Abstract
BACKGROUND:
Attention deficit hyperactivity disorder (ADHD) is a considerably common childhood-onset neurodevelopmental disorder, often associated with socio-behavioral and academic difficulties. There is an increased risk for development of a range of future problems such as psychiatric disorders, difficulties in employment, and relationships. The aim of this study was to know the prevalence and determinants of ADHD among primary school children in district Dehradun and to assess the learning difficulties and classroom behavior in these students.
MATERIALS AND METHODS:
In this cross-sectional study, overall, 228 students (aged 6–12 years) studying in a primary school were assessed for ADHD after seeking the written informed consent from their parents. The data were analyzed using Excel sheet and SPSS software (22.0 version). For all qualitative measures, frequency and percentages were calculated, and for quantitative measures, mean and standard deviation were calculated. For analysis of categorical values, Chi-square test was used. P < 0.05 was considered statistically significant.
RESULTS:
The prevalence of ADHD was found to be 11.8% based on the teacher tool only and 1.75% based on the parent and teacher tools combined. ADHD was found to be significantly more in males. Inattention was the most prevalent subtype of ADHD, and children screened positive for ADHD had significant learning difficulties at various levels.
CONCLUSION:
The possibility of ADHD in students with academic difficulties should not be ignored as children with ADHD usually face significant problems at school such as learning difficulties and have been shown to be at increased risk for a broad range of negative outcomes. Early identification and treatment of ADHD can significantly reduce the rates of some of these poor outcomes. Screening these children in the early years will help the parents, children, teachers, and community at large.
Keywords: Attention deficit disorder with hyperactivity, disabled children, learning disabilities, mass screening
Introduction
Attention deficit hyperactivity disorder (ADHD) is a substantially common neurobehavioral disorder with childhood onset. It is usually diagnosed when the child starts having academic difficulties in school. The symptoms usually appear in early childhood and may continue to persist during adolescence and adulthood. The worldwide prevalence estimates of ADHD are highly diversified. In past decades, various authors have reported highly heterogeneous prevalence rates across the world, ranging from as low as 1% to as high as nearly 20% among school-age children and adolescents.[1,2]
ADHD is a pertinacious condition of carelessness, lack of attention, and hyperactivity leading to functional impairment in different settings, such as scholastic and social settings. Children with ADHD may present with considerable disablement, often including underperformance in academics, poor relationship with peers, and lack of/negative communication with parents. This exposes them to increased risk of substance use and other risk-taking behaviors among other negative consequences.[3] Although the symptoms of ADHD may tone down with age, some people never completely outgrow their ADHD symptoms.
According to the “Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V),” ADHD has been differentiated into “three subtypes – primarily hyperactive-impulsive, primarily inattentive, or combined.”[4] Its etiology is not yet clearly understood, although multiple factors, namely genetic,[5] environmental, and neurobiological factors,[6] antenatal risk factors,[7] or risk factors during early childhood as well as social risk factors, have been implicated in its causation.[8]
Children with ADHD are usually at added on risk for a wide range of negative outcomes, if not diagnosed and treated timely. This condition can give rise to a variety of psychosocial consequences, ranging from depression, learning disabilities, school failure, and dropout to conduct disorders in children. In adult life, they are at heightened risk to have failed relationships, workplace frustrations due to underachievement, inferiority complex, and substance abuse.[9,10] Some of these poor outcomes can be significantly altered by early identification of ADHD and appropriate and timely intervention.
As the problems of children with ADHD often go beyond the disorder itself, the assessment should not only address the primary condition but also other characteristics of ADHD such as behavioral, emotional, and social aspects. This information often serves as a platform for determining how well the family members/caretakers will be able to implement treatment strategies. Early screening of these children will help the parents, children, teachers, and community at large.
Keeping all the above facts in mind and due to the paucity of research toward this topic in this part of northern India, this study was carried out under the Short-Term Studentship (STS) of the Indian Council of Medical Research (ICMR) to find out the prevalence of ADHD in primary school children in district Dehradun, Uttarakhand, with the objectives to know the prevalence and determinants of ADHD among primary school children in district Dehradun and to assess the learning difficulties and classroom behavior in these students.
