Abstract
Background
Falls remain a common and debilitating problem in hospitals worldwide. The aim of this study was to investigate the effects of falls prevention interventions on falls rates and the risk of falling in hospital.
Design
Systematic review and meta-analysis.
Participants
Hospitalised adults.
Intervention
Prevention methods included staff and patient education, environmental modifications, assistive devices, policies and systems, rehabilitation, medication management and management of cognitive impairment. We evaluated single and multi-factorial approaches.
Outcome measures
Falls rate ratios (rate ratio: RaR) and falls risk, as defined by the odds of being a faller in the intervention compared to control group (odds ratio: OR).
Results
There were 43 studies that satisfied the systematic review criteria and 23 were included in meta-analyses. There was marked heterogeneity in intervention methods and study designs. The only intervention that yielded a significant result in the meta-analysis was education, with a reduction in falls rates (RaR = 0.70 [0.51–0.96], P = 0.03) and the odds of falling (OR = 0.62 [0.47–0.83], P = 0.001). The patient and staff education studies in the meta-analysis were of high quality on the GRADE tool. Individual trials in the systematic review showed evidence for clinician education, some multi-factorial interventions, select rehabilitation therapies, and systems, with low to moderate risk of bias.
Conclusion
Patient and staff education can reduce hospital falls. Multi-factorial interventions had a tendency towards producing a positive impact. Chair alarms, bed alarms, wearable sensors and use of scored risk assessment tools were not associated with significant fall reductions.
Keywords: falls, hospital, physiotherapy, prevention, education, exercise, older people, systematic review
Key Points
Falls in hospitals can be prevented with evidence-based patient education.
Health professional education about falls prevention can also reduce the rate of falls and fall-related injuries.
Significant falls reduction in hospitals did not occur with bed or chair alarms, or use of sensors.
Introduction
Hospital falls remain a problem worldwide, despite sustained falls prevention efforts in public and private healthcare settings [1, 2]. Falls rates, which are usually expressed per 1,000 bed days, typically range from 2 to 8 in acute hospitals, geriatric wards and emergency [3–5]. In rehabilitation hospitals where patients are encouraged to mobilise, falls rates typically range from 3 to 16 per 1,000 bed days [6, 7]. Injuries occur in around 30% of hospital falls [8, 9]. There can be minor injuries such as lacerations, contusions, sprains and strains as well as more serious injuries such as head injuries, fractures and death [8–10]. Anxiety and fear of falling can also arise [11].
Hospital falls prevention strategies include patient education, clinician education, environmental adaptations, the use of assistive devices, therapeutic exercises, medication reviews, optimal nutrition, management of cognitive impairment and falls mitigation policies, systems and leadership [1, 12, 13]. Some examples of systems include post-fall team ‘huddles’ [14], falls reports at nursing handover [15], auditing [16] and reporting monthly falls [12]. Some of these interventions have been investigated in isolation eg. [14, 15]. Others have been evaluated as part of a multi-factorial approach to mitigating hospital falls eg. [1, 17].
Patients do not always realise their risk of falling whilst in hospital [12, 18, 19] even though people over the age of 65 years and those 50 years or older with two or more co-morbidities are at high risk [20]. A Cochrane review [1] published in 2018 found little robust evidence in support of hospital falls mitigation interventions and concluded that ‘multifactorial interventions may reduce the rate of falls, although this is more likely in a rehabilitation or geriatric ward setting (low quality evidence)’. As well as noting few clinical trials of high quality, the Cochrane review excluded patients with stroke and included care homes. Many new trials have been published in the last 4 years hence we conducted a new systematic review and meta-analysis of the hospital falls literature without mixing the results with aged care home settings. Uniquely, we also included an analysis of the effects of scored falls risk screening tools as these are often used as a fall mitigation strategy [5, 20].
The primary aim was to evaluate the effects of single- and multi-factorial interventions on falls rates and risk in hospitals, and to grade the strength of evidence and quality of the studies. The research question was: ‘What are the effects of falls prevention interventions on falls outcomes for adults in hospital settings [10]?’
Methods
The design and conduct of this review and analysis was informed by principles in the Cochrane guidelines [21] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. The review was prospectively registered on PROSPERO (2017: CRD 42017058887).
Search strategy
The Medline, CINAHL, PsycInfo, Embase, AMED, PEDro and Cochrane electronic databases were searched from all records until 31 May 2021. Search terms were entered with three concepts: (i) falls (ii) hospital setting (iii) study design. Terms within each concept were combined with the OR Boolean operator, and the three concepts were combined with the AND Boolean operator. Each of the terms were then aligned to MeSH subject headings and then searched via keywords. Examples of terms used for concept 1 included ‘falls’, ‘fall prevention’ and ‘accidental fall’. Examples of terms used in concept 2 were ‘acute care’, ‘rehabilitation’, ‘hospital’, ‘hospitalisation’, ‘ward’ and ‘clinic’. Examples of terms used in concept 3 were ‘randomised controlled trial’ (RCT), ‘trial’, ‘controlled clinical trial’ and ‘study’. Journal contents pages and articles in press from medical and ageing journals were also hand searched, and reference lists were screened. Publication details were sent to bibliographic software and any duplicates were removed.
Eligibility criteria
Studies were included in the systematic review if they: (i) were published in English; (ii) included a falls intervention in a hospital setting; (iii) investigated falls as a primary or secondary outcome and falls data were reported and (iv) included a contemporary comparison group (either as a RCT, quasi-randomised, cluster RCT, comparative study or quasi-experimental study). In the meta-analysis we only included studies for which the falls rate ratios and odds ratios (ORs) were provided by authors or could be calculated from the data reported. Conference proceedings, case studies, clinical commentaries, website reports and reviews were excluded. Studies were excluded if they only had paediatric samples or an historical comparison group or if they only reported falls in a list of adverse events.
The titles of manuscripts were first screened for eligibility by four researchers. Full abstracts were then independently screened by three pairs of reviewers. Any abstracts that failed to align with the inclusion criteria or had exclusions were removed. Complete text versions of the selected manuscripts were retrieved, and three pairs of reviewers independently analysed them. Discrepancies were discussed by our review team until consensus was reached.
Outcomes and data extraction
The primary falls outcomes were (i) reduction in the rate of falls (falls per unit of person time, such as bed days (typically falls per 1,000 bed days)), designated as the rate ratio (RaR); (ii) reduction in falls risk, defined by the odds of being a faller in the intervention compared to control group (OR). For each article, we extracted the setting, inclusion and exclusion criteria, random allocation procedure, participant demographics and diagnosis, falls interventions and how falls were measured and recorded.
