Abstract
Objectives:
To identify scalable evidence-based suicide prevention strategies.
Methods:
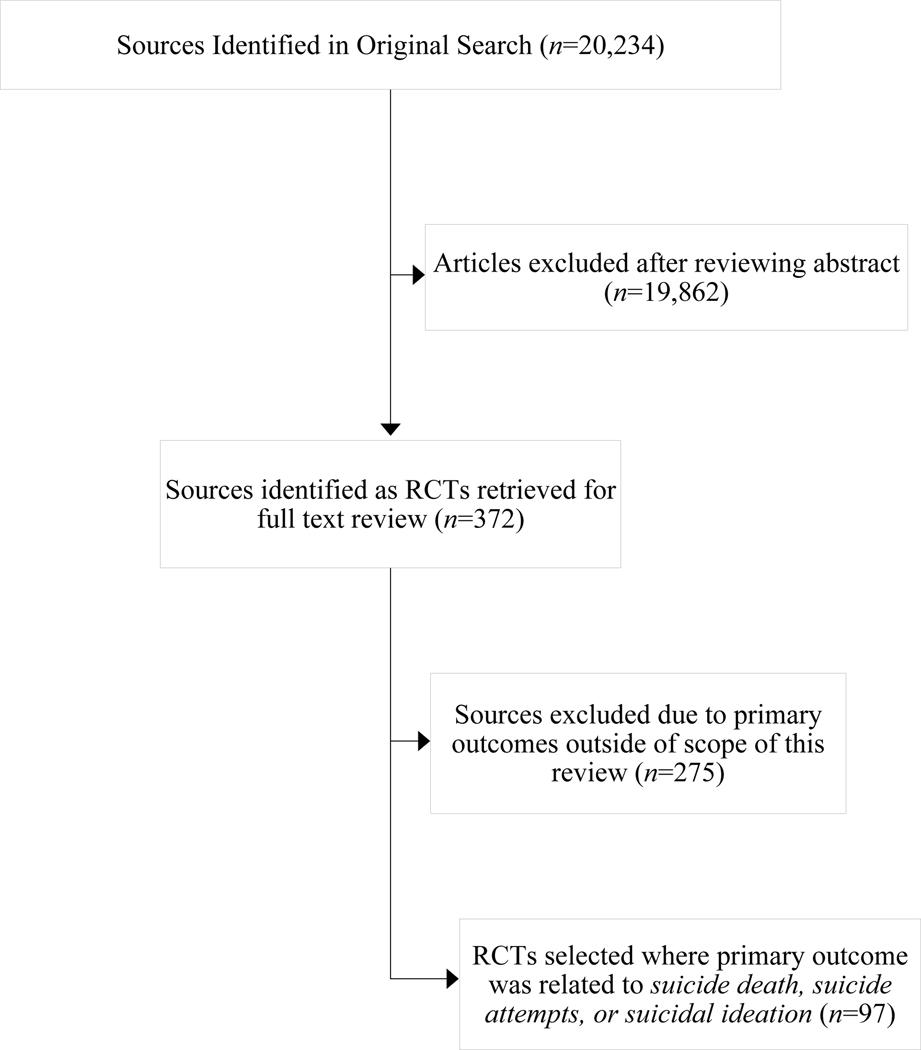
Searching PubMed and Google Scholar between September 2005-December 2019 identified 20,234 articles. These included 97 RCTs with suicidal behavior or ideation as primary outcomes, and epidemiological studies of limiting access to lethal means, educational approaches and antidepressant studies.
Results:
Training primary care physicians in depression recognition and treatment prevents suicide. Educating youth regarding depression and suicidal behavior, and active outreach of psychiatric patients after discharge or a suicidal crisis, prevents suicidal behavior. Meta-analyses find antidepressants prevent suicide attempts, but individual RCTs appear under-powered. Ketamine reduces suicidal ideation in hours but is untested for suicidal behavior prevention. CBT and DBT prevent suicidal behavior. Active screening for suicidal ideation or behavior is not proven to be better than just screening for depression. Education of gatekeepers about youth suicidal behavior lacks effectiveness. No RCTs are reported for gatekeeper training for adult suicidal behavior prevention. Algorithm-driven electronic health records (EHR) screening, internet-based screening and smartphone passive monitoring to identify high-risk patients are under-studied. Means restriction, including firearms, prevents suicide, but is rarely employed in the U.S., even though firearms are used in half of all U.S. suicides.
Conclusions:
Training general practitioners warrants wider implementation and testing in other non-psychiatrist physician settings. RCTs are required to compare effectiveness of education of adult gatekeepers versus educating higher risk adults including most psychiatric patients. Active follow-up of patients after discharge or a suicide-related crisis should be routine and restricting firearm access by at-risk individuals warrants wider-use. Combination approaches in healthcare systems show promise in reducing suicide in U.K., Denmark and U.S., but evaluating benefit attributable to each component is essential. Further suicide rate reduction requires evaluating newer approaches like EHR-derived algorithms, internet-based screening methods, ketamine’s benefit for preventing attempts and passive monitoring of acute suicide risk change.
Introduction
Suicide is the tenth leading cause of death in the U.S. with 48,344 suicide deaths in 2018, and the second leading cause of death in ages 15–34 yrs.(1) Alarmingly, the age-adjusted suicide rate has steadily risen 36.7% from 2000 to 2018 (10.4/100,000 to 14.2/100,00).(2, 3) This situation may be even worse. The 40.7% increase in the unintentional death rate from 2000 to 2017 is almost entirely due to unspecified falls (up 86.5%) and unintentional poisonings (up 98.5%), two causes that include misclassified suicides. The first U.S. national suicide prevention plan was proposed in 2000,(4) but from 2000 to 2012, the U.S. slipped from the 72nd to the 31st percentile worldwide in terms of suicide rate.(5) We will show that U.S. suicide rate increase relative to the rest of the world has happened in the context of under-utilized, proven suicide prevention options.
A critical review of suicide prevention methods is facilitated by an exponential increase in effectiveness data. The most widely cited review of suicide prevention was published in 2005.(6) From 2005 to 2019, over four times as many articles on suicide prevention were published compared with the previous 40 years (1966–2005). Therefore, we review all randomized controlled trials (RCTs) examining suicide, nonfatal suicide attempts and suicidal ideation. Benefits of reducing access to the most lethal methods used for suicide and the impact of prescribing antidepressants were examined using epidemiologic studies, mostly time series studies, some with contemporaneous geographic controls, identified using the same search engines. We focused on suicidal behavior as an outcome and not suicidal ideation, because there is closer a relationship between suicide deaths and nonfatal suicide attempts than there is between suicidal ideation and suicide deaths.(7)
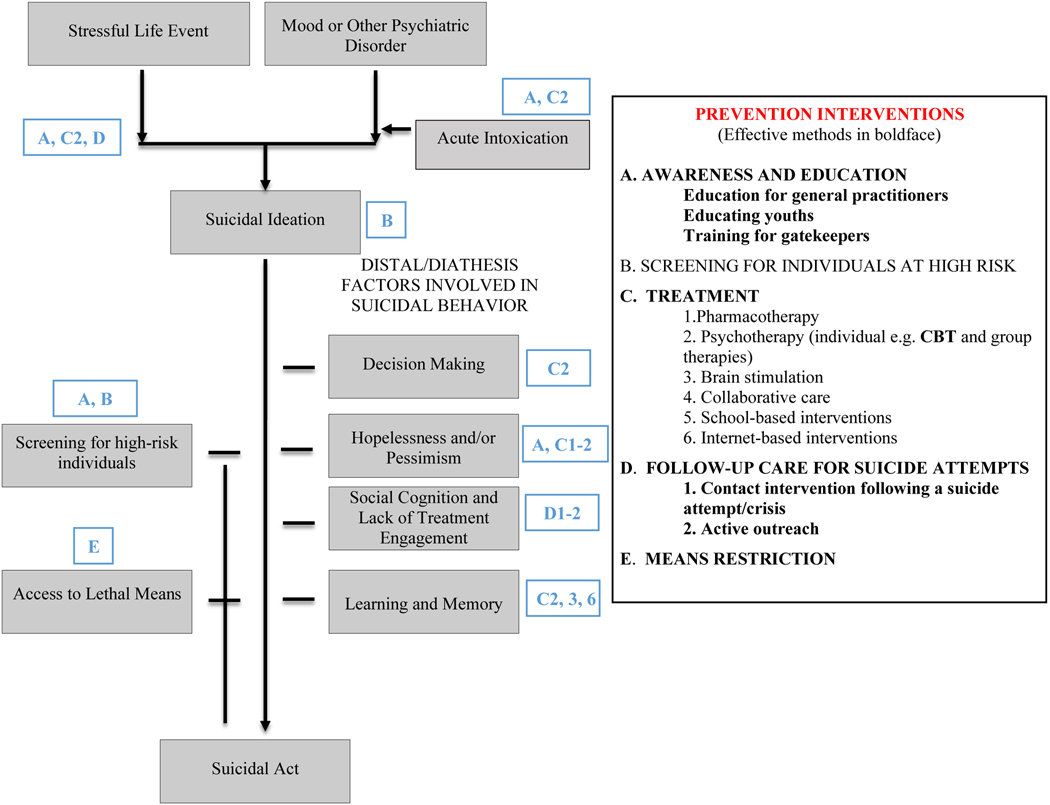
Suicide risk can be understood in terms of a stress diathesis model (8) (Figure 1) where stress results from an internal stressor, usually a psychiatric illness, present in about 90% of all suicides and most commonly major depression, and/or an external stressor involving life events. The diathesis is a combination of heightened perception of emotional distress, a greater propensity to act on emotion, less learning and problem-solving capacity and a hypersensitivity to negative social signals and diminished sensitivity to positive social signals.(8) The diathesis moderates suicide risk, and that risk can be influenced by acute alcohol or drug abuse adversely via mood or disinhibition (Figure 1). Prevention measures can be aligned with these model components (Figure 1). Each method was judged by two criteria: (1) Does it prevent suicide attempts and not just suicidal ideation? and (2) Can it be scaled up to city, county, state and national levels, a requirement for broader suicide prevention?
