Abstract
Background
Substance use disorder (SUD) is the continued use of one or more psychoactive substances, including alcohol, despite negative effects on health, functioning, and social relations. Problematic drug use has increased by 10% globally since 2013, and harmful use of alcohol is associated with 5.3% of all deaths. Direct effects of music therapy (MT) on problematic substance use are not known, but it may be helpful in alleviating associated psychological symptoms and decreasing substance craving.
Objectives
To compare the effect of music therapy (MT) in addition to standard care versus standard care alone, or to standard care plus an active control intervention, on psychological symptoms, substance craving, motivation for treatment, and motivation to stay clean/sober.
Search methods
We searched the following databases (from inception to 1 February 2021): the Cochrane Drugs and Alcohol Specialised Register; CENTRAL; MEDLINE (PubMed); eight other databases, and two trials registries. We handsearched reference lists of all retrieved studies and relevant systematic reviews.
Selection criteria
We included randomised controlled trials comparing MT plus standard care to standard care alone, or MT plus standard care to active intervention plus standard care for people with SUD.
Data collection and analysis
We used standard Cochrane methodology.
Main results
We included 21 trials involving 1984 people. We found moderate‐certainty evidence of a medium effect favouring MT plus standard care over standard care alone for substance craving (standardised mean difference (SMD) –0.66, 95% confidence interval (CI) –1.23 to –0.10; 3 studies, 254 participants), with significant subgroup differences indicating greater reduction in craving for MT intervention lasting one to three months; and small‐to‐medium effect favouring MT for motivation for treatment/change (SMD 0.41, 95% CI 0.21 to 0.61; 5 studies, 408 participants). We found no clear evidence of a beneficial effect on depression (SMD –0.33, 95% CI –0.72 to 0.07; 3 studies, 100 participants), or motivation to stay sober/clean (SMD 0.22, 95% CI –0.02 to 0.47; 3 studies, 269 participants), though effect sizes ranged from large favourable effect to no effect, and we are uncertain about the result. There was no evidence of beneficial effect on anxiety (mean difference (MD) –0.17, 95% CI –4.39 to 4.05; 1 study, 60 participants), though we are uncertain about the result. There was no meaningful effect for retention in treatment for participants receiving MT plus standard care as compared to standard care alone (risk ratio (RR) 0.99, 95% 0.93 to 1.05; 6 studies, 199 participants).
There was a moderate effect on motivation for treatment/change when comparing MT plus standard care to another active intervention plus standard care (SMD 0.46, 95% CI –0.00 to 0.93; 5 studies, 411 participants), and certainty in the result was moderate. We found no clear evidence of an effect of MT on motivation to stay sober/clean when compared to active intervention, though effect sizes ranged from large favourable effect to no effect, and we are uncertain about the result (MD 0.34, 95% CI –0.11 to 0.78; 3 studies, 258 participants). There was no clear evidence of effect on substance craving (SMD –0.04, 95% CI –0.56 to 0.48; 3 studies, 232 participants), depression (MD –1.49, 95% CI –4.98 to 2.00; 1 study, 110 participants), or substance use (RR 1.05, 95% CI 0.85 to 1.29; 1 study, 140 participants) at one‐month follow‐up when comparing MT plus standard care to active intervention plus standard care. There were no data on adverse effects.
Unclear risk of selection bias applied to most studies due to incomplete description of processes of randomisation and allocation concealment. All studies were at unclear risk of detection bias due to lack of blinding of outcome assessors for subjective outcomes (mostly self‐report). We judged that bias arising from such lack of blinding would not differ between groups. Similarly, it is not possible to blind participants and providers to MT. We consider knowledge of receiving this type of therapy as part of the therapeutic effect itself, and thus all studies were at low risk of performance bias for subjective outcomes.
We downgraded all outcomes one level for imprecision due to optimal information size not being met, and two levels for outcomes with very low sample size.
Authors' conclusions
Results from this review suggest that MT as 'add on' treatment to standard care can lead to moderate reductions in substance craving and can increase motivation for treatment/change for people with SUDs receiving treatment in detoxification and short‐term rehabilitation settings. Greater reduction in craving is associated with MT lasting longer than a single session. We have moderate‐to‐low confidence in our findings as the included studies were downgraded in certainty due to imprecision, and most included studies were conducted by the same researcher in the same detoxification unit, which considerably impacts the transferability of findings.
Keywords: Humans, Anxiety, Anxiety/therapy, Bias, Craving, Music Therapy, Substance-Related Disorders, Substance-Related Disorders/therapy
Plain language summary
Music therapy for people with substance use disorder
What was the aim of this review?
We aimed to assess if music therapy given in addition to standard care was effective for people with substance use disorders, in terms of impacting substance craving, motivation for treatment, and motivation for staying sober/clean. We were also interested in evidence about effects on depression and anxiety, as these are risk factors for relapse.
Key messages
Music therapy as 'add on' treatment to standard care likely reduces substance craving and increases motivation for treatment for adults in detoxification and rehabilitation settings. Music therapy lasting longer than a single session is associated with greater reductions in substance craving. There is no evidence of an effect on depressive symptoms, anxiety, motivation to stay sober/clean, or retention in treatment. There were no data on adverse events.
Why is it important to do this review?
This review can help determine if music therapy has a beneficial impact on certain aspects of problematic substance use and motivation for treatment.
What did this review study?
Substance use disorder is the continued use of drugs, both illegal drugs and prescription medicines, with or without alcohol, even when these substances cause health problems or negatively affect social functioning. Approximately 35 million people worldwide engage in problematic drug use, and more than three million deaths each year are attributed to the harmful consumption of alcohol. Music therapy addresses the mental and physical needs of people undergoing substance use treatment, through use of a range of active and receptive forms of musical engagement that enable various health‐promoting neurobiological, psychological, and social processes. Music therapists are health professionals who use specific music interventions to help their clients manage emotions, cope with triggers, experience mastery, and form healthy interpersonal relationships.
What were the main results of the review?
We included 21 studies with 1984 people. All participants were diagnosed with substance use disorder, with 52% reporting alcohol as their substance of choice. In two studies, participants had co‐occurring mental health diagnoses. All studies were completed in either detoxification settings or longer‐term substance use treatment facilities. Studies compared music therapy added to standard care to standard care alone or to other types of intervention that would be a typical part of treatment for substance use, such as verbal therapy. The quality of the performed trials and the reported results varied, which affected our confidence in the results.
Our findings suggest that music therapy added to standard care likely reduces substance craving when compared to standard care alone for people with substance use disorders receiving treatment in detoxification and short‐term rehabilitation settings. Music therapy intervention lasting longer than a single session is associated with greater reduction in craving. Furthermore, music therapy likely improves motivation for treatment/change more than standard care alone, and may improve motivation for treatment/change more than other active treatments. We found no evidence of an effect of music therapy on depressive symptoms, anxiety, and motivation to stay sober/clean.
We have low‐to‐moderate confidence in our findings, and caution that it might be difficult to transfer our findings to other settings, since most included studies were conducted by the same researcher in the same detoxification unit.
We know that substance craving is diminished better when there is more than one session of music therapy, but we do not know if the number of music therapy sessions received impacts other outcomes. Additionally, we do not know if one form of music therapy works better than others for these outcomes.
Only one study reported a source of funding (National Key R&D Program of China, primary funder).
How up‐to‐date is this review?
This evidence is current to 1 February 2021.
Summary of findings
Summary of findings 1. Music therapy plus standard care versus standard care alone for people with substance use disorders.
| Music therapy plus standard care versus standard care alone for people with substance use disorders | ||||||
|
Patient or population: people with substance use disorders Setting: detox and inpatient/outpatient rehabilitation settings Intervention: music therapy plus standard care Comparison: standard care alone | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with standard care | Risk with music therapy | |||||
|
Psychological symptoms (depression) Assessed with: various scales Scale: various (higher score worse) Follow‐up: end of treatment |
— | Mean depression in music therapy was 0.33 standard deviations lower (0.72 lower to 0.07 higher) |
— | 100 (3 RCTs) | ⊕⊕⊕⊝ Moderatea |
— |
|
Psychological symptoms (anxiety) Assessed with: Self‐report Anxiety Scale Scale: 20–80 (higher score worse) Follow‐up: end of treatment |
The mean anxiety score for standard care was 46.1 | Music therapy was 0.17 lower (4.39 lower to 4.05 higher) |
— | 60 (1 RCT) | ⊕⊕⊝⊝ Lowb |
— |
|
Substance craving Assessed with: Scale: various (higher score worse) Follow‐up: end of treatment |
— | Mean substance craving in music therapy was 0.66 standard deviations lower (1.23 lower to 0.10 lower) |
— | 254 (3 RCTs) | ⊕⊕⊕⊝ Moderatea |
— |
|
Motivation for treatment/change Assessed with: various scales Scale: various (higher score better) Follow‐up: end of treatment |
— | Mean motivation for treatment in music therapy was 0.41 standard deviations higher (0.21 higher to 0.61 higher) |
— | 408 (5 RCTs) | ⊕⊕⊕⊝ Moderatea |
— |
|
Motivation to stay sober/clean Assessed with: various scales Scale: various (higher score better) Follow‐up: end of treatment |
— | Mean motivation for sobriety in music therapy was 0.22 standard deviations higher (0.02 lower to 0.47 higher) |
— | 269 (3 RCTs) | ⊕⊕⊕⊝ Moderatea |
— |
|
Retention in treatment Assessed with: number participants retained at end of treatment |
Study population | RR 0.99 (0.93 to 1.05) | 199 (6 RCTs) | ⊕⊕⊕⊝ Moderatea |
Higher retention better. | |
| 725 per 1000 | 718 per 1000 (674 to 761) | |||||
| Serious adverse events | — | — | — | — | — | No studies reported serious adverse events. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio. | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level for imprecision: optimal information size not met. bDowngraded two levels for imprecision: very low sample size.
Summary of findings 2. Music therapy plus standard care compared to active intervention plus standard care.
|
Patient or population: people with substance use disorders Setting: detox and inpatient/outpatient rehabilitation settings Intervention: music therapy plus standard care Comparison: active intervention plus standard care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with active intervention | Risk with music therapy | |||||
|
Psychological outcomes (depression) Assessed with: Beck Depression Inventory Scale: 0–63 (higher score worse) Follow‐up: end of treatment |
Mean depression for active intervention was 20.3 | Music therapy was 1.49 lower (4.98 lower to 2.00 higher) |
— | 110 (1 RCT)a | ⊕⊕⊕⊝ Moderateb |
— |
|
Substance craving Assessed with: various scales Scale: various (higher score worse) Follow‐up: end of treatment |
— | Mean substance craving in music therapy was 0.04 standard deviations lower (0.56 lower to 0.48 higher) |
— | 232 (3 RCTs)a | ⊕⊕⊝⊝ Lowb,c |
— |
|
Motivation for treatment/change Assessed with: various scales Scale: various (higher score better) Follow‐up: end of treatment |
— | Mean motivation for treatment in music therapy was 0.46 standard deviations higher (0 lower to 0.93 higher) |
— | 411 (5 RCTs)a | ⊕⊕⊕⊝ Moderateb |
— |
|
Motivation to stay sober/clean Assessed with: Likert Scale: 1–7 (higher score better) Follow‐up: end of treatment |
Mean motivation to stay sober in active intervention ranged from 6.2 to 6.4 | Music therapy was 0.34 higher (0.11 lower to 0.78 higher) |
— | 258 (3 RCTs)a | ⊕⊕⊕⊝ Moderateb |
— |
| Retention in treatment | — | — | — | — | — | No studies reported retention in treatment. |
| Serious adverse events | — | — | — | — | — | No studies reported serious adverse events. |
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aNumber of participants adjusted for cluster randomisation. bDowngraded one level for imprecision: optimal information size not met. cDowngraded one level for inconsistency: substantial heterogeneity (I2 = 70%) likely affecting interpretation of results and with no plausible explanation.
Background
Description of the condition
Problematic substance use and related high‐risk behaviour have a negative impact on individuals, families, and global public health. The burden of problematic substance use to systems such as healthcare, criminal justice, and unemployment/welfare is substantial (WHO 2018). The World Health Organization (WHO) Global Status Report on Alcohol and Health 2018 cited 3.0 million deaths in 2016 were attributable to the harmful use of alcohol, representing 5.3% of all deaths (WHO 2018, p.63). In addition, 5.1% of the global burden of disease, expressed as 132.6 million net disability‐adjusted life years, can be attributed to alcohol consumption (WHO 2018, p.64). Problematic use of drugs and alcohol is a widespread issue; approximately 35.6 million people worldwide experienced drug use disorder in 2018, amounting to 0.62% of the adult population (aged 15 to 64 years) (UNODC 2020), and 4.9% of the world's population aged 15 years or older demonstrated either harmful use of alcohol or alcohol dependence (WHO 2018). While both the number of deaths related to alcohol use and the number of people engaging in harmful alcohol consumption appear to have stabilised from 2013 to 2018, the number of people engaging in problematic drug use increased by approximately 10% since 2013 (UNODC 2018). This increase is mainly attributed to the increase in opioid use, where global opium production has more than doubled between 2015 and 2017 (UNODC 2018). Opioids also continue to cause the most harm, as 66% of deaths that are directly drug‐related are caused by opium and its derivatives (UNODC 2020).
Substance use disorders (SUDs) may be defined as the use of one or more psychoactive substances, medically prescribed or not (WHO 1994), in a manner that results in continued use despite significant substance‐related problems in areas of the person's cognitive, behavioural, physiological, or social functioning (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM‐5), APA 2013). People who inject drugs are at higher risk of death. This harm is partly due to fatal overdoses or the transmission of lethal infectious diseases (UNODC 2018). More than half of people who inject drugs live with hepatitis C and approximately 12% of them are diagnosed with HIV (UNODC 2018). Worldwide, an estimated one in every six people with problematic drug use receives necessary treatment; if all people with problematic drug use sought treatment, the resulting cost would represent 0.3% to 0.4% of the global gross domestic product (INCB 2019). Although the economic burden of treatment is considerable, the costs of crime‐related law enforcement and judiciary services and healthcare provision for untreated problematic drug use remain far higher than that of prevention and treatment (INCB 2019).
Research‐based principles of substance use addiction treatment suggest that SUD is a complex but treatable disease (NIDA 2018). Successfully treating people who have SUDs demands a diversity of treatment procedures and areas of treatment focus, due to the diversity of personal characteristics and substance(s) used. Treatment must meet the complex biopsychosocial needs of the person involved, and thus must be multidisciplinary in nature. Longer lengths of residential substance use treatment are associated with better engagement in aftercare programmes and lower levels of substance use at long‐term follow‐up (Arbour 2011; Moos 2007). Improved treatment retention also predicts lower recidivism rates in criminally convicted individuals with co‐occurring substance use and mental health disorders (Jaffe 2012). Supporting retention in multidisciplinary treatment remains a crucial aspect of addressing the harms caused by SUDs, but at the same time remains one of the greatest challenges. In the USA, approximately 26% of people with problematic substance use drop out of public treatment programmes (SAMHSA 2019). People with problematic substance use who have co‐occurring mental health disorders demonstrate even lower treatment retention rates. Gender‐specific retention strategies are an important means of promoting treatment retention among people with problematic substance use with co‐occurring mental health disorders (Choi 2015).
People with SUDs often experience emotional dysfunction, which can contribute to the development of the disorder. People with SUDs commonly experience co‐occurring affective disorders such as depression and anxiety (London 2004), as well as post‐traumatic stress disorder (Ouimette 2005; van Dam 2012). In addition, people with SUDs demonstrate dysfunction in emotion regulation, such as dampened inhibition of intense affects and abnormal emotional reactions to emotional stimuli (Chen 2018; O'Daly 2012; Wilcox 2016). Research demonstrates functional changes in emotion‐related brain areas in people with SUDs, including abnormalities in the activation of the insula and amygdala, as well as hypoactivity in the anterior cingulate cortex and ventromedial prefrontal cortex (Gilman 2008; Salloum 2007).
Description of the intervention
Music therapy (MT) is "the systematic use of specific musical interventions (based upon musical, aesthetic, clinical, scientific, and practice‐based research as well as tacit knowledge) by an accredited music therapist to realise individual treatment goals within a therapeutic alliance" (NVvMT 2017, pp.11–12). In MT, therapeutic change occurs via engagement in musical experiences and by the relationships that develop through them (Bruscia 1998). Music therapists engage participants in a range of active and receptive approaches to listening to, discussing, creating, improvising, and performing music. MT may incorporate varying levels of verbal processing, depending upon the needs of the participant(s) and the theoretical orientation of the music therapist. Sessions can occur with individuals, groups, or with communities, and may include various approaches such as songwriting; discussion and analysis of song lyrics; instrumental or vocal improvisation, or both; music performance; and music‐assisted relaxation. MT may be practised from a variety of theoretical orientations, and in the setting of substance use treatment may include elements of cognitive‐behavioural; humanistic; psychodynamic or neurobiological theory, or both; among others. MT is an integrated part of multidisciplinary substance use treatment in many countries. Music therapists work within abstinence‐based, controlled use, and harm reduction contexts (Aldridge 2010; Ghetti 2004), in inpatient treatment centres, community mental health centres, adult day and ambulant healthcare centres, state and general hospitals, therapeutic communities, and aftercare programmes (Aldridge 2010; Ghetti 2004; Silverman 2009).
The modern profession of MT began in the 1940s and 1950s, with the establishment of academic and clinical training programmes in the USA, Austria, and the UK, followed by developments in other parts of Europe, North and South America, Africa, Australia, and Asia (Bunt 2014). The academic preparation required for professional practice currently varies by country, although many countries require master's level training in MT.
How the intervention might work
MT addresses the biopsychosocial needs of people undergoing multidisciplinary substance use treatment. Various forms of engagement in musical experiences are systematically and intentionally employed by music therapists to trigger specific neurological, biological, psychological, and social mechanisms. Music therapists understand and utilise the various ways that music induces emotions, including via brain stem reflexes, rhythmic entrainment, evaluative conditioning, emotional contagion, visual imagery, episodic memory, musical expectancy, and aesthetic judgement (Juslin 2013; Juslin 2019). This emotional activation and improved emotion regulation can then lead to increased motivation and sustained engagement in the therapeutic music process, enabling progress towards therapeutic goals (Bruscia 2014). MT approaches are sequenced over time in direct relation to participants' needs and readiness, building upon their resources (Rolvsjord 2010) and introducing therapeutic challenges when appropriate (Bruscia 2014).
Music therapy as emotion regulation
Music therapists are informed by an awareness of the neurobiological impacts of music on human emotions, and consider this level of influence as they engage with participants in music‐making. At a neurobiological level, music that provokes peak experiences stimulates neural reward and emotion systems similar to those that are activated by (illicit) drug use (Blood 2001), which can result in dopamine release (Salimpoor 2011). Owing to these patterns of neural activity, music can be shaped by a qualified music therapist to promote positive mood states, including euphoria, and to enable emotion regulation (Hakvoort 2020; Koelsch 2015; Salimpoor 2011; Sena Moore 2013). As music provides a means of promoting positive mood states (Koelsch 2014), it may consequently buffer against the risk of relapse that is associated with negative mood states (Koob 2013). Furthermore, pleasurable music can promote the release of dopamine to positively affect the reward system (Blum 2010), and can inhibit activity in areas of the limbic system in a way that inhibits transmission of pain perception (Neugebauer 2004). Music therapists intentionally utilise musical experiences to enable these mechanisms of emotion regulation, reward, and pain relief.
People with SUD often use substances as a strategy for coping with difficult emotions. In addition to impacting neurological systems associated with emotion regulation and reward, MT enables the development of a broader and more flexible array of strategies for coping with emotions (Dijkstra 2010). MT offers a means for expressing and working through a broad range of emotions in an adaptive way, which is particularly helpful for participants who have difficulty expressing emotions verbally (Baker 2007). Some participants may need to experience and work through emotions non‐verbally as a prerequisite to being able to benefit from verbal forms of therapy.
Music therapy and substance craving
Since music readily acts upon neural activity, special consideration is necessary when using music therapeutically in people with SUDs. Individuals with SUDs can experience a decrease in substance craving after listening to songs they identify as helping them stay clean/sober, but they may also experience an increase in substance craving after listening to songs they identify as making them want to use substances (Short 2015). Thus, important aims of MT within substance use treatment include gaining awareness of healthy and unhealthy uses of music, and understanding how context impacts perception of the music (Hohmann 2017; McFerran 2016). Furthermore, strong personal associations between music and substance use, some of which can contribute to relapse when left unexamined, can be successfully addressed and reversed in MT (Horesh 2010). Individuals learn to recognise, retrain, and integrate state‐specific emotional responses to music as part of their lifestyle (Fachner 2017).
Music therapy for motivation
People with SUDs who participate in MT may experience increased motivation to engage in treatment, which may then generalise to other facets of substance use treatment (Hohmann 2017; Horesh 2010). Gains in motivation for change are also evident in people with co‐occurring mental health disorders who engage in MT (Ross 2008). Motivation for treatment may be understood in terms of the distinct dimensions of readiness and resistance, where readiness represents the level of interest in and commitment to substance use treatment, and resistance represents scepticism towards the potential benefits of treatment or opposition to engaging in treatment (Longshore 2006). The degree of readiness serves as a significant predictor of treatment retention, while the level of resistance predicts actual drug use (Longshore 2006). Promoting treatment retention as a means of enabling better overall outcomes therefore requires improving readiness for treatment and reducing resistance to treatment.
Music therapy for social engagement
MT provides a broad range of effects for people with SUDs, from neurobiological to social and cultural levels (Aldridge 2010). The social and interpersonal benefits of engaging in music provide communal experiences that offer opportunities for connection and expression, while also enabling coping, stress reduction, and re‐activation. MT in group settings enables participants to become aware of maladaptive coping and interpersonal patterns, to have these challenged within a supportive context, and to practice new ways of relating to their emotions and to other people (Dijkstra 2010). Participants who have difficulty forming relationships with others may find that MT offers a non‐verbal means of being with and relating to others. Expansion of positive social experiences through MT can be an essential factor in increasing motivation for continued treatment.
In summary, MT has a direct neurobiological impact on areas of the brain implicated in substance use, including emotion regulation and reward. MT also indirectly impacts substance use behaviour by supporting social engagement, improving coping skills, and increasing motivation for treatment. As a large number of people with SUD also have co‐occurring mental health disorders, the effects of MT for mental health disorders may have relevance in the context of substance use treatment. Active engagement in MT can alleviate anxiety and depression in people with serious mental health disorders (Geretsegger 2017), and those with depression, where it can also improve global functioning (Aalbers 2017). A reduction in depression and anxiety, and improvement in social, occupational, and psychological functioning may then improve adherence to treatment and enable better outcomes for substance users. By motivating engagement in treatment, facilitating development of therapeutic rapport, and musically approaching strong emotions as a means of expanding coping skills (Dijkstra 2010; Ghetti 2013) and attention span (van Alphen 2019), MT may promote readiness for treatment and reduce resistance, while also equipping people with emotional, interpersonal, cognitive, and musical skills that can help them positively manage their SUD.
