Abstract
Background:
Diabetes is associated with higher risk of hospitalization, morbidity, and mortality from influenza. We assessed influenza vaccination coverage among adults aged ≥18 years with diabetes during the 2007–08 through 2017–18 influenza seasons and identified factors independently associated with vaccination during the 2017–18 season.
Methods:
We analyzed data from the 2007–2018 National Health Interview Surveys, using Kaplan-Meier survival analysis to estimate season-specific influenza vaccination coverage. Multivariable logistic regression was conducted to examine whether diabetes was independently associated with self-reported influenza vaccination in the past 12 months and identify factors independently associated with vaccination among adults with diabetes using the 2017–18 data.
Results:
During the 2007–08 through 2017–18 influenza seasons, influenza vaccination coverage among adults aged ≥18 years with diabetes ranged from 62.6% to 64.8%. In the 2017–18 influenza season, coverage was significantly higher among adults with diabetes (64.8%) compared with those without diabetes (43.9%). Having diabetes was independently associated with an increased prevalence of vaccination after controlling for other factors. Among adults with diabetes, living at or above poverty level, having more physician contacts, having usual place for health care, and being unemployed were independently associated with increased prevalence of vaccination; being 18–64 years and non-Hispanic black were independently associated with decreased prevalence of vaccination.
Conclusions:
Despite specific recommendations for influenza vaccination among people with diabetes, more than one-third of adults with diabetes are unvaccinated. Targeted efforts are needed to increase influenza vaccination coverage among adults with diabetes.
Keywords: Influenza vaccination coverage, diabetes
Introduction
Diabetes is one of the leading causes of morbidity and mortality throughout the world [1]. Individuals with diabetes are particularly susceptible to influenza [2]. Previous studies have shown that diabetes is associated with higher risk of hospitalization, morbidity, and mortality from influenza [3–6]. The Advisory Committee on Immunization Practices (ACIP) and the American Diabetes Association strongly recommend people aged ≥6 months with diabetes receive an influenza vaccination each year [2, 7].
Influenza vaccination coverage among adults aged ≥18 years with diabetes was recently reported to be 61.6% overall in the United States, below the Healthy People 2020 influenza vaccination target of 70% for all adults [8, 9]. One 2015 study examined factors associated with influenza vaccination among adults aged 18–64 years with chronic underlying medical conditions, including diabetes [10], and another study published in 2003 examined impact of access-to-care factors on influenza vaccination among adults with diabetes [11]. However, few studies have been conducted to address factors associated with influenza vaccination specifically among adults with diabetes in the United States. As the prevalence of diabetes in the United States continues to increase [12], efforts to promote influenza vaccination will be vital to reduce influenza-associated complications among adults with diabetes. Assessing influenza vaccination uptake and factors associated with vaccination is important for planning and implementing strategies to improve coverage among persons with diabetes.
This study assesses influenza vaccination coverage among adults aged ≥18 years with and without diabetes during the 2017–18 influenza season, identifies factors associated with influenza vaccination, examines if diabetes was independently associated with self-reported influenza vaccination during the 2017–18 season, and evaluates trends in influenza vaccination coverage among adults with and without diabetes during the 2007–08 through 2017–18 influenza seasons.
Methods
Data from the 2007–2018 National Health Interview Survey (NHIS) were analyzed. The NHIS is a probability-based annual household survey with face-to-face interviews conducted by the National Center for Health Statistics, Centers for Disease Control and Prevention (CDC) [13]. In the sample adult core, one adult per family in each sampled household was randomly selected and asked to complete the sample adult questionnaire, which included questions regarding receipt of influenza vaccination. The final sample adult response rate ranged from 67.8% in 2007 to 53.1% in 2018 [14, 15].
Respondents were asked if they had received an influenza vaccination in the past 12 months, and if so, in which month and year. Missing month and year were imputed (from 1.0% in the 2007–08 season to 3.8% in the 2017–18 season) using the hot-deck imputation method [16]. Individuals who reported that a doctor or other health professional ever told them that they had diabetes (excluding gestational diabetes) were categorized as adults with diabetes. Race/ethnicity was defined using individuals’ self-identification as non-Hispanic white, non-Hispanic black, Hispanic (persons identified as Hispanic might be of any race), non-Hispanic Asian, and non-Hispanic other or multiple races; the five racial/ethnic categories were mutually exclusive. Individuals who reported “working for pay at a job or business,” “with a job or business but not at work,” or “working, but not for pay, at a family-owned job or business” were categorized as “employed”, and individuals who reported “looking for work” or “not working at a job or business and not looking for work” were categorized as “unemployed.” Poverty thresholds for 2017 and 2018 were used for categorizing poverty level in Tables 1 to 3. The poverty thresholds used in the 2018 NHIS were estimated from several sources: weighted average Census poverty thresholds from 2016, average Consumer Price Index from 2016, actual Consumer Price Index values for January–July 2016, and projected Consumer Price Index values for August–December 2016 [15]. The poverty thresholds used in the 2017 NHIS were also estimated from several sources: weighted average Census poverty thresholds from 2015, average Consumer Price Index from 2015, actual Consumer Price Index values for January–July 2015, and projected Consumer Price Index values for August–December 2016 [17]. Having a high-risk condition other than diabetes was defined as follows: individuals who had ever been told by a physician they had emphysema, chronic obstructive pulmonary disease, coronary heart disease, angina, heart attack, or other heart condition; having been diagnosed with cancer in the past 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they had lymphoma, leukemia, or blood cancer; during the past 12 months, having been told by a physician they had chronic bronchitis or weak or failing kidneys; or reporting an asthma episode or attack in the past 12 months. Physical activity was defined as routine engagement in regular light to moderate (at least five times per week for at least 30 minutes at a time) or strenuous (at least three times per week for at least 20 minutes at a time) exercise using the definition from the American College of Sports Medicine Guidelines during the survey period [18].
