Summary
Background
Infertility and intimate partner violence (IPV) are of serious concern globally, yet the prevalence of IPV against infertile women has not been quantified at the regional or global level. We aimed to estimate the prevalence of IPV against infertile women and its variation in low-income and middle-income countries (LMICs).
Methods
We did a systematic literature search of 11 databases for articles published between database inception and Sept 30, 2021, and performed meta-analyses to estimate the pooled prevalence and 95% CI of IPV against infertile women in LMICs. We used subgroup analyses and meta-regressions to explore variation in the prevalence by study period (2010 and before vs after 2010), study region (Africa, west Asia, south Asia, and east Asia), type of infertility (primary or secondary), risk of bias (high, moderate, or low), sample size (continuous variable), and measuring tools (the modified Abuse Assessment Screen, the WHO Violence Against Women instrument, or the revised Conflict Tactics Scales). This study is registered with PROSPERO, CRD42021248448.
Findings
Of 2661 references identified (2637 via database searches and 24 via secondary searches), 120 full-text articles were reviewed, and we identified 30 relevant studies conducted in nine LMICs between 2000 and 2019. 25 studies met the inclusion criteria for meta-analysis, with a total sample size of 7164 participants. The 12-month prevalence of IPV among infertile women was 36·0% (95% CI 20·4–55·2), compared with a lifetime prevalence of 47·2% (31·7–63·3). The most common type of IPV was psychological violence, with a prevalence of 24·6% (11·3–45·6) over 12 months and 51·5% (38·8–64·0) over a lifetime (slightly higher than the pooled overall rate due to different data sources), respectively; followed by physical violence (11·9% [5·2–25·1] and 20·2% [12·1–31·7]); sexual violence (8·7% [2·6–25·0] and 11·5% [6·1–20·7]); and economic coercion (2·6% [0·4–13·7] and 9·8% [5·7–16·5]). Significant variations of lifetime prevalence estimates were presented by study period (R2=39·46%), region (R2=50·95%), and measuring tools (R2=54·27%).
Interpretation
A high prevalence of IPV against infertile women is evident despite heterogeneity across studies. IPV screening, counselling, and structural interventions should be tailored to address this urgent issue at multiple levels of society.
Funding
China Medical Board and WHO.
Introduction
Infertility, defined as the inability to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse, has significant implications for the health and wellbeing of couples of reproductive age.1 Globally, the prevalence of infertility varies greatly due to its varying definition and demographical differences, ranging anywhere from 3% to 30%.2, 3, 4 Besides the medical advances in the treatment of infertility as a pathological condition, concerted actions should be taken to address the consequences of infertility on other aspects of human wellbeing, prominent among them violence against infertile women.
Intimate partner violence (IPV) is the most common form of violence against women,5 defined as any form of violence by a current or former male intimate partner within a union, and can present as physical, psychological or emotional, or sexual violence, or as economic coercion and controlling behaviours.5, 6, 7 The most recent estimate from WHO indicates that, worldwide, 27% of ever-married or ever-partnered women aged 15–49 years have experienced physical or sexual violence (or both) committed by intimate partners at least once in their lifetime, whereas the prevalence over a 12-month period was 13%.5
Published evidence, mostly from low-income and middle-income countries (LMICs), has suggested that infertile women might have a higher risk of IPV than that of the general population, but prevalence estimates vary substantially between studies, even within the same countries. For example, studies have reported past 12-month prevalence rates as follows: 35·9% in Nigeria,8 61·8% in Iran,9 30·4% in Nepal,10 15·0–87·8% in Turkey,11, 12 and 10·5–26·9% in China.13, 14 Stellar and colleagues attempted to establish the relationship between infertility and an increased risk of experiencing IPV in LMICs, but ultimately produced a narrative report only.15 A few reviews of domestic violence among infertile women that included both IPV and the violence perpetrated by other family members, none of which distinguished IPV from domestic violence,16, 17, 18 synthesised prevalence estimates measured over different periods of time (in the past 12 months or lifetime),17, 18 or restricted their results to a narrative report.16
Research in context.
Evidence before this study
Infertility and intimate partner violence (IPV) threaten women's sexual and reproductive health. We searched 11 databases using a comprehensive search strategy to identify studies on IPV among infertile women published between database inception and Sept 30, 2021. Full details of our literature search are given in the Methods section. One previous review attempted to establish a relationship between infertility and IPV, but produced a narrative report only. The prevalence of IPV against infertile women at the regional or global levels remains unknown, given the absence of a systematic review and meta-analysis on this topic.
Added value of this study
In this systematic review and meta-analysis, we estimated the pooled prevalence of IPV against infertile women in low-income and middle-income countries (LMICs). Our findings suggest that at least one in three infertile women suffer from IPV over a 12-month period and about one in two over their lifetime. Psychological violence is the most common form of IPV, followed by physical violence, sexual violence, and economic coercion. Infertile women were more likely to suffer from physical violence and sexual violence over their lifetime than were fertile women. The findings of the existing studies indicate significant heterogeneity in prevalence estimates, and evidence is restricted to a few countries.
Implications of all the available evidence
IPV against infertile women is highly prevalent but has been understudied worldwide. Further research should prioritise the establishment of a consistent approach in data definition and data collection, as well as longitudinal studies to explore the bidirectional association between IPV and infertility. More high-quality studies and updated data will enable policy makers to better address the factors that lead to infertile women's disproportionate experiences with IPV in various contexts.
Given that both IPV and infertility are major health concerns, quantifying the magnitude and characteristics of IPV against infertile women is necessary to identify research priorities and practical interventions. Therefore, we aimed to quantify the prevalence of IPV against infertile women in LMICs and examine the variations among studies. The findings of this study will provide evidence to support the development of priority actions in future research and policies.
Methods
Search strategy and selection criteria
We developed a search strategy to identify relevant studies in consultation with a health sciences librarian (QG). First, 11 online academic databases were searched, with no language restrictions, for papers published between database inception and Sept 30, 2021: PubMed, PsycINFO, CINAHL Plus, Embase, MEDLINE, Web of Science, ProQuest Dissertations & Theses Global, ProQuest International Bibliography of the Social Sciences, Chinese Wanfang Database, Chinese CNKI Database, and China Biology Medicine Database. Search terms were a combination of free text and controlled vocabulary (ie, MeSH terms) for each database (appendix 2 pp 1–5), including: “domestic violence”, “domestic abuse”, “intimate partner violence”, “marital violence”, “family abuse”, “spousal violence”, “maltreatment”, “mistreatment”, “infertility”, “infertile”, “sterile”, “infecundity”, and “childlessness”.
Second, we removed duplicates from the list of literature retrieved in the first step using Endnote 20.0 software (Clarivate, PA, USA). We performed a secondary search for grey literature in Google Scholar and WHO Global Index Medicus, and by checking the reference lists of identified relevant studies.
Third, two reviewers (YF and YW) screened the literature independently in two stages: title and abstract screening followed by full-text retrieval and screening using our eligibility criteria. Disagreements were resolved through discussions between the two reviewers, or with the help of a third reviewer (JQ). The studies confirmed as relevant by consensus were included. Inclusion criteria were original studies that reported the prevalence of IPV against infertile women, full-text access in the electronic library databases of Harvard University and Peking University, and written in English or Chinese. We excluded studies that were irrelevant to IPV or infertility; editorials, commentaries, book or book chapters, reviews, conference papers, abstracts only, or brief communications; studies that used qualitative methods only or interventional research; studies that were not conducted in LMICs; studies that did not distinguish IPV from domestic violence, or did not distinguish infertility from childlessness or having no sons; and studies that did not report the prevalence of IPV in the infertile group or study period. If several publications used the same dataset, the publication that provided the most data was selected.
