Abstract
Study Design:
Cross-sectional survey.
Objectives:
Degenerative cervical myelopathy (DCM) is a common syndrome of acquired spinal cord impairment caused by canal stenosis secondary to arthritic changes of the spine. International guidelines consider physiotherapy an option for mild, stable DCM; however, few studies have been conducted on nonoperative management. The objective was to determine current usage and perceptions of nonoperative physiotherapy for DCM.
Methods:
Persons with DCM were recruited to a web-based survey. Participants with complete responses that had not received surgery were included (n = 167). Variables included symptom duration, treatment history, current disability, and demographic characteristics.
Results:
Disease and demographic characteristics were equivalent between those who did and did not receive physiotherapy. In all, 19.5% of physiotherapy recipients reported subjective benefit from physiotherapy. Those perceiving benefit had significantly higher mJOA (modified Japanese Orthopaedic Association) scores, lower neck pain scores, and shorter symptom duration. In multivariate logistic regression analysis, those with mild DCM were more likely to perceive benefit than those with severe DCM, as were those with moderate DCM (to a lesser extent). Individuals whose diagnosis was delayed 1 to 2 years were less likely to perceive benefit than those that waited 0 to 6 months.
Conclusions:
The provision of nonoperative physiotherapy in the management of DCM is inconsistent and appears to differ from international guidelines. Few patients perceived benefit from physiotherapy; however, this was more likely in those with mild DCM and in those with shorter symptom durations. Further work is needed to establish the appropriate role of physiotherapy for this population.
Keywords: myelopathy, spondylosis, cervical, degenerative, neuro, spinal cord injury
Introduction
Degenerative cervical myelopathy (DCM) is a progressive neurological condition, characterized by symptomatic cervical cord compression secondary to age-related changes in the cervical spine. 1 DCM is the commonest spinal cord disorder worldwide, 1 with up to 5% prevalence estimated in individuals aged older than 40 years. Given an aging population, an increase in prevalence and disease burden from DCM is anticipated.
The cervical spinal cord processes and transmits information between the brain and the body. Abnormal function of the spinal cord causes diverse symptoms including pain, paresthesia, weakness, unsteadiness, frequent falls, loss of dexterity and incontinence. 2 This substantially impacts quality of life; one recent study found people with DCM have among the worst health-related quality of life (Short Form–36 [SF-36]) scores of any chronic disease. 3
Surgical decompression is the only evidence-based treatment demonstrated to halt DCM progression and offer worthwhile but often incomplete recovery.4,5 The natural history of DCM is poorly understood and the rate of symptom progression in an individual is highly variable and difficult to predict. In people with mild DCM, the risks of surgery may outweigh any benefit. For these individuals, physiotherapy may have a role 6 with limited data suggesting that outcomes from nonoperative management may be comparable to surgery. 7 Consequently, recent international guidelines only recommended surgery for progressive, moderate, or severe disease. Conservative management, including physiotherapy, is recommended for mild, stable forms of the condition. Although it is unlikely to alter degenerative changes, physiotherapy may improve neck conditioning; pain reduction; monitoring of progression, and disease education.
Guidelines are key for knowledge translation, and their dissemination is continuing. These recommendations are typically based on clinical studies designed by health care professionals, which often overlook the perspective of people with DCM.8-10 The aim of this study was to survey people with cervical myelopathy to determine if they had received physiotherapy and their perceptions of that treatment. We did not capture the intent of the physiotherapy or expectations of treatment.
Methods
The survey was designed and is reported following the Checklist for Reporting Results of Internet E-Surveys. 11
Survey Design
An online survey was designed using SurveyMonkey (Survey Monkey), Facebook (Facebook), Twitter (Twitter), Google AdWords (Google), and Myelopathy.org, a UK-registered charity, with a large online, international community of people with DCM. The website is a hub for support groups, educational resources, and information about DCM research.
The survey questions be found in Supplementary Material 1. Questions assessed disease time course, treatment history, current disability, and respondent demographics. Respondents were asked if they had received physiotherapy and, if so, whether they found it helpful. Current disability was assessed in part through the patient-derived modified Japanese Orthopaedic Association (p-mJOA) score. The mJOA is a composite score based on upper and lower limb motor function, upper limb sensation and sphincter function, that is widely used to assess myelopathy severity. 12 It is fully validated for this purpose, including when self-reported. 13
Data was stored on password-protected computers. The sequence of questions and order of responses was the same for all respondents.
Ethical Approval and Informed Consent
The study was ethically approved by a university ethics committee and was performed in accordance with the relevant guidelines and regulations.
All respondents completed the questionnaire voluntarily and were informed before doing so that their responses would be used anonymously for research purposes. The initial page stated the study objectives and host organization details. This acted as electronic consent and continuation was taken as agreement. No respondent-identifiable information was stored.
Participants
Respondents with DCM who had not received surgery at the time of the survey were included. Those that had received surgery were excluded.
Recruitment
The recruitment process has been described previously. 14 An open survey design was used. People with DCM were recruited to an online questionnaire administered by SurveyMonkey. Social media posts, supported by Myelopathy.org, recruited participants, alongside advertisements implemented with Google AdWords. Respondents were not contacted outside the survey.
