Abstract
Introduction
The mobile digital culture (MDC) supports individual lives, communities, and real-time organizational surveillance during COVID-19 emergencies. Hence, the study examined the advancement in smart health devices evidence in smartphone apps technologies in surveillance, control, and tracking potential virus areas among high-risk populations.
Objective
The study explored how environmental condition and MDC mediates between knowledge of App and mobile usability in the prevention of COVID-19 infection in high-risk areas.
Methods
Using the concept of UTAUT, the study conceptualized that mobile usability, MDC, knowledge of App and environmental condition, are essential for COVID-19 mitigation. A cross-sectional method was adopted through an online survey to assess data from n = 459 mobile users. The association of the study models was appraised through structural equation models (Amos v.24.0).
Result
We found mobile usability, knowledge of App, and MDC were statistically significant to COVID-19 mitigation. Environment condition as mediator had no effect in the study models. However, moderating effect of MDC shows a negative influence on the association between COVID-19 mitigation and knowledge of apps.
Conclusion
Future policies should consider the development of mHealth technology to improve end-user experience. Also, future policies should entail data privacy to reduce the infringement of data collected. This approach will lead to a confidential, high acceptance of usability of mHealth apps infectious disease prevention.
Keywords: Mobile health, Mobile digital culture, Knowledge apps, Technology surveillance, Covid-19 mitigation
Abbreviations: CSM, Collaborative self-management; EC, Environmental Conditions; IEQ, Indoors Environmental Qualities; NCIRD, National Centre for Immunization and Respiratory Diseases; MDC, Mobile Digital Culture; MU, Mobile Usability; UTAUT, Unified Theory of Acceptance and Use of Technology
Credit author statement
Sayibu Muhideen: Conceptualization, Methodology, data collection and analysis; Jianxun Chu: supervision of data collection and proofreading; Akintunde Y. Tosin: exploration, investigation and editing; Olayemi Hafeez Rufai: reviewing of data and coding, proofreading; Glory George Ufor and Tunde Simeon Amosun: validation and editing.
1. Introduction
Health technologies have played a significant role by supporting the global population in reducing the risk exposure of the COVID-19 pandemic. The ubiquity of smartphones has increased access to healthcare services, supporting clinical practices, and enhanced public health strategic surveillance of COVID-19 infection (Hilty et al., 2021). Some of the strategies for the pandemic risk mitigation hammered on social distancing, personal hygiene, masking up, along with the adoption of smart devices capable of tracking people in geographically low- and high-risk areas (Güemes et al., 2021). Therefore, smart thermometer health technologies offer robust support in any healthcare system to improve health and provide syndromic protection that facilitates real-time surveillance evaluation of the population.
The individual usage of mobile technology for self-care became a health digital culture during the COVID-19 crisis. Advancement in health technology has offered two-way interactive communication approaches like “video chat visits” through smartphones, chatboxes with automated algorithms (Kritikos, 2020). Thus, technological efforts of governments and the European Union through public health policies have solicited for the following ten scientific dimensions: Artificial Intelligence (AI); Blockchain; open-sourced technologies; telehealth technologies; 3-dimensional printing; gene-editing technologies; nanotechnologies; synthetic biology; drones; robot, all mentioned are innovative means of fighting COVID-19 pandemic crisis (Kritikos, 2020), which are parallel to mobile-infused thermometer sensors for self-care and self-check operationalization.
Therefore, digital culture present an emerging trends, situations, and changes regulated and innovated by the scientific knowledge of times and things (Deuze, 2006). The digital culture conceptualization and initiatives describe how mobile technology influences people attitudes during COVID-19 in healthcare systems and emergencies. Establishing technology systems like innovative smart-pocket tool, smart thermometer are timely emergency health compliance to International Health Regulation (IHR) and for WHO member states to meet standard measures for COVID-19 surveillance SARS-Cov-2 (Jamison, 2018; WHO, 2021).The digital culture molds global health among societies, communities, organizational transformation over mobilized perception of attitude, behavioral reactions to mitigation. . The current study attempts to establish the relationship between mobile digital culture (MDC) and the mobile behaviors and usability experience in population evidence in the COVID-19 pandemic risk mitigation.
Digital literacy has influenced cultures, behaviors, attitudes, and habits due to global health technology advancement and emerging internet of things (IoT). The smart thermometer apps detectors available in android and iOS smartphones have the capacity to detect body temperature, monitoring, and surveillance (Miller et al., 2018). Generally, scholars and academics have subsumed the emerging values of ubiquitous smartphones and personal computers crucial for public health function (Velavan & Meyer, 2020). Undoubtedly, mobile cultures have succinctly paved the way for innovation in human social health management and clinical decision-making. The smartphone inclusive policy mitigation is MDC observed positive or negative attitude towards technology benefits and challenges to humanity. The MDC serves as a compliment to keep up the health records of institutions and organizations through electronic health record that supports testing and monitoring human body temperature, enabling organizations to accelerate health surveillance. The concept of digital mobile culture is tied to the technology revolution shaping human behavioral fragmentation within societies and to affect social cohesion. .
In Scope, the current research conceptualized mobile usability, knowledge of App, and MDC as a strategy in COVID-19 infection prevention and control. The study approaches mobile health surveillance technology as a potent strategy to mitigate COVID-19 infection by employing self-test body temperature enabled by smartphones. Since mobile devices have internet services, global positioning system (GPS), camera sensors, and the capacity to measure heartbeats and blood pressure, they become instrumental in tracking infections in low to high-risk populations (C. Lee Ventola, 2014). The main research objective is to examine how MDC and environmental condition influence mobile usability and knowledge of App as a viable strategy in COVID-19 risk mitigation.
1.1. Related literature
The healthcare system's challenges due to its face-to-face nature make virtual consultations innovative health maintenance approach. The concepts of health consultation and an integrated automated system of reaching out to distance communities is innovative and became pronounced during the COVID-19 outbreak (Nicolini, 2021). Health technologies have provided support in improving patients' health outcomes (Akintunde et al., 2021). For instance, mHealth is evidential web-based technology that has improved patients' asthmatic collaborative self-management (CSM)) ( Sacco et al., 2020). The CSM mHealth platform was accessible on smartphones, tablets, or desktops with user-centered features, that support processing information with ease and convenience at any time. As a multifunctional mHealth platform with the capacity to monitor patients' breathe and self-monitoring of patient's asthma it supports: (1) breathe control, (2) real-time action plan, (3) real-time environmental conditions, and (4) interactive communication. Patients reported self-satisfaction in the platform's usability in managing asthma, control management system, and confidence in the platform management system (Morita et al., 2019). Substantial utilization of the CSM mHealth platform was evidence of the internal and external validity of the intervention. Patient satisfaction and general population acceptance show more utilization associated with environmental relevance.
In real-world circumstances of solving the COVID-19 pandemic, environmental conditions as facilitating agents to technology usability are significant. In practical cases, smartphone application and usability in web-based cannabis user treatment, major treatment of depression of mental healthcare, children with insomnia apnea treatment issues delivered evidence-based results (Jonas et al., 2019). The environmental changing condition often necessitates the technology ambiance given latter life smartphones usability application (app) extensively assisted the society. A Sydney Australian focus-group experiment found a reliable and valid app that accelerated efficiency in the external environment condition, providing accurate weather readability, transport options, community navigation movement in smartphones usability (Wilson, Leigh Ann; O'Loughlin, K; Hector, R; Black, DA; 2021). Agbota et al. (2014) found an environmental monitoring scheme on cultural impact in a quest for relatively easy use and remote access. The prototype of environmental monitors included remote sensors, temperature, and humidity sensors, which opened up real-time visualization of measurements. In a related development, Noguchi et al. (2018) established in findings that, aging population necessitated building designs with indoor environmental quality (IEQ) to mainly accommodate individual needs and demands. The architectural designers and professionals incorporated usability applications monitored by smartphones, engaged in building capacity in subjectivity and objectivity of the end-users. Other studies supported the efforts advocated for mobile technology usability in the community environment healthy evaluation of parks to provide youth with healthy physical activities, promoted by smartphone guidance (Besenyi et al., 2018).
