Abstract
Objective/Background:
The role of the sleep environment and presleep conditions that may influence adolescents’ sleep are understudied. The aims of the current study were to examine linear and nonlinear associations between the sleep environment and presleep conditions and adolescents’ daytime sleepiness and sleep/wake problems.
Method:
Participants included 313 adolescents (Mage = 17.39 years, SD = 10.38 months; 51.4% girls, 48.6% boys; 59.1% White/European American, 40.3% Black/African American) from a wide range of socioeconomic backgrounds living in the southeastern United States. Adolescents completed surveys assessing the sleep environment (e.g., light, bedding), four presleep conditions (i.e., general worries, family concerns, arousal, somatic complaints), and sleep (daytime sleepiness, sleep/wake problems).
Results:
Sleep environment disruptions and worse presleep conditions were positively associated with sleepiness and sleep/wake problems in a linear fashion. Nonlinear associations emerged such that levels of sleepiness increased rapidly between low and average levels of the sleep environment and two presleep conditions (worries, arousal); the slope leveled off between average and high levels. Moreover, linear effects of environmental disruptions, family concerns, somatic complaints, and presleep arousal on sleep/wake problems were moderated by race and/or SES, indicating that positive associations between some presleep conditions and sleep/wake problems were more pronounced for Black and lower SES youth.
Conclusions:
Results support the importance of the sleep environment and multiple presleep conditions and assessments of both linear and nonlinear effects for a better understanding of factors that may contribute to sleep. Additionally, results indicate the sleep environment and some presleep conditions may be more consequential for disadvantaged youth.
Keywords: presleep conditions, presleep arousal, sleep environment, sleep, sleepiness
Short and poor-quality sleep is common in adolescence (Gradisar et al., 2011) and has implications for numerous aspects of development, including physical and mental health, risky behaviors, and academic achievement (Shochat et al., 2014). For example, short sleep duration, poor-quality sleep, and subjective sleep problems are associated with poor school performance (Dewald et al., 2010) as well as internalizing symptoms and externalizing behaviors (Gregory & Sadeh, 2012; Shimizu et al., 2021). Daytime sleepiness also has a negative relation with adolescents’ mental health (O’Callaghan et al., 2021; Shimizu et al., 2020) and academic performance (Philbrook et al., 2018). Several biological, psychological, and societal factors contribute to sleepiness and sleep/wake problems in this developmental period (Carskadon, 2011). For instance, developmental changes in the circadian phase (Crowley et al., 2007), increased screen time and technology use (Hale & Guan, 2015), and increased academic demands (Fuligni & Hardway, 2006) contribute to later bedtimes and difficulty falling asleep, whereas school start times necessitate waking early in the morning (Carskadon, 2011). The convergence of these influences results in insufficient sleep and daytime sleepiness (Owens, 2014). However, less is known about how the sleep environment and presleep general worries, family concerns, arousal, and somatic complaints (collectively referred to as the sleep environment and presleep conditions) may contribute to sleep problems in adolescence, where the associations may be more consequential given developmental changes in sleep.
The current study examines associations between the sleep environment and presleep conditions and sleep in a community sample of adolescents. Two sleep parameters are examined including sleepiness (i.e., difficulty staying awake or falling asleep during daytime activities) and sleep/wake problems (i.e., problems initiating or maintaining sleep at night or waking in the morning). A secondary aim was the assessment of race (Black/African American, White/European American) and family socioeconomic status (SES) as moderators of these relations.
A growing body of research has found that the sleep environment is associated with sleep among children, with room temperature (i.e., too hot or cold) being the most commonly reported sleep hindrance across multiple studies (e.g., Bagley et al., 2015; Rubens et al., 2019). Noise within the home (e.g., family members talking, snoring) and outside the home (e.g., road traffic, alarms) are also common disruptions to sleep (Mayne et al., 2021; Spilsbury et al., 2016). Too much light (Ikeda et al., 2014) and the presence of screens (e.g., television, smartphones) in the bedroom are linked to greater sleep disturbances among youth (Hale & Guan, 2015). Uncomfortable bedding (Bagley et al., 2015; Ikeda et al., 2014) and sharing a bed with others may additionally disrupt youths’ sleep (Ikeda et al., 2014; Li et al., 2008). Fewer studies have considered the sleep environment more holistically (Rubens et al., 2020; Peltz et al., 2021). For example, Bagley and colleagues (2015) demonstrated that a poor sleep environment (e.g., noise, uncomfortable bed, temperature, light) was associated with sleep/wake problems and daytime sleepiness among children using a subset of the sample on which this study is built (age 10-12). In the present study, we build on the literature by examining relations between several potential sleep environment disruptions (e.g., light, noise, bedding) and sleep parameters in late adolescence.
In addition to the physical sleep environment, presleep conditions may contribute to problems sleeping. In the present investigation, four distinct conditions were considered: general worries, family concerns, arousal, and somatic complaints. Although these constructs may be associated, they are distinct, and assessment of each of them individually is likely to provide key knowledge about their relations with sleep. Prior research has shown that worry (i.e., presleep worry or general trait worry) was related to shorter sleep duration, longer sleep onset latency, and poorer sleep quality in a recent meta-analysis, although most of the examined studies utilized adult samples (Clancy et al., 2020). In addition, general presleep worries were associated with greater sleep/wake problems and daytime sleepiness among children (Bagley et al., 2015). Yet only a few studies have examined presleep worries in adolescence, a unique developmental period characterized by poor sleep and increased stress (Owens, 2014), and results from these studies were inconclusive (Bartel et al., 2015). Contributing to this literature, we examined relations between general presleep worries (about school, friends, family, kids, or other worries) and sleep in adolescence.
Although most existing research has not examined the content of presleep worries, family stressors may lead youth to worry, disrupting the sense of security necessary to facilitate sleep (Dahl, 1996). For instance, parental problem drinking is associated with children’s emotional insecurity (Keller et al., 2011), as well as with shorter and poorer quality sleep among children (Kelly & El-Sheikh, 2019). Furthermore, parents’ marital conflict has been linked with short sleep duration, poor sleep quality, and greater daytime sleepiness (Kelly & El-Sheikh, 2011). Characteristics of the parent-child relationship, including parent-child conflict (Kelly et al., 2014), closeness (Bell & Belsky, 2008), and parental acceptance (Zeringue et al., 2021), have also been found to relate to adolescents’ sleep. Thus, presleep family concerns (i.e., worries about the parent-child relationship, parents’ marital relationship, and parents’ drinking) may be particularly detrimental to youths’ sleep, and was examined as an individual construct.
Presleep arousal (Yeh et al., 2015), a related yet distinct construct from worries, encompasses cognitive (e.g., being unable to stop thinking) and physiological processes (e.g., rapidly beating heart) experienced while attempting to fall asleep (Gregory et al., 2008). Among adults, presleep arousal is robustly associated with greater sleep/wake problems (e.g., Schneider et al., 2019). The smaller number of investigations with youth indicate that such arousal is associated with sleep disturbances in community samples of children (Gregory et al., 2008; Heath et al., 2018), as well as youth with anxiety disorders (Alfano et al., 2010). However, studies examining associations with daytime sleepiness are lacking. Building on this small literature, we assessed the associations between presleep arousal, indicated by cognitive and physiological arousal, and sleep.
Moreover, not much is known about relations between somatic complaints before or during sleep and sleep in adolescence. Somatic symptoms throughout the day and chronic pain are associated with sleep difficulties in youth (Norell-Clarke & Hagquist, 2018; Palermo et al., 2007), yet a smaller body of research has addressed nighttime somatic complaints that may keep youth awake. We extend existing evidence by testing relations between presleep somatic complaints (e.g., pain, stomachache, headache) and sleep.
The vast majority of the literature between sleep and other domains of functioning has examined linear relations. Assessment of linear relations assumes that rate of change in the outcomes is the same across all levels of the predictors (Cohen et al., 2003). However, the rate of change in sleep may not be the same across all levels of sleep environment disruptions or presleep conditions. A few studies have examined nonlinear associations between sleep parameters and adolescent adjustment. For example, among younger children and adolescents, both shorter and longer sleep duration were related to greater internalizing and externalizing problems, a U-shaped relationship (Fuligni et al., 2018; James & Hale, 2017; Mears et al., 2020). In one study, nonlinear associations between sleepiness and internalizing problems were found, although the findings varied by gender (Shimizu et al., 2020).
Scant attention has been paid to potential nonlinear associations between the sleep environment or presleep conditions and sleep. However, such associations are plausible. For example, the negative effects of such conditions may appear at lower levels of sleep disturbances and then plateau. Alternatively, relations may be most evident at higher levels of sleep disruptions. In one empirical example with adolescents, nonlinear associations demonstrated sharp increases in both sleep latency and midsleep awakenings at more than two hours of screen media use before bed (Hisler et al., 2020). Towards a more thorough examination of research questions, we assessed both linear and nonlinear associations among the sleep environment, presleep conditions, and sleep.