Intervention category
Study interventions were grouped according to the following taxonomy: (i) a single intervention which was one of the following: (a) direct education of patients or clinicians; (b) environment modifications (e.g. flooring, lighting, ramps, signs); (c) assistive devices (e.g. call bell, alert bracelet, bed alarm, traction socks, walking frame, stick, chair assist, lowered bed, technologies); (d) systems, service models, social context, leadership, policies or procedures to prevent falls; (e) rehabilitation, physiotherapy, physical activities, or other therapeutic exercises delivered in hospital; (f) medication management; (g) dietary modification, including vitamins, or (ii) multi-factorial interventions which combined two or more approaches. Each individual study was grouped according to the most predominant intervention type, unless multiple intervention arms were specified. The taxonomy was a simplified version of that used in the prior Cochrane review [1]; we used the phrase ‘education’ rather than ‘knowledge interventions’ and environment/assistance was separated into environment modifications and assistive devices.
Data synthesis
For the rate of falls, the RaR and 95% confidence intervals (CI) that were reported in each paper were used. If both adjusted and unadjusted rate ratios were reported, we preferentially used estimates that had been adjusted for clustering (if applicable) and if multiple estimates were available due to adjustment for co-variates, we included the one which the authors either specified a priori in the trial registration or highlighted in their study summary (abstract or conclusion). When not reported, we emailed authors to obtain the data.
To synthesise the risk of falling, we used ORs and reported 95% CI if available. If both adjusted and unadjusted estimates were reported we used the unadjusted estimate, unless the adjustment was for clustering (e.g. clustering of patients within sites). If an OR and 95% CI were not reported and appropriate data were available, we calculated an OR and 95% CI in Review Manager [22]. For these calculations, we used the number of participants randomised to each group. For cluster correcting, the Intra-cluster Correlation Coefficient (ICC) from Hill et al. [7] was used. The cluster correction was also applied for quasi-experimental designs. Thus, for Barker (2016) we had to calculate an OR for the fallers versus non-fallers analysis based on raw data, then apply a variance inflation factor. The Dykes (2010) study did not present an adjusted OR for the fallers versus non-fallers outcome (just an adjusted P-value) and we calculated this based on the raw data, adjusting the ICC by applying a variance inflation factor.
Within each intervention category the generic inverse variance method in Review Manager was used to run the meta-analysis and we created forest plots using R. This required entering the natural logarithm of the RaR or OR and standard error (SE) for each trial, which were calculated in Microsoft Excel [23].
Risk of bias assessment
The included studies in the systematic review were assessed for risk of bias. The Cochrane Risk of Bias 2 Instrument was used to evaluate risk of bias for randomised or quasi-RCT [21]. The Cochrane Cluster Randomized Parallel Group Trials 2 Instrument was used for cluster randomised controlled trials [21].
Studies were assessed independently for risk of bias by three reviewers from our review team and consultation with a fourth reviewer. Risk of bias figures were prepared for the RCTs and a summary table was produced for the RCTs. We selected a valid instrument for other study designs, such as quasi-experimental designs, from the Joanna Briggs Institute (JBI) Critical Appraisal Tools database [24]. The reviewers assigned risk of bias as low, medium or high.
GRADE strength of evidence
For each meta-analysis, the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) instrument was used to appraise the strength of evidence for the falls rates and risk [25, 26]. Randomised trials were appraised separately from non-RCTs. Components assessed were study design, risk of bias, indirectness, imprecision and inconsistency.
Consensus on exercise reporting template
Two reviewers independently extracted all exercise intervention component data from the included studies by using the Consensus on Exercise Reporting (CERT) checklist. The CERT has 16 categories and 19 separate items considered essential in the reporting of reproducible exercise interventions [27]. Each item was scored 1 (clearly reported) or 0 (not reported or not clearly described), and a score out of a total of 19 was calculated.
Results
Systematic review results
As shown in the PRISMA diagram (Supplementary File Figure 1), the electronic database search identified 11,186 studies; 26 were identified from the manual search of reference lists and relevant journals. After 3,006 duplicates were removed 8,206 articles remained as the total yield. From reviewing titles and abstracts 7,976 studies were excluded, and the full text of the remaining 230 studies were downloaded for detailed assessment. Of these 187 were excluded and 43 studies were included in the systematic review. Two additional studies assessing the efficacy of Falls Risk Assessment Tools (FRATs) as a fall mitigation strategy were also included [28, 29]. Supplementary File Table 1 summarises the characteristics of the included studies. Supplementary File Figures 2–3 and Supplementary File Tables 2–4 summarise the evaluations associated with the systematic review and meta-analysis, such as risk of bias, method quality, components of multi-factorial interventions, GRADE results and CERT results.
For the systematic review, multi-factorial interventions were evaluated in 16 studies [5, 30–44] (Supplementary File Table 1 and Table 4). Seven papers investigated the effect of providing assistive devices such as low beds, sensors and bed and chair alarms [45–51]. Five evaluated exercise or rehabilitation therapies [52–56]. Two evaluated the effects of patient education [7, 57] and one was on clinician education [7]. Ten investigations evaluated hospital systems, service models, policies and procedures to reduce falls [58–67]. Three investigated environmental modifications [52, 68, 69] and one analysed the effects of medication (Vitamin D prescription) [70].
Meta-analysis results: single interventions
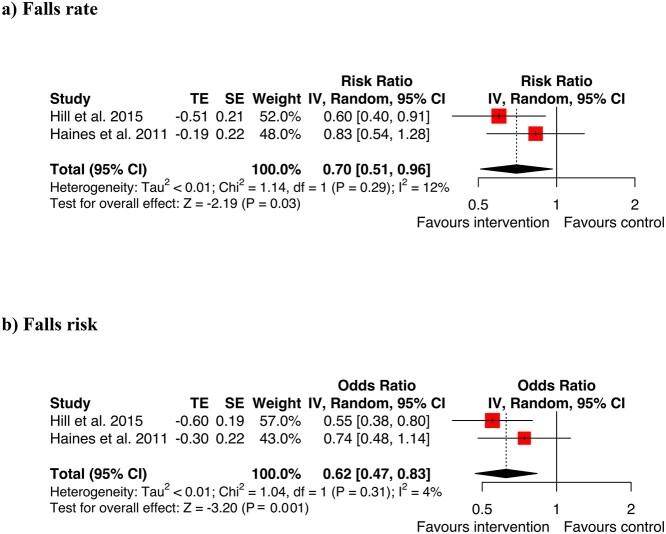
Education
Two trials assessed three different patient educational packages [7, 57] (Figure 1, Supplementary File Table 1). Haines et al. [57] analysed a comprehensive educational program and a version with only educational materials. As the comprehensive program was most like Hill [7], this package was used for the meta-analysis which showed positive results for both the odds of falling and rate of falls. The overall summary RaR was 0.70 [0.51–0.96], Z = −2.19, P = 0.03 (Figure 1). The overall summary OR was 0.62 [0.47–0.83], Z = −3.20, P = 0.001. The patient education studies in the meta-analysis were rated by GRADE as having a high strength of evidence (Supplementary File Table 5). The trial by Hill et al. [7] also incorporated staff education, showing beneficial effects on falls.