Significantly, the virtual environmental conditions coupled with collaborative technology changes are increasing potentials and opportunities in everyday life. The perpetual social environment and individual factors, such as gender and age, have significance in the virtual environment such as perceived usability, ease of use, and effort expectancy. A study found gender more aggressive and proactive with women's technology-related anxiety and immersion (Schmidt et al., 2013). Our virtual environment progressively targets the emotional-inducing stimuli for exposure therapy, yet differences in responses from the environment matter. Fetscherin, M., and Lattemann, C, and cited Schmidt et al. (2013) found no relationship between technology virtual related-anxiety environment and intention to use technology. Therefore, environmental conditions enabling collaborative and interactive usability will ensure technology agglomeration.
Mobile applications (apps) are increasingly gaining popularity, and interventions targeted systematic phonics knowledge and phonological awareness skills. The content quality and usability of the apps determined structural appraisals and data extractions. mHealth apps have transformed health access, communication, patient monitoring, and evaluations (Furlong et al., 2021). The demand and usability of mobile phones worldwide reached 5.2 billion recently, thus 67% of the global population (Chen et al., 2010). The usability of mobile apps incorporated in managing health-related issues is becoming increasingly popular and demanding (O’Dea, 2021). Recent findings indicated Apple recorded 45,478 health care apps in their App Store during early 2020 (Bol et al., 2018) and a total of 204 billion app downloads in 2019, which equates to US $120 billion on app-related spending (Department, 2021). Bol et al. (2018) literature established the Google Store and iTunes Stores readiness and ubiquitous, essential benefits and significance of mobile health apps for preventive and control health and health care. Also found about 3,195,204 active mobile apps usability technology in the iTunes app store and the 3,612,250 active apps in the Google Play store, 95,851 and 105,912, respectively (AppBrains, 2020). European (2012) stated “e-health – when applied effectively— delivers more personalized ‘citizen-centric’ healthcare, which is more targeted, effective and efficient and helps reduce errors, as well as the length of hospitalization. It facilitates socio-economic inclusion and equality, quality of life and patient empowerment through greater transparency, access to services and information and the use of social media for health.” Therefore, the legal implication and policy barking the status quo of mHealth is aligned mobile digital transformation strategies of health and healthcare. How can mHealth adaptation enable the control and prevention of COVID-19 through geographical surveillance in low and high-risk areas of the virus?
Nonetheless, this study observed mobile usability concerning knowledge of apps: the youth (digital generation), the literates in society (high-level education and with eHealth skills). Our study attempted to confirm if the knowledge of apps positively relates to mobile usability in terms of digital culture. Ye et al. (2021) and Lane et al. (2020) the Dementia Care App has critically supported the improvement of the Quality of Life (QOL) of people with dementia and family healthcare with a reduction in caregivers workload. Similarly, the usability features of the apps must be simplified to the end-users. Therefore, the mHealth capacity and environmental conditions to engage health surveillance, temperature detections and testing with the mobile digital transformation of COVID-19 are laudable. The usability of mobile health apps, efficiency, effectiveness, and satisfactory application in detecting or testing temperature is in the pipeline of technology inclusion. Other attributions: learnability, memorability, errors, simplicity, understanding, and level of performance are in the offering (Johnson et al., 2020). Quality of Life in healthcare has recently been tied to technology advancement, and a promising crowd sources technology potential improved the COVID-19 tracing and tracking across the social gathering. Mobile digital culture, smartphones, and web-based health applications sweeping across all human races are relevant for the future (Vokinger et al., 2020). In a related plethora of literature, knowledge of apps in mHealth assiduously intervened in critical moments of the COVID-19 epidemic, by leveraging access to healthcare on social distancing, usability is significant to the benefits of the general population across age, gender, and education (Inal et al., 2020).
Inal et al. (2020) research found how evidential mHealth apps usability evaluations from computer science experts and human-computer interactions regarding features and mobility of the apps. The COVID-19 pandemic exposed most developed and developing countries lacking mobile digital culture transformation to deal with health issues. Such are cases of a scientific laboratories lacking decentralizations for virus testing, verification, and confirmation that influence timely interventions and hinder technology ambiance action necessary for institutions and nations (Shao & Hao, 2020). Mobile ubiquity makes it imperative and a crowdsourced digital tool for temperature testing, Electronic Health Records (EHR), health monitoring, and citizen's virus position tracking. The mobile digital culture is an element of many mHealth apps that actively or passively (user smartphone sensors) collect and store people's health data. When aggregated, it can be informative about the current state of the COVID-19 epidemic (Vokinger et al., 2020). The mobile digital technology enables the testing temperature of human pulse, tracking the COVID-19 virus at a certain distance in a crowded setting, and enabled monitoring and proximity tracer.
Electronic health data is fragile, and recent COVID-19 mHealth data is no exception, which requires some level of confidentiality and privacy of the highest degree. Experts have bemoaned the privacy perspective over the regulatory collection of data through mobile digital systems is extremely sensitive, for which legal privacy safeguards are of paramount importance (Buckee et al., 2020). For instance, the study collection of geolocation data poses robust challenges for privacy, confidentiality depending on the accuracy of geolocation positioning and proximal internal distance measurements (Richardson et al., 2015). Also, the extensive data system is under this collection, entreating a broad range of anonymity of information, vigorous authorities, and legality as formidable health practices in the COVID-19 strategic mitigation. Also, mHealth apps details rarely provide enough terms and conditions to the end users to ascertain the risk for privacy rights infringement or data collections and ownership. Again, this precariousness cause confusion, and eventually lead to low acceptance and usability in the mitigation process. Therefore, user's rights, obligations, and understanding the trend is vital for potentially reliable and privacy-preserving knowledge of the app, well-intended goals for the control and preventive measures of apps for better epidemic monitoring and tracking (Vokinger et al., 2020). In essence, the global health promulgation of social distance policy can be intervening with surveillance of mHealth monitoring and tracking innovative means of strategic mitigation of the pandemic.
Inal et al. (2020), following the research analogous reformation of the technology application in health, presented new insight to understand usability. In the findings, most treated reliance on mHealth is availability (Carey et al., 2016), device and communication affordance (Bauer et al., 2018; De Korte et al., 2018), the novelty of mHealth, and user acceptance (Barrio et al., 2017; De Korte et al., 2018), positive scientific knowledge of mHealth and contextual evidence (Deady et al., 2018) highly critical to replicate, and technology device sensors. Potentially, it pointed to a successful implementation of mHealth in some jurisdictions of previous research (De Korte et al., 2018) that need to be streamlined. This evidence also scales upon cost-effectiveness in applying the mHealth phenomenon (De Korte et al., 2018; Ruggiero et al., 2015) in the COVID-19 pandemic. In most instances, the usability of mHealth apps is appropriate for healthy people than patients, who might not be physically or emotionally fit to comprehend the knowledge of the app. Evaluating the effective application of the technology outcome in relation to social distancing in test temperature and surveillance mitigation of COVID-19 is what this designed research is intended doing.
2. Methods and materials
2.1. Study design
The cross-sectional survey stratified the sample into groups of African continent, Asia and Europe according to health workers, industrial workers, and institutions across population and locations. The distributed questionnaires created two online links that validated the study during the pre-test and pilot study. The convenient sampling techniques were adopted through an online survey. A total of 600 questionnaires were distributed, with 88% response rate with only 459 samples data retained to be quantitatively analyzed. The quantitative method is deeply appropriate due to the conceptual framework proposed in the study. The online questionnaire were adopted to reaffirmed on the concept of the mobile digital culture and mobile usability. Some questions were excluded after the pilot study was conducted to ensure complete comprehension among target groups. The study encapsulated previous theoretical development from technology adoption that have been verified and validated (Dwivedi et al., 2019; Lulin et al., 2020; Venkatesh et al., 2003).
