Abstract
Hydroxytyrosol (HT) and punicalagin (PC) exert cardioprotective and antiatherosclerotic effects. This study evaluated the effect of an oral supplement containing HT and PC (SAx) on dyslipidemia in an adult population. A randomized, double-blind, controlled, crossover trial was conducted over a 20-week period. SAx significantly reduced the plasma levels of triglycerides (TG) in subjects with hypertriglyceridemia (≥150 mg/dL) (from 200.67 ± 51.38 to 155.33 ± 42.44 mg/dL; p < 0.05), while no such effects were observed in these subjects after the placebo. SAx also significantly decreased the plasma levels of low-density lipoprotein cholesterol (LDL-C) in subjects with high plasma levels of LDL-C (≥160 mg/dL) (from 179.13 ± 16.18 to 162.93 ± 27.05 mg/dL; p < 0.01), while no such positive effect was observed with the placebo. In addition, the placebo significantly reduced the plasma levels of high-density lipoprotein cholesterol (HDL-C) in the total population (from 64.49 ± 12.65 to 62.55 ± 11.57 mg/dL; p < 0.05), while SAx significantly increased the plasma levels of HDL-C in subjects with low plasma levels of HDL-C (<50 mg/dL) (from 44.25 ± 3.99 to 48.00 ± 7.27 mg/dL; p < 0.05). In conclusion, the supplement containing HT and PC exerted antiatherosclerotic and cardio-protective effects by considerably improving dyslipidemia in an adult population, without co-adjuvant treatment or adverse effects.
Keywords: cardiovascular disease, atherosclerosis, hydroxytyrosol, punicalagin, dyslipidemia, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides
1. Introduction
Cardiovascular diseases (CVDs) remain the leading cause of disease burden in the world. An estimated 17.9 million people died from CVDs in 2019, representing 32% of all global deaths [1]. The recommendation by the World Health Organization (WHO) to help reduce the global burden of CVD is designed to provide counseling and adequate treatment for at least 50% of eligible people (defined) as aged 40 years or older and at high risk of CVD) by 2025 [2]. People considered to be at high risk for CVD are those with one or more risk factors, such as dyslipidemia, arterial hypertension, diabetes, or previously established disease [3]. To reduce the global burden of CVD, early detection and primary prevention are essential [3], and the WHO considers subjects aged 40–80 years, without a known baseline history of CVD, to be the target population in primary prevention efforts [2].
It has been widely recognized that most CVDs can be prevented by addressing behavioral risk factors, such as unhealthy diet, physical inactivity, and harmful tobacco and alcohol use, as well as appropriate control of risk conditions for CVDs, including dyslipidemia, arterial hypertension, diabetes and obesity [4]. Although the remarkable success of pharmacotherapy and preventive efforts have been introduced in the past decades, CVDS still constitutes a public health challenge as a top cause of morbidity, loss of useful life years, and mortality worldwide [1]. Therefore, any efforts for the prevention of CVD should be strongly encouraged.
Atherosclerosis, otherwise known as an atherosclerotic vascular disease (ASVD), is the main cause of mortality in CVD [5]. In ASVD, the buildup of plaques within blood vessels, resulting in the restriction of blood flow, with a potential risk of rupture, contributes to the development of heart attacks (myocardial infarction) and strokes, which can be fatal [6].
Dyslipidemia is one of the major risk factors for the development and progression of ASVD and CVDs [7,8]. Dyslipidemia includes a wide range of lipid abnormalities and may involve a combination of increased plasma levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG), or decreased high-density lipoprotein cholesterol (HDL-C). The prevention and sensible management of dyslipidemia can positively modify CV morbimortality [8]. Therefore, an effective solution with few or no adverse effects and high adherence, could reduce the ASVD morbimortality and, CVDs.
Polyphenols are becoming increasingly accepted as therapeutic substances for addressing a wide range of diseases, such as ASVD and CVDs [9,10,11,12,13,14,15,16,17,18,19,20,21,22], and their risk factors [9,11,12,13,14,15,16,17,20,21,22,23,24,25,26]. Diverse studies have reported an inverse correlation between polyphenol consumption and the risk of CV events [10,18,23,27] and overall mortality [23,28,29,30]. Among these bioactive compounds, hydroxytyrosol (HT), from olives, and punicalagin (PC), from pomegranates, are noteworthy for their antioxidant, antiatherosclerotic, cardioprotective, neuroprotective, anticancer, and other effects [13,26,31,32,33,34,35,36]; in this article, we focus on their cardioprotective and antiatherosclerotic effects. According to various in vitro and in vivo studies, the cardioprotective and antiatherosclerotic properties of HT and PC can normalize dyslipidemia, arterial prehypertension and hypertension, diabetes mellitus, oxidative and nitrative statuses, proinflammatory statuses, prothrombotic statuses, endothelial dysfunction, obesity, metabolic syndrome, and mitochondrial dysfunction, modulate the expression of cardioprotective and antiatherosclerotic genes, and reduce the adverse effects of drug treatment, etc. [9,13,14,16,26,31,32,34,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52], through multiple pathways [9,13,16,26,31,32,33,34,45,46,47].
In a previous crossover, randomized, double-blind and controlled study, oral supplementation with a combination of HT and PC in middle-aged healthy adults showed anti-atherosclerotic effects by improving endothelial function, blood pressure and levels of circulating oxidized LDL, with more marked improvements in subjects with alterations of these atherosclerotic markers [14]. Data obtained in this clinical trial regarding the effect of this oral supplement on the lipid profile, especially in subjects with dyslipidemia are reported.
2. Materials and Methods
The present study was registered at http://clinicaltrials.gov under the number NCT02042742 (access date: 23 January 2014).
2.1. Design and Subjects
This was a crossover, randomized, double-blind and placebo-controlled clinical trial, which was conducted over 20 weeks. A full description of the methodology of the study has been previously reported [14]. Briefly, eligible participants were assigned at random to two double-blind 8-week treatment periods receiving the supplement or placebo separated by a washout period of 4 weeks. Participants (n = 84) were men and women, aged 45–65 years, recruited at the Nutrition Department of Hospital University La Paz in Madrid, Spain, who voluntarily agreed to take part in the study and gave written consent. Exclusion criteria were body mass index (BMI) ≥30 kg/m2, subjects receiving drug treatment for CV risk (e.g., dyslipidemia, hypertension, diabetes mellitus, etc.), presence of family background of premature vascular disease, metabolic syndrome, severe liver or renal dysfunction, cancer, and mental illness or low cognitive ability. Other exclusion criteria were the use of nutritional supplements, intensive physical activity, alcohol use (>30 g/day), and hypersensitivity or allergy to olive and pomegranate by-products. Women still experiencing menstrual cycles were also excluded.
All subjects gave their informed consent to take part in the study, which was approved by the Scientific Research and Ethics Committee of the HULP (Code 3799) in accordance with The Ethical Standards of The Declaration of Helsinki [53].
2.2. Intervention and Study Variables
The supplement (SAx) (Pomalive®, Euromed S.A., Mollet del Vallès, Barcelona, Spain) (patent in concession process) contained 3.3 mg of HT from a standardized olive fruit extract (Mediteanox®,) 65 mg of PC from a standardized pomegranate fruit extract (Pomanox® P30) and 331.7 mg of maltodextrin. Identically appearing placebo capsules contained 400 mg of maltodextrin. Subjects were instructed to take three capsules/day of the assigned product (SAx or placebo) with their meals and were instructed to maintain their normal dietary habits. They received the exact number of capsules (in blister packaging) required for each 8-week intervention period (SAx or placebo) during pre-period visits at the study center. Visits were scheduled at baseline and before and after each intervention period. Study variables included the following: (a) diet assessment, (b) anthropometric measurements, (c) vital signs, (d) biochemical analysis of the lipid profile, and (e) compliance with the study products and adverse effects.
The diet was recorded over three days (including one day of the weekend) [20]. Participants registered the weight of foods or, alternatively, cups, spoonfuls, etc., used for household measurements. Records were reviewed by a nutritionist during the study visits in the presence of the participant. The DIAL software (Alce Ingenieria S.L., Las Rozas de Madrid, MD, Spain) was used for the calculation of the energetic and nutritional content of foods and beverages consumed.
Anthropometric data (weight, height, BMI) were collected using standard techniques, adhering to international norms set out by the WHO [54] in the morning by trained personnel with the subject barefoot and wearing only underwear. A bioelectrical impedance analyzer (BIA) was used for estimating body composition (EFG ElectroFluidGraph®, Akern S.R.L., Pontassieve, Fl, Italy). Blood pressure and heart rate were measured using a 420 Spot Vital Signs Monitor (Welch Allyn, Skaneateles Falls, NY, USA), determining the mean of three readings.
At the beginning and end of each 8-week intervention period, fasting blood samples were collected for biochemical analysis. Samples were analyzed on the Olympus AU5400 Automated Chemistry Analyzer (Olympus Corporation, Izasa, CA, USA) for levels of total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C) and triglycerides. Results are expressed as mg/dL, values that were considered dyslipidemia were ≥200 mg/dL, ≥150 mg/dL, ≥160 mg/dL, and <50 mg/dL for total cholesterol, triglycerides, LDL-C, and HDL-C levels, respectively.
The participants’ compliance was determined through interviews and a comparison between the number of capsules supplied and that returned in the middle and at the end of each intervention period. When a participant had consumed ≥90% of the capsules supplied, he/she was deemed compliant. Any adverse effects observed during the study were logged. Any unfavorable, unwanted effects (diarrhea, constipation, nausea, vomiting, halitosis, etc.) that were reported by a participant and/or observed by the researchers were defined as adverse effects. No participants showed adverse effects during the study. The participants were informed of their right to leave the study at any time.