Figure 1.
Targets and Methods of Suicide Prevention
Method
The search used PubMed and Google Scholar for the period 2005 to 2019, in accordance with PRISMA standards for systematic reviews.(9) Search identifiers were suicide, suicide attempt, suicidal behavior and suicidal ideation combined separately with each of the following identifiers: prevention, control, depression, health education, health promotion, public opinion, mass screening, family physicians, medical education, primary health care, antidepressant medications, mood stabilizers, atypical antipsychotics, psychotherapy, schools, adolescents, methods, firearms, overdose, poisoning, gas poisoning, internet and mass media. The search was restricted to articles in English. RCTs with primary outcomes of interest: completed suicide, attempted suicide or suicidal ideation, were included because RCTs provide strongest evidence of efficacy of a prevention strategy. As evaluation of restricting access to more lethal methods of suicide, use of EMRs for screening algorithms and medication effects on suicide as an outcome, require large population studies due to the low base rate of suicide, we reviewed epidemiological studies emphasizing time-series designs, and studies at the city, county or general practitioner (GP) network level that employed a geographic control or practice control sites. Such studies, together with system level studies, provide an indication of prevention methods that can be scaled up to a national level (10). These studies were identified using the same search terms and engines as were employed for RCTs. From the 20,234 articles identified or their bibliographies, 97 RCTs and 30 epidemiologic studies with suicide, attempted suicide or suicidal ideation as primary outcomes of interest were selected to evaluate prevention strategies (Table 1; Figure 2). Abstracts were reviewed to select studies for inclusion, and methods and results were obtained from the full text. Results are summarized for the main suicide prevention approaches in Table 1 in terms of proportion of positive outcome studies, and where there were replicated positive findings for reducing suicide attempts, we made a judgement as to whether that method is scalable based on complexity in terms of training and delivery as well as cost in terms of time and personnel. This approach is consistent with what others have recommended(10), as it builds from individual RCTs, preferably carried out in different localities or countries, in determining whether a prevention method can potentially be deployed more widely.
Table 1.
Randomized Controlled Trials of Suicidal Behavior Prevention Interventions
| Intervention | Studies (N) | Intervention superior to control | Intervention not superior to control | Scalability (Yes, No**) | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| General Practitioner Education* | 12 | 10 | 83% | 2 | 17% | Yes |
| Education for Youth Suicidal Behavior (Targeting Youth for Training/Education) | 3 | 3 | 100% | 0 | 0% | Yes |
| Education for Youth Suicidal Behavior Prevention (Targeting Adults for Training/Education) | 6 | 1 | 17% | 5 | 83% | Yes |
| Pharmacotherapy | 17 | 4 | 24% | 13 | 76% | Yes |
| Psychotherapy (CBT, DBT) | 18 | 9 | 50% | 9 | 50% | Yes (CBT) |
| Medication and Psychotherapy | 3 | 1 | 33% | 2 | 67% | NA |
| Group Psychotherapy | 2 | 1 | 50% | 1 | 50% | NA |
| Contact and/or Active Outreach | 10 | 7 | 70% | 3 | 30% | Yes |
| Brain Stimulation | 2 | 0 | 0% | 2 | 100% | NA |
| Collaborative Care | 1 | 1 | 100% | 0 | 0% | NA |
| Firearms Restriction*** | 49 | 48 | 98% | 1 | 2% | Yes |
| Internet Based | 3 | 0 | 0% | 3 | 100% | NA |
Note: Studies were only included if suicide attempts, events or self-injury were outcome measures and not solely suicidal ideation.
Contains 2 RTCs and 10 quasi-experimental studies.
Scalability was only assessed when findings of efficacy have been replicated.
Contains quasi-experimental and ecological studies
Figure 2.
Selection of Articles for Review
Results
EDUCATION
We examined education directed at health care professionals, patients or gatekeepers (military, first responders, school staff, clergy, college campus counselors, human resource departments and the general public).
General Practitioner and Non-Psychiatrist Physician Education
Doctors in primary care and other non-psychiatric care settings see 45% of future suicide decedents in the 30 days prior to suicide, and 77% within 12 months of suicide,(11) about double the rate consulting mental health professionals. Therefore, educating non-psychiatrist physicians may prevent far more suicides than further training for psychiatrists. Training primary care doctors and nurses at the local and state level to better screen and treat depression with supplemental help available from psychiatrists, lowered suicide rates,(12–19) nonfatal suicide attempts(20, 21) and ideation(22) (Table 2). These findings support results from earlier studies (23–25) and studies of self-harm.(26) Repeated education sessions reduced suicide rates progressively for years.(12, 21) In contrast, a single day training session produced no benefit for suicide deaths over 3-years.(27) Areas with suicide rates 3–10 times higher than the U.S., have shown that screening for depression combined with referral for depression treatment by a primary care doctor or psychiatrist lowered suicide rates relative to a contemporaneous geographic control.(12, 15–17) Conversely, a study of 40 primary care medical practices in the Netherlands found a drop in depression recognition from 65% to 44% was associated with higher suicide attempt rates in men.(28)
Table 2.
Studies of General Practitioner and Non-Psychiatric Physicians Education
| Source | Prevention Strategy | Length of intervention | Population | Study Type | Location | Outcome |
|---|---|---|---|---|---|---|
| Oyama, 2005(15) | Educational intervention for nurse depression screening and GP management | 8-yrs, screening and depression management | Older adults | Quasi-experimental* | Japan | Greater female suicide reduction in intervention region compared with control region (IRR =.35). No regional difference in male suicides. |
| Oyama, Fujita et. al, 2006(17) | Educational intervention for nurse depression screening and GP management | 10-yrs, screening and depression management | Older adults | Quasi-experimental* | Japan | Greater reduction in intervention region female suicide at a trend level compared with control region (IRR =.23). No regional difference in male suicides. |
| Oyama, Goto et. al, 2006(16) | Educational intervention for nurse depression screening and GP management | 10-yrs, screening and Depression management | Older adults | Quasi-experimental* | Japan | Greater reduction in female suicide rates in intervention region compared with control region (IRR =.43). No regional differences in male suicides. |
| Oyama, Ono et. al, 2006(14) | Educational intervention for nurse depression screening and GP management | 5-yrs, screening and Depression management | Older adults | Quasi-experimental* | Japan | Trend level reduction in female suicide rate in the intervention region (IRR=.26) but not in the control region. No change in male suicide rate. |
| Henriksson & Isacsson, 2006(18) | Yearly 2-day GP training sessions | 8-yrs, GP screening and depression treatment | Adults | Quasi-experimental* | Sweden | Pre-intervention (1970–1994), suicide rate was higher in Jamtland county than Sweden (p<.05), but during intervention period (19952002) it dropped in intervention region, so the two rates no longer differed. |
| Szanto et al., 2007(12) | Annual educational program for GPs and their nurses | 5-yrs, GP supervised depression management | Adults | Quasi-experimental* | Hungary | Decrease in suicide rate in intervention region greater than the larger county (p<.001) and Hungary (p<.001). |
| Alexopoulo s et al., 2009(22) | 2-yrs of GP training and case managers | 2-yrs with algorithm-based tx advice | Older adults | RCT## | United States | Intervention group more likely than to receive antidepressants or psychotherapy (p<.001), and those with major depression had lower rates of SI at 4, 8, and 24 months (p=.04). No difference in SB. |
| Hegerl et al., 2010(21) | 2-Yr, four-level intervention program including GP education | 2-yrs, GP depression management | Adults | Quasi-Experimental* | Germany | Intervention region had greater reduction in suicidal acts (suicides + SA) (p<.0065) and SA (p<.0005) versus control from baseline to 1-year follow-up of the 2-year intervention (2000–2003). The reduction in SA was more pronounced for high-lethality than low-lethality methods and persisted for four years. |
| Hübner-Liebermann et al., 2010(19) | 5-yrs of four-level intervention program including GP education in depression management | 5-yrs, GP depression management | Adults | Quasi-experimental* | Germany | The suicide rate declined in the intervention region (p=.02) but not in the control region. |
| Roškar et al., 2010(27) | One-day GP educational program | 3-yrs of GP depression management | Adults | Quasi-Experimental** | Slovenia | Intervention group had greater increase in antidepressant prescriptions (p<.05) compared with controls but no group differences in suicide rate. |
| Almeida et al., 2012(26) | 2-yrs, GP practice audit with feedback on depression and self-harm, educational materials and control education GP group. | 2-yrs of GP depression management | Older adults | RCT# | Australia | Intervention group had less self-harm behaviors (0R=.80, p<.05) over 2-yrs. |
| Hegerl et al., 2019(20) | 2-yrs, four-level intervention program including GP training, GP consultation hotline | 2-yrs of GP depression treatment | Adults | Quasi-experimental* | Germany, Hungary, Ireland & Portugal | In Portugal, the intervention region saw a greater reduction in suicidal acts (suicides + SA) (p=.05) and SA (p=.02) compared with control region. No group differences found in 3 other countries. |
Studies used a control region as a comparison and examined time periods before and after intervention onset. For such community level intervention studies there were no inclusion or exclusion criteria employed.
Study used physicians who did not attend GP training as control group for two regions and had one region as additional control, pre-post intervention time periods were examined.
OR=Odds Ratio; IRR= incidence rate ratio; tx = treatment
General Practitioner Inclusion Criteria: on a list provided by Australasian Medical Publishing Company, worked at least 2 days per week, had at least 50 patients aged 60+ who spoke English, and were not planning to retire or move practice within the next two years. Sample size: GP N=373 (with N=21,762 patients aged 60+), intervention GP N=188 (N= 11,402 patients aged 60+), control GP N=185 (N= 10,360 patients aged 60+).
