Highlights
-
•
A considerable number of digital interventions for skin cancer prevention have been evaluated.
-
•
Most skin cancer digital interventions focus on sun protection-related outcomes.
-
•
Most interventions use web-based digital technology (websites, webpages, mobile apps) rather than videos, emails or text messages alone as the delivery platform.
-
•
Multi-component digital interventions are effective in promoting sun protection and skin self-examination.
-
•
Almost all studies found digital interventions to be equally or more effective compared to non-digital interventions.
Keywords: Skin cancer, Digital intervention, Sun protection, Skin examination
Abstract
The skin cancer incidence rate has been rising, and digital health interventions can promote skin cancer prevention and detection behaviors. A systematic review was conducted to investigate the outcomes of digital interventions that promote sun protection and skin self-examination (SSE). This review examined studies that utilized randomized controlled designs or quasi-experiments, included outcomes related to sun safety or SSE, employed at least one digital platform, and were published in English from January 2000 to October 2020. A total of 62 studies were included in the review. Digital modalities included web-based (e.g., websites) alone (n = 29), mobile-based (e.g., mobile apps) alone (n = 12), game-based (n = 1), emails or text messages alone (n = 8), videos alone (n = 6), social media (n = 3), both text messages and mobile apps (n = 2), or both text messages and video (n = 1). Most studies (n = 44) only evaluated sun protection-related outcomes, seven studies assessed SSE outcomes only, nine studies examined both, and two assessed other related outcomes. Digital interventions are effective compared to non-intervention control conditions in promoting sun safety or SSE. Almost all studies found digital interventions to be equally or more effective compared to non-digital interventions. This review suggests that although the digital interventions varied, they showed promising effects on improving sun protection or SSE outcomes. Future research should include more sophisticated phase-based and rigorous longitudinal research designs, additional investigation of social media and other newer technologies, as well as more detailed reporting of methods and results.
1. Introduction
There is a growing burden of skin cancer among at-risk populations in the United States (US) and worldwide (Apalla et al., 2017). Trends for Non-Hispanic White people in the US and for populations living in the United Kingdom (UK), Sweden, Norway, Australia and New Zealand showed that there was an annual increase of more than 3% in melanoma cases from 1982 to 2011, and these trends are projected to continue at a similar rate until 2022 (Whiteman et al., 2016). In the US alone, the estimated number of new cases of melanoma in 2020 is 100,350, which constitutes 5.6% of all new cancer cases (NCI, 2020). In particular, adults aged 65 years and older, and women aged between 18 and 64 years are at highest risk for melanoma (Guy et al., 2015). As of 2011, the average number of potential life years lost per melanoma-related death was approximately 15, and costs attributable to melanoma-related outcomes were estimated to be $US39.2 million for morbidity and $US3.3 billion for mortality, respectively (Guy & Ekwueme, 2011).
Given the substantial health and economic burden of melanoma, preventive measures (e.g., sun protection) and early detection efforts (e.g., skin self-examination) are warranted. Optimal and frequent use of sunscreen and other sun protection methods (e.g., wearing wide-brimmed hats, long-sleeved shirts, and staying in the shade) has been found to be associated with reduced melanoma risk (Lazovich et al., 2011). It has also been found that increased skin awareness and examination may be associated with survival rate among patients with melanoma (Curiel-Lewandrowski et al., 2012, Mishra et al., 2019, Paddock et al., 2016, Rutten et al., 2009). The use of a range of sun protection methods and routine SSE have the potential to prevent skin cancers and improve early detection and melanoma treatment outcomes. However, there are some important gaps that need to be addressed. Interventions that promote sun protection should focus on improving behavioral outcomes rather than promoting knowledge only (Goulart & Wang, 2010). Interventions aimed at increasing SSE have only been moderately successful. Interventions that employ novel strategies such as digital education programs other than mere photographs of lesions to improve the accuracy of SSE on patients’ own skin during self-examination may be needed to enhance outcomes (Hamidi et al., 2010).
In recent years, there has been a significant increase in health interventions that use a variety of digital modalities to target health behaviors and psychosocial outcomes due to their potential wide reach and cost effectiveness (Viola et al., 2020). Digital health interventions are interventions that are delivered through digital technologies such as smartphones, websites, or text messaging in order to improve health and health care (Murray et al., 2018). Due to the rapid increase in engagement in digital health, it is important to harness the potential of digital interventions. Although there is some evidence that individuals are receptive to these types of innovative interventions (Dennis et al., 2015) and would like to receive tailored information and training regarding melanoma prevention (Hall & Murchie, 2014), little is known about the efficacy of various types of digital modalities to promote sun protection and/or SSE among at-risk groups (Murray et al., 2018).
Prior systematic reviews have not comprehensively evaluated the effects of skin cancer-related interventions delivered through digital platforms. Previous skin cancer-related reviews focused on mobile technologies only (Finch et al., 2016), general technology, environment and theory (Taber et al., 2018), or SSE only (Ersser et al., 2019); whereas, the current review aimed to investigate the effects of various types of digital skin cancer interventions or experiments on both sun protection and SSE-related outcomes. Thus, this systematic review had two goals: to determine the frequency with which various digital platforms had been used for skin cancer-related interventions and to identify and summarize the cognitive or behavioral effects of skin cancer-related interventions using digital approaches. The findings of this review can inform the field by providing an up-to-date comprehensive assessment of the effects of digital interventions that used different modalities to promote skin cancer prevention-related outcomes and identify gaps for future research.
2. Methods
2.1. Systematic review reporting and approach
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to conduct and report the results of this systematic review (Moher, 2009). The review protocol was entered in the international prospective register of systematic reviews (PROSPERO; ID: 159491). We used a narrativerather than a quantitative approach to analyze the results due to the heterogeneity across extracted studies in terms of methods and outcomes. Institutional Review Board approval was not required for this review since it did not involve original data collection or analyses from human subjects.
2.2. Study inclusion criteria
The Population, Intervention, Comparison, Outcomes, and Study types (PICOS) framework (Methley et al., 2014) was used to guide the study inclusion criteria as follows: (1) Population—all populations, with the exception of interventions that targeted health care providers (e.g., to improve diagnosis of potential skin lesions); (2) Intervention—one of the interventions or experimental groups should be delivered entirely through a digital format such as social media, webpages, websites, apps, videos, emails, or text messages; (3) Comparison group(s)—tested the effect of an intervention or experimental condition compared to one or more other interventions and/or a control condition where no intervention was provided; (4) Outcomes—cognitive or behavioral outcomes related to sun safety (e.g., tanning, sunscreen use) or skin self-examination; (5) Study Design—randomized or quasi-experimental intervention; (6) Published in a peer-reviewed, English language journal and (7) Published (including online first) from January 1, 2000 to October 13, 2020. Digital formats combined with other non-digital formats such as in person or printed materials were excluded since the unique effects of each could not be determined.
2.3. Literature search and study screening
We used two approaches to identify potential studies for this review: a systematic search and checking reference lists of relevant review studies. A systematic search was conducted in the databases CINAHL, PsycINFO, PubMed, and Web of Science for peer-reviewed journals that were published from January 2000 to October 2020. The first author worked with a research librarian to optimize the search terms and search strategy. We used a combination of search terms including three categories: (1) skin cancer/sun protection/skin self-examination terms such as “sun protect*”, “sunscreen agents”, “sun safety”, “protective cloth*”, “sunburn*”, and so n; and (2) study design such as experiment or randomized control trial (RCT) and so on; and (3) digital platform such as social media, app, digital, Internet, web-based, website, text messaging, and so on. In order to identify additional potentially relevant studies, we reviewed the studies included in previous relevant systematic reviews and also searched for citations of those reviews. Data pertaining to specific aspects of each study were extracted: authors and year, sample(s) and size, mean age of participants, digital media, and comparison groups (Table 1). Additional information including allocation, group design, and use of theory, study length, targeted outcomes, and results are shown in Appendix A (Table A. Expanded study characteristics of included studies).
Table 1.