2.3. Statistical Analysis
In the present clinical trial, a sample size of 38 subjects was determined to be necessary to achieve 90% power (at α = 0.05) with a potential 20% dropout [14,55]. Qualitative data are presented as both counts and percentages. Quantitative data are presented as means ± standard deviations (SDs). The Kolmogorov–Smirnov test was used to assess whether the data were normally distributed, and Levene’s test was used to evaluate the homogeneity of the variances. The denominator’s degrees of freedom were estimated using Satterthwaite’s formula. The possible sequence effects, period effects, and residual effects that can occur in this type of crossover study were analyzed. Multiple comparisons were adjusted for using the Bonferroni method. Two-sided tests were applied, and a p-value < 0.05 was considered statistically significant. The statistical analyses were performed using the linear mixed model in the SAS Statistical Analysis Software, version 9.3 (SAS Institute Inc., Cary, NC, USA).
3. Results
3.1. Recruitment and Study Population
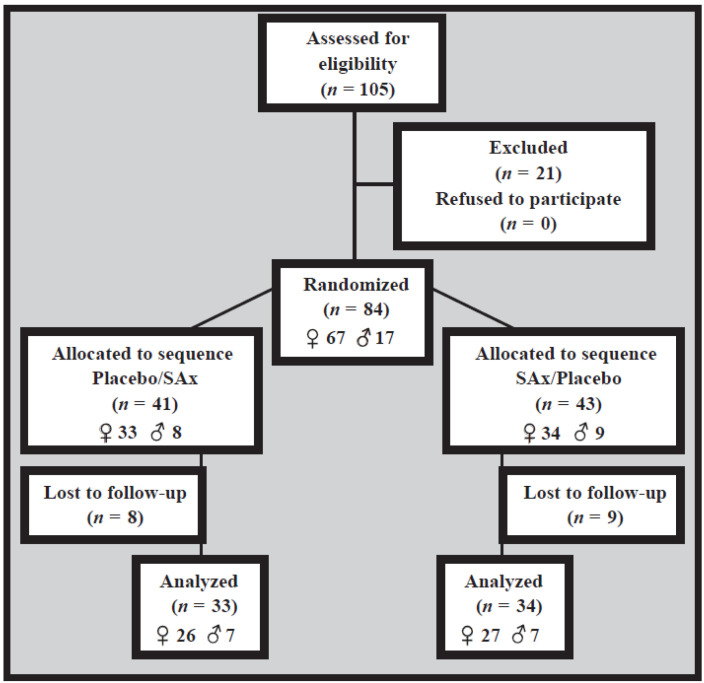
The present clinical trial was performed between February and June 2013. This study involved 84 apparently healthy subjects (17 males (20.2%) and 67 females (79.8%)) who were found to be suitable for inclusion. There were 17 participants subsequently lost to follow-up (nine in the SAx/Placebo sequence and eight in the Placebo/SAx sequence) for personal reasons (n = 15) and noncompliance with the treatment instructions (n = 2). As such, 67 participants (14 males (20.9%) and 53 females (79.1%)) completed the present 20-week clinical trial; only their results were included in the statistical analyses (Figure 1).
Figure 1.
Flow chart depicting the present study.
3.2. Baseline Characteristics
Regarding the baseline state in the present clinical trial, there were no significant differences between the participants assigned to the different intervention sequences (Placebo/SAx and SAx/Placebo) in gender, age, smoking habits, anthropometry, lipid profiles, or other variables. The average age of the population was 53.0 ± 4.5 years, and the average BMI was 24.6 ± 3.1 kg/m2 (Table 1).
Table 1.
Baseline characteristics of the participants.
| Placebo/SAx (n = 33) |
SAx/Placebo (n = 34) |
||
|---|---|---|---|
| Gender | (Female %, n) | 78.79 (26) | 79.41 (27) |
| Age | (years) | 53.21 ± 4.2 | 52.79 ± 4.8 |
| Smoking | (Smokers %, n) | 18.18 (6) | 26.47 (9) |
| Weight | (kg) | 66.26 ± 11.8 | 64.08 ± 10.9 |
| BMI | (kg/m2) | 24.64 ± 2.9 | 24.56 ± 3.2 |
| Waist circumference | (cm) | 80.51 ± 9.2 | 82.58 ± 9.8 |
| FM | (%) | 29.18 ± 6.7 | 28.76 ± 6.4 |
| FFM | (%) | 70.82 ± 6.7 | 71.24 ± 6.4 |
| MM | (%) | 48.03 ± 7.7 | 47.87 ± 5.5 |
| SBP | (mmHg) | 110.3 ± 13.1 | 110.9 ± 12.9 |
| DBP | (mmHg) | 74.06 ± 10.8 | 73.75 ± 9.5 |
| HR | (bpm) | 67.36 ± 8.9 | 70.41 ± 7.5 |
| TC | (mg/dL) | 226.7 ± 29.6 | 224.6 ± 35.4 |
| LDL-C | (mg/dL) | 144.3 ± 23.9 | 145.3 ± 28.6 |
| HDL-C | (mg/dL) | 66.25 ± 12.9 | 62.00 ± 12.6 |
| TG | (mg/dL) | 80.56 ± 24.6 | 86.52 ± 44.0 |
Data presented as means ± standard deviations (SDs). SAx: oral supplementation with hydroxytyrosol (HT) and punicalagin (PC); BMI: body mass index; FM: fat mass; FFM: fat-free mass; MM: muscle mass; SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; and TG: triglycerides. There were no significant differences in the baseline state between the two intervention sequences.
3.3. Dietary and Anthropometric Variables
Regarding the results for the dietary and anthropometric variables compared between the beginning and end of the different intervention periods, no significant differences were observed, nor were significant differences found between the different periods in terms of the changes in these variables (Table 2).
Table 2.
The dietary and anthropometric variables at the beginning and end of the supplementation, and placebo periods.
| SAx (n = 67) |
Placebo (n = 67) |
|||
|---|---|---|---|---|
| Energy | (kcal/day) | Start | 1923 ± 513.6 | 1864 ± 471.9 |
| End | 1891 ± 549.4 | 1881 ± 569.5 | ||
| Change | −31.88 ± 463.2 | 17.07 ± 355.5 | ||
| Carbohydrates | (%) | Start | 38.06 ± 6.5 | 38.46 ± 8.9 |
| End | 37.62 ± 6.3 | 39.06 ± 6.5 | ||
| Change | −0.439 ± 5.7 | 0.598 ± 8.1 | ||
| Proteins | (%) | Start | 17.24 ± 3.7 | 17.44 ± 2.9 |
| End | 17.43 ± 3.6 | 17.60 ± 3.1 | ||
| Change | 0.193 ± 4.4 | 0.164 ± 3.5 | ||
| Lipids | (%) | Start | 41.42 ± 6.3 | 40.48 ± 8.8 |
| End | 41.36 ± 5.7 | 40.19 ± 5.9 | ||
| Change | −0.067 ± 5.3 | −0.287 ± 8.0 | ||
| SFA | (%) | Start | 12.33 ± 2.9 | 12.46 ± 4.0 |
| End | 12.38 ± 2.8 | 12.03 ± 2.9 | ||
| Change | 0.049 ± 2.7 | −0.433 ± 4.2 | ||
| MUFA | (%) | Start | 19.10 ± 3.6 | 18.82 ± 4.9 |
| End | 19.56 ± 4.0 | 19.29 ± 3.5 | ||
| Change | 0.453 ± 3.8 | 0.470 ± 4.2 | ||
| PUFA | (%) | Start | 6.45 ± 2.3 | 5.60 ± 1.6 |
| End | 5.98 ± 1.7 | 5.46 ± 1.8 | ||
| Change | −0.470 ± 2.4 | −0.134 ± 1.4 | ||
| Total Cholesterol | (mg/dL) | Start | 350.5 ± 172.8 | 303.9 ± 150.4 |
| End | 328.1 ± 133.8 | 323.0 ± 115.9 | ||
| Change | −22.35 ± 210.8 | 19.04 ± 130.1 | ||
| Fiber | (g/d) | Start | 21.95 ± 7.8 | 21.71 ± 8.0 |
| End | 21.68 ± 8.9 | 20.47 ± 7.3 | ||
| Change | −0.275 ± 8.2 | −1.234 ± 6.5 | ||
| Weight | (kg) | Start | 65.10 ± 11.3 | 65.10 ± 11.2 |
| End | 64.93 ± 11.2 | 64.85 ± 11.3 | ||
| Change | −0.173 ± 1.3 | −0.249 ± 1.0 | ||
| BMI | (kg/m2) | Start | 24.58 ± 3.0 | 24.63 ± 3.0 |
| End | 24.51 ± 3.0 | 24.48 ± 3.0 | ||
| Change | −0.068 ± 0.5 | −0.151 ± 0.6 | ||
| Waist Circumference | (cm) | Start | 81.85 ± 9.0 | 81.24 ± 9.8 |
| End | 81.82 ± 9.6 | 81.25 ± 9.6 | ||
| Change | −0.034 ± 2.9 | 0.008 ± 3.7 | ||
| FM | (%) | Start | 29.16 ± 6.6 | 28.90 ± 6.5 |
| End | 29.56 ± 6.8 | 29.79 ± 7.2 | ||
| Change | 0.400 ± 2.8 | 0.891 ± 3.7 | ||
| FFM | (%) | Start | 70.84 ± 6.6 | 71.10 ± 6.5 |
| End | 70.44 ± 6.8 | 70.21 ± 7.2 | ||
| Change | −0.400 ± 2.8 | −0.891 ± 3.7 | ||
| MM | (%) | Start | 47.63 ± 6.2 | 47.52 ± 6.5 |
| End | 46.67 ± 5.7 | 46.44 ± 5.8 | ||
| Change | −0.970 ± 5.1 | −1.082 ± 5.8 |
Data expressed as means ± standard deviations (SDs). SAx: oral supplementation with hydroxytyrosol (HT) and punicalagin (PC); SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids; BMI: body mass index; FM: fat mass; FFM: fat-free mass; and MM: muscle mass. In the present clinical trial, no significant differences were observed between the beginning and end of the different intervention periods or in the changes.
