Abstract
Depression is a severe mental disorder that places a significant economic burden on public health. The reciprocal link between the trillions of bacteria in the gut, the microbiota, and depression is a controversial topic in neuroscience research and has drawn the attention of public interest and press coverage in recent years. Mounting pieces of evidence shed light on the role of the gut microbiota in depression, which is suggested to involve immune, endocrine, and neural pathways that are the main components of the microbiota-gut-brain axis. The gut microbiota play major roles in brain development and physiology and ultimately behavior. The bidirectional communication between the gut microbiota and brain function has been extensively explored in animal models of depression and clinical research in humans. Certain gut microbiota strains have been associated with the pathophysiology of depression. Therefore, oral intake of probiotics, the beneficial living bacteria and yeast, may represent a therapeutic approach for depression treatment. In this review, we summarize the findings describing the possible links between the gut microbiota and depression, focusing mainly on the inflammatory markers and sex hormones. By discussing preclinical and clinical studies on probiotics as a supplementary therapy for depression, we suggest that probiotics may be beneficial in alleviating depressive symptoms, possibly through immune modulation. Still, further comprehensive studies are required to draw a more solid conclusion regarding the efficacy of probiotics and their mechanisms of action.
Keywords: gut microbiota, inflammation, depression, sex hormones, probiotics
Gut Microbiota in Health
The trillions of bacteria inhabiting our gastrointestinal (GI) tract are referred to as “gut microbiota” and are well known to exert a marked influence on the host during homeostasis (Thursby and Juge, 2017). Approximately 160 species of bacteria are living in the human colon, with Bacteroidetes and Firmicutes being the dominant bacterial phyla in healthy individuals (Qin et al., 2010; Huttenhower et al., 2012; Sommer and Backhed, 2013; Rajilic-Stojanovic and de Vos, 2014). The gut microbiota are separated from immune cells by two mucus layers and a single layer of epithelial cells (Johansson et al., 2013; Mowat and Agace, 2014), allowing the regulation of the immune system and vice versa (Round and Mazmanian, 2009; Gensollen et al., 2016). They benefit the host by strengthening the gut integrity (Natividad and Verdu, 2013), providing nutrients such as vitamins (LeBlanc et al., 2013; Rowland et al., 2018), promoting resistance to colonization by pathogenic species (Cameron and Sperandio, 2015; Pacheco and Sperandio, 2015; Sassone-Corsi and Raffatellu, 2015; Baumler and Sperandio, 2016) and harvesting energy (den Besten et al., 2013). Therefore, a pathological alteration of the gut microbiota composition, known as dysbiosis, can have serious consequences on the health of the host, ranging from chronic GI diseases to neuropsychiatric disorders (Guinane and Cotter, 2013; Petersen and Round, 2014; Schroeder and Backhed, 2016).
The high-throughput and low-cost sequencing methods that have become available over the last decade enabled the investigation of the gut microbiota (Thursby and Juge, 2017). The bacterial species are nowadays easily distinguished via targeting the bacterial 16S ribosomal RNA gene that is present in all bacteria with enough sequence conservation and nine highly variable regions for phylogenetic analyses (Mizrahi-Man et al., 2013; Poretsky et al., 2014). To characterize the nature of the human microbiota and pave the way for a better understanding of human health and disease, the Human Microbiome Project (HMP) was carried out over 10 years and two phases (Turnbaugh et al., 2007; Proctor et al., 2019). Additionally, it can identify new diagnostic biomarkers of health, which will enhance our knowledge of the nutritional requirements of humans (Turnbaugh et al., 2007).
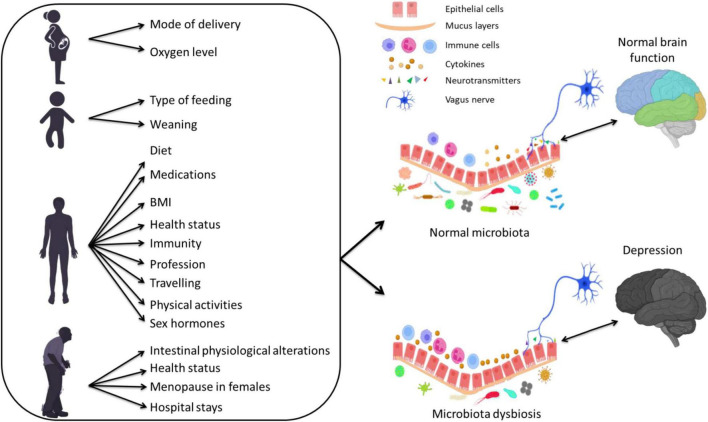
Different factors are known to shape the gut microbiota compositions including age (Odamaki et al., 2016; Hill et al., 2017; Aleman and Valenzano, 2019), host genetics (Kovacs et al., 2011; Org et al., 2016; Elderman et al., 2018; Kim et al., 2020), drugs (Wilson and Nicholson, 2009; Maier et al., 2018; Vich Vila et al., 2020), body mass index (BMI) (Ley et al., 2005; Yun et al., 2017; Gao et al., 2018; Stanislawski et al., 2018; Bai et al., 2019), diet, mode of delivery (Salminen et al., 2004; Rutayisire et al., 2016; Akagawa et al., 2019; Reyman et al., 2019), and environmental factors (Li et al., 2014; Osadchiy et al., 2019) (Figure 1). In particular, dietary modification exert a large effect on the gut microbiota (Walker et al., 2011; Zoetendal et al., 2012; David et al., 2014; Carmody et al., 2015) and can produce a shift in several bacterial species within 24 h (Wu et al., 2011). Also, antibiotics affect microbiota composition by depleting resident microbiota and subsequent enrichment of certain antibiotic-resistant strains, leading to pathogenic effects (Morgun et al., 2015). Other non-antibiotic drugs, such as proton-pump inhibitors, but also several psychiatric drugs, are known to have an extensive impact on the human gut microbiota (Maier et al., 2018).
FIGURE 1.
The effect of several factors during different stages of life on the gut microbiota composition and their association with depression via altering inflammatory responses.
Microbiota Dysbiosis in Depression
Depression is a debilitating neuropsychiatric disorder that involves persistent low mood and loss of interest that can be long-lasting or recurrent, substantially decreasing the quality of life (Wittchen et al., 2011; Lim et al., 2012; Murray et al., 2013; Whiteford et al., 2013). Symptoms usually are a reduced interest or pleasure in previously pleasurable activities, loss of sexual desire, changes in appetite, weight loss or gain, sleep disorders and motor retardation, along with recurrent thoughts of guilt and death (McCarter, 2008). It affects approximately 4.4% of the world’s population with an incidence rate above the rate of global population growth (Flux and Lowry, 2020). Despite the high prevalence rate of depression and the ongoing efforts to enhance the skills of healthcare providers, this mental disorder remains underdiagnosed and undertreated (Williams et al., 2017). The late diagnosis and treatment of depression are associated with a reduced treatment outcome, underscoring the importance of early intervention (Riedel et al., 2011).
The development of depression involves a complex interplay of biological, genetic, and environmental factors (Lopizzo et al., 2015). In addition to the strong association between gut microbiota and autism, schizophrenia and attention deficit hyperactivity disorder (for a review, see Eltokhi et al., 2020), accumulating shreds of evidence over the past 10 years support the hypothesis that gut microbiota may determine the initial risk and persistence of depression and contribute to treatment and resilience (for reviews, see Mangiola et al., 2016; Rogers et al., 2016; Flux and Lowry, 2020). The gut microbiota can signal to the CNS by way of neurohormones, vagal tonus, immune activation and metabolites that can alter eating behavior and mood (Martin et al., 2018). Moreover, healthy diets such as the Mediterranean one are suggested to reduce the risk of depression (Sanchez-Villegas et al., 2007; Skarupski et al., 2013; Pagliai et al., 2018; Konstantinos and Evangelia, 2019; Lassale et al., 2019) via modulation of the gut microbiota composition (De Filippis et al., 2016; Garcia-Mantrana et al., 2018; Krznaric et al., 2019; Nagpal et al., 2019). Confirming the role of gut microbiota in depression, a large epidemiological study revealed that the destabilization of the gut microbiota composition by antibiotics resulted in a 20–50% increased risk of depression (Lurie et al., 2015). Moreover, the underrepresentation of Firmicutes in the gut has been associated with depression (Huang et al., 2018), and 25.8% of individuals with inflammatory bowel disease (IBD) suffered from depression in the previous year (Lai and Cai, 2018).
Preclinical studies on rodents have investigated the link between gut microbiota and depression at a deeper level than clinical studies (Flux and Lowry, 2020). Studies mostly from the microbiota-devoid germ-free mice or mice treated with broad-spectrum antibiotics have shown that specific microbiota can impact brain physiology and behavior including deficiencies in learning, memory, recognition, and emotional behaviors (Gareau et al., 2011; Smith, 2015; Foster et al., 2017), accompanied by structural changes in the brain (Zhang et al., 2015; Principi and Esposito, 2016; Dinan and Cryan, 2017; Fung et al., 2017; Martin and Mayer, 2017). Different rodent models that showed high face validity to human depression have been used in microbiota research (Krishnan and Nestler, 2011). These models include olfactory bulbectomy (Harkin et al., 2003), social stress models (Toyoda, 2017), maternal separation (MS) models of early life adversity (Matthews and Robbins, 2003; Neumann et al., 2005; O’Mahony et al., 2009), repeated restraint stress models (Glavin et al., 1994; Bailey et al., 2010), chronic unpredictable mild stress (Duan et al., 2021; Zhang et al., 2021), and diet-induced obesity (Bruce-Keller et al., 2015; Bridgewater et al., 2017; Agusti et al., 2018; Soto et al., 2018) (for a review, see Flux and Lowry, 2020). The depression-like behaviors in rodents are measured by several behavioral experiments including forced swim, tail-suspension, sucrose preference, splash and learned helplessness tests (Eltokhi et al., 2018). Confirming the link between gut microbiota and depression, stressed germ-free mice showed high circulating levels of depression-sustaining hormones such as ACTH and corticosterone (Sudo et al., 2004). Moreover, the transplantation of fecal matter from depressed patients into microbiota-depleted rats exhibited depressive-like behavior in the rats (Kelly et al., 2016).
Clinical evidence for the role of the microbiota in depression is provided by an alteration in the number of microbiota and their diversity in individuals with depression when compared to healthy controls (for a summary, see Table 1). A study of fecal samples from patients with major depressive disorder (MDD) documented increased counts of Bacteroidales and decreased counts of Lachnospiraceae (Naseribafrouei et al., 2014). The analysis of fecal matters from MDD patients revealed a negative, albeit weak, correlation between the abundance of Faecalibacterium and the severity of the depressive symptoms (Jiang et al., 2015), and a positive correlation between Enterobacteriaceae and Alistipes counts and depression (Jiang et al., 2015). In another clinical study, lower Bifidobacterium and/or Lactobacillus counts were more common in patients with MDD compared to healthy controls (Aizawa et al., 2016). Two other studies revealed a different abundance of bacterial families and taxa between patients with MDD and healthy controls (Chen Z. et al., 2018; Chung et al., 2019). Moreover, in a Chinese MDD cohort, alterations of microbiota composition were found in MDD patients with an overrepresentation of Actinobacteria and underrepresentation of Bacteroidetes (Zheng et al., 2016). Investigating a group suffering from treatment-resistant MDD revealed a link between microbiota neuroactive capacity and the quality of life and depression (Valles-Colomer et al., 2019). Similar gut microbiota dysbiosis between Irritable bowel syndrome (IBS), depression, and IBS/depression co-morbid patients confirms the close link between the gut microbiota composition and depression (Liu et al., 2016). Although several previous studies demonstrated that depression was linked to marked alterations in gut microbiota composition, contradicting results regarding the enrichment of certain microbiota phyla in individuals with depression were obtained (Table 1). This inconsistency may have resulted from differences in study design, sample sizes, demographic and clinical severity of patients, unmeasured confounding factors and/or the used statistical methods. Additionally, most of these studies had several limitations including small sample sizes and a lack of data on the dietary habits of the tested subjects, which hinders obtaining a solid conclusion about the suitability of the microbiota as a biomarker of depression. It is still unsure whether changes in the microbiota are a cause or a result of depression. As depression is associated with changes in dietary habits, sleep and stress, the gut microbiota dysbiosis may well be a consequence rather than a cause. On the other hand, the depressive phenotype was shown to be transmissible by fecal microbiota transplantation (FMT) from MDD patients to germ-free rodents, revealing increased anxiety and depressive-like behavior in rodents (Kelly et al., 2016; Zheng et al., 2016). This strongly suggests that the alterations of the gut microbiota associated with depression may be a cause, rather than a consequence of the disorder.
TABLE 1.
Clinical studies investigating a correlation between the human fecal microbiota and depression.
