Abstract
Study Design:
Meta-analysis.
Objective:
To compare outcomes between minimally invasive scoliosis surgery (MISS) and traditional posterior instrumentation and fusion in the correction of adolescent idiopathic scoliosis (AIS).
Methods:
A literature search was performed using MEDLINE, PubMed, EMBASE, Google scholar and Cochrane databases, including studies reporting outcomes for both MISS and open correction of AIS. Study details, demographics, and outcomes, including curve correction, estimated blood loss (EBL), operative time, postoperative pain, length of stay (LOS), and complications, were collected and analyzed.
Results:
A total of 4 studies met the selection criteria and were included in the analysis, totaling 107 patients (42 MIS and 65 open) with a mean age of 16 years. Overall there was no difference in curve correction between MISS (73.2%) and open (76.7%) cohorts. EBL was significantly lower in the MISS (271 ml) compared to the open (527 ml) group, but operative time was significantly longer (380 min for MISS versus 302 min for open). There were no significant differences between the approaches in pain, LOS, complications, or reoperations.
Conclusion:
MISS was associated with less blood loss but longer operative times compared to traditional open fusion for AIS. There was no difference in curve correction, postoperative pain, LOS, or complications/reoperations. While MISS has emerged as a feasible option for the surgical management of AIS, further research is warranted to compare these 2 approaches.
Keywords: idiopathic scoliosis, minimally invasive scoliosis surgery, adolescent idiopathic scoliosis, open surgery, spinal fusion, posterior fusion, minimally invasive surgery
Introduction
Defined as a coronal Cobb angle >10 degrees, idiopathic scoliosis is the most common spinal disorder in pediatric and adolescent populations, occurring in approximately 1-3% of the community.1-5 While mild curves occur with high frequency, the incidence of AIS based on the magnitude of deformity varies, with severe deformity being less common. Curves >10 degrees, for example, have an incidence of 1-3%, whereas the incidence decreases to 0.15% to 0.3% for curves of >30 degrees. 1 Management options for AIS vary and are dependent on curve morphology and magnitude and remaining growth potential, and range from nonoperative measures such as observation and bracing to surgical correction.
For severe or progressive cases that require operative management, the primary goals of surgery are to correct the deformity, restore coronal and sagittal balance, and ultimately achieve solid arthrodesis.6-8 Historically, the gold standard in the surgical correction of AIS has been traditional open posterior instrumentation and fusion. 9 This technique is typically performed using a large midline incision with extensive subperiosteal stripping of the posterior elements and is associated with substantial blood loss, significant postoperative pain, surgical site infection, and poor cosmesis.8-10
Minimally invasive scoliosis surgery (MISS) has been proposed as a potential means of improving on these shortcomings. Compared to traditional open surgery, the potential benefits of MISS include smaller incisions with less soft tissue disruption, decreased blood loss, early mobilization, and shorter postoperative hospitalization.11,12 Though it offers these theoretical advantages, this less invasive approach can be more technically demanding and may rely, to a greater extent, on intraoperative imaging with potential for increased radiation exposure to the patient and staff. While there have been reports of acceptable outcomes associated with minimally invasive correction of AIS,8,9,12-16 to our knowledge no direct comparison between MISS and traditional open surgery has been conducted and the differences between these 2 approaches remains largely unclear. The aim of this meta-analysis is to review the literature comparing outcomes between MISS and traditional posterior instrumentation and fusion in the correction of AIS.
Materials and Methods
A systematic review and meta-analysis were conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 17 A search was performed in the MEDLINE, PubMed, EMBASE, Google scholar and Cochrane databases using the search terms “adolescent idiopathic scoliosis”, “open surgery”, and “minimally invasive surgery”. The final search was performed on December 31, 2019. In addition to these databases, the references of each article were also assessed manually for potential inclusion in the study.
