Abstract
Acne is the most common skin condition in the United States and affects approximately 85% of people ages 12–24. As a multifactorial disease, the pathogenesis of acne involves overproduction of sebum, irregular shedding of the cutaneous cells, accretion of Cutibacterium acnes at the pilosebaceous unit, and inflammation. To date, conventional therapies for acne include topical retinoids, over-the-counter bactericidal agents, and systematic treatments, such as oral antibiotics and isotretinoin. However, the potential for significant side effects and risk of antibiotic resistance remain limitations in these therapies, in turn reducing patient compliance and adherence to acne treatment regimens. Therefore, the use of natural plant-derived treatments or phytotherapeutics as an alternative or adjuvant to conventional treatments is attractive to patients due to their safety and minimal risk for side effects. Cannabidiol (CBD) is a non-psychoactive phytocannabinoid of the Cannabis sativa (hemp) plant. The therapeutic use of CBD has been implicated in many diseases with an inflammatory aspect, including cancers, neurodegeneration, immunological disorders, and dermatological diseases. However, the use of CBD for acne treatment remains a novel window of opportunity. Herein, we summarize the available and relevant data, highlighting the potential use of CBD in acne for its anti-inflammatory properties. To that extent, CBD and other cannabis constituents such as cannabis seeds were found to reduce inflammation and expression of inflammatory cytokines including TNF-α and IL-1β when evaluated in acne-like conditions. Treatment with these cannabis extracts was also found to be safe and well tolerated, further strengthening the prospect of CBD as an anti-inflammatory therapeutic for acne.
Keywords: cannabidiol, CBD, acne, inflammation, therapeutic
Introduction
As the 8th most prevalent disease, Acne vulgaris (acne) affects an estimated 9.4% of the world’s population.1 In the United States alone, acne is estimated to affect at least 40 million individuals and is the most common skin disorder.2,3 Although most common in adolescents, acne may begin in younger children and persist through adulthood as well.2 Unfortunately, this widespread disease is associated with discomfort, scarring of the skin, as well as emotional and psychological distresses.1 Furthermore, by affecting 85% of adolescents, acne is often associated with significant psychosocial effects including, negative self-perception and self-esteem in addition to decreased social interactions and overall quality of life.4 Despite this, treatment options and treatment compliance remain barriers.5,6
Acne
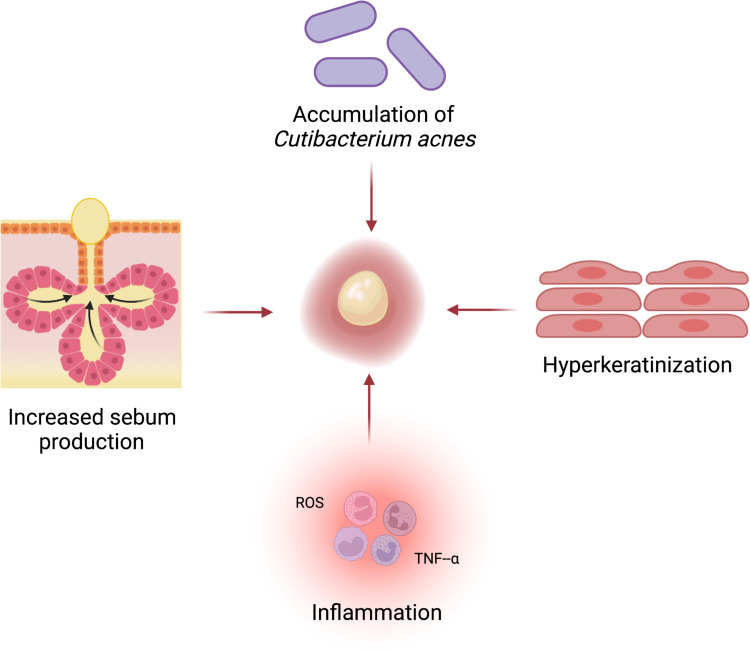
Acne is a multifactorial disease; therefore, the onset and progression of the disease can be triggered by an interplay of many factors including stress, and hormonal and nutritional alterations.7,8 Pathologically, acne is an inflammatory disease affecting the pilosebaceous units. The pilosebaceous unit consists of the hair follicle and shaft, and sebaceous gland; these sebaceous pores are found on the face, chest, and back.9,10 Excess sebum production (hyperseborrhea), abnormal shedding of the cutaneous cells (hyperkeratinization), accumulation of Cutibacterium acnes (C. acnes) at the pilosebaceous unit, and inflammation are elemental to the disruption of sebaceous gland activity and pathogenesis of acne (Figure 1).7,10,11 Androgen hormones, particularly testosterone, stimulate sebum production and are linked to the formation of comedones.12 Comedones are formed when the pilosebaceous units become plugged with sebum and can be classified as open comedones (blackheads) or closed comedones (whiteheads). Follicular hyperkeratinization occurs when cutaneous cells that line the sebaceous follicle, primarily keratinocytes, do not become