Study characteristics of included studies.
| Authors, yeara | Comparison groups | Sample (N) | Mean age (years) | Outcomesb | Digital media |
|---|---|---|---|---|---|
| Agha-Mir-Salim et al., 2020 (UK) | Digital vs. Printed | 279 university students | n/a | SP | Facebook (FB) |
| Gough et al., 2017 (Northern Ireland) | Digital vs. Digital | Pre-337; post-429 | Pre-35.6; post-35.2 | SP | |
| Mingoia et al., 2019 | Digital vs. No-intervention control | 84 White women | 22.3 | SP | Private FB group |
| Armstrong et al., 2011 | Digital vs. Printed | 94 adults | 39.6 ± 14 | SP | Online video |
| Bleakley et al., 2020 | Digital vs. Digital | 1044 non-Hispanic White adults | 30.2 | SP | Videos |
| Jordan et al., 2020 | Digital vs. Digital | 480 White women | 21.8 | SP | Videos |
| Idriss et al., 2009 | Digital vs. Printed | 78 adults | 35.8 ± 13.0 | SP | Video-based |
| Stock et al., 2009 | Digital vs. No-intervention control | 148 adult male outdoor workers | 46.5 | SP | Photo-aging Video |
| Tsai et al., 2018 | Digital vs. Printed | 143 African Americans adults | C: 45; I: 39.6 | SP | Video |
| Böttcher et al., 2019 (Germany) | Digital vs. Printed | 137 Organ transplant recipients | 12.6 | SP | Video, SMS |
| Armstrong et al., 2009 | Digital vs. No-intervention control | 70 adults | 33.6 | SP | Text messaging |
| Baker et al., 2016 | Digital vs. Digital | 512 adults | 31.87 | Both | Text messaging |
| Darlow and Heckman, 2017 | Digital vs. Digital | 102 women | 24.4 | SP | Text messaging |
| Dixon et al., 2007 (Australia) | Digital vs. Digital | 557 Australian adult workers | n/a | SP | |
| Evans and Mays, 2016 | Digital vs. Digital | 21 young adult women | 24.9 | SP | Text messaging |
| Gold et al., 2011 (Australia) | Digital vs. Digital | 358 Australian mobile advertising subscribers | Median: 25.3 | SP | Text messaging |
| Szabó et al., 2015 (Hungary) | Digital vs. Oral | 149 staff members and relatives from a clinic in Hungary | 36.94 ± 10.25 | SP | Text messaging |
| Youl et al., 2015 (Australia) | Digital vs. Digital | 546 Australian adults | n/a | Both | Text messaging |
| Bernhardt, 2001 | Digital vs. Digital | 83 undergraduates | 21.6 | SP | Web-based |
| Bowen et al., 2015 | Digital vs. No-intervention control | 311 families with at least one case of melanoma | 56.11 | Both | Web-based |
| Bowen et al., 2017 | Digital vs. No-intervention control | 313 families with at least one case of melanoma | Cases: 56.1; FDR’s: 51; Parents: 37.1 | Melanoma risk/Communication and agreement | Web-based |
| Bowen et al., 2019 | Digital vs. No-intervention control | 311 families with at least one case of melanoma | 51.32 | Both | Web-based |
| Buendia Eisman et al., 2013 (Spain) | Digital vs. No-intervention control | 1290 adolescents in schools in Spain | 13.75 | SP | Web-based |
| Cho et al., 2020 | Digital vs. No-intervention control | 518 college women | 20.13 | SP | Web-based |
| Craciun et al., 2012a, Craciun et al., 2012b | Digital vs. No-intervention control | 292 adults | 25.33 (18–65) | SP | Web-based |
| Craciun et al., 2012a, Craciun et al., 2012b | Digital vs. No-intervention control | 205 women | 25.04 | SP | Web-based |
| Heckman et al., 2016 | Digital vs. No-intervention control | 629 adults at risk for skin cancer | 21.8 | Both | Web-based |
| Heckman et al., 2017 | Digital vs. No-intervention control | 594 at risk for skin cancer | 21.98 | SP | Web-based |
| Hillhouse et al., 2017 | Digital vs. Digital | 443 female teens | 15.2 | SP | Web-based |
| Lemal and Van den Bulck, 2010 (Belgium) | Digital vs. No-intervention control | 230 Flemish university students | 20.3 | Both | Web-based |
| Lustria, 2007 | Digital vs. Digital | 441 undergraduates | 19.3 | Skin cancer comprehension | Web-based |
| Manne et al. 2020 | Digital vs. Digital | 75 partners | 39.5 | SP | Web-based |
| Stapleton et al., 2015 | Digital vs. No-intervention control | 187 young adult women who reported indoor tanning (IT) ≥ 1 in the past 12 months | 19.78 | SP | Web-based |
| White et al., 2015 (Australia) | Digital vs. Digital | 532 Australian adults | 39.3 | SP | Web-based |
| Sontag and Barnes, 2017, Sontag and Noar, 2017 | Digital vs. Digital | 190 undergraduates | 20.29 | SP | Web-based |
| van ’t Riet et al., 2010 | Digital vs. Digital | 124 undergraduates | 20.7 | SSE | Web-based |
| Mays and Evans, 2017 | Digital vs. Digital | 552 young adult White women and who reported IT | 24.9 | SP | Web-based |
| Jensen et al., 2017 | Digital vs. Digital | 635 adults | 32.43 | SSE | Web-based |
| Landau et al., 2018 | Digital vs. Digital | Study 1 (187), Study 2 (192), Study 3 (186) | Study 1: 33.54; Study 2: 19; Study 3: 34.72 | SP | Web-based |
| Lee and Kang, 2018 | Digital vs. Digital | 397 undergraduates | Study 1: 20.39; Study 2: 20.58 | SP | Web-based |
| Lewis, 2013 | Digital vs. Digital | ≥ 18, parents of at least one child between the ages of 5 years and 9 years (498;467) | 35.1%: 30–39 | SP | Web-based |
| Mays and Tercyak, 2015 | Digital vs. Digital | 682 young White women who reported IT ≥ 1 in the past year | 24.3 | SP | Web-based |
| Mays and Zhao, 2016 | Digital vs. Digital | 475 young adult women who reported IT ≥ 1 in the past year | 24.7 | SP | Web-based |
| Mingoia et al., 2019 (Australia) | Digital vs. Digital | 151 Australian young Adults | 18–29 | SP | Web-based |
| Myrick, 2019 | Digital vs. Digital | 1068 adults | 34.78 | Both | Web-based |
| Sontag and Barnes, 2017, Sontag and Noar, 2017 | Digital vs. Digital | 568 female sorority members | 19.8 | SP | Web-based |
| Vollmann et al., 2021 | Digital vs. Digital | 509 adults without skin cancer | 39 | SP | Web-based |
| Lansdown et al., 2020 (UK) | Digital vs. No-intervention control | 112 adults | 18–65 | SP | SMS and mobile app |
| Nioi et al., 2020 (UK) | Digital vs. No-intervention control | 178 adults in construction industry | 18–65 | SP | SMS and mobile app |
| Brinker et al., 2020 (Germany) | Digital vs. No-intervention control | 1573 Brazilian pupils | 15.9 | Both | Mobile app |
| Buller et al., 2015a, Buller et al., 2015b | Digital vs. No-intervention control | 193 adults & smartphone owners | n/a | SP | Mobile app |
| Buller et al., 2015a, Buller et al., 2015b | Digital vs. No-intervention control | 454 Non-Hispanic or Hispanic white | 68.5% <45 years | SP | Mobile app |
| Hacker et al., 2018(Australia) | Digital vs. No-intervention control | 107 Australian young adults | 25.8 | SP | Mobile app and dosimeter |
| Janda et al., 2020 (Australia) | Digital vs. Digital | 234 adults at risk for skin cancer | 41.1 | SSE | Mobile teledermoscopy |
| Manahan et al., 2015(Australia) | Digital vs. Digital | 58 Australian adults at high risk for melanoma | 39%: 50–54 | SSE | Mobile teledermoscopy |
| Marek et al., 2018 | Digital vs. Digital | 69 adults patients owning an iPhone/iPad | 54.3 | SSE | Mobile app |
| Niu et al., 2019 | Digital vs. Digital | 134 undergraduates | 19.94 | SP | Mobile and web-based |
| Robinson et al., 2015 | Digital vs. Digital | 170 kidney transplant recipients | 51.0 | SP | Mobile app |
| Robinson et al., 2016 | Digital vs. Digital | 170 kidney transplant recipients | C: 49.0; I: 51.0 | SP | Mobile app |
| Robinson et al., 2014 | Digital vs. In-person vs. Printed | 500 pairs of patients having stage 0 to IIB melanoma and their significant others | Workbook: 55.19; Electronic: 55.19; In-person: 54.70 | SSE | Mobile-a tablet device |
| Walter et al., 2020 (UK) | Digital + Written vs. Written | 238 adults | Median: 55 | SSE | Mobile app |
| Maganty et al., 2018 | Comparison groups | 60 patients from Mayo Clinic | 59.1 | Both | Game-based |
Note. a United States-based study unless noted.
b SP = sun protection, SSE = skin self-examination, Both = sun protection and skin self-examination.
The first column of the table was ordered by modalities.
2.4. Study quality coding
The quality of each study was evaluated using a nine-item yes/no checklist adapted from prior research (Ersser et al., 2019, Murray et al., 2018, Teixeira et al., 2015) including the Effective Public Health Practice Project Quality Assessment Tool (Armijo-Olivo et al., 2012) that evaluated the following criteria: (1) Did the study include a theoretical framework for the intervention/experiment? (2) Was participant selection bias minimized (e.g., using random recruitment)? (3) Did the study use randomized allocation? (4) Were the psychometric properties of all outcome measures acceptable? (5) Did the authors report a power calculation related to the sample size? (6) Did the report mention attrition rate/retention rate of the study? (7) Did the study account for potential confounders? (8) Did the analyses use acceptable statistical methods? and (9) Were inclusion/exclusion criteria clear? The number of “Yes” answers was recorded for each study with possible scores ranging from 0 to 9.
