Abstract
General thoracic surgery operations in Egypt are performed mainly by cardiothoracic surgeons and less oftenly by dedicated thoracic surgeons and general surgeons. This is mainly due to the relatively small number of thoracic surgeons in relation to population as only 210 cardiothoracic surgery specialists and 458 consultants are registered with the Egyptian Medical Syndicate (EMS) in a country with a population of more than 100 million people. Thoracic surgeons in Egypt are faced with a number of burdens, including the need to propagate the service to advanced technology infront of the obstacle of limited resources. Other burdens include higher incidence of TB, trauma and foreign body inhalation related to cultural backgrounds. More centres now are major video-assisted thoracic surgery (VATS) providing centres and others are specialized in more complex surgeries like complicated airway procedures and radical surgery for mesothelioma. As part of the international community, the COVID-19 pandemic has put more burdens on the thoracic surgery service as most centres have reduced their elective surgery workload to less than half of usual. Interestingly, the pandemic has allowed a self-referral screening programme with widespread Computed Tomography (CT) chest being performed among the population allowing thoracic surgeons to operate more on early stage lung cancer. The academic challenges for thoracic surgeons are even more with need for developing national databases. Nevertheless, thoracic surgeons in Egypt are optimistic regarding the future. The rising interest among the younger population will push training programs to meet the interests of enthusiastic junior surgeons. While the ancient history of thoracic surgery in Egypt seems to be extraordinary, the future perspectives promise to be more rewarding.
Keywords: Video-assisted thoracic surgery (VATS), thoracic surgery, chest, Egypt, lung neoplasm, cancer, tuberculosis
History
Ancient Egypt showed an interesting insight into chest problems including the discovery of tuberculosis bacilli and pectus excavatum in mummies (1,2). Modern thoracic surgery in Egypt carries a history which is largely undiscovered and is worth mentioning. As elsewhere, modern thoracic surgery started as an effort to fight tuberculosis. It used to be carried out by “lung specialists” slowly moving to be the job of surgeons with the increase in their patient numbers (3). Egypt witnessed the first ever use of median sternotomy, when Milton, the principal medical officer at Kasr el Aini Hospital in Cairo, published in 1897 the technique of median sternotomy for resection of tuberculous sternum, first on cadavers then clinically (4,5). The first Egyptian sanatorium, Fouad I Sanatorium at Helwan, was founded in 1926. The first two managers for this sanatorium were the Swiss lung specialists Dr. Rene Burnand (Figure 1) and Dr. Eric Zimmerli followed by the first Egyptian sanatorium manager, whom we believe he was the first Egyptian lung specialist and self-taught thoracic surgeon, Dr. Abdel Raouf Hassan (Figure 2). In his book, Fouad I sanatorium, Helwan. Reminiscences of Twenty Years (6), Hassan describes the efforts to establish the first sanatorium where good nutrition, rest and surgery were the main pillars of treatment in the pre antituberculosis drugs era. It seems that Dr. Hassan was the first and only thoracic surgeon for 10 years (3), until another surgeon, Dr. Zakaria Massoud (Figure 3), followed in 1939 , trained abroad before joining Fouad Sanatorium then moved to Abbasia Chest Hospital to become the chief chest surgeon at Ministry of Health and the first to perform major resections via thoracotomy, performing all range of thoracic operations, rigid bronchoscopy and mentor thoracic surgery practice of the newly assigned surgeons in university hospitals and Ministry of Health (3,6,7). The third surgeon who followed was Dr. Helmy Bassili Boctor who join the sanatorium in 1946 as the sanatorium surgeon after completing his FRCS in England in 1941 and working as a registrar at the Brompton Hospital, the first Egyptian to hold this post, He performed many lobectomies and pneumonectomies, He found he had just as good results by operating between the ribs instead of resecting a rib, He published his results in many journals (8,9).
Figure 1.
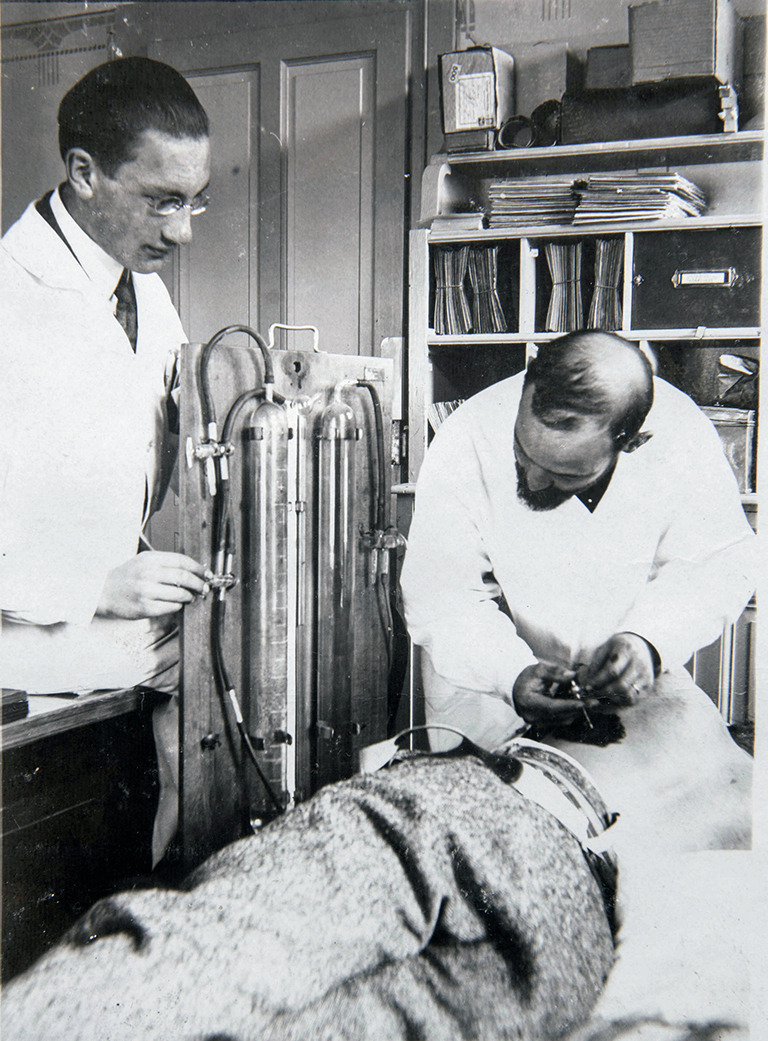
Rene Burnand performing artificial pneumothorax around 1927 (Photo courtesy of Celine Burnand with permission).
Figure 2.

Abdel-Raouf Hassan, the first Egyptian manager of Fouad Sanatorium (Photo courtesy of Hassan Abdel-Raouf Hassan with permission).
Figure 3.

Dr. Zakaria Massoud (Photo courtesy of Dr. Huda Z. Massoud with permission).
Dr. Abdel Raouf Hassan died at the age of 53 as a result of skin cancer in his left index finger, probably due to exposure to excessive radiation while localizing cavitary lesions under the screen to perform Monaldi’s operation. Days before his death Dr. Hassan had been admitted to hospital for care of the dissemination of cancer in his body after amputation of his left index finger. At that time, he was informed about a 14-year-old girl with a cavitary lesion requiring intervention. So he operated on this girl for 7 hours while astonishingly awaiting his death doing his favourite Monaldi’s procedure (10).