Why it is important to do this review
MT is used as a non‐pharmacological psychotherapeutic intervention in a variety of multidisciplinary substance use treatment settings ranging from acute‐phase treatment for detoxification through community aftercare programmes for people with SUDs (Aldridge 2010; Silverman 2009). Individual studies demonstrate improvements in motivation to engage in treatment and reduction in psychological symptoms (Albornoz 2011; Silverman 2012). Previous systematic reviews of MT for SUDs are either out of date or did not include quantitative meta‐analysis of study outcomes (Carter 2020; Hohmann 2017; Mays 2008; Megranahan 2018; Silverman 2003). Due to the increasing volume of international research into MT for SUDs, and the need to establish an evidence base for practice and policy, a rigorous and comprehensive systematic review of randomised controlled trials (RCTs) specific to MT within multidisciplinary treatment is warranted.
Objectives
Main objective
To compare the effect of music therapy (MT) in addition to standard care versus standard care alone, or to standard care plus an active control intervention, on psychological symptoms, substance craving, motivation for treatment, and motivation to stay clean/sober.
Secondary objective
To assess the impact of the number of MT sessions on study outcomes.
Methods
Criteria for considering studies for this review
Types of studies
RCTs, including the first phase of cross‐over trials, and cluster‐RCTs.
Types of participants
People with problem substance use, with a formal diagnosis of SUD. Substances considered were illicit drugs, medication, and alcohol. We excluded nicotine addiction, due to the dissimilar impact on social and functional domains. We excluded non‐substance addiction (e.g. Internet addiction, gambling addiction). Diagnosis of SUD was based upon diagnostic criteria from Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM‐IV‐TR; APA 2000) or DSM‐5 (APA 2013), and from the International Classification of Diseases 10th Version: Online 2019 (ICD‐10) (WHO 2019), codes F10 to F16 (mental and behavioural disorders due to psychoactive substance use) (with the exclusion of caffeine (part of F15)), and F18 to F19 (mental and behavioural disorders due to use of volatile solvents or multiple drug use and use of other psychoactive substances). There were no restrictions by age or other participant characteristics, thus we included both adolescents and adults. Participants could have been dual‐diagnosed with mental health problems or learning problems. Participants could have received intervention in inpatient, outpatient, therapeutic community, or supportive aftercare settings.
Types of interventions
Experimental intervention
Music therapy added to standard care
To be included, the intervention must have been labelled 'music therapy', and conducted by a qualified music therapist. MT involves a music therapist and one or more participants, engaging in specifically created music experiences to help them achieve their highest potentials of health (Bruscia 2014). MT interventions could have consisted of a variety of receptive or active approaches that use music to promote therapeutic change. Receptive approaches could have included listening to music as a basis for guided discussion and examination of feelings and thoughts or to impact mood, as well as other aims. Active approaches could have included opportunities for the participant to interact with music and music‐making processes through songwriting, singing, or playing instruments. We included both individual and group MT interventions. MT could have been offered as a part of multidisciplinary substance use treatment, and could have been practised from an integrated treatment orientation (e.g. cognitive behaviour therapy). MT could have been any length of session and course of treatment.
Control intervention
Standard care alone
Standard care represented treatment as usual, and included any conventional treatment (including pharmacotherapy) offered at the treatment setting as long as that treatment did not involve MT. Examples of services offered as part of standard care for SUDs include: psychotherapy, relapse prevention counselling, peer‐led groups including 12‐step programmes, case management, pharmacological detoxification, pharmacotherapy including methadone maintenance treatment, and recreational and sports activities. Wait‐list control occurred in conjunction with standard care, and consisted of participants assigned to a waiting list to receive MT after the active treatment group.
Active control intervention
Participants allocated to an active control intervention received a structurally equivalent condition that lasted the same duration as the MT intervention and controlled for non‐specific effects of the therapist's presence and attention, presence of the music, or presence of some other therapeutic element. Only participants assigned to the active control intervention received this particular intervention. An example of an active control intervention is verbal therapy that is provided in addition to standard care, and consists of discussion of themes related to motivation for change, relapse prevention, and managing substance use triggers. In this case, verbal therapy serves to control for the presence of the therapist and the discussion of treatment‐related themes, but it lacks a key proposed element of therapeutic change, namely musical engagement.
Types of comparisons
MT plus standard care versus standard care alone.
MT plus standard care versus standard care plus another active intervention.
Types of outcome measures
Outcomes could have been measured and reported either dichotomously or continuously. Data sources could have included both standardised and non‐standardised instruments. We included data from rating scales when they were from participant self‐report or rated by an independent evaluator (i.e. not the music therapist).
Primary outcomes
Psychological symptoms (e.g. depression, anxiety, anger; e.g. measured by Beck Depression Inventory (BDI; Beck 1996), Hamilton Rating Scale for Depression (HRSD; Hamilton 1960), state portion of the State‐Trait Anxiety Inventory (STAI), or visual analogue scales).
Substance craving (e.g. measured by Brief Substance Craving Scale (BSCS; Somoza 1995), or visual analogue scales).
Motivation for treatment/change (e.g. measured by Readiness to Change Questionnaire (RTCQ; Heather 1999), Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES; Miller 1996), University of Rhode Island Change Assessment Scale (URICA; McConnaughy 1983), or visual analogue scales).
Motivation to stay sober/clean (e.g. measured by Commitment to Sobriety Scale (CSS; Kelly 2014), or visual analogue scales).
We collected outcomes reported immediately following completion of the intervention, short‐term follow‐up up to three months after completion of the intervention, and long‐term follow‐up at more than three months after completion of the intervention.
Secondary outcomes
Alcohol or substance use, or both, in terms of amount, frequency, or peak use (as measured by self‐report, report by independent evaluators, urine analysis, or blood samples, as appropriate).
Retention in treatment (as measured by number of participants remaining in treatment at the end of the study).
Severity of substance dependence/use, as measured by validated scales (e.g. Addiction Severity Index (ASI; McLellan 1992), Drinking Inventory Consequences (DrInC; NIAA 2003), or the Severity of Dependence Scale (SDS; Gossop 1995)).
Serious adverse events (e.g. relapse requiring hospitalisation, suicide attempts, or suicide).
We measured serious adverse events as a binary variable related to the presence or absence of adverse events, including relapse requiring hospitalisation, suicide attempts, or suicide.
Search methods for identification of studies
Electronic searches
The electronic searches included the following databases:
the Cochrane Drugs and Alcohol Group's Specialised Register of Trials (1 February 2021);
the Cochrane Central Register of Controlled Trials (CENTRAL, Issue 1 2021);
MEDLINE (PubMed) (January 1966 to 1 February 2021);
Embase (embase.com) (January 1974 to 1 February 2021);
CINAHL (EBSCOhost) (1982 to 1 February 2021);
ERIC (eric.ed.gov) (1964 to 8 February 2021);
ISI Web of Science (1 February 2021);
PsycINFO (EBSCOhost) (1872 to 1 February 2021);
International Bibliography of the Social Sciences (IBSS) (1951 to 8 February 2021);
ProQuest Dissertations & Theses (1997 to 8 February 2021);
Google Scholar (8 February 2021, first 100 hits).
We searched the following trials registries on 30 January 2021:
ClinicalTrials.gov (www.clinicaltrials.gov);
WHO International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/).
We imposed no restrictions by language, date, gender, age, or tag terms. See Appendix 1 for search terms used in strategies for this review.
Searching other resources
Handsearching and reference searching
We handsearched the reference lists of all included studies. We also examined the reference lists of relevant review articles (e.g. Hohmann 2017; Mays 2008; Megranahan 2018; Silverman 2003).
Data collection and analysis
Selection of studies
We used the Covidence software platform for citation screening, including merging search results and removing duplicates, and for full‐text review (Covidence). Two review authors and content area experts (XJC, CGh) independently examined each title and abstract to remove obviously irrelevant reports, and a third review author (LH or CGo) resolved disagreements. We then obtained full texts for all potentially relevant reports, and linked multiple reports of the same study, when applicable. Two review authors (XJC, CGh) independently examined each full‐text report to determine eligibility, and resolved disagreements in consultation with two other review authors (LH, CGo). We contacted study investigators when necessary, to clarify study eligibility. We illustrated the study selection process in a PRISMA diagram (Figure 1).
1.
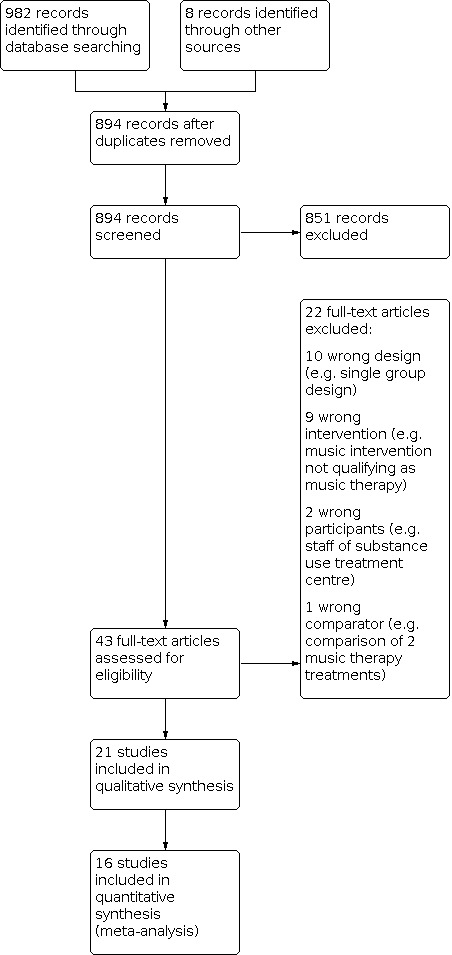
PRISMA Flow Diagram
Data extraction and management
Two review authors (XJC, CGh) independently performed data extraction using Covidence (Covidence), and exported data to Review Manager Web (RevMan Web 2021). When necessary, we contacted study investigators to obtain missing data. We resolved disagreements in consultation with two review authors (LH, CGo), and archived their content and resolution. We extracted information from each study regarding:
methods (including design and aspects related to assessing risk of bias);
country and setting;
characteristics and number of participants;
characteristics of experimental and comparison groups, including the number of participants allocated to each, and length of MT in minutes/hours/sessions;
outcomes and time points;
results;
funding of the study;
conflict of interest of study authors.
Assessment of risk of bias in included studies
Two review authors (XJC, CGh) independently assessed risks of bias using the Cochrane risk of bias tool (Higgins 2011), in conjunction with the Covidence software platform (Covidence). We resolved disagreements by consulting two review authors (AB, CGo). The first part of the tool describes what was reported to have happened in the study, while the second part assigns a judgement relating to the risk of bias for that entry, as low, high, or unclear risk. We made such judgements using the criteria indicated by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), adapted to the addiction field. Appendix 2 includes a detailed description of the risk of bias criteria that we used. The eight domains include:
sequence generation (selection bias);
allocation concealment (selection bias);
blinding of participants and providers (performance bias) (objective outcomes);
blinding of outcome assessors (detection bias);
incomplete outcome data (attrition bias);
selective outcome reporting (reporting bias);
blinding of participants and providers (performance bias) (subjective outcomes);
blinding of outcome assessors (detection bias) (subjective outcomes).
We considered blinding of participants and providers, and blinding of outcome assessors (avoidance of performance bias and detection bias) separately for objective outcomes (e.g. alcohol or substance use, or both, as measured by urine analysis or blood samples; retention in treatment; serious adverse events) and subjective outcomes (e.g. psychological symptoms, substance craving, motivation for treatment/change, motivation to stay sober/clean, participant self‐report of substance use, participant self‐report of severity of substance dependence/use). We assessed incomplete outcome data for each outcome (avoidance of attrition bias), with the exception of 'retention in treatment'. We included all eligible studies, regardless of the level of the risks of bias, when presenting main findings for each outcome; however, we discussed the risks of bias and provide a cautious interpretation within the Discussion and Authors' conclusions sections of the review. We rated a study as being at a high risk of attrition bias when attrition was greater than 20%.
Measures of treatment effect
We assessed serious adverse events and retention in treatment at the end of treatment, while we measured efficacy measures at three different time points: immediately post‐intervention, short‐term follow‐up (up to three months after completion of the intervention), and long‐term follow‐up (more than three months after completion of the intervention).
Dichotomous data
We calculated the risk ratio (RR) and corresponding 95% confidence interval (95% CI) for dichotomous data.
Continuous data
For continuous data from parallel‐group and cluster‐randomised RCTs, we selected the mean and standard deviation (SD) endpoint data for experimental and control groups. When outcomes were measured on the same scale or could be transferred to the same scale in all studies, we calculated the mean difference (MD) on the original metric. When studies used different scales to measure the same outcome, we calculated the standardised mean difference (SMD) and corresponding 95% CI for continuous outcomes.
Unit of analysis issues
Cross‐over trials
When appropriate, we planned to combine results of cross‐over trials with those of parallel‐group trials, analysing data from the first phase only (i.e. before cross‐over) to avoid carry‐over effects.
Cluster‐randomised trials
When studies accounted for clustering in their analysis, inclusion of the data in meta‐analysis was straightforward. When clustering was not accounted for in an included study, we attempted to contact the study investigators to obtain the intraclass correlation coefficient (ICC) of their clustered data. When we could not obtain the ICC, we used external estimates from similar studies (Higgins 2011). If no such estimates were available, we assumed ICC = 0.05; this is likely to lead to conservative estimates as lower values than that are typical (Higgins 2011, Section 16.3.4).
Studies with multiple treatment groups
When studies had more than one relevant MT intervention, we planned to combine all such experimental groups into a single group, as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
We followed intention‐to‐treat principles and included all known data from all randomised participants. We used the following sensitivity analyses to examine the impact of missing data. For continuous outcomes, we planned to remove studies with high attrition (more than 20%). For dichotomous outcomes, we assumed that the unobserved cases had a negative outcome. We reported on the potential impact of missing data when assessing risks of bias.
Assessment of heterogeneity
If the number of included studies is low or studies have small sample size, or both, statistical tests for heterogeneity may have low power and be difficult to interpret (Higgins 2011). We conducted descriptive analyses of heterogeneity by visually examining forest plots for consistency of results and by calculating the I2 statistic, which represents the percentage of effect estimate variability that is due to heterogeneity instead of sampling error (Higgins 2011). We planned to supplement the I2 statistic with a calculation of the Chi2 statistic to assess the likelihood that the heterogeneity was genuine, and to consider possible sources of heterogeneity.
Assessment of reporting biases
We planned to test for asymmetry of funnel plots when there were at least 10 studies in a meta‐analysis, and to explore likely reasons for asymmetry when it was present. However, none of our meta‐analyses contained a sufficient number of studies to warrant assessment of asymmetry.
Data synthesis
We combined the outcomes from the individual trials through meta‐analysis where possible (comparability of intervention and outcomes between trials), using a random‐effects model, because we expected a certain degree of heterogeneity among trials. In cases where meta‐analysis was not appropriate, we reported results for each individual study.
Subgroup analysis and investigation of heterogeneity
Heterogeneity in the included studies was interpreted in accordance with the approximate guide for interpretation of the I2 statistic provided in the Cochrane Handbook for Systematic Reviews of Interventions (Section 9.5.2; Higgins 2011). Heterogeneity of 0% to 40% was considered to most likely not be important, 30% to 60% was considered moderate heterogeneity, 50% to 90% substantial heterogeneity, and 75% to 100% considerable heterogeneity.
When there was significant heterogeneity, we planned to use subgroup analyses to examine the impact of the number of sessions, type of substance, and presence of dual‐diagnosis (i.e. SUD and mental disorder). For subgroup analysis of the number of sessions, we planned to use the following cut‐off points for respective subgroups: three sessions or more versus one or two sessions for outcomes that might show an effect of short intervention, such as are found in detoxification settings (i.e. retention in treatment, reduction in psychological symptoms, improvement in motivation for treatment/change, substance craving); and 10 or more sessions versus fewer than 10 sessions for outcomes typically requiring longer‐term treatment, such as those within rehabilitation settings (i.e. reduction in substance use, severity of substance dependence/use, cessation of substance use, serious adverse events).
Sensitivity analysis
We planned to perform a sensitivity analysis of the review outcomes, removing trials with high attrition rates (i.e. studies with attrition rates higher than 20%), as unequal attrition from studies may indicate unsatisfactory or intolerable treatment.
Summary of findings and assessment of the certainty of the evidence
Grading of the evidence
We assessed the overall certainty of the evidence for the primary outcome using the GRADE system. The GRADE Working Group developed a system for grading the certainty of evidence, which takes into account issues related both to internal and external validity, such as directness, consistency, imprecision of results, and publication bias (Atkins 2004; Guyatt 2008; Guyatt 2011).
The GRADE system uses the following criteria for assigning grades of evidence:
high: we are very confident that the true effect lies close to that of the estimate of the effect;
moderate: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different;
low: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect;
very low: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
Grading is decreased for the following reasons:
serious (–1) or very serious (–2) study limitation for risk of bias;
serious (–1) or very serious (–2) inconsistency between study results;
some (–1) or major (–2) uncertainty about directness (the correspondence between the population, the intervention, or the outcomes measured in the studies actually found and those under consideration in our systematic review);
serious (–1) or very serious (–2) imprecision of the pooled estimate;
publication bias strongly suspected (–1).
Summary of findings table
We included summary of findings tables to present the main findings of the review in a transparent and simple tabular format. The summary of findings tables include:
main findings from the primary outcomes: psychological symptoms, substance craving, motivation for treatment/change, motivation to stay sober/clean; and findings from outcomes that might reflect undesirable effects: retention in treatment, and serious adverse events;
a measure of the typical burden of these outcomes (e.g. illustrative comparative risk);
absolute and relative magnitude of effect;
number of participants and studies addressing these outcomes;
a rating of the overall certainty of evidence for each outcome;
space for comments.
We used GRADEprofiler (GRADEpro) to assist in the preparation of the summary of findings tables (GRADEpro GDT).
Results
Description of studies
See: Characteristics of included studies and Characteristics of excluded studies tables.
Results of the search
Electronic searches of the 11 databases (see Electronic searches) retrieved 982 records. We identified two additional studies that met inclusion criteria by handsearching systematic reviews and contacting authors. Our searches of the trials registers identified six eligible records. Our screening of the reference lists of the included publications did not reveal additional RCTs. Therefore, we had 990 records.
Once duplicates had been removed, we had 894 records. We excluded 851 records based on titles and abstracts. We obtained the full text of the remaining 43 records. We excluded 22 studies (see Characteristics of excluded studies table). We identified no studies awaiting classification or ongoing studies.
We included 21 studies reported in 23 references in the qualitative synthesis, and 16 of those in quantitative synthesis (meta‐analysis). For a further description of our screening process, see the study flow diagram (Figure 1).
Included studies
We included 21 studies (1984 participants), all of which used a parallel design and offered MT in addition to standard care. Fifteen studies were cluster‐RCTs (Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2012; Silverman 2014; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2017; Silverman 2019a; Silverman 2019b; Silverman 2020; Silverman 2021). Eleven studies had two arms and compared MT plus standard care to standard care alone (Albornoz 2009; Heiderscheit 2005; James 1988; Murphy 2008; Silverman 2012; Silverman 2015b; Silverman 2016b; Silverman 2019b; Silverman 2020; Silverman 2021; Wu 2020), or to an active control intervention (i.e. verbal therapy) (Silverman 2009; Silverman 2010; Silverman 2011a). Five studies had three arms, either comparing MT plus standard care to another active intervention plus standard care and to standard care alone (Eshaghi Farahmand 2020; Silverman 2014; Silverman 2017), or comparing MT plus standard care to two active interventions plus standard care (Silverman 2011b; Silverman 2015a; Silverman 2019a). One study had four arms comparing two MT interventions to two active control interventions (Silverman 2016a).
Full description of the included studies is provided in the Characteristics of included studies table, and a summary of study characteristics is described below.
Participants
Participants in all included studies met criteria for diagnosis of SUD. Studies confirmed diagnosis according to DSM‐IV or ICD‐10 criteria in the study report. In cases where such information was lacking, study investigators confirmed diagnosis via email (Albornoz 2009; Heiderscheit 2005; Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2012; Silverman 2014; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2017). In addition to SUD, participants in Albornoz 2009 were diagnosed with comorbid depression, and in Heiderscheit 2005 most had comorbid mental health diagnoses.
The participants' substances of choice were varied, including alcohol, cocaine, heroin, and prescription drugs. Fourteen studies reported on substance of choice with weighted means across the studies of 51.6% alcohol, 30.1% heroin, 14.7% prescription tablets, 1.6% cocaine/crack, and 10.8% other drugs (Heiderscheit 2005; Silverman 2011b; Silverman 2012; Silverman 2014; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2017; Silverman 2019a; Silverman 2019b; Silverman 2020; Silverman 2021; Wu 2020).
Ages of participants were heterogeneous across studies but mainly included adults older than 18 years. One study included adolescents only (James 1988), while a second included both adolescents and adults with an age range of 16 to 60 years (Albornoz 2009). In the studies including adults only, weighted mean age across studies was 38.8 years with mean ages ranging from 34.9 years (Silverman 2020) to 55.9 years (Heiderscheit 2005).
Two studies recruited only males (Albornoz 2009; Eshaghi Farahmand 2020), and one study recruited only females (Wu 2020). The rest of the studies included both males and females. Weighted mean percentage of males across studies including both men and women was 55%, with studies ranging from 43.9% (Silverman 2009) to 78.9% (Heiderscheit 2005).
Two studies reported number of years of substance use: Heiderscheit 2005 reported a range of substance use from one year to 44 years and mean 20.8 (SD 10.9) years, and Wu 2020 reported mean 5.41 (SD 2.1) years. Fifteen studies reported the number of times that participants were admitted to a rehabilitation/detoxification facility ranging from once to nine times (Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2012; Silverman 2014; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2017; Silverman 2019a; Silverman 2019b; Silverman 2020; Silverman 2021).
All studies with the exception of four (Albornoz 2009; Eshaghi Farahmand 2020; James 1988; Wu 2020) reported on race of participants. Across studies reporting participant race, all of which took place in the USA, a weighted mean of 82.7% of participants identified as Caucasian (assumed to be white people), 5.1% African American, 5% Native American, and 8.7% other race. Two studies documented level of education: Heiderscheit 2005 reported 89% of participants held at least a high school degree, and Wu 2020 reported mean 10 (SD 1.6) years of education.
Setting
Fifteen studies occurred in a short‐term inpatient detoxification setting (Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2012; Silverman 2014; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2017; Silverman 2019a; Silverman 2019b; Silverman 2020; Silverman 2021), two in a residential substance use treatment facility (Murphy 2008; Wu 2020), one in a chemical dependency treatment programme within a residential health facility (Heiderscheit 2005), and two in facilities offering inpatient and outpatient substance use treatment (Albornoz 2009; Eshaghi Farahmand 2020). One study took place in China (Wu 2020), one in Iran (Eshaghi Farahmand 2020), and one in Venezuela (Albornoz 2009), with the remaining studies taking place in the USA.
Sample size
There were 1984 participants in the 21 included studies. Sample size in individual studies ranged from 19 (Heiderscheit 2005) to 144 (Silverman 2016b). In the analyses, we reduced the effective sample size of three cluster‐RCTs where there was no adjustment for clustering (Silverman 2009 – 16 clusters; Silverman 2011a – 28 clusters; Silverman 2011b – 27 clusters) using an imputed ICC (as described in Unit of analysis issues).