| References | Sample | Sample size (patients/controls) | Mean age in years ± SD | Gender (males/females) | Changes in taxonomic composition in patients | Limitations/notes |
| Naseribafrouei et al., 2014 | Fecal sample | 55 Patients: 37 Controls: 18 | Patients: 49.2 ± 13.9 Controls: 46.1 ± 13.9 | Patients: (17/20) Controls: (7/11) | -High taxonomic level: ↑Bacteroidales ↓Lachnospiraceae -Low taxonomic level: ↑correlating OTUs of clades within the genus Alistipes and Oscillibacter |
- A lack of data on the dietary habits of subjects - A small cohort with a risk of overseeing effects |
| Jiang et al., 2015 | Fecal sample | 76 Active-MDD: 29 Responded-MDD: 17 Controls: 30 | Patients: Active-MDD: 25.3 ± 5.4 Responded-MDD: 27.1 ± 5.4 Controls: 26.8 ± 5.4 | Patients: Active-MDD: (18/11) Responded-MDD: (9/8) Controls: (15/15) | -High taxonomic level: ↑Bacteroidete ↑Proteobacteria ↑Actinobacteria ↓Firmicutes -Low taxonomic level: ↑Enterobacteriaceae ↑Alistipes ↓Faecalibacterium |
- A lack of data on the dietary habits of subjects - Possible effects of atypical antipsychotic medications - Further studies are required to evaluate the suitability of the microbiome as a biomarker. |
| Zheng et al., 2016 | Fecal sample | 121 Drug-naïve MDD: 39 Treated-MDD: 19 Controls: 63 | Patients: 40.6 ± 11.7 Controls: 41.8 ± 12.3 | Patients: (22/36) Controls: (23/40) | -High taxonomic level: ↑Actinobacteria ↓Bacteroidetes -Low taxonomic level: ↑OUTs assigned to the families Actinomycineae, Coriobacterineae, Lactobacillaceae, Streptococcaceae, Clostridiales incertae sedis XI (Parvimonas), Eubacteriaceae, Lachnospiraceae (Anaerostipes, Blautia, Dorea, Lachnospiracea incertae sedis), Ruminococcaceae (Clostridium IV) and Erysipelotrichaceae incertae sedis ↓OUTs assigned to the families Bacteroidaceae, Rikenellaceae (Alistipes), Lachnospiraceae (Coprococcus, Clostridium XlVa, Lachnospiraceae incertae sedis, Roseburia and Faecalibacterium), Acidaminococcaceae (Phascolarctobacterium), Veillonellaceae(Megamonas) and Sutterellaceae |
- No examination of other neuropsychiatric disorders with similar clinical presentations to MDD - A possibility of site-specific and ethnic biases in microbial phenotypes |
| Aizawa et al., 2016 | Fecal sample | 100 Patients: 43 Controls: 57 | Patients: 39.4 ± 10.0 Controls: 42.8 ± 12.7 | Patients: (25/18) Controls: (22/35) | ↓Bifidobacterium A tendency of ↓Lactobacillus |
- Investigating only Bifidobacterium and Lactobacillus -Possible effects of antidepressant medications - Effects of diet were not fully taken into account in the analysis. |
| Chen Z. et al., 2018 | Fecal sample | 20 Patients: 10 Controls: 10 | Patients: 43.9 ± 13.8 Controls: 39.6 ± 9.0 | Patients: (5/5) Controls: (5/5) | -High taxonomic level: ↑Firmicutes ↑Actinobacteria ↓Bacteroidetes ↓Proteobacteria -Low taxonomic level: ↑Lachnospiraceae ↑Actinomycetaceae ↑Nocardiaceae ↑Bifidobacteriaceae ↑Erysipelotrichaceae ↑Clostridiaceae ↑Ruminococcaceae ↑Porphyromonadaceae ↑Streptomycetaceae ↓Enterobacteriaceae ↓Sutterellaceae ↓Oscillospiraceae ↓Chitinophagaceae ↓Marinilabiliaceae ↓Rikenellaceae ↓Prevotellaceae |
- A limited sample size - No detailed data on diet habits, alcohol intake, or residence - Possible effects of antidepressant medications |
| Chung et al., 2019 | Fecal sample | 73 Patients: 36 Controls: 37 | Patients: 45.83 ± 14.08 Controls: 41.19 ± 12.73 | Patients: (8/28) Controls: (14/23) | -High taxonomic level: ↑Actinobacteria ↑Firmicutes ↓Bacteroidetes ↓Proteobacteria -Low taxonomic level: ↑Peptostreptococcaceae ↑Porphyromonadaceae ↑Streptococcaceae ↑Bifidobacteriaceae ↑Lachnospiraceae ↓Prevotellaceae ↓Alcaligenaceae |
- A cross-sectional study design with no causal inference between the microbiota alterations and depression - A moderate sample size that provided no stable results with cluster analysis to further discuss the impacts of dietary patterns on microbiota compositions - Possible effects of antidepressant medications -The dietary information was subjective to recall bias. |
↑indicates an increase; ↓ indicates a decrease; MDD, Major depressive disorder; OTUs, Operational Taxonomic Units.
Notably, several studies have shown that depression itself can affect the gut microbiota diversity via signals from the CNS to the gut environment, for example by changing secretion and motility in the stomach and gut. In an olfactory bulbectomy mouse model of depression, alteration of microbiota composition in the colon was suggested to be caused by increased activation of the stress response and alterations in colonic motility (Park et al., 2013). Moreover, diet disturbance in depression by the consumption of highly palatable foods is a major pathway from depression to gut microbiota dysbiosis (Rogers et al., 2016). Additionally, depression can reshape the gut microbiota composition by altering metabolic responses to food through hormones, inflammation, and autonomic alterations (Madison and Kiecolt-Glaser, 2019). For example, women suffering from depression had higher cortisol and fat oxidation levels (Kiecolt-Glaser et al., 2015), which can have a downstream effect on the gut microbiota (den Besten et al., 2013; Farzi et al., 2018). Other studies revealed that multiple classes of antidepressants also have anti-microbial properties against pathogenic bacteria (Macedo et al., 2017). For example, the antidepressant fluoxetine enriched the bacterial species associated with the regulation of BMI in mice (Lyte et al., 2019). The next-generation antidepressant ketamine plays a role in regulating the gut microbiota diversity (Yang et al., 2017) and showed increased Lactobacillus, Turicibacter, and Sarcina counts in the rat fecal microbiota and reduced opportunistic pathogens Mucispirillum and Ruminococcus (Getachew et al., 2018). To this end, the aforementioned studies suggest that the link between gut microbiota composition, antidepressants and depression is reciprocal.
The Effect of Gut Microbiota on Local and Circulating Inflammatory Markers and Its Relation to Depression
Depression has been associated with inflammation and its components such as inflammatory cytokines for more than 20 years (Ader and Cohen, 1985; Maes, 1995; Maes et al., 2012; Patel, 2013; Skaper et al., 2014; Miller and Raison, 2016; Leonard, 2018). Several gene variants are involved in both immune activation and depression (Barnes et al., 2017). Moreover, depression is known to be associated with polymorphisms in inflammation-related genes (Mikova et al., 2001; Kokai et al., 2002; Wong et al., 2008). Elevated levels of pro-inflammatory cytokines including Interleukin (IL)-1, IL-6, IL-8, and IL-12 were reported in individuals suffering from depression (Dowlati et al., 2010; Duivis et al., 2013; Lamers et al., 2013; Kim et al., 2016). Furthermore, IL-6, tumor necrosis factor-alpha (TNF-α), and IL-1β are implicated in the pathophysiology of depression (Brebner et al., 2000), and individuals with depression often have elevated circulating IL-1β, IL-6, and TNF with reduced levels of interferon-gamma (IFN-γ), IL-10, and IL-4 (Goldsmith et al., 2016). Longitudinal studies linked the high levels of pro-inflammatory cytokines with future risk for depression (van den Biggelaar et al., 2007; Gimeno et al., 2009). The pro-inflammatory cytokines have been connected to a pattern of sickness behaviors that include depressed mood, lethargy, heightened pain sensitivity, and sleep and appetite disturbances: all hallmarks of depression (Flux and Lowry, 2020). Moreover, non-specific inflammatory markers such as haptoglobin, fibrinogen, and C-reactive protein (CRP) are increased in depressed patients (Sluzewska et al., 1996).
Supporting the relationship between inflammation and depression, significant inflammatory activity in rodent models of depression has been identified (Song and Wang, 2011). Moreover, several antidepressants have been shown to reduce the endogenous production of pro-inflammatory cytokines along with a modification of immune reactivity in the CNS (Capuron et al., 2002; Nazimek et al., 2017; Gałecki et al., 2018). Tricyclic antidepressants inhibit the release of pro-inflammatory cytokines IL-6, IL-1β, and TNF-α (Xia et al., 1996). Additionally, the next-generation antidepressant ketamine has been shown to decrease depressive symptoms via a decrease in circulating IL-1β levels (Tan et al., 2017), a protein known to cause neuroinflammation and depressive behaviors (Dunn et al., 2005; Dunn, 2006; Swiergiel and Dunn, 2007; Ransohoff and Brown, 2012). Conversely, anti-inflammatory drugs have been shown to enhance recovery in patients with depression (Mendlewicz et al., 2006; Muller et al., 2006), and depressive symptoms are observed clinically with the administration of IFNs (Baranyi et al., 2013; Mahajan et al., 2014). IL-10 knockout mice displayed a decreased latency to immobility in a forced swim test as a measure of depression, which was rescued by the administration of IL-10 (Mesquita et al., 2008) that is known to inhibit pro-inflammatory cytokine production (Ledeboer et al., 2000). Recent evidence indicated that microbiota dysbiosis is associated with the development of several chronic inflammatory disorders such as IBD (Ni et al., 2017). Notably, several gut microbial taxa with differential abundance patterns common to immune-mediated inflammatory diseases were identified (Forbes et al., 2018). Several genera including Lactobacillus, Bifidobacterium, and Faecalibacterium have been shown to stimulate the anti-inflammatory cytokine including IL-10 (Sokol et al., 2008) and downregulate inflammatory cytokines (Llopis et al., 2009).
As the gut microbiota play a fundamental effect on the gut inflammatory and immune responses, it is highly likely that the role of gut microbiota dysbiosis in the pathophysiology of depression is induced by immune and inflammation responses (Slyepchenko et al., 2017). Evidence of increased bacterial translocation due to the disruption of tight junctions and barrier integrity of the GI tract has now surfaced in the pathogenesis of depression (Slyepchenko et al., 2017). The non-invasive bacterial translocation to the mesenteric lymph nodes, the lamina propria, and the peripheral blood results in immune activation and increased production of pro-inflammatory cytokines. Heightened IgA and IgM-mediated immune responses to lipopolysaccharide, a component of the cell walls of gram-negative bacteria, in MDD support the notion of increased gut microbiota translocation due to a leaky gut (Maes et al., 2008).
Evidence from rodent experiments confirms the link between microbiota and depression via inflammatory markers. Socially stressed mice showing increased fecal Oscillospira and a decreased fecal Firmicutes/Bacteroidetes ratio developed depression-like symptoms (Zhang et al., 2017). These symptoms were rescued via an intravenous treatment with an anti-mouse IL-6 receptor antibody (MR16-1) that significantly decreased Oscillospira counts and attenuated the decrease in the fecal Firmicutes/Bacteroidetes ratio (Zhang et al., 2017). Genetic deletion or pharmacological inhibition of Caspase-1 that cleaves IL-1β and IL-18 into their mature isoforms exhibited reduced depression- and anxiety-like behaviors in a chronic restraint stress model, combined with an increase in Akkermansia species that is associated with decreased inflammation and a rebalancing of the gut microbiota (Alcocer-Gomez et al., 2014; Anhe et al., 2015; Yang et al., 2015). Recent work has targeted the effects of the inflammasome in studying the relationship between the immune system, gut microbiota and depression (Inserra et al., 2018). It was hypothesized that the increased NLRP3 signaling due to stress/depression can lead to an overrepresentation of pro-inflammatory bacterial clades within the gut microbiota (Inserra et al., 2018). This pathological change in the gut microbiota composition may even strengthen the stress/depression phenotype and increase the risk of other NLRP3-related co-morbid disorders. Notably, several pieces of evidence have shown that the link between microbiota, inflammation and depression is indeed reciprocal (Figure 2). Microbiota dysbiosis in inflammatory diseases such as IBS can lead to depression (Tribbick et al., 2015; Liu et al., 2016). Conversely, repeated stress and/or depression increases pro-inflammatory signaling (Rohleder, 2014), leading to microbiota dysbiosis and increased representation of pro-inflammatory bacterial clades (Rogers et al., 2016; Wong et al., 2016; Zheng et al., 2016).
FIGURE 2.
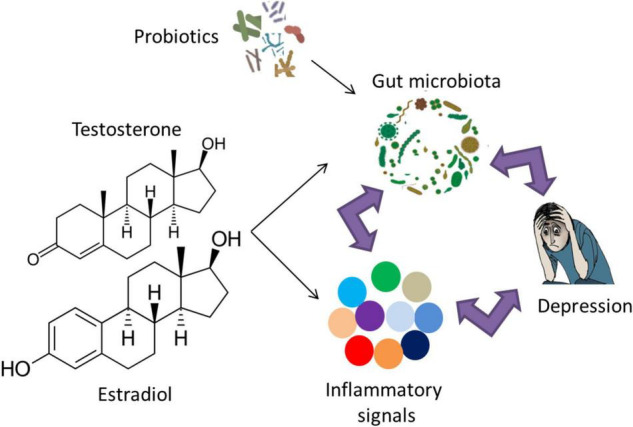
The reciprocal link between gut microbiota, inflammation and depression. The role of probiotic supplementation in turning the gut microbiota composition into a healthier form may lead to normal brain function and alleviation of depressive symptoms via modulation of inflammatory responses. Examples of probiotic genera include Lactobacillus, Bifidobacterium, Lactococcus, Propionibacterium, Bulgaricus, and Streptococcus. Notably, sex hormones affect gut microbiota and/or inflammatory signals, which may play a role in the sex bias of depression.
Influence of Sex Hormones on the Gut Microbiota Composition and Gender Bias in Depression
Depression is more frequent in women than men with a ratio of 2:1, which was reported globally and independent of race or ethnicity (Weissman and Klerman, 1977; Cyranowski et al., 2000; Andrade et al., 2003; Ford and Erlinger, 2004; Patten et al., 2006; Bromet et al., 2011; Salk et al., 2017). The finding of similar female: male prevalence ratios worldwide suggests that the differential risk is highly dependent on biological sex differences rather than race, culture or other potentially confounding social and economic factors (Albert, 2015). As the onset of depressive disorders in women peaks in their reproductive years, the increased prevalence of depression may be explained, in part, by sex hormones. Indeed, the female hormonal fluctuation during puberty, menstruation, pregnancy, and menopause is a trigger for depression (Albert, 2015). Estrogen and progesterone affect neurotransmitter, neuroendocrine, and circadian systems that have been implicated in mood disorders (Wharton et al., 2012). Androgens seem to have anxiolytic properties, whereas estrogen receptor activation has opposite consequences, with ERα having largely anxiogenic-like properties and ERβ serving to generate anxiolytic-like effects (Borrow and Handa, 2017). Furthermore, rates of depression in females correlate with the low levels of estrogen that occur throughout the life cycle (Albert et al., 2015). The risk of depression appears to increase during the perimenopausal transition (Cohen et al., 2006), with hormone replacement therapy being effective in the prevention of postmenopausal depression in women (Gordon and Girdler, 2014). In this light, a study has indicated that women who reported using an oral contraceptive showed reduced rates of MDD compared with non-users (Cheslack-Postava et al., 2015), suggesting a protective role of estrogen against depression. In contrast, other studies have shown depression and worsened mood as potential adverse effects of hormonal contraceptive use (Wiebe et al., 2011; Gingnell et al., 2013; Skovlund et al., 2016; de Wit et al., 2020). The heterogeneity in these findings may be explained by differences in study populations (de Wit et al., 2020).
Current evidence confirming the role of sex hormones on depression incidence relies mainly on rodent work. A recent study has explored the effect of treatment with a 5-α-reductase inhibitor that converts steroid hormones testosterone and progesterone into dihydrotestosterone and dihydroprogesterone, respectively on depression-like behavior in rats, as well as 1 month of treatment withdrawal (Diviccaro et al., 2019). The withdrawal from the 5-α-reductase inhibitor was associated with elevated depression-like symptoms, as measured by the forced swim test (Diviccaro et al., 2019). Interestingly, a change in sex hormone concentration is associated with an altered immune profile and a shift in inflammation responses (Figure 2; Kupelian et al., 2009; Casimir et al., 2010; Karim et al., 2010; Maggio et al., 2011; Bobjer et al., 2013; Park and Lee, 2020; Grandys et al., 2021) (for reviews, see Monteiro et al., 2014; Au et al., 2016; Mohamad et al., 2018; Slavich and Sacher, 2019). The alteration of inflammatory responses due to sex hormones suggests their combined role in the pathophysiology of depression.
Although gut microbiota differed in males and females, castrated male mice showed similar microbiota composition to females, suggesting an influence of androgens on the gut microbiota composition (Markle et al., 2013; Yurkovetskiy et al., 2013). Moreover, testosterone treatment after gonadectomy rescued the alteration in the gut microbiota composition that was observed in the untreated males (Org et al., 2016). Several studies have shown a direct effect of estrogen on the gut microbiota composition (Flores et al., 2012; Cox-York et al., 2015; Chen and Madak-Erdogan, 2016; Org et al., 2016). Treatment with a 5-α-reductase inhibitor was associated with increased Bacteroidetes and Prevotellaceae counts, and the withdrawal was associated with a reduction in the family Ruminococcaceae and the genera Oscillospira and Lachnospira (Diviccaro et al., 2019). Interestingly, there seems to be a reciprocal interaction between gut microbiota and sex hormones leading to a change in the level of sex hormones because of differences in gut microbiota (Markle et al., 2013) and that gut microbiota regulate the production and/or utilization of testosterone and cause a difference in metabolism (Colldén et al., 2019).