Racial and socioeconomic disparities in sleep are well established. Short sleep duration and poor sleep quality are found among Black youth (Guglielmo et al., 2018) and those from lower-SES families (El-Sheikh et al., 2013; Marco et al., 2012), as compared to their White and higher SES counterparts, respectively. Similarly, Black and lower-SES youth also report greater daytime sleepiness (Philbrook et al., 2018). Racial and socioeconomic disparities in the sleep environment are also prevalent. Multiple environmental disruptions to sleep were commonly reported among a sample of low-income Black adolescents (Rubens et al., 2019), and racial differences in the quality of housing contributed to sleep disparities between White and Black adults (Johnson et al., 2018). Further, the quality of the physical home environment (e.g., overall noise levels; Doane et al., 2019) as well as the conditions of the sleep environment (e.g., noise while trying to sleep; Bagley et al., 2015) each mediated relations between SES and children’s sleep. Higher SES allows families to invest in a physical environment that supports healthy sleep, for example by providing comfortable bedding and temperature control (El-Sheikh et al., 2013). Higher SES is additionally associated with fewer presleep worries among children (Bagley et al., 2015).
Consistent with dual-risk (Sameroff, 1983) and health disparities (Buckhalt, 2011) perspectives, exposure to disruptions in the sleep environment and worse presleep conditions may be particularly disadvantageous for the sleep of lower-SES or Black individuals who are already disadvantaged by racial/ethnic or socioeconomic barriers (e.g., being historically minoritized, experiencing discrimination; El-Sheikh, Kelly et al., 2017; El-Sheikh, Zeringue et al., 2021). Additionally, the allostatic load model (Goldstein & McEwen, 2002) suggests that environmental stressors (e.g., living in poverty, experiencing discrimination) influence how the body responds to stress over time. Indeed, Black and lower SES adolescents exhibit higher allostatic loads (Rainisch & Upchurch, 2013), which may alter physiological responses to stress (El-Sheikh, Hinnant et al., 2017; El-Sheikh et al., 2020) and lead to an increased sensitivity to concurrent stressors associated with the sleep environment.
In sum, race and SES are associated with the sleep environment and presleep conditions, as well as greater sleep problems, although much less is known about whether race or SES moderate examined relations. In one of the few studies to examine interaction effects, Spilsbury and colleagues (2005) conducted observational assessments of the homes of urban children. They found that race moderated the association between the overall home environment and sleep duration, such that a higher quality home environment related to better sleep among Black but not White children. We are not aware of studies that have examined race or SES as moderators of relations between the sleep environment or presleep conditions and sleep in youth. However, race and SES moderated the relations between family and community stressors (e.g., parent relationship dissolution, community violence; Philbrook et al., 2020; Rudd et al., 2021) and sleep problems in youth. The overall pattern of effects demonstrated that risk variables were especially associated with sleep problems among Black or lower SES youth. Additionally, some positive factors (e.g., physical activity) have been found to interact with race or SES to predict sleep (Gillis et al., 2021), suggesting that a better sleep environment and less adverse presleep conditions may reduce sleep problems among Black or lower SES youth.
The Present Study
The first study aim was to examine linear and nonlinear associations between the sleep environment and presleep conditions (general worries, family concerns, arousal, and somatic complaints) and two sleep parameters (i.e., daytime sleepiness and sleep/wake problems) in a community sample of adolescents. We expected that a more disruptive sleep environment and worse presleep conditions would demonstrate positive linear associations with sleepiness and sleep/wake problems. Assessment of nonlinear associations was exploratory.
The second aim was to examine whether race (Black, White) and family SES moderated the aforementioned associations. We expected that the examined relations would be particularly evident for Black and lower SES youth. That is, a poorer sleep environment and worse presleep conditions may be particularly detrimental for Black or lower SES youth. At the same time, given evidence showing protective effects in the context of positive environmental factors for Black and lower SES youth (e.g., Gillis et al., 2021), it is also plausible that a less disruptive environment and better presleep conditions may be particularly beneficial for Black or lower SES youth, attenuating racial and socioeconomic disparities in sleep. Of note is that these two plausabilities are not mutually exclusive.
Method
Participants
The present study included participants from the fourth wave of a larger longitudinal study examining sleep and health disparities in children (Auburn University Sleep Study), which was approved by the university’s institutional review board. All adolescents who participated in previous waves were invited to participate in this study wave. At the initial wave (2009-2010 school year), 282 participants were recruited through letters distributed at local public schools in the southeastern United States (for more detail see Shimizu et al., 2020). At the current wave (2017–2018 school year), 126 additional families were recruited from the same school districts using the same recruitment methods. Youth did not have a diagnosed sleep disorder or learning disability based on mothers’ reports at recruitment. A total of 323 adolescents participated at the current wave, however, ten participants were excluded from our analyses because they were missing data on all five predictors and both outcomes. Adolescents who participated in previous waves (1–3) made up the majority of the sample (62.5%).
The analytic sample included 313 adolescents (Mage = 17.39 years, SD = 10.38 months) and was comprised of 51.4% girls, 48.6% boys (59.1% White/European American, 40.3% Black/African American). The majority of youth were attending high school physically (84.0%), 4.8% were attending high school online or were homeschooled, 1.3% were attending physical junior high school, 4.5% were attending college, 3.2% were working and not in school, and 2.2% were unemployed. According to the federal poverty guidelines at the time of data collection (U.S. Department of Commerce; www.commerce.gov), participants included 18.9% living in poverty, 19.9% low income, 39.4% middle class, and 21.8% upper middle class.
Procedure
Data were collected during the 2017–2018 school year, excluding holidays. Adolescent assent/consent and parental consent was obtained, and families received monetary compensation for participation. For brevity, only pertinent procedures are described. Mothers reported on family size and annual family income during a brief telephone questionnaire. Adolescents completed online surveys to assess the main study variables.
Measures
The Sleep Environment and Presleep Conditions
A modified version of The Sleep Environment Inventory (SEI; Mezick et al., 2008) was used to assess three presleep conditions: sleep physical environmental factors, presleep somatic complaints, and presleep worries. The 20-item measure assesses factors commonly reported as reasons for disrupted sleep. Adolescents rated each item that “keeps them from sleeping well” during the last week. The response choices included 0 (no/not applicable) and 1 (yes). The environmental factors subscale includes ten of the SEI items (Table 1; e.g., “Noise outside”), which were summed to create a total score (α = 0.82). The presleep worries subscale consists of five of the items (Table 1; e.g., “About schoolwork”), which were summed to create a total score (α = 0.82). Finally, five of the items were summed to create the presleep somatic complaints subscale (Table 1; α = 0.70; e.g., “Stomachache”).
Table 1.
Correlations between the individual items of the various sleep environment and presleep conditions measures with SES, race, and sleep.
| % endorsement | SES | Race | Sleepiness | Sleep/Wake Problems |
|
|---|---|---|---|---|---|
| Sleep Environment | |||||
| Noise outside | 24.4% | −.12 | .03 | .11 | .30** |
| Noise inside | 34.0% | −.09 | −.03 | .23** | .26** |
| Someone snoring | 20.9% | −.13 | .03 | .11 | .23** |
| Uncomfortable bed | 26.0% | −.14* | −.03 | .15* | .26** |
| Temperature of room | 55.6% | −.07 | −.09 | .14* | .21** |
| TV, radio, or computer | 24.6% | −.08 | .00 | .11 | .24** |
| Too much light | 22.2% | −.01 | −.06 | .12* | .20** |
| Received calls or texts | 48.2% | −.07 | .07 | .17** | .27** |
| Bed crowding | 10.2% | −.10 | −.14 | .07 | .19* |
| Pet in room | 27.3% | −.07 | −.14* | .20** | .23** |
| Presleep Worries | |||||
| About schoolwork | 34.5% | −.07 | −.06 | .22** | .26** |
| About family | 23.9% | −.15* | .08 | .17** | .31** |
| About friends | 25.7% | −.03 | −.18** | .17** | .22** |
| About other kids | 13.8% | −.07 | −.04 | .12* | .21** |
| About other things | 35.4% | −.01 | −.14* | .19** | .28** |
| Presleep Somatic Complaints | |||||
| Bathroom | 47.8% | −.09 | −.08 | .19** | .27** |
| Pain | 33.3% | −.16* | −.05 | .18** | .22** |
| Trouble breathing | 11.2% | −.05 | −.05 | .13* | .21** |
| Stomachache | 27.3% | −.15* | −.03 | .15* | .26** |
| Sick | 26.0% | −.06 | −.05 | .17** | .19** |
Note: 0 = White, 1 = Black.
p ≤ .05
p < .01
Adolescents also completed the Presleep Arousal Scale, which consists of 18 items assessing cognitive and physiological presleep arousal (PSA; Nicassio et al., 1985). Adolescents were instructed to describe how intensely they experience each item as they tried to fall asleep in their own bedroom on a scale of 1 (not at all) to 5 (extremely). Example items assessing physiological arousal include “A jittery, nervous feeling in your body,” “Perspiration in palms of your hands or other parts of your body,” and “A tight, tense feeling in your muscles.” Example cognitive arousal items include “Can’t shut off your thoughts,” “Worry about problems other than sleep,” and “Review or ponder events of the day.” The response choices were summed to create a total presleep arousal score (α = 0.91; consistent with Schneider et al., 2019).