Administration
A link to the survey was hosted on a landing page on Myelopathy.org. The survey was not administered via email. Completion was voluntary, and no incentives were offered. Responses were collected from October 2015 to August 2017. A total of 42 survey items were distributed over 15 survey pages. Responses with incomplete answers to medical management questions were excluded. Missing data analysis was performed to evaluate potential bias from excluded responses (Supplementary Material 2). Respondents were able to review their answers before survey submission.
Response Rates
Google Analytics, a Web-based analytics service, was used to measure the number of visitors to Myelopathy.org. Survey view rate was 6.3% (1663/26 501), participation rate was 67.0% (1114/1663), and completion rate for the overall survey was 69.8% (778/1114) (Supplementary Material 3).
Preventing Multiple Entries From the Same Individual
Duplicate responses were limited by respondent IP addresses.
Statistical Analysis
Descriptive analyses are reported as means ± standard deviations for continuous variables and frequencies and percentages for categorical variables, unless otherwise specified.
Univariate analyses were performed to compare those who received physiotherapy with those who did not, and those who perceived benefit from physiotherapy with those who did not. The chi-square test of homogeneity was used for categorical variables that met minimum expected count requirements; Fisher’s exact test was used for those that did not. The Mann-Whitney U test was used for respondent age.
A multivariate logistic regression was performed to control for potential confounding variables. Variables with a P < .10 in univariate analysis were included in multivariate analysis. Multivariate regression was not performed to analyze receipt of physiotherapy, as no variables had a P < .10 in univariate analysis. Multivariate regression was performed to analyze perceived benefit from physiotherapy; the assumption of no multicollinearity was met and the Hosmer and Lemeshow goodness of fit test indicated that the model was a good fit. Four standardized residuals had values of >2 standard deviations; these were retained in the analysis. The final model statistically significantly predicted the dependent variable over and above the intercept-only model, χ2(14) = 29.470, P = .009. The ability of the model to predict perceived benefit from physiotherapy was assessed by receiver operating characteristic (ROC) curve analysis.
Analyses were conducted using SPSS Statistics software, version 26 (IBM Corporation). Significance was set at P < .05.
Results
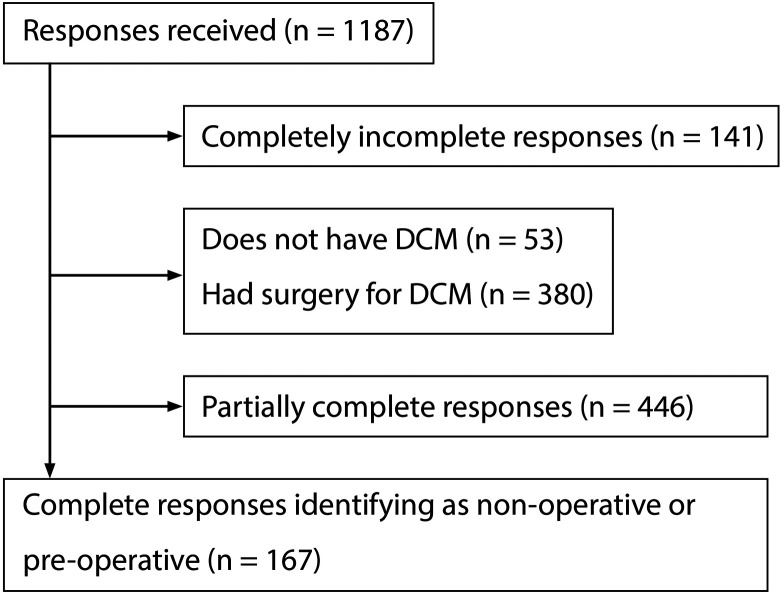
Participants, with complete survey responses, that had not received surgery (n = 167) were included in this analysis (Figure 1). Mean age was 54 years, and over two-thirds of respondents were female (120/167, 72.3%). Most respondents (Table 1) were from the United Kingdom (86/167, 51.5%) or the United States (56/167 33.5%), and were White/Caucasian (147/166, 88.6%). Approximately half of respondents were employed, either full-time (53/167, 31.7%) or part-time (27/167, 16.2%). Almost one-third stated being unable to work due to disability (47/167, 28.1%).
Figure 1.
Flow diagram of response selection.
Table 1.
Cohort Demographics (n = 167).