Figure 1.
Meta-analysis education for (a) falls rate (b) falls risk.
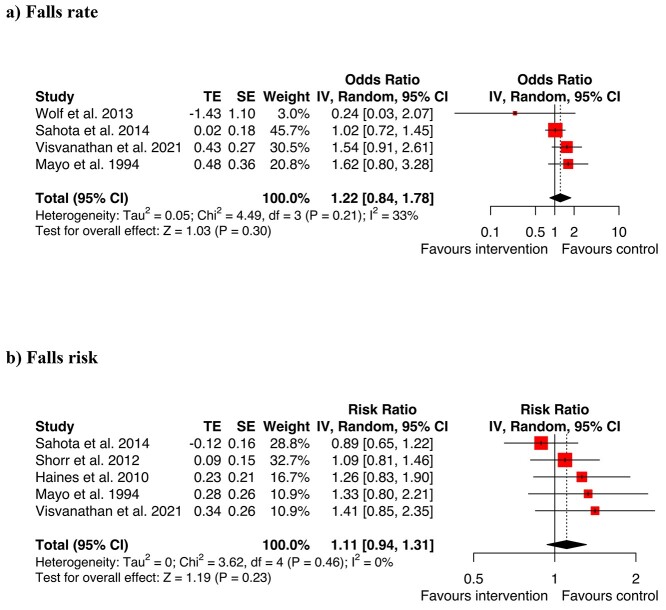
Assistive devices
Four studies included in the meta-analysis assessed the rate of falling associated with assistive devices and five assessed falls risk associated with devices such as bed alarms, wearable sensors and alert bracelets (Figure 2). The overall results for assistive devices showed no significant effects on rate of falls or odds of falling (RaR = 1.22, CI 0.84–1.78, Z = 1.03, P = 0.30; OR = 1.1, CI 0.94–1.31, Z = 1.19, P = 0.23). The study by Healey et al. [44] could not be included in the meta-analysis because effect sizes and CI for rate or odds of falls in hospitals alone were not reported. The study by Tideiksaar [49] et al. on bed alarms did not have effects sizes and CI reported in a way enabling inclusion in the meta-analysis. It had non-significant results and a high risk of bias when evaluated with the Cochrane risk of bias tool.
Figure 2.
Meta-analysis assistive devices for (a) falls rate (b) falls risk.
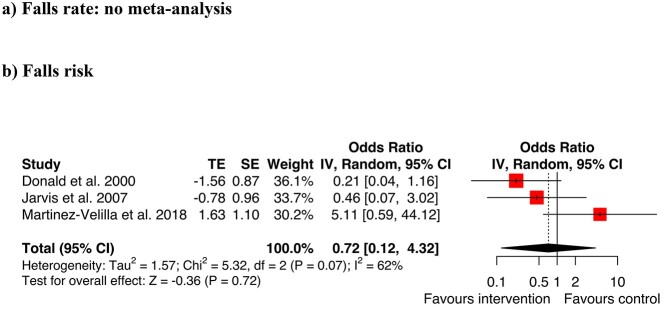
Rehabilitation and exercise therapies
ORs for three studies were included in a meta-analysis [52, 53, 56]. The analysis did not show an overall reduction in falls risk with rehabilitation and exercise therapies (OR = 0.72, CI 0.12–4.32; Z = −0.36, P = 0.72, Figure 3). Only the rehabilitation study by Treacy [55] reported the RaR, with no significant change in the rate of falls (IRR:1.13, 95% CI 0.65–1.96, P = 0.662). The trial by Padula et al. [54] could not be included in this meta-analysis because effect sizes and CI for the rate of falls were not reported. It was of moderate quality, scoring 6/9 using the JBI quasi-experimental appraisal tool and reported similar falls rates between intervention and control groups.
Figure 3.
Meta-analysis additional rehabilitation for (a) falls rate (b) falls risk.
Systems
The system-based falls mitigation interventions that were implemented varied in content and approach. The data from these nine studies were not pooled in a meta-analysis as effect sizes were not reported. The use of hourly rounding, bedside handover, electronic surveillance or a patient safety officer did not significantly reduce the rate of hospital falls in five studies [58, 60–62, 65]. In a trial involving medical review of patient falls, the falls rate per 1,000 patient days was 10.6 in the control group compared to 1.5 in the experimental group following medical review and accompanying actions. This difference was statistically significant (P < 0.004) [59].
Hardin et al. [63] reported a significant reduction in falls per 1,000 admissions between intervention (web cameras in patient rooms) and control groups. Despite favourable results, this paper was not able to be included in the meta-analysis because the effect sizes and CI for the rate of falls or odd of falls were not reported or available. It was rated as having some concerns for risk of bias. Bott et al. [64] reported a reduction in falls with the use of an embodied conversational agent. There was no mention of whether this was statistically significant, and the study had a medium risk of bias. Sheppard et al. [66] conducted a time series analysis on the effects of implementing the NICE falls prevention clinical guidelines. They found fewer falls per 1,000 occupied bed days in the intervention period (5.89) compared to the control period (6.62). This study had a high risk of bias (Supplementary File Table 2). Montejano-Lozoya et al. [67] assessed the effect of an educational intervention for hospital nurses. There was a higher incidence of falls in the control group compared with the intervention group although the sample size was comparatively low. The risk of bias for this study was high (Supplementary File Table 3).
