Abstract
Objectives
In the United States, Black individuals have higher stroke incidence and mortality when compared to white individuals and are also at risk of having lower stroke knowledge and awareness. With the need to implement focused interventions to decrease stroke disparities, the objective of this study is to evaluate the feasibility and efficacy of an emergency department-based educational intervention aimed at increasing stroke awareness and preparedness among a disproportionately high-risk group.
Materials and Methods
Over a three-month timeframe, an emergency department-based, prospective educational intervention was implemented for Black patients in an urban, academic emergency department. All participants received stroke education in the forms of a video, written brochure and verbal counseling. Stroke knowledge was assessed pre-intervention, immediately post-intervention, and at one-month post-intervention.
Results
One hundred eighty-five patients were approached for enrollment, of whom 100 participants completed the educational intervention as well as the pre- and immediate post- intervention knowledge assessments. Participants demonstrated increased stroke knowledge from baseline knowledge assessment (5.35 ± 1.97) at both immediate post-intervention (7.66 ± 2.42, p<.0001) and one-month post-intervention assessment (7.21 ± 2.21, p<.0001).
Conclusions
Emergency department-based stroke education can result in improved knowledge among this focused demographic. The emergency department represents a potential site for educational interventions to address disparities in stroke knowledge.
Keywords: stroke education, stroke disparities, health disparities, stroke, emergency department education
INTRODUCTION
Stroke is a leading cause of death and long-term disability in the United States (US).1 Along with many known modifiable risk factors, ethnic and racial differences in risk for stroke have also been identified. Specifically, Black individuals have a higher incidence of stroke when compared to whites and have the highest stroke death rate among racial groups in the US.2 The racial disparity in stroke incidence and mortality is most notable in younger adults. The stroke incidence rate among Black adults age 45–54 is four times higher than that of white adults of the same age.3 Stroke mortality in Blacks is three times that of non-Hispanic whites for patients younger than 65 years.4 While overall stroke mortality is decreasing, the disparity has persisted, with death rates for Black adults declining at a slower rate than whites.5 In order to decrease these stroke disparities, it is important to focus on the factors contributing to higher incidence and mortality in Black communities with focused interventions to address these factors.6
A component of this excess risk among Black adults is attributed to higher prevalence of vascular risk factors including hypertension, diabetes, and obesity.7 However, this is a complex issue that extends beyond patient level characteristics and also involves other factors including disparities in stroke awareness and access to care. Inequities have been described in access to acute stroke treatment and rates of thrombectomy, stroke rehabilitation, and stroke preventative services.8, 9 Multiple studies also describe racial/ethnic disparities in public awareness and recognition of common stroke symptoms.10, 11, 12, 13 For example, Black individuals are less likely to recognize headache, visual symptoms, and difficulty speaking as stroke symptoms.13 Given the time sensitive nature required for stroke intervention and treatment, education campaigns have been developed to improve public awareness of the stroke risk factors, signs/symptoms of stroke, and knowledge of appropriate actions to take when concerned for stroke.14
Previous models of interventions for stroke knowledge disparities have centered around community education and among patients discharged from the hospital setting.15, 16, 17, 18, 19 The Emergency Department (ED) represents a possible site for an education-based intervention to address stroke knowledge that has not yet been adequately explored. For many at-risk patients, the ED may be their only point of contact with the healthcare system, particularly those who use the ED rather than routine primary care visits for management of chronic risk factors. Given the potential impact on high risk patients in this setting, we designed a study to evaluate the effectiveness of an ED-based educational intervention aimed at increasing stroke awareness and preparedness.
METHODS
Study design and setting
This study was a prospective single-arm educational intervention among patients presenting to the ED at an urban academic medical center in the Southeast United States that is both a Level 1 trauma center and comprehensive stroke center. Enrollment was conducted from December 2020 to February 2021. Follow-up took place from January 2021 to April 2021. The study received approval from the University of Alabama at Birmingham Institutional Review Board, and participants provided verbal consent to participate in the study.
Trained study personnel, primarily two medical student research assistants, screened ED patients, enrolled all participants, delivered the educational intervention in a standardized manner, performed follow-up phone interviews, and collected study data.