Table 1.
Weighted distribution of demographic and access-to-care characteristics among adults with and without diabetes — National Health Interview Survey, United States, 2017–18 influenza season
| With diabetes | Without diabetes | |||
|---|---|---|---|---|
| Unweighted | Weighted % | Unweighted | Weighted % | |
| Characteristic | sample size | sample size | ||
| Total | 2,686 | 9.6 | 21,792 | 90.4 |
| Age (in years) | ||||
| 18–49 | 436 | 20.6 | 10,797 | 57.7* |
| 50–64 | 916 | 37.9 | 5,477 | 24.5 |
| ≥65 | 1,334 | 41.5 | 5,518 | 17.8 |
| Sex | ||||
| Male | 1,336 | 52.6 | 9,785 | 47.9* |
| Female | 1,350 | 47.4 | 12,007 | 52.1 |
| Race/ethnicity | ||||
| Non-Hispanic white | 1,738 | 60.7 | 15,225 | 63.9* |
| Non-Hispanic black | 363 | 13.1 | 2,191 | 11.4 |
| Hispanic | 372 | 17.5 | 2,682 | 16.1 |
| Non-Hispanic Asian | 112 | 5.1 | 1,127 | 6.1 |
| Non-Hispanic other or multiple races | 101 | 3.6 | 567 | 2.6 |
| Marital Status | ||||
| Married | 1,199 | 56.5 | 9,742 | 52.0* |
| Widowed/divorced/separated | 1,030 | 26.4 | 5,528 | 15.6 |
| Never married | 452 | 17.1 | 6,482 | 32.3 |
| Education | ||||
| High school or less | 1,240 | 46.3 | 7,375 | 34.6* |
| Some college or college graduate | 1,211 | 45.3 | 11,473 | 52.4 |
| Above college graduate | 220 | 8.3 | 2,886 | 13.0 |
| Employment status | ||||
| Employed | 914 | 38.2 | 13,352 | 65.7* |
| Not employed | 1,772 | 61.8 | 8,430 | 34.3 |
| Poverty level | ||||
| At or above poverty | 2,130 | 85.8 | 18,236 | 89.5* |
| Below poverty | 419 | 14.2 | 2,526 | 10.5 |
| Region ‡ | ||||
| Northeast | 388 | 15.1 | 3,482 | 17.5* |
| Midwest | 623 | 21.4 | 5,198 | 22.1 |
| South | 1,110 | 41.0 | 7,988 | 36.7 |
| West | 565 | 22.5 | 5,124 | 23.7 |
| US born status | ||||
| Yes | 2,302 | 81.7 | 18,439 | 81.3 |
| No | 383 | 18.3 | 3,346 | 18.7 |
| Physician contacts within past year | ||||
| None | 115 | 4.8 | 3,605 | 18.4* |
| 1 | 171 | 6.7 | 3,954 | 19.6 |
| 2–3 | 596 | 23.6 | 5,955 | 27.8 |
| 4–9 | 1,043 | 38.6 | 5,055 | 21.9 |
| ≥10 | 718 | 26.3 | 2,925 | 12.3 |
| Hospitalization within past year | ||||
| Yes | 509 | 18.0 | 1,911 | 7.8* |
| No | 2,174 | 82.0 | 19,867 | 92.2 |
| Usual place for health care | ||||
| Yes | 2,571 | 96.2 | 18,682 | 85.2* |
| No | 101 | 3.8 | 2,976 | 14.8 |
| Health insurance | ||||
| Yes | 2,542 | 93.9 | 19,699 | 89.7* |
| No | 138 | 6.1 | 2,021 | 10.3 |
| Persons with high-risk conditions other than diabetes † | ||||
| Yes | 1,244 | 43.4 | 4,472 | 17.6* |
| No | 1,429 | 56.6 | 17,271 | 82.4 |
| Physical activity | ||||
| Yes | 644 | 25.9 | 8,816 | 41.5* |
| No | 2,023 | 74.1 | 12,798 | 58.5 |
p<0.05 by Chi-square test comparing distribution among those with and without diabetes.
Persons with high-risk conditions other than diabetes included persons who have heart disease, lung diseases, end-stage renal failure, chronic obstructive pulmonary disease, or cancer (excluding non-melanoma skin cancer).
Northeast: Maine, New Hampshire, Vermont, Massachusetts, Rhode Island, Connecticut, New York, New Jersey, and Pennsylvania; Midwest: Ohio, Michigan, Indiana, Wisconsin, Illinois, Minnesota, Iowa, Missouri, North Dakota, South Dakota, Nebraska, and Kansas; South: Delaware, Maryland, Virginia, District of Columbia, West Virginia, Kentucky, North Carolina, South Carolina, Tennessee, Georgia, Florida, Alabama, Mississippi, Arkansas, Louisiana, Texas, and Oklahoma; West: Montana, Idaho, Wyoming, Colorado, New Mexico, Arizona, Utah, Nevada, California, Oregon, Washington, Alaska, and Hawaii.
Table 3.