cohesive with one another, resulting in rapid shedding of these cells, and subsequent microcomedone formation.13 Colonization of C. acnes at the sebaceous follicle may also lead to comedogenesis and subsequent presentation of acne. C. acnes, formerly termed Propionibacterium acnes (P. acnes), is a gram-positive anaerobic commensal bacteria found as part of the skin’s microbiota in all individuals to maintain skin homeostasis.7,14 However, colonization of C. acnes at the pilosebaceous units, particularly in areas densely packed with sebaceous follicles that harbor a lipid-rich environment, is a pathological hallmark of acne.12 While C. acnes is present cutaneously in all individuals, the onset of acne is dependent on individual immunological responses to the bacteria, triggering the formation of comedones and the release of inflammatory mediators.12 Detection of C. acnes initiates an inflammatory response by the immune system, triggering the release of inflammatory cells, such as lymphocytes and neutrophils, and their subsequent release of inflammatory chemicals, such as reactive oxygen species (ROS) and tumor necrosis factor-alpha (TNF-α).15 Consequently, these inflammatory mediators contribute to the inflammation and the subsequent chemical insult to the follicle epithelium and proximate dermis.12,16
Figure 1.
Acne pathogenesis. Interplay of increased sebum production, accumulation of C. acnes, hyperkeratinization, and inflammation resulting in the formation of comedones. Created with BioRender.com.
Current Treatments for Acne
The management of acne involves topical and systematic treatments (Table 1). Topical retinoids such as tretinoin and erythromycin are commonly prescribed as comedolytic agents and for their anti-inflammatory properties.10 Topical over-the-counter formulations containing salicylic acid and benzoyl peroxide are also used as bactericidal agents to treat mild-to-moderate acne.3 Systematic treatment of acne primarily includes tetracycline family antibiotics, such as minocycline and doxycycline.17 These oral antibiotics are commonly prescribed for moderate-to-severe acne. In patients with very severe acne in which antibiotics are no longer effective, oral Isotretinoin is often prescribed to control the presence of C. acnes, and to reduce sebum production and inflammation.10,18 Additionally, oral contraceptives, such as those with low-dose estrogen, may also be prescribed for persistent acne for anti-androgenic effects.10
Table 1.
Current Acne Treatments
| Mild Acne | Moderate Acne | Severe Acne | |
|---|---|---|---|
| Topical | Bactericidal agents (Benzoyl Peroxide, Salicylic Acid) Topical retinoids |
Topical retinoids (Tetracycline, Tretinoin, Erythromycin) | Bactericidal agents Topical retinoids |
| Systematic | – | Oral Tetracyclines (Minocycline, Doxycycline) Oral contraceptives |
Isotretinoin Oral Contraceptives |
Nonetheless, there are significant limitations to these conventional treatments, leading to low patient adherence and compliance.5,19 For example, topical retinoids may irritate the skin, with side effects including burning, drying, itching, and redness.5,19 These effects may lead to early termination of the treatment by the patient. Furthermore, long-term use of topical and oral antibiotics may lead to bacterial and antimicrobial antibiotic resistance.5,6 Although generally regarded as safe, Isotretinoin is also known to exhibit embryotoxic and teratogenic properties.5,19 These potential adverse side effects may deter patients from commencing or continuing their acne treatment, therefore highlighting the need for new, natural, and safe therapies. As many plant derivatives have already been widely investigated for their innate anti-inflammatory properties for the treatment of acne, herein, we draw attention to Cannabidiol as a potential anti-inflammatory phytotherapeutic for acne.
