Abstract
Background
It requires thoughtful planning and work to successfully apply and sustain research-supported interventions like healthcare treatments, social support, or preventive programs in practice. Implementation support practitioners (ISPs) such as facilitators, technical assistance providers, knowledge brokers, coaches or consultants may be involved to actively support the implementation process. This article presents knowledge and attitudes ISPs bring to their work.
Methods
Building on a previously developed program logic, a systematic integrative review was conducted. Literature was sourced by searching nine electronic data bases, organizational websites, and by launching a call for publications among selected experts and social media. Article screening was performed independently by two researchers, and data from included studies were extracted by members of the research team and quality-assured by the lead researcher. The quality of included RCTs was assessed based on a framework by Hodder and colleagues. Thematic Analysis was used to capture information on knowledge and attitudes of ISPs across the included studies. Euler diagrams and heatmaps were used to present the results.
Results
Results are based on 79 included studies. ISPs reportedly displayed knowledge about the clinical practice they work with, implementation / improvement practice, the local context, supporting change processes, and facilitating evidence-based practice in general. In particular, knowledge about the intervention to be implemented and its target population, specific improvement / implementation methods and approaches, organizational structures and sensitivities, training, and characteristics of (good) research was described in the literature. Seven themes describing ISPs’ attitudes were identified: 1) professional, 2) motivated / motivating / encouraging / empowering, 3) empathetic / respectful / sensitive, 4) collaborative / inclusive, 5) authentic, 6) creative / flexible / innovative / adaptive, and 7) frank / direct / honest. Pertaining to a professional attitude, being responsive and focused were the most prevalent indicators across included publications.
Conclusion
The wide range and complexity of knowledge and attitudes found in the literature calls for a comprehensive and systematic approach to collaboratively develop a professional role for ISPs across disciplines. Embedding the ISP role in different health and social welfare settings will enhance implementation capacities considerably.
Introduction
Organizational efforts supporting the implementation of research-supported interventions (RSIs) are required to bring about change effectively. Be it (health) care treatments, social support, or preventive programs—implementing RSIs often requires work at multiple levels of a system to successfully apply and sustain these complex interventions in practice [1, 2]. Implementation usually involves various parties, such as organizations, health professionals, and care recipients, and collaboration between them [3]. Thus, the implementation of RSIs is not a fast-selling item, but requires thoughtful planning, coordination and an acquisition and allocation of resources supportive to the implementation process. Such a process can be time-intensive, even more so when the goal is to implement the new RSI in a sustainable fashion [4].
Implementation support activities aim to facilitate implementation processes. While facilitation can be operationalized in numerous ways, one possibility is to provide active implementation support in the form of human resources. As opposed to either letting implementation happen or helping it happen, Greenhalgh and colleagues suggest to ‘make it happen’ by installing active expert support roles [5]. In the current literature, implementation support roles are often operationalized and described in the form of e.g., facilitators, technical assistance providers, knowledge brokers, coaches, or consultants. Albers et al. worked towards providing a more unified approach to understanding implementation support roles and conceptualize the people fulfilling those roles as Implementation Support Practitioners [6].
Implementation Support Practitioners (ISPs) have been defined as professionals supporting the implementation of RSIs, programs and/or policies and their sustainability in practice, by working together with stakeholders to effectively deliver such practices. ISPs can be located internally or externally to an implementing organization. They can also be part of an intermediary or purveyor organization, which are established with the aim to disseminate information about and provide assistance for the adoption of an intervention [7]. Their main goal is to build implementation capacities within the individuals and organizations they support. Implementation capacities are defined as the knowledge, skills and attitudes needed to implement innovation. Acquiring implementation capacities enables an organization to, for example, select contextually appropriate implementation frameworks, strategies or tools and apply these to different scenarios in real world health services [6].
In order to understand how ISPs can support the implementation of change in practice, Albers, Metz, and Burke developed a preliminary logic for ISPs [6]. This logic describes that the implementation intervention (the ISP role) is operating through a mechanism of change, namely an interplay between resources (position, professional background, skills, knowledge, attitudes) and reasoning (the evoked response in the stakeholders), to generate an output (implementation capacities) which finally results in an outcome (implementation outcome, i.e., successful implementation). Whether resources can unfold, and reasoning occurs depends on the interplay between the context in which the implementation process is embedded and the active contribution of the ISP.
There have been previous efforts to describe the competencies that are required to succeed in providing active implementation support [8, 9]. However, these studies typically examine distinct ISP roles (e.g., knowledge broker or facilitators) rather than showing an overarching picture of active implementation support role competencies. A key premise of the work presented in this article has been to integrate the knowledge of competencies across comparable implementation support roles to build a shared knowledge base. Based on this premise, this work aimed to identify what (a) knowledge and (b) attitudes the literature describes as being present in ISPs and influencing their work.
Concepts under study
Knowledge and attitudes are closely related concepts that have a central role in implementation science and practice as determinants of individual and organizational behavior. For example, attitudes are a key component of the theory of planned behavior [10], commonly used to examine implementation in health and human services [11, 12], and have shown to predict outcomes, e.g., research utilization among nurses [13]. Considerable efforts have been made to enable attitude measurement in implementation science in order to better understand its contribution to implementation processes [14–16]. Knowledge on the other hand is a central construct in determinant frameworks–such as the Consolidated Framework for Implementation Research [17]–and has been highlighted in numerous studies as a persistent barrier to evidence uptake and implementation including healthcare [18, 19], social welfare [20, 21] and education [22]. It is therefore relevant to also consider the role of these two constructs for the work of ISPs. In the following, they are described and defined in light of this role.
Knowledge
In the context of implementation support, knowledge is defined as “the factual information ISPs bring to and acquire about the contexts in which they work” (p. 5) [6]. A comprehensive knowledge base—for example, knowledge about the intervention, program, or policy to be implemented; implementation concepts; or certain organizational structures—is an indispensable requisite for ISPs. Knowledge can be used as an instrument for change, and also defines individuals as influential and as experts [23]. It therefore can be seen as an active resource the ISP can draw upon and simultaneously as a passive requirement to shape stakeholders’ perception of an ISP’s credibility. A literature review on concepts in knowledge transfer highlights that opinion leaders need to be perceived as knowledgeable by their stakeholders and willing to share their knowledge with them [23].
Although current literature highlights the importance of a knowledge base for ISPs’ work [9, 24, 25], in-depth research on a detailed conceptualization of ISPs’ knowledge is yet limited. Among the few studies exploring the role of knowledge for implementation facilitation is a realist review published by McCormack and colleagues [26]. It suggests that the combination of academic and local knowledge and practical experience in change agents is important for successful knowledge translation [26]. Moreover, the above-mentioned literature review describes that knowledge of opinion leaders is often product- and situation-specific [23].
Attitudes
According to social psychology, attitudes are "a relatively enduring organization of beliefs, feelings, and behavioral tendencies towards socially significant objects, groups, events or symbols" (p. 150) [27]. These tendencies are expressed “by evaluating a particular entity with some degree of favor or disfavor” (p. 1) [28]. Hence, ISPs’ attitudes can be defined as the cognitive predispositions that influence their implementation support-related activities and decisions [6, 29]. In the literature, multiple attitudes have been assigned to facilitators, including the willingness to think innovatively and positively and be curious and open to suggestions [9, 30, 31]. A generally positive attitude of change agents affecting knowledge utilization is highlighted in a realist review of interventions to promote evidence-informed healthcare [26]. In a scoping review of facilitation roles (p. 6) [25], champions were described as “driven” [32] and “passionate about their work” [33], and characterized by an overall belief in the necessity of the change to be implemented [34, 35]. Similarly, Metz et al. [29] describe commitment as a core principle among ISPs, which may include patience, resilience, and the willingness to challenge the current status quo.
Aim
This research is part of an ongoing international collaborative program of work on implementation support practice and practitioners involving the National Implementation Research Network (NIRN), University of North Carolina, the European Implementation Collaborative (EIC) and the Centre for Effective Services (Ireland). This collaboration involved the conduct of a systematic integrative review of studies reporting on multiple aspects of the work of ISPs, including ISP skills [36] and the mechanisms of change that may explain how ISP efforts generate change in others [37]. The present article reports on ISP knowledge and attitudes.
The aim of this third and final part of the review was to describe both the knowledge base and the mindset ISPs utilize in their work, thereby complementing existing work in this field based on an accumulated definition of the role of an ISP (as opposed to separate roles) and addressing the distinct features of ISP knowledge and attitudes (as opposed to characteristics in general). Together, all findings of this review will help to refine the previously developed ISP program logic [6] and contribute to theory building in the field of implementation science and practice.
Methods
A systematic integrative review method was applied to consolidate findings on ISP knowledge and attitudes from a diverse body of literature. The overarching review was conducted in five stages [38]: 1) problem identification, 2) literature search, 3) data evaluation, 4) data analysis, and 5) data presentation. These five stages are outlined below, with the focus on the study of knowledge and attitudes of ISPs. A detailed description of the overall methods used to conduct the review is provided in Albers et al. [36] and in the respective electronic results addendum (S1 Appendix, pp. 1–2) [39]. The review was conducted by a team of five researchers with expertise in systematic literature reviews (BA and CV), content expertise related to social work (BA and LBa), health services (CV, PD, and LB), and education (BA).
Our methodology and findings are reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA and PRISMA-S) guidelines and checklists (S2 Appendix) [40]. As the corresponding review materials have already been made public via Open Science Framework [39] it is not registered elsewhere.
Problem identification
Discussions in the research team based on a preliminary ISP program logic developed by Albers et al. [6] resulted in the agreement that the current understanding of which knowledge is required, and which attitudes are beneficial for the work of ISPs is limited (question under study).
Literature search
To achieve a representative collection of literature about the question under study, five search strategies were used to identify relevant publications: 1) systematic search of nine electronic data bases (ASSIA, CINAHL, Criminal Justice Abstracts, ERIC, Family and Society Studies Worldwide, Medline, PsycInfo, Scopus and SocIndex), 2) search of organizational websites, 3) call for publications among selected experts, 4) open call for publications through social media (i.e. Twitter, LinkedIn), and 5) reference check for all included studies. Searches were conducted between February and April 2019. The search string for the systematic search of the electronic data bases as well as the detailed inclusion and exclusion criteria applied are described in S1 Appendix (pp. 1–4) and in Table 1, respectively.