Selection of participants
Trained study personnel screened patients upon their arrival to the ED while in the ED waiting room using inclusion and exclusion criteria listed below. Given the increased risk for stroke, Black patients triaged with non-life-threatening complaints were approached for participation in the study. Patients presenting with a medical condition limiting their ability to safely participate, including patients with concern for acute stroke, acute myocardial infarction, trauma, acute psychosis, those triaged as high acuity (Emergency Severity Index 1 or 2), and patients with vital sign instability were excluded. Patients were also excluded if they were in police custody, were non-English speaking, or had no phone number to provide for follow-up call. Finally, this study was conducted during the COVID-19 pandemic, so for the safety of both participants and study personnel, patients with symptoms suggesting COVID-19 were excluded.
Participants’ evaluation and medical care were not delayed by these interventions. If any study activities were interrupted by medical care, the patient was approached later in their ED evaluation to complete the necessary activities. Participants who were unable to complete the entire initial encounter including the immediate post-intervention assessment were excluded from the final analysis.
Interventions
Prior to the educational intervention, participants provided contact information for follow-up and basic demographic information. Participants then underwent a baseline knowledge assessment (Appendix 1). The 12-question multiple choice quiz used was adapted with permission from the Emergency Department Patient Education Center Stroke Quiz.20 Each correct answer was worth one point for a total possible score of 12. Four additional self-efficacy questions adapted from previously validated self-efficacy scales were also included in this quiz.21 For the self-efficacy questions, the participants were asked to rate “How confident are you that you can…” on a five-point scale (0=not at all confident, 1=somewhat confident, 2=moderately confident, 3=very confident, 4=completely confident). For example, “How confident are you that you can recognize the signs of stroke in yourself?” Participants were given the option to fill out the assessment themselves or have it read to them by study personnel, and therefore literacy was not a limiting factor for participation. After the baseline assessment, patients participated in a multimodal educational intervention consisting of a two-and-a-half minute stroke educational video developed by the Centers for Disease Control and Prevention (CDC), a stroke patient education handout also developed by the CDC, and a scripted one-on-one counseling session with study personnel.22, 23 The video and handout developed by the CDC is available on their website for no charge, and our reference of and use of this material does not constitute endorsement or recommendation by the U.S. Government, Department of Health and Human Services, or CDC.24 The counseling session aimed to reinforce salient points covered in the video and the educational brochure. The three modes of education provided information on a lay description of stroke, signs/symptoms of stroke, both modifiable and non-modifiable risk factors for stroke, and appropriate action to take when concerned for stroke. The information covered in the quiz was covered in at least one of the three educational modalities. The total duration of the educational intervention was 10–15 minutes.
Outcomes
Immediately following the educational intervention, participants completed an identical post-intervention knowledge assessment. All patients enrolled received the study intervention.
Follow-up consisted of a phone interview approximately one month after initial enrollment during which the participants completed the knowledge assessment for a third time. At least six attempts were made to follow-up all participants including phone calls to alternate numbers and communication via email, when provided.
Data analysis
Data were collected and entered into a coded spreadsheet to ensure confidentiality. Data analysis included descriptive statistics, independent t-tests and ANOVA (i.e., initial 12-point knowledge assessment by sex[male, female], insurance status [private, Medicare/Medicaid, self-pay], education level [some high school/high school, some college/college, other], primary care physician [yes, no]) and paired sample t-tests (i.e., pre/post, post/follow-up, and pre/follow-up 12-point knowledge assessment comparisons). A p-value of <0.05 was considered significant. All statistical analyses were performed using JMP® Pro 14 (SAS Institute Inc., Cary, NC, 1989–2021).
RESULTS
Of the 185 patients who were approached, 103 participants (55.7%) consented and were enrolled in the study. Three participants were not included in the final data analysis because they were unable to complete the post-intervention knowledge assessment. Two of these excluded participants had study participation interrupted by necessary medical care and one participant declined further participation after the initial knowledge assessment. Of the 100 participants eligible for follow-up, 57 participants (57%) completed this follow-up knowledge assessment. This process is summarized in Figure 1.
Figure. 1.