Multivariate logistic regression analyses of adults with and without diabetes who reported receiving influenza vaccination,* by demographic and access-to-care characteristics — National Health Interview Survey, United States, 2017–18 season
| Adjusted prevalence ratio among adults with diabetes | Adjusted prevalence ratio among adults without diabetes | |
|---|---|---|
| Characteristic | (95% CI)† | (95% CI)† |
| Age (in years) | ||
| 18–49 | 0.63 (0.55–0.72)‡ | 0.62 (0.59–0.65)‡ |
| 50–64 | 0.85 (0.78–0.92)‡ | 0.71 (0.68–0.75)‡ |
| ≥65 | Reference | Reference |
| Sex | ||
| Male | 0.96 (0.89–1.03) | 0.93 (0.90–0.96)‡ |
| Female | Reference | Reference |
| Race/ethnicity | ||
| Non-Hispanic white | Reference | Reference |
| Non-Hispanic black | 0.86 (0.75–0.98)‡ | 0.91 (0.85–0.98)‡ |
| Hispanic | 0.95 (0.84–1.07) | 1.06 (1.00–1.13) |
| Non-Hispanic Asian | 1.13 (0.96–1.33) | 1.16 (1.06–1.27) |
| Non-Hispanic other or multiple races | 1.15 (0.97–1.36) | 0.88 (0.77–1.01) |
| Marital Status | ||
| Married | 1.10 (0.98–1.22) | 1.12 (1.07–1.18)‡ |
| Widowed/divorced/separated | 1.04 (0.92–1.17) | 1.03 (0.97–1.09) |
| Never married | Reference | Reference |
| Education | ||
| High school or less | Reference | Reference |
| Some college or college graduate | 0.95 (0.87–1.03) | 1.15 (1.10–1.21)‡ |
| Above college graduate | 1.11 (0.99–1.25) | 1.45 (1.37–1.54)‡ |
| Employment status | ||
| Employed | Reference | Reference |
| Not employed | 1.10 (1.01–1.20)‡ | 1.03 (0.98–1.08) |
| Poverty level | ||
| At or above poverty | 1.17 (1.03–1.33)‡ | 1.00 (0.93–1.07) |
| Below poverty | Reference | Reference |
| Region | ||
| Northeast | Reference | Reference |
| Midwest | 0.98 (0.87–1.11) | 1.02 (0.96–1.08) |
| South | 0.97 (0.86–1.09) | 0.96 (0.90–1.02) |
| West | 0.98 (0.86–1.11) | 0.97 (0.91–1.04) |
| US born status | ||
| Yes | Reference | Reference |
| No | 0.98 (0.87–1.12) | 0.96 (0.89–1.03) |
| Physician contacts within past year | ||
| None | Reference | Reference |
| 1 | 1.09 (0.82–1.45) | 1.48 (1.35–1.62)‡ |
| 2–3 | 1.09 (0.87–1.38) | 1.74 (1.60–1.89)‡ |
| 4–9 | 1.25 (0.99–1.57) | 1.82 (1.67–1.98)‡ |
| ≥10 | 1.38 (1.09–1.74)‡ | 1.88 (1.72–2.06)‡ |
| Hospitalization within past year | ||
| Yes | 1.05 (0.96–1.16) | 1.06 (0.99–1.13) |
| No | Reference | Reference |
| Usual place for health care | ||
| Yes | 1.64 (1.14–2.36)‡ | 1.34 (1.24–1.45)‡ |
| No | Reference | Reference |
| Health insurance | ||
| Yes | 1.25 (1.00–1.55) | 1.51 (1.35–1.69)‡ |
| No | Reference | Reference |
| Persons with high-risk conditions other than diabetes § | ||
| Yes | 0.95 (0.89–1.02) | 1.12 (1.07–1.17)‡ |
| No | Reference | Reference |
| Physical activity | ||
| Yes | 1.06 (0.98–1.15) | 1.04 (1.00–1.08) |
| No | Reference | Reference |
Respondents were asked if they had received an influenza shot or nasal spray in the past 12 months, and if so, in which month and year.
Adjusted prevalence ratios, adjusted for all variables included in the table.
p<0.05 by t-test for comparison within each covariate category with the indicated reference level.
Persons with high-risk conditions other than diabetes included persons who have heart disease, lung diseases, end-stage renal failure, chronic obstructive pulmonary disease, or cancer (excluding non-melanoma skin cancer).
SUDAAN (Research Triangle Institute, Research Triangle Park, NC, version 11.01) was used to calculate point estimates and 95% confidence intervals (CI). To better assess influenza vaccination coverage during the 2007–08 through 2017–18 seasons, we reported coverage restricted to individuals interviewed during August of the prior year through June of the next year and vaccinated during July of the prior year through May of the next year using the Kaplan-Meier analysis procedure [19]. In the 2007–08 through the 2017–18 seasons, the NHIS analytic sample size among adults ranged from 17,216 to 33,110. Individuals who refused to answer the influenza vaccination question or did not know their vaccination status (about 2.7% annually) were excluded from the analysis. Chi-squared tests were used to compare characteristics of the study population between adults with and without diabetes. T-tests were conducted to test differences in influenza vaccination coverage between those with and without diabetes, and differences within each characteristic category compared to their respective reference levels.
Multivariate logistic regression was conducted using 2017–18 NHIS data to identify factors independently associated with influenza vaccination among adults with and without diabetes. Prevalence ratios were estimated using predictive marginals from the logistic regression models. A separate logistic regression model was conducted, including diabetes status as an independent variable, to determine if diabetes status was an independent predictor of vaccination. All variables used in the bivariate analyses were included in the full multivariable model. A linear trend analysis was conducted to assess influenza vaccination coverage by age group during the 2007–08 through 2017–18 influenza seasons. All analyses were weighted to represent the age, sex, and racial/ethnic composition of the U.S. non-institutionalized, civilian population. All tests were 2-tailed with the significance level set at α<0.05.
Results
Table 1 shows the characteristics of the study population. Of the 24,478 respondents in the NHIS sample adult core interviewed August 2017 through June 2018, 9.6% (n = 2,686) reported being diagnosed with diabetes. The majority of adults with diabetes were aged 18–64 years (58.5%), male (52.6%), non-Hispanic white (60.7%), married (56.5%), had some college or higher education (53.6%), unemployed (61.8%), at or above poverty (85.8%), had two or more physician contacts in the past year (88.5%), had a usual place for health care (96.2%), had health insurance (93.9%), had no high-risk conditions other than diabetes (56.6%), and reported no regular exercise (74.1%) (Table 1). Population distributions differed significantly between adults with diabetes and adults without diabetes for all assessed characteristics except whether the individual had been born in the United States (Table 1).