3.4. Lipid Profile Variables
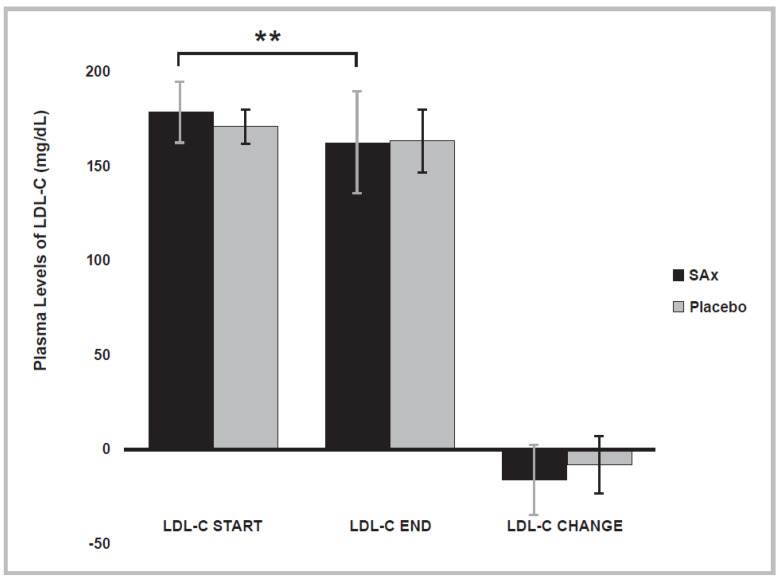
Table 3 shows the values obtained for the lipid-profile variables examined. Figure 2 shows a significant reduction after SAx treatment was observed in the plasma levels of LDL-C in subjects with initially high plasma levels of LDL-C (≥160 mg/dL) (SAx period start: 179.13 ± 16.18; end: 162.93 ± 27.05 mg/dL; p < 0.004). This significant effect did not occur in these subjects following placebo treatment.
Table 3.
Lipid-profile variables at the beginning and end of the supplementation and placebo periods in population with dyslipidemia.
| SAx (n = 67) |
Placebo (n = 67) |
|||
|---|---|---|---|---|
| TC | (mg/dL) (n = 49) |
Start End Change |
237.6 ± 26.0 234.9 ± 25.1 −2.776 ± 18.8 |
238.4 ± 20.0 233.0 ± 22.8 −5.388 ± 18.8 |
| LDL-C | (mg/dL) | Start | 179.1 ± 16.2 | 171.6 ± 9.1 |
| (n = 16) | End | 162.9 ± 27.1 ** | 163.6 ± 16.9 | |
| Change | −16.20 ± 18.5 | −8.063 ± 15.1 | ||
| HDL-C | (mg/dL) | Start | 44.25 ± 4.0 | 41.50 ± 5.2 |
| (n = 8) | End | 48.00 ± 7.3 * | 43.75 ± 8.3 | |
| Change | 3.750 ± 4.0 | 2.250 ± 5.4 | ||
| TG | (mg/dL) | Start | 200.7 ± 51.4 | 186.0 ± 51.5 |
| (n = 4) | End | 155.3 ± 42.4 * | 170.5 ± 50.3 | |
| Change | −45.33 ± 10.5 | −15.50 ± 73.1 |
Data expressed as means ± standard deviations (SDs); SAx: oral supplementation with hydroxytyrosol (HT) and punicalagin (PC); TC: total cholesterol; LDL-C: low-density lipoprotein cholesterol; HDL-C: high-density lipoprotein cholesterol; and TG: triglycerides. In the present clinical trial, significant differences were observed between the beginning and end of the SAx period (* p < 0.05, ** p < 0.01). There were no significant differences in the placebo period or in the changes in the different intervention periods.
Figure 2.
The plasma levels of low-density lipoprotein cholesterol (LDL-C) significantly decreased after SAx treatment (oral supplementation with hydroxytyrosol (HT) and punicalagin (PC)) (black color) in subjects with high plasma levels of LDL-C, a risk factor for CVD, (n = 16) (** p < 0.01). This effect was not observed after placebo treatment (gray color). The data represent the adjusted means ± standard deviations (SDs) from multivariate models.
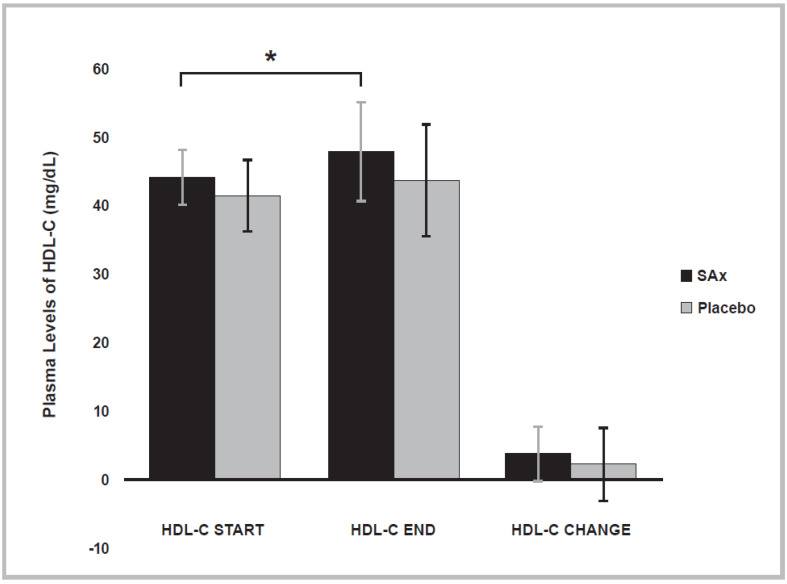
In addition, at the end of the placebo period, a significant decrease in the plasma levels of HDL-C was observed in the total population (Placebo period start: 64.49 ± 12.65; end: 62.55 ± 11.57 mg/dL; p < 0.016). After the SAx period, a significant increase in the plasma levels of HDL-C was observed in subjects with initially low plasma levels of HDL-C (SAx period start: 44.25 ± 3.99; end: 48.00 ± 7.27 mg/dL; p < 0.033). After the placebo period, this significant effect on plasma HDL-C levels was not observed in these subjects (Placebo period start: 41.50 ± 5.19; end: 43.75 ± 8.26 mg/dL; p < 0.464) (Figure 3). In the present clinical trial, only women showed low plasma levels of HDL-C. There were no men who presented low plasma levels of HDL-C.
Figure 3.
Plasma levels of high-density lipoprotein cholesterol (HDL-C) significantly increased after SAx treatment (oral supplementation with hydroxytyrosol (HT) and punicalagin (PC)) (black color) in subjects with low plasma levels of HDL-C, a risk factor for CVD, (n = 8) (* p < 0.05). This effect was not observed after placebo treatment (gray color). The data represent the adjusted means ± standard deviations (SDs) from multivariate models.
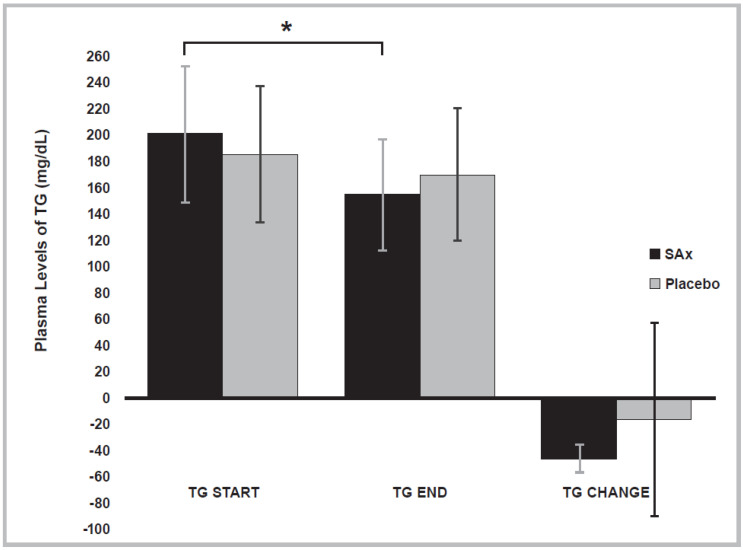
At the end of the SAx period, a significant decrease in the plasma levels of TG was observed in subjects with hypertriglyceridemia (≥150 mg/dL) (SAx period start: 200.67 ± 51.38; end: 155.33 ± 42.44 mg/dL; p < 0.017). This significant effect on the plasma levels of TG was not present after the placebo period in these subjects (Placebo period start: 186.00 ± 51.54; end: 170.50 ± 50.32 mg/dL; p < 0.700) (Figure 4).
Figure 4.
Plasma levels of triglycerides (TG) significantly decreased following SAx treatment (oral supplementation with hydroxytyrosol (HT) and punicalagin (PC)) (black color) in subjects with hypertriglyceridemia, a risk factor for CVD, (n = 4) (* p < 0.05). This effect was not observed after placebo treatment (gray color). The data repreScheme.
3.5. Compliance and Adverse Effects
No significant differences were observed in the numbers of capsules consumed between the different intervention periods or treatment sequences. More than 90% of the capsules provided were consumed by all the participants. No adverse effects derived from the consumption of any treatment were reported.
4. Discussion
The present clinical trial is the first study to evaluate the effects of the regular consumption of an oral supplement containing HT and PC on ASVD and CVD markers, such as dyslipidemia (high TC, high LDL-C, low HDL-C, and high TG), in primary prevention in an adult population. The intake of three capsules daily, which contained HT (9.9 mg) and PC (195 mg), for an 8-week period significantly decreased the plasma levels of LDL-C and TG and significantly increased the HDL-C levels in an adult population with dyslipidemia without co-adjuvant treatment, and no adverse effects were observed, even though they frequently occur when using lipid-lowering drugs (e.g., myopathies, renal dysfunction, hepatic dysfunction, rhabdomyolysis, flushing, itching, gastrointestinal irritation, and stomach ulcers) [56,57,58,59,60,61]. In addition, the supplement resulted in a high adherence to the treatment among the participants (>90%). As observed in our previous article, the supplement containing HT and PC produced a significant improvement in ASVD and CVD markers, such as endothelial dysfunction, arterial prehypertension and hypertension (both systolic blood pressure (SBP) and diastolic blood pressure (DBP)) as well as circulating plasma levels of oxLDL [14]. Several studies have shown improvements in dyslipidemia following the intake of HT [9,37,49,62,63,64,65,66,67] or PC [46,68,69,70,71,72,73]. However, most of the studies that have evaluated the effects of these bioactive compounds were performed in vitro or in experimental animals [37,49,50,52,62,63,67,71,74]; only some have involved humans [9,38,64,65,73], and even fewer have evaluated these compounds outside food matrices [14,66,68,75] or studied their combined synergistic effect [14].