| Variable | n | % |
|---|---|---|
| Gender | 166 | |
| Female | 120 | 72.3 |
| Male | 46 | 27.7 |
| Age, years, mean (SD) | 53.9 | (10.8) |
| Country of current residence | 167 | |
| United Kingdom | 86 | 51.5 |
| United States | 56 | 33.5 |
| Canada | 11 | 6.6 |
| Australia | 3 | 1.8 |
| Other | 11 | 6.6 |
| Ethnicity | 166 | |
| White/Caucasian | 147 | 88.6 |
| Asian | 9 | 5.4 |
| Hispanic | 6 | 3.6 |
| Black or African American | 2 | 1.2 |
| Mixed | 1 | 0.6 |
| Prefer not to answer | 1 | 0.6 |
| Employment status | 167 | |
| Employed, full-time | 53 | 31.7 |
| Employed, part-time | 27 | 16.2 |
| Disabled, not able to work | 47 | 28.1 |
| Unemployed, looking for work | 5 | 3 |
| Unemployed, not looking for work | 7 | 4.2 |
| Retired | 28 | 16.8 |
| Annual income, UK£ | 165 | |
| 0-9999 | 14 | 8.5 |
| 10 000-24 999 | 24 | 14.5 |
| 25 000-49 999 | 41 | 24.8 |
| 50 000-99 999 | 24 | 14.5 |
| 100 000-149 999 | 5 | 3 |
| 150 000+ | 5 | 3 |
| Prefer not to answer | 52 | 31.5 |
| Education level | 164 | |
| Less than high school degree | 18 | 11 |
| High school degree or equivalent (eg, GED) | 30 | 18.3 |
| Some college but no degree | 33 | 20.1 |
| Associate degree | 16 | 9.8 |
| Bachelor’s degree | 31 | 18.9 |
| Graduate degree | 36 | 22 |
Physiotherapy Provision/Usage Did Not Predict Severity of Disability
A total of 49% of respondents had received physiotherapy (82/167). There was no significant difference in disability between those who did and did not receive physiotherapy (Nurick 1.9 ± 1.4 vs 2.0 ± 1.4, P = .850; mJOA, P = .311, Table 2). In total, 79.3% of individuals who received physiotherapy had moderate or severe DCM, compared with 70.6% of individuals who did not receive physiotherapy. There were no significant differences in time to diagnosis, duration of symptoms, pain scores or demographic measures between those who did and did not receive physiotherapy.
Table 2.
Physiotherapy Usage, Between-Group Comparison (n = 167).
| Variable | Received physiotherapy: | P | |
|---|---|---|---|
| Yes | No | ||
| Sample size, n | 82 | 85 | — |
| Gender: female, n (%) | 63 (77.8) | 57 (67.1) | .123a |
| Age of respondent, years, mean | 53.5 | 56 | .683b |
| Dependence on others to support daily activities, n (%) | 5 (47.2) | 29 (34.1) | .255b |
| Time to diagnosis, n (%) | 82 | 85 | .120b |
| 0-6 months | 18 (22.0) | 27 (31.8) | |
| 7-12 months | 9 (11.0) | 15 (17.6) | |
| 1-2 years | 23 (28.0) | 12 (14.1) | |
| 2-5 years | 23 (28.0) | 20 (23.5) | |
| >5 years | 9 (11.0) | 11 (12.9) | |
| Duration of symptoms, n (%) | 82 | 85 | .465b |
| 0-1 year | 15 (18.3) | 18 (21.2) | |
| 2-3 years | 32 (39.0) | 22 (25.9) | |
| 3-10 years | 23 (28.0) | 32 (37.6) | |
| 10-25 years | 11 (13.4) | 12 (14.1) | |
| >25 years | 1 (1.2) | 1 (1.2) | |
| Nurick score, mean ± SD | 1.9 ±1.4 | 2.0 ±1.4 | .850b |
| mJOA score, mean ± SD | 11.9 ±3.1 | 12.8 ±2.9 | .311b,d |
| ≤11, n (%) | 34 (41.5) | 27 (31.8) | |
| 12-14, n (%) | 31 (37.8) | 33 (38.8) | |
| ≥15, n (%) | 17 (20.7) | 25 (29.4) | |
| Current neck pain score, mean | 5.4 | 4.9 | .811b |
| Best neck pain score, mean | 3.9 | 3.6 | .781c |
| Worst neck pain score, mean | 7.4 | 6.9 | .487c |
| Education level, n (%) | 80 | 84 | .258b |
| Less than high school degree | 6 (7.5) | 12 (14.3) | |
| High school degree or equivalent | 15 (18.8) | 15 (17.9) | |
| Some college but no degree | 17 (21.3) | 16 (19) | |
| Associate degree | 7 (8.8) | 9 (10.7) | |
| Bachelor’s degree | 15 (18.8) | 16 (19) | |
| Graduate degree | 20 (25) | 16 (19) | |
| Ethnicity, n (%) | 82 | 84 | .915c |
| White/Caucasian | 72 (87.8) | 75 (89.3) | |
| Black or African American | 3 (3.7) | 3 (3.6) | |
| Asian | 6 (7.3) | 3 (3.6) | |
| Other | 1 (1.2) | 3 (3.6) | |
| Country of residence, n (%) | 82 | 80 | .615b |
| United Kingdom | 46 (56.1) | 40 (50) | |
| United States | 23 (28) | 33 (41.3) | |
| Canada | 6 (7.3) | 5 (6.3) | |
| Australia | 1 (1.2) | 2 (2.5) | |
| Other | 6 (7.3) | 0 (0) | |
Abbreviation: mJOA, modified Japanese Orthopaedic Association.
a Mann-Whitney U test.
b Chi-square test.
c Fisher’s exact test.
d For this analysis, scores were grouped into ≤11 (severe), 12-14 (moderate), ≥15 (mild).