Table 1. Overview of inclusion and exclusion criteria.
| Included | Excluded | |
|---|---|---|
| Study designs | Any primary study design, including, e.g.: • Randomized, controlled studies • Quasi-experimental studies • Pre-post evaluations • Case studies |
• Systematic reviews of any study designs • Theoretical / conceptual studies • Expert commentary • Opinion pieces • Conference proceedings • Books / book chapters • Editorials • Other publications that are / report “non-studies” • Dissertations / theses |
| Population | • The target population(s) of the study are implementation specialists. | • The target population(s) of the study are current or future implementation researchers or other non-ISPs. |
| Sectors | • Health care (including mental health) • Social care / social welfare (including child welfare, aged care, labor market services, crime and justice, family services etc.) • Education (including ECE, primary, secondary and high school services) |
• IT • Environmental services • Any other service sector not listed in the left column. |
| Content | • The study focuses on supporting the implementation of a research-supported program, practice or policy AND • the study involves a person or a team or an intermediary organization providing implementation support to others AND • the study provides information about / conceptualizes / assesses implementation know how / skills / capacity • Examples of interventions that could be of relevance: • Implementation training • Implementation coaching • Technical assistance • Implementation coaching • Implementation facilitation • Implementation policies • Implementation mentorship |
• Studies focused on the specific knowledge, skills, capacities required to implement e.g. specific clinical interventions • Studies focused on factors that support successful practice-science / community-university partnerships • Studies focused on online solutions only (repositories providing electronic implementation resources and nothing else) |
| Geography | • High income countries • Low / middle income countries |
No exclusion based on geography |
| Languages | • English • German • Danish • Swedish • Norwegian |
Any other language not listed |
| Publication date | No limitations | No limitations |
Data evaluation
The researchers double-screened the titles, abstracts, and full-texts independently using the platform Covidence. Conflicts were solved by a third member of the team. Data was extracted from the included studies by using a standardized data extraction form consisting of 19 items (i.e., study design and aim, method, geography, sector, setting, sampling strategy, sample size, clinical intervention, ISP information, outputs, and outcomes). Data from each included study was extracted by one research team member. The quality of the data extraction was assured by the lead author.
The quality assessment of included studies was focused on randomized controlled trials only. This decision was taken by the research team considering the purpose and character of this review. Based on a framework by Hodder et al. [41] all included RCTs were quality assessed regarding consistency in terminology use, integration of theory, and consideration of benefits and harms of implementation interventions. The quality assessment tool as well as the results are included in the S1 Appendix (pp. 20–22).
Data analysis
For the analysis of key information about ISPs, included studies were uploaded to the online qualitative data analysis platform dedoose [42]. While the data analysis included a wide range of information about ISPs, this article reports on the data focused on knowledge and attitudes only. Thematic Analysis [43–45] was used to capture patterns and themes across all textual data describing knowledge and attitudes of ISPs. Thematic Analysis followed six steps: (1) data familiarization; (2) systematic data coding; (3) theme development; (4) review; (5) consolidation; and (6) reporting. Each included study was reviewed as part of the systematic coding, a process that occurred in two rounds. After an initial familiarization with the data (1), open, inductive coding (2) was used to identify all textual information describing particular knowledge or attitudes that ISPs use in their work. The focus was on the semantic level of texts, i.e., the direct linguistic meaning of words. Brief instructions, outlining what to pay attention to when reviewing texts and providing examples of different types of knowledge and attitudes, functioned as a guide for this step. Text excerpts for both categories were exported from dedoose, resulting in two separate spreadsheets, including all information on ISP knowledge and on ISP attitudes. The spreadsheets were reviewed separately to quality assure all coding and highlight key content for each excerpt. The second round of coding–data comparison–involved further inductive coding at the conceptual level of text information moving beyond the purely linguistic meaning of words and instead identifying broader themes (3) present in the literature. All text excerpts were reviewed in detail (4), preliminary ideas for themes were identified and refined through constant comparison with other text excerpts belonging to the same category and theme. This process resulted in distinct categories of types of knowledge and attitudes of ISPs and their detailed operationalization (5). The results were synthesized narratively and are reported in the following (6).
Data presentation and exploration
The results of the data analysis are summarized in the present article including several visualizations (i.e., Euler diagrams and heatmaps). Euler diagrams are a graphical depiction of relationships between sets or groups, where circles represent distinct sets and their overlap illustrates a relationship between those sets [46]. The diagrams were developed based on the total amount of studies reporting a distinct category of knowledge or attitudes (size of circles) and the total amount of studies reporting on two or more distinct categories of knowledge or attitudes (overlap between circles). Heatmaps were developed by comparing the number of included studies reporting on the position (i.e., internal, external, internal-external, research) of ISPs with the number of included studies reporting on certain types of knowledge and attitudes.
Results
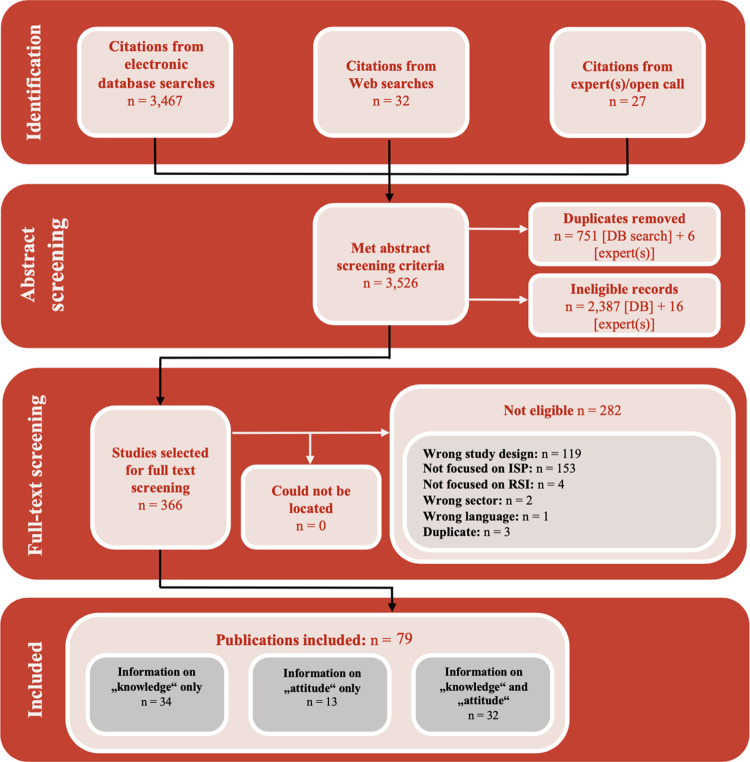
The integrative review identified 79 studies which reported on knowledge and/or attitudes of ISPs [47–125]. Fig 1 shows the flow of studies through the review process. S3 Appendix provides an overview of the main study characteristics of the included studies as well as an indication of the degree to which the included studies reported on information about ISP’s knowledge or attitudes or both.
Fig 1. Flow of studies through the review process.
What background do ISPs have?
School teachers, social workers, psychologists, psychiatrists, nurses, physicians, dietitians, occupational therapists, physiotherapists, epidemiologists, and pharmacists were the most dominant education descriptors across ISPs. Less specific markers used to describe this specialist status were “clinically trained” [69], “clinical practitioners” [94] or with “clinical expertise” [120]. Generalists with an educational background in, for example, anthropology, political science, or organizational change were rarely used as ISPs. Only seven studies described e.g., “non-clinicians with an interest in knowledge transfer” (p. 2) [120] or individuals with project or data management background [100] as involved in implementation support, and in these cases, they were part of a set up that also included clinical specialists.
ISPs were generally described as experienced as they had worked in their profession for some time. While few studies detailed this experience in years, those that did, portrayed ISPs as having a minimum of three years’ experience of working in the field in which they provided implementation support [63, 101, 119], oftentimes exceeding even 10 years of experience [77, 99, 101, 116, 119].
What knowledge do ISPs display?
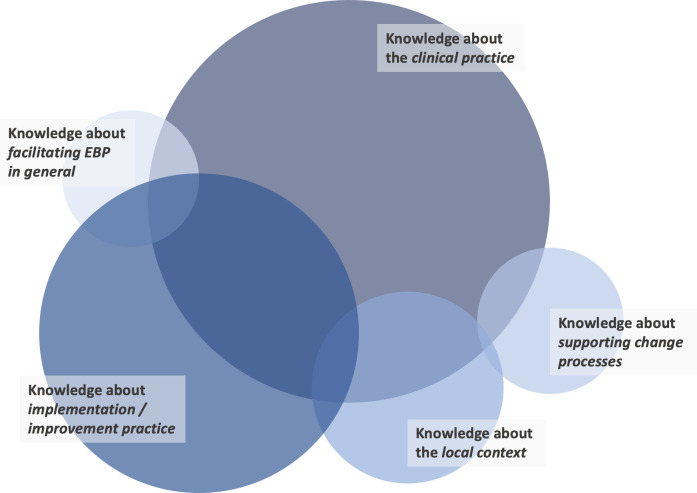
Sixty-six papers reported on ISP knowledge use. Across these publications, five types of knowledge were identified, including ISPs’ knowledge about 1) the clinical practice, 2) implementation / improvement practice, 3) the local context, 4) supporting change processes, and 5) facilitating evidence-based practice (EBP) in general. Fig 2 visualizes these findings. Each of the five themes consists of several sub-themes which are reported in the following to convey rich detail on the types of knowledge that ISPs rely on as part of their work. A comprehensive overview of the types of knowledge that were described in included publications, together with a reference to the article in which these descriptions appeared, is provided in S4 Appendix.
Fig 2. The five most present types of knowledge of ISPs in the included articles.
The size of the circle indicates the number of studies which reported the specific knowledge area: knowledge about the clinical practice (n = 49), knowledge about implementation / improvement practice (n = 39), knowledge about the local context (n = 24), knowledge about supporting change processes (n = 20), knowledge about facilitating evidence-based practice (EBP) in general (n = 16). Publications were included in this visualization when they reported on at least one type of knowledge. The overlap between circles shows the co-presence of knowledge areas.
Knowledge about clinical practice
Of 49 publications providing information on knowledge about clinical practice, 36 highlighted that ISPs use knowledge about the intervention to be implemented and its target population. Knowledge about the broader research in the clinical area in which ISPs operated was described in 20 publications, e.g., by presenting ISPs as providing “information such as articles, standardized assessments of participation and other evidence-based materials” (p. 443) and facilitating the integration of this research evidence into learning processes [48].
Knowledge about implementation / improvement practices
Information about ISPs’ use of implementation and/or improvement practice knowledge could be extracted from 39 publications. Fourteen of these suggest a need for ISPs to be familiar with specific implementation/improvement approaches, such as walk-through exercises, flow charting, nominal group technique, Plan-Do-Study-Act cycles, and process mapping. Further types of knowledge referred to in four publications each were knowledge about the principles of high-quality implementation and facilitation and about one’s own role as ISP. The latter was especially notable in studies of knowledge brokers, which emphasized the necessity of ISPs understanding “the purpose of their activities in promoting knowledge and use of the tools” (p. 1583) [116], “the primary functions of their role” (p. 61) [107], or their “roles and responsibilities” (p. 5) [77]. This “understanding of own role” information was not included in studies of other ISP roles.
