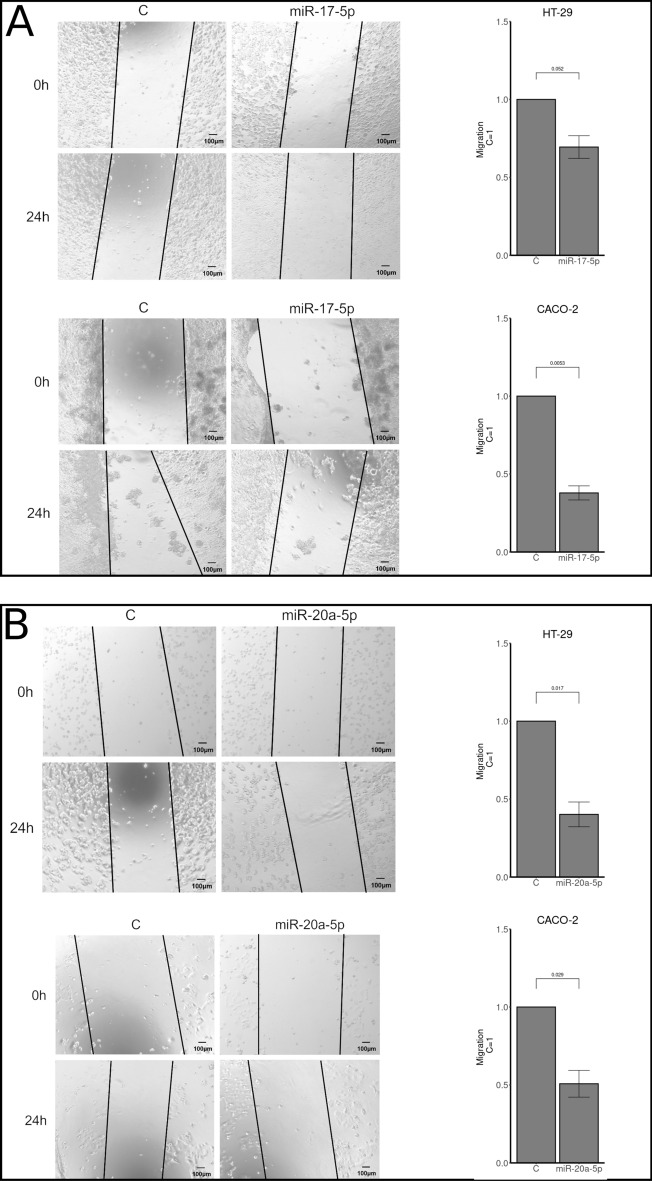
HT-29 and CACO-2 cell lines were tested for viability using MTT assays and invasion using transwell assays. No differences in viability or invasion were observed when either miR-17-5p or miR-20a-5p was over expressed compared to controls (Figs. 2 and 3). For migration analyses, using wound healing assays, reduced migration rates after miR-17-5p and miR-20a-5p over expression was observed for both cell lines (Fig. 4). These findings were statistically significant for both miR-17-5p (p < 0.001) and miR-20a-5p (p = 0.029) in the CACO-2 cell line. For the HT-29 cell line, the results for miR-20a-5p were statistically significant (p = 0.017) and borderline significant for miR-17-5p (p = 0.052).
Figure 2.
MTT assays comparing viability in cells transfected with either miR-17-5p (rows 1 and 2) or miR-20a-5p (rows 3 and 4) with control in the CACO-2 (rows 1 and 3) and HT-29 (rows 2 and 4) cell lines.
Figure 3.
Transwell assays as measures of invasion/migration in CACO-2 and HT-29 cell lines transfected with miR-17-5p (panel A) or miR-20a-5p (panel B). Results are plotted as a mean of 3 experiments + /− SEM and relative to control (C = 1).
Figure 4.
Wound healing assays as measures of migration in CACO-2 and HT-29 cell lines transfected with miR-17-5p (panel A) or miR-20a-5p (panel B). Results are plotted as a mean of 3 experiments + /− SEM and relative to control (C = 1).