Cannabidiol
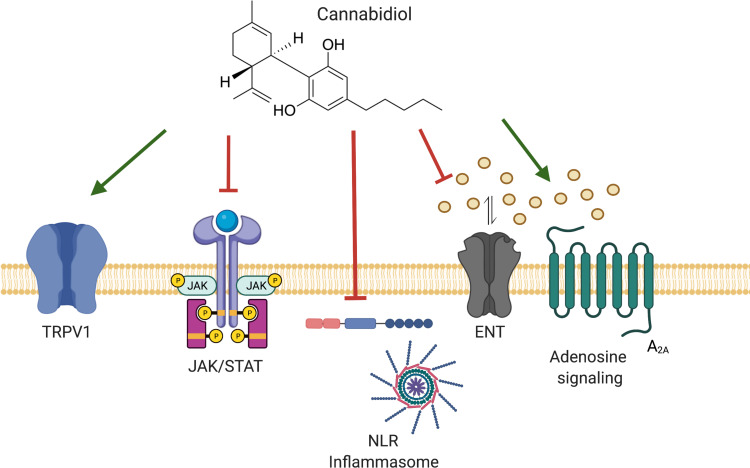
Cannabidiol (CBD) is a non-psychoactive biochemical constituent of the Cannabis sativa (hemp) plant. In recent years, the investigation and use of CBD for its anti-inflammatory and immunomodulatory effects has become extensive amongst the scientific community.20 The therapeutic potential of CBD has been extensively supported in various immunological, neurodegenerative, cancer, cardiovascular, and dermatological diseases, as conditions with an inflammatory component.21 To date, Epidiolex remains the first and sole FDA-approved prescription CBD drug used to treat seizures. Mechanistically, CBD decreases inflammation and subsequent cytokine production through modulation of the immune system and suppression of immune responses.22 We have previously reviewed the anti-inflammatory and immune suppressive effects of CBD through modulation of critical signaling pathways and receptors.23 As CBD does not have a high affinity for CB1 and CB2 receptors, the pharmacological activity of CBD is suggested to be independent of these receptors. Instead, CBD has been studied to modulate pro-inflammatory transient receptor potential vanilloid 1 channel (TRPV1), such that treatment with TRPV1 antagonists reversed the anti-inflammatory and immune suppressive effects of CBD (Figure 2).23–25 CBD also modulates the Janus kinase/signal transducers and activators of transcription (JAK/STAT) signaling pathway, a fundamental regulator of immune responses, by inhibiting cytokines that facilitate the activation of the cascade (Figure 2).23,26,27 Since constitutive activation of JAK/STAT has been implicated in the pathogenesis of immunological diseases and cancers, CBD-induced reduction of pro-inflammatory signaling is desirable.27,28 To that extent, CBD has been shown to suppress inflammatory cytokine initiators of JAK/STAT, such as TNF-α, Interferon-γ (IFN- γ), Interleukin-1 (IL-1), IL-2, and IL-6 in vitro and in vivo.23,26,28 CBD has been shown to prevent nucleotide-binding oligomerization domain-like receptors (NLR) inflammasome complex activation, suppressing the production of pro-inflammatory cytokines, such as IL-1β and IL-18 that are critical in regulating NF-κB, MAPK, and IFN pro-inflammatory pathways (Figure 2).23,29,30 Furthermore, CBD has also been studied to modulate adenosine signaling by inhibiting rapid cellular uptake of adenosine by the equilibrative nucleoside transporter (Figure 2) (ENT).31–33 Adenosine is a purine nucleoside that exhibits protective effects and attenuates inflammation by activating G protein-coupled adenosine receptor, A2A.23,33,34 By inhibiting intracellular adenosine uptake, CBD promotes endogenous adenosine signaling as a protective mechanism during inflammatory and immune response.23,35 Taken together, a mechanistic understanding of the pharmacological reduction of inflammation by CBD further supports therapeutic exploration of CBD as a novel and unique anti-inflammatory option. Next, we specifically highlight the potential use of CBD for acne treatment.23
Figure 2.