Knowledge about the local context
Being knowledgeable of the local context for an implementation effort emerged as another type of knowledge described as central to the work of ISPs across 24 publications. Most prominent was knowledge about organizational structures and sensitivities discussed in nine publications, as well as about local conditions mentioned in six publications. Both refer to knowing the facilities, staff and the physical environment in which implementation support is provided, and to being familiar with existing hierarchies, work cultures, workflows, policies and values [109, 115, 121, 125]. The latter is also described as “organizational structure and climate” by Saldana and Chamberlain [78].
Knowledge about supporting change processes
Further 20 studies described ISPs as using knowledge about change processes and supporting these. Five described ISPs as being knowledgeable about how to train and educate others. Training provided by ISPs focused on e.g., “the importance of program fidelity; group facilitation skills, marketing and recruiting techniques; and the participant consent and evaluation data collection processes” (p. 1009) [75]. Knowing how to effectively communicate and how to lead or facilitate groups including participation in group processes, decision-making, and conflict resolution was mentioned by three publications respectively.
Knowledge about facilitating EBP in general
Information on facilitating EBP in general were provided by 16 publications. EBP is defined as the process of “integrating individual practice expertise with the best available external evidence from systematic research as well as considering the values and expectations of clients” (p. 289) [126]. In this context, RSIs are considered the best available external evidence. While five articles presented knowledge about characteristics of quality research, knowledge about the key principles of EBP, knowledge translation, together with general principles of high-quality practice and strategies for sourcing evidence were mentioned by three publications respectively. For instance, Aasekjær et al. [94] describe a post-professional program that taught the different steps in EBP, based on which ISPs reported to have gained “insight into the use of research in healthcare decision making” (p. 6) and an understanding of how “to acquire practical means by which they could further improve clinical practice” (p. 6).
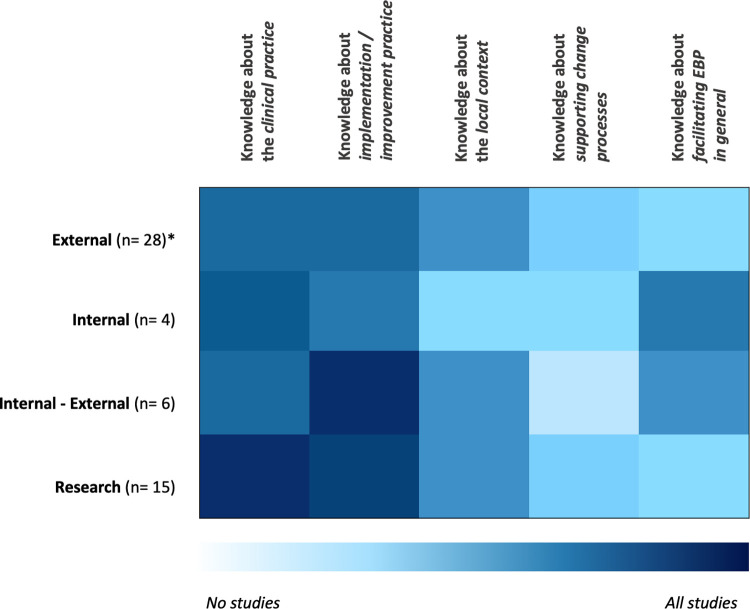
Does the knowledge of ISPs differ according to their position?
ISPs can occupy different positions when providing implementation support. They may be part of the implementing organization and/or team (internal), or they may be external providers of implementation support, belonging to a different organization than those supported. In some studies, implementation support was provided through groups of ISPs, some of which were located internally while others were externally recruited. Furthermore, multiple studies included ISPs belonging to a research organization providing implementation support as part of a research study. Different locations might influence the competencies the ISP needs to work effectively. Fig 3 visualizes the relationship between types of knowledge and positions of the ISP in terms of their co-occurrence in the included studies. A darker blue field indicates that a certain type of knowledge was predominantly reported in publications reporting on a certain position of the ISP in the implementation process. Knowledge about the clinical practice and about implementation/improvement practices was reported across studies describing all different ISPs positions (internal, external, internal-external to the organization, or in research), with a slight emphasis on clinical practice knowledge for ISPs located in research and implementation/improvement practice knowledge for ISPs positioned internally-externally. Knowledge about facilitating EBP was most prominent in publications focused on ISPs with an internal position. Studies on externally positioned ISPs and those connected to research teams reported knowledge about clinical practice, implementation/improvement practice and the local context (first three domains in Fig 3) more often than knowledge about the facilitation of EBP and change processes (last two domains in Fig 3).
Fig 3. The five most present types of knowledge of ISPs in the included articles according to distinct position.
*n = number of reported studies; positions were included with a minimum of n = 4 reported studies.
What attitudes do ISPs display?
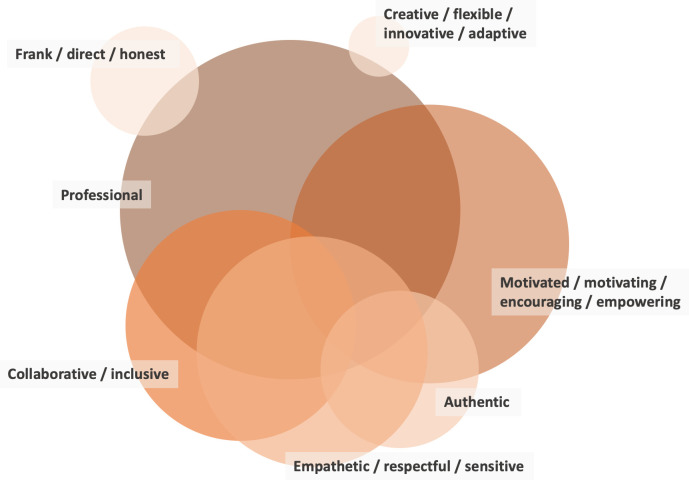
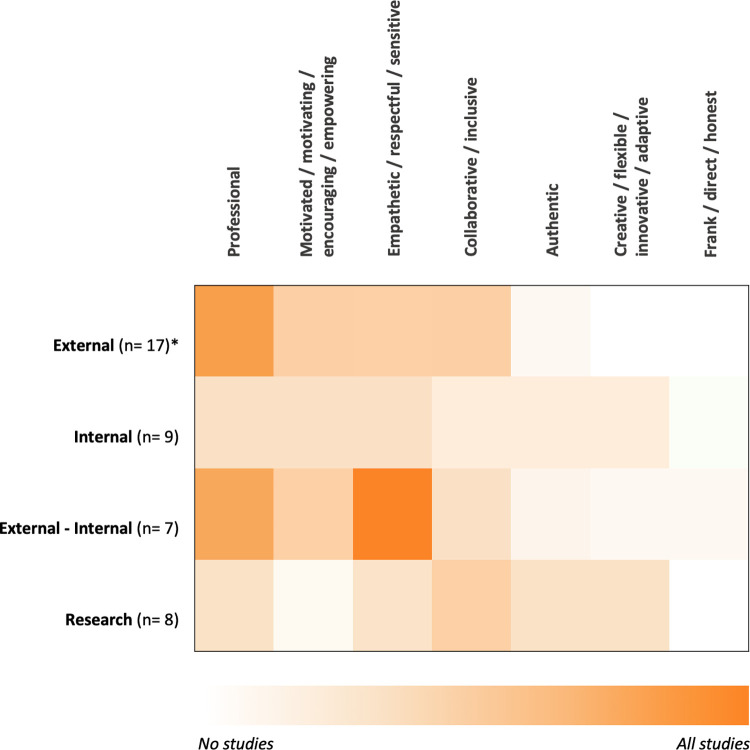
One hundred and forty-six text excerpts about ISP attitudes described as influential to their work could be extracted from 45 publications. Across these, seven broad categories of attitudes emerged: 1) professional, 2) motivated / motivating / encouraging / empowering, 3) empathetic / respectful / sensitive, 4) collaborative / inclusive, 5) authentic, 6) creative / flexible / innovative / adaptive, 7) frank / direct / honest. Fig 4 visualizes those seven most present types of ISP attitudes. A comprehensive overview of the types of attitudes that were described in included publications, together with a reference to the article in which these descriptions appeared, is provided in S5 Appendix.
Fig 4. The seven most present attitudes of ISPs in the included articles.
The size of the circles indicates the number of studies which reported the specific attitude: professional attitude (n = 28), motivated / motivating / encouraging / empowering attitude (n = 25), empathetic / respectful / sensitive attitude (n = 20), collaborative / inclusive attitude (n = 19), authentic attitude (n = 13), creative / flexible / innovative / adaptive attitude (n = 9), frank / direct / honest attitude (n = 5). Publications were included in this visualization when they reported on at least one type of attitudes. The overlap between circles shows the co-presences of attitudes as reported in the articles.
Professional
Twenty-eight publications described a professional attitude as central to ISPs’ work. Detailed descriptors of this professionality were an ability to stay focused, on e.g., the key focus population, stakeholders, or intentions behind an implementation initiative [122, 125], or to help maintain its momentum [113, 121]. It also implied for ISPs to be consistent, e.g., in their approach to promoting an intervention [103], and to be responsive, e.g., to the needs and sensitivities of stakeholders [82, 95, 99], including being accessible when called for [86, 91, 108]. Few studies discussed the importance of putting boundaries around this responsivity, ensuring, e.g., that ISPs only cover needs for which no local capacities exist [118]. Part of professionality was also to be perceived as credible [93], e.g., on the basis of clinical expertise [106], an understanding of the RSI in focus [91] or of the local context into which this RSI was implemented [119]. Studies of facilitators, knowledge brokers and intermediaries also highlighted resilience and persistence as necessary features of a professional attitude, described as a need to be “thick skinned” [101], standing up to “peers, over whom one does not have official power” (p. 1020) [113], and enduring a lack of support [121] or weeks of no visible progress or success [84].
Motivated / motivating / encouraging / empowering. A motivated / motivating / encouraging / empowering attitude of ISPs was described in 50 text excerpts from 25 studies. A consistent element described for this mindset was enthusiasm–for research in general [107], the RSI that ISPs supported in particular [99, 111], the broader project in which they were involved [100, 101, 113], and for their own role as ISP [106]. It was often this enthusiasm that was presented as a fuel for the encouraging mindset, one that could be shared with those supported [106] or even compensate for a lack of enthusiasm elsewhere in the organization [121]. Reflective of an encouraging ISP attitude was being appreciative of strengths and successes present in the implementation context [97, 100, 102, 110], providing constructive, motivating feedback and support [83, 87, 94, 106], validating and encouraging the work of implementers [108, 119, 123] and providing “the energy and direction to stay on track” (p. 422) [89]. As such, the encouraging attitude focuses on the positive.