The first reported thoracotomy for trauma was done by a young surgeon, Dr. Hassan Ali Ibrahim, during the 1948 War. Faced with a fighter pilot who presented hemodynamically unstable with a retained bullet in his left chest, he noticed that the bullet was moving simultaneously with heartbeat under fluoroscopy, so he diagnosed it as a cardiac injury with cardiac tamponade. In a later account, he described his confusion as he had never opened up a chest before and his fear that the patient might die. Then he realized that the patient survived his injury on the battlefield and during transfer to the hospital so he could withstand surgery. He performed his first thoracotomy ever and found the bullet indented in the right ventricle. He removed it, and no adverse event happened. The patient recovered uneventfully and resumed his career in the Air Force (11), followed by a successful diplomatic career and passed away peacefully decades later. As a consequence of this experience, Dr. Hassan Ali Ibrahim, went abroad to obtain formal cardiothoracic surgery training and returned home to become a thoracic surgeon, until younger colleagues obtained fellowships and returned home to practice as dedicated thoracic surgeons by performing thoracoplasty, then advanced to constrictive pericarditis (12) and lung resections (13) Those went on to form the nidus of cardiothoracic surgery practice in Egypt, namely Fouad I, (Cairo) university cardiothoracic department which was established in 1951 by professor Dr. Salah El Malah, making it the first academic thoracic surgery Department in Egypt. Closed heart Surgery followed 2 years later (14), mainly closed mitral commissurotomy. The first open-heart surgery using surface cooling in Egypt was done in 1958 (15) and was a case of secundum ASD, followed by open-heart surgery using heart-lung machine in 1965 (16). Thoracoscopy was known since the early days of Fouad sanatorium as mentioned above, then gradually vanished with anti-tuberculous drugs era then regained popularity in the early 90s mainly for pleural and pericardial effusion drainage (17,18), moving steadily towards VATS lobectomy then uniportal VATS in 2016 (19). Currently, four centers across Egypt offer routine VATS lobectomy for amenable cases together with other VATS operations, with 3 other centers offering VATS thymectomy, decortication and sub lobar resection.
Education in cardiothoracic and thoracic surgery
To choose thoracic surgery as a career, a candidate should choose a thoracic surgery training program on one of two pathways. The first pathway is to join a cardiothoracic surgery residency program in one of the national universities. The other pathway is to apply for the thoracic surgery Egyptian fellowship program at the Ministry of Health (MOH), which has been established in 2005. It is a 6-year program, including 2 years of general surgery, 6 months of cardiac surgery then a dedicated thoracic surgery training for the rest of the program. It allows the admission of foreign clinical fellows mainly from Yamen, Libya, Sudan, and Iraq. So far, the fellowship program has trained 25 surgeons and certified 15 surgeons. Availability of thoracic surgery training seats is relatively limited and subjected to the yearly needs of the training organizations.
The university cardiothoracic surgery residency training program is mainly a mix of cardiac and thoracic surgery training. It lasts for 3–5 years according to the specifications of each university. Through this period, the candidate should get general surgery training of 6 months to 1 year. At the end of this pathway, the candidate gets a cardiothoracic surgery Master degree or general surgery Master degree with cardiothoracic surgery training experience. This is usually followed by doctorate degree, The first medical doctorate degree in Cardiothoracic surgery was granted in 1984 from Cairo university then the other universities started their own degrees. The current majority of thoracic surgeons in Egypt are graduates of this system.
Reconsidering the last ten years, we can touch the revolutionary wave of advanced thoracic surgery in Egypt. This wave started with many devoted subspecialized thoracic surgeons joining several overseas clinical fellowships for years under the patronage of The Ministry of Higher Education or even self-funded. Then, those surgeons returned to Egypt and started to develop programs for (VATS) and advanced complex thoracic surgery.
Thoracic operations in Egypt are done mainly by cardiothoracic surgeons less often by dedicated thoracic surgeons, general surgeons, pediatric surgeons, and oncology surgeons. This occurs mainly due to the relatively small number of thoracic surgeons in relation to population as only 210 cardiothoracic surgery specialists and 355 consultants A-level, 10 consultants B-level and 93 consultants C-level are registered with the Egyptian Medical Syndicate (EMS) in relation to a population of more than 100 million (20). These numbers represent cardiothoracic surgeons with the vast majority of them dedicated to cardiac surgery practice and having a minor thoracic surgery practice. Gender inequality is also obvious, with only 13 female cardiothoracic surgeons registered so far.
For a long time, thoracic surgery had no separate certification pathway so most cardiothoracic surgeons had to be trained in and perform both cardiac and thoracic surgery cases. Few surgeons dedicate their efforts to thoracic surgery alone and are mostly operating on complex cases and engaged in initiating a minimally invasive thoracic surgery practice. Due to the lack of thoracic surgery service in trauma centers, several general surgeons start to get training in thoracic surgery to help patients in remote areas mainly performing ER thoracotomies and evacuation of retained hemothorax. Surgical oncologists operate on upper GIT, performing esophageal surgery with a limited number of surgical oncologists dedicating their practice to thoracic oncology surgery, mainly performing esophageal cancer, lung cancer and mesothelioma surgery (21,22).
Health care system: Who pays for surgery?
There are three major categories of thoracic surgery service in Egypt; the first and largest is the public governmental sector, which offers full reimbursement for all basic diagnostic and therapeutic interventions. The hospitals integrated in this sector (which include University hospitals, ministry of health public hospitals and national cancer centers) serve more than half of all Egyptian patients. Secondly, is the health insurance sector, which allows for the same standard options provided by the public hospitals in addition to limited additional diagnostics and therapeutic options. They serve mainly children from birth till finishing higher education, current and retired employees. This accounts for about 35% to 40% of patients with a likelihood to expand this coverage as there is a new project for comprehensive health insurance started in 2018 and is expected to attain full coverage in 2023. Finally, there are private hospitals/clinics that cater to out-of-pocket payers and those with national and international private insurance coverage (23). Today we have 31 thoracic surgery services: 18 in university hospitals, 7 in public hospitals and 6 in military hospitals. The number of private thoracic surgery units is not estimated as academic and public hospital surgeons are allowed to work in private hospitals outside their working hours, so they are highly mobile between large varieties of private hospitals.
Current situation and workload
The pattern of thoracic surgery cases is much different from that of the West and China and may be more similar to other countries like India in the form of more predominance of inflammatory diseases which include TB and fungal infection and bronchiectasis much more than lung cancer. Another example is the much different demographic distribution as Egypt has lower smoking rates in females compared to most countries (24). That necessitates having a national database to improve registry, research, and multicenter trials to develop our more realistic guidelines that match with the type of patient, our economics and the available services.
Authors collected data from the clinical audit of 9 major thoracic surgery centers. Results show a mean 1,533 cases per year were performed during the last 3 years (A major center was defined as center with more than 100 major cases per year) with mean of 170.3 per center (ranging from 100–330). As per operation, analysis of the last 3 years showed that the most common operation done was decortication either open or VATS followed by lobectomy and thymectomy in most centers. VATS decortication showed good results in terms of hospital stay, pain and need for another intervention with less rates of conversion to open thoracotomy with improvement of the learning curve (25-28).
