Abstract
Background
Interventional radiographers have substantially contributed to patient care during the pandemic by providing imaging guidance during minimally invasive procedures. The aim of this research is to quantify the impact of the pandemic on an interventional radiographers’ wellbeing during the COVID-19 pandemic.
Methods
Ethical approval was obtained at the outset of this study. An explanatory sequential mixed methods approach, using questionnaires and interviews, was used to explore and evaluate interventional radiographers' wellbeing; physical, mental and social. An electronic self-administered questionnaire was administered to interventional radiographers and a semi-structured interview was conducted on two respondents.
Results
Responses were received from 40 interventional radiographers. Physical, mental and social wellbeing of interventional radiographers deteriorated since the onset of COVID-19. All forms of wellbeing were negatively impacted during the pandemic with mental wellbeing (82.5%) the most impacted, closely followed by physical (75%) and social wellbeing (50%). Half of responding interventional radiographers reported being “highly stressed” while working during COVID-19. Physical activity levels decreased, caffeine consumption increased and consumption of a healthy diet decreased. Almost all interventional radiographers (95%) had anxiety about passing the virus onto family or friends and 60% of noted a deterioration in relationship with friends. Three key themes identified included the importance of teamwork, the physical demand and mental impacts of working in interventional radiology during the pandemic.
Conclusions
The COVID-19 pandemic has had a negative effect on interventional radiographers' wellbeing. The implications of staff having a diminished sense of wellbeing is that productivity is likely to have been reduced and potentially related burnout can lead to illness. This research highlights the need to focus on identifying methods of addressing the shortcomings in support services and identifying the specific needs of interventional radiographers to improve their wellbeing.
Keywords: Interventional radiographer, COVID-19, Wellbeing, Radiology services, COVID-19 impact
Résumé
Contexte
Les radiographes d'intervention ont largement contribué aux soins des patients pendant la pandémie en fournissant des conseils d'imagerie pendant les procédures peu invasives. L'objectif de cette recherche est de quantifier l'impact de la pandémie sur le bien-être des radiographes d'intervention pendant la pandémie de COVID-19.
Méthodologie
L'approbation éthique a été obtenue dès le début de cette étude. Une approche séquentielle explicative de méthodes mixtes, utilisant des questionnaires et des entretiens, a été utilisée pour explorer et évaluer le bien-être physique, mental et social des radiographes interventionnels. Un questionnaire électronique auto-administré a été administré aux radiographes d'intervention et un entretien semi-structuré a été mené auprès de deux répondants.
Résultats
Des réponses ont été reçues de 40 radiographes d'intervention. Le bien-être physique, mental et social des radiographes d'intervention s'est détérioré depuis le début de la pandémie de COVID-19. Toutes les formes de bien-être ont été affectées négativement pendant la pandémie, le bien-être mental (82,5 %) étant le plus touché, suivi de près par le bien-être physique (75 %) et social (50 %). La moitié des radiographes d'intervention ayant répondu à l'enquête ont déclaré avoir été « très stressés » en travaillant pendant la pandémie. Le niveau d'activité physique a diminué, la consommation de caféine a augmenté et la consommation d'une alimentation saine a diminué. Presque tous les radiographes d'intervention (95 %) étaient anxieux à l'idée de transmettre le virus à leur famille ou à leurs amis et 60 % d'entre eux ont noté une détérioration de leurs relations avec leurs amis. Trois thèmes clés ont été identifiés : l'importance du travail en équipe, la demande physique et les impacts mentaux du travail en radiologie interventionnelle pendant la pandémie.
Conclusion
La pandémie de COVID-19 a eu un effet négatif sur le bien-être des radiologues interventionnels. Les implications d'un personnel ayant un sentiment de bien-être diminué sont que la productivité est susceptible d'avoir été réduite et que l'épuisement professionnel potentiellement lié peut conduire à la maladie. Cette recherche met en évidence la nécessité de se concentrer sur l'identification des méthodes permettant de combler les lacunes des services de soutien et d'identifier les besoins spécifiques des radiographes d'intervention pour améliorer leur bien-être.
Introduction
The first confirmed case of COVID-19 in Ireland was identified on February 29th, 2020, with the first death being reported on March 11th, 2020 [1]. Emerging studies have identified the psychological and physical impact of the COVID19 pandemic on frontline hospital staff in general [2], [3], [4]. Radiographers are frontline healthcare professionals and have helped support the optimal delivery of patient care during the COVID-19 pandemic [5]. Studies of radiographers have identified changes to clinical working patterns, service delivery, personal protective equipment (PPE) shortages and an increase in workplace-related stress amongst practising radiographers [5], [6], [7]. Interventional radiographers are a subgroup of frontline highly trained and skilled hospital staff who typically provide imaging to support minimally invasive procedures in highly pressured environments.
Interventional radiology (IR) plays an essential role in the management of acute sequelae of COVID-19. COVID-19 can result in an infection of the airway cells caused by the SARS-CoV-2 virus and this can lead severe systemic inflammation [8]. There is a recognised link between the SARS-CoV-2 infection and changes to the vasculature and cardiovascular system. Due to a combination of inflammation, platelet, and endothelial dysfunction there has been a noted increase in the incidence of cerebrovascular and general vascular events [8,9]. Such sequelae include strokes requiring thrombectomies and blood clots requiring catheter thrombolysis, both treatments offered within IR [10,11].
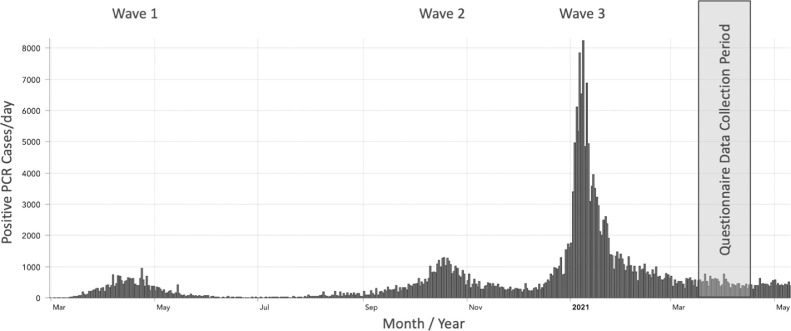
Following the onset of the COVID-19 pandemic, interventional radiographer working patterns changed significantly. Firstly, global IR workloads were subject to fluctuations as the number of COVID-19 cases increased. Many elective procedures were temporarily suspended to coincide with “waves” (Fig. 1 ) or increases in the hospitalisation of COVID-19 positive patients [12]. On the other hand interventional radiographers needed to perform many emergency procedures as part of the management of patients who had COVID-19 or suffered from the after effects of the virus. For example, there was an increase in the number of patients presenting with pulmonary embolus (PE) post-COVID recovery who needed additional treatment [13].