Empathetic/Respectful/Sensitive
In 20 studies, ISPs were described as pursuing an empathetic / respectful / sensitive attitude, mirrored in a sensitivity toward the challenges and barriers faced by the stakeholders they assist. This implied recognizing the uniqueness of different implementation contexts [85], listening actively [90], being non-judgmental [119] and non-authoritative [92, 112] in their work, sometimes also providing emotional support [119], and meeting stakeholders at whatever developmental stage they were in regarding their change process [118].
Collaborative/Inclusive
A collaborative / inclusive attitude was reported as a central ISP characteristic in 19 studies. It represents a willingness to recognize and actively engage a broad diversity of individual or organizational stakeholders and their perspectives in the implementation support process. In studies, this willingness was described as “an interest in others” (p. 13) [85] displayed in inclusive efforts to involve stakeholders in the implementation and to listen to their perspectives with an open mind [94, 100, 101, 118]. It also showed in actively engaging with stakeholders [106], and in continuously building new relationships [117], thereby adding to the relational resource ISPs represented for their stakeholders [111, 125]. In the support of those most directly involved in an RSI implementation, pursuing a collaborative mindset could also show in ISP efforts to tone down one’s role as an expert and instead position oneself as a “partner” to those supported [119], for example, by continuously inviting stakeholders to provide input [100], to define the agenda for the support required [95], and to “share thoughts before the coach shares” (p. 33) [92]. Few studies discussed the potential tensions that might emerge from this collaborative attitude, for example for ISPs who also hold an evaluative role and monitor fidelity and other implementation performance data for those they support [95, 108].
Authentic
Further 13 studies described an authentic attitude to be important for ISPs, representing a state in which ISPs are prone to be real, true, or genuine in their work. Authenticity was described in primarily two ways, both of which were presented as also contributing to ISPs’ credibility among their stakeholders: 1) ISPs went into the field and supported stakeholders directly at the frontline of service delivery [96, 105, 119] or 2) ISPs embodied the knowledge and methods they taught others and used these directly in their implementation support techniques [85, 95, 108, 109, 113]. The former was described as a willingness and ability to support implementation directly in, e.g., classrooms or clinics through “hands on” support, demonstrating how an RSI can be applied in real practice. The latter was reported as ISPs’ willingness and ability to “walk the talk” by role-modelling the knowledge and techniques that they wanted others to use in their own coaching, consulting, or facilitation, for example, the principles of EBP or Motivational Interviewing. Other aspects of authenticity covered in studies were ISP self-awareness [121], willingness to give the implementation support provided “a personal touch” (p. 110) [115] and to genuinely empathize with stakeholders based on a true understanding of the realities of practice [123].
Creative/Flexible/Innovative/Adaptive
Nine studies included descriptions of a creative / flexible / innovative / adaptive attitude as a key characteristic of ISPs, referring to the ISP being flexible in their approach to supporting implementation processes and tailoring this approach to different stakeholders and contexts. This includes to accommodate the preferences and constraints that individuals, organizations and systems present as part of an implementation initiative [115]. In displaying flexibility, ISPs ensure making information and support relevant and useful to their stakeholders; they source, use and combine implementation resources as well as strategies in creative ways [88, 98], “think outside the box” (p. 135) [101], and remain curious [111, 116] throughout an implementation process. This curiosity was described as being supportive of their own learning, about new ISP techniques and tools, thereby further expanding their flexibility. None of the included studies discussed how ISPs manage potential tensions existing between a flexible attitude and the need to ensure that the implementation of RSIs adheres to specific quality criteria.
Frank/Direct/Honest
Five studies indicated ISPs to have a frank / direct / honest attitude, which refers to a certain straightforwardness when working with stakeholders involved in the implementation of RSIs. For instance, Akin et al. [81] presented authenticity and transparency as two important interrelated attitudes. Olson et al. [92] use the term “forthright” (p. 33) to describe a similar attitude, suggesting that ISPs should be direct when working with their stakeholders. Similarly, Waterman and colleagues highlight that “honesty, directness and focusing on what needed to be done were effective in helping staff to persist” (p. 9) [122].
Do the attitudes of ISPs differ according to their position?
Fig 5 shows that studies reporting on ISPs located internally-externally to the organization also report predominantly on an empathetic / respectful / sensitive attitude. A professional attitude is mostly reported in studies of ISPs who are located externally or internally-externally. No other attitude is particularly highlighted in relation to a specific position of the ISP.
Fig 5. The seven most present attitudes of ISPs in literature according to distinct position.
*n = number of reported studies; positions were included with a minimum of n = 4 reported studies.
Discussion
Based on a systematic, integrative review, distinct types of knowledge and attitudes were identified that ISPs reportedly use in their work. This includes five types of knowledge: knowledge about the clinical practice, implementation / improvement practice, the local context, supporting change processes, and facilitating EBP in general. Particularly salient was ISPs’ use of knowledge about the RSI to be supported in its implementation and its target population, specific improvement / implementation methods and approaches, organizational structures and sensitivities, training, and characteristics of (good) research. Seven distinct attitudes were identified that characterize ISPs: motivated / motivating / encouraging / empowering, empathetic / respectful / sensitive, collaborative / inclusive, authentic, creative / flexible / innovative / adaptive, and frank / direct / honest attitude. A professional attitude was the most reported, with being responsive and being focused as the most prevalent indicators across included publications. The order of mentioned attitudes represents the frequency with which they were reported in the literature. Attitudes were often identified in combination, meaning that single publications reported on several attitudes of ISPs at a time.
These findings are aligned with those from a previous review [25] describing that a broad range of facilitating roles depends on being highly knowledgeable in relation to their clinical area, context and the research relevant to their work. Similarly, understanding context, research processes, knowledge translation and dissemination, and EBP were highlighted as needed by ISPs in a scoping review of the literature on knowledge translation [9]. These two previous reviews also describe what this review understands as attitudes. Mallidou et al. [9] identified five key attitudes of knowledge translators including being confident, having trust, valuing research, being committed to self-directed lifelong learning, and valuing teamwork. Additionally, the authors found that knowledge translators were reported throughout the literature as being “pragmatic and flexible, positive, persuasive, entrepreneurial, proactive, enthusiastic, open-minded, autonomous, independent, self-sufficient and self-motivated, creative, and committed to principles of equity, inclusivity, respect and cultural competence” (p. 10) [9]. These latter characteristics were labelled personality traits and therefore listed separately from attitudes. Yet another label is used by Cranley et al. [25], who identified attributes as part of their review on different facilitating roles. These were being credible, trustworthy, enthusiastic, creative, passionate, empowering, encouraging, approachable, flexible and available, as well as being a driving force and motivating. A realist review of interventions and strategies to promote evidence-informed healthcare describes change agents as having a positive attitude, and as being credible, organized, accountable, reflective, and accessible [26]. Fewer but similar characteristics were identified in a review of the literature on technical assistance concluding that technical assistance providers need to be collaborative, strength-based (i.e., inspiring and reinforcing), and trustworthy [127]. A commonality of these findings is that they describe ISPs as needing attitudes supportive of meeting the stakeholders involved in the implementation process within their contexts and of actively guiding them towards new territory. While the former may be best met through respect, empathy, pragmatism, approachability, and flexibility, the latter may be best approached based on drive, honesty, independence, persuasion, and proactivity.
Taken together, the literature this review included draws a picture of ISPs as requiring deep specialist knowledge and a mixed set of attitudes promoting their responsiveness to as well as leadership of stakeholders. The increasing number of studies reporting the involvement of ISPs in RSI implementation also reflects that implementation support roles have gained importance in human services–with this review demonstrating that there is merit in integrating the existing knowledge for ISP roles, which may be labelled differently but are otherwise highly similar in purpose and activities. Integrating and using this knowledge further in considering how to best develop, utilize, and evaluate ISPs in health and human services is of concern to both research and practice.
In having integrated multiple bodies of knowledge focused on different ISP roles in this review, we provide researchers engaged in examining the work of ISPs with a knowledge base that can function as a launch pad for more detailed studies of the role of knowledge and attitudes in implementation support work. It lends itself to intentional efforts of knowledge building and attitude development in ISPs and to studies of how such efforts can influence the implementation capacities of service providers in health and human services. It also invites to compare the effectiveness of different ISPs with different profiles of knowledge and attitudes or to examine how the presence of different types of ISP knowledge and attitudes can be secured and brought to bear through implementation support teams rather than individual ISPs. Furthermore, there is a basis for studying the relationship between ISP knowledge and attitudes. The Knowledge, Attitude, and Practice model (KAP) emphasizes the interrelation between knowledge and attitudes and how they, together, impact behavior in practice [128]. It describes a linear relationship, where (a lack of) knowledge affects attitude and attitude in turn influences behavior. The authors argue that knowledge and attitudes are relational and cannot be interpreted independently from each other. Furthermore, they are dynamic concepts and change over time, in that acquisition of knowledge may lead to changed attitudes. How this occurs is highly dependent on the context, including, e.g., resources, the setting, and individuals involved. It was beyond the scope of this review to understand associations and correlations between ISP knowledge and attitudes and the behavioral consequences of such interaction. Questions of interest for future research may therefore be, for example: Do ISP attitudes change with growing knowledge? What are optimal strategies and conditions for ISP knowledge building? Can knowledge be actively used to shape attitudes of ISPs—and how? Are there specific types of ISP knowledge and attitudes that are particularly important to effectively support implementation and enabling implementation behavior change in others? Pursuing these and other pertinent questions about ISPs will help to better understand this particular role in evidence implementation and to build effective implementation support capacities for practice.
For those working in implementation practice, i.e., at the frontline of human service delivery or in intermediary organizations [129], it will be clear from this review that ISP roles represent expertise that is not easily built as part of a professional career as, e.g., psychologist, nurse, or social worker. The complex combination of specialist and generalist knowledge and task oriented as well as interpersonal attitudes draws a picture of ISP competence that goes beyond the basic training and professional development offered through traditional educational institutions operating in the human service sector. Instead, ISPs will often have built their expertise through a mix of formal and informal educational and professional development activities and continuous on-the-job training embedded in different roles and positions that ISPs have held over longer periods of time.
The results from this review can be used as a starting point for considering more systematically how to utilize and/or develop ISP roles. Decision makers in service and intermediary organizations can use the profile of ISP knowledge and attitudes presented here to understand what to look out for when recruiting ISPs or what to consider when training and developing staff with the aim to establish ISP functions in an agency or organization. By recognizing the role of ISPs, its inherent complexity and diverse resource requirements, organizations can prepare for how to best facilitate and support this position in their local context through, e.g., ongoing education and training, supportive infrastructure and networks, or mentor- and leadership. This is even more pertinent in light of the particular characteristics of the ISP role, including to operate at multiple hierarchical levels of an organization or system, to liaise between different individual and organizational stakeholders, and to balance the need to be a team player with the need to always also provide the perspective of an “outsider”. These characteristics explain why ISPs need a broad knowledge base and range of attitudes, and simultaneously indicate that the development and use of such knowledge and attitudes requires organizational as well as leadership support.