This study is registered with PROSPERO, CRD42021248448, and followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (appendix 2 pp 6–8).19
Data extraction and risk of bias assessment
The two reviewers (YF and YW) extracted and cross-checked data in each relevant study, including the characteristics of study participants, study settings, instruments for assessing IPV, and prevalence estimates of IPV and its subtypes. In parallel, the two reviewers assessed the relevant studies using the 10-item Hoy risk of bias tool (appendix 2 p 9), designed for prevalence studies.20 Each item was rated on a dichotomous scale, with 1 indicating low risk of bias and 0 indicating high risk of bias. An overall score was calculated for each study as the mean score of the two reviewers, ranging from 0 to 10, with a score of at least 9 indicating a low risk of bias, 7–8 indicating a moderate risk, and less than 7 indicating a high risk. We calculated inter-rater reliability using the kappa coefficient for each item, and the Spearman's rank correlation coefficient for the summed score of each study (appendix 2 pp 10–11).
Data analysis
We performed meta-analyses to synthesise the prevalence of IPV against infertile women and its subtypes: psychological violence, physical violence, sexual violence, and economic coercion. We excluded studies that only reported the prevalence in scores rather than in rates, and studies that did not report the prevalence in the past 12 months or lifetime. We calculated prevalence rates over the past 12 months or lifetime from raw proportions or percentages reported in the selected studies. If a study reported two or more violence acts separately in a violence subtype (such as verbal, ridicule, and threat of divorce in psychological violence or beaten and hurt in physical violence), we used the maximum prevalence value of the violent act when performing meta-analysis, although this approach risks underestimating the actual prevalence.
To consider variations in the included studies in terms of study participants and instruments for assessing IPV, we used a random-effects model (DerSimonian and Laird method) to calculate pooled estimates and the 95% CI. For studies that reported IPV prevalence in both infertile and fertile women, we also performed random-effects models to calculate the pooled odds ratio (OR) and 95% CI between the two groups. Higgins’ I2 statistic and Q test were used to detect heterogeneity across studies. An I2 value greater than 50% or a p value of less than 0·05 indicated significant heterogeneity.21 We used Egger's test and funnel plots to assess potential publication bias, for which p<0·1 was regarded as significant.21
We used subgroup analyses and univariate meta-regressions to explore the prevalence variation across studies. Subgroup analyses were categorised by study period (2010 and before vs after 2010), study region, type of infertility (primary or secondary), and the risk of bias (high, moderate, or low). For study region, the initial categories were set as Africa, Asia, central and South America, and Europe; however, we adapted the final categories to Africa (Nigeria, Egypt, and Rwanda), west Asia (Turkey and Iran), south Asia (India, Pakistan, and Nepal), and east Asia (China), according to the geographical distribution of relevant studies retrieved from our literature search. Primary infertility was defined as the absence of livebirth or clinical pregnancy for women in a union; secondary infertility was defined as the absence of livebirth or clinical pregnancy for women in a union since their last livebirth or clinical pregnancy.3
In univariate meta-regressions, the dependent variable was the IPV prevalence and the independent variables were study period (dummy variable: 2010 and before), study region (dummy variable: Africa), type of infertility (dummy variable: primary), risk of bias (dummy variable: high), or sample size (defined as a continuous variable). We used a random-effects meta-regression model with restricted maximum likelihood. The proportion of variance of prevalence estimates explained by any meta-regression model was estimated via the R2 statistic.22
To further explore the variation of prevalence rates measured by different tools, we also performed a subgroup analysis and univariate meta-regression of the lifetime overall prevalence rates across three commonly used tools—the modified Abuse Assessment Screen,23 the WHO Violence Against Women instrument,24 and the revised Conflict Tactics Scales8, 9—which were selected once the included studies were determined.
All analyses were done using R software (version 4.1.2; Bell Laboratories, Madison, WI, USA), and all statistical tests were two-sided.
Role of the funding source
The funders of the study played no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
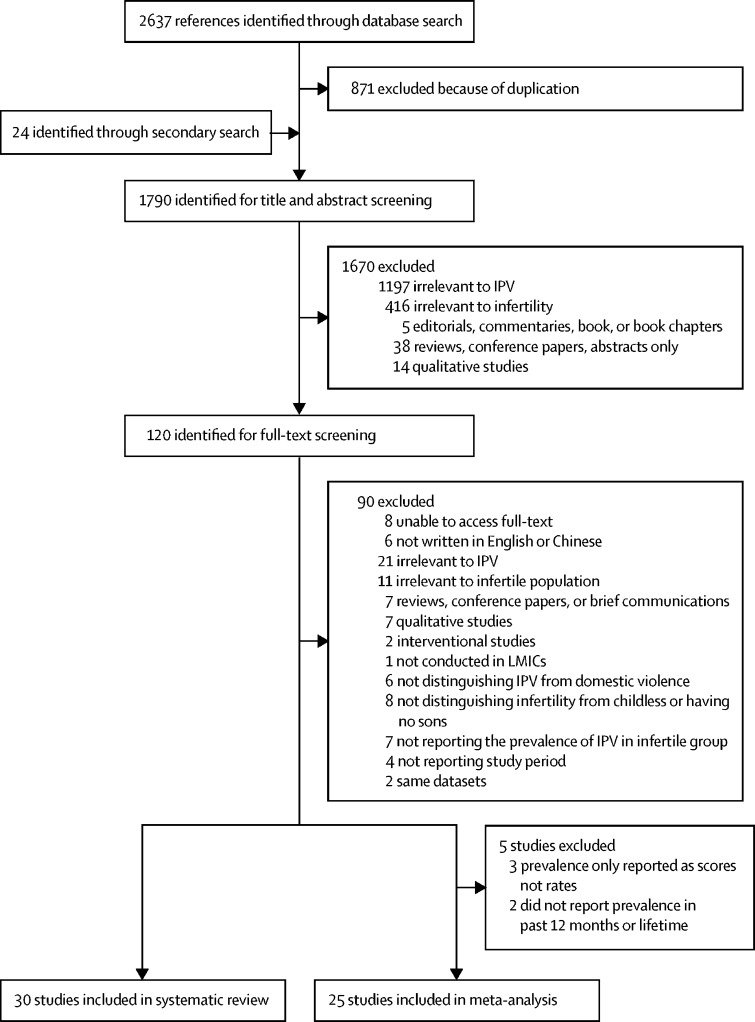
Of the 2661 references identified (2637 via database searches and 24 via secondary searches), 120 full-text articles were reviewed, and 30 relevant studies8, 9, 10, 11, 12, 13, 14, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47 were identified as eligible for systematic review (figure 1). Table 1 describes the study setting, characteristics of study participants, and the tools used to assess IPV in the 30 relevant studies (8308 participants). These studies were conducted between 2000 and 2019, with sample sizes ranging from 30 to 774, including eight from Turkey,11, 12, 27, 33, 37, 40, 43, 44 seven from Iran,9, 31, 34, 35, 39, 45, 46 three from Nigeria,8, 29, 30 three from Egypt,38, 41, 47 three from India,32, 36, 42 three from China,13, 14, 25 one from Rwanda,28 one from Pakistan,26 and one from Nepal.10 Most studies (26 of 30) were hospital-based or clinic-based surveys. Three12, 13, 14 were conducted in family planning centres and one28 was a community-based survey.
Figure 1.
Study profile
IPV against women is defined as any form of violence by a current or former male intimate partner within a union, whereas domestic violence against infertile women includes both IPV and the violence perpetrated by other family members. IPV=intimate partner violence. LMICs=low-income and middle-income countries.
Table 1.