ADHD is common in school-going children, but the parents may not recognize the early signs of the health conditions; it is further difficult for them if they belonged from poor socioeconomic background in difficult hilly areas like this study area. The recognition of this problem in early years of schooling is important as students with ADHD often struggle in their studies and are punished due to their classroom disruptive behavior, which can be addressed with timely intervention. Teachers, if trained properly, are able to screen the children and then counsel the parents to get proper referral and early intervention in the difficult hilly areas.
Materials and Methods
Study design and setting
This cross-sectional analytical study was carried out in a primary school in district Dehradun, Uttarakhand, India.
Study participants and sampling
This Short-Term Scholarship (STS) project was conducted under ICMR; purposive sampling was adopted to select the primary school. First of all, three approachable primary schools in Dehradun city were contacted and permission was sought from the school authorities to carry out the study. For this, meetings were arranged with the principals and the purpose of the study was explained. One of the school management agreed and gave permission for the survey. Written permission was procured from the school.
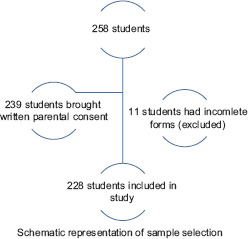
All the students in the age group of 6 years to 12 years were eligible to enter the survey. They were given a consent form, which they had to get signed by their parents/guardians. Parents were also asked about their choice of language on the assessment forms (Hindi/English). When the students brought back the signed consent forms, teachers and parents were given forms to fill about the behavior of the child and his/her scholastic performance. Teachers were oriented by the investigator to fill the forms and their queries were answered. Students were given the phone number of the investigator, so that parents can clear any doubts related to the questionnaire, if any. Forms with ≥20% of missing data were excluded from the analysis. Out of 258 students, 239 students brought written parental consent among them 11 students had incomplete forms (excluded). Overall, 228 students submitted the completed forms.
Data collection tool and technique
Data collection instrument (study tool):
Three types of forms were used to collect the information.
Baseline information form
“Vanderbilt ADHD Diagnostic Parent Rating Scale (VADPRS)
Vanderbilt ADHD Diagnostic Teacher Rating Scale (VADTRS).”
Baseline information form
A pretested, semi-structured data collection form was used to gather baseline information from parents regarding child's age, gender, class, parents’ education and occupation, sociodemographic profile, and any family history of ADHD, if known, etc.
Vanderbilt ADHD Diagnostic Rating Scale
The diagnosis of ADHD is based on criteria indicated by the “DSM-V.” For screening the children, Vanderbilt ADHD Diagnostic Rating Scale (VADRS) was used. The National Institute for Children's Health Quality Vanderbilt Assessment Scale is a psychological assessment tool used by health-care professionals to help screen ADHD by assessing various symptoms and their effects on behavior and academic performance in children aged 6–12.
“Assessment: Both parent and teacher assessment scales have two components:”
“Symptom assessment
-
Impairment in performance.”
- “The Symptom Assessment Component screens for symptoms relevant to inattentive and hyperactive ADHD subtypes
- To meet criteria for ADHD diagnoses, one must have 6 positive responses to either the core 9 inattentive symptoms or core 9 hyperactive symptoms, or both”
-
“Both the parent and the teacher versions ask the respondent to rate the frequency of a child's behaviors on a 0–3 scale as follows:”
- “0: never”
- “1: occasionally”
- “2: often”
- “3: very often”
- “Positive response is either a score of 2 or 3 (often to very often)”
- “The final 8 questions of both versions ask the respondent to rate the child's performance in school and his or her interactions with others on a 1–5 scale, with 1–2 meaning problematic, 3 meaning average, and 4–5 meaning above average”
- “To meet criteria for ADHD, there must be at least one score for the performance set that is either a 4 or 5, as these scores indicate impairment in performance.”