Mesothelioma surgery was among the most common operations done made in two centers likely very close to the industrial areas where asbestos is still in use. One center had an average of 12 esophagectomies per year. Most other centers do not have a regular esophageal surgery or do not operate on them independently, instead they operate in collaboration with GI surgeons. VATS cases to total cases per institution were (30.5%) ranging from 17.8% to 51.2%.
Lung cancer surgery in Egypt
Regional variations in lung cancer epidemiology have been well documented and are attributable to societal, economic and lifestyle differences across different regions. The estimated number of new lung cancer cases in the Middle East area (MEA) in 2018 was approximately 80,000 (29). There is a high variance in incidence and mortality due to lung cancer in MEA. As per GLOBOCAN 2020 (30), Turkey reported the highest age standardized rate (ASR) for incidence as well as mortality rate per 100,000 population at 40.0 and 35.9, while Saudi Arabia had the lowest ASR at 5.1 new cases and 4.6 deaths per 100,000 population. The Egyptian rates are shown in Table 1 and represent numbers at the lower end of the spectrum among Middle East and African countries
Table 1. Number of new lung cancer cases and cancer related death in Egypt (31).
| Country | New cases (% of cancer cases) | Deaths (% of total cancer-related deaths) |
Age standardized incidence rate per 100,000 | Age standardized mortality rate per 100,000 |
|---|---|---|---|---|
| Egypt | 4.9 | 6.5 | 8 | 7.2 |
International guidelines recommended surgical resection as a treatment of choice in patients with stage I–II non-small cell lung cancer (NSCLC), who present with good performance status and have a resectable and operable disease (32). Thus, Egyptian thoracic surgeons along with other specialists should be involved in determining the safest and most effective management approach. Staging and diagnosis prior to surgery facilitate optimal surgery strategy and help to avoid unnecessary surgeries.
Minimally invasive techniques like VATS or robotic-assisted thoracic surgery (RATS) have been found to decrease the length of postoperative hospital stay and improved long-term survival (32). Thoracoscopic lobectomy is associated with lower postoperative mortality and morbidity (33-36). Based on its favorable profile on postoperative recovery and morbidity, VATS is now considered as the standard of care for patients with early-stage resectable NSCLC (37,38). RATS is not available in Egypt but out of 35 centers performing thoracic surgery, only four centers would perform routine thoracoscopic lobectomy for early-stage NSCLC. Heterogeneity in the level of diagnostic and therapeutic options remains the crux of the lung cancer problem in Egypt (23).
Egypt lies at the confluence of Asian and Caucasian races, posing a separate ethnic background for determining the treatment approach. In addition, Egypt, being part of the MEA, is a large geographical area comprising people of several other races and ethnicities. This increases the importance of application of an MDT-based multi-modal approach to deliver the best possible NSCLC treatment. Unfortunately, fewer than 10% of all patients with lung cancer have access to a multidisciplinary team (23).
Involvement of primary care physicians in the MDT panel may help in the capacity building of this group, which would ultimately result into early disease recognition and initiating therapy earlier (39). Further, MDT may have a role in encouraging population-based surveillance systems generating epidemiological data on NSCLC epidemiology in Egypt, encouraging the clinical trials of newer adjuvant-targeted therapies to enhance access to newer therapies. There is a lack of availability of the specialists at a given time and financial constrains to provide tools of communication and arrange frequent MDTs (40,41). Hence, the limited configuration of an effective MDT needs to be determined to maximize the cost-effectiveness and serve as many patients as possible. Providing teams with resources and the latest technology to connect virtually will help in knowledge sharing across the specialties more effectively and benefit a larger patient population. Ardila et al. recently proposed a deep learning algorithm that uses a patient’s current and prior CT volumes to predict the risk of NSCLC (42). Integrating artificial intelligence approaches in diagnostics can be an approach that an MDT could use to optimize the diagnostics with more accuracy and consistency especially with a low number of expert Egyptian thoracic surgeons and a large geographical area requiring coverage.
The burden of tuberculosis in Egypt
Tuberculosis has been in Egypt since the very beginning as reports suggest from studying the papyri, certain funerary portraits from the walls of tomb chambers and meticulous examination of the actual mummified bodies of the ancient Egyptians (1). In their report “tuberculosis in Egypt “Abaza and Sami stated in 1947 that artificial pneumothorax was induced in 1,354 patients (in the dispensaries and sanatoria, excluding the cases done at the University Hospital and private practice which were quite numerous) during the year 1945. It is interesting to know that they reported that 37% (500 patients) of those cases had thoracoscopic section of adhesions done by 4 operators. Phrenic nerve paralysis was used in 14% of admissions as an occasional accessory to artificial pneumothorax in cases with adhesions not suitable for intrapleural pneumonolysis. The nerve was crushed in the majority of cases. During the same year, 37 thoracoplasties were done in the two main sanatoria, representing 1.4 percent of admissions. Extrapleural pneumothorax had been tried since 1939 at the University Hospital and the sanatoria but complications made it an unpreferred approach (3). Meanwhile, Monaldi’s trans-pleural decompression was adopted by Dr. Abdel Raouf Hassan and he modified specific instruments to do it (43). In 2019, the estimated number of new TB cases was about 10 million people world-wide. Meanwhile, the incidence rate of TB in Egyptian community in 2019 was 12 per 100,000 people according to the World Health Organization estimate in 2020 (44). Egypt has been involved in early detection, delivery of suitable chemotherapeutic drugs, and prevention of TB transmission (45).
Registration of TB cases is executed all over Egypt by the National TB Strategy of the National Tuberculosis Control Program (NTP). Over the past years, there has been great success in lowering the numbers of TB cases by applying Directly Observed Therapy Short Course (DOTS) strategy for TB management which helps to lower the disease burden (46).
Although medical therapy for pulmonary tuberculosis has expressed great results in the vast majority of cases, approximately 5% of them are still in need for surgical intervention (47,48) and due to severe pleural and hilar adhesions, thoracotomy has been employed more than thoracoscopic procedures in Egypt. Meanwhile, several studies still report the safety and applicability of using VATS in the surgical management of pulmonary TB (48,49).
Surgical management of pulmonary tuberculosis has begun 70 years ago, and many surgical methods have been developed as previously mentioned. Nowadays, The most frequent indications for surgery in our current practice include patients with drug-resistant TB who have persistent positive sputum for acid fast bacilli, patients on medical treatment with persistent localized cavity or bronchiectasis, entrapped lungs and recurrent or massive hemoptysis (50).
Indeed, the success of surgery requires a certain level of substantial thoracic surgical experience as cases are usually complex in addition to cooperation between thoracic surgeons and chest physicians for appropriate perioperative medical management (51).
The burden of foreign body inhalation
Foreign body (FB) aspiration is indeed a life-threatening condition with high morbidity rate (10% to 20%) worldwide (52). As the nature of aspirated FB is variable according to age, gender, dietary habits, and socioeconomic status (53), the most common aspirated FB in Egypt are nuts, beans, scarf pins and plastic objects (54,55). Other uncommon foreign bodies are also reported in Egypt like inhaled bullets and inhaled earrings (55).