Characteristics of studies included in the systematic review and meta-analysis
|
Study characteristics |
Prevalence of IPV |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Country | Setting | Assessment tool | Sample size | Type of infertility | Duration of violence | Overall | Psychological | Physical | Sexual | Economic | Risk of bias | |
| Leung et al, 200525 | 2000–01 | China | Hospital or clinic based | Modified Abuse Assessment Screen | 500* | Primary or secondary | Lifetime | 1·8% | .. | .. | .. | .. | High |
| Sami and Ali, 200626 | 2003 | Pakistan | Hospital or clinic based | Researcher-made questionnaire | 400 | Secondary | Lifetime | .. | Blame for infertility: 38·2%; threat of divorce: 7·8% | 9·0% | .. | .. | High |
| Li et al, 200513 | 2004 | China | Family planning centre | Researcher-made questionnaire | 687 | Primary | Past 12 months | 10·5% | 3·2% | 5·1% | 1·0% | 1·2% | Low |
| Guo et al, 200614 | 2004 | China | Family planning centre | Researcher-made questionnaire | 490 | Primary | Past 12 months | 26·9% | 17·6% | 22·7% | 2·7% | 4·3% | Low |
| Yildizhan et al, 200927 | 2007–08 | Turkey | Hospital or clinic based | Modified Abuse Assessment Screen | 122 | Primary (Female factor) | Lifetime | 33·6% | Verbal: 21·3%; ridicule: 14·8%; threat of divorce: 29·5% | 10·7% | 2·5% | 9·8% | High |
| Dhont et al, 201128 | 2007–09 | Rwanda | Community based | Researcher-made questionnaire | 312* | Primary or secondary | Lifetime | .. | Threat: 17·3%; chased: 26·9% | Beaten: 23·4%; hurt: 14·1% | 11·9% | .. | Low |
| Omoaregba et al, 201129 | 2008 | Nigeria | Hospital or clinic based | Researcher-made questionnaire | 100* | Primary or secondary | Lifetime | Verbal and physical: 35·0% | .. | .. | .. | .. | High |
| Edirne et al, 201012 | 2009 | Turkey | Family planning centre | Researcher-made questionnaire | 82 | Primary or secondary | Past 12 months | 87·8% | .. | .. | .. | .. | High |
| Ardabily et al, 20119 | 2009–10 | Iran | Hospital or clinic based | Revised Conflict Tactics Scale | 400 | Primary (Female factor) | Past 12 months | 61·8% | 33·8% | 20·0% | 8·0% | .. | High |
| Aduloju et al, 201530 | 2012–13 | Nigeria | Hospital or clinic based | Modified Abuse Assessment Screen | 170 | Primary or secondary | Lifetime | 31·2% | .. | .. | .. | .. | High |
| Farzadi et al, 201431 | 2013 | Iran | Hospital or clinic based | Researcher-made questionnaire | 200 | Primary or secondary | Past 12 months | .. | 82·0% | 45·0% | 54·0% | .. | High |
| Iliyasu et al, 20168 | 2013 | Nigeria | Hospital or clinic based | Revised Conflict Tactics Scale | 373 | Primary or secondary | Past 12 months | 35·9% | Non-verbal 33·8%; verbal: 12·6% | 6·7% | 29·8% | 23·9% | Low |
| Sahin et al, 201811 | 2013 | Turkey | Hospital or clinic based | Researcher-made questionnaire | 774 | Primary or secondary | Past 12 months | 15·0% | Non-verbal 12·5%; verbal: 2·5% | 2·5% | 4·9% | 0·0% | Moderate |
| Satheesan and Satyaranayana, 201832 | 2013–14 | India | Hospital or clinic based | Domestic Violence Questionnaire | 30 | Primary (Female factor) | Lifetime | 46·7% | 46·0% | 16·0% | 7·0% | .. | Moderate |
| Akpinar et al, 201933 | 2014–2015 | Turkey | Hospital or clinic based | Modified Abuse Assessment Screen | 142 | Primary (Female factor) | Lifetime | 47·9% | 36·6% | 9·2% | 2·8% | .. | High |
| Rahebi et al, 201934 | 2015 | Iran | Hospital or clinic based | WHO Violence Against Women instrument | 200* | Primary | Lifetime | 83·5% | 70·0% | 68·0% | 60·0% | .. | Moderate |
| Alijani et al, 201935 | 2015–16 | Iran | Hospital or clinic based | Revised Conflict Tactics Scales | 379 | Primary or secondary | Lifetime | 88·9% | Non-verbal 85·8%; verbal: 48·3% | 25·9% | 28·8% | 88·9% | High |
| Bondade et al, 201836 | 2016 | India | Hospital or clinic based | WHO Violence Against Women instrument | 100 | Primary | Lifetime | 50·0% | 34·0% | 11·0% | 5·0% | 50·0% | Moderate |
| Sis Çelik and Kırca, 201837 | 2016 | Turkey | Hospital or clinic based | Infertile Women's Exposure to Violence Determination Scale | 423 | Primary or secondary | Lifetime | 67·4% | .. | .. | .. | .. | Low |
| Ghoneim et al, 202138 | 2016–19 | Egypt | Hospital or clinic based | NorVold Domestic Abuse Questionnaire | 306* | Primary or secondary | Lifetime | .. | 41·2% | .. | .. | .. | Moderate |
| Poornowrooz et al, 201939 | 2017 | Iran | Hospital or clinic based | Domestic Violence Inventory | 147* | Primary or secondary | Lifetime | 56·5% | 52·4% | 34·0% | 27·2% | .. | High |
| Coşkuner Potur et al, 201940 | 2017 | Turkey | Hospital or clinic based | Infertile Women's Exposure to Violence Determination Scale | 315 | Primary or secondary | Lifetime | .. | 47·3% | 7·6% | 0·6% | .. | Moderate |
| Ghaly et al, 201941 | 2017–18 | Egypt | Hospital or clinic based | Infertile Women's Exposure to Violence Determination Scale | 300 | Primary | Lifetime | .. | 96·3% | 50·7% | 45·7% | .. | High |
| Silwal and Thapa, 202010 | 2018 | Nepal | Hospital or clinic based | Nepal demographic and health survey: items on domestic violence | 112 | Primary or secondary | Past 12 months | 30·4% | .. | .. | .. | .. | High |
| Nabi et al, 202042 | 2018–19 | India | Hospital or clinic based | WHO Violence Against Women instrument | 100 | Primary | Lifetime | 51·0% | 29·0% | 16·0% | 6·0% | .. | Moderate |
| Akyüz et al, 201343† | 2009 | Turkey | Hospital or clinic based | Scale for marital violence against women | 228* | Primary | Lifetime | 67·2 (±8·0) | Non-verbal 16·2 (±2·0); verbal: 13·7 (±2·1) | 10·5 (±1·7) | 12·5 (±2·2) | 14·4 (±2·6) | Moderate |
| Akyüz et al, 201444† | 2009 | Turkey | Hospital or clinic based | Scale for marital violence against women | 139 | Primary | Lifetime | 67·0 (±8·3) | .. | .. | .. | .. | Moderate |
| Taebi et al, 201645† | 2013 | Iran | Hospital or clinic based | Partner Abuse Scale: Non-physical | 131 | Primary infertility | Lifetime | 20·3 (±13·4) | .. | .. | .. | .. | High |
| Sheikhan et al, 201446† | 2010–11 | Iran | Hospital or clinic based | Researcher-made questionnaire | 400 | Primary or secondary | Past 3 months | 34·7% | 74·3% | 5·3% | 47·3% | .. | High |
| Mansour and Mohdy, 201847† | 2017–18 | Egypt | Hospital or clinic based | Researcher-made questionnaire | 246 | Primary or secondary (Female factor) | Past 3 months | .. | Embarrassing or humiliating in front of others: 83·7%; restricting women's relationships with her family: 57·3%; scurrility, humiliation, or yelling: 42·3% | Kicking: 76·0%; slapping: 71·5%; pushing or shoving: 71·1% | Abstaining: 79·7%; showing dissatisfaction: 75·2%; intimidate wife to have sex: 45·5% | Cutting financial allowance: 48·0% | High |
Prevalence data are provided as % (SD) or score (SD); SD was not always available. If a study reported two or more items separately in a violence subtype (such as verbal, ridicule, and threat of divorce in psychological violence, or beaten and hurt in physical violence), we used the maximum prevalence value when performing meta-analysis. IPV=intimate partner violence.