In addition, and modeling after the format of the Presleep Arousal Scale (Nicassio et al., 1985), we created an additional five-item scale that assessed presleep family concerns. Adolescents described how intensely they experience each item as they tried to fall asleep in their own bedroom on a scale of 1 (not at all) to 5 (extremely). The five items were: “Worry about adults in the home arguing,” “Worry about your relationship with your mother,” “Worry about your relationship with your father,” “Worry about your mother drinking alcohol,” “Worry about your father drinking alcohol.” The response choices were summed to create a total presleep family concerns score (α = 0.77).
Sleep/wake parameters
Daytime sleepiness and sleep/wake problems were measured via the School Sleep Habits Survey (Wolfson & Carskadon, 1998). Sleepiness is a nine-item subscale asking adolescents if, in the last two weeks, they have struggled to stay awake in various situations such as “Traveling in a bus, plane, train, or car,” “During a test,” and “While working on a computer.” One item regarding driving a car was removed. Responses were on a scale from 1 to 4 (1 = no, 2 = struggled to stay awake, 3 = fallen asleep 4 = both struggled to stay awake and fallen asleep; α = .84).
Sleep/wake problems is a ten-item subscale asking youth how often they have experienced problems falling or staying asleep or waking in the morning in the past two weeks (α = .83). Items include “Stayed up until at least 3 am,” “Needed more than one reminder to get up in the morning,” and “Had nightmares or bad dreams during the night.” Responses were on a scale from 1 to 5. Items were coded so that 1 = never, 2 = once, 3 = twice, 4 = several times, and 5 = every day/night.
Covariates
Several covariates were included in the models: age, race, socioeconomic status (SES), and sex. Race was dichotomized such that 0 = White and 1 = Black. SES was defined by income-to-needs ratio based on mother-reported family income and family size.
Results
Plan of Analysis
Descriptive statistics and bivariate correlations were examined, and t-tests were conducted to examine sex and race differences for all study variables. All variables were checked for skewness, and values greater than three standard deviations from the mean were winsorized to the value equal to three standard deviations above or below the mean (Cousineau & Chartier, 2010). One value was winsorized for age, two for SES, four for presleep arousal, seven for presleep family concerns, four for sleepiness, and three for sleep/wake problems. Additionally, two participants identified their ethnicity as Latinx/Hispanic. For the purposes of race moderation, these two participants’ race data was considered missing. All predictor variables were mean-centered to reduce collinearity and aid in the interpretability of coefficients (Dalal & Zickar, 2012).
Analyses were conducted in MPlus version 8.4 (Muthén & Muthén, 1998–2017) using full information maximum likelihood estimation to handle missing data (Enders & Bandalos, 2001). Variables were entered in a series of models, rather than simultaneously, to facilitate interpretation of the main effects of the predictors. For a given sleep outcome (sleepiness and sleep/wake problems), control variables were entered first, followed by environmental disruptions or one of the four presleep condition predictors. Next, nonlinear (i.e., quadratic) relationships between the presleep condition predictor and a sleep outcome were tested; non-significant quadratic effects were removed for parsimony prior to testing moderation (Kline, 2010). Finally, interactions between race or SES and the linear effects of environmental disruptions or presleep conditions on sleep were examined. Interactions between race/SES and each significant nonlinear effect were also examined, but none were significant, and thus these results are not presented. Significant interactions were plotted at +/− 1 SD from the mean or at 0 for White participants and 1 for Black participants (Preacher et al., 2006).
Preliminary Analyses
Bivariate correlations between individual items from the Sleep Environment Inventory (used to yield environmental factors, presleep worries, and presleep somatic complaints scales) and race, SES, sleepiness, and sleep/wake problems are presented in Table 1. Sixteen of the 20 items representing the presleep constructs were correlated with sleepiness, and all 20 items were correlated with sleep/wake problems.
Descriptive statistics and bivariate correlations between covariates, the sleep environment and four presleep conditions scales, and sleep/wake parameters are presented in Table 2. The sleep environment and the four presleep conditions were modestly but consistently associated with both sleepiness and sleep/wake problems in expected directions. Independent samples t-tests showed no sex differences on any study variable. White participants had higher SES (t(300) = 8.21, M(SD)White = 3.32(1.77), M(SD)Black = 1.86(1.33), d = 0.91), higher levels of presleep arousal (t(262) = 2.56, M(SD)White = 28.28(10.56), M(SD)Black = 25.05(9.31), d = 0.32), and fewer sleep/wake problems (t(228) = −2.47, M(SD)White = 20.59(6.89), M(SD)Black = 23.11(8.56), d = 0.32) compared to Black adolescents. There were no other differences by race on any study variable. Participants who were missing data on the SEI or PSA scales (17.5% missing at least one scale) did not differ from participants without missing data on sex, race, SES, age, sleepiness, or sleep/wake problems.
Table 2.
Descriptive statistics and correlations among study variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Sex | - | ||||||||||
| 2 Age | .03 | - | |||||||||
| 3 Race | −.01 | −.11* | - | ||||||||
| 4 SES | .07 | .01 | −.41** | - | |||||||
| 5 ED | −.05 | −.01 | −.06 | −.13* | - | ||||||
| 6 PSW | −.05 | .02 | −.09 | −.09 | .67** | - | |||||
| 7 PSFC | −.02 | .00 | .04 | −.07 | .39** | .47** | - | ||||
| 8 PSA | −.01 | −.03 | −.16* | .01 | .47** | .56** | .50** | - | |||
| 9 PSSC | −.11 | .01 | −.08 | −.15* | .66** | .54** | .33** | .41** | - | ||
| 10 Sleepy | .03 | −.04 | .08 | −.06 | .22** | .24** | .21** | .28** | .23** | - | |
| 11 SWP | −.07 | .04 | .16** | −.26** | .37** | .34** | .34** | .31** | .31** | .47** | - |
| N | 313 | 313 | 311 | 307 | 261 | 258 | 265 | 266 | 260 | 311 | 310 |
| Min | - | 180.03 | - | 0 | 0 | 0 | 1 | 13 | 0 | 9 | 9 |
| Max | - | 239.96 | - | 8.61 | 10 | 5 | 14.63 | 58.15 | 5 | 28.12 | 45.36 |
| Mean | 51.4% | 208.68 | 40.6% | 2.74 | 2.69 | 1.31 | 6.26 | 27.06 | 1.42 | 14.16 | 21.59 |
| (SD) | Female | (10.38) | Black | (1.76) | (2.42) | (1.63) | (2.32) | (10.20) | (1.47) | (4.37) | (7.68) |
Note: SES = Socioeconomic Status, ED = Environmental Disruptions, PSW = Presleep Worries, PSFC = Presleep Family Concerns, PSA = Presleep Arousal, PSSC = Presleep Somatic Complaints, Sleepy = Sleepiness, and SWP = Sleep/Wake Problems. 0 = Female, 1 = Male. 0 = White, 1 = Black.
p < .05
p < .01.
Sleepiness
The first set of regression models tested linear and nonlinear relations between sleep environment disruptions and presleep conditions with sleepiness, as well as the moderating role of race and SES in these associations (Table 3). The covariates sex, age, race, and SES were not associated with sleepiness (not presented in the tables for parsimony). After accounting for the covariates, the sleep environment and each of the four presleep conditions showed positive linear associations with sleepiness. Moreover, three of the linear main effects were modified by a nonlinear main effect predicting sleepiness. Specifically, there was a rapid acceleration in sleepiness between low to average levels of environmental factors (Figure 1a), presleep worries (Figure 1b), and presleep arousal (Figure 1c). In all models, the negative nonlinear term modified the positive linear term such that sleepiness initially rapidly increased but then plateaued at average levels of the sleep environment, presleep general worries, and arousal. Thus, the increase in sleepiness was less steep between average and high levels of the sleep environment, presleep general worries, and arousal.
Table 3.