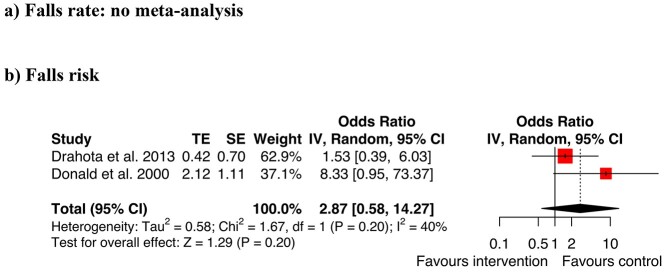
Environmental modifications
Two studies evaluated the outcomes of different types of flooring (Figure 4). Donald [52] investigated if carpet (intervention arm) was safer than vinyl (control arm). Drahota et al. [68] compared a thicker floor (intervention arm; 8.3 mm vinyl over a fibreglass mat) with standard flooring (control arm; 2 mm vinyl or thermoplastic tiles). Both reported results trending towards higher falls rates and risks for the intervention conditions. When combined in a summary meta-analysis, the overall difference between conditions was not statistically significant and the CIs were large (OR = 2.87, CI 0.58–14.27, Z = 1.29, P = 0.20). An investigation by Hanger [69] analysed the effects of low impact flooring and reported median falls rates. Because medians were used, the data could not be pooled with the other studies in the meta-analysis. Hanger [69] found a small and non-significant reduction in falls rates with low impact flooring.
Figure 4.
Meta-analysis environmental modifications for (a) falls rate (b) falls risk.
Medications
One study, by Burleigh et al. [70] investigated the effects of delivering vitamin D plus calcium to hospitalised patients, compared with calcium alone. Although the number of fallers was less in the intervention group (n = 36) compared to the control group (n = 45) this reduction was not statistically significant (RR 0.82 CI 0.59–1.16). This article was rated as having a low risk of bias using the Cochrane risk of bias 2 tool (Supplementary File Figure 2).
Meta-analysis results for multi-factorial interventions
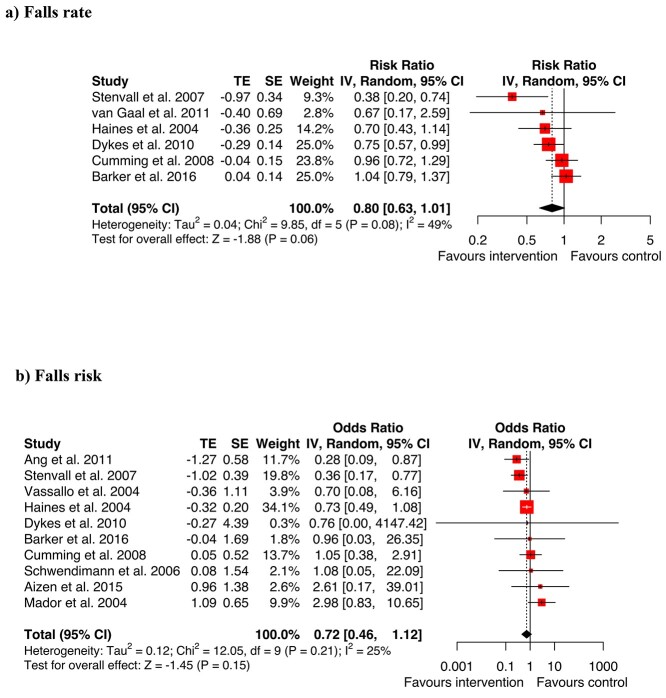
The meta-analysis of multi-factorial studies (Figure 5) showed a trend towards an overall reduction in the rate of hospital falls, although this did not quite reach statistical significance (RaR = 0.8, 95% CI 0.63–1.01, Z = −1.88, P = 0.06). The OR could be calculated for 10 of the multi-factorial studies [5, 30–34, 38–41]. Overall, the meta-analysis did not identify a statistically significant reduction in falls risk (OR = 0.72, CI 0.46–1.12, Z = −1.45, P = 0.15).
Figure 5.
Meta-analysis multifactorial interventions for (a) falls rate (b) falls risk.
There were positive results for individual multi-factorial trials by Ang [31], Dykes [33], Haines [34], Stenvall [40] and Vassallo [41]. The multi-factorial falls prevention studies by Healey, Monro et al. [35] and Healey, Low et al. [44] also reported significant reductions in the risk of falls (Healey et al. 2004., P = 0.006); and in the rate of falls (Healey 2014: P = 0.01). The two Healey studies were excluded from the meta-analysis and forest plots because effect sizes and CIs for rate of falls or odds of falls in hospitals alone were not reported or available. Likewise, the multi-factorial studies by Koh [36] and Krauss [37] had non-significant results and were not included in the meta-analysis because OR or RaR could not be calculated. A multi-factorial falls prevention study by Wald [42] found no significant difference between intervention and control groups (4.8 versus 6.7 falls per 1,000 patient days, 95% CI −9.63 to 13.3). It was not able to be included in the meta-analysis because an estimate of the rate ratio effect was not reported or able to be calculated as the distributions were not available.
Scored falls risk screening tools
Scored FRATs have been historically used in hospitals as another fall mitigation strategy. Clinicians typically assign FRAT scores out of 10 for each patient to guide the assignment of interventions based on the score. Despite their widespread use in the past, there is limited evidence of their efficacy. Two recent large RCTs assessed the effectiveness of these tools and found that removal of the risk scoring component of the FRAT did not result in inferior fall outcome [28, 29] (Supplementary File Table 6). Jellett et al. (2020) [28] conducted their stepped-wedge trial across nine hospital units across 10 months and found that the rate of falls was not impacted by divesting from the use of a scored FRAT and time was saved. Morris et al. (2021) [29] conducted a parallel cluster RCT across 10 hospitals over 3 months and found that removing the requirement to perform scored risk screening did not negatively impact fall rates.
Risk of bias
Fifteen of the 43 included studies in the systematic review were RCTs. Risk of bias was assessed with the Cochrane Risk of Bias 2 Instrument [21] (Supplementary File Figure 2). For two of the studies, there were two trial arms and each arm was appraised separately [52, 57]. Many of the RCTs had a low risk of bias [31, 34, 40, 52, 55–57, 70]. Four were at medium risk of bias [38, 46, 47, 52]. There were concerns about the randomisation methods, deviations from the planned intervention in some studies, or issues with measurement of the outcomes. Some trials were assessed to have a high risk of bias, with concerns about randomisation, or protocol deviations [49, 50, 53, 59], or missing outcome data [49, 53]. Risk of bias for RCTs as a percentage is shown in Supplementary File Figure 3.
Thirteen of the included studies were cluster RCTs (cRCTs). For these, the risk of bias was assessed with the Cochrane Cluster Randomised Parallel Group Trials 2 Instrument [21] (Supplementary File Table 2). Six of the cRCTs had a low risk of bias [5, 7, 33, 43, 45, 48]. Six were rated as having ‘some concerns’ due to issues with randomisation [30, 44, 68], imbalance in participant characteristics [68], deviations from the intended interventions [30, 44, 68], missing outcome data [35], or problems with measurement of the outcome [32, 63]. One had a high risk of bias due to problems with randomisation, identification and recruitment of participants, deviations from the planned intervention, measurement issues and selection of reported results [66].