Patient Inclusion Criteria: treated at one of the 20 primary care practices participating in the study, aged 60+, met DSM-IV criteria for major or minor depression, defined as 3–4 depressive symptoms, score on the 24-item Hamilton Depression Rating Scale (HAM-D) ≥10, and a duration of at least 1 month. Sample size: Patients N=599, intervention N=320, control N=279.
Education for Youth Suicidal Behavior Prevention
Although 4/9 prevention studies in youth reported less suicidal behavior (Table S1), 7/9 found less ideation (Table S1). A key factor appears to be the population targeted for education. Targeting high school students prevented student suicide attempts (29, 30) whereas targeting teachers (29) and all but one parent study (Table S1), did not find benefit. Of the two successful educational programing studies in high schools, the first study, involving 168 high schools and 11,110 students, randomizing high schools to either a teacher/staff gatekeeper education program, a professional screening program with referral of identified at-risk students, student education about mental health (YAM) or a control group. YAM prevented suicidal behavior relative to the control condition, but the screening intervention and educating teachers/staff gatekeepers did not. In the second study, 4,133 high students were randomized to a mental health and suicide education program or control group. Less suicidal behavior was observed in the active intervention group relative to the control group over the next year. There are no controlled trials of targeted gatekeeper education in adults. Depression-management education of doctors lowers adult suicide rates (Table 2), but extending the education to other gatekeepers and the general public is not proven to further lower nonfatal and fatal suicide attempt rates.(31)
System-Level Education
A system-level approach shows promise in lowering suicide risk and involves applying a combination of education, training and screening. Such an approach lacks the capacity to measure the separate effect of each intervention component. One study examined the impact on suicide rates in 1,126 U.S. counties of interventions, funded by the Garrett Lee Smith Act, directed at young persons (ages 10–24 yrs.).(32) The legislation funded a range of interventions, including gatekeeper training (N=125,000) and screening programs to identify at risk youth (N=29,000 were screened). Of note, 73% of education recipients were students, and based on the Wasserman et al high school study(29), emphasizing student education may have been crucial for gatekeeper education being effective. Education also included mental health professionals and emergency department staff. The intervention counties exhibited a decline in youth suicide rates that did not extend to other causes of death in youth or to adult suicide rates, compared with 969 demographical and sociologically comparable counties where this program was not implemented. These findings indicate the benefit for suicide was found in the intervention counties and confined to the demographic group targeted by the intervention. Moreover, this benefit lasted for 2 years beyond the intervention, and was proportional to the number of years the program ran.(32) Follow-up found the benefit faded once programming stopped regardless of years it was implemented.
System-wide health care changes have not been tested in a randomized study but promising results have emerged from opportunistic before and after studies.(33) One study in the United Kingdom (34) found benefit for an array of clinical service changes including improved depression management, continuity of care from adolescent patient services to adult patient services, improved community services and lower staff turnover and found reduced suicide rates with incident rate ratios of .71–.79. The decline in suicide rates was observed in the study sample of 19,248 suicides who were in treatment within 12 months of death studied 1997–2012. This study did not control for changes in the secular suicide rate, and there was no randomization of the intervention, despite the fact that the poorest districts where the interventions were deployed had the greatest declines in suicide rates.(35) Denmark used to have one of the highest suicide rates in the World. In 1980, the annual suicide rate was 38/100,000 in those over age 15 yrs. Since 2007, the rate has stabilized at 11.4/100,000. The Danish suicide prevention effort has many components, and one of the most important was means restriction but other elements included a 66% increase in psychiatric services since 2000, establishment of Suicide Prevention Clinics, Psychiatric Emergency Outreach Teams and post-discharge program called Strengthening Outpatient Care After Discharge.(36) A U.S. study examined the effect of staff education and frequent screening of suicide risk in all psychiatric patients in the Henry Ford Health System that resulted in 9 consecutive quarters without a suicide compared with 80/100,000 suicides in 2000. The program ran from 2001–2007, and the rate declined to zero in the period 2008–2010, inspiring the notion of zero suicide as a goal for health care systems.
Implementing and sustaining such results is aspirational and is worthy of further evaluation.(33)
SCREENING
Screening for suicide risk to identify otherwise undetected at-risk individuals,(30, 37) if coupled with effective referral for evaluation and treatment, was found by some studies to prevent suicidal behavior.(15–17, 37, 38) However, other studies did not finding screening and referral of at-risk high school students to be effective.(29) Brief screening tools like the P4, that assesses the 4P’s (past suicide attempt, suicide plan, probability of completing suicide and preventive factors), or the Columbia Suicide Severity Rating Scale (C-SSRS), that assesses severity of previous suicidal behavior and current suicidal ideation, may improve triage.(37, 39) The 2014 United States Preventative Services Task Force report concluded there is insufficient evidence that screening, specifically for suicide risk in primary care, identified new cases beyond screening for a psychiatric disorder, distress or a past suicide attempt.(40) The C-SSRS predicted suicide attempts with an OR of 4.8 (95% CI 2.23–10.32, p<.001) in adolescents and young adults following an emergency psychiatric evaluation.(41) Screening in the U.S. military(42) indicated current ideation added predictive power to a history of a previous suicide attempt. More complex EMR-based screening, bypassing gatekeepers, may improve identification of higher risk patients.(43–47)
TREATMENT INTERVENTIONS
Pharmacotherapy
Seventeen pharmacotherapy trials with suicidal behavior as an outcome (Table S2a), including twelve studies in adults, five pediatric studies and seven RCT meta-analyses(48–54), have appeared since the FDA(51) adopted black box warnings in 2004 and 2006 regarding psychotropic medication-related suicide risk in children and young adults, respectively. Medications reduced suicidal behavior in 4/12 adult studies,(55–58) but those effective medications belonged to pharmacologically diverse classes. More promisingly, antidepressants reduced suicidal ideation in 9/12 studies that reported effects on suicidal ideation.(55, 57, 59–65) Meta-analyses of RCT data show more impressive benefit for suicidal behavior than individual RCTs. Meta-analyses of both RCT and pharmaco-epidemiological studies often found stronger effects than single RCTs, perhaps because they included a larger sample. Pharmaco-epidemiologic studies often involve a much larger sample and follow outcomes over a longer time frame and apply less stringent participant exclusion criteria, resulting in the inclusion of a more clinically relevant patient population, including dual diagnosis and more severe presentations. A meta-analysis of all FDA-registered randomized placebo-controlled studies of fluoxetine and venlafaxine found these medications decreased suicidal ideation and behavior.(49, 52) An FDA meta-analysis found antidepressants lowered risk of suicidal behavior in older age groups, but subsequent pharmaco-epidemiological studies found SSRIs reduced suicidal behavior more broadly, including in young adults.(66, 67)
There may be advantages for specific types of antidepressants. SSRIs target serotonin, and appeared more effective than noradrenergic drugs for suicidal ideation.(59, 61) Contrary to earlier FDA findings, SSRIs may work without increasing risk of treatment-emergent suicidal ideation or behavior, even in youth.(67–69) Longitudinal pharmaco-epidemiologic studies in adolescents, young adults and older adults indicated that the greatest risk for a suicide attempt was in the month before antidepressant medication began, and after the medication was initiated, the risk declined progressively over months.(66, 67, 70) Ketamine, an NMDA glutamate receptor antagonist, reduced suicidal ideation within 1–4 hours in major depression(71–75) and bipolar disorder.(76, 77) Used adjunctively with other psychotropic medications, one RCT found ketamine’s benefit for suicidal ideation persisted for weeks,(72) but its effect on suicidal behavior has never been evaluated. The FDA approved intra-nasal esketamine for the treatment of depression with suicidal ideation, but not for the treatment of suicidal ideation. A meta-analysis found that intravenous ketamine improved suicidal ideation but other routes of administration lacked proof of efficacy.(78) The intra-nasal route may be less effective because of more erratic absorption and more side effects than the more slowly administered intravenous dose.(78)
Two of four RCTs showed benefit for suicidal behavior with lithium compared with various other medications.(55, 58, 79, 80) A meta-analysis of RCTs in bipolar disorder found no data on lithium’s effect on suicide prevention(81), however a meta-analysis of non-randomized studies suggested that risk of attempts and suicide was 5 times less with lithium treatment.(82) Although one study found no correlation between bipolar disorder and many other psychiatric disorders with lithium levels in drinking water (83), 11/16 ecological studies report these levels were linked to lower suicide rates.(84)
Three adolescent and young adult RCT studies found antidepressants reduced suicidal ideation,(62, 64, 65) one did not,(85) and none found a reduction in suicide behavior. One systematic review of antidepressants in pediatric populations found SSRIs increased odds of a suicide attempt,(53) but most subsequent meta-analyses and epidemiological studies in both pediatric(48),(50) and adult populations(49, 52, 66, 67, 86) reported a more favorable risk-benefit ratio than the FDA analyses,(51, 87) including benefits for suicidal behavior. The FDA meta-analysis of pediatric RCTs did not find a difference in suicidal behavior between placebo and active drugs(88), and even in the adolescent studies that reported more suicidal events compared with placebo, the number needed to harm (suicide-related event or ideation) is much greater than the number needed to benefit.(89)
Psychotherapy
Psychotherapy RCT studies are summarized in Table S3a. Cognitive behavior therapy (CBT) decreased suicidal behavior risk in adults and adolescents with depression, adults with borderline personality disorder (BPD), and halved suicide re-attempt rates in patients presenting to an emergency department following a recent suicide attempt compared with treatment as usual (TAU).(90) CBT for suicidal individuals is designed to help high-risk individuals apply more effective coping strategies (e.g., cognitive restructuring) in the context of stressors and problems that trigger suicidal behaviors. Therapists also are trained to identify patient-specific factors that maintain suicidal behaviors (90, 91). In substance use disorders, CBT reduced attempt frequency compared with TAU in adolescents(92) but not in adults.(93) CBT may work by improving negative problem orientation and emotion regulation,(94) reducing impulsiveness(95) and attenuating suicidal ideation.(96)
Dialectical behavior therapy (DBT) for BPD in adolescents, college students and adults prevented suicide attempts, hospitalization for suicidal ideation and lessened medical consequences of self-harm behaviors compared with treatment as usual (Table S3a). Treatment dose may be a factor because a single-session of dialectical behavior therapy did not reduce suicidal ideation,(97) whereas most effective studies employed a 20-week DBT intervention.(98, 99)
Psychodynamic psychotherapies for BPD prevent suicidal or self-harm behavior in most controlled studies (Table S3a). There are no replicated studies of other types of psychotherapeutic interventions showing prevention of suicidal behavior. Even if psychotherapies were effective, only CBT appears to be scalable (Table 2).