An example of this is the study of Cao et al., who observed how dyslipidemia could be prevented by 17-week of supplementation with HT. The study evaluated the effects of various doses of HT (low-dose: 10 mg/kg/day, and high-dose: 50 mg/kg/day) vs. metformin (225 mg/kg/day) in mice with diverse metabolic disorders induced by a high-fat-diet (HFD), or in mice with obesity and type 2 diabetes mellitus (T2DM) (db/db-model mice). Low-dose HT produced significantly decreased fasting glucose levels in the db/db-model mice that were similar to those of the metformin group. In Cao et al.’s study, low- and high-dose HT notably and significantly improved the lipid profile in both the HFD and db/db mice without adverse effects, while metformin did not produce this positive effect in those mice. All the lipid variables were significantly increased under HFD treatment and effectively improved after treatment with both low- and high-dose HT (decreased plasma LDL-C levels (p < 0.01), decreased plasma TG levels (p < 0.01), reduced plasma free fatty acid levels (p < 0.01), increased plasma HDL-C levels and improved LDL-C/HDL-C ratios (p < 0.01)). As in our study, due to an increase in the plasma HDL-C levels, a significant reduction in TC was not observed by Cao et al. In addition, HT supplementation could decrease lipid deposits within the livers and muscle tissues of the HFD mice, through the inhibition of the sterol regulatory element-binding protein 1c/fatty acid synthase (SREBP–1c/FAS) pathway, reducing SREBP-1c levels, a well-known regulator of fatty acid and cholesterol synthesis in the liver [52].
The improvement of dyslipidemia with HT has also been reported in other studies, such as the study of Tabernero et al., where they evaluated the effect of HT and its lipophilic derivatives in rats with diverse metabolic disorders induced by a cholesterol-rich diet. The hypercholesterolemic diet was supplemented with 0.04% HT in the different HT groups. After 8-week, a significant reduction in the plasma levels of LDL-C and TC was observed in the HT groups, and there was not a significant decrease in plasma TG [62]. This amelioration of dyslipidemia with HT was also observed in the study of Zhang et al., in which HT was administered at a dose of 10 mg/kg/day orally to mice for 16-weeks. After this period of time, a marked and significant reduction in the plasma levels of the lipid parameters (TC, LDL-C, and TG) and an increase in the plasma levels of HDL-C were observed in the HT group, compared to the control group (by approximately 17.4% (p = 0.004), 15.2% (p = 0.003), 17.9% (p = 0.009), and 26.9% (p = 0.033), respectively)). HT improved hepatic steatosis and lipid deposition. The possible pathways for improving lipemia include the regulation of cholesterol metabolism via decreasing the phosphorylation of p38, followed by the activation of AMP-activated protein kinase (AMPK) and inactivation of nuclear factor-kappa B (NF-κB), which, in turn, trigger the blockade of sterol regulatory element-binding protein 2/proprotein convertase subtilisin/kexin type 9 (SREBP2/PCSK9) and the upregulation of low-density lipoprotein receptor (LDLR), apolipoprotein A-I (ApoAI), and ATP-binding membrane cassette transport protein A1 (ABCA1). These steps finally lead to a reduction in LDL-C and an increase in HDL-C in the circulation [67].
A crossover clinical trial with 60 prehypertensive men conducted by Lockyer et al. evaluated the effects of a phenolic-rich olive leaf extract (136.2 mg of oleuropein; 6.4 mg of HT) on lipid profiles, among other variables, during 6-week of treatment, followed by 4-week of washout. In the phenolic-rich olive leaf extract group, after 6-week, the researchers reported a reduction in the plasma levels 308 of TC (−0.32 (±SD 0.70) mmol/L, p = 0.002), LDL-C (−0.19 (±SD 0.56) mmol/L, p = 0.017), and TG (−0.18 (±SD 0.48) mmol/L, p = 0.008)); however, no significant changes were observed in the differences between the study treatments. Although these lipid-lowering effects were obtained in subjects who did not suffer from dyslipidemia, the researchers suggest that the possible mechanisms by which these lipid-lowering effects occur include a decrease in the activities of key cholesterol-regulatory enzymes, such as 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGR) (the main target of statins) and acyl-coenzyme A: cholesterol acyltransferase (ACAT), resulting in decreased cholesterol biosynthesis, impacting the flow of bile (increasing biliary cholesterol and bile acid concentrations) and leading to its increased fecal excretion [66].
On the other hand, with respect to the results observed with PC on lipid profiles, some authors, such as Kang et al., have observed improvements in dyslipidemia in mice, with these metabolic disorders induced by a HFD. Their study evaluated the effects of administering various doses of PC (low-dose: 10 mg/kg/day, and high-dose: 100 mg/kg/day) to these mice for 12-week. After PC administration, at both doses, there was a significant decrease in the plasma levels of TG, TC, and LDL-C, and a significant increase in those of HDL-C (low-dose: 14%, 16%, 42%, and 19%, respectively, and high-dose: 23%, 25%, 67%, and 35%, respectively) compared with the control HFD (n = 6) [46]. A pomegranate leaf extract (PLE) rich in PC produced improvements in the lipid profile in a mouse model in which hyperlipidemia and obesity were induced by a HFD. The treatment group was provided with 400 or 800 mg/kg/day of PLE for 5-week. The results after 5-week were very encouraging. Apart from the improvements in the other parameters evaluated, the study showed a marked and significant reduction in the plasma levels of TC and TG, and a significant improvement in the TC/HDL-C ratio (low-dose: approximately 35% (p < 0.01) and 56% (p < 0.01), respectively, and high-dose: approximately 29% (p < 0.05), 60% (p < 0.01), and 24% (p < 0.05), respectively)) versus the HFD group (n = 11). PLE also significantly attenuated the rise in plasma TG and inhibited intestinal fat absorption in these mice. PLE showed a significant difference in decreasing the appetite of obese mice fed a HFD but showed no effect in mice fed a normal diet [70].
In clinical trials, such as the one conducted by Esmaillzadeh et al., in 22 patients with T2DM and dyslipidemia, 14 women (63.6%) and eight men (36.4%) presented improvements in their lipid profiles after the consumption of 40 g/day of a concentrated pomegranate juice (CPJ) rich in PC for 8-weeks. Although these results showed a significant reduction in the plasma levels of TC (approximately 4%; p = 0.006) and LDL-C (approximately 8%; p = 0.006), and the LDL-C/HDL-C (approximately 10%; p < 0.001) and TC/HDL-C ratios (approximately 6%; p < 0.001), there were no significant changes in the plasma levels of TG or HDL-C versus the control group (pre-study period of 8-weeks without CPJ). There were no significant changes between these two periods. The researchers suggested, as a possible mechanism for the improvement of dyslipidemia through the consumption of a CPJ rich in PC, that a reduction in the liver’s levels of cholesterol esters but not an elevation in the fecal excretion of cholesterol or bile acids might affect cholesterol biosynthesis in the liver [73]. Along the same lines are the results observed by Estrada-Luna et al., in women with acute coronary syndrome (ACS), who took a daily dose of 20 g of microencapsulated pomegranate (MiPo) rich in PC for 4-week. After the consumption of MiPo by 11 subjects, there was an improvement in the lipid profiles in the fasting and postprandial conditions, among other parameters evaluated, as evidenced by a significant reduction in the plasma TG (p < 0.05; 16%, 8%, and 42% at 0, 4, and 8 h, respectively), TC (p < 0.05; between 8% and 15% at all of the three registered times), and LDL-C levels. The most important decrease reported with MiPo treatment was in the plasma LDL-C levels, in both the fasting and postprandial conditions, at any time on the treatment curve (27% in the fasting conditions (p < 0.05), and 36% at 4 h (p < 0.05) and 35% at 8 h in the postprandial conditions (p < 0.05)) compared to those in the pre-supplementation conditions. The fasting plasma levels of HDL-C significantly increased by 11% (p < 0.05). These improvements may be due, according to the researchers, to the activation of peroxisome proliferator-activated receptor-α (PPAR-α) and peroxisome proliferator-activated receptor-γ (PPAR-γ), to the overexpression of lipoprotein lipase (LPL) activity, and possibly, to a reduction in the intestinal absorption of TG [68].
The improvements in dyslipidemia observed with the administration of only these bioactive compounds are of great importance since atherogenic dyslipidemia (abnormal changes in the plasma lipid profile, such as a decrease in HDL-C levels and increase in TG and LDL-C levels) is strongly associated with ASVD and the progression of CV complications [76]. The following are among several reasons for this strong association: the elevation of the plasma levels of LDL-C is one of the primary mechanisms in initiating the development of ASVD by inducing its entrance and retention in the arterial intima and leading to extracellular cholesterol accumulation and the formation of cholesteryl ester droplet-engorged macrophage foam cells with transformation to an inflammatory and prothrombotic phenotype in the blood vessels. These major pathways favor the formation of a plaque necrotic core, containing cellular and extracellular debris and LDL-C-derived cholesterol crystals, in addition to increasing the risk of LDL-C’s oxidation to oxLDL [77,78,79,80]. This is a relevant consideration, as high circulating plasma levels of oxLDL is one of the most important markers in the atherogenic process [81], is associated with all stages of ASVD [81], and is a predictor of future CV events, in both CVD-symptomatic subjects [82,83] and apparently healthy or CVD-asymptomatic subjects [79]. A reduction in the plasma levels of HDL-C decreases its antiatherogenic capacity (reverse LDL-C transport, antioxidant effects by inhibiting LDL-C oxidation, vasodilation, anti-inflammatory effects, antithrombotic effects, antiapoptotic effects, vascular endothelial repair, etc.). This highlights the inverse relationship that exists between low plasma levels of HDL-C and CV risk [84], the former behaving as an independent predictor of CVD [84,85,86,87,88]. In addition, an increase in the plasma levels of TG, giving rise to hypertriglyceridemia, is atherogenic through multiple mechanisms, some of which contribute to the formation of lipid deposits in the arterial intima, increasing monocyte activity, stimulating the synthesis of proinflammatory cytokines and procoagulant factors, and promoting endothelial dysfunction [89]. Hypertriglyceridemia also contributes to atherogenesis through its association with other metabolic alterations, such as the reduction of plasma HDL-C levels or the elevation of the plasma levels of small and dense LDL-C, to name a few [89]. In addition, atherogenic dyslipidemia influences the development of important early markers of CV risk, such as endothelial dysfunction [8,90,91,92,93,94] or high circulating plasma levels of oxLDL [94,95,96]. In the development of endothelial dysfunction, there has been speculation that certain mechanisms may be involved, such as the overexpression of the enzyme nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, the activation of c-Jun N-terminal kinase 2 (JNK2) [97,98], an increase in the production of superoxide anion radical (O2−) [98], an increase in the production of asymmetric dimethylarginine (ADMA) [99], and a rise in the circulating plasma levels of oxLDL [100], among other reactive oxygen species (ROS) [100]. On the other hand, subjects with dyslipidemia per se present higher plasma levels of oxLDL than those without these pathologies, as elevated plasma lipid levels are a strong predictor of high circulating plasma levels of oxLDL in diverse types of populations [77,101,102]. Consequently, the described improvements in the plasma lipid profiles of dyslipidemic subjects could contribute significantly to the reduction of endothelial dysfunction and high circulating plasma levels of oxLDL, improvements observed in the current study that we reported in our previous article [14]. One possible limitation of this study is the sample size.