3. Results
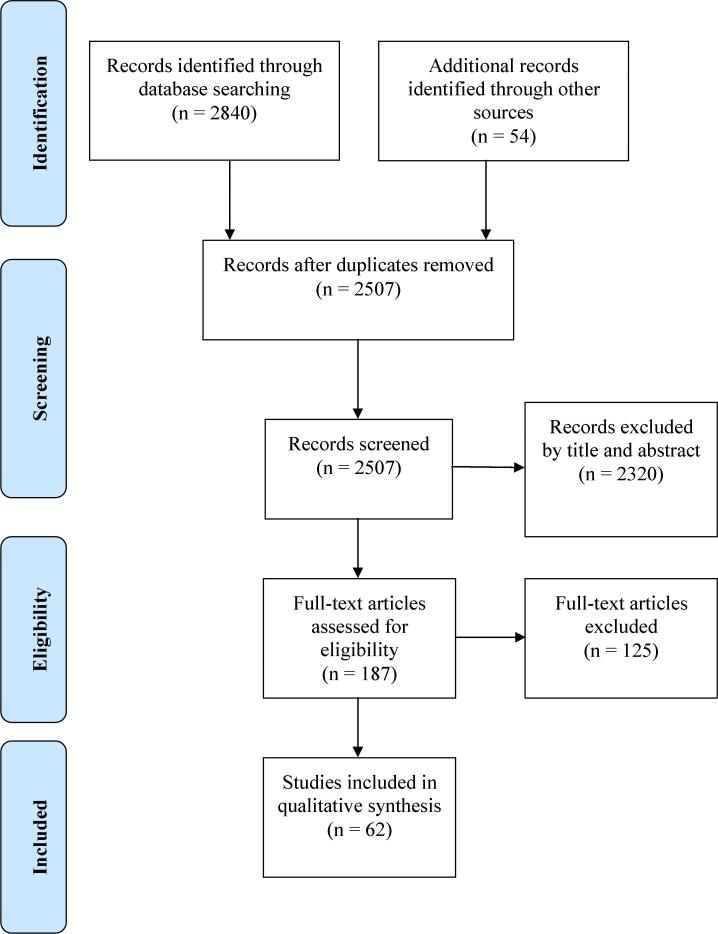
A total of 2,840 articles were generated from the electronic database search by subject terms and 54 additional articles were found through the reference lists of relevant review studies. After removal of duplicates, 2507 studies were screened. Among them, 2320 records were excluded by title and abstract, and 187 full-text articles were assessed. The first two authors (ZN and TB) screened all articles based on article titles, abstracts, and full texts as needed. Discrepancies about article inclusion between the two authors were resolved by the third author (CH). With 125 full-text articles excluded, the final number of included studies for the review was 62. A flow diagram of the literature search process is shown in Fig. 1.
Fig. 1.
PRISMA flow diagram.
3.1. Study characteristics
Study characteristics of included studies are displayed in Table 1. Most studies were conducted in the United States (n = 44), followed by Australia (n = 8), the UK (n = 4), Germany (2), Northern Ireland (n = 1), Hungary (n = 1), Spain (n = 1), and Belgium (n = 1). The sample size of included studies ranged from 21 (Evans & Mays, 2016) to 1290 (Buendia Eisman et al., 2013). The mean age of the study samples ranged from 13.75 (Buendia Eisman et al., 2013) to 59.1 (Maganty et al., 2018) years. Only one study (Gough et al., 2017) used a quasi-experimental design; whereas, the rest (n = 61) reported using randomized assignment of the participants into different study groups. More than two-thirds of the studies used at least one theoretical framework or construct to guide their intervention or experimental design (n = 40). Forty-nine studies used a pre-post measurement study design and 11 articles (Bleakley et al., 2020, Jordan et al., 2020, Landau et al., 2018, Lee and Kang, 2018, Lewis, 2013, Lustria, 2007, Manahan et al., 2015, Nioi et al., 2020, Niu et al., 2019, Sontag and Barnes, 2017, Sontag and Noar, 2017) used posttest design only. The study duration varied from immediately post intervention (n = 32) to 12-month follow-up (n = 8). It is worthy noticing that some publications reported results from the same study, such as the two Heckman et al. studies (Heckman et al., 2016, Heckman et al., 2017) and Robinson et al.’s studies in 2015 and 2016 (Robinson et al., 2015; Robinson et al., 2016).
3.2. Intervention modalities
Among the studies included in this review, most interventions or experiments were delivered through web-based (n = 29) and mobile-based platforms (n = 12), followed by delivery via email or text messages alone (n = 8) (Armstrong et al., 2009, Baker et al., 2016, Darlow and Heckman, 2017, Dixon et al., 2007, Evans and Mays, 2016, Gold et al., 2011, Szabó et al., 2015, Youl et al., 2015), videos (n = 6) (Armstrong et al., 2011, Bleakley et al., 2020, Idriss et al., 2009, Jordan et al., 2020, Stock et al., 2009, Tsai et al., 2018), social media (n = 3) (Agha-Mir-Salim et al., 2020, Gough et al., 2017, Mingoia et al., 2019), both text messages and mobile apps (n = 2) (Lansdown et al., 2020, Nioi et al., 2020), both text messages and video (n = 1) (Böttcher et al., 2019), and a game (n = 1) (Maganty et al., 2018).
Web-based modalities were the most popular digital methods used for skin cancer interventions. Twenty-one studies utilized interactive websites or webpages to deliver their interventions (Bernhardt, 2001, Bowen et al., 2015, Bowen et al., 2017, Bowen et al., 2019, Buendia Eisman et al., 2013, Cho et al., 2020, Craciun et al., 2012a, Craciun et al., 2012b, Heckman et al., 2016, Heckman et al., 2017, Hillhouse et al., 2017, Lemal and Van den Bulck, 2010, Lustria, 2007, Manne et al., 2020, Mays and Evans, 2017, Mingoia et al., 2019, Sontag and Barnes, 2017, Stapleton et al., 2015, van ’t Riet et al., 2010, Vollmann et al., 2021, White et al., 2015). Eight studies (Jensen et al., 2017, Landau et al., 2018, Lee and Kang, 2018, Lewis, 2013, Mays and Tercyak, 2015, Mays and Zhao, 2016, Myrick, 2019, Sontag and Noar, 2017) presented intervention materials embedded in online surveys (e.g., via Qualtrics). Intervention materials embedded in online surveys such as in Qualtrics usually tend to lead to a linear process for participants and are different than a process of a well-established website-based intervention. The content of web-based interventions includes generic sun protection messages vs. tailored messages, comprehensive information about SSE and sun protection, indoor tanning information, narrative vs. non-narrative messages about SSE and sun protection, sun safety partners, different framing of skin cancer, SSE, and indoor tanning, etc. More details about the intervention content are shown in Appendix A (Table A).
Six studies (Buller et al., 2015a, Buller et al., 2015b, Hacker et al., 2018, Marek et al., 2018, Robinson et al., 2015; Robinson et al., 2016) used mobile apps to deliver the intervention/experiments; whereas, two studies (Niu et al., 2019, Robinson et al., 2014) used mobile-based materials (e.g., mobile webpages, electronic interactive program), and two studies used mobile tele-dermoscopy (Manahan et al., 2015). Mobile apps usually cost more in development and have more functions and flexibilities for users than mobile webpages, electronic interactive program, and mobile tele-dermoscopy.
Ten additional studies employed message-based methods including text messages (n = 6) (Armstrong et al., 2009, Baker et al., 2016, Darlow and Heckman, 2017, Evans and Mays, 2016, Gold et al., 2011, Youl et al., 2015), text messages with a mobile app (n = 2) (Lansdown et al., 2020, Nioi et al., 2020), text messages vs. videos (n = 1) (Böttcher et al., 2019), emails (n = 1) (Dixon et al., 2007), or both text messages and emails (n = 1) (Szabó et al., 2015). The content of text messages or emails included reminders, sun protection advice, tailored messages, behavioral tracking messages, weather forecast, gain-loss framed messages, and/or multimedia content.
Six studies used videos only as the digital delivery method (Armstrong et al., 2011, Bleakley et al., 2020, Idriss et al., 2009, Stock et al., 2009, Tsai et al., 2018), among which three studies compared video vs. brochure/pamphlet (Armstrong et al., 2011, Idriss et al., 2009, Tsai et al., 2018), and three studies compared different video content across groups (i.e., sunscreen video vs. seeking shade video vs. covering up video vs. general sun protection video (Bleakley et al., 2020); photoaging video vs. skin cancer video vs. no video (Stock et al., 2009); well-being video vs. appearance video vs. skin cancer video (Jordan et al., 2020).
Only three studies used social media as the digital media platform to conduct the interventions: two studies (Agha-Mir-Salim et al., 2020, Mingoia et al., 2019) using Facebook and one using Twitter (Gough et al., 2017). One study used a game-based (Maganty et al., 2018) intervention.
