Abstract
Background
Smartphone-based online education gained popularity during and after the COVID-19 pandemic. Although recent studies have highlighted the association between problematic smartphone use (PSU) and mental health symptoms, the potential role of online learning in this relationship remains unclear. This study aimed to analyze the relationships between higher education modes, PSU, and related psychological symptoms in university students.
Methods
A total of 1,629 Chinese university students from five provinces completed a web-based questionnaire survey between March 2020 and October 2021. Demographic characteristics and learning conditions were recorded. All participants completed the Smartphone Addiction Scale-Short Version, Patient Health Questionnaire, Generalized Anxiety Disorder Scale, and Athens Insomnia Scale. Multiple regressions models and stratified analyses were used to examine the association between online education mode, PSU, and symptoms of depression, anxiety, and insomnia.
Results
The prevalence of PSU was 58.5%. Students who relied primarily on online learning had a higher prevalence of depressive symptoms (29.95% vs. 22.24%), anxiety symptoms (25.13% vs. 18.91%), and insomnia symptoms (75.89% vs. 70.27%) than those who relied on traditional face-to-face learning (Ps < 0.05). After adjusting for covariates, subjects with PSU were more likely to report depressive symptoms (AdjOR = 3.14, 95% CI = 2.26–4.37), anxiety symptoms (AdjOR = 3.73, 95% CI = 2.13–4.59), and insomnia symptoms (AdjOR = 2.96, 95% CI = 2.23–3.92) than those without PSU. Furthermore, the associations of PSU with depressive symptoms (OR = 4.66 vs. 2.33, P for interaction = 0.015) and anxiety symptoms (OR = 6.05 vs. 2.94, P for interaction = 0.021) were more pronounced in the online learning group.
Conclusion
Our study provides preliminary evidence that Chinese university students have serious smartphone addiction problems, which are associated with depressive, anxiety, and insomnia symptoms. Online learning is found to exacerbate PSU and mental health problems. Our findings provide valuable information for targeted psychological interventions in the post-COVID-19 era.
Keywords: online learning, problematic smartphone use, mental health, COVID-19, college students
Introduction
The COVID-19 pandemic, a global public health emergency, has had significant impacts on China's healthcare and higher education system (1). The emergence of SARS-CoV-2 Delta and Omicron variants, currently spreading worldwide, has given rise to a new wave of the pandemic (2). On March 11th, 2020, the World Health Organization declared that the COVID-19 outbreak was a global pandemic, and governments have since implemented a series of strict social isolation policies to control the novel coronavirus (3). To avoid the spread of coronavirus among students, universities have adopted a variety of teaching methods, among which online learning has rapidly gained popularity (4). Online education has been found to significantly reduce the COVID-19 infection rate in students, and to effectively maintain the normal higher education teaching activities (5). Recent evidence suggested that the advancements of digital technology supported the effectiveness of online education (6).
However, just like every coin has two sides, online learning has some disadvantages. Other than the quality of education organization, scholars have also focused on the hidden negative effects of online leaning, such as Internet addiction and related mental health problems (7, 8). Both cross-sectional and longitudinal studies have confirmed that different types of Internet-related addiction behaviors were associated with psychological distress among mainland Chinese students during the COVID-19 school suspension (9, 10). Survey data have revealed that education supervision and related psychological problems are challenges that have yet to be overcome in the future education progress (11). While online learning is more flexible than traditional face-to-face learning, it increases the frequency of smartphone use among students. Recent studies have reported increased smartphone addiction and mental health problems since the COVID-19 outbreak (12, 13), yet it remains unclear whether online education contributes to this.
Since the COVID-19 outbreak in Wuhan in December 2019, the Chinese government has implemented effective social distancing measures, and students were forced to keep away from universities. Since the summer of 2020, most Chinese university students have been released from quarantine and returned to school. During and after the pandemic, a growing number of colleges have been implementing a transition from traditional face-to-face teaching methods to online teaching or a hybrid teaching, which has become the new normal. Researchers have expressed mixed views about the online education mode. Pei and Wuin concluded that online learning could enhance knowledge and skills to a greater degree than face-to-face learning (14). However, Hasan and Bao reported that the sudden transformation to distance learning was a challenge for students, and significantly exacerbated students' psychological stress (15). The severity of the COVID-19 pandemic has varied in different countries and areas. Despite the fact that China has effectively brought the coronavirus pandemic under control, new sporadic and imported COVID cases continue to emerge across the country. Thus, higher education methods must be tailored to these indeterminate epidemic conditions. For example, if there are no new cases in an area for a long time, local universities can maintain face-to-face and centralized teaching; however, if a new coronavirus epidemic occurs, universities must replace face-to-face teaching with online teaching until the local epidemic is effectively controlled.
During the COVID-19 pandemic, smartphones have played a vital role for health care and higher education progress (16), and university students have relied more on the Internet and smartphones for both social and learning activities (16). Some psychologists have regarded smartphone addiction and related psychological problems as a new hidden crisis of the COVID-19 pandemic (17). Recent systematic reviews have described the psychological distress and related influence factors during COVID-19 (18, 19). Over the past 2 years, several studies also reported the associations between COVID-19 psychological problems and smartphone addiction (20–22). In a large cross-sectional survey that included 89,588 Chinese college students, 41.1% reported anxiety symptoms (23). Recent studies have also revealed that the intensity and time of electronic device usage increased during the COVID-19 pandemic, and was positively correlated with various mental health problems (24, 25). Another national survey conducted by Ma et al. with 746,217 Chinese college students found that the prevalence of probable acute stress, depressive symptoms, and anxiety symptoms were 34.9, 21.1, and 11%, and the risks of developing depression and anxiety disorders among the student sample increased with the exposure time to electronic devices (26). Sleep problems appear to have been common during the ongoing COVID-19 pandemic. In Alimoradi et al.'s recent meta-analysis, sleep problems were found to be associated with higher levels of psychological distress (27). In one of our published studies, problematic smartphone use (PSU) was found to be associated with fatigue symptoms and sleep quality in medical students (28). However, limited research has examined the different mental health patterns caused by online education, especially in China. The present study will fill this gap in the literature by examining the potential role of online learning in the relationship between PSU and related mental health outcomes.