Fig. 1.
Graph illustrating the number of positive PCR cases (waves) in Ireland over time.
During the pandemic differences in the work practices of interventional and general radiographers became more evident than before [6,14]. Interventional radiographers were often involved in the emergency treatment of patients with COVID-19 who required intervention. This mandated the wearing of full radiation protection shielding as well as personal protective equipment (PPE) sometimes for substantial periods of time often with minimal comfort breaks. General radiographers were typically not subjected to wearing lead aprons for such long periods of time as the acquisition of imaging studies did not necessitate wearing lead protection and took less time to perform than IR procedures.
Evidence of the many ways in which the COVID-19 pandemic has affected all aspects of life is continuously being published. Research has identified that pre-pandemic, radiographers and other healthcare professionals were suffering the effects of occupational stress, fatigue and burnout [15], [16], [17]. To date the wellbeing amongst interventional radiographers during the pandemic has not been assessed. This study seeks to explore the effects of working during the COVID-19 pandemic by quantifying its impact on the wellbeing of interventional radiographers in Ireland.
Methods
This research employed a sequential explanatory mixed methods research design. A sequential explanatory approach involves collecting quantitative data first and using the results to help build a collection of qualitative data. Ethical approval was obtained from the Social Research Ethics Committee University College Cork (CT-SREC-2020-29) and all the respondents provided consent prior to participation in the questionnaire and interviews.
Eligible participants included all interventional radiographers who worked prior to and during the COVID-19 pandemic in any hospital in Ireland. Participants included those who work in public, private and voluntary hospitals which were the three hospital types providing IR services in Ireland. To facilitate participation a comprehensive list of hospitals with IR suites, including cardiac catheterisation labs were collated using an extensive web search and correspondence with local radiographers.
Questionnaire-based data collection
An electronic self-administered questionnaire (Google Forms, Google LLC, Mountain View, CA) was used in the first part of this study (See Supplementary Material). Recruitment for the questionnaire was voluntary and the questionnaire link was posted on social media (Facebook, Twitter and LinkedIn) to target only interventional radiographers. Radiology Service Managers were also emailed and asked to distribute the questionnaire among their interventional radiographers. A snowballing technique was also used as a method to recruit further participants.
The questionnaire was piloted among two academic supervisors, four radiographers and eight radiography students to test for reliability and validity [18]. The questionnaire included a total of forty-two questions, the majority being closed questions (n=36) with some open extended response items (n=6). The final element in the questionnaire allowed participants to volunteer to participate in an online interview. The response timeframe for the questionnaire was four weeks (18th March 2021 to15th April 2021; Fig. 1). A period of four weeks was chosen since evidence suggests that this facilitates the inclusion of >95% of participants who would be willing to respond [19].
Statistical analysis
Responses from the questionnaire were analysed using descriptive statistics and represented in tables and figures. SPSS Version 26 (IBM Inc, Armonk, NY) was used for statistical analysis.
Interview-based data collection
A semi-structured interview was conducted by study researchers which included two interventional radiographers. One was a Basic Grade radiographer working in a private hospital and the second was a Clinical Specialist Radiographer working in a public hospital. Participants volunteered following completion of the online questionnaire. Each participant was assigned a number and asked to attend an online interview. An interview guide was developed in accordance with the results of the quantitative research and was reviewed by academic supervisors. The interview guide began with some general questions and used three themes identified as relevant from the questionnaire.
Participants were asked to complete a consent form in advance of the interview. Detail was given on the nature of the study, the right to withdraw and the risk and benefits of taking part. Interviews took place on Microsoft Teams (Microsoft Corp, Redmond, WA) and were recorded with the full knowledge and consent of the participant. Once all the interviews were audio recorded a process of transcription and analysis commenced. In addressing validity, transcriptions and coding were reviewed by an independent assessor.
Qualitative analysis
A five phase thematic analysis approach was used in the qualitative interview analysis [20]. Step one involved numbering each line of the transcription and noting key ideas. The transcript was also anonymised at this point. The second step involved the generation of initial codes. Coding was conducted with the assistance of the software NVIVO 10 (QSR International, Doncaster, Australia). To establish the credibility of the coding, inter-rater reliability was used. An alternative researcher was asked to code the information and a discussion was had about any differences or similarities identified. The third step involved defining and naming of interpretative codes and dividing them into themes. The fourth step involved identifying patterns across the data set and cross checking with themes. A thematic map was then generated (Table 2 ; Fig. 6). The final step involved defining and naming themes. The themes were identified in the data set and grouped accordingly and quotes from participants will accompany each theme in the research paper. Data synthesis was the final step of this process and collated all the pieces together from both the quantitative questionnaires and qualitative interviews to provide key findings and conclusions.
Table. 2.