Selection Criteria
Clinical studies were evaluated and included if they were written in English and reported a comparative cohort of traditional open versus minimally invasive surgical techniques for the treatment of AIS. Nonclinical studies, literature reviews, expert opinions, case reports, and those not reporting both MISS and open surgical treatment of AIS were excluded. Studies were reviewed by 2 of the study authors (AA, YA), who performed title and abstract reviews separately. The full texts of the articles meeting inclusion criteria based on title and abstract were then reviewed for final inclusion into the study, with authors coming to a consensus in instances of disagreement.
Quality Evaluation
Only non-randomized trials evaluating MISS versus open surgical correction of AIS were identified. Therefore, included studies were evaluated using the Newcastle–Ottawa Scale. 18 This quality assessment was performed independently by 2 authors (AA, YA).
Data Extraction and Analysis
The data items that were collected included (1) study characteristics (author name, study year, level of evidence, follow-up period, and number of patients), (2) patient demographics (age, sex), (3) number of patients undergoing MISS and open surgery, (4) subgroups as per Lenke classification, and (5) outcome measures. The primary outcome measure was major curve correction, determined using the following calculation: (Post-operative curve magnitude – Pre-operative curve magnitude) x 100. The secondary outcomes were blood loss (ml), operative time (minutes), VAS pain score, hospital length of stay (days), and complication and reoperation rates. The data was extracted by 2 authors independently.
The data analysis was performed by constructing a random-effects model using open Meta-Analysis Software. For continuous variables, the mean difference was utilized for estimating effect, with the values depicted in a forest plot diagram. For both types of variables, a 95% confidence interval (CI) was used. Statistical heterogeneity across the studies was tested using I 2 .
Surgical Technique
As reported in the included studies, traditional open scoliosis surgery was performed through a standard posterior midline approach with subperiosteal muscle dissection, pedicle screw insertion (freehand or fluoroscopy-guided), facetectomy/decortication and posterior release, followed by rod insertion and manual correction maneuvers. The MISS approach was performed using 1 to 3 midline incisions (∼3-5 cm in length) with subsequent skin and subcutaneous tissue mobilization to provide access to facet joints and pedicle screw starting points through a Wiltse approach. Pedicle screws were placed using O-arm navigation or via direct visualization and freehand technique, followed by subfascial rod insertion and manual reduction maneuvers with posterolateral fusion around the facets.
Results
Study Characteristics and Patient Demographics
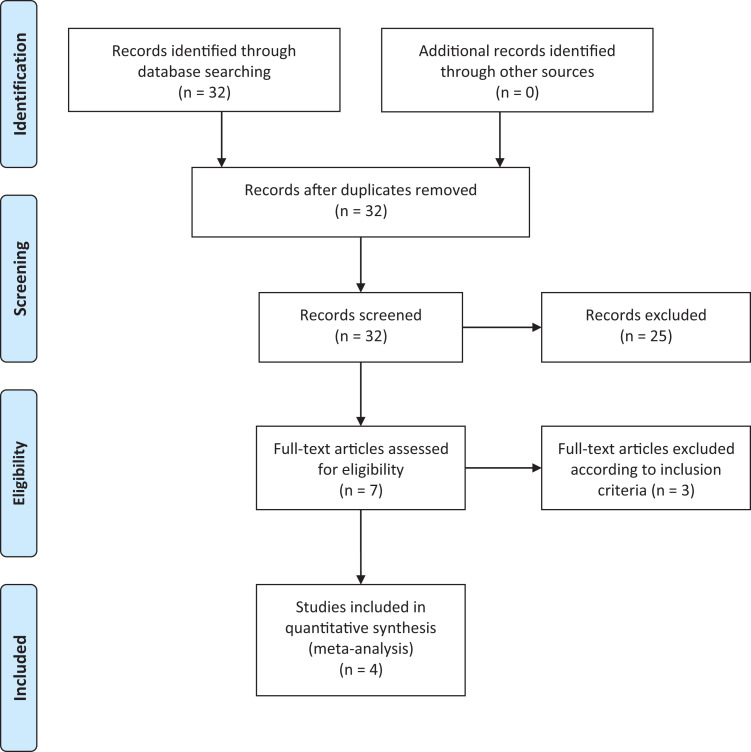
A total of 4 studies were included in the analysis according to PRISMA guidelines (Figure 1). Demographic data and distribution of MISS versus open are detailed in Table 1. All of the included studies were level III retrospective cohort studies comprising a total of 107 patients (89 female) with a mean age of 16 (range 11-21years) years. A total of 42 MISS and 65 open procedures were performed. Two studies reported cases for Lenke 5C exclusively while 2 reported mixed Lenke classification subtypes (Table 2A). Pre-op curve magnitude and the number of fused levels are reported in Table 2B.