2.2. Data collection and study population
The COVID-19 risk mitigation assessment considers institutions and organizations' innovative intervention measures evidenced in the control and administration of China COVID-19 pandemic center (National Center for Immunization and Respiratory Diseases (NCIRD), 2021). These measurements approach took into account community mitigation action plan assessments of the COVID-19 risk mitigation (Webpage, 2021). Mobile usability concerns, knowledge of App, environmental conditions, mobile digital culture were explored in association with the COVID-19 risk mitigation. Participants were surveyed from Africa, Asia, and Europe with hyperlink shared on social media platforms (WeChat, WhatsApp, and Facebook). Data collection was done at different time periods. First data collection was conducted from across Asia (WeChat platform), second part Africa (WhatsApp platform), and Europe (Facebook and emails), which lasted for three months. Table 1 explained all the predicting variables and predictor, and proposed hypotheses justified. Similarly, the study conceptual framework presented all the relationships proposed in the study in Fig. 1 . The total respondents across all time (n = 459) was statistically logical to represent the study population. Considering the time bound and target population.
Table 1.
Definition of Study Constructs and Hypotheses developed.
| Variables | Definition | Sources |
|---|---|---|
| Mobile Usability | This measure assesses the degree to which people can easily and quickly use electronic devices and smart phones to measure health status i.e smart-thermometer for body temperature. | (Bevan & Curson, 1997; Carey et al., 2016; Saleh et al., 2015; Zhao et al., 2021) (Tao et al., 2020) |
| Knowledge of App | The ability of end users to comprehend with technologies which include user flexibility and understanding the working idea of the app. | (International Pharmaceutical Federation, 2019; Jou et al., 2016; Zhao et al., 2021) |
| Environmental Condition | Refers to people's perceptions of the resources and support available to perform a mobile technology action in a setting. A condition that enable accessible use of technology | Venkatesh et al. (2003) |
| Mobile digital culture | User accumulated knowledge or skills of mobile technology that influences willingness to participate in technology oriented events or activities in institutions. | (Hilty et al., 2021; Leander & Vasudevan, 2009) |
| Risk Mitigation | The degree of taken safety precautions and control measures of the pandemic. Personal, communication measure as part of actionable control and prevent the spread of COVID-19 in communities, organizations. | (National Center for Immunization and Respiratory Diseases (NCIRD), 2021) 2021) (Dubey et al., 2020) |
|
Hypotheses Development |
||
| H1: | Mobile Relative Usability has a positive relationship with an environmental condition in using the technology for Covid-19 mitigation. | |
| H2: | Environmental condition has a positive relationship with Covid-19 mitigation strategy among institutions/organizations. | |
| H3: | Mobile usability has positive effects on knowledge of the mobile app for the surveillance of Covid-19 mitigation. | |
| H4: | Knowledge of app has positive effects on the mobile digital culture as surveillance technology of Covid-19 mitigation. | |
| H5: | Mobile digital culture has positive effects on social Covid-19 mitigation strategies. | |
| H6: | Knowledge of mobile app moderates on environmental conditions that enable the Covid-19 mitigation in institutions/organizations. | |
| H7: | Mobile digital culture moderates on knowledge of App that enable the Covid-19 mitigation strategies in institutions/organizations. | |
| H8: | Environmental condition mediates between mobile usability and Covid-19 mitigation. | |
Fig. 1.
Conceptual model framework.
2.3. Procedures and measures
The online hyperlink shared distinctively explained all predictors and predicting variables. The five constructs adapted from previous studies are mobile usability (MU), environmental conditions (EC), knowledge of apps (K-App), mobile digital culture (MDC) in predicting COVID-19 risk mitigation. Based on various modifications and refinements on the constructs, the Unified Theory of Acceptance and Use of Technology, through reconstructed 51 online questionnaires measure usability of technology (I. et al., 2014; Przysucha et al., 2017; Inal et al., 2020), environmental condition (Venkatesh et al., 2003), knowledge of apps (Furlong et al., 2021), mobile digital culture (Jaana & Paré, 2020), and COVID-19 risk mitigation (Güemes et al., 2020). The COVID-19 risk mitigation solely relies on the World Health Organization framework (Dubey et al., 2020; Walkthrough, 2020). Table 1 also indicated sources of the study measures. The mobile digital culture focused on eight measuring instruments focused on ubiquity, affordability, temperature test, surveillance, remote sensors with eight questions (Goggin, 2020; Jaana & Paré, 2020). Knowledge of app was measured with five questions related to people understanding of using application to access, test-detect, and collaborate with health authorities with health information (Song et al., 2021). Other measurements were adopted from Unified Theory of Acceptance and Use of Technology modified to suit this study; environmental condition were five questions that explore how the environmental friendliness and easy use of the mobile smartphones. UTAUT is an accumulated research theories and models enclosed novelty of Technology Acceptance (Ahmad, 2014; Venkatesh et al., 2003). The unified constructs of different measurements, developed theory with many facets UTAUT: effort expectancy, performance expectancy, social influence, intention to use, but only the former was utilized in this study analysis occationed EC mobile culture (Pinchot et al., 2010; Venkatesh et al., 2003). With each of these constructs, five questions in each case. Likert scale was used for respondents to assess their agreement or disagreement in each construct ranging from strongly agree to strongly disagree (1–5) (Zainudin Awang et al., 2016).
3. Data analysis
The philosophical and psychometric assessment of the study constructs were evaluated applying the confirmatory factor analysis and structural equation models from Amos 24.0 (Shek & Yu, 2014). The categories of the constructs were simultaneously tested using a single model assessment of validity and reliability. SEM is well established for quantitative technique in handling multivariate or multiple constructs analysis simultaneously, considers errors, regression weight, correlated measurement errors, and constructs content and internal validity (Awang et al., 2017; Mcneish, 2017; Mohammad-Alizadeh-Charandabi et al., 2016). The outcome of these strengths applied to the study involving mediation and moderation effects (A. Hayes, 2013, pp. 3–4; Mackinnon & Dwyer, 1993), employed in the analysis of highest order (Afthanorhan et al., 2019). Furthermore, these applied circumstances could enable the study to determine the quality of measurement model assessment of good fitness (i.e: Comparative Fit Index (CFI), Incremental Fitness Index (IFI), Tucker-Lewis Index (TLI), Normed Fitness Index (NFI), Goodness Fit-index (GFI), and Adjust goodness Fit Index AGFI). Also, among other discussions is operationalized mobile usability within the mobile digital culture and remote surveillance of the COVID-19 in low to high risk population.