Several studies have addressed the effects of sex on the gut microbiota in humans, which is suggested to be mediated, at least in part, by a difference in sex hormones levels (Figure 2; Mueller et al., 2006; Li et al., 2008; Ding and Schloss, 2014; Dominianni et al., 2015; Haro et al., 2016; Singh and Manning, 2016; Borgo et al., 2018; Gao et al., 2018; Sinha et al., 2019; Takagi et al., 2019) (for a recent review, see Kim et al., 2020). The sex differences in the gut microbiota composition mediated by sex hormones may exert adverse inflammatory and psychological effects related to depression and other neuropsychiatric disorders (Yurkovetskiy et al., 2013). For instance, adult women have reduced Bacteroidetes counts in their gut compared to age-matched men (Dominianni et al., 2015). Interestingly, the low levels of Bacteroidetes were previously observed in the fecal microbiota from patients diagnosed with clinical depression (Naseribafrouei et al., 2014). A study in a Chinese cohort revealed increased Actinobacteria levels in female MDD patients compared to female controls but reduced Bacteroidetes levels in male MDD patients compared to male controls (Chen J. J. et al., 2018).
In summary, the sex differences in the gut microbiota composition due to the effect of sex hormones may play a role in the sex bias of depression.
Probiotics as an Adjunctive Therapeutic Option for Depression
Given the strong association between the gut microbiota and the pathophysiology of depression, modulation of the gut microbiota composition can be a promising method for ameliorating the behavioral symptoms related to depression along with other neuropsychiatric disorders (Larroya-Garcia et al., 2019). One way for maintaining a healthy gut microbiota composition is mediated by the supplementation of probiotics; the consumable microbes intended to promote a healthy microbiota and can provide a benefit to the host when administered in adequate amounts (Butel, 2014) (Figure 2). The main bacterial genera used as probiotics in preclinical and clinical studies are the Lactobacillus and Bifidobacterium genera (Genedi et al., 2019). Studies involving animal models demonstrated that probiotics improved cognition, mood, anxiety, and stress (Sudo et al., 2004; Desbonnet et al., 2010; Bravo et al., 2011; Ait-Belgnaoui et al., 2014; Smith et al., 2014; Mohle et al., 2016; Bruce-Keller et al., 2018; Chunchai et al., 2018; Hadizadeh et al., 2019). Probiotics have also been studied in non-psychiatric individuals, and initial work showed improvements in cognitive function (Marotta et al., 2019) along with reducing constipation in different populations (Chmielewska and Szajewska, 2010; Miller and Ouwehand, 2013; Dimidi et al., 2014). Probiotic supplementation showed an enhancement in sleep, autonomic balance, and bowel habits and reduced stress and cortisol levels in Japanese medical students (Nishida et al., 2017). Moreover, healthy women who drank a probiotic-containing fermented milk product for 1 month showed lower brain activation when exposed to emotional stimuli (Tillisch et al., 2013). In a randomized controlled trial in healthy individuals, multispecies probiotics were able to reduce cognitive reactivity toward sad moods via a reduction in rumination and aggressive thoughts (Steenbergen et al., 2015). The Lactobacillus helveticus and Bifidobacterium longum probiotic mix given to healthy individuals for 1 month alleviated psychological distress compared to a control group, similar to the results seen in rats (Messaoudi et al., 2011). Moreover, the healthy individuals in the bottom third on the depressed/elated dimension reported improved mood after drinking probiotic-containing milk for 3 weeks (Benton et al., 2007).
The desire for a more effective treatment and a prevention of depression seems perpetually at the top of the list in terms of global health concerns to reduce the burden of this condition. The idea of treating depression with probiotics roots back to 1910 when Dr. George Porter Phillips reported that a gelatin-whey formula comprised of lactic-acid-producing bacteria decreased depressive symptoms in melancholic adults (Phillips, 1910). Preclinical studies and clinical trials have increasingly investigated the roles of probiotics in the treatment of depressive-like behaviors. In rodents, there is considerable evidence suggesting the effect of probiotics in decreasing the depression-like behaviors. Lactobacillus rhamnosus administration reduced stress-induced anxiety- and depressive-like behaviors in mice (Bravo et al., 2011). Bifidobacterium longum improved the depressive-like phenotype during the tail suspension test in a mouse model of heightened anxiety (Savignac et al., 2014). Likewise, daily Lactobacillus helveticus NS8 treatment reduced anxiety- and depressive-like behavioral dysfunctions in adult specific-pathogen-free rats facing chronic restraint stress in comparison to a selective serotonin reuptake inhibitor (SSRI) treatment (Liang et al., 2015). In a chronic mild stress model of depression, mice receiving a three-strain probiotic blend, Lactobacillus helveticus, Lactobacillus plantarum, and Bifidobacterium longum, displayed improved depression-like behavioral responses accompanied by a reduced TNF-α and interferon (IFN)-γ levels (Li et al., 2018). In another study, the administration of Faecalibacterium prausnitzii via oral gavage for 4 weeks in a chronic unpredictable mild stress model in rats resulted in decreased depression-like behaviors accompanied by increased IL-10 and decreased IL-6 and CRP levels (Hao et al., 2019). In another study, an administration of a probiotic formulation containing Lactobacillus plantarum, Lactobacillus rhamnosus, Bifidobacterium lactis, Bifidobacterium breve, and Pediococcus pentosaceus alleviated depressive-like behaviors in mice and decreased corticosterone level by restoring the gut microbiota composition (Liu et al., 2020). In Fischer and Long Evans rats subjected to maternal deprivation, a probiotic mixture composed of Lactobacillus helveticus, Bifidobacterium longum, Lactococcus lactis, and Streptococcus thermophilus reduced anxiety- and depression-like behaviors accompanied by a change in the levels of certain metabolites (Daugé et al., 2020).
Clinical studies revealed contradicting results regarding the efficiency of probiotics in decreasing depressive symptoms (for a summary, see Table 2). In an 8-week, randomized, double-blind, placebo-controlled clinical trial, a triple-strain probiotic mix, Lactobacillus acidophilus, Lactobacillus casei, and Bifidobacterium bifidum, resulted in improvements in depression scores in BDI in an MDD cohort (Akkasheh et al., 2016). Additionally, other beneficial metabolic effects were revealed including a significant reduction in inflammatory markers such as serum insulin, homeostasis model assessment of insulin resistance and serum hs-CRP (Akkasheh et al., 2016). Another 8-week, randomized, double-blind, placebo-controlled clinical trial examining the effect of a probiotic mix of Lactobacillus helveticus and Bifidobacterium longum on mild to moderate MDD reported a decrease in depression score in BDI (Kazemi et al., 2019). Interestingly, a randomized, placebo-controlled, double-blind study reported that daily Lactobacillus rhamnosus during pregnancy and into the post-partum period significantly decreased postnatal anxiety and depression scores (Slykerman et al., 2017). Another study testing the add-on effect of probiotic and prebiotic, the non-digestible plant-based carbohydrates that serve as nutrition for resident bacteria, on fluoxetine revealed a decrease in the score of hamilton rating scale for depression (HAM-D) compared to the placebo after 6 weeks of treatment (Ghorbani et al., 2018). One study provided petrochemical workers with either a probiotic capsule, probiotic yogurt, or conventional yogurt control, with both probiotic conditions resulting in a reduction of depressive symptoms on the general health questionnaire (GHQ) and depression anxiety and stress scale (DASS) scores as compared to control (Mohammadi et al., 2016). In another study, the efficacy of Bacillus coagulans administration on MDD in IBS patients was tested and revealed an improvement in HAM-D, Montgomery-Asberg Depression Rating Scale (MADRS), Center for Epidemiological Studies Depression Scale (CES-D) as well as reduced serum myeloperoxidase, an inflammatory biomarker (Majeed et al., 2018). In a recent open-label pilot study, a probiotic supplement containing Lactobacillus helveticus and Bifidobacterium longum administrated once per day for 8 weeks showed an improvement in affective clinical symptoms after 4 weeks, which was sustained till the end of the study (Wallace and Milev, 2021).
TABLE 2.
Clinical trials on probiotic supplementation in individuals with depression.
| References | Sample size (INT/PL) | Mean age in years ± SD | Gender (males/females) | Study compound and duration | A change in INT group | Limitations/notes |
| Akkasheh et al., 2016 | MDD: 40 INT: 20 PL: 20 |
INT: 38.30 ± 12.10 PL: 36.20 ± 8.20 |
INT: (3/17) PL: (3/17) |
- The study was performed for 8 weeks. - INT received probiotic capsules daily and consisted of Lactobacillus acidophilus (2 × 109 CFU/g), Lactobacillus casei (2 × 109 CFU/g), and Bifidobacterium bifidum (2 × 109 CFU/g). - PL received capsules containing starch but no bacteria. |
- ↓ BDI - ↓Serum insulin levels, homeostasis model assessment of insulin resistance, and serum hs-CRP concentrations - ↑Plasma total glutathione levels - No change in fasting plasma glucose, homeostatic model assessment of beta-cell function, quantitative insulin sensitivity check index, lipid profiles, or total antioxidant capacity levels |
- No analysis of other biomarkers of inflammation or oxidative stress - A short intervention - Not knowing which strain in the probiotic supplements caused the treatment effect |
| Mohammadi et al., 2016 | petrochemical workers: 70 INT 1: 25 INT 2: 25 PL: 20 |
INT 1: 33.20 ± 6.40 INT 2: 31.50 ± 5.80 PL: 33.10 ± 6.10 |
INT 1: (12/13) INT 2: (12/13) PL: (12/8) |
- The study was performed for 6 weeks. - INT 1 received 100 g/day probiotic yogurt (Lactobacillus acidophilus LA5 and Bifidobacterium lactis BB12 with a total of min 1 × 107 CFU) + one placebo capsule. - INT 2 received one probiotic capsule daily (Lactobacillus casei 3 × 103, Lactobacillus acidophilus 3 × 107, Lactobacillus rhamnosus 7 × 109, Lactobacillus bulgaricus 5 × 108, Bifidobacterium breve 2 × 1010, Bifidobacterium longum 1 × 109, Streptococcus thermophilus 3 × 108 CFU/g and 100 mg fructo-oligosaccharide with lactose as carrier substances) + 100 g/day conventional yogurt. - PL received 100 g/day conventional yogurt (Streptococcus thermophilus and Lactobacillus bulgaricus) + one placebo capsule (the same substance without bacteria). |
- ↑GHQ in INT 1 and INT 2 - ↓DASS scores in INT 1 and INT 2 - No change of GHQ or DASS scores in PL |
- A short intervention -No assessment of the rate that short-chain fatty acids were produced by probiotics in the gut |
| Slykerman et al., 2017 | Pregnant women of 14–16 weeks gestation: 423 INT: 212 PL: 211 |
INT: 33.50 ± 4.24 PL: 33.70 ± 4.44 |
Only females | - The study was performed until 6 months postpartum if breastfeeding. -INT received a daily Lacticaseibacillus rhamnosus HN001 at a dose of 6 × 109 CFU. -PL received a daily placebo (corn-derived maltodextrin). |
- ↓Depression and anxiety scores in EPDS and STAI6 - ↓Clinically relevant anxiety on screening |
- The EPDS and STAI6 are screening tools for postnatal depression and anxiety, but not diagnostic. -The information was collected retrospectively, and neither the EPDS nor the STAI6 has been validated using the questions phrased in the past tense. |
| Ghorbani et al., 2018 | Individuals with moderate depression: 40 INT: 20 PL: 20 |
INT: 34.45 ± 3.95 PL: 35.50 ± 5.27 |
INT: (6/14) PL: (6/14) |
- All Patients received fluoxetine (20 mg/d) for 4 weeks before and throughout the whole study. - The study was performed for 6 weeks. - INT received 2 capsules daily containing 500 mg probiotics (Lactobacillus casei 3 × 108 CFU/g, Lactobacillus acidophilus 2 × 108 CFU/g, Lactobacillus bulgaricus 2 × 109 CFU/g, Lactobacillus rhamnosus 3 × 108 CFU/g, Bifidobacterium breve 2 × 108 CFU/g, Bifidobacterium longum, 1 × 109 CFU/g, Streptococcus thermophilus 3 × 108 CFU/g) and 100 mg fructooligosaccharide as prebiotic. - PL received 2 placebo capsules daily containing 1,000 mg magnesium stearate. |
- ↓HAM-D score at the endpoint of the intervention | - A short period of follow-up - A small number of participants |
| Majeed et al., 2018 | MDD: 40 INT: 20 PL: 20 |
INT: 40.36 ± 10.28 PL: 43.88 ± 9.85 |
INT: (3/17) PL: (3/17) |
- The study was performed for 90 days. - INT received a daily dose of 2 × 109 CFU Bacillus coagulans MTCC 5856 (600 mg) that contained also, microcrystalline cellulose, starch, sodium starch glycolate and magnesium stearate. -PL received placebo tablets that had the same ingredients except for Bacillus coagulans MTCC 5856. |
- ↓HAM-D, MADRS, CES-D, IBS-QOL in INT - ↓CGI-I, CGI-S, Dementia – TFS, GI-DQ, mESS in INT - ↓ Serum myeloperoxidase in INT but not PL |
- A short period of follow-up - A small number of participants |
| Kazemi et al., 2019 | MDD: 110 INT 1: 38 INT 2: 36 PL: 36 |
INT 1: 36.15 ± 7.85 INT 2: 37.35 ± 7.97 PL: 36.00 ± 8.47 |
INT 1: (11/27) INT 2: (9/27) PL: (12/24) |
- The study was performed for 8 weeks. - INT 1 received probiotic product consisting of freeze-dried Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 (CNCM strain I-3470) bacteria (10 × 109 CFU) per 5 g sachet + xylitol, maltodextrin, plum flavor and malic acid - INT 2 received a prebiotic product consisting of galactooligosaccharide and 0.2% Plum flavor - PL received a product consisting of xylitol, maltodextrin, plum flavor and malic acid. |
- ↓BDI score in INT 1 compared to PL - ↓Kynurenine/tryptophan ratio compared to PL - ↑Tryptophan/isoleucine ratio compared to PL - No change of BDI score in INT 2 compared to PL - ↓Tryptophan/BCAAs ratio in INT 2 compared to PL |
- 10 subjects from INT 1, 9 from INT 2 and 10 from PL dropped out before the trial completion - A lack of fecal microbiome analysis - The intervention was conducted at different times of the year - No control of changes in lifestyle, diet, vitamin D status, etc. - Different used antidepressant drugs |
| Wallace and Milev, 2021 | MDD: 10 INT: 10 |
INT: 25.20 ± 7.00 | INT: (3/7) | - The study was performed for 8 weeks. - INT received a probiotic supplement containing Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 at a dose of 3 × 109 CFU once per day. |
- ↓MADRS, QIDS-SR16 and SHAPS scores - ↓GAD-7 and STAI scores - ↑Sleep quality measured by PSQI |