Summary of the key qualitative results
| Themes | Sub Themes | Quotations |
|---|---|---|
| Importance of Teamwork | Functionality of Interventional Radiology |
“Didn't necessarily get busier but more work involved in the patients that came down” “Some days are busier than others. Its busy with code strokes but not busy due to less patients presenting to hospital for treatment unless they have to” “More cleaning, more consideration of transporting patients from wards” |
| Staff shortages |
“Pressure from staffing levels has been extremely difficult.” “Fewer staff due to COVID-19 infections or self-isolation” |
|
| Shared experience |
“The core principle of Interventional Radiology is team.” “A sense of camaraderie, that everyone's going through the same thing at the moment.” “Everybody just worked together as much as they could to get as much done as we could” “I would say that the team and the camaraderie was important, like I felt that our radiology service manager was exceptional. So that said, there was faith. You know everybody had faith in that leadership” |
|
| Physical Demand | Increased workload |
“Namely stroke presentation and thrombectomies increased” “Despite reducing elective [cases] the amount of acute vascular work had skyrocketed” “More work involved in setting up the rooms and cleaning the rooms post procedure” “Extra cleaning to be done after every patient” |
| Lead aprons and PPE |
“There was many times where like we were fully in PPE for three hours including leads. I think that was an extra demand which I don't think that the other Radiographers would have experienced” “If it is a particularly long procedure, you know it can get very claustrophobic” |
|
| Physical aches, pains and falls |
“At the end of the day, you're just not even mentally drained but physically drained as well.” “We had two staff members fall during procedures due to fatigue and long periods of concentration” |
|
| Mental Impact | Work/Life balance |
“It's well and good trying to look for support, but like if you actually don't have time to get the support, you know that's very hard as well” “With gyms closed, exercise became more challenging you know, So that that was a result of work and fatigue and lockdown.” "It became important to set yourself in routine even like sleep wise just to make sure that you can function on a day to day basis” “Simply no time for friends outside of work” |
| Anxiety and Fear |
“With the amount of work, we do and the type of patients we see like it does [take] a mental toll on you, especially like when you see like patients coming back and they're just getting sicker and sicker.” “Much more mentally fatigued in the second wave” “Witnessing other staff members mental health suffer as a result of increase of workload, fear and tiredness has been difficult” “As a carer for an elderly parent I worry about passing it to her” |
|
| Social Isolation |
“You kind of almost become immune to the situation” “Extremely vulnerable partner, found it very stressful and essentially lived apart” “(Isolation) would have phased you at the start, your just used to it now and you just kind of get on with it like the procedures and stuff, they have to be done. Patients have to get their care.” |
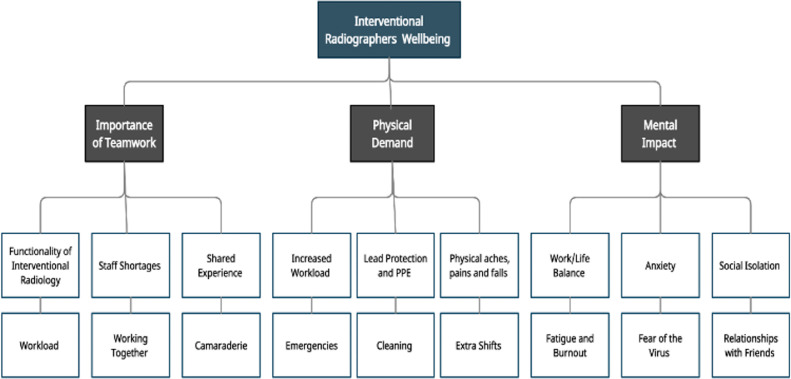
Fig. 6.
Thematic Map generated from the qualitative interviews.
Results
Quantitative results
Participant's characteristics
Forty participants completed the questionnaire over a period of one month. Detailed data on clinical experience, workplace setting, professional status are presented in Table 1 .
Table. 1.
Participants’ characteristics, clinical experience and interventional radiology experience
| Characteristic | Groups | Count (n) | (%) |
|---|---|---|---|
| Clinical experience | Less than 5 years | 11 | 27.5% |
| 5-9 years | 7 | 17.5% | |
| 10-19 years | 15 | 37.5% | |
| 20-29 years | 6 | 15% | |
| 30-39 years | 1 | 2.5% | |
| Workplace setting | Public | 32 | 80% |
| Private | 7 | 17.5% | |
| Voluntary | 1 | 2.5% | |
| Professional Status | Basic Grade Radiographer | 13 | 32.5% |
| Senior Radiographer | 14 | 35% | |
| Clinical Specialist | 13 | 32.5% | |
| Interventional radiology experience | Less than 2 years | 10 | 25% |
| 2-4 years | 9 | 22.5% | |
| 5-9 years | 7 | 17.5% | |
| 10-14 years | 5 | 12.5% | |
| 15-19 years | 5 | 12.5% | |
| 20-25 years | 4 | 10% | |
| Frequency working in interventional radiology | Daily | 15 | 37.5% |
| Weekly | 16 | 40% | |
| Monthly | 9 | 22.5% |
Experience Pre-COVID-19
Prior to COVID-19, all interventional radiographers reported liking working in IR with 100% (n=40) rating it greater or equal to 6 out of 10 and 35% (n=14) giving ten out of ten. Interventional radiographers identified “Enjoyable” (n=38, 95%) and “Rewarding” (n=37, 92%) as the two factors that they strongly agreed with which described working in IR.
Experience during COVID-19
Interventional radiographers’ opinion of work changed negatively during the pandemic for 50% (n=20) respondents with only 7.5% (n=3) noting a positive change in their opinion of work. Interventional radiographers identified that work was twice as “tiring” when compared with work pre-pandemic. Interventional radiographers identified “Tiring” (n=32, 80%) and “High pressured” (n=28, 70%) as the two factors that they strongly agreed with that described working in IR. Some 55% (n=22) of interventional radiographers did not notice a significant difference between the first and second waves of the pandemic and similarly 57.5% (n=23) noted no difference between the third and preceding waves (Fig. 1).
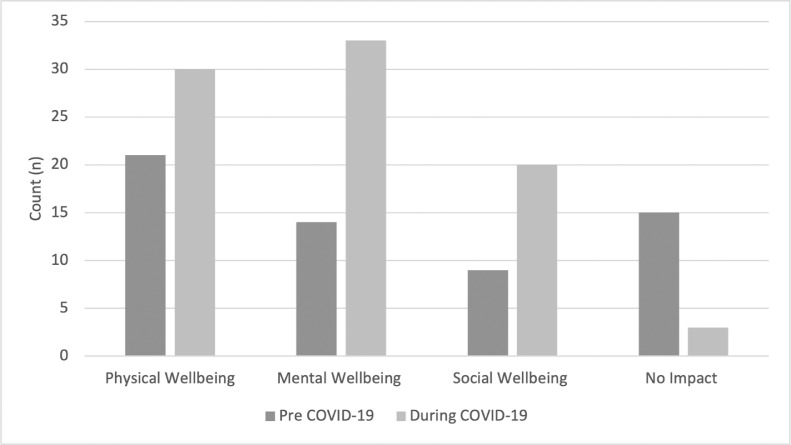
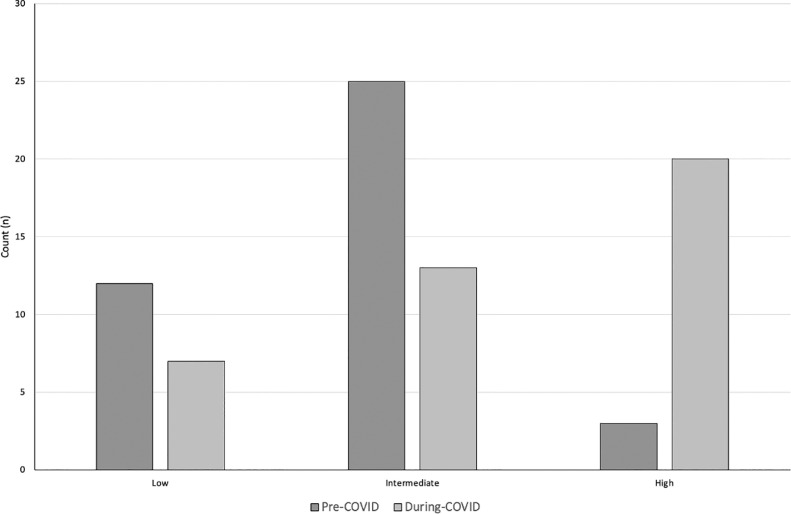
The responses of the interventional radiographers regarding wellbeing pre- and during COVID-19 is illustrated in Fig. 2 . The biggest difference seen is within mental wellbeing with 35% (n=14) of interventional radiographers being impacted pre-COVID and 82.5% (n=33) during COVID-19. Interventional radiographers reported being more stressed while working during COVID-19 with 50% (n=20) of respondent's feeling “highly stressed” (Fig. 3 ).