Bivariate analyses of influenza vaccination coverage
Table 2 shows influenza vaccination coverage by diabetes status, and demographic and access-to-care characteristics among adults during the 2017–18 influenza season. Overall, influenza vaccination coverage among adults aged ≥18 years was significantly higher among those with diabetes (64.8%) than without (43.9%). Vaccination coverage among adults with diabetes was significantly higher compared with those without diabetes across all socio-demographic and access-to-care characteristics except for adults aged ≥65 years (Table 2). Among adults with diabetes, influenza vaccination coverage was significantly higher among those who were married, widowed, divorced, or separated compared with those who were never married; had above college education; were unemployed; lived at or above poverty level; had two or more physician contacts in the past year; were hospitalized in the past year; had a usual place for health care; and had health insurance compared with their respective reference levels (Table 2). Influenza vaccination coverage was significantly lower among adults with diabetes aged <65 years and non-Hispanic blacks compared with those ≥65 or non-Hispanic whites, respectively (Table 2).
Table 2.
Influenza vaccination coverage* by demographic and access-to-care characteristics among adults with and without diabetes — National Health Interview Survey, United States, 2017–18 season
| With diabetes | Without diabetes | |||
|---|---|---|---|---|
| Weighted % vaccinated | Weighted % vaccinated | |||
| Characteristic | (95% CI) | (95% CI) | ||
| Total | 64.8 (61.7–67.9) | 43.9 (42.7–45.1)‡ | ||
| Age (in years) | ||||
| 18–49 | 45.9 (38.6–53.9)§ | 34.5 (33.0–36.1)‡,§ | ||
| 50–64 | 63.0 (58.0–68.0)§ | 45.7 (43.6–47.8)‡,§ | ||
| ≥65|| | 75.3 (71.4–79.0) | 71.3 (69.1–73.5) | ||
| Sex | ||||
| Male | 64.1 (59.9–68.3) | 39.6 (38.0–41.3)‡,§ | ||
| Female|| | 65.6 (61.1–70.0) | 47.9 (46.3–49.5)‡ | ||
| Race/ethnicity | ||||
| Non-Hispanic white|| | 67.6 (64.1–71.1) | 47.2 (46.0–48.5)‡ | ||
| Non-Hispanic black | 54.4 (46.4–62.9)§ | 36.9 (33.3–40.8)‡,§ | ||
| Hispanic | 58.6 (48.5–68.9) | 35.6 (32.5–38.9)‡,§ | ||
| Non-Hispanic Asian | 71.5 (59.3–82.7) | 48.4 (43.7–53.3)‡ | ||
| Non-Hispanic other or multiple races | 74.7 (58.4–88.3) | 34.8 (28.9–41.4)‡,§ | ||
| Marital Status | ||||
| Married | 67.5 (63.6–71.4)§ | 49.2 (47.6–50.9)‡,§ | ||
| Widowed/divorced/separated | 66.9 (61.9–71.7)§ | 50.7 (48.4–52.9)‡,§ | ||
| Never married|| | 52.5 (45.0–60.4) | 32.0 (30.1–33.9)‡ | ||
| Education | ||||
| High school or less|| | 64.4 (59.8–68.9) | 36.5 (34.6–38.5)‡ | ||
| Some college or college graduate | 64.1 (59.3–68.8) | 44.6 (43.0–46.2)‡,§ | ||
| Above college graduate | 74.8 (65.9–83.0)§ | 60.7 (58.0–63.4)‡,§ | ||
| Employment status | ||||
| Employed|| | 55.8 (50.9–61.0) | 39.5 (38.1–41.0)‡ | ||
| Not employed | 70.6 (66.9–74.2)§ | 52.5 (50.6–54.5)‡,§ | ||
| Poverty level | ||||
| At or above poverty | 66.3 (62.9–69.6)§ | 44.8 (43.6–46.1)‡,§ | ||
| Below poverty|| | 51.9 (43.2–61.1) | 34.9 (31.9–38.2)‡ | ||
| Region | ||||
| Northeast|| | 68.4 (60.2–76.4) | 48.4 (45.5–51.4)‡ | ||
| Midwest | 63.6 (57.8–69.4) | 45.5 (43.6–47.5)‡ | ||
| South | 61.7 (57.2–66.3) | 42.1 (40.0–44.2)‡,§ | ||
| West | 69.2 (61.4–76.7) | 42.1 (39.6–44.6)‡,§ | ||
| US born status | ||||
| Yes|| | 65.4 (62.2–68.6) | 44.8 (43.6–46.1)‡ | ||
| No | 61.3 (52.8–69.9) | 40.2 (37.3–43.3)‡,§ | ||
| Physician contacts within past year | ||||
| None|| | 39.6 (28.5–53.1) | 17.7 (16.0–19.6)‡ | ||
| 1 | 52.7 (41.5–64.8) | 38.0 (35.7–40.5)‡,§ | ||
| 2–3 | 57.6 (51.1–64.2)§ | 50.0 (47.7–52.3)‡`,§ | ||
| 4–9 | 69.4 (64.2–74.5)§ | 55.8 (53.4–58.4)‡,§ | ||
| ≥10 | 72.0 (66.9–76.8)§ | 56.7 (53.8–59.7)‡,§ | ||
| Hospitalization within past year | ||||
| Yes | 71.5 (65.3–77.5)§ | 57.5 (53.6–61.5)‡,§ | ||
| No|| | 63.3 (59.8–66.7) | 42.7 (41.5–44.0)‡ | ||
| Usual place for health care | ||||
| Yes | 66.1 (63.0–69.2)§ | 48.5 (47.2–49.8)‡,§ | ||
| No|| | 39.2 (27.8–53.3) | 17.7 (15.7–19.9)‡ | ||
| Health insurance | ||||
| Yes | 66.1 (63.0–69.2)§ | 47.3 (46.1–48.6)‡,§ | ||
| No|| | 39.2 (27.8–53.3) | 14.6 (12.3–17.2)‡ | ||
| Persons with high-risk conditions other than diabetes † | ||||
| Yes | 66.6 (62.3–70.9) | 58.4 (56.2–60.7)‡,§ | ||
| No|| | 63.2 (59.0–67.4) | 40.8 (39.5–42.1)‡ | ||
| Physical activity | ||||
| Yes | 62.6 (57.0–68.3) | 43.9 (42.2–45.6)‡ | ||
| No|| | 65.4 (61.8–68.9) | 44.0 (42.5–45.5)‡ | ||
Respondents were asked if they had received an influenza shot or nasal spray in the past 12 months, and if so, in which month and year. Interviews conducted during August 2017 through June 2018 were used to estimate vaccination coverage during July 2017 through May 2018 using Kaplan–Meier survival analysis.