Molecular and signaling pathway targets of CBD. The underlying anti-inflammatory properties of CBD may be attributed to agonism of transient receptor potential vanilloid 1 (TRPV1), inhibition of Janus kinase/signal transducers and activators of transcription (JAK/STAT) and signaling, inhibition of the nucleotide-binding oligomerization domain-like receptors (NLR) inflammasome complex activation, inhibition of adenosine uptake by the equilibrative nucleoside transporter (ENT), and promotion of adenosine signaling by the adenosine receptor (A2A). Created with BioRender.com.
CBD and Acne
In a study evaluating the effects of CBD on human sebaceous glands, CBD was evaluated in the context of immortalized human sebocytes under “acne-like” conditions.20 In this study, CBD was shown to dose-dependently inhibit excessive lipid synthesis (lipogenesis) in sebocyte cultures that were pre-treated with “pro-acne” inducing inflammatory compounds such as arachidonic acid, linoleic acid, and testosterone.20 The anti-inflammatory effects of CBD were also observed in the reduction of inflammatory cytokine TNF-α. Lipopolysaccharides36 were used to pre-treat sebocytes to induce “pro-acne” inflammatory conditions. Subsequently, TNF-α concentrations in sebocytes were measured after 24 h with or without CBD (10 μM).20 Treatment with CBD was found to decrease TNF-α mRNA expression and the expression of other inflammatory cytokines including, IL-1β and IL-6 in the sebocytes.20 Results from this study strongly demonstrate the clinical potential of CBD in the treatment of acne.20 In a separate study, the potential anti-acne effects of another cannabis plant derivative, hemp seed hexane extracts (HSHE), were evaluated in an in vitro model of acne.37 Like CBD, hemp seed extracts also do not exhibit psychotropic properties and are suggested to have potential anti-inflammatory effects. In a human keratinocyte cell line, 0.6% was HSHE reduced C. acnes-induced inflammation in human keratinocytes through down-regulation of pro-inflammatory cytokines, IL-1β and IL-8.37 Additionally, 0.6% HSHE was found to significantly inhibit overproduction of inflammatory radical nitric oxide in the same cells, further supporting the conventional development of hemp-derived constituents, such as HSHE as natural, safe, and effective anti-inflammatory acne treatments.37 In a human study evaluating the safety and efficacy of cannabis seed extracts for acne, 3% cannabis seed extracts were found to reduce inflammation-induced redness of the skin, known as erythema.38 Changes in skin erythema were measured every 2 weeks for a total of 12 weeks. Treatment with the 3% cannabis seeds extract cream was found to significantly reduce skin erythema after each 2-week observation, and a notable gradual reduction in erythema was observed across the 12-week study.38 Furthermore, the application of 3% cannabis seeds extract cream on the cheeks, twice a day, for 12 weeks was found to be safe, well tolerated, non-allergenic, and non-irritating in the patient volunteers.38
Discussion
Acne is the most prevalent condition in the US, affecting nearly 50 million people.2,3 As a widespread disease that affects most people at some point in their lifetime, the effects of acne include significant irritation and scarring of the skin, in addition to emotional and psychosocial distress. Furthermore, treatment options and compliance remain challenges due to the potential adverse side effects of conventional treatments and the increasing emergence of antibiotic resistance, suggesting the need for new, natural, and safe acne therapies. As CBD possesses anti-inflammatory activities, CBD has been widely studied in various inflammatory and immunological disorders, including Alzheimer’s diseases, diabetes, multiple sclerosis, and rheumatoid arthritis, setting a precedent for investigation of CBD in other inflammatory conditions, such as acne. Understanding of the pharmacodynamics of CBD reveals modulation of critical inflammatory and immunological pathways and receptors leading to a decrease in inflammation and subsequent cytokine production, further supporting the anti-inflammatory effects of CBD. Evaluation of CBD in acne-like conditions revealed suppressed expression of pro-inflammatory cytokines, TNF-α, IL-1β, and IL- 6. CBD also reduced excessive lipid synthesis.