Duration and frequency of intervention
There were two populations of studies in the review, those with interventions spanning from one week (James 1988) to 13 weeks (Wu 2020), and those consisting of a single session. Within the first category, studies offered MT either once per week (Albornoz 2009; Eshaghi Farahmand 2020; Heiderscheit 2005; Wu 2020), approximately twice per week (Murphy 2008), or four times per week (James 1988). The remaining 15 studies were single‐session interventions (all studies by Silverman). The five studies with duration of MT longer than three weeks had MT session lengths of approximately 60 (Murphy 2008), 90 (Eshaghi Farahmand 2020; Heiderscheit 2005; Wu 2020), and 120 minutes (Albornoz 2009). The single‐session studies had MT session length of approximately 45 minutes (all studies by Silverman).
Interventions
We included the following comparisons: MT plus standard care versus standard care alone (including wait‐list control) and MT plus standard care versus active control intervention plus standard care.
Music therapy
MT interventions that were included in our analyses were labelled as "music therapy," were conducted by a trained music therapist, and were consistent with the definition of MT provided in our inclusion criteria. MT methods varied across the included studies. Eleven studies used lyric analysis, which consisted of singing through or listening to a particular song and discussing lyrics in relation to a chosen substance use‐related theme (e.g. promoting motivation for change or relapse prevention, or both) and most often with a cognitive‐behavioural psychotherapeutic orientation (James 1988; Silverman 2009; Silverman 2010; Silverman 2011b; Silverman 2014; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2019a; Silverman 2021; Wu 2020). Seven studies used a semi‐structured songwriting process with themes related to identifying motivators for change, addressing substance use triggers, identifying coping skills and developing strategies to promote change and abstinence (Silverman 2011a; Silverman 2012; Silverman 2015a; Silverman 2017; Silverman 2019a; Silverman 2019b; Silverman 2020). Two studies used a highly specialised psychodynamically oriented receptive approach known as Guided Imagery and Music (GIM), in which participants listen to programmes of therapist‐selected classical music and engage in free associated imagery to work through unconscious material (Heiderscheit 2005; Murphy 2008). The therapist brings images to participants' awareness and guides participants to explore, deal with, and solve specific unconscious issues. Three studies used improvisational MT consisting of instrumental improvisation followed by processing of emotions and thoughts verbally or through other expressive means (Albornoz 2009; Eshaghi Farahmand 2020; Wu 2020). Two studies used combinations of the aforementioned methods (Eshaghi Farahmand 2020; Wu 2020), where singing, instrument playing and analysis of music lyrics or poems was used as a means for emotional expression and paired with verbal processing.
All studies offered MT within a group of two to 10 participants. One study included a reflective homework assignment with the aim of encouraging participants to continue contemplating the topics addressed during MT after conclusion of the session (Silverman 2011b).
Comparator interventions
Comparator interventions consisted of either standard care or an active control.
Standard care
All studies offered MT in addition to standard care. Standard care consisted of an array of standard services within the substance use treatment programme including individual or group (or both) psychotherapy, peer‐led groups including 12‐step programmes, pharmacotherapy, recreational and sports activities, medical care, and social work services. Fourteen studies compared MT plus standard care to standard care alone (Albornoz 2009; Eshaghi Farahmand 2020; Heiderscheit 2005; James 1988; Murphy 2008; Silverman 2012; Silverman 2014; Silverman 2015b; Silverman 2016b; Silverman 2017; Silverman 2019b; Silverman 2020; Silverman 2021; Wu 2020).
Verbal therapy
Eight studies used verbal therapy as an active control (Eshaghi Farahmand 2020; Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2014; Silverman 2015a; Silverman 2016a). One study used a two‐month course of group cognitive behaviour therapy as a comparative intervention (Eshaghi Farahmand 2020), verbal therapy consisted of identifying goals, discussing triggers and craving, evaluating coping strategies, practising health decision‐making, and learning problem‐solving skills. In the remaining seven studies, all of which had single‐session interventions, verbal therapy consisted of non‐music, scripted verbal therapy group focused on themes such as relapse prevention, motivation for change, drug avoidance self‐efficacy, and discussion of triggers and coping skills. In these seven Silverman studies, themes used in verbal therapy corresponded with content offered during the course of the MT intervention within the same study. Thus, in the Silverman studies, verbal therapy served as a non‐musical equivalent of the MT intervention (Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2014; Silverman 2015a; Silverman 2016a).
Recreational music
Five studies used recreational music as an active control (Silverman 2011b; Silverman 2015a; Silverman 2016a; Silverman 2017; Silverman 2019a). In these studies, recreational music consisted of a "Rock and Roll" music bingo game with accompanying discussion of musical artists, songs, and memories; it did not include a focus on issues specifically related to substance use. As such, the recreational music groups controlled for the non‐specific effects of therapist attention and for the presence of music, but lacked the therapeutic mechanism thought to be necessary to enable change in substance use behaviour. A music therapist, who was also the primary researcher, conducted recreational music groups.
Thus, 10 studies compared MT plus standard care to another active intervention plus standard care; either verbal therapy (Eshaghi Farahmand 2020; Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2014; Silverman 2015a; Silverman 2016a), or recreational music (Silverman 2011b; Silverman 2015a; Silverman 2016a; Silverman 2017; Silverman 2019a).
Outcomes
Primary outcomes
Psychological symptoms (depression)
Depression symptoms were assessed using various standardised and non‐standardised scales.
The BDI is a self‐report measure of depression consisting of 21 items with total scores ranging from 0 to 63, and higher scores indicating more severe depression (Beck 1996). Three studies used the BDI (Albornoz 2009; Murphy 2008; Silverman 2011a), one of which also used the HRSD (Albornoz 2009).
The HRSD is a clinician‐rated scale to assess depressive symptoms, consisting of either 17 or 21 items (scoring is based on the first 17), with total scores ranging from 0 to 54 and higher scores indicating more severe depression (Hamilton 1960). Albornoz 2009 used the 17‐item version of the HRSD.
The SDS is a self‐report measure of depression consisting of 20 items with total scores ranging from 20 to 80, and higher scores indicating more severe depression (Zung 1965). One study used the SDS (Wu 2020).
One study used the Likert scale self‐report measurement of depression (Silverman 2011a), which is a 7‐point scale with higher scores indicating more severe depression.
Psychological symptoms (anxiety)
Anxiety was measured by a standardised scale.
Substance craving
Substance craving was measured by three standardised scales. Lower scores on each of the standardised scales were indicative of lower levels of substance craving.
The BSCS is a 16‐item self‐report scale that measures level of craving for substances over the previous 24 hours, with lower scores indicating less substance craving (Somoza 1995). The BSCS evaluates the intensity, frequency, and duration of substance craving, and has a score ranging from 0 to 12. The BSCS includes two separate craving scales, so that respondents can complete separate forms to rate cravings for two different substances. When data were available from more than one scale (Silverman 2011b), we included only the first scale since not all participants had completed a second scale. Two studies used the BSCS and asked participants to evaluate current level of substance craving (Silverman 2011b; Silverman 2016b).
The Alcohol Craving Questionnaire‐Short Form Revised (ACQ‐SF‐R) is a 12‐item self‐report scale that assesses current craving for alcohol, with lower scores indicating less intense craving (Singleton 2003). One study used the ACQ‐SF‐R (Silverman 2017), and substituted "drug use" in place of "drinking" within the form, in order to accommodate diversity of problematic substance use among participants.
The Obsessive Compulsive Drug Use Scale (OCDUS) is a 13‐item self‐report scale that assesses level of craving drugs in the past weeks, lower scores indicate less intense craving (Franken 2002). One study used the OCDUS (Eshaghi Farahmand 2020).
Motivation for treatment/change
Motivation for treatment/change was measured by six standardised self‐report scales. High scores on all scales were indicative of better motivation for treatment/change.
The Texas Christian University Treatment Motivation Scale – Client Evaluation of Self at Intake (CESI) is a 29‐item self‐report scale with 5‐point Likert scales for each item and higher scores indicating greater motivation for change (Simpson 2008). The CESI is composed of four subscales: problem recognition, desire for help, treatment readiness, and pressures for treatment; the four subscales can be added for a total motivation score. One study used the CESI, where we used the total motivation score (Silverman 2015b).
The CMR is an 18‐item self‐report scale (DeLeon 1993). Each item is rated on a 5‐point Likert scale (from "strongly disagree" to "strongly agree"; negatively worded items are reversed in the scoring, so that higher scores indicate greater motivation. The items are summed into four subscales reflecting different aspects of motivation. One study used the CMR, which reported data for subscales only (Silverman 2012). For the purpose of this review, we selected the two subscales most closely related to our included outcome "motivation for treatment/change," namely the "Motivation (internal recognition of the need to change)" and "Readiness (readiness for treatment)" subscales, and we calculated a mean effect size across the two.
The Importance, Confidence, Readiness Ruler (ICR) consists of three 10‐point Likert scales that measure overall motivation to change (including readiness to change), and total scores range from 0 to 30 with higher scores indicating higher motivation for change (Miller 2002). The ICR may be completed in an interview or self‐completion format. One included study used the ICR, and we used the total score (Murphy 2008).
The Readiness to Change Questionnaire – Treatment Version (RTCQ‐TV) consists of a 15‐item self‐report scale to assess level of motivation and readiness to stop or control drinking (Heather 1999). The scale contains subscales aligning with Prochaska and DiClemente's stages of change model (Prochaska 1983), namely, Precontemplation, Contemplation and Action stages. One included study used the RTCQ‐TV, and reported data for subscales only (Silverman 2011b). For the purpose of this review, we selected the two subscales most closely related to our included outcome "motivation for treatment/change," namely the "Contemplation" and "Action" subscales, and we calculated a mean effect size across the two subscales.
The SOCRATES is a 19‐item self‐report scale that assesses motivation for change, treatment eagerness, and readiness to change (Miller 1996). A total score can be computed and ranges from 19 (low) to 95 (high), with higher scores indicating greater motivation to change. The SOCRATES has versions for alcohol and for drug use. Two included studies used the SOCRATES, one providing total scores (Silverman 2009), and the other providing scores for subscales of Recognition and Taking Steps, which we combined to calculate a mean effect size across the two subscales (Silverman 2021).
The University of Rhode Island Change Assessment (URICA) is a 32‐item self‐report scale that assesses motivation for change (McConnaughy 1983). The URICA has four subscales aligning with Prochaska and DiClemente's stages of change model (Prochaska 1983), namely, Precontemplation, Contemplation, Action, and Maintenance. The subscales can be combined arithmetically (Contemplation + Action + Maintenance – Precontemplation) to yield a Readiness to Change score, with higher scores indicating greater readiness for change. Each subscale consists of eight items using 5‐point Likert scales ranging from 1 to 5 (resulting in scores ranging from 8 to 40). Subscale scores can be used to trace changes in attitudes related to the specific stages of change. One included study used the URICA, and reported data for subscales only (Silverman 2011a). For the purpose of this review, we selected the two subscales most closely related to our included outcome "motivation for treatment/change," namely the "Contemplation" and "Action" subscales, and we calculated a mean effect size across the two.
Total scores were available for CESI, ICR, and SOCRATES. In the other scales, we combined the subscales that were most closely related to the constructs of motivation and action (e.g. Contemplation and Action scales of RTCQ‐TV and URICA; Motivation and Readiness in the CMR) by calculating mean effect size.
In addition to standardised scales, two studies used self‐report Likert scales for motivation for treatment/change, both of which used a 7‐point scale with higher scores indicating greater motivation for treatment (Silverman 2014; Silverman 2015a).
Motivation to stay sober/clean
Motivation to stay sober/clean was measured by two standardised scales and by Likert scale.
The CSS is a 5‐item self‐report scale that measures degree of motivation to cessation and abstinence from drug or alcohol use (Kelly 2014). Total scores range from 5 to 30, with higher scores indicating greater commitment to abstinence. One study used the CSS (Silverman 2021).
The Questionnaire of Motivation for Abstaining from Drugs (QMAD) is a 36‐item self‐report measure of motivation for abstaining from drugs (Wu 2008). Total scores range from 36 to 180, with higher scores indicating greater motivation. One study used the QMAD (Wu 2020).
Three studies used a 7‐point Likert scale, with higher scores indicating greater motivation to stay sober/clean (Silverman 2011b; Silverman 2014; Silverman 2015a).
Given that participants had assumedly entered substance use treatment in order to change problematic substance use behaviour, in this review 'motivation to stay sober/clean' is considered to be a specific manifestation of the construct 'motivation to change,' and therefore warrants both inclusion as an outcome and separate analysis.
Secondary outcomes
Alcohol or substance use
One study assessed substance use during a follow‐up telephone call at one month after discharge from substance use treatment by asking participants if they had maintained sobriety (Silverman 2011a). Respondents could reply: yes, somewhat, or no. We scored this outcome as a dichotomous variable with the responses 'somewhat' and 'no' scored as 'no'.
Retention in treatment
The review authors calculated retention in treatment for six studies based on the number of participants remaining at the end of treatment (Albornoz 2009; Eshaghi Farahmand 2020; Heiderscheit 2005; James 1988; Murphy 2008; Wu 2020). The remaining included studies used single‐session interventions, and thus, it was not possible to calculate this outcome for those studies. Retention in treatment was defined as the number of participants remaining in each group at the end of treatment.
Severity of substance dependence/use
None of the included studies examined severity of substance dependence/use.
Serious adverse events
None of the included studies reported data on serious adverse events.
Excluded studies
We excluded 22 studies. Ten studies required full‐text review to confirm that they were not RCTs or controlled clinical trials (Baker 2007; Bibb 2018; Dingle 2008; Gardstrom 2013; Howard 1997; Moe 2011; Murphy 2015; Oklan 2014; Taylor 2005; Wheeler 1985). Nine studies did not use MT as the intervention, either using music but not qualifying as MT (Chandrasekar 2020; Gallant 1997; Lu 2005; Mathis 2017; Sewak 2018; Stamou 2016; Stamou 2017), using combination of therapies (Malcolm 2002), or not having music intervention (Haddock 2003). Two studies included an ineligible population, such as a mix of patients and staff (Hammer 1996), or mental health patients without diagnosis of SUD (Silverman 2016c). One study did not include a relevant control intervention (Jones 2005).
Risk of bias in included studies
The results of the assessment of risk of bias are represented in the risk of bias section of the Characteristics of included studies tables, in Figure 2, and in Figure 3.
2.

Review authors' judgements about each risk of bias item presented as percentages across all included studies. Objective outcome was only assessed in six of the included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
Random sequence generation was achieved in individually randomised studies, via use of random number blocks (Albornoz 2009), coin toss (Heiderscheit 2005), computer program (Murphy 2008), or an independent statistician not directly involved with the research (Wu 2020). We judged these four studies at low risk of bias. Two individually randomised studies did not specify method of sequence generation (Eshaghi Farahmand 2020; James 1988), and these studies were judged at unclear risk of selection bias. Of 15 cluster‐randomised trials, four specified that the randomisation sequence was generated with a computer (Silverman 2014; Silverman 2017; Silverman 2019a; Silverman 2021); in the remaining 11 cluster‐randomised trials this was unclear. We judged the four studies at low risk of bias, and the remaining 11 studies at unclear risk of bias (Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2012; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2019b; Silverman 2020).
Allocation concealment
One study used sequentially numbered envelopes, so that participants and investigators involved could not have foreseen treatment assignment (Albornoz 2009). One study used coin toss for randomisation, which does not assure adequate concealment of allocation, and thus was judged at unclear risk of selection bias (Heiderscheit 2005). In the remaining 19 studies, information about allocation was either insufficient or not further specified (Eshaghi Farahmand 2020; James 1988; Murphy 2008; Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2011b; Silverman 2012; Silverman 2014; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2017; Silverman 2019a; Silverman 2019b; Silverman 2020; Silverman 2021; Wu 2020). Therefore, we judged them to be at unclear risk of bias.
Blinding
We divided both blinding of participants and personnel and blinding of outcome assessment according to subjective and objective outcomes.
Performance bias
With MT intervention, it is not possible to blind participants and therapists. We consider knowledge of receiving this type of therapy as part of the therapeutic effect itself, and thus did not consider lack of blinding of participants and personnel as a source of bias. Accordingly, all studies were at low risk of performance bias for both objective and subjective outcomes.
Detection bias
The only objective outcome included in this review was retention in treatment, which we calculated based on the number of participants from each group remaining at the conclusion of treatment. We judged that lack of blinding of outcome assessors in this case was unlikely to influence the outcome. All studies were judged at low risk of bias related to objective outcomes. All subjective outcomes for all studies (with the exception of observer‐rated depression (HRSD) in Albornoz 2009) were assessed by self‐report and thus, all studies were judged at high risk for detection bias related to subjective outcomes.
Incomplete outcome data
We judged 16 studies to be at low risk of attrition bias (Albornoz 2009; Heiderscheit 2005; James 1988; Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2017; Silverman 2019a; Silverman 2019b; Silverman 2020; Silverman 2021; Wu 2020). For six of these studies, reports indicated no missing outcome data (Albornoz 2009; Heiderscheit 2005; James 1988; Silverman 2019a; Silverman 2019b; Wu 2020). For the remaining 10 studies, missing outcome data were balanced in number across intervention groups, with similar reasons for missing data across groups (Silverman 2009; Silverman 2010; Silverman 2011a; Silverman 2015a; Silverman 2015b; Silverman 2016a; Silverman 2016b; Silverman 2017; Silverman 2020; Silverman 2021). We judged four studies at unclear risk of bias, due to no stated reason for missing outcome data (Murphy 2008; Silverman 2011b; Silverman 2012), or due to an imbalance of missing data across groups (Silverman 2014). One study was at unclear risk of bias due to stating in exclusion criteria that participants who did not attend all intervention sessions were excluded, and not clearly stating the number of participants analysed in each group (Eshaghi Farahmand 2020).
Selective reporting
All 21 studies appeared to be free of selective reporting, and we therefore judged them at low risk of reporting bias.
Other potential sources of bias
We identified no other sources of bias.
Effects of interventions
Comparison 1: music therapy plus standard care versus standard care alone
See Table 1.
Primary outcomes
Psychological symptoms
Depression
Three studies with 100 participants provided data on self‐reported depression symptoms (various scales) at end of intervention. There was no clear evidence of effect of MT on depression, though the CIs ranged from large favourable effect to no effect (SMD –0.33, 95% CI –0.72 to 0.07; P = 0.61; moderate‐certainty evidence; Analysis 1.1). Heterogeneity between the studies was minimal (I2 = 0%). One study with 60 participants reported data from short‐term follow‐up at three months, showing no clear evidence of effect of MT, though the CIs included meaningful effects in both directions (MD –1.13, 95% CI –6.33 to 4.07; P = 0.67; Analysis 1.2).
1.1. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 1: Psychological outcomes (depression self‐report; various tools, BDI, HRSD, SDS; high = poor)
1.2. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 2: Psychological outcomes short‐term follow‐up (depression self‐report, SDS; high = poor)
Anxiety
One study with 60 participants reported data on self‐reported anxiety (SAS) at end of intervention. There was no clear evidence of effect, but the CIs included meaningful effects in both directions (MD –0.17, 95% CI –4.39 to 4.05; P = 0.94; low‐certainty evidence; Analysis 1.3). The same study with 60 participants reported data from short‐term follow‐up at three months showing no clear evidence of effect of MT, but the CIs included meaningful effects in both directions (MD –1.49, 95% CI –5.74 to 2.76; P = 0.49; Analysis 1.4).
1.3. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 3: Psychological outcomes (anxiety self‐report; SAS; high = poor)
1.4. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 4: Psychological outcomes short‐term follow‐up (anxiety self‐report; SAS; high = poor)
Substance craving
Three studies with 254 participants provided data on self‐reported substance use craving at end of intervention using various standardised scales. There was evidence of an effect of medium magnitude favouring MT, with wide CI ranging from very large to small effect (SMD –0.66, 95% CI –1.23 to –0.10; P = 0.02; moderate‐certainty evidence; Analysis 1.5). Heterogeneity between the studies was substantial (I2 = 74%). Significant subgroup differences indicated a greater reduction in craving for MT intervention lasting one to three months (P = 0.007).
1.5. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 5: Substance craving (various scales; BSCS, ACQ‐SF‐R; high = poor)
Motivation for treatment/change
Five studies with 408 participants provided data on self‐reported motivation for treatment/change at end of intervention, using various scales. There was evidence of a small‐to‐medium effect favouring MT (SMD 0.41, 95% CI 0.21 to 0.61; P < 0.0001; moderate‐certainty evidence; Analysis 1.6). There was minimal heterogeneity between studies (I2 = 0%).
1.6. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 6: Motivation for treatment/change (various scales; CESI, ICR, CMR; high = good)
Motivation to stay sober/clean
Three studies with 269 participants provided data on self‐reported motivation to stay sober/clean at end of intervention, using various scales. There was no clear evidence of effect of MT, though the CIs ranged from no effect to a medium‐sized favourable effect (SMD 0.22, 95% CI –0.02 to 0.47; P = 0.07; moderate‐certainty evidence; Analysis 1.7). Heterogeneity across studies was minimal (I2 = 0%). One study with 60 participants reported data from short‐term follow‐up at three months, showing no clear evidence of effect of MT, though CIs ranged from no effect to a large effect (MD 9.29, 95% CI –4.60 to 23.18; P = 0.19; Analysis 1.8).
1.7. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 7: Motivation to stay sober/clean (various scales, high = good)
1.8. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 8: Motivation to stay sober/clean short‐term follow‐up (QMAD, high = good)
Secondary outcomes
Alcohol or substance use
No studies reported alcohol or substance use.
Retention in treatment
Six studies reported no meaningful effect on retention in treatment (RR 0.99, 95% CI 0.93 to 1.05; P = 0.75; moderate‐certainty evidence; Analysis 1.9). Heterogeneity across studies was minimal (I2 = 0%).
1.9. Analysis.

Comparison 1: Music therapy plus standard care versus standard care alone, Outcome 9: Retention in treatment (high = good)
Severity of substance dependence/use
No studies reported severity of substance dependence/use.
Serious adverse events
No studies reported serious adverse events.
Comparison 2: music therapy plus standard care versus another active intervention plus standard care
See Table 2.
Primary outcomes
Psychological symptoms
Depression
One study with 110 participants provided data on self‐reported depression symptoms (BDI) at end of intervention. There was no clear evidence of effect of MT, though CI ranged from moderate favourable effect to no effect (MD –1.49, 95% CI –4.98 to 2.00; P = 0.40; moderate‐certainty evidence; Analysis 2.1). One study with 54 participants provided data from short‐term follow‐up at one month, with no evidence of an effect, though the CIs included meaningful effects in both directions (MD 0.03, 95% CI –1.05 to 1.11; P = 0.96; Analysis 2.2).
2.1. Analysis.

Comparison 2: Music therapy plus standard care versus active intervention plus standard care, Outcome 1: Psychological outcomes (depression self‐report; BDI; high = poor)
2.2. Analysis.

Comparison 2: Music therapy plus standard care versus active intervention plus standard care, Outcome 2: Psychological outcomes short‐term follow‐up (depression self‐report; Likert; high = poor)
Anxiety
No studies reported anxiety.