Statistical analysis
The data were analyzed using Excel sheet and SPSS software (22.0 version) IBM, Chicago, U.S. “SPSS”. For all qualitative measures, frequency and percentages were calculated, and for quantitative measures, mean and standard deviation were calculated. For analysis of categorical values, Chi-square test was used. P < 0.05 was considered statistically significant.
Ethical considerations
The study protocol was duly approved by the ICMR and Institutional Ethics Committee of Swami Rama Himalayan University, Dehradun.
Results
Out of 258 students, who fitted in the eligibility criteria, 239 children (92.6%) brought back the consent form signed by their parents and were entered into the study. Forms of 11 students could not be included due to incomplete information, so finally data from 228 students were used for analysis. Most of the students (21.1%) were 7 years old, while only 4 students (1.8%) were 12 years old. The mean age of the students was 8.3 (±1.7) years with a range of 6–12 years. The mean age of the girls was almost similar to that of boys. Males outnumbered female students (52.2% and 47.8%, respectively), and the M: F ratio was found to be 1.09.
Figure 1 shows that based on the teacher tool (VADTRS), the prevalence of ADHD among the studied children came out to be 11.8% (27 out of 228). When VADPRS (parent tool) was also considered, the prevalence fell to 1.75% (4 out of 228 students). For further analysis, results based on VADTRS (teacher tool) are being presented.
Figure 1.
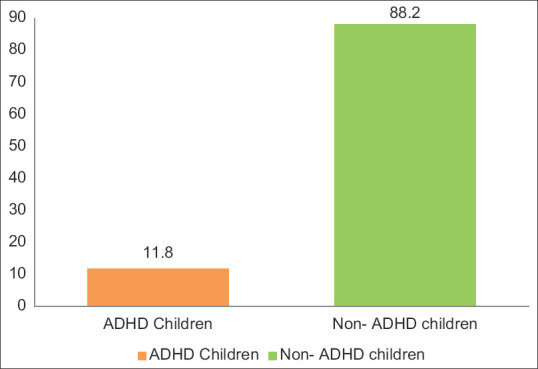
Prevalence of attention deficit hyperactivity disorder among primary school children
The prevalence of ADHD was found to be maximum in students in 12 years’ age group (75.0%), though the number was very small, followed by 9 years’ age group [Table 1]. The prevalence seems to be rising after 7 years of age. ADHD was found to be significantly more in male students (17.6%) as compared to female students (5.5%). The M: F ratio of ADHD was 3.5.
Table 1.
Prevalence of attention deficit hyperactivity disorder by age and gender
| Variables | Number of children (n) | ADHD present, n (%) | No ADHD, n (%) | P |
|---|---|---|---|---|
| Age (years) | ||||
| 6 | 40 | 2 (5.0) | 38 (95.0) | 24.130, P<0.001 |
| 7 | 48 | 1 (2.1) | 47 (97.9) | |
| 8 | 41 | 6 (14.6) | 35 (85.4) | |
| 9 | 31 | 6 (19.4) | 25 (80.6) | |
| 10 | 37 | 6 (16.2) | 31 (83.8) | |
| 11 | 27 | 3 (11.1) | 24 (88.9) | |
| 12 | 4 | 3 (75.0) | 1 (25.0) | |
| Gender | ||||
| Male | 119 | 21 (17.6) | 98 (82.4) | 8.035, P=0.005 |
| Female | 109 | 6 (5.5) | 103 (94.5) |
ADHD=Attention deficit hyperactivity disorder
Inattention was the most prevalent subtype of ADHD and it was observed highest in the 8–9 years’ age group [Table 2]. Only one hyperactive child was found, who was in the age group of 6–7 years. Combined subtype was the second common type, with maximum occurrence in the older age group, i.e., 10–12 years. The proportion of inattentive type of ADHD was highest among all subtypes of ADHD in both genders, followed by combined subtype. Only one male student was screened positive for hyperactivity/impulsivity.
Table 2.