Many mechanistic studies have explored the relationship between PSU and clinical health outcomes, and specific theories have highlighted the potential effects of learning environment factors on health outcomes in student samples. PSU affects mental health through a variety of complex pathways, leading to symptoms of depression, anxiety, and loneliness (29). Some well-established theoretical frameworks are benefit for explaining the association of psychopathological symptoms with PSU. One of the most recognized theoretical frameworks is the Interaction of Person-Affect-Cognition-Execution (I-PACE) model (30). According to the I-PACE model, individuals' demographic background and psychological status, such as personality, emotional, cognitive, and executive functions can significantly predict Internet or smartphone addiction. As described by the Compensatory Internet Use Theory (CIUT), if individuals are in a negative situation, they may escape reality by surfing the internet, thus increasing the chance of addiction symptoms (31). The CIUT theory also places an emphasis on the importance of environmental factors in addiction risk. For instance, when college students rely primarily on the Internet for learning, they enter a more isolated social environment. Excessive smartphone use can lead to increased exposure to blue and short electromagnetic waves, which results in eye symptoms, sleep disturbances, and physical fatigue (25). In addition, online learning students are often less likely to receive effective educational supervision and timely assistance (32). Thus, the physical and mental health problems of these students should be paid more attention. Based on the existing theoretical mechanisms and relevant research findings, it seems possible that education mode is associated with PSU and mental health in university students. We thus proposed the following research hypotheses:
Hypothesis 1 (H1). PSU is positively associated with levels of depression, anxiety, and insomnia symptoms.
Hypothesis 2 (H2). Different learning modes are associated with different PSU levels in university students.
Hypothesis 3 (H3). Different learning modes are associated with different mental health statuses in university students.
Hypothesis 4 (H4). Education modes may moderate the relationship between PSU and mental health problems.
Materials and Methods
Participants and Ethics
Participants were 1,629 full-time university students recruited from eight colleges in Beijing, Shanghai, Xi'an, Zhejiang, and Jiangxi province. The Ethics Committee of Beijing Hospital approved the study (2020BJYEC-231-01). Respondents provided electronic signatures of informed consent in the web-based survey system before the investigation. The size of the sample population was selected based on the following criteria: As recommended by some scholars, a sample item ratio >20 and sample independent variable ratio >10 are sufficient (33). Thus, the appropriate recommended sample size was 200, and we successfully collected data from over 1,000 participants.
Procedures
A web-based online survey was conducted between March 2020 and October 2021. Well-trained student counselors from each university were responsible for sending and receiving the questionnaires, and all respondents volunteered to participate in the study. In the online survey system, subjects were not allowed to submit the online questionnaire until they had completed all the questions. A total of 1,780 questionnaires were collected; 55 questionnaires with a response time <5 min and 21 questionnaires with unidentifiable demographic information were excluded. Moreover, if all questions in the four scales were answered in an identical or repetitive manner, the questionnaire was identified as invalid (n = 75). Overall, 151 invalid questionnaires were excluded, and 1,629 (recovery rate = 91.52%) valid questionnaires were included in the final analysis. We investigated students' recent learning conditions through a binary question that asked subjects to report which learning method had been used most frequently in the past 1 month. Based on their responses, subjects were divided into an online learning group and traditional face-to-face learning group. Education level was classified as bachelor, master, and doctoral. Grade was classified as graduating students or not. Residence was classified as urban and rural. Education satisfaction was assessed using a 5-point Likert scale (“bad/unsatisfied” = 1–3 points; “good/satisfied” = 4–5 points). If subjects self-reported engaging in regular exercise, they were defined as having an exercise habit, and those who self-reported occasional exercise or no exercise were defined as having no exercise habit.
Measurement
Smartphone Addiction Scale-Short Version
The Smartphone Addiction Scale-Short Version (SAS-SV) developed by Kwon and colleagues was used to measure the severity of problematic smartphone use (34). The scale consists of 10 items that are scored on a 6-point Likert scale, and the summed score ranges from 10 to 60. An example question is, “I feel impatient or restless when I'm not holding my smartphone”. Subjects were asked to rate how much they agreed with each statement (“disagree” = 1 point; “agree” = 6 points). According to the thresholds recommended for adolescents, male participants with a summed score ≥31 and female participants with a summed score ≥33 were identified as having PSU. The SAS-SV has been shown to have good reliability and validity in the Chinese population (35). The Cronbach's α coefficient of the SAS-SV was 0.91 in this study.
9-Item Patient Health Questionnaire
The 9-item Patient Health Questionnaire (PHQ-9) (36) is a valid self-administered depression screening tool, and was used to measure the level of depressive symptoms. The scale includes 9 items that are scored on a 4-point Likert scale to assess the presence of depressive symptoms during the last week (“not at all” = 0 points; “several days” = 1 point; “more than half the week” = 2 points; “almost every day” = 3 points). Higher scores indicate more severe depressive symptoms. The summed PHQ-9 score ranges from 0 to 27, and subjects with a total score ≥10 were defined as exhibiting depressive symptoms. A recent meta-analysis confirmed that a cutoff of 10 or above can maximize the combined sensitivity and specificity (37). The PHQ-9 showed good internal consistency, with a Cronbach's α coefficient of 0.89 in the current study.
7-Item Generalized Anxiety Disorder Scale
The 7-item Generalized Anxiety Disorder Scale (GAD-7) is a self-report measurement that screens the presence of generalized anxiety disorders over the previous 2 weeks (38). The scale consists seven statements about worry or somatic tension, which are rated on a 4-point Likert scale (“not at all” = 0 points; “several days” = 1 point; “more than half the week” = 2 points; “almost every day” = 3 points). Higher scores indicate more severe anxiety symptoms. Given that the GAD-7 has a low sensitivity for detecting mild symptoms, previous studies have reported that the GDA-7's appropriate screening cutoff is ≥10 in both clinical samples and the general population (39), and its Cronbach's α coefficient was 0.93 in this study.