3.1. Results
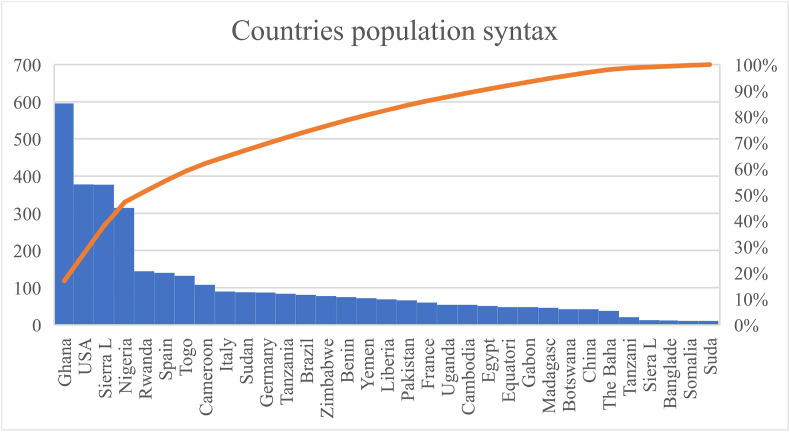
The study responses were across regions Africa, Asia, and Europe in Fig. 2 (see Fig. 1). The Pareto Chat showed in Fig. 2 plots of the distribution of countries’ representation, which is presented in descending order of frequency, with a cumulative orange line a secondary axis as a percentage of the total. Generally, participation in Sub-Sahara Africa, the USA, and Europe was statistically satisfied, 88%, 58%, and 23%, respectively. The concept and power of social media as an effective tool confirmed the MDC of data collected. The respondents globally who participated in this survey were from Ghana, Nigeria, Pakistan, Sierra Leone, Rwanda, Spain, and the USA, leading poles from high, medium, and low countries Fig. 2. The study setting expected a higher response rate from Asian continent, this could be attributed to apathy of the population. Social media influence was ensured from the USA and Spain participants, majority of these respondents participated via the hyperlink shared on Facebook. Significantly, X-axis from point of 0–100 adjusted upward higher with Ghana, the USA, Sierra Leone, Nigeria. Downward trend of the bar graphs started with Rwanda to Sudan being the least from Fig. 2.
Fig. 2.
Country distribution of study respondents.
Table 2 indicates the age range 15–19 years and (20–30years) class group are the 21st Century generation users of smartphones, and highly responsive to the survey. The Ph. D, Post-graduates and bachelor levels were rated (33%, 42%, and 20%). In comparison, the male to female response rates 76% and 24%. Among the constructs under study, the highest mean score is the COVID-19 risk mitigation 4.2222 with a standard deviation of 0.583, environmental condition and knowledge of app means score: 3.71 and 3.71 while standard deviation 0.67 and 0.68 respectively. The mobile digital culture mean score is 3.66 with a standard deviation of 0.54 and the mobile usability mean score 3.46 with a standard deviation of 0.63 from Table 1.
Table 2.
Demographics of the study.
| Control Variables | Frequency | Percent | Mean | Std. Deviation | |
|---|---|---|---|---|---|
| Age | 15–19 years | 195 | 42.5 | 1.67 | 0.667 |
| 20–30years | 231 | 50.3 | |||
| 30–40years | 24 | 5.2 | |||
| 40–50years | 9 | 2 | |||
| Gender | Male | 348 | 75.8 | 1.24 | 0.429 |
| Female | 111 | 24.2 | |||
| Education | High School | 6 | 1.3 | 4.03 | 0.886 |
| College | 15 | 3.3 | |||
| Bachelor | 93 | 20.3 | |||
| Post-Graduate | 192 | 41.8 | |||
| Ph. D | 153 | 33.3 | |||
| Experience | 3.65 | 0.994 | |||
| Mobile Usability | 3.4616 | 0.62630 | |||
| Environmental Condition | 3.7059 | 0.69661 | |||
| Knowledge of App | 3.7033 | 0.68027 | |||
| Mobile Digital culture | 3.6609 | 0.54304 | |||
| Covid-19 Risk Mitigation | 4.2222 | 0.58261 | |||
Table 3 indicated the correlation of all constructs observed in the study, showing positive correlation and the diagonal highlighted represented reliability and validity obtained from SPSS v. 25.0. In the same vein, the study also reported composite reliability, average variance extracted, factor loadings, construct correlations, and discriminant validity. In addition, the structural model analysis assessment is based on output obtained to digest and justify the study objectives. Furthermore, the model obtained from Amos got some poor loadings less than the threshold 0.7, but scholarly accepted statistically loading <0.69 (Martynova et al., 2018). Poor loadings affected some constructs, which eventually gave in lower goodness fit of IFI and AGFI but scholarly considered (Awang, 2015). From modification indices some items were covaried to enhance loading and model fitness, these included: item from MU (e1-e3), KPP (e15-e16), MDC (e9-e10), EC (e7-e5) and COVID-19 RM (e5-e18) as well as (e17-e18). Based on Awang (2015) and Hair et al. (2017), alterations deleted items must not exceed 20% of the observed or unobserved variables to improve the fitness and impactful model fitness.
Table 3.
Constructs correlation & validated goodness-fit.
| Constructs | Values | |||||
|---|---|---|---|---|---|---|
| Chi-square/df | 3.946 < 3.0 | |||||
| RMSEA | .080 < 0.08 | |||||
| CFI | .921 > 0.95 | |||||
| IFI | .921 > 0.90 | |||||
| .892 > 0.90 | ||||||
| TLI | .872 > 0.95 | |||||
| AGFI | .918> > 0.95 | |||||
| GFI | ||||||
|
Correlations | ||||||
|
Correlation |
1 |
2 |
3 |
4 |
5 |
|
| MU | 0.815 | |||||
| MDC | .593a | 0.878 | ||||
| EC | .549a | .534a | 0.847 | |||
| C19RM | .517a | .641a | .643a | 0.807 | ||
| KPP | .514a | .562a | .567a | .644a | 0.853 | |
Note: MU = mobile usability, MDC = mobile-digital culture, EC = environmental condition, C19RM = Covid-19 risk mitigation, KPP = knowledge of app.
Correlation is significant at the 0.01 level (2-tailed).
3.2. Confirmatory factor analysis results
This research consisted of 5 observed latent variables, with COVID-19 mitigation being the outcome variable. About seven hypotheses were proposed in the study premised on mobile usability, knowledge of the app, and MDC measured as categorical variables. It is significant to note that mobile usability is a first-order construct that relies on mediation to determine be outcome of COVID-19 mitigation. Meanwhile, the dimension is considered a second-order and highest-order construct. Procedure considered in the study analysis.
Besides, Table 4 of the hypotheses results indicated and confirmed this study proposition of H1: Mobile Relative Usability has a positive relationship with an environmental condition in using the technology for Covid-19 mitigation indicated (β = 0.28, t = 3.705, p < .001***) is confirmed. H2: Environmental condition has a positive relationship with Covid-19 mitigation strategy among institutions/organizations also confirmed (β = 0.31, t = 4.62, p < .001***). Further, H3: Mobile usability has a positive effects on knowledge of the mobile app for the surveillance of Covid-19 mitigation showed significant at (β = 0.72, t = 7.55, p < .001***). Likewise, H4: Knowledge of app has positive effects on the mobile digital culture as surveillance technology of Covid-19 mitigation is confirmed (β = 0.31, t = 6.29, p < .001***). Again, H5: Mobile digital culture has positive effects on social Covid-19 mitigation strategies statistically significant at (β = 0.25, t = 3.377, p < .001) all the hypothesized is statistically significant to the study except the mediation.
Table 4.
Unstandardized Regression Weight of the Hypotheses of the study.
| Hypotheses | Estimate | S.E. | t-value | p-value | Inferences | ||
|---|---|---|---|---|---|---|---|
| H1 EC | <--- | MU | 0.281 | 0.076 | 3.705 | *** | Supported |
| H2 CRM | <--- | EC | 0.313 | 0.068 | 4.621 | *** | Supported |
| H3 KPP | <--- | MU | 0.721 | 0.095 | 7.558 | *** | Supported |
| H4 MDC | <--- | KPP | 0.306 | 0.048 | 6.392 | *** | Supported |
| H5 CRM | <--- | MDC | 0.246 | 0.073 | 3.377 | *** | Supported |
| H6 EC | <--- | KPP | 0.238 | 0.065 | 3.655 | *** | Supported |
| H7 EC | <--- | MDC | 0.254 | 0.078 | 3.268 | 0.001 | Supported |
Note: MU = mobile usability, MDC = mobile-digital culture, EC = environmental condition, C19RM = Covid-19 risk mitigation, KPP = knowledge of app.
3.3. Hypotheses tested results
.