Sample size of infertile women, rather than the total sample size in each study.
Only included in systematic review, excluded from meta-analysis.
All of the 30 relevant studies used questionnaires to measure self-reported IPV victimisation, although there was a variety of tools chosen: ten11, 12, 13, 14, 26, 28, 29, 31, 46, 47 used a self-developed tool, four25, 27, 30, 33 used the modified Abuse Assessment Screen, three37, 40, 41 used the Infertile Women's Exposure to Violence Determination Scale (IWEVDS), three34, 36, 42 used the WHO Violence Against Women instrument, three8, 9, 35 used the revised Conflict Tactics Scales, and two43, 44 used the Scale for Marital Violence against Women (SMVW). Other instruments used for measuring violence included the Partner Abuse Scale: Non-physical (PASNP),45 the Domestic Violence Questionnaire,32 the NorVold Domestic Abuse Questionnaire (NORAQ),38 the Domestic Violence Inventory,39 and extracted items related to IPV in national health surveys.10 Nine assessment tools are described in appendix 2 (p 12). Of them, four tools (IWEVDS, SMVW, PASNP, and NORAQ) can measure the magnitude of IPV as a continuous score.
For the risk of bias assessment, high inter-rater reliability between the two reviewers was demonstrated, as indicated by the kappa coefficient for each item (mean 0·88, range 0·71–1·00; appendix 2 p 10) and the Spearman's rank correlation coefficient for the summed score of each study (r=0·89, p<0·0001). The 30 studies obtained a mean score of 7·0 (SD 1·4, range 6–10); five studies were ranked low risk, nine were ranked moderate risk, and 16 were ranked high risk (appendix 2 p 11).
After excluding five studies (three reporting only the prevalence in scores rather than in rates43, 44, 45 and two not reporting the prevalence in past 12 months or lifetime46, 47), we included 25 studies (with 7164 study participants) for meta-analyses: eight studies reported IPV prevalence over a 12-month period (3118 participants) and 17 studies reported IPV prevalence over a lifetime (4046 participants).
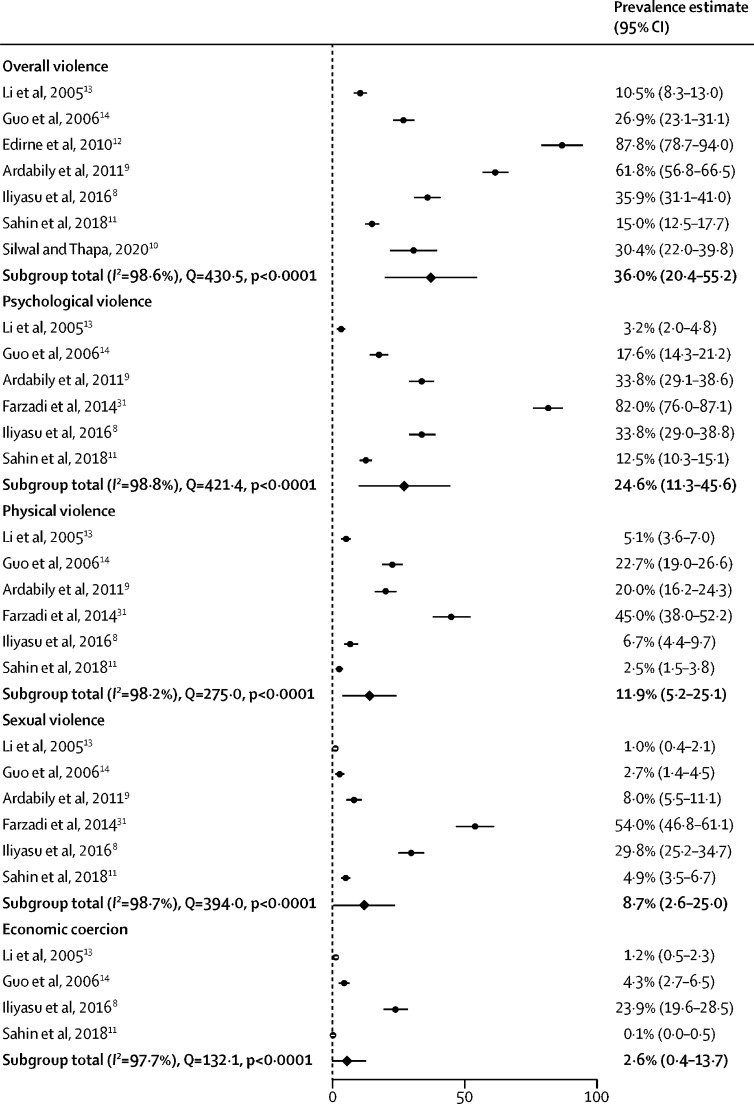
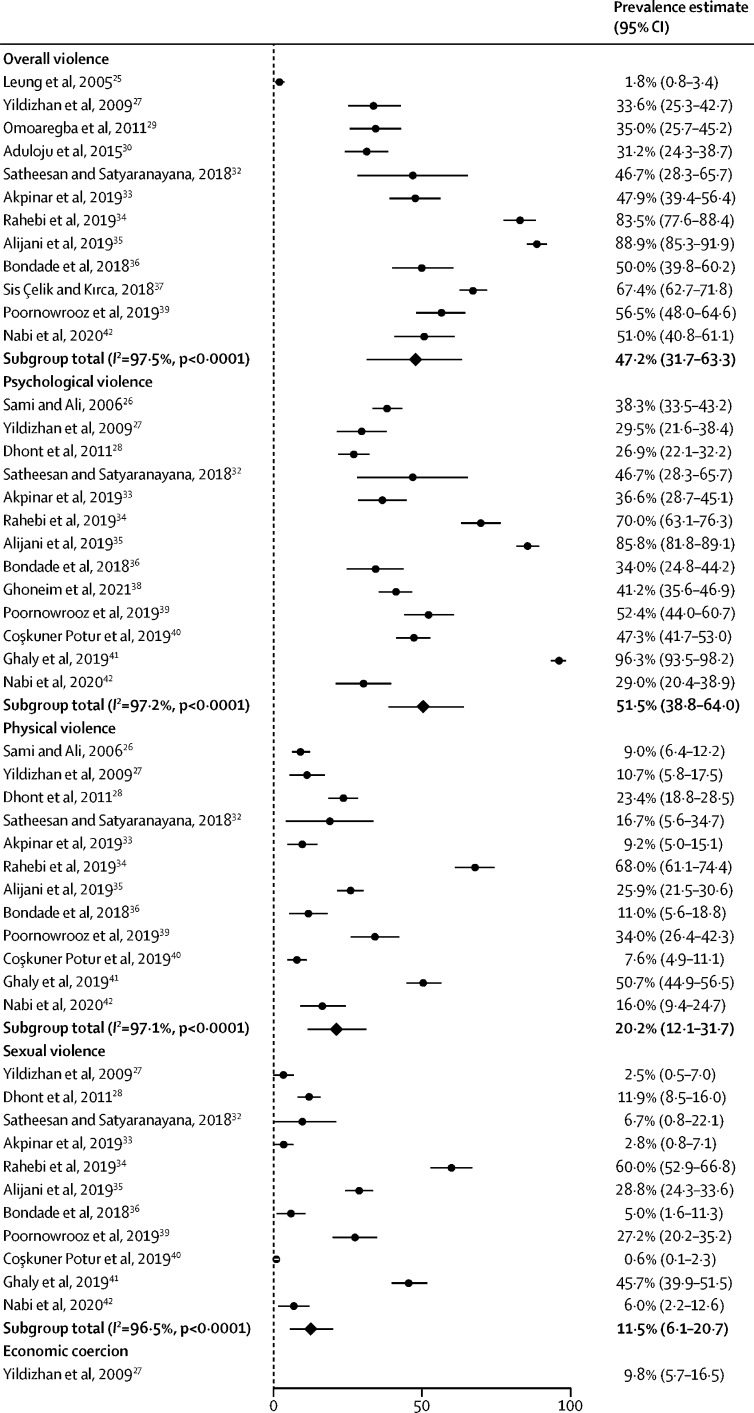
The overall pooled prevalence of IPV over a 12-month period was 36·0% (95% CI 20·4–55·2): 24·6% (11·3–45·6) for psychological violence, 11·9% (5·2–25·1) for physical violence, 8·7% (2·6–25·0) for sexual violence, and 2·6% (0·4–13·7) for economic coercion (figure 2). The overall pooled prevalence of IPV over a lifetime was 47·2% (31·7–63·3): 51·5% (38·8–64·0) for psychological violence, 20·2% (12·1–31·7) for physical violence, 11·5% (6·1–20·7) for sexual violence, and 9·8% (5·7–16·5) for economic coercion (figure 3). The pooled prevalence of lifetime psychological IPV is slightly higher than the overall pooled lifetime prevalence because different studies contributed to the two estimates. Substantial heterogeneity across studies was seen in the pooled estimations, with Higgins’ I2 values of 96·5–98·8% (Q test p<0·0001). For prevalence in the past 12-month or lifetime, Egger's test showed significant publication bias (p<0·1) in physical violence and sexual violence (appendix 2 pp 13–14).
Figure 2.
Prevalence of intimate partner violence in the past 12 months, by subtypes of violence
Figure 3.
Lifetime prevalence of intimate partner violence, by subtypes of violence