-A small number of participants - An open-label design and lack of placebo - A reduced generalizability of the results - The sample was disproportionately skewed toward young adult females. |
| Östlund-Lagerström et al., 2016 | General older adults: 249 INT: 125 PL: 124 |
INT: 72.60 ± 5.80 PL: 72.00 ± 5.60 |
INT: (54/71) PL: (43/81) |
-The study was performed for 12 weeks. -INT received a product consisting of a stick-pack containing freeze-dried Lactobacillus reuteri DSM 17938 (1 × 108 CFU/stick-pack), rhamnose, galactooligosaccharide and maltodextrin to a total weight of 1 g. -PL received a product consisting of maltodextrin. |
- No change in GSRS, depression or anxiety scores - No change in the stress level (PSS scores) - No change in EQ-VAS or EQ-5D-index scores assessing the quality of life - No change in stool frequency |
- A possibility that participants suffering from IBS were included in the study - An additional more fine-tuned instrument such as the ROME III symptom criteria, might have increased the sensitivity - The use of a low dose of Lactobacillus reuteri - The study was underpowered. |
| Romijn et al., 2017 | Individuals with low mood: 79 INT: 40 PL: 39 |
INT: 35.80 ± 14.00 PL: 35.10 ± 14.50 |
INT: (8/32) PL: (9/30) |
- The study was performed for 8 weeks. -INT received a product consisting of freeze-dried Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 bacteria at a dosage of 3 × 109 CFU per 1.5 g sachet + xylitol, maltodextrin, plum flavor and malic acid. -PL received a product consisting of xylitol, maltodextrin, plum flavor and malic acid. |
- No change in MADRS, CGI-S, CGI-I, QIDS-SR16, GAF, DASS - No difference in biomarker levels |
- No measurement of BMI, body fat, dietary intake and physical activity -A lack of intestinal microbiome analysis -A small sample size - A short length of the intervention period |
| Rudzki et al., 2019 | MDD: 60 INT: 30 PL: 30 |
INT: 39.13 ± 9.96 PL: 38.90 ± 12.00 |
INT: (7/23) PL: (10/20) |
- The study was performed for 8 weeks. -Both INT and PL received SSRI treatment during the whole study. - INT received 2 capsules daily with each containing 10 × 109 CFU of probiotic bacteria Lactobacillus Plantarum 299v. - PL received 2 capsules daily containing crystalline cellulose powder. |
- No change in HAM-D 17, SCL-90 or PSS - Improvement of work speed in APT - Improvement of CVLT total recall -↓Kynurenine concentration -↑3HKYN:KYN ratio |
-A small sample size - No measurements of intestinal permeability - No measurement of QUIN or vitamin B levels |
| Reininghaus et al., 2020 | Inpatient MDD: 61 INT: 28 PL: 33 |
INT: 43.00 ± 14.31 PL: 40.11 ± 11.45 |
INT: (8/20) PL: (6/27) |
- The study was performed for 4 weeks. -INT and PL received 125 mg D-Biotin. -INT received probiotics containing Bifidobacterium bifidum W23, Bifidobacterium lactis W51, Bifidobacterium lactis W52, Lactobacillus acidophilus W22, Lacticaseibacillus casei W56, Lacticaseibacillus paracasei W20, Lactiplantibacillus plantarum W62, Lactobacillus salivarius W24 and Lactococcus lactis W19 + 30 mg of common horsetail, 30 mg of fish collagen and 30 mg of keratin plus matrix -PL received a product containing 30 mg of common horsetail, 30 mg of fish collagen and 30 mg of keratin plus matrix. |
- No difference between INT and PL in any of the psychiatric scales - No difference in intestinal barrier function -↑Ruminococcus gauvreauii in INT -↑Taxonomically related Coprococcus |
- A short length of the intervention Period -The strong decrease in depression in both groups may have masked the difference between them - Changes in nutritional habits might have influenced the results. -A difference at baseline for smoking status between both groups - The high number of females may have skewed the results. |
The clinical studies of Östlund-Lagerström et al. (2016), Romijn et al. (2017), Rudzki et al. (2019), Reininghaus et al. (2020) did not reveal a significant improvement in the depression phenotype. INT, Intervention; PL, Placebo; CFU, Colony-forming units, SSRI, Selective serotonin reuptake inhibitor; BDI, Beck Depression Inventory; GHQ, General health questionnaire; DASS, Depression anxiety and stress scale; EPDS, Edinburgh Postnatal Depression Scale; STAI6, State Trait Anxiety Inventory 6 item version; HAM-D, Hamilton rating scale for depression; MADRS, Montgomery–Asberg Depression Rating Scale; CES-D, Center for Epidemiological Studies Depression Scale; IBS-QOL, Irritable Bowel Syndrome Quality of Life Questionnaire; CGI-I, Clinical Global Impression-Improvement rating Scale; CGI-S, Clinical Global Impression Severity Rating Scale; Dementia – TFS, Dementia – Total frequency scoring; GI-DQ, Gastrointestinal Discomfort Questionnaire; mESS, Modified Epworth Sleepiness Scale; QIDS-SR16, Quick Inventory of Depressive Symptomatology; SHAPS, Snaith-Hamilton Pleasure Scale; GAD-7, Generalized Anxiety Disorder 7-item scale; STAI, State Trait Anxiety Inventory; PSQI, Pittsburgh Sleep Quality Index; GSRS, Gastrointestinal symptoms rating scale; PSS, Perceived stress scale; GAF, Global Assessment of Functioning; SCL-90, Symptom Checklist; APT, Attention and Perceptivity Test; CVLT, California Verbal Learning Test.
Other studies in the literature failed to show any improvement of depression scores in MADRS following 8 weeks of primary treatment with probiotics mix of Lactobacillus helveticus and Bifidobacterium longum (Romijn et al., 2017). Moreover, there was no change in psychological symptoms and the concentrations of CRP, IL-1β, IL-6, or TNF between baseline and the end of the study (Romijn et al., 2017). Worth notice is that individuals in this study were not taking any antidepressant medication at the time of the study, and their depressive history was entirely self-reported without a formal diagnostic interview (Romijn et al., 2017). In another study of individuals diagnosed with MDD, SSRI treatment supplemented with Lactobacillus plantarum did not exhibit any improvement in depressive symptoms and did not change the levels of circulating TNF, IL-6, or IL-1β, although there was an increase in cognitive functioning (Rudzki et al., 2019). In another study, the health properties of Lactobacillus reuteri DSM17938 were investigated in individuals older than 65 and revealed no improvement in digestive health, general wellbeing, stress, anxiety, or depression (Östlund-Lagerström et al., 2016). In a randomized clinical study in 2020, a combination of 9 bacterial species Bifidobacterium bifidum W23, Bifidobacterium lactis W51, Bifidobacterium lactis W52, Lactobacillus acidophilus W22, Lactobacillus casei W56, Lactobacillus paracasei W20, Lactobacillus plantarum W62, Lactobacillus salivarius W24, and Lactobacillus lactis W19 in addition to biotin yielded no improvement in psychiatric symptoms in patients with MDD (Reininghaus et al., 2020).
Conclusion
Gut microbiota were incorporated into neurobiological models of depression via an effect on immune, endocrine, and nervous system responses, allowing a more comprehensive model of depression (Figure 2). The strong association between microbiota dysbiosis and depression could pave the way for enhancing diagnostic accuracy and patient phenotyping for treatment selection. Moreover, it can advance the treatment and prevention of depression by modifying the gut microbiota composition and offer an important future strategy in psychiatry via nutritional interventions, prebiotic or probiotic supplementations. Although preclinical mechanistic experimental data indicated that the manipulation of the gut microbiota with probiotics may have antidepressant and anxiolytic effects, there is limited clinical evidence for the efficacy of probiotics in depression at present. Notably, several probiotic studies that failed to show an improvement in depression revealed also no change in pro-inflammatory markers. Given the reciprocal link between microbiota, inflammation and depression discussed in this review, we believe that probiotics may partially exert their roles through a modification of the immune system. Generally, additional randomized clinical trials in patients with depression are necessary to fully evaluate their therapeutic potential on the clinical diagnosis and inflammatory biomarkers. Different factors should be kept into consideration to maximize the benefit of probiotic supplementation. The microbial diversity obtained by incorporating multiple strains of organisms is suggested to be more effective than using a single organism. Investigations at a finer taxonomic level coupled with multi-omic techniques such as transcriptomics, proteomics, and metabolomics are also needed to exclude confounding factors as much as possible. Since sex hormones can affect the inflammation biomarkers, with probiotics causing different inflammatory responses in female and male mice (Karunasena et al., 2014; Lee et al., 2017), sex should be taken into account in studies on gut microbiota, probiotics and depression.
Author Contributions
AE conceptualized and wrote the first draft. IES edited and reviewed the final draft. Both authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
AE sincerely appreciates the continuous support from Shaimaa Madbouly and Rolf Sprengel.
Funding
AE is partially supported by a postdoc stipend from the Fritz Thyssen Foundation. IES has received funding from the Stanley Medical Foundation.
References
- Ader R., Cohen N. (1985). High time for psychoimmunology. Nature 315 103–104. 10.1038/315103b0 [DOI] [PubMed] [Google Scholar]
- Agusti A., Moya-Pérez A., Campillo I., Montserrat-De, La Paz S., Cerrudo V., et al. (2018). Bifidobacterium pseudocatenulatum CECT 7765 ameliorates neuroendocrine alterations associated with an exaggerated stress response and anhedonia in obese mice. Mol. Neurobiol. 55 5337–5352. 10.1007/s12035-017-0768-z [DOI] [PubMed] [Google Scholar]
- Ait-Belgnaoui A., Colom A., Braniste V., Ramalho L., Marrot A., Cartier C., et al. (2014). Probiotic gut effect prevents the chronic psychological stress-induced brain activity abnormality in mice. Neurogastroenterol. Motil. 26 510–520. 10.1111/nmo.12295 [DOI] [PubMed] [Google Scholar]
- Aizawa E., Tsuji H., Asahara T., Takahashi T., Teraishi T., Yoshida S., et al. (2016). Possible association of Bifidobacterium and Lactobacillus in the gut microbiota of patients with major depressive disorder. J. Affect. Disord. 202 254–257. 10.1016/j.jad.2016.05.038 [DOI] [PubMed] [Google Scholar]
- Akagawa S., Tsuji S., Onuma C., Akagawa Y., Yamaguchi T., Yamagishi M., et al. (2019). Effect of delivery mode and nutrition on gut microbiota in neonates. Ann. Nutr. Metab. 74 132–139. 10.1159/000496427 [DOI] [PubMed] [Google Scholar]
- Akkasheh G., Kashani-Poor Z., Tajabadi-Ebrahimi M., Jafari P., Akbari H., Taghizadeh M., et al. (2016). Clinical and metabolic response to probiotic administration in patients with major depressive disorder: a randomized, double-blind, placebo-controlled trial. Nutrition 32 315–320. 10.1016/j.nut.2015.09.003 [DOI] [PubMed] [Google Scholar]
- Albert K., Pruessner J., Newhouse P. (2015). Estradiol levels modulate brain activity and negative responses to psychosocial stress across the menstrual cycle. Psychoneuroendocrinology 59 14–24. 10.1016/j.psyneuen.2015.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albert P. R. (2015). Why is depression more prevalent in women? J. Psychiatry Neurosci. 40 219–221. 10.1503/jpn.150205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcocer-Gomez E., De Miguel M., Casas-Barquero N., Nunez-Vasco J., Sanchez-Alcazar J. A., Fernandez-Rodriguez A., et al. (2014). NLRP3 inflammasome is activated in mononuclear blood cells from patients with major depressive disorder. Brain Behav. Immun. 36 111–117. 10.1016/j.bbi.2013.10.017 [DOI] [PubMed] [Google Scholar]
- Aleman F. D. D., Valenzano D. R. (2019). Microbiome evolution during host aging. PLoS Pathog. 15:e1007727. 10.1371/journal.ppat.1007727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade L., Caraveo-Anduaga J. J., Berglund P., Bijl R. V., De Graaf R., Vollebergh W., et al. (2003). The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int. J. Methods Psychiatr. Res. 12 3–21. 10.1002/mpr.138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anhe F. F., Roy D., Pilon G., Dudonne S., Matamoros S., Varin T. V., et al. (2015). A polyphenol-rich cranberry extract protects from diet-induced obesity, insulin resistance and intestinal inflammation in association with increased Akkermansia spp. population in the gut microbiota of mice. Gut 64 872–883. 10.1136/gutjnl-2014-307142 [DOI] [PubMed] [Google Scholar]
- Au A., Feher A., Mcphee L., Jessa A., Oh S., Einstein G. (2016). Estrogens, inflammation and cognition. Front. Neuroendocrinol. 40 87–100. 10.1016/j.yfrne.2016.01.002 [DOI] [PubMed] [Google Scholar]
- Bai J., Hu Y., Bruner D. W. (2019). Composition of gut microbiota and its association with body mass index and lifestyle factors in a cohort of 7-18 years old children from the American Gut Project. Pediatr. Obes. 14:e12480. 10.1111/ijpo.12480 [DOI] [PubMed] [Google Scholar]
- Bailey M. T., Dowd S. E., Parry N. M. A., Galley J. D., Schauer D. B., Lyte M. (2010). Stressor exposure disrupts commensal microbial populations in the intestines and leads to increased colonization by Citrobacter rodentium. Infect. Immun. 78 1509–1519. 10.1128/IAI.00862-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baranyi A., Meinitzer A., Stepan A., Putz-Bankuti C., Breitenecker R. J., Stauber R., et al. (2013). A biopsychosocial model of interferon-alpha-induced depression in patients with chronic hepatitis C infection. Psychother. Psychosom. 82 332–340. 10.1159/000348587 [DOI] [PubMed] [Google Scholar]
- Barnes J., Mondelli V., Pariante C. M. (2017). Genetic contributions of inflammation to depression. Neuropsychopharmacology 42 81–98. 10.1038/npp.2016.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumler A. J., Sperandio V. (2016). Interactions between the microbiota and pathogenic bacteria in the gut. Nature 535 85–93. 10.1038/nature18849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benton D., Williams C., Brown A. (2007). Impact of consuming a milk drink containing a probiotic on mood and cognition. Eur. J. Clin. Nutr. 61 355–361. 10.1038/sj.ejcn.1602546 [DOI] [PubMed] [Google Scholar]