Regressions between presleep conditions and sleepiness.
| Environmental Disruptions |
Presleep Worries | Presleep Family Concerns |
Presleep Arousal | Presleep Somatic Complaints |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | |
| Linear Presleep Conditions | ||||||||||
| Presleep Condition | .37(.11) | .21*** | .61(.16) | .23*** | .39(.11) | .21*** | .12(.03) | .29*** | .65(.18) | .22*** |
| R2 | 5.0% | 6.1% | 5.2% | 9.0% | 5.5% | |||||
| Nonlinear Presleep Conditions | ||||||||||
| Presleep condition2 | −.10(.04) | −.22** | −.39(.11) | −.32*** | .02(.04) | .07 | −.01(.00) | −.21** | −.16(.13) | −.10 |
| ΔR2 | 3.1% | 4.1% | 0.1% | 2.5% | 0.6% | |||||
Note: All regressions control for race, sex, SES, and age which together account for 0.9% of the variance in sleepiness.
p < .01
p < .001.
Figure 1.
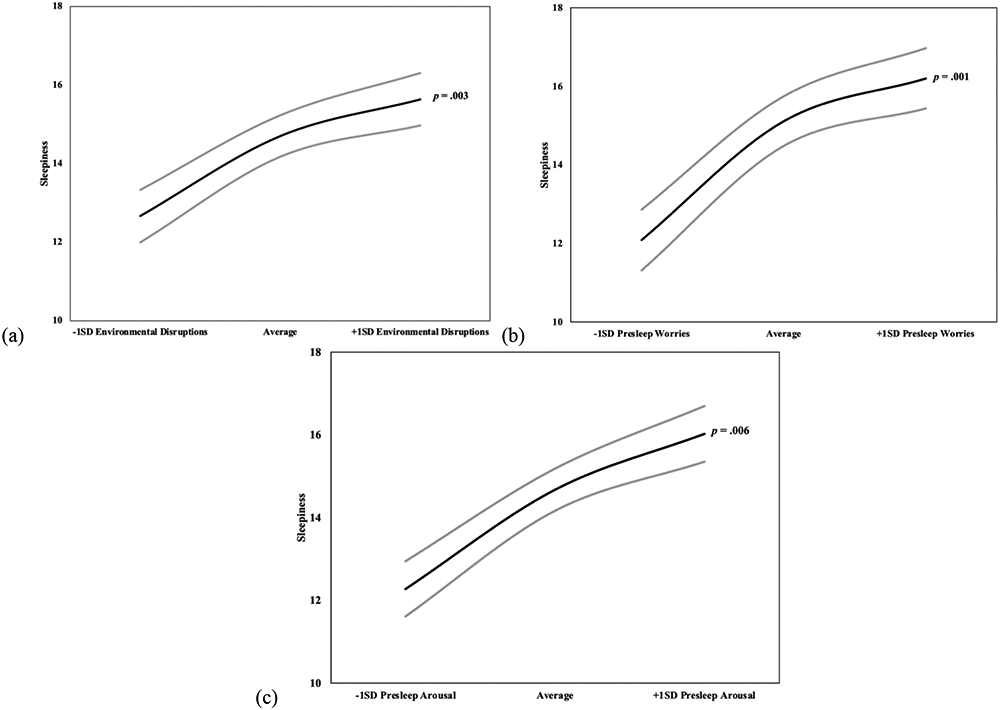
Nonlinear effect for standardized (a) sleep environmental disruptions2 (b) presleep worries2 and (c) presleep arousal2 predicting sleepiness. Points were plotted at +/− 1 SDs for predictors. 95% confidence intervals are presented in gray.
Note: −1-SD environmental disruptions and presleep worries is approximately 0 and +1-SD is approximately 5 and 3, respectively.
Specifically, in comparison to low levels of environmental disruptions, youth reported more sleepiness at average levels of such disruptions, while between average and high levels of disruptions youth reported a less steep increase in sleepiness (Figure 1a). Comparison of predicted means in sleepiness at low (M = 12.67) and average (M = 14.70) levels of environmental disruptions indicated a 0.47 SD difference in sleepiness. In addition, compared to average levels of environmental disruptions, sleepiness was slightly higher when disruptions were increased (M = 15.64), a difference of 0.21 SD. Sleepiness was higher between low (M = 12.09) and average (M = 15.12) worries, a 0.70 SD difference. Furthermore, sleepiness was slightly higher between average and high (M = 16.20) levels of presleep worries, a 0.25 SD difference in sleepiness. In addition, sleepiness was higher between low (M = 12.28) and average (M = 14.68) levels of arousal, a 0.55 SD difference, whereas the difference in sleepiness was somewhat less pronounced between average and high (M = 16.03) levels of arousal, a 0.31 SD difference. None of the linear or nonlinear associations were moderated by race or SES.
Sleep/Wake Problems
The second set of regression models tested linear and nonlinear relations between sleep environment disruptions and presleep conditions and sleep/wake problems and the moderating role of race and SES (Table 4). For a summary of results, see Table 5. None of the linear effects were modified by quadratic effects, and thus the nonlinear terms were not retained in models. The covariates sex, age, and race did not relate to sleep/wake problems. SES showed a negative association with sleep/wake problems (B(SE) = −0.99(0.27), β = −0.23, p < .001). Environmental disruptions and the four presleep conditions were positively and linearly associated with sleep/wake problems, and SES and race moderated some of the examined relations.
Table 4.
Regressions between presleep conditions and sleep/wake problems.
| Environmental Disruptions |
Presleep Worries | Presleep Family Concerns |
Presleep Arousal | Presleep Somatic Complaints |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | B(SE) | β | |
| Linear Presleep Conditions | ||||||||||
| Presleep Condition | 1.21(.18) | .38*** | 1.63(.27) | .34*** | 1.07(.18) | .32*** | .27(.04) | .35*** | 1.63(.30) | .31*** |
| R2 | 21.4% | 18.7% | 17.6% | 19.5% | 16.8% | |||||
| 2-way Interactions with Race and SES | ||||||||||
| Presleep Condition x Race | .73(.38) | .11* | .62(.55) | .06 | 1.06(.37) | .16** | .20(.09) | .13* | .48(.63) | .04 |
| ΔR2 | 1.0% | 0.3% | 2.5% | 1.7% | 0.1% | |||||
| Presleep Condition x SES | −.11(.10) | −.06 | .03(.17) | .01 | −.34(.15) | −.14* | −.01(.02) | −.03 | −.39(.19) | −.12* |
| ΔR2 | 0.5% | 0.0% | 1.8% | 0.0% | 1.6% | |||||
Note: All regressions control for race, sex, SES, and age which together account for 7.6% of the variance in sleep/wake problems. 0 = White, 1 = Black.
p < .05
p < .01
p < .001.
Table 5.
Summary of significant linear and nonlinear effects.
| Sleep/Wake Problems | Sleepiness | |
|---|---|---|
| Environmental Disruptions | Linear x Race | Nonlinear |
| Presleep Worries | Linear | Nonlinear |
| Presleep Family Concerns | Linear x Race Linear x SES |
Linear |
| Presleep Arousal | Linear x Race | Nonlinear |
| Presleep Family Concerns | Linear x SES | Linear |
As shown in Figure 2, the pattern of interaction effects illustrated that environmental disruptions were associated with higher levels of sleep/wake problems for both White and Black adolescents, although the slope was steeper for Black adolescents. At lower levels of environmental disruptions, the predicted means of sleep/wake problems were similarly low for White (M = 18.85) and Black (M = 18.94) adolescents. However, at higher levels of environmental disruptions, Black youth (M = 26.67) had more sleep problems than their White counterparts (M = 22.88), a 0.49 SD difference. Among Black adolescents, sleep/wake problems were higher at more, versus fewer, environmental disruptions, equivalent to a difference of one full SD in sleep/wake problems.
Figure 2.
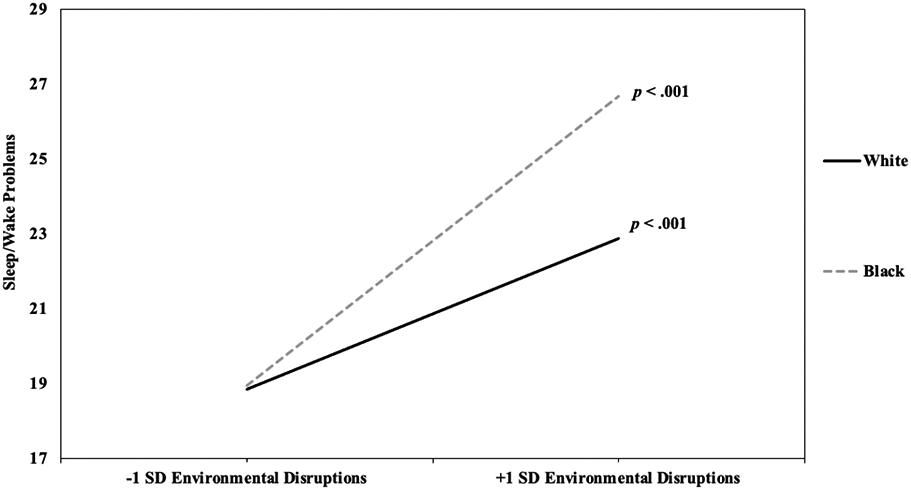
Race as a moderator of the relation between sleep environmental disruptions and sleep/wake problems.