Univariate analyses
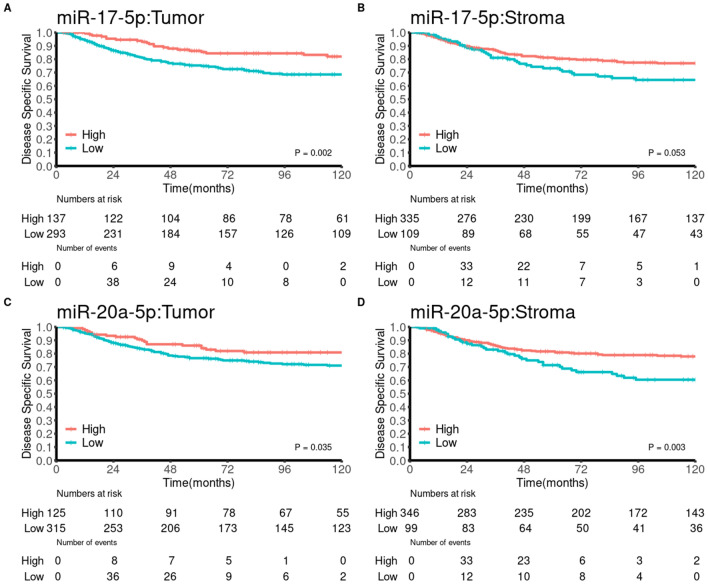
Univariate survival analyses of clinicopathological variables were presented previously25. In brief, age, weight loss, pathological stage, histological grade, vascular infiltration, and resection margins were significant indicators of DSS. Univariate analyses of the investigated markers are presented in Table 2 and Fig. 5. High miR-17-5p expression in tumor was a significant indicator of DSS (p = 0.002), while high miR-20a-5p expression was a significant indicator of DSS in tumor (p = 0.035) and stroma (p = 0.003).
Table 2.
Univariate analyses of miR-17-5p and miR-20a-5p in tumor and stroma (log-rank, n = 452).
| N | 5Y | M | HR (95% CI) | p | |
|---|---|---|---|---|---|
| miR-17-5p in tumor | 0.002 | ||||
| Low | 293(65) | 75 | NA | 1.000 | |
| High | 137(30) | 86 | NA | 0.48(0.32–0.72) | |
| Missing | 22(5) | ||||
| miR-17-5p in stroma | 0.053 | ||||
| Low | 109(24) | 73 | NA | 1.000 | |
| High | 335(74) | 81 | NA | 0.67(0.42–1.05) | |
| Missing | 8(2) | ||||
| miR-20a-5p in tumor | 0.035 | ||||
| Low | 315(70) | 77 | NA | 1.000 | |
| High | 125(28) | 86 | NA | 0.6(0.39–0.92) | |
| Missing | 12(3) | ||||
| miR-20a-5p in stroma | 0.003 | ||||
| Low | 99(22) | 71 | NA | 1.000 | |
| High | 346(77) | 82 | NA | 0.55(0.35–0.88) | |
| Missing | 7(2) | ||||
N, number, 5Y, 5-year survival, M, median survival, p, p-value, HR, hazard ratio, CI, confidence interval, NA, not applicable.
Statistically significant values in bold.
Figure 5.
Disease-specific survival curves for expression of miR-17-5p and miR-20a-5p using the optimal cut-offs for each marker.
Multivariate analyses
Multivariate analyses are summarized in Table 3. All significant variables from the univariate analyses were entered into the initial analyses. In the final models, high miR-17-5p expression in tumor was independently associated with favorable DSS (HR = 0.43, CI 0.26–0.71, p < 0.001), while high miR-20a-5p expression remained an independent predictor of favorable DSS in both tumor and stroma, (HR = 0.60, CI 0.37–0.97, p = 0.037) and (HR = 0.63, CI 0.42–0.95, p = 0.027), respectively.
Table 3.
Multivariate models for miR-17-5p in tumor (I) and for miR-20a-5p in tumor (II) and stroma (III), (cox proportional hazards tests, n = 452).