Persons with high-risk conditions other than diabetes included persons who have heart disease, lung diseases, end-stage renal failure, chronic obstructive pulmonary disease, or cancer (excluding non-melanoma skin cancer).
p<0.05 by t-test for comparison between adults with and without diabetes within each level of each characteristic.
p<0.05 by t-test for comparison within each variable with the indicated reference level.
Reference level.
Multivariate analyses of influenza vaccination coverage
Table 3 shows adjusted prevalence ratios of influenza vaccination by diabetes status and demographic and access-to-care characteristics among adults during the 2017–18 influenza season. Having ten or more physician contacts within the past year and having a usual place for health care were the common factors that were independently associated with increased prevalence of vaccination compared with the reference groups across diabetes status (with diabetes and without diabetes); being younger (aged 18–64 years) and non-Hispanic blacks were the common factors that were independently associated with decreased prevalence of vaccination compared with the reference groups (Table 3). Being unemployed and living at/above poverty level were independently associated with increased prevalence of vaccination among adults with diabetes but not among those without diabetes (Table 3). In addition, in multivariate analyses with diabetes status as the independent variable, adults with diabetes were found to have a significantly associated increased prevalence of vaccination (adjusted prevalence ratio 1.1 [95% CI = 1.1–1.2], p<0.05) compared with those without diabetes after controlling for all of demographic and access-to-care characteristics assessed, and one interaction term between age group and diabetes status (data not shown). The interaction between age group and diabetes status was significant, especially, among those with diabetes vs. without diabetes of adults aged 50–64 years and ≥65 years (data not shown).
Trend test of influenza vaccination coverage
Figure 1 shows the trends in influenza vaccination coverage from the 2007–08 to 2017–18 seasons. From the 2007–08 to 2017–18 influenza seasons, influenza vaccination coverage among adults aged ≥18 years with diabetes ranged from 62.6% to 64.8% (data not shown), and linear trend tests indicated coverage did not significantly change for adults with diabetes aged ≥18 years (data not shown), 18–49 years, 50–64 years, and ≥65 years. In contrast, coverage significantly increased for adults aged ≥18 years, 18–49 years, 50–64 years, and ≥65 years without diabetes during the 2007–08 through 2017–18 seasons. For all years, within each age group, coverage was significantly higher among adults with than without diabetes (data not shown).
Figure 1.
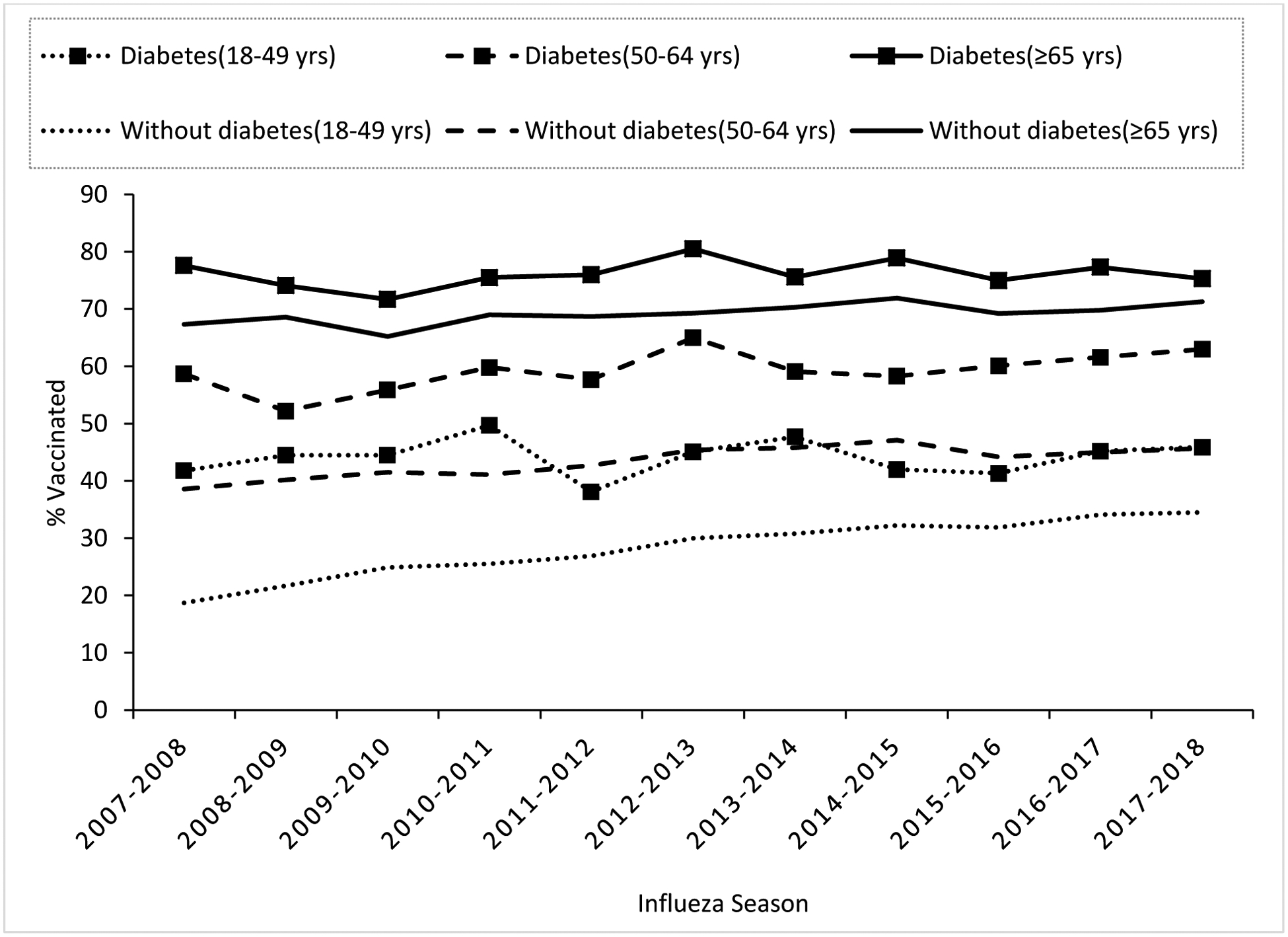
Seasonal influenza vaccination coverage trends by age group among adults with and without diabetes — National Health Interview Survey, United States, 2007–08 through the 2017–18 influenza seasons*.