Substance craving
Three studies with 232 participants provided data on self‐reported substance use craving at end of intervention, using various scales. There was no evidence of effect after correcting for clustering, though the CIs included meaningful effects in both directions (SMD –0.04, 95% CI –0.56 to 0.48; P = 0.89; low‐certainty evidence; Analysis 2.3). Heterogeneity between the studies was substantial (I2 = 70%), affected interpretation of results and had no plausible explanation. Significant subgroup differences (P = 0.02) indicate a greater reduction in craving for active control intervention lasting one to three months.
2.3. Analysis.

Comparison 2: Music therapy plus standard care versus active intervention plus standard care, Outcome 3: Substance craving (various scales, high = poor)
Motivation for treatment/change
Five studies with 411 participants reported data for motivation for treatment/change at end of treatment, using various standardised scales. A moderate effect favoured MT, though CI ranged from no effect to large favourable effect (SMD 0.46, 95% CI –0.00 to 0.93; P = 0.05; moderate‐certainty evidence; Analysis 2.4). Heterogeneity between studies was significant (I2 = 80%). Heterogeneity could not be explained by number of sessions, type of substance or presence of dual‐diagnosis, as these were consistent across studies. When removing the study that was likely responsible for the observed heterogeneity (Silverman 2015a), the CIs still ranged from no effect to a meaningful favourable effect, so investigating heterogeneity did not affect interpretation of results.
2.4. Analysis.

Comparison 2: Music therapy plus standard care versus active intervention plus standard care, Outcome 4: Motivation for treatment/change (various tools; RTCQ‐TV, SOCRATES, URICA; higher = good)
Motivation to stay sober/clean
Three studies with 258 participants provided data on self‐reported motivation to stay sober/clean at end of intervention using a Likert scale. There was no clear evidence of effect of MT, though the CIs ranged from no effect to large favourable effect (MD 0.34, 95% CI –0.11 to 0.78; P = 0.14; moderate‐certainty evidence; Analysis 2.5). Heterogeneity between studies was substantial (I2 = 87%), but did not affect interpretation of results.
2.5. Analysis.

Comparison 2: Music therapy plus standard care versus active intervention plus standard care, Outcome 5: Motivation to stay sober/clean (Likert, high = good)
Secondary outcomes
Alcohol or substance use
One study provided data for self‐report of active substance use at short‐term (one‐month post‐discharge). This outcome was unobserved for 83/140 (59%) participants. We imputed/assumed the negative outcome for unobserved cases (non‐respondents) as specified in the protocol. There was no meaningful difference between MT and standard care (RR 1.05, 95% CI 0.85 to 1.29; Analysis 2.6), though the CIs of 0.85 (15% less substance use) to 1.29 (29% more substance use) may include meaningful effects in both directions.
2.6. Analysis.

Comparison 2: Music therapy plus standard care versus active intervention plus standard care, Outcome 6: Substance use short‐term follow‐up (self‐report)
Retention in treatment
No studies reported retention in treatment.
Severity of substance dependence/use
No studies reported severity of substance dependence/use.
Serious adverse events
No studies reported serious adverse events.
Discussion
Summary of main results
This review evaluated the effectiveness of MT as an add‐on to standard care for people with SUDs. We included 21 RCTs with 1984 participants, with 15 studies assessing the effect of one‐hour MT intervention. Studies included a variety of MT methods, including lyric analysis or songwriting with themes related to substance use treatment and having a cognitive behavioural theoretical orientation, psychodynamically focused receptive methods to process unconscious material, clinical improvisation to identify and work through thoughts and emotions, or a combination of these methods. The included studies compared MT plus standard care to standard care alone or to active interventions plus standard care (verbal therapy or recreational music) for people with SUD.
We found a medium‐sized effect in favour of MT on substance craving for participants receiving MT plus standard care, compared to standard care alone (Table 1), with moderate certainty, meaning we are moderately confident in the effect estimate. Greater reduction in craving was associated with MT intervention lasting longer than a single session, though this result was based on one small study. There was a small‐to‐medium effect favouring MT for motivation for treatment/change, with moderate certainty, for participants receiving MT plus standard care, as compared to standard care alone. However, such effects on motivation for treatment/change were driven by four (of five) studies being one‐hour MT intervention by the same researcher/research group. There was no clear evidence of effect for depression, anxiety, motivation to stay sober, or retention in treatment for participants receiving MT plus standard care as compared to standard care alone. There were no data available for substance use or severity of use.
A moderate effect on motivation for treatment/change was retained when comparing MT plus standard care to another active intervention plus standard care, though certainty in the result was lower (Table 2). There was no clear evidence of effect on depression, substance craving, motivation to stay sober, or substance use when comparing MT plus standard care to active intervention plus standard care. There were no data on anxiety or retention in treatment when comparing MT plus standard care versus active intervention plus standard care.
Overall completeness and applicability of evidence
The results of this review suggest that the evidence base for the use of MT for SUDs is emerging. Outcomes that may predict future success in reducing or stopping substance use, such as motivation for change, motivation for sobriety, and symptoms of craving have received most attention, along with outcomes related to the mental health of people with SUD, such as depressive symptoms. Outcomes related to reducing or stopping substance use are less often assessed. Like other therapies, MT is often provided in addition to a complement of strategies comprising standard care, thus it may be difficult to isolate its unique contribution to a person's reduction in substance use.
It was not possible to determine if the effects of MT vary depending upon the type of substance(s) used, or if certain types of MT intervention have a differential impact on outcomes. Within the 17 studies reporting race of participants (all from the US), a weighted mean of 82.7% of participants identified as Caucasian (assumed to be white people) and 5.11% as African American. Since the US census from 2020 cites respondents' race as 76.3% "white alone" and 13.4% "black or African American alone" (U.S. Census 2020), it is possible that this review may not be fully representative of responses from race minority groups. The included studies predominantly involved adults aged 18 years and older, and thus it would be important to also evaluate the effects of MT for younger substance users.
The results of this review may have limited generalisability, as 15/21 included studies were conducted in short‐term detoxification settings with length of stay shorter than five days. Participants in medical detoxification units undergo intense somatic experiences related to the process of pharmacological detoxification, and thus may respond differently to therapies than people in stabilisation or long‐term treatment settings. Similarly, with the exception of three studies, the review evidence comes from treatment settings in the USA, and thus, cultural variations in treatment practices, healthcare systems, and attitudes towards treatment from other geographic locations may not be reflected in the current results. Results we report related to psychological symptoms are reflective of standard care received during addiction treatment, and thus such results might be different in treatment settings primarily focusing on mental health. Finally, and important to note, 15 of the included studies were conducted by the same researcher on the same detoxification unit, a factor that may substantially limit the applicability of findings.
Quality of the evidence
Overall, we found mostly moderate‐ and low‐certainty evidence for the outcomes included in this review. The methodological quality of included studies varied. All studies used subjective outcomes. Most studies did not describe the method of allocation concealment, leading to a judgement of unclear risk of selection bias. We rated all included studies at unclear risk of detection bias due to lack of blinding of outcome assessors for subjective outcomes. Since most outcomes assessed in this review were self‐report measures completed by participants, it was not possible to blind outcome assessors for these subjective outcomes. However, we judged that the likelihood of bias arising from such lack of blinding would not differ between groups, and thus we did not rate these studies at high risk for bias. Similarly, it is not possible to blind participants and providers to MT. We consider knowledge of receiving this type of therapy as part of the therapeutic effect itself, and thus did not consider lack of blinding of participants and personnel as a source of bias. Accordingly, all studies were at low risk of performance bias for subjective outcomes.
We downgraded all outcomes one level for imprecision due to the optimal information sizes not being met. In addition, anxiety under Comparison 1 and substance craving under Comparison 2 were downgraded an additional level for very low sample size. We downgraded substance craving in Comparison 2 one level for inconsistency due to substantial heterogeneity with no plausible explanation that likely affected interpretation of results.
It is unknown if any participants in the studies by Silverman participated in more than one study. We contacted the author, but he was not permitted by the institutional review board to track participants beyond the closure of each study. However, due to the very short duration of interventions and follow‐up in these studies, we judged the risk of statistical dependencies related to potential repeated participation of individuals to be minimal.
Potential biases in the review process
We undertook an extensive search of databases and additional sources and applied no restrictions concerning nationality or language within the search process; thus we believe that we have identified and included in the present systematic review all potentially relevant studies. All abstracts screened were available in English and we checked the English translation of one study report against its original language using a fluent speaker, but it is possible that despite our thorough search process, abstracts in languages other than English were missed. We contacted study investigators directly to obtain full texts when only abstracts were available through typical search procedures. Furthermore, we contacted investigators of relevant studies when data in the reports were insufficient.
Agreements and disagreements with other studies or reviews
Our findings of a moderate effect of MT on substance craving and small‐to‐moderate effect on motivation for treatment are inconsistent with a systematic review of the psychosocial intervention of motivational interviewing (Smedslund 2011), which found no significant effect for readiness for change, though they found a significant effect on extent of substance abuse for motivational interviewing versus no treatment. The significant impacts of motivational interviewing found in Smedslund 2011 were not retained when comparing the intervention to standard care or to other active treatment, whereas in our review, the significant effects of MT were retained in comparison to standard care.
Similarly, our findings are inconsistent with a systematic review of opioid users in maintenance treatment, which found no significant effect for any outcome when psychosocial interventions were taken together, nor any specific psychosocial intervention with strong efficacy (Amato 2011a). However, the predominance of studies in detoxification settings and with users of varying forms of addiction in our review may partially explain this difference in findings.
We noted a high proportion of participants retained in treatment in our included studies (177/199, 89%), though there were no clear differences in effect on retention for participants receiving MT. Our failure to find a difference in retention in treatment or reduction in substance use contrasts with the systematic review of Amato 2011b, who found a reduction in treatment dropout and in opiate use when psychosocial interventions were added to pharmacological treatment for opioid users in detoxification, and to Minozzi 2016 who found a reduction in dropout rate when psychosocial treatment was added to standard care for adults who misuse psychostimulants. Our findings concur with the lack of effect on treatment retention (at end of treatment and at three months) Klimas 2018 found when assessing the effect of psychosocial interventions on alcohol use in concurrent substance/alcohol users.
The psychosocial interventions Klimas 2018 describe had low frequency of sessions, with motivational interviewing consisting of three, one‐hour sessions spaced two weeks apart, and brief intervention consisting of a single session lasting less than 30 minutes. Though the single‐session MT methods provided in detoxification settings in our review are associated with beneficial effects on substance craving and motivation for treatment, it is possible that longer‐term interventions would be necessary to promote change in outcomes such as reduction in substance use, or long‐standing psychological states like depression. Such a possibility aligns with evidence from a systematic review of MT for people with serious mental disorders, where small effects on depressive symptoms were evidenced after three to 10 sessions of MT and large effects after 16 to 51 sessions (Gold 2009). Our findings suggest that MT may have a small effect on reducing depressive symptoms, based on three studies with intervention lasting from one to three months, though we are uncertain of this effect. Due to a lack of evidence, we cannot yet determine a dose–response relationship for MT used in substance use treatment, but our finding regarding greater reduction in substance craving for higher number of MT sessions indicates that further research is needed.
Authors' conclusions
Implications for practice.
Although we have moderate‐to‐low confidence in our findings as the included studies were downgraded in certainty due to imprecision, and most included studies were conducted by the same researcher in the same detoxification unit, which considerably impacts the transferability of findings, the results from this review suggest that music therapy (MT) as 'add‐on' treatment to standard care can lead to moderate reductions in substance craving and can increase motivation for treatment/change. These findings are clinically meaningful, as substance users undergoing detoxification can experience significant drug craving, which in turn can contribute to relapse. Since previous research demonstrates that music listening may either reduce craving or increase it depending upon the listener's associations with that piece of music (Short 2015), the expertise of a music therapist is important to assure that substance users in treatment are able to work through healthy and unhealthy responses to music in a therapeutic way (Horesh 2010).
Implications for research.
Research concerning MT for people with substance use disorder (SUD) could be improved by: engaging in research in a broader diversity of treatment settings, while decreasing heterogeneity within and between studies; carefully considering the associations between mental health and addiction; evaluating the impact of length of treatment; assessing outcomes at medium‐ and long‐term follow‐up; matching MT intervention to phase of substance use treatment; and determining mechanisms of therapeutic change.
Decreasing heterogeneity
There exists a high level of heterogeneity within substance use treatment in general, which makes it challenging to research this field and translate research to practice. Heterogeneity is present in relation to type and number of substances being abused; treatment ideology of the facility; staff profile of the facility; length of stay; types of therapies offered; and socioeconomic, cultural, and ideological backgrounds of the patients served. MT may have stronger effects with users of certain substances, within facilities of certain treatment orientations, or with certain forms of MT based on treatment phase. Future research should take such differences into account and test MT in more homogeneous groups to determine the specific effect of MT in particular treatment settings and for particular types of addiction.
For future research it is important to broaden outcome measures and test the specific effects of MT and the types of treatment in which MT might have an adjuvant effect. Although Alcoholics Anonymous /Narcotics Anonymous has a consequent understanding that misuse is a chronic disease where total abstinence is the only cure, many patients requesting treatment have other types of motivation. Therefore, it is important to track the severity of substance abuse/dependence in the form of measures such as Alcohol Use Disorders Identification Test (AUDIT; Babor 1992) and Drug Use Disorders Identification Test (DUDIT; Berman 2005). More important than total abstinence might be the ability to reduce harms and control substance use in order to be able to obtain work, maintain decent housing, and develop healthy social networks. These recovery‐oriented and person‐centred treatment outcomes should be more fully integrated into the way that MT is implemented and empirically evaluated.
Considering the associations between mental health and addiction
Substance use often serves as self‐medication for different types of symptoms such as irritation, depression, anxiety, and racing thoughts (Quello 2005). The effects of MT or lack of effects might be dominated more by mental health status than by addiction behaviour. Therefore, it is important in future research to control for change in mental health symptoms during treatment to better understand underlining processes that MT might have on addiction measures.
Length of treatment and timing of follow‐up
Fifteen of the included studies had a total treatment length of one hour or less. Due to the intractable nature of behavioural patterns associated with SUDs, it is likely that longer periods of intervention would be required in order to impact substance use behaviour at long‐term follow‐up. Thus, more research is needed that investigates the differential impact of treatment length on substance use behaviour.
If longer lengths of stay in substance use treatment are associated with better engagement in aftercare programmes and lower levels of substance use at long‐term follow‐up (Arbour 2011; Moos 2007), we need to research the impact of MT on retention in treatment over longer periods. In our findings, MT demonstrates a small‐to‐medium effect on increasing motivation for treatment as compared to standard care alone. Since the risk of dropping out of substance use treatment is relatively high, the positive effect of MT on motivation for treatment may have a significant impact on treatment retention, but should be investigated further.
We are in particular need of research that evaluates the long‐term impact of MT for people with SUDs. We recommend evaluating substance use patterns in the second year following treatment, due to the high level of relapse reported in the first year following treatment. In addition to assessing reduction or cessation in substance use, we recommend that future research assess capacity for emotion regulation (e.g. Stroop test [MacLeod 1991]), and evaluate withdrawal symptoms.
Implications for research related to detoxification settings
In future research, we recommend that MT intervention be matched to the most pressing needs of specific phases of treatment. For example, in detoxification settings, reducing discomfort from withdrawal symptoms and substance craving may take precedence. The main aim during detoxification is to mitigate the effects of abstinence and possible complications of withdrawal such as convulsions and acute Wernicke's syndrome. During active stages of drug use and withdrawal, patients are highly aroused and physiological parameters and anxiety levels are closely monitored (Urbano 2017). There are strict regimens where abstinence arousal symptoms are counted and drugs, often in the form of benzodiazepine derivatives working on the gamma‐aminobutyric acid (GABA) system of the brain, are the treatment of choice (Holleck 2019). For alcohol withdrawal treatment, reducing glutamate overactivity is the key in reducing risk of brain toxicity and increasing the neuroprotective potential during withdrawal.
Due to their physiological state, most patients have limited capacity for engaging in cognitive‐mediated processes as a part of specific substance use treatment during the medical detoxification stage. Instead, patients require reduction in physiological arousal, and assistance with regulation. Music‐assisted relaxation may be used to decrease perceived pain and discomfort, manage anxiety, and reduce physiological arousal during detoxification. More studies should be conducted in detoxification settings using MT as an adjuvant therapy to test the effects on abstinence symptoms using, for example, the internationally recognised instrument Clinical Institute Withdrawal Assessment (CIWA) (e.g. Sullivan 1989) on a specific group such as alcohol withdrawal. Additional pertinent outcomes include need for medication, reduction in CIWA score, and patient satisfaction with the treatment.
Patients undergo significant drug craving during detoxification, and for many patients drugs offer a way to cope with the adverse effects of abstinence. Our finding that MT (as compared to standard care) led to a decrease in substance craving within detoxification settings is therefore clinically significant, but further research should be done to evaluate this finding.
Implications for research related to stabilisation and long‐term treatment
During the stabilisation period following detoxification, MT interventions incorporating psychoeducation may be used to teach coping strategies, provide experiences of mastery, enable social connection, and promote emotion regulation. Long‐term treatment may then focus on further developing skills for emotion regulation, promoting cognitive skill development, and reinforcing coping strategies and social skills. Research can evaluate whether MT interventions are more effective when intentionally matched to the phases of substance use treatment. Controlled trials from stabilisation and long‐term treatment settings are currently under‐represented in experimental research, and thus these settings should be emphasised in future research.
Mechanisms of therapeutic change
There are several neurological pathways through which music and MT may impact a person with a SUD, including systems involved in reward, craving, arousal, emotion regulation, and executive function (Blum 2017; Fachner 2017; Salimpoor 2011). Future research should explore the mechanisms that explain how different forms of MT work, including impacts on the reward system, dopaminergic system (Salimpoor 2011), GABA, and amygdala function (Blood 2001). The reward system is linked to the initial development of addictive behaviour, and as tolerance increases over time with repeated use, there is diminishing reward response. MT may be used to activate or repair the reward system, in a way that might support the management of substance craving and the enabling of beneficial emotion regulation that in combination might support relapse prevention.
History
Protocol first published: Issue 2, 2017
Acknowledgements
We thank the Cochrane Drugs and Alcohol Group for assessing the protocol (Ghetti 2020) and supporting preparation of the review. We thank Elin Kirkhus Johansen, in her role as research assistant, for assisting in preparing this review.
Appendices
Appendix 1. Search strategy
Cochrane Drugs and Alcohol Group Specialised Register (via CRSLive)
#1 music AND INREGISTER
#2 sing OR singing OR song* OR choral* OR choir* OR melod* OR lyric* AND INREGISTER
#3 #1 OR #2
Cochrane Central Register of Controlled Trials (CENTRAL)
#1 (Substance‐Related Disorders):MH AND CENTRAL:TARGET
#2 (Amphetamines):MH AND CENTRAL:TARGET
#3 (Cannabis):MH AND CENTRAL:TARGET
#4 (Cocaine):MH AND CENTRAL:TARGET
#5 (Designer Drugs):MH AND CENTRAL:TARGET
#6 (Heroin):MH AND CENTRAL:TARGET
#7 (Methamphetamine):MH AND CENTRAL:TARGET
#8 (Narcotics):MH AND CENTRAL:TARGET
#9 (Street Drugs):MH AND CENTRAL:TARGET
#10 (amphetamine* or drug* or polydrug or substance or cannabis or cocaine or "hash oil*" or hashish or heroin or lsd or marihuana or marijuana or methadone or mdma or morphine or ecstasy or methamphetamine* or narcotics or opioid* or opiate* or opium):ti,ab AND CENTRAL:TARGET
#11 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10
#12 (Alcohol Drinking):MH AND CENTRAL:TARGET
#13 (alcohol* near (abstain* or abstin* or abus* or addict* or consum* or dependen* or disorder* or drink* or excess* or misus* or problem* or risk* or withdrawal*)):ti,ab,kw AND CENTRAL:TARGET
#14 #12 OR #13
#15 (Music Therapy):MH AND CENTRAL:TARGET
#16 (Music):MH AND CENTRAL:TARGET
#17 music*:ti,ab,kw AND CENTRAL:TARGET
#18 (sing or singing or song* or choral* or choir* or melod* or lyric*):ti,ab,kw AND CENTRAL:TARGET
#19 #15 OR #16 OR #17 OR #18
#20 #14 OR #11
#21 (abstin* or abstain* or abuse* or addict* or dependen* or misuse or overdose or withdrawal* or disorder*):ti,ab,kw AND CENTRAL:TARGET
#22 #21 AND #11
#23 #12 OR #13 OR #22
#24 #19 AND #23
MEDLINE (PubMed)
Substance‐Related Disorders[MeSH]
Amphetamines[MeSH] OR Cannabis[MeSH] OR Cocaine[MeSH] OR Designer Drugs[MeSH] OR Heroin[MeSH] OR Methamphetamine[MeSH] OR Narcotics[MeSH] OR Street Drugs[MeSH] OR amphetamine*[tiab] OR drug*[tiab] OR polydrug[tiab] OR substance[tiab] OR cannabis[tiab] OR cocaine[tiab] OR "hash oil*"[tiab] OR hashish[tiab] OR heroin[tiab] OR lsd[tiab] OR marihuana[tiab] OR marijuana[tiab] OR methadone[tiab] OR mdma[tiab] OR morphine[tiab] OR ecstasy[tiab] OR methamphetamine*[tiab] OR narcotics[tiab] OR opioid*[tiab] OR opiate*[tiab] OR opium[tiab]
#1 OR #2
abstin*[tiab] OR abstain*[tiab] OR abuse*[tiab] OR addict*[tiab] OR dependen*[tiab] OR misuse[tiab] OR overdose[tiab] OR withdrawal*[tiab] OR disorder*[tiab]
#3 AND #4
Alcohol Drinking[MeSH]
((alcohol*[tiab] AND (abstain*[tiab] OR abstin*[tiab] OR abus*[tiab] OR addict*[tiab] OR consum*[tiab] OR dependen*[tiab] OR disorder*[tiab] OR drink*[tiab] OR excess*[tiab] OR misus*[tiab] OR problem*[tiab] OR risk*[tiab] OR withdrawal*[tiab]))
#5 OR #6 OR #7
"Music Therapy"[Mesh]
"Music"[Mesh]
music*[tiab]
sing[tiab] OR singing[tiab] OR song*[tiab] OR choral*[tiab] OR choir*[tiab] OR melod*[tiab] OR lyric*[tiab]
#9 OR #10 OR #11 OR #12
randomized controlled trial[pt]
controlled clinical trial[pt]
randomized[tiab]
placebo[tiab]
drug therapy[sh]
randomly[tiab]
trial[tiab]
groups[tiab]
groups[tiab]
#14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22
(animals[mh] NOT humans[mh])
#23 NOT #24
#8 AND #13 AND #25
Embase (embase.com)
exp drug abuse/
exp substance abuse/
((amphetamine* or barbiturate* or benzodiazepine* or cannabis or cocaine or drug* or hallucinogen* or hashish or heroin or lsd or marihuana or marijuana or methadone or mdma or ecstasy or methamphetamine* or opioid* or opiate* or opium or tranquilizer* or tranquiliser* or inhalant* or stimulant or polydrug or substance) adj5 (abstin* or abstain* or abuse* or addict* or dependen* or misuse or overdose or withdrawal* or disorder*)).ab,kw,ti.
(alcohol* adj5 (abstain* or abstin* or abus* or addict* or consum* or dependen* or disorder* or drink* or excess* or misus* or problem* or risk* or withdrawal*)).ti,ab.