Fig. 2.
Bar chart illustrating the impact of working in IR on physical, mental, and social wellbeing among interventional radiographers pre-COVID and during COVID-19.
Fig. 3.
Bar chart illustrating the perceived stress levels among interventional radiographers pre-COVID and during COVID-19.
Work in Interventional Radiology
Pre-COVID the most common procedures identified by interventional radiographers were insertion of access lines including PICCs, port-a-caths and haemodialysis lines followed by nephrostomies and peripheral angioplasty procedures. During COVID-19 the most common procedures remained the same as pre-COVID but with the rise of peripheral angioplasty and embolization cases.
Interventional radiographers noted an increase in incidence of cerebrovascular accidents (CVA) and other clotting conditions relating to COVID-19. At sites where patients could be treated for a CVA, 75% (n=30) of interventional radiographers noted an increase in the number of related-procedures. In sites where there were cardiac interventional services, 75% of interventional radiographers noted an increase in patients presenting for treatments with myocardial infarctions. 85% of participating radiographers reported an increase in the presentations of IR-treated PE and a 45% reported an increase in patients presenting with other non-neurological/cardiac/pulmonary clotting disorders requiring IR.
A small proportion of interventional radiographers (n=12, 30%) identified their working pattern as ‘irregular’, based on their own interpretation, and of the remaining respondents 27.5% (n=11) noted an increase, 22.5% (n=9) noted a decrease and 20% (n=8) did not think there was any change to their work patterns. Interventional radiographers attributed the change in work pattern to several factors including “sicker patients” “increase in service demands” and “staffing issues” as having a direct impact on the functionality of IR.
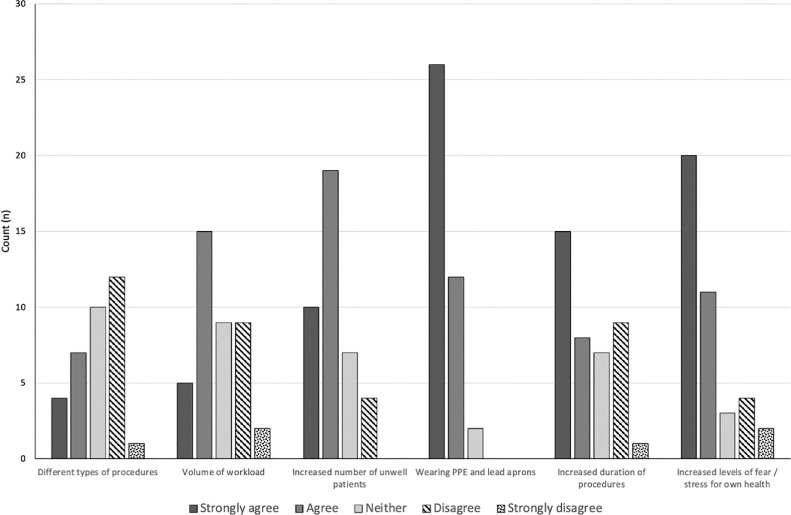
Six factors impacted interventional radiographers the most while working with COVID-19 patients (Fig. 4 ). The dominant factor that impacted interventional radiographers was wearing lead rubber aprons and PPE for prolonged periods of time, where 95% (n=38) reported that it had a significant impact on them while working with COVID-19 patients.
Fig. 4.
Graph illustrating the factors impacting wellbeing when working with COVID-19 patients in interventional radiology.
Wellbeing
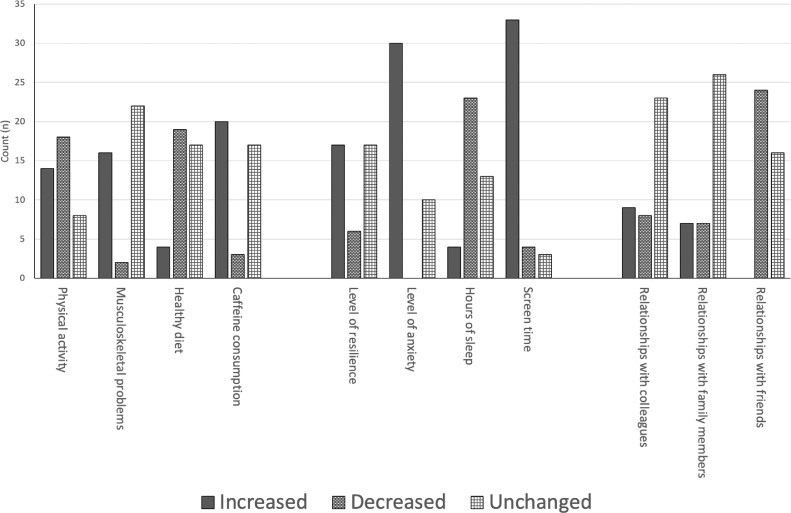
The wellbeing of interventional radiographers was affected in a variety of ways and is illustrated in Fig. 5 . Many interventional radiographers had anxiety about passing the virus onto family or friends (n=38, 95%). The majority were personally fearful of getting the virus and becoming sick (n=34, 85%). Similarly, 82.5% (n=33) felt occupational stress had a negative impact on their mental wellbeing and 87.5% (n=35) felt social isolation due to their occupation. Other factors that affected their mental wellbeing included having “extremely vulnerable partners,” “acting as a carer for elderly parents” and “witnessing extremely ill patients struggling to breathe.”
Fig. 5.
Illustration of the impact of COVID-19 on interventional radiographers’ wellbeing.
Interventional radiographers did not identify any meaningful change in their relationship with colleagues (n=23, 57.5%), whereas a similar proportion identified an improvement (n=9, 22.5%) or deterioration (n=10, 20%) in their relationship with colleagues. Conversely, 60% (n=24) of interventional radiographers noted a deterioration in relationship with friends with 40% (n=16) noting no change.