Comparison of Pharmacotherapy and Psychotherapy
Given efficacy evidence for pharmacotherapy and psychotherapy separately, combinations of both showed no advantage for suicidal behavior (Table S3b).
Group Psychotherapy
Group psychotherapies reduced suicidal ideation in 5/10 studies(100–109) and suicide in one,(100) but none reported reducing nonfatal suicide attempts (Table S3c). Cost effectiveness and potential for scaling are moot without replicated efficacy for suicidal behavior.
Contact and/or Active Outreach following a Suicide Attempt or Suicidal Ideation Crisis
The greatest risk of suicidal behavior is after discharge from the emergency room (ER) or hospital inpatient units.(110–112) Follow-up contact interventions as simple as sending postcards prevented suicide attempt in 2/4 studies (Table S4), consistent with older studies that found a robust benefit for reducing suicidal behaviors.(110) Enhancing treatment engagement and compliance following an ER visit or hospital stay through follow-up contact calls, reduced attempts or ideation in 4/5 studies (Table S4). These interventions are scalable as shown by a multi-national study reporting psychoeducation paired with phone or in-person contact reduced the suicide rate over 18-months in suicide attempters.(113) Another study used a similar approach by sending caring text messages over one year to active military personnel who had reported a suicide attempt (50%) or suicidal ideation, but not in the context of discharge from hospital or ED. The intervention lowered subsequent suicide attempts by almost half.(114) A cohort comparison study of safety planning interventions, administered in ED with follow-up telephone contact produced a 45% reduction in suicidal behaviors vs. TAU.(115)
Brain Stimulation
Repetitive transcranial magnetic stimulation (rTMS) and electroconvulsive therapy (ECT) reduced suicidal ideation, but samples were too small to evaluate effects on attempts (Table S2b). Deep Brain Stimulation has also not been shown to prevent suicide attempts (Table S2b).
Collaborative Care
Collaborative care involves embedding psychiatric healthcare expertise within a primary care setting, army units and schools to enhance mental health care. This benefited suicidal ideation, but mostly did not prevent suicidal behavior. The exceptions are a collaborative care program involving lay health workers in both primary and private care settings(116), and depression screening studies in which psychiatrists oversaw the antidepressant treatment resulting in reduced suicide rates in both men and women (Table 2). By contrast, when GPs delivered this treatment, it worked in women but not men (Table 2).
Internet-Based Interventions
Internet-based interventions have not been shown to prevent suicidal behavior (Table S5) but are highly scalable. Only 3/10 studies reported benefit for suicidal ideation(117–123) (Table S5). Internet-based interventions can reach most untreated at-risk individuals and provide low-cost screening, psychoeducation and web-based psychotherapeutic treatment interventions. Adolescents disclosed comparable information about their mental health via web-based and paper-and-pencil screening forms.(123) Online interventions increased suicide-prevention related knowledge,(124) but not all improved suicide literacy or reduced suicide stigma.(122) Internet CBT, with or without phone follow-up, was not more effective compared with waitlist controls for reducing suicidal ideation.(121, 125) A game-like mobile app showed promise in reducing self-injury and suicide plans, but not suicidal ideation.(126)
MEANS RESTRICTION
Restricting access to the most available and lethal means for suicide, such as firearms, lowered suicide rates using the restricted method,(127–137) and lowered overall suicide rates when the method was sufficiently widely used.(127, 130–135) Pesticide ingestion was employed in approximately one-third of suicides worldwide, mostly in rural Asia and Latin America.(138) Centralized locked or guarded storage facilities combined with use of less toxic chemicals have contributed to a worldwide decline in pesticide suicides.(129) Banning pesticides in Sri Lanka reduced pesticide-related suicide rates without a concurrent increase in non-pesticide suicide deaths.(139) Firearm suicide rate was closely related to firearm ownership rate.(140) Firearms are used in half of all U.S. suicides.(130, 131) Gun access restriction and gun safety robustly reduced firearm suicides with only modest method substitution.(127, 132–135) Firearm buyback programs have reduced firearm-related suicides (141), but legal precedents and public opinion have undermined gun control and buyback programs, so the U.S. has not been able to emulate implementation of such programs, or achieve the reduction in firearm suicides seen in other countries. Improved gun safety is more feasible than reducing gun ownership in the U.S. because of legal impediments to national gun control, and most guns used for suicide were purchased years prior to the suicide.(132) Other proven means restriction approaches include better car catalytic converters that reduce carbon monoxide content,(136, 142) switching from coal gas to natural gas, which has low carbon monoxide content,(128) and barriers at hotspots such as bridges and railway stations.(137)
Discussion
Applying the criteria of replicated efficacy for preventing suicidal behavior (Table 1) and scalability means that the best options for suicide prevention are: (1) educating primary care physicians in depression management and evaluating the expansion of such programs to other non-psychiatric medical specialties such as internists and obstetrician gynecologists; (2) educating high school students about mental health and evaluating extension of this approach to college students; (3) means restriction; and (4) pre-discharge education and follow-up contact and outreach for ER and hospital psychiatric patient discharges and in patients following a suicide crisis. Effective, but less scalable, are (5) specific psychotherapies (CBT, DBT). Finally, there are unproven options that are scalable and promising: (6) fast-acting medications like ketamine; and (7) internet-based screening and treatment delivery and continuous passive monitoring of risk.
Educating non-psychiatrist primary care physicians to better diagnose and treat major depression prevents suicide and non-fatal suicide attempts (Table 2). Several related observations explain why. Approximately 90% of suicides have a current diagnosable psychiatric disorder, most commonly a major depression that was untreated at time of death.(111, 143, 144) In 2015, 9.8 million persons (4% of all those aged 18 years and older) in the U.S. had serious thoughts about attempting suicide and yet more than half received no mental services in the prior year. The result: 1.47 million persons (0.6%) made a suicide attempt.(145) Despite a large increase in antidepressant prescription rates,(49, 52, 59, 66, 86, 146) when suicide decedents seek help, they go to non-psychiatrist physicians.
The debate about the safety of antidepressant in adolescents and young adults needs to be informed by the 17 RCTs (Table S2a) as well as meta-analytic and pharmaco-epidemiologic studies(48–50, 52–54, 66, 67, 86) published since the FDA promulgated the black box warnings for many classes of psychotropic medications. Both pediatric and adult studies of antidepressant effects on suicidal behavior show reductions in suicidal behavior in meta-analyses, more readily than in individual RCTs, probably because the low base rate of suicide attempts requires larger sample sizes. Ketamine reduces suicidal ideation within 1–4 hours, instead of weeks like other antidepressants, in major depression(71–73) and bipolar disorder.(76, 77) Rapid, robust reduction of suicidal ideation may dramatically increase patient safety, but its effect on suicidal behavior is unknown and a priority for suicide prevention research. More information is needed on the relative efficacy of intra-nasal and intravenous ketamine. The urgency around finding effective COVID-19 antiviral medications needs to be brought to the evaluation of medications that may act as rapidly to prevent suicide.
Educating other gatekeepers about the signs of suicide risk and need to refer for help raises questions about who to focus on for the best results (Table S1). Two studies in high schools found pupil education prevented suicide attempts (29, 30), with one finding it more effective than teacher/gatekeeper training, the latter was no better than the control arm of the study.(29) In the absence of data from RCTs on whether training adult gatekeepers prevents suicidal behavior in adults, colleges, universities, military and police try educate everyone in their system.
Screening for suicidal ideation in school, college, medical clinic and military populations, seeks to identify otherwise undetected at-risk individuals. Although it does not induce subsequent suicidal ideation,(38, 147) screening a non-help-seeking population for suicidal ideation and nonfatal suicide attempts, beyond screening for major depression, remains a debated approach.(40) Newer promising approaches may involve using smartphone technology to detect risk(148, 149) and algorithm-guided electronic medical record screening.(43, 44, 46, 150)
CBT, DBT and individual psychodynamic psychotherapies prevent suicide attempts, but aside from CBT, scalability limits their value in suicide prevention. Combining medication with individual psychotherapy does not offer any measurable advantage. No brain stimulation therapies have demonstrated suicide behavior prevention.
Sleep disturbance(151) and effects on mood and decision-making by acute alcohol intake(152) are risk factors for suicidal behavior that warrant further evaluation as potential prevention targets.
The greatest risk for repeating a suicide attempt is in the month following an index attempt, and particularly after discharge of a psychiatric patient from an emergency department or inpatient hospital unit.(110–112) Pre-discharge education and assertive outreach after discharge, prevent suicide attempts (Table 2; Table S1). Surprisingly, this approach has not been widely adopted in the U.S. and may reflect gaps in continuity of care between inpatient and outpatient systems and between emergency departments and outpatient care. Calibrating suicide prevention efforts to times of greater risk as well as to patients showing higher risk clinical profiles would be more efficient and potentially effective.
The internet has great potential for suicide prevention by screening, education, outreach, referral, monitoring of ongoing risk and treatment, but applications are new and testing their efficacy still in progress.(120–122, 153) Internet-based interventions are economical and scalable, reaching untreated at-risk individuals and offering help to anyone with a phone and WiFi access. Passive monitoring via a smartphone is an inexpensive, but untested, method for tracking risk.