As shown in Figure 3a, higher levels of family concerns were associated with higher levels of sleep/wake problems for both White and Black adolescents, although the slope was steeper for Black adolescents. For both White (M = 19.92) and Black (M = 18.42) adolescents, sleep/wake problems were similarly low for those with less family concerns. However, at higher levels of such concerns, Black youth (M = 25.80) had more sleep/wake problems than White adolescents (M = 22.39), a difference of 0.44 SD. Among Black adolescents, those with higher levels of family concerns reported more sleep/wake problems than those with lower levels of such concerns, a 0.96 SD difference.
Figure 3.
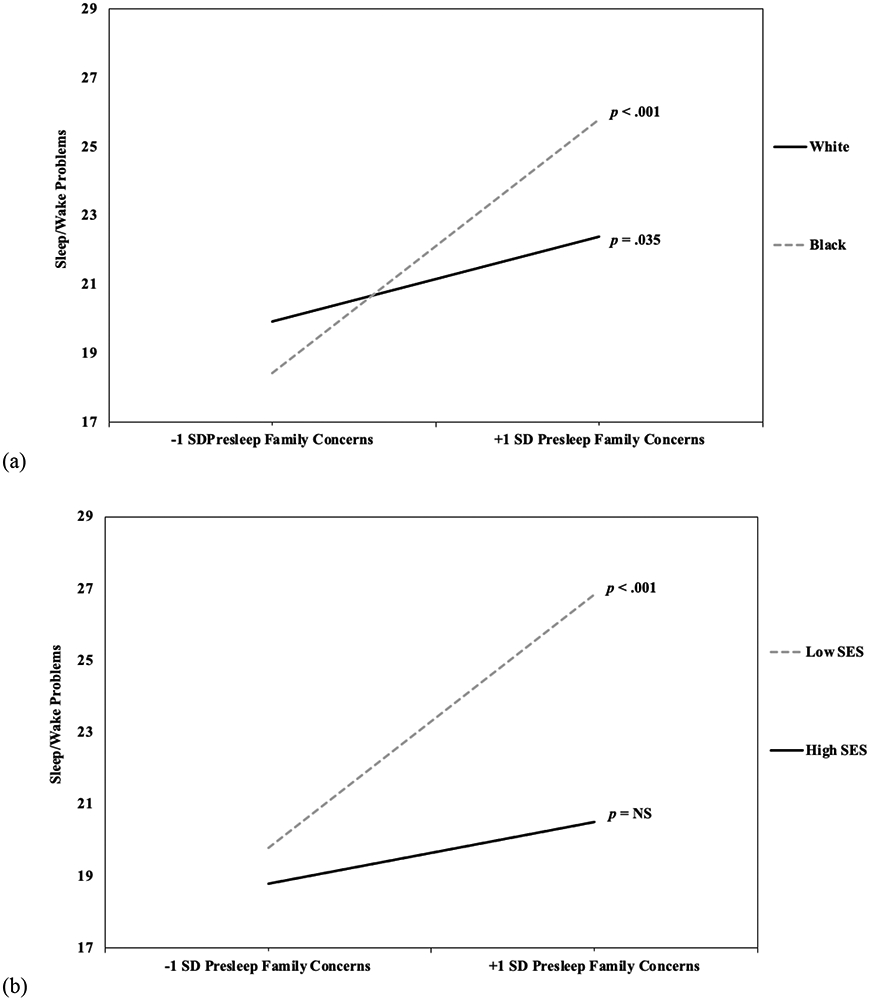
(a) Race and (b) SES as a moderator of the relation between presleep family concerns and sleep/wake problems.
As shown in Figure 3b, more presleep family concerns were associated with higher levels of sleep/wake problems only for lower SES youth. Higher SES youth had relatively low sleep/wake problems regardless of family concerns. At lower levels of these concerns, lower (M = 19.78) and higher (M = 18.80) SES youth had similarly low sleep/wake problems. At greater levels of concerns, lower SES youth (M = 26.84) had more sleep/wake problems compared to their higher SES counterparts (M = 20.52). For lower SES adolescents, sleep/wake problems were higher at more, versus less, family concerns, a 0.92 SD difference.
As shown in Figure 4, there was a positive association between presleep arousal and sleep/wake problems for both White and Black adolescents, although the relation was more pronounced for the latter. At lower levels of arousal, the predicted means of sleep/wake problems were similarly low for White (M = 18.96) and Black (M = 19.06) adolescents. However, at higher levels of such arousal, predicted means of sleep/wake problems were higher for Black (M = 27.38) compared to White (M = 22.64) adolescents. Further, among Black adolescents, those with higher levels of presleep arousal reported more sleep/wake problems than those with lower levels, equivalent to a 1.08 SD difference.
Figure 4.

Race as a moderator of the relation between presleep arousal and sleep/wake problems.
As shown in Figure 5, there was a significant positive association between presleep somatic complaints and sleep/wake problems for lower SES adolescents, and a marginal positive association for higher SES adolescents. Adolescents with low levels of somatic complaints reported relatively low levels of sleep/wake problems, regardless of family SES. However, at increased levels of such complaints, predicted means of sleep/wake problems were higher for less affluent (M = 26.12) compared to more affluent (M = 21.13) adolescents. For lower SES adolescents, sleep/wake problems were higher at more compared to less somatic complaints, a 0.82 SD difference.
Figure 5.
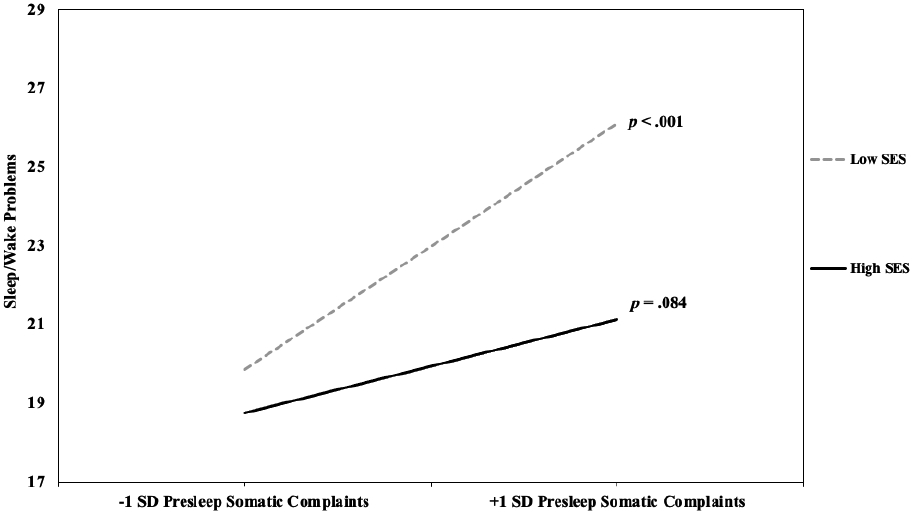
SES as a moderator of the relation between presleep somatic complaints and sleep/wake problems.
Discussion
We examined linear and nonlinear associations between the sleep environment, multiple presleep conditions, and sleep in a socioeconomically diverse sample composed of 60% White and 40% Black youth. Contributing to a relatively small body of literature with adolescents, and consistent with expectations, findings provide evidence of positive linear relations between the sleep environment and all presleep conditions examined (general worries, family concerns, arousal, and somatic complaints) and both daytime sleepiness and sleep/wake problems. Moreover, the sleep environment and both presleep worries and arousal showed nonlinear associations with daytime sleepiness. Consistent with hypotheses, some moderation effects were found and revealed that, in the context of more disruptions in the sleep environment and worse presleep conditions (excluding presleep worries), elevated risk of sleep/wake problems was particularly evident among Black and/or lower-SES adolescents. In the context of better presleep conditions and fewer environmental disruptions, racial and socioeconomic disparities in sleep/wake problems were reduced or eliminated.