Bronchoscopy with its diagnostic and therapeutic benefits is employed in many centers all over Egypt. The mean number of bronchoscopies carried out in 7 major thoracic centers is 1,428/year with a mean of 204 per center (ranging from 71 to 324) This is a true burden to the health workers due to the unbalanced geographical distribution which serves a large number of populations through a wide area that lacks experienced doctors who can manage patients with FB aspiration. Reports of chest physicians, pediatricians, ENT doctors whom perform bronchoscopy for foreign body inhalation are increasing in Egypt (56,57).
Rigid bronchoscope under general anesthesia is widely utilized for FB extraction in most Egyptian institutions due to its higher ventilation and visualization power compared to fiberoptic bronchoscopy. Furthermore, it is characteristic of its firm grip to grasp and manipulate the FB particularly for impacted FB. Conversely, other reports showed satisfactory results with using fiberoptic bronchoscope to remove distally located FB in adults and children (52,56,58,59).
In our current practice, scarf pins are a common inhaled FB particularly in young and middle-aged females who wears headscarves due to religious or traditional causes. The usual management includes the use of a rigid bronchoscope and less frequently flexible bronchoscopy (60). Those metal pins may travel down to the tertiary carina and its extraction can be troublesome, with an increased risk of iatrogenic airway injury. In few cases, the use of fluoroscopy-guided bronchoscopy, thoracotomy or video-assisted thoracoscopic surgery may be required for extraction. Postural drainage without using the forceps were also reported by Sersar in 2011 under the name of “Egyptian technique” (61). Elsayed et al. used the binding technique to get the scarfpin when it is impacted on the bronchial wall (62). Another novel technique was introduced to retrieve the aspirated metallic pin by inserting a magnet fixed to the bronchoscope sucker which proved as safe as the conventional approach (63).
It is important to ensure combination of rigid, flexible bronchoscopies together with varieties of forceps and other solutions for difficult extraction in every bronchoscopic unit dealing with emergency cases of foreign body inhalation. Continuous communication between thoracic surgeons, anesthesiologists, and pediatricians will provide optimal pre- and post-procedure management.
Chest trauma in Egypt
While old reports showed that blunt trauma due to road traffic accident is the 5th cause of death in Egypt (64), we consider this as an underestimated problem as there is no national reporting system to evaluate the exact burden of trauma. A study conducted before 2011 in a major trauma center in Egypt demonstrated that chest injuries were considered the second cause of mortality (17.7%) after head injuries (34.6%) for all registered deaths by cause of injury (65). This has changed dramatically during the subsequent years of Egyptian revolution where reports showed more than 60% of all cases of chest injuries were due to penetrating trauma (Figure 4) (67). Thoracic surgeons are part of trauma teams in all tertiary and university hospitals across Egypt. Thorax trauma severity score (TTSS) combines patient-related parameters with the anatomical and physiological parameters, and it can be easily calculated in the emergency room. It has been evaluated on Egyptian patients in two large trauma centres (68) Recent employment of VATS in trauma has led to shortened hospital stay and the less need for delayed open thoracotomy (69). Use of plating largely replaced wiring for surgical fixation of flail chest and sternal fracture (70-72).
Figure 4.

Lateral chest film: showing a whole blade of kitchen knife extending from spine posterior to just retrosternal anteriorly with the inserted chest tube (66).
Academic thoracic surgery
The Egyptian Society of Cardiothoracic Surgery (ESCTS) is the official responsible organization for the field of cardiothoracic surgery in Egypt. It was founded as a part of the Egyptian Society of Physicians in 1993, then as a separate society in 1996. It is concerned with education, research, training and spread of knowledge of cardiothoracic surgery in Egypt. The Cardiothoracic Surgeon (CTS) is an official publication of the Egyptian Society of Cardiothoracic Surgery, it is an open access journal dedicated to research across all fields of cardiac and thoracic surgery. The journal is currently receiving nearly equal contributions from national and international authors (Figure 5). CTS is the continuation of “the Journal of the Egyptian Society of Cardio-thoracic surgery” (JESCTS); The first issue of ECTS journal was published in 1994. It was first called The Bulletin of the Egyptian Society of Cardio-Thoracic Surgery. From January 1996, its name was changed to Journal of the Egyptian Society of Cardio-Thoracic Surgery (JESCTS) and started to have ISSN: 1110-578X. By the end of 2018 its name was changed again to Cardiothoracic Surgeon (CTS). Another Journal of the society was also started by that time carrying the name Egyptian Cardiothoracic Surgeon (ECTS) (73).
Figure 5.
Cover of “The Cardiothoracic Surgeon” Journal.
The number of surgeons who were promoted to associate professors and professors in the last 5 years were 48 and 28 respectively. Language is not a barrier as English is the second commonly used language in Egypt. Historically, almost all cardiothoracic surgeons in Egypt could manage most conventional thoracic surgeries. However, this has changed following the emergence of cardiac surgery centers, the increasing burden of cardiac patients requiring surgery during the least decades, and the establishment of a separate fellowship of cardiac surgery, moreover, a limited number of surgeons subspecialize as dedicated thoracic surgeons.
The imprints of western and eastern thoracic training schools are widely shown in the current advanced thoracic surgery practice in Egypt. Overseas training varied between Italy, Great Britain, Turkey, India and China (Shanghai Pulmonary Hospital) (60). So, we can find some Egyptian centers performing uniportal VATS (Figure 6), multiportal VATS, subxiphoidal VATS or mixed approaches according to the teaching school of the operating surgeon taking into consideration the increasing tendency toward uniportal surgery between many Egyptian surgeons. At those advanced centers, VATS lobectomy, VATS segmentectomy, VATS thymectomy, VATS decortication, thoracoscopic repair of chest wall deformities, and complex major thoracic procedures as sleeve resections, complex airway reconstruction and radical mesothelioma surgeries can be safely performed.
Figure 6.

Adoption of new techniques; uniportal VATS (Assiut University Heart Hospital, Assiut, Egypt). VATS, video-assisted thoracic surgery. This image is published with the participants’ consent.
By turn, to train other willing thoracic surgeons, multiple national training animal lab workshops are held on yearly basis under the patronage of the Egyptian society of cardiothoracic surgeons. Assiut VATS annual workshop (19), VATS workshop at the annual meeting of the Egyptian society of cardiothoracic surgeons and the occasional cadaveric thoracic surgery workshops (Figure 7) are considered as the main current national/international workshops to transfer expertise to the next generations of thoracic surgeons. Other minor workshops exist as well, but they do not run on regular basis. Visiting surgeons are another way for thoracic surgery training in Egypt through which some experienced surgeons move to other centers to perform personally or help others in performing some advanced surgeries. This could be applied by some national surgeons moving inside Egypt or by international surgeons visiting Egypt from time to time(19). On the other hand, some senior registrars who have basic knowledge get short time observerships at some advanced centers to get more knowledge about minimally invasive surgery.
Figure 7.

Junior surgeons during wet lab training session; Cadaveric VATS workshop (NTI, Cairo, Egypt. May 2018). VATS, video-assisted thoracic surgery; NTI, National Training Institute. This image is published with the participants’ consent.