Most suicide attempter survivors do not ultimately die by suicide, which is why means restriction, targeting the most lethal methods, saves many lives.(154, 155) Surprisingly, faced with no access to their chosen method, most individuals do not turn to alternative means for suicide, as shown for coal and gas(156) or firearm restriction.(127) Means restriction needs to target the main means used in each region. Firearms are used in half of all suicides in the U.S.(1) Yet restricting access of at-risk individuals to firearms in the U.S. is under-utilized.(132) Gun buy-back programs have worked in other countries(141) and, together with safer gun storage, are needed in the U.S. because most firearms used for suicide were purchased years earlier.(157) Pesticides are highly lethal, the leading suicide method worldwide, and the decline in suicide deaths worldwide is largely due to restricting access to pesticides where those deaths happen, namely in rural China,(138, 158) India(129) and Sri Lanka.(159)
LIMITATIONS OF THE STUDY
The major limitation of this review is the uneven quality and quantity of data available for different suicide prevention strategies. Within strategies there is heterogeneity of study populations in terms of psychiatric illness, proportion of higher risk patients such as those with a history of a past suicide attempt, age, ethnicity and proportion of males (because males have 3–4 times the suicide rate of females). Higher risk groups (e.g., Native Americans, First Nations), demographic groups like children and the elderly, and psychiatric disorders like schizophrenia, eating disorders or substance use disorders, are understudied. Small sample sizes, too few studies and lack of replication studies prevent firm conclusions about many approaches. Suicidal ideation as an outcome measure is not as closely related to suicide as are nonfatal suicide attempts. Evaluating complex interventions with multiple components makes it hard to determine the effective elements. Finally, there is a need for objective criteria for determining which interventions are capable of being scaled up from local studies to national level deployment.
CONCLUSIONS
Education of primary care physicians, and potentially internists and obstetricians, in the diagnosis and treatment of depression is a robust suicide prevention approach. Other proven scalable strategies (Table 1) are: (1) follow-up of discharged and other acutely suicidal patients with active outreach; (2) CBT; and (3) means restriction. Education directed at youth prevents suicidal behavior but when directed at teachers does not; no RCT data are available for prevention of adult suicide. Any prevention program requires outcome assessment that must include suicidal behavior and preferably mediating effects such as help-seeking behavior, treatment provision and treatment compliance. The biggest challenge in suicide prevention is improving the identification of who is at high risk and when. Determination of imminent risk is needed for calibration of prevention efforts to high risk periods by employment of rapid reduction of suicidal ideation and means restriction. Fast-acting medications like ketamine may have a role during acute suicide risk but are untested for prevention of suicide attempts. Determination of imminent risk has evolved towards continuous monitoring via mobile devices.(148, 149) Future work is needed to evaluate such approaches and how to integrate them into prevention responses.
Supplementary Material
Acknowledgements:
Funding from the National Institute of Mental Health (NIMH) provided partial support for JJM (5P50MH090964) and RPA (U01MH108168) to prepare this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or NIMH. Sadia Choudhury, Ph.D., Rahil Kamath, B.A., Grace Allison, B.A., and Kira Alqueza, B.A., helped with the literature search and supplemental tables.
Conflicts of Interest: JJM receives royalties from the Research Foundation for Mental Hygiene for commercial use of the C-SSRS. CAM has no conflicts to report. RPA is a member of the Research Grants Committee for the American Foundation for Suicide Prevention. The design, preparation, review, and approval of the manuscript as well as the decision to submit the manuscript for publication was entirely done by the authors JJM, CAM and RPA.
References
- 1.Prevention CfDCa. WISQARS: Fatal injury reports, national and regional, 1999–2018 2020, February 20 [Available from: https://webappa.cdc.gov/sasweb/ncipc/mortrate.html.
- 2.Xu J, Murphy S, Kochanek K, Arias E. Mortality in the United States. National Center for Health Statistics. 2018;NCHS data brief, no 267. [Google Scholar]
- 3.Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014: US Department of Health and Human Services, Centers for Disease Control and …; 2016. [Google Scholar]
- 4.Health UDo, Services H. National strategy for suicide prevention: Goals and objectives for action. Rockville, MD: Author; 2001. [PubMed] [Google Scholar]
- 5.OECD. Suicide rates 2017. [Available from: https://data.oecd.org/healthstat/suiciderates.htm.
- 6.Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies: a systematic review. Jama. 2005;294(16):2064–74. [DOI] [PubMed] [Google Scholar]
- 7.Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry. 2008;192(2):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Heeringen K, Mann JJ. The neurobiology of suicide. The Lancet Psychiatry. 2014;1(1):63–72. [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–9. [DOI] [PubMed] [Google Scholar]
- 10.Duflo E, editor Scaling up and evaluation. Annual World Bank Conference on Development Economics 2004; 2004. [Google Scholar]
- 11.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. American Journal of Psychiatry. 2002;159(6):909–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Szanto K, Kalmar S, Hendin H, Rihmer Z, Mann JJ. A suicide prevention program in a region with a very high suicide rate. Archives of general psychiatry. 2007;64(8):914–20. [DOI] [PubMed] [Google Scholar]
- 13.Rutz W. Preventing suicide and premature death by education and treatment. Journal of affective disorders. 2001;62(1–2):123–9. [DOI] [PubMed] [Google Scholar]
- 14.Oyama H, Ono Y, Watanabe N, Tanaka E, Kudoh S, Sakashita T, et al. Local community intervention through depression screening and group activity for elderly suicide prevention. Psychiatry and clinical neurosciences. 2006;60(1):110–4. [DOI] [PubMed] [Google Scholar]
- 15.Oyama H, Watanabe N, Ono Y, Sakashita T, Takenoshita Y, Taguchi M, et al. Community‐based suicide prevention through group activity for the elderly successfully reduced the high suicide rate for females. Psychiatry and clinical neurosciences. 2005;59(3):337–44. [DOI] [PubMed] [Google Scholar]
- 16.Oyama H, Goto M, Fujita M, Shibuya H, Sakashita T. Preventing elderly suicide through primary care by community-based screening for depression in rural Japan. Crisis. 2006;27(2):58–65. [DOI] [PubMed] [Google Scholar]
- 17.Oyama H, Fujita M, Goto M, Shibuya H, Sakashita T. Outcomes of community-based screening for depression and suicide prevention among Japanese elders. The Gerontologist. 2006;46(6):821–6. [DOI] [PubMed] [Google Scholar]
- 18.Henriksson S, Isacsson G. Increased antidepressant use and fewer suicides in Jämtland county, Sweden, after a primary care educational programme on the treatment of depression. Acta psychiatrica Scandinavica. 2006;114(3):159–67. [DOI] [PubMed] [Google Scholar]
- 19.Hübner-Liebermann B, Neuner T, Hegerl U, Hajak G, Spießl H. Reducing suicides through an alliance against depression? General hospital psychiatry. 2010;32(5):514–8. [DOI] [PubMed] [Google Scholar]
- 20.Hegerl U, Maxwell M, Harris F, Koburger N, Mergl R, Székely A, et al. Prevention of suicidal behaviour: Results of a controlled community-based intervention study in four European countries. PloS one. 2019;14(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hegerl U, Mergl R, Havers I, Schmidtke A, Lehfeld H, Niklewski G, et al. Sustainable effects on suicidality were found for the Nuremberg alliance against depression. European archives of psychiatry and clinical neuroscience. 2010;260(5):401–6. [DOI] [PubMed] [Google Scholar]
- 22.Alexopoulos GS, Reynolds III M, Charles F, Bruce ML, Katz IR, Raue PJ, Mulsant BH, et al. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. American Journal of Psychiatry. 2009;166(8):882–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rutz W, Von Knorring L, Wålinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta psychiatrica Scandinavica. 1989;80(2):1514. [DOI] [PubMed] [Google Scholar]
- 24.Takahashi K. Suicide prevention for the elderly in Matsunoyama Town, Higashikubiki County Niigata Prefecture: Psychiatric care for elderly depression in the community. Psychiatr Neurol Jpn. 1998;100:469–85. [PubMed] [Google Scholar]
- 25.Oyama H, Koida J, Sakashita T, Kudo K. Community-based prevention for suicide in elderly by depression screening and follow-up. Community mental health journal. 2004;40(3):249–63. [DOI] [PubMed] [Google Scholar]
- 26.Almeida OP, Pirkis J, Kerse N, Sim M, Flicker L, Snowdon J, et al. A randomized trial to reduce the prevalence of depression and self-harm behavior in older primary care patients. The Annals of Family Medicine. 2012;10(4):347–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roškar S, Podlesek A, Zorko M, Tavčar R, Dernovšek MZ, Groleger U, et al. Effects of training program on recognition and management of depression and suicide risk evaluation for Slovenian primary-care physicians: follow-up study. Croatian medical journal. 2010;51(3):23742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Beurs DP, Hooiveld M, Kerkhof AJ, Korevaar JC, Donker GA. Trends in suicidal behaviour in Dutch general practice 1983–2013: a retrospective observational study. BMJ open. 2016;6(5):e010868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wasserman D, Hoven CW, Wasserman C, Wall M, Eisenberg R, Hadlaczky G, et al. School-based suicide prevention programmes: the SEYLE cluster-randomised, controlled trial. The Lancet. 2015;385(9977):1536–44. [DOI] [PubMed] [Google Scholar]
- 30.Aseltine RH, James A, Schilling EA, Glanovsky J. Evaluating the SOS suicide prevention program: a replication and extension. BMC public health. 2007;7(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hegerl U, Althaus D, Schmidtke A, Niklewski G. The alliance against depression: 2-year evaluation of a community-based intervention to reduce suicidality. Psychological medicine. 2006;36(9):1225–33. [DOI] [PubMed] [Google Scholar]