3.3. Types of outcomes
All possible outcomes (including primary and secondary outcomes) from the studies in this systematic review are presented in Appendix A (Table A). Forty-four studies (71.0%) focused on only sun protection or ultraviolet radiation (UV) exposure-related outcomes, among which four studies examined self-reported sunburns (Buendia Eisman et al., 2013, Gold et al., 2011; Robinson et al., 2016, Stapleton et al., 2015). Seven studies (11.3%) focused on SSE-related outcomes only (Jensen et al., 2017, Maganty et al., 2018, Manahan et al., 2015, Marek et al., 2018, Robinson et al., 2014, van ’t Riet et al., 2010). Nine studies (14.5%) assessed both sun protection and SSE-related outcomes (Baker et al., 2016, Bowen et al., 2015, Bowen et al., 2019, Heckman et al., 2016, Lemal and Van den Bulck, 2010, Myrick, 2019, Youl et al., 2015). One study evaluated skin cancer knowledge only (Lustria, 2007), and one assessed the frequency of communication about family cancer history and agreement among family beliefs regarding melanoma risk (Bowen et al., 2017).
Twenty-eight studies assessed cognitive outcomes related to sun protection or SSE only (Agha-Mir-Salim et al., 2020, Bleakley et al., 2020, Craciun et al., 2012b, Evans and Mays, 2016, Gough et al., 2017, Hillhouse et al., 2017, Idriss et al., 2009, Jensen et al., 2017, Landau et al., 2018, Lee and Kang, 2018, Lewis, 2013, Lustria, 2007, Maganty et al., 2018, Mays and Evans, 2017, Mays and Tercyak, 2015, Mays and Zhao, 2016, Mingoia et al., 2019, Myrick, 2019, Niu et al., 2019, Robinson et al., 2014, Robinson et al., 2015, Sontag and Barnes, 2017, Sontag and Noar, 2017, Stapleton et al., 2015, van ’t Riet et al., 2010). Examples of cognitive outcomes that were assessed included knowledge of skin cancer or melanoma, perceived risk of getting skin cancer, skin cancer or melanoma awareness, attitudes toward UV exposure, beliefs underlying indoor tanning, sunscreen knowledge, self-efficacy in wearing sunscreen, self-efficacy for detection of melanoma, and beliefs underlying doing SSE (Agha-Mir-Salim et al., 2020, Bernhardt, 2001, Evans and Mays, 2016, Gold et al., 2011, Gough et al., 2017, Hillhouse et al., 2017, Idriss et al., 2009, Tsai et al., 2018, van ’t Riet et al., 2010, Armstrong et al., 2011).
Fifteen studies examined only behavioral outcomes related to sun protection, exposure, or skin examination (Baker et al., 2016, Bowen et al., 2015, Bowen et al., 2019; Buller et al., 2015a, Buller et al., 2015b, Dixon et al., 2007, Heckman et al., 2016, Lemal and Van den Bulck, 2010, Manahan et al., 2015, Marek et al., 2018, Youl et al., 2015). Examples of sun protection or exposure behaviors that were examined included wearing sunscreen, hat and protective clothing, behaviors related to UV exposure (e.g., wearing clothes that expose the skin to sun), indoor and outdoor tanning behaviors, engaging in outdoor exercise, yardwork, or gardening, being outdoors for more than a few minutes at a time, looking for additional information on skin cancer, and talking to family members about skin cancer. Examples of SSE-related behaviors were conducting skin self-examination including checking all areas of the body and the use of professional total body photography to conduct SSE. Two studies examined not only sun protection and SSE behaviors but also provider screening behaviors (Bowen et al., 2015, Bowen et al., 2019).
Nineteen studies assessed both cognitive and behavioral outcomes, all of which were related to sun protection or UV exposure. The outcomes measured included sun protection behaviors, attitudes, sunscreen knowledge, adherence to sunscreen application, self-reported UV exposure, and action and coping planning-related to sun protection. Only one study used a biologic measure of sun protection (melanin index, a measure of skin pigmentation) (Robinson et al., 2016), and all others assessed self-reported dependent variables.
3.4. Effects of interventions on outcomes
Due to the heterogeneity of the intervention modalities, study designs, and primary and secondary outcomes, no particular type of intervention was found to be more effective than other types of interventions. Effects of interventions were summarized based on digital vs. no-intervention control groups, digital vs non-digital interventions, and digital vs. digital interventions to compare the effectiveness of different digital skin cancer intervention design.
Nineteen studies compared digital modalities with no-intervention control groups, and thirty-four compared different digital modalities or digital messages with one another. Fifteen of the former studies showed support for the effectiveness of digital interventions on skin cancer-related outcomes such as deceasing positive tanning attitudes, increasing sun protection behaviors, improving SSE performance, etc. (Armstrong et al., 2009, Bowen et al., 2017, Bowen et al., 2015, Bowen et al., 2019, Brinker et al., 2020, Buendia Eisman et al., 2013, Buller et al., 2015a, Cho et al., 2020, Hacker et al., 2018, Heckman et al., 2016, Heckman et al., 2017, Lemal and Van den Bulck, 2010, Mingoia et al., 2019, Nioi et al., 2020, Stock et al., 2009). The rest four studies compared digital modalities with no-intervention control groups showed mixed results such as digital intervention was effective on more shade use but less sunscreen use than controls (Buller et al., 2015a, Buller et al., 2015b, Craciun et al., 2012a, Lansdown et al., 2020, Stapleton et al., 2015). The results of the studies that compared digital interventions to one another varied, and the three social media study results were mixed.
There are nine studies that used non-digital conditions as comparison groups, which included printed materials, and in-person oral sessions. Among nine studies comparing digital intervention with non-digital comparison groups, four studies found that digital intervention groups (videos and/or text messaging) were more effective at increasing sun protection behaviors, knowledge, self-efficacy, and melanoma awareness than non-digital interventions (Armstrong et al., 2011, Idriss et al., 2009, Szabó et al., 2015). Three other studies found that digital interventions including videos, apps, reminders, and/or games compared to non-digital interventions such as those using printed materials were both effective at improving sun protection behaviors, knowledge, self-efficacy, SSE rates, and detection of melanoma features (Maganty et al., 2018, Marek et al., 2018, Tsai et al., 2018). One study found that printed materials were more effective than digital interventions. Agha-Mir-Salim et al. (Agha-Mir-Salim et al., 2020) compared effects of Facebook posts with those of information leaflets and found that the printed leaflets increased skin cancer knowledge and sun protection knowledge more than Facebook posts. One study reported mixed results that an SSE intervention via a tablet device was as effective as that via a workbook in increasing self-confidence for identifying and monitoring moles. However, when it came to a skill-based quiz, the digital intervention was more effective than the workbook intervention but less effective than an in-person intervention for SSE (Robinson et al., 2014). Additionally, digital modalities tended to generate better results in measures of user experience such as satisfaction (Marek et al., 2018) and enjoyment (Maganty et al., 2018) compared to other modalities.
The studies that included digital comparison groups yielded results that varied by the nature of the interventions. Studies that used gain- and loss-framing, narrative factors, interactivity, messages that focused on different health topics and/or other elements varied significantly on their effects on different outcomes. For example, one study found that participants in a technical instructions of mobile tele-dermoscopy plus detailed SSE instructions group (intervention) were more like to report lesions than those in a technical instructions only group (control). Another study reported that the use of mobile tele-dermoscopy did not increase sensitivity for the detection of skin cancers compared with naked-eye skin self-examination (Janda et al., 2020). Based on studies using factorial designs, digital tailored messages (Bernhardt, 2001), forming action and coping plans (Hacker et al., 2018), and loss-framed messages related to tanning (Lee and Kang, 2018, Mays and Tercyak, 2015) worked better in improving skin cancer-related outcomes than the comparison conditions.
The results regarding the impact of social media interventions were mixed. One study had a digital comparison groups (Agha-Mir-Salim et al., 2020, Gough et al., 2017), and two studies had a non-intervention control group (Mingoia et al., 2019). Compared to control groups, social media interventions exerted effects such as improved skin cancer knowledge (i.e., Twitter) (Gough et al., 2017) and decreased pro tanning attitudes and tanning intentions (i.e., Facebook private groups) (Mingoia et al., 2019). One study found that printed leaflets increased skin cancer and sun knowledge more than Facebook posts (Agha-Mir-Salim et al., 2020). It is worth mentioning that studies that utilized multicomponent interventions (Bowen et al., 2017, Bowen et al., 2015, Bowen et al., 2019) and used more than one type of digital modality (Lansdown et al., 2020, Nioi et al., 2020, Szabó et al., 2015) also exerted positive effects on sun protection or SSE outcomes.