Subgroup analyses and univariate meta-regressions examined the source of heterogeneity using several covariates: study period, region, type of infertility, risk of bias, and sample size. Significantly increased prevalence estimates for overall violence in the past 12 months (table 2) were found in studies with high risk of bias (R2=35·74%) and studies with smaller sample sizes (R2=44·17%). We found that, when compared with studies conducted earlier (2010 and before), studies done after 2010 reported significantly higher lifetime prevalence estimates (R2=39·46%). Similarly, studies conducted in west Asia had significantly higher lifetime prevalence estimates (R2=50·95%) than studies done in Africa. Neither past-12-months nor lifetime prevalence differed by type of infertility. Detailed results of each subtype can be found in appendix 2 (pp 15–28).
Table 2.
Subgroup analyses and meta-regressions for the pooled prevalence of overall IPV
|
Subgroup analysis |
Meta-regression analysis |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Number of studies | Sample size | Prevalence of IPV, % (95% CI) | I2 (%) | β (SE) | Odds ratio (95% CI) | p value | R2 (%) | ||
| Past 12 months | |||||||||
| Year | |||||||||
| 2010 and before | 4 | 1659 | 45·0 (17·5–76·0) | 99·1 | Ref | Ref | Ref | <0·01 | |
| After 2010 | 3 | 1259 | 25·9 (13·3–44·2) | 96·9 | −0·195 (0·212) | 0·823 (0·543–1·247) | 0·357 | .. | |
| Infertility type | |||||||||
| Primary | 3 | 1577 | 29·2 (8·8–63·6) | 99·3 | Ref | Ref | Ref | <0·01 | |
| Primary or secondary | 4 | 1341 | 41·6 (20·2–66·6) | 98·0 | 0·092 (0·226) | 1·096 (0·705–1·704) | 0·684 | .. | |
| Region | |||||||||
| Africa | 1 | 373 | 35·9 (31·2–40·9) | .. | Ref | Ref | Ref | <0·01 | |
| West Asia | 3 | 1256 | 55·4 (16·1–88·9) | 99·3 | 0·188 (0·356) | 1·207 (0·601–2·425) | 0·598 | .. | |
| South Asia | 1 | 112 | 30·4 (22·6–39·5) | .. | −0·056 (0·438) | 0·946 (0·401–2·231) | 0·899 | .. | |
| East Asia | 2 | 1177 | 17·2 (6·3–39·1) | 98·0 | −0·172 (0·378) | 0·842 (0·401–1·766) | 0·648 | .. | |
| Risk of bias | |||||||||
| High | 3 | 594 | 62·5 (33·3–84·8) | 96·5 | Ref | Ref | Ref | 35·74 | |
| Moderate | 1 | 774 | 15·0 (12·6–17·7) | .. | −0·451 (0·253) | 0·637 (0·388–1·046) | 0·075 | .. | |
| Low | 3 | 1550 | 22·5 (10·9–40·7) | 97·9 | −0·357 (0·180) | 0·670 (0·492–0·996) | 0·047 | .. | |
| Sample size | 7 | 2918 | .. | .. | −0·001 (0·000) | 0·999 (0·999–1·000) | 0·018 | 44·17 | |
| Lifetime | |||||||||
| Year | |||||||||
| 2010 and before | 3 | 722 | 14·9 (3·0–49·7) | 97·6 | Ref | Ref | Ref | 39·46 | |
| After 2010 | 9 | 1691 | 60·4 (45·7–73·4) | 96·4 | 0·355 (0·127) | 1·426 (1·112–1·829) | 0·005 | .. | |
| Infertility type | |||||||||
| Primary | 6 | 694 | 53·3 (37·0–68·9) | 93·0 | Ref | Ref | Ref | <0·01 | |
| Primary or secondary | 6 | 1719 | 41·0 (18·1–68·6) | 98·6 | −0·055 (0·146) | 0·946 (0·711–1·260) | 0·706 | .. | |
| Region | |||||||||
| Africa | 2 | 270 | 32·6 (27·3–38·4) | 0·0 | Ref | Ref | Ref | 50·95 | |
| West Asia | 6 | 1413 | 65·8 (47·7–80·3) | 97·2 | 0·303 (0·140) | 1·354 (1·029–1·781) | 0·031 | .. | |
| South Asia | 3 | 230 | 50·0 (43·6–56·4) | 0·0 | 0·163 (0·160) | 1·177 (0·860–1·611) | 0·308 | .. | |
| East Asia | 1 | 500 | 1·8 (0·9–3·4) | .. | −0·313 (0·207) | 0·731 (0·487–1·097) | 0·131 | .. | |
| Risk of bias | |||||||||
| High | 7 | 1560 | 37·1 (17·0–63·0) | 98·3 | Ref | Ref | Ref | <0·01 | |
| Moderate | 4 | 430 | 59·8 (38·0–78·3) | 93·3 | 0·161 (0·155) | 1·175 (0·867–1·592) | 0·298 | .. | |
| Low | 1 | 423 | 67·4 (62·8–71·7) | .. | 0·253 (0·260) | 1·288 (0·774–2·144) | 0·331 | .. | |
| Sample size | 12 | 2413 | .. | .. | <–0·0001 (0·001) | 1·000 (0·998–1·002) | 0·986 | <0·01 | |
Random-effects meta-regression model, with restricted maximum likelihood method used. Detailed results of each subtype are given in appendix 2 (pp 15–28). IPV=intimate partner violence.