- Bobjer J., Katrinaki M., Tsatsanis C., Lundberg Giwercman Y., Giwercman A. (2013). Negative association between testosterone concentration and inflammatory markers in young men: a nested cross-sectional study. PLoS One 8:e61466. 10.1371/journal.pone.0061466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgo F., Garbossa S., Riva A., Severgnini M., Luigiano C., Benetti A., et al. (2018). Body mass index and sex affect diverse microbial niches within the gut. Front. Microbiol. 9:213. 10.3389/fmicb.2018.00213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrow A. P., Handa R. J. (2017). Estrogen receptors modulation of anxiety-like behavior. Vitam. Horm. 103 27–52. 10.1016/bs.vh.2016.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo J. A., Forsythe P., Chew M. V., Escaravage E., Savignac H. M., Dinan T. G., et al. (2011). Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc. Natl. Acad. Sci. U.S.A. 108 16050. 10.1073/pnas.1102999108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brebner K., Hayley S., Zacharko R., Merali Z., Anisman H. (2000). Synergistic effects of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha: central monoamine, corticosterone, and behavioral variations. Neuropsychopharmacology 22 566–580. 10.1016/S0893-133X(99)00166-9 [DOI] [PubMed] [Google Scholar]
- Bridgewater L. C., Zhang C., Wu Y., Hu W., Zhang Q., Wang J., et al. (2017). Gender-based differences in host behavior and gut microbiota composition in response to high fat diet and stress in a mouse model. Sci. Rep. 7:10776. 10.1038/s41598-017-11069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromet E., Andrade L. H., Hwang I., Sampson N. A., Alonso J., De Girolamo G., et al. (2011). Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 9:90. 10.1186/1741-7015-9-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce-Keller A. J., Salbaum J. M., Berthoud H. R. (2018). Harnessing gut microbes for mental health: getting from here to there. Biol. Psychiatry 83 214–223. 10.1016/j.biopsych.2017.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce-Keller A. J., Salbaum J. M., Luo M., Blanchard E. I. V., Taylor C. M., Welsh D. A., et al. (2015). Obese-type gut microbiota induce neurobehavioral changes in the absence of obesity. Biol. Psychiatry 77 607–615. 10.1016/j.biopsych.2014.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butel M. J. (2014). Probiotics, gut microbiota and health. Med. Mal. Infect. 44 1–8. 10.1016/j.medmal.2013.10.002 [DOI] [PubMed] [Google Scholar]
- Cameron E. A., Sperandio V. (2015). Frenemies: signaling and nutritional integration in pathogen-microbiota-host interactions. Cell Host Microbe 18 275–284. 10.1016/j.chom.2015.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capuron L., Hauser P., Hinze-Selch D., Miller A. H., Neveu P. J. (2002). Treatment of cytokine-induced depression. Brain Behav. Immun. 16 575–580. 10.1016/s0889-1591(02)00007-7 [DOI] [PubMed] [Google Scholar]
- Carmody R. N., Gerber G. K., Luevano J. M., Gatti D. M., Somes L., Svenson K. L., et al. (2015). Diet dominates host genotype in shaping the murine gut microbiota. Cell Host Microbe 17 72–84. 10.1016/j.chom.2014.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casimir G. J., Mulier S., Hanssens L., Zylberberg K., Duchateau J. (2010). Gender differences in inflammatory markers in children. Shock 33 258–262. 10.1097/SHK.0b013e3181b2b36b [DOI] [PubMed] [Google Scholar]
- Chen Z., Li J., Gui S., Zhou C., Chen J., Yang C., et al. (2018). Comparative metaproteomics analysis shows altered fecal microbiota signatures in patients with major depressive disorder. Neuroreport 29 417–425. 10.1097/WNR.0000000000000985 [DOI] [PubMed] [Google Scholar]
- Chen J. J., Zheng P., Liu Y. Y., Zhong X. G., Wang H. Y., Guo Y. J., et al. (2018). Sex differences in gut microbiota in patients with major depressive disorder. Neuropsychiatr. Dis. Treat. 14 647–655. 10.2147/NDT.S159322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K. L., Madak-Erdogan Z. (2016). Estrogen and microbiota crosstalk: Should we pay attention? Trends Endocrinol. Metab. 27 752–755. 10.1016/j.tem.2016.08.001 [DOI] [PubMed] [Google Scholar]
- Cheslack-Postava K., Keyes K. M., Lowe S. R., Koenen K. C. (2015). Oral contraceptive use and psychiatric disorders in a nationally representative sample of women. Arch. Womens Ment. Health 18 103–111. 10.1007/s00737-014-0453-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmielewska A., Szajewska H. (2010). Systematic review of randomised controlled trials: probiotics for functional constipation. World J. Gastroenterol. 16 69–75. 10.3748/wjg.v16.i1.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chunchai T., Thunapong W., Yasom S., Wanchai K., Eaimworawuthikul S., Metzler G., et al. (2018). Decreased microglial activation through gut-brain axis by prebiotics, probiotics, or synbiotics effectively restored cognitive function in obese-insulin resistant rats. J. Neuroinflammation 15:11. 10.1186/s12974-018-1055-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung Y. E., Chen H. C., Chou H. L., Chen I. M., Lee M. S., Chuang L. C., et al. (2019). Exploration of microbiota targets for major depressive disorder and mood related traits. J. Psychiatr. Res. 111 74–82. 10.1016/j.jpsychires.2019.01.016 [DOI] [PubMed] [Google Scholar]
- Cohen L. S., Soares C. N., Vitonis A. F., Otto M. W., Harlow B. L. (2006). Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch. Gen. Psychiatry 63 385–390. 10.1001/archpsyc.63.4.385 [DOI] [PubMed] [Google Scholar]
- Colldén H., Landin A., Wallenius V., Elebring E., Fändriks L., Nilsson M. E., et al. (2019). The gut microbiota is a major regulator of androgen metabolism in intestinal contents. Am. J. Physiol. Endocrinol. Metab. 317 E1182–E1192. 10.1152/ajpendo.00338.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox-York K. A., Sheflin A. M., Foster M. T., Gentile C. L., Kahl A., Koch L. G., et al. (2015). Ovariectomy results in differential shifts in gut microbiota in low versus high aerobic capacity rats. Physiol. Rep. 3:e12488. 10.14814/phy2.12488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranowski J. M., Frank E., Young E., Shear M. K. (2000). Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch. Gen. Psychiatry 57 21–27. 10.1001/archpsyc.57.1.21 [DOI] [PubMed] [Google Scholar]
- Daugé V., Philippe C., Mariadassou M., Rué O., Martin J.-C., Rossignol M.-N., et al. (2020). A probiotic mixture induces anxiolytic- and antidepressive-like effects in fischer and maternally deprived long evans rats. Front. Behav. Neurosci. 14:581296. 10.3389/fnbeh.2020.581296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- David L. A., Maurice C. F., Carmody R. N., Gootenberg D. B., Button J. E., Wolfe B. E., et al. (2014). Diet rapidly and reproducibly alters the human gut microbiome. Nature 505 559–563. 10.1038/nature12820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Filippis F., Pellegrini N., Vannini L., Jeffery I. B., La Storia A., Laghi L., et al. (2016). High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut 65 1812–1821. 10.1136/gutjnl-2015-309957 [DOI] [PubMed] [Google Scholar]
- de Wit A. E., Booij S. H., Giltay E. J., Joffe H., Schoevers R. A., Oldehinkel A. J. (2020). Association of use of oral contraceptives with depressive symptoms among adolescents and young women. JAMA Psychiatry 77 52–59. 10.1001/jamapsychiatry.2019.2838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Besten G., Van Eunen K., Groen A. K., Venema K., Reijngoud D. J., Bakker B. M. (2013). The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J. Lipid Res. 54 2325–2340. 10.1194/jlr.R036012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desbonnet L., Garrett L., Clarke G., Kiely B., Cryan J. F., Dinan T. G. (2010). Effects of the probiotic Bifidobacterium infantis in the maternal separation model of depression. Neuroscience 170 1179–1188. 10.1016/j.neuroscience.2010.08.005 [DOI] [PubMed] [Google Scholar]
- Dimidi E., Christodoulides S., Fragkos K. C., Scott S. M., Whelan K. (2014). The effect of probiotics on functional constipation in adults: a systematic review and meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 100 1075–1084. 10.3945/ajcn.114.089151 [DOI] [PubMed] [Google Scholar]
- Dinan T. G., Cryan J. F. (2017). Gut instincts: microbiota as a key regulator of brain development, ageing and neurodegeneration. J. Physiol. 595 489–503. 10.1113/JP273106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding T., Schloss P. D. (2014). Dynamics and associations of microbial community types across the human body. Nature 509 357–360. 10.1038/nature13178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diviccaro S., Giatti S., Borgo F., Barcella M., Borghi E., Trejo J. L., et al. (2019). Treatment of male rats with finasteride, an inhibitor of 5alpha-reductase enzyme, induces long-lasting effects on depressive-like behavior, hippocampal neurogenesis, neuroinflammation and gut microbiota composition. Psychoneuroendocrinology 99 206–215. 10.1016/j.psyneuen.2018.09.021 [DOI] [PubMed] [Google Scholar]
- Dominianni C., Sinha R., Goedert J. J., Pei Z., Yang L., Hayes R. B., et al. (2015). Sex, body mass index, and dietary fiber intake influence the human gut microbiome. PLoS One 10:e0124599. 10.1371/journal.pone.0124599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowlati Y., Herrmann N., Swardfager W., Liu H., Sham L., Reim E. K., et al. (2010). A meta-analysis of cytokines in major depression. Biol. Psychiatry 67 446–457. 10.1016/j.biopsych.2009.09.033 [DOI] [PubMed] [Google Scholar]
- Duan J., Huang Y., Tan X., Chai T., Wu J., Zhang H., et al. (2021). Characterization of gut microbiome in mice model of depression with divergent response to escitalopram treatment. Transl. Psychiatry 11:303. 10.1038/s41398-021-01428-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duivis H. E., Vogelzangs N., Kupper N., De Jonge P., Penninx B. W. (2013). Differential association of somatic and cognitive symptoms of depression and anxiety with inflammation: findings from the Netherlands Study of Depression and Anxiety (NESDA). Psychoneuroendocrinology 38 1573–1585. 10.1016/j.psyneuen.2013.01.002 [DOI] [PubMed] [Google Scholar]
- Dunn A. J. (2006). Effects of cytokines and infections on brain neurochemistry. Clin. Neurosci. Res. 6 52–68. 10.1016/j.cnr.2006.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn A. J., Swiergiel A. H., Beaurepaire R. D. (2005). Cytokines as mediators of depression: What can we learn from animal studies? Neurosci. Biobehav. Rev. 29 891–909. 10.1016/j.neubiorev.2005.03.023 [DOI] [PubMed] [Google Scholar]
- Elderman M., Hugenholtz F., Belzer C., Boekschoten M., Van Beek A., De Haan B., et al. (2018). Sex and strain dependent differences in mucosal immunology and microbiota composition in mice. Biol. Sex Differ. 9:26. 10.1186/s13293-018-0186-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eltokhi A., Janmaat I. E., Genedi M., Haarman B. C. M., Sommer I. E. C. (2020). Dysregulation of synaptic pruning as a possible link between intestinal microbiota dysbiosis and neuropsychiatric disorders. J. Neurosci. Res. 98 1335–1369. 10.1002/jnr.24616 [DOI] [PubMed] [Google Scholar]
- Eltokhi A., Rappold G., Sprengel R. (2018). Distinct phenotypes of Shank2 mouse models reflect neuropsychiatric spectrum disorders of human patients with SHANK2 Variants. Front. Mol. Neurosci. 11:240. 10.3389/fnmol.2018.00240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farzi A., Fröhlich E. E., Holzer P. (2018). Gut Microbiota and the neuroendocrine system. Neurotherapeutics 15 5–22. 10.1007/s13311-017-0600-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores R., Shi J., Fuhrman B., Xu X., Veenstra T. D., Gail M. H., et al. (2012). Fecal microbial determinants of fecal and systemic estrogens and estrogen metabolites: a cross-sectional study. J. Transl. Med. 10:253. 10.1186/1479-5876-10-253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flux M. C., Lowry C. A. (2020). Finding intestinal fortitude: integrating the microbiome into a holistic view of depression mechanisms, treatment, and resilience. Neurobiol. Dis. 135 104578. 10.1016/j.nbd.2019.104578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes J. D., Chen C.-Y., Knox N. C., Marrie R.-A., El-Gabalawy H., De Kievit T., et al. (2018). A comparative study of the gut microbiota in immune-mediated inflammatory diseases—does a common dysbiosis exist? Microbiome 6:221. 10.1186/s40168-018-0603-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford D. E., Erlinger T. P. (2004). Depression and C-reactive protein in US adults: data from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 164 1010–1014. 10.1001/archinte.164.9.1010 [DOI] [PubMed] [Google Scholar]
- Foster J. A., Rinaman L., Cryan J. F. (2017). Stress & the gut-brain axis: regulation by the microbiome. Neurobiol. Stress 7 124–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung T. C., Olson C. A., Hsiao E. Y. (2017). Interactions between the microbiota, immune and nervous systems in health and disease. Nat. Neurosci. 20 145–155. 10.1038/nn.4476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gałecki P., Mossakowska-Wójcik J., Talarowska M. (2018). The anti-inflammatory mechanism of antidepressants – SSRIs, SNRIs. Prog. Neuropsychopharmacol. Biol. Psychiatry 80 291–294. 10.1016/j.pnpbp.2017.03.016 [DOI] [PubMed] [Google Scholar]
- Gao X., Zhang M., Xue J., Huang J., Zhuang R., Zhou X., et al. (2018). Body mass index differences in the gut microbiota are gender specific. Front. Microbiol. 9:1250. 10.3389/fmicb.2018.01250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Mantrana I., Selma-Royo M., Alcantara C., Collado M. C. (2018). Shifts on gut microbiota associated to mediterranean diet adherence and specific dietary intakes on general adult population. Front. Microbiol. 9:890. 10.3389/fmicb.2018.00890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gareau M. G., Wine E., Rodrigues D. M., Cho J. H., Whary M. T., Philpott D. J., et al. (2011). Bacterial infection causes stress-induced memory dysfunction in mice. Gut 60 307–317. 10.1136/gut.2009.202515 [DOI] [PubMed] [Google Scholar]
- Genedi M., Janmaat I. E., Haarman B., Sommer I. E. C. (2019). Dysregulation of the gut-brain axis in schizophrenia and bipolar disorder: probiotic supplementation as a supportive treatment in psychiatric disorders. Curr. Opin. Psychiatry 32 185–195. 10.1097/YCO.0000000000000499 [DOI] [PubMed] [Google Scholar]
- Gensollen T., Iyer S. S., Kasper D. L., Blumberg R. S. (2016). How colonization by microbiota in early life shapes the immune system. Science 352 539–544. 10.1126/science.aad9378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Getachew B., Aubee J. I., Schottenfeld R. S., Csoka A. B., Thompson K. M., Tizabi Y. (2018). Ketamine interactions with gut-microbiota in rats: relevance to its antidepressant and anti-inflammatory properties. BMC Microbiol. 18:222. 10.1186/s12866-018-1373-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghorbani Z., Nazari S., Etesam F., Nourimajd S., Ahmadpanah M., Razeghi Jahromi S. (2018). The Effect of synbiotic as an adjuvant therapy to fluoxetine in moderate depression: a randomized multicenter trial. Arch. Neurosci. 5:e60507. [Google Scholar]