3.4. Structural model
Fig. 3 showed all the estimates represented effect on COVID-19 risk mitigation at R2 = 0.40; thus, variable in the model explained about 40%, which is the overall statistical predictability of the outcome variables. Overall model fit measure is the coefficient of the determinant of the path weight average in Fig. 3. Cohen (1992) and Leguina (2015) indicated that any variance above 0.20 is statistically accepted to explain the power of the background variables. For which MDC is R2 = 22%, while environmental condition is R2 = 30%, and knowledge of app is R2 = 55% in Fig. 3. Therefore, the performance of the standardized path outcome of COVID-19 risk mitigation is of the highest average score over MDC surveillance in mobile apps to determine the pandemic's low and high population areas.
Fig. 3.
Standardized results of path coefficient analysis.
However, the mediation by Sobel test shows that EC presences do not shrink nor cause effects of COVID-19 mitigation (Baron, R. M., & Kenny, 1986). Ideally, the mediation effect could have occurred if MU on EC to COVID-19 risk mitigation shrinks the indirect effect while the latter made no difference significantly. Conversely, mobile usability on knowledge of app showed a direct effect of (β = 0.72). The findings reveal that mobile usability is highly impactful on health applications within the category of MDC for acceptable use of the COVID-19 communication mitigation strategy. The probability of getting an application for remote surveillance COVID-19 mitigation is an absolute value of 0.001***. Predictively, the COVID-19 risk mitigation adaption of apps surveillance and tracking virus on geographical population is statistically significantly different from zero at 0.001***. Fig. 3 path coefficient showed that effects of MU (β = 0.26***, t = 3.705) and Knowledge of App (β = 0.30***, t = 3.655), on MDC (β = 0.49***, t = 6.392) and MDC on EC (β = −0.20***, t = 3.265) are significant to COVID-19 risk mitigation.
3.5. Moderation interaction
Fig. 4 plot shows the two-way interaction effect of COVID-19 risk mitigation and knowledge of apps, showed MDC dampens the negative relationship between COVID-19 mitigation and knowledge of apps as proposed. H7: Mobile digital culture moderates on knowledge of App to enable the COVID-19 risk mitigation strategy is confirmed. The constructs' performance by a score of regression weight already indicated a vital path index of mobile usability on knowledge of app categorized as mobile digital culture technology. Using Andrews Haye's condition process from SPSS to calculate the covariance matrix of regression estimates plotted on an excel spreadsheet for the outcome in Fig. 3 above (A. F. Hayes, 2017). Significantly and graphically emphasis is placed on MDC mathematical statistical value as impactful construct of the study novelty of COVID-19 risk mitigation.
Fig. 4.
Interaction effects of MDC on COVID-19 risk mitigation and K-App.
4. Discussions
The present study investigated how mobile digital culture (MDC) directly and indirectly affected environmental conditions (EC) associated with mobile usability (MU) and knowledge of App on COVID-19 risk mitigation. Previously, literature on the subject dwelled on blood pulse, heartbeat, muscle fatigue, and image-based information access (Chen et al., 2010; Güemes et al., 2021; Sakoi et al., 2007; Song et al., 2021). Minimal attention is placed on the innovative integration of human attitudes, behaviors, emotions attached to smartphones into self-care and reducing the risk of the COVID-19 virus. The current study extrapolated mobile usability, knowledge of Apps, and MDC to understand their influence on COVID-19 risk mitigation. Culture is a way of life; digital culture, suggested by Deuze (2006), is an emerging trend, situation, and change regulated by the technologies associated with habits and attitudes. The phenomenon of mobile technology have been a flexible tool of information tracking human health. Its application to the COVID-19 situation, long overdue, will help people-to-people access self-care health routine checks via mobile technologies. Congruence to the present study is the syndromic surveillance initiative by the Jonh Hopkins University COVID-cloud control mechanism of smartphone application for collection of body temperature with spatio-temporal clustering techniques (Güemes et al., 2021). Also, the smartphone driven thermometer application for real-time groups population (Aryal & Becerik-Gerber, 2019a, 2019b).
The direct relationship between MU and EC conceptualized in this study is valid and resonates with other studies (Besenyi et al., 2018; Hermes et al., 2019; Morita et al., 2019). Similarly, knowledge of APP and EC is also significant by data response and consistent to literature (Morita et al., 2019). Again, the EC relationship with COVID-19 risk mitigation is statistically significant. However, EC mediation did not show a statistical difference. Nonetheless, moderation of MDC found dampened negative interaction of knowledge of App and COVID-19 mitigation. Therefore, elaborating on the potential of mobile technology emerging universal culture is an alternative to support COVID-19 surveillance in low and high geographical areas. Health Apps and software abilities to capture health information in text and sound; blood pressure, weight, blood sugar, energy level, are MDC (Bauer et al., 2018; Hilty et al., 2021; Jaana & Paré, 2020; Li et al., 2020). This technology posed a useful potential to ensure the operational productivity of all institutions and organizations.
The 21st Century MDC has open avenues on mobile usability for developers and technology-infused Apps that can remotely conduct surveillance in low and high COVID-19 infection areas. The COVID-19 signs and symptoms are nonspecific, but the CDC identified mobility of the virus and recommended daily data collection through a national network system with an MDC factor. A recent syndromic study emerged in the United Kingdom and the USA on COVID-19 signs and symptoms mobile systemic tracker (Spector, 2021). The mobile digital culture is evidenced during COVID-19 monitoring as an alternative justification of mobile surveillance for smart-thermometer met MDC and technology changing culture. The concepts of state systemic developed mHealth App, can automatically collect human body temperature timely and on daily basis.
The COVID-19 mitigation requires scientific knowledge of smartphones, because, the virus is movable. Currently, spatial science, AI, and machine learning algorithsm efficacy to locate cluster of the viruses, is rudiment of MDC algorithsm. Towards this initiative, the study objectives challenges mHealth application to track and monitor the pandemic in high-low geographical areas. The MDC's ability to control geographical maps with GPS, further track COVID-19 without completing a survey, information synced with App to self-test, sensor human body temperature linked with signs and symptoms of the COVID-19 risk mitigation. Secondly, the ability of technology developers to infuse sensors to self-check human body temperature with smart-thermometer. The latter is a vital phenomenon for a real-time enclosed area continuous monitoring and tracking of the COVID-19 pandemic countryside and further validating the algorithm.
4.1. Limitation of the study
The research explored the acceptance of MDC as a phenomenon that regulates human behavior, attitude, and ubiquitous smart health. Mobile usability, knowledge of App were found to have a positive relationship with environmental condition that predicts MDC. Likewise, knowledge of App positive effects on MDC. As a key determiner of people's usability of mHealth App, MDC moderation on Knowledge of App dampens a negative relationship with COVID-19 risk mitigation. The indirect effects of MU, Knowledge of App, MDC, EC showed much difference except the mediating variable. Due to the research focus, we could not account for MU on MDC, and moderation on EC. Moreover, the sample focused on diverse culture, and further research can dichotomize study areas in terms of MDC differences concerning mHealth usability. A larger population could also make a difference in future research. Presented is the observation and evaluation from social sciences, philosophical and psychological perspective.
5. Conclusion
This study is significant in monitoring and tracking people in enclosed settings, where mHealth Apps of MDC attitudes and behaviors serve COVID-19 risk mitigation. The development of mobile usability is commensurate with mobile technology to remote surveillance monitoring of the COVID-19 pandemic. MDC presents an opportunity to circumvent the current promulgated social distance, physical distance, and lockdown of institutions. High in-come group economies have magnified mobile technology in the health sector represented 64% and low-middle income economies 53%. The Americans (75%), Europe (64%), South East Asia (62%), this empirical evidence indicated the adoption rates of telemedicine among countries a breakthrough MDC (Chen et al., 2010). Mobile digital culture is redefining human behavior, attitude and an Android app provides smart-thermometer for the periodic checks. Government policy is intended to meet the MDC trend of mobile communication, intervention software that can track and check human body temperature to control COVID-19 risk mitigation strategy. While policy considerations must not exclude the development of infringement data collection among mHealth end users, certain risks and benefits must be considered. This evidence will lead to a high level acceptance of the usability of mHealth apps for COVID-19 control and prevention.