Our subgroup analysis and univariate meta-regression across three commonly used tools—the modified Abuse Assessment Screen, the WHO Violence Against Women instrument, and the revised Conflict Tactics Scales—showed significant variation in the overall prevalence rates of IPV over a lifetime (R2=54·27%; appendix 2 p 29).
Lifetime IPV prevalence in included studies are compared between infertile women and fertile women in appendix 2 (p 30). Infertile women were more likely to experience physical violence (OR 2·03 [95% CI 1·39–2·97]) and sexual violence (OR 2·55 [1·67–3·89]) than were fertile women, but overall violence and psychological violence did not differ between the two groups (OR 1·29 [0·24–6·79] vs OR 1·76 [0·91–3·40]).
Discussion
In this systematic review and meta-analysis, we summarised the available evidence and used meta-analytical methods to estimate the prevalence of IPV against infertile women in LMICs, despite substantial cross-study heterogeneity. The pooled prevalence of IPV against infertile women in nine LMICs was found to be 36·0% over a 12-month period and 47·2% over a lifetime, with psychological violence being the most common form, followed by physical violence, sexual violence, and economic coercion. Compared with WHO's global estimates of rates of IPV for ever-married or ever-partnered women of reproductive age (13% and 27%, respectively),5 albeit with various differences in measuring tools and subtypes of IPV measured, our findings show that infertile women in LMICs could be more vulnerable to IPV than the general female population. This finding is supported by the comparison between infertile women and fertile women in this review: the infertile group have a higher risk of suffering from physical violence (OR 2·03 [95% CI 1·39–2·97]) and sexual violence (OR 2·55 [1·67–3·89]) in their lifetime than do the fertile group. However, given that these ORs are within the zone of potential bias (0·3<OR<3)48 and the small sample size of the selected studies, further research is necessary to substantiate our findings.
Despite its high prevalence, IPV against infertile women has been under-researched. First, existing evidence has been restricted to a few LMICs in each region, with no studies in Latin American countries. Despite the language restrictions used for this review, the pervasive unavailability of data reaffirms the dearth of research on IPV against infertile women in the academic community. Second, most existing studies recruited study participants from clinics or hospitals, which is likely to result in the underestimation of IPV prevalence among infertile women who did not seek fertility treatment. Third, tools measuring IPV against infertile women are scarce despite the large variety in the IPV tools adopted in existing studies. IWEVDS is perhaps the only tool specifically designed for the context of infertility, but it has only been applied and validated in Turkey and Egypt.37, 40, 49, 50 Therefore, further research should prioritise population-based surveys, the standardised conceptualisation and measurement of IPV and its forms, and the development of specific measuring tools for infertile women and cross-cultural adaptations.
Our subgroup analyses and meta-regression results show that the prevalence of IPV against infertile women was significantly heterogeneous across different study periods, study regions, and both types of infertility. The more recent studies (published after 2010) seem to be more likely to report a higher prevalence than those conducted earlier. Considerable regional discrepancies in IPV prevalence were seen; infertile women in west Asia appeared to have a higher risk of lifetime violence than those in Africa. Study populations with mixed types of infertility (primary and secondary) might have a higher prevalence than those with primary infertility. Secondary infertility is usually associated with female factors (declined female reproductive functions caused by ageing and disease), whereas primary infertility is evenly caused by male and female factors.51, 52 Thus, women with secondary infertility might be blamed more for their infertility than those with primary infertility. However, due to significant cross-study heterogeneities and the small number of studies in each subgroup, these findings should be further verified through future research.
Although IPV against infertile women was common in all populations included in this analysis, the high prevalence in LMICs might be associated with culture-specific gender norms. Gender inequality underpins violence against women, which is ingrained in sociocultural norms and institutionalised through laws and regulations that perpetuate greater wealth and power for men than women.53, 54 In a patriarchal structure (either a society or a family), men often treat women as their private property and marriage as the means to produce offspring. Besides violence perpetrated by their husband or partner, infertile women often experience domestic violence by other members of the family too,10, 37, 38 or are even ridiculed and isolated by their peers or communities.55, 56 At the same time, infertile women are often reluctant to disclose their experiences of IPV due to shame or guilt about their infertility.15, 57 Such circumstances highlight that motherhood can often deeply shape women's self-identity, marital relationships, family dynamics, and social image, and accentuates the feeling that women bear a disproportionate share of the burden of infertility. As gender inequalities are deeply embedded in IPV against infertile women, we argue that applying gender theories to infertility research will make clear the gendered structural connections between infertility and IPV. In addition, in exploring the association between IPV and infertility, there seems to be an established assumption that infertility can lead to IPV in most cases. However, we cannot ignore that IPV can also lead to infertility; physical, sexual, or psychological traumas can affect the physiological or behavioural mechanisms of fertility,58 which are also gender-based ramifications of reproductive health. Moreover, given the increasing prevalence of homosexual partnerships wherein children are desired, IPV and other psychological problems accompanying infertility should be taken more seriously in these partnerships, especially in countries and territories where surrogacy or adoption is prohibited for homosexual couples.
Research on effective interventions against IPV toward infertile women remains largely absent. At the individual level, providing psychosocial interventions and training and engaging health-care providers are effective strategies to reduce IPV against women in the general population.59, 60 Marital counselling, in particular, has been an effective intervention for infertile couples with a history of IPV or psychological trauma.61, 62 Thus, IPV screening and counselling could be introduced in infertility clinics to identify IPV, facilitate early intervention, and improve timely referral to specialised agencies—eg, groups or institutions specialised in psychological intervention, or public security agencies and authorities if there is evidence of a crime. Furthermore, in recent years, researchers have increasingly emphasised the importance of structural interventions on IPV at multiple socioecological levels.63, 64 Therefore, it is necessary to generate tailored interventions to address the root causes of IPV in the infertile population at multiple levels of the society.
This study has several limitations. First, because of the challenges and gaps in knowledge we have discussed, the findings of the existing studies present significant heterogeneity and publication bias. More consistent approaches in data definition and data collection might enable policy makers to better address the factors that lead to the disproportionate levels of IPV against infertile women. Second, existing data on IPV are restricted to a few countries and are not available for populations living in the rest of the world. High quality and contemporary data from more countries are crucial to understanding and addressing IPV. Third, due to significant cross-study heterogeneities and the few studies with subgroup analyses available for this review, further research is necessary to explore the related factors of IPV against infertile women at various levels, such as measurement tools, study setting, country, ethnicity, or other cultural contexts.
In summary, on average at least one in three infertile women in LMICs experience IPV over a 12-month period and about one in two over a lifetime, which might be underestimated given that the sources of participants in the current study were primarily infertility clinics or hospitals. Considering the high degree of heterogeneity across studies, we call for further studies into IPV against infertile women using a consistent approach in data definition and data collection, as well as longitudinal studies to explore the bidirectional association between IPV and infertility. IPV screening, counselling and structural interventions should be tailored to identify, facilitate early intervention, and address IPV against infertile women at multiple levels of society.
Data sharing
All datasets generated and analysed for this work are available in the main text and appendix 2 (pp 1–32).
Declaration of interests
YW reports grants from the China Medical Board, USA, and JQ reports grants from WHO during the conduct of this study. All other authors declare no competing interests.
Acknowledgments
Acknowledgments
This study was funded by the China Medical Board, USA (CMB OC1–21–431) and WHO (GJ2–2021-WHOSO-10). There were no other external funding sources. We thank all authors and participants in the studies included in this review.