| I | II | III | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| miR-17-5p in tumor | ||||||
| Low | 1 | |||||
| High | 0.43(0.26–0.71) | < 0.001 | ||||
| Missing | ||||||
| miR-20a-5p in tumor | ||||||
| Low | 1 | |||||
| High | 0.60(0.37–0.97) | 0.037 | ||||
| Missing | ||||||
| miR-20a-5p in stroma | ||||||
| Low | 1 | |||||
| High | 0.63(0.42–0.95) | 0.027 | ||||
| Missing | ||||||
| Age at diagnosis | 1.03(1.01–1.05) | 0.002 | 1.03(1.01–1.05) | 0.009 | 1.02(1.01–1.04) | 0.013 |
| Differentiation | ||||||
| Well differentiated | 1 | |||||
| Moderately differentiated | 0.91(0.42–2.01) | 0.822 | ||||
| Poorly differentiated | 0.61(0.25–1.51) | 0.286 | ||||
| Undifferentiated | 7.97(1.93–32.95) | 0.004 | ||||
| pTNM | ||||||
| pTNM-stage I | 1 | 1 | 1 | |||
| pTNM-stage II | 2.32(0.89–6.03) | 0.085 | 2.18(0.85–5.58) | 0.105 | 2.16(0.84–5.55) | 0.108 |
| pTNM-stage III | 8.27(3.26–21.01) | < 0.001 | 7.85(3.16–19.55) | < 0.001 | 7.58(3.04–18.88) | < 0.001 |
p, p-value, HR, hazard ratio, CI, confidence interval, pTNM, pathological tumor-node-metastasis.
Statistically significant values in bold.
Discussion
We present results showing favorable prognosis for colon cancer patients with high expression of miR-17-5p or miR-20a-5p. Patients with high expression of miR-17-5p in tumor tissue had a 5-year DSS of 86% compared with 75% for low expression. Patients with high expression of miR-20a-5p in tumor and stromal tissue had a 5-year DSS of 86% and 82% vs 77% and 71% for low expression, respectively (Table 2 and Fig. 1). Our results diverge from previous findings in similar cohorts and highlights important considerations for future studies on miRs in gastrointestinal cancer patients.
Contrasting our findings, most previous studies in gastrointestinal cancers related high miR-17-5p expression to impaired prognosis26. However, the number of high-quality studies exploring the prognostic value of miR-17-5p expression in localized colon cancer is limited. A meta-analysis from 2018, investigated the prognostic impact of miR-17-5p expression in gastrointestinal cancers16. Pooled analyses suggested that high expression of miR-17-5p predicted both poor overall survival (HR = 1.86, CI 1.55–2.25, p < 0.001) and poor disease-free survival (HR = 1.43, CI 1.01–2.03, p = 0.046). Of interest, ~ half of the identified publications reported non-significant results and/or were based on miR expression in serum/plasma, all studies included patients with advanced disease and several distinct cancers were represented27. Similar to our study, three studies report the prognostic impact of miR-17-5p expression in tissue from CRC patients27–29. Contrary to our study, these studies included stage I-IV patients, used overall survival as endpoint and did not distinguish between colon and rectal cancer. Both Ma and Fang et al. reported that high levels of miR-17-5p in tumor tissue, identified using ISH, was associated with impaired survival in Asian CRC patients28,29. Diaz et al. did not observe a survival difference in European patients27. This latter observation may suggest a demographic difference in CRC patients as proposed by others30. Moreover, although all three studies reported a similar percentage of miR-17-5p high patients, both Ma and Fang et al. observed increased miR-17-5p expression in stage III and IV patients28,29. Similar to our study, Diaz et al. observed a decline in miR-17-5p expression with increasing stage27. These results further corroborate the notion of a demographic difference for these biomarkers. In addition, neither Ma and Fang nor Diaz properly address the potential confounder introduced with patients with metastatic disease or rectal cancer.
Several previous studies stated that miR-20a-5p is upregulated both in feces and tumor tissue from colon cancer patients 12,31,32. In our study, we observed that high expression of miR-20a-5p, both in tumor and stromal tissue, was related to a favorable disease-specific survival. Our findings contradict a recent meta-analysis assessing the efficacy of miR-20a as a diagnostic and prognostic biomarker for colorectal cancer24. The meta-analysis, comprised of thirty-two studies, six including colon cancer patients only, concluded that miR-20a-5p expression was associated with impaired overall survival. However, similar to studies in miR-17-5p, several issues including differences in methodology, patient demographics and study endpoints precludes direct comparison with our study. Of interest, Signs et al. explored the impact of miR-20a-5p expression in the stromal compartment of colitis-associated cancer. They observed that stromal miR-20a-5p expression was higher in normal colon compared to a colitic or cancerous colon. Further, low levels of miR-20a-5p correlated with low levels of the inflammatory and oncogenic chemokine CXCL8 secreted by stromal fibroblasts. Stromal downregulation of miR-20a expression appeared to occur prior to epithelial upregulation. This suggests that downregulated miR-20a-5p expression in fibroblasts in the colitic field is responsible for the upregulation of CXCL8 responsible for tumorigenesis in colitis-associated cancer33. These findings are in line with our results, where high stromal expression of miR-20a-5p correlates to better outcome for the patients.