Ethical consideration this
This research has adhered strictly to the Helsinki Declaration on Human research and participants information was treated based on global standards on ethics. The participants of this survey consented to participate in this study.
Funding
This is academic research, therefore, received no specific funding support.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Afthanorhan A., Awang Z., Rashid N., Foziah H., Ghazali P.L. Assessing the effects of service quality on customer satisfaction. Management Science Letters. 2019;9(1):13–24. doi: 10.5267/j.msl.2018.11.004. [DOI] [Google Scholar]
- Agbota H., Mitchell J.E., Odlyha M., Strlič M. Remote assessment of cultural heritage environments with wireless sensor array networks. Sensors. 2014;14(5):8779–8793. doi: 10.3390/s140508779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad M.I. Unified theory of acceptance and use of technology. Fourth International Conference on ICT in Our Lives. 2014;17(5):1–4. doi: 10.1080/1097198X.2010.10856507. 2014. [DOI] [Google Scholar]
- Akintunde T.Y., Akintunde O.D., Musa T.H., Sayibu M., Tassang A.E., Reed L., Chen S. Expanding telemedicine to reduce the burden on the healthcare systems and poverty in Africa for a post-coronavirus disease 2019 (COVID-19) pandemic reformation. Global Health Journal. 2021 doi: 10.1016/J.GLOHJ.2021.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AppBrains . 2020. Top categories on Google Play | AppBrai. AppBrains android.https://www.appbrain.com/stats/android-market-app-categories [Google Scholar]
- Aryal A., Becerik-Gerber B. A comparative study of predicting individual thermal sensation and satisfaction using wrist-worn temperature sensor, thermal camera and ambient temperature sensor. Building and Environment. 2019;160(May):106223. doi: 10.1016/j.buildenv.2019.106223. [DOI] [Google Scholar]
- Aryal A., Becerik-Gerber B. BuildSys 2019 - Proceedings of the 6th ACM International Conference on Systems for Energy-Efficient Buildings, Cities, and Transportation. 2019. Skin temperature extraction using facial landmark detection and thermal imaging for comfort assessment; pp. 71–80. [DOI] [Google Scholar]
- Awang Z. Structural Equation Modelling using amos grafic (2nd Editio) Kuala Lumpur: Universiti Sultan Zainal Abidin; 2015. Validating the measurement model: CFA. [Google Scholar]
- Awang Z., Afthanorhan A., Mamat M. The Likert scale analysis using parametric based Structural Equation Modeling (SEM) Computational Methods in Social Sciences. 2016;4(1):13–21. doi: 10.5539/mas.v9n9p58. [DOI] [Google Scholar]
- Awang Z., Afthanorhan A., Mamat M., Aimran N. Modeling structural model for higher order constructs (HOC) using marketing model. World Applied Sciences Journal. 2017;35(8):1434–1444. doi: 10.5829/idosi.wasj.2017.1434.1444. [DOI] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator vari- able distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrio P., Ortega L., López H., Gual A. Self-management and shared decision-making in alcohol dependence via a mobile app: A pilot study. International Journal of Behavioral Medicine. 2017;24(5):722–727. doi: 10.1007/s12529-017-9643-6. [DOI] [PubMed] [Google Scholar]
- Bauer A.M., Hodsdon S., Bechtel J.M., Fortney J.C. Applying the principles for digital development: Case study of a smartphone app to support collaborative care for rural patients with posttraumatic stress disorder or bipolar disorder. Journal of Medical Internet Research. 2018;20(6) doi: 10.2196/10048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besenyi G.M., Schooley B., Turner-McGrievy G.M., Wilcox S., Wilhelm Stanis S.A., Kaczynski A.T. The electronic community park audit tool (eCPAT): Exploring the use of mobile technology for youth empowerment and advocacy for healthy community policy, systems, and environmental Change. Frontiers in Public Health. 2018;6(NOV):1–15. doi: 10.3389/fpubh.2018.00332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan N., Curson I. Methods for measuring usability. Human-Computer Interaction INTERACT. 1997;’97:672–673. doi: 10.1007/978-0-387-35175-9_126. [DOI] [Google Scholar]
- Bol N., Helberger N., Weert J.C.M. Differences in mobile health app use: A source of new digital inequalities? The Information Society. 2018;34(3):183–193. doi: 10.1080/01972243.2018.1438550. [DOI] [Google Scholar]
- Buckee C.O., Balsari S., Chan J., Crosas M., Dominici F., Gasser U., Grad Y.H., Grenfell B., Halloran M.E., Kraemer M.U.G., Lipsitch M., Metcalf C.J.E., Meyers L.A., Perkins T.A., Santillana M., Scarpino S.V., Viboud C., Wesolowski A., Schroeder A. Aggregated mobility data could help fight COVID-19. Science. 2020;368(6487):145–146. doi: 10.1126/science.abb8021. [DOI] [PubMed] [Google Scholar]
- Carey T.A., Haviland J., Tai S.J., Vanags T., Mansell W. MindSurf: A pilot study to assess the usability and acceptability of a smartphone app designed to promote contentment, wellbeing, and goal achievement. BMC Psychiatry. 2016;16(1):1–9. doi: 10.1186/s12888-016-1168-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Koskela M., Hyväkkä J. Vol. 3. 2010. Image based information access for mobile phones. (Proceedings - international Workshop on Content-Based Multimedia Indexing). [DOI] [Google Scholar]
- C. Lee Ventola M. Mobile devices and apps for health care professionals: Uses and benefits. PMC. 2014;39(5):356–364. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029126/ [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- De Korte E.M., Wiezer N., Janssen J.H., Vink P., Kraaij W. Evaluating an mHealth app for health and well-being at work: Mixed-method qualitative study. JMIR MHealth and UHealth. 2018;6(3):1–17. doi: 10.2196/mhealth.6335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deady M., Johnston D., Milne D., Glozier N., Peters D., Calvo R., Harvey S. Preliminary effectiveness of a smartphone app to reduce depressive symptoms in the workplace: Feasibility and acceptability study. JMIR MHealth and UHealth. 2018;6(12) doi: 10.2196/11661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department S.R. Apple app store: Number of available medical apps as of Q3 2020. Statista - das statistik-portal. 2021. https://www.statista.com/statistics/779910/health-apps-available-ios-worldwide/
- Deuze M. Participation, remediation, bricolage: Considering principal components of a digital culture. The Information Society. 2006;22(2):63–75. doi: 10.1080/01972240600567170. [DOI] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome: Clinical Research Reviews. 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwivedi Y.K., Rana N.P., Jeyaraj A., Clement M., Williams M.D. Re-examining the unified theory of acceptance and use of technology (UTAUT): Towards a revised theoretical model. Information Systems Frontiers. 2019;21:719–734. doi: 10.1007/s10796-017-9774-y. [DOI] [Google Scholar]
- Furlong L., Serry T., Erickson S., Morris M.E. Tablet-based apps for phonics and phonological awareness: Protocol for evidence-based appraisal of content, quality, and usability. JMIR Research Protocols. 2021;10(2):1–10. doi: 10.2196/23921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goggin G. Mobile paradoxes: European emergence of mobile internet, users, and markets. Internet Histories. 2020;4(2):161–177. doi: 10.1080/24701475.2020.1741968. [DOI] [Google Scholar]