3.5. Study quality
Our study quality assessment checklist was derived from previous research (Murray et al., 2018, Teixeira et al., 2015), and the score for each study is shown in Appendix B (Table B). Scores of study quality ranged from 3 to 8, and the mean score was 5.68. Studies were likely to meet criteria for randomized allocation (n = 61), appropriate statistical analysis (n = 60), clear participant inclusion or exclusion criteria (n = 52), mentioning attrition rate/retention rate (n = 46), and including a theoretical framework for the intervention/experiment (n = 40). The four categories for which the fewest studies met quality criteria were acceptable psychometric properties of all of the outcome measures (n = 40), accounting for potential confounders (n = 33), reporting a power calculation (n = 16), and random selection of the participants (n = 9).
4. Discussion
4.1. Principal results
The use of digital tools in improving health behaviors has been on the rise in the past two decades (Boß et al., 2016). This study reviewed the effects of digital interventions on skin cancer prevention- or detection-related outcomes including sun protection and SSE. Whereas prior skin cancer intervention-related reviews have focused on mobile technologies only (Finch et al., 2016), general technology, environment and theory (Taber et al., 2018), and SSE only (Ersser et al., 2019), the current study assessed the effects of various types of digital interventions or experiments on both sun protection and SSE-related outcomes. The findings from this review covered a more comprehensive list of studies and the results on mobile-based interventions are consistent with the previous review focusing on mobile technologies (Finch et al., 2016). These findings can be informative for future programs aiming to employ digital methods to design or implement effective skin cancer-related interventions.
The most popular digital methods for skin cancer-related interventions were web-based platforms including webpages on mobile devices and computers. Compared to non-web-based interventions, web-based interventions have more flexibility and more features available for intervention design (Wantland et al., 2004). Intervention materials embedded in online surveys often tend to mimic certain features of other types of websites, and researchers usually have more control over the participants in the study, which may have advantages for testing specific hypotheses. However, the effects may not be the same as the effects from other types of websites since individuals’ browsing habits may be limited by the embedded materials. Text messages, emails, and videos were also often used to promote sun protection or SSE-related health outcomes. The relatively wide application of text messages, emails or videos as digital tools to deliver interventions can be attributed to their relatively low cost, large potential audience, and ease of adoption (Ostherr et al., 2016, Willoughby and Furberg, 2015). Surprisingly, social media was less used compared to other digital modalities, which could be due to the recency of the platforms, complexity of the structures, lower levels of control and transparency, and privacy issues on social networking sites (Pagoto et al., 2016). Consistent with findings from a previous review of skin cancer interventions, we did not find any study that used integrated technologies such as a combination of objective measure of UV-relevant behaviors, sensors, or user-centered systems designed based on gathering data/feedback from users (Taber et al., 2018), which would be major advancements.
Most of the studies provided promising evidence to support that digital methods are effective in improving cognitive and behavioral outcomes related to sun protection or SSE. For example, most of the studies that compared digital intervention groups with non-intervention control groups reported desirable improvements in sun protection or SSE outcomes. Additionally, skin cancer interventions that used digital modalities such as videos, text messaging, mobile apps, and/or games had equal or greater effects at increasing sun protection or SSE-related perceptions and/or behaviors than printed materials, in-person oral presentations, or human partners. However, studies comparing digital intervention groups with non-digital intervention groups displayed conflicting findings. Non-digital materials could be more effective in increasing skin cancer knowledge than digital interventions (Agha-Mir-Salim et al., 2020) or less effective than digital interventions in some situations (Armstrong et al., 2011, Idriss et al., 2009, Szabó et al., 2015). Some studies also suggested no difference between digital interventions and non-digital interventions (Maganty et al., 2018, Mays and Evans, 2017, Tsai et al., 2018).
The digital methods used and their effects on study outcomes varied across studies. Among the studies that used social media, one study indicated that the Facebook intervention was less effective than printed materials (Agha-Mir-Salim et al., 2020). However, studies that used formative research methods or pilot tested the efficacy of social media for skin cancer-related outcomes have found positive effects of social media interventions (Coups et al., 2018, Stapleton et al., 2018). More skin cancer interventions should explore the potential influences of social media on both sun protection and SSE-related outcomes given the powerful impact of misinformation and the indoor tanning industry on young adults through social media (Falzone et al., 2017, Pagoto et al., 2019). Social media are used to promote tanning advertisements, and the potential counter effects of skin cancer-related campaigns and interventions on social media warrant further investigation (Ricklefs et al., 2016). Video interventions were more effective at improving sun protection behaviors and melanoma knowledge compared to pamphlet interventions, (Armstrong et al., 2011, Idriss et al., 2009). Using electronic messages (emails and texts) resulted in greater sunscreen use than non-digital comparison groups (Szabó et al., 2015).
Studies comparing digital interventions groups with other digital intervention groups (e.g., loss-framed messages vs. gain-framed messages) or using quasi- or factorial experimental designs showed varied results. Specific types of interventions such as tailoring vs. non-tailoring or loss-framing vs. gain-framing may have various effects on different outcomes (e.g., perceptions or behaviors, sun protection or SSE). The effects of these interventions varied across studies and even within one study. For instance, in one study examining indoor tanning intentions, pictorial messages were perceived to be more effective than text-only messages; whereas, text-only messages were more believable than pictorial ones (Sontag & Noar, 2017). Findings regarding effectiveness of tailored interventions are not always consistent since individual needs for tailored information are different and it is hard to find one best mean to tailor interventions for all (Buller et al., 2015a, Buller et al., 2015b). Overall, the findings showed high heterogeneity related to different study designs, intervention and comparison conditions, and outcome measures.
The mixed findings regarding the effectiveness of digital versus non-digital interventions could be due to the discrepancies across the message content, outcome measurements, or participants. However, our review highlights the importance of designing more comprehensive digital interventions with appropriate digital methods and advocates for pilot testing with the target population before conducting large-scale intervention trials (Ersser et al., 2019). While reviewing the study designs, we found that few interventions provided design details or gave comprehensive examples of the messages they used in the interventions. For example, when we tried to determine the potential reason(s) why the Facebook intervention was less effective than printed leaflets, no information such as Facebook post examples, engagement level of the materials, and whether they used multimedia in the posts were presented (Agha-Mir-Salim et al., 2020). Thus, we advocate for reporting more details in digital intervention studies, which can help us understand change mechanisms and inform future research or campaigns.
In the current review, we included many brief experimental (or quasi-experimental) studies. The effects of the interventions in those studies may lack long-term impact. Most of the factorial experiments were designed to distinguish the effects of a specific factor or element (e.g., gain- or loss-framing) and no follow-up assessment was included. On the contrary, other RCTs of skin cancer-related outcomes tended to examine effects of a multicomponent intervention with one or more follow-up assessments and therefore focused on the overall impact and long-term effect rather than disentangling the effects of different elements. Therefore, we encourage future studies to combine 1) the advantages of factorial designs such as testing effectiveness of different message designs and 2) longitudinal RCT design which assess long-term effects of optimized interventions to enhance the efficacy of skin cancer interventions studies.
4.2. Strength and limitations
This review has several strengths. It focused on both sun protection and SSE outcomes, compared effects of digital interventions with at least one comparison group which were almost all randomized, and included a variety of populations from different countries and regions. The current review also has some limitations, including the focus on English-language studies only. We did not conduct quantitative data analysis due to the high heterogeneity of included studies. Additionally, this review excluded studies that used a non-experimental design, which means that all single-arm interventions were not assessed. This inclusion criterion might have excluded some potentially effective digital interventions.
5. Conclusions
This review showed a high level of heterogeneity within digital sun safety and SSE interventions. In general, web-based platforms were most utilized as digital skin cancer interventions. Skin cancer interventions using digital modalities have focused mostly on sun protection or sun exposure outcomes and less on SSE. Overall, the findings of this study showed that most skin cancer interventions employing one or more digital modalities and components had a positive impact on skin cancer-related outcomes. Future studies could develop multicomponent digital interventions using integrated features and data sources and compare their effects with those of single-featured interventions, such as combining message framing with mobile apps and/or text message reminders. Future research should also employ more rigorous phase-based and longitudinal research designs, interventions with multiple effective components, as well as objective measures and more sophisticated technology in order to improve skin cancer-related behaviors.