To further elucidate the role of miR-17-5p and miR-20a-5p, we investigated their functional aspects in two colon cancer cell lines. HT-29 and CACO-2 are known to form low-grade/early-stage cancer when grown in nude mice and are thus likely representative of localized colon cancer34,35. Interestingly, over expression of the miRs did not impact viability or invasion and mitigated migration in both cell lines. These results strengthen our findings in patients with localized colon cancer, where over expression of miR-17-5p and miR-20a-5p predicted better outcome for the patients. Corroborating our findings, several groups observed that over expression and/or suppression of miR-17-5p and miR-20a-5p subsequently mitigated and promoted migration in colon cancer cells36,37. Of particular interest, Ast et al. investigated the role of miR-17-5p and tumor-stromal cell interaction in the setting of CRC carcinogenesis38. By co-culturing colon cancer cells and colon fibroblasts transfected with a miR-17 mimic, they noticed significantly reduced cell invasion. Increased expression of miR-17 also significantly reduced the invasive activity of fibroblasts. However, other groups report that over expression of miR-17-5p and miR-20a-5p increases proliferation, migration and invasion in colon cancer cell lines, thus highlighting the complex role of these miRs in distinct settings28,29,39.
The conflicting results hamper both interest and implementation of use of miR-17-5p and miR-20a-5p as biomarkers in colon cancer. Nevertheless, according to clinicaltrials.gov, Wu Song and co-workers are validating a signature of six miRs to predict chemotherapy response in stage II colon cancer40. This trial is based on their previous work41, but no results are as of yet presented from their trial. Regardless of the outcome from the ongoing validation by Wu Song, our data indicate that positive results need to be validated and not automatically extrapolated to other demographic groups.
Conclusion
In conclusion, we have shown that high expression of miR-17-5p in tumor tissue and high expression of miR-20a-5p in both tumor and stroma are independent indicators of favorable disease-specific survival for localized colon cancer. Our findings contradict previous studies in colorectal cancer, and highlights that potential differences in methodology, patient demographics and endpoints may highly influence the prognostic value of these biomarkers. Further, although data from several pre-clinical studies and our cell line studies corroborates our findings, contrasting results exists also in this domain. Due to these contradictions, prospective trials resolving these issues have to be conducted before clinical implementation of miR-17-5p and miR-20a-5p as prognostic or predictive biomarkers in colon cancer can be considered.
Materials and methods
Study population
Patients who underwent radical surgery for colon cancer, in various hospitals in Northern Norway from 1998–2007, were eligible for inclusion. Initially, 861 patients were identified. Of these, 409 patients were excluded, mainly due to metastatic disease/prior malignancy within the last 5 years before diagnosis, missing tissue blocks/inadequate tissue for TMA construction or miscoding (mainly rectal cancer). Hence, 452 patients were included in the study. Follow-up was completed December 1, 2017. Detailed information about the study population was previously published25.
Tissue Microarray construction
All colon cancer cases were reviewed by two pathologists, and the most representative areas of tumor without necrosis were selected. A 0.6 mm-diameter stylet was used to sample a total of 4 cores securing both tumor and stroma from each included patient. The TMAs were assembled using a tissue-arraying instrument (Beecher Instruments, Silver Springs, MD, USA). The detailed methodology has previously been reported42.
In situ hybridization (ISH)
The microRNA in situ hybridization method was performed on the Ventana Discovery Ultra platform for IHC and ISH. The protocol was developed by Roche, (Tucson, USA), based on the manual protocol previously published by Jorgensen et al.43.
Double‐DIG labeled miRCURY LNA detection probes and control probes from Exiqon (Exiqon AS, Denmark) was used to define the expression level of miR-20a-5p and miR-17-5p in colon cancer FFPE tissue. Detection kits and buffers purchased from Roche gave the chromogenic visualization of the microRNAs.