Figure 1.
PRISMA 2009 flow diagram.
Table 1.
Characteristics of Included Studies.
| Study name | Year | Country | Design | Level of Evidence | Patients (n) | Type of management | N | Age (y) | Gender M/F (n) | Follow up (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| Urbanski et al | 2019 | Poland | Retrospective | III | 8 | Group 1:MISS | 4 | 15.5 | 7/1 | - |
| Cohort | Group2:Open | 4 | 21.2 | |||||||
| Zhu et al | 2017 | China | Retrospective | III | 45 | Group 1:MISS | 15 | 15.5 | 5/40 | 32 |
| Cohort | Group2:Open | 30 | 15.1 | |||||||
| Sarwahi et al | 2016 | USA | Retrospective | III | 22 | Group 1:MISS | 7 | 14.3 | 3/19 | 24 |
| Cohort | Group2:Open | 15 | 15.2 | |||||||
| Miyanji et al | 2013 | Canada | Retrospective | III | 32 | Group 1:MISS | 16 | 16.8 | 3/29 | - |
| Cohort | Group2:Open | 16 | 16.4 |
Table 2.
A: Included Studies According Lenke Classification. B: Pre-Op Curve Magnitude and Number of Fused Levels.
| A Study Name | Year | MISS | Open | ||
| Urbanski et al | 2019 | 5C | 5C | ||
| Zhu et al | 2017 | 5C | 5C | ||
| Sarwahi et al | 2016 | 1, 2,5 | 1,2,4,5,6 | ||
| Miyanji et al | 2013 | 1,2,3,4 | 1,2,3,4,6 | ||
| Pre-Op curve magnitude | number of fused levels | ||||
| B Study Name | Year | MISS | Open | MISS | Open |
| Urbanski et al | 2019 | 57.2 ± 10.6 | 47 ± 7.7 | 6.5 ± 0.8 | 5.75 ± 0.4 |
| Zhu et al | 2017 | 48.3 ± 4.2 | 50.9 ± 5.4 | 4.9 ± 0.5 | 5.7 ± 0.5 |
| Sarwahi et al | 2016 | 48.2 ± 6.8 | 46.5 ± 1.3 | 9 ± 1.7 | 11.5 ± 0.5 |
| Miyanji et al | 2013 | 56 ± 5 | 56 ± 8 | - | - |
Quality Assessment
The quality of included studies was assessed according to the Newcastle-Ottawa Scale (Table 3). Of the 4 studies, 2 were high-quality with score 8-9 and 2 were moderate with score 6-7.
Table 3.
Quality Assessment.
| Study name | Year | LOE | Selection | Comparability | Exposure | Overall score |
|---|---|---|---|---|---|---|
| Urbanski et al | 2019 | III | *** | ** | ** | 7 |
| Zhu et al | 2017 | III | **** | ** | *** | 9 |
| Sarwahi et al | 2016 | III | *** | ** | *** | 8 |
| Miyanji et al | 2013 | III | *** | ** | * | 6 |
Newcastle–Ottawa Scale.