8-Item Athens Insomnia Scale
Sleep quality was measured using the 8-item Athens Insomnia Scale (AIS-8) (40). The AIS-8 is a self-assessment psychometric instrument that includes 8 items scored on a 6-point Likert scale, with a total score of 0–24. Items assess sleep induction, awakenings during the night, final awakening, total sleep duration, sleep quality, well-being, functioning capacity, and daytime sleepiness. Individuals with a summed AIS-8 score ≥6 were classified as having insomnia symptoms (41). In this study, the Cronbach's α coefficient of the scale was 0.87.
Statistical Analysis
Continuous variables were presented as the mean ± standard deviation (M ± SD), and categorical variables as numbers and percentages [n (%)]. To test whether different education modes are associated with levels of smartphone addiction problems and related mental health symptoms (H2 and H3), student's t-test and Chi-square test were used to compare the PSU and psychological status between online learning and face-to face learning subgroups. We used Harman's single factor method to test the common method bias, which is common in multiple self-assessment questionnaires (42). All the items in the observational measurements were included in an exploratory factor analysis. If the first factor to be extracted explains <40% of the total variation, there is no common method bias. To confirmed the positively associations between PSU levels and psychological problems (H1), a series of linear regression models were used to test the correlations between SAS-SV, PHQ-9, GAD-7, and AIS-8 scores. Multiple logistic regression analyses were used to analyze the association between PSU and the risk of depressive, general anxiety, and insomnia symptoms. Subjects without PSU were used as the reference group, and odds ratios (ORs) with 95% confidence intervals (CIs) were calculated after adjusting for potential confounders. To test the moderating role of learning modes on the relationship between PSU and mental health symptoms (H4), cross-product terms were added to each model. We also performed subgroup logistic regression analyses for participants, stratified by online learning and face-to face learning subgroups. Statistical significance was defined as a two-sided p-value of 0.05, and CIs were computed at the 95% level. Statistical analyses were performed using Statistic Package for Social Science version 22.0 for windows (IBM Corporation, Armonk, NY, USA).
Results
Demographic Characteristics
The mean age of participants was 23.85 ± 3.53 years. A total of 788 (48.37%) reported online learning to be their most frequently used learning mode, and 841 (51.63%) reported traditional face-to-face learning as their most frequently used learning mode. Among the 1,629 participants, 65.25% were female, 19.89% were graduating students, and 70.04% were urban residents; 76.98% were satisfied with the current education system, and 36.28% had exercise habits.
PSU and Psychological Health
The mean SAS-SV score was 33.81 ± 9.81, with a PSU prevalence of 58.5%. The prevalence of depressive, anxiety, and insomnia symptoms were 25.97, 21.92, and 72.99%, respectively. As shown in Table 1, the online learning group had a higher prevalence of PSU (62.82% vs. 54.46%, P < 0.001), depressive symptoms (29.95% vs. 22.24%, P = 0.003), anxiety symptoms (25.13% vs. 18.91%, P < 0.001), and insomnia symptoms (75.89% vs. 70.27%, P = 0.006) than the face-to-face learning group.
Table 1.
Problematic smartphone use and psychological symptoms of all 1,629 students.
| Measurements | Overall (n = 1629) | Online learning group (n = 788) | Face-to-face learning group (n = 841) | t /χ2 | P -value |
|---|---|---|---|---|---|
| SAS-SV score, (m ± SD) | 33.81 ± 9.81 | 34.86 ± 10.20 | 32.69 ± 9.81 | 5.419 | <0.001 |
| PHQ-9 score, (m ± SD) | 7.75 ± 4.56 | 8.15 ± 4.42 | 7.51 ± 4.93 | 3.945 | 0.002 |
| GAD-7 score, (m ± SD) | 6.72 ± 4.33 | 7.11 ± 4.04 | 6.24 ± 4.69 | 4.537 | <0.001 |
| AIS-8 score, (m ± SD) | 8.39 ± 4.61 | 8.63 ± 4.54 | 7.91 ± 4.76 | 2.504 | 0.015 |
| Problematic smartphone use, n (%) | 953 (58.50) | 495 (62.82) | 458 (54.46) | 19.241 | <0.001 |
| Depression symptom, n (%) | 423 (25.97) | 236(29.95) | 187 (22.24) | 9.123 | 0.003 |
| Anxiety symptom, n (%) | 357 (21.92) | 198 (25.13) | 159 (18.91) | 19.728 | <0.001 |
| Insomnia symptoms, n (%) | 1189 (72.99) | 598 (75.89) | 591 (70.27) | 7.446 | 0.006 |
SAS-SV, Smartphone Addiction Scale-Short Version; PHQ-9, 9-item Patient Health Questionnaire; GAD-7, 7-item Generalized Anxiety Disorder Scale; AIS-8, 8-item Athens Insomnia Scale.