In planning for such support, it may be of value to keep in mind that the full range of ISP knowledge and attitudes presented here rarely will be found in a single individual. The purpose of this work is not to create unrealistic expectations for and excessive demands on ISPs. Instead, the knowledge and attitude profile may be viewed as containing building blocks for developing implementation support capacities across multiple individuals in an organization, who also may collaborate as a team and thereby complement each other in their expertise and experience. This may also ease the flexible tailoring of ISP offerings to different projects, settings and stakeholder groups, because there is higher probability for a greater bandwidth of knowledge and attitudes across multiple individuals. The findings from this review and related results from the project into which it is embedded [6, 36, 37] provides a knowledge base for setting up implementation support teams representing the relevant complementary knowledge, attitudes, and skills needed to enable and facilitate implementation processes.
Additionally, educational institutions may want to consider this knowledge base for the development of training opportunities targeting ISPs. The lack of educational offerings and opportunities for those operating in implementation practice, rather than science, has been discussed in the literature as a gap that prevents implementation science knowledge from being used in organizations and systems working to establish cultures of EBP [130–133]. Developing such offerings in ways that build on existing specialist education curricula for, e.g., nurses, psychologists, social workers or allied health practitioners and expand this knowledge based on a generalist, multidisciplinary and implementation informed focus can help different health and human service sectors to more easily build the capacities they need in their work to enhance the uptake of evidence in practice.
Limitations
This article is the result of a systematically conducted integrative review. Multiple limitations need to be considered when interpreting and using study findings.
The integrative review builds on concept saturation, which means that not all available studies reporting on distinct ISP roles (e.g., facilitator) might have been included. The research team recommends readers especially interested in a particular implementation support role to consult the corresponding literature base.
Furthermore, the search string was created using novel and diverse implementation terminology. While we worked to be as inclusive as possible to include a broad range of ISP terms, the fact that the field of implementation science is young and its terminology is not always aligned, studies which used related but different terminology might not have been identified. Readers should also note that this review aggregates findings from studies predominantly conducted in health and mental health, and to a lesser degree in social welfare and education. While some findings may be applicable to multiple sectors, other findings may be sector specific and require adaption when transferred to other settings.
Important to note as well is that the boundaries between knowledge and attitudes are not always clear when presented in different studies. The distinctions made in this article are a result of ongoing discussions in our research team and thus of group interpretation. Additionally, the results of this paper were based on a dichotomy differing between whether particular knowledge and attitudes were present or not in an included study. The quantity or quality of specific types of knowledge or attitude described in studies were not considered. This means that the included visualizations represent the number of articles mentioning a specific type of knowledge or attitude rather than the total number of mentions of knowledge or attitude within and across articles. Although our work reveals minor differences in ISP knowledge and attitudes according to their position, these findings need to be interpreted with caution, as they are based on a small number of studies. Moreover, this review focused solely on attitudes of ISPs defined as active mindsets or perception filters as opposed to characteristics or attributes in general.
Finally, studies included in this review used a variety of, e.g., observational, quantitative, qualitative and other research methods. These methods influence study results in that, for example, it makes a difference whether attitudes are self- or externally assessed, as self-perception might vary from the perception by others. This review did not take such potential differences into account and treated extracted data from across studies in the same way independently of the data collection method used.
Conclusion
Throughout the literature, ISPs display the use of a broad knowledge base and of a palette of attitudes in their work–aimed at matching both the diverse settings and situations they work in and the, at times, contradicting demands on their support. The most common knowledge areas among ISPs are knowledge about the clinical practice, implementation / improvement practice, the local context, supporting change processes, and facilitating EBP in general. The most reported attitude themes that characterize ISPs are motivated / motivating / encouraging / empowering, empathetic / respectful / sensitive, collaborative / inclusive, authentic, creative / flexible / innovative / adaptive, and frank / direct / honest. These findings show that ISPs are required to be both flexible and firm, to provide support as well as leadership, and to be specialists as well as generalists in their work with and bridge-building between varying individual and organizational stakeholders and their needs and interests. This complexity and its inherent tension call for a comprehensive and systematic approach to developing the ISP as a professional role and to embedding it in different health and social welfare organizations and systems. Developing this approach collaboratively across implementation science, practice, and education will be a crucial step towards building enhanced implementation capacities in human services.
Supporting information
Implementation Support Skills–Findings from a Systematic Integrative Review.
(PDF)
(PDF)
(PDF)
The publication IDs indicate the corresponding articles in which the descriptors were identified.
(PDF)
The publication IDs indicate the corresponding articles in which the descriptors were identified.
(PDF)
Data Availability
All corresponding materials are contained within the paper and the OSF database (https://osf.io/9kfqr/).
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337: a1655. doi: 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ornstein JT, Hammond RA, Padek M, Mazzucca S, Brownson RC. Rugged landscapes: complexity and implementation science. Implement Sci. 2020;15: 85. doi: 10.1186/s13012-020-01028-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.May CR, Johnson M, Finch T. Implementation, context and complexity. Implement Sci. 2016;11: 141. doi: 10.1186/s13012-016-0506-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birken SA, Haines ER, Hwang S, Chambers DA, Bunger AC, Nilsen P. Advancing understanding and identifying strategies for sustaining evidence-based practices: a review of reviews. Implement Sci. 2020;15: 88. doi: 10.1186/s13012-020-01040-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Q. 2004;82: 581–629. doi: 10.1111/j.0887-378X.2004.00325.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albers B, Metz A, Burke K. Implementation support practitioners—a proposal for consolidating a diverse evidence base. BMC Health Serv Res. 2020;20: 368. doi: 10.1186/s12913-020-05145-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Proctor E, Hooley C, Morse A, McCrary S, Kim H, Kohl PL. Intermediary/purveyor organizations for evidence-based interventions in the US child mental health: characteristics and implementation strategies. Implement Sci. 2019;14: 3. doi: 10.1186/s13012-018-0845-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dogherty EJ, Harrison M, Graham I, Keeping-Burke L. Examining the use of facilitation within guideline dissemination and implementation studies in nursing. Int J Evid Based Healthc. 2014;12: 105–27. doi: 10.1097/XEB.0000000000000008 [DOI] [PubMed] [Google Scholar]
- 9.Mallidou AA, Atherton P, Chan L, Frisch N, Glegg S, Scarrow G. Core knowledge translation competencies: a scoping review. BMC Health Serv Res. 2018;18: 502. doi: 10.1186/s12913-018-3314-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ajzen I. From Intentions to Actions: A Theory of Planned Behavior. In: Action Control. Berlin, Heidelberg: Springer Berlin Heidelberg; 1985. pp. 11–39. doi: 10.1007/978-3-642-69746-3_2 [DOI] [Google Scholar]
- 11.Lo SB, Ryba MM, Brothers BM, Andersen BL. Predicting implementation of an empirically supported treatment for cancer patients using the theory of planned behavior. Health Psychol. 2019;38: 1075–1082. doi: 10.1037/hea0000794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinmetz H, Knappstein M, Ajzen I, Schmidt P, Kabst R. How Effective are Behavior Change Interventions Based on the Theory of Planned Behavior? Z Psychol. 2016;224: 216–233. doi: 10.1027/2151-2604/a000255 [DOI] [Google Scholar]
- 13.Squires JE, Estabrooks CA, Gustavsson P, Wallin L. Individual determinants of research utilization by nurses: a systematic review update. Implement Sci. 2011;6: 1. doi: 10.1186/1748-5908-6-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aarons GA. Mental health provider attitudes toward adoption of evidence-based practice: the Evidence-Based Practice Attitude Scale (EBPAS). Ment Health Serv Res. 2004;6: 61–74. doi: 10.1023/b:mhsr.0000024351.12294.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel AK, Jain P, Kujur A, Patel A. A Study of Knowledge, Attitude and Practice Pattern of Adult Immunization. Int J Heal Clin Res. 2021;4: 120–123. [Google Scholar]
- 16.Skavberg Roaldsen K, Halvarsson A. Reliability of the Swedish version of the Evidence-Based Practice Attitude Scale assessing physiotherapist’s attitudes to implementation of evidence-based practice. PLoS One. 2019;14: e0225467. doi: 10.1371/journal.pone.0225467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4: 50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patelarou AE, Patelarou E, Brokalaki H, Dafermos V, Thiel L, Melas CD, et al. Current evidence on the attitudes, knowledge and perceptions of nurses regarding evidence-based practice implementation in European community settings: a systematic review. J Community Health Nurs. 2013;30: 230–44. doi: 10.1080/07370016.2013.838501 [DOI] [PubMed] [Google Scholar]