* Interviews from August of the prior year through June of the next year of each influenza season were used to estimate coverage from July of the prior year through May of the next year using Kaplan-Meier survival analysis. Coverage significantly increased for adults without diabetes aged 18–49 years, 50–64 years, and ≥65 years during the 2007–08 through 2017–18 seasons.
Discussion
Influenza vaccination coverage and factors associated with vaccination among adults with diabetes in the United States have been previously investigated [8, 11]. However, this study was the first study on trends in influenza vaccination coverage among adults with and without diabetes during the 2007–08 through 2017–18 influenza seasons in the United States. Influenza vaccination coverage among adults with diabetes has not changed significantly over the 11 influenza seasons assessed in this study and has remained below the national target of 70% for all adults [9]. Bivariate analysis and multivariate models identified multiple factors associated with higher or lower likelihood of vaccination among persons with diabetes. Among persons with diabetes, vaccination coverage varied significantly by demographic and access-to-care characteristics known to be associated with higher likelihood of influenza vaccination, including older age, being non-Hispanic white, having a usual place for health care, and having multiple contacts with physicians within the past year [10, 11, 20–23].
As has been reported previously [10, 20–22], this study showed that influenza vaccination coverage was lower among younger adults with diabetes. Older adults who have diabetes have significantly higher influenza vaccination coverage, likely related to greater likelihood of having other high-risk conditions or co-morbidities, more physician visits, and a usual place for health care [10], more at risk for influenza complications, and thus having more opportunities for education about influenza and influenza vaccination. Improving awareness of recommendations for adult vaccination and providing vaccination in work settings might improve coverage in younger adults with diabetes. Additionally, health care providers treating adults with diabetes should ensure that these patients are offered appropriate vaccinations regardless of age. Findings from this study indicated that, among adults with diabetes, non-Hispanic whites were more likely than non-Hispanic blacks to receive influenza vaccination. This result is similar to the findings from previous studies [10, 23]. In general, older African American adults reported more negative attitudes toward influenza vaccination than older white adults [24]. Additionally, non-Hispanic black adults are more likely to have low family income, higher poverty rates, and be uninsured [25]. Studies of standardized offering of influenza vaccines have demonstrated reductions in racial and ethnic vaccination coverage disparities [26]. Activities to reduce the number of uninsured adults and related barriers to care could help reduce racial/ethnic vaccination differences as well.
Influenza vaccination coverage among adults with diabetes who were unemployed was significantly higher than those who were employed. Of adults who were unemployed (unemployed includes “retired”), more than 58% were those aged ≥65 years. Adults with diabetes aged ≥65 years who are unemployed may be more likely to have other high-risk conditions, and thus may have more chances to access the medical system and receive vaccinations.
Select access-to-care characteristics were associated with influenza vaccination among adults with diabetes. In particular, as noted in a previous study [11], those who had ≥10 physician contacts in the past 12 months more frequently reported vaccination than those who did not. In this study, there were missed opportunities for influenza vaccination among persons with diabetes, even those reporting multiple contacts with physicians. For example, approximately 95.2% of adults with diabetes reported having one or more physician contacts in the past year, but a substantial proportion of these (~28.0%) still reported not having received an influenza vaccination. A previous study reported that although most physicians thought that it is very important for high-risk patients—including those with diabetes—to receive influenza vaccination, only 86% of generalists and 75% of subspecialists very strongly recommended influenza vaccination to their elderly and high-risk patients [27]. In addition, according to the 2017 National Practice Survey from the American Association of Diabetes Educators, only 31% of diabetes educators offer information or discuss immunization with patients [28]. In addition to health care providers not recommending influenza vaccination to their high-risk patients, missed opportunities for influenza vaccination also might be due to refusal of vaccination by patients, because they do not believe influenza vaccination is effective or fear side effects of the vaccine [22, 29]. Physicians and diabetes educators should routinely discuss needed vaccinations with persons who have diabetes and recommend vaccination.
Our study also showed that approximately 4.8% of adults with diabetes did not visit a physician in the past year, yet among those who reported not having a physician contact, about 40% reported having received influenza vaccination. Although persons with diabetes who reported two or more physician contacts within the past year were much more likely to have received influenza vaccination than those reporting no contacts, this finding indicates that even those who do not see physicians regularly but who have a high-risk condition like diabetes still may receive vaccination. Campaigns to increase influenza vaccination access in nonmedical settings [30, 31], especially pharmacies [32, 33], could thus be an effective way to improve vaccination coverage among such adults.