1 or 2 or 3 or 4
exp music therapy/
music.ti,ab,kw.
(sing or singing or song* or choral* or choir* or melod* or lyric*).ti,ab.
6 or 7 or 8
5 and 9
exp randomized controlled trial/
exp crossover procedure/
exp double blind procedure/
exp single blind procedure/
(random* or placebo* or allocat* or crossover* or 'cross over' or trial or (doubl* adj2 blind*)).ti,ab.
11 or 12 or 13 or 14 or 15
10 and 16
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature)
S36 S33 AND S34 AND S35
S35 S8 OR S35
S34 S8 AND S16
S33 S30 OR S31 OR S32
S32 TI(sing or singing or song* or choral* or choir* or melod* or lyric*)or AB(sing or singing or song* or choral* or choir* or melod* or lyric*)
S31 TI music or AB music
S30 (MM "Music Therapy")
S29 S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28
S28 MH "Quantitative Studies"
S27 TI placebo* or AB placebo*
S26 MH "Placebos"
S25 TI random* allocat* or AB random* allocat*
S24 MH "Random Assignment"
S23 TI randomi?ed control* trial* or AB randomi?ed control* trial*
S22 AB ( singl* or doubl* or trebl* or tripl* ) and AB ( blind* or mask* )
S21 TI ( singl* or doubl* or trebl* or tripl* ) and TI ( blind* or mask* )
S20 TI clinic* N1 trial* or AB clinic* N1 trial*
S19 PT Clinical trial
S18 MH "Clinical Trials+"
S17 S8 AND S16
S16 S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15
S15 (MH "Ketamine")
S14 (MH "Amphetamines+")
S13 (MH "Methadone")
S12 (MH "Hallucinogens+")
S11 MH "Designer Drugs"
S10 MH "Narcotics"
S9 TX(polydrug or alcohol or opioid or opiate or opium or hallucinogen or cocaine or benzodiazepine* or amphetamine*or “anti‐anxiety‐agents” or barbiturate* or “lysergic acid” or ketamine or cannabis or marihuana or marijuana or hashish or inhalant* or solvent or steroid* or methadone or morphine)
S8 S5 or S6
S7 S1 or S2 or S3 or S4
S6 TX(use* N2 drug) or TX(use* N2 disorder) or TX(use* N2 illicit)
S5 TX(addict* OR overdos* OR intoxicat* OR abstin* OR abstain OR withdraw* OR abus* OR misus* OR disorder* OR dependen*)
S4 TX(substance N3 addict*) or TX(substance N3 dependen*) or TX(substance N3 abuse*) or TX(substance N3 misus*)
S3 TX(drug N3 addict*) or TX(drug N3 dependen*) or TX(drug N3 abuse*) or TX(drug N3 misus*)
S2 (MH "Psychoses, Substance‐Induced+")
S1 (MH "Substance Use Disorders+")
ERIC
S1. TI amphetamine* OR drug* OR polydrug OR substance OR cannabis OR cocaine OR "hash oil*" OR hashish OR heroin OR lsd OR marihuana OR marijuana OR methadone OR mdma OR morphine OR ecstasy OR methamphetamine* OR narcotics OR opioid* OR opiate* OR opium
S2. AB amphetamine* OR drug* OR polydrug OR substance OR cannabis OR cocaine OR "hash oil*" OR hashish OR heroin OR lsd OR marihuana OR marijuana OR methadone OR mdma OR morphine OR ecstasy OR methamphetamine* OR narcotics OR opioid* OR opiate* OR opium
S3. S1 AND S2
S4. TI abstin* OR abstain* OR abuse* OR addict* OR dependen* OR misuse OR overdose OR withdrawal* OR disorder*
S5. AB abstin* OR abstain* OR abuse* OR addict* OR dependen* OR misuse OR overdose OR withdrawal* OR disorder*
S6. S4 AND S5
S7. S3 AND S6
S8. TI ((alcohol* AND (abstain* OR abstin* OR abus* OR addict* OR consum* OR dependen* OR disorder* OR drink* OR excess* OR misus* OR problem* OR risk* OR withdrawal*))
S9. AB ((alcohol* AND (abstain* OR abstin* OR abus* OR addict* OR consum* OR dependen* OR disorder* OR drink* OR excess* OR misus* OR problem* OR risk* OR withdrawal*))
S10. S8 AND S9
S11. S7 OR S10
S12. “music therapy”
S13. “music”
S14. TI music*
S15. AB music*
S16. S14 AND S15
S17. TI sing OR singing OR song* OR choral* OR choir* OR melod* OR lyric*
S18. AB sing OR singing OR song* OR choral* OR choir* OR melod* OR lyric*
S19. S17 AND S18
S20. S12 OR S13 OR S16 OR S19
S21. Randomized controlled trial
S22. Controlled clinical trial
S23. TI randomized
S24. AB randomized
S25. S23 AND S24
S26. TI placebo
S27. AB placebo
S28. S26 and S27
S29. SU drug therapy
S30. TI randomly
S31. AB randomly
S32. S30 AND S31
S33. TI trial
S34. AB trial
S35. S33 AND S34
S36. TI groups
S37. AB groups
S38. S36 AND S37
S39. S21 OR S22 OR S25 OR S28 OR S29 OR S32 OR S35 OR S38
S40. S11 AND S20
S41. S39 AND S40
ISI Web of Science (Thomson Reuters)
TS=(((amphetamine* OR barbiturate* OR benzodiazepine* OR cannabis OR cocaine OR drug* OR hallucinogen* OR hashish OR heroin OR lsd OR marihuana OR marijuana OR methadone OR mdma OR ecstasy OR methamphetamine* OR opioid* OR opiate* OR opium OR tranquilizer* OR tranquiliser* OR inhalant* OR stimulant OR polydrug OR substance) NEAR/5 (abus* OR abstin* OR dependen* OR addict* OR disorder* OR misuse)))
TS= clinical trial* OR TS=research design OR TS=comparative stud* OR TS=evaluation stud* OR TS=controlled trial* OR TS=follow‐up stud* OR TS=prospective stud* OR TS=random* OR TS=placebo* OR TS=(single blind*) OR TS=(double blind*)
TS=(music or sing or singing or song* or choral* or choir* or melod* or lyric*)
#3 AND #2 AND #1
Indexes=SCI‐EXPANDED, SSCI, A&HCI, CPCI‐S, CPCI‐SSH, ESCI Timespan=All years
PsycINFO
exp "substance use disorder"/
exp drug addiction/
(amphetamine* or drug* or polydrug or substance or cannabis or cocaine or hash oil* or hashish or heroin or lsd or marihuana or marijuana or methadone or mdma or morphine or ecstasy or methamphetamine* or narcotics or opioid* or opiate* or opium).mp.
1 or 2 or 3
(abstin* or abstain* or abuse* or addict* or dependen* or misuse or overdose or withdrawal* or disorder*).tw.
4 and 5
exp Alcohol Abuse/ or exp Alcoholism/
alcohol*.tw.
(abstain* or abstin* or abus* or addict* or consum* or dependen* or disorder* or drink* or excess* or misus* or problem* or risk* or withdrawal*).tw.
8 and 9
7 or 10
6 or 11
exp Music Therapy/
music*.mp.
(sing or singing or song* or choral* or choir* or melod* or lyric*).tw.
13 or 14 or 15
12 and 16
exp Clinical Trials/
(random* or (clinical adj3 trial*) or (reserch adj3 design*) or (evaluat adj3 stud*) or (prospective* adj3 stud*)).tw.
((singl* or doubl* or trebl* or tripl*) adj3 (blind* or mask*)).tw.
18 or 19 or 20
17 and 21
International Bibliography of the Social Sciences (IBSS)
(((ab(amphetamine* OR drug* OR polydrug OR substance OR cannabis OR cocaine OR "hash oil*" OR hashish OR heroin OR lsd OR marihuana OR marijuana OR methadone OR mdma OR morphine OR ecstasy OR methamphetamine* OR narcotics OR opioid* OR opiate* OR opium) AND ti(amphetamine* OR drug* OR polydrug OR substance OR cannabis OR cocaine OR "hash oil*" OR hashish OR heroin OR lsd OR marihuana OR marijuana OR methadone OR mdma OR morphine OR ecstasy OR methamphetamine* OR narcotics OR opioid* OR opiate* OR opium)) AND (ab(abstin* OR abstain* OR abuse* OR addict* OR dependen* OR misuse OR overdose OR withdrawal* OR disorder*) AND ti(abstin* OR abstain* OR abuse* OR addict* OR dependen* OR misuse OR overdose OR withdrawal* OR disorder*))) OR ((ti(alcohol*) AND ab(alcohol*)) AND (ti((abstain* OR abstin* OR abus* OR addict* OR consum* OR dependen* OR disorder* OR drink* OR excess* OR misus* OR problem* OR risk* OR withdrawal*)) AND ab((abstain* OR abstin* OR abus* OR addict* OR consum* OR dependen* OR disorder* OR drink* OR excess* OR misus* OR problem* OR risk* OR withdrawal*))))) AND (all("music therapy") OR all("music") OR (ab(music*) AND ti(music*)) OR (ti(sing OR singing OR song* OR choral* OR choir* OR melod* OR lyric*) AND ab(sing OR singing OR song* OR choral* OR choir* OR melod* OR lyric*))) AND (su(randomized controlled trial) OR su(controlled clinical trial) OR (ti(randomized) AND ab(randomized)) OR (ti(randomly) AND ab(randomly)) OR (ti(trial) AND ab(trial)) OR (ti(groups) AND ab(groups)))
ProQuest Dissertations & Theses
(((ab(amphetamine* OR drug* OR polydrug OR substance OR cannabis OR cocaine OR "hash oil*" OR hashish OR heroin OR lsd OR marihuana OR marijuana OR methadone OR mdma OR morphine OR ecstasy OR methamphetamine* OR narcotics OR opioid* OR opiate* OR opium) AND ti(amphetamine* OR drug* OR polydrug OR substance OR cannabis OR cocaine OR "hash oil*" OR hashish OR heroin OR lsd OR marihuana OR marijuana OR methadone OR mdma OR morphine OR ecstasy OR methamphetamine* OR narcotics OR opioid* OR opiate* OR opium)) AND (ab(abstin* OR abstain* OR abuse* OR addict* OR dependen* OR misuse OR overdose OR withdrawal* OR disorder*) AND ti(abstin* OR abstain* OR abuse* OR addict* OR dependen* OR misuse OR overdose OR withdrawal* OR disorder*))) OR ((ti(alcohol*) AND ab(alcohol*)) AND (ti((abstain* OR abstin* OR abus* OR addict* OR consum* OR dependen* OR disorder* OR drink* OR excess* OR misus* OR problem* OR risk* OR withdrawal*)) AND ab((abstain* OR abstin* OR abus* OR addict* OR consum* OR dependen* OR disorder* OR drink* OR excess* OR misus* OR problem* OR risk* OR withdrawal*))))) AND (all("music therapy") OR all("music") OR (ab(music*) AND ti(music*)) OR (ti(sing OR singing OR song* OR choral* OR choir* OR melod* OR lyric*) AND ab(sing OR singing OR song* OR choral* OR choir* OR melod* OR lyric*))) AND (su(randomized controlled trial) OR su(controlled clinical trial) OR (ti(randomized) AND ab(randomized)) OR (ti(randomly) AND ab(randomly)) OR (ti(trial) AND ab(trial)) OR (ti(groups) AND ab(groups)))
Google Scholar (first 100 hits)
("music therapy" AND (substance OR alcohol* OR abus* OR dependen* OR addict*) AND ("randomized controlled trial" OR "randomised controlled trial" OR "clinical controlled trial" OR “cluster randomized”))
Clinical Trials Register (via clinicaltrials.gov/)
Substance use disorder AND "Music therapy"
Addiction AND "Music therapy"
substance use AND music
drug abuse AND music
drug abuse AND "music therapy"
Substance‐Related Disorders AND Music
Substance‐Related Disorders AND "music therapy"
detox AND music (therapy)
abstinence AND music
cannabis AND music OR sing* OR music therapy
alcohol‐related disorder AND music V sing* OR music therapy
amphetamine* AND music
cocaine & music AND sing* OR music therapy
World Health Organization Register (via apps.who.int/trialsearch/)
Substance use disorder AND "Music therapy"
Substance use disorder & AND Music
Addiction AND "Music therapy"
substance use AND music
drug abuse AND music
drug abuse AND "music therapy"
Substance‐Related Disorders AND Music
Substance‐Related Disorders AND "music therapy"
detox AND music (therapy)
abstinence AND music
cannabis AND music V music therapy
cannabis AND sing*
alcohol‐related disorder AND music OR sing* OR music therapy
amphetamine* AND music
amphetamine AND "music therapy"
cocaine AND music OR music therapy
Appendix 2. Criteria for the assessment of risk of bias
| No. | Item | Judgement | Description |
| 1 | Random sequence generation (selection bias) | Low risk | The investigators described a random component in the sequence generation process such as: random‐number table; computer random‐number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots; minimisation. |
| High risk | The investigators described a non‐random component in the sequence generation process such as: odd or even date of birth; date (or day) of admission; hospital or clinic record number; alternation; judgement of the clinician; preference of the participant; results of a laboratory test or a series of tests; availability of the intervention. | ||
| Unclear risk | Insufficient information about the sequence generation process to permit judgement of 'low risk' or 'high risk'. | ||
| 2 | Allocation concealment (selection bias) | Low risk | Investigators enrolling participants could not have foreseen assignment because 1 of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, Internet‐based, and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes. |
| High risk | Investigators enrolling participants could possibly have foreseen assignments and thus introduced selection bias because 1 of the following methods was used: open random allocation schedule (e.g. a list of random numbers); assignment envelopes without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure. | ||
| Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk'. This is usually the case if the method of concealment was not described or not described in sufficient detail to allow a definite judgement. | ||
| 3 | Blinding of participants and providers (performance bias) Objective outcomes |
Low risk | No blinding or incomplete blinding, but the review authors judged that the outcome was not likely to have been influenced by lack of blinding; blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken. |
| High risk | No blinding or incomplete blinding, and the outcome was likely to be influenced by lack of blinding; blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome was likely to be influenced by lack of blinding. | ||
| Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk'; the study did not address this outcome. | ||
| 4 | Blinding of participants and providers (performance bias) Subjective outcomes |
Low risk | Blinding of participants and providers ensured, and unlikely that the blinding could have been broken |
| High risk | No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding; blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding, | ||
| Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk'; the study did not address this outcome. | ||
| 5 | Blinding of outcome assessor (detection bias) Objective outcomes |
Low risk | No blinding of outcome assessment, but the review authors judged that the outcome measurement was not likely to be influenced by lack of blinding; blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. |
| High risk | No blinding of outcome assessment, and the outcome measurement was likely to be influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement was likely to be influenced by lack of blinding. | ||
| Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk'; the study did not address this outcome. | ||
| 6 | Blinding of outcome assessor (detection bias) Subjective outcomes |
Low risk | Blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. |
| High risk | No blinding of outcome assessment, and the outcome measurement was likely to be influenced by lack of blinding; blinding of outcome assessment, but likely that the blinding could have been broken, and the outcome measurement was likely to be influenced by lack of blinding. | ||
| Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk'; the study did not address this outcome. | ||
| 7 | Incomplete outcome data (attrition bias) For all outcomes except retention in treatment |
Low risk | No missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data had been imputed using appropriate methods; all randomised participants were reported/analysed in the group they were allocated to by randomisation, irrespective of non‐compliance and co‐interventions (intention‐to‐treat). |
| High risk | Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across interventions groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; 'as‐treated' analysis done with substantial departure of the intervention received from that assigned at randomisation. | ||
| Unclear risk | Insufficient reporting of attrition/exclusions to permit judgement of 'low risk' or 'high risk' (e.g. number randomised not stated, no reasons for missing data provided; the study did not address this outcome). | ||
| 8 | Selective reporting (reporting bias) | Low risk | The study protocol was available and all of the study's prespecified (primary and secondary) outcomes that were of interest in the review were reported in the prespecified way; the study protocol was not available but it was clear that the published reports included all expected outcomes, including those that were prespecified (convincing text of this nature may be uncommon) |
| High risk | Not all of the study's prespecified primary outcomes were reported; ≥ 1 primary outcomes was reported using measurements, analysis methods, or subsets of the data (e.g. subscales) that were not prespecified; ≥ 1 reported primary outcomes were not prespecified (unless clear justification for their reporting was provided, such as an unexpected adverse effect); ≥ 1 outcomes of interest in the review were reported incompletely so that they could not be entered in a meta‐analysis; the study report failed to include results for a key outcome that would be expected to have been reported for such a study. | ||
| Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk'. | ||
| 9 | Other sources of bias | Low risk | The study appeared free of other sources of bias. |
| High risk | There was ≥ 1 important risk of bias; e.g. the study had a potential source of bias related to the specific study design used; or had been claimed to have been fraudulent; or had some other problem. | ||
| Unclear risk | There may be a risk of bias, but there was either: insufficient information to assess whether an important risk of bias existed; or insufficient rationale or evidence that an identified problem would introduce bias. |
Data and analyses
Comparison 1. Music therapy plus standard care versus standard care alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Psychological outcomes (depression self‐report; various tools, BDI, HRSD, SDS; high = poor) | 3 | 100 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.72, 0.07] |
| 1.1.1 Immediately after end of intervention (longer‐term interventions, e.g. rehab: approximately 1–3 months) | 3 | 100 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.72, 0.07] |
| 1.2 Psychological outcomes short‐term follow‐up (depression self‐report, SDS; high = poor) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐6.33, 4.07] |
| 1.2.1 Short‐term follow‐up (3 months) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.13 [‐6.33, 4.07] |
| 1.3 Psychological outcomes (anxiety self‐report; SAS; high = poor) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.3.1 Immediately after end of intervention (longer‐term interventions, e.g. rehab: approximately 1–3 months) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐4.39, 4.05] |
| 1.4 Psychological outcomes short‐term follow‐up (anxiety self‐report; SAS; high = poor) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.49 [‐5.74, 2.76] |
| 1.4.1 Short‐term follow‐up (3 months) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐1.49 [‐5.74, 2.76] |
| 1.5 Substance craving (various scales; BSCS, ACQ‐SF‐R; high = poor) | 3 | 254 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.23, ‐0.10] |
| 1.5.1 Immediately after end of intervention (1‐day interventions, e.g. in detox) | 2 | 218 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.64, ‐0.09] |
| 1.5.2 Immediately after end of intervention (longer‐term interventions, e.g. rehab: approximately 1–3 months) | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.47 [‐2.21, ‐0.72] |
| 1.6 Motivation for treatment/change (various scales; CESI, ICR, CMR; high = good) | 5 | 408 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.21, 0.61] |
| 1.6.1 Immediately after end of intervention (1‐day interventions, e.g. detox) | 4 | 392 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.20, 0.64] |
| 1.6.2 Immediately after end of intervention (longer‐term interventions, e.g. rehab: approximately 1–3 months) | 1 | 16 | Std. Mean Difference (IV, Random, 95% CI) | 0.29 [‐0.70, 1.29] |
| 1.7 Motivation to stay sober/clean (various scales, high = good) | 3 | 269 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.02, 0.47] |
| 1.7.1 Immediately after end of intervention (1‐day interventions, e.g. detox) | 2 | 209 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.15, 0.55] |
| 1.7.2 Immediately after end of intervention (longer‐term interventions, e.g. rehab: approximately 1–3 months) | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | 0.26 [‐0.25, 0.77] |
| 1.8 Motivation to stay sober/clean short‐term follow‐up (QMAD, high = good) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 9.29 [‐4.60, 23.18] |
| 1.8.1 Short‐term follow‐up (3 months) | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 9.29 [‐4.60, 23.18] |
| 1.9 Retention in treatment (high = good) | 6 | 199 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.93, 1.05] |
| 1.9.1 Immediately after end of intervention (longer‐term interventions, e.g. rehab: approximately 1–3 months) | 6 | 199 | Risk Ratio (IV, Random, 95% CI) | 0.99 [0.93, 1.05] |
Comparison 2. Music therapy plus standard care versus active intervention plus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Psychological outcomes (depression self‐report; BDI; high = poor) | 1 | 110 | Mean Difference (IV, Random, 95% CI) | ‐1.49 [‐4.98, 2.00] |
| 2.1.1 Immediately after end of intervention (1‐day interventions, e.g. detox) | 1 | 110 | Mean Difference (IV, Random, 95% CI) | ‐1.49 [‐4.98, 2.00] |
| 2.2 Psychological outcomes short‐term follow‐up (depression self‐report; Likert; high = poor) | 1 | 54 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.05, 1.11] |
| 2.2.1 Short‐term follow‐up (1 month after treatment) | 1 | 54 | Mean Difference (IV, Random, 95% CI) | 0.03 [‐1.05, 1.11] |
| 2.3 Substance craving (various scales, high = poor) | 3 | 232 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.56, 0.48] |
| 2.3.1 Immediately after end of intervention (1‐day interventions, e.g. detox) | 2 | 196 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.57, 0.03] |
| 2.3.2 Immediately after end of intervention (longer‐term interventions, e.g. rehab: approximately 1–3 months) | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | 0.64 [‐0.03, 1.31] |
| 2.4 Motivation for treatment/change (various tools; RTCQ‐TV, SOCRATES, URICA; higher = good) | 5 | 411 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [‐0.00, 0.93] |
| 2.4.1 Immediately after end of intervention (1‐day interventions, e.g. detox) | 5 | 411 | Std. Mean Difference (IV, Random, 95% CI) | 0.46 [‐0.00, 0.93] |
| 2.5 Motivation to stay sober/clean (Likert, high = good) | 3 | 258 | Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.11, 0.78] |
| 2.5.1 Immediately after end of intervention (1‐day interventions, e.g. detox) | 3 | 258 | Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.11, 0.78] |
| 2.6 Substance use short‐term follow‐up (self‐report) | 1 | 140 | Risk Ratio (IV, Random, 95% CI) | 1.05 [0.85, 1.29] |
| 2.6.1 Short‐term follow‐up (1‐month post‐discharge) | 1 | 140 | Risk Ratio (IV, Random, 95% CI) | 1.05 [0.85, 1.29] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Albornoz 2009.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Randomisation method: block randomisation using random number lists, completed by statistician Allocation concealment: sequentially numbered envelopes created to ensure allocation concealment |
|
| Participants |
Baseline characteristics MT + SC
SC
Overall
Inclusion criteria: some type of addiction problem, including addiction or abuse of psychotropic and pharmacological substances, including alcohol; recently admitted to treatment programme for substance abuse at the centre; scores on BDI or HRSD that indicated that they were significantly depressed (i.e. > 10 on BDI, and > 7 on HRSD). Exclusion criteria: unable to communicate (aphasia); diagnosed with mental retardation and incapable of symbolic thinking; hearing losses that impaired their abilities to hear music or the spoken word; not receiving medication for depression. Pretreatment: no significant difference between groups on pretest BDI (Albornoz 2009, p.35), and no significant differences between groups on pretest HRSD (p.37). Confirmation of population eligibility (from study author): email 9 July 2017: "Participants were diagnosed by psychiatrist/psychologist with the related substance abuse/addiction/dependence diagnoses as per DSM‐IV/ICD‐10". |
|
| Interventions |
Intervention characteristics MT + SC
SC
|
|
| Outcomes |
Self‐report depression (BDI)
Depression – observational report (HRSD)
Retention in treatment
|
|
| Identification |
Sponsorship source: none Country: Venezuela Setting: inpatient and outpatient substance use treatment facility Author's name: Yadira Albornoz Institution: Universidad de los Andes‐Venezuela Email: yadira98@hotmail.com Address: Universidad de los Andes‐Venezuela, Mérida, Venezuela Declarations of interest: no conflicts of interest reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: p.24 – random number lists in blocks (generated by statistician). |
| Allocation concealment (selection bias) | Low risk | Judgement comment: sequentially numbered envelopes were created to ensure allocation concealment. |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: outcome assessor blinded for retention in treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: no missing outcome data. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers for MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: psychologist completing HRSD was blinded to treatment allocation and participant medical and psychiatric history. Not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Eshaghi Farahmand 2020.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Allocation concealment: method for allocation concealment not specified Randomisation method: the researcher interviewed and surveyed the inclusion and exclusion criteria and 60 people were selected by purposive sampling; then, randomly divided into 3 groups. The researcher then randomly selected into 2 experimental groups and 1 control group. Then 1 of the experimental groups was randomly assigned to 8 sessions of MT and the other group 8 sessions of CBT by the researcher. The control group received no training. |
|
| Participants |
Baseline characteristics MT + SC
CBT + SC
SC
Overall
Inclusion criteria: addicts on methadone maintenance treatment; aged 18–40 years; male gender; no physical problems; no history of exposure to psychological training; no history of stimulant use Exclusion criteria: failure of the sample group or family to participate in each phase of the study; having physical or mental problems; history of psychiatric problems; professional athletes; aged > 40 years; history of stimulant use Pretreatment: not specified |
|
| Interventions |
Intervention characteristics MT + SC
CBT + SC
SC
|
|
| Outcomes |
Craving (OCDUS)
Retention in treatment
Not used: QoL (Quality of Life Questionnaire); positive cognitive emotion regulation and negative cognitive emotion regulation (Cognitive Emotion Regulation Questionnaire) |
|
| Identification |
Sponsorship source: none mentioned Country: Iran Setting: addiction treatment clinic affiliated with Tehran Health Organization Author's name: Seyed Reza Eshaghi Farahmand, Hassan Ahadi Institution: Department of Health Psychology, Kish International Branch, Islamic Azad University; Department of Psychology, Allameh Tabataba'i University Email: drhahadi5@gmail.com Address: Department of Psychology, Allameh Tabataba'i University, Tehran, Iran Declarations of interest: no conflicts of interest reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: researcher randomly allocated 60 people meeting inclusion criteria to 3 groups. 2 of these groups were randomly allocated as experimental groups and 1 as control group. 1 experimental group was randomly allocated to MT, and the other to CBT. Control group received no training. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: method of allocation concealment not specified. |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: outcome assessor blinded for retention in treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: number of participants analysed in each group was not clearly specified. Participants who did not attend all sessions were excluded. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Heiderscheit 2005.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Randomisation method: coin flip Allocation concealment: unclear, insufficient information |
|
| Participants |
Baseline characteristics MT + SC
SC
Overall
Inclusion criteria: admitted to the inpatient chemical dependency programme at a skilled nursing facility Exclusion criteria: non‐English speaking; diagnosis of dementia, psychosis, or psychotic state Pretreatment: the difference in number of previous treatment episodes between the experimental and control groups was not statistically significant. The difference between groups on the length of current treatment was not statistically significant. Confirmation of population eligibility (from study author): author confirmed via email on 14 September 17: "All the clients enrolled in the study carried a primary diagnosis of substance dependence/abuse per the DSM‐IV, as it was an addictions treatment program". |
|
| Interventions |
Intervention characteristics MT + SC
SC
|
|
| Outcomes |
Retention in treatment