- 19.Verloo H, Melly P, Hilfiker R, Pereira F. Effectiveness of Educational Interventions to Increase Knowledge of Evidence-Based Practice Among Nurses and Physiotherapists in Primary Health Care: Protocol for a Systematic Review. JMIR Res Protoc. 2020;9: e17621. doi: 10.2196/17621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scurlock-Evans L, Upton D. The role and nature of evidence: a systematic review of social workers’ evidence-based practice orientation, attitudes, and implementation. J evidence-informed Soc Work. 2015;12: 369–99. doi: 10.1080/15433714.2013.853014 [DOI] [PubMed] [Google Scholar]
- 21.Spensberger F, Kollar I, Gambrill E, Ghanem C, Pankofer S. How to Teach Evidence-Based Practice in Social Work: A Systematic Review. Res Soc Work Pract. 2020;30: 19–39. doi: 10.1177/1049731519852150 [DOI] [Google Scholar]
- 22.Basckin C, Strnadová I, Cumming TM. Teacher beliefs about evidence-based practice: A systematic review. Int J Educ Res. 2021;106: 101727. doi: 10.1016/j.ijer.2020.101727 [DOI] [Google Scholar]
- 23.Thompson DS, Estabrooks CA, Scott-Findlay S, Moore K, Wallin L. Interventions aimed at increasing research use in nursing: a systematic review. Implement Sci. 2007;2: 15. doi: 10.1186/1748-5908-2-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nagykaldi Z, Mold JW, Aspy CB. Practice facilitators: a review of the literature. Fam Med. 2005;37: 581–8. Available: http://www.ncbi.nlm.nih.gov/pubmed/16145629 [PubMed] [Google Scholar]
- 25.Cranley LA, Cummings GG, Profetto-McGrath J, Toth F, Estabrooks CA. Facilitation roles and characteristics associated with research use by healthcare professionals: a scoping review. BMJ Open. 2017;7: e014384. doi: 10.1136/bmjopen-2016-014384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCormack B, Rycroft-Malone J, Decorby K, Hutchinson AM, Bucknall T, Kent B, et al. A realist review of interventions and strategies to promote evidence-informed healthcare: a focus on change agency. Implement Sci. 2013;8: 107. doi: 10.1186/1748-5908-8-107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hogg MA, Vaughan G. Introduction to social psychology. 4th ed. Frenchs Forest, Sydney, Australia: Pearson Education Australia; 2005. [Google Scholar]
- 28.Eagly AH, Chaiken S. The psychology of attitudes. Harcourt Brace Jovanovich College Publishers; 1993. [Google Scholar]
- 29.Metz A, Albers B, Burke K, Bartley L, Louison L, Ward C, et al. Implementation Practice in Human Service Systems: Understanding the Principles and Competencies of Professionals Who Support Implementation. Hum Serv Organ Manag Leadersh Gov. 2021;45: 238–259. doi: 10.1080/23303131.2021.1895401 [DOI] [Google Scholar]
- 30.Elledge C, Avworo A, Cochetti J, Carvalho C, Grota P. Characteristics of facilitators in knowledge translation: An integrative review. Collegian. 2019;26: 171–182. doi: 10.1016/j.colegn.2018.03.002 [DOI] [Google Scholar]
- 31.Sandström B, Borglin G, Nilsson R, Willman A. Promoting the implementation of evidence-based practice: a literature review focusing on the role of nursing leadership. Worldviews evidence-based Nurs. 2011;8: 212–23. doi: 10.1111/j.1741-6787.2011.00216.x [DOI] [PubMed] [Google Scholar]
- 32.Damschroder LJ, Banaszak-Holl J, Kowalski CP, et al. The role of the champion in infection prevention: results from a multisite qualitative study. Qual Saf Health Care 2009;18:434–40. doi: 10.1136/qshc.2009.034199 [DOI] [PubMed] [Google Scholar]
- 33.Shifaza F, Evans D, Bradley H, Ullrich S. Developing evidence-based practice champions in the Maldives. Int J Nurs Pract. 2013;19: 596–602. doi: 10.1111/ijn.12106 [DOI] [PubMed] [Google Scholar]
- 34.Gotlib Conn L, McKenzie M, Pearsall EA, McLeod RS. Successful implementation of an enhanced recovery after surgery programme for elective colorectal surgery: a process evaluation of champions’ experiences. Implement Sci. 2015;10: 99. doi: 10.1186/s13012-015-0289-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ervin NE. Clinical coaching: a strategy for enhancing evidence-based nursing practice. Clin Nurse Spec. 2005;19: 296–301. doi: 10.1097/00002800-200511000-00008 [DOI] [PubMed] [Google Scholar]
- 36.Albers B, Metz A, Burke K, Bührmann L, Bartley L, Driessen P, et al. Implementation Support Skills: Findings From a Systematic Integrative Review. Res Soc Work Pract. 2021;31: 147–170. doi: 10.1177/1049731520967419 [DOI] [Google Scholar]
- 37.Albers B, Metz A, Burke K, Bührmann L, Bartley L, Driessen P, et al. The Mechanisms of Implementation Support–Findings from a Systematic Integrative Review. Res Soc Work Pract. 2021;32: 259–280. doi: 10.1177/10497315211042375 [DOI] [Google Scholar]
- 38.Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52: 546–53. doi: 10.1111/j.1365-2648.2005.03621.x [DOI] [PubMed] [Google Scholar]
- 39.Albers B, Bührmann L, Driessen P, Bartley L, Varsi C. Implementation support skills—Electronic Results Addendum. 2020. Available: https://osf.io/9kfqr/ [Google Scholar]
- 40.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hodder RK, Wolfenden L, Kamper SJ, Lee H, Williams A, O’Brien KM, et al. Developing implementation science to improve the translation of research to address low back pain: A critical review. Best Pract Res Clin Rheumatol. 2016;30: 1050–1073. doi: 10.1016/j.berh.2017.05.002 [DOI] [PubMed] [Google Scholar]
- 42.Dedoose. Web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA: SocioCultural Research Consultants, LLC; 2018. [Google Scholar]
- 43.Braun V, Clarke V. Thematic analysis revised-final. Qual Res Psychol. 2006;3: 77–101. [Google Scholar]
- 44.Braun V, Clarke V. Thematic analysis. In: APA handbook of research methods in psychology, Vol 2: Research designs: Quantitative, qualitative, neuropsychological, and biological. Washington: American Psychological Association; 2012. pp. 57–71. doi: 10.1037/13620-004 [DOI] [Google Scholar]
- 45.Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2021;18: 328–352. doi: 10.1080/14780887.2020.1769238 [DOI] [Google Scholar]
- 46.Colman AM. A Dictionary of Psychology. Oxford University Press; 2008. doi: 10.1093/acref/9780199534067.001.0001 [DOI] [Google Scholar]
- 47.Acolet D, Allen E, Houston R, Wilkinson AR, Costeloe K, Elbourne D. Improvement in neonatal intensive care unit care: A cluster randomised controlled trial of active dissemination of information. Arch Dis Child Fetal Neonatal Ed. 2011;96: 434–439. doi: 10.1136/adc.2010.207522 [DOI] [PubMed] [Google Scholar]
- 48.Anaby D, Korner-Bitensky N, Law M, Cormier I. Focus on participation for children and youth with disabilities: Supporting therapy practice through a guided knowledge translation process. Br J Occup Ther. 2015;78: 440–449. doi: 10.1177/0308022614563942 [DOI] [Google Scholar]
- 49.Beidas RS, Edmunds JM, Marcus SC, Kendall PC. Training and consultation to promote implementation of an empirically supported treatment: A randomized trial. Psychiatr Serv. 2012;63: 660–665. doi: 10.1176/appi.ps.201100401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bradshaw CP, Pas ET, Goldweber A, Rosenberg MS, Leaf PJ. Integrating school-wide positive behavioral interventions and supports with tier 2 coaching to student support teams: The PBISplus model. Adv Sch Ment Health Promot. 2012;5: 177–193. doi: 10.1080/1754730X.2012.707429 [DOI] [Google Scholar]
- 51.Brown KM, Elliott SJ, Leatherdale ST. Researchers Supporting Schools to Improve Health: Influential Factors and Outcomes of Knowledge Brokering in the COMPASS Study. J Sch Health. 2018;88: 54–64. doi: 10.1111/josh.12578 [DOI] [PubMed] [Google Scholar]
- 52.Byrnes A, Young A, Mudge A, Banks M, Clark D, Bauer J. Prospective application of an implementation framework to improve postoperative nutrition care processes: Evaluation of a mixed methods implementation study. Nutr Diet. 2018;75: 353–362. doi: 10.1111/1747-0080.12464 [DOI] [PubMed] [Google Scholar]
- 53.Caron E, Dozier M. Effects of Fidelity-Focused Consultation on Clinicians’ Implementation: An Exploratory Multiple Baseline Design. Adm Policy Ment Heal Ment Heal Serv Res. 2019;46: 445–457. doi: 10.1007/s10488-019-00924-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chinman M, McCarthy S, Hannah G, Byrne TH, Smelson DA. Using Getting To Outcomes to facilitate the use of an evidence-based practice in VA homeless programs: A cluster-randomized trial of an implementation support strategy. Implement Sci. 2017;12: 1–12. doi: 10.1186/s13012-016-0533-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chinman M, Ebener P, Malone PS, Cannon J, D’Amico EJ, Acosta J. Testing implementation support for evidence-based programs in community settings: A replication cluster-randomized trial of Getting To Outcomes®. Implement Sci. 2018;13: 1–16. doi: 10.1186/s13012-017-0699-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dobbins M, Traynor RL, Workentine S, Yousefi-Nooraie R, Yost J. Impact of an organization-wide knowledge translation strategy to support evidence-informed public health decision making. BMC Public Health. 2018;18: 1–15. doi: 10.1186/s12889-018-6317-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duffy JL, Prince MS, Johnson EE, Alton FL, Flynn S, Faye AM, et al. Enhancing Teen Pregnancy Prevention in Local Communities: Capacity Building Using the Interactive Systems Framework. Am J Community Psychol. 2012;50: 370–385. doi: 10.1007/s10464-012-9531-9 [DOI] [PubMed] [Google Scholar]
- 58.Feinberg ME, Ridenour TA, Greenberg MT. The longitudinal effect of technical assistance dosage on the functioning of Communities That Care prevention boards in Pennsylvania. J Prim Prev. 2008;29: 145–165. doi: 10.1007/s10935-008-0130-3 [DOI] [PubMed] [Google Scholar]
- 59.Fortney JC, Pyne JM, Ward-Jones S, Bennett IM, Diehl J, Farris K, et al. Implementation of evidence-based practices for complex mood disorders in primary care safety net clinics. Fam Syst Heal. 2018;36: 267–280. doi: 10.1037/fsh0000357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Funderburk B, Chaffin M, Bard E, Shanley J, Bard D, Berliner L. Comparing Client Outcomes for Two Evidence-Based Treatment Consultation Strategies. J Clin Child Adolesc Psychol. 2015;44: 730–741. doi: 10.1080/15374416.2014.910790 [DOI] [PubMed] [Google Scholar]
