Key Points
Question
What are the trends in 10-year mortality and hospitalization for recurrence among Medicare beneficiaries with acute myocardial infarction (AMI) in the US who survived 30 days after hospitalization?
Findings
In this cohort study including 3 982 266 beneficiaries with AMI, rates of 10-year mortality and hospitalization for recurrence were 72.7% and 27.1%, respectively. Men, Black patients, and dual Medicare-Medicaid–eligible patients had higher risks of adverse outcomes, and significant annual reductions in 10-year outcomes (mortality, 1.5%; recurrence, 2.7%) were observed.
Meaning
In this study, 10-year mortality and hospitalization for AMI recurrence among AMI survivors improved over the past 25 years, but there were differences in outcomes and trends over time by demographic subgroups.
This cohort study evaluates trends in 10-year all-cause mortality and hospitalization for recurrent acute myocardial infarction by demographic subgroups and examines the association between recurrence and mortality.
Abstract
Importance
Short-term outcomes after acute myocardial infarction (AMI) have improved, but little is known about longer-term outcomes.
Objective
To evaluate trends in 10-year all-cause mortality and hospitalization for recurrent AMI by demographic subgroups and examine the association between recurrence and mortality.
Design, Setting, and Participants
Medicare fee-for-service beneficiaries who survived after AMI from 1995 to 2019. Subgroups were defined by age, sex, race, dual Medicare-Medicaid–eligible status, and residence in health priority areas (geographic areas with persistently high adjusted mortality and hospitalization rates). Data were analyzed from October 2020 to February 2022.
Exposure
Medicare fee-for-service beneficiaries who survived an AMI.
Main Outcomes and Measures
Ten-year all-cause mortality and hospitalization for recurrent AMI, beginning 30 days from the index AMI admission.
Results
Of an included 3 982 266 AMI survivors, 1 952 450 (49.0%) were female, and the mean (SD) age was 78.0 (7.4) years. Ten-year mortality and recurrent AMI rates were 72.7% (95% CI, 72.6-72.7) and 27.1% (95% CI, 27.0-27.2), respectively. Adjusted annual reductions were 1.5% (95% CI, 1.4-1.5) for mortality and 2.7% (95% CI, 2.6-2.7) for recurrence. In subgroup analyses balancing patient characteristics, hazard ratios (HRs) for mortality and recurrence were 1.13 (95% CI, 1.12-1.13) and 1.07 (95% CI, 1.06-1.07), respectively, for men vs women; 1.05 (95% CI, 1.05-1.06) and 1.08 (95% CI, 1.07-1.09) for Black vs White patients; 0.96 (95% CI, 0.95-0.96) and 1.00 (95% CI, 1.00-1.01) for other race (including American Indian and Alaska Native, Asian, Hispanic, other race or ethnicity, and unreported) vs White patients; 1.24 (95% CI, 1.24-1.24) and 1.21 (95% CI, 1.20-1.21) for dual Medicare-Medicaid–eligible vs non–dual Medicare-Medicaid–eligible patients; and 1.06 (95% CI, 1.06-1.07) and 1.00 (95% CI, 1.00-1.01) for patients in health priority areas vs other areas. For patients hospitalized in 2007 to 2009, the last 3 years for which full 10-year follow-up data were available, 10-year mortality risk was 13.9% lower than for those hospitalized in 1995 to 1997 (adjusted HR, 0.86; 95% CI, 0.85-0.87) and 10-year recurrence risk was 22.5% lower (adjusted HR, 0.77; 95% CI, 0.76-0.78). Mortality within 10 years after the initial AMI was higher for patients with a recurrent AMI (80.6%; 95% CI, 80.5-80.7) vs those without recurrence (72.4%; 95% CI, 72.3-72.5).
Conclusions and Relevance
In this study, 10-year mortality and hospitalization for recurrence rates improved over the last decades for patients who survived the acute period of AMI. There were marked differences in outcomes and temporal trends across demographic subgroups, emphasizing the urgent need for prioritization of efforts to reduce inequities in long-term outcomes.
Introduction
Rates of all-cause 30-day mortality and readmissions for acute myocardial infarction (AMI), 1-year mortality for AMI, and 1-year recurrent AMI have declined over the past few decades in the US.1,2 However, we know less about the progress in longer-term outcomes among those who survive the acute period after AMI. Ideally, improvements in quality and type of care translate into both early mortality gains, which have been documented,1,2,3,4,5 and survivors with lower risk of adverse outcomes. Attention toward secondary prevention in the past decades should also have improved outcomes among survivors. Long-term outcomes can provide insight as to whether short-term improvements translate into better long-term outcomes or whether early gains are subsequently lost. However, there have been few large-scale studies to determine if long-term outcomes have improved.
We used national Medicare fee-for-service data to assess 10-year all-cause mortality and hospitalization for recurrence after AMI from 1995 to 2019, a period with intense focus on improving the quality of hospital care for AMI.5,6,7,8,9 Most AMI occurs in people 65 years and older; this Medicare database is the largest, most comprehensive source of long-term AMI outcome data in the US. We evaluated trends in outcomes overall and by demographic subgroups, and we assessed the association between hospitalization for recurrent AMI and mortality. We also examined trends in mortality and recurrence according to ST-segment elevation myocardial infarction (STEMI) diagnosis and assessed the change in coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI) by demographic subgroups.
Methods
The Yale University Institutional Review Board approved the study and waived informed consent for use of the deidentified database. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Sample
We used Medicare data to identify all beneficiaries 66 years or older enrolled in the fee-for-service program from 1995 to 2019 who were discharged alive after AMI from an acute care hospital in the US. AMI was identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and ICD-10-CM principal discharge diagnosis code (ICD-9-CM codes 410.xx, except 410.x2; ICD-10-CM codes I21.01, I21.02, I21.09, I21.11, I21.19, I21.21, I21.29, I21.3, and I21.4). STEMI was defined according to the principal discharge diagnosis code (ICD-9-CM code 410.9 and ICD-10-CM code I213). For patients with more than 1 AMI hospitalization, we selected the first as the initial event. We linked patients who were transferred from one hospital to another into a single episode of care. To ensure we captured the first AMI, we restricted the cohort to those who were enrolled in Medicare fee-for-service and AMI-free for at least 12 months before the initial AMI (1994 data were used to verify these criteria for patients in 1995). We excluded patients with a length of stay (LOS) of 1 day or less who did not have an intensive care unit or coronary care unit stay and were discharged to home because these patients were unlikely to have had an AMI. We also excluded patients who had invalid dates of death and hospitalization and those who died within 30 days from the initial AMI admission date. This 30-day window allowed us to overcome potential bias from the decline in LOS during the follow-up period. Because the maximum number of diagnosis codes in Medicare data increased from 10 to 25 in 2011, we restricted data from 2011 to 2019 to the first 10 diagnosis codes to align with data from 1995 to 2010.2,10
Patient Characteristics and Demographic Subgroups
Patient characteristics included demographic, comorbidity, and index hospitalization information (eMethods and eTable 1 in the Supplement). Demographic subgroups were defined by age (aged 65 to 79 years and 80 years and older), self-reported sex (male and female), self-reported race (Black, White, and other races [including American Indian and Alaska Native, Asian, Hispanic, other race or ethnicity, and unreported]), living in a health priority area defined as a geographic area with persistently high adjusted mortality and hospitalization rates,11 and dual Medicare-Medicaid eligibility.12,13
Outcomes
The outcomes were all-cause mortality and hospitalization for recurrent AMI within 10 years, beginning 30 days from the initial AMI admission date. Mortality information was obtained from the Medicare data. Patients who were alive on December 31, 2019, were censored. Information on recurrent AMI was obtained from Medicare inpatient data. For patients with more than 1 recurrent AMI, the first and last recurrences were assessed. Patients were excluded from the recurrent AMI sample if they were transferred to another hospital after the initial AMI hospitalization and the principal discharge diagnosis code in the transferred-in hospital was not an AMI. We assessed the changes in the rate of in-hospital CABG or PCI, both during the index AMI hospitalization and within 10 years after discharge for AMI. CABG and PCI information was acquired from the inpatient claims data.