Like CBD, hemp seed extracts are also derived from cannabis, and while they are suggested to have anti-inflammatory properties, they do not exhibit psychoactive effects. Nevertheless, hemp seed extracts have also been shown to reduce C. acnes-induced inflammation and inflammatory cytokine production of IL-1β and IL-8. Additionally, these hemp seed extracts also significantly protect cells from overproduction of inflammatory radicals and nitric oxides, further supporting the use of hemp-derived constituents as potential natural, safe, and effective anti-inflammatory therapies. Moreover, in a small patient study, treatment with another cannabis derivative, cannabis seed extract cream, was found to be efficacious in reducing skin inflammation, as well as safe and non-irritating. Accordingly, the use of CBD for reducing inflammation in acne is supported and should be further explored. Since the pathogenesis of acne is complex and multifactorial, limitations include the lack of reliable animal models to mimic acne conditions and test therapeutics.39 Additionally, there is an evident need for large-scale human studies to understand the impact of CBD on acne at the clinical level.40 Future studies may also optimize the concentration and delivery of CBD for the treatment of acne. In conclusion, CBD may be beneficial as an adjuvant anti-inflammatory treatment for acne.
Acknowledgments
SD thanks the Miller School of Medicine of the University of Miami for the Lucille P. Markey Chair in Biochemistry and Molecular Biology.
Funding Statement
This research received no external funding.
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.Tan JK, Bhate K. A global perspective on the epidemiology of acne. Br J Dermatol. 2015;172(Suppl 1):3–12. doi: 10.1111/bjd.13462 [DOI] [PubMed] [Google Scholar]
- 2.Cordain L, Lindeberg S, Hurtado M, et al. Acne vulgaris: a disease of Western civilization. Arch Dermatol. 2002;138(12):1584–1590. doi: 10.1001/archderm.138.12.1584 [DOI] [PubMed] [Google Scholar]
- 3.Titus S, Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012;86(8):734–740. [PubMed] [Google Scholar]
- 4.Dunn LK, O’Neill JL, Feldman SR. Acne in adolescents: quality of life, self-esteem, mood, and psychological disorders. Dermatol Online J. 2011;17(1):1. [PubMed] [Google Scholar]
- 5.Habeshian KA, Cohen BA. Current issues in the treatment of acne vulgaris. Pediatrics. 2020;145(Suppl 2):S225–S230. doi: 10.1542/peds.2019-2056L [DOI] [PubMed] [Google Scholar]
- 6.Castillo DE, Nanda S, Keri JE. Propionibacterium (cutibacterium) acnes bacteriophage therapy in acne: current evidence and future perspectives. Dermatol Ther. 2019;9(1):19–31. doi: 10.1007/s13555-018-0275-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dreno B, Pécastaings S, Corvec S, et al. Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: a brief look at the latest updates. J Eur Acad Dermatol Venereol. 2018;32(Suppl 2):5–14. doi: 10.1111/jdv.15043 [DOI] [PubMed] [Google Scholar]
- 8.Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945–73 e33. doi: 10.1016/j.jaad.2015.12.037 [DOI] [PubMed] [Google Scholar]
- 9.Martel JL, Miao JH, Badri T. Anatomy, Hair Follicle. Treasure Island (FL): StatPearls; 2021. [PubMed] [Google Scholar]
- 10.Gollnick H, Cunliffe W, Berson D, et al. Management of acne: a report from a global alliance to improve outcomes in acne. J Am Acad Dermatol. 2003;49(1 Suppl):S1–S37. doi: 10.1067/mjd.2003.618 [DOI] [PubMed] [Google Scholar]