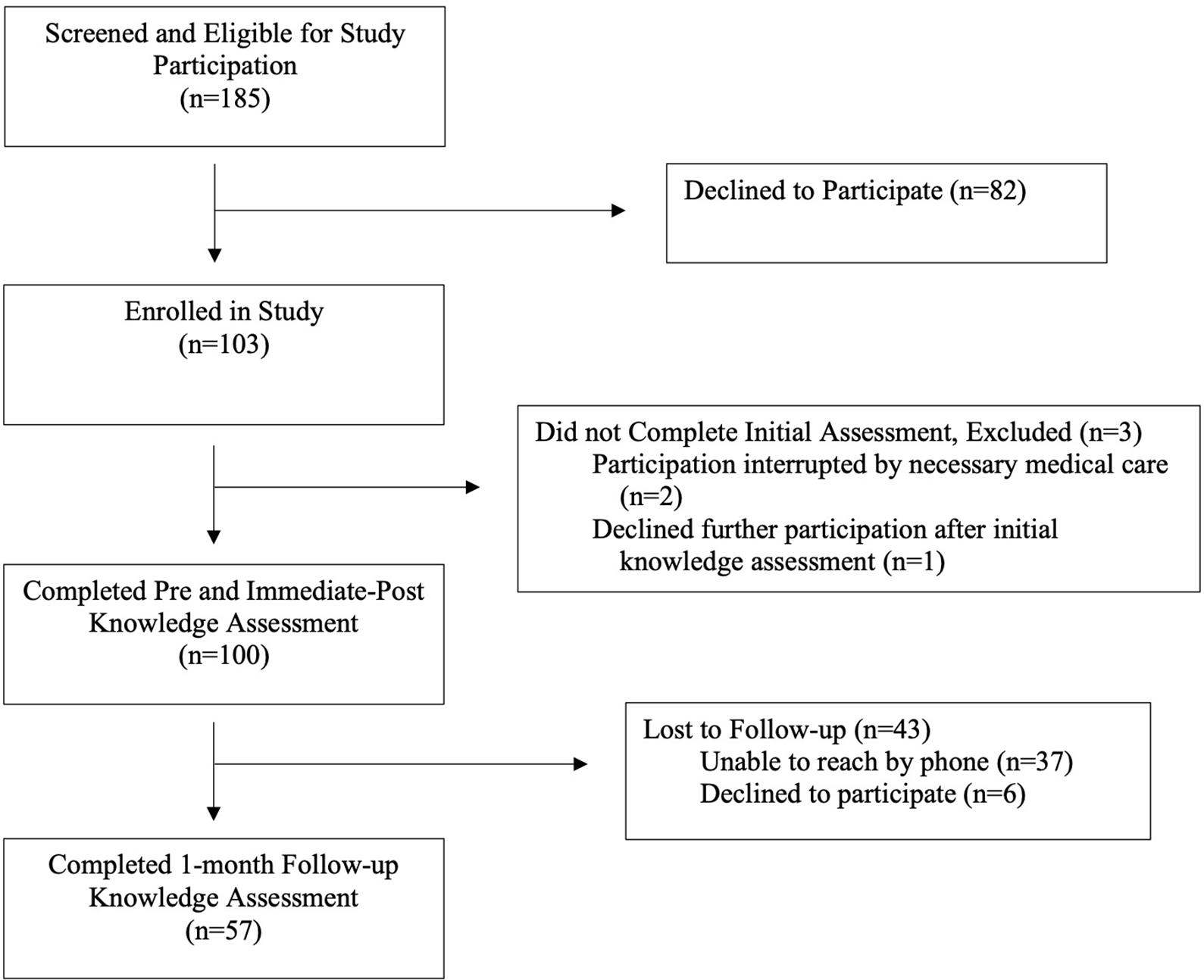
Participant Screening and Enrollment
The participant demographics are summarized in Table 1. The mean age of the participants was 45.6 years (range 19–93 years). The sample consisted of slightly more men (52%) than women. Almost one-third (30%) of the participants were uninsured. Fifty-eight percent of the participants had a high school degree or less. More than three-fourths (86%) of the participants had at least one stroke risk factor; the most common was obesity (46%) followed by current tobacco use (42%) and hypertension (37%), respectively.
Table 1.