Statistical Analysis
To facilitate data presentation, we divided the 25-year study period into 5-year intervals (1995 to 1999, 2000 to 2004, 2005 to 2009, 2010 to 2014, and 2015 to 2019) and provide patient characteristics by these intervals. Overall and subgroup-specific observed rates (with 95% CIs) of 10-year mortality, recurrent AMI, switching to Medicare Advantage, and post-AMI CABG or PCI were estimated based on survival functions. Race subgroups in the main analysis included American Indian and Alaska Native, Asian, Black, Hispanic, White, and other race or ethnicity, or unreported.
We assessed 10-year mortality trends by fitting Cox proportional hazards models of time to death as a function of the patient baseline characteristics in Table 1 and an ordinal time indicator for year (1995 [time = 0] to 2019 [time = 24]; hazard ratio [HR] represents the annual trend in mortality). We repeated the models for 10-year recurrent AMI. Patients who switched to Medicare Advantage after the initial AMI were considered lost to follow-up, and deaths before recurrence were accounted for using the Fine and Gray method for competing risks.14
Table 1. Patient Baseline Characteristics by Index Hospitalization Period.
| Characteristic | Time interval, No. (%) | ||||
|---|---|---|---|---|---|
| 1995-1999 | 2000-2004 | 2005-2009 | 2010-2014 | 2015-2019 | |
| Demographic characteristics | |||||
| Patients, No. | 975 387 | 966 755 | 758 299 | 654 365 | 627 460 |
| Age, mean (SD), y | 77.4 (7.0) | 78.2 (7.2) | 78.5 (7.6) | 78.3 (7.8) | 77.4 (7.7) |
| Sex | |||||
| Female | 485 727 (49.8) | 490 924 (50.8) | 380 104 (50.1) | 314 602 (48.1) | 281 093 (44.8) |
| Male | 489 660 (50.2) | 475 831 (49.2) | 378 195 (49.9) | 339 763 (51.9) | 346 367 (55.2) |
| Race and ethnicity | |||||
| American Indian and Alaska Native | 832 (0.1) | 2342 (0.2) | 3420 (0.5) | 3461 (0.5) | 4266 (0.7) |
| Asian | 3745 (0.4) | 6923 (0.7) | 7908 (1.0) | 8841 (1.4) | 9592 (1.5) |
| Black | 60 217 (6.2) | 66 708 (6.9) | 55 326 (7.3) | 51 099 (7.8) | 47 175 (7.5) |
| Hispanic | 9658 (1.0) | 16 800 (1.7) | 12 637 (1.7) | 10 762 (1.6) | 9501 (1.6) |
| White | 884 688 (90.7) | 858 236 (88.8) | 667 198 (88.0) | 569 273 (87.0) | 540 434 (86.1) |
| Other or unreported race | 16 247 (1.7) | 15 746 (1.6) | 11 810 (1.6) | 10 929 (1.7) | 16 492 (2.6) |
| Dual Medicare-Medicaid–eligible | 134 593 (13.8) | 154 725 (16.0) | 127 354 (16.8) | 111 988 (17.1) | 95 159 (15.2) |
| Not enrolled in Medicare Part B | 5574 (0.6) | 16 047 (1.7) | 17 028 (2.2) | 21 518 (3.3) | 28 182 (4.5) |
| Living in a health priority area | 203 828 (20.9) | 199 346 (20.6) | 160 190 (21.1) | 140 333 (21.4) | 132 437 (21.1) |
| Living in an area with income <25th percentile of national average | 97 341 (10.0) | 95 233 (9.9) | 72 609 (9.6) | 62 970 (9.6) | 59 765 (9.5) |
| Admission characteristics | |||||
| From a skilled nursing facility or intermediate care facility | 6272 (0.6) | 6768 (0.7) | 6435 (0.8) | 11 035 (1.7) | 7142 (1.1) |
| From an emergency department | 634 747 (65.1) | 694 318 (71.8) | 542 757 (71.6) | 496 968 (75.9) | 475 076 (75.7) |
| Emergent or urgent admission | 827 941 (84.9) | 902 875 (93.4) | 711 475 (93.8) | 617 343 (94.3) | 597 762 (95.3) |
| Anterior MI | 193 228 (19.8) | 129 083 (13.4) | 78 562 (10.4) | 53 696 (8.2) | 37 369 (6.0) |
| Inferior, lateral, or posterior MI | 255 263 (26.2) | 174 611 (18.1) | 109 302 (14.4) | 82 574 (12.6) | 75 644 (12.1) |
| Rural hospital | 136 220 (14.0) | 129 254 (13.4) | 91 961 (12.1) | 74 666 (11.4) | 68 172 (10.9) |
| Large teaching hospital | 140 400 (14.4) | 162 910 (16.9) | 138 996 (18.3) | 110 917 (17.0) | 101 640 (16.2) |
| Private, not-for-profit hospital | 646 948 (66.3) | 686 147 (71.0) | 565 772 (74.6) | 485 693 (74.2) | 464 940 (74.1) |
| CABG-capable hospital | 479 623 (49.2) | 543 794 (56.2) | 482 144 (63.6) | 438 228 (67.0) | 415 433 (66.2) |
| Comorbidities | |||||
| Prior heart failure | 109 750 (11.3) | 115 595 (12.0) | 90 165 (11.9) | 73 077 (11.2) | 66 126 (10.5) |
| Prior MI | 31 370 (3.2) | 14 160 (1.5) | 12 954 (1.7) | 13 077 (2.0) | 12 344 (2.0) |
| Unstable angina | 49 507 (5.1) | 38 659 (4.0) | 20 263 (2.7) | 14 009 (2.1) | 15 552 (2.5) |
| Atherosclerotic disease | 645 186 (66.1) | 647 012 (66.9) | 530 174 (69.9) | 471 143 (72.0) | 395 444 (63.0) |
| Respiratory failure | 16 383 (1.7) | 16 787 (1.7) | 23 467 (3.1) | 29 002 (4.4) | 36 209 (5.8) |
| Hypertension | 478 499 (49.1) | 555 736 (57.5) | 435 077 (57.4) | 364 470 (55.7) | 296 659 (47.3) |
| Prior stroke | 16 399 (1.7) | 17 174 (1.8) | 12 790 (1.7) | 10 797 (1.6) | 9503 (1.5) |
| Cerebral vascular disease other than stroke | 40 068 (4.1) | 53 249 (5.5) | 37 210 (4.9) | 31 502 (4.8) | 22 263 (3.5) |
| Kidney failure | 38 133 (3.9) | 81 554 (8.4) | 145 166 (19.1) | 165 112 (25.2) | 178 123 (28.4) |
| COPD | 194 634 (20.0) | 212 184 (21.9) | 165 604 (21.8) | 126 879 (19.4) | 112 931 (18.0) |
| Pneumonia | 81 835 (8.4) | 110 296 (11.4) | 100 411 (13.2) | 85 658 (13.1) | 70 098 (11.2) |
| Protein-calorie malnutrition | 11 216 (1.1) | 18 632 (1.9) | 22 661 (3.0) | 28 347 (4.3) | 29 866 (4.8) |
| Dementia | 51 540 (5.3) | 80 943 (8.4) | 72 149 (9.5) | 67360 (10.3) | 57 282 (9.1) |
| Functional disability | 14 394 (1.5) | 17 564 (1.8) | 12 686 (1.7) | 11 827 (1.8) | 13 384 (2.1) |
| Peripheral vascular disease | 49 528 (5.1) | 72 352 (7.5) | 60 208 (7.9) | 51 355 (7.8) | 40 265 (6.4) |
| Cancer | 31 111 (3.2) | 53 288 (5.5) | 44 146 (5.8) | 37 323 (5.7) | 34 505 (5.5) |
| Trauma in past year | 37 519 (3.8) | 50 746 (5.2) | 45 120 (6.0) | 34 533 (5.3) | 27 460 (4.4) |