Funding source
This work was supported by the New Jersey Commission on Cancer Research (grant number: DCHS19PPC012) and the National Cancer Institute (grant number: P30CA072720).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank the librarian’s help (Yingting Zhang) on the search process.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2022.101709.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Agha-Mir-Salim L., Bhattacharyya A., Hart D., Lewandowska M., Spyropoulou E., Stinson L., Tiefenbach J. A randomised controlled trial evaluating the effectiveness of Facebook compared to leaflets in raising awareness of melanoma and harmful sun-related behaviour among young adults. Eur. J. Cancer Prev. 2020;29(1):89–91. doi: 10.1097/CEJ.0000000000000519. [DOI] [PubMed] [Google Scholar]
- Apalla Z., Lallas A., Sotiriou E., Lazaridou E., Ioannides D. Epidemiological trends in skin cancer. Dermatol. Practical Conceptual. 2017;7(2):1. doi: 10.5826/dpc.0702a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armijo-Olivo S., Stiles C.R., Hagen N.A., Biondo P.D., Cummings G.G. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. J. Evaluation Clin. Practice. 2012;18(1):12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- Armstrong, A. W., Idriss, N. Z., & Kim, R. H. (2011). Effects of video-based, online education on behavioral and knowledge outcomes in sunscreen use: a randomized controlled trial. Patient Education and Counseling, 83(2), 273-277. [DOI] [PubMed]
- Armstrong A.W., Watson A.J., Makredes M., Frangos J.E., Kimball A.B., Kvedar J.C. Text-message reminders to improve sunscreen use: a randomized, controlled trial using electronic monitoring. Arch. Dermatol. 2009;145(11):1230–1236. doi: 10.1001/archdermatol.2009.269. [DOI] [PubMed] [Google Scholar]
- Baker J., Finch L., Soyer H.P., Marshall A.L., Baade P., Youl P., Janda M. Mediation of improvements in sun protective and skin self-examination behaviours: results from the healthy text study. Psycho-Oncology. 2016;25(1):28–35. doi: 10.1002/pon.4007. [DOI] [PubMed] [Google Scholar]
- Bernhardt J.M. Tailoring messages and design in a Web-based skin cancer prevention intervention. Int. Electron. J. Health Educ. 2001;4:290–297. [Google Scholar]
- Bleakley A., Jordan A.B., Strasser A.A., Lazovich D., Glanz K. Testing general versus specific behavioral focus in messaging for the promotion of sun protection behaviors. Ann. Behav. Med. 2020;54(2):108–118. doi: 10.1093/abm/kaz032. [DOI] [PubMed] [Google Scholar]
- Boß L., Lehr D., Reis D., Vis C., Riper H., Berking M., Ebert D.D. Reliability and validity of assessing user satisfaction with web-based health interventions. J. Med. Internet Res. 2016;18(8):e234. doi: 10.2196/jmir.5952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böttcher S., Buck C., Zeeb H., Laschewski G., Hauer C., Wagner G., Sachse M.M. Randomised controlled trial to evaluate the influence of mHealth and eHealth skin cancer prevention education among young organ transplant recipients: the HIPPOlino intervention study. BMJ Open. 2019;9(12):e028842. doi: 10.1136/bmjopen-2018-028842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen D.J., Albrecht T., Hay J., Eggly S., Harris-Wei J., Meischke H., Burke W. Communication among melanoma family members. J. Health Commun. 2017;22(3):198–204. doi: 10.1080/10810730.2016.1259374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen D.J., Burke W., Hay J.L., Meischke H., Harris J.N. Effects of web-based intervention on risk reduction behaviors in melanoma survivors. J. Cancer Surviv. 2015;9(2):279–286. doi: 10.1007/s11764-014-0412-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen D.J., Hay J., Meischke H., Mayer J.A., Harris-Wai J., Burke W. Randomized trial of a web-based survivor intervention on melanoma prevention behaviors of first-degree relatives. Cancer Causes Control. 2019;30(3):225–233. doi: 10.1007/s10552-018-1096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinker T.J., Faria B.L., de Faria O.M., Klode J., Schadendorf D., Utikal J.S., Mons U., Krieghoff-Henning E., Lisboa O.C., Oliveira A.C.C., Lino H.A., Bernardes-Souza B. Effect of a face-aging mobile app–based intervention on skin cancer protection behavior in secondary schools in Brazil: a cluster-randomized clinical trial. JAMA Dermatol. 2020;156(7):737. doi: 10.1001/jamadermatol.2020.0511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buendia Eisman A., Arias Santiago S., Moreno-Gimenez J., Cabrera-León A., Prieto L., Castillejo I., Conejo-Mir J. An Internet-based programme to promote adequate UV exposure behaviour in adolescents in Spain. J. Eur. Acad. Dermatol. Venereol. 2013;27(4):442–453. doi: 10.1111/j.1468-3083.2012.04455.x. [DOI] [PubMed] [Google Scholar]
- Buller D.B., Berwick M., Lantz K., Buller M.K., Shane J., Kane I., Liu X. Evaluation of immediate and 12-week effects of a smartphone sun-safety mobile application: a randomized clinical trial. JAMA Dermatol. 2015;151(5):505–512. doi: 10.1001/jamadermatol.2014.3894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buller D.B., Berwick M., Lantz K., Buller M.K., Shane J., Kane I., Liu X. May). Smartphone mobile application delivering personalized, real-time sun protection advice: a randomized clinical trial. JAMA Dermatol. 2015;151(5):497–504. doi: 10.1001/jamadermatol.2014.3889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H., Song C., Adams D. Efficacy and mediators of a web-based media literacy intervention for indoor tanning prevention. J. Health Commun. 2020;25(2):105–114. doi: 10.1080/10810730.2020.1712500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coups E.J., Manne S.L., Pagoto S.L., Criswell K.R., Goydos J.S. Facebook intervention for young-onset melanoma patients and their family members: pilot and feasibility study. JMIR Dermatol. 2018;1(2):e3. doi: 10.2196/derma.9734. [DOI] [Google Scholar]
- Craciun C., Schuz N., Lippke S., Schwarzer R. Enhancing planning strategies for sunscreen use at different stages of change. Health Educ. Res. 2012;27(5):857–867. doi: 10.1093/her/cys091. [DOI] [PubMed] [Google Scholar]
- Craciun C., Schüz N., Lippke S., Schwarzer R. Facilitating sunscreen use in women by a theory-based online intervention: a randomized controlled trial. J. Health Psychol. 2012;17(2):207–216. doi: 10.1177/1359105311414955. [DOI] [PubMed] [Google Scholar]
- Curiel-Lewandrowski C., Chen S.C., Swetter S.M., M.-P.-W.-G.-P.-S.-L. Sub-Committee Screening and prevention measures for melanoma: is there a survival advantage? Curr. Oncol. Reports. 2012;14(5):458–467. doi: 10.1007/s11912-012-0256-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darlow S., Heckman C. Results from a tailored SMS and behavior-tracking pilot study on sun-safe behaviors in young women. Health Education & Behavior. 2017;44(6):937–944. doi: 10.1177/1090198117699507. [DOI] [PubMed] [Google Scholar]
- Dennis, M., Masthoff, J., Smith, K. A., Murchie, P., & Hall, S. (2015). Designing a tablet-based intervention to support self-checking for melanoma. Proceedings of the 5th International Conference on Digital Health 2015.