5. Conclusions
The daily intake of a supplement containing HT (9.9 mg) and PC (195 mg) for 8-weeks was shown to improve dyslipidemia in an adult population with metabolic disorders. Therefore, the regular consumption of a supplement composed of HT and PC may reduce the CV risks that these subjects face. Further clinical trials are needed to confirm the favorable effects of these polyphenols in humans.
Acknowledgments
We thank the Biostatistics Department of the HULP for their continuous support.
Abbreviations
| ABCA1 | ATP-binding membrane cassette transport protein A1 |
| ACAT | acyl-coenzyme a: cholesterol acyltransferase |
| ACS | acute coronary syndrome |
| ADMA | asymmetric dimethylarginine |
| AMPK | AMP-activated protein kinase |
| ApoAI | apolipoprotein A-I |
| ASVD | atherosclerotic vascular disease |
| BMI | body mass index |
| CPJ | concentrated pomegranate juice |
| CV | cardiovascular |
| CVD | cardiovascular disease |
| db/db | mice with obesity and type 2 diabetes mellitus |
| DBP | diastolic blood pressure |
| FFM | fat-free mass |
| FM | fat mass |
| HDL-C | high-density lipoprotein cholesterol |
| HFD | high-fat-diet |
| HMGR | 3-hydroxy-3-methylglutaryl coenzyme A reductase |
| HR | heart rate |
| HT | hydroxytyrosol |
| HULP | University Hospital La Paz |
| JNK2 | c-Jun N-terminal kinase 2 |
| LDL-C | low-density lipoprotein cholesterol |
| LDLR | low-density lipoprotein receptor |
| LPL | lipoprotein lipase |
| MM | muscle mass |
| MiPo | microencapsulated pomegranate |
| MUFA | monounsaturated fatty acids |
| NADPH | nicotinamide adenine dinucleotide-phosphate |
| NF-κB | nuclear factor-kappa B |
| O2- | superoxide anion radical |
| oxLDL | oxidized low-density lipoprotein |
| PC | punicalagin |
| PLE | pomegranate leaf extract |
| PPAR-α | peroxisome proliferator-activated receptor-α |
| PPAR-γ | peroxisome proliferator-activated receptor-γ |
| PUFA | polyunsaturated fatty acids |
| ROS | reactive oxygen species |
| SBP | systolic blood pressure |
| SFA | saturated fatty acids |
| SREBP-1c | sterol regulatory element-binding protein 1c |
| FAS | fatty acid synthase |
| SREBP2 | sterol regulatory element-binding protein 2 |
| PCSK9 | proprotein convertase subtilisin/kexin type 9 |
| T2DM | type 2 diabetes mellitus |
| TC | total cholesterol |
| TG | triglycerides |
Author Contributions
Conceptualization, R.Q.-F., B.L.-P., and C.G.C.; investigation, R.Q.-F., B.L.-P., L.M.B. and C.G.C.; writing—original draft preparation, R.Q.-F.; writing—review and editing, R.Q.-F., A.Z., B.L.-P. and C.G.C.; visualization, S.P.M.; supervision, C.G.C. and B.L.-P.; funding acquisition, B.L.-P., L.M.B. and C.G.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Scientific Research and Ethics Committee of the HULP (Approval Code: 3799).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
A.Z. is employed by Euromed S.A. but had no role in the design, collection and/or analysis of the data.
Patent
In concession process.
Funding Statement
The present clinical trial was supported by the Euromed S.A. group through the HENUFOOD project (CEN-20101016) from the CENIT program of Economy and Competitiveness Ministry 481 of Spain (MINECO) and the University Hospital La Paz.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO Cardiovascular Diseases (CVDs) [(accessed on 19 February 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- 2.Kaptoge S., Pennells L., De Bacquer D., Cooney M.T., Kavousi M., Stevens G., Riley L.M., Savin S., Khan T., Altay S., et al. World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions. Lancet Glob. Health. 2019;7:e1332–e1345. doi: 10.1016/S2214-109X(19)30318-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Cardiovascular Diseases (CVDs) [(accessed on 7 September 2016)]. Available online: http://www.who.int/mediacentre/factsheets/fs317/en/
- 4.WHO . Global Atlas on Cardiovascular Disease Prevention and Control. The World Health Organization Press in Collaboration with the World Heart Federation and the World Stroke Organization; Geneva, Switzerland: 2011. [Google Scholar]
- 5.Roth G.A., Johnson C., Abajobir A., Abd-Allah F., Abera S.F., Abyu G., Ahmed M., Aksut B., Alam T., Alam K., et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu H., Daugherty A. Atherosclerosis. Arter. Thromb Vasc Biol. 2016;35:485–491. doi: 10.1161/ATVBAHA.115.305380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kopin L., Lowenstein C.J. Dyslipidemia. Ann. Intern. Med. 2017;167:ITC81–ITC95. doi: 10.7326/AITC201712050. [DOI] [PubMed] [Google Scholar]
- 9.Tejada S., Pinya S., Del Mar Bibiloni M., Tur J.A., Pons A., Sureda A. Cardioprotective effects of the polyphenol hydroxytyrosol from olive oil. Curr. Drug Targets. 2016;18:1477–1486. doi: 10.2174/1389450117666161005150650. [DOI] [PubMed] [Google Scholar]
- 10.Tresserra-Rimbau A., Rimm E.B., Medina-Remón A., Martínez-González M.A., de la Torre R., Corella D., Salas-Salvadó J., Gómez-Gracia E., Lapetra J., Arós F., et al. Inverse association between habitual polyphenol intake and incidence of cardiovascular events in the PREDIMED study. Nutr. Metab. Cardiovasc. Dis. 2014;24:639–647. doi: 10.1016/j.numecd.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 11.Marx W., Kelly J., Marshall S., Nakos S., Campbell K., Itsiopoulos C. The effect of polyphenol-rich interventions on cardiovascular risk factors in haemodialysis: A systematic review and meta-analysis. Nutrients. 2017;9:1345. doi: 10.3390/nu9121345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dyck G.J.B., Raj P., Zieroth S., Dyck J.R.B., Ezekowitz J.A. The effects of resveratrol in patients with cardiovascular disease and heart failure: A narrative review. Int. J. Mol. Sci. 2019;20:904. doi: 10.3390/ijms20040904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu L.M., Dong X., Xue X.D., Zhang J., Li Z., Wu H.J., Yang Z.L., Yang Y., Wang H.S. Protection of the myocardium against ischemia/reperfusion injury by punicalagin through an SIRT1-NRF-2-HO-1-dependent mechanism. Chem. Biol. Interact. 2019;306:152–162. doi: 10.1016/j.cbi.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 14.Quirós-Fernández R., López-Plaza B., Bermejo L.M., Palma-Milla S., Gómez-Candela C. Supplementation with hydroxytyrosol and punicalagin improves early atherosclerosis markers involved in the asymptomatic phase of atherosclerosis in the adult population: A randomized, placebo-controlled, crossover trial. Nutrients. 2019;11:640. doi: 10.3390/nu11030640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santhakumar A.B., Battino M., Alvarez-Suarez J.M. Dietary polyphenols: Structures, bioavailability and protective effects against atherosclerosis. Food Chem. Toxicol. 2018;113:49–65. doi: 10.1016/j.fct.2018.01.022. [DOI] [PubMed] [Google Scholar]
- 16.Cheng Y.C., Sheen J.M., Hu W.L., Hung Y.C. Polyphenols and Oxidative Stress in Atherosclerosis-Related Ischemic Heart Disease and Stroke. Oxid. Med. Cell. Longev. 2017;2017:8526438. doi: 10.1155/2017/8526438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bahramsoltani R., Ebrahimi F., Farzaei M.H., Baratpourmoghaddam A., Ahmadi P., Rostamiasrabadi P., Rasouli Amirabadi A.H., Rahimi R. Dietary polyphenols for atherosclerosis: A comprehensive review and future perspectives. Crit. Rev. Food Sci. Nutr. 2019;59:114–132. doi: 10.1080/10408398.2017.1360244. [DOI] [PubMed] [Google Scholar]
- 18.Mendonça R.D., Carvalho N.C., Martin-Moreno J.M., Pimenta A.M., Lopes A.C.S., Gea A., Martinez-Gonzalez M.A., Bes-Rastrollo M. Total polyphenol intake, polyphenol subtypes and incidence of cardiovascular disease: The SUN cohort study. Nutr. Metab. Cardiovasc. Dis. 2019;29:69–78. doi: 10.1016/j.numecd.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 19.Gorzynik-Debicka M., Przychodzen P., Cappello F., Kuban-Jankowska A., Gammazza A.M., Knap N., Wozniak M., Gorska-Ponikowska M. Potential health benefits of olive oil and plant polyphenols. Int. J. Mol. Sci. 2018;19:547. doi: 10.3390/ijms19030686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Serino A., Salazar G. Protective role of polyphenols against vascular inflammation, aging and cardiovascular disease. Nutrients. 2019;11:53. doi: 10.3390/nu11010053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.George E.S., Marshall S., Mayr H.L., Trakman G.L., Tatucu-Babet O.A., Lassemillante A.C.M., Bramley A., Reddy A.J., Forsyth A., Tierney A.C., et al. The effect of high- polyphenol extra virgin olive oil on cardiovascular risk factors: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2019;59:2772–2795. doi: 10.1080/10408398.2018.1470491. [DOI] [PubMed] [Google Scholar]