COVID-19 and thoracic surgery service in Egypt
The impact of COVID-19 on Egypt has been serious as it has been on most of the world. In Egypt, from 3 January 2020 to 4 June 2021, there have been 265,489 confirmed cases of COVID-19 with 15,222 deaths, reported to WHO. As of 1 June 2021, a total of 2,698,411 vaccine doses have been administered (74).
The impact of the COVID-19 era on lung screening practice is interesting in Egypt as the cost of chest CT scan was as low as 25$ in private radiology centers, compared to 125$ for PCR, so we notice a high number of self-referrals to get a scan to exclude COVID-19 infection then consult a physician regarding abnormal findings and this has made a significant impact on the number of patients requiring surgery for accidentally discovered lesions but reports of this impact not yet been published. This comes contradictory with reports from several centers in the world that had an established LDCT lung cancer screening program reported that COVID-19 caused significant disruption in lung cancer screening, leading to a decrease in new patients screened and an increased proportion of nodules suspicious for malignancy once screening resumed (75,76).
Consequently, the thoracic surgery service has been negatively impacted with many centers cutting down their elective surgery service. Returning to the usual surgical routine is within the scope of every surgeon now. Several factors need to be taken into consideration; the limited resources as the chain of supplies, number of nurses, available ICU beds, personal protective equipment (PPE), the limited access to diagnostic procedures as pulmonary function tests, bronchoscopy and the availability of PCR, and other tests for every patient and medical staff (77).
Since February 2020, all healthcare services have been much affected by the COVID pandemic, including thoracic surgery services in Egypt. According to the phase of the pandemic there were different regulations regarding the continuation or suspension of elective surgery to enable the best use of doctors, nurses, and ICU beds to face the pandemic and decrease the incidence of cross infection, but there were clear instructions to manage emergencies and cancer related conditions without any delay. A tentative guide for thoracic surgeons in Egypt was jointly prepared by a number of major centers to help decision making during the COVID era (77). It was noticed that some cases of elective surgery like pectus excavatum were operated much less during this pandemic than before.
There is currently no lung transplantation program in Egypt, but advanced modalities have been utilized for the management of severe COVID-19 namely veno-venous ECMO. Although the outcome has been found to be dismal in Egypt with 100% mortality out of 16 cases, there have been reports coming from Egypt reporting the worldwide mortality to be around 49% (78,79). One reason to explain the poor outcome for ECMO in Egypt could be the delayed installment of the artificial lung after deterioration on prolonged mechanical ventilation which has been shown to be associated with a worse outcome for COVID-19 patients (79).
Future perspective and challenges
Undoubtedly, there has been an increasing number of dedicated thoracic surgeons over the past few years especially after the growing attraction of minimally invasive thoracic surgery which turned the heads away from the glory of cardiac surgery.
In an increasingly fast-changing medical world, above all in surgery, it has become crucial for thoracic surgeons not only to offer their patients the best safe and updated treatment but also to contribute to clinical research by sharing their results (80) Indeed, above all in academic settings, surgeons are frequently asked to provide postoperative results about new treatments, fast-tracking protocols, outcomes in old patients with several comorbidities, etc. Patients may be offered online data about the results of a specific surgeon whom they wish to lead their medical care. Additionally, hospitals are interested in evaluating the quality of care in an increasingly more conscious cost-effectiveness environment. The lack of properly designed databases can lead to deficiencies in reporting trials and prospective studies in cardiothoracic surgery (81).
Lung cancer mortality has dropped in several nations due to successful public health campaigns, such as smoking cessation (82) and therapeutic improvements particularly in the field of immunotherapy. In addition, annual low-dose CT (LDCT) screening programs have been found to reduce mortality from lung cancer by at least 20% among high-risk patients in large clinical trials (83,84). Several thoracic surgeons in Egypt are involved in establishing a national led project to instate a lung cancer screening program which may be aided by funding from international medical companies interested in detecting early lung cancer patients.
Thoracic surgery in Egypt had suffered from a long period of disinterest but during the last decade, we have observed an increasing passion to thoracic surgery again with the introduction of VATS as the main surgical approach to much of thoracic surgeries even that involving inflammatory diseases what was once thought of as not amenable for minimally invasive approach due to dense adhesions (85).
Advanced technologies have always been attractive to young surgeons, Moreover propagating VATS as the standard of care with being much illustrative for training shortens the learning curve for young surgeons and urges them to accept this specialty much readily than before, Also large centers like Shanghai center, with more than 8,000 cases per year, offer training opportunities for different countries with over 80% of the cases done via VATS which would attract more young residents to specialty (86,87).
Screening programs have always been the dream of all healthcare providers for lung cancer patients worldwide to be able to detect these patients earlier in order to have a much better prognosis. Egypt does not have a formal screening program but most of the doctors believe that low dose CT in high-risk groups is the most appropriate (88).
Lung transplantation in Egypt is a multifactorial dilemma. The religious part of this dilemma was much cleared after the announcement of the Grand Sheikh of Al-Azhar Mohammed Sayed Tantawi in 1997 that he wanted to donate his organs after death to patients in need (89). But still the social acceptance is very low, necessitating directed public programs of education involving medical, religious, and legal authorities to encourage Egyptians to accept the concept of cadaveric organ donation.
Conclusions
Thoracic surgeons in Egypt are optimistic about the future of their specialty. The rising interest among the younger population will push training programs to meet the interests of enthusiastic junior surgeons. Robotic surgery has been introduced in non-thoracic surgery and is likely to arrive in the field of thoracic surgery. The academic achievements of thoracic surgeons in Egypt seem to have an international impact and with more collaboration, a better impact is likely. While the ancient history of thoracic surgery in Egypt seems to be extra ordinary, the future perspectives promise to be more rewarding and the next decade may carry the trueness of the current dreams of thoracic surgeons in Egypt.
Supplementary
The article’s supplementary files as
Acknowledgments
The authors are extremely grateful for all cardiothoracic surgeons in Egypt whom their work and support made this review possible. The authors would like to thank Dr. Mohamed Abdelghany for his extreme effort and help in searching for the historical section and English-language editing of the manuscript; Dr. Said Abdelrazik, Mr. Atef Elazazy and Afif-Eldin Elsherif library for providing a copy of A. R Hassan Book; Ms. Celine Burnand for providing photos from her grandfather’s collection; Mr. Hassan Abdel Raouf Hassan and his family for providing information, photos and original copies of Abdel Raouf Hassan books; Dr. Zakaria Massoud’s family, Prof. Adel Adawy, Prof. Osama Farouk and the Egyptian Medical Association for their assistance in finding the historical articles; Dr. Ahmed Hussein and the Egyptian Medical Syndicate for providing information form their registry; Prof. Sameh Elamin, Prof. Mahmoud Elbatawy, Prof. Omar Shabban, Dr. Mona Mina, Prof. Mokhtar Madkour and Dr. Maiada K. Hashem for their wonderful effort and cooperation.
Funding: None.
Ethical Statement: the authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alan D. L. Sihoe) for the series “Thoracic Surgery Worldwide” published in Journal of Thoracic Disease. The article has undergone external peer review.