- Güemes A., Ray S., Aboumerhi K., Desjardins M.R., Kvit A., Corrigan A.E., Fries B., Shields T., Stevens R.D., Curriero F.C., Etienne-Cummings R. medRxiv. 2020. A syndromic surveillance tool to detect anomalous clusters of COVID-19 symptoms in the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Güemes A., Ray S., Aboumerhi K., Desjardins M.R., Kvit A., Corrigan A.E., Fries B., Shields T., Stevens R.D., Curriero F.C., Etienne-Cummings R. A syndromic surveillance tool to detect anomalous clusters of COVID-19 symptoms in the United States. Scientific Reports. 2021;11(1):1–11. doi: 10.1038/s41598-021-84145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair J., Hollingsworth C.L., Randolph A.B., Chong A.Y.L. 2017. An updated and expanded assessment of PLS-SEM in information systems research. Industrial Management and Data Systems. [DOI] [Google Scholar]
- Hayes A. Guilford; New York, NY: 2013. Introduction to mediation, moderation, and conditional process analysis. https://doi.org/978-1-60918-230-4. [Google Scholar]
- Hayes A.F. Vols. 1–72. 2017. www.afhayes.com (Using SPSS: A Little Syntax Guide). Www.Afhayes.Com, December. [Google Scholar]
- Hermes S., Lurz M., Böhm M., Krcmar H. Evaluating the usability and usefulness of a mobile application for training visual mnemonic techniques in participants with subjective cognitive decline: An exploratory pilot study. Procedia Computer Science. 2019;160:439–444. doi: 10.1016/j.procs.2019.11.067. [DOI] [Google Scholar]
- Hilty D.M., Crawford A., Teshima J., Nasatir-Hilty S.E., Luo J., Chisler L.S.M., Gutierrez Hilty Y.S.M., Servis M.E., Godbout R., Lim R.F., Lu F.G. Mobile health and cultural competencies as a foundation for Telehealth care: Scoping review. Journal of Technology in Behavioral Science. 2021;6(2):197–230. doi: 10.1007/s41347-020-00180-5. [DOI] [Google Scholar]
- Inal Y., Wake J.D., Guribye F., Nordgreen T. Usability evaluations of mobile mental health technologies: Systematic review. Journal of Medical Internet Research. 2020;22(1):1–19. doi: 10.2196/15337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaana M., Paré G. Comparison of mobile health technology use for self-tracking between older adults and the general adult population in Canada: Cross-sectional survey. JMIR MHealth and UHealth. 2020;8(11):1–14. doi: 10.2196/24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamison D.T., Gelband H., Horton S., Jha P., Laxminarayan R., Mock C.N., R.N. In: D. T. J. H. G. S. H. P. Jha, R. L. C. N. M. R. Nugent, editors. Vol. 9. Third Edit; 2018. Disease control priorities, 3rd edition: Improving health and reducing poverty. (The Lancet). Issue 10125). . License: Creative Commons Attribution CC BY 3.0 IGO Translations—If. [DOI] [Google Scholar]
- Johnson S.G., Potrebny T., Larun L., Ciliska D., Olsen N.R. Usability methods and attributes reported in usability studies of mobile apps for health care education: Protocol for a scoping review. JMIR Research Protocols. 2020;9(8):1–6. doi: 10.2196/19072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas B., Tensil M.D., Leuschner F., Strüber E., Tossmann P. Predictors of treatment response in a web-based intervention for cannabis users. Internet Interventions. 2019;18(February):100261. doi: 10.1016/j.invent.2019.100261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jou M., Tennyson R.D., Wang J., Huang S.Y. A study on the usability of E-books and app in engineering courses: A case study on mechanical drawing. Computers and Education. 2016;92(93):181–193. doi: 10.1016/j.compedu.2015.10.004. [DOI] [Google Scholar]
- Lane D.A., McMahon N., Gibson J., Weldon J.C., Farkowski M.M., Lenarczyk R., Watkins C.L., Dilaveris P., Caiani E.G., Potpara T.S. Mobile health applications for managing atrial fibrillation for healthcare professionals and patients: A systematic review. Europace. 2020;22(10):1567–1578. doi: 10.1093/europace/euaa269. [DOI] [PubMed] [Google Scholar]
- Leander K.M., Vasudevan L. The Routledge Handbook of Multimodal Analysis; 2009. Multimodality and mobile culture; pp. 127–139. April 2015. [Google Scholar]
- Leguina A. A primer on partial least squares structural equation modeling (PLS-SEM) International Journal of Research and Method in Education. 2015;38(2):220–221. doi: 10.1080/1743727X.2015.1005806. [DOI] [Google Scholar]
- Li H., Lewis C., Chi H., Singleton G., Williams N. Mobile health applications for mental illnesses: An Asian context. Asian Journal of Psychiatry. 2020;54(January):102209. doi: 10.1016/j.ajp.2020.102209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lulin Z., Owusu-Marfo J., Asante Antwi H., Antwi M.O., Xu X. SAGE Open; 2020. Nurses' readiness in the adoption of Hospital electronic information management systems in Ghana: The application of the structural equation modeling and the UTAUT model. [DOI] [Google Scholar]
- Mackinnon D.P., Dwyer J.H. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17(2):144–158. doi: 10.1177/0193841X9301700202. [DOI] [Google Scholar]
- Martynova E., West S.G., Liu Y. Review of principles and practice of structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal. 2018 doi: 10.1080/10705511.2017.1401932. [DOI] [Google Scholar]
- Mcneish D. Psychological methods thanks coefficient alpha, we’ll take it from here thanks coefficient alpha, we’ll take it from here. 2017. Psychological Methods. Advance Online Publication. [DOI] [PubMed]
- Miller A.C., Singh I., Koehler E., Polgreen P.M. A smartphone-driven thermometer application for real-time population- and individual-level influenza surveillance. Clinical Infectious Diseases. 2018;67(3):388–397. doi: 10.1093/cid/ciy073. [DOI] [PubMed] [Google Scholar]
- Mohammad-Alizadeh-Charandabi S., Mirghafourvand M., Asghari Jafarabadi M., Mohammadi A., Soltanpour S. Psychometric properties of the Iranian version of the inventory of functional status after childbirth (IFSAC) Iranian Red Crescent Medical Journal. 2016;19(5) doi: 10.5812/ircmj.30210. [DOI] [Google Scholar]
- Morita P.P., Yeung M.S., Ferrone M., Taite A.K., Madeley C., Lavigne A.S., To T., Diane Lougheed M., Gupta S., Day A.G., Cafazzo J.A., Licskai C. A patient-centered mobile health system that supports asthma self-management (breathe): Design, development, and utilization. JMIR MHealth and UHealth. 2019;7(1):1–17. doi: 10.2196/10956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Immunization and Respiratory Diseases (NCIRD), D. of V. D . 2021. How to mitigate COVID-19 transmission in densely populated areas globally.https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/global-urban-areas.html [Google Scholar]
- Nicolini E.S.M. Bevila) Sptinger; cham: 2021. Smart technologies for the environmental design of Smaller Urban Centres. [DOI] [Google Scholar]
- Noguchi M., Ma N., Woo C.M.M., Chau H.W., Zhou J. The usability study of a proposed environmental experience design framework for active ageing. Buildings. 2018;8(12) doi: 10.3390/buildings8120167. [DOI] [Google Scholar]
- O'Dea S. 2021. Smartphone users worldwide 2016-2023.https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/ [Google Scholar]
- Pinchot J.L., Paullet K.L., Rota D.R. How mobile technology is changing our culture. Conference on Information Systems Applied Research. 2010;1–10 [Google Scholar]
- Przysucha M., Flemming D., Hübner U. The benefits of a formative evaluation for developing a highly innovative software: The case of the HandoverEHR. Studies in Health Technology and Informatics. 2017 doi: 10.3233/978-1-61499-678-1-619. [DOI] [PubMed] [Google Scholar]
- Richardson D.B., Kwan M.P., Alter G., McKendry J.E. Replication of scientific research: Addressing geoprivacy, confidentiality, and data sharing challenges in geospatial research. Annals of GIS. 2015;21(2):101–110. doi: 10.1080/19475683.2015.1027792. [DOI] [Google Scholar]