25% (n=10) of interventional radiographers agreed that there was adequate support available. 45% (n=18) disagreed and 30% (n=12) had no opinion. The majority of interventional radiographers did not know what support was available nor how to access it.
Qualitative interview results
As stated a Basic Grade and a Clinical Specialist Radiographer took part in the qualitative interviews. Three main themes were identified (Fig. 6 ) and included 1) importance of teamwork, 2) physical demand of IR and 3) mental impact of IR. These themes were explored and informed by quotations from participants (Table 2 ).
Discussion
Previous pandemics, such as the Severe Acute Respiratory Syndrome (SARS) outbreak of 2002, puts into context the hardships that radiographers can experience when working in healthcare. In previous pandemics, healthcare workers were noted to suffer “fear, anxiety, anger and frustration” [21]. Several studies identified that high levels of fatigue were induced by the requirements to take on additional workloads and work longer hours [22] In some cases, approximately 10% of staff reported experiencing post-traumatic stress due to the outbreak [23]. Pandemics have been noted to have detrimental effects on healthcare workers, however the impact of the COVID-19 pandemic on healthcare workers has previously not been reported. Given the scale of the pandemic and the requirements for managing related sequalae within IR, it was important to evaluate effects on radiographers working in specialist IR practice. Wellbeing is a concept that is diverse and can be influenced by many factors. This current study on three key components of the wellbeing of IR radiographers: physical; mental; and social. This publication is the first to consider the experiences of Irish radiographers working in IR during the COVID-19 pandemic.
Physical wellbeing
Interventional radiographers physical wellbeing may be affected by persistent use of lead protection and the increased requirements for cleaning, potentially making them susceptible to musculoskeletal injuries (MSI). MSI has been reported as one of the biggest causes of work-related illness and injury due to physical workload [17]. Interpretation of our data suggests that the physical wellbeing of interventional radiographers was not notably affected pre-COVID. This is likely to be due to working practices being suitably designed to maintain physical wellbeing, for example regular breaks and appropriate staff rotation. However, during the pandemic, interventional radiographers predominately described work as “tiring” and that changes in the functionality of IR and increases in physical demands affected their ability to do their work. Cleaning was identified as a challenge, particularly as IR suites can contain multiple devices and equipment that can be difficult to clean effectively [24]. Adopting strict infection control protocols was essential in mitigating cross infection [25]. Literature has shown examples of strict PPE protocols being adopted in IR, such as adopting PPE requirements to correlate with risk level. In many cases suspected and confirmed COVID-19 infection cases required “full PPE” [26]. The nature of IR procedures involves a “greater risk of acquiring and transmitting infection due to the close patient contact, length of procedures and invasive patient care the service provides” [27]. This therefore reinforced the need for staff to take substantial protective measures at all times. Increases in cleaning frequencies and the need for full PPE are likely to have resulted in increased physical demands for interventional radiographers. This feature has also been reported by operating department personnel working during the pandemic [28].
Over 80% of interventional radiographers identified a deterioration in their physical wellbeing after the onset of the pandemic. Physical wellbeing was particularly affected as people became more inactive, ate a poorer diet, consumed more caffeine, and suffered from more frequent musculoskeletal problems. Physical activity levels decreased among 45% participants while 35% noted an increase in activity levels. This increase may be due to the strong emphasis on physical activity during lockdown periods. However, the closure of gyms due to COVID-19 restrictions [29] and potentially a reluctance to socialise may have contributed to a decrease in physical activity. International literature also identifies a decrease in physical activity levels and subsequent increase in sedentary behaviour during the pandemic [30].
Many interventional radiographers suffered from the physical demand of their job whilst working in IR suites. Wearing PPE and lead shielding for prolonged periods of time was the most significant factor identified by the participants. Research has shown that wearing PPE for extended durations can have a physiological burden on healthcare workers, sequalae include headaches, fatigue, skin reactions and difficulty in breathing [31], [32], [33]. The physiological burden of wearing lead aprons is also likely to be compounded by the additional requirements to wear PPE.
Mental wellbeing
It has been reported that in some cases a large number of healthcare workers reported ‘burnout’ during the pandemic [34,35]. Local feedback identified that “three out of four staff met the definition for burnout” [36]. Within this context ‘burnout’ is likely to have been defined based on individual definitions but more broadly ‘a work-related stress syndrome resulting from chronic exposure to job stress’ [37]. Further studies have suggested significant problems with depression and anxiety amongst staff occurred during the pandemic [38]. Early reports on radiographer wellbeing during the initial stages of the COVID-19 identified burnout among 40% of staff [39]. A recent study from the United Kingdom identified that nearly 64% of staff experienced workplace related stress [6]. Within this work ‘contracting the infection and perceived inadequacy of PPE ‘were identified as two significant stressors. Similar findings have been reported from studies involving radiographers around the world [40], [41], [42].
During the COVID-19 pandemic, a large proportion of interventional radiographers (83%) identified a deterioration of their mental wellbeing. Interventional radiographers highlighted the fears and anxiety they had about getting the virus and the mental toll that social isolation took. Interventional radiographers identified heightened anxiety around seeing patients who were acutely unwell from COVID-19. Research has shown that some healthcare workers are presenting with post-traumatic stress symptoms (PTSS) as a result [43]. Frontline workers “represent a specific at-risk population for post-traumatic symptoms” due to their interactions with sick patients suggesting a significant impact on workers mental wellbeing [43]. Social isolation was compounded by the national lockdowns imposed but also by the nature of the interventional radiographers occupation. Working within IR during the pandemic required radiographers to be in close contact with patients who had contracted COVID-19 for extended periods of time. Fear of potential cross-infection to friends and family is likely to have added to the issue of social isolation. Occupational stress had a substantial effect on interventional radiographers with 50% of them identifying themselves as ‘highly stressed’. The combination of emotional distress with a high pressured role requiring high levels of concentration resulted in a negative impact on interventional radiographers mental wellbeing and could potentially lead to the onset of “occupational diseases” [40]. Within IR, high levels of concentration are often required to ensure that the real-time area of interest remains within the field of view, this can often be over extended periods due to the nature of the work. This highlights the need for support services and “secondary care mental health services” to deal with the significant burden that COVID-19 has had on interventional radiographers mental wellbeing [44].