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-723/prf
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-21-723/coif). The series “Thoracic Surgery Worldwide” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
References
- 1.Cave AJE. The evidence for the incidence of tuberculosis in ancient Egypt. Br J Tuberc 1939;33:142-52. 10.1016/S0366-0850(39)80016-3 [DOI] [Google Scholar]
- 2.Kwiecinski J. Pectus excavatum in mummies from ancient Egypt. Interact Cardiovasc Thorac Surg 2016;23:993-5. 10.1093/icvts/ivw249 [DOI] [PubMed] [Google Scholar]
- 3.ABAZA MS , SAMI A. Tuberculosis in Egypt. Tubercle 1947;28:10-4. 10.1016/S0041-3879(47)80069-8 [DOI] [PubMed] [Google Scholar]
- 4.Milton H. MEDIASTINAL SURGERY. Lancet 1897;149:872-5. 10.1016/S0140-6736(01)96474-8 [DOI] [Google Scholar]
- 5.Ravitch MM. Progress in resection of the chest wall for tumor with reminiscences of Dr. Blalock. Johns Hopkins Med J 1982;151:43-53. [PubMed] [Google Scholar]
- 6.Hassan AR. Fouad I sanatorium, Helwan. Reminiscences of Twenty Years. 1946. [Google Scholar]
- 7.MASSOUD Z. Present concepts in the field of collapse therapy. J Egypt Med Assoc 1956;39:97-103. [PubMed] [Google Scholar]
- 8.BOCTOR HB . A case of bronchogenic carcinoma; pneumonectomy; metastases. J Egypt Med Assoc 1947;30:210-6. [PubMed] [Google Scholar]
- 9.BOCTOR HB . Semb thoracoplasty; a modification. J Egypt Med Assoc 1954;37:1212-5. [PubMed] [Google Scholar]
- 10.Elkhayat H. Operating while awaiting one’s death. YouTube.com2021. p. Available online: https://youtu.be/R8DtsnENwKU.
- 11.IBRAHIM H. A case of bullet in the pericardium. J Egypt Med Assoc 1951;34:36-40. [PubMed] [Google Scholar]
- 12.el-Mallah SH, Balbaa A, Abou Senna G, et al. Constrictive pericarditis with a report on 25 cases treated surgically. J Egypt Med Assoc 1968;51:490-508. [PubMed] [Google Scholar]
- 13.EL MALLAH SH , HASHEM M. Localized bilharzial granuloma of the lung simulating a tumour. Thorax 1953;8:148-51. 10.1136/thx.8.2.148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Megahed GE, Megahed GM, el-Mallah S, et al. Assessment of the effect of mitral commissurotomy on the cardiac output. J Egypt Med Assoc 1967;50:39-51. [PubMed] [Google Scholar]
- 15.el-Mallah SH, Balbaa AI, Abu-Senna GO, et al. Open heart surgery. The method used and the results in fifty two patients. J Egypt Med Assoc 1968;51:603-13. [PubMed] [Google Scholar]
- 16.cardiothoracic surgery deaprtment Asu, Egypt 50 years of cardiothoracic surgery in Egypt YouTube2014. p. Available online: https://youtu.be/ZpMM8yPJKR.
- 17.Abou El-Kassem AS. Video assisted thoracoscopy for the management of malignant pleural effusion. Journal of Egyptian Society of Cardiothoracic Surgery 1996;4:95-104. [Google Scholar]
- 18.Amer S, Helal A, El-Ashkar M. Video-assisted thoracoscopic managment of pericardial effusion. Journal of Egyptian Society of Cardiothoracic Surgery 1996;4:71-112. [Google Scholar]
- 19.Elkhayat H, Gonzalez-Rivas D. Right pneumonectomy for carcinoid tumor extending through the intermediate bronchus and the interlobar artery. J Vis Surg 2016;2:89. 10.21037/jovs.2016.04.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bank W. World Development Indicators. The World Bank. 2021. Available online: https://datacommons.org/place/country/EGY?topic=Demographics. Accessed 25 June 2021 2021.
- 21.Rahouma M, Aziz H, Ghaly G, et al. Survival in Good Performance Malignant Pleural Mesothelioma Patients; Prognostic Factors and Predictors of Response Asian Pac J Cancer Prev 2017;18:2073-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rahouma Ahmed M, Elkassem F, Loay I, et al. P2.04-031 Predictors of Pathological Complete Response (TRG=1) among Esophageal Cancer Cases; NCI Pooled Data. J Thorac Oncol 2017;12:S1015-6. 10.1016/j.jtho.2016.11.1411 [DOI] [Google Scholar]
- 23.Board CAIROJCE. The State of Lung Cancer in Egypt: Progress Is at Hand. In: IASLC news IASLC 2018. Available online: https://www.iaslc.org/iaslc-news/ilcn/state-lung-cancer-egypt-progress-hand. Accessed 07 June 2021.
- 24.Giovino GA, Mirza SA, Samet JM, et al. Tobacco use in 3 billion individuals from 16 countries: an analysis of nationally representative cross-sectional household surveys. Lancet 2012;380:668-79. 10.1016/S0140-6736(12)61085-X [DOI] [PubMed] [Google Scholar]
- 25.Elkhayat H. Uniportal VATS approach for treatment of empyema: Challenges and recommendations. Multimed Man Cardiothorac Surg 2018. doi: . 10.1510/mmcts.2018.058 [DOI] [PubMed] [Google Scholar]
- 26.Elkhayat H, Sallam M, Kamal M, et al. Thoracoscopic decortication for stage III empyema; a minimal invasive approach in a delayed presentation disease. Journal of the Egyptian Society of Cardio-Thoracic Surgery 2018;26:301-7. 10.1016/j.jescts.2018.10.003 [DOI] [Google Scholar]
- 27.Elsayed HH, Mostafa A, Fathy E, et al. Thoracoscopic management of early stages of empyema: is this the golden standard? J Vis Surg 2018;4:114. 10.21037/jovs.2018.05.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Farrag MA, Al Bawab HY, Mohamed Abd Elfattah NM, et al. Evaluation of the role of video - assisted thoracoscopic surgery in management of empyema. Egyptian Journal of Bronchology 2018;12:419-26. [Google Scholar]
- 29.Jazieh AR, Algwaiz G, Errihani H, et al. Lung Cancer in the Middle East and North Africa Region. J Thorac Oncol 2019;14:1884-91. 10.1016/j.jtho.2019.02.016 [DOI] [PubMed] [Google Scholar]
- 30.Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 31.GLOBOCAN. GLOBOCAN 2020: New Global Cancer Data. UICC. 2020. Available online: https://www.uicc.org/news/globocan-2020-new-global-cancer-data. Accessed 4/9/2021 2021.