Perceived Benefit of Physiotherapy Is Greater in Those With Mild DCM
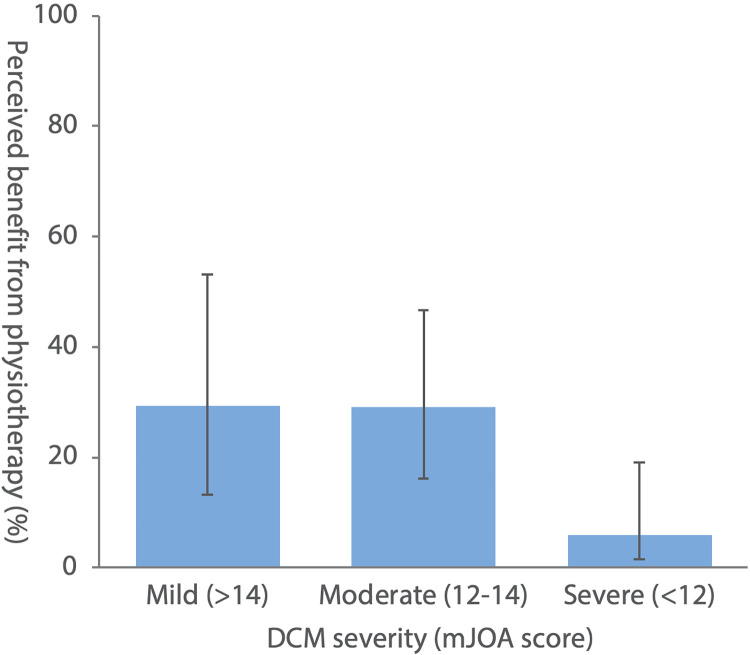
One-fifth of physiotherapy recipients stated a subjective benefit (16/82, 19.5%) of physiotherapy. A total of 29.4% (5/17) of respondents with mild DCM (mJOA ≥15) perceived benefit from physiotherapy, compared with 29.0% (9/31) of respondents with moderate DCM (mJOA 12-14), and 5.9% (2/34) of respondents with severe DCM (mJOA ≤12, Figure 2). Those perceiving benefit from physiotherapy had significantly higher mJOA scores than those that did not perceive benefit (P = .032, Table 3). There was no significant difference in Nurick score between those who perceived benefit and those who did not (1.6 ± 1.4 vs 2.0 ± 1.4; P = .398). Current neck pain scores were significantly lower in those who perceived benefit (3.9 ± 2.9 vs 5.7 ± 2.4, P = .031); however, there was no significant difference between groups for best and worst neck pain scores. Respondents perceiving benefit had shorter symptom duration (P = .049) than those not perceiving benefit. There was no significant difference in time to diagnosis, dependence on others, or demographic measures, except for ethnicity (P = .042).
Figure 2.
Perceived benefit of physiotherapy (%) versus degenerative cervical myelopathy (DCM) severity (modified Japanese Orthopaedic Association [mJOA] score). Error bars represent 95% binomial confidence intervals.
Table 3.
Perceived Benefit of Physiotherapy: Univariate Analysis (n = 82).
| Variable | Benefit perceived? | P | |
|---|---|---|---|
| Yes | No | ||
| Sample size, n | 16 | 66 | |
| Gender: female, n (%) | 11 (68.8) | 52 (78.8) | .733a |
| Age of respondent, mean | 53.9 | 53.9 | .693c |
| Dependence on others to support daily activities, n (%) | 4 (25.0) | 31 (47.0) | .111b |
| Time to diagnosis, n (%) | 16 | 66 | .055c |
| 0-6 months | 8 (50) | 10 (15.2) | |
| 7-12 months | 1 (6.3) | 8 (12.1) | |
| 1-2 years | 2 (12.5) | 21 (31.8) | |
| 2-5 years | 3 (18.8) | 20 (30.3) | |
| >5 years | 2 (12.5) | 7 (10.6) | |
| Duration of symptoms, n (%) | 16 | 66 | .049c |
| 0-1 year | 6 (37.5) | 9 (13.6) | |
| 2-3 years | 3 (18.8) | 29 (43.9) | |
| 3-10 years | 3 (18.8) | 20 (30.3) | |
| 10-25 years | 4 (25) | 7 (10.6) | |
| >25 years | 0 (0) | 1 (1.5) | |
| Nurick score, mean ± SD | 1.6 ±1.4 | 2.0 ±1.4 | .398c |
| mJOA score, mean ± SD | 13.7 ±2.2 | 11.4 ±3.2 | .032b,d |
| ≤11, n (%) | 2 (12.5) | 32 (48.5) | |
| 12-14, n (%) | 9 (56.3) | 22 (33.3) | |
| ≥15, n (%) | 5 (31.3) | 12 (18.2) | |
| Current neck pain score, mean | 3.9 | 5.7 | .031c |
| Best neck pain score, mean | 2.6 | 4.2 | .218c |
| Worst neck pain score, mean | 6.4 | 7.7 | .297c |
| Education level, n (%) | 15 | 65 | .960c |
| Less than high school degree | 2 (13.3) | 4 (6.2) | |
| High school degree or equivalent | 2 (13.3) | 13 (20) | |
| Some college but no degree | 1 (6.7) | 16 (24.6) | |
| Associate degree | 0 (0) | 7 (10.8) | |
| Bachelor’s degree | 4 (26.7) | 11 (16.9) | |
| Graduate degree | 6 (40) | 14 (21.5) | |
| Ethnicity, n (%) | 16 | 66 | .042c |
| White/Caucasian | 12 (75) | 60 (90.9) | |
| Black or African American | 0 (0) | 3 (4.5) | |
| Asian | 4 (25) | 2 (3) | |
| Other | 0 (0) | 1 (1.5) | |
| Country of residence, n (%) | 13 | 63 | .325c |
| United Kingdom | 7 (53.8) | 39 (61.9) | |
| United States | 5 (38.5) | 18 (28.6) | |
| Canada | 1 (7.7) | 5 (7.9) | |
| Australia | 0 (0) | 1 (1.6) | |
| Other | 0 (0) | 0 (0) | |
Abbreviation: mJOA, modified Japanese Orthopaedic Association.