Distribution of attention deficit hyperactivity disorder subtypes within age group and gender
| ADHD subtype | Inattention (n=18) | Hyperactivity/impulsivity (n=1) | Combined subtype (n=8) |
|---|---|---|---|
| Age group (years) | |||
| 6-7 | 2 (11.1) | 1 (100.0) | 0 |
| 8-9 | 9 (50.0) | 0 | 3 (37.5) |
| 10-12 | 7 (38.9) | 0 | 5 (62.5) |
| Gender | |||
| Male | 13 (72.2) | 1 (100.0) | 7 (87.5) |
| Female | 5 (27.8) | 0 | 1 (12.5) |
Figures in parentheses are percentages. ADHD=Attention deficit hyperactivity disorder
More than half of the students with ADHD were having significant learning difficulties at various levels [Table 3]. About two-third of the ADHD students were found to be having problems with assignment completion and organizational skills and problematic relationships with peers and were disrupting classes (classroom behavior). All these behaviors were found to be significantly more in ADHD students as compared to their neurotypical peers.
Table 3.
Attention deficit hyperactivity disorder and learning difficulties
| Learning difficulties | ADHD (n=27) | Non-ADHD (n=201) | Total (n=228) | χ2, P* | OR (unadjusted) | CI |
|---|---|---|---|---|---|---|
| Difficulty in reading | 17 (63.0) | 20 (10.0) | 37 (16.2) | 49.21, <0.001 | 15.385 | 6.209-38.123 |
| Difficulty in writing | 16 (59.3) | 32 (15.9) | 48 (21.1) | 26.89, <0.001 | 7.682 | 3.265-18.074 |
| Difficulty in mathematics | 16 (59.3) | 21 (10.4) | 37 (16.2) | 41.72, <0.001 | 12.486 | 5.116-30.385 |
| Poor academic performance | 16 (59.3) | 20 (10.0) | 36 (15.8) | 45.53, <0.001 | 13.164 | 5.374-37.244 |
| Problematic classroom behavior | 18 (66.7) | 45 (22.4) | 63 (27.6) | 23.39, <0.001 | 6.933 | 2.916-16.486 |
Figures in parentheses are percentages. *Fisher’s exact test applied where necessary. ADHD=Attention deficit hyperactivity disorder, OR=Odds ratio, CI=Confidence interval
Discussion
Based on teacher's scoring of VADRS (VADTRS), the prevalence of ADHD was found to be 11.8%. Our finding hits the higher border of the global prevalence of 4%–12%.[11] Venkata and Panicker[12] from Coimbatore reported similar prevalence, though lower prevalence was reported in different surveys from India.[13,14,15] Our findings are comparable to a survey conducted in the US in 2016, where the researchers reported that 9.4% of US children aged 2–17 years were diagnosed with ADHD.[16] Hebrani et al.[17] and Mostafaee et al.[18] reported similar findings from Iran, however, higher prevalence, i.e., 16.4%, was reported from Saudi Arabia in 2015.
When parent scoring (VADPRS) was also considered along with teacher scoring (VADTRS), the prevalence fell drastically to 1.75%. Ramya, Gautham, and Pandit also reported the prevalence of ADHD as low as 1.3% in school-going children in 2017 using the Conners’ Teacher Rating Scale.[13] In yet another study conducted in urban school children in Bangalore, 2.3% of children were diagnosed to have ADHD.[14] Lower prevalence of ADHD in school-age children has been reported all over the world. A systematic analysis of 102 studies conducted in different regions of the world had shown the prevalence rate of ADHD to be about 5.29% in children.[19] Similarly, prevalence of 6.4% of ADHD was reported in children from an urban school of New Delhi by Yewatkar D V.[15] This difference in prevalence of ADHD in different regions could be due to different methodologies; environmental, social, and cultural differences; and variability in identification and diagnostic guideline tools/instruments employed in studies.