- Ruggiero K.J., Bunnell B.E., Andrews A.R., III, Davidson T.M., Hanson R.F., Danielson C.K., Saunders B.E., Soltis K., Yarian C., Chu B., Adams Z.W. Development and pilot evaluation of a tablet-based application to improve quality of care in child mental health treatment. JMIR Research Protocols. 2015;4(4):e143. doi: 10.2196/resprot.4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco G., Lléonart S., Simon R., Noublanche F., Annweiler C. Communication technology preferences of hospitalized and institutionalized frail older adults during COVID-19 confinement: Cross-sectional survey study. JMIR MHealth and UHealth. 2020;8(9):1–7. doi: 10.2196/21845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakoi T., Tsuzuki K., Kato S., Ooka R., Song D., Zhu S. Thermal comfort, skin temperature distribution, and sensible heat loss distribution in the sitting posture in various asymmetric radiant fields. Building and Environment. 2007;42(12):3984–3999. doi: 10.1016/j.buildenv.2006.10.050. [DOI] [Google Scholar]
- Saleh A., Bintiisamil R., Fabil N.B. Extension of pacmad model for usability evaluation metrics using goal question metrics (Gqm) approach. Journal of Theoretical and Applied Information Technology. 2015;79(1):90–100. [Google Scholar]
- Schmidt M., Kafka J.X., Kothgassner O.D., Hlavacs H., Beutl L., Felnhofer A. Vol. 8253. LNCS; 2013. Why does it always rain on me? Influence of gender and environmental factors on usability, technology related anxiety and immersion in virtual environments. (Lecture Notes in Computer Science (Including Subseries Lecture Notes in Artificial intelligence and Lecture Notes in Bioinformatics)). 392–402. [DOI] [Google Scholar]
- Shao W., Hao F. Confidence in political leaders can slant risk perceptions of COVID–19 in a highly polarized environment. Social Science & Medicine. 2020;261(June):113235. doi: 10.1016/j.socscimed.2020.113235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shek D.T.L., Yu L. Confirmatory factor analysis using AMOS: A demonstration. International Journal on Disability and Human Development. 2014;13(2):191–204. doi: 10.1515/ijdhd-2014-0305. [DOI] [Google Scholar]
- International Pharmaceutical Federation . In: International Pharmaceutical federation. Copyright 2019 International Pharmaceutical Federation (FIP) International Pharmaceutical Federation (FIP) Andries Bickerweg 5 2517 JP The Hague The Netherlands. S. M., Z. K., Sertić M., editors. 2019. Use of mobile health tools in pharmacy practice 2019. (www.fip.org All. www.fip.org) [Google Scholar]
- Song X., Li H., Gao W. MyoMonitor: Evaluating muscle fatigue with commodity smartphones. Smart Health. 2021;19(December 2020):100175. doi: 10.1016/j.smhl.2020.100175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spector T. ZOE COVID-19 sciences and your body. ZOE COVID-19. 2021. https://covid.joinzoe.com/home3
- I., S., H.O., A., T., S., J., V., A., L., B.M., M., B., K., O.C., B., P., O. Svagard I., Austad H.O., Seeberg T., Vedum J., Liverud A., Mathiesen B.M., Keller B., Bendixen O.C., Osborne P., Strisland F. A usability study of a mobile monitoring system for congestive heart failure patients. Studies in Health Technology and Informatics. 2014 [PubMed] [Google Scholar]
- Tao D., Shao F., Wang H., Yan M., Qu X. Integrating usability and social cognitive theories with the technology acceptance model to understand young users' acceptance of a health information portal. Health Informatics Journal. 2020;26(2):1347–1362. doi: 10.1177/1460458219879337. [DOI] [PubMed] [Google Scholar]
- Velavan T.P., Meyer C.G. The COVID-19 epidemic. Tropical Medicine and International Health. 2020;25(3):278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesh V., Morris M., Davis G., Davis F. Technology acceptance model - research. MIS Quarterly. 2003;27:425–478. [Google Scholar]
- Vokinger K.N., Nittas V., Witt C.M., Fabrikant S.I., Von Wyl V. Digital health and the COVID-19 epidemic: An assessment framework for apps from an epidemiological and legal perspective. Swiss Medical Weekly. 2020;150(19–20):1–9. doi: 10.4414/smw.2020.20282. [DOI] [PubMed] [Google Scholar]
- Walkthrough M. 2020. How to plan and Execute a COVID-19 mitigation Walkthrough getting schools ready for IN-person learning. [Google Scholar]
- Webpage C. Implementation of mitigation strategies for communities with local COVID-19 transmission. 2021. https://www.cdc.gov/coronavirus/2019-ncov/community/community-mitigation.html CDC COVID-19.
- Wilson, LA (Wilson, Leigh Ann)[1] ; O'Loughlin, K (O'Loughlin, Kate)[1] ; Hector, R (Hector, Robyn)[1] ; Black, DA (Ann Black, D. 1. Using a smartphone application (app) to assist older adults to navigate their local area during extreme weather events and changing environmental conditions: A qualitative study. Australasian Journal on Ageing. 2021;40(1):E95–E99. doi: 10.1111/ajag.12858. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) Vol. 2. World Health Organization; 2021. Critical Preparedness, readiness and response actions for COVID-19: Interim guidance. (WHO Global site). Issue 27 May 2021). https://doi.org/Retrieved from https://www.who.int/publications-detail/critical-preparedness-readiness-and-response-actions-for-covid-19%0Ahttps://www.who.int/publications/i/item/critical-preparedness-readiness-and-response-actions-for-covid-19%0Ahttps://www.who.int/en/ [Google Scholar]
- Ye B., How T.V., Chu C.H., Mihailidis A. Dementia care apps for people with dementia and informal caregivers: A systematic review protocol. Gerontology. 2021;7:1–6. doi: 10.1159/000514838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao N., Seitinger S., Richer R., Paradiso J.A. Smart Health Real-time work environment optimization using multimodal media and body sensor network. Smart Health. 2021;19(December 2020):100164. doi: 10.1016/j.smhl.2020.100164. [DOI] [Google Scholar]
Further reading
- Jemal H., Kechaou Z., Ben Ayed M., Alimi A.M. International Symposium on Technology and Society; 2016. Cloud computing and mobile devices based system for healthcare application. Proceedings, 2016-March, 1–5. [DOI] [Google Scholar]
- Kounadi O., Leitner M. Why does geoprivacy matter? The scientific publication of confidential data presented on maps. Journal of Empirical Research on Human Research Ethics. 2014;9(4):34–45. doi: 10.1177/1556264614544103. [DOI] [PubMed] [Google Scholar]
- Naslund J.A., Aschbrenner K.A., Bartels S.J. How people with serious mental illness use smartphones, mobile apps, and social media. Psychiatric Rehabilitation Journal. 2016;39(4):364–367. doi: 10.1037/prj0000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson J., Wright S.M., Carlisle A.M., Sweeney M.A., McHugo G.J. The working well mobile phone app for individuals with serious mental illnesses: Proof-of-Concept, mixed-methods feasibility study. JMIR Mental Health. 2018;5(4):e11383. doi: 10.2196/11383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordgreen T., Blom K., Andersson G., Carlbring P., Havik O.E. Effectiveness of guided Internet-delivered treatment for major depression in routine mental healthcare - an open study. Internet Interventions. 2019;18(June):100274. doi: 10.1016/j.invent.2019.100274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr M., Isaacs J., Godbout R., Witmans M., Corkum P. A usability study of an internet-delivered behavioural intervention tailored for children with residual insomnia symptoms after obstructive sleep apnea treatment. Internet Interventions. 2019;18(April):100265. doi: 10.1016/j.invent.2019.100265. [DOI] [PMC free article] [PubMed] [Google Scholar]