a Mann-Whitney U test.
b Chi-square test.
c Fisher’s exact test.
d For this analysis, scores were grouped into ≤11 (severe), 12-14 (moderate), ≥15 (mild)
In multivariate logistic regression analysis, disease severity (classified by mJOA score 5 ) was independently associated with perceived benefit from physiotherapy (Table 4). Those with mild DCM (mJOA >14) were more likely to perceive benefit from physiotherapy than those with severe DCM (mJOA <12; OR = 28.5, 95% CI = 2.0-410.8, P = .014). Those with moderate DCM (mJOA 12-14) were also more likely to perceive benefit from physiotherapy than those with severe DCM, however, to a lesser extent (OR = 12.7, 95% CI = 1.3-126.2, P = .030). Individuals who waited 1 to 2 years to receive a diagnosis of DCM were less likely to perceive benefit from physiotherapy than those that waited 0 to 6 months (OR = 0.04, 95% CI = <0.01-0.8, P = .035). Respondent ethnicity and symptom duration did not significantly predict perceived benefit from physiotherapy. Receiver operating characteristic (ROC) curve analysis showed the area under the ROC curve (AUC) was 0.866, reflecting excellent predictive performance of the model. 15
Table 4.
Perceived Benefit of Physiotherapy: Multivariate Analysis (n = 82).
| Variable | P | OR | 95% CI for OR |
|---|---|---|---|
| Ethnicity | |||
| White/Caucasian | — | — | — |
| Asian | .066 | 14.41 | 0.84–247.68 |
| Black or African American | .999 | <0.01 | <0.01 to <0.01 |
| Other | .302 | 12.1 | 0.11–1381.38 |
| mJOA score | |||
| ≤11 | — | — | — |
| 12-14 | .030* | 12.72 | 1.28–126.19 |
| ≥15 | .014* | 28.51 | 1.98–410.38 |
| Time to diagnosis | |||
| 0-6 months | — | — | — |
| 6-12 months | .124 | 0.07 | <0.01–2.04 |
| 1-2 years | .035* | 0.04 | <0.01–0.80 |
| 2-5 years | .075 | 0.08 | <0.01–1.29 |
| >5 years | .148 | 0.09 | <0.01–2.33 |
| Duration of symptoms | |||
| 0-1 year | — | — | — |
| 2-3 years | .836 | 1.3 | 0.11–16.24 |
| 3-10 years | .851 | 1.33 | 0.07–26.06 |
| 10-25 years | .065 | 18.43 | 0.84–405.94 |
| >25 years | 1 | <0.01 | <0.01 to <0.01 |
| Current neck pain (1-10) | .522 | 0.04 | 0.79–1.61 |
Abbreviation: mJOA, modified Japanese Orthopaedic Association.
*P < .05.
Discussion
This is the first study to survey the provision and perception of physiotherapy in the non-operative management of DCM. The majority of recipients of physiotherapy had moderate or severe DCM. A minority of respondents perceived benefit from physiotherapy. Perceived benefit was greatest in milder forms of the disease or in respondents with shorter symptom duration. One-third of those with mild or moderate DCM perceived benefit, compared to less than 10% of those with severe DCM. Respondents were most likely to perceive benefit if diagnosed within 6 months of the symptom onset.
Physiotherapy Provision Is Inconsistent and Does Not Align With International Guidelines
Our analysis found no difference in disease characteristics between those who received and did not receive physiotherapy. International guidelines recommend nonoperative physiotherapy as an option for mild, stable DCM. 5 Most physiotherapy recipients in this survey had moderate or severe disease, for whom surgery is recommended. As the international guidelines were released during this survey, this should be considered preimplementation practice. People with DCM can self-refer to physiotherapy in certain jurisdictions, hence the physiotherapy community should be an important target for knowledge translation of international guidelines; it is important that those with moderate or severe DCM understand the limitations of physiotherapy and the importance of early surgical referral. Nevertheless, physiotherapy appears to be underused in cases where it is indicated; most respondents with mild DCM had not received physiotherapy.
Few Perceive Benefit From Physiotherapy, but Perception of Benefit Is More Likely in Those With Milder DCM and Shorter Symptom Duration
Overall, a minority of respondents perceived benefit from physiotherapy (20%). This proportion was greatest in those with mild DCM (30%), and lowest in those with severe DCM (6%). Multivariate analysis found participants with mild DCM were 13 times more likely to perceive benefit than those with moderate DCM, and 29 times more likely than those with severe DCM. The evidence for conservative management of mild DCM is limited.7,16 These findings support reserving physiotherapy for milder disease presentations.