Fifteen of the included studies in the systematic review had a non-randomised design [36, 37, 39, 41, 42, 51, 54, 58, 60–62, 64, 65, 67, 69]. Supplementary Table 3 shows that many of these scored well on method quality [36, 37, 39, 41, 42, 51, 58, 60–62, 65, 69]. Three had a medium risk of bias; one associated with the statistical analysis, differences in participants in control and experimental groups and a lack of multiple measurements [54] another due to differences in participants, lack of follow-up and statistical analysis [64] and one had differences in participants in the control and experimental groups, uncertainty regarding multiple measurements, and unclear reporting of follow up measures [67]. The studies on divesting from scored FRAT screening both had a low risk of bias (Supplementary Table 6).
For the odds of falling, the GRADE showed strong evidence for education [7, 57] and low for assistive devices [46, 47] (Supplementary Table 5). The strength of evidence as rated using GRADE was very low for additional rehabilitation therapies [52, 53, 56], environmental modifications [52, 68], RCT multi-factorial interventions [5, 30–34, 38, 40] and non-RCT multi-factorial interventions [39, 41]. For the rate of falls, the strength of evidence was rated high by GRADE for education [7, 57] and moderate for assistive devices. It was very low for multi-factorial studies (Supplementary Table 5).
CERT results
There were nine studies that included an exercise component to prevent hospital falls [32, 34, 39, 40, 52–56]. Supplementary Table 7 shows the CERT evaluation, with low comprehensiveness of exercise reporting overall. The mean was 8.6 (SD 4.3) out of a possible score of 19. Three studies had a CERT score greater than 10 [34, 55, 56]. Some required reference to previous studies, website links, or published protocols. One weblink to an exercise manual was inactive and the author provided the details [34]. Five well described CERT items were instructor qualifications (9/9 included studies), reporting of adverse events (9/9), the setting (9/9), supervision (8/9) and whether the exercise intervention was generic or tailored to individual needs (7/9). The poorly described elements were exercise equipment (3/9), individual or group delivery (4/9), exercise adherence (2/9), exercise motivation strategies (0/9), exercise progression (2/9), exercise details (4/9) and whether the exercise intervention was delivered as planned (3/9).
Discussion
Falls in hospital are the most common safety incident affecting older people and are a frequent cause of concern for staff, complaints by families and sometimes coroner inquests or civil claims. Beyond the findings of earlier reviews (e.g. [1, 2, 13, 17, 20] this latest meta-analysis adds new information showing that education has a positive effect on hospital falls rates and risk. Large randomised trials [7, 57] showed the benefits of engaging patients and clinicians in education and training, in agreement with a recent scoping review by Heng [12]. In contrast, our meta-analysis found no evidence of falls reduction using scored falls risk screening tools, bed alarms, chair alarms or sensors.
Select studies of multi-factorial interventions showed favourable effects on hospital falls rates. These included combinations of at least two interventions such as patient or staff education, procedures around nurse handover, fast responses to call buttons, regular toileting, environmental modifications, assistive devices, exercise therapies, safe footwear, medication management, diet or management of cognitive impairment. The most favourable result for a multi-factorial RCT was by Stenvall et al. [40]. This trial had a low risk of bias and included rehabilitation, staff education, changes to systems, policies and procedures, diet and environmental modifications. However, patients allocated to the intervention arm of this study were cared for on a ward that had fewer beds (24 versus 27), yet 1.7 more full time equivalent allied health staff. Therefore, the importance of the falls interventions versus the enhanced staffing level was unclear.
Another multi-factorial RCT by Haines et al. [34] showed favourable results. They evaluated the targeted provision of therapeutic exercises, patient education, risk alert signs and hip protectors. In contrast, a high quality, cluster RCT by Barker et al. [5] that compared usual care with a nurse-led ‘6-PACK’ program did not find superior results for a multi-factorial approach to falls prevention. The 6-PACK program combined a FRAT with alert signs, bathroom supervision, a toileting program, clinician education, ensuring walking sticks and frames were in reach, low–low beds, bed and or chair alarms [5]. Several of the included interventions, such as use of low beds, FRATS and bed and/or chair alarms have limited or negative effects on hospital falls [45, 47, 48]. This contrasts with the beneficial effects reported for toileting programs [72], bathroom supervision [73] and other systems to mitigate falls [73].
A small number of individual studies reported a trend towards physiotherapy or additional rehabilitation therapies lowering hospital falls rates, however these were not significant [52, 55]. The GRADE analysis showed an overall low level of certainty for the results for the rehabilitation therapy trials included in the meta-analysis [52, 53, 56]. There was no evidence that low beds, bed alarms or chair alarms reduced hospital falls or injuries, in agreement with Oliver et al. [74]. In fact, our systematic review showed that for low beds and bed or chair alarms the rate of falls trended towards being higher [45, 48, 49].
There were several limitations of this analysis. We did not evaluate injury data associated with falls due to inconsistent definitions applied by studies. In addition, we did not examine the effects of care-giver education on falls risk or rates. It could be helpful to enlist family members as care providers to be part of the social network around patients, especially for patients with cognitive impairment, who have disproportionately high falls rates [75–78]. It was beyond the scope of this analysis to quantify the outcome of quality improvement (QI) initiatives, especially those pertaining to health professional education and training, despite growing traction of QI [76–78]. Preventing falls in real life clinical settings sometimes means iterative, locally driven QI with continuous monitoring of changes in local falls and injury data and health professional behaviours [79]. At an organisational level, hospital staff working on patient safety are interested in what works locally to produce sustained reductions in falls in addition to considering the gold-standard evidence afforded by global systematic reviews and meta-analyses [80]. In this regard education is arguably a powerful tool, although it is not clear which elements of educational design and delivery have the most optimal effects [7, 81]. The falls intervention taxonomy that we used differed to a small extent from Lamb [82], limiting direct comparisons with the prior Cochrane review. Finally, we did not review studies on falls in the home, community or residential aged care, given the different epidemiology related to falls and injuries in these environments [83–86]. Only studies published in English were included.
To conclude, no single definitive method exists for hospital falls prevention. This analysis of the global literature showed that education was the most effective strategy for reducing the rate and risk of hospital falls and multi-factorial interventions had a tendency to produce a positive impact.
Supplementary Material
Acknowledgements
We acknowledge the contributions of Elizabeth Lawrence, La Trobe University librarian, in assisting us with the literature search. We also thank the Healthscope team for supporting the falls prevention project.