Acknowledgments
Contributors
YW and JQ designed the study, and all authors oversaw its implementation. YW and YF coordinated and performed all review activities, including searches, study selection (including inclusion and exclusion of abstracts), data extraction, and quality assessment. YW, YF, TT, and FK did the data analyses. QG and SZ improved the methods of this study. YW and YF wrote the initial draft of the manuscript. PG, CL, DEB, and JQ contributed to the writing and subsequent versions of the manuscript. All authors reviewed the study findings and read and approved the final version before submission.
Contributor Information
David E Bloom, Email: dbloom@hsph.harvard.edu.
Jie Qiao, Email: jie.qiao@263.net.
Supplementary Material
References
- 1.Starrs AM, Ezeh AC, Barker G, et al. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. Lancet. 2018;391:2642–2692. doi: 10.1016/S0140-6736(18)30293-9. [DOI] [PubMed] [Google Scholar]
- 2.Gurunath S, Pandian Z, Anderson RA, Bhattacharya S. Defining infertility—a systematic review of prevalence studies. Hum Reprod Update. 2011;17:575–588. doi: 10.1093/humupd/dmr015. [DOI] [PubMed] [Google Scholar]
- 3.Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9 doi: 10.1371/journal.pmed.1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keiding N, Ali MM, Eriksson F, Matsaseng T, Toskin I, Kiarie J. The use of time to pregnancy for estimating and monitoring human fecundity from demographic and health surveys. Epidemiology. 2021;32:27–35. doi: 10.1097/EDE.0000000000001296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . World Health Organization; Geneva: 2021. Violence against women prevalence estimates, 2018: global, regional and national prevalence estimates for intimate partner violence against women and global and regional prevalence estimates for non-partner sexual violence against women. [Google Scholar]
- 6.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. 2006;368:1260–1269. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 7.Yount KM, Krause KH, VanderEnde KE. Economic coercion and partner violence against wives in Vietnam: a unified framework? J Interpers Violence. 2016;31:3307–3331. doi: 10.1177/0886260515584350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iliyasu Z, Galadanci HS, Abubakar S, et al. Phenotypes of intimate partner violence among women experiencing infertility in Kano, Northwest Nigeria. Int J Gynaecol Obstet. 2016;133:32–36. doi: 10.1016/j.ijgo.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Ardabily HE, Moghadam ZB, Salsali M, Ramezanzadeh F, Nedjat S. Prevalence and risk factors for domestic violence against infertile women in an Iranian setting. Int J Gynaecol Obstet. 2011;112:15–17. doi: 10.1016/j.ijgo.2010.07.030. [DOI] [PubMed] [Google Scholar]
- 10.Silwal A, Thapa B. Prevalence of domestic violence among infertile women attending subfertility clinic of a tertiary hospital. JNMA J Nepal Med Assoc. 2020;58:372–376. doi: 10.31729/jnma.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sahin S, Ilcioglu K, Unsal A. Domestic violence and anxiety levels in infertile women. Cukurova Med J. 2018;43:777–784. [Google Scholar]
- 12.Edirne T, Arica SG, Gucuk S, et al. Use of complementary and alternative medicines by a sample of Turkish women for infertility enhancement: a descriptive study. BMC Complement Altern Med. 2010;10:11. doi: 10.1186/1472-6882-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Y, Cheng Y, Huang N, et al. Current situation of domestic violence among infertile couples in rural areas of Dengfeng City. Zhongguo Fuyou Baojian. 2005;20:3128–3130. [Google Scholar]
- 14.Guo X, Cheng Y, Huang N, et al. Analysis on situation and influence factors of domestic violence among infertility couples. Chin J Publ Health. 2006;22:552–554. [Google Scholar]
- 15.Stellar C, Garcia-Moreno C, Temmerman M, van der Poel S. A systematic review and narrative report of the relationship between infertility, subfertility, and intimate partner violence. Int J Gynaecol Obstet. 2016;133:3–8. doi: 10.1016/j.ijgo.2015.08.012. [DOI] [PubMed] [Google Scholar]
- 16.Hajizade-Valokolaee M, Khani S, Fooladi E, Peivandi S. Related factors of violence against women with infertility: a systematic review study based on an ecological approach. Electron Physician. 2017;9:5834–5843. doi: 10.19082/5834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zarif Golbar Yazdi H, Aghamohammadian Sharbaf H, Kareshki H, Amirian M. Psychosocial consequences of female infertility in Iran: a meta-analysis. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.518961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharifi F, Jamali J, Larki M, Roudsari RL. Domestic violence against infertile women: a systematic review and meta-analysis. Sultan Qaboos Univ Med J. 2021;22:14–27. doi: 10.18295/squmj.5.2021.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339 [PMC free article] [PubMed] [Google Scholar]
- 20.Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–939. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 21.Lipsey MW, Wilson DB. SAGE publications; Thousand Oaks, CA: 2001. Practical meta-analysis. [Google Scholar]
- 22.Gutwinski S, Schreiter S, Deutscher K, Fazel S. The prevalence of mental disorders among homeless people in high-income countries: an updated systematic review and meta-regression analysis. PLoS Med. 2021;18 doi: 10.1371/journal.pmed.1003750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pun KD, Rishal P, Darj E, et al. Domestic violence and perinatal outcomes - a prospective cohort study from Nepal. BMC Public Health. 2019;19:671. doi: 10.1186/s12889-019-6967-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nybergh L, Taft C, Krantz G. Psychometric properties of the WHO Violence Against Women instrument in a female population-based sample in Sweden: a cross-sectional survey. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-002053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leung TW, Leung WC, Ng EH, Ho PC. Quality of life of victims of intimate partner violence. Int J Gynaecol Obstet. 2005;90:258–262. doi: 10.1016/j.ijgo.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 26.Sami N, Ali TS. Psycho-social consequences of secondary infertility in Karachi. J Pak Med Assoc. 2006;56:19–22. [PubMed] [Google Scholar]
- 27.Yildizhan R, Adali E, Kolusari A, Kurdoglu M, Yildizhan B, Sahin G. Domestic violence against infertile women in a Turkish setting. Int J Gynaecol Obstet. 2009;104:110–112. doi: 10.1016/j.ijgo.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 28.Dhont N, van de Wijgert J, Coene G, Gasarabwe A, Temmerman M. ‘Mama and papa nothing’: living with infertility among an urban population in Kigali, Rwanda. Hum Reprod. 2011;26:623–629. doi: 10.1093/humrep/deq373. [DOI] [PubMed] [Google Scholar]
- 29.Omoaregba JO, James BO, Lawani AO, Morakinyo O, Olotu OS. Psychosocial characteristics of female infertility in a tertiary health institution in Nigeria. Ann Afr Med. 2011;10:19–24. doi: 10.4103/1596-3519.76567. [DOI] [PubMed] [Google Scholar]
- 30.Aduloju PO, Olagbuji NB, Olofinbiyi AB, Awoleke JO. Prevalence and predictors of intimate partner violence among women attending infertility clinic in south-western Nigeria. Eur J Obstet Gynecol Reprod Biol. 2015;188:66–69. doi: 10.1016/j.ejogrb.2015.02.027. [DOI] [PubMed] [Google Scholar]