- 32.Godoy Garraza L, Kuiper N, Goldston D, McKeon R, Walrath C. Long‐term impact of the Garrett Lee Smith Youth Suicide Prevention Program on youth suicide mortality, 2006–2015. Journal of child psychology and psychiatry. 2019;60(10):1142–7. [DOI] [PubMed] [Google Scholar]
- 33.Stanley B, Mann JJ. The need for innovation in health care systems to improve suicide prevention. JAMA psychiatry. 2020;77(1):96–8. [DOI] [PubMed] [Google Scholar]
- 34.Kapur N, Ibrahim S, While D, Baird A, Rodway C, Hunt IM, et al. Mental health service changes, organisational factors, and patient suicide in England in 1997–2012: a before-and-after study. The Lancet Psychiatry. 2016;3(6):526–34. [DOI] [PubMed] [Google Scholar]
- 35.While D, Bickley H, Roscoe A, Windfuhr K, Rahman S, Shaw J, et al. Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: a cross-sectional and before-and-after observational study. The Lancet. 2012;379(9820):1005–12. [DOI] [PubMed] [Google Scholar]
- 36.Nordentoft M, Erlangsen A. Suicide—turning the tide. American Association for the Advancement of Science; 2019. [DOI] [PubMed]
- 37.Dube P, Kurt K, Bair MJ, Theobald D, Williams LS. The p4 screener: evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. Primary care companion to the Journal of clinical psychiatry. 2010;12(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crawford MJ, Thana L, Methuen C, Ghosh P, Stanley SV, Ross J, et al. Impact of screening for risk of suicide: randomised controlled trial. The British Journal of Psychiatry. 2011;198(5):379–84. [DOI] [PubMed] [Google Scholar]
- 39.Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia–Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. American journal of psychiatry. 2011;168(12):1266–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siu AL, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, et al. Screening for depression in adults: US Preventive Services Task Force recommendation statement. Jama. 2016;315(4):380–7. [DOI] [PubMed] [Google Scholar]
- 41.Horwitz AG, Czyz EK, King CA. Predicting future suicide attempts among adolescent and emerging adult psychiatric emergency patients. Journal of Clinical Child & Adolescent Psychology. 2015;44(5):751–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kessler RC, Stein MB, Petukhova MV, Bliese P, Bossarte RM, Bromet EJ, et al. Predicting suicides after outpatient mental health visits in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Molecular psychiatry. 2017;22(4):544–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schoenbaum M, Kessler RC, Gilman SE, Colpe LJ, Heeringa SG, Stein MB, et al. Predictors of suicide and accident death in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS): results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA psychiatry. 2014;71(5):493–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simon GE, Rutter CM, Do Peterson MO, Whiteside U, Operskalski B, Ludman EJ. Do PHQ depression questionnaires completed during outpatient visits predict subsequent suicide attempt or suicide death? Psychiatric services (Washington, DC). 2013;64(12):1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kessler RC, Warner CH, Ivany C, Petukhova MV, Rose S, Bromet EJ, et al. Predicting suicides after psychiatric hospitalization in US Army soldiers: the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). JAMA psychiatry. 2015;72(1):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Simon GE, Shortreed SM, Johnson E, Beck A, Coleman KJ, Rossom RC, et al. Between‐visit changes in suicidal ideation and risk of subsequent suicide attempt. Depression and anxiety. 2017;34(9):794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Obeid JS, Dahne J, Christensen S, Howard S, Crawford T, Frey LJ, et al. Identifying and predicting intentional self-harm in electronic health record clinical notes: deep learning approach. JMIR medical informatics. 2020;8(7):e17784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu Y, Bai S, Lan X, Qin B, Huang T, Xie P. Randomized controlled trials of serotoninnorepinephrine reuptake inhibitor in treating major depressive disorder in children and adolescents: a meta-analysis of efficacy and acceptability. Brazilian journal of medical and biological research. 2016;49(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gibbons RD, Hur K, Brown CH, Davis JM, Mann JJ. Benefits from antidepressants: synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. Archives of general psychiatry. 2012;69(6):572–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bridge JA, Iyengar S, Salary CB, Barbe RP, Birmaher B, Pincus HA, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: a meta-analysis of randomized controlled trials. Jama. 2007;297(15):1683–96. [DOI] [PubMed] [Google Scholar]
- 51.Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Archives of general psychiatry. 2006;63(3):332–9. [DOI] [PubMed] [Google Scholar]
- 52.Gibbons RD, Brown CH, Hur K, Davis JM, Mann JJ. Suicidal thoughts and behavior with antidepressant treatment: reanalysis of the randomized placebo-controlled studies of fluoxetine and venlafaxine. Archives of general psychiatry. 2012;69(6):580–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fergusson D, Doucette S, Glass KC, Shapiro S, Healy D, Hebert P, et al. Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials. BMJ (Clinical research ed). 2005;330(7488):396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cipriani A, Zhou X, Del Giovane C, Hetrick SE, Qin B, Whittington C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis. The Lancet. 2016;388(10047):881–90. [DOI] [PubMed] [Google Scholar]
- 55.Khan A, Khan SR, Hobus J, Faucett J, Mehra V, Giller EL, et al. Differential pattern of response in mood symptoms and suicide risk measures in severely ill depressed patients assigned to citalopram with placebo or citalopram combined with lithium: role of lithium levels. Journal of psychiatric research. 2011;45(11):1489–96. [DOI] [PubMed] [Google Scholar]
- 56.Thomas S, Drici M, Hall G, Crocq M, Everitt B, Lader M, et al. Safety of sertindole versus risperidone in schizophrenia: principal results of the sertindole cohort prospective study (SCoP). Acta psychiatrica Scandinavica. 2010;122(5):345–55. [DOI] [PubMed] [Google Scholar]
- 57.Zisook S, Lesser IM, Lebowitz B, Rush AJ, Kallenberg G, Wisniewski SR, et al. Effect of antidepressant medication treatment on suicidal ideation and behavior in a randomized trial: an exploratory report from the Combining Medications to Enhance Depression Outcomes Study. The Journal of clinical psychiatry. 2011;72(10):1322–32. [DOI] [PubMed] [Google Scholar]
- 58.Lauterbach E, Felber W, Müller‐Oerlinghausen B, Ahrens B, Bronisch T, Meyer T, et al. Adjunctive lithium treatment in the prevention of suicidal behaviour in depressive disorders: a randomised, placebo‐controlled, 1‐year trial. Acta psychiatrica Scandinavica. 2008;118(6):46979. [DOI] [PubMed] [Google Scholar]
- 59.Grunebaum MF, Ellis SP, Duan N, Burke AK, Oquendo MA, Mann JJ. Pilot randomized clinical trial of an SSRI vs bupropion: effects on suicidal behavior, ideation, and mood in major depression. Neuropsychopharmacology. 2012;37(3):697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weisler R, Khan A, Trivedi MH, Yang H, Eudicone J, Pikalov A, et al. Analysis of suicidality in pooled data from 2 double-blind, placebo-controlled aripiprazole adjunctive therapy trials in major depressive disorder. The Journal of clinical psychiatry. 2011;72(4):54855. [DOI] [PubMed] [Google Scholar]
- 61.Perroud N, Uher R, Marusic A, Rietschel M, Mors O, Henigsberg N, et al. Suicidal ideation during treatment of depression with escitalopram and nortriptyline in genome-based therapeutic drugs for depression (GENDEP): a clinical trial. BMC medicine. 2009;7(1):60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.von Knorring A-L, Olsson GI, Thomsen PH, Lemming OM, Hultén A. A randomized, double-blind, placebo-controlled study of citalopram in adolescents with major depressive disorder. Journal of clinical psychopharmacology. 2006;26(3):311–5. [DOI] [PubMed] [Google Scholar]
- 63.Canuso CM, Singh JB, Fedgchin M, Alphs L, Lane R, Lim P, et al. Efficacy and safety of intranasal esketamine for the rapid reduction of symptoms of depression and suicidality in patients at imminent risk for suicide: results of a double-blind, randomized, placebo-controlled study. American journal of psychiatry. 2018;175(7):620–30. [DOI] [PubMed] [Google Scholar]
- 64.March JS, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes. Archives of general psychiatry. 2007;64(10):1132–44. [DOI] [PubMed] [Google Scholar]
- 65.Brent DA, Emslie GJ, Clarke GN, Asarnow J, Spirito A, Ritz L, et al. Predictors of spontaneous and systematically assessed suicidal adverse events in the treatment of SSRIresistant depression in adolescents (TORDIA) study. American Journal of Psychiatry. 2009;166(4):418–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gibbons RD, Brown CH, Hur K, Marcus SM, Bhaumik DK, Mann JJ. Relationship between antidepressants and suicide attempts: an analysis of the Veterans Health Administration data sets. American Journal of Psychiatry. 2007;164(7):1044–9. [DOI] [PubMed] [Google Scholar]
- 67.Simon GE, Savarino J, Operskalski B, Wang PS. Suicide risk during antidepressant treatment. American Journal of Psychiatry. 2006;163(1):41–7. [DOI] [PubMed] [Google Scholar]
- 68.Thase ME, Edwards J, Durgam S, Chen C, Chang C-T, Mathews M, et al. Effects of vilazodone on suicidal ideation and behavior in adults with major depressive disorder or generalized anxiety disorder: post-hoc analysis of randomized, double-blind, placebo-controlled trials. International clinical psychopharmacology. 2017;32(5):281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thase ME, Gommoll C, Chen C, Kramer K, Khan A, Durgam S. Measures of suicidality in phase 3 clinical trials of levomilnacipran ER in adults with major depressive disorder. CNS spectrums. 2017;22(6):475–83. [DOI] [PubMed] [Google Scholar]
- 70.Valuck RJ, Libby AM, Sills MR, Giese AA, Allen RR. Antidepressant treatment and risk of suicide attempt by adolescents with major depressive disorder. CNS drugs. 2004;18(15):111932. [DOI] [PubMed] [Google Scholar]