Correlations Between SAS-SV, PHQ-9, GAD-7, and AIS-8 Scores
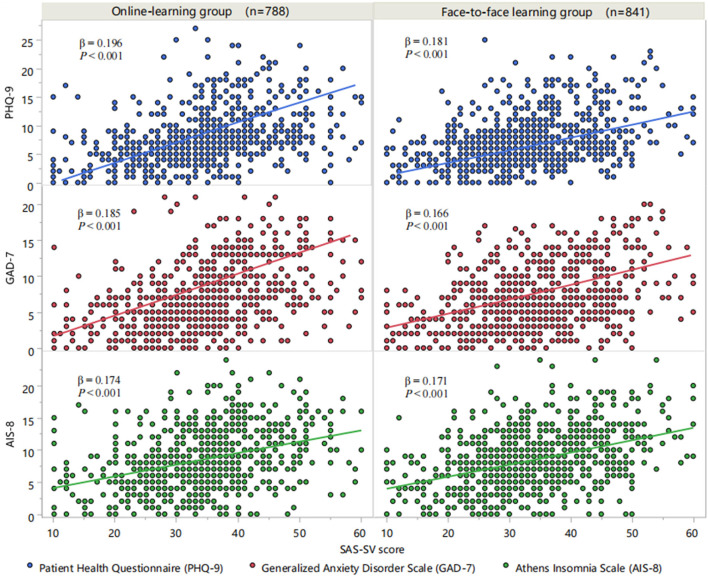
An exploratory factor analysis was performed on all 34 items in the SAS-SV, PHQ-9, GAD-7, and AIS-8, and five common factors with eigenvalues >1 were obtained. The first common factor explained 14.62% of the total variance which indicated that there was no common method bias in the current dataset. The association of the SAS-SV score with psychological measurements in the online learning group and face-to-face learning group was shown in Figure 1, respectively. As summarized in Table 2, the SAS-SV score (independent variable) and the PHQ-9, GAD-7, and AIS-8 scores (dependent variables) were included as continuous variables; education mode was a dichotomous variable. In Model 1, the SAS-SV score was significantly correlated with PHQ-9, GAD-7, and AIS-8 scores (Ps < 0.001). After adjusting for age, sex, grade, education level, residence, satisfaction, and exercise habits, statistical significance was also found in Model 3. To test the significance of multiplicative interaction of the SAV-SV score and education mode, we then added an interaction term (SAS-SV × education mode) to Model 2; the interaction term was statistically significant in the correlation of the SAS-SV score with the PHQ-9 score (P = 0.002) and GAD-7 score (P = 0.002), but not with the AIS-8 score (P = 0.426). The results were not substantially altered when covariates were adjusted in Model 4.
Figure 1.
Associations between SAS-SV and PHQ-9, GAD-7, and AIS-8 scores. SAS-SV, Smartphone Addiction Scale-Short Version; PHQ-9, 9-item Patient Health Questionnaire; GAD-7, 7-item Generalized Anxiety Disorder Scale; AIS-8, 8-item Athens Insomnia Scale.
Table 2.
Linear regression analysis of SAS-SV, PHQ-9, GAD-7, and AIS-8 scores.
| Dependent variable | Independent variable | Crude model 1 | Crude model 2 | Adjusted model 3 | Adjusted model 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | P-value | β | SE | P-value | β | SE | P-value | β | SE | P-value | ||
| PHQ-9 | SAS-SV | 0.187 | 0.013 | <0.001 | 0.196 | 0.016 | <0.001 | 0.158 | 0.013 | <0.001 | 0.195 | 0.017 | <0.001 |
| online learning group | – | – | – | 0.175 | 0.065 | 0.029 | – | – | – | 0.168 | 0.071 | 0.032 | |
| SAS-SV × education mode | – | – | – | −0.037 | 0.016 | 0.002 | – | – | – | −0.039 | 0.016 | 0.003 | |
| GAD-7 | SAS-SV | 0.179 | 0.012 | <0.001 | 0.206 | 0.015 | <0.001 | 0.162 | 0.012 | <0.001 | 0.203 | 0.015 | <0.001 |
| online learning group | – | – | – | 0.244 | 0.015 | 0.016 | – | – | – | 0.291 | 0.155 | 0.026 | |
| SAS-SV × education mode | – | – | – | −0.045 | 0.015 | 0.002 | – | – | – | −0.045 | 0.015 | 0.002 | |
| AIS-8 | SAS-SV | 0.172 | 0.014 | <0.001 | 0.181 | 0.017 | <0.001 | 0.163 | 0.014 | <0.001 | 0.184 | 0.017 | <0.001 |
| online learning group | – | – | – | 0.136 | 0.071 | 0.057 | – | – | – | 0.152 | 0.075 | 0.038 | |
| SAS-SV × education mode | – | – | – | −0.013 | 0.017 | 0.426 | – | – | – | −0.016 | 0.017 | 0.344 | |
SAS-SV, Smartphone Addiction Scale-Short Version; PHQ-9, 9-item Patient Health Questionnaire; GAD-7, 7-item Generalized Anxiety Disorder Scale; AIS-8, 8-item Athens Insomnia Scale; SE, standard error.
Crude Model 1: SAS-SV.
Crude Model 2: Model 1+ online learning group + SAS-SV × education mode.
Adjusted Model 3: Model 1+ age, sex, grade, education level, residence, satisfaction, and exercise habits.
Adjusted Model 4: Model 3+ online learning group + SAS-SV × education mode.
Stratified Analyses of Associations Between PSU and Psychological Symptoms
In the stratified logistic regression analyses, PSU (independent variable) and mental health symptoms (dependent variables) were included as dichotomous variables, and participants without PSU comprised the reference groups. As shown in Table 3, PSU was an independent influencing factor for depressive symptoms (AdjOR = 3.14, 95% CI = 2.26–4.37), anxiety symptoms (AdjOR = 3.73, 95% CI = 2.13–4.59), and insomnia symptoms (AdjOR = 2.96, 95% CI = 2.23–3.92), in both the crude and adjusted models. The multivariable adjusted OR of PSU for depressive symptoms in the online learning group was more pronounced than in the face-to-face learning group (OR = 4.66 vs. 2.33, P for interaction = 0.015). Similar results were found in the relationship between PSU and anxiety symptoms (OR = 6.05 vs. 2.94, P for interaction = 0.021). For the association between PSU and insomnia symptoms, no significant interaction effect was found (OR = 3.29 vs. 2.86, P for interaction = 0.589).
Table 3.
