Cardiovascular disease (CVD) remains the leading cause of death worldwide. While clinicians appropriately treat established CVD risk factors, the potential CVD risks from climate change warrant further investigation. With ongoing climate change, the intensity and duration of heatwaves and temperature extremes will likely escalate over the coming decades. As a specific example, the Arabian Peninsula is an inherently hot and hyper-arid region where temperatures are already soaring to unprecedented levels 1, yet to date scant data are available regarding the relationship between climate change and CVD mortality in this region. Kuwait is a representative country in the corner of the Arabian Peninsula, where the highest temperature on earth in the last 76 years was recently recorded 1. Should emissions of greenhouse gases continue at the present rate, the projected temperatures in the Arabian Peninsula will exceed the threshold of human adaptability by the end of this century 2. In this investigation, we specifically assessed the effects of extreme ambient temperatures in Kuwait on CVD mortality over a seven year period.
We applied a time-series design to measure cardiovascular-specific daily mortality in Kuwait from 2010 to 2016, as well as the 24-hour average ambient temperatures across the country 3. The population of Kuwait is approximately 4.1 million. Cause-specific mortality data was obtained from the Department of Vital Statistics, Ministry of Health, Kuwait. Cardiovascular mortality was defined using International Classification of Diseases codes from death certificates (ICD-10 I00-I99). We used distributed lag non-linear models (dlnm) to capture delayed effects of temperature on mortality over a span of 30 days. The dlnm models allow the estimation of non-linear effects at specific time lags and across all lags. We modeled the lag using a cubic natural spline with three degrees of freedom placed equally on the log scale. Negative binomial regression was used to account for overdispersion. All results were adjusted for air pollutants (ozone and PM10; particles with aerodynamic diameter <10μm), relative