- 61.Garbacz SA, Watkins ND, Diaz Y, Barnabas ER, Schwartz B, Eiraldi R. Using conjoint behavioral consultation to implement evidence-based practices for students in low-income urban schools. Prev Sch Fail Altern Educ Child Youth. 2016;61: 198–210. doi: 10.1080/1045988X.2016.1261078 [DOI] [Google Scholar]
- 62.Gustafson DH, Quanbeck AR, Robinson JM, Ford JH, Pulvermacher A, French MT, et al. Which elements of improvement collaboratives are most effective? A cluster-randomized trial. Addiction. 2013;108: 1145–1157. doi: 10.1111/add.12117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hagermoser Sanetti LM, Fallon LM, Collier-Meek MA. Increasing teacher treatment integrity through performance feedback provided by school personnel. Psychol Sch. 2013;50: 134–150. doi: 10.1002/pits.21664 [DOI] [Google Scholar]
- 64.Hagermoser Sanetti LM, Williamson KM, Long ACJ, Kratochwill TR. Increasing In-Service Teacher Implementation of Classroom Management Practices Through Consultation, Implementation Planning, and Participant Modeling. J Posit Behav Interv. 2018;20: 43–59. doi: 10.1177/1098300717722357 [DOI] [Google Scholar]
- 65.Brown CH, Chamberlain P, Saldana L, Padgett C, Wang W, Cruden G. Evaluation of two implementation strategies in 51 child county public service systems in two states: results of a cluster randomized head-to-head implementation trial. Implement Sci. 2014;9: 134. doi: 10.1186/s13012-014-0134-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Holtrop JS, Baumann J, Arnold AK, Torres T. Nurses as practice change facilitators for healthy behaviors. J Nurs Care Qual. 2008;23: 123–131. doi: 10.1097/01.NCQ.0000313761.79396.37 [DOI] [PubMed] [Google Scholar]
- 67.Hurlburt M, Aarons GA, Fettes D, Willging C, Gunderson L, Chaffin MJ. Interagency Collaborative Team model for capacity building to scale-up evidence-based practice. Child Youth Serv Rev. 2014;39: 160–168. doi: 10.1016/j.childyouth.2013.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kelly JA, Somlai AM, DiFranceisco WJ, Otto-Salaj LL, McAuliffe TL, Hackl KL, et al. Bridging the gap between the science and service of HIV prevention: Transferring effective research-based HIV prevention interventions to community AIDS service providers. Am J Public Health. 2000;90: 1082–1088. doi: 10.2105/ajph.90.7.1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kirchner JAE, Ritchie MJ, Pitcock JA, Parker LE, Curran GM, Fortney JC. Outcomes of a Partnered Facilitation Strategy to Implement Primary Care–Mental Health. J Gen Intern Med. 2014;29: 904–912. doi: 10.1007/s11606-014-3027-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leeman J, Myers A, Grant JC, Wangen M, Queen TL. Implementation strategies to promote community-engaged efforts to counter tobacco marketing at the point of sale. Transl Behav Med. 2017;7: 405–414. doi: 10.1007/s13142-017-0489-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mader EM, Fox CH, Epling JW, Noronha GJ, Swanger CM, Wisniewski AM, et al. A practice facilitation and academic detailing intervention can improve cancer screening rates in primary care safety net clinics. J Am Board Fam Med. 2016;29: 533–542. doi: 10.3122/jabfm.2016.05.160109 [DOI] [PubMed] [Google Scholar]
- 72.Murray ME, Khoury DY, Farmer EMZ, Burns BJ. Is more better? Examining whether enhanced consultation/coaching improves implementation. Am J Orthopsychiatry. 2018;88: 376–385. doi: 10.1037/ort0000296 [DOI] [PubMed] [Google Scholar]
- 73.Nadeem E, Gleacher A, Pimentel S, Hill LC, McHugh M, Hoagwood KE. The Role of Consultation Calls for Clinic Supervisors in Supporting Large-Scale Dissemination of Evidence-Based Treatments for Children. Adm Policy Ment Heal Ment Heal Serv Res. 2013;40: 530–540. doi: 10.1007/s10488-013-0491-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Parchman ML, Noel PH, Culler SD, Lanham HJ, Leykum LK, Romero RL, et al. A randomized trial of practice facilitation to improve the delivery of chronic illness care in primary care: Initial and sustained effects. Implement Sci. 2013;8: 1–7. doi: 10.1186/1748-5908-8-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Peterson DJ, Christiansen AL, Guse CE, Layde PM. Community Translation of Fall Prevention Interventions: The Methods and Process of a Ramdomized Trial. J Community Psychol. 2015;43: 1005–1018. doi: 10.1002/jcop.21728 [DOI] [Google Scholar]
- 76.Ritchie MJ, Parker LE, Edlund CN, Kirchner JE. Using implementation facilitation to foster clinical practice quality and adherence to evidence in challenged settings: A qualitative study. BMC Health Serv Res. 2017;17: 1–15. doi: 10.1186/s12913-016-1943-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Russell DJ, Rivard LM, Walter SD, Rosenbaum PL, Roxborough L, Cameron D, et al. Using knowledge brokers to facilitate the uptake of pediatric measurement tools into clinical practice: A before-after intervention study. Implement Sci. 2010;5: 1–17. doi: 10.1186/1748-5908-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Saldana L, Chamberlain P. Supporting Implementation: The Role of Community Development Teams to Build Infrastructure. Am J Community Psychol. 2012;50: 334–346. doi: 10.1007/s10464-012-9503-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stirman SW, Pontoski K, Creed T, Xhezo R, Evans AC, Beck AT, et al. A Non-randomized Comparison of Strategies for Consultation in a Community-Academic Training Program to Implement an Evidence-Based Psychotherapy. Adm Policy Ment Heal Ment Heal Serv Res. 2017;44: 55–66. doi: 10.1007/s10488-015-0700-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Williams NJ, Glisson C, Hemmelgarn A, Green P. Mechanisms of Change in the ARC Organizational Strategy: Increasing Mental Health Clinicians’ EBP Adoption Through Improved Organizational Culture and Capacity. Adm Policy Ment Heal Ment Heal Serv Res. 2016;44: 269–283. doi: 10.1007/s10488-016-0742-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Akin BA. Practitioner views on the core functions of coaching in the implementation of an evidence-based intervention in child welfare. Child Youth Serv Rev. 2016;68: 159–168. doi: 10.1016/j.childyouth.2016.07.010 [DOI] [Google Scholar]
- 82.Beidas RS, Edmunds JM, Cannuscio CC, Gallagher M, Downey MM, Kendall PC. Therapists Perspectives on the Effective Elements of Consultation Following Training. Adm Policy Ment Heal Ment Heal Serv Res. 2013;40: 507–517. doi: 10.1007/s10488-013-0475-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brown KM, Elliott SJ, Robertson-Wilson J, Vine MM, Leatherdale ST. Can knowledge exchange support the implementation of a health-promoting schools approach? Perceived outcomes of knowledge exchange in the COMPASS study. BMC Public Health. 2018;18: 351. doi: 10.1186/s12889-018-5229-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chew S, Armstrong N, Martin G. Institutionalising knowledge brokering as a sustainable knowledge translation solution in healthcare: how can it work in practice? Evid Policy A J Res Debate Pract. 2013;9: 335–351. doi: 10.1332/174426413X662734 [DOI] [Google Scholar]
- 85.Hurtubise K, Rivard L, Héguy L, Berbari J, Camden C. Virtual Knowledge Brokering: Describing the Roles and Strategies Used by Knowledge Brokers in a Pediatric Physiotherapy Virtual Community of Practice. J Contin Educ Health Prof. 2016;36: 186–194. doi: 10.1097/CEH.0000000000000101 [DOI] [PubMed] [Google Scholar]
- 86.Kaasalainen S, Ploeg J, Donald F, Coker E, Brazil K, Martin-Misener R, et al. Positioning clinical nurse specialists and nurse practitioners as change champions to implement a pain protocol in long-term care. Pain Manag Nurs. 2015;16: 78–88. doi: 10.1016/j.pmn.2014.04.002 [DOI] [PubMed] [Google Scholar]
- 87.Kauth MR, Sullivan G, Blevins D, Cully JA, Landes RD, Said Q, et al. Employing external facilitation to implement cognitive behavioral therapy in VA clinics: a pilot study. Implement Sci. 2010;5: 75. doi: 10.1186/1748-5908-5-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kristensen HK, Hounsgaard L. Implementation of coherent, evidence-based pathways in Danish rehabilitation practice. Disabil Rehabil. 2013;35: 2021–2028. doi: 10.3109/09638288.2013.768301 [DOI] [PubMed] [Google Scholar]
- 89.Lavoie-Tremblay M, Richer MC, Marchionni C, Cyr G, Biron AD, Aubry M, et al. Implementation of Evidence-Based Practices in the Context of a Redevelopment Project in a Canadian Healthcare Organization. J Nurs Scholarsh. 2012;44: 418–427. doi: 10.1111/j.1547-5069.2012.01480.x [DOI] [PubMed] [Google Scholar]
- 90.Lessard S, Bareil C, Lalonde L, Duhamel F, Hudon E, Goudreau J, et al. External facilitators and interprofessional facilitation teams: a qualitative study of their roles in supporting practice change. Implement Sci. 2016;11: 97. doi: 10.1186/s13012-016-0458-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mackenzie T, Innes J, Boyd M, Keane B, Boxall J, Allan S. Evaluating the role and value of a national office to coordinate Liverpool Care Pathway implementation in New Zealand. Int J Evid Based Healthc. 2011;9: 252–60. doi: 10.1111/j.1744-1609.2011.00219.x [DOI] [PubMed] [Google Scholar]
- 92.Olson JR, McCarthy KJ, Perkins DF, Borden LM. A formative evaluation of a coach-based technical assistance model for youth- and family-focused programming. Eval Program Plann. 2018;67: 29–37. doi: 10.1016/j.evalprogplan.2017.11.002 [DOI] [PubMed] [Google Scholar]
- 93.Rosen CS, Nguyen T, Bernardy NC, Hamblen JL, Ruzek JI, Friedman MJ. Evaluation of a Mentoring Program for PTSD Clinic Managers in the U.S. Department of Veterans Affairs. Psychiatr Serv. 2012;63: 1047–1050. doi: 10.1176/appi.ps.201100446 [DOI] [PubMed] [Google Scholar]
- 94.Aasekjær K, Waehle HV, Ciliska D, Nordtvedt MW, Hjälmhult E. Management Involvement-A Decisive Condition When Implementing Evidence-Based Practice. Worldviews Evidence-Based Nurs. 2016;13: 32–41. doi: 10.1111/wvn.12141 [DOI] [PubMed] [Google Scholar]
- 95.Barac R, Kimber M, Johnson S, Barwick M. The effectiveness of consultation for clinicians learning to deliver motivational interviewing with fidelity. J Evidence-Informed Soc Work. 2018;15: 510–533. doi: 10.1080/23761407.2018.1480988 [DOI] [PubMed] [Google Scholar]
- 96.Becker KD, Bradshaw CP, Domitrovich C, Ialongo NS. Coaching teachers to improve implementation of the good behavior game. Adm Policy Ment Heal Ment Heal Serv Res. 2013;40: 482–493. doi: 10.1007/s10488-013-0482-8 [DOI] [PubMed] [Google Scholar]