Slides were baked at 60 °C overnight, and then transferred to the Discovery Ultra for ISH staining. Sections were deparaffinized at 68 °C for three cycles in Ventana EZ buffer. Heat retrieval was performed at 95 °C with Discovery Cell Conditioning Solution (CC1) for 40 min to make access for the probes. Optimized concentrations of probe controls and target miR probes were manually applicated, miR-20a-5p, 50 nM, and miR-17-5p, 20 nM. The hybridization reaction was carried out for 60 min at 54 °C for miR-17-5p and 40 °C for miR-20a-5p followed by two stringency washes with 2.0X SSC buffer. Possible unspecific bindings were blocked with AB blocking solution for 16 min. Alkaline phosphatase-conjugated anti DIG (Anti-DIG-AP) was incubated for 20 min for immunologic detection. Substrate enzymatic reactions were carried out with NBT/BCIP for 60–120 min to give a blue precipitate. The slides were counterstained with Nuclear Fast Red for contrast staining. Slides were dehydrated through an increasing gradient of ethanol solutions to xylene and mounted with Histokitt mounting medium.
Good sensitivity level of the ISH method and minimal RNA degradation in tissue was confirmed by U6, snRNA control probe at a concentration of 1.5 nM. 10 nM scramble miR negative control indicated no unspecific staining from reagents or tissues. The level of microRNA expression in other tissues than colon cancer was confirmed by a TMA multi tissue control. Optimizations regarding temperatures, times, and concentrations were done for each probe and reagent.
In situ hybridization scoring/QuPath
The details of the digital workflow is described thoroughly in our previous paper25. In brief, TMA slides were digitized and processed in QuPath v.0.1.3 according to Bankhead et al.44. Tissue within each TMA core was identified and tiled. Image features were used to train a Random Forest model. Each tile was classified as either tumor, stroma, necrosis or other. After classification, tiles were converted into continuous areas and the mean intensity of miR-17-5p and miR-20a-5p within tumor and stroma was calculated. The scripts used to process the TMAs are included in the supplementary file.
All possible dichotomized cut-offs were evaluated. For any subsequent analyses, the optimal cut-off was chosen.
Cell line experiments
Cell cultures
The functional aspects of miR-17-5p and miR-20a-5p were tested in two colon cancer cell lines: CACO-2 (ATCC HTB-37) and HT-29 (ATCC HTB-38) both derived from colon adenocarcinoma. They have been authenticated and recently tested negative for mycoplasma contamination. The cell lines were tested for viability, migration and invasion in the absence and presence of miR-17-5p and miR-20a-5p as previously described by Stoen et al.45,46. The most important steps of each assay are referred below.
Cell culture and transfection
Cells were transiently transfected with either 10 µM has-miR-17-5p Pre-miR miRNA Precursor (catalog# PM12412, Thermo Fisher Scientific, USA) or has-miR-20a-5p Pre-miR miRNA Precursor (catalog# AM17100, Thermo Fisher Scientific, USA), alongside the Cy3 Dye-Labeled Pre-miR Negative Control #1 (catalog# AM17120, Thermo Fisher Scientific, USA) using the transfection reagent Lipofectamine RNAiMAX (catalog#13,778,075, Thermo Fisher Scientific, USA). Transfected Cy3 Dye-Labeled Pre-miR Negative Control emits fluorescent light when exposed to UV-light, and using a fluorescence microscope, the transfection efficiency was estimated to 80–95%.
Viability assay
Cells were cultured in 96-well plates and incubated with 12 mM of [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide] (MTT, 5 mg/ml) (cat.# M6494, Invitrogen, OR, USA). Formazan crystals were solubilized by addition of 0,01 M HCl/SDS (cat.# 28,312, Thermo Scientific, IL, USA) and the absorbance was measured in the CLARIOstar plate reader (BMG Labtech, Ortenberg, Germany) at 570 nm.
Migration/wound healing assay
Cells were grown in a 24-well plate, washed with PBS and incubated in a serum free medium with mitomycin C (10 µg/L) to avoid cell proliferation. The cells were “wounded” using a 200 µl sterile pipette tip and then washed to remove detached cells and debris. After 4 h the cells were transfected. To measure wound healing in controls and transfected cells, photographs of the same areas of the wound were taken at 0 and 24 h. Images were captured using a Nikon Eclipse TS100 inverted optical microscope and analyzed by Micrometrics SE Premium 4 software. Areas occupied by migrating cells after 24 h were calculated by subtracting the background levels at 0 h.