Previous studies have reported associations between the sleep environment (e.g., Bagley et al., 2015; Peltz et al., 2021) and presleep conditions (e.g., Bartel et al., 2015; Heath et al., 2018) and various sleep/wake parameters. Much of the research on the sleep environment has focused on one or a few indicators, such as screens in the bedroom (Hale & Guan, 2015), neighborhood noise (Mayne et al., 2021), light exposure (Ikeda et al., 2014), or bed sharing (Li et al., 2008), rather than assessing a more inclusive measure of environmental disruptions (Bagley et al., 2015; Rubens et al., 2019). Using a more comprehensive measure of the sleep environment (10 items, e.g., light, noise, bedding), we found evidence consistent with hypotheses that adolescents’ daytime sleepiness and sleep/wake problems linearly increased with environmental disruptions, consistent with studies of children (Bagley et al., 2015; Doane et al., 2019) and adults (Johnson et al., 2021). Furthermore, similar to literature supportive of nonlinear relations between adolescent sleep and adjustment (e.g., Shimizu et al., 2020; Fuligni et al., 2018), as well as media use before going to bed and sleep (Hisler et al., 2020), results demonstrated nonlinear associations between the sleep environment and sleepiness in youth. From low to average levels of environmental disruptions, there was a sharper increase in sleepiness than between average to high levels. These results suggest that even a few environmental disruptions increase the risk of daytime sleepiness. These findings are the first of their kind and demonstrate the importance of assessments of nonlinear relations.
General worries (Clancy et al., 2020) and presleep arousal (Schneider et al., 2019) are well established correlates and predictors of sleep, however, few studies have examined multiple and more nuanced indicators of presleep conditions with youth. Consistent with expectations and contributing to existing evidence, all presleep conditions examined (i.e., presleep worries, family concerns, arousal, and somatic complaints) were linearly associated with daytime sleepiness and sleep/wake problems. To our knowledge, all studies examining relations between presleep conditions in youth and sleep have assessed linear associations. In addition to linear relations, general worries and presleep arousal showed nonlinear relations with daytime sleepiness. Specifically, there were initially sharp increases in sleepiness from low to average levels of these presleep conditions and less steep increases between average and high levels, consistent with findings for sleep environment disruptions. It should be noted that the existence of some nonlinear effects does not diminish the importance of the consistent linear effects. It is not clear why nonlinear effects emerged for some but not all examined relations, and these results should be considered preliminary pending findings from other studies.
There is a substantial literature documenting health disparities in sleep for youth who are historically minoritized or exposed to socioeconomic disadvantage (El-Sheikh et al., 2013; Guglielmo et al., 2018). Race and SES have also been found to moderate relations between several risk factors (e.g., community violence concerns, parental relationship dissolution) and short and poor-quality sleep (Rudd et al., 2021; Philbrook et al., 2020). Our findings are novel in demonstrating that some associations between both the sleep environment and presleep conditions and sleep were moderated by race or SES (analyses of moderation by race controlled for SES and vice versa). More sleep environment disruptions and worse presleep arousal and family concerns were linearly associated with sleep/wake problems for both Black and White adolescents, yet the relation was more pronounced for the former. Supportive of dual-risk and health disparities perspectives (Buckhalt, 2011; El-Sheikh, Kelly et al., 2017), we found increased vulnerability to sleep problems for historically minoritized youth. Black youth may experience more stressors on average (e.g., racial discrimination; Yip, 2018) which result in disruptions in physiological functioning that may directly impact sleep (El-Sheikh, Hinnant et al., 2017) and exacerbate the effects of other stressors on sleep (Philbrook et al., 2020). Thus, stress may explain why disruptions in the sleep environment and worse presleep conditions have stronger impacts on sleep/wake problems among Black youth. Importantly, our findings also demonstrate protection against sleep problems in the context of fewer environmental disruptions and better presleep conditions such that Black adolescents have similar sleep to White adolescents, reducing this health disparity.
We also found that SES moderated associations between some presleep conditions and adolescents’ sleep/wake problems. Previous research has supported the notion that the sleep environment and family risk factors are possible explanatory mechanisms linking socioeconomic disparities and sleep (e.g., Doane et al., 2019; Guglielmo et al., 2018). We found that higher levels of somatic complaints and family concerns were related to higher levels of sleep/wake problems only for lower-SES adolescents. Higher-SES youth reported fewer sleep/wake problems regardless of whether presleep conditions were better or worse. Somatic complaints are more common among lower income youth (Reynolds et al., 2001), and our findings contribute evidence that nighttime somatic complaints exacerbate the influence of lower family SES on sleep. Our study also showed that presleep family concerns are particularly detrimental for lower SES adolescents, consistent with evidence that different family stressors are more strongly related to sleep for such youth (Kelly & El-Sheikh, 2011; Rudd et al., 2021). Demonstrative of protection, lower-SES youth had similar sleep to their higher-SES counterparts when they had fewer presleep somatic complaints or family concerns, reducing socioeconomic disparities in sleep.
The study has several strengths and weaknesses. We utilized a relatively large sample that included a high representation of adolescents exposed to socioeconomic adversity as well as a relatively high proportion of Black participants. However, all participants lived in small towns and rural communities in the southeastern United States. In addition, only Black and White youth participated, further limiting the generalizability of the findings. A strength of the study is the inclusion of adolescents’ perspectives on the sleep environment and several presleep conditions. Although a well-established questionnaire was used to derive the two sleep parameters, findings are based exclusively on self-reports. Previous research has shown that White adults overestimate their sleep duration more often than Black adults through comparison of objectively and subjectively measured sleep (for a review see Johnson et al., 2019). It is unclear to what extent racial differences in sleep/wake problems may reflect differences in reporting, rather than the experience of sleep/wake problems. Another potentially important avenue for research is the assessment of daily associations between the sleep environment or presleep conditions and sleep that night (e.g., Tavernier et al., 2017).
Overall, findings contribute to an emerging body of literature showing that the sleep environment and multiple presleep conditions are related linearly and nonlinearly to sleep, highlighting the importance of assessments of the latter, which is underrepresented in the sleep literature at large. It appears that reducing even moderate levels of environmental disruptions, presleep general worries, or arousal could protect against or lessen daytime sleepiness among adolescents. Findings from moderation analyses indicate the importance of assessment of individual differences including SES and race. The sleep environment and presleep conditions were particularly important for lower-SES and Black adolescents as fewer sleep environment disruptions and better presleep conditions reduced or eliminated the disparity in sleep/wake problems, and the converse was true with more disruptions and worse presleep conditions. Intervention research has shown that changing conditions of the sleep environment such as providing a better bed (Mindell et al., 2016) or educating families about better sleep hygiene (Sonney et al., 2020; Wolfson et al., 2015) contributes to decreases in sleep problems. Therapeutic interventions targeting anxiety specifically (Blake, Snoep et al., 2017) and interventions including cognitive behavioral therapy aimed at reducing conditions such as presleep arousal (Blake, Schwartz et al., 2017) have also been shown to improve sleep. Therefore, these conditions may be useful targets for intervention programs particularly in communities that are historically minoritized or socioeconomically disadvantaged. Furthermore, sleep disparities are often structurally rooted, reflecting racial and economic disparities in housing conditions and exposure to stressors (Johnson et al., 2018). Thus, in addition to individual intervention efforts, addressing structural factors at a societal level, for example, by providing income and housing assistance and reducing structural racism, would also provide needed resources to improve the sleep environment, thereby reducing sleep disparities.
Supplementary Material
Highlights.
The sleep environment and presleep conditions relate to adolescent sleep problems.
Presleep environment, worries, and arousal show nonlinear relations with sleepiness.
Some relations with sleep/wake problems were stronger among Black adolescents.
Family and somatic concerns relate to sleep/wake problems only for lower SES youth.
Funding
This research was supported by grants from the National Heart, Lung, and Blood Institute at the National Institutes of Health (NIH R01-HL093246, R01-HL136752) awarded to Dr. Mona El-Sheikh.
Footnotes
Conflicts of Interest
The authors have no relevant financial or non-financial interests to disclose. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or material discussed in this manuscript.
Ethical Approval
The study was conducted in accordance with ethical standards. All study procedures received IRB approval from Auburn University prior to data were collection.
Informed Consent
Parents provided informed consent for adolescents to participate and adolescents provided assent to participate.