From the 2007–08 through 2017–18 influenza seasons, no significant changes in influenza vaccination coverage for adults with diabetes were observed even though influenza vaccination coverage among adults without diabetes increased in the same time period. The reasons for this plateau in vaccination coverage are not well understood. Even though influenza vaccination recommendations have expanded to include all persons aged ≥6 months since the 2010–11 season [34], the ACIP continues to emphasize that persons with high-risk conditions including diabetes should be a focus of vaccination efforts [2].
The findings in this study are subject to several limitations. First, these analyses included only the non-institutionalized population and cannot be generalized to persons residing in nursing homes and other institutions. Second, influenza vaccination status was based on self-report and might be subject to recall and social desirability bias. However, self-reported influenza vaccination status has been shown to have relatively high agreement with influenza vaccination from medical records [35, 36]. Third, diagnoses of persons with diabetes and other high-risk conditions were determined from self-report and not validated by medical records. However, self-report of diabetes is highly accurate from physical examination and laboratory testing [37]. Finally, in the multivariate models, however, no specific causal model or hypothesis was posed for the relationship of vaccination with each of the demographic, health status, and access-to-care characteristics considered in this report; thus, the significant findings from both bivariate and multivariate analysis should be considered in interpreting the findings from this report.
Conclusions
Despite longstanding specific recommendations for influenza vaccination among persons with diabetes, more than one-third were unvaccinated. Because persons with diabetes report a high rate of routine medical care compared with those without diabetes, use of standing order programs and reminder and recall systems for patients and providers during influenza season could have a large impact on improving vaccination coverage [38]. Campaigns to increase influenza vaccination at nonmedical settings (such as workplaces and pharmacies) for persons who do not routinely use or have access to medical settings [38] may also increase vaccination rates. Primary care physicians and diabetes educators [28] need to make a concerted effort to discuss and help persons with diabetes obtain regular preventative vaccinations to maximize their protection of preventable infectious diseases. Pharmacy vaccination is important because of this group’s likelihood of frequent pharmacy encounters to purchase glucometer strips or similar supplies [39]. Pharmacies, could thus be an effective way to improve influenza vaccination coverage among persons with diabetes.
In addition, according to the 2020 National Diabetes Statistics Report [40], 21.4% of people with diabetes are undiagnosed. The importance of increasing diagnosis of diabetes is essential, so people with diabetes can receive the treatment they need and be encouraged to get influenza vaccination. Increasing adult influenza vaccination in general population is also important because it would increase protection among these undiagnosed adults who are unaware of their increased risk of influenza. CDC has implemented state-based diabetes control programs to encourage health care professionals to recommend influenza vaccination [30]. Continued surveillance of diabetes-related preventive-care practices, burden, and magnitude will be important for monitoring the effectiveness of strategies to improve the quality of diabetes care among persons with diabetes [41], including receipt of influenza vaccination.
Acknowledgments
Authors thank Mary Ann Hall, James A. Singleton, and Kimberly Nguyen for their important review of this manuscript.
Abbreviations:
- ACIP
Advisory Committee on Immunization Practices
- NHIS
National Health Interview Survey
- CDC
Centers for Disease Control and Prevention
- CI
confidence intervals
Footnotes
Conflict of Interest
All authors have no conflicts of interest to be stated.
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of CDC.
References
- 1.International Diabetes Federation. About diabetes. Available from https://www.idf.org/aboutdiabetes/complications.html. Accessed 20 May 2019.
- 2.Centers for Disease Control and Prevention. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2019–20 Influenza Season. MMWR 2019; 68(3):1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouter KP, Diepersloot RJ, van Romunde LK, et al. Effect of epidemic influenza on ketoacidosis, pneumonia and death in diabetes mellitus: a hospital register survey of 1976–1979 in The Netherlands. Diabetes Res Clin Pract 1991;12(1):61–68. [DOI] [PubMed] [Google Scholar]
- 4.Colquhoun AJ, Nicholson KG, Botha JL, Raymond NT. Effectiveness of influenza vaccine in reducing hospital admissions in people with diabetes. Epidemiol Infect 1997;119(3):335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Valdez R, Narayan KMV, Geiss LS, Engelgau MM. The impact of diabetes mellitus on mortality associated with pneumonia and influenza among non-Hispanic black and white U.S. adults. Am J Public Health 1999;89(11):1715–1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. Immunization and the prevention of influenza and pneumococcal disease in people with diabetes. Diabetes Care 2003;26(Suppl. 1):S126–S128. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association. Comprehensive medical evaluation and assessment of comorbidities: standards of medical care in diabetes–2019. Diabetes Care 2019; 42(Suppl 1):S34–S45. [DOI] [PubMed] [Google Scholar]
- 8.Villarroel MA, Vahratian A. Vaccination coverage among adults with diagnosed diabetes: United States, 2015. NCHS Data Brief 2016;265:1–8. [PubMed] [Google Scholar]
- 9.U.S. DHHS: Immunization and infectious diseases. Available from https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases. Accessed 21 February 2019.
- 10.Lu PJ, O’Halloran A, Ding H, Srivastav A, Williams WW. Uptake of influenza vaccination and missed opportunities among adults with high-risk conditions, United States, 2013. Am J Med 2016;129(6):636.e1–636.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egede LE. Association between number of physician visits and influenza vaccination coverage among diabetic adults with access to care. Diabetes Care 2003;26(9):2562–2567. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention: Diagnosed Diabetes. Available from https://gis.cdc.gov/grasp/diabetes/DiabetesAtlas.html. Accessed 21 February 2019.
- 13.Centers for Disease control and Prevention: National Health Interview Survey. Available from https://www.cdc.gov/nchs/data/factsheets/factsheet_nhis.htm. Accessed 21 February 2019.
- 14.Centers for Disease Control and Prevention: 2007 National Health Interview Survey (NHIS): Public use data release. Available from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2007/srvydesc.pdf. Accessed 21 February 2019.