- Gimeno D., Kivimaki M., Brunner E. J., Elovainio M., De Vogli R., Steptoe A., et al. (2009). Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychol. Med. 39 413–423. 10.1017/S0033291708003723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gingnell M., Engman J., Frick A., Moby L., Wikström J., Fredrikson M., et al. (2013). Oral contraceptive use changes brain activity and mood in women with previous negative affect on the pill–a double-blinded, placebo-controlled randomized trial of a levonorgestrel-containing combined oral contraceptive. Psychoneuroendocrinology 38 1133–1144. 10.1016/j.psyneuen.2012.11.006 [DOI] [PubMed] [Google Scholar]
- Glavin G. B., Paré W. P., Sandbak T., Bakke H.-K., Murison R. (1994). Restraint stress in biomedical research: An update. Neurosci. Biobehav. Rev. 18 223–249. 10.1016/0149-7634(94)90027-2 [DOI] [PubMed] [Google Scholar]
- Goldsmith D. R., Rapaport M. H., Miller B. J. (2016). A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol. Psychiatry 21 1696–1709. 10.1038/mp.2016.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon J. L., Girdler S. S. (2014). Hormone replacement therapy in the treatment of perimenopausal depression. Curr. Psychiatry Rep. 16:517. 10.1007/s11920-014-0517-1 [DOI] [PubMed] [Google Scholar]
- Grandys M., Majerczak J., Zapart-Bukowska J., Duda K., Kulpa J. K., Zoladz J. A. (2021). Lowered serum testosterone concentration is associated with enhanced inflammation and worsened lipid profile in men. Front. Endocrinol. 12:735638. 10.3389/fendo.2021.735638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guinane C. M., Cotter P. D. (2013). Role of the gut microbiota in health and chronic gastrointestinal disease: understanding a hidden metabolic organ. Therap. Adv. Gastroenterol. 6 295–308. 10.1177/1756283X13482996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadizadeh M., Hamidi G. A., Salami M. (2019). Probiotic supplementation improves the cognitive function and the anxiety-like behaviors in the stressed rats. Iran. J. Basic Med. Sci. 22 506–514. 10.22038/ijbms.2019.33956.8078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao Z., Wang W., Guo R., Liu H. (2019). Faecalibacterium prausnitzii (ATCC 27766) has preventive and therapeutic effects on chronic unpredictable mild stress-induced depression-like and anxiety-like behavior in rats. Psychoneuroendocrinology 104 132–142. 10.1016/j.psyneuen.2019.02.025 [DOI] [PubMed] [Google Scholar]
- Harkin A., Kelly J., Leonard B. (2003). A revew of the relevance and validity of olfactory bulbectomy as a model of depression. Clin. Neurosci. Res. 3 253–262. 10.1016/s1566-2772(03)00087-2 [DOI] [Google Scholar]
- Haro C., Rangel-Zuniga O. A., Alcala-Diaz J. F., Gomez-Delgado F., Perez-Martinez P., Delgado-Lista J., et al. (2016). Intestinal Microbiota Is Influenced by Gender and Body Mass Index. PLoS One 11:e0154090. 10.1371/journal.pone.0154090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill C. J., Lynch D. B., Murphy K., Ulaszewska M., Jeffery I. B., O’shea C. A., et al. (2017). Evolution of gut microbiota composition from birth to 24 weeks in the INFANTMET Cohort. Microbiome 5:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Shi X., Li Z., Shen Y., Shi X., Wang L., et al. (2018). Possible association of Firmicutes in the gut microbiota of patients with major depressive disorder. Neuropsychiatr. Dis. Treat. 14 3329–3337. 10.2147/NDT.S188340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huttenhower C., Gevers D., Knight R., Abubucker S., Badger J. H., Chinwalla A. T., et al. (2012). Structure, function and diversity of the healthy human microbiome. Nature 486 207–214. 10.1038/nature11234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inserra A., Rogers G. B., Licinio J., Wong M.-L. (2018). The Microbiota-inflammasome hypothesis of major depression. Bioessays 40:1800027. 10.1002/bies.201800027 [DOI] [PubMed] [Google Scholar]
- Jiang H., Ling Z., Zhang Y., Mao H., Ma Z., Yin Y., et al. (2015). Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav. Immun. 48 186–194. 10.1016/j.bbi.2015.03.016 [DOI] [PubMed] [Google Scholar]
- Johansson M. E., Sjövall H., Hansson G. C. (2013). The gastrointestinal mucus system in health and disease. Nat. Rev. Gastroenterol. Hepatol. 10 352–361. 10.1038/nrgastro.2013.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim R., Stanczyk F., Hodis H., Cushman M., Lobo R., Hwang J., et al. (2010). Associations between markers of inflammation and physiological and pharmacological levels of circulating sex hormones in postmenopausal women. Menopause 17 785–790. 10.1097/gme.0b013e3181cc50b2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karunasena E., Mcmahon K. W., Chang D., Brashears M. M. (2014). Host responses to the pathogen Mycobacterium avium subsp. paratuberculosis and beneficial microbes exhibit host sex specificity. Appl. Environ. Microbiol. 80 4481–4490. 10.1128/AEM.01229-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemi A., Noorbala A. A., Azam K., Eskandari M. H., Djafarian K. (2019). Effect of probiotic and prebiotic vs placebo on psychological outcomes in patients with major depressive disorder: a randomized clinical trial. Clin. Nutr. 38 522–528. 10.1016/j.clnu.2018.04.010 [DOI] [PubMed] [Google Scholar]
- Kelly J. R., Borre Y., O’ Brien C., Patterson E., El Aidy S., Deane J., et al. (2016). Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat. J. Psychiatr. Res. 82 109–118. 10.1016/j.jpsychires.2016.07.019 [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser J. K., Habash D. L., Fagundes C. P., Andridge R., Peng J., Malarkey W. B., et al. (2015). Daily stressors, past depression, and metabolic responses to high-fat meals: a novel path to obesity. Biol. Psychiatry 77 653–660. 10.1016/j.biopsych.2014.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y. K., Na K. S., Myint A. M., Leonard B. E. (2016). The role of pro-inflammatory cytokines in neuroinflammation, neurogenesis and the neuroendocrine system in major depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 64 277–284. 10.1016/j.pnpbp.2015.06.008 [DOI] [PubMed] [Google Scholar]
- Kim Y. S., Unno T., Kim B. Y., Park M. S. (2020). Sex differences in gut microbiota. World J. Mens Health 38 48–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokai M., Kashiwamura S., Okamura H., Ohara K., Morita Y. (2002). Plasma interleukin-18 levels in patients with psychiatric disorders. J. Immunother. 25(Suppl. 1), S68–S71. 10.1097/00002371-200203001-00011 [DOI] [PubMed] [Google Scholar]
- Konstantinos A., Evangelia M. (2019). Adherence to Mediterranean diet and risk of depression later in life. A cross sectional study in East Attica, Greece. Glob. Psychiatry 2 201–209. 10.2478/gp-2019-0012 [DOI] [Google Scholar]
- Kovacs A., Ben-Jacob N., Tayem H., Halperin E., Iraqi F. A., Gophna U. (2011). Genotype is a stronger determinant than sex of the mouse gut microbiota. Microb. Ecol. 61 423–428. 10.1007/s00248-010-9787-2 [DOI] [PubMed] [Google Scholar]
- Krishnan V., Nestler E. J. (2011). Animal models of depression: molecular perspectives. Curr. Top. Behav. Neurosci. 7 121–147. 10.1007/7854_2010_108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krznaric Z., Vranesic Bender D., Mestrovic T. (2019). The Mediterranean diet and its association with selected gut bacteria. Curr. Opin. Clin. Nutr. Metab. Care 22 401–406. 10.1097/MCO.0000000000000587 [DOI] [PubMed] [Google Scholar]
- Kupelian V., Chiu G., Araujo A., Williams R., Clark R., Mckinlay J. (2009). Association of sex hormones and C-reactive protein levels in men. Clin. Endocrinol. 72 527–533. 10.1111/j.1365-2265.2009.03713.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai W., Cai S. (2018). Comment on “Prevalence of Anxiety and Depression in Patients with Inflammatory Bowel Disease”. Can. J. Gastroenterol. Hepatol. 2018 6747630–6747630. 10.1155/2018/6747630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamers F., Vogelzangs N., Merikangas K. R., De Jonge P., Beekman A. T., Penninx B. W. (2013). Evidence for a differential role of HPA-axis function, inflammation and metabolic syndrome in melancholic versus atypical depression. Mol. Psychiatry 18 692–699. 10.1038/mp.2012.144 [DOI] [PubMed] [Google Scholar]
- Larroya-Garcia A., Navas-Carrillo D., Orenes-Pinero E. (2019). Impact of gut microbiota on neurological diseases: diet composition and novel treatments. Crit. Rev. Food Sci. Nutr. 59 3102–3116. 10.1080/10408398.2018.1484340 [DOI] [PubMed] [Google Scholar]
- Lassale C., Batty G. D., Baghdadli A., Jacka F., Sánchez-Villegas A., Kivimäki M., et al. (2019). Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol. Psychiatry 24 965–986. 10.1038/s41380-018-0237-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBlanc J. G., Milani C., De Giori G. S., Sesma F., Van Sinderen D., Ventura M. (2013). Bacteria as vitamin suppliers to their host: a gut microbiota perspective. Curr. Opin. Biotechnol. 24 160–168. 10.1016/j.copbio.2012.08.005 [DOI] [PubMed] [Google Scholar]
- Ledeboer A., Breve J. J., Poole S., Tilders F. J., Van Dam A. M. (2000). Interleukin-10, interleukin-4, and transforming growth factor-beta differentially regulate lipopolysaccharide-induced production of pro-inflammatory cytokines and nitric oxide in co-cultures of rat astroglial and microglial cells. Glia 30 134–142. [DOI] [PubMed] [Google Scholar]
- Lee J. Y., Kim N., Nam R. H., Sohn S. H., Lee S. M., Choi D., et al. (2017). Probiotics reduce repeated water avoidance stress-induced colonic microinflammation in Wistar rats in a sex-specific manner. PLoS One 12:e0188992. 10.1371/journal.pone.0188992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard B. E. (2018). Inflammation and depression: a causal or coincidental link to the pathophysiology? Acta Neuropsychiatr. 30 1–16. 10.1017/neu.2016.69 [DOI] [PubMed] [Google Scholar]
- Ley R. E., Backhed F., Turnbaugh P., Lozupone C. A., Knight R. D., Gordon J. I. (2005). Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. U.S.A. 102 11070–11075. 10.1073/pnas.0504978102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Jia H., Cai X., Zhong H., Feng Q., Sunagawa S., et al. (2014). An integrated catalog of reference genes in the human gut microbiome. Nat. Biotechnol. 32 834–841. 10.1038/nbt.2942 [DOI] [PubMed] [Google Scholar]
- Li M., Wang B., Zhang M., Rantalainen M., Wang S., Zhou H., et al. (2008). Symbiotic gut microbes modulate human metabolic phenotypes. Proc. Natl. Acad. Sci. U.S.A. 105 2117–2122. 10.1073/pnas.0712038105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li N., Wang Q., Wang Y., Sun A., Lin Y., Jin Y., et al. (2018). Oral probiotics ameliorate the behavioral deficits induced by chronic mild stress in mice via the gut microbiota-inflammation axis. Front. Behav. Neurosci. 12:266. 10.3389/fnbeh.2018.00266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang S., Wang T., Hu X., Luo J., Li W., Wu X., et al. (2015). Administration of Lactobacillus helveticus NS8 improves behavioral, cognitive, and biochemical aberrations caused by chronic restraint stress. Neuroscience 310 561–577. 10.1016/j.neuroscience.2015.09.033 [DOI] [PubMed] [Google Scholar]
- Lim S. S., Vos T., Flaxman A. D., Danaei G., Shibuya K., Adair-Rohani H., et al. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 2224–2260. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q. F., Kim H. M., Lim S., Chung M. J., Lim C. Y., Koo B. S., et al. (2020). Effect of probiotic administration on gut microbiota and depressive behaviors in mice. Daru 28 181–189. 10.1007/s40199-020-00329-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Zhang L., Wang X., Wang Z., Zhang J., Jiang R., et al. (2016). Similar fecal microbiota signatures in patients with diarrhea-predominant irritable bowel syndrome and patients with depression. Clin. Gastroenterol. Hepatol. 14 1602–1611.e5. 10.1016/j.cgh.2016.05.033 [DOI] [PubMed] [Google Scholar]
- Llopis M., Antolin M., Carol M., Borruel N., Casellas F., Martinez C., et al. (2009). Lactobacillus casei downregulates commensals’ inflammatory signals in Crohn’s disease mucosa. Inflamm. Bowel Dis. 15 275–283. 10.1002/ibd.20736 [DOI] [PubMed] [Google Scholar]
- Lopizzo N., Bocchio Chiavetto L., Cattane N., Plazzotta G., Tarazi F. I., Pariante C. M., et al. (2015). Gene-environment interaction in major depression: focus on experience-dependent biological systems. Front. Psychiatry 6:68. 10.3389/fpsyt.2015.00068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie I., Yang Y. X., Haynes K., Mamtani R., Boursi B. (2015). Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study. J. Clin. Psychiatry 76 1522–1528. 10.4088/JCP.15m09961 [DOI] [PubMed] [Google Scholar]
- Lyte M., Daniels K. M., Schmitz-Esser S. (2019). Fluoxetine-induced alteration of murine gut microbial community structure: evidence for a microbial endocrinology-based mechanism of action responsible for fluoxetine-induced side effects. PeerJ 7:e6199. 10.7717/peerj.6199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macedo D., Filho A. J. M. C., Soares, De Sousa C. N., Quevedo J., Barichello T., et al. (2017). Antidepressants, antimicrobials or both? Gut microbiota dysbiosis in depression and possible implications of the antimicrobial effects of antidepressant drugs for antidepressant effectiveness. J. Affect. Disord. 208 22–32. 10.1016/j.jad.2016.09.012 [DOI] [PubMed] [Google Scholar]
- Madison A., Kiecolt-Glaser J. K. (2019). Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr. Opin. Behav. Sci. 28 105–110. 10.1016/j.cobeha.2019.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes M. (1995). Evidence for an immune response in major depression: a review and hypothesis. Prog. Neuropsychopharmacol. Biol. Psychiatry 19 11–38. 10.1016/0278-5846(94)00101-m [DOI] [PubMed] [Google Scholar]
- Maes M., Berk M., Goehler L., Song C., Anderson G., Galecki P., et al. (2012). Depression and sickness behavior are Janus-faced responses to shared inflammatory pathways. BMC Med. 10:66. 10.1186/1741-7015-10-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes M., Kubera M., Leunis J. C. (2008). The gut-brain barrier in major depression: intestinal mucosal dysfunction with an increased translocation of LPS from gram negative enterobacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression. Neuro Endocrinol. Lett. 29 117–124. [PubMed] [Google Scholar]
- Maggio M., Ceda G. P., Lauretani F., Bandinelli S., Corsi A. M., Giallauria F., et al. (2011). SHBG, sex hormones, and inflammatory markers in older women. J. Clin. Endocrinol. Metab. 96 1053–1059. 10.1210/jc.2010-1902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahajan S., Avasthi A., Grover S., Chawla Y. K. (2014). Incidence of depression in patients with chronic hepatitis C receiving combination therapy of pegylated interferon-alpha and ribavirin. Psychother. Psychosom. 83 308–309. 10.1159/000358527 [DOI] [PubMed] [Google Scholar]