Outcomes
Surgical correction
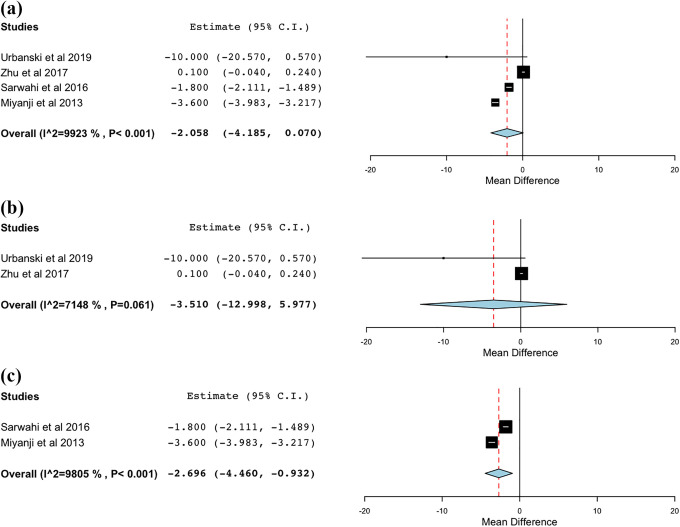
Major curve correction for MISS and open approaches is shown in Figure 2. There was no significant difference in preoperative curve magnitude between cohorts (Table 2B). There was no statistically significant difference in the major curve correction between the MISS (73.2%, CI 66.4%- 80.1%) and open (76.7%, CI 70.1%-83.3%) cohorts (MD: -2.05; CI -4.18 to 0.07; I2:99.2%). On subgroup analysis by curve type, there was similarly no statistically significant difference in curve correction between MISS (73.7%, CI 63.8%-83.6%) and open (78.3%, CI 78.1%-78.4) cohorts for Lenke 5C curves. However, there was a statistically significant difference in correction achieved for Lenke 1-4 curve types, with the MISS group (72.8%, CI 55.9%-89.65%) having a lower overall correction compared to the open group (75.5%, CI 60.4%-90.5%) (p < 0.001).
Figure 2.
Curve correction. (a) Overall; (b) Lenke 5; (c) Lenke 1-4.
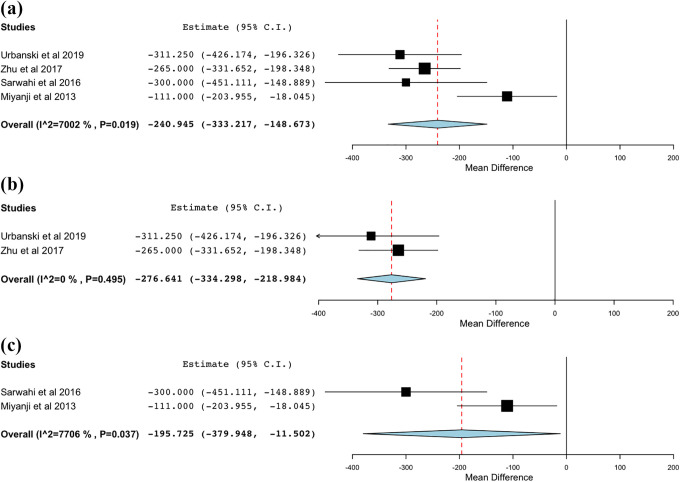
Estimated blood loss
Estimated blood loss was recorded for the open and MISS groups (Figure 3). The MISS group had significantly lower EBL (271.1 ml, CI 146.3 ml -395.8 ml) compared to the traditional open group (527 ml, CI 337.7 ml -717.7 ml) (p = 0.019). This significant difference persisted on subgroup analysis, with the MISS group having significantly lower blood loss for both the Lenke 5C (mean difference, -276.6 mL) and Lenke 1-4 (mean difference, -195.7 mL) groups.
Figure 3.
Estimated blood loss. (a) Overall; (b) Lenke 5; (c) Lenke 1-4.