- 32.McDonald F, De Waele M, Hendriks LE, et al. Management of stage I and II nonsmall cell lung cancer. Eur Respir J 2017;49:1600764. 10.1183/13993003.00764-2016 [DOI] [PubMed] [Google Scholar]
- 33.Alam N, Flores RM. Video-assisted thoracic surgery (VATS) lobectomy: the evidence base. JSLS 2007;11:368-74. [PMC free article] [PubMed] [Google Scholar]
- 34.Cheng D, Downey RJ, Kernstine K, et al. Video-assisted thoracic surgery in lung cancer resection: a meta-analysis and systematic review of controlled trials. Innovations (Phila) 2007;2:261-92. 10.1097/imi.0b013e3181662c6a [DOI] [PubMed] [Google Scholar]
- 35.Shaw JP, Dembitzer FR, Wisnivesky JP, et al. Video-assisted thoracoscopic lobectomy: state of the art and future directions. Ann Thorac Surg 2008;85:S705-9. 10.1016/j.athoracsur.2007.11.048 [DOI] [PubMed] [Google Scholar]
- 36.Whitson BA, Andrade RS, Boettcher A, et al. Video-assisted thoracoscopic surgery is more favorable than thoracotomy for resection of clinical stage I non-small cell lung cancer. Ann Thorac Surg 2007;83:1965-70. 10.1016/j.athoracsur.2007.01.049 [DOI] [PubMed] [Google Scholar]
- 37.Elkhouly A, Pompeo E. Conversion to thoracotomy in thoracoscopic surgery: damnation, salvation or timely choice? Shanghai Chest 2018;2:2. 10.21037/shc.2017.12.03 [DOI] [Google Scholar]
- 38.Elkhouly AG, Sorge R, Rogliani P, et al. Ergonomical Assessment of Three-Dimensional Versus Two-Dimensional Thoracoscopic Lobectomy. Semin Thorac Cardiovasc Surg 2020;32:1089-96. 10.1053/j.semtcvs.2020.05.018 [DOI] [PubMed] [Google Scholar]
- 39.Nwagbara UI, Ginindza TG, Hlongwana KW. Health systems influence on the pathways of care for lung cancer in low- and middle-income countries: a scoping review. Global Health 2020;16:23. 10.1186/s12992-020-00553-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Powell HA, Baldwin DR. Multidisciplinary team management in thoracic oncology: more than just a concept? Eur Respir J 2014;43:1776-86. 10.1183/09031936.00150813 [DOI] [PubMed] [Google Scholar]
- 41.Prabhakar CN, Fong KM, Peake MD, et al. The effectiveness of lung cancer MDT and the role of respiratory physicians. Respirology 2015;20:884-8. 10.1111/resp.12520 [DOI] [PubMed] [Google Scholar]
- 42.Ardila D, Kiraly AP, Bharadwaj S, et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat Med 2019;25:954-61. 10.1038/s41591-019-0447-x [DOI] [PubMed] [Google Scholar]
- 43.Hassan AR. Endo-cavitary Aspiration (Monaldi Operation): New Developments in Technique, Instruments and Aparatus. Association of Authorship, Tanslation & Publication Press; 1949. [Google Scholar]
- 44.Organization WH. Tuberculosis Country Profiles. 2020. Available online: https://worldhealthorg.shinyapps.io/tb_profiles/?_inputs_&entity_type=%22country%22&lan=%22EN%22&iso2=%22EG%22. Accessed 29 May 2021 2021.
- 45.Sobh E, Kinawy SA, Abdelkarim YM, et al. The pattern of tuberculosis in Aswan Chest Hospital, Egypt. Int J Mycobacteriol 2016;5:333-40. 10.1016/j.ijmyco.2016.08.001 [DOI] [PubMed] [Google Scholar]
- 46.Negm MF, Allam AH, Goda TM, et al. Tuberculosis in Upper and Lower Egypt before and after directly observed treatment short-course strategy: a multi-governorate study. Egyptian Journal of Bronchology 2019;13:722-9. 10.4103/ejb.ejb_47_19 [DOI] [Google Scholar]
- 47.Botianu PV, Dobrica AC, Butiurca A, et al. Complex space-filling procedures for intrathoracic infections - personal experience with 76 consecutive cases. Eur J Cardiothorac Surg 2010;37:478-81. [DOI] [PubMed] [Google Scholar]
- 48.Han Y, Zhen D, Liu Z, et al. Surgical treatment for pulmonary tuberculosis: is video-assisted thoracic surgery "better" than thoracotomy? J Thorac Dis 2015;7:1452-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yen YT, Wu MH, Lai WW, et al. The role of video-assisted thoracoscopic surgery in therapeutic lung resection for pulmonary tuberculosis. Ann Thorac Surg 2013;95:257-63. 10.1016/j.athoracsur.2012.09.034 [DOI] [PubMed] [Google Scholar]
- 50.Mohsen T, Zeid AA, Haj-Yahia S. Lobectomy or pneumonectomy for multidrug-resistant pulmonary tuberculosis can be performed with acceptable morbidity and mortality: a seven-year review of a single institution’s experience. J Thorac Cardiovasc Surg 2007;134:194-8. 10.1016/j.jtcvs.2007.03.022 [DOI] [PubMed] [Google Scholar]
- 51.Mohamed E, Ghaffar AA, Aboelwafa W, et al. Indications and outcomes of pneumonectomy for benign diseases: A single-center experience. The Egyptian Cardiothoracic Surgeon 2021;3:70-9. [Google Scholar]
- 52.Nasir ZM, Subha ST. A Five-Year Review on Pediatric Foreign Body Aspiration. Int Arch Otorhinolaryngol 2021;25:e193-9. 10.1055/s-0040-1709739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hamad AM, Elmistekawy EM, Ragab SM. Headscarf pin, a sharp foreign body aspiration with particular clinical characteristics. Eur Arch Otorhinolaryngol 2010;267:1957-62. 10.1007/s00405-010-1295-y [DOI] [PubMed] [Google Scholar]
- 54.Sersar SI, Rizk WH, Bilal M, et al. Inhaled foreign bodies: presentation, management and value of history and plain chest radiography in delayed presentation. Otolaryngol Head Neck Surg 2006;134:92-9. 10.1016/j.otohns.2005.08.019 [DOI] [PubMed] [Google Scholar]
- 55.Elkhayat H, Ayyad MAS. Outcomes of Impaction of Unusual Foreign Bodies in the Aero-digestive Tracts. J Surg Clin Pract 2017;1. [Google Scholar]
- 56.Korraa E, Madkour A, Wagieh K, et al. Bronchoscopic foreign body extraction in a pulmonary medicine department: a retrospective review of egyptian experience. J Bronchology Interv Pulmonol 2010;17:39-44. 10.1097/LBR.0b013e3181cd5ca2 [DOI] [PubMed] [Google Scholar]
- 57.Albirmawy OA, Elsheikh MN. Foreign body aspiration, a continuously growing challenge: Tanta University experience in Egypt. Auris Nasus Larynx 2011;38:88-94. 10.1016/j.anl.2010.05.010 [DOI] [PubMed] [Google Scholar]
- 58.Madkour A, Sharkawy S, Elmansoury A. The efficacy of fiberoptic bronchoscopy through laryngeal mask airway in pediatric foreign body extraction. Egyptian Journal of Bronchology 2014;8:57. 10.4103/1687-8426.137354 [DOI] [Google Scholar]
- 59.Ma W, Hu J, Yang M, et al. Application of flexible fiberoptic bronchoscopy in the removal of adult airway foreign bodies. BMC Surg 2020;20:165. 10.1186/s12893-020-00825-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Al-Sarraf N, Jamal-Eddine H, Khaja F, et al. Headscarf pin tracheobronchial aspiration: a distinct clinical entity. Interact Cardiovasc Thorac Surg 2009;9:187-90. 10.1510/icvts.2009.207548 [DOI] [PubMed] [Google Scholar]