| Other major psychiatric disorders | 12 962 (1.3) | 16 632 (1.7) | 13 233 (1.7) | 13 494 (2.1) | 10 389 (1.7) |
| Liver disease | 7758 (0.8) | 18 050 (1.9) | 16 011 (2.1) | 15 185 (2.3) | 16 158 (2.6) |
| Depression | 25 004 (2.6) | 45 589 (4.7) | 39 943 (5.3) | 37 885 (5.8) | 36 157 (5.8) |
| Diabetes | 299 804 (30.7) | 287 373 (29.7) | 228 447 (30.1) | 214 482 (32.8) | 222 404 (35.4) |
| Asthma | 15 351 (1.6) | 20 775 (2.1) | 18 315 (2.4) | 16 713 (2.6) | 21 766 (3.5) |
| Anemia | 137 095 (14.1) | 199 373 (20.6) | 169 179 (22.3) | 163 757 (25.0) | 148 184 (23.6) |
| Parkinson or Huntington disease | 11 163 (1.1) | 15 244 (1.6) | 10 954 (1.4) | 9096 (1.4) | 9021 (1.4) |
| In-hospital care | |||||
| Underwent PCI or CABG | 218 120 (22.4) | 307 898 (31.8) | 314 406 (41.5) | 309 962 (47.4) | 257 922 (41.1) |
| More than 1 complicationa | 51 965 (5.3) | 47 886 (5.0) | 41 075 (5.4) | 32 668 (5.0) | 23 032 (3.7) |
| Length of stay, mean (SD), d | 7 (6.5) | 6 (6.6) | 6 (6.1) | 5 (5.2) | 5 (5.1) |
| Discharged to home | 500 269 (51.3) | 471971 (48.8) | 374 554 (49.4) | 344 808 (52.7) | 348 714 (55.6) |
| Transferred to another acute care hospital | 202 751 (20.8) | 181 658 (18.8) | 95 480 (12.6) | 60 543 (9.3) | 53 557 (8.5) |
Abbreviations: CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Complications were identified using Clinical Classifications Software (CCS) and included infections (CCS-2 to CCS-10, CCS-126, CCS-135, CCS-159); complications of devices, procedures, and medical care (CSS-237 and CCS-238); and injury/contusion (CCS-239) (eTable 1 in the Supplement).
To address potential bias related to differences in patient characteristics between demographic subgroups, we calculated subgroup-specific stabilized inverse probability weights (IPW) estimating the conditional probability of a patient to be in a given subgroup based on the baseline demographic, admission, and comorbidity characteristics in Table 1.15,16,17 A Cox model was fit with 10-year mortality as the outcome and the subgroup-specific category as a covariate, weighted by the stabilized IPW. We repeated this model for all subgroups and for 10-year recurrence. We used the Cole-Hernan method,18 which incorporates IPW, to produce adjusted Kaplan-Meier survival curves. We repeated the above analyses for the change in the rate of post-AMI CABG or PCI.
To assess the association between 10-year recurrent AMI and 10-year mortality, we fit an extended Cox model of mortality as a function of the time to recurrent AMI, adjusting for patient baseline characteristics. For patients with more than 1 recurrence, we selected the last event for analysis.
To evaluate differences in 10-year mortality and recurrence rates in the early and later periods in which all patients were eligible for a full 10-year follow-up, we restricted patients to those initially hospitalized with AMI in 1995 to 1997 and 2007 to 2009 and fit Cox models of mortality as a function of patient baseline characteristics with 2007 to 2009 as a binary indicator. We combined the 3-year data to reduce sampling variance. We repeated this model for the demographic subgroups and for 10-year recurrence.
In secondary analyses, we assessed differences in outcomes between patients with STEMI and non-STEMI. Analyses were conducted using SAS version 9.4 (SAS Institute). Statistical tests used a 2-sided α of .05.
Results
Study Sample and Baseline Characteristics
There were 3 982 266 unique patients with AMI who were alive 30 days after the AMI admission; 1 952 450 (49.0%) were female, and the mean (SD) age was 78.0 (7.4) years. A total of 2 700 441 patients (67.8%) were hospitalized from 1995 to 2009 and had the potential for a full 10-year follow-up period. Mean (SD) age varied from 77.0 (6.8) years in 1995 to 78.7 (7.7) in 2008 to 77.1 (7.6) in 2019, and it varied by demographic subgroups (eFigure 1 in the Supplement). Between 1995 (n = 200 141) and 2019 (n = 118 021), the proportions of women varied from 98 676 (49.3%) to 50 927 (43.2%); Black patients from 12 000 (6.0%) to 8440 (7.2%); patients of other race (including American Indian and Alaska Native, Asian, Hispanic, other race or ethnicity, and unreported) from 5081 (2.5%) to 8234 (7.0%); and dual Medicare-Medicaid–eligible patients from 25 739 (12.9%) to 16 613 (14.1%). There was little variance in the proportion of patients living in a health priority area (40 847 [20.4%] in 1995 to 24 741 [21.0%] in 2019). The 5 most common baseline comorbidities among 3 982 266 included patients with AMI were atherosclerosis (2 688 959 [67.5%]), hypertension (2 130 441 [53.5%]), diabetes (1 252 510 [31.5%]), anemia (817 588 [20.5%]), and chronic obstructive pulmonary disease (812 232 [20.4%] (Table 1). Aggregated patient characteristics by demographic subgroups unweighted and weighted by IPW are in eTables 2 to 5 in the Supplement.
Between 1995 and 2019, the median (IQR) LOS varied from 7.0 (4.0-10.0) days to 3.0 (2.0-6.0) days, and the proportions of patients who were admitted to a rural hospital varied from 27 423 of 200 141 (13.7%) to 12 453 of 118 021 (10.6%), those who were discharged to home varied from 106 514 (53.2%) to 67 597 (57.3%), and those with multiple in-hospital complications during the index AMI hospitalization varied from 11 116 (5.6%) to 3863 (3.3%). Urinary tract infections (368 733 of 3 982 266 [9.3%]), device complications (249 448 of 3 982 266 [6.3%]), and complications of surgical procedures or medical care (247 634 of 3 982 266 [6.2%]) were the most frequent individual complications. Over the 25-year period, 11.4% (95% CI, 11.4-11.5) of patients switched to Medicare Advantage within 10 years after the initial AMI hospitalization.