Previous work has shown that delays to DCM diagnosis are common. 17 Delays are associated with greater disease severity 18 and limit surgical outcomes. 1 In this study, those with delayed diagnosis were less likely to perceive benefit from physiotherapy, independent of their disease severity.
The natural history of DCM is poorly understood and represents a research priority as identified by AO Spine RECODE-DCM.9,19 While unpredictable in rate, emerging evidence indicates that DCM is progressive, even in milder clinically stable forms. Using laboratory gait analysis, 20 Kalsi-Ryan et al 21 have demonstrated subclinical progression in mild DCM over 1 to 2 years. Additionally, using quantitative magnetic resonance imaging, Martin et al 22 identified subclinical evidence of DCM. As physiotherapy aims to reduce symptoms and physical impairment rather than modifying the disease process, these findings may align with the trend for early only benefit to physiotherapy.
Limitations
The survey was conducted through Myelopathy.org. Respondents were given a description of DCM its symptoms and asked if they had been diagnosed by a medical professional; it is possible that some respondents did not have DCM. To limit recall bias, time-related questions used categorical ranges, and there was no survey time limit.
Most survey respondents were female; however, gender is not known to be a risk factor for DCM or to affect its prognosis.23,24 No differences in perception and provision of physiotherapy between genders were observed in this study. Though minority ethnic groups had a small representation, the breakdown (88.6% White, 1.2% Black, 5.4% Asian), is comparable to the UK population (86% White, 3.3% Black, 7.5% Asian). 25 Multivariate analysis was used, minimizing bias due to demographic characteristics.
Missing data analysis showed that with one exception, missing data did not introduce statistically significant bias (Supplementary Material 2). Respondents with incomplete answers had a longer time to diagnosis than those with complete answers. Multivariate analysis minimized the impact of introduced bias on other variables; it is unlikely that absent responses have affected our findings.
Respondents were asked if they had received physiotherapy or surgery, but not whether they had been offered it; some may have been offered therapy but declined or not yet received it, and individuals declining surgery may have been offered physiotherapy to minimize impairment.
This survey was retrospective; participants were asked if they had perceived benefit from physiotherapy but disability scores (eg, mJOA and Nurick) were contemporary. This temporal difference may have overestimated the proportion of people with moderate and severe DCM receiving physiotherapy and may have led to recall bias. The use of multivariate analysis, including symptom duration, has attempted to mitigate this.
Finally, the logistic regression odds ratios have broad confidence intervals. This reflects small samples sizes due to low rates of perceived physiotherapy benefit. Our conclusions remain valid when using values at the interval extremes.
Future Directions
The role of physiotherapy was identified as an important research uncertainty during the AO Spine RECODE-DCM James Lind Alliance research priority setting partnership. The findings here align with the published literature: there is likely a group who benefit. Clearer identification of this subgroup and the physiotherapy parameters (type and dosage) that deliver the most benefit will be key to ensuring better outcomes, alongside the dissemination of recommendations to clinical practice.
New approaches to DCM assessment will be important to optimize management. Many current assessments lack the sensitivity to detect or track small changes in disease severity, particularly in early and mild forms of the disease. Improved sensitivity would enable earlier detection of patients who have progressed from mild to moderate DCM, or who have progressive DCM (ie, have moved into the zone of surgical intervention being recommended by the AO Spine guidelines).19,26 The development of new clinical assessments for DCM is a further AO Spine RECODE-DCM research priority. 19
Other emergent techniques, such as the use of microstructural magnetic resonance imaging, serological biomarkers, and genetic analysis, may enhance hospital-based assessment and bring the benefits of personalized medicine to the diagnosis and management of DCM. 27
Conclusions
The provision physiotherapy in the management of DCM is inconsistent and differs from the recommendations of international guidelines. Few people with cervical myelopathy perceive benefit from physiotherapy but the greatest perceived benefit was found in respondents with mild DCM. Further work is needed to establish the appropriate role of physiotherapy for this population.