- 15.Centers for Disease Control and Prevention: 2018 National Health Interview Survey (NHIS): Public use data release. Available from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2018/srvydesc.pdf. Accessed 6 December 2019.
- 16.Zhai Y, Santibanez TA, Kahn KE, Srivastav A. Parental-reported full Influenza vaccination coverage of children in the U.S. Am J Prev Med 2017; 52(4): e103–e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention: 2017 National Health Interview Survey. Available from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2017/srvydesc.pdf. Accessed 6 December 2019.
- 18.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exercise 2007;39(8):1423–1434. [DOI] [PubMed] [Google Scholar]
- 19.Lu PJ, Ding H, Black CL. H1N1 and seasonal influenza vaccination of U.S. healthcare personnel, 2010. Am J Prev Med 2012; 43(3):282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shin HY, Chung JH, Hwang HJ, Kim TH. Factors influencing on influenza vaccination and its trends of coverage in patients with diabetes in Korea: A population-based cross-sectional study. Vaccine 2018;36(1):91–97. [DOI] [PubMed] [Google Scholar]
- 21.Yu MC, Chou YL, Lee PL, Yang YC, Chen KT. Influenza vaccination coverage and factors affecting adherence to influenza vaccination among patients with diabetes in Taiwan. Hum Vaccin Immunother 2014;10(4):1028–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiménez-Garcia R, Lopez-de-Andres A, Hernandez-Barrera V, et al. Influenza vaccination in people with type 2 diabetes, coverage, predictors of uptake, and perceptions. Results of the MADIABETES cohort a 7 year follow up study. Vaccine 2017; 35(1):101–108. [DOI] [PubMed] [Google Scholar]
- 23.Athamneh LN, Sansgiry SS. Influenza vaccination in patients with diabetes: disparities in prevalence between African Americans and Whites. Pharm Pract (Granada) 2014; 12(2):410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lindley MC, Wortley PM, Winston CA, Bardenheier BH. The role of attitudes in understanding disparities in adult influenza vaccination. Am J Prev Med 2006; 31(4):281–285. [DOI] [PubMed] [Google Scholar]
- 25.U.S. Census Bureau: Income, Poverty and Health Insurance Coverage in the United States: 2017. Available from https://www.census.gov/newsroom/press-releases/2018/income-poverty.html. Accessed 6 December 2019.
- 26.Schwartz KL, Neale AV, Northrup J, et al. Racial similarities in response to standardized offer of influenza vaccination. J Gen Intern Med 2006;21:346–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nichol KL, Zimmerman R. Generalist and subspecialist physicians’ knowledge, attitudes, and practices regarding influenza and pneumococcal vaccinations for elderly and other high-risk patients: a nationwide survey. Arch Intern Med 2001;161(22):2702–2708 [DOI] [PubMed] [Google Scholar]
- 28.American Association of Diabetes Educators (AADE): Vaccination practice for people with diabetes. 2017. Available from https://www.diabeteseducator.org/docs/default-source/practice/educator-tools/vaccination-practices-for-adults-with-diabetesv2.pdf?sfvrsn=2. Accessed 12 March 2019.
- 29.Alvarez CE, Clichici L, Patricia Guzmán-Libreros A, Navarro-Francés M, Ena J. Survey of vaccination practices in patients with diabetes: A report examining patient and provider perceptions and barriers. J Clin Transl Endocrinol 2017;9:15–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention (CDC). Influenza and pneumococcal vaccination rates among persons with diabetes mellitus--United States, 1997. MMWR Morb Mortal Wkly Rep 1999;48(42):961–967. [PubMed] [Google Scholar]
- 31.Postema AS, Breiman RF. National Vaccine Advisory Committee: Adult immunization programs in nontraditional settings: quality standards and guidance for program evaluation. MMWR Recomm Rep 2000;49(RR-1):1–13. [PubMed] [Google Scholar]
- 32.Lu PJ, O’Halloran A, Ding H, Williams WW, Bridges CB, Kennedy ED. National and state-specific estimates of place of influenza vaccination among adult populations - United States, 2011–12 influenza season. Vaccine. 2014;32(26):3198–3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC). National and state-level place of flu vaccination among vaccinated adults in the United States, 2014–15 Flu Season. Available at: https://www.cdc.gov/flu/fluvaxview/place-vaccination-2014-15.htm. Accessed April 30, 2020.
- 34.Centers for Disease Control and Prevention (CDC). Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices. MMWR 2010; 59(RR08);1–62. [Google Scholar]
- 35.Zimmerman RK, Raymund M, Janosky JE, Nowalk MP, Fine MJ. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine 2003;21(13–14):1486–1491. [DOI] [PubMed] [Google Scholar]
- 36.Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect 2006;135(1):139–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bowlin SJ, Morrill BD, Nafziger AN, Lewis C, Pearson TA. Reliability and changes in validity of self-reported cardiovascular disease risk factors using dual response: the Behavioral Risk Factor Survey. J Clin Epidemiol 1996;49(5):511–517. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. Vaccine-Preventable Diseases. Improving Vaccination Coverage in Children, Adolescents, and Adults: A Report on Recommendations from the Task Force on Community Preventive Services. MMWR Recomm Rep 1999;48(RR-8):1–15. [PubMed] [Google Scholar]
- 39.American Association of Diabetes Educators (AADE): 3 Ways to Improve Access to Vaccines for People with Diabetes in Your Practice. 2019. Available from https://https://www.diabeteseducator.org/news/perspectives/aade-blog-details/adces-perspectives-on-diabetes-care/2019/10/08/3-ways-to-improve-access-to-vaccines-for-people-with-diabetes-in-your-practice. Accessed 22 May 2020.
- 40.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020. [Google Scholar]
- 41.Centers for Disease Control and Prevention: United States Diabetes Surveillance System. Available from https://www.cdc.gov/diabetes/data/index.html. Accessed 21 February 2019.