Ten-Year Mortality
Over the 25-year period, observed 10-year all-cause mortality was 72.7% (95% CI, 72.6-72.7) for patients hospitalized with AMI, declining over time as represented by the 5-year intervals (Figure 1). Observed rates of 10-year mortality were higher for patients who were female, Black, dual Medicare-Medicaid–eligible status, and living in health priority areas (Table 2). After accounting for differences in patient characteristics, male patients had a higher risk of mortality than female patients (Figure 2; Table 2). The respective IPW-adjusted mortality HRs were 1.13 (95% CI, 1.12-1.13) for male vs female patients, 1.05 (95% CI, 1.05-1.06) for Black vs White patients, 1.24 (95% CI, 1.24-1.24) for dual Medicare-Medicaid–eligible vs noneligible patients, and 1.06 (95% CI, 1.06-1.07) for patients living in health priority areas vs other areas (eFigure 2 in the Supplement). Compared with White patients, patients of other races (including American Indian and Alaska Native, Asian, Hispanic, other race or ethnicity, and unreported) had a lower risk of 10-year mortality (HR, 0.96; 95% CI, 0.95-0.96). These findings did not change substantially after restricting the models to patients who had the potential for a full 10-year follow-up (eFigure 3 and eTable 6 in the Supplement). The adjusted annual reduction in 10-year mortality was 1.5% (95% CI, 1.4-1.5). The reductions were smaller for patients who were 80 years and older, male, American Indian and Alaska Native, White, and living in a health priority area (Figure 3).
Figure 1. Observed Kaplan-Meier Curves for 10-Year Mortality and Recurrence.
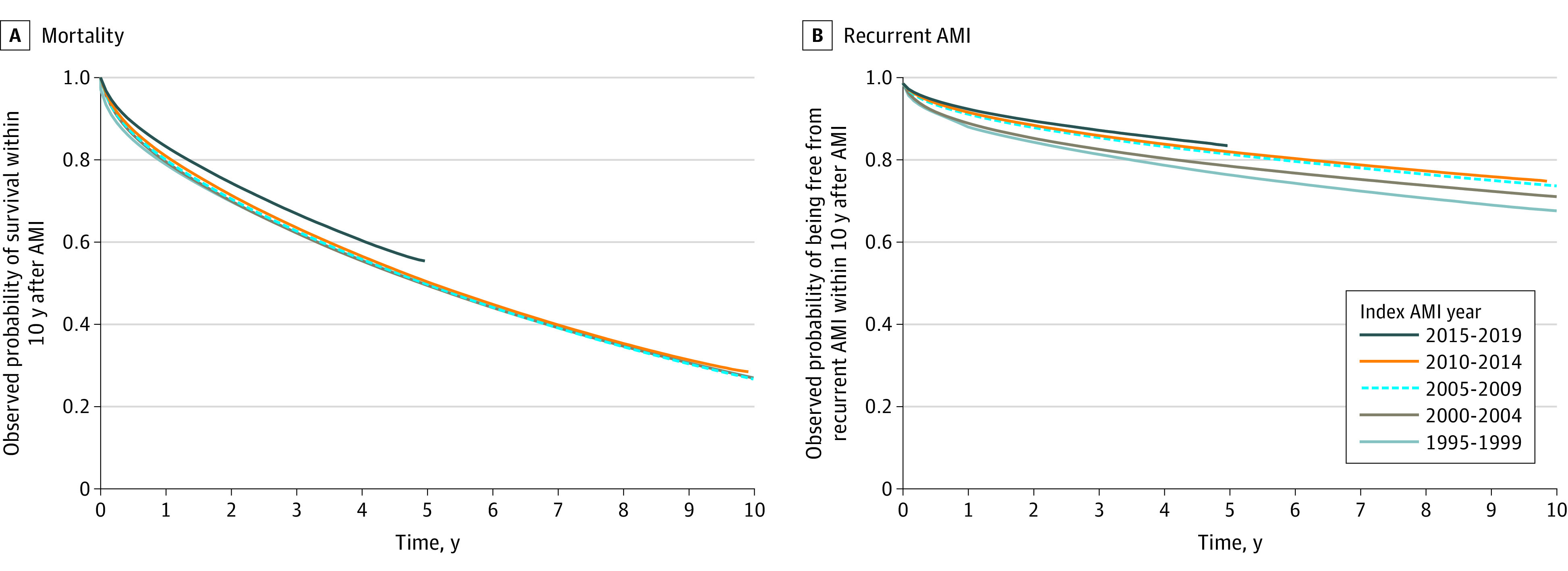
The observed Kaplan-Meier curves compare the probability of survival and being free from recurrence within 10 years after an initial acute myocardial infarction (AMI) hospitalization in 5-year intervals.
Table 2. Ten-Year All-Cause Mortality and Hospitalization for Recurrent Acute Myocardial Infarction (AMI) by Demographic Subgroups From 1995 to 2019.
| Subgroup | % (95% CI) | |||
|---|---|---|---|---|
| Observed rate | Inverse probability–weighted rate | |||
| Mortality | Recurrent AMI | Mortality | Recurrent AMI | |
| Female | 75.2 (75.2-75.3) | 27.8 (27.7-27.9) | 71.1 (71.1-71.2) | 26.6 (26.5-26.7) |
| Male | 70.6 (70.6-70.7) | 26.6 (26.5-26.7) | 74.6 (74.5-74.6) | 28.0 (27.8-28.1) |
| American Indian and Alaska Native | 73.3 (72.3-74.2) | 27.7 (26.3-29.0) | 74.3 (73.4-75.2) | 25.3 (23.9-26.6) |
| Asian | 70.3 (69.7-70.9) | 26.9 (26.1-27.7) | 73.7 (73.2-74.1) | 27.1 (26.4-27.8) |
| Black | 78.3 (78.1-78.5) | 32.3 (31.9-32.6) | 75.7 (75.5-75.8) | 30.3 (29.9-30.6) |
| Hispanic | 74.3 (73.9-74.7) | 32.8 (32.1-33.5) | 71.4 (71.0-71.8) | 28.1 (27.4-28.7) |
| White | 72.6 (72.6-72.7) | 26.8 (26.7-26.9) | 73.0 (73.0-73.1) | 27.1 (27.0-27.2) |
| Other or unreported race | 66.2 (65.8-66.6) | 26.5 (25.9-27.0) | 71.8 (71.4-72.1) | 27.2 (26.6-27.7) |
| Dual Medicare-Medicaid–eligible | 83.2 (83.1-83.3) | 33.3 (33.1-33.5) | 79.7 (79.5-79.8) | 31.4 (31.2-31.6) |
| Noneligible | 71.0 (71.0-71.1) | 26.3 (26.2-26.4) | 72.1 (72.1-72.2) | 26.8 (26.7-26.9) |
| Health priority area | 73.9 (73.8-74.0) | 27.8 (27.6-28.0) | 74.6 (74.5-74.7) | 27.5 (27.2-27.6) |
| Nonpriority area | 72.7 (72.6-72.7) | 27.1 (27.0-27.1) | 72.4 (72.4-72.5) | 27.1 (27.0-27.2) |
Figure 2. Adjusted Kaplan-Meier Curves for 10-Year Mortality and Recurrence by Demographic Subgroups.