Participant Demographics [n(%)]
| Variable | Total (n=100) |
Follow-Up | |
|---|---|---|---|
| Yes (n=57) |
No (n=43) |
||
| Sex * | |||
| Male | 52 (52) | 21 (36.84) | 27 (62.79) |
| Female | 48(48) | 36 (63.16) | 16 (37.21) |
| Age (years) | |||
| Mean ± SD | 45.58 ± 15.61 | 45.21 ± 14.38 | 46.07 ± 17.27 |
| Median, Range | 44, 19–93 | 45, 19–69 | 41, 20–93 |
| Highest Level of Education Completed | |||
| Some High School | 20 (20) | 8 (14.04) | 12 (27.91) |
| High School | 38 (38) | 21 (36. 84) | 17 (39.54) |
| Some College | 23 (23) | 14 (24.56) | 9 (20.93) |
| College | 14 (14) | 11 (19.0) | 3 (6.98) |
| Masters/Professional Degree | 3 (3) | 2 (3.51) | 1 (2.33) |
| Other | 2 (2) | 1 (1.75) | 1 (2.33) |
| Insurance Status | |||
| Self-Pay | 30 (30) | 15 (26.32) | 15 (34.88) |
| Medicaid | 19 (19) | 11 (19.30) | 8 (18.61) |
| Medicare | 25 (25) | 13 (22.81) | 12 (27.91) |
| Private | 26 (26) | 18 (31.58) | 8 (18.61) |
| Medical History | |||
| Hypertension | 37 (37) | 24 (42.11) | 13 (30.23) |
| Diabetes*** | 19 (19) | 15 (26.32) | 4 (9.30) |
| Hyperlipidemia | 20 (20) | 14 (24.56) | 6(13.95) |
| Obesity (BMI ≥ 30) | 46 (46) | 28 (49.12) | 18 (41.86) |
| Atrial Fibrillation | 7 (7) | 6 (10.53) | 1 (2.33) |
| Prior stroke | 5 (5) | 3 (5.26) | 2 (4.65) |
| Prior transient ischemic attack | 5 (5) | 4 (7.02) | 1 (2.33) |
| Smoking-current** | 42 (42) | 18 (31.58) | 24 (55.81) |
| Smoking-former | 20 (20) | 9 (15.79) | 11 (25.58) |
| Number of Stroke Risk Factors | |||
| 0 | 14 (14) | 9 (15.79) | 5(11.63) |
| 1 | 35 (35) | 20 (35.09) | 15 (34.88) |
| 2*** | 27 (27) | 9 (15.79) | 18 (41.86) |
| ≥3* | 24 (24) | 19 (33.33) | 5(11.63) |
| PCP? * | |||
| Yes | 64 (64) | 43 (75.44) | 21 (48.84) |
| No | 36 (36) | 14 (24.56) | 22 (51.16) |
BMI: Body Mass Index, PCP: Primary care physician
p<.01
p=.015
p=.03
Participants’ knowledge assessment scores were significantly higher after the educational intervention (Table 2). Participants scored an average of 19.3 percent higher on the immediate post-intervention assessment when compared to the initial knowledge assessment (t(99)=11.61, p<.0001). Between the immediate post-intervention time point and one-month follow-up, participants’ scores decreased by an average of 7.9 percent (t(56)=−3.85, p=.0003). However, knowledge assessment scores at one-month follow-up remained 12.4 percent higher than scores on the initial assessment (t(56)=5.28, p<.0001). When stratified by age (Table 2), older adults age 65 and older did not have a significant increase their scores on the knowledge assessment after the intervention. While pre-intervention scores among age groups did not significantly differ, younger adults scored significantly higher on the one-month follow-up assessment when compared to those 65 years and older.
Table 2.