Not used: Interpersonal problems (IIP‐SC), sense of coherence (Sense of Coherence Scale), immunofunction (salivary immunoglobulin A) |
|
| Identification |
Sponsorship source: none Country: USA Setting: adult inpatient substance abuse treatment programme Author's name: Annette Lynne Heiderscheit Institution: Augsburg College Email: heidersc@augsburg.edu Declarations of interest: no conflicts of interest reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: random assignment by use of coin toss. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: used a coin flip, which does not assure adequate concealment of allocation. |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: outcome assessor blinded for retention in treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: no missing outcome data. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
James 1988.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Allocation concealment: not specified Randomisation method: not specified |
|
| Participants |
Baseline characteristics MT + SC
SC
Overall
Inclusion criteria: primary diagnosis of substance abuse or substance dependency (APA 1980); adolescents currently admitted to inpatient unit for treatment of chemical dependency Exclusion criteria: not specified Pretreatment: no significant differences between groups in chronological age, male:female ratio, level of education and length of hospitalisation. No significant differences between groups on pretest scores of local of control |
|
| Interventions |
Intervention characteristics MT + SC
SC
|
|
| Outcomes |
Retention in treatment
Not used: Locus of control (External Internal Locus of Control) |
|
| Identification |
Sponsorship source: – Country: USA Setting: inpatient chemical dependency unit in a free‐standing facility Comments: – Author's name: Mark R James Institution: Elizabeth General Medical Center Declarations of interest: no conflicts of interest reported. |
|
| Notes | Email (7 July 2017) from author confirmed report included 2 studies James 1988a and James 1988b. Only James 1988a met eligibility criteria. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: insufficient information about the sequence generation to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: no missing outcome data. |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Murphy 2008.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Randomisation method: computer program that randomly assigned participants to groups (graphpad.com) Allocation concealment: not sufficiently described |
|
| Participants |
Baseline characteristics MT + SC
SC
Overall
Inclusion criteria: ≥ 18 years; competent to consent to participation; meets the DSM‐IV criteria for substance abuse or substance dependence; able to understand English in order to comprehend the interview questions, questionnaires, and consent forms Exclusion criteria: no information Pretreatment: no significant differences between MT and SC groups on BDI at pretest, and no significant differences between groups on ICR at pretest. |
|
| Interventions |
Intervention characteristics MT + SC
SC
|
|
| Outcomes |
Self‐report depression (BDI)
Retention in treatment
Motivation for change – ICR
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient drug and alcohol residential treatment facility Comments: Murphy (2008) is author's dissertation Author's name: Kathleen M Murphy Institution: Temple University Email: kmmurphy@loyno.edu Declarations of interest: no conflicts of interest reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: randomisation was applied using a computer program. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information to permit judgement. |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: outcome assessor blinded for objective outcome (retention in treatment). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement (number of randomised not stated, no reasons for missing data provided). |
| Selective reporting (reporting bias) | Low risk | Judgement comment: all outcome data were reported. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2009.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: not specified Randomisation method: consumers in 16 sessions were randomised into experimental or control conditions by session. The numbers 1 to 16 were randomised into 2 groups and each group was assigned to a condition. Participants were allocated to the group of the first session they attended. |
|
| Participants |
Baseline characteristics MT + SC
Verbal therapy + SC
Overall
Inclusion criteria: inpatient on detoxification unit Exclusion criteria: none mentioned Pretreatment: no significant differences between groups in relation to: number of consumers taking part in each session who volunteered to be research participants; total number of consumers in each session; research participants' ages; number of times in rehabilitation/detoxification facility Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
Verbal therapy + SC
|
|
| Outcomes |
Motivation for treatment/change – SOCRATES
Not used: Working alliance (HAQ‐II) |
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Declarations of interest: no conflicts of interest reported |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: insufficient information about the sequence generation process to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2010.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: method for allocation concealment not specified Randomisation method: consumers in 24 sessions were randomised into experimental or control conditions by session. The numbers 1–24 were randomised into 2 groups and each group was assigned to a condition. Participants were allocated to the group of the first session they attended. |
|
| Participants |
Baseline characteristics MT + SC
Verbal therapy + SC
Overall
Inclusion criteria: inpatient on detoxification unit Exclusion criteria: none mentioned Pretreatment: no significant differences between groups at baseline in regard to: number of inpatients who volunteered to be research participants; total number of inpatients in each session; participants' ages; number of times participants had been admitted to a rehabilitation/detoxification facility. Confirmation of population eligibility (from study author): author confirmed by email (13 September 2017) that participants met inclusion criteria for this review. |
|
| Interventions |
Intervention characteristics MT + SC
Verbal therapy + SC
|
|
| Outcomes | Not used: withdrawal symptoms (Adjective Rating Scale for Withdrawal); internal external locus of control (The Drinking‐related Internal‐external Locus of Control Scale) | |
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit of a large teaching hospital Comments: author confirmed by email (13 September 2017) that participants met inclusion criteria for this review. Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Declarations of interest: no conflicts of interest reported. |
|
| Notes | Email (13 September 2017) from author confirmed that participants met our criteria. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: consumers in 24 sessions were randomised into experimental or control conditions by session. The numbers 1–24 were randomised into 2 groups and each group was assigned to a condition. Participants were allocated to the group of the first session they attended. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: method for allocation concealment not specified. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2011a.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: not specified Randomisation method: participants in 28 sessions were randomised into experimental or control conditions by session. The numbers 1–28 were randomised into 2 groups and each group was assigned to a condition. |
|
| Participants |
Baseline characteristics MT + SC
Verbal therapy + SC
Overall
Inclusion criteria: inpatients in an adult detoxification unit Exclusion criteria: none specified Pretreatment: no significant differences between groups in regard to: number of consumers taking part in each session who volunteered to be research participants; total number of consumers in each session; participants' ages. Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
Verbal therapy + SC
|
|
| Outcomes |
Self‐report depression (BDI)
Depression – self‐report via Likert‐type scale
Motivation for change – URICA Contemplation subscale
Motivation for change – URICA Action subscale
Substance use – self‐report
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Declarations of interest: no conflicts of interest reported. |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: participants in 28 sessions were randomised into experimental or control conditions by session. The numbers 1–28 were randomised into 2 groups and each group was assigned to a condition. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement unlikely to be influenced differentially between groups. |
Silverman 2011b.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: methods related to allocation concealment not specified Randomisation method: participants in 27 sessions were cluster randomised into conditions A, B, or C by session. The numbers 1–27 were randomised into 3 groups and each group was assigned to a condition. |
|
| Participants |
Baseline characteristics MT + SC
Verbal therapy + SC
Recreational music + SC
Overall
Inclusion criteria: inpatient status on detoxification unit (author confirmed that participants had SUD) Exclusion criteria: none specified Pretreatment: no significant differences between groups at pretest for: number of inpatients electing to be part of the session; total number of inpatients in each session; total number of times participants had been admitted to a substance abuse or detox facility; age. Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
Verbal therapy + SC
Recreational music + SC
|
|
| Outcomes |
Readiness to change (precontemplation) – RTCQ‐TV, Precontemplation subscale
Readiness to change (contemplation) – RTCQ‐TV, Contemplation subscale
Readiness to change (action) – RTCQ‐TV, Action subscale
Substance craving – BSCS
Motivation to stay sober/clean – Likert‐type scale
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Comments: unit was part of a larger University hospital Author's name: Michael J Silverman Institution: University of Minnesota Declarations of interest: no conflicts of interest reported. |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: method of sequence generation not specified. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: information on allocation concealment not specified. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: reasons for missing data not provided. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2012.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: method of allocation concealment not specified Randomisation method: consumers in 16 sessions were randomised into experimental or control conditions by session. The numbers 1–16 were randomised into 2 groups and each group was assigned to a condition. Participants were allocated to the group of the first session they attended. |
|
| Participants |
Baseline characteristics MT + SC
SC (wait‐list control)
Overall
Inclusion criteria: inpatient status on detoxification unit Exclusion criteria: none specified Pretreatment: no statistically significant differences between groups at baseline in regard to: number of inpatients who volunteered to be research participants; total number of inpatients in each session; participants' ages; number of times participants had been admitted to a rehabilitation/detoxification facility. No significant differences between groups in gender; race/ethnicity; drug of choice. Confirmation of population eligibility (from study author): author confirmed by email that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
SC (wait‐list control)
|
|
| Outcomes |
Motivation for treatment – Circumstances, Motivation, and Readiness Scales for Substance Abuse Treatment, Motivation subscale
Readiness for treatment – Circumstances, Motivation, and Readiness Scales for Substance Abuse Treatment, Readiness subscale
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit of a large teaching hospital Author's name: Michael J Silverman Institution: University of Minnesota Declarations of interest: no conflicts of interest reported |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: methods of sequence generation not specified. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: method for allocation concealment not specified. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: reasons for missing outcome data not specified. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2014.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: not specified Randomisation method: cluster randomisation via a computer program into conditions by session. Numbers 1–24 were randomised into 3 groups, and each group was assigned to a condition. |
|
| Participants |
Baseline characteristics MT + SC
Verbal therapy + SC
SC (wait‐list control)
Overall
Inclusion criteria: adult inpatients on a detoxification unit Exclusion criteria: not specified Pretreatment: no statistically significant differences between groups for age; number of previous admissions; length of stay on detoxification unit; number of participants taking part in each session who volunteered to be research participants; total number of participants in each session. No statistically significant differences between groups for gender; ethnic background; or drug of choice. Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
Verbal therapy + SC
SC (wait‐list control)
|
|
| Outcomes |
Motivation to stay sober/clean – Likert‐type scale
Motivation for treatment – Likert‐type scale
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Declarations of interest: no conflicts of interest reported |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: participants in 24 sessions were cluster randomised via a computer program into conditions by session. The numbers 1–24 were randomised into 3 groups, and each group was assigned to a condition. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: imbalance in numbers of missing data across intervention groups. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2015a.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: not specified Randomisation method: participants in 15 sessions were cluster randomised into conditions by session. The numbers 1–15 were randomised into 3 groups and each group was assigned to a condition. Not otherwise specified. |
|
| Participants |
Baseline characteristics MT + SC
Verbal therapy + SC
Recreational music + SC
Overall
Inclusion criteria: inpatient on detoxification unit Exclusion criteria: none mentioned Pretreatment: no significant differences between groups in regard to: number of participants taking part in each session who volunteered to be research participants; total number of participants in each session; total number of times participants had been admitted to a substance abuse facility; age; gender; race/ethnicity; drug of choice. Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
Verbal therapy + SC
Recreational music + SC
|
|
| Outcomes |
Motivation to stay sober/clean – Likert‐type scale
Motivation for treatment – Likert‐type scale
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Declarations of interest: no conflicts of interest reported |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: participants in 15 sessions were cluster randomised into conditions by session. The numbers 1–15 were randomised into 3 groups and each group was assigned to a condition. Not otherwise specified. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2015b.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: not specified Randomisation method: throughout 18 MT treatment sessions, the researcher cluster randomised consumers into experimental or control conditions by session. The numbers 1–18 were randomised into 2 groups, and each group was assigned to either the experimental or control condition. |
|
| Participants |
Baseline characteristics MT + SC
SC (wait‐list control)
Overall
Inclusion criteria: inpatient on detoxification unit; ability to read English Exclusion criteria: none mentioned Pretreatment: no significant differences between groups in regard to: number of consumers taking part in each session who volunteered to be research participants; total number of consumers in each session; participants' age; number of times had been in rehabilitation/detoxification facility; gender; race/ethnicity; drug of choice. Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
SC (wait‐list control)
|
|
| Outcomes |
Motivation for treatment – the Texas Christian University Treatment Motivation Scale – CESI
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Declarations of interest: no conflicts of interest reported. |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: throughout 18 MT treatment sessions, the researcher cluster randomised participants into experimental or control conditions by session. The numbers 1–18 were randomised into 2 groups, and each group was assigned to either the experimental or control condition. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2016a.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: method for allocation concealment not specified Randomisation method: participants in 24 sessions were randomised into 1 of 4 conditions by session. The numbers 1–24 were randomised into 4 groups and each group was assigned to a condition. Participants were allocated to the group of the first session they attended. If a participant who had already participated in the study was readmitted due to relapse, she or he was eligible for the therapy session but ineligible for research study inclusion. |
|
| Participants |
Baseline characteristics MT (lyric analysis with live music) + SC
MT (lyric analysis with recorded music) + SC
Verbal therapy + SC
Recreational music + SC
Overall
Inclusion criteria: inpatient on a detoxification unit Exclusion criteria: none mentioned Pretreatment: no significant differences between groups in regard to: number of participants taking part in each session who volunteered to be research participants; total number of participants in each session; age; number of days had been an inpatient on the unit; total number of times participants had been admitted to a rehabilitation/detoxification facility. Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT (lyric analysis with live music) + SC
MT (lyric analysis with recorded music) + SC
Verbal therapy + SC
Recreational music + SC
|
|
| Outcomes | Not used: working alliance (WAI‐S); trust in therapist (Wake Forest Physician Trust Scale) | |
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Address: School of Music, University of Minnesota, Minneapolis, Minnesota, USA Declarations of interest: no conflicts of interest reported |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: participants in 24 sessions were randomised into 1 of 4 conditions by session. The numbers 1–24 were randomised into 4 groups and each group was assigned to a condition. Participants were allocated to the group of the first session they attended. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2016b.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: not specified Randomisation method: consumers in 24 sessions were randomised into experimental or control conditions by session. Thus, each session was assigned to an experimental or control condition consistent with cluster randomisation. |
|
| Participants |
Baseline characteristics MT + SC
SC (wait‐list control)
Overall
Inclusion criteria: inpatient on short‐term detoxification unit; able to read and write in English Exclusion criteria: none specified Pretreatment: no significant differences between groups in regard to participants' ages; number of times admitted to a rehabilitation/detoxification facility; number of days on the detoxification unit; gender; ethnic background; drug of choice. Significant between‐group differences in number of patients taking part in each session who volunteered to be research participants and total number of participants in each session (wait‐list control group had greater means than experimental group for both). Confirmation of population eligibility (from study author): author confirmed that participants had diagnosis of SUD. |
|
| Interventions |
Intervention characteristics MT + SC
SC (wait‐list control)
|
|
| Outcomes |
Substance craving – BSCS
Not used: symptoms of withdrawal (Adjective Rating Scale for Withdrawal)
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Declarations of interest: no conflicts of interest reported |
|
| Notes | Email (13 September 2017) from author confirmed that participants met criteria for SUD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: insufficient information about the sequence generation process to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2017.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: no information on allocation concealment Randomisation method: throughout 24 MT treatment sessions, the researcher cluster‐randomised consumers into conditions by session. A computer program was used for randomisation. The numbers 1–24 were randomised into 3 groups and each group was assigned to MT (songwriting), recreational music, or wait‐list control. |
|
| Participants |
Baseline characteristics MT + SC
Recreational music + SC
SC (wait‐list control)
Overall
Inclusion criteria: inpatient status on detoxification unit; ability to read English Exclusion criteria: none stated Pretreatment: significant between‐group differences in number of patients taking part in each session who volunteered to be research participants and the total number of participants in each session (with MT having lower means than the recreational music and wait‐list control conditions). No statistically significant between‐group differences in participants' ages; number of times participants had been in a rehabilitation/detoxification facility; or demographic variables of gender, race/ethnicity, or primary drug. |
|
| Interventions |
Intervention characteristics MT + SC
Recreational music + SC
SC (wait‐list control)
|
|
| Outcomes |
Substance craving – Alcohol Craving Questionnaire – Short Form – Revised (ACQ‐SF‐R)
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Address: University of Minnesota, Minneapolis, Minnesota, USA Declarations of interest: no conflicts of interest reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: use of computerised random‐number generator. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2019a.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: method for allocation concealment not specified Randomisation method: through 24 sessions, participants were cluster‐randomised into 3 groups via a computer program. Participants were allocated the group of the first session they attended. |
|
| Participants |
Baseline characteristics MT (lyric analysis) + SC
MT (song writing) + SC
Recreational music + SC
Overall
Inclusion criteria: inpatient on short‐term detoxification unit (thus, with diagnosis of SUD); ability to read English Exclusion criteria: none mentioned Pretreatment: no significant differences between groups in regard to: number of people taking part in each session who volunteered to be research participants; total number of participants in each session; age; number of times they had been in rehabilitation/detoxification facility; gender; ethnic background; primary drug. |
|
| Interventions |
Intervention characteristics MT (lyric analysis) + SC
MT (song writing) + SC
Recreational music + SC
|
|
| Outcomes |
Not used: Group experience (Ferrara Group Experiences Scale) |
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit of a large teaching hospital Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Address: Music Therapy Department, University of Minnesota, Minneapolis, USA Declarations of interest: no conflicts of interest reported. |
|
| Notes | Email (25 March 2021) from author confirmed report is the same as the Silverman 2021. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: participants in 24 sessions were cluster randomised via a computer program into conditions by session. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: no incomplete outcome data. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2019b.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: method for allocation concealment not specified Randomisation method: throughout 20 total treatment sessions/clusters, the researcher randomised participants into experimental or control conditions by session/cluster. The researcher randomised the numbers 1–20 into 2 groups and each group was assigned to either the experimental or control condition. Participants were allocated the group of the first session they attended. |
|
| Participants |
Baseline characteristics MT + SC
SC (wait‐list control)
Overall
Inclusion criteria: adults hospitalised on a detoxification unit (meeting diagnosis for SUD); able to read English Exclusion criteria: none mentioned Pretreatment: no statistically significant differences between groups at baseline in regard to: number of people taking part in each session who volunteered to be research participants; total number of participants in each session; ages; number of times admitted to a SUD rehabilitation or detoxification facility; gender; race/ethnicity; primary drug. |
|
| Interventions |
Intervention characteristics MT + SC
SC (wait‐list control)
|
|
| Outcomes |
Not used: Shame, guilt, pride (State Shame and Guilt Scale) |
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit of a large teaching hospital Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Address: University of Minnesota, Minneapolis, Minnesota, USA Declarations of interest: no conflicts of interest reported |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: the researcher randomised the numbers 1–20 into 2 groups and each group was assigned to either the experimental (over 10 sessions/clusters) or control (over 10 sessions/clusters) condition. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: method for allocation concealment not specified. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: no missing outcome data. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT interventions. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2020.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: method for allocation concealment not specified Randomisation method: throughout 24 sessions, the researcher cluster‐randomised people on the unit into experimental or control conditions by session. The numbers 1–24 were randomised into 2 groups and each group was assigned to either the experimental or control condition. Participants were allocated the group of the first session they attended. |
|
| Participants |
Baseline characteristics MT + SC
SC (wait‐list control)
Overall
Inclusion criteria: adult inpatient on detoxification unit (meeting diagnostic criteria for substance dependency); ability to read English. Exclusion criteria: none mentioned Pretreatment: no significant differences between groups in regard to: total number of times participants had been admitted to a substance abuse facility; days on the unit; number of patients taking part in each session who volunteered to be research participants; total number of participants in each session; age; gender; ethnic background; drug of choice. |
|
| Interventions |
Intervention characteristics MT + SC
SC (wait‐list control)
|
|
| Outcomes |
Not used: Perceived stigma (Perceived Stigma and Addiction Scale (PSAS)); Perceived social support (the Multidimensional Scale of Perceived Social Support (MSPSS)) |
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit of a large teaching hospital Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Address: Music Therapy, University of Minnesota, Minneapolis, Minnesota, USA Declarations of interest: no conflicts of interest reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Judgement comment: throughout 24 sessions, the researcher cluster‐randomised people on the unit into experimental or control conditions by session. The numbers 1–24 were randomised into 2 groups and each group was assigned to either the experimental or control condition. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: information on allocation concealment not specified. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Silverman 2021.