Stratified logistic regression analyses of PSU and mental health symptoms across education modes.
| Dependent variable | Subgroup | No. of participants | No. of symptoms | Prevalence | Crude ORsa | Adjusted ORsb | P for |
|---|---|---|---|---|---|---|---|
| (%) | (95% CI) | (95% CI) | interaction | ||||
| Depressive symptoms | Total sample | 1629 | 423 | 25.97 | |||
| PSU | 953 | 334 | 35.05 | 3.37(2.45-4.64) | 3.14(2.26–4.37) | 0.015 | |
| Non-PSU | 676 | 89 | 13.17 | 1 | 1 | ||
| Online group | 788 | 236 | 29.95 | ||||
| PSU | 495 | 205 | 41.41 | 4.31(2.64-5.67) | 4.66(2.83–6.75) | ||
| Non-PSU | 293 | 31 | 10.58 | 1 | 1 | ||
| Face-to-face group | 841 | 187 | 22.24 | ||||
| PSU | 458 | 129 | 28.17 | 2.39(2.38-4.85) | 2.33(2.31–4.82) | ||
| Non-PSU | 383 | 58 | 15.14 | 1 | 1 | ||
| Anxiety symptoms | Total sample | 1629 | 357 | 21.92 | |||
| PSU | 953 | 264 | 27.70 | 3.51(2.42-5.07) | 3.73(2.13–4.59) | 0.021 | |
| Non-PSU | 676 | 93 | 13.76 | 1 | |||
| Online group | 788 | 198 | 25.13 | ||||
| PSU | 495 | 163 | 32.93 | 5.67(3.46-9.09) | 6.05(3.49–9.67) | ||
| Non-PSU | 293 | 35 | 11.95 | 1 | 1 | ||
| Face-to-face group | 841 | 159 | 18.91 | ||||
| PSU | 458 | 101 | 22.05 | 3.09(2.04-4.67) | 2.94(1.93–4.49) | ||
| Non-PSU | 383 | 58 | 15.14 | 1 | 1 | ||
| Insomnia symptoms | Total sample | 1629 | 1189 | 72.99 | |||
| PSU | 953 | 761 | 79.85 | 2.97(2.27-3.88) | 2.96(2.23–3.92) | 0.589 | |
| Non-PSU | 676 | 428 | 63.31 | 1 | 1 | ||
| Online group | 788 | 598 | 75.89 | ||||
| PSU | 495 | 415 | 83.84 | 3.24(2.87-5.35) | 3.29(2.87–5.72) | ||
| Non-PSU | 293 | 183 | 62.46 | 1 | 1 | ||
| Face-to-face group | 841 | 591 | 70.27 | ||||
| PSU | 458 | 346 | 75.55 | 2.87(2.13-3.87) | 2.86(2.11–3.89) | ||
| Non-PSU | 383 | 245 | 63.97 | 1 | 1 |
PSU, problematic smartphone use; OR, odds ratio.
Non-adjusted model.
Adjusted for age, sex, grade, educational level, residence, satisfaction, and exercise habits.
Participants with no PSU comprised the reference groups.
Discussion
This study found significant correlations between online learning modes, smartphone addiction problems, and multiple mental health symptoms after the COVID-19 outbreak in a representative student sample in China. The high prevalence of PSU (58.5%) was comparable to that of previous studies conducted during the COVID-19 pandemic. According to a recent global survey, about 70% of Internet users around the world, especially the younger generation, were using smartphones or mobile phones more frequently as a result of the COVID-19 outbreak (13). Another cross-sectional study reported a PSU prevalence of 43.3% among an adult sample from Macao, China (43). In the current study, the prevalence of depressive, anxiety, and insomnia symptoms were 25.97, 21.92, and 72.99%, respectively. Similarly, in a recent study conducted in East China, 35.15, 36.32, and 17.24% of college students studying completely online at home during the COVID-19 pandemic reported symptoms of depression, anxiety, and stress, respectively (44). A recently published paper reported that after the COVID-19 pandemic, the estimated number of people with major depression increased from 193 million to 246 million globally, and the number of people with anxiety increased from 298 million to 374 million (45). A recent meta-analysis reported that the pooled prevalence of anxiety symptoms and of depressive symptoms in Chinese college students were 31 and 34%, respectively (46). These findings indicate that mental health disorders, especially sleep problems, remained serious among university students during the “new normal” of the COVID-19 pandemic.
The prevalence of PSU (62.82% vs. 54.46%) was higher in the online learning group than in the traditional face-to-face learning group, as were symptoms of depression (29.95% vs. 22.24%), anxiety (25.13% vs. 18.91%), and insomnia (75.89% vs. 70.27%). The significant differences between the online and face-to-face learning groups could be explained in several ways. First, online learning is a model that uses electronic technology and media to provide instructional teaching support (11). As a direct result, students increase the frequency of smartphone use and access, which in turn increases the potential risk of overuse. Many hours of online study can also lead to physical symptoms, which are closely linked to psychological problems (47). Second, college students who study in a more isolated online environment experience more study pressure and confusion than students who study intensively in the classroom. Compared to centralized learning, this model of learning lacks opportunities for interaction, such as face-to-face cooperative learning and on-site discussion; this may reduce social and peer support, and thus augment symptoms of depression and anxiety. In another study, college students learning remotely were found to be more isolated and to have a lower level of self-confidence (48). Third, during the transition to online learning, student satisfaction may decrease due to problems such as disorganized teaching activities and imperfect teaching platforms. Satisfaction with the teaching environment and quality may also be associated with university students' mental health problems. Similar to the present study, Bolatov found an increase trend of depression, anxiety, and burnout symptoms in Kazakhstan medical students after the transition from traditional learning to online learning (49). Another Polish study also showed that a completely online learning mode had a negative impact on the mental health of college students during the COVID-19 pandemic (50). In turn, a longitudinal study from the US found the opposite with a gradual alleviation in COVID-19-related stress and sleep problems of college students when transitioning to online learning mode (41). These inconsistent results may be explained by the radically different epidemic situations and lockdown measures between the US and China, which could have resulted in different attitudes toward and participation in online learning in college students.