- Maier L., Pruteanu M., Kuhn M., Zeller G., Telzerow A., Anderson E. E., et al. (2018). Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 555 623–628. 10.1038/nature25979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majeed M., Nagabhushanam K., Arumugam S., Majeed S., Ali F. (2018). Bacillus coagulans MTCC 5856 for the management of major depression with irritable bowel syndrome: a randomised, double-blind, placebo controlled, multi-centre, pilot clinical study. Food Nutr. Res. 62:1218. 10.29219/fnr.v62.1218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangiola F., Ianiro G., Franceschi F., Fagiuoli S., Gasbarrini G., Gasbarrini A. (2016). Gut microbiota in autism and mood disorders. World J. Gastroenterol. 22 361–368. 10.3748/wjg.v22.i1.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markle J. G., Frank D. N., Mortin-Toth S., Robertson C. E., Feazel L. M., Rolle-Kampczyk U., et al. (2013). Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science 339 1084–1088. 10.1126/science.1233521 [DOI] [PubMed] [Google Scholar]
- Marotta A., Sarno E., Del Casale A., Pane M., Mogna L., Amoruso A., et al. (2019). Effects of probiotics on cognitive reactivity, mood, and sleep quality. Front. Psychiatry 10:164. 10.3389/fpsyt.2019.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C. R., Mayer E. A. (2017). Gut-brain axis and behavior. Nestle Nutr. Inst. Workshop Ser. 88 45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C. R., Osadchiy V., Kalani A., Mayer E. A. (2018). The brain-gut-microbiome axis. Cell. Mol. Gastroenterol. Hepatol. 6 133–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews K., Robbins T. W. (2003). Early experience as a determinant of adult behavioural responses to reward: the effects of repeated maternal separation in the rat. Neurosci. Biobehav. Rev. 27 45–55. 10.1016/s0149-7634(03)00008-3 [DOI] [PubMed] [Google Scholar]
- McCarter T. (2008). Depression overview. Am. Health Drug Benefits 1 44–51. [PMC free article] [PubMed] [Google Scholar]
- Mendlewicz J., Kriwin P., Oswald P., Souery D., Alboni S., Brunello N. (2006). Shortened onset of action of antidepressants in major depression using acetylsalicylic acid augmentation: a pilot open-label study. Int. Clin. Psychopharmacol. 21 227–231. 10.1097/00004850-200607000-00005 [DOI] [PubMed] [Google Scholar]
- Mesquita A. R., Correia-Neves M., Roque S., Castro A. G., Vieira P., Pedrosa J., et al. (2008). IL-10 modulates depressive-like behavior. J. Psychiatr. Res. 43 89–97. 10.1016/j.jpsychires.2008.02.004 [DOI] [PubMed] [Google Scholar]
- Messaoudi M., Lalonde R., Violle N., Javelot H., Desor D., Nejdi A., et al. (2011). Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br. J. Nutr. 105 755–764. 10.1017/S0007114510004319 [DOI] [PubMed] [Google Scholar]
- Mikova O., Yakimova R., Bosmans E., Kenis G., Maes M. (2001). Increased serum tumor necrosis factor alpha concentrations in major depression and multiple sclerosis. Eur. Neuropsychopharmacol. 11 203–208. 10.1016/s0924-977x(01)00081-5 [DOI] [PubMed] [Google Scholar]
- Miller A. H., Raison C. L. (2016). The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat. Rev. Immunol. 16 22–34. 10.1038/nri.2015.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller L. E., Ouwehand A. C. (2013). Probiotic supplementation decreases intestinal transit time: meta-analysis of randomized controlled trials. World J. Gastroenterol. 19 4718–4725. 10.3748/wjg.v19.i29.4718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizrahi-Man O., Davenport E. R., Gilad Y. (2013). Taxonomic classification of bacterial 16S rRNA genes using short sequencing reads: evaluation of effective study designs. PLoS One 8:e53608. 10.1371/journal.pone.0053608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamad N., Wong S. K., Hasan W., Jolly J., Fozi F., Ima-Nirwana S., et al. (2018). The relationship between circulating testosterone and inflammatory cytokines in men. Aging Male 22 1–12. 10.1080/13685538.2018.1482487 [DOI] [PubMed] [Google Scholar]
- Mohammadi A. A., Jazayeri S., Khosravi-Darani K., Solati Z., Mohammadpour N., Asemi Z., et al. (2016). The effects of probiotics on mental health and hypothalamic-pituitary-adrenal axis: a randomized, double-blind, placebo-controlled trial in petrochemical workers. Nutr. Neurosci. 19 387–395. 10.1179/1476830515y.0000000023 [DOI] [PubMed] [Google Scholar]
- Mohle L., Mattei D., Heimesaat M. M., Bereswill S., Fischer A., Alutis M., et al. (2016). Ly6C(hi) monocytes provide a link between antibiotic-induced changes in gut microbiota and adult hippocampal neurogenesis. Cell Rep. 15 1945–1956. 10.1016/j.celrep.2016.04.074 [DOI] [PubMed] [Google Scholar]
- Monteiro R., Teixeira D., Calhau C. (2014). Estrogen signaling in metabolic inflammation. Mediators Inflamm. 2014:615917. 10.1155/2014/615917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgun A., Dzutsev A., Dong X., Greer R. L., Sexton D. J., Ravel J., et al. (2015). Uncovering effects of antibiotics on the host and microbiota using transkingdom gene networks. Gut 64 1732–1743. 10.1136/gutjnl-2014-308820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowat A. M., Agace W. W. (2014). Regional specialization within the intestinal immune system. Nat. Rev. Immunol. 14 667–685. 10.1038/nri3738 [DOI] [PubMed] [Google Scholar]
- Mueller S., Saunier K., Hanisch C., Norin E., Alm L., Midtvedt T., et al. (2006). Differences in fecal microbiota in different European study populations in relation to age, gender, and country: a cross-sectional study. Appl. Environ. Microbiol. 72 1027–1033. 10.1128/AEM.72.2.1027-1033.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller N., Schwarz M. J., Dehning S., Douhe A., Cerovecki A., Goldstein-Muller B., et al. (2006). The cyclooxygenase-2 inhibitor celecoxib has therapeutic effects in major depression: results of a double-blind, randomized, placebo controlled, add-on pilot study to reboxetine. Mol. Psychiatry 11 680–684. 10.1038/sj.mp.4001805 [DOI] [PubMed] [Google Scholar]
- Murray C. J., Atkinson C., Bhalla K., Birbeck G., Burstein R., Chou D., et al. (2013). The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA 310 591–608. 10.1001/jama.2013.13805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagpal R., Shively C., Register T., Craft S., Yadav H. (2019). Gut microbiome-Mediterranean diet interactions in improving host health. F1000Res. 8:699. 10.12688/f1000research.18992.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naseribafrouei A., Hestad K., Avershina E., Sekelja M., Linlokken A., Wilson R., et al. (2014). Correlation between the human fecal microbiota and depression. Neurogastroenterol. Motil. 26 1155–1162. 10.1111/nmo.12378 [DOI] [PubMed] [Google Scholar]
- Natividad J. M., Verdu E. F. (2013). Modulation of intestinal barrier by intestinal microbiota: pathological and therapeutic implications. Pharmacol. Res. 69 42–51. 10.1016/j.phrs.2012.10.007 [DOI] [PubMed] [Google Scholar]
- Nazimek K., Strobel S., Bryniarski P., Kozlowski M., Filipczak-Bryniarska I., Bryniarski K. (2017). The role of macrophages in anti-inflammatory activity of antidepressant drugs. Immunobiology 222 823–830. 10.1016/j.imbio.2016.07.001 [DOI] [PubMed] [Google Scholar]
- Neumann I. D., Wigger A., Krömer S., Frank E., Landgraf R., Bosch O. J. (2005). Differential effects of periodic maternal separation on adult stress coping in a rat model of extremes in trait anxiety. Neuroscience 132 867–877. 10.1016/j.neuroscience.2005.01.034 [DOI] [PubMed] [Google Scholar]
- Ni J., Wu G. D., Albenberg L., Tomov V. T. (2017). Gut microbiota and IBD: causation or correlation? Nat. Rev. Gastroenterol. Hepatol. 14 573–584. 10.1038/nrgastro.2017.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishida K., Sawada D., Kuwano Y., Tanaka H., Sugawara T., Aoki Y., et al. (2017). Daily administration of paraprobiotic Lactobacillus gasseri CP2305 ameliorates chronic stress-associated symptoms in Japanese medical students. J. Funct. Foods 36 112–121. 10.1016/j.jff.2017.06.031 [DOI] [Google Scholar]
- Odamaki T., Kato K., Sugahara H., Hashikura N., Takahashi S., Xiao J.-Z., et al. (2016). Age-related changes in gut microbiota composition from newborn to centenarian: a cross-sectional study. BMC Microbiol. 16:90. 10.1186/s12866-016-0708-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Mahony S. M., Marchesi J. R., Scully P., Codling C., Ceolho A.-M., Quigley E. M. M., et al. (2009). Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol. Psychiatry 65 263–267. 10.1016/j.biopsych.2008.06.026 [DOI] [PubMed] [Google Scholar]
- Org E., Mehrabian M., Parks B. W., Shipkova P., Liu X., Drake T. A., et al. (2016). Sex differences and hormonal effects on gut microbiota composition in mice. Gut Microbes 7 313–322. 10.1080/19490976.2016.1203502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osadchiy V., Martin C. R., Mayer E. A. (2019). The gut-brain axis and the microbiome: mechanisms and clinical implications. Clin. Gastroenterol. Hepatol. 17 322–332. 10.1016/j.cgh.2018.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Östlund-Lagerström L., Kihlgren A., Repsilber D., Björkstén B., Brummer R. J., Schoultz I. (2016). Probiotic administration among free-living older adults: a double blinded, randomized, placebo-controlled clinical trial. Nutr. J. 15:80. 10.1186/s12937-016-0198-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacheco A. R., Sperandio V. (2015). Enteric pathogens exploit the microbiota-generated nutritional environment of the gut. Microbiol. Spectr. 3:10.1128/microbiolspec.MBP-0001-2014. 10.1128/microbiolspec.MBP-0001-2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagliai G., Sofi F., Vannetti F., Caiani S., Pasquini G., Molino Lova R., et al. (2018). Mediterranean diet, food consumption and risk of late-life depression: the mugello study. J. Nutr. Health Aging 22 569–574. 10.1007/s12603-018-1019-3 [DOI] [PubMed] [Google Scholar]
- Park A. J., Collins J., Blennerhassett P. A., Ghia J. E., Verdu E. F., Bercik P., et al. (2013). Altered colonic function and microbiota profile in a mouse model of chronic depression. J. Neurogastroenterol. Motil. 25 733–e575. 10.1111/nmo.12153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J. M., Lee Y. J. (2020). Serum oestradiol levels are inversely associated with C-reactive protein levels in premenopausal women, but not postmenopausal women. J. Int. Med. Res. 48:300060520961228. 10.1177/0300060520961228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel A. (2013). Review: the role of inflammation in depression. Psychiatr. Danub. 25(Suppl. 2), S216–S223. [PubMed] [Google Scholar]
- Patten S. B., Wang J. L., Williams J. V., Currie S., Beck C. A., Maxwell C. J., et al. (2006). Descriptive epidemiology of major depression in Canada. Can. J. Psychiatry 51 84–90. 10.1177/070674370605100204 [DOI] [PubMed] [Google Scholar]
- Petersen C., Round J. L. (2014). Defining dysbiosis and its influence on host immunity and disease. Cell. Microbiol. 16 1024–1033. 10.1111/cmi.12308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips J. G. P. (1910). The treatment of melancholia by the lactic acid Bacillus. J. Ment. Sci. 56 422–430. 10.1192/bjp.56.234.422 [DOI] [Google Scholar]
- Poretsky R., Rodriguez R. L., Luo C., Tsementzi D., Konstantinidis K. T. (2014). Strengths and limitations of 16S rRNA gene amplicon sequencing in revealing temporal microbial community dynamics. PLoS One 9:e93827. 10.1371/journal.pone.0093827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Principi N., Esposito S. (2016). Gut microbiota and central nervous system development. J. Infect. 73 536–546. 10.1016/j.jinf.2016.09.010 [DOI] [PubMed] [Google Scholar]
- Proctor L. M., Creasy H. H., Fettweis J. M., Lloyd-Price J., Mahurkar A., Zhou W., et al. (2019). The integrative human microbiome project. Nature 569 641–648. 10.1038/s41586-019-1238-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin J., Li R., Raes J., Arumugam M., Burgdorf K. S., Manichanh C., et al. (2010). A human gut microbial gene catalogue established by metagenomic sequencing. Nature 464 59–65. 10.1038/nature08821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajilic-Stojanovic M., de Vos W. M. (2014). The first 1000 cultured species of the human gastrointestinal microbiota. FEMS Microbiol. Rev. 38 996–1047. 10.1111/1574-6976.12075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransohoff R. M., Brown M. A. (2012). Innate immunity in the central nervous system. J. Clin. Invest. 122 1164–1171. 10.1172/jci58644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reininghaus E. Z., Platzer M., Kohlhammer-Dohr A., Hamm C., Mörkl S., Bengesser S. A., et al. (2020). PROVIT: supplementary probiotic treatment and vitamin B7 in Depression-A Randomized Controlled Trial. Nutrients 12:3422. 10.3390/nu12113422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyman M., Van Houten M. A., Van Baarle D., Bosch A. A. T. M., Man W. H., Chu M. L. J. N., et al. (2019). Impact of delivery mode-associated gut microbiota dynamics on health in the first year of life. Nat. Commun. 10:4997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel M., Moller H. J., Obermeier M., Adli M., Bauer M., Kronmuller K., et al. (2011). Clinical predictors of response and remission in inpatients with depressive syndromes. J. Affect. Disord. 133 137–149. 10.1016/j.jad.2011.04.007 [DOI] [PubMed] [Google Scholar]
- Rogers G. B., Keating D. J., Young R. L., Wong M. L., Licinio J., Wesselingh S. (2016). From gut dysbiosis to altered brain function and mental illness: mechanisms and pathways. Mol. Psychiatry 21 738–748. 10.1038/mp.2016.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohleder N. (2014). Stimulation of systemic low-grade inflammation by psychosocial stress. Psychosom. Med. 76 181–189. 10.1097/PSY.0000000000000049 [DOI] [PubMed] [Google Scholar]
- Romijn A. R., Rucklidge J. J., Kuijer R. G., Frampton C. (2017). A double-blind, randomized, placebo-controlled trial of Lactobacillus helveticus and Bifidobacterium longum for the symptoms of depression. Aust. N. Z. J. Psychiatry 51 810–821. 10.1177/0004867416686694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Round J. L., Mazmanian S. K. (2009). The gut microbiota shapes intestinal immune responses during health and disease. Nat. Rev. Immunol. 9 313–323. 10.1038/nri2515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland I., Gibson G., Heinken A., Scott K., Swann J., Thiele I., et al. (2018). Gut microbiota functions: metabolism of nutrients and other food components. Eur. J. Nutr. 57 1–24. 10.1007/s00394-017-1445-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudzki L., Ostrowska L., Pawlak D., Malus A., Pawlak K., Waszkiewicz N., et al. (2019). Probiotic Lactobacillus Plantarum 299v decreases kynurenine concentration and improves cognitive functions in patients with major depression: a double-blind, randomized, placebo controlled study. Psychoneuroendocrinology 100 213–222. 10.1016/j.psyneuen.2018.10.010 [DOI] [PubMed] [Google Scholar]