Declaration of Conflicts of Interest
Terry Haines has provided expert witness testimony on the subject of the prevention of falls in hospitals to K&L Gates Law Firm, and Minter Ellison Law Firm in the past 36 months.
Declaration of Sources of Funding
This systematic review was conducted as part of a National Health & Medical Research Council Australia partnership grant (1152853) in partnership with Healthscope, Holmesglen Institute, La Trobe University and a number of other Australian universities. Professor Anne-Marie Hill receives support through a National Health and Medical Research Council of Australia Career Development Fellowship and by the Royal Perth Hospital Research Foundation (S01/2021). Professor Steven Michael McPhail is supported by a National Health and Medical Research Council fellowship (#1161138). The funder had no role in the design, execution, analysis and interpretation of data, or writing of the study.
References
- 1. Cameron ID, Dyer SM, Panagoda CEet al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018; 9: 1–292. CD005465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Avanecean D, Calliste D, Contreras T, Lim Y, Fitzpatrick A. Effectiveness of patient-centered interventions on falls in the acute care setting compared to usual care: a systematic review. JBI Database System Rev Implement Rep 2017; 15: 3006–48. [DOI] [PubMed] [Google Scholar]
- 3. Bouldin ELD, Andresen EM, Dunton NEet al. Falls among adult patients hospitalized in the United States: prevalence and trends. J Patient Saf 2013; 9: 13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sato N, Hase N, Osaka A, Sairyo K, Katoh S. Falls among hospitalized patients in an acute care hospital: analyses of incident reports. J Med Invest 2018; 65: 81–4. [DOI] [PubMed] [Google Scholar]
- 5. Barker AL, Morello RT, Wolfe Ret al. 6-PACK programme to decrease fall injuries in acute hospitals: cluster randomised controlled trial. BMJ 2016; 352: h6781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Haines T, Kuys SS, Morrison G, Clarke J, Bew P. Balance impairment not predictive of falls in geriatric rehabilitation wards. The Journals of Gerontology: Series A 2008; 63: 523–8. [DOI] [PubMed] [Google Scholar]
- 7. Hill A, McPhail S, Waldron Net al. Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet 2015; 385: 2592–9. [DOI] [PubMed] [Google Scholar]
- 8. Hester AL, Tsai P-F, Rettiganti M, Mitchell A. Predicting injurious falls in the hospital setting: implications for practice. Am J Nurs 2016; 116: 24–31. [DOI] [PubMed] [Google Scholar]
- 9. Hill A-M, Hoffmann T, Hill Ket al. Measuring falls events in acute hospitals-a comparison of three reporting methods to identify missing data in the hospital reporting system. J Am Geriatr Soc 2010; 58: 1347–52. [DOI] [PubMed] [Google Scholar]
- 10. Slade SC, et al. Effects of falls prevention interventions on falls outcomes for hospitalised adults: protocol for a systematic review with meta-analysis. BMJ Open 2017; 7: e017864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hallford DJ, Nicholson G, Sanders K, McCabe MP. The association between anxiety and falls: a meta-analysis. J Gerontol 2016; 72: 729–41. [DOI] [PubMed] [Google Scholar]
- 12. Heng H, Jazayeri D, Shaw L, Kiegaldie D, Hill AM, Morris ME. Hospital falls prevention with patient education: a scoping review. BMC Geriatr 2020; 20: 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tricco AC, Thomas SM, Veroniki AAet al. Comparisons of interventions for preventing falls in older adults: a systematic review and meta-analysis. JAMA 2017; 318: 1687–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ryan S, Ward M, Vaughan Det al. Do safety briefings improve patient safety in the acute hospital setting? A systematic review. J Adv Nurs 2019; 75: 2085–98. [DOI] [PubMed] [Google Scholar]
- 15. Toye C, Slatyer S, Kitchen Set al. Bed moves, ward environment, staff perspectives and falls for older people with high falls risk in an acute hospital: a mixed methods study. Clin Interv Aging 2019; 14: 2223–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stephenson M, McArthur A, Giles K, Lockwood C, Aromataris E, Pearson A. Prevention of falls in acute hospital settings: a multi-site audit and best practice implementation project. International J Qual Health Care 2016; 28: 92–8. [DOI] [PubMed] [Google Scholar]
- 17. Miake-Lye IM, Hempel S, Ganz DA, Shekelle PG. Inpatient fall prevention programs as a patient safety strategy: a systematic review. Ann Intern Med 2013; 158: 390–6. [DOI] [PubMed] [Google Scholar]
- 18. Haines TP, Lee D-CA, O'Connell B, McDermott F, Hoffmann T. Why do hospitalized older adults take risks that may lead to falls? Health Expect 2015; 18: 233–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hill A-M, Francis-Coad J, Haines TPet al. ‘My independent streak may get in the way’: how older adults respond to falls prevention education in hospital. BMJ Open 2016; 6: e012363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. National Institute for Health and Care Excellence . Falls in Older People: Assessing Risk and Prevention [Internet]. London: NICE, 2013; Available from: https://www.nice.org.uk/guidance/cg161. [PubMed] [Google Scholar]
- 21. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6 (updated July 2019) Wiley; 2019. [Available from: http://www.training.cochrane.org/handbook]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Review Manager Web (RevMan Web) The Cochrane Collaboration, 2020.
- 23. Microsoft Excel . Microsoft Corporation, 2018.
- 24. Joanna Briggs Institute . 2020. [Available from: https://joannabriggs.org/critical_appraisal_tools 10.1002/9781119536604 [DOI]
- 25. McMaster University dbEP, Inc. GRADEpro GDT: GRADEpro Guideline Decelopment Tool [Software], 2015.