- 71.Price RB, Iosifescu DV, Murrough JW, Chang LC, Al Jurdi RK, Iqbal SZ, et al. Effects of ketamine on explicit and implicit suicidal cognition: A randomized controlled trial in treatment‐resistant depression. Depression and anxiety. 2014;31(4):335–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grunebaum MF, Galfalvy HC, Choo T-H, Keilp JG, Moitra VK, Parris MS, et al. Ketamine for rapid reduction of suicidal thoughts in major depression: a midazolam-controlled randomized clinical trial. American Journal of Psychiatry. 2018;175(4):327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fan W, Yang H, Sun Y, Zhang J, Li G, Zheng Y, et al. Ketamine rapidly relieves acute suicidal ideation in cancer patients: a randomized controlled clinical trial. Oncotarget. 2017;8(2):2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Domany Y, Shelton RC, McCullumsmith CB. Ketamine for acute suicidal ideation. An emergency department intervention: A randomized, double‐blind, placebo‐controlled, proof‐of‐concept trial. Depression and anxiety. 2020;37(3):224–33. [DOI] [PubMed] [Google Scholar]
- 75.Phillips JL, Norris S, Talbot J, Birmingham M, Hatchard T, Ortiz A, et al. Single, repeated, and maintenance ketamine infusions for treatment-resistant depression: a randomized controlled trial. American Journal of Psychiatry. 2019;176(5):401–9. [DOI] [PubMed] [Google Scholar]
- 76.Zarate CA Jr, Brutsche NE, Ibrahim L, Franco-Chaves J, Diazgranados N, Cravchik A, et al. Replication of ketamine’s antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biological psychiatry. 2012;71(11):939–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Grunebaum MF, Ellis SP, Keilp JG, Moitra VK, Cooper TB, Marver JE, et al. Ketamine versus midazolam in bipolar depression with suicidal thoughts: A pilot midazolam‐controlled randomized clinical trial. Bipolar disorders. 2017;19(3):176–83. [DOI] [PubMed] [Google Scholar]
- 78.Dadiomov D, Lee K. The effects of ketamine on suicidality across various formulations and study settings. Mental Health Clinician. 2019;9(1):48–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Girlanda F, Cipriani A, Agrimi E, Appino MG, Barichello A, Beneduce R, et al. Effectiveness of lithium in subjects with treatment-resistant depression and suicide risk: results and lessons of an underpowered randomised clinical trial. BMC research notes. 2014;7(1):731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Oquendo MA, Galfalvy HC, Currier D, Grunebaum MF, Sher L, Sullivan GM, et al. Treatment of suicide attempters with bipolar disorder: a randomized clinical trial comparing lithium and valproate in the prevention of suicidal behavior. American journal of psychiatry. 2011;168(10):1050–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Geddes JR, Burgess S, Hawton K, Jamison K, Goodwin GM. Long-term lithium therapy for bipolar disorder: systematic review and meta-analysis of randomized controlled trials. American Journal of Psychiatry. 2004;161(2):217–22. [DOI] [PubMed] [Google Scholar]
- 82.Baldessarini RJ, Tondo L, Davis P, Pompili M, Goodwin FK, Hennen J. Decreased risk of suicides and attempts during long‐term lithium treatment: a meta‐analytic review. Bipolar disorders. 2006;8(5p2):625–39. [DOI] [PubMed] [Google Scholar]
- 83.Parker WF, Gorges RJ, Gao YN, Zhang Y, Hur K, Gibbons RD. Association between groundwater lithium and the diagnosis of bipolar disorder and dementia in the United States. JAMA psychiatry. 2018;75(7):751–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Del Matto L, Muscas M, Murru A, Verdolini N, Anmella G, Fico G, et al. Lithium and suicide prevention in mood disorders and in the general population: A systematic review. Neuroscience & Biobehavioral Reviews. 2020. [DOI] [PubMed]
- 85.Emslie GJ, Findling RL, Yeung PP, Kunz NR, Li Y. Venlafaxine ER for the treatment of pediatric subjects with depression: results of two placebo-controlled trials. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(4):479–88. [DOI] [PubMed] [Google Scholar]
- 86.Gibbons RD, Hur K, Bhaumik DK, Mann JJ. The relationship between antidepressant medication use and rate of suicide. Archives of general psychiatry. 2005;62(2):165–72. [DOI] [PubMed] [Google Scholar]
- 87.Hammad T. Review and evaluation of clinical trial data: Relationship between psychotropic drugs and pediatric suicide. Online document: http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-10-TAB08-Hammads-Review.pdf. 2004.
- 88.Stone M, Laughren T, Jones ML, Levenson M, Holland PC, Hughes A, et al. Risk of suicidality in clinical trials of antidepressants in adults: analysis of proprietary data submitted to US Food and Drug Administration. BMJ (Clinical research ed). 2009;339:b2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mann JJ, Emslie G, Baldessarini RJ, Beardslee W, Fawcett JA, Goodwin FK, et al. ACNP Task Force report on SSRIs and suicidal behavior in youth. Neuropsychopharmacology. 2006;31(3):473–92. [DOI] [PubMed] [Google Scholar]
- 90.Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Jama. 2005;294(5):563–70. [DOI] [PubMed] [Google Scholar]
- 91.Rudd MD, Bryan CJ, Wertenberger EG, Peterson AL, Young-McCaughan S, Mintz J, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. American journal of psychiatry. 2015;172(5):441–9. [DOI] [PubMed] [Google Scholar]
- 92.Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: a randomized trial. Journal of consulting and clinical psychology. 2011;79(6):728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Morley KC, Sitharthan G, Haber PS, Tucker P, Sitharthan T. The efficacy of an opportunistic cognitive behavioral intervention package (OCB) on substance use and comorbid suicide risk: A multisite randomized controlled trial. Journal of consulting and clinical psychology. 2014;82(1):130. [DOI] [PubMed] [Google Scholar]
- 94.Slee N, Spinhoven P, Garnefski N, Arensman E. Emotion regulation as mediator of treatment outcome in therapy for deliberate self‐harm. Clinical Psychology & Psychotherapy. 2008;15(4):205–16. [DOI] [PubMed] [Google Scholar]
- 95.Ghahramanlou-Holloway M, Bhar S, Brown G, Olsen C, Beck AT. Changes in problem-solving appraisal after cognitive therapy for the prevention of suicide. Psychological Medicine. 2012;42(6):1185–93. [DOI] [PubMed] [Google Scholar]
- 96.Slee N, Garnefski N, van der Leeden R, Arensman E, Spinhoven P. Cognitivebehavioural intervention for self-harm: randomised controlled trial. The British Journal of Psychiatry. 2008;192(3):202–11. [DOI] [PubMed] [Google Scholar]
- 97.Ward-Ciesielski EF, Tidik JA, Edwards AJ, Linehan MM. Comparing brief interventions for suicidal individuals not engaged in treatment: A randomized clinical trial. Journal of affective disorders. 2017;222:153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Twoyear randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of general psychiatry. 2006;63(7):757–66. [DOI] [PubMed] [Google Scholar]
- 99.Mehlum L, Tørmoen AJ, Ramberg M, Haga E, Diep LM, Laberg S, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(10):1082–91. [DOI] [PubMed] [Google Scholar]
- 100.Rabovsky K, Trombini M, Allemann D, Stoppe G. Efficacy of bifocal diagnosisindependent group psychoeducation in severe psychiatric disorders: results from a randomized controlled trial. European archives of psychiatry and clinical neuroscience. 2012;262(5):431–40. [DOI] [PubMed] [Google Scholar]
- 101.Kaminer Y, Burleson JA, Goldston DB, Burke RH. Suicidal ideation among adolescents with alcohol use disorders during treatment and aftercare. The American Journal on Addictions. 2006;15:s43–s9. [DOI] [PubMed] [Google Scholar]
- 102.Hsiao F-H, Lai Y-M, Chen Y-T, Yang T-T, Liao S-C, Ho RT, et al. Efficacy of psychotherapy on diurnal cortisol patterns and suicidal ideation in adjustment disorder with depressed mood. General hospital psychiatry. 2014;36(2):214–9. [DOI] [PubMed] [Google Scholar]
- 103.Ebrahimi H, Kazemi AH, Khoshknab MF, Modabber R. The effect of spiritual and religious group psychotherapy on suicidal ideation in depressed patients: A randomized clinical trial. Journal of caring sciences. 2014;3(2):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhang H, Neelarambam K, Schwenke TJ, Rhodes MN, Pittman DM, Kaslow NJ. Mediators of a culturally-sensitive intervention for suicidal African American women. Journal of Clinical Psychology in Medical Settings. 2013;20(4):401–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hazell PL, Martin G, Mcgill K, Kay T, Wood A, Trainor G, et al. Group therapy for repeated deliberate self-harm in adolescents: failure of replication of a randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(6):662–70. [DOI] [PubMed] [Google Scholar]
- 106.Green J, Wood A, Kerfoot M, Trainor G, Roberts C, Rothwell J, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ (Clinical research ed). 2011;342:d682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Blum N, St. John D, Pfohl B, Stuart S, McCormick B, Allen J, et al. Systems Training for Emotional Predictability and Problem Solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. American Journal of Psychiatry. 2008;165(4):468–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.McAuliffe C, McLeavey BC, Fitzgerald T, Corcoran P, Carroll B, Ryan L, et al. Group problem-solving skills training for self-harm: randomised controlled trial. The British Journal of Psychiatry. 2014;204(5):383–90. [DOI] [PubMed] [Google Scholar]
- 109.Simpson GK, Tate RL, Whiting DL, Cotter RE. Suicide prevention after traumatic brain injury: A randomized controlled trial of a program for the psychological treatment of hopelessness. The Journal of Head Trauma Rehabilitation. 2011;26(4):290–300. [DOI] [PubMed] [Google Scholar]
- 110.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatric services. 2001;52(6):828–33. [DOI] [PubMed] [Google Scholar]
- 111.Olfson M, Blanco C, Marcus SC. Treatment of adult depression in the United States. JAMA internal medicine. 2016;176(10):1482–91. [DOI] [PubMed] [Google Scholar]