Supplemental Material
Supplemental Material, sj-pdf-1-gsj-10.1177_2192568220961357 for Provision and Perception of Physiotherapy in the Nonoperative Management of Degenerative Cervical Myelopathy (DCM): A Cross-Sectional Questionnaire of People Living With DCM by Max B. Butler, Oliver D. Mowforth, Abdul Badran, Michelle Starkey, Timothy Boerger, Iwan Sadler, Julia Tabrah, Caroline Treanor, Lucy Cameron Grad Dip Phys, Sukhvinder Kalsi-Ryan, Rodney J. Laing, Benjamin M. Davies and Mark R. N. Kotter in Global Spine Journal
Supplemental Material, sj-pdf-2-gsj-10.1177_2192568220961357 for Provision and Perception of Physiotherapy in the Nonoperative Management of Degenerative Cervical Myelopathy (DCM): A Cross-Sectional Questionnaire of People Living With DCM by Max B. Butler, Oliver D. Mowforth, Abdul Badran, Michelle Starkey, Timothy Boerger, Iwan Sadler, Julia Tabrah, Caroline Treanor, Lucy Cameron Grad Dip Phys, Sukhvinder Kalsi-Ryan, Rodney J. Laing, Benjamin M. Davies and Mark R. N. Kotter in Global Spine Journal
Supplemental Material, sj-pdf-3-gsj-10.1177_2192568220961357 for Provision and Perception of Physiotherapy in the Nonoperative Management of Degenerative Cervical Myelopathy (DCM): A Cross-Sectional Questionnaire of People Living With DCM by Max B. Butler, Oliver D. Mowforth, Abdul Badran, Michelle Starkey, Timothy Boerger, Iwan Sadler, Julia Tabrah, Caroline Treanor, Lucy Cameron Grad Dip Phys, Sukhvinder Kalsi-Ryan, Rodney J. Laing, Benjamin M. Davies and Mark R. N. Kotter in Global Spine Journal
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This report is independent research arising from a Clinician Scientist Award, CS-2015-15-023, supported by the National Institute for Health Research. We gratefully acknowledge support by the Cambridge NIHR Brain Injury MedTech Cooperative. MRNK is funded by a NIHR Clinician Scientist Award CS-2015-15-023. BMD is supported by a Royal College of Surgeons Research Fellowship and a NIHR Clinical Doctoral Research Fellowship. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
ORCID iD: Max B. Butler, BSc, BA  https://orcid.org/0000-0002-2536-0534
https://orcid.org/0000-0002-2536-0534
Ethical Approval: The study was ethically approved by the University of Cambridge Human Biology Research Ethics Committee. All research was performed in accordance with the relevant guidelines and regulations.
Informed Consent: All respondents completed the questionnaire voluntarily and were informed before doing so that their responses would be used anonymously for research purposes. The initial page stated the study objectives and host organization details. This acted as electronic consent and continuation was taken as agreement.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Davies BM, Mowforth OD, Smith EK, Kotter MR. Degenerative cervical myelopathy. BMJ. 2018;360:k186. doi:10.1136/bmj.k186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davies BM, Munro CF, Kotter MR. A novel insight into the challenges of diagnosing degenerative cervical myelopathy using web-based symptom checkers. J Med Internet Res. 2019;21:e10868. doi:10.2196/10868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oh T, Lafage R, Lafage V, et al. Comparing quality of life in cervical spondylotic myelopathy with other chronic debilitating diseases using the Short Form Survey 36-Health Survey. World Neurosurg. 2017;106:699–706. doi:10.1016/j.wneu.2016.12.124 [DOI] [PubMed] [Google Scholar]
- 4.Fehlings MG, Ibrahim A, Tetreault L, et al. A global perspective on the outcomes of surgical decompression in patients with cervical spondylotic myelopathy: results from the prospective multicenter AOSpine International Study on 479 patients. Spine (Phila Pa 1976). 2015;40:1322–1328. doi:10.1097/BRS.0000000000000988 [DOI] [PubMed] [Google Scholar]
- 5.Parthiban J, Alves OL, Chandrachari KP, Ramani P, Zileli M.Value of surgery and nonsurgical approaches for cervical spondylotic myelopathy: WFNS Spine Committee Recommendations. Neurospine. 2019;16:403–407. doi:10.14245/ns.1938238.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Badran A, Davies BM, Bailey HM, Kalsi-Ryan S, Kotter MR. Is there a role for postoperative physiotherapy in degenerative cervical myelopathy? A systematic review. Clin Rehabil. 2018;32:1169–1174. doi:10.1177/0269215518766229 [DOI] [PubMed] [Google Scholar]
- 7.Rhee J, Tetreault LA, Chapman JR, et al. Nonoperative versus operative management for the treatment degenerative cervical myelopathy: an updated systematic review. Global Spine J. 2017;7(3 suppl):35S–41S. doi:10.1177/2192568217703083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies BM, McHugh M, Elgheriani A, et al. Reported outcome measures in degenerative cervical myelopathy: a systematic review. PLoS One. 2016;11:e0157263. doi:10.1371/journal.pone.0157263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davies BM, Khan DZ, Mowforth OD, et al. RE-CODE DCM (REsearch objectives and common data elements for degenerative cervical myelopathy): a consensus process to improve research efficiency in DCM, through establishment of a standardized dataset for clinical research and the definition of the research priorities. Global Spine J. 2019;9(1 suppl):65S–76S. doi:10.1177/2192568219832855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davies B, Mowforth O, Sadler I, et al. Recovery priorities in degenerative cervical myelopathy: a cross-sectional survey of an international, online community of patients. BMJ Open. 2019;9:e031486. doi:10.1136/bmjopen-2019-031486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6:e34. doi:10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davies BM, McHugh M, Elgheriani A, et al. The reporting of study and population characteristics in degenerative cervical myelopathy: a systematic review. PLoS One. 2017;12:e0172564. doi:10.1371/journal.pone.0172564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhee JM, Shi WJ, Cyriac M, et al. The P-mJOA: a patient-derived, self-reported outcome instrument for evaluating cervical myelopathy: comparison with the mJOA. Clin Spine Surg. 2018;31:E115–E120. doi:10.1097/BSD.0000000000000591 [DOI] [PubMed] [Google Scholar]