The prevalence of ADHD was found to be higher in age groups of 8, 9, and 10 years, which is consistent with the findings of Venkata and Panicker, who reported the highest prevalence of ADHD in the children aged 9 and 10 years in their study.[12]
The present study reports that the prevalence of ADHD was significantly more in male students (17.6%) as compared to female students (5.5%). Many authors[20,21,22] have reported similar findings, and ADHD has been reported to be 3–5 times more common in boys than in girls. The reason for this could be the fact that ADHD in girls is usually of inattention type and therefore less easily identified due to subdued symptoms. The male-female ratio of ADHD, in our study, was found to be 3.5:1, quite similar to many other studies identifying a higher occurrence of ADHD in male gender with the ratios ranging from 10:1 in referred sample in clinics to 3:1 in a community-based survey.[12,23]
It was seen that more than half of the students with ADHD were having clear-cut learning difficulties at various levels. All these behaviors were found to be significantly more in ADHD students as compared to their neurotypical peers. This is in agreement with the fact that there is a degree of functional impairment present in children suffering from ADHD. Ramya, Gautham, and Pandit also reported that ADHD was associated with poor school performance in 24.4% of the subjects.[13] It was reported earlier in 2007 that children showing symptoms of inattention, hyperactivity, and impulsivity with or without formal diagnoses of ADHD also show poor scholastic outcomes.[24]
Limitation and recommendation
The main limitation of the study was the short time period; due to this, only one primary school could be covered for the study, thus the sample size was small.
Based on the findings of this study, it can be said that many students having learning difficulties might be having ADHD. These children are considered to be normal by the parents but are scolded by their teachers due to poor academic performance as well as due to their disruptive behavior in the class. Primary school teachers, if made aware and empowered, are able to identify children with attention or hyperactivity problems at a younger age group. A universal school-based screening program for ADHD can help in identifying and referring these children at an early point leading to minimization of the negative outcomes in these children.
Conclusion
ADHD is a neurobiological problem characterized by behavioral difficulties that can interfere with child's daily life, causing trouble at school and home. The prevalence of ADHD among surveyed primary school children was found to be 11.8% based on teachers’ scoring. More than half of the students with ADHD were found to be having learning difficulties at various levels. ADHD, if not addressed appropriately in time, can inhibit, or slow the normal social, emotional, and academic progress of the child.
Consent
Consent was obtained from the parents/guardians of the students.
Ethical clearance
Ethical clearance was taken from IEC.
Financial support and sponsorship
This study was financially supported by the ICMR under STS program.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment and ethical moral code
The authors are thankful to ICMR for approving and funding this study under STS. We want to thank the SRH University, Dehradun, to allow us to conduct this research. We are also grateful to the teachers at the school that we surveyed, as well as the parents of the students who participated in this study.
References
- 1.Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345–65. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- 2.Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics. 2012;9:490–9. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barry TD, Sturner RA, Seymour K, Howard BH, McGoron L, Bergmann P, et al. School-based screening to identify children at risk for attention-deficit/hyperactivity disorder: Barriers and implications. Child Health Care. 2016;45:241–65. doi: 10.1080/02739615.2014.948160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein JN, Loren RE. Changes in the definition of ADHD in DSM-5: Subtle but important. Neuropsychiatry (London) 2013;3:455–8. doi: 10.2217/npy.13.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gizer IR, Ficks C, Waldman ID. Candidate gene studies of ADHD: A meta-analytic review. Hum Genet. 2009;126:51–90. doi: 10.1007/s00439-009-0694-x. [DOI] [PubMed] [Google Scholar]
- 6.Curatolo P, D’Agati E, Moavero R. The neurobiological basis of ADHD. Ital J Pediatr. 2010;36:79. doi: 10.1186/1824-7288-36-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amiri S, Malek A, Sadegfard M, Abdi S. Pregnancy-related maternal risk factors of attention-deficit hyperactivity disorder: A case-control study. ISRN Pediatr. 2012;2012:458064. doi: 10.5402/2012/458064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galéra C, Pingault JB, Michel G, Bouvard MP, Melchior M, Falissard B, et al. Clinical and social factors associated with attention-deficit hyperactivity disorder medication use: Population-based longitudinal study. [Last accessed on 2019 Oct 26];Br J Psychiatry. 2014 205:291–7. doi: 10.1192/bjp.bp.113.141952. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25104834 . [DOI] [PubMed] [Google Scholar]
- 9.Feiz P, Emamipour S. A survey on prevalence rate of attention-deficit hyperactivity disorder among elementary school students (6-7 years old) in Tehran. Procedia-Soc Behav Sci. 2013;84:1732–5. [doi: 10.1016/j.sbspro. 2013.07.022] [Google Scholar]
- 10. [Last accessed on 2019 Oct 26]. Available from: https://www.nichq.org/sites/default/files/resource-file/NICHQ_Vanderbilt_Assessment_Scales.pdf .