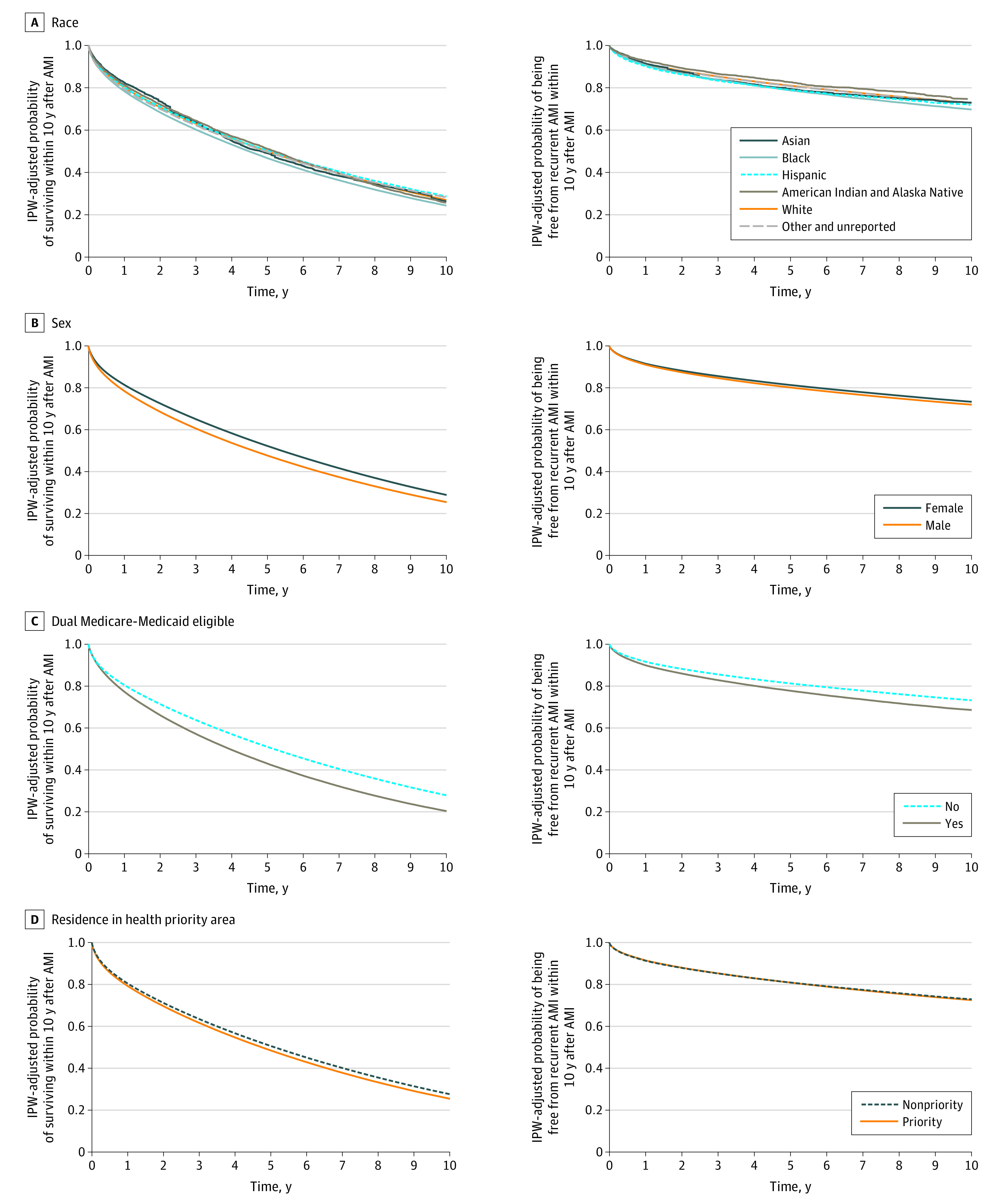
The inverse probability weight (IPW)–adjusted Kaplan-Meier curves compare the probability of survival and being free from recurrence within 10 years after acute myocardial infarction (AMI) by subgroups. Variables used to estimate the IPW included the demographic, admission, and comorbidity characteristics in Table 1. All patients had a 10-year follow-up.
Figure 3. Adjusted Annual Trends in 10-Year Mortality and Recurrent Acute Myocardial Infarction (AMI) by Demographic Subgroups.
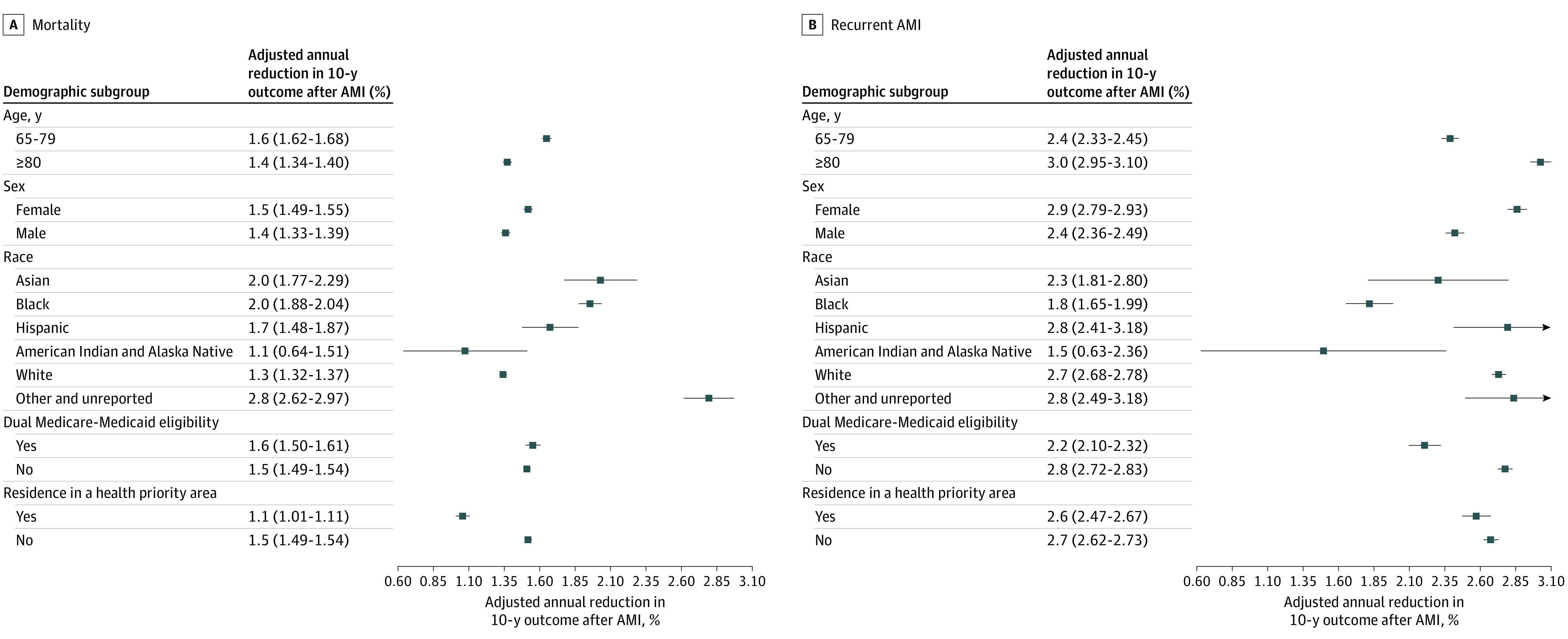
Estimates were obtained from Cox models that adjusted for patient characteristics. A time variable was included in the models. Annual reductions were calculated by subtracting the hazard ratio of the time variable from 1.0. Other race includes American Indian and Alaska Native, Asian, Hispanic, other race and ethnicity, and unreported.
For patients hospitalized in 1995 to 2009, median survival time among those who died changed from 1019 (95% CI, 1008.3-1028.4) days to 1062 (95% CI, 1050.2-1073.8) days (eFigure 4 in the Supplement). The risk of 10-year mortality was 13.9% lower for patients hospitalized in 2007 to 2009 compared with those hospitalized in 1995 to 1997 (HR, 0.86; 95% CI, 0.85-0.87). The reduction varied across subgroups (eTable 7 in the Supplement).