Invasion assay
Cells were seeded in ThincertR chambers (Greiner Bio-one, Kremsmünster, Austria) with polyethylene terephthalate membranes (8 mm pore size) pre-coated with 50 mL of phenol red-free Matrigel (Gibco). These chambers were placed in 24-well plates containing culture medium with 10% FBS in the lower chamber. Cells in the upper chambers were transfected and incubated for 48 h at 37 °C. The chambers were washed thoroughly with 10 mM PBS, fixed in 4% paraformaldehyde for 30 min, and stained with 0.2% crystal violet for 10 min. Non-invading cells, from the membrane upper surface, were removed using a cotton swab. The membranes containing the invaded cells (under the membrane surface), were photographed. Images of three random microscope fields were captured in duplicate, using an inverted optical microscope Nikon Eclipse TS100. The areas of cell invasion were determined by Image J software.
Statistical methods
Statistical tests were performed in Rstudio 2021.09.0 build 351 (RStudio PBC) using R version 4.0.4. DSS (disease-specific survival) was defined as the interval from surgery to the time of colon cancer death. Before analyses, expression of all miRs were rescaled to a range between 0 and 1 using max–min scaling. For univariate analyses, the Kaplan–Meier method was used to visualize associations between molecular marker expression and survival. The log-rank test was used to assess the statistical significance of the differences between the survival curves. Multivariate analyses were performed using a backward conditional Cox regression analysis with a probability for stepwise entry and removal at 0.05 and 0.10, respectively. A p-value < 0.05 was considered statistically significant.
Ethics declaration
The study was conducted according to the guidelines of the Declaration of Helsinki, and was approved by the Regional Committee for Medical and Health Research Ethics North (REK Nord, protocol ID: 2011/2151). The need for informed consent was waived by REK Nord due to the retrospective nature of the study. The reporting of clinicopathological variables, survival data and biomarker expression was conducted in accordance with the REMARK guidelines47.
Supplementary Information
Acknowledgements
We would like to thank Magnus L Persson for preparing the TMA-slides.
Author contributions
All authors contributed to study design. H.S collected the clinical data. L.T.B collected and revised the pathological specimens. M.I.P conducted the ISH experiments. A.P.L conducted the cell line experiments. H.S, T.K.K and S.A analyzed and interpreted the data. H.S and T.K.K wrote the manuscript. All authors revised the manuscript.
Funding
Open Access funding provided by UiT The Arctic University of Norway. The publication charges for this article have been funded by a grant from the publication fund of UiT The Arctic University of Norway.
Data availability
Data will be shared upon reasonable request to the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-11090-2.
References
- 1.Global Cancer Observatory. Available at: https://gco.iarc.fr/. (Accessed: 12th January 2021)
- 2.Edwards BK, et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544–573. doi: 10.1002/cncr.24760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitzpatrick-Lewis D, et al. Screening for colorectal cancer: A systematic review and meta-analysis. Clin. Colorectal Cancer. 2016;15:298–313. doi: 10.1016/j.clcc.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Lewis BP, Burge CB, Bartel DP. Conserved seed pairing, often flanked by adenosines, indicates that thousands of human genes are microRNA targets. Cell. 2005;120:15–20. doi: 10.1016/j.cell.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 5.Bartel DP. MicroRNAs: Target recognition and regulatory functions. Cell. 2009;136:215–233. doi: 10.1016/j.cell.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang B, Pan X, Cobb GP, Anderson TA. microRNAs as oncogenes and tumor suppressors. Dev. Biol. 2007;302:1–12. doi: 10.1016/j.ydbio.2006.08.028. [DOI] [PubMed] [Google Scholar]
- 7.Tanzer A, Stadler PF. Molecular evolution of a microRNA cluster. J. Mol. Biol. 2004;339:327–335. doi: 10.1016/j.jmb.2004.03.065. [DOI] [PubMed] [Google Scholar]