- Dixon H.G., Hill D.J., Karoly D.J., Jolley D.J., Aden S.M. Solar UV forecasts: a randomized trial assessing their impact on adults' sun-protection behavior. Health Educ. Behav. 2007;34(3):486–502. doi: 10.1177/1090198106294644. [DOI] [PubMed] [Google Scholar]
- Ersser S.J., Effah A., Dyson J., Kellar I., Thomas S., McNichol E., Caperon E., Hewitt C., Muinonen‐Martin A.J. Effectiveness of interventions to support the early detection of skin cancer through skin self-examination: a systematic review and meta-analysis. Br. J. Dermatol. 2019;180(6):1339–1347. doi: 10.1111/bjd.17529. [DOI] [PubMed] [Google Scholar]
- Evans W.D., Mays D. Design and feasibility of a text messaging intervention to prevent indoor tanning among young adult women: A pilot study. JMIR mHealth and uHealth. 2016;4(4):e137. doi: 10.2196/mhealth.6493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falzone A.E., Brindis C.D., Chren M.-M., Junn A., Pagoto S., Wehner M., Linos E. Teens, tweets, and tanning beds: rethinking the use of social media for skin cancer prevention. Am. J. Prev. Med. 2017;53(3):S86–S94. doi: 10.1016/j.amepre.2017.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch L., Janda M., Loescher L.J., Hacker E. Can skin cancer prevention be improved through mobile technology interventions? A systematic review. Prev. Med. 2016;90:121–132. doi: 10.1016/j.ypmed.2016.06.037. [DOI] [PubMed] [Google Scholar]
- Gold J., Aitken C.K., Dixon H.G., Lim M.S.C., Gouillou M., Spelman T., Wakefield M., Hellard M.E. A randomised controlled trial using mobile advertising to promote safer sex and sun safety to young people. Health Educ. Res. 2011;26(5):782–794. doi: 10.1093/her/cyr020. [DOI] [PubMed] [Google Scholar]
- Gough A., Hunter R.F., Ajao O., Jurek A., McKeown G., Hong J., Barrett E., Ferguson M., McElwee G., McCarthy M., Kee F. Tweet for behavior change: using social media for the dissemination of public health messages. JMIR Public Health and Surveillance. 2017;3(1):e14. doi: 10.2196/publichealth.6313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goulart J.M., Wang S.Q. Knowledge, motivation, and behavior patterns of the general public towards sun protection. Photochem. Photobiol. Sci. 2010;9(4):432–438. doi: 10.1039/b9pp00122k. [DOI] [PubMed] [Google Scholar]
- Guy G.P., Ekwueme D.U. Years of potential life lost and indirect costs of melanoma and non-melanoma skin cancer. Pharmacoeconomics. 2011;29(10):863–874. doi: 10.2165/11589300-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Guy G.P., Jr, Machlin S.R., Ekwueme D.U., Yabroff K.R. Prevalence and costs of skin cancer treatment in the US, 2002–2006 and 2007–2011. Am. J. Prev. Med. 2015;48(2):183–187. doi: 10.1016/j.amepre.2014.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker E., Horsham C., Vagenas D., Jones L., Lowe J., Janda M. A mobile technology intervention with ultraviolet radiation dosimeters and smartphone apps for skin cancer prevention in young adults: randomized controlled trial. JMIR mHealth and uHealth. 2018;6(11):e199. doi: 10.2196/mhealth.9854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall S., Murchie P. Can we use technology to encourage self-monitoring by people treated for melanoma? A qualitative exploration of the perceptions of potential recipients. Support. Care Cancer. 2014;22(6):1663–1671. doi: 10.1007/s00520-014-2133-3. [DOI] [PubMed] [Google Scholar]
- Hamidi R., Peng D., Cockburn M. Efficacy of skin self-examination for the early detection of melanoma. Int. J. Dermatol. 2010;49(2):126–134. doi: 10.1111/j.1365-4632.2009.04268.x. [DOI] [PubMed] [Google Scholar]
- Heckman C.J., Darlow S.D., Ritterband L.M., Handorf E.A., Manne S.L. Efficacy of an intervention to alter skin cancer risk behaviors in young adults. Am. J. Prev. Med. 2016;51(1):1–11. doi: 10.1016/j.amepre.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman C.J., Handorf E.A., Darlow S.D., Ritterband L.M., Manne S.L. An online skin cancer risk-reduction intervention for young adults: Mechanisms of effects. Health Psychol. 2017;36(3):215–225. doi: 10.1037/hea0000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillhouse J., Turrisi R., Scaglione N.M., Cleveland M.J., Baker K., Florence L.C. A web-based intervention to reduce indoor tanning motivations in adolescents: a randomized controlled trial. Prev. Sci. 2017;18(2):131–140. doi: 10.1007/s11121-016-0698-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idriss N.Z., Alikhan A., Baba K., Armstrong A.W. Online, video-based patient education improves melanoma awareness: a randomized controlled trial. Telemedicine and e-Health. 2009;15(10):992–997. doi: 10.1089/tmj.2009.0055. [DOI] [PubMed] [Google Scholar]
- Janda M., Horsham C., Vagenas D., Loescher L.J., Gillespie N., Koh U., Curiel-Lewandrowski C., Hofmann-Wellenhof R., Halpern A., Whiteman D.C., Whitty J.A., Smithers B.M., Soyer H.P. Accuracy of mobile digital teledermoscopy for skin self-examinations in adults at high risk of skin cancer: an open-label, randomised controlled trial. The Lancet Digital Health. 2020;2(3):e129–e137. doi: 10.1016/S2589-7500(20)30001-7. [DOI] [PubMed] [Google Scholar]
- Jensen J.D., Yale R.N., Krakow M., John K.K., King A.J. Theorizing foreshadowed death narratives: examining the impact of character death on narrative processing and skin self-exam intentions. J. Health Commun. 2017;22(1):84–93. doi: 10.1080/10810730.2016.1252816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan A.B., Bleakley A., Alber J.M., Lazovich DeAnn, Glanz K. Developing and testing message strategies to reduce indoor tanning. Am. J. Health Behav. 2020;44(3):292–301. doi: 10.5993/AJHB.44.3.2. [DOI] [PubMed] [Google Scholar]
- Landau M.J., Arndt J., Cameron L.D. Do metaphors in health messages work? Exploring emotional and cognitive factors. J. Exp. Soc. Psychol. 2018;74:135–149. doi: 10.1016/j.jesp.2017.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansdown T.C., Cowan S., Nioi A., Cowie H., Wendelboe-Nelson C., Rashid S., Ritchie P., Cherrie J.W. Vitamin D and UV exposure in construction workers—a randomized control trial using text messaging to promote positive behaviours. J. Public Health. 2020;42(3):594–601. doi: 10.1093/pubmed/fdz056. [DOI] [PubMed] [Google Scholar]
- Lazovich D., Vogel R.I., Berwick M., Weinstock M.A., Warshaw E.M., Anderson K.E. Melanoma risk in relation to use of sunscreen or other sun protection methods. Cancer Epidemiology and Prevention Biomarkers. 2011;20(12):2583–2593. doi: 10.1158/1055-9965.EPI-11-0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M.J., Kang H. Designing skin cancer prevention messages: Should we emphasize gains or losses? Message framing, risk type, and prior experience. Am. J. Health Promotion. 2018;32(4):939–948. doi: 10.1177/0890117117729584. [DOI] [PubMed] [Google Scholar]
- Lemal M., Van den Bulck J. Testing the effectiveness of a skin cancer narrative in promoting positive health behavior: A pilot study. Prev. Med. 2010;51(2):178–181. doi: 10.1016/j.ypmed.2010.04.019. [DOI] [PubMed] [Google Scholar]
- Lewis N. Priming effects of perceived norms on behavioral intention through observability. J. Appl. Soc. Psychol. 2013;43:E97–E108. doi: 10.1111/jasp.12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustria M.L.A. Can interactivity make a difference? Effects of interactivity on the comprehension of and attitudes toward online health content. J. Am. Soc. Inform. Sci. Technol. 2007;58(6):766–776. [Google Scholar]
- Maganty N., Ilyas M., Zhang N., Sharma A. Online, game-based education for melanoma recognition: a pilot study. Patient Educ. Couns. 2018;101(4):738–742. doi: 10.1016/j.pec.2017.11.003. [DOI] [PubMed] [Google Scholar]
- Manahan M.N., Soyer H.P., Loescher L.J., Horsham C., Vagenas D., Whiteman D.C., Olsen C.M., Janda M. A pilot trial of mobile, patient-performed teledermoscopy. Br. J. Dermatol. 2015;172(4):1072–1080. doi: 10.1111/bjd.13550. [DOI] [PubMed] [Google Scholar]
- Manne S., Buller D., Devine K., Heckman C., Pagoto S., Frederick S., Mitarotondo A. Sun safe partners online: pilot randomized controlled clinical trial. J Med Internet Res. 2020;22(9):e18037. doi: 10.2196/18037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marek A.J., Chu E.Y., Ming M.E., Khan Z.A., Kovarik C.L. Piloting the use of smartphones, reminders, and accountability partners to promote skin self-examinations in patients with total body photography: a randomized controlled trial. Am. J. Clin. Dermatol. 2018;19(5):779–785. doi: 10.1007/s40257-018-0372-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays D., Evans W.D. The effects of gain-, loss-, and balanced-framed messages for preventing indoor tanning among young adult women. J. Health Commun. 2017;22(7):604–611. doi: 10.1080/10810730.2017.1332119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays D., Tercyak K.P. Framing indoor tanning warning messages to reduce skin cancer risks among young women: implications for research and policy. Am. J. Public Health. 2015;105(8):e70–e76. doi: 10.2105/AJPH.2015.302665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays D., Zhao X. The influence of framed messages and self-affirmation on indoor tanning behavioral intentions in 18-to 30-year-old women. Health Psychol. 2016;35(2):123–130. doi: 10.1037/hea0000253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Methley A.M., Campbell S., Chew-Graham C., McNally R., Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Services Res. 2014;14(1):579. doi: 10.1186/s12913-014-0579-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mingoia J., Hutchinson A.D., Gleaves D.H., Wilson C. The impact of a social media literacy intervention on positive attitudes to tanning: a pilot study. Comput. Hum. Behav. 2019;90:188–195. [Google Scholar]
- Mishra K., Barnhill R.L., Paddock L.E., Fine J.A., Berwick M. Histopathologic variables differentially affect melanoma survival by age at diagnosis. Pigment Cell Melanoma Res. 2019;32(4):593–600. doi: 10.1111/pcmr.12770. [DOI] [PubMed] [Google Scholar]
- Moher D. a Liberati, J. Tetzlaff, DG Altman, P. Grp, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Reprinted from Annals of Internal Medicine) Phys. Ther. 2009;89:873–880. [PubMed] [Google Scholar]
- Murray J.M., Brennan S.F., French D.P., Patterson C.C., Kee F., Hunter R.F. Mediators of behavior change maintenance in physical activity interventions for young and middle-aged adults: a systematic review. Ann. Behav. Med. 2018;52(6):513–529. doi: 10.1093/abm/kay012. [DOI] [PubMed] [Google Scholar]
- Myrick J.G. An experimental test of the roles of audience involvement and message frame in shaping public reactions to celebrity illness disclosures. Health Commun. 2019;34(9):1060–1068. doi: 10.1080/10410236.2018.1461170. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute Melanoma of the Skin — Cancer Stat Facts. (Available at:) https://seer.cancer.gov/statfacts/html/melan.html (Accessed August 6, 2020).