- 112.Bostwick JM, Pabbati C, Geske JR, McKean AJ. Suicide attempt as a risk factor for completed suicide: even more lethal than we knew. American journal of psychiatry. 2016;173(11):1094–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fleischmann A, Bertolote JM, Wasserman D, De Leo D, Bolhari J, Botega NJ, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bulletin of the World Health Organization. 2008;86:703–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Comtois KA, Kerbrat AH, DeCou CR, Atkins DC, Majeres JJ, Baker JC, et al. Effect of augmenting standard care for military personnel with brief caring text messages for suicide prevention: a randomized clinical trial. JAMA psychiatry. 2019;76(5):474–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Stanley B, Brown GK, Brenner LA, Galfalvy HC, Currier GW, Knox KL, et al. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA psychiatry. 2018;75(9):894–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. The Lancet. 2010;376(9758):2086–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wilks CR, Lungu A, Ang SY, Matsumiya B, Yin Q, Linehan MM. A randomized controlled trial of an Internet delivered dialectical behavior therapy skills training for suicidal and heavy episodic drinkers. Journal of affective disorders. 2018;232:219–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.O’Toole MS, Arendt MB, Pedersen CM. Testing an app-assisted treatment for suicide prevention in a randomized controlled trial: effects on suicide risk and depression. Behavior therapy. 2019;50(2):421–9. [DOI] [PubMed] [Google Scholar]
- 119.Tighe J, Shand F, Ridani R, Mackinnon A, De La Mata N, Christensen H. Ibobbly mobile health intervention for suicide prevention in Australian Indigenous youth: a pilot randomised controlled trial. BMJ open. 2017;7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.van Spijker BA, van Straten A, Kerkhof AJ. Effectiveness of online self-help for suicidal thoughts: results of a randomised controlled trial. PloS one. 2014;9(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Christensen H, Farrer L, Batterham PJ, Mackinnon A, Griffiths KM, Donker T. The effect of a web-based depression intervention on suicide ideation: secondary outcome from a randomised controlled trial in a helpline. BMJ open. 2013;3(6):e002886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Taylor-Rodgers E, Batterham PJ. Evaluation of an online psychoeducation intervention to promote mental health help seeking attitudes and intentions among young adults: randomised controlled trial. Journal of affective disorders. 2014;168:65–71. [DOI] [PubMed] [Google Scholar]
- 123.Van De Looij‐Jansen PM, De Wilde EJ. Comparison of web‐based versus paper‐and‐pencil self‐administered questionnaire: Effects on health indicators in Dutch adolescents. Health services research. 2008;43(5p1):1708–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Till B, Tran US, Voracek M, Niederkrotenthaler T. Beneficial and harmful effects of educative suicide prevention websites: randomised controlled trial exploring Papageno v. Werther effects. The British Journal of Psychiatry. 2017;211(2):109–15. [DOI] [PubMed] [Google Scholar]
- 125.Hetrick SE, Yuen HP, Bailey E, Cox GR, Templer K, Rice SM, et al. Internet-based cognitive behavioural therapy for young people with suicide-related behaviour (Reframe-IT): a randomised controlled trial. Evidence-based mental health. 2017;20(3):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Franklin JC, Fox KR, Franklin CR, Kleiman EM, Ribeiro JD, Jaroszewski AC, et al. A brief mobile app reduces nonsuicidal and suicidal self-injury: evidence from three randomized controlled trials. Journal of Consulting and Clinical Psychology. 2016;84(6):544. [DOI] [PubMed] [Google Scholar]
- 127.Reisch T, Steffen T, Habenstein A, Tschacher W. Change in suicide rates in Switzerland before and after firearm restriction resulting from the 2003 “Army XXI” reform. American journal of psychiatry. 2013;170(9):977–84. [DOI] [PubMed] [Google Scholar]
- 128.Sarchiapone M, Mandelli L, Iosue M, Andrisano C, Roy A. Controlling access to suicide means. International journal of environmental research and public health. 2011;8(12):4550–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Vijayakumar L, Jeyaseelan L, Kumar S, Mohanraj R, Devika S, Manikandan S. A central storage facility to reduce pesticide suicides-a feasibility study from India. BMC public health. 2013;13(1):850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Thompson AJ. Gun violence in the United States: a public health epidemic. Public Health–Social and Behavioral Health Edited by Maddock J Intech. 2012:501–22.
- 131.Anglemyer A, Horvath T, Rutherford G. The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis. Annals of internal medicine. 2014;160(2):101–10. [DOI] [PubMed] [Google Scholar]
- 132.Mann JJ, Michel CA. Prevention of firearm suicide in the United States: what works and what is possible. American journal of psychiatry. 2016;173(10):969–79. [DOI] [PubMed] [Google Scholar]
- 133.Andrés AR, Hempstead K. Gun control and suicide: The impact of state firearm regulations in the United States, 1995–2004. Health policy (Amsterdam, Netherlands). 2011;101(1):95–103. [DOI] [PubMed] [Google Scholar]
- 134.McGinty EE, Webster DW, Barry CL. Gun policy and serious mental illness: priorities for future research and policy. Psychiatric Services. 2014;65(1):50–8. [DOI] [PubMed] [Google Scholar]
- 135.McPhedran S, Baker J. Suicide prevention and method restriction: evaluating the impact of limiting access to lethal means among young Australians. Archives of suicide research. 2012;16(2):135–46. [DOI] [PubMed] [Google Scholar]
- 136.Thomsen AH, Gregersen M. Suicide by carbon monoxide from car exhaust-gas in Denmark 1995–1999. Forensic science international. 2006;161(1):41–6. [DOI] [PubMed] [Google Scholar]
- 137.Pirkis J, Spittal MJ, Cox G, Robinson J, Cheung YTD, Studdert D. The effectiveness of structural interventions at suicide hotspots: a meta-analysis. International journal of epidemiology. 2013;42(2):541–8. [DOI] [PubMed] [Google Scholar]
- 138.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: systematic review. BMC public health. 2007;7(1):357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Knipe DW, Chang S-S, Dawson A, Eddleston M, Konradsen F, Metcalfe C, et al. Suicide prevention through means restriction: Impact of the 2008–2011 pesticide restrictions on suicide in Sri Lanka. PloS one. 2017;12(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Anestis MD, Houtsma C. The association between gun ownership and statewide overall suicide rates. Suicide and Life‐Threatening Behavior. 2018;48(2):204–17. [DOI] [PubMed] [Google Scholar]
- 141.Chapman S, Alpers P, Agho K, Jones M. Australia’s 1996 gun law reforms: faster falls in firearm deaths, firearm suicides, and a decade without mass shootings. Injury Prevention. 2006;12(6):365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Routley V. Motor vehicle exhaust gas suicide: review of countermeasures. Crisis. 2007;28(S1):28–35. [DOI] [PubMed] [Google Scholar]
- 143.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychological medicine. 2003;33(3):395–405. [DOI] [PubMed] [Google Scholar]
- 144.Niederkrotenthaler T, Logan JE, Karch DL, Crosby A. Characteristics of US suicide decedents in 2005–2010 who had received mental health treatment. Psychiatric services. 2014;65(3):387–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Piscopo K, Lipari R, Cooney J, Glasheen C. Suicidal Thoughts and Behavior among Adults: Results from the 2015 National Survey on Drug Use and Health. NSDUH Data Review. 2016.
- 146.Gibbons RD, Hur K, Brown CH, Mann JJ. Gabapentin and suicide attempts. Pharmacoepidemiology and drug safety. 2010;19(12):1241–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gould MS, Marrocco FA, Kleinman M, Thomas JG, Mostkoff K, Cote J, et al. Evaluating iatrogenic risk of youth suicide screening programs: a randomized controlled trial. Jama. 2005;293(13):1635–43. [DOI] [PubMed] [Google Scholar]
- 148.Allen NB, Nelson BW, Brent D, Auerbach RP. Short-term prediction of suicidal thoughts and behaviors in adolescents: Can recent developments in technology and computational science provide a breakthrough? Journal of affective disorders. 2019;250:163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Torous J, Larsen ME, Depp C, Cosco TD, Barnett I, Nock MK, et al. Smartphones, sensors, and machine learning to advance real-time prediction and interventions for suicide prevention: a review of current progress and next steps. Current psychiatry reports. 2018;20(7):51. [DOI] [PubMed] [Google Scholar]
- 150.Barak-Corren Y, Castro VM, Javitt S, Hoffnagle AG, Dai Y, Perlis RH, et al. Predicting suicidal behavior from longitudinal electronic health records. American journal of psychiatry. 2017;174(2):154–62. [DOI] [PubMed] [Google Scholar]
- 151.Malik S, Kanwar A, Sim LA, Prokop LJ, Wang Z, Benkhadra K, et al. The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: a systematic review and meta-analysis. Systematic reviews. 2014;3(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Borges G, Cherpitel CJ, Orozco R, Ye Y, Monteiro M, Hao W, et al. A dose–response estimate for acute alcohol use and risk of suicide attempt. Addiction biology. 2017;22(6):1554–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Van Spijker BA, Majo MC, Smit F, van Straten A, Kerkhof AJ. Reducing suicidal ideation: cost-effectiveness analysis of a randomized controlled trial of unguided web-based self-help. Journal of medical Internet research. 2012;14(5):e141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Daigle MS. Suicide prevention through means restriction: Assessing the risk of substitution: A critical review and synthesis. Accident Analysis & Prevention. 2005;37(4):625–32. [DOI] [PubMed] [Google Scholar]
- 155.Yip PS, Caine E, Yousuf S, Chang S-S, Wu KC-C, Chen Y-Y. Means restriction for suicide prevention. The Lancet. 2012;379(9834):2393–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kreitman N. The coal gas story. United Kingdom suicide rates, 1960–71. Journal of Epidemiology & Community Health. 1976;30(2):86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Miller M, Hemenway D. The relationship between firearms and suicide: a review of the literature. Aggression and violent behavior. 1999;4(1):59–75. [Google Scholar]
- 158.Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries. Oxford university press; 2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gunnell D, Fernando R, Hewagama M, Priyangika W, Konradsen F, Eddleston M. The impact of pesticide regulations on suicide in Sri Lanka. International journal of epidemiology. 2007;36(6):1235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.