- 11.Brown RT, Freeman WS, Perrin JM, Stein MT, Amler RW, Feldman HM, et al. Prevalence and assessment of attention-deficit/hyperactivity disorder in primary care settings. Pediatrics. 2001;107:E43. doi: 10.1542/peds.107.3.e43. [DOI] [PubMed] [Google Scholar]
- 12.Venkata JA, Panicker AS. Prevalence of attention deficit hyperactivity disorder in primary school children. Indian J Psychiatry. 2013;55:338–42. doi: 10.4103/0019-5545.120544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hs R, As G, Pandit LV. Prevalence of attention deficit hyperactivity disorder in school going children aged between 5-12 years in Bengaluru. Curr Pediatr Res. 2017;21:321–6. [Google Scholar]
- 14.Mannapur R, Munirathnam G, Hyarada M, Saranappa S, Bylagoudar S. Prevalence of attention deficit hyperactivity disorder among urban school children. Int J Contemp Pediatr. 2016;3:240–2. [Google Scholar]
- 15.Yewatkar DV, Pande DP, Bangde LA, Joshi T. Prevalence of attention deficit hyperactivity disorder in an urban school of a developing country. Int J Res Med Sci. 2015;3:3759–62. [Google Scholar]
- 16.Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment Among U.S. children and adolescents, 2016. J Clin Child Adolesc Psychol. 2018;47:199–212. doi: 10.1080/15374416.2017.1417860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hebrani P, Abdolahian E, Behdani F, Vosoogh I, Javanbakht A. The prevalence of attention deficit hyperactivity disorder in preschool-age children in Mashhad, north-East of Iran. [Last accessed on 2019 Oct 26];Arch Iran Med. 2007 10:147–51. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17367214 . [PubMed] [Google Scholar]
- 18.Hamidzadeh A, Kharatha M, Bazghaleh M, Basirinejad H, Aghdam NF, Ebrahimi H. The prevalence of attention-deficit hyperactivity disorder and its related risk factors among children at elementary school in Shahroud. J Educ Health Promot. 2021;10:341. doi: 10.4103/jehp.jehp_46_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–8. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 20.Ramtekkar UP, Reiersen AM, Todorov AA, Todd RD. Sex and age differences in attention-deficit/hyperactivity disorder symptoms and diagnoses: Implications for DSM-V and ICD-11. J Am Acad Child Adolesc Psychiatry. 2010;49:217–28.e1. [PMC free article] [PubMed] [Google Scholar]
- 21.Vadsaria K, Jabbar A, Azam I, Rizvi S, Haider G, Naqvi H. Coping Styles and Depression among Patients with Solid Organ Cancers Attending Two Tertiary Care Hospitals of Karachi: A Cross Sectional Study. Open Journal of Epidemiology. 2017;7:69–83. [Google Scholar]
- 22.Willcutt EG. The prevalence of DSM-IV ADHD: A meta-analytic review. [Last accessed on 2019 Oct 26];Neurotherapeutics. 2012 9:490–9. doi: 10.1007/s13311-012-0135-8. Available from: http://link.springer.com/article/100.1007/s13311-012-0135-8/fulltext.html . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biederman J, Mick E, Faraone SV, Braaten E, Doyle A, Spencer T, et al. Influence of gender on attention deficit hyperactivity disorder in. Am J Psychiatry. 2002;159:36–42. doi: 10.1176/appi.ajp.159.1.36. [DOI] [PubMed] [Google Scholar]
- 24.Loe IM, Feldman HM. Academic and educational outcomes of children with ADHD. J Pediatric Psychol. 2007;32:643–54. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]