Eighty percent of interventional radiographers noticed an increase in their screen time and a decrease in the hours that they slept each night. An increase in screen usage may be a result of a lack of opportunities for face-to-face social interactions. Evidence supports the theory that screen usage and sleep are intrinsically linked as ‘blue light’ from screens can directly impact on a person's sleep hygiene and sleep quality [49,50]. A reduction in sleep can also have a detrimental effect on an individual's health in particular their mood and level of fatigue [51]. One study identified that the majority of frontline worker had poor sleep since the onset of the pandemic and over 60% suffered from “sleep disruptions due to device use” [52]. Research has shown that among healthcare workers, their “level of anxiety were significantly associated with the levels of stress, which negatively affected their sleep quality” [48]. Although a direct link with screen time and IR practice was not a key aim or focus of this research, as authors we feel it important to document these findings. Such findings can provide useful comparators when considering screen time / mobile device utilisation in general and comparisons with other healthcare professions, including radiographers working in other imaging modalities.
Social wellbeing
Interventional radiographers social wellbeing may be affected as healthcare workers have identified periods of isolation and fear due to the perceived threat that they may pose to the general public due to the high-risk nature of the job [45,46]. Stigma among frontline staff was identified as having a direct impact on a person's abilities to have social interactions [47]. A study from Wuhan, China identified “anxiety, stress, and self-efficacy” directly depended on their degree of social support and quality of sleep [48].
Social wellbeing of interventional radiographers was impacted by the onset of COVID-19 in two ways. Firstly, 60% of interventional radiographers identified deterioration in relationships with their friends. Many frontline healthcare workers including interventional radiographers were feared by the general population for transmitting the virus to others. Recent research carried out identified that a third of respondents “avoided healthcare workers” for fear of infection, highlighting the stigmatisation and social isolation that many faced during the pandemic [53]. Secondly, interventional radiographers noted an improvement in their relationship with their colleagues. This may be as a result of the shared experiences between interventional radiographers within a team. This was validated in the qualitative interviews; both participants spoke of the importance of teamwork and the positive impact that this had on their ability to do their work. Research has presented mixed experiences regarding improvements in multidisciplinary collaboration during COVID-19 [54]. Within the study by Anjara et al. [54], participants described greater collaboration as one of the most significant developments arising from COVID-19. Staff described feelings of working together as one team and that they felt the need to pull together and meet the challenges, i.e personal risks of contracting COVID-19, and goals presented by the pandemic.
Impact of COVID-19
Health services in Ireland were significantly disrupted by COVID-19. Some hospitals were more affected than others and in unique ways. This is reflected in an even distribution of experiences regarding changes to workload with a slight majority (30%) noting that their workload was irregular. Public hospitals primarily treated acutely unwell patients infected with the SARS-CoV-2 virus. This was reflected in the responses from interviewees as public hospitals dealt with more COVID-19 positive patients in their interventional services resulting in a fluctuation in their elective services. Conversely, private hospitals did not treat significant numbers of COVID-19 patients, however their elective lists were still disrupted but not to the same degrees as those in the public hospitals. This is reflected in recent literature which acknowledges the fluctuations in workload and service delivery during the pandemic [55].
Recommendations
Key challenges to radiology departments that were identified included staffing shortages, functionality of IR and subsequent impact on interventional radiographers wellbeing. In order to address these challenges, in the opinion of the authors’, the following steps should be taken. Firstly, departments should seek to mitigate this by ensuring optimum numbers of staff are trained in IR to cover the service provided. Such training numbers should also factor in likely staff absences from subsequent waves in the pandemic [56]. In addition, adequate breaks should be given to staff during long procedures. Secondly, departments should consider consistent communication, strong leadership and specific strategies to minimise the amount of work related stress particularly felt by interventional radiographers. Finally, ongoing education and departmental specific training is needed to address wellbeing. A focus should be put on wellbeing by designating a wellbeing officer / champion to proactively promote wellbeing among interventional radiographers and encourage staff to take time to seek support services.
Studies have reported occupational stress, fatigue and burnout relating to the COVID-19 pandemic and those working in healthcare and across radiography in general [5], [6], [7]. For future studies, it would be useful to conduct a comparison of the adverse effects of the COVID-19 pandemic on radiographers working across the different imaging modalities.
Limitations
There is no comprehensive list of hospitals or departments that provides interventional services which made it difficult in identifying specific sites to target the questionnaire which resulted in a reliance of interventional radiographers to pass on the questionnaire among colleagues. A comprehensive list of locations would be useful for future research as it would assist in identifying specific cohorts of radiographers. It is widely acknowledged that there will be differences in working practices between public and private hospitals. Further, possibly different, variations in terms of IR practice may have existed during the COVID-19 pandemic but due to the relatively small sample size this would have been difficult to quantify from the survey findings. Such a comparison could be the focus of future research.
There are currently 2,570 radiographers registered in Ireland according to the regulatory body (CORU). It was difficult to identify an accurate response rate for this research as there is no specific number of interventional radiographers in Ireland. It is difficult to quantify what proportion were involved in the study. However, this sample is likely representative in terms of a variety of clinical experience and professional status and therefore the survey findings can be considered generalisable. It should be noted that the number of interviewees in the qualitative element of the study was two. Questions could arise as to any potential biases that may have existed in the two participants or the generalisability of their contributions. Our study was mixed methods in design and sought interview responses to help enhance the quantitative data provided by the 40 questionnaires respondents. Sample size should be considered when interpreting findings from this study. It is also worthy of note that a number of respondents had worked in IR for less than four years. If the cohort in general had greater experience in IR then some of the pooled responses could have been different.
Terminology differences and internal definitions of participants must be a consideration when interpreting the results of this study. A feature of our questionnaire was to allow participants to base responses on their own definitions of factors relating to working within the COVID-19 pandemic. If we had presented respondents with pre-defined definitions then this could have resulted in some variability in the results.
Lastly, this study is subject to a degree of self-reporting bias as participants were asked to volunteer to take part in the interview element of the study. This study also incorporated some recall bias as participants were asked to recall events and experiences from over one year ago prior to the onset of COVID-19. To minimise this risk in further research, a standardised questionnaire could be used as a methods of data collection.
Conclusion
This study quantifies the negative effect that the COVID-19 pandemic had on the physical, mental and social wellbeing of interventional radiographers. The reasons for these changes were identified which can be used to focus future efforts to prevent illness, prevent burnout and restore productivity. This research highlights the need to monitor the wellbeing of interventional radiographers and other health professionals. Further research should seek to identify methods of addressing the shortcomings in support services and identifying the specific needs of the interventional radiographers to improve their wellbeing.
Acknowledgments
Acknowledgements
The authors would like to thank the interventional radiographers who agree to participate in this research.