| Study characteristics | ||
| Methods |
Study design: cluster RCT Study grouping: parallel group Allocation concealment: method for allocation concealment not specified Randomisation method: throughout 22 total treatment sessions, the researcher cluster randomised participants into conditions by session using a computer program. Numbers 1–22 were randomised into 2 groups and each group was assigned to either the lyric analysis or control condition. |
|
| Participants |
Baseline characteristics MT + SC
SC (wait‐list control)
Overall
Inclusion criteria: adults hospitalised on detoxification unit (and meeting criteria for SUD); able to read English Exclusion criteria: none mentioned Pretreatment: no statistically significant differences between groups at baseline for: ages; number of times admitted to a SUD rehabilitation/detoxification facility; number of service users taking part in each session who volunteered to be research participants; total number of service users in each session; gender; race; primary substance. |
|
| Interventions |
Intervention characteristics MT + SC
SC (wait‐list control)
|
|
| Outcomes |
Motivation for treatment/change (SOCRATES – Taking Steps subscale)
Motivation for treatment/change (Recognition scale of SOCRATES)
Motivation to stay clean/sober (CSS)
|
|
| Identification |
Sponsorship source: none Country: USA Setting: inpatient detoxification unit of a large teaching hospital Author's name: Michael J Silverman Institution: University of Minnesota Email: silvermj@umn.edu Address: School of Music, University of Minnesota, Minneapolis, Minnesota, USA Declarations of interest: no conflicts of interest reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: participants in 22 sessions were cluster randomised via a computer program into conditions by session. The numbers 1–22 were randomised into 2 groups and each group was assigned to either the lyric analysis or control condition. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Reasons for missing outcome data unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Judgement comment: not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
Wu 2020.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Allocation concealment: participants in the MT group knew they were receiving MT intervention but did not know the detailed interventional content in the control group. Also, the psychotherapist was blinded to the aims and design of this study. Randomisation method: a statistician who was not directly involved in the research randomised participants to 1 of the groups using the sample random‐sampling method. |
|
| Participants |
Baseline characteristics MT + SC
SC
Overall
Inclusion criteria: meeting DSM‐5 criteria for MUD; > 6 years of education; providing written informed consent; scoring ≥ 50 on Self‐Rating Depression Scale Exclusion criteria: serious physical or neurological illness; substance dependence other than MUD, nicotine use, and social alcohol drinking Pretreatment: there were no differences between the MT group and the SC group for gender, education, marital status, employment, or drug use history. |
|
| Interventions |
Intervention characteristics MT + substance use
SC
|
|
| Outcomes |
Motivation to stay clean from drugs (QMAD)
Depression (SDS)
Anxiety (SAS)
Retention in treatment
Not used: Emotion regulation strategies (Emotion Regulation Questionnaire); Empathy (Interpersonal Reactivity Index) |
|
| Identification |
Sponsorship source: National Key R&D Program of China [2017YFC1310400], National Nature Science Foundation [81771436, 81601164, U1502228], Shanghai Municipal Health and Family Planning Commission [2017ZZ02021], Municipal Human Resources Development Program for Outstanding Young Talents in Medical and Health Sciences in Shanghai [2017YQ013], Shanghai Key Laboratory of Psychotic Disorders [13DZ2260500], and Program of Shanghai Academic Research Leader [17XD1403300]. Country: China Setting: compulsory drug rehabilitation centre Author's name: Qianying Wu; Min Zhao Institution: Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine Email: drminzhao@gmail.com Address: Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China Declarations of interest: no conflicts of interest reported. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Judgement comment: a statistician who was not directly involved in the research randomised participants to 1 group using the sample random‐sampling method. |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: method of allocation concealment not specified. |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Not possible to blind participants and providers to MT intervention. |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: outcome assessor blinded for retention in treatment. Other outcome measures were performed by blinded researchers who were not involved in the treatment sessions. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: no missing outcome data. |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no selective outcome reporting. |
| Blinding of participants and providers (performance bias) (subjective outcomes) | Low risk | Not possible to blind participants and providers to MT intervention. Participants in the MT group knew they were receiving MT but did not know the detailed interventional content in the SC group. Interventionist was blinded to aims and purposes of the study. |
| Blinding of outcome assessor (detection bias) (subjective outcomes) | Unclear risk | Judgement comment: not possible to blind outcome assessor for self‐report outcomes, though measurement not likely to be influenced differentially between groups. |
ACQ‐SF‐R: Alcohol Craving Questionnaire‐Short Form Revised; BDI: Beck Depression Inventory; BMGIM: Bonny Method of Guided Imagery and Music; BSCS: Brief Substance Craving Scale; CBT: cognitive behavioural therapy; CESI: Client Evaluation of Self at Intake; CSC: Commitment to Sobriety Scale; DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; DSM‐5: Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; GIM: Guided Imagery and Music; HAQ‐II: Helping Alliance Questionnaire – II; HRSD: Hamilton Rating Scale for Depression; ICD‐10: International Classification of Diseases 10th Version; ICR: Importance, Confidence, Readiness Ruler; IIP‐SC: Inventory of Interpersonal Problems Short Circumplex; MT: music therapy; OCDUS: Obsessive Compulsive Drug Use Scale; QMAD: Questionnaire of Motivation for Abstaining from Drugs; QoL: quality of life; RCT: randomised controlled trial; RTCQ‐TV: Readiness to Change Questionnaire – Treatment Version; SAS: Self‐rating Anxiety Scale; SC: standard care; SD: standard deviation; SDS: Severity of Dependence Scale; SOCRATES: Stages of Change Readiness and Treatment Eagerness Scale; SUD: substance use disorder; URICA: University of Rhode Island Change Assessment Scale; WAI‐S: Working Alliance Inventory – Short Form.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Baker 2007 | Wrong study design: not randomised controlled trial |
| Bibb 2018 | Wrong study design: not randomised controlled trial |
| Chandrasekar 2020 | Wrong intervention: use of music not qualifying as music therapy |
| Dingle 2008 | Wrong study design: not randomised controlled trial |
| Gallant 1997 | Wrong intervention: use of music not qualifying as music therapy |
| Gardstrom 2013 | Wrong study design: not randomised controlled trial |
| Haddock 2003 | Wrong intervention: intervention did not include music |
| Hammer 1996 | Wrong participant population: mix of patients and staff |
| Howard 1997 | Wrong study design: not randomised controlled trial |
| Jones 2005 | Wrong comparator: lacked relevant control group |
| Lu 2005 | Wrong intervention: use of music not qualifying as music therapy |
| Malcolm 2002 | Wrong intervention: used combination of therapies |
| Mathis 2017 | Wrong intervention: use of music not qualifying as music therapy |
| Moe 2011 | Wrong study design: not randomised controlled trial |
| Murphy 2015 | Wrong study design: not randomised controlled trial |
| Oklan 2014 | Wrong study design: not randomised controlled trial |
| Sewak 2018 | Wrong intervention: use of music not qualifying as music therapy |
| Silverman 2016c | Wrong patient population: psychiatric patients not diagnosed with substance use disorders |
| Stamou 2016 | Wrong intervention: use of music not qualifying as music therapy |
| Stamou 2017 | Wrong intervention: use of music not qualifying as music therapy |
| Taylor 2005 | Wrong study design: not randomised controlled study |
| Wheeler 1985 | Wrong study design: not randomised controlled study |
Differences between protocol and review
When appropriate, we had planned to combine results of cross‐over trials with those of parallel‐group trials, analysing data from the first phase only (i.e. before cross‐over) to avoid carry‐over effects, but the search identified no cross‐over trials.
When studies had more than one relevant MT intervention, we planned to combine all such experimental groups into a single group, as recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), but the search identified no such studies.
None of our meta‐analyses contained a sufficient number of studies to warrant assessment of funnel plots. There were no meta‐analyses of multiple trials in which one or more trials had attrition rates higher than 20%, and thus it was not possible to conduct a sensitivity analysis.
Contributions of authors
Conceiving the review: XJC, CGh, CGo.
Designing the review: XJC, CGh, CGo.
Co‐ordinating the review: CGh.
Data collection for the review: designing search strategies: CGh; undertaking searches: CGh, LH; screening search results: CGh, XJC.
Appraising risk of bias in the included studies: AB, XJC, CGh.
Extracting data from reports: XJC, CGh.
Writing to authors for additional information: XJC, CGh.
Resolving disagreements in eligibility or data extraction: CGo, LH.
Data management for the review: AB, XJC, CGh.
Analysis of data: AB, CGh, CGo.
Assessment of certainty in the body of evidence: CGh, CGo.
Interpretation of data: AB, XJC, JF, CGh, CGo, LL.
Writing the review: AB, XJC, CGh, CGo, LH, LL.
Securing funding for the review: CGh.
Sources of support
Internal sources
-
The Grieg Academy, University of Bergen, Norway
Provision of salary for review authors
-
NORCE Norwegian Research Centre AS, Bergen, Norway
Provision of salary for review authors
External sources
-
POLYFON Kunnskapsklynge for musikkterapi, Norway
Provision of funding for research assistant
Declarations of interest
CGh: none.
XJC: none.
AB: none.
LH: none.
LL: none.
JF: none.
CG: none.
New
References
References to studies included in this review
Albornoz 2009 {published data only}
- Albornoz Y.The effects of group improvisational music therapy on depression in adolescents and adults with substance abuse: a randomized controlled trial. Nordic Journal of Music Therapy 2011;20(3):208-24. [DOI: 10.1080/08098131.2010.522717] [DOI] [Google Scholar]
- Albornoz Y.The Effects of Group Improvisational Music Therapy on Depression in Adolescents and Adults with Substance Abuse [Doctoral dissertation]. Philadelphia (PA): Temple University, 2009. [Google Scholar]
Eshaghi Farahmand 2020 {published data only}
- Eshaghi Farahmand S, Ahadi H, Kalhornia Golkar M, Sedaghat M.Comparison of the effectiveness of music therapy and cognitive behavioral therapy on quality of life, craving and emotion regulation in patients under methadone maintenance therapy. Iranian Journal of Psychiatry and Clinical Psychology 2020;26(2):170-87. [DOI: 10.32598/ijpcp.26.2.3212.1] [DOI] [Google Scholar]
Heiderscheit 2005 {published data only}
- Heiderscheit A.The effects of the Bonny Method of Guided Imagery and Music (GIM) on interpersonal problems, sense of coherence, and salivary immunoglobulin A of adults in chemical dependency treatment. Music & Medicine 2017;9(1):24-36. [Google Scholar]
- Heiderscheit AL.The Effects of the Bonny Method of Guided Imagery and Music (GIM) on Adults in Chemical Dependency Treatment: Sense of Coherence, Salivary Immunoglobulin A and Interpersonal problems [Doctoral dissertation]. Minneapolis (MN): University of Minnesota, 2005. [UNIVERSITY OF MINNESOTA DIGITAL CONSERVANCY: hdl.handle.net/11299/160300] [Google Scholar]
James 1988 {published data only}
- James MR.Music therapy values clarification: a positive influence on perceived locus of control. Journal of Music Therapy 1988;25(4):206-15. [Google Scholar]
Murphy 2008 {published data only}
- Murphy KM.The Effects of Group Guided Imagery and Music on the Psychological Health of Adults in Substance Abuse Treatment [Doctoral dissertation]. Philadelphia (PA): Temple University, 2008. [Google Scholar]
Silverman 2009 {published data only}
- Silverman MJ.The effect of lyric analysis on treatment eagerness and working alliance in consumers who are in detoxification: a randomized clinical effectiveness study. Music Therapy Perspectives 2009;27(2):115-21. [DOI: 10.1093/mtp/27.2.115] [DOI] [Google Scholar]
Silverman 2010 {published data only}
- Silverman MJ.The effect of a lyric analysis intervention on withdrawal symptoms and locus of control in patients on a detoxification unit: a randomized effectiveness study. Arts in Psychotherapy 2010;37(3):197-201. [DOI: 10.1016/j.aip.2010.04.001] [DOI] [Google Scholar]
Silverman 2011a {published data only}
- Silverman MJ.Effects of music therapy on change and depression on clients in detoxification. Journal of Addictions Nursing 2011;22(4):185-92. [DOI: 10.3109/10884602.2011.616606] [DOI] [Google Scholar]
Silverman 2011b {published data only}
- Silverman MJ.Effects of music therapy on change readiness and craving in patients on a detoxification unit. Journal of Music Therapy 2011;48(4):509-31. [DOI: 10.1093/jmt/48.4.509] [DOI] [PubMed] [Google Scholar]
Silverman 2012 {published data only}
- Silverman MJ.Effects of group songwriting on motivation and readiness for treatment on patients in detoxification: a randomized wait-list effectiveness study. Journal of Music Therapy 2012;49(4):414-29. [DOI: 10.1093/jmt/49.4.414] [DOI] [PubMed] [Google Scholar]
Silverman 2014 {published data only}
- Silverman MJ.Effects of music therapy on drug avoidance self-efficacy in patients on a detoxification unit: a three-group randomized effectiveness study. Journal of Addictions Nursing 2014;25(4):172-81. [DOI: 10.1097/JAN.0000000000000047] [DOI] [PubMed] [Google Scholar]
Silverman 2015a {published data only}
- Silverman MJ.Effects of educational music therapy on knowledge of triggers and coping skills, motivation, and treatment eagerness in patients on a detoxification unit: a three-group cluster-randomized effectiveness study. Korean Journal of Music Therapy 2015;17(2):81-101. [DOI: 10.21330/kjmt.2015.17.2.81] [DOI] [Google Scholar]
Silverman 2015b {published data only}
- Silverman MJ.Effects of lyric analysis interventions on treatment motivation in patients on a detoxification unit: a randomized effectiveness study. Journal of Music Therapy 2015;52(1):117-34. [DOI: 10.1093/jmt/thu057] [DOI] [PubMed] [Google Scholar]
Silverman 2016a {published data only}
- Silverman MJ.Effects of live and educational music therapy on working alliance and trust with patients on detoxification unit: a four-group cluster-randomized trial. Substance Use & Misuse 2016;51(13):1741-50. [DOI: 10.1080/10826084.2016.1197263] [DOI] [PubMed] [Google Scholar]
Silverman 2016b {published data only}
- Silverman MJ.Effects of a single lyric analysis intervention on withdrawal and craving with inpatients on a detoxification unit: a cluster-randomized effectiveness study. Substance Use & Misuse 2016;51(2):241-9. [DOI: 10.3109/10826084.2015.1092990] [DOI] [PubMed] [Google Scholar]
Silverman 2017 {published data only}
- Silverman MJ.Effects of group-based educational songwriting on craving in patients on a detoxification unit: a cluster-randomized effectiveness study. Psychology of Music 2017;Advance online publication:1-14. [DOI: 10.1177/0305735617743103] [DOI] [Google Scholar]
- Silverman MJ.Effects of group-based educational songwriting on craving in patients on a detoxification unit: a cluster-randomized effectiveness study. Psychology of Music 2019;47(2):241-54. [DOI: 10.1177/0305735617743103] [DOI] [Google Scholar]
Silverman 2019a {published data only}
- Silverman MJ.Quantitative comparison of group-based music therapy experiences in adults with substance use disorder on a detoxification unit: a three-group cluster-randomized study. Arts & Health 2019;Advance online publication:1-14. [DOI: 10.1080/17533015.2019.1608568] [DOI] [PubMed] [Google Scholar]
- Silverman MJ.Quantitative comparison of group-based music therapy experiences in adults with substance use disorder on a detoxification unit: a three-group cluster-randomized study. Arts & Health 2021;13(1):49-62. [DOI: 10.1080/17533015.2019.1608568] [DOI] [PubMed] [Google Scholar]
Silverman 2019b {published data only}
- Silverman MJ.Songwriting to target state shame, guilt, and pride in adults with substance use disorder on a detoxification unit: a cluster-randomized study. Substance Use & Misuse 2019;54(8):1345-54. [DOI: 10.1080/10826084.2019.1580742] [DOI] [PubMed] [Google Scholar]
Silverman 2020 {published data only}
- Silverman MJ.Therapeutic songwriting for perceived stigma and perceived social support in adults with substance use disorder: a cluster-randomized effectiveness study. Substance Use & Misuse 2020;55(5):763-71. [DOI: 10.1080/10826084.2019.1701037] [DOI] [PubMed] [Google Scholar]
Silverman 2021 {published data only}
- Silverman MJ.A randomized study of lyric analysis on recognition, taking steps, and commitment to sobriety in adults on a detoxification unit. Journal of Substance Use 2021;Advance online publication:1-7. [DOI: 10.1080/14659891.2021.1879292] [DOI] [Google Scholar]
Wu 2020 {published data only}
- Wu Q, Chen T, Wang Z, Chen S, Zhang J, Bao J, et al.Effectiveness of music therapy on improving treatment motivation and emotion in female patients with methamphetamine use disorder: a randomized controlled trial. Substance Abuse 2020;41(4):493-500. [DOI: 10.1080/08897077.2019.1675117] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Baker 2007 {published data only}
- Baker FA, Gleadhill LM, Dingle GA.Music therapy and emotional exploration: exposing substance abuse clients to the experiences of non-drug-induced emotions. The Arts in Psychotherapy 2007;34(4):321-30. [DOI: ] [Google Scholar]
Bibb 2018 {published data only}
- Bibb J, Castle D, Bonomo Y, McFerran KS.Reducing anxiety through music therapy at a community residential alcohol and drug withdrawal unit. Journal of Addictive Behaviors, Therapy & Rehabilitation 2018;7:2. [Google Scholar]
Chandrasekar 2020 {unpublished data only}
- Chandrasekar S.Music vs relaxation training in craving reduction in alcohol dependence syndrome. clinicaltrials.gov/show/NCT04351217 (first received 17 April 2020). [CLINICALTRIALS.GOV: clinicaltrials.gov/ct2/show/NCT04351217]
Dingle 2008 {published data only}
- Dingle GA, Gleadhill L, Baker FA.Can music therapy engage patients in group cognitive behaviour therapy for substance abuse treatment? Drug and Alcohol Review 2008;27(2):190-6. [DOI: ] [DOI] [PubMed] [Google Scholar]
Gallant 1997 {published data only}
- Gallant W, Holosko M, Gorey KM, Lesiuk TL.Music as a form of intervention with out-patient alcoholic couples: a quasi-experimental investigation. Canadian Journal of Music Therapy 1997;5(1):67-84. [Google Scholar]
Gardstrom 2013 {published data only}
- Gardstrom SC, Bartkowski J, Willenbrink J, Diestelkamp WS.The impact of group music therapy on negative affect of people with co-occurring substance use disorders and mental illnesses. Music Therapy Perspectives 2013;31(2):116-26. [Google Scholar]
Haddock 2003 {published data only}
- Haddock G, Barrowclough C, Tarrier N, Moring J, O'Brien R, Schofield N, et al.Cognitive-behavioural therapy and motivational intervention for schizophrenia and substance misuse. 18-month outcomes of a randomised controlled trial. British Journal of Psychiatry 2003;183:418-26. [DOI] [PubMed] [Google Scholar]
Hammer 1996 {published data only}
- Hammer SE.The effects of guided imagery through music on state and trait anxiety. Journal of Music Therapy 1996;33(1):47-70. [DOI: ] [Google Scholar]
Howard 1997 {published data only}
- Howard AA.The effects of music and poetry therapy on the treatment of women and adolescents with chemical addictions. Journal of Poetry Therapy 1997;11(2):81-102. [Google Scholar]
Jones 2005 {published data only}
- Jones JD.A comparison of songwriting and lyric analysis techniques to evoke emotional change in a single session with people who are chemically dependent. Journal of Music Therapy 2005;42(2):94-110. [DOI: ] [DOI] [PubMed] [Google Scholar]
Lu 2005 {unpublished data only}
- Lu S-F.Test a music therapy programme's effectiveness on anxiety and depression in alcoholics. 16th International Nursing Research Congress 2005; Jul 14–16 2005; Hawaii.