humidity, and other factors that can confound the relationship in a time-series design (time trends, seasonality, and day of the week) as described previously 3. By design, individual characteristics including age, sex, body mass index, smoking, and others, cannot confound the observed relationship because a) they do not vary from day to day, and b) they cannot be associated with the daily fluctuations of ambient temperatures. However, these factors can be important effect modifiers. Our analysis was repeated for overall, sex-specific and age-group-specific cardiovascular mortality. The work described in this article has been approved by The Standing Committee for Coordination of Health and Medical Research, Ministry of Health, Kuwait. The work was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki).
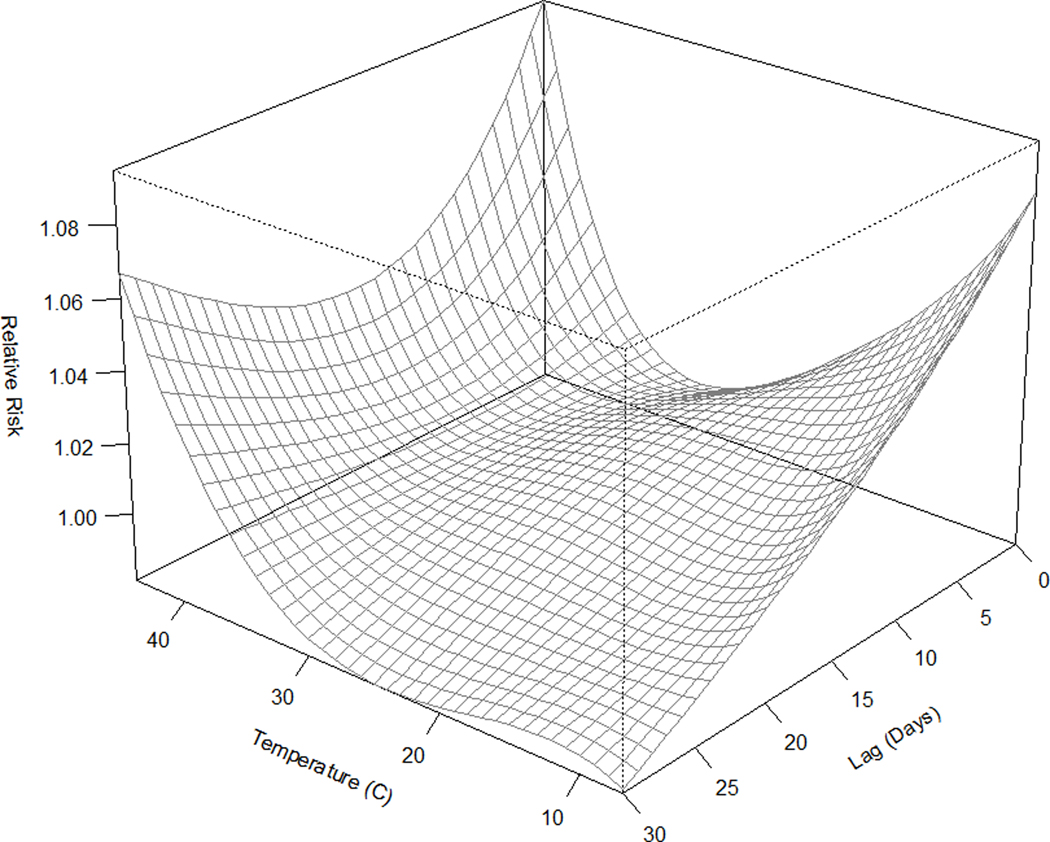
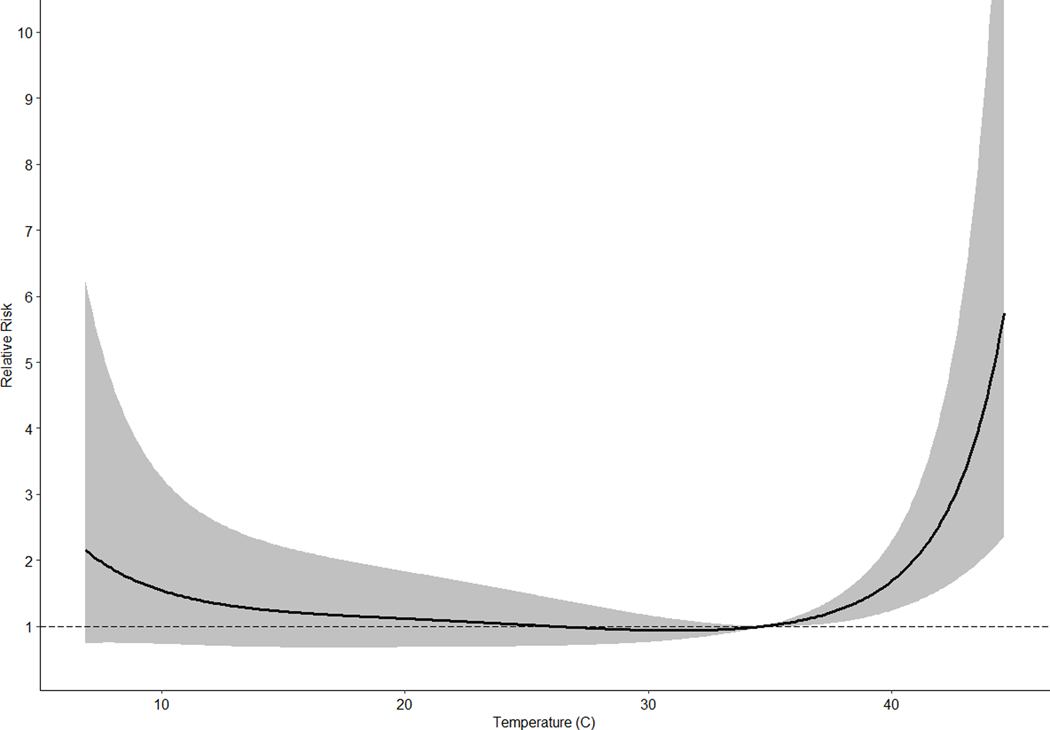
Across the entire country, a total of 15,609 cardiovascular deaths occurred over the study period of 2532 days (1.4% missing) with an average rate of 6.2±2.7 cardiovascular deaths per day. The 24-hour average ambient temperature in Kuwait was 27.9±9.5°C (82.2±49.1°F); the minimum mortality temperature (MMT; temperature associated with lowest mortality) was 34.7°C (94.5°F), and the extreme temperature (99th percentile) was 42.7°C (108.9°F). The average PM10 and ozone levels were 190.7±201.2 μg/m3 and 0.023±0.008 ppm, respectively. The relative risk of dying from a cardiovascular cause at the extreme temperature compared to the MMT was 3.09 (95% CI: 1.72–5.55). Similarly, the relative risks of dying from a cardiovascular cause among males and females were 3.53 (1.74–7.16) and 2.36 (0.83–6.66), respectively. Those aged 15–64 years had a relative risk of 3.84 (1.57–7.70), while older adults above 65 had a relative risk of 2.29 (0.96–5.48). The CVD temperature-mortality relationship at specific lags is shown in the three-dimensional plot (Figure A). Across all lags, the exposure-response relationship was U-shaped, and the risk of adjusted CVD mortality increased with increasing temperature beyond the MMT (Figure B).