The multiple regression analysis showed that subjects with PSU were more likely to report depressive symptoms (AdjOR = 3.14, 95% CI = 2.26–4.37), anxiety symptoms (AdjOR = 3.73, 95% CI = 2.13–4.59), and insomnia symptoms (AdjOR = 2.96, 95% CI = 2.23–3.92). These findings are consistent with previous studies in adolescents (51, 52) and college students (53, 54). A cross-sectional study with adult US participants found a positive relationship between the time spent online searching for information about COVID-19 and GAD-7 scores (55). In Hao et al.'s study, academic burnout, anxiety, and resilience were significantly associated with PSU in Chinese undergraduate students during the pandemic (56). Furthermore, we found that the association of PSU with depressive symptoms (OR = 4.66 vs. 2.33, P for interaction = 0.015) and with anxiety symptoms (OR = 6.05 vs. 2.94, P for interaction = 0.021) was more pronounced in the online learning group. This unique interaction further strengthened the potential negative effect of the online education mode on mental health status during the COVID-19 epidemic. This finding suggested that college students who participate in online learning might be more prone to depression or anxiety symptoms when they developed smartphone addiction problems. The moderating role of education mode on PSU and psychological problems has not been previously reported; this result is therefore of great value for the future development of targeted interventions and psychological counseling for specific student groups. The I-PACE model and CIUT could support the associations between PSU with depression and anxiety. Namely, the outbreak of COVID-19 and the sudden change in learning patterns can be regarded as an abnormal change in the environment; thus, students who are in a negative or worried mood are more inclined to seek mental compensation from mobile phones or the Internet. In addition, excessive use of smartphones is conducive to addiction to the virtual world, which can result in social phobia and loneliness, and can trigger or aggravate depression (57). We argue that the effects of smartphones on mental health need to be vigilantly monitored in students learning online. Timely educational monitoring and targeted psychological interventions are necessary to maintain the new normal of distance learning in the post-COVID-19 era. For example, occupational psychological therapies have shown potential effects in alleviating psychological distress and sleep problems (58). Besides, some clinical mechanisms are beneficial to support the associations of psychological disorders and PSU. Inhibition of melatonin secretion caused by nocturnal light stimulation is a recognized physiological pathway that leads to sleep deprivation. Radio frequency electromagnetic fields generated during the use of mobile phones can affect the normal blood flow of the brain and metabolic function of the body, thus exacerbating emotional disorders and inhibiting slow-wave sleep (59).
Limitations
Several limitations of the current study should be acknowledged. First, no causal inferences can be made due to the study's cross-sectional design. Longitudinal research should be conducted in the future. Second, although the web-based survey was the best option to reach subjects during the COVID-19 epidemic period, the response bias was inevitable. Third, smartphone addiction and mental health-related information were collected from self-report questionnaires, which were less reliable than clinical diagnoses. Our future direction is the application of objective measurements, as some previous studies have done (25, 60).
Conclusions
Our study provides evidence that Chinese university students have serious smartphone addiction problems that are associated with depressive, anxiety, and insomnia symptoms. Online learning was found to exacerbate PSU and mental health problems. This suggests that attention should be paid not only to the organization of teaching activities, but also to students' mental health status.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Beijing Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CZ and HY proposed the concept and design. CZ and JC analyzed and interpreted the data and wrote the manuscript. JH, YL, and HY drafted and edited the manuscript. CZ, JC, and HY supervised the study and obtained funding. All authors read and approved the final version of the manuscript.
Funding
This study was supported by the National Key R&D Program of China (2020YFC2002700); the Education and Teaching Research Project of Peking University Health Science Center (2020YB42), and the Fundamental Research Funds for the Central University (3332021077). We sincerely thank all investigators and students who participated in this study, for their joint effort and cooperation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.881074/full#supplementary-material
References
- 1.Smith C A. Covid-19: healthcare students face unique mental health challenges. BMJ. (2020) 369:m2491. 10.1136/bmj.m2491 [DOI] [PubMed] [Google Scholar]
- 2.Wang C, Han J. Will the COVID-19 pandemic end with the Delta and Omicron variants? Environ Chem Lett. (2022) 15:1–11. 10.1007/s10311-021-01369-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee Y, Lui L M W, Chen-Li D, Liao Y, Mansur R B, Brietzke E, et al. Government response moderates the mental health impact of COVID-19: A systematic review and meta-analysis of depression outcomes across countries. J Affect Disord. (2021) 290:364–77. 10.1016/j.jad.2021.04.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Camargo CP, Tempski PZ, Busnardo FF, Martins MA, Gemperli R. Online learning and COVID-19: a meta-synthesis analysis. Clinics (Sáo Paulo). (2020) 75:e2286. 10.6061/clinics/2020/e2286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalil R, Mansour A E, Fadda WA, Almisnid K, Aldamegh M, Al-Nafeesah A, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students' perspectives. BMC Med Educ. (2020) 20:285. 10.1186/s12909-020-02208-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen IH, Jeffrey HG, Lee ZH, Fu QL. Formative assessment with interactive whiteboards: A one-year longitudinal study of primary students' mathematical performance. Comput Educ. (2020) 150:103833. 10.1016/j.compedu.2020.103833 [DOI] [Google Scholar]