- 8.Mendell JT. miRiad roles for the miR-17-92 cluster in development and disease. Cell. 2008;133:217–222. doi: 10.1016/j.cell.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olive V, Jiang I, He L. Mir-17-92, a cluster of miRNAs in the midst of the cancer network. Int. J. Biochem. Cell Biol. 2010;42:1348–1354. doi: 10.1016/j.biocel.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ventura A, et al. Targeted deletion reveals essential and overlapping functions of the miR-17∼92 family of miRNA clusters. Cell. 2008;132:875–886. doi: 10.1016/j.cell.2008.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He L, et al. A microRNA polycistron as a potential human oncogene. Nature. 2005;435:828–833. doi: 10.1038/nature03552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volinia S, et al. A microRNA expression signature of human solid tumors defines cancer gene targets. Proc. Natl. Acad. Sci. U.S.A. 2006;103:2257–2261. doi: 10.1073/pnas.0510565103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu J, et al. Human microRNA clusters: Genomic organization and expression profile in leukemia cell lines. Biochem. Biophys. Res. Commun. 2006;349:59–68. doi: 10.1016/j.bbrc.2006.07.207. [DOI] [PubMed] [Google Scholar]
- 14.O’Donnell KA, Wentzel EA, Zeller KI, Dang CV, Mendell JT. c-Myc-regulated microRNAs modulate E2F1 expression. Nature. 2005;435:839–843. doi: 10.1038/nature03677. [DOI] [PubMed] [Google Scholar]
- 15.Mogilyansky E, Rigoutsos I. The miR-17/92 cluster: A comprehensive update on its genomics, genetics, functions and increasingly important and numerous roles in health and disease. Cell Death Differ. 2013;20:1603–1614. doi: 10.1038/cdd.2013.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang Z, et al. Prognostic value of miR-17-5 p in gastrointestinal cancers: a systematic review and meta-analysis. Onco. Targets. Ther. 2018;11:5991–5999. doi: 10.2147/OTT.S157670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fan M, Sethuraman A, Brown M, Sun W, Pfeffer LM. Systematic analysis of metastasis-associated genes identifies miR-17-5p as a metastatic suppressor of basal-like breast cancer. Breast Cancer Res. Treat. 2014;146:487–502. doi: 10.1007/s10549-014-3040-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei Q, Li Y-X, Liu M, Li X, Tang H. MiR-17-5p targets TP53INP1 and regulates cell proliferation and apoptosis of cervical cancer cells. IUBMB Life. 2012;64:697–704. doi: 10.1002/iub.1051. [DOI] [PubMed] [Google Scholar]
- 19.Ottman R, Levy J, Grizzle WE, Chakrabarti R. The other face of miR-17-92a cluster, exhibiting tumor suppressor effects in prostate cancer. Oncotarget. 2016;7:73739–73753. doi: 10.18632/oncotarget.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu X, Zhu S, Tao Z, Ye S. High circulating miR-18a, miR-20a, and miR-92a expression correlates with poor prognosis in patients with non-small cell lung cancer. Cancer Med. 2018;7:21–31. doi: 10.1002/cam4.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang M, et al. Circulating miR-17-5p and miR-20a: Molecular markers for gastric cancer. Mol. Med. Rep. 2012;5:1514–1520. doi: 10.3892/mmr.2012.745. [DOI] [PubMed] [Google Scholar]
- 22.Chang CC, et al. MicroRNA-17/20a functions to inhibit cell migration and can be used a prognostic marker in oral squamous cell carcinoma. Oral Oncol. 2013;49:923–931. doi: 10.1016/j.oraloncology.2013.03.430. [DOI] [PubMed] [Google Scholar]
- 23.Fan MQ, et al. Decrease expression of microRNA-20a promotes cancer cell proliferation and predicts poor survival of hepatocellular carcinoma. J. Exp. Clin. Cancer Res. 2013;32:21. doi: 10.1186/1756-9966-32-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moody L, Dvoretskiy S, An R, Mantha S, Pan YX. The efficacy of miR-20a as a diagnostic and prognostic biomarker for colorectal cancer: A systematic review and meta-analysis. Cancers. 2019;11:1111. doi: 10.3390/cancers11081111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Selven H, Busund L-TR, Andersen S, Bremnes RM, Kilvær TK. High expression of microRNA-126 relates to favorable prognosis for colon cancer patients. Sci. Rep. 2021;11:9592. doi: 10.1038/s41598-021-87985-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huang C, Yu M, Yao X. MicroRNA-17 and the prognosis of human carcinomas: A systematic review and meta-analysis. BMJ Open. 2018;8:e018070. doi: 10.1136/bmjopen-2017-018070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Díaz R, et al. Deregulated expression of miR-106a predicts survival in human colon cancer patients. Genes Chromosom. Cancer. 2008;47:794–802. doi: 10.1002/gcc.20580. [DOI] [PubMed] [Google Scholar]