Among patients who died within 10 years, approximately 30% died during the first year after AMI. For patients hospitalized between 1995 and 2009, mortality within the first year decreased from 30.5% (95% CI, 30.3-30.8) to 27.2% (95% CI, 27.0-27.5). There were no marked differences in this pattern between subgroups.
In secondary analyses, observed 10-year mortality was higher for patients with STEMI (80.3%; 95% CI, 80.1-80.5) than for patients with non-STEMI (72.2%; 95% CI, 72.1-72.2). Patients with STEMI had the most prominent decline, represented by the 5-year intervals (eFigure 5 and eTable 9 in the Supplement). This finding did not change substantially after accounting for patient baseline characteristics. The adjusted risk of death was 15% (HR, 1.15; 95% CI, 1.14-1.16) higher for patients with STEMI vs non-STEMI. Overall, the adjusted annual reductions in mortality were 1.9% (95% CI, 1.8-2.0) for patients with STEMI and 1.4% (95% CI, 1.4-1.4) for patients with non-STEMI.
Ten-Year Hospitalization for Recurrent AMI
Over the 25-year period, the observed 10-year recurrent AMI rate was 27.1% (95% CI, 27.0-27.2), and it declined over time (Figure 1). Observed rates of recurrence within 10 years were higher for patients who were female, Black, dual Medicare-Medicaid eligible, and living in health priority areas (Table 2). After accounting for differences in patient characteristics, male patients had higher risk of recurrence than female patients (Figure 2; Table 2). The respective IPW-adjusted recurrence HRs were 1.07 (95% CI, 1.06-1.07) for male vs female patients, 1.08 (95% CI, 1.07-1.09) for Black vs White patients, and 1.21 (95% CI, 1.20-1.21) for dual Medicare-Medicaid–eligible vs noneligible patients (eFigure 2 in the Supplement). There were no marked differences by health priority area or for other race (American Indian and Alaska Native, Asian, Hispanic, other race or ethnicity, and unreported) vs White patients. These findings did not change substantially after restricting models to patients with the potential for a full 10-year follow-up (eFigure 3 and eTable 6 in the Supplement). The adjusted annual reduction in 10-year recurrence was 2.7% (95% CI, 2.6-2.7). The reductions in recurrence were smaller for patients aged 65 to 79 years, male, American Indian and Alaska Native, Black, and dual Medicare-Medicaid eligible (Figure 3).
For patients hospitalized between 1995 and 2009, the median days to the first AMI recurrence among those with a recurrence increased from 424 (95% CI, 408.6-439.4) to 488 (95% CI, 472.7-503.3) (eFigure 4 in the Supplement). The risk of 10-year recurrence was 22.5% lower for patients hospitalized in 2007 to 2009 compared with those hospitalized in 1995 to 1997 (HR, 0.77; 95% CI, 0.76-0.78). The reduction varied across subgroups (eTable 7 in the Supplement).
In secondary analyses, the observed 10-year recurrence rate was higher for patients with STEMI (30.4%; 95% CI, 30.0-30.7) vs non-STEMI (27.0%; 95% CI, 26.9-27.1). Patients with STEMI had the larger change, represented by the 5-year intervals (eFigure 5 and eTable 8 in the Supplement). After accounting for patient baseline characteristics, those with STEMI had an overall 8% (HR, 0.92; 95% CI, 0.90-0.94) lower risk for recurrent AMI than those with non-STEMI. Overall, the adjusted annual declines in recurrence were 2.4% (95% CI, 2.1-2.6) and 2.7% (95% CI, 2.6-2.7) for patients with STEMI and non-STEMI, respectively.
Association Between Hospitalization for Recurrence and Mortality
Mortality within 10 years after the initial AMI was higher for patients with a recurrent AMI (80.6%; 95% CI, 80.5-80.7) vs those without a recurrence (72.4%; 95% CI, 72.3-72.5). This pattern was observed across subgroups (eTable 9 in the Supplement). Recurrent AMI was associated with an increased risk of 10-year mortality (HR, 1.89; 95% CI, 1.88-1.90).
Ten-Year In-Hospital CABG or PCI Rate
Overall, 1 408 308 of 3 982 266 patients (35.4%) had CABG or PCI during the index AMI hospitalization. Patients who were 80 years or older (vs aged 65 to 79 years), female (vs male), Black (vs White), other race (vs White), and dual Medicare-Medicaid eligible (vs noneligible) had lower rates of CABG or PCI, while patients who were in health priority areas had a higher rate. This difference in treatments persisted across the 5-year intervals (eTable 10 in the Supplement). Among patients who did not have CABG or PCI during the index hospitalization, 16.6% (95% CI, 16.5-16.6) had CABG or PCI during the 10-year follow-up period. The difference in treatments found in the index hospitalization persisted during the follow-up period (eTable 11 in the Supplement).
Discussion
In this 25-year national study of Medicare fee-for-service beneficiaries who were alive 30 days after an AMI, both 10-year mortality and hospitalization for recurrent AMI decreased steadily over time. Taken together with previously reported reductions in short-term mortality,1,2,19,20 this study reveals that these reductions were associated with important continuing improvements over time. Although there were reductions across all demographic subgroups examined, marked inequities persisted between subgroups. We identified a strong association between hospitalization for recurrent AMI and mortality as well as changes in the profile of people hospitalized with AMI over time. There were persistent differences in CABG or PCI treatments across demographic subgroups, both during the index hospitalization and the follow-up period. All patients die eventually, and the goal cannot be zero mortality. However, variations in mortality, high AMI recurrence, and CABG or PCI rates indicate opportunities for improvement.
This study has several notable features. We observed patients up to 10 years after AMI, which is an important period with limited information in the literature. Previous studies primarily focused on the period immediately after AMI hospitalization or within 1 year, with few21,22 assessing outcomes over a 10-year period and none assessing 10-year outcomes on a national scale. We observed that 73% of patients with AMI died within 10 years, which highlights the importance of primary AMI prevention. The 10-year recurrent AMI rate was 27%, which is 3-fold higher than the previously reported 1-year recurrence rate of 8.9% in 2010.23 We found that the median time to recurrent AMI within 10 years was 488 days (95% CI, 472.7-503.3) in 2009, the last year that all patients were eligible for a full 10-year follow-up. This extended time to recurrence indicates the importance of follow-up for patients with AMI beyond the traditional 1-year period. Additionally, having a recurrent event was associated with an 8–percentage point increase in 10-year mortality risk, suggesting that reducing recurrent events may also be associated with an improvement in long-term mortality for AMI survivors.
We assessed inequities in long-term outcomes and trends by important demographic subgroups. Medicare patients who were Black, living in a health priority area, and of low socioeconomic status (represented by dual Medicare-Medicaid eligibility) had higher adjusted risks of 10-year mortality and hospitalization for recurrent AMI. Women had higher observed rates of mortality and recurrence; however, after accounting for differences in patient characteristics, the risks of these outcomes were higher for men. The higher unadjusted rates for women are consistent with prior studies24 and likely reflect the older age of women at the time of AMI and differences in comorbidity distribution and presentation. Although we found improved 10-year outcomes overall during the past few decades, annual reductions in outcomes varied between subgroups, and demographic differences have persisted. As an example, a 70-year-old White man and Black man had expected 10-year mortality of 56.1% and 73.1%, respectively, in 1995 and 49.9% and 68.4% in 2009. For a 70-year-old White woman and Black woman, the expected rates of 10-year mortality were 57.6% and 68.2%, respectively, in 1995 and 54.3% and 66.0% in 2009. A 70-year-old dual Medicare-Medicaid–eligible man and noneligible man had expected 10-year mortality of 77.3% and 55.5%, respectively, in 1995 and 70.0% and 48.8% in 2009. For a 70-year-old dual Medicare-Medicaid–eligible woman and noneligible woman, the expected rates of 10-year mortality were 73.3% and 55.2%, respectively, in 1995 and 71.6% and 50.0% in 2009. These findings indicate the need for further studies to address inequities in long-term AMI outcomes, with particular attention to quality of care and social determinants of health.