Malcolm 2002 {published data only}
- Malcolm BP.Evaluating the effect of drug treatment on coping resources among homeless men. Dissertation Abstracts International Section A: Humanities and Social Sciences 2002;62(12-A):4333. [Google Scholar]
Mathis 2017 {published data only}
- Mathis WS, Han X.The acute effect of pleasurable music on craving for alcohol: a pilot crossover study. Journal of Psychiatric Research 2017;90:143-7. [DOI: 10.1016/j.jpsychires.2017.04.008] [DOI] [PubMed] [Google Scholar]
Moe 2011 {published data only}
- Moe T.Group guided imagery and music therapy for inpatients with substance abuse disorder. Journal of the Association for Music & Imagery 2011;13:77-98. [Google Scholar]
Murphy 2015 {published data only}
- Murphy KM.Music therapy in addictions treatment. In: Wheeler BL, editors(s). Music Therapy Handbook. New York (NY): Guilford Press, 2015:354-66. [Google Scholar]
Oklan 2014 {published data only}
- Oklan AM, Henderson SJ.Treating inhalant abuse in adolescence: a recorded music expressive arts intervention. Psychomusicology: Music, Mind, and Brain 2014;24(3):231. [Google Scholar]
Sewak 2018 {published data only}
- Sewak R, Spielholz NI.Relapse prevention: using sound to reduce the probability of recidivism and suffering following detoxification. Medical Hypotheses 2018;118:84-91. [DOI: 10.1016/j.mehy.2018.06.023] [DOI] [PubMed] [Google Scholar]
Silverman 2016c {published data only}
- Silverman MJ.Effects of educational music therapy on illness management knowledge and mood state in acute psychiatric inpatients: a randomized three group effectiveness study. Nordic Journal of Music Therapy 2016;25(1):57-75. [DOI: 10.1080/08098131.2015.1008559] [DOI] [Google Scholar]
Stamou 2016 {published data only}
- Stamou V, Chatzoudi T, Stamou L, Romo L, Graziani P.Music-assisted systematic desensitization for the reduction of craving in response to drug-conditioned cues: a pilot study. Arts in Psychotherapy 2016;51:36-45. [DOI: 10.1016/j.aip.2016.08.003] [DOI] [Google Scholar]
Stamou 2017 {published data only}
- Stamou V, Clerveaux R, Stamou L, Le Rocheleuil S, Berejnoi L, Romo L, et al.The therapeutic contribution of music in music-assisted systematic desensitization for substance addiction treatment: a pilot study. Arts in Psychotherapy 2017;56:30-44. [DOI: ] [Google Scholar]
Taylor 2005 {published data only}
- Taylor JY, Eliason MJ.Narrative art and music intervention with incarcerated abused women. Communicating Nursing Research 2005;38:453. [Google Scholar]
Wheeler 1985 {published data only}
- Wheeler BL.The relationship between musical and activity elements of music therapy sessions and client responses: an exploratory study. Music Therapy 1985;5(1):52-60. [DOI: ] [Google Scholar]
Additional references
Aalbers 2017
- Aalbers S, Fusar-Poli L, Freeman RE, Spreen M, Ket JC, Vink AC, et al.Music therapy for depression. Cochrane Database of Systematic Reviews 2017, Issue 11. Art. No: CD004517. [DOI: 10.1002/14651858.CD004517.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Albornoz 2011
- Albornoz Y.The effects of group improvisational music therapy on depression in adolescents and adults with substance abuse: a randomized controlled trial. Nordic Journal of Music Therapy 2011;20(3):208-24. [Google Scholar]
Aldridge 2010
- Aldridge D, Fachner J, editor(s).Music Therapy and Addictions. London (UK): Jessica Kingsley Publishers, 2010. [Google Scholar]
Amato 2011a
- Amato L, Minozzi S, Davoli M, Vecchi S.Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database of Systematic Reviews 2011, Issue 10. Art. No: CD004147. [DOI: 10.1002/14651858.CD004147.pub4] [DOI] [PubMed] [Google Scholar]
Amato 2011b
- Amato L, Minozzi S, Davoli M, Vecchi S.Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD005031. [DOI: 10.1002/14651858.CD005031.pub4] [DOI] [PubMed] [Google Scholar]
APA 1980
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 3rd edition. Washington (DC): American Psychiatric Association, 1980. [Google Scholar]
APA 2000
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 4th, text revision edition. Washington (DC): American Psychiatric Association, 2000. [Google Scholar]
APA 2013
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Washington (DC): American Psychiatric Association, 2013. [Google Scholar]
Arbour 2011
- Arbour S, Hambley J, Ho V.Predictors and outcome of aftercare participation of alcohol and drug users completing residential treatment. Substance Use & Misuse 2011;46(10):1275-87. [DOI] [PubMed] [Google Scholar]
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al, GRADE Working Group.Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Babor 1992
- Babor TF, la Fuente JR, Saunders J, Grant M.AUDIT. The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Health Care. Geneva (Switzerland): World Health Organization, 1992. [Google Scholar]
Baker 2007
- Baker FA, Gleadhill LM, Dingle GA.Music therapy and emotional exploration: exposing substance abuse clients to the experiences of non-drug induced emotions. Arts in Psychotherapy 2007;34(4):321-30. [DOI: 10.1016/j.aip.2007.04.005] [DOI] [Google Scholar]
Beck 1996
- Beck AT, Steer RA, Brown GK.Manual for the Beck Depression Inventory – II. San Antonio (TX): Psychological Corporation, 1996. [Google Scholar]
Berman 2005
- Berman AH, Bergman H, Palmstierna T, Schlyter F.Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. European Addiction Research 2005;11(1):22-31. [DOI] [PubMed] [Google Scholar]
Blood 2001
- Blood AJ , Zatorre RJ.Intensely pleasurable responses to music correlate with activity in the brain regions implicated in reward and emotion. Proceedings of the National Academy of Sciences of the United States of America 2001;98(20):11818-23. [DOI: 10.1073/pnas.191355898] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blum 2010
- Blum K, Chen TJ, Chen AL, Madigan M, Downs BW, Waite RL, et al.Do dopaminergic gene polymorphisms affect mesolimbic reward activation of music listening response? Therapeutic impact on Reward Deficiency Syndrome (RDS). Medical Hypotheses 2010;74(3):513-20. [DOI] [PubMed] [Google Scholar]
Blum 2017
- Blum K, Simpatico T, Febo M, Rodriquez C, Dushaj K, Li M, et al.Hypothesizing music intervention enhances brain functional connectivity involving dopaminergic recruitment: common neuro-correlates to abusable drugs. Molecular Neurobiology 2017;54(5):3753-8. [DOI: 10.1007/s12035-016-9934-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruscia 1998
- Bruscia KE.Defining Music Therapy. 2nd edition. Gilsum (NH): Barcelona Publishers, 1998. [Google Scholar]
Bruscia 2014
- Bruscia K.Defining Music Therapy. 3rd edition. University Park (IL): Barcelona Publishers, 2014. [Google Scholar]
Bunt 2014
- Bunt L, Stige B.Music Therapy: an Art Beyond Words. 2nd edition. London (UK): Routledge, 2014. [Google Scholar]
Carter 2020
- Carter TE, Panisch LS.A systematic review of music therapy for psychosocial outcomes of substance use clients. International Journal of Mental Health and Addiction 2020;2020:1-18. [DOI: 10.1007/s11469-020-00246-8] [DOI] [Google Scholar]
Cather 2005
- Cather C.Functional cognitive-behavioural therapy: a brief, individual treatment for functional impairments resulting from psychotic symptoms in schizophrenia. Canadian Journal of Psychiatry 2005;50:258-63. [DOI] [PubMed] [Google Scholar]
Chen 2018
- Chen XJ, Wang CG, Liu W, Gorowska M, Wang DM, Li YH.Identification of the features of emotional dysfunction in female individuals with methamphetamine use disorder measured by musical stimuli modulated startle reflex. Frontiers in Human Neuroscience 2018;12:230. [DOI: 10.3389/fnhum.2018.00230] [DOI] [PMC free article] [PubMed] [Google Scholar]
Choi 2015
- Choi S, Adams SM, Morse SA, MacMaster S.Gender differences in treatment retention among individuals with co-occurring substance abuse and mental health disorders. Substance Use & Misuse 2015;50(5):653-63. [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence.Version accessed 26 August 2020. Melbourne, Australia: Veritas Health Innovation, 2020. Available at covidence.org.
DeLeon 1993
- DeLeon G.Circumstances, motivation, and readiness scales for substance abuse treatment. New York (NY): DeLeon G, 1993. [Google Scholar]
Dijkstra 2010
- Dijkstra IT, Hakvoort LG.'How to deal with music'? Music therapy with clients suffering from addiction problems: enhancing coping strategies. In: Aldridge D, Fachner J, editors(s). Music Therapy and Addictions. London (UK): Jessica Kingsley Publishers, 2010:88-102. [Google Scholar]
Fachner 2017
- Fachner J.Retraining of drug reward, music cues and state-dependent recall in music therapy. Music & Medicine 2017;9(1):8-14. [Google Scholar]
Franken 2002
- Franken IH, Hendriksa VM, den Brink W.Initial validation of two opiate craving questionnaires: the obsessive compulsive drug use scale and the desires for drug questionnaire. Addictive Behaviors 2002;27(5):675-85. [DOI: 10.1016/s0306-4603(01)00201-5] [DOI] [PubMed] [Google Scholar]
Geretsegger 2017
- Geretsegger M, Mössler KA, Bieleninik Ł, Chen XJ, Heldal TO, Gold C.Music therapy for people with schizophrenia and schizophrenia-like disorders. Cochrane Database of Systematic Reviews 2017, Issue 5. Art. No: CD004025. [DOI: 10.1002/14651858.CD004025.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ghetti 2004
- Ghetti CM.Incorporating music therapy into the harm reduction approach to managing substance use problems. Music Therapy Perspectives 2004;22(2):84-90. [Google Scholar]
Ghetti 2013
- Ghetti CM.Effect of music therapy with emotional-approach coping on preprocedural anxiety in cardiac catheterization: a randomized controlled trial. Journal of Music Therapy 2013;50(2):93-122. [DOI] [PubMed] [Google Scholar]
Gilman 2008
- Gilman JM, Hommer DW.Modulation of brain response to emotional images by alcohol cues in alcohol-dependent patients. Addiction Biology 2008;13(3-4):423-34. [DOI: 10.1111/j.1369-1600.2008.00111.x] [DOI] [PubMed] [Google Scholar]
Gold 2009
- Gold C, Solli HP, Krüger V, Lie SA.Dose–response relationship in music therapy for people with serious mental disorders: systematic review and meta-analysis. Clinical Psychology Review 2009;29:193-207. [DOI: 10.1016/j.cpr.2009.01.001] [DOI] [PubMed] [Google Scholar]
Gossop 1995
- Gossop M, Darke S, Griffiths P, Hando J, Powis B, Hall W, et al.The Severity of Dependence Scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction 1995;90(5):607-14. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT.Version accessed 26 August 2020. Hamilton (ON): McMaster University (developed by Evidence Prime), 2020. Available at gradepro.org.
Guyatt 2008
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al.GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336(7560):924. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al.GRADE guidelines 1. Introduction – GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383-94. [DOI] [PubMed] [Google Scholar]
Hakvoort 2020
- Hakvoort L, Jong S, de Ree M, Kok T, Macfarlane C, Haan H.Music therapy to regulate arousal and attention in patients with substance use disorder and posttraumatic stress disorder: a feasibility study. Journal of Music Therapy 2020;57(3):353-78. [DOI: 10.1093/jmt/thaa007] [DOI] [PubMed] [Google Scholar]
Hamilton 1960
- Hamilton M.A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry 1960;23(1):56-62. [DOI: 10.1136/jnnp.23.1.56] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heather 1999
- Heather N, Luce A, Peck D, Dunbar B, James I.The development of a treatment version of the Readiness to Change Questionnaire. Addiction Research 1999;7:63-8. [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s).Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Hohmann 2017
- Hohmann L, Bradt J, Stegemann T, Koelsch S.Effects of music therapy and music-based interventions in the treatment of substance use disorders: a systematic review. PLoS One 2017;12(11):e0187363. [DOI: 10.1371/journal.pone.0187363] [DOI] [PMC free article] [PubMed] [Google Scholar]
Holleck 2019
- Holleck JL, Merchant N, Gunderson CG.Symptom-triggered therapy for alcohol withdrawal syndrome: a systematic review and meta-analysis of randomized controlled trials. Journal of General Internal Medicine 2019;34(6):1018-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Horesh 2010
- Horesh T.Drug addicts and their music: a story of a complex relationship. In: Aldridge D, Fachner J, editors(s). Music Therapy and Addictions. London (UK): Jessica Kingsley Publishers, 2010:57-74. [Google Scholar]
INCB 2019
- International Narcotics Control Board.Report of the International Narcotics Control Board for 2019. www.incb.org/documents/Publications/AnnualReports/AR2019/Annual_Report_Chapters/AR2019_Chapter_III.pdf (accessed 6 June 2021).
Jaffe 2012
- Jaffe A, Du J, Huang D, Hser Y-I.Drug-abusing offenders with comorbid mental disorders: problem severity, treatment participation, and recidivism. Journal of Substance Abuse Treatment 2012;43(2):244-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Juslin 2013
- Juslin PN.From everyday emotions to aesthetic emotions: towards a unified theory of musical emotions. Physics of Life Reviews 2013;10(3):235-66. [DOI: 10.1016/j.plrev.2013.05.008] [DOI] [PubMed] [Google Scholar]
Juslin 2019
- Juslin PN.Musical Emotions Explained. Oxford (UK): Oxford University Press, 2019. [Google Scholar]
Kelly 2014
- Kelly JF, Greene MC.Beyond motivation: initial validation of the commitment to recovery scale. Journal of Substance Abuse Treatment 2014;46(2):257-63. [DOI: 10.1016/j.sat.2013.06.010] [DOI] [PMC free article] [PubMed] [Google Scholar]
Klimas 2018
- Klimas J, Fairgrieve C, Tobin H, Field C-A, O'Gorman CS, Glynn LG, et al.Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database of Systematic Reviews 2018, Issue 12. Art. No: CD009269. [DOI: 10.1002/14651858.CD009269.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Koelsch 2014
- Koelsch S.Brain correlates of music-evoked emotions. Nature Reviews. Neuroscience 2014;15(3):170-80. [DOI] [PubMed] [Google Scholar]
Koelsch 2015
- Koelsch S.Music-evoked emotions: principles, brain correlates, and implications for therapy. Annals of the New York Academy of Sciences 2015;1337:193-201. [DOI] [PubMed] [Google Scholar]
Koob 2013
- Koob GF.Addiction is a reward deficit and stress surfeit disorder. Frontiers in Psychiatry 2013;4:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
London 2004
- London ED, Simon SL, Berman SM, Mandelkern MA, Lichtman AM, Bramen J, et al.Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Archives of General Psychiatry 2004;61(1):73-84. [DOI: 10.1001/archpsyc.61.1.73] [DOI] [PubMed] [Google Scholar]
Longshore 2006
- Longshore D, Teruya C.Treatment motivation in drug users: a theory-based analysis. Drug and Alcohol Dependence 2006;81(2):179-88. [DOI] [PubMed] [Google Scholar]
MacLeod 1991
- MacLeod CM.Half a century of research on the Stroop effect: an integrative review. Psychological Bulletin 1991;109(2):163-203. [DOI] [PubMed] [Google Scholar]
Mays 2008
- Mays KL, Clark DL, Gordon AJ.Treating addiction with tunes: a systematic review of music therapy for the treatment of patients with addictions. Substance Abuse 2008;29(4):51-9. [DOI] [PubMed] [Google Scholar]
McConnaughy 1983
- McConnaughy EA, Prochaska JO, Velicer WF.Stages of change in psychotherapy: measurement and sample profiles. Psychotherapy: Theory, Research and Practice 1983;20(3):368-75. [Google Scholar]
McFerran 2016
- McFerran KS.Contextualising the relationship between music, emotions and the well-being of young people: a critical interpretive synthesis. Musicae Scientiae 2016;20(1):103-21. [Google Scholar]
McLellan 1992
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al.The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 1992;9(3):199-213. [DOI: 10.1016/0740-5472(92)90062-s] [DOI] [PubMed] [Google Scholar]
Megranahan 2018
- Megranahan K, Lynskey MT.Do creative arts therapies reduce substance misuse? A systematic review. Arts in Psychotherapy 2018;57:50-8. [DOI: 10.1016/j.aip.2017.10.005] [DOI] [Google Scholar]
Miller 1996
- Miller WR, Tonigan JS.Assessing drinker's motivation for change: the Stages Of Change Readiness And Treatment Eagerness Scale (SOCRATES). Psychology of Addictive Behaviors 1996;10:81-9. [Google Scholar]
Miller 2002
- Miller WR, Rollnick S.Motivational Interviewing: Preparing People for Change. 2nd edition. New York (NY): Guilford Press, 2002. [Google Scholar]
Minozzi 2016
- Minozzi S, Saulle R, Crescenzo F, Amato L.Psychosocial interventions for psychostimulant misuse. Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No: CD011866. [DOI: 10.1002/14651858.CD011866.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moos 2007
- Moos RH, Moos BS.Treated and untreated alcohol-use disorders: course and predictors of remission and relapse. Evaluation Review 2007;31(6):564-84. [DOI] [PubMed] [Google Scholar]
Neugebauer 2004
- Neugebauer V, Li W, Bird GC, Han JS.The amygdala and persistent pain. Neuroscientist 2004;10(3):221-34. [DOI] [PubMed] [Google Scholar]
NIAA 2003
- National Institute on Alcohol Abuse and Alcoholism.The Drinker Inventory of Consequences (DrInC). pubs.niaaa.nih.gov/publications/projectmatch/match04.pdf (accessed prior to 8 May 2022).
NIDA 2018
- National Institute on Drug Abuse.Principles of Drug Addiction Treatment: a Research-based Guide. 3rd edition. Bethesda (MD): National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services, 2018. [Google Scholar]
NVvMT 2017
- Nederlandse Vereniging voor Muziektherapie (NVvMT) [The Dutch Association for Music Therapy].Beroepscompetentieprofiel muziektherapeut [Professional competence profile – music therapist]. Utrecht (the Netherlands): NVvMT, 2017. [Google Scholar]
O'Daly 2012
- O'Daly OG, Trick L, Scaife J, Marshall J, Ball D, Phillips ML, et al.Withdrawal-associated increases and decreases in functional neural connectivity associated with altered emotional regulation in alcoholism. Neuropsychopharmacology 2012;37(10):2267-76. [DOI: 10.1038/npp.2012.77] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ouimette 2005
- Ouimette P, Read J, Brown PJ.Consistency of retrospective reports of DMS-IV Criterion A traumatic stressors among substance use disorder patients. Journal of Traumatic Stress 2005;18(1):43-51. [DOI: 10.1002/jts.20009] [DOI] [PubMed] [Google Scholar]
Prochaska 1983
- Prochaska JO, DiClemente CC.Stages and processes of self-change of smoking: toward an integrative model of change. Journal of Consulting and Clinical Psychology 1983;51(3):390-5. [DOI: 10.1037/0022-006X.51.3.390] [DOI] [PubMed] [Google Scholar]
Quello 2005
- Quello SB, Brady KT, Sonne SC.Mood disorders and substance use disorder: a complex comorbidity. Science & Practice Perspectives 2005;3(1):13-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2021 [Computer program]
- Review Manager Web (RevMan Web).Version 3.3.0. The Cochrane Collaboration, 2021. Available at revman.cochrane.org.
Rolvsjord 2010
- Rolvsjord R.Resource-Oriented Music Therapy in Mental Health Care. Dallas (TX): Barcelona Publishers, 2010. [Google Scholar]
Ross 2008
- Ross S, Cidambi I, Dermatis H, Weinstein J, Ziedonis D, Roth S, et al.Music therapy: a novel motivational approach for dually diagnosed patients. Journal of Addictive Diseases 2008;27(1):41-53. [DOI: 10.1300/J069v27n01_05] [DOI] [PubMed] [Google Scholar]
Salimpoor 2011
- Salimpoor VN, Benovoy M, Larcher K, Dagher A, Zatorre RJ.Anatomically distinct dopamine release during anticipation and experience of peak emotion to music. Nature Neuroscience 2011;14(2):257-62. [DOI: 10.1038/nn.2726] [DOI] [PubMed] [Google Scholar]
Salloum 2007
- Salloum JB, Ramchandani VA, Bodurka J, Rawlings R, Momenan R, George D, et al.Blunted rostral anterior cingulate response during a simplified decoding task of negative emotional facial expressions in alcoholic patients. Alcoholism: Clinical and Experimental Research 2007;31(9):1490-504. [DOI: 10.1111/j.1530-0277.2007.00447.x] [DOI] [PubMed] [Google Scholar]
SAMHSA 2019
- Substance Abuse and Mental Health Services Administration.Center for Behavioral Health Statistics and Quality. Treatment Episode Data Set (TEDS): 2017. Admissions to and Discharges from Publicly-Funded Substance Use Treatment. Rockville (MD): Substance Abuse and Mental Health Services Administration, 2019. [Google Scholar]
Sena Moore 2013
- Sena Moore K.A systematic review on the neural effects of music on emotion regulation: implications for music therapy practice. Journal of Music Therapy 2013;50(3):198-242. [DOI] [PubMed] [Google Scholar]
Short 2015
- Short AD, Dingle GA.Music as an auditory cue for emotions and cravings in adults with substance use disorders. Psychology of Music 2015;44(3):559-73. [Google Scholar]
Silverman 2003
- Silverman MJ.Music therapy and clients who are chemically dependent: a review of literature and pilot study. Arts in Psychotherapy 2003;30(5):273-81. [Google Scholar]
Silverman 2009
- Silverman MJ.A descriptive analysis of music therapists working with consumers in substance abuse rehabilitation: current clinical practice to guide future research. Arts in Psychotherapy 2009;36(3):123-30. [Google Scholar]
Silverman 2012
- Silverman MJ.Effects of group songwriting on motivation and readiness for treatment on patients in detoxification: a randomized wait-list effectiveness study. Journal of Music Therapy 2012;49(4):414-29. [DOI] [PubMed] [Google Scholar]
Simpson 2008
- Simpson DD.TCU Treatment Assessment Forms. Texas Christian University, Institute of Behavioral Research; Fort Worth (TX).
Singleton 2003
- Singleton EG, Tiffany ST, Henningfield JE.The Alcohol Craving Questionnaire (ACQ-Now). In: Allen JP, Wilson VB, editors(s). Assessing alcohol problems: a guide for clinicians and researchers. 2nd edition. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism, 2003:271-81. [NIH PUBLICATION NO.: 03-3745] [Google Scholar]
Smedslund 2011
- Smedslund G, Berg RC, Hammerstrøm KT, Steiro A, Leiknes KA, Dahl HM, et al.Motivational interviewing for substance abuse. Cochrane Database of Systematic Reviews 2011, Issue 5. Art. No: CD008063. [DOI: 10.1002/14651858.CD008063.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Somoza 1995
- Somoza E, Dyrenforth S, Goldsmith J, Mezinskis J, Cohen M.In search of a universal drug craving scale. Annual Meeting of the American Psychiatric Association; 1995 May 5–25; Miami (FL).
Sullivan 1989
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM.Assessment of alcohol withdrawal: the revised Clinical Institute Withdrawal Assessment for alcohol scale (CIWA-Ar). British Journal of Addiction 1989;84(11):1353-7. [DOI] [PubMed] [Google Scholar]
U.S. Census 2020
- US Census Bureau.Quick Facts. www.census.gov/quickfacts/fact/table/US/PST045221 (accessed prior to 14 April 2022). [RETRIEVED JULY 1 FROM: www.census.gov/quickfacts/fact/table/US/PST045219]
UNODC 2018
- United Nations Office on Drugs and Crime.World drug report 2018 (sales no. E.18.XI.9). www.unodc.org/wdr2018/prelaunch/WDR18_Booklet_1_EXSUM.pdf (accessed 26 August 2020).
UNODC 2020
- UNODC.United Nations On Drugs and Crime. World Drug Report 2020 (Sales no. E.20.XI.9). wdr.unodc.org/wdr2020/en/exsum.html (accessed 6 June 2021).
Urbano 2017
- Urbano FJ, Bisagno V, Garcia-Rill E.Arousal and drug abuse. Behavioural Brain Research 2017;333:276-81. [DOI: 10.1016/j.bbr.2017.07.013] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Alphen 2019
- Alphen R, Stams GJ, Hakvoort L.Musical attention control training for psychotic psychiatric patients: an experimental pilot study in a forensic psychiatric hospital. Frontiers in Neuroscience 2019;13:570. [DOI: 10.3389/fnins.2019.00570] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Dam 2012
- Dam D, Vedel E, Ehring T, Emmelkamp PM.Psychological treatments for concurrent posttraumatic stress disorder and substance use disorder: a systematic review. Clinical Psychology Review 2012;32(3):202-14. [DOI: 10.1016/j.cpr.2012.01.004] [DOI] [PubMed] [Google Scholar]
WHO 1994
- World Health Organization.Lexicon of Alcohol and Drug Terms. Geneva (Switzerland): World Health Organization, 1994. [Google Scholar]
WHO 2018
- World Health Organization.Global Status Report on Alcohol and Health 2018. Geneva (Switzerland): World Health Organization, 2018. [Google Scholar]
WHO 2019
- World Health Organization.International Statistical Classification of Diseases and Related Health Problems (ICD-10). icd.who.int/browse10/2019/en (accessed 26 August 2020).
Wilcox 2016
- Wilcox CE, Pommy JM, Adinoff B.Neural circuitry of impaired emotion regulation in substance use disorders. American Journal of Psychiatry 2016;173(4):344-61. [DOI: 10.1176/appi.ajp.2015.15060710] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2008
- Wu X, Zeng H, Li L, Chen Y.Designing questionnaire on motivation for abstaining from drugs. Chinese Journal of Drug Dependence 2008;17(6):465-8. [Google Scholar]
Zung 1965
- Zung WK.A self-rating depression scale. Archives of General Psychiatry 1965;12:63-70. [DOI] [PubMed] [Google Scholar]
Zung 1971
- Zung WK.A rating instrument for anxiety disorders. Psychosomatics 1971;12(6):371-79. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Ghetti 2020
- Ghetti C, Chen X-J, Brenner AK, Hakvoort LG, Lien L, Fachner J, et al.Music therapy for people with substance use disorders. Cochrane Database of Systematic Reviews 2020, Issue 10. Art. No: CD012576. [DOI: 10.1002/14651858.CD012576.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