- 7.Guven Ozdemir N, Sonmez M. The relationship between nursing students' technology addiction levels and attitudes toward e-learning during the COVID-19 pandemic: a cross-sectional study. Perspect Psychiatr Care. (2021) 57:1442–8. 10.1111/ppc.12710 [DOI] [PubMed] [Google Scholar]
- 8.Zis P, Artemiadis A, Bargiotas P, Nteveros A, Hadjigeorgiou G M. Medical Studies during the COVID-19 Pandemic: The Impact of Digital Learning on Medical Students' Burnout and Mental Health. Int J Environ Res Public Health. (2021) 18:349. 10.3390/ijerph18010349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen CY, Chen IH, Hou WL, Potenza MN, O'Brien KS, Lin CY, et al. The relationship between children's problematic internet-related behaviors and psychological distress during the onset of the COVID-19 pandemic: a longitudinal study. J Addict Med. (2022) 16:e73–80. 10.1097/ADM.0000000000000845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen IH, Chen CY, Pakpour AH, Griffiths MD, Lin CY. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. (2020) 59:1099–102.e1. 10.1016/j.jaac.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rajab MH, Gazal AM, Alkattan K. Challenges to online medical education during the COVID-19 pandemic. Cureus. (2020) 12:e8966. 10.7759/cureus.8966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, et al. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J Affect Disord. (2020) 275:112–8. 10.1016/j.jad.2020.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caponnetto P, Inguscio L, Valeri S, Maglia M, Polosa R, Lai C, et al. Smartphone addiction across the lifetime during Italian lockdown for COVID-19. J Addict Dis. (2021) 39:441–9. 10.1080/10550887.2021.1889751 [DOI] [PubMed] [Google Scholar]
- 14.Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. (2019) 24:1666538. 10.1080/10872981.2019.1666538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasan N, Bao Y. Impact of “e-Learning crack-up” perception on psychological distress among college students during COVID-19 pandemic: A mediating role of “fear of academic year loss”. Child Youth Serv Rev. (2020) 118:105355. 10.1016/j.childyouth.2020.105355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iyengar K, Upadhyaya GK, Vaishya R, Jain V. COVID-19 and applications of smartphone technology in the current pandemic. Diabetes Metab Syndr. (2020) 14:733–7. 10.1016/j.dsx.2020.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ratan ZA, Zaman SB, Islam SMS, Hosseinzadeh H. Smartphone overuse: a hidden crisis in COVID-19. Health Policy Technol. (2021) 10:21–2. 10.1016/j.hlpt.2021.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Olashore A, Akanni O, Fela-Thomas A, Khutsafalo K. The psychological impact of COVID-19 on health-care workers in African Countries: A systematic review. Asian J Soc Health Behav. (2021) 4:85–97. 10.4103/shb.shb_32_21 [DOI] [Google Scholar]
- 19.Rajabimajd N, Alimoradi Z, Griffiths M. Impact of COVID-19-related fear and anxiety on job attributes: A systematic review. Asian J Soc Health Behav. (2021) 5:51–5. 10.4103/shb.shb_24_21 [DOI] [Google Scholar]
- 20.Luo X, Estill J, Wang Q, Lv M, Liu Y, Liu E, et al. The psychological impact of quarantine on coronavirus disease 2019 (COVID-19). Psychiatry Res. (2020) 291:113193. 10.1016/j.psychres.2020.113193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goethals L, Barth N, Guyot J, Hupin D, Celarier T, Bongue B. Impact of home quarantine on physical activity among older adults living at home during the COVID-19 pandemic: qualitative interview study. JMIR Aging. (2020) 3:e19007. 10.2196/19007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mattioli AV, Sciomer S, Cocchi C, Maffei S, Gallina S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr Metab Cardiovasc Dis. (2020) 30:1409–17. 10.1016/j.numecd.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fu W, Yan S, Zong Q, Anderson-Luxford D, Song X, Lv Z, et al. Mental health of college students during the COVID-19 epidemic in China. J Affect Disord. (2021) 280:7–10. 10.1016/j.jad.2020.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bilal, Latif F, Bashir M F, Komal B, Tan D. Role of electronic media in mitigating the psychological impacts of novel coronavirus (COVID-19). Psychiatry Res. (2020) 289:113041. 10.1016/j.psychres.2020.113041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huckins J F., daSilva A W, Wang W, Hedlund E, Rogers C, Nepal S K, et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. J Med Internet Res. (2020) 22:e20185. 10.2196/20185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. (2020) 29:e181. 10.1017/S2045796020000931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alimoradi Z, Broström A, Tsang HWH, Griffiths MD, Haghayegh S, Ohayon MM, et al. Sleep problems during COVID-19 pandemic and its' association to psychological distress: a systematic review and meta-analysis. EClinicalMedicine. (2021) 36:100916. 10.1016/j.eclinm.2021.100916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang C, Zeng P, Tan J, Sun S, Zhao M, Cui J, et al. Relationship of problematic smartphone use, sleep quality, and daytime fatigue among quarantined medical students during the COVID-19 pandemic. Front Psychiatry. (2021) 12:755059. 10.3389/fpsyt.2021.755059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park N, Lee H. Social implications of smartphone use: Korean college students' smartphone use and psychological well-being. Cyberpsychol Behav Soc Netw. (2012) 15:491–7. 10.1089/cyber.2011.0580 [DOI] [PubMed] [Google Scholar]
- 30.Jhone JH, Song IH, Lee MS, Yoon JY, Bhang SY. Is the I-PACE (Interaction of Person-Affect-Cognition-Execution) model valid in South Korea? The effects of adverse childhood experiences (ACEs) on internet gaming disorder and the mediating effect of stress on adolescents. J Behav Addict. (2021). 10.1556/2006.2021.00081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arrivillaga C, Rey L, Extremera N. Psychological distress, rumination and problematic smartphone use among Spanish adolescents: An emotional intelligence-based conditional process analysis. J Affect Disord. (2022) 296:1–8. 10.1016/j.jad.2021.09.021 [DOI] [PubMed] [Google Scholar]
- 32.Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. (2020) 10:e042378. 10.1136/bmjopen-2020-042378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. (2011) 17:268–74. 10.1111/j.1365-2753.2010.01434.x [DOI] [PubMed] [Google Scholar]