- 61.Sersar SI. The Egyptian technique revisited (Sersar-Mansoura technique). How to remove some inhaled foreign bodies through rigid bronchoscopy without using a forceps. Rev Port Pneumol 2011;17:222-4. 10.1016/j.rppneu.2011.05.004 [DOI] [PubMed] [Google Scholar]
- 62.Elsayed AAA, Mansour AA, Amin AAA, et al. Bending of an Aspirated Pin During Rigid Bronchoscopy: Safeguards and Pitfalls. J Bronchology Interv Pulmonol 2018;25:245-7. 10.1097/LBR.0000000000000490 [DOI] [PubMed] [Google Scholar]
- 63.Elsayed HH, Mostafa AM, Soliman S, et al. A magnet built on bronchoscopic suction for extraction of tracheobronchial headscarf pins: a novel technique and review of a tertiary centre experience. Interact Cardiovasc Thorac Surg 2016;22:531-6. 10.1093/icvts/ivw006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.World Health Organization. Regional Office for the Eastern M. Injury surveillance: a tool for decision-making: annual injury surveillance report, Egypt, 2009. 2010. [Google Scholar]
- 65.Mahran DG, Farouk OA, Qayed M, et al. Hospitalized injuries and deaths in a trauma unit in upper Egypt. Int J Crit Illn Inj Sci 2013;3:235-40. 10.4103/2229-5151.124108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eslam M, Elkhayat H, Amin A, et al. Retrieving a missed whole kitchen knife blade from a victim’s chest cavity. Can lateral chest X-ray film still be used in penetrating chest trauma patient? Journal of the Egyptian Society of Cardio-Thoracic Surgery 2016;24:341-4. 10.1016/j.jescts.2016.12.003 [DOI] [Google Scholar]
- 67.El Saied AM, Rizk WH. Penetrating Chest Injuries after Egyptian Revolution. Clinics in Surgery 2020;5:1082-85. [Google Scholar]
- 68.Zahran MR, Elwahab AAEMA, El Nasr MMA, et al. Evaluation of the predictive value of thorax trauma severity score (TTSS) in thoracic-traumatized patients. The Cardiothoracic Surgeon 2020;28:3. 10.1186/s43057-020-0015-7 [DOI] [Google Scholar]
- 69.Elkhayat H, Salama Ayyad M, Emad M, et al. Thoracoscopic evacuation compared with reinsertion of thoracostomy tube in persistent traumatic hemothorax. Journal of Current Medical Research and Practice 2018;3:81-6. 10.4103/JCMRP.JCMRP_123_18 [DOI] [Google Scholar]
- 70.Elkhayat H, Nousseir H. Fixing a Traumatic Sternal Fracture Using Stainless Steel Wires. Trauma Mon 2016;21:e27231. 10.5812/traumamon.27231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Abd-Elnaim MK, Ahmed E-M, Mohamed Abd-Elkader O, et al. Plating versus wiring for fixation of traumatic rib and sternal fractures. Journal of the Egyptian Society of Cardio-Thoracic Surgery 2017;25:356-61. 10.1016/j.jescts.2017.08.005 [DOI] [Google Scholar]
- 72.Ahmed K, Nady MA. Sternal reconstruction using locking compression plates (LCP): our experience in Egypt, a case series. J Cardiothorac Surg 2020;15:224. 10.1186/s13019-020-01266-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Surgery ESoC. The Cardiothoracic Surgeon. springeropen Online. 2021. Available online: https://cts.springeropen.com/about. Accessed 8 July 2021 2021.
- 74.Organization WH. WHO Coronavirus (COVID-19) Dashboard. World Health Organization. 2021. Available online: https://covid19.who.int/region/emro/country/eg. Accessed 4 June 2021 2021.
- 75.Dinmohamed AG, Visser O, Verhoeven RHA, et al. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. Lancet Oncol 2020;21:750-1. 10.1016/S1470-2045(20)30265-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Van Haren RM, Delman AM, Turner KM, et al. Impact of the COVID-19 Pandemic on Lung Cancer Screening Program and Subsequent Lung Cancer. J Am Coll Surg 2021;232:600-5. 10.1016/j.jamcollsurg.2020.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ghoniem A, Abdellateef A, Osman AI, et al. A tentative guide for thoracic surgeons during COVID-19 pandemic. Cardiothoracic Surgeon 2020;28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Elsayed HH. Dexamethasone for treatment of severe COVID-19, a surprise? The Cardiothoracic Surgeon 2020;28:22. 10.1186/s43057-020-00032-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Elsayed HH, Hassaballa AS, Ahmed TA, et al. Extracorporeal membrane oxygenation (ECMO) in patients with severe COVID-19 adult respiratory distress syndrome: a systematic review and meta-analysis. The Cardiothoracic Surgeon 2021;29:9. 10.1186/s43057-021-00046-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nachira D, Bertolaccini L, Ismail M, et al. How to create a surgical database? J Thorac Dis 2018;10:6352-5. 10.21037/jtd.2018.10.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jellison S, Nolan J, Vo N, et al. Reporting of interventions used in anesthesiology trials: analysis using the Template for Intervention Description and Replication (TIDieR) checklist. J Clin Epidemiol 2020;118:115-6. 10.1016/j.jclinepi.2019.11.004 [DOI] [PubMed] [Google Scholar]
- 82.Moolgavkar SH, Holford TR, Levy DT, et al. Impact of reduced tobacco smoking on lung cancer mortality in the United States during 1975-2000. J Natl Cancer Inst 2012;104:541-8. 10.1093/jnci/djs136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.National Lung Screening Trial Research Team ; Church TR, Black WC, et al. Results of initial low-dose computed tomographic screening for lung cancer. N Engl J Med 2013;368:1980-91. 10.1056/NEJMoa1209120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med 2020;382:503-13. 10.1056/NEJMoa1911793 [DOI] [PubMed] [Google Scholar]
- 85.Elkhayat H, Kaya S, Ghoneim A, et al. Video assisted thoracoscopic surgery (VATS) safety and feasibility in benign pathologies. J Tuberc Ther 2017;1:103. [Google Scholar]
- 86.Sihoe AD. Opportunities and challenges for thoracic surgery collaborations in China: a commentary. J Thorac Dis 2016;8:S414-26. 10.21037/jtd.2016.03.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Elkhayat H, Gonzalez-Rivas D, Yang Y, et al. Video Assisted Thoracoscopic Surgery Workshop in Shanghai Pulmonary Hospital: A Thoracic Surgeon’s Lifetime visit made Easy. Suntext Review of Surgery 2020;1:109. [Google Scholar]
- 88.Mohamed-Hussein A, Makhlouf H, Adam M. Attitudes of lung cancer screening practice in chest physicians in middle-income countries: an update. The Egyptian Journal of Chest Diseases and Tuberculosis 2018;67:281. 10.4103/ejcdt.ejcdt_35_17 [DOI] [Google Scholar]
- 89.Budiani D. Facilitating Organ Transplants in Egypt: An Analysis of Doctors’ Discourse. Body & Society 2007;13:125-49. 10.1177/1357034X07082256 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