Footnotes
Contributors: All authors contributed to the conception or design of the work, the acquisition, analysis, or interpretation of the data. All authors were involved in drafting and commenting on the paper and have approved the final version.
Declaration of Competing Interest: No conflicts of interests to declare. Mark McEntee is Deputy Editor at JMIRS but was blinded to the decision making process.
Funding: This research did not receive any grant.
Ethical approval: Research ethical approval was granted by the institution: University College Cork Social Research Ethics Committee: CT-SREC-2020-29.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmir.2022.05.006.
Appendix. Supplementary materials
References
- 1.Health Protection Surveillance Centre. Health Protection Surveillance Centre 2020 COVID-19 Cases in Ireland. https://www.hpsc.ie/a-z/respiratory/coronavirus/novelcoronavirus/
- 2.Temsah MH, Al-Sohime F, Alamro N, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health. Jun 2020;13(6):877–882. doi: 10.1016/j.jiph.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Billings J, Ching BCF, Gkofa V, Greene T, Bloomfield M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv Res. Sep 06 2021;21(1):923. doi: 10.1186/s12913-021-06917-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis S, Mulla F. Diagnostic radiographers' experience of COVID-19, Gauteng South Africa. Radiography (Lond) 2021;27(2):346–351. doi: 10.1016/j.radi.2020.09.009. 05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shanahan MC, Akudjedu TN. Australian radiographers' and radiation therapists' experiences during the COVID-19 pandemic. J Med Radiat Sci. Jun 2021;68(2):111–120. doi: 10.1002/jmrs.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akudjedu TN, Mishio NA, Elshami W, et al. The global impact of the COVID-19 pandemic on clinical radiography practice: A systematic literature review and recommendations for future services planning. Radiography (Lond) 2021;27(4):1219–1226. doi: 10.1016/j.radi.2021.07.004. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akudjedu TN, Botwe BO, Wuni AR, Mishio NA. Impact of the COVID-19 pandemic on clinical radiography practice in low resource settings: The Ghanaian radiographers' perspective. Radiography (Lond) 2021;27(2):443–452. doi: 10.1016/j.radi.2020.10.013. 05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gu SX, Tyagi T, Jain K, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol. 2021;18(3):194–209. doi: 10.1038/s41569-020-00469-1. 03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soumya RS, Unni TG, Raghu KG. Impact of COVID-19 on the cardiovascular system: a review of available reports. Cardiovasc Drugs Ther. 2021;35(3):411–425. doi: 10.1007/s10557-020-07073-y. 06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merkler AE, Parikh NS, Mir S, et al. Risk of ischemic stroke in patients with Covid-19 versus patients with influenza. medRxiv. May 21 2020 doi: 10.1101/2020.05.18.20105494. [DOI] [Google Scholar]
- 11.Wang A, Mandigo GK, Yim PD, Meyers PM, Lavine SD. Stroke and mechanical thrombectomy in patients with COVID-19: technical observations and patient characteristics. J Neurointerv Surg. Jul 2020;12(7):648–653. doi: 10.1136/neurintsurg-2020-016220. [DOI] [PubMed] [Google Scholar]
- 12.How GY, Pua U. Trends of interventional radiology procedures during the COVID-19 pandemic: the first 27 weeks in the eye of the storm. Insights into Imaging. 2020/12/09. 2020;11(1):131. doi: 10.1186/s13244-020-00938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vadukul P, Sharma DS, Vincent P. Massive pulmonary embolism following recovery from COVID-19 infection: inflammation, thrombosis and the role of extended thromboprophylaxis. BMJ Case Rep. Sep 13 2020;13(9) doi: 10.1136/bcr-2020-238168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naylor S, Booth S, Harvey-Lloyd J, Strudwick R. Experiences of diagnostic radiographers through the Covid-19 pandemic. Radiography (Lond) 2022;28(1):187–192. doi: 10.1016/j.radi.2021.10.016. 02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh N, Knight K, Wright C, et al. Occupational burnout among radiographers, sonographers and radiologists in Australia and New Zealand: Findings from a national survey. J Med Imaging Radiat Oncol. Jun 2017;61(3):304–310. doi: 10.1111/1754-9485.12547. [DOI] [PubMed] [Google Scholar]
- 16.Sehlen S, Vordermark D, Schäfer C, et al. Job stress and job satisfaction of physicians, radiographers, nurses and physicists working in radiotherapy: a multicenter analysis by the DEGRO Quality of Life Work Group. Radiat Oncol. Feb 06 2009;4:6. doi: 10.1186/1748-717X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hulls PM, Money A, Agius RM, de Vocht F. Work-related ill-health in radiographers. Occup Med (Lond) Aug 11 2018;68(6):354–359. doi: 10.1093/occmed/kqy076. [DOI] [PubMed] [Google Scholar]
- 18.Williams A. How to...write and analyse a questionnaire. J Orthod. Sep 2003;30(3):245–252. doi: 10.1093/ortho/30.3.245. [DOI] [PubMed] [Google Scholar]
- 19.Zheng J. How many days does it take for respondents to respond to your survey? Accessed 27th March, 2022. https://www.surveymonkey.com/curiosity/time-to-respond/
- 20.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. 2006/01/01. [DOI] [Google Scholar]
- 21.Maunder R, Hunter J, Vincent L, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. May 13 2003;168(10):1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 22.Grace SL, Hershenfield K, Robertson E, Stewart DE. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics. Sep-Oct 2005;46(5):385–391. doi: 10.1176/appi.psy.46.5.385. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. May 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De-Gregorio MA, Guirola JA, Magallanes M, et al. COVID-19 Outbreak: Infection Control and Management Protocol for Vascular and Interventional Radiology Departments-Consensus Document. Cardiovasc Intervent Radiol. Aug 2020;43(8):1208–1215. doi: 10.1007/s00270-020-02493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iezzi R, Valente I, Cina A, et al. Longitudinal study of interventional radiology activity in a large metropolitan Italian tertiary care hospital: how the COVID-19 pandemic emergency has changed our activity. Eur Radiol. Dec 2020;30(12):6940–6949. doi: 10.1007/s00330-020-07041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gogna A, Punamiya S, Gopinathan A, et al. Preparing IR for COVID-19: The Singapore Experience. J Vasc Interv Radiol. 2020;31(6):869–875. doi: 10.1016/j.jvir.2020.03.021. 06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chandy PE, Nasir MU, Srinivasan S, Klass D, Nicolaou S, B-Babu S. Interventional radiology and COVID-19: evidence-based measures to limit transmission. Diagn Interv Radiol. May 2020;26(3):236–240. doi: 10.5152/dir.2020.20166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Swaminathan R, Mukundadura BP, Prasad S. Impact of enhanced personal protective equipment on the physical and mental well-being of healthcare workers during COVID-19. Postgraduate Med J. 2022;98(1157):231. doi: 10.1136/postgradmedj-2020-139150. [DOI] [PubMed] [Google Scholar]