Participant Knowledge Assessment Scores
| Knowledge Assessment (12 points possible) | Total (n=100) | Age <35 (n=29) | Age 35–64 (n=60) | Age 65+ (n=11) |
|---|---|---|---|---|
|
| ||||
| Pre- Intervention | 5.35 ± 1.97 | 5.13 ± 2.21 | 5.48 ± 1.96 | 5.18 ± 1.33 |
| Mean ± SD | 5, 1–11 | 4, 1–10 | 5, 1–11 | 5, 3–8 |
| Median, Range | ||||
|
| ||||
| Immediate Post- Intervention | 7.66 ± 2.42* 8, 2–12 |
8.10 ± 2.47*
8, 3–12 |
7.67 ± 2.38*
8, 2–12 |
6.45 ± 2.25 7, 3–10 |
| Mean ± SD | ||||
| Median, Range | ||||
|
| ||||
| One-month Post- Intervention | 7.21 ± 2.21*,† 7, 1–11 |
7.29 ± 2.23* 7.5, 3–10 |
7.36 ± 2.24*,† 8, 1–11 |
5.5 ± 1.29 5.5, 4–7 |
| Mean ± SD | ||||
| Median, Range | ||||
p<.001 compared to Pre- score, paired samples
p<0.005 compared to Immediate Post- score, paired samples
Ordinal information was most commonly forgotten at one-month follow-up. For example, on the initial assessment, 17% of participants chose the correct answer for the question that required participants to rank stroke among the nation’s leading causes of death. This improved to 70% on the immediate post-intervention assessment, but only 21.1% of participants remembered this at one-month follow-up. Alternatively, knowledge about what a stroke is, risk factors for stroke and warning signs of stroke was most commonly gained after the intervention and also retained at one-month follow-up. Furthermore, post-intervention participant knowledge regarding actions to take when concerned for stroke was pronounced. Participants who chose the correct action of calling 9–1-1 if they noticed warning signs of a stroke in themselves or someone else increased from 82 percent to 96 percent immediately after the educational intervention. Those who correctly chose to call for help right away after noticing these signs increased from 85 percent on pre-intervention assessment to 95 percent at one-month follow-up.
Male participants scored significantly lower on the initial knowledge assessment than did female participants (4.92 versus 5.75 respectively, p=.034). Those with Medicare/ Medicaid and those in the self-pay category scored significantly lower than did those with private insurance (5.14 versus 4.97 versus 6.15 respectively, p=.049). Participants with only “some high school education”/ high school degree scored significantly lower than did participants with “some college education”/ college degree (4.83 versus 6.24 respectively, p=.006). Those with no stroke risk factors scored significantly lower on the initial assessment than those with at least one stroke risk factor (4.29 versus 5.52 respectively, p=.029). Finally, participants who reported having no primary care physician (PCP) scored significantly lower than those with a PCP (4.53 versus 5.81 respectively, p=.001).
Participants reported significantly increased confidence in all four self-efficacy statements both immediately and at one-month follow-up. At one-month follow-up, 93 percent of participants indicated they were “very confident” or “completely confident” in both recognizing the signs of stroke in themselves (compared to 31 percent indicating this level of confidence pre-intervention) and also in a family member/friend (compared to 42 percent pre-intervention). Also, at one-month follow-up, 96.5 percent of participants indicated they were “very confident” or “completely confident” regarding calling 9–1-1 if they or someone near them had signs of a possible stroke as well as getting to the hospital immediately after noticing the warning signs of a stroke, compared to 84 percent of participants indicating this level of confidence for both hypothetical actions before the intervention.
Forty-three percent of participants were lost to follow-up (Figure 1), a majority of whom could not be reached by phone. Some participants declined further participation at the time of the follow-up phone call. Those who were lost to follow-up, when compared to those who completed the follow-up assessment, were significantly more likely to be male (62.79 percent versus 36.84 percent, p=.01) and lack a primary care physician (51.16 percent versus 24.56 percent, p=.006) when compared to those who completed the one-month follow-up assessment (Table 1). The participants who did not complete the follow-up assessment were also more likely to have a high school education or less (67.44 percent versus 50.88 percent) and be uninsured (34.88 percent versus 26.32 percent) when compared to those who completed the follow-up, though these trends did not reach statistical significance.
A final sub-group of patients warranting special attention are those who declined participation in the study prior to enrollment. Those declining participation in the study were more likely to be female (62.2 percent) and had a mean age of 40, which is in contrast to the overall study population which was more likely to be male (52 percent) and slightly older (mean age of 45.6). The chief complaint wasn’t collected on all patients who declined participation. However, this information was collected on some of the participants and of these, over two-thirds (69%) were presenting to the ED with a chief complaint of acute pain (n=35).