Previous studies showed that nationwide quality improvement in care for cardiovascular disease was a major factor in observed declines in 30-day mortality after AMI.2,25,26 Our study indicates the need for continuous quality improvements in postacute care to achieve better longer-term outcomes. We found that the first year after AMI was the most important period for long-term survival. Among patients who died within 10 years, more than 30% died within the first year. This finding highlights the importance of high-quality postacute care immediately after AMI hospitalization for secondary prevention.23,27,28,29,30 The high rate of hospitalization for recurrence over 10 years and the 8–percentage point increase in the risk of 10-year mortality with a recurrent event further demonstrate the need for quality care to reduce recurrence and improve long-term mortality for AMI survivors.
Limitations
Our study has limitations. We focused on Medicare fee-for-service beneficiaries 66 years or older, and the findings may not reflect Medicare Advantage beneficiaries or younger patients. Because Medicare data do not provide individual race and ethnicity variables, we were unable to separate Hispanic ethnicity from White, Black, and other race, which might underestimate the Hispanic population. Comorbidities were defined using diagnosis codes. Because the maximum number of diagnosis codes in Medicare data increased from 10 to 25 in 2011,31 we restricted 2011 to 2019 data to the first 10 codes to align with 1995 to 2010 data. Nevertheless, the change in the number of diagnosis codes could have influenced results, although there was no obvious discontinuity in the rates. Limited by available data, we were unable to incorporate the use of secondary prevention medications, postacute care information on medication adherence, nursing home stays, home health services, and physician office visits, which are associated with outcomes. We were unable to evaluate troponin levels because these data are unavailable in Medicare data. The percentage of patients in Medicare fee-for-service decreased over the study period.32 The effect of the change is not known because we adjusted for patient characteristics, and it is not known how patients with AMI in Medicare Advantage might be different from those in Medicare fee-for-service and how that may have changed over time. Patients with AMI in Medicare fee-for-service may be changing in ways that are unmeasured and yet influence outcomes over time. Moreover, this study focused on recurrent AMI among those hospitalized, and some of these events may not have led to admissions, including sudden deaths. The association between mortality and recurrent AMI could introduce an immortal time bias. However, because all patients who survived after the initial AMI hospitalization were at risk for both death and recurrence, this bias is likely minor.
Conclusions
In this study, we found that rates of 10-year mortality and hospitalization for recurrence improved over the last decades for patients who survived the acute period of AMI. Marked differences in outcomes and temporal trends were observed across demographic subgroups. National efforts to reduce inequities in long-term outcomes should be health care priorities in the US for the coming decade.
eMethods. Expanded patient characteristics.
eReferences.
eTable 1. Clinical Classifications Software categories.
eTable 2. Overall patient characteristics by race: unweighted and weighted.
eTable 3. Overall patient characteristics by sex: unweighted and weighted.
eTable 4. Overall patient characteristics by dual Medicare-Medicaid eligibility: unweighted and weighted.
eTable 5. Overall patient characteristics by living in a health priority area: unweighted and weighted.
eTable 6. Inverse probability weight–adjusted rates of 10-year mortality and recurrence by demographic subgroups and index hospitalization year for all patients eligible for 10 years of follow-up.
eTable 7. Change in risk of 10-year mortality and recurrent AMI for patients hospitalized in 2007-2009 compared with 1995-1997 by demographic subgroups.
eTable 8. Observed rates of 10-year mortality and recurrent AMI by index hospitalization year and STEMI diagnosis.
eTable 9. Inverse probability weight–adjusted mortality rates for patients with and without a recurrent AMI by demographic subgroups.
eTable 10. Observed rate of CABG or PCI during the index AMI hospitalization by year and demographic subgroups.
eTable 11. Observed 10-year rate of CABG or PCI after the index AMI hospitalization by demographic subgroups.
eFigure 1. Distribution of mean age by demographic subgroups: 1995-2019.
eFigure 2. Adjusted hazard ratios for the associations of demographic subgroups with 10-year mortality and recurrent AMI.
eFigure 3. Adjusted Kaplan-Meier curves for 10-year mortality and recurrence by demographic subgroups: 1995-2009.
eFigure 4. Median days to death or recurrent AMI by index hospitalization year.
eFigure 5. Observed Kaplan-Meier curves for 10-year mortality and recurrent AMI by STEMI diagnosis and index hospitalization year.
References
- 1.Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999-2011. Circulation. 2014;130(12):966-975. doi: 10.1161/CIRCULATIONAHA.113.007787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krumholz HM, Normand ST, Wang Y. Twenty-year trends in outcomes for older adults with acute myocardial infarction in the United States. JAMA Netw Open. 2019;2(3):e191938. doi: 10.1001/jamanetworkopen.2019.1938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley EH, Herrin J, Elbel B, et al. Hospital quality for acute myocardial infarction: correlation among process measures and relationship with short-term mortality. JAMA. 2006;296(1):72-78. doi: 10.1001/jama.296.1.72 [DOI] [PubMed] [Google Scholar]
- 4.French WJ, Reddy VS, Barron HV. Transforming quality of care and improving outcomes after acute MI: lessons from the National Registry of Myocardial Infarction. JAMA. 2012;308(8):771-772. doi: 10.1001/jama.2012.9500 [DOI] [PubMed] [Google Scholar]
- 5.Krumholz HM, Wang Y, Chen J, et al. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995-2006. JAMA. 2009;302(7):767-773. doi: 10.1001/jama.2009.1178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonow RO, Bennett S, Casey DE Jr, et al. ; American College of Cardiology; American Heart Association Task Force on Performance Measures (Writing Committee to Develop Heart Failure Clinical Performance Measures); Heart Failure Society of America . ACC/AHA clinical performance measures for adults with chronic heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Heart Failure Clinical Performance Measures) endorsed by the Heart Failure Society of America. J Am Coll Cardiol. 2005;46(6):1144-1178. doi: 10.1016/j.jacc.2005.07.012 [DOI] [PubMed] [Google Scholar]
- 7.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998-1999 to 2000-2001. JAMA. 2003;289(3):305-312. doi: 10.1001/jama.289.3.305 [DOI] [PubMed] [Google Scholar]
- 8.Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (Acute Coronary Treatment and Intervention Outcomes Network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2(5):491-499. doi: 10.1161/CIRCOUTCOMES.108.847145 [DOI] [PubMed] [Google Scholar]
- 9.Yeh RW, Normand SL, Wang Y, Barr CD, Dominici F. Geographic disparities in the incidence and outcomes of hospitalized myocardial infarction: does a rising tide lift all boats? Circ Cardiovasc Qual Outcomes. 2012;5(2):197-204. doi: 10.1161/CIRCOUTCOMES.111.962456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsugawa Y, Figueroa JF, Papanicolas I, Orav EJ, Jha AK. Assessment of strategies for managing expansion of diagnosis coding using risk-adjustment methods for Medicare data. JAMA Intern Med. 2019;179(9):1287-1290. doi: 10.1001/jamainternmed.2019.1005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krumholz HM, Normand ST, Wang Y. Geographical health priority areas for older Americans. Health Aff (Millwood). 2018;37(1):104-110. doi: 10.1377/hlthaff.2017.0744 [DOI] [PubMed] [Google Scholar]