- 34.Kwon M, Kim D J, Cho H, Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS One. (2013) 8:e83558. 10.1371/journal.pone.0083558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luk T T, Wang M P, Shen C, Wan A, Chau P H, Oliffe J, et al. Short version of the smartphone addiction scale in Chinese adults: Psychometric properties, sociodemographic, and health behavioral correlates. J Behav Addict. (2018) 7:1157–65. 10.1556/2006.7.2018.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ye X, Shu HL, Feng X, Xia DM, Wang ZQ, Mi WY, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire-9 (C-PHQ-9) in patients with psoriasis: a cross-sectional study. BMJ Open. (2020) 10:e033211. 10.1136/bmjopen-2019-033211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. 10.1136/bmj.l1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 39.Kujanpää T, Ylisaukko-Oja T, Jokelainen J, Hirsikangas S, Kanste O, Kyngäs H, et al. Prevalence of anxiety disorders among Finnish primary care high utilizers and validation of Finnish translation of GAD-7 and GAD-2 screening tools. Scand J Prim Health Care. (2014) 32:78–83. 10.3109/02813432.2014.920597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. (2000) 48:555–60. 10.1016/S0022-3999(00)00095-7 [DOI] [PubMed] [Google Scholar]
- 41.Gusman MS, Grimm KJ, Cohen AB, Doane LD. Stress and sleep across the onset of the novel coronavirus disease 2019 pandemic: impact of distance learning on US college students' health trajectories. Sleep. (2021) 44:zsab193. 10.1093/sleep/zsab193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. (2003) 88:879–903. 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- 43.Zhang MX, Chen JH, Tong KK, Yu EW, Wu AMS. Problematic Smartphone Use during the COVID-19 Pandemic: Its Association with Pandemic-Related and Generalized Beliefs. Int J Environ Res Public Health. (2021) 18:5724. 10.3390/ijerph18115724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chang WW, Zhang L, Wen LY, Su H, Jin YL. Association Between Online Self-Directed Learning Ability and Negative Emotions Among College Students During the COVID-19 Pandemic: A Cross-Sectional Study in Anhui Province, East China. Front Psychol. (2021) 12:720911. 10.3389/fpsyg.2021.720911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Collaborators C-MD. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chang JJ, Ji Y, Li YH, Pan HF, Su PY. Prevalence of anxiety symptom and depressive symptom among college students during COVID-19 pandemic: a meta-analysis. J Affect Disord. (2021) 292:242–54. 10.1016/j.jad.2021.05.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee M, Hong Y, Lee S, Won J, Yang J, Park S, et al. The effects of smartphone use on upper extremity muscle activity and pain threshold. J Phys Ther Sci. (2015) 27:1743–5. 10.1589/jpts.27.1743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McCutcheon K, Lohan M, Traynor M, Martin D. A systematic review evaluating the impact of online or blended learning vs face-to-face learning of clinical skills in undergraduate nurse education. J Adv Nurs. (2015) 71:255–70. 10.1111/jan.12509 [DOI] [PubMed] [Google Scholar]
- 49.Bolatov AK, Seisembekov TZ, Askarova AZ, Baikanova RK, Smailova DS, Fabbro E. Online-Learning due to COVID-19 Improved Mental Health Among Medical Students. Med Sci Educ. (2020) 31:1–10. 10.1007/s40670-020-01165-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drelich-Zbroja A, Jamroz-Wiśniewska A, Kuczyńska M, Zbroja M, Cyranka W, Drelich K, et al. The impact of study mode (online vs. hybrid) on early symptoms of depression and coping strategies among university students in poland in time of covid-19 pandemic-preliminary. Study Brain Sci. (2021) 11:1–18. 10.3390/brainsci11121578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Augner C, Hacker GW. Associations between problematic mobile phone use and psychological parameters in young adults. Int J Public Health. (2012) 57:437–41. 10.1007/s00038-011-0234-z [DOI] [PubMed] [Google Scholar]
- 52.Ha JH, Chin B, Park DH, Ryu SH, Yu J. Characteristics of excessive cellular phone use in Korean adolescents. Cyberpsychol Behav. (2008) 11:783–4. 10.1089/cpb.2008.0096 [DOI] [PubMed] [Google Scholar]
- 53.Demirci K, Akgönül M, Akpinar A. Relationship of smartphone use severity with sleep quality, depression, and anxiety in university students. J Behav Addict. (2015) 4:85–92. 10.1556/2006.4.2015.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lei LY, Ismail MA, Mohammad JA, Yusoff MSB. The relationship of smartphone addiction with psychological distress and neuroticism among university medical students. BMC Psychol. (2020) 8:97. 10.1186/s40359-020-00466-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Singh P, Cumberland WG, Ugarte D, Bruckner TA, Young SD. Association Between Generalized Anxiety Disorder Scores and Online Activity Among US Adults During the COVID-19 Pandemic: Cross-Sectional Analysis. J Med Internet Res. (2020) 22:e21490. 10.2196/21490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hao Z, Jin L, Huang J, Lyu R, Cui Q. Academic burnout and problematic smartphone use during the covid-19 pandemic: the effects of anxiety and resilience. Front Psychiatry. (2021) 12:725740. 10.3389/fpsyt.2021.725740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yen C F, Tang T C, Yen J Y, Lin H C, Huang C F, Liu S C, et al. Symptoms of problematic cellular phone use, functional impairment and its association with depression among adolescents in Southern Taiwan. J Adolesc. (2009) 32:863–73. 10.1016/j.adolescence.2008.10.006 [DOI] [PubMed] [Google Scholar]
- 58.Fan C, Drumheller K. Using occupational therapy process addressing sleep-related problems in neurorehabilitation: A cross-sectional modeling study. Asian J Soc Health Behav. (2021) 4:149–55. [Google Scholar]
- 59.Kwon MS, Vorobyev V, Kännälä S, Laine M, Rinne JO, Toivonen T, et al. GSM mobile phone radiation suppresses brain glucose metabolism. J Cereb Blood Flow Metab. (2011) 31:2293–301. 10.1038/jcbfm.2011.128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kwok C, Leung PY, Poon KY, Fung X. The effects of internet gaming and social media use on physical activity, sleep, quality of life, and academic performance among university students in Hong Kong: A preliminary study. Asian J Soc Health Behav. (2021) 4:36–44. 10.4103/shb.shb_81_20 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.