- 28.Fang L, et al. MicroRNA-17-5p promotes chemotherapeutic drug resistance and tumour metastasis of colorectal cancer by repressing PTEN expression. Oncotarget. 2014;5:2974–2987. doi: 10.18632/oncotarget.1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma Y, et al. Elevated oncofoetal miR-17-5p expression regulates colorectal cancer progression by repressing its target gene P130. Nat. Commun. 2012;3:1–12. doi: 10.1038/ncomms2276. [DOI] [PubMed] [Google Scholar]
- 30.Bovell LC, et al. The prognostic value of MicroRNAs varies with patient race/ethnicity and stage of colorectal cancer. Clin. Cancer Res. 2013;19:3955–3965. doi: 10.1158/1078-0432.CCR-12-3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ahmed FE, et al. Diagnostic microRNA markers to screen for sporadic human colon cancer in stool: I. Proof of principle. Cancer Genom. Proteomics. 2013;10:93–113. [PubMed] [Google Scholar]
- 32.Schetter AJ, et al. MicroRNA expression profiles associated with prognosis and therapeutic outcome in colon adenocarcinoma. J. Am. Med. Assoc. 2008;299:425–436. doi: 10.1001/jama.299.4.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Signs SA, et al. Stromal miR-20a controls paracrine CXCL8 secretion in colitis and colon cancer. Oncotarget. 2018;9:13048. doi: 10.18632/oncotarget.24495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.HT-29|ATCC. Available at: https://www.atcc.org/products/htb-38. (Accessed: 2nd February 2022)
- 35.Caco-2 [Caco2]|ATCC. Available at: https://www.atcc.org/products/htb-37. (Accessed: 2nd February 2022)
- 36.Kim TW, et al. MicroRNA-17–5p regulates EMT by targeting vimentin in colorectal cancer. Br. J. Cancer. 2020;123:1123–1130. doi: 10.1038/s41416-020-0940-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jiang H, et al. Quantitatively controlling expression of miR-17∼92 determines colon tumor progression in a mouse tumor model. Am. J. Pathol. 2014;184:1355–1368. doi: 10.1016/j.ajpath.2014.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ast V, et al. MiR-192, miR-200c and miR-17 are fibroblast-mediated inhibitors of colorectal cancer invasion. Oncotarget. 2018;9:35559–35580. doi: 10.18632/oncotarget.26263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xi XP, et al. MicroRNA-17 induces epithelial-mesenchymal transition consistent with the cancer stem cell phenotype by regulating CYP7B1 expression in colon cancer. Int. J. Mol. Med. 2016;38:499–506. doi: 10.3892/ijmm.2016.2624. [DOI] [PubMed] [Google Scholar]
- 40.microRNAs Tool for Stratifying Stage II Colon Cancer—Tabular View—ClinicalTrials.gov. Available at: https://clinicaltrials.gov/ct2/show/record/NCT02635087?term=mir-20&draw=2&rank=3&view=record. (Accessed: 9th February 2022)
- 41.Zhang JX, et al. Prognostic and predictive value of a microRNA signature in stage II colon cancer: A microRNA expression analysis. Lancet Oncol. 2013;14:1295–1306. doi: 10.1016/S1470-2045(13)70491-1. [DOI] [PubMed] [Google Scholar]
- 42.Bremnes RM, et al. High-throughput tissue microarray analysis used to evaluate biology and prognostic significance of the E-cadherin pathway in non-small-cell lung cancer. J. Clin. Oncol. 2002;20:2417–2428. doi: 10.1200/JCO.2002.08.159. [DOI] [PubMed] [Google Scholar]
- 43.Jørgensen S, Baker A, Møller S, Nielsen BS. Robust one-day in situ hybridization protocol for detection of microRNAs in paraffin samples using LNA probes. Methods. 2010;52:375–381. doi: 10.1016/j.ymeth.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 44.Bankhead P, et al. QuPath: Open source software for digital pathology image analysis. Sci. Rep. 2017;7:16878. doi: 10.1038/s41598-017-17204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stoen MJ, et al. High expression of miR-17–5p in tumor epithelium is a predictor for poor prognosis for prostate cancer patients. Sci. Rep. 2021;11:1–12. doi: 10.1038/s41598-021-93208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stoen MJ, et al. Overexpression of mir-20a-5p in tumor epithelium is an independent negative prognostic indicator in prostate cancer—A multi-institutional study. Cancers (Basel) 2021;13:4096. doi: 10.3390/cancers13164096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sauerbrei W, Taube SE, McShane LM, Cavenagh MM, Altman DG. Reporting recommendations for tumor marker prognostic studies (REMARK): An abridged explanation and elaboration. J. Natl Cancer Inst. 2018;110:803–811. doi: 10.1093/jnci/djy088. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be shared upon reasonable request to the corresponding author.