- 22.Reis J.F., Monteiro V.V.S., Gomes S.R., Carmo M.M., Costa G.V., Ribera P.C., Monteiro M.C. Action mechanism and cardiovascular effect of anthocyanins: A systematic review of animal and human studies. J. Transl. Med. 2016;14:315. doi: 10.1186/s12967-016-1076-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Del Bo C., Bernardi S., Marino M., Porrini M., Tucci M., Guglielmetti S., Cherubini A., Carrieri B., Kirkup B., Kroon P., et al. Systematic Review on Polyphenol Intake and Health Outcomes: Is there Sufficient Evidence to Define a Health-Promoting Polyphenol-Rich Dietary Pattern? Nutrients. 2019;11:1355. doi: 10.3390/nu11061355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Suganya N., Bhakkiyalakshmi E., Sarada D.V.L., Ramkumar K.M. Reversibility of endothelial dysfunction in diabetes: Role of polyphenols. Br. J. Nutr. 2016;116:223–246. doi: 10.1017/S0007114516001884. [DOI] [PubMed] [Google Scholar]
- 25.Aprotosoaie A., Miron A., Trifan A., Luca V., Costache I.-I. The Cardiovascular Effects of Cocoa Polyphenols—An Overview. Diseases. 2016;4:39. doi: 10.3390/diseases4040039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robles-Almazan M., Pulido-Moran M., Moreno-Fernandez J., Ramirez-Tortosa C., Rodriguez-Garcia C., Quiles J.L., Ramirez-Tortosa M. Hydroxytyrosol: Bioavailability, toxicity, and clinical applications. Food Res. Int. 2018;105:654–667. doi: 10.1016/j.foodres.2017.11.053. [DOI] [PubMed] [Google Scholar]
- 27.Tangney C.C., Rasmussen H.E. Polyphenols, inflammation, and cardiovascular disease. Curr. Atheroscler. Rep. 2013;15:324. doi: 10.1007/s11883-013-0324-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Covas M.-I., Nyyssönen K., Poulsen H.E., Kaikkonen J., Zunft H.-J.F., Kiesewetter H., Gaddi A., de la Torre R., Mursu J., Bäumler H., et al. The effect of polyphenols in olive oil on heart disease risk factors: A randomized trial. Ann. Intern. Med. 2006;145:333–341. doi: 10.7326/0003-4819-145-5-200609050-00006. [DOI] [PubMed] [Google Scholar]
- 29.Kuriyama S., Shimazu T., Ohmori K., Kikuchi N., Nakaya N., Nishino Y., Tsubono Y., Tsuji I. Green Tea Consumption and Mortality Due to Cardiovascular Disease, Cancer, and All Causes in Japan. The Ohsaki Study. JAMA-J. Am. Med. Assoc. 2006;296:1255–1265. doi: 10.1001/jama.296.10.1255. [DOI] [PubMed] [Google Scholar]
- 30.Bondonno N.P., Dalgaard F., Kyrø C., Murray K., Bondonno C.P., Lewis J.R., Croft K.D., Gislason G., Scalbert A., Cassidy A., et al. Flavonoid intake is associated with lower mortality in the Danish Diet Cancer and Health Cohort. Nat. Commun. 2019;10:3651. doi: 10.1038/s41467-019-11622-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhong J., Reece E.A., Yang P. Punicalagin exerts protective effect against high glucose- induced cellular stress and neural tube defects. Biochem. Biophys. Res. Commun. 2015;467:179–184. doi: 10.1016/j.bbrc.2015.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen B., Tuuli M.G., Longtine M.S., Shin J.S., Lawrence R., Inder T., Michael Nelson D. Pomegranate juice and punicalagin attenuate oxidative stress and apoptosis in human placenta and in human placental trophoblasts. Am. J. Physiol. Endocrinol. Metab. 2012;302:E1142–E1152. doi: 10.1152/ajpendo.00003.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang J., Min J., Li B., Hong S., Liu C., Hu M., Li Y., Yang J., Hong L. Therapeutic Effects of Punicalagin Against Ovarian Carcinoma Cells in Association With β-Catenin Signaling Inhibition. Int. J. Gynecol. Cancer. 2016;26:1557–1563. doi: 10.1097/IGC.0000000000000805. [DOI] [PubMed] [Google Scholar]
- 34.De Nigris F., Williams-Ignarro S., Sica V., Lerman L.O., D’Armiento F.P., Byrns R.E., Casamassimi A., Carpentiero D., Schiano C., Sumi D., et al. Effects of a Pomegranate Fruit Extract rich in punicalagin on oxidation-sensitive genes and eNOS activity at sites of perturbed shear stress and atherogenesis. Cardiovasc. Res. 2007;73:414–423. doi: 10.1016/j.cardiores.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 35.Adaramoye O., Erguen B., Nitzsche B., Höpfner M., Jung K., Rabien A. Punicalagin, a polyphenol from pomegranate fruit, induces growth inhibition and apoptosis in human PC- 3 and LNCaP cells. Chem. Biol. Interact. 2017;274:100–106. doi: 10.1016/j.cbi.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 36.Pathakoti K., Goodla L., Manubolu M., Tencomnao T. Metabolic Alterations and the Protective Effect of Punicalagin Against Glutamate-Induced Oxidative Toxicity in HT22 Cells. Neurotox. Res. 2017;31:521–531. doi: 10.1007/s12640-016-9697-2. [DOI] [PubMed] [Google Scholar]
- 37.Fki I., Sahnoun Z., Sayadi S. Hypocholesterolemic effects of phenolic extracts and purified hydroxytyrosol recovered from olive mill wastewater in rats fed a cholesterol-rich diet. J. Agric. Food Chem. 2007;55:624–631. doi: 10.1021/jf0623586. [DOI] [PubMed] [Google Scholar]
- 38.Mateos R., Martínez-López S., Arévalo B.G., Amigo-Benavent M., Sarriá B., Bravo- Clemente L. Hydroxytyrosol in functional hydroxytyrosol-enriched biscuits is highly bioavailable and decreases oxidised low density lipoprotein levels in humans. Food Chem. 2016;205:248–256. doi: 10.1016/j.foodchem.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 39.López-Villodres J.A., Abdel-Karim M., De La Cruz J.P., Rodríguez-Pérez M.D., Reyes J.J., Guzmán-Moscoso R., Rodriguez-Gutierrez G., Fernández-Bolaños J., González-Correa J.A. Effects of hydroxytyrosol on cardiovascular biomarkers in experimental diabetes mellitus. J. Nutr. Biochem. 2016;37:94–100. doi: 10.1016/j.jnutbio.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 40.Sánchez-Fidalgo S., Sánchez de Ibargüen L., Cárdeno A., Alarcón de la Lastra C. Influence of extra virgin olive oil diet enriched with hydroxytyrosol in a chronic DSS colitis model. Eur. J. Nutr. 2012;51:497–506. doi: 10.1007/s00394-011-0235-y. [DOI] [PubMed] [Google Scholar]
- 41.Aparicio-Soto M., Sánchez-Fidalgo S., González-Benjumea A., Maya I., Fernández-Bolaños J.G., Alarcón-de-la-Lastra C. Naturally Occurring Hydroxytyrosol Derivatives: Hydroxytyrosyl Acetate and 3,4-Dihydroxyphenylglycol Modulate Inflammatory Response in Murine Peritoneal Macrophages. Potential Utility as New Dietary Supplements. J. Agric. Food Chem. 2015;63:836–846. doi: 10.1021/jf503357s. [DOI] [PubMed] [Google Scholar]
- 42.Silva S., Sepodes B., Rocha J., Direito R., Fernandes A., Brites D., Freitas M., Fernandes E., Bronze M.R., Figueira M.E. Protective effects of hydroxytyrosol-supplemented refined olive oil in animal models of acute inflammation and rheumatoid arthritis. J. Nutr. Biochem. 2015;26:360–368. doi: 10.1016/j.jnutbio.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 43.Atrahimovich D., Samson A.O., Khattib A., Vaya J., Khatib S. Punicalagin Decreases Serum Glucose Levels and Increases PON1 Activity and HDL Anti-Inflammatory Values in Balb/c Mice Fed a High-Fat Diet. Oxid. Med. Cell. Longev. 2018;2018:2673076. doi: 10.1155/2018/2673076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu X., Cao K., Lv W., Feng Z., Liu J., Gao J., Li H., Zang W., Liu J. Punicalagin attenuates endothelial dysfunction by activating FoxO1, a pivotal regulating switch of mitochondrial biogenesis. Free Radic. Biol. Med. 2019;135:251–260. doi: 10.1016/j.freeradbiomed.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 45.Zhang Y., Cao Y., Chen J., Qin H., Yang L. A New Possible Mechanism by Which Punicalagin Protects against Liver Injury Induced by Type 2 Diabetes Mellitus: Upregulation of Autophagy via the Akt/FoxO3a Signaling Pathway. J. Agric. Food Chem. 2019;67:13948–13959. doi: 10.1021/acs.jafc.9b05910. [DOI] [PubMed] [Google Scholar]
- 46.Kang B., Kim C.Y., Hwang J., Jo K., Kim S., Suh H.J., Choi H.S. Punicalagin, a Pomegranate-Derived Ellagitannin, Suppresses Obesity and Obesity-Induced Inflammatory Responses Via the Nrf2/Keap1 Signaling Pathway. Mol. Nutr. Food Res. 2019;63:e1900574. doi: 10.1002/mnfr.201900574. [DOI] [PubMed] [Google Scholar]