- Rutayisire E., Huang K., Liu Y., Tao F. (2016). The mode of delivery affects the diversity and colonization pattern of the gut microbiota during the first year of infants’ life: a systematic review. BMC Gastroenterol. 16:86. 10.1186/s12876-016-0498-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salk R. H., Hyde J. S., Abramson L. Y. (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol. Bull. 143 783–822. 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salminen S., Gibson G. R., Mccartney A. L., Isolauri E. (2004). Influence of mode of delivery on gut microbiota composition in seven year old children. Gut 53 1388–1389. 10.1136/gut.2004.041640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Villegas A., Henríquez P., Bes-Rastrollo M., Doreste J. (2007). Mediterranean diet and depression. Public Health Nutr. 9 1104–1109. [DOI] [PubMed] [Google Scholar]
- Sassone-Corsi M., Raffatellu M. (2015). No vacancy: how beneficial microbes cooperate with immunity to provide colonization resistance to pathogens. J. Immunol. 194 4081–4087. 10.4049/jimmunol.1403169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savignac H. M., Kiely B., Dinan T. G., Cryan J. F. (2014). Bifidobacteria exert strain-specific effects on stress-related behavior and physiology in BALB/c mice. Neurogastroenterol. Motil. 26 1615–1627. 10.1111/nmo.12427 [DOI] [PubMed] [Google Scholar]
- Schroeder B. O., Backhed F. (2016). Signals from the gut microbiota to distant organs in physiology and disease. Nat. Med. 22 1079–1089. 10.1038/nm.4185 [DOI] [PubMed] [Google Scholar]
- Singh P., Manning S. D. (2016). Impact of age and sex on the composition and abundance of the intestinal microbiota in individuals with and without enteric infections. Ann. Epidemiol. 26 380–385. 10.1016/j.annepidem.2016.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha T., Vich Vila A., Garmaeva S., Jankipersadsing S. A., Imhann F., Collij V., et al. (2019). Analysis of 1135 gut metagenomes identifies sex-specific resistome profiles. Gut Microbes 10 358–366. 10.1080/19490976.2018.1528822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaper S. D., Facci L., Giusti P. (2014). Neuroinflammation, microglia and mast cells in the pathophysiology of neurocognitive disorders: a review. CNS Neurol. Disord. Drug Targets 13 1654–1666. 10.2174/1871527313666141130224206 [DOI] [PubMed] [Google Scholar]
- Skarupski K. A., Tangney C. C., Li H., Evans D. A., Morris M. C. (2013). Mediterranean diet and depressive symptoms among older adults over time. J. Nutr. Health Aging 17 441–445. 10.1007/s12603-012-0437-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skovlund C. W., Mørch L. S., Kessing L. V., Lidegaard Ø. (2016). Association of hormonal contraception with depression. JAMA Psychiatry 73 1154–1162. 10.1001/jamapsychiatry.2016.2387 [DOI] [PubMed] [Google Scholar]
- Slavich G., Sacher J. (2019). Stress, sex hormones, inflammation, and major depressive disorder: extending Social Signal Transduction Theory of Depression to account for sex differences in mood disorders. Psychopharmacology 236 1–17. 10.1007/s00213-019-05326-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sluzewska A., Rybakowski J., Bosmans E., Sobieska M., Berghmans R., Maes M., et al. (1996). Indicators of immune activation in major depression. Psychiatry Res. 64 161–167. 10.1016/s0165-1781(96)02783-7 [DOI] [PubMed] [Google Scholar]
- Slyepchenko A., Maes M., Jacka F. N., Kohler C. A., Barichello T., Mcintyre R. S., et al. (2017). Gut microbiota, bacterial translocation, and interactions with diet: pathophysiological links between major depressive disorder and non-communicable medical comorbidities. Psychother. Psychosom. 86 31–46. 10.1159/000448957 [DOI] [PubMed] [Google Scholar]
- Slykerman R. F., Hood F., Wickens K., Thompson J. M. D., Barthow C., Murphy R., et al. (2017). Effect of Lactobacillus rhamnosus HN001 in Pregnancy on Postpartum Symptoms of Depression and Anxiety: a Randomised Double-blind Placebo-controlled Trial. EBioMedicine 24 159–165. 10.1016/j.ebiom.2017.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C. J., Emge J. R., Berzins K., Lung L., Khamishon R., Shah P., et al. (2014). Probiotics normalize the gut-brain-microbiota axis in immunodeficient mice. Am. J. Physiol. Gastrointest. Liver Physiol. 307 G793–G802. 10.1152/ajpgi.00238.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P. A. (2015). The tantalizing links between gut microbes and the brain. Nature 526 312–314. 10.1038/526312a [DOI] [PubMed] [Google Scholar]
- Sokol H., Pigneur B., Watterlot L., Lakhdari O., Bermudez-Humaran L. G., Gratadoux J. J., et al. (2008). Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. U.S.A. 105 16731–16736. 10.1073/pnas.0804812105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommer F., Backhed F. (2013). The gut microbiota–masters of host development and physiology. Nat. Rev. Microbiol. 11 227–238. 10.1038/nrmicro2974 [DOI] [PubMed] [Google Scholar]
- Song C., Wang H. (2011). Cytokines mediated inflammation and decreased neurogenesis in animal models of depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 35 760–768. 10.1016/j.pnpbp.2010.06.020 [DOI] [PubMed] [Google Scholar]
- Soto M., Herzog C., Pacheco J. A., Fujisaka S., Bullock K., Clish C. B., et al. (2018). Gut microbiota modulate neurobehavior through changes in brain insulin sensitivity and metabolism. Mol. Psychiatry 23 2287–2301. 10.1038/s41380-018-0086-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanislawski M. A., Dabelea D., Wagner B. D., Iszatt N., Dahl C., Sontag M. K., et al. (2018). Gut Microbiota in the First 2 Years of Life and the Association with Body Mass Index at Age 12 in a Norwegian Birth Cohort. mBio 9:e01751-18. 10.1128/mBio.01751-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steenbergen L., Sellaro R., Van Hemert S., Bosch J. A., Colzato L. S. (2015). A randomized controlled trial to test the effect of multispecies probiotics on cognitive reactivity to sad mood. Brain Behav. Immun. 48 258–264. 10.1016/j.bbi.2015.04.003 [DOI] [PubMed] [Google Scholar]
- Sudo N., Chida Y., Aiba Y., Sonoda J., Oyama N., Yu X. N., et al. (2004). Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J. Physiol. 558 263–275. 10.1113/jphysiol.2004.063388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swiergiel A. H., Dunn A. J. (2007). Effects of interleukin-1β and lipopolysaccharide on behavior of mice in the elevated plus-maze and open field tests. Pharmacol. Biochem. Behav. 86 651–659. 10.1016/j.pbb.2007.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takagi T., Naito Y., Inoue R., Kashiwagi S., Uchiyama K., Mizushima K., et al. (2019). Differences in gut microbiota associated with age, sex, and stool consistency in healthy Japanese subjects. J. Gastroenterol. 54 53–63. 10.1007/s00535-018-1488-5 [DOI] [PubMed] [Google Scholar]
- Tan S., Wang Y., Chen K., Long Z., Zou J. (2017). Ketamine alleviates depressive-like behaviors via down-regulating inflammatory cytokines induced by chronic restraint stress in mice. Biol. Pharm. Bull. 40 1260–1267. 10.1248/bpb.b17-00131 [DOI] [PubMed] [Google Scholar]
- Thursby E., Juge N. (2017). Introduction to the human gut microbiota. Biochem. J. 474 1823–1836. 10.1042/bcj20160510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tillisch K., Labus J., Kilpatrick L., Jiang Z., Stains J., Ebrat B., et al. (2013). Consumption of fermented milk product with probiotic modulates brain activity. Gastroenterology 144 1394. 10.1053/j.gastro.2013.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toyoda A. (2017). Social defeat models in animal science: What we have learned from rodent models. Anim. Sci. J. 88 944–952. 10.1111/asj.12809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tribbick D., Salzberg M., Ftanou M., Connell W. R., Macrae F., Kamm M. A., et al. (2015). Prevalence of mental health disorders in inflammatory bowel disease: an Australian outpatient cohort. Clin. Exp. Gastroenterol. 8 197–204. 10.2147/CEG.S77567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbaugh P. J., Ley R. E., Hamady M., Fraser-Liggett C. M., Knight R., Gordon J. I. (2007). The human microbiome project. Nature 449 804–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valles-Colomer M., Falony G., Darzi Y., Tigchelaar E. F., Wang J., Tito R. Y., et al. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nat. Microbiol. 4 623–632. 10.1038/s41564-018-0337-x [DOI] [PubMed] [Google Scholar]
- van den Biggelaar A. H., Gussekloo J., De Craen A. J., Frolich M., Stek M. L., Van Der Mast R. C., et al. (2007). Inflammation and interleukin-1 signaling network contribute to depressive symptoms but not cognitive decline in old age. Exp. Gerontol. 42 693–701. 10.1016/j.exger.2007.01.011 [DOI] [PubMed] [Google Scholar]
- Vich Vila A., Collij V., Sanna S., Sinha T., Imhann F., Bourgonje A. R., et al. (2020). Impact of commonly used drugs on the composition and metabolic function of the gut microbiota. Nat. Commun. 11:362. 10.1038/s41467-019-14177-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker A. W., Ince J., Duncan S. H., Webster L. M., Holtrop G., Ze X., et al. (2011). Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J. 5 220–230. 10.1038/ismej.2010.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace C. J. K., Milev R. V. (2021). The efficacy, safety, and tolerability of probiotics on depression: clinical results from an open-label pilot study. Front. Psychiatry 12:618279. 10.3389/fpsyt.2021.618279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman M. M., Klerman G. L. (1977). Sex differences and the epidemiology of depression. Arch. Gen. Psychiatry 34 98–111. 10.1001/archpsyc.1977.01770130100011 [DOI] [PubMed] [Google Scholar]
- Wharton W., Gleason C. E., Olson S. R., Carlsson C. M., Asthana S. (2012). Neurobiological underpinnings of the estrogen - mood relationship. Curr. Psychiatry Rev. 8 247–256. 10.2174/157340012800792957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteford H. A., Degenhardt L., Rehm J., Baxter A. J., Ferrari A. J., Erskine H. E., et al. (2013). Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 382 1575–1586. 10.1016/s0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- Wiebe E. R., Brotto L. A., Mackay J. (2011). Characteristics of women who experience mood and sexual side effects with use of hormonal contraception. J. Obstet. Gynaecol. Can. 33 1234–1240. 10.1016/S1701-2163(16)35108-8 [DOI] [PubMed] [Google Scholar]
- Williams S., Chung G., Muennig P. (2017). Undiagnosed depression: a community diagnosis. SSM Popul. Health 3 633–638. 10.1016/j.ssmph.2017.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson I. D., Nicholson J. K. (2009). The role of gut microbiota in drug response. Curr. Pharm. Des. 15 1519–1523. 10.2174/138161209788168173 [DOI] [PubMed] [Google Scholar]
- Wittchen H. U., Jacobi F., Rehm J., Gustavsson A., Svensson M., Jonsson B., et al. (2011). The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur. Neuropsychopharmacol. 21 655–679. 10.1016/j.euroneuro.2011.07.018 [DOI] [PubMed] [Google Scholar]
- Wong M. L., Dong C., Maestre-Mesa J., Licinio J. (2008). Polymorphisms in inflammation-related genes are associated with susceptibility to major depression and antidepressant response. Mol. Psychiatry 13 800–812. 10.1038/mp.2008.59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M. L., Inserra A., Lewis M. D., Mastronardi C. A., Leong L., Choo J., et al. (2016). Inflammasome signaling affects anxiety- and depressive-like behavior and gut microbiome composition. Mol. Psychiatry 21 797–805. 10.1038/mp.2016.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu G. D., Chen J., Hoffmann C., Bittinger K., Chen Y.-Y., Keilbaugh S. A., et al. (2011). Linking long-term dietary patterns with gut microbial enterotypes. Science 334 105–108. 10.1126/science.1208344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia Z., Depierre J. W., Nassberger L. (1996). Tricyclic antidepressants inhibit IL-6, IL-1 beta and TNF-alpha release in human blood monocytes and IL-2 and interferon-gamma in T cells. Immunopharmacology 34 27–37. 10.1016/0162-3109(96)00111-7 [DOI] [PubMed] [Google Scholar]
- Yang C., Qu Y., Fujita Y., Ren Q., Ma M., Dong C., et al. (2017). Possible role of the gut microbiota–brain axis in the antidepressant effects of (R)-ketamine in a social defeat stress model. Transl. Psychiatry 7:1294. 10.1038/s41398-017-0031-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T., Santisteban M. M., Rodriguez V., Li E., Ahmari N., Carvajal J. M., et al. (2015). Gut dysbiosis is linked to hypertension. Hypertension 65 1331–1340. 10.1161/hypertensionaha.115.05315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yun Y., Kim H.-N., Kim S. E., Heo S. G., Chang Y., Ryu S., et al. (2017). Comparative analysis of gut microbiota associated with body mass index in a large Korean cohort. BMC Microbiol. 17:151. 10.1186/s12866-017-1052-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurkovetskiy L., Burrows M., Khan A. A., Graham L., Volchkov P., Becker L., et al. (2013). Gender bias in autoimmunity is influenced by microbiota. Immunity 39 400–412. 10.1016/j.immuni.2013.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J. C., Yao W., Dong C., Yang C., Ren Q., Ma M., et al. (2017). Blockade of interleukin-6 receptor in the periphery promotes rapid and sustained antidepressant actions: a possible role of gut–microbiota–brain axis. Transl. Psychiatry 7:e1138. 10.1038/tp.2017.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M., Li A., Yang Q., Li J., Wang L., Liu X., et al. (2021). Beneficial Effect of Alkaloids From Sophora alopecuroides L. on CUMS-induced depression model mice via modulating gut microbiota. Front. Cell. Infect. Microbiol. 11:665159. 10.3389/fcimb.2021.665159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y. J., Li S., Gan R. Y., Zhou T., Xu D. P., Li H. B. (2015). Impacts of gut bacteria on human health and diseases. Int. J. Mol. Sci. 16 7493–7519. 10.3390/ijms16047493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng P., Zeng B., Zhou C., Liu M., Fang Z., Xu X., et al. (2016). Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol. Psychiatry 21 786–796. 10.1038/mp.2016.44 [DOI] [PubMed] [Google Scholar]
- Zoetendal E. G., Raes J., Van Den Bogert B., Arumugam M., Booijink C. C., Troost F. J., et al. (2012). The human small intestinal microbiota is driven by rapid uptake and conversion of simple carbohydrates. ISME J. 6 1415–1426. 10.1038/ismej.2011.212 [DOI] [PMC free article] [PubMed] [Google Scholar]