- 14.Davies B, Kotter M. Lessons from recruitment to an internet-based survey for degenerative cervical myelopathy: comparison of free and fee-based methods. JMIR Res Protoc. 2018;7:e18. doi:10.2196/resprot.6567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd ed. John Wiley; 2013. [Google Scholar]
- 16.Rhee JM, Shamji MF, Erwin WM, et al. Nonoperative management of cervical myelopathy: a systematic review. Spine (Phila Pa 1976). 2013;38(22 suppl 1):S55–S67. doi:10.1097/BRS.0b013e3182a7f41d [DOI] [PubMed] [Google Scholar]
- 17.Hilton B, Tempest-Mitchell J, Davies B, Kotter M. Route to diagnosis of degenerative cervical myelopathy in a UK healthcare system: a retrospective cohort study. BMJ Open. 2019;9:e027000. doi:10.1136/bmjopen-2018-027000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pope DH, Mowforth OD, Davies BM, Kotter MRN. Diagnostic delays lead to greater disability in degenerative cervical myelopathy and represent a health inequality. Spine (Phila Pa 1976). 2020;45:368–377. doi:10.1097/BRS.0000000000003305 [DOI] [PubMed] [Google Scholar]
- 19.AO Foundation. The top ten research priorities for DCM. Accessed June 3, 2020. https://aospine.aofoundation.org/research/recode-dcm/priorities
- 20.Kalsi-Ryan S, Rienmueller AC, Riehm L, et al. Quantitative assessment of gait characteristics in degenerative cervical myelopathy: a prospective clinical study. J Clin Med. 2020;9:752. doi:10.3390/jcm9030752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalsi-Ryan S, Clout J, Rostami P, Massicotte EM, Fehlings MG. Duration of symptoms in the quantification of upper limb disability and impairment for individuals with mild degenerative cervical myelopathy (DCM). PLoS One. 2019;14:e0222134. doi:10.1371/journal.pone.0222134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin AR, De Leener B, Cohen-Adad J, et al. Can microstructural MRI detect subclinical tissue injury in subjects with asymptomatic cervical spinal cord compression? A prospective cohort study. BMJ Open. 2018;8:e019809. doi:10.1136/bmjopen-2017-019809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shimomura T, Sumi M, Nishida K, et al. Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment. Spine (Phila Pa 1976). 2007;32:2474–2479. doi:10.1097/BRS.0b013e3181573aee [DOI] [PubMed] [Google Scholar]
- 24.Bednarik J, Kadanka Z, Dusek L, et al. Presymptomatic spondylotic cervical myelopathy: an updated predictive model. Eur Spine J. 2008;17:421–431. doi:10.1007/s00586-008-0585-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Office for National Statistics. Ethnicity and national identity in England and Wales: 2011. Accessed May 11, 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/ethnicityandnationalidentityinenglandandwales/2012-12-11
- 26.Mowforth OD, Davies BM, Kotter MR. The use of smart technology in an online community of patients with degenerative cervical myelopathy. JMIR Form Res. 2019;3:e11364. doi:10.2196/11364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Badhiwala JH, Ahuja CS, Akbar MA, et al. Degenerative cervical myelopathy—update and future directions. Nat Rev Neurol. 2020;16:108–124. doi:10.1038/s41582-019-0303-0 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-gsj-10.1177_2192568220961357 for Provision and Perception of Physiotherapy in the Nonoperative Management of Degenerative Cervical Myelopathy (DCM): A Cross-Sectional Questionnaire of People Living With DCM by Max B. Butler, Oliver D. Mowforth, Abdul Badran, Michelle Starkey, Timothy Boerger, Iwan Sadler, Julia Tabrah, Caroline Treanor, Lucy Cameron Grad Dip Phys, Sukhvinder Kalsi-Ryan, Rodney J. Laing, Benjamin M. Davies and Mark R. N. Kotter in Global Spine Journal
Supplemental Material, sj-pdf-2-gsj-10.1177_2192568220961357 for Provision and Perception of Physiotherapy in the Nonoperative Management of Degenerative Cervical Myelopathy (DCM): A Cross-Sectional Questionnaire of People Living With DCM by Max B. Butler, Oliver D. Mowforth, Abdul Badran, Michelle Starkey, Timothy Boerger, Iwan Sadler, Julia Tabrah, Caroline Treanor, Lucy Cameron Grad Dip Phys, Sukhvinder Kalsi-Ryan, Rodney J. Laing, Benjamin M. Davies and Mark R. N. Kotter in Global Spine Journal
Supplemental Material, sj-pdf-3-gsj-10.1177_2192568220961357 for Provision and Perception of Physiotherapy in the Nonoperative Management of Degenerative Cervical Myelopathy (DCM): A Cross-Sectional Questionnaire of People Living With DCM by Max B. Butler, Oliver D. Mowforth, Abdul Badran, Michelle Starkey, Timothy Boerger, Iwan Sadler, Julia Tabrah, Caroline Treanor, Lucy Cameron Grad Dip Phys, Sukhvinder Kalsi-Ryan, Rodney J. Laing, Benjamin M. Davies and Mark R. N. Kotter in Global Spine Journal