- 47.Giamogante F., Marrocco I., Cervoni L., Eufemi M., Chichiarelli S., Altieri F. Punicalagin, an active pomegranate component, is a new inhibitor of PDIA3 reductase activity. Biochimie. 2018;147:122–129. doi: 10.1016/j.biochi.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 48.Stefanon B., Colitti M. Original Research: Hydroxytyrosol, an ingredient of olive oil, reduces triglyceride accumulation and promotes lipolysis in human primary visceral adipocytes during differentiation. Exp. Biol. Med. 2016;241:1796–1802. doi: 10.1177/1535370216654226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xie Y.D., Chen Z.Z., Li N., Lu W.F., Xu Y.H., Lin Y.Y., Shao L.H., Wang Q.T., Guo L.Y., Gao Y.Q., et al. Hydroxytyrosol nicotinate, a new multifunctional hypolipidemic and hypoglycemic agent. Biomed. Pharmacother. 2018;99:715–724. doi: 10.1016/j.biopha.2018.01.123. [DOI] [PubMed] [Google Scholar]
- 50.Mahmoudi A., Hadrich F., Feki I., Ghorbel H., Bouallagui Z., Marrekchi R., Fourati H., Sayadi S. Oleuropein and hydroxytyrosol rich extracts from olive leaves attenuate liver injury and lipid metabolism disturbance in bisphenol A-treated rats. Food Funct. 2018;9:3220–3234. doi: 10.1039/C8FO00248G. [DOI] [PubMed] [Google Scholar]
- 51.Zheng A., Li H., Xu J., Cao K., Li H., Pu W., Yang Z., Peng Y., Long J., Liu J., et al. Hydroxytyrosol improves mitochondrial function and reduces oxidative stress in the brain of db/db mice: Role of AMP-activated protein kinase activation. Br. J. Nutr. 2015;113:1667–1676. doi: 10.1017/S0007114515000884. [DOI] [PubMed] [Google Scholar]
- 52.Cao K., Xu J., Zou X., Li Y., Chen C., Zheng A., Li H., Li H., Szeto I.M.-Y., Shi Y., et al. Hydroxytyrosol prevents diet-induced metabolic syndrome and attenuates mitochondrial abnormalities in obese mice. Free Radic. Biol. Med. 2014;67:396–407. doi: 10.1016/j.freeradbiomed.2013.11.029. [DOI] [PubMed] [Google Scholar]
- 53.Puri K.S., Suresh K.R., Gogtay N.J., Thatte U.M. Declaration of Helsinki, 2008: Implications for stakeholders in research. J. Postgrad. Med. 2009;55:131–134. doi: 10.4103/0022-3859.52846. [DOI] [PubMed] [Google Scholar]
- 54.FAO. UNICEF. WHO Methodology of nutritional surveillance. World Health Organ. Tech. Rep. Ser. 1976;593:1–66. Report of a Joint FAO/UNICEF/WHO Expert Committee. [PubMed] [Google Scholar]
- 55.Sorensen K.E., Celermajer D.S., Spiegelhalter D.J., Georgakopoulos D., Robinson J., Thomas O., Deanfield J.E. Non-invasive measurement of human endothelium dependent arterial responses: Accuracy and reproducibility. Br. Heart J. 1995;74:247–253. doi: 10.1136/hrt.74.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yebyo H.G., Aschmann H.E., Kaufmann M., Puhan M.A. Comparative effectiveness and safety of statins as a class and of specific statins for primary prevention of cardiovascular disease: A systematic review, meta-analysis, and network meta-analysis of randomized trials with 94,283 participants. Am. Heart J. 2019;210:18–28. doi: 10.1016/j.ahj.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 57.Sathasivam S. Statin induced myotoxicity. Eur. J. Intern. Med. 2012;23:317–324. doi: 10.1016/j.ejim.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 58.Schandelmaier S., Briel M., Saccilotto R., Olu K.K., Arpagaus A., Hemkens L.G., Nordmann A.J. Niacin for primary and secondary prevention of cardiovascular events. Cochrane Database Syst. Rev. 2017;6:CD009744. doi: 10.1002/14651858.CD009744.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nguyen K.A., Li L., Lu D., Yazdanparast A., Wang L., Kreutz R.P., Whipple E.C., Schleyer T.K. A comprehensive review and meta-analysis of risk factors for statin-induced myopathy. Eur. J. Clin. Pharmacol. 2018;74:1099–1109. doi: 10.1007/s00228-018-2482-9. [DOI] [PubMed] [Google Scholar]
- 60.Okopień B., Bułdak Ł., Bołdys A. Benefits and risks of the treatment with fibrates—A comprehensive summary. Expert Rev. Clin. Pharmacol. 2018;11:1099–1112. doi: 10.1080/17512433.2018.1537780. [DOI] [PubMed] [Google Scholar]
- 61.Squizzato A., Galli M., Romualdi E., Dentali F., Kamphuisen P.W., Guasti L., Venco A., Ageno W. Statins, fibrates, and venous thromboembolism: A meta-analysis. Eur. Heart J. 2010;31:1248–1256. doi: 10.1093/eurheartj/ehp556. [DOI] [PubMed] [Google Scholar]
- 62.Tabernero M., Sarriá B., Largo C., Martínez-López S., Madrona A., Espartero J.L., Bravo L., Mateos R. Comparative evaluation of the metabolic effects of hydroxytyrosol and its lipophilic derivatives (hydroxytyrosyl acetate and ethyl hydroxytyrosyl ether) in hypercholesterolemic rats. Food Funct. 2014;5:1556–1563. doi: 10.1039/C3FO60677E. [DOI] [PubMed] [Google Scholar]
- 63.Jemai H., Fki I., Bouaziz M., Bouallagui Z., El Feki A., Isoda H., Sayadi S. Lipid-lowering and antioxidant effects of hydroxytyrosol and its triacetylated derivative recovered from olive tree leaves in cholesterol-fed rats. J. Agric. Food Chem. 2008;56:2630–2636. doi: 10.1021/jf072589s. [DOI] [PubMed] [Google Scholar]
- 64.Perrone M.A., Gualtieri P., Gratteri S., Ali W., Sergi D., Muscoli S., Cammarano A., Bernardini S., Renzo L.D., Romeo F. Effects of postprandial hydroxytyrosol and derivates on oxidation of LDL, cardiometabolic state and gene expression: A nutrigenomic approach for cardiovascular prevention. J. Cardiovasc. Med. 2019;20:419–426. doi: 10.2459/JCM.0000000000000816. [DOI] [PubMed] [Google Scholar]
- 65.Peyrol J., Riva C., Amiot M.J. Hydroxytyrosol in the prevention of the metabolic syndrome and related disorders. Nutrients. 2017;9:306. doi: 10.3390/nu9030306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lockyer S., Rowland I., Spencer J.P.E., Yaqoob P., Stonehouse W. Impact of phenolic-rich olive leaf extract on blood pressure, plasma lipids and inflammatory markers: A randomised controlled trial. Eur. J. Nutr. 2017;56:1421–1432. doi: 10.1007/s00394-016-1188-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang X., Qin Y., Wan X., Liu H., Iv C., Ruan W., Lu L., He L., Guo X. Hydroxytyrosol Plays Antiatherosclerotic Effects through Regulating Lipid Metabolism via Inhibiting the p38 Signal Pathway. Biomed Res. Int. 2020;2020:5036572. doi: 10.1155/2020/5036572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Estrada-Luna D., Carreón-Torres E., Bautista-Perez R., Betanzos-Cabrera G., Dorantes- Morales A., Luna-Luna M., Vargas-Barrón J., Mejía A.M., Fragoso J.M., Carvajal-Aguilera K., et al. Microencapsulated Pomegranate Reverts High-Density Lipoprotein (HDL)-Induced Endothelial Dysfunction and Reduces Postprandial Triglyceridemia in Women with Acute Coronary Syndrome. Nutrients. 2019;11:1710. doi: 10.3390/nu11081710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bagri P., Ali M., Aeri V., Bhowmik M., Sultana S. Antidiabetic effect of Punica granatum flowers: Effect on hyperlipidemia, pancreatic cells lipid peroxidation and antioxidant enzymes in experimental diabetes. Food Chem. Toxicol. 2009;47:50–54. doi: 10.1016/j.fct.2008.09.058. [DOI] [PubMed] [Google Scholar]
- 70.Lei F., Zhang X.N., Wang W., Xing D.M., Xie W.D., Su H., Du L.J. Evidence of anti-obesity effects of the pomegranate leaf extract in high-fat diet induced obese mice. Int. J. Obes. 2007;31:1023–1029. doi: 10.1038/sj.ijo.0803502. [DOI] [PubMed] [Google Scholar]
- 71.Atrahimovich D., Khatib S., Sela S., Vaya J., Samson A.O. Punicalagin Induces Serum Low- Density Lipoprotein Influx to Macrophages. Oxid. Med. Cell. Longev. 2016;2016:7124251. doi: 10.1155/2016/7124251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Banihani S., Swedan S., Alguraan Z. Pomegranate and type 2 diabetes. Nutr. Res. 2013;33:341–348. doi: 10.1016/j.nutres.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 73.Esmaillzadeh A., Tahbaz F., Gaieni I., Alavi-Majd H., Azadbakht L. Concentrated pomegranate juice improves lipid profiles in diabetic patients with hyperlipidemia. J. Med. Food. 2004;7:305–308. doi: 10.1089/jmf.2004.7.305. [DOI] [PubMed] [Google Scholar]