- 29.Forde C, Wyse J, Barrett E. Time and belief in exercise importance predict increased activity during initial COVID-19 restrictions in Ireland. Health Promot Int. Jul 19 2021 doi: 10.1093/heapro/daab113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stockwell S, Trott M, Tully M, et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport & Exercise Medicine. 2021;7(1) doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choudhury A, Singh M, Khurana DK, et al. Physiological Effects of N95 FFP and PPE in Healthcare Workers in COVID Intensive Care Unit: A Prospective Cohort Study. Indian J Crit Care Med. Dec 2020;24(12):1169–1173. doi: 10.5005/jp-journals-10071-23671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rosner E. Adverse effects of prolonged mask use among healthcare professionals during COVID-19. J Infect Dis Epidemiol. 2020;6(3):130. [Google Scholar]
- 33.Vidua RK, Chouksey VK, Bhargava DC, Kumar J. Problems arising from PPE when worn for long periods. Med Leg J. Nov 2020;88(1_suppl):47–49. doi: 10.1177/0025817220935880. [DOI] [PubMed] [Google Scholar]
- 34.Lasalvia A, Amaddeo F, Porru S, et al. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021;11(1) doi: 10.1136/bmjopen-2020-045127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bradley M, Chahar P. Burnout of healthcare providers during COVID-19. Cleveland Clinic J Med. 2020 doi: 10.3949/ccjm.87a.ccc051. [DOI] [PubMed] [Google Scholar]
- 36.Chernoff P, Adedokun C, O'Sullivan I, McManus J, Payne A. Burnout in the Emergency Department hospital staff at Cork University Hospital. Ir J Med Sci. May 2019;188(2):667–674. doi: 10.1007/s11845-018-1871-5. [DOI] [PubMed] [Google Scholar]
- 37.De-Hert S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local Reg Anesth. 2020;13:171–183. doi: 10.2147/LRA.S240564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic. A systematic review and meta-analysis. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Foley SJ, O'Loughlin A, Creedon J. Early experiences of radiographers in Ireland during the COVID-19 crisis. Insights Imaging. Sep 25 2020;11(1):104. doi: 10.1186/s13244-020-00910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pereira JM, Silva C, Freitas D, Salgado A. Burnout among Portuguese radiographers during the COVID-19 pandemic. Radiography (Lond) 2021;27(4):1118–1123. doi: 10.1016/j.radi.2021.05.001. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mahajan A, Sharma P. Psychological impact of COVID-19 on radiology: Emotional wellbeing versus psychological burnout. Indian J Radiol Imaging. Jan 2021;31(1):S11–S14. doi: 10.4103/ijri.IJRI_579_20. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zanardo M, Cornacchione P, Marconi E, et al. Occupational burnout among radiation therapy technologists in Italy before and during COVID-19 pandemic. J Med Imaging Radiat Sci. 03. 2022;53(1):58–64. doi: 10.1016/j.jmir.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rossi R, Socci V, Pacitti F, et al. Mental Health Outcomes Among Healthcare Workers and the General Population During the COVID-19 in Italy. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.608986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O'Connor K, Wrigley M, Jennings R, Hill M, Niazi A. Mental health impacts of COVID-19 in Ireland and the need for a secondary care mental health service response. Ir J Psychol Med. 2021;38(2):99–107. doi: 10.1017/ipm.2020.64. 06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int J Environ Res Public Health. 04 26. 2020;17(9) doi: 10.3390/ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav Immun Health. Oct 2020;8 doi: 10.1016/j.bbih.2020.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Juan Y, Yuanyuan C, Qiuxiang Y, et al. Psychological distress surveillance and related impact analysis of hospital staff during the COVID-19 epidemic in Chongqing, China. Compr Psychiatry. 2020;11(103) doi: 10.1016/j.comppsych.2020.152198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xiao H, Zhang Y, Kong D, Li S, Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. Mar 05 2020;26 doi: 10.12659/MSM.923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Exelmans L, Van-den-Bulck J. Bedtime mobile phone use and sleep in adults. Soc Sci Med. Jan 2016;148:93–101. doi: 10.1016/j.socscimed.2015.11.037. [DOI] [PubMed] [Google Scholar]
- 50.Grimaldi-Puyana M, Fernández-Batanero JM, Fennell C, Sañudo B. Associations of Objectively-Assessed Smartphone Use with Physical Activity, Sedentary Behavior, Mood, and Sleep Quality in Young Adults: A Cross-Sectional Study. Int J Environ Res Public Health. 2020;17(10) doi: 10.3390/ijerph17103499. 05 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Appleton SL, Reynolds AC, Gill TK, Melaku YA, Adams R. Waking to use technology at night, and associations with driving and work outcomes: a screenshot of Australian adults. Sleep. 2020;43(8) doi: 10.1093/sleep/zsaa015. 08 12. [DOI] [PubMed] [Google Scholar]
- 52.Stewart NH, Koza A, Dhaon S, Shoushtari C, Martinez M, Arora VM. Sleep Disturbances in Frontline Health Care Workers During the COVID-19 Pandemic: Social Media Survey Study. J Med Internet Res. 2021;23(5):e27331. doi: 10.2196/27331. 05 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taylor S, Landry CA, Rachor GS, Paluszek MM, Asmundson GJG. Fear and avoidance of healthcare workers: An important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. 2020;10(75) doi: 10.1016/j.janxdis.2020.102289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anjara S, Fox R, Rogers L, De-Brún A, McAuliffe E. Teamworking in Healthcare during the COVID-19 Pandemic: A Mixed-Method Study. Int J Environ Res Public Health. 10 01. 2021;18(19) doi: 10.3390/ijerph181910371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xu Y, Mandal I, Lam S, et al. Impact of the COVID-19 pandemic on interventional radiology services across the world. Clin Radiol. 2021;76(8):621–625. doi: 10.1016/j.crad.2021.05.001. 08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khorasanee R, Grundy T, Isted A, Breeze R. The effects of COVID-19 on sickness of medical staff across departments: A single centre experience. Clin Med (Lond) Mar 2021;21(2):e150–e154. doi: 10.7861/clinmed.2020-0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.