- 11.Dreno B. What is new in the pathophysiology of acne, an overview. J Eur Acad Dermatol Venereol. 2017;31(Suppl 5):8–12. doi: 10.1111/jdv.14374 [DOI] [PubMed] [Google Scholar]
- 12.Fox L, Csongradi C, Aucamp M, et al. Treatment modalities for acne. Molecules. 2016;21(8):1063. doi: 10.3390/molecules21081063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thiboutot DM. The role of follicular hyperkeratinization in acne. J Dermatol Treat. 2000;11(2):S5–S8. doi: 10.1080/095466300750163645 [DOI] [Google Scholar]
- 14.Platsidaki E, Dessinioti C. Recent advances in understanding Propionibacterium acnes (Cutibacterium acnes) in acne. F1000Res. 2018;7:1953. doi: 10.12688/f1000research.15659.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurokawa I, Danby FW, Ju Q, et al. New developments in our understanding of acne pathogenesis and treatment. Exp Dermatol. 2009;18(10):821–832. doi: 10.1111/j.1600-0625.2009.00890.x [DOI] [PubMed] [Google Scholar]
- 16.Akamatsu H, Horio T, Hattori K. Increased hydrogen peroxide generation by neutrophils from patients with acne inflammation. Int J Dermatol. 2003;42(5):366–369. doi: 10.1046/j.1365-4362.2003.01540.x [DOI] [PubMed] [Google Scholar]
- 17.Sutaria AH, Masood S, Schlessinger J. Acne Vulgaris. Treasure Island (FL): StatPearls; 2021. [PubMed] [Google Scholar]
- 18.Layton A. The use of isotretinoin in acne. Dermatoendocrinol. 2009;1(3):162–169. doi: 10.4161/derm.1.3.9364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moradi Tuchayi S, Alexander T, Nadkarni A, et al. Interventions to increase adherence to acne treatment. Patient Prefer Adherence. 2016;10:2091–2096. doi: 10.2147/PPA.S117437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olah A, Tóth BI, Borbíró I, et al. Cannabidiol exerts sebostatic and antiinflammatory effects on human sebocytes. J Clin Invest. 2014;124(9):3713–3724. doi: 10.1172/JCI64628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atalay S, Jarocka-Karpowicz I, Skrzydlewska E. Antioxidative and anti-inflammatory properties of cannabidiol. Antioxidants. 2019;9(1):21. doi: 10.3390/antiox9010021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nagarkatti P, Pandey R, Rieder SA, et al. Cannabinoids as novel anti-inflammatory drugs. Future Med Chem. 2009;1(7):1333–1349. doi: 10.4155/fmc.09.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peyravian N, Deo S, Daunert S, et al. Cannabidiol as a novel therapeutic for immune modulation. Immunotargets Ther. 2020;9:131–140. doi: 10.2147/ITT.S263690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Costa B, Giagnoni G, Franke C, Trovato AE, Colleoni M. Vanilloid TRPV1 receptor mediates the antihyperalgesic effect of the nonpsychoactive cannabinoid, cannabidiol, in a rat model of acute inflammation. Br J Pharmacol. 2004;143(2):247–250. doi: 10.1038/sj.bjp.0705920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fonseca BM, Correia-da-silva G, Teixeira NA. Cannabinoid-induced cell death in endometrial cancer cells: involvement of TRPV1 receptors in apoptosis. J Physiol Biochem. 2018;74(2):261–272. doi: 10.1007/s13105-018-0611-7 [DOI] [PubMed] [Google Scholar]
- 26.Malfait AM, Gallily R, Sumariwalla PF, et al. The nonpsychoactive cannabis constituent cannabidiol is an oral anti-arthritic therapeutic in murine collagen-induced arthritis. Proc Natl Acad Sci U S A. 2000;97(17):9561–9566. doi: 10.1073/pnas.160105897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kozela E, Pietr M, Juknat A, Rimmerman N, Levy R, Vogel Z. Cannabinoids Delta(9)-tetrahydrocannabinol and cannabidiol differentially inhibit the lipopolysaccharide-activated NF-kappaB and interferon-beta/STAT proinflammatory pathways in BV-2 microglial cells. J Biol Chem. 2010;285(3):1616–1626. doi: 10.1074/jbc.M109.069294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weiss L, Zeira M, Reich S, et al. Cannabidiol lowers incidence of diabetes in non-obese diabetic mice. Autoimmunity. 2006;39(2):143–151. doi: 10.1080/08916930500356674 [DOI] [PubMed] [Google Scholar]