Figure:
3D plot of adjusted temperature-mortality relationship at specific time lags from distributed lag non-linear models (dlnm). The z-axis shows the relative risk of CVD mortality with respect to the MMT (34.7°C; 94.5°F) and the other axes represent 24-hour average temperature (°C) and lag period (days). The 3D plot only shows the general pattern of the relationship without the confidence intervals around the estimates. (B) 2D plot of adjusted temperature-mortality relationship for a cumulative distributive lag of 30 days with 95% confidence intervals.
The association between high ambient temperatures and cardiovascular mortality has been demonstrated in vulnerable subgroups in several parts of the world 4. However, in Kuwait, the average temperature is notably higher than other regions in the world previously studied 3. In this study, we specifically assessed the effects of heat on cardiovascular mortality and found that the relative risks of cardiovascular death in Kuwait at extreme temperatures were remarkably high, with a doubling to tripling of CVD mortality.
Possible pathophysiologic mechanisms implicated in CVD mortality from heat include exaggerated thermoregulatory mechanisms and systemic inflammation. During high ambient temperatures, thermoregulatory mechanisms augment blood flow to the skin to ameliorate heat, requiring an increase in cardiac output and potentially precipitating myocardial ischemia in susceptible individuals. When thermoregulatory processes become exhausted, core body temperature may rise precipitously. A rising core temperature may trigger a homeostatic but misaligned systemic inflammatory response ultimately resulting in endothelial dysfunction and direct cytotoxic effects 5, which may provoke acute coronary syndromes.
In summary, in one of the hottest regions in the world, we provide new evidence that higher ambient temperatures associate with higher CVD mortality, with higher relative risks not observed in prior studies. Urgent public health interventions by the international community including heightened awareness among clinicians including cardiologists is warranted.
Acknowledgments
Transparency and Openness Promotion (TOP)
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding Sources:
This publication was made possible by United States Environmental Protection Agency (US EPA) grant RD-835872. Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the US EPA. Further, the US EPA does not endorse the purchase of any commercial products or services mentioned in the publication. The project was also funded by Kuwait Foundation for the Advancement of Sciences under the project code: CR19–13NH-01.
Footnotes
Conflict of Interest Disclosures
Dr. Alahmad has no conflict of interest to disclose.
Dr. Khraishah has no conflict of interest to disclose.
Dr. Shakarchi has no conflict of interest to disclose.
Dr. Albaghdadi has no conflict of interest to disclose.
Dr. Rajagopalan has no conflict of interest to disclose.
Dr. Koutrakis has no conflict of interest to disclose.
Dr. Jaffer has received sponsored research grants from Canon and Siemens; he is a consultant for Boston Scientific, Abbott Vascular, Siemens, Philips, Acrostak, Equity interest, and Intravascular Imaging Incorporated. Massachusetts General Hospital has a patent Licensing arrangement with Canon, and Dr. Jaffer has the right to receive royalties.
References
- 1.Merlone A, Al2010Dashti H, Faisal N, Cerveny RS, AlSarmi S, Bessemoulin P, Brunet M, Driouech F, Khalatyan Y, Peterson TC et al. Temperature extreme records: World Meteorological Organization metrological and meteorological evaluation of the 54.0°C observations in Mitribah, Kuwait and Turbat, Pakistan in 2016/2017. Int J Climatol. 2019; 39;5154–5169. [Google Scholar]
- 2.Pal JS, Eltahir EAB. Future temperature in southwest Asia projected to exceed a threshold for human adaptability. Nat Clim Chang. 2015;6;197. [Google Scholar]
- 3.Alahmad B, Shakarchi A, Alseaidan M, Fox M. The effects of temperature on short-term mortality risk in Kuwait: A time-series analysis. Environ Res. 2019;171:278–284. [DOI] [PubMed] [Google Scholar]
- 4.Basu R High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health. 2009;8:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epstein Y, Yanovich R. Heatstroke. N Engl J Med. 2019;380:2449–2459. [DOI] [PubMed] [Google Scholar]