- Nioi A., Wendelboe-Nelson C., Cowan S., Cherrie M., Rashid S., Cowie H., Davis A., Ritchie P., Lansdown T.C., Cherrie J.W. Nudging construction workers towards better sun-safety behaviour: summary of the evidence for practitioners. Policy and Practice in Health and Safety. 2020;18(1):25–33. [Google Scholar]
- Niu Z., Jeong D.C., Coups E.J., Stapleton J.L. An experimental investigation of human presence and mobile technologies on college students’ sun protection intentions: Between-subjects study. JMIR mHealth and uHealth. 2019;7(8):e13720. doi: 10.2196/13720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostherr K., Killoran P., Shegog R., Bruera E. Death in the digital age: a systematic review of information and communication technologies in end-of-life care. J. Palliative Med. 2016;19(4):408–420. doi: 10.1089/jpm.2015.0341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paddock L.E., Lu S.E., Bandera E.V., Rhoads G.G., Fine J., Paine S., Barnhill R., Berwick M. Skin self-examination and long-term melanoma survival. Melanoma Res. 2016;26(4):401–408. doi: 10.1097/CMR.0000000000000255. [DOI] [PubMed] [Google Scholar]
- Pagoto S., Waring M.E., May C.N., Ding E.Y., Kunz W.H., Hayes R., Oleski J.L. Adapting behavioral interventions for social media delivery. J. Med. Internet Res. 2016;18(1):e24. doi: 10.2196/jmir.5086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagoto S., Waring M.E., Xu R. A call for a public health agenda for social media research. J. Med. Internet Res. 2019;21(12):e16661. doi: 10.2196/16661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricklefs C.A., Asdigian N.L., Kalra H.L., Mayer J.A., Dellavalle R.P., Holman D.M., Crane L.A. Indoor tanning promotions on social media in six US cities# UVTanning# tanning. Transl. Behav. Med. 2016;6(2):260–270. doi: 10.1007/s13142-015-0378-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J.K., Friedewald J.J., Desai A., Gordon E.J. Response Across the Health-Literacy Spectrum of Kidney Transplant Recipients to a Sun-Protection Education Program Delivered on Tablet Computers: Randomized Controlled Trial. JMIR Cancer. 2015;1(2) doi: 10.2196/cancer.4787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, J. K., Friedewald, J. J., Desai, A., & Gordon, E. J. (2016, Jan). A Randomized Controlled Trial of a Mobile Medical App for Kidney Transplant Recipients: Effect on Use of Sun Protection. Transplant Direct, 2(1). doi: 10.1097/txd.0000000000000561. [DOI] [PMC free article] [PubMed]
- Robinson J.K., Gaber R., Hultgren B., Eilers S., Blatt H., Stapleton J., Mallett K., Turrisi R., Duffecy J., Begale M., Martini M., Bilimoria K., Wayne J. Skin self-examination education for early detection of melanoma: a randomized controlled trial of Internet, workbook, and in-person interventions. J. Med. Internet Res. 2014;16(1):e7. doi: 10.2196/jmir.2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutten L.F., Hesse B.W., Moser R.P., Mccaul K.D., Rothman A.J. Public perceptions of cancer prevention, screening, and survival: comparison with state-of-science evidence for colon, skin, and lung cancer. J. Cancer Educ. 2009;24(1):40–48. doi: 10.1080/08858190802664610. [DOI] [PubMed] [Google Scholar]
- Sontag J.M., Barnes S.R. The visual framing of graphics when used in preventative health digital news packages: exploring the use of a narrative structure as the message infrastructure. J. Visual Commun. Med. 2017;40(3):109–119. doi: 10.1080/17453054.2017.1366824. [DOI] [PubMed] [Google Scholar]
- Sontag J.M., Noar S.M. Assessing the potential effectiveness of pictorial messages to deter young women from indoor tanning: an experimental study. J. Health Commun. 2017;22(4):294–303. doi: 10.1080/10810730.2017.1281361. [DOI] [PubMed] [Google Scholar]
- Stapleton J.L., Manne S.L., Darabos K., Greene K., Ray A.E., Turner A.L., Coups E.J. Randomized controlled trial of a web-based indoor tanning intervention: Acceptability and preliminary outcomes. Health Psychol. 2015;34(Suppl):1278–1285. doi: 10.1037/hea0000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapleton J.L., Manne S.L., Day A.K., Levonyan-Radloff K., Pagoto S.L. Healthy body image intervention delivered to young women via Facebook groups: formative study of engagement and acceptability. JMIR Res. Protocols. 2018;7(2):e54. doi: 10.2196/resprot.9429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stock M.L., Gerrard M., Gibbons F.X., Dykstra J.L., Mahler H.I.M., Walsh L.A., Kulik J.A. Sun protection intervention for highway workers: long-term efficacy of UV photography and skin cancer information on men's protective cognitions and behavior. Ann. Behav. Med. 2009;38(3):225–236. doi: 10.1007/s12160-009-9151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabó C., Ócsai H., Csabai M., Kemény L. A randomised trial to demonstrate the effectiveness of electronic messages on sun protection behaviours. J. Photochem. Photobiol., B. 2015;149:257–264. doi: 10.1016/j.jphotobiol.2015.06.006. [DOI] [PubMed] [Google Scholar]
- Taber J.M., Dickerman B.A., Okhovat J.-P., Geller A.C., Dwyer L.A., Hartman A.M., Perna F.M. Skin cancer interventions across the cancer control continuum: Review of technology, environment, and theory. Prev. Med. 2018;111:451–458. doi: 10.1016/j.ypmed.2017.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira P.J., Carraça E.V., Marques M.M., Rutter H., Oppert J.-M., De Bourdeaudhuij I., Lakerveld J., Brug J. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med. 2015;13(1):84. doi: 10.1186/s12916-015-0323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai S., Frank S.H., Bordeaux J.S. Improving sun-protective behaviors and self-skin examinations among African Americans: a randomized controlled trial. Dermatol. Surg. 2018;44(4):512–518. doi: 10.1097/DSS.0000000000001366. [DOI] [PubMed] [Google Scholar]
- van ’t Riet J., Ruiter R.A.C., Werrij M.Q., De Vries H. Self-efficacy moderates message-framing effects: the case of skin-cancer detection. Psychol. Health. 2010;25(3):339–349. doi: 10.1080/08870440802530798. [DOI] [PubMed] [Google Scholar]
- Viola A., Panigrahi G., Devine K.A. Digital interventions for adolescent and young adult cancer survivors. Curr. Opinion Supportive Palliative Care. 2020;14(1):51–59. doi: 10.1097/SPC.0000000000000480. [DOI] [PubMed] [Google Scholar]
- Vollmann M., Engelhardt G., Salewski C. Effects of a brief multimodal online intervention on the intention to conduct sun protective behaviours through targeting illness representations about skin cancer: a randomized controlled trial. Psychology & Health. 2021;36(3):253–270. doi: 10.1080/08870446.2020.1775831. [DOI] [PubMed] [Google Scholar]
- Walter F.M., Pannebakker M.M., Barclay M.E., Mills K., Saunders C.L., Murchie P., Corrie P., Hall P., Burrows N., Emery J.D. Effect of a skin self-monitoring smartphone application on time to physician consultation among patients with possible melanoma: a phase 2 randomized clinical trial. JAMA network open. 2020;3(2) doi: 10.1001/jamanetworkopen.2020.0001. e200001-e200001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wantland D.J., Portillo C.J., Holzemer W.L., Slaughter R., McGhee E.M. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J. Med. Internet Res. 2004;6(4) doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K.M., Starfelt L.C., Young R.M., Hawkes A.L., Cleary C., Leske S., Wihardjo K. Mar). A randomised controlled trial of an online theory-based intervention to improve adult Australians' sun-protective behaviours. Prev. Med. 2015;72:19–22. doi: 10.1016/j.ypmed.2014.12.025. [DOI] [PubMed] [Google Scholar]
- Whiteman D.C., Green A.C., Olsen C.M. The growing burden of invasive melanoma: projections of incidence rates and numbers of new cases in six susceptible populations through 2031. J, Invest. Dermatol. 2016;136(6):1161–1171. doi: 10.1016/j.jid.2016.01.035. [DOI] [PubMed] [Google Scholar]
- Willoughby J.F., Furberg R. Underdeveloped or underreported? Coverage of pretesting practices and recommendations for design of text message–based health behavior change interventions. J. Health Commun. 2015;20(4):472–478. doi: 10.1080/10810730.2014.977468. [DOI] [PubMed] [Google Scholar]
- Youl P.H., Soyer H.P., Baade P.D., Marshall A.L., Finch L., Janda M. Can skin cancer prevention and early detection be improved via mobile phone text messaging? A randomised, attention control trial. Prev. Med. 2015;71:50–56. doi: 10.1016/j.ypmed.2014.12.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.