DISCUSSION
Health disparities are profoundly apparent in EDs throughout the US. The ED is a unique setting in that it is available at any time, and service to both the advantaged and disadvantaged is guaranteed under the law.25 With nearly 140 million people seeking care each year, the ED has been described as “the only site where the most disenfranchised persons can be reached.” 26, 27 Furthermore, many patients with chronic illnesses use the ED rather than routine primary care for both their emergent and non-emergent medical needs.28 As summarized in Table 1, a majority of the participants in our study had at least one stroke risk factor. Of note, this study population consisted of lower acuity patients and therefore likely underestimates the presence of risk factors of the general ED population. Nonetheless, this demonstrates the prevalence of patients with risk factors in this setting. Given the general accessibility of the ED and the reality that the ED may be the only point of contact with the healthcare system for many at-risk patients, the ED is potentially an ideal site for providing education to improve stroke knowledge and awareness. This study demonstrates that an ED-based educational intervention is feasible and effective at promoting short-term retention of high-yield information about stroke awareness among a disproportionately high-risk group.
Prior studies in this setting have yielded encouraging results. Stroke educational interventions performed in the ED, specifically those utilizing multiple methods for education, have been shown to be effective in increasing both immediate and retained stroke knowledge.20, 29, 30 These previous studies enrolled all-comers in the fast-track, low acuity waiting room of an urban ED. 20, 29, 30 The present study employs the ED as a location for providing this education specifically for Black patients as a means to address stroke disparities, particularly disparities in stroke knowledge. We demonstrate that stroke education does improve immediate and short-term knowledge among this demographic. Furthermore, the sustained increase in knowledge of appropriate action to take when concerned for stroke suggests that behavioral intent was positively affected by this intervention. Also, knowledge about stroke risk factors and stroke signs/symptoms was significantly increased by the intervention and retained at follow-up. This is crucial as behavioral intent to promptly seek medical attention when concerned for stroke is only beneficial if one is able to recognize signs/symptoms of stroke in themselves or someone else.
We found less familiar facts about stroke, such as where this disease process ranks among causes of death, to have lower retention at follow-up. While the concept of stroke a leading cause of death is an important principle, the exact ranking of it among causes of death may be less relevant. Future interventions should focus material and evaluation on knowledge that could ultimately improve patient outcome (e.g. recognition of stroke signs/symptoms and appropriate action when these are recognized) in order to improve knowledge retention.
Further analysis revealed factors that may be associated with lower initial stroke knowledge scores. Prior studies have suggested older age and lower level of education as being predictive of lower stroke knowledge. 31 Also, some studies have found lower stroke knowledge among men, though data are conflicting.31 Although our study did not find significant difference in initial knowledge scores among different age groups, older participants did have significantly lower scores when compared to younger adults at one-month follow-up. While this intervention proved effective for education of younger and middle-aged adults, further investigation is needed to develop an appropriate strategy for providing stroke education to older adults. In our study, participants who scored lowest on the initial stroke assessment were male, had a high school education or less, had Medicare/Medicaid or were self-pay, had no stroke risk factors, and did not have a primary care physician. It will be important to consider these factors when planning future focused educational interventions for those at risk for lowest baseline stroke knowledge.
As stated previously, 57 percent of participants completed the one-month follow-up assessment. Further analysis of the participants who didn’t complete the follow-up assessment is also important in planning future interventions. While we can’t determine if the group lost to follow-up would actually differ in level of knowledge retained, this group may represent a higher risk group. Those lost to follow-up were more likely to be male and to lack a primary care physician. There was also a trend, though it did not reach significance, toward lost-to-follow-up participants having a high school education or less and being uninsured. It’s important to note the demographic similarities between participants lost to follow-up and participants with the lowest pre-assessment knowledge scores. Black individuals who are male or lack a primary care physician as well as those without insurance or with only a high school degree or less may be particularly important groups to focus on with future interventions.
When planning ED-based education, it is important to keep in mind that patients typically present with a specific medical issue or concern. It is reasonable to suppose that those presenting with acutely painful conditions may be less willing to participate in an educational intervention. It may initially seem as if this may provide a barrier to implementation of this intervention in this setting. This does not, however, exclude the ED a site for these interventions. Patients typically come with at least one family member or friend who would presumably not have the same level of distraction that the patient may have. Even if a patient is distracted by pain or busy receiving medical evaluation, the patient’s family members or friends present who may also be suitable targets to receive education. Unfortunately, we were not able to include visitors in our study because they were not allowed in the ED during the enrollment period given COVID-19 precautions. ED visitors, however, are an important group to consider with future educational interventions.