- 26. Guyatt G, Oxman AD, Akl EAet al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011; 64: 383–94. [DOI] [PubMed] [Google Scholar]
- 27. Slade SC, Dionne CE, Underwood Met al. Consensus on exercise reporting template (CERT): modified Delphi study. Phys Ther 2016; 96: 1514–24. [DOI] [PubMed] [Google Scholar]
- 28. Jellett J, Williams C, Clayton D, Plummer V, Haines T. Falls risk score removal does not impact inpatient falls: a stepped-wedge, cluster-randomised trial. J Clin Nurs 2020; 29: 4505–13. [DOI] [PubMed] [Google Scholar]
- 29. Morris ME, Haines T, Hill AMet al. Divesting from a scored hospital fall risk assessment tool (FRAT): a cluster randomized non-inferiority trial. J Am Geriatr Soc 2021; 69: 2598–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Aizen E, Lutsyk G, Wainer L, Carmeli S. Effectiveness of individualized fall prevention program in geriatric rehabilitation hospital setting: a cluster randomized trial. Aging Clin Exp Res 2015; 27: 681–8. [DOI] [PubMed] [Google Scholar]
- 31. Ang E, Mordiffi SZ, Wong HB. Evaluating the use of a targeted multiple intervention strategy in reducing patient falls in an acute care hospital: a randomized controlled trial. J Adv Nurs 2011; 67: 1984–92. [DOI] [PubMed] [Google Scholar]
- 32. Cumming RG, Sherrington C, Lord SRet al. Cluster randomised trial of a targeted multifactorial intervention to prevent falls among older people in hospital. BMJ 2008; 336: 758–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dykes PC, Carroll DL, Hurley A, Lipsitz S, Benoit A, Chang F. Fall prevention in acute care hospitals: a randomized trial. JAMA 2010; 304: 1912–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Haines T, Bennell K, Osborne R, Hill K. Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial. Br Med J 2004; 328: 676–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Healey F, Monro A, Cockram A, Adams V, Heseltine D. Using targeted risk factor reduction to prevent falls in older in-patients: a randomised controlled trial. Age Ageing 2004; 33: 390–5. [DOI] [PubMed] [Google Scholar]
- 36. Koh SL, Hafizah N, Lee JY, Loo YL, Muthu R. Impact of a fall prevention programme in acute hospital settings in Singapore. Singapore Med J 2009; 50: 425–32. [PubMed] [Google Scholar]
- 37. Krauss MJ, Tutlam N, Constantinou E, Johnson S, Jackson D, Fraser VJ. Intervention to prevent falls on the medical service in a teaching hospital. Infect Control Hosp Epidemiol 2008; 29: 539–45. [DOI] [PubMed] [Google Scholar]
- 38. Mador JE, Giles L, Whitehead C, Crotty M. A randomized controlled trial of a behavior advisory service for hospitalized older patients with confusion. Int J Geriatr Psychiatry 2004; 19: 858–63. [DOI] [PubMed] [Google Scholar]
- 39. Schwendimann R, Milisen K, Buhler H, De Geest S. Fall prevention in a Swiss acute care hospital setting reducing multiple falls [Erratum appears in J Gerontol Nurs. 2006; 32: 56]. J Gerontol Nurs 2006; 32: 13–22. [DOI] [PubMed] [Google Scholar]
- 40. Stenvall M, Olofsson B, Lundstrom Met al. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporos Int 2007; 18: 167–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Vassallo M, Vignaraja R, Sharma Jet al. The effect of changing practice on fall prevention in a rehabilitative hospital: the hospital injury prevention study. J Am Geriatr Soc 2004; 52: 335–9. [DOI] [PubMed] [Google Scholar]
- 42. Wald HL, Glasheen JJ, Guerrasio J, Youngwerth JM, Cumbler EU. Evaluation of a hospitalist-run acute care for the elderly service. J Hosp Med 2011; 6: 313–21. [DOI] [PubMed] [Google Scholar]
- 43. Gaal BG, Schoonhoven L, Mintjes JAet al. Fewer adverse events as a result of the SAFE or SORRY? Programme in hospitals and nursing homes. Part I: primary outcome of a cluster randomised trial. Int J Nurs Stud 2011; 48: 1040–8. [DOI] [PubMed] [Google Scholar]
- 44. Healey F, Lowe D, Darowski Aet al. Falls prevention in hospitals and mental health units: an extended evaluation of the FallSafe quality improvement project. Age Ageing 2014; 43: 484–91. [DOI] [PubMed] [Google Scholar]
- 45. Haines TP, Bell RAR, Varghese PN. Pragmatic, cluster randomized trial of a policy to introduce low-low beds to hospital wards for the prevention of falls and fall injuries. J Am Geriatr Soc 2010; 58: 435–41. [DOI] [PubMed] [Google Scholar]
- 46. Mayo NE, Gloutney L, Levy AR. A randomized trial of identification bracelets to prevent falls among patients in a rehabilitation hospital. Arch Phys Med Rehabil 1994; 75: 1302–8. [PubMed] [Google Scholar]
- 47. Sahota O, Drummond A, Kendrick Det al. REFINE (REducing falls in in-patieNt elderly) using bed and bedside chair pressure sensors linked to radio-pagers in acute hospital care: a randomised controlled trial. Age Ageing 2014; 43: 247–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Shorr RI, Michelle Chandler A, Mion LCet al. Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients: a cluster randomized trial. Ann Intern Med 2012; 157: 692–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Tideiksaar R, Feiner CF, Maby J. Falls prevention: the efficacy of a bed alarm system in an acute-care setting. Mt Sinai J Med 1993; 60: 522–7. [PubMed] [Google Scholar]
- 50. Wolf KH, Hetzer K, zu Schwabedissen HM, Wiese B, Marschollek M. Development and pilot study of a bed-exit alarm based on a body-worn accelerometer. Z Gerontol Geriatr 2013; 46: 727–33. [DOI] [PubMed] [Google Scholar]
- 51. Visvanathan R, Ranasinghe DC, Lange Ket al. Effectiveness of the wearable sensor-based ambient intelligent geriatric management (AmbIGeM) system in preventing falls in older people in hospitals. J Gerontol Series A 2021; 77: 155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Donald I, Pitt K, Armstrong E, Shuttleworth H. Preventing falls on an elderly care rehabilitation ward. Clin Rehabil 2000; 14: 178–85. [DOI] [PubMed] [Google Scholar]
- 53. Jarvis N, Kerr K, Mockett S. Pilot study to explore the feasibility of a randomised controlled trial to determine the dose effect of physiotherapy on patients admitted to hospital following a fall. Pract Evidence 2007; 2: 4–12. [Google Scholar]
- 54. Padula CA, Disano C, Ruggiero Cet al. Impact of lower extremity strengthening exercises and mobility on fall rates in hospitalized adults. J Nurs Care Qual 2011; 26: 279–85. [DOI] [PubMed] [Google Scholar]
- 55. Treacy D, Schurr K, Lloyd B, Sherrington C. Additional standing balance circuit classes during inpatient rehabilitation improved balance outcomes: an assessor-blinded randomised controlled trial. Age Ageing 2015; 44: 580–6. [DOI] [PubMed] [Google Scholar]