Credit Author Statement
LM participated in the statistical analysis, interpretation of the data, and drafted the manuscript; MZ participated in the writing and revising of the manuscript; OM participated in the writing and revising of the manuscript; JB participated in the conceptualization of the study and writing of the manuscript; ME participated in the design and coordination of the study, and the writing and revision of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alfano CA, Pina AA, Zerr AA, & Villalta IK (2010). Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry & Human Development, 41(2), 156–167. 10.1007/s10578-009-0158-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagley EJ, Kelly RJ, Buckhalt JA, & El-Sheikh M (2015). What keeps low-SES children from sleeping well: The role of presleep worries and sleep environment. Sleep Medicine, 16(4), 496–502. 10.1016/j.sleep.2014.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartel KA, Gradisar M, & Williamson P (2015). Protective and risk factors for adolescent sleep: A meta-analytic review. Sleep Medicine Reviews, 21, 72–85. 10.1016/j.smrv.2014.08.002 [DOI] [PubMed] [Google Scholar]
- Bell BG, & Belsky J (2008). Parents, parenting, and children's sleep problems: Exploring reciprocal effects. British Journal of Developmental Psychology, 26(4), 579–593. 10.1348/026151008X285651 [DOI] [Google Scholar]
- Blake M, Schwartz O, Waloszek JM, Raniti M, Simmons JG, Murray G, Blake L, Dahl RE, Bootzin R, McMakin DL, Dudgeon P, Trinder J, & Allen NB (2017). The SENSE study: Treatment mechanisms of a cognitive behavioral and mindfulness-based group sleep improvement intervention for at-risk adolescents. Sleep, 40(6). 10.1093/sleep/zsx061 [DOI] [PubMed] [Google Scholar]
- Blake MJ, Snoep L, Raniti M, Schwartz O, Waloszek JM, Simmons JG, Murray G, Blake L, Landau ER, Dahl RE, Bootzin R, McMakin DL, Dudgeon P, Trinder J, & Allen NB (2017). A cognitive-behavioral and mindfulness-based group sleep intervention improves behavior problems in at-risk adolescents by improving perceived sleep quality. Behaviour Research and Therapy, 99, 147–156. 10.1016/j.brat.2017.10.006 [DOI] [PubMed] [Google Scholar]
- Clancy F, Prestwich A, Caperon L, Tsipa A, & O’Connor DB (2020). The association between worry and rumination with sleep in non-clinical populations: A systematic review and meta-analysis. Health Psychology Review, 14(4), 427–448. 10.1080/17437199.2019.1700819 [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, & Aiken LS (2013). Applied multiple regression/correlation analysis for the behavioral sciences. Routledge. [Google Scholar]
- Cousineau D, & Chartier S (2010). Outliers detection and treatment: A review. International Journal of Psychological Research, 3(1), 58–67. [Google Scholar]
- Carskadon MA (2011). Sleep in adolescents: The perfect storm. Pediatric Clinics of North America, 58(3), 637–647. 10.1016/j.pcl.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley SJ, Acebo C, & Carskadon MA (2007). Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Medicine, 8(6), 602–612. 10.1016/j.sleep.2006.12.002 [DOI] [PubMed] [Google Scholar]
- Dahl RE (1996). The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology, 8(1), 3–27. 10.1017/S0954579400006945 [DOI] [Google Scholar]
- Dalal DK, & Zickar MJ (2012). Some common myths about centering predictor variables in moderated multiple regression and polynomial regression. Organizational Research Methods, 15(3), 339–362. 10.1177/1094428111430540 [DOI] [Google Scholar]
- Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, & Bögels SM (2010). The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Medicine Reviews, 14, 179–189. 10.1016/j.smrv.2009.10.004 [DOI] [PubMed] [Google Scholar]
- Doane LD, Breitenstein RS, Beekman C, Clifford S, Smith TJ, & Lemery-Chalfant K (2019). Early life socioeconomic disparities in children’s sleep: The mediating role of the current home environment. Journal of Youth and Adolescence, 48(1), 56–70. 10.1007/s10964-018-0917-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, & Buckhalt JA (2013). Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychology, 32(8), 849–859. 10.1037/a0030413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Hinnant JB, & Philbrook LE (2017). Trajectories of sleep and cardiac sympathetic activity indexed by pre-ejection period in childhood. Journal of Sleep Research, 26, 578–586. 10.1111/jsr.12491 [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly RJ, & Philbrook LE (2017). Sleep and development: Familial and socio-cultural considerations. In McHale S, King V & Buxton O (Eds.) Family contexts of sleep and health across the life course (pp. 25–49). Springer. 10.1007/978-3-319-64780-7_2 [DOI] [Google Scholar]
- El-Sheikh M, Shimizu M, Philbrook LE, Erath SA, & Buckhalt JA (2020). Sleep and development in adolescence in the context of socioeconomic disadvantage. Journal of Adolescence, 83, 1–11. 10.1016/j.adolescence.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Zeringue MM, Saini EK, Fuller-Rowell TE, & Yip T (2021). Discrimination and adjustment in adolescence: the moderating role of sleep. Sleep. 10.1093/sleep/zsab215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8(3), 430–457. 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- Fuligni AJ, Arruda EH, Krull JL, & Gonzales NA (2018). Adolescent sleep duration, variability, and peak levels of achievement and mental health. Child Development, 89(2), e18–e28. 10.1111/cdev.12729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ, & Hardway C (2006). Daily variation in adolescents' sleep, activities, and psychological well- being. Journal of Research on Adolescence, 16(3), 353–378. 10.1111/j.1532-7795.2006.00498.x [DOI] [Google Scholar]
- Gillis BT, Shimizu M, Philbrook LE, & El-Sheikh M (2021). Racial disparities in adolescent sleep duration: Physical activity as a protective factor. Cultural Diversity and Ethnic Minority Psychology, 27(1), 118–122. 10.1037/cdp0000422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradisar M, Gardner G, & Dohnt H (2011). Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Medicine, 12(2), 110–118. 10.1016/j.sleep.2010.11.008 [DOI] [PubMed] [Google Scholar]
- Gregory AM, & Sadeh A (2012). Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews, 16(2), 129–136. 10.1016/j.smrv.2011.03.007 [DOI] [PubMed] [Google Scholar]
- Gregory AM, Willis TA, Wiggs L, Harvey AG, & STEPS team. (2008). Presleep arousal and sleep disturbances in children. Sleep, 31(12), 1745–1747. 10.1093/sleep/31.12.1745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guglielmo D, Gazmararian JA, Chung J, Rogers AE, & Hale L (2018). Racial/ethnic sleep disparities in US school-aged children and adolescents: A review of the literature. Sleep Health, 4(1), 68–80. 10.1016/j.sleh.2017.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, & Guan S (2015). Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Medicine Reviews, 21, 50–58. 10.1016/j.smrv.2014.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath M, Johnston A, Dohnt H, Short M, & Gradisar M (2018). The role of pre-sleep cognitions in adolescent sleep-onset problems. Sleep Medicine, 46, 117–121. 10.1016/j.sleep.2018.03.002 [DOI] [PubMed] [Google Scholar]
- Hisler G, Twenge JM, & Krizan Z (2020). Associations between screen time and short sleep duration among adolescents varies by media type: Evidence from a cohort study. Sleep Medicine, 66, 92–102. 10.1016/j.sleep.2019.08.007 [DOI] [PubMed] [Google Scholar]
- Ikeda M, Kaneita Y, Yamamoto R, Itani O, Kondo S, Osaki Y, Kanda H, Higuchi S, & Ohida T (2014). Sleep environments of Japanese adolescents: An epidemiological study. Sleep and Biological Rhythms, 12(2), 116–126. 10.1111/sbr.12050 [DOI] [Google Scholar]
- James S, & Hale L (2017). Sleep duration and child well-being: A nonlinear association. Journal of Clinical Child & Adolescent Psychology, 46(2), 258–68. 10.1080/15374416.2016.1204920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DA, Jackson CL, Guo N, Sofer T, Laden F, & Redline S (2021). Perceived home sleep environment: Associations of household-level factors and in-bed behaviors with actigraphy-based sleep duration and continuity in the Jackson Heart Sleep Study. Sleep. 10.1093/sleep/zsab163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson DA, Thorpe RJ, McGrath JA, Jackson WB, & Jackson CL (2018). Black–white differences in housing type and sleep duration as well as sleep difficulties in the United States. International Journal of Environmental Research and Public Health, 15(4), 564. 10.3390/ijerph15040564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller PS, Gilbert LR, Koss KJ, Cummings EM, & Davies PT (2011). Parental problem drinking, marital aggression, and child emotional insecurity: A longitudinal investigation. Journal of Studies on Alcohol and Drugs, 72(5), 711–722. 10.15288/jsad.2011.72.711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly RJ, & El-Sheikh M (2011). Marital conflict and children's sleep: Reciprocal relations and socioeconomic effects. Journal of Family Psychology, 25(3), 412–422. 10.1037/a0023789 [DOI] [PubMed] [Google Scholar]