- 31.Farzadi L, Ghasemzadeh A, Asl ZB, Mahini M, Shirdel H. Intimate partner violence against infertile women. J Clin Res Govern. 2014;3:147–151. [Google Scholar]
- 32.Satheesan S, Satyaranayana V. Quality of marital relationship, partner violence, psychological distress, and resilience in women with primary infertility. Int J Community Med Public Health. 2018;5:734–739. [Google Scholar]
- 33.Akpinar F, Yilmaz S, Karahanoglu E, et al. Intimate partner violence in Turkey among women with female infertility. Sex Relationship Ther. 2019;34:3–9. [Google Scholar]
- 34.Rahebi SM, Rahnavardi M, Rezaie-Chamani S, Nazari M, Sabetghadam S. Relationship between domestic violence and infertility. East Mediterr Health J. 2019;25:537–542. doi: 10.26719/emhj.19.001. [DOI] [PubMed] [Google Scholar]
- 35.Alijani F, Khosravi A, Mousavi M, Delarosa V. The associated factors of domestic violence against infertile women. J Res Dev Nurs Midwifery. 2019;16:61–70. [Google Scholar]
- 36.Bondade S, Iyengar RS, Shivakumar BK, Karthik KN. Intimate partner violence and psychiatric comorbidity in infertile women - a cross-sectional hospital based study. Indian J Psychol Med. 2018;40:540–546. doi: 10.4103/IJPSYM.IJPSYM_158_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sis Çelik A, Kırca N. Prevalence and risk factors for domestic violence against infertile women in a Turkish setting. Eur J Obstet Gynecol Reprod Biol. 2018;231:111–116. doi: 10.1016/j.ejogrb.2018.10.032. [DOI] [PubMed] [Google Scholar]
- 38.Ghoneim HM, Taha OT, Ibrahim ZM, Ahmed AA. Violence and sexual dysfunction among infertile Egyptian women. J Obstet Gynaecol Res. 2021;47:1572–1578. doi: 10.1111/jog.14689. [DOI] [PubMed] [Google Scholar]
- 39.Poornowrooz N, Jamali S, Haghbeen M, Javadpour S, Sharifi N, Mosallanezhad Z. The comparison of violence and sexual function between fertile and infertile women: a study from Iran. J Clin Diagn Res. 2019;13:QC9–Q11. [Google Scholar]
- 40.Coşkuner Potur D, Onat G, Doğan Merih Y. An evaluation of the relationship between violence exposure status and personality characteristics among infertile women. Health Care Women Int. 2019;40:1135–1148. doi: 10.1080/07399332.2019.1622704. [DOI] [PubMed] [Google Scholar]
- 41.Ghaly AS, Essa RM, Yassin ST. Intimate partner violence against infertile women. IOSR J Nurs Health Sci. 2019;8:10–25. [Google Scholar]
- 42.Nabi J, Wani RA, Dar SA, Majeed N. A cross sectional study on psychiatric morbidity and intimate partner violence in treatment seeking infertile women visiting a tertiary care hospital. Int J Contemp Med Res. 2020;7:H1–H5. [Google Scholar]
- 43.Akyüz A, Seven M, Sahiner G, Bilal B. Studying the effect of infertility on marital violence in Turkish women. Int J Fertil Steril. 2013;6:286–293. [PMC free article] [PubMed] [Google Scholar]
- 44.Akyüz A, Sahiner G, Seven M, Bakır B. The effect of marital violence on infertility distress among a sample of Turkish women. Int J Fertil Steril. 2014;8:67–76. [PMC free article] [PubMed] [Google Scholar]
- 45.Taebi M, Gandomani SJ, Nilforoushan P, GholamiDehaghi A. Association between infertility factors and non-physical partner abuse in infertile couples. Iran J Nurs Midwifery Res. 2016;21:368–371. doi: 10.4103/1735-9066.185577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sheikhan Z, Ozgoli G, Azar M, Alavimajd H. Domestic violence in Iranian infertile women. Med J Islam Repub Iran. 2014;28:152. [PMC free article] [PubMed] [Google Scholar]
- 47.Mansour F, Mohdy HA. Intimate partner violence among women with female infertility. American J Nurs Res. 2018;6:309–316. [Google Scholar]
- 48.Grimes DA, Schulz KF. False alarms and pseudo-epidemics: the limitations of observational epidemiology. Obstet Gynecol. 2012;120:920–927. doi: 10.1097/AOG.0b013e31826af61a. [DOI] [PubMed] [Google Scholar]
- 49.Ozturk R, Taner A, Guneri SE, Yilmaz B. Another face of violence against women: infertility. Pak J Med Sci. 2017;33:909–914. doi: 10.12669/pjms.334.12862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lotfy M, Hamdy MA, Mansour AFI, et al. Prevalence and risk factors for domestic violence among infertile Egyptian women: a cross-sectional study. Eur J Contracept Reprod Health Care. 2019;24:362–367. doi: 10.1080/13625187.2019.1642467. [DOI] [PubMed] [Google Scholar]
- 51.Carson SA, Kallen AN. Diagnosis and management of infertility: a review. JAMA. 2021;326:65–76. doi: 10.1001/jama.2021.4788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vander Borght M, Wyns C. Fertility and infertility: definition and epidemiology. Clin Biochem. 2018;62:2–10. doi: 10.1016/j.clinbiochem.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 53.García-Moreno C, Zimmerman C, Morris-Gehring A, et al. Addressing violence against women: a call to action. Lancet. 2015;385:1685–1695. doi: 10.1016/S0140-6736(14)61830-4. [DOI] [PubMed] [Google Scholar]
- 54.The Lancet Preventing violence against women: beyond 16 days. Lancet. 2021;398 doi: 10.1016/S0140-6736(21)02781-1. [DOI] [PubMed] [Google Scholar]
- 55.Ofosu-Budu D, Hanninen V. Living as an infertile woman: the case of southern and northern Ghana. Reprod Health. 2020;17:69. doi: 10.1186/s12978-020-00920-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tabong PT, Adongo PB. Infertility and childlessness: a qualitative study of the experiences of infertile couples in Northern Ghana. BMC Pregnancy Childbirth. 2013;13:72. doi: 10.1186/1471-2393-13-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cui W. Mother or nothing: the agony of infertility. Bull World Health Organ. 2010;88:881–882. doi: 10.2471/BLT.10.011210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Coker AL. Does physical intimate partner violence affect sexual health? A systematic review. Trauma Violence Abuse. 2007;8:149–177. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- 59.Turner DT, Riedel E, Kobeissi LH, et al. Psychosocial interventions for intimate partner violence in low and middle income countries: a meta-analysis of randomised controlled trials. J Glob Health. 2020;10 doi: 10.7189/jogh.10.010409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kalra N, Hooker L, Reisenhofer S, Di Tanna GL, García-Moreno C. Training healthcare providers to respond to intimate partner violence against women. Cochrane Database Syst Rev. 2021;5 doi: 10.1002/14651858.CD012423.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Poorheidari M, Ganji J, Hasani-Moghadam S, Azizi M, Alijani F. The effects of relationship enrichment counseling on marital satisfaction among infertile couples with a history of domestic violence. J Nurs Midwifery Sci. 2021;8:1–8. [Google Scholar]
- 62.Aiyenigba AO, Weeks AD, Rahman A. Managing psychological trauma of infertility. Afr J Reprod Health. 2019;23:76–91. doi: 10.29063/ajrh2019/v23i2.8. [DOI] [PubMed] [Google Scholar]
- 63.Bourey C, Williams W, Bernstein EE, Stephenson R. Systematic review of structural interventions for intimate partner violence in low- and middle-income countries: organizing evidence for prevention. BMC Public Health. 2015;15 doi: 10.1186/s12889-015-2460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Michau L, Horn J, Bank A, Dutt M, Zimmerman C. Prevention of violence against women and girls: lessons from practice. Lancet. 2015;385:1672–1684. doi: 10.1016/S0140-6736(14)61797-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All datasets generated and analysed for this work are available in the main text and appendix 2 (pp 1–32).