LIMITATIONS
Forty-three percent of participants were lost to follow-up at one month, placing the study at risk of attrition bias. Also, the participants in this study were limited to one racial group, this chosen because of the known increased risk for stroke and existing disparities. We are therefore unable to ascertain the generalizability to other high-risk groups. The study was also conducted during the COVID-19 pandemic, which may have influenced the patients coming to the ED, also limiting the generalizability of our findings during non-COVID times. Lastly, although this study measured behavioral intent, actual behavioral change as a result of the intervention was not assessed.
When considering barriers to implementation of this intervention in other ED’s, it is important to consider the personnel requirement. As mentioned above, this study utilized trained study personnel in the intervention portion to deliver the verbal counseling. This component reinforced key material covered in both the video and the brochure. While it is ideal to have this counseling component as a second verbal component to minimize any literacy barriers and to reinforce the material, it is possible to deliver two of the three components of the intervention with minimal personnel requirement.
CONCLUSION
In conclusion, this study indicates that stroke education provided in the ED results in improved knowledge among Black individuals. Given these positive results among this demographic, the ED is a promising site for future educational interventions to address disparities in stroke knowledge.
Supplementary Material
Financial support
Research reported in this manuscript was supported by the National Institute of Neurological Disorders And Stroke of the National Institutes of Health under Award Numbers U01NS086872 and U24NS107223. Content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of interest
EFS reports no conflict of interest.
LAW reports no conflict of interest.
TIG reports no conflict of interest.
TEM reports no conflict of interest.
MRH reports no conflict of interest.
RML reports no conflict of interest.
JB reports no conflict of interest.
CB reports no conflict of interest.
MJL reports no conflict of interest.
Presentations
Preliminary data was presented at NIH StrokeNet Professional Development Webinar-Trainee Presentations on May 11, 2021.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Virani SS, Alonso A, Benjamin EJ, et al. on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics- 2020 update: a report from the American Heart Association. Circulation 2020;141:e1–e458.31887075 [Google Scholar]
- 2.Yang Q, Tong X, Schieb L, et al. Vital Signs: Recent trends in stroke death rates — United States, 2000–2015. MMWR Morb Mortal Wkly Rep 2017;66:933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howard VJ, Kliendorfer DO, Judd SE, et al. Disparities in stroke incidence contributing to disparities in stroke mortality. Ann Neurol 2011;69:619–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howard V Reasons underlying racial differences in stroke incidence and mortality. Stroke 2013;44:S126–S128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howard G Ancel Keys Lecture: Adventures (and misadventures) in understanding (and reducing) disparities in stroke mortality Stroke. 2013;44:3254–3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Howard G, Moy CS, Howard VJ, et al. Where to focus efforts to reduce the black-white disparity in stroke mortality. Stroke 2016;47:1893–1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stroke risk factors not within your control. Stroke.org. https://www.stroke.org/en/about-stroke/stroke-risk-factors/stroke-risk-factors-not-within-your-control. Updated Oct 10, 2018. Accessed Jan 13, 2021.