- 29.Liu C, Ma H, Slitt AL, Seeram NP. Inhibitory effect of cannabidiol on the activation of NLRP3 Inflammasome is associated with its modulation of the P2X7 receptor in human monocytes. J Nat Prod. 2020;83(6):2025–2029. doi: 10.1021/acs.jnatprod.0c00138 [DOI] [PubMed] [Google Scholar]
- 30.Libro R, Scionti D, Diomede F, et al. Cannabidiol modulates the immunophenotype and inhibits the activation of the inflammasome in human gingival mesenchymal stem cells. Front Physiol. 2016;7:559. doi: 10.3389/fphys.2016.00559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Almeida DL, Devi LA. Diversity of molecular targets and signaling pathways for CBD. Pharmacol Res Perspect. 2020;8(6):e00682. doi: 10.1002/prp2.682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carrier EJ, Auchampach JA, Hillard CJ. Inhibition of an equilibrative nucleoside transporter by cannabidiol: a mechanism of cannabinoid immunosuppression. Proc Natl Acad Sci U S A. 2006;103(20):7895–7900. doi: 10.1073/pnas.0511232103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liou GI, Auchampach JA, Hillard CJ, et al. Mediation of cannabidiol anti-inflammation in the retina by equilibrative nucleoside transporter and A2A adenosine receptor. Invest Ophthalmol Vis Sci. 2008;49(12):5526–5531. doi: 10.1167/iovs.08-2196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hasko G, Cronstein BN. Adenosine: an endogenous regulator of innate immunity. Trends Immunol. 2004;25(1):33–39. doi: 10.1016/j.it.2003.11.003 [DOI] [PubMed] [Google Scholar]
- 35.Mecha M, Feliú A, Iñigo PM, et al. Cannabidiol provides long-lasting protection against the deleterious effects of inflammation in a viral model of multiple sclerosis: a role for A2A receptors. Neurobiol Dis. 2013;59:141–150. doi: 10.1016/j.nbd.2013.06.016 [DOI] [PubMed] [Google Scholar]
- 36.Gottlieb JF, Benedetti F, Geoffroy PA, et al. The chronotherapeutic treatment of bipolar disorders: a systematic review and practice recommendations from the ISBD task force on chronotherapy and chronobiology. Bipolar Disord. 2019;21(8):741–773. doi: 10.1111/bdi.12847 [DOI] [PubMed] [Google Scholar]
- 37.Jin S, Lee MY, Chen W. The ameliorative effect of hemp seed hexane extracts on the Propionibacterium acnes-induced inflammation and lipogenesis in sebocytes. PLoS One. 2018;13(8):e0202933. doi: 10.1371/journal.pone.0202933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ali A, Akhtar N. The safety and efficacy of 3% Cannabis seeds extract cream for reduction of human cheek skin sebum and erythema content. Pak J Pharm Sci. 2015;28(4):1389–1395. [PubMed] [Google Scholar]
- 39.Olah A, Markovics A, Szabó-Papp J, et al. Differential effectiveness of selected non-psychotropic phytocannabinoids on human sebocyte functions implicates their introduction in dry/seborrhoeic skin and acne treatment. Exp Dermatol. 2016;25(9):701–707. doi: 10.1111/exd.13042 [DOI] [PubMed] [Google Scholar]
- 40.Baswan SM, Klosner AE, Glynn K, et al. Therapeutic Potential of Cannabidiol (CBD) for skin health and disorders. Clin Cosmet Investig Dermatol. 2020;13:927–942. doi: 10.2147/CCID.S286411 [DOI] [PMC free article] [PubMed] [Google Scholar]