- 56. Martinez-Velilla N, Casas-Herrero A, Zambom-Ferraresi Fet al. Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Intern Med 2019; 179: 28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Haines TP, Hill AM, Hill KDet al. Patient education to prevent falls among older hospital inpatients: a randomized controlled trial. Arch Intern Med 2011; 171: 516–24. [DOI] [PubMed] [Google Scholar]
- 58. Krepper R, Vallejo B, Smith Cet al. Evaluation of a standardized hourly rounding process (SHaRP). J Healthc Qual 2014; 36: 62–9. [DOI] [PubMed] [Google Scholar]
- 59. Michalek C, Wehling M, Schlitzer J, Frohnhofen H. Effects of "Fit fOR The Aged" (FORTA) on pharmacotherapy and clinical endpoints--a pilot randomized controlled study. Eur J Clin Pharmacol 2014; 70: 1261–7. [DOI] [PubMed] [Google Scholar]
- 60. Nedved P, Chaudhry R, Pilipczuk D, Shah S. Impact of the unit-based patient safety officer. J Nurs Adm 2012; 42: 431–4. [DOI] [PubMed] [Google Scholar]
- 61. Castro-Avila A, Bloor K, Thompson C. The effect of external inspections on safety in acute hospitals in the National Health Service in England: a controlled interrupted time-series analysis. J Health Serv Res Policy 2019; 24: 182–90. [DOI] [PubMed] [Google Scholar]
- 62. Daley B, Fetherman B, Turner J. Staffing utilization and fall prevention with an electronic surveillance video system: a randomized controlled study. J Nurs Care Qual 2020; 36: 57–61. [DOI] [PubMed] [Google Scholar]
- 63. Hardin SR, Dienemann J, Rudisill P, Mills KK. Inpatient fall prevention: use of in-room webcams. J Patient Saf 2013; 9: 29–35. [DOI] [PubMed] [Google Scholar]
- 64. Bott N, Wexler S, Drury Let al. A protocol-driven, bedside digital conversational agent to support nurse teams and mitigate risks of hospitalization in older adults: case control pre-post study. J Med Internet Res 2019; 21: e13440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Malfait S, Eeckloo K, Van Opdorp L, Van Biesen W, Van Hecke A. The impact of bedside handovers on relevant clinical indicators: a matched-controlled multicentre longitudinal study. J Adv Nurs (John Wiley & Sons, Inc) 2020; 76: 2104, jan.14406–12. [DOI] [PubMed] [Google Scholar]
- 66. Sheppard D, Clarke E, Hemming K, Martin J, Lilford R. An opportunistic evaluation of a routine service improvement project to reduce falls in hospital. BMC Health Serv Res 2021; 21: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Montejano-Lozoya R, Miguel-Montoya I, Gea-Caballero V, Mármol-López MI, Ruíz-Hontangas A, Ortí-Lucas R. Impact of nurses' intervention in the prevention of falls in hospitalized patients. Int J Environ Res Public Health 2020; 17: 6048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Drahota AK, Ward D, Udell JEet al. Pilot cluster randomised controlled trial of flooring to reduce injuries from falls in wards for older people. Age Ageing 2013; 42: 633–40. [DOI] [PubMed] [Google Scholar]
- 69. Hanger HC. Low-impact flooring: does it reduce fall-related injuries? J Am Med Dir Assoc 2017; 18: 588–91. [DOI] [PubMed] [Google Scholar]
- 70. Burleigh E, Potter J, McColl J. Does vitamin D stop hospital inpatients falling? -- a randomised controlled trial. Age Ageing 2006; 35: i40–i. [DOI] [PubMed] [Google Scholar]
- 71. Malfait S, Eeckloo K, Van Opdorp L, Van Biesen W, Van Hecke A. The impact of bedside handovers on relevant clinical indicators: a matched-controlled multicentre longitudinal study. J Adv Nurs 2020; 76: 2104–12. [DOI] [PubMed] [Google Scholar]
- 72. Tzeng HM, Yin CY. Nurses' solutions to prevent inpatient falls in hospital patient rooms. Nurs Econ 2008; 26: 179–87. [PubMed] [Google Scholar]
- 73. Renteln-Kruse W, Krause T. Incidence of in-hospital falls in geriatric patients before and after the introduction of an interdisciplinary team-based fall-prevention intervention. J Am Geriatr Soc 2007; 55: 2068–74. [DOI] [PubMed] [Google Scholar]
- 74. Oliver D, Healey F, Haines TP. Preventing falls and fall-related injuries in hospitals. Clin Geriatr Med 2010; 26: 645–92. [DOI] [PubMed] [Google Scholar]
- 75. Van Doorn C, Gruber-Baldini AL, Zimmerman Set al. Dementia as a risk factor for falls and fall injuries among nursing home residents. J Am Geriatr Soc 2003; 51: 1213–8. [DOI] [PubMed] [Google Scholar]
- 76. Gleason CE, Gangnon RE, Fischer BL, Mahoney JE. Increased risk for falling associated with subtle cognitive impairment: secondary analysis of a randomized clinical trial. Dement Geriatr Cogn Disord 2009; 27: 557–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Shaw L, Kiegaldie D, Farlie M. Education interventions for health professionals on falls prevention in health care settings: a 10-year scoping review. BMC Geriatr 2020; 20: 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Shaw LK, Kiegaldie D, Morris ME, Jones C. Improving hospital falls screening and mitigation using a health professional education framework. Nurse Educ Today 2021; 98: 104695. [DOI] [PubMed] [Google Scholar]
- 79. Montero-Odasso M, Velde N, Alexander NBet al. New horizons in falls prevention and management for older adults: a global initiative. Age Ageing 2021; 50: 1499–507. [DOI] [PubMed] [Google Scholar]
- 80. Montero-Odasso MM, Kamkar N, Pieruccini-Faria Fet al. Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. JAMA Netw Open 2021; 4: e2138911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Heng H, Slade SC, Jazayeri Det al. Patient perspectives on hospital falls prevention education. Front Public Health 2021; 9: 592440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Lamb SE, Becker C, Gillespie LDet al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials 2011; 12: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Kerse N, Peri K, Robinson Eet al. Does a functional activity programme improve function, quality of life, and falls for residents in long term care? Cluster randomised controlled trial BMJ 2008; 337: a1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sherrington C, Fairhall N, Wallbank Get al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med 2020; 54: 885–91. [DOI] [PubMed] [Google Scholar]
- 85. Pillay J, Riva JJ, Tessier LAet al. Fall prevention interventions for older community-dwelling adults: systematic reviews on benefits, harms, and patient values and preferences. Syst Rev 2021; 10: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Logan PA, Horne JC, Gladman JRFet al. Multifactorial falls prevention programme compared with usual care in UK care homes for older people: multicentre cluster randomised controlled trial with economic evaluation. BMJ 2021; 375: e066991. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.