- 12.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, hospitalizations, and expenditures for the Medicare population aged 65 years or older, 1999-2013. JAMA. 2015;314(4):355-365. doi: 10.1001/jama.2015.8035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wadhera RK, Wang Y, Figueroa JF, Dominici F, Yeh RW, Joynt Maddox KE. Mortality and hospitalizations for dually enrolled and nondually enrolled Medicare beneficiaries aged 65 years or older, 2004 to 2017. JAMA. 2020;323(10):961-969. doi: 10.1001/jama.2020.1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496-509. doi: 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- 15.de Havenon A, Ney JP, Callaghan B, et al. Impact of COVID-19 on outcomes in ischemic stroke patients in the United States. J Stroke Cerebrovasc Dis. 2021;30(2):105535. doi: 10.1016/j.jstrokecerebrovasdis.2020.105535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dess RT, Hartman HE, Mahal BA, et al. Association of Black race with prostate cancer-specific and other-cause mortality. JAMA Oncol. 2019;5(7):975-983. doi: 10.1001/jamaoncol.2019.0826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rebeiro PF, Abraham AG, Horberg MA, et al. Sex, race, and HIV risk disparities in discontinuity of HIV care after antiretroviral therapy initiation in the United States and Canada. AIDS Patient Care STDS. 2017;31(3):129-144. doi: 10.1089/apc.2016.0178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cole SR, Hernán MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed. 2004;75(1):45-49. doi: 10.1016/j.cmpb.2003.10.004 [DOI] [PubMed] [Google Scholar]
- 19.Johansson S, Rosengren A, Young K, Jennings E. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord. 2017;17(1):53. doi: 10.1186/s12872-017-0482-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smolina K, Wright FL, Rayner M, Goldacre MJ. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ Cardiovasc Qual Outcomes. 2012;5(4):532-540. doi: 10.1161/CIRCOUTCOMES.111.964700 [DOI] [PubMed] [Google Scholar]
- 21.Koek HL, Soedamah-Muthu SS, Kardaun JW, et al. Short- and long-term mortality after acute myocardial infarction: comparison of patients with and without diabetes mellitus. Eur J Epidemiol. 2007;22(12):883-888. doi: 10.1007/s10654-007-9191-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watanabe N, Takagi K, Tanaka A, et al. Ten-year mortality in patients with ST-elevation myocardial infarction. Am J Cardiol. 2021;149:9-15. doi: 10.1016/j.amjcard.2021.03.008 [DOI] [PubMed] [Google Scholar]
- 23.Chaudhry SI, Khan RF, Chen J, et al. National trends in recurrent AMI hospitalizations 1 year after acute myocardial infarction in Medicare beneficiaries: 1999-2010. J Am Heart Assoc. 2014;3(5):e001197. doi: 10.1161/JAHA.114.001197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bucholz EM, Butala NM, Rathore SS, Dreyer RP, Lansky AJ, Krumholz HM. Sex differences in long-term mortality after myocardial infarction: a systematic review. Circulation. 2014;130(9):757-767. doi: 10.1161/CIRCULATIONAHA.114.009480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kontos MC, Rennyson SL, Chen AY, Alexander KP, Peterson ED, Roe MT. The association of myocardial infarction process of care measures and in-hospital mortality: a report from the NCDR®. Am Heart J. 2014;168(5):766-775. doi: 10.1016/j.ahj.2014.07.005 [DOI] [PubMed] [Google Scholar]
- 26.Ryan AM, Burgess JF Jr, Tompkins CP, Wallack SS. The relationship between Medicare’s process of care quality measures and mortality. Inquiry. 2009;46(3):274-290. doi: 10.5034/inquiryjrnl_46.03.274 [DOI] [PubMed] [Google Scholar]
- 27.Cholesterol Treatment Trialists’ Collaboration . Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomised controlled trials. Lancet. 2019;393(10170):407-415. doi: 10.1016/S0140-6736(18)31942-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krumholz HM, Radford MJ, Ellerbeck EF, et al. Aspirin for secondary prevention after acute myocardial infarction in the elderly: prescribed use and outcomes. Ann Intern Med. 1996;124(3):292-298. doi: 10.7326/0003-4819-124-3-199602010-00002 [DOI] [PubMed] [Google Scholar]
- 29.Krumholz HM, Radford MJ, Wang Y, Chen J, Heiat A, Marciniak TA. National use and effectiveness of beta-blockers for the treatment of elderly patients after acute myocardial infarction: National Cooperative Cardiovascular Project. JAMA. 1998;280(7):623-629. doi: 10.1001/jama.280.7.623 [DOI] [PubMed] [Google Scholar]
- 30.Zullo AR, Mogul A, Corsi K, et al. Association between secondary prevention medication use and outcomes in frail older adults after acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2019;12(4):e004942. doi: 10.1161/CIRCOUTCOMES.118.004942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.US Centers for Medicare & Medicaid Services . 5010 implementation—processing additional International Classification of Diseases, 9th Revision-Clinical Modification (ICD-9-CM) diagnosis and procedure codes in Pricer, Grouper, and the Medicare Code Editor (MCE). Accessed November 27, 2018. https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R2028CP.pdf
- 32.Murphy-Barron C, Pyenson B, Ferro C, Emery M. Comparing the Demographics of Enrollees in Medicare Advantage and Fee-For-Service Medicare. Accessed June 25, 2021. https://bettermedicarealliance.org/publication/comparing-the-demographics-of-enrollees-in-medicare-advantage-and-fee-for-service-medicare/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Expanded patient characteristics.
eReferences.
eTable 1. Clinical Classifications Software categories.
eTable 2. Overall patient characteristics by race: unweighted and weighted.
eTable 3. Overall patient characteristics by sex: unweighted and weighted.
eTable 4. Overall patient characteristics by dual Medicare-Medicaid eligibility: unweighted and weighted.
eTable 5. Overall patient characteristics by living in a health priority area: unweighted and weighted.
eTable 6. Inverse probability weight–adjusted rates of 10-year mortality and recurrence by demographic subgroups and index hospitalization year for all patients eligible for 10 years of follow-up.
eTable 7. Change in risk of 10-year mortality and recurrent AMI for patients hospitalized in 2007-2009 compared with 1995-1997 by demographic subgroups.
eTable 8. Observed rates of 10-year mortality and recurrent AMI by index hospitalization year and STEMI diagnosis.
eTable 9. Inverse probability weight–adjusted mortality rates for patients with and without a recurrent AMI by demographic subgroups.
eTable 10. Observed rate of CABG or PCI during the index AMI hospitalization by year and demographic subgroups.
eTable 11. Observed 10-year rate of CABG or PCI after the index AMI hospitalization by demographic subgroups.
eFigure 1. Distribution of mean age by demographic subgroups: 1995-2019.
eFigure 2. Adjusted hazard ratios for the associations of demographic subgroups with 10-year mortality and recurrent AMI.
eFigure 3. Adjusted Kaplan-Meier curves for 10-year mortality and recurrence by demographic subgroups: 1995-2009.
eFigure 4. Median days to death or recurrent AMI by index hospitalization year.
eFigure 5. Observed Kaplan-Meier curves for 10-year mortality and recurrent AMI by STEMI diagnosis and index hospitalization year.