- 8.Brinjikji W, Rabinstein AA, Cloft HJ. Socioeconomic disparities in the utilization of mechanical thrombectomy for acute ischemic stroke. J Stroke Cerebrovasc Dis 2014; 23(5): 979–984. [DOI] [PubMed] [Google Scholar]
- 9.Cruz-Flores S, Rabinstein A, Biller J, et al. Racial-ethnic disparities in stroke care: The American experience. Stroke 2011;42(7): 2091–2116. [DOI] [PubMed] [Google Scholar]
- 10.Greenlund KJ, Neff LJ, Zheng Z, et al. Low public recognition of major stroke symptoms. Am J Prev Med 2003; 25(4): 315–319. [DOI] [PubMed] [Google Scholar]
- 11.Alkadry MG, Bhandari R, Wilson CS, et al. Racial disparities in stroke awareness: African Americans and caucasians. J Health Hum Serv Adm 2011; 33(4): 462–490. [PubMed] [Google Scholar]
- 12.Ojike N, Ravenell J, Seixas A, et al. Racial disparity in stroke awareness in the US: An analysis of the 2014 National Health Interview Survey. J Neuro Neurophysiol 2016; 7(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharrief AZ, Johnson BJ, Abada S, et al. Stroke knowledge in African Americans: A narrative review. Ethnicity & Disease 2016; 25(2): 255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang J, Keenan NL, Ayala C, et al. Awareness of stroke warning symptoms—13 states and the District of Columbia, 2005. MMWR 2008;57:481–5. [PubMed] [Google Scholar]
- 15.Stern EB, Berman M, Thomas JJ, et al. Community education for stroke awareness: An efficacy study. Stroke 1999; 30(4): 720–723. [DOI] [PubMed] [Google Scholar]
- 16.Kleindorfer D, Miller R, Sailor-Smith S, et al. Challenges of community-based research-The beauty shop stroke education project. Stroke 2008; 39:2331–2335. [DOI] [PubMed] [Google Scholar]
- 17.Boden-Albala B Education strategies for stroke prevention. Stroke 2013;44:S48–S51. [DOI] [PubMed] [Google Scholar]
- 18.Ing MM, Linton KF, Vento MA, et al. Investigation of stroke needs (INVISION) study: Stroke awareness and education. Hawaii J Med Public Health 2015; 74(4): 141–145. [PMC free article] [PubMed] [Google Scholar]
- 19.Denny MC, Vahidy F, Vu KYT, et al. Video-based educational intervention associated with improved stroke literacy, self-efficacy, and patient satisfaction. PLoS One 2017; 12(3): e0171952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan Y, Nagurka R, Richardson LD, et al. Effectiveness of stroke education in the emergency department waiting room. J Stroke Cerebrovasc Dis 2010;19(3):209–215. [DOI] [PubMed] [Google Scholar]
- 21.Fors A, Ulin K, Cliffordson C, et al. The cardiac self-efficacy scale, a useful tool with potential to evaluate person-centered care. European Journal of Cardiovascular Nursing 2015; 14(6): 536–543. [DOI] [PubMed] [Google Scholar]
- 22.Recognize the signs and symptoms of stroke. https://www.youtube.com/watch?v=mkpbbWZvYmw&feature=emb_title. Oct 26, 2015. Accessed Jan 13, 2021. [Google Scholar]
- 23.Know the facts about stroke. cdc.gov. https://www.cdc.gov/stroke/docs/Know_the_Facts_About_Stroke.pdf. Accessed Jan 13, 2021.
- 24. [Updated Dec 12, 2019. Accessed Jan 13, 2021.]. Using CDC.gov-Use of agency materials. cdc.gov. https://www.cdc.gov/other/agencymaterials.html.
- 25.Gordon JA. The hospital emergency department as a social welfare institution. Ann Emerg Med 1999;33:321–325. [DOI] [PubMed] [Google Scholar]
- 26.FastStats-Emergency department visits. cdc.gov. https://www.cdc.gov/nchs/fastats/emergency-department.htm. Updated November 10, 2020. Accessed December 5, 2020.
- 27.Bernstein E, Goldfrank LR, Kellerman AL, et al. A public health approach to emergency medicine: Preparing for the twenty-first century. Acad Emerg Med 1994;1:277–286. [DOI] [PubMed] [Google Scholar]
- 28.Capp R, Kelley L, Ellis P, et al. Reasons for frequent emergency department use by medicaid enrollees: A qualitative study. Acad Emerg Med 2016;23:476–481. [DOI] [PubMed] [Google Scholar]
- 29.Chan Y, Lavery R, Fox N, et al. Effect of an educational video on emergency department patients stroke knowledge. J Emerg Med 2008;34:215–220. [DOI] [PubMed] [Google Scholar]
- 30.Chan YY, Richardson LD, Nagurka R, et al. Stroke education in an emergency department waiting room: A comparison of methods. Health Promot Perspect 2015;5:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nicol MB, Thrift AG. Knowledge of risk factors and warning signs of stroke. Vasc Health Risk Manag 2005;1:137–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