- 97.Bidassie B, Williams LS, Woodward-Hagg H, Matthias MS, Damush TM. Key components of external facilitation in an acute stroke quality improvement collaborative in the Veterans Health Administration. Implement Sci. 2015;10: 1–9. doi: 10.1186/s13012-014-0195-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cameron D, Russell DJ, Rivard L, Darrah J, Palisano R. Knowledge Brokering in Children’s Rehabilitation Organizations: Perspectives from Administrators. J Contin Educ Health Prof. 2011;31: 28–33. doi: 10.1002/chp.20098 [DOI] [PubMed] [Google Scholar]
- 99.Chaffin M, Hecht D, Aarons G, Fettes D, Hurlburt M, Ledesma K. EBT Fidelity Trajectories Across Training Cohorts Using the Interagency Collaborative Team Strategy. Adm Policy Ment Heal Ment Heal Serv Res. 2016;43: 144–156. doi: 10.1007/s10488-015-0627-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dogherty EJ, Harrison MB, Baker C, Graham ID. Following a natural experiment of guideline adaptation and early implementation: A mixed-methods study of facilitation. Implement Sci. 2012;7: 1–12. doi: 10.1186/1748-5908-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dogherty EJ, Harrison MB, Graham ID, Vandyk AD, Keeping-Burke L. Turning knowledge into action at the point-of-care: The collective experience of nurses facilitating the implementation of evidence-based practice. Worldviews Evidence-Based Nurs. 2013;10: 129–139. doi: 10.1111/wvn.12009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dusenbury L, Hansen WB, Jackson‐Newsom J, Pittman DS, Wilson C V., Nelson‐Simley K, et al. Coaching to enhance quality of implementation in prevention. Health Educ. 2010;110: 43–60. doi: 10.1108/09654281011008744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Eiraldi R, Mautone JA, Khanna MS, Power TJ, Orapallo A, Cacia J, et al. Group CBT for Externalizing Disorders in Urban Schools: Effect of Training Strategy on Treatment Fidelity and Child Outcomes. Behav Ther. 2018;49: 538–550. doi: 10.1016/j.beth.2018.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Elnitsky CA, Powell-Cope G, Besterman-Dahan KL, Rugs D, Ullrich PM. Implementation of Safe Patient Handling in the U.S. Veterans Health System: A Qualitative Study of Internal Facilitators’ Perceptions. Worldviews Evidence-Based Nurs. 2015;12: 208–216. doi: 10.1111/wvn.12098 [DOI] [PubMed] [Google Scholar]
- 105.Gerrish K, Mcdonnell A, Nolan M, Guillaume L, Kirshbaum M, Tod A. The role of advanced practice nurses in knowledge brokering as a means of promoting evidence-based practice among clinical nurses. J Adv Nurs. 2011;67: 2004–2014. doi: 10.1111/j.1365-2648.2011.05642.x [DOI] [PubMed] [Google Scholar]
- 106.Gerrish K, Nolan M, Mcdonnell A, Tod A, Kirshbaum M, Guillaume L. Factors Influencing Advanced Practice Nurses’ Ability to Promote Evidence-Based Practice among Frontline Nurses. Worldviews Evidence-Based Nurs. 2012;9: 30–39. doi: 10.1111/j.1741-6787.2011.00230.x [DOI] [PubMed] [Google Scholar]
- 107.Graaf G, McBeath B, Lwin K, Holmes D, Austin MJ. Supporting Evidence-Informed Practice in Human Service Organizations: An Exploratory Study of Link Officers. Hum Serv Organ Manag Leadersh Gov. 2017;41: 58–75. doi: 10.1080/23303131.2016.1192575 [DOI] [Google Scholar]
- 108.Gunderson LM, Willging CE, Trott Jaramillo EM, Green AE, Fettes DL, Hecht DB, et al. The good coach: implementation and sustainment factors that affect coaching as evidence-based intervention fidelity support. J Child Serv. 2018;13: 1–17. doi: 10.1108/JCS-09-2017-0043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jacobson N, Johnson R, Deyo B, Alagoz E, Quanbeck A. Systems consultation for opioid prescribing in primary care: A qualitative study of adaptation. BMJ Qual Saf. 2018;28: 397–404. doi: 10.1136/bmjqs-2018-008160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kousgaard MB, Thorsen T. Positive experiences with a specialist as facilitator in general practice. Dan Med J. 2012;59: A4443. Available: http://www.ncbi.nlm.nih.gov/pubmed/22677241 [PubMed] [Google Scholar]
- 111.Leathers SJ, Spielfogel JE, Blakey J, Christian E, Atkins MS. The Effect of a Change Agent on Use of Evidence-Based Mental Health Practices. Adm Policy Ment Heal Ment Heal Serv Res. 2016;43: 768–782. doi: 10.1007/s10488-015-0694-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mancini AD, Moser LL, Whitley R, McHugo GJ, Bond GR, Finnerty MT, et al. Assertive community treatment: Facilitators and barriers to implementation in routine mental health settings. Psychiatr Serv. 2009;60: 189–195. doi: 10.1176/ps.2009.60.2.189 [DOI] [PubMed] [Google Scholar]
- 113.McCullough MB, Gillespie C, Petrakis BA, Jones EA, Park AM, Lukas CVD, et al. Forming and activating an internal facilitation group for successful implementation: A qualitative study. Res Soc Adm Pharm. 2017;13: 1014–1027. doi: 10.1016/j.sapharm.2017.04.007 [DOI] [PubMed] [Google Scholar]
- 114.Mitchell RE, Stone-Wiggins B, Stevenson JF, Florin P. Cultivating Capacity. J Prev Interv Community. 2004;27: 67–87. doi: 10.1300/J005v27n02_05 [DOI] [Google Scholar]
- 115.Quanbeck A, Brown RT, Zgierska AE, Jacobson N, Robinson JM, Johnson RA, et al. A randomized matched-pairs study of feasibility, acceptability, and effectiveness of systems consultation: A novel implementation strategy for adopting clinical guidelines for Opioid prescribing in primary care. Implement Sci. 2018;13. doi: 10.1186/s13012-017-0691-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rivard LM, Russell DJ, Roxborough L, Ketelaar M, Bartlett DJ, Rosenbaum P. Promoting the Use of Measurement Tools in Practice: A Mixed-Methods Study of the Activities and Experiences of Physical Therapist Knowledge Brokers. Phys Ther. 2010;90: 1580–1590. doi: 10.2522/ptj.20090408 [DOI] [PubMed] [Google Scholar]
- 117.Rosella LC, Bornbaum C, Kornas K, Lebenbaum M, Peirson L, Fransoo R, et al. Evaluating the Process and Outcomes of a Knowledge Translation Approach to Supporting Use of the Diabetes Population Risk Tool (DPoRT) in Public Health Practice. Can J Progr Eval. 2018;33: 21–48. doi: 10.3138/cjpe.31160 [DOI] [Google Scholar]
- 118.Rushovich BR, Bartley LH, Steward RK, Bright CL. Technical Assistance: A Comparison Between Providers and Recipients. Hum Serv Organ Manag Leadersh Gov. 2015;39: 362–379. doi: 10.1080/23303131.2015.1052124 [DOI] [Google Scholar]
- 119.Shernoff ES, Lakind D, Frazier SL, Jakobsons L. Coaching Early Career Teachers in Urban Elementary Schools: A Mixed-Method Study. School Ment Health. 2015;7: 6–20. doi: 10.1007/s12310-014-9136-6 [DOI] [Google Scholar]
- 120.Tierney S, Kislov R, Deaton C. A qualitative study of a primary-care based intervention to improve the management of patients with heart failure: the dynamic relationship between facilitation and context. BMC Fam Pract. 2014;15: 153. doi: 10.1186/1471-2296-15-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.van der Zijpp TJ, Niessen T, Eldh AC, Hawkes C, McMullan C, Mockford C, et al. A Bridge Over Turbulent Waters: Illustrating the Interaction Between Managerial Leaders and Facilitators When Implementing Research Evidence. Worldviews Evidence-Based Nurs. 2016;13: 25–31. doi: 10.1111/wvn.12138 [DOI] [PubMed] [Google Scholar]
- 122.Waterman H, Boaden R, Burey L, Howells B, Harvey G, Humphreys J, et al. Facilitating large-scale implementation of evidence based health care: insider accounts from a co-operative inquiry. BMC Health Serv Res. 2015;15: 60. doi: 10.1186/s12913-015-0722-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Williams L, Burton C, Rycroft-Malone J. What works: a realist evaluation case study of intermediaries in infection control practice. J Adv Nurs. 2013;69: 915–26. doi: 10.1111/j.1365-2648.2012.06084.x [DOI] [PubMed] [Google Scholar]
- 124.Worton SK, Hasford J, Macnaughton E, Nelson G, MacLeod T, Tsemberis S, et al. Understanding Systems Change in Early Implementation of Housing First in Canadian Communities: An Examination of Facilitators/Barriers, Training/Technical Assistance, and Points of Leverage. Am J Community Psychol. 2018;61: 118–130. doi: 10.1002/ajcp.12219 [DOI] [PubMed] [Google Scholar]
- 125.Yazejian N, Metz A, Morgan J, Louison L, Bartley L, Fleming WO, et al. Co-creative technical assistance: essential functions and interim outcomes. Evid Policy A J Res Debate Pract. 2019;15: 339–352. doi: 10.1332/174426419X15468578679853 [DOI] [Google Scholar]
- 126.Gambrill E. Evidence-Based Practice: An Alternative to Authority-Based Practice. Fam Soc J Contemp Soc Serv. 1999;80: 341–350. doi: 10.1606/1044-3894.1214 [DOI] [Google Scholar]
- 127.Katz J, Wandersman A. Technical Assistance to Enhance Prevention Capacity: a Research Synthesis of the Evidence Base. Prev Sci. 2016;17: 417–28. doi: 10.1007/s11121-016-0636-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kwol VS, Eluwole KK, Avci T, Lasisi TT. Another look into the Knowledge Attitude Practice (KAP) model for food control: An investigation of the mediating role of food handlers’ attitudes. Food Control. 2020;110: 107025. doi: 10.1016/j.foodcont.2019.107025 [DOI] [Google Scholar]
- 129.Bullock HL, Lavis JN. Understanding the supports needed for policy implementation: a comparative analysis of the placement of intermediaries across three mental health systems. Heal Res policy Syst. 2019;17: 82. doi: 10.1186/s12961-019-0479-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mosson R, Augustsson H, Bäck A, Åhström M, von Thiele Schwarz U, Richter A, et al. Building implementation capacity (BIC): a longitudinal mixed methods evaluation of a team intervention. BMC Health Serv Res. 2019;19: 287. doi: 10.1186/s12913-019-4086-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Park JS, Moore JE, Sayal R, Holmes BJ, Scarrow G, Graham ID, et al. Evaluation of the “Foundations in Knowledge Translation” training initiative: preparing end users to practice KT. Implement Sci. 2018;13: 63. doi: 10.1186/s13012-018-0755-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Provvidenza C, Townley A, Wincentak J, Peacocke S, Kingsnorth S. Building knowledge translation competency in a community-based hospital: a practice-informed curriculum for healthcare providers, researchers, and leadership. Implement Sci. 2020;15: 54. doi: 10.1186/s13012-020-01013-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Slot-Heijs JJ, Collard DCM, Pettigrew S, Vinck J, Edell D, Barriguete A, et al. The training and support needs of 22 programme directors of community-based childhood obesity interventions based on the EPODE approach: an online survey across programmes in 18 countries. BMC Health Serv Res. 2020;20: 870. doi: 10.1186/s12913-020-05709-1 [DOI] [PMC free article] [PubMed] [Google Scholar]