- 74.Rouhi S.Z.T., Sarker M.M.R., Rahmat A., Alkahtani S.A., Othman F. The effect of pomegranate fresh juice versus pomegranate seed powder on metabolic indices, lipid profile, inflammatory biomarkers, and the histopathology of pancreatic islets of Langerhans in streptozotocin-nicotinamide induced type 2 diabetic Sprague-Daw. BMC Complement. Altern. Med. 2017;17:156. doi: 10.1186/s12906-017-1667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.De Bock M., Derraik J., Brennan C., Biggs J., Morgan P., Hodgkinson S., Hofman P., Cutfield W. Olive (Olea europaea L.) leaf polyphenols improve insulin sensitivity in middle- aged overweight men: A randomized, placebo-controlled, crossover trial. PLoS ONE. 2013;8:e57622. doi: 10.1371/journal.pone.0057622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Uydu H.A., Bostan M., Atak M., Yilmaz A., Demir A., Akçan B., Sümer F., Baltaş N., Karadaǧ Z., Uǧurlu Y., et al. Cholesterol forms and traditional lipid profile for projection of atherogenic dyslipidemia: Lipoprotein subfractions and erythrocyte membrane cholesterol. J. Membr. Biol. 2014;247:127–134. doi: 10.1007/s00232-013-9611-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ramos-Arellano L.E., Muñoz-Valle J.F., De la Cruz-Mosso U., Salgado-Bernabé A.B., Castro-Alarcón N., Parra-Rojas I. Circulating CD36 and oxLDL levels are associated with cardiovascular risk factors in young subjects. BMC Cardiovasc. Disord. 2014;14:54. doi: 10.1186/1471-2261-14-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Holvoet P., Mertens A., Verhamme P., Bogaerts K., Beyens G., Verhaeghe R., Collen D., Muls E., Van de Werf F. Circulating oxidized LDL is a useful marker for identifying patients with coronary artery disease. Arterioscler. Thromb. Vasc. Biol. 2001;21:844–848. doi: 10.1161/01.ATV.21.5.844. [DOI] [PubMed] [Google Scholar]
- 79.Meisinger C., Baumert J., Khuseyinova N., Loewel H., Koenig W. Plasma oxidized low- density lipoprotein, a strong predictor for acute coronary heart disease events in apparently healthy, middle-aged men from the general population. Circulation. 2005;112:651–657. doi: 10.1161/CIRCULATIONAHA.104.529297. [DOI] [PubMed] [Google Scholar]
- 80.Borén J., John Chapman M., Krauss R.M., Packard C.J., Bentzon J.F., Binder C.J., Daemen M.J., Demer L.L., Hegele R.A., Nicholls S.J., et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: Pathophysiological, genetic, and therapeutic insights: A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 2020;41:2313–2330. doi: 10.1093/eurheartj/ehz962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Trpkovic A., Resanovic I., Stanimirovic J., Radak D., Mousa S.A., Cenic-Milosevic D., Jevremovic D., Isenovic E.R. Oxidized low-density lipoprotein as a biomarker of cardiovascular diseases. Crit. Rev. Clin. Lab. Sci. 2015;52:70–85. doi: 10.3109/10408363.2014.992063. [DOI] [PubMed] [Google Scholar]
- 82.Tsutsui T., Tsutamoto T., Wada A., Maeda K., Mabuchi N., Hayashi M., Ohnishi M., Kinoshita M. Plasma oxidized low-density lipoprotein as a prognostic predictor in patients with chronic congestive heart failure. J. Am. Coll. Cardiol. 2002;39:957–962. doi: 10.1016/S0735-1097(02)01721-7. [DOI] [PubMed] [Google Scholar]
- 83.Ehara S., Ueda M., Naruko T., Haze K., Itoh A., Otsuka M., Komatsu R., Matsuo T., Itabe H., Takano T., et al. Elevated levels of oxidized low density lipoprotein show a positive relationship with the severity of acute coronary syndromes. Circulation. 2001;103:1955–1960. doi: 10.1161/01.CIR.103.15.1955. [DOI] [PubMed] [Google Scholar]
- 84.Rader D.J., Hovingh G.K. HDL and cardiovascular disease. Lancet. 2014;384:618–625. doi: 10.1016/S0140-6736(14)61217-4. [DOI] [PubMed] [Google Scholar]
- 85.Assmann G., Schulte H., Cullen P., Seedorf U. Assessing risk of myocardial infarction and stroke: New data from the Prospective Cardiovascular Münster (PROCAM) study. Eur. J. Clin. Investig. 2007;37:925–932. doi: 10.1111/j.1365-2362.2007.01888.x. [DOI] [PubMed] [Google Scholar]
- 86.Rodríguez A.D., Cumplido A.S., Nuñez-Cortés J.M., Rodríguez de Miguel M., Orera-Peña M.L. The application of atherogenic dyslipidaemia consensus recommendations in the primary care setting. DAT-AP study. Clin. Res. Arterioscler. 2017;29:178–184. doi: 10.1016/j.arteri.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 87.Wan Ahmad W.N.H., Sakri F., Mokhsin A., Rahman T., Mohd Nasir N., Abdul-Razak S., Yasin M.M., Mohd Ismail A., Ismail Z., Nawawi H. Low serum high density lipoprotein cholesterol concentration is an independent predictor for enhanced inflammation and endothelial activation. PLoS ONE. 2015;10:e0116867. doi: 10.1371/journal.pone.0116867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Estrada-Luna D., Ortiz-Rodriguez M.A., Medina-Briseño L., Carreón-Torres E., Izquierdo- Vega J.A., Sharma A., Cancino-Díaz J.C., Pérez-Méndez O., Belefant-Miller H., Betanzos-Cabrera G. Current therapies focused on high-density lipoproteins associated with cardiovascular disease. Molecules. 2018;23:2730. doi: 10.3390/molecules23112730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Lawler P.R., Kotrri G., Koh M., Goodman S.G., Farkouh M.E., Lee D.S., Austin P.C., Udell J.A., Ko D.T. Real-world risk of cardiovascular outcomes associated with hypertriglyceridaemia among individuals with atherosclerotic cardiovascular disease and potential eligibility for emerging therapies. Eur. Heart J. 2020;41:86–94. doi: 10.1093/eurheartj/ehz767. [DOI] [PubMed] [Google Scholar]
- 90.Kuvin J.T., Rämet M.E., Patel A.R., Pandian N.G., Mendelsohn M.E., Karas R.H. A novel mechanism for the beneficial vascular effects of high-density lipoprotein cholesterol: Enhanced vasorelaxation and increased endothelial nitric oxide synthase expression. Am. Heart J. 2002;144:165–172. doi: 10.1067/mhj.2002.123145. [DOI] [PubMed] [Google Scholar]
- 91.Ansar S., Koska J., Reaven P.D. Postprandial hyperlipidemia, endothelial dysfunction and cardiovascular risk: Focus on incretins. Cardiovasc. Diabetol. 2011;10:61. doi: 10.1186/1475-2840-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nagashima H., Endo M. Pitavastatin prevents postprandial endothelial dysfunction via reduction of the serum triglyceride level in obese male subjects. Heart Vessel. 2011;26:428–434. doi: 10.1007/s00380-010-0071-7. [DOI] [PubMed] [Google Scholar]
- 93.Badimon L., Storey R.F., Vilahur G. Update on lipids, inflammation and atherothrombosis. Thromb. Haemost. 2011;105:34–42. doi: 10.1160/THS10-11-0717. [DOI] [PubMed] [Google Scholar]
- 94.Helkin A., Stein J.J., Lin S., Siddiqui S., Maier K.G., Gahtan V. Dyslipidemia Part 1—Review of Lipid Metabolism and Vascular Cell Physiology. Vasc. Endovasc. Surg. 2016;50:107–118. doi: 10.1177/1538574416628654. [DOI] [PubMed] [Google Scholar]
- 95.Bing H., Wang J., Zhang C., Cai H. Positive correlation between in vivo oxidized LDL and LDL immune complexes. Clin. Biochem. 2004;37:72–75. doi: 10.1016/j.clinbiochem.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 96.Marin M.T., Dasari P.S., Tryggestad J.B., Aston C.E., Teague A.M., Short K.R. Oxidized HDL and LDL in adolescents with type 2 diabetes compared to normal weight and obese peers. J. Diabetes Complicat. 2015;29:679–685. doi: 10.1016/j.jdiacomp.2015.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Osto E., Matter C.M., Kouroedov A., Malinski T., Bachschmid M., Camici G.G., Kilic U., Stallmach T., Boren J., Iliceto S., et al. c-Jun N-terminal kinase 2 deficiency protects against hypercholesterolemia-induced endothelial dysfunction and oxidative stress. Circulation. 2008;118:2073–2080. doi: 10.1161/CIRCULATIONAHA.108.765032. [DOI] [PubMed] [Google Scholar]
- 98.Warnholtz A., Mollnau H., Oelze M., Wendt M., Münzel T. Antioxidants and endothelial dysfunction in hyperlipidemia. Curr. Hypertens. Rep. 2001;3:53–60. doi: 10.1007/s11906-001-0081-z. [DOI] [PubMed] [Google Scholar]
- 99.Böger R.H. Association of Asymmetric Dimethylarginine and Endothelial Dysfunction. Clin. Chem. Lab. Med. 2003;41:1467–1472. doi: 10.1515/CCLM.2003.225. [DOI] [PubMed] [Google Scholar]
- 100.Vasconcelos E.M.A., Degasperi G.R., de Oliveira H.C.F., Vercesi A.E., de Faria E.C., Castilho L.N. Reactive oxygen species generation in peripheral blood monocytes and oxidized LDL are increased in hyperlipidemic patients. Clin. Biochem. 2009;42:1222–1227. doi: 10.1016/j.clinbiochem.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 101.Holvoet P., Harris T.B., Tracy R.P., Verhamme P., Newman A.B., Rubin S.M., Simonsick E.M., Colbert L.H., Kritchevsky S.B. Association of High Coronary Heart Disease Risk Status with Circulating Oxidized LDL in the Well-Functioning Elderly. Arterioscler. Thromb. Vasc. Biol. 2003;23:1444–1448. doi: 10.1161/01.ATV.0000080379.05071.22. [DOI] [PubMed] [Google Scholar]
- 102.Kopprasch S., Pietzsch J., Kuhlisch E., Fuecker K., Temelkova-Kurktschiev T., Hanefeld M., Kühne H., Julius U., Graessler J. In vivo evidence for increased oxidation of circulating LDL in impaired glucose tolerance. Diabetes. 2002;51:3102–3106. doi: 10.2337/diabetes.51.10.3102. [DOI] [PubMed] [Google Scholar]