- Kelly RJ, & El-Sheikh M (2019). Reciprocal relations between parental problem drinking and children's sleep: The role of socioeconomic adversity. Child Development, 90(6), 1987–2000. 10.1111/cdev.13074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly RJ, Marks BT, & El-Sheikh M (2014). Longitudinal relations between parent–child conflict and children’s adjustment: The role of children’s sleep. Journal of Abnormal Child Psychology, 42(7), 1175–1185. 10.1007/s10802-014-9863-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2010). Principles and practice of structural equation modeling (3rd Ed). New York, NY: The Guilford Press. [Google Scholar]
- Li S, Jin X, Yan C, Wu S, Jiang F, & Shen X (2008). Bed-and room-sharing in Chinese school-aged children: Prevalence and association with sleep behaviors. Sleep Medicine, 9(5), 555–563. 10.1016/j.sleep.2007.07.008 [DOI] [PubMed] [Google Scholar]
- Marco CA, Wolfson AR, Sparling M, & Azuaje A (2012). Family socioeconomic status and sleep patterns of young adolescents. Behavioral Sleep Medicine, 10(1), 70–80. 10.1080/15402002.2012.636298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayne SL, Mitchell JA, Virudachalam S, Fiks AG, & Williamson AA (2021). Neighborhood environments and sleep among children and adolescents: A systematic review. Sleep Medicine Reviews, 101465. 10.1016/j.smrv.2021.101465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mears DP, Tomlinson TA, & Turanovic JJ (2020). The goldilocks rule—too little, too much, and “just right”: Curvilinear effects of sleep duration on delinquency. Justice Quarterly, 1–28. 10.1080/07418825.2020.1729393 [DOI] [Google Scholar]
- Mezick EJ, Matthews KA, Hall M, Strollo PJ Jr, Buysse DJ, Kamarck TW, … & Reis SE (2008). Influence of race and socioeconomic status on sleep: Pittsburgh Sleep SCORE project. Psychosomatic Medicine, 70(4), 410–416. 10.1097/PSY.0b013e31816fdf21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell JA, Sedmak R, Boyle JT, Butler R, & Williamson AA (2016). Sleep well!: A pilot study of an education campaign to improve sleep of socioeconomically disadvantaged children. Journal of Clinical Sleep Medicine, 12(12), 1593–1599. 10.5664/jcsm.6338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998-2017). Mplus user’s guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nicassio PM, Mendlowitz DR, Fussell JJ, & Petras L (1985). The phenomenology of the pre-sleep state: The development of the pre-sleep arousal scale. Behaviour Research and Therapy, 23(3), 263–271. 10.1016/0005-7967(85)90004-X [DOI] [PubMed] [Google Scholar]
- Norell-Clarke A, & Hagquist C (2018). Child and adolescent sleep duration recommendations in relation to psychological and somatic complaints based on data between 1985 and 2013 from 11 to 15 year-olds. Journal of Adolescence, 68, 12–21. 10.1016/j.adolescence.2018.07.006 [DOI] [PubMed] [Google Scholar]
- O’Callaghan VS, Couvy-Duchesne B, Strike LT, McMahon KL, Byrne EM, & Wright MJ (2021). A meta-analysis of the relationship between subjective sleep and depressive symptoms in adolescence. Sleep Medicine, 79, 134–144. 10.1016/j.sleep.2021.01.011 [DOI] [PubMed] [Google Scholar]
- Owens JA (2014). Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics, 134(3), e921–e932. 10.1542/peds.2014-1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo TM, Toliver-Sokol M, Fonareva I, & Koh JL (2007). Objective and subjective assessment of sleep in adolescents with chronic pain compared to healthy adolescents. The Clinical Journal of Pain, 23(9), 812–820. 10.1097/AJP.0b013e318156ca63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltz J, Rogge R, Buckhalt J, & Elmore Staton L (2021). The development and psychometrics of an assessment of children’s sleep environments. Sleep Abstract Supplement, 44, A241. [Google Scholar]
- Philbrook LE, Buckhalt JA, & El- Sheikh M (2020). Community violence concerns and adolescent sleep: Physiological regulation and race as moderators. Journal of Sleep Research, 29(3), e12897. 10.1111/jsr.12897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philbrook LE, Shimizu M, Buckhalt JA, & El-Sheikh M (2018). Sleepiness as a pathway linking race and socioeconomic status with academic and cognitive outcomes in middle childhood. Sleep Health, 4(5), 405–412. 10.1016/j.sleh.2018.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, & Bauer DJ (2006). Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31(4), 437–448. 10.3102/10769986031004437 [DOI] [Google Scholar]
- Rainisch BKW, & Upchurch DM (2013). Sociodemographic correlates of allostatic load among a national sample of adolescents: Findings from the National Health and Nutrition Examination Survey, 1999–2008. Journal of Adolescent Health, 53(4), 506–511. 10.1016/j.jadohealth.2013.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds LK, O'Koon JH, Papademetriou E, Szczygiel S, & Grant KE (2001). Stress and somatic complaints in low-income urban adolescents. Journal of Youth and Adolescence, 30(4), 499–514. 10.1023/A:1010401417828 [DOI] [Google Scholar]
- Rubens SL, Gudiño OG, Ford LM, Soliemannjad RR, & Contreras PD (2020). Association between the sleep environment and sleep problems in low-income Latinx youth. Children's Health Care, 49(3), 287–302. 10.1080/02739615.2020.1727323 [DOI] [Google Scholar]
- Rubens SL, Miller MA, & Zeringue MM (2019). The sleep environment and its association with externalizing behaviors in a sample of low- income adolescents. Journal of Community Psychology, 47(3), 628–640. 10.1002/jcop.22142 [DOI] [PubMed] [Google Scholar]
- Rudd BN, Reilly ME, Holtzworth-Munroe A, D’Onofrio BM, & Waldron M (2021). Interactive effects of parental separation and socioeconomic status on child sleep quality and child development. Journal of Child and Family Studies. 10.1007/s10826-021-01989-1 [DOI] [Google Scholar]
- Schneider MN, Denis D, Buysse DJ, Kovas Y, & Gregory AM (2019). Associations between pre-sleep arousal and insomnia symptoms in early adulthood: A twin and sibling study. Sleep, 42(5), zsz029. 10.1093/sleep/zsz029 [DOI] [PubMed] [Google Scholar]
- Shochat T, Cohen-Zion M, & Tzischinsky O (2014). Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Medicine Reviews, 18(1), 75–87. 10.1016/j.smrv.2013.03.005 [DOI] [PubMed] [Google Scholar]
- Sonney JT, Thompson HJ, Landis CA, Pike KC, Chen ML, Garrison MM, & Ward TM (2020). Sleep intervention for children with asthma and their parents (SKIP Study): A novel web-based shared management pilot study. Journal of Clinical Sleep Medicine, 16(6), 925–936. 10.5664/jcsm.8374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spilsbury JC, Frame J, Magtanong R, & Rork K (2016). Sleep environments of children in an urban US setting exposed to interpersonal violence. Behavioral Sleep Medicine, 14(6), 585–601. 10.1080/15402002.2015.1048449 [DOI] [PubMed] [Google Scholar]
- Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner HL, & Redline S (2005). Effects of the home environment on school-aged children's sleep. Sleep, 28(11), 1419–1427. 10.1093/sleep/28.11.1419 [DOI] [PubMed] [Google Scholar]
- Shimizu M, Gillis BT, Buckhalt JA, & El-Sheikh M (2020). Linear and nonlinear associations between sleep and adjustment in adolescence. Behavioral Sleep Medicine, 18(5), 690–704. 10.1080/15402002.2019.1665049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu M, Zeringue MM, Erath SA, Hinnant JB, & El-Sheikh M (2021). Trajectories of sleep problems in childhood: Associations with mental health in adolescence. Sleep, 44, 1–10. 10.1093/sleep/zsaa190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavernier R, Heissel JA, Sladek MR, Grant KE, & Adam EK (2017). Adolescents' technology and face-to-face time use predict objective sleep outcomes. Sleep Health, 3(4), 276–283. 10.1016/j.sleh.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson AR, & Carskadon MA (1998). Sleep schedules and daytime functioning in adolescents. Child Development, 69(4), 875–887. 10.1111/j.1467-8624.1998.tb06149.x [DOI] [PubMed] [Google Scholar]
- Wolfson AR, Harkins E, Johnson M, & Marco C (2015). Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health, 1(3), 197–204. 10.1016/j.sleh.2015.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh ZT, Wung SK, & Lin CM (2015). Pre-sleep arousal as a mediator of relationships among worry, rumination, and sleep quality. International Journal of Cognitive Therapy, 8(1), 21–34. 10.1521/ijct.2015.8.1.21 [DOI] [Google Scholar]
- Yip T (2018). Ethnic/racial identity—A double-edged sword? Associations with discrimination and psychological outcomes. Current Directions in Psychological Science, 27(3), 170–175. 10.1177/0963721417739348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeringue MM, Erath SA, & El-Sheikh M (2021). Exposure to peer aggression and adolescent sleep problems: Moderation by parental acceptance. Journal of Family Psychology. 10.1037/fam0000713 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