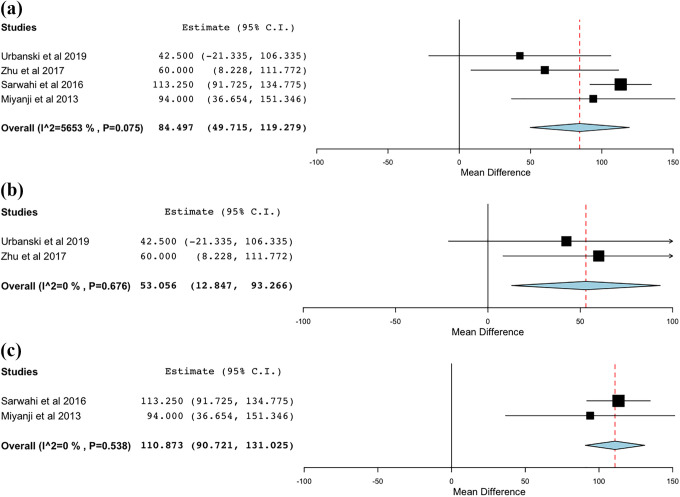
Operative time
The operative times were recorded between MISS and traditional open approaches and compared in Figure 4. Overall, the MISS approach was associated with significantly longer operative times (379.9 min, CI 229.1 min - 530.6 min) compared to the open approach (301.5 min, CI 173.3- 439.7). These differences persisted on subgroup analysis with the MISS approach having significantly longer operative time in the Lenke 5C (mean difference, 53 min) and Lenke 1-4 (mean difference, 110.8 min) groups.
Figure 4.
Operation time. (a) Overall; (b) Lenke 5; (c) Lenke 1-4.
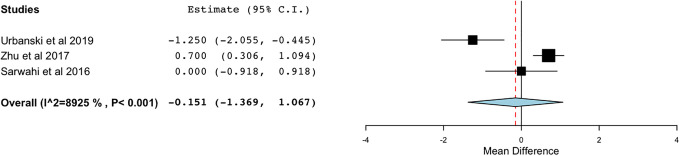
Post-operative VAS pain
VAS pain scores were reported by 3 of the studies (Figure 5). Mean pain scores were 4.1 (2.2- 6.1) for the MIS group and 4.3 (2.8-5.9) for the traditional open group with no significant difference between groups (MD: -0.15; 95% CI [-1.36, 1.06] I2: 89.2%).
Figure 5.
Pain score.
Length of stay
Length of stay was reported by 3 studies (Figure 6). Mean LOS was 5.1 days (CI 3.3 days - 7.04 days) for the MISS group and 6.4 days (CI 6.2 days - 6.7 days) for the traditional open group with no significant difference between groups (MD: -1.02; 95% CI: [-3.12, 1.06] I2: 98.7%).
Figure 6.
Hospital stay.
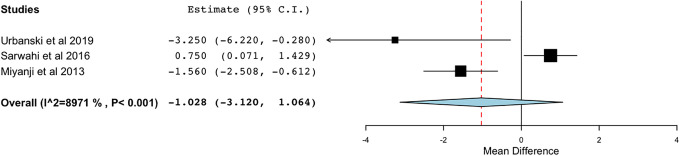
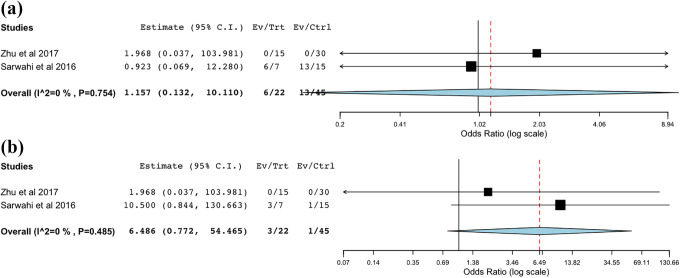
Complications and reoperation
Complications and reoperations were reported by 2 studies (Figure 7). The overall complication rate in the MISS group was 43.5% compared to 43.7% in the open cohort, with no statistical difference between the 2 (OR: 1.15; 95% CI: [0.13, 10.1] I2: 0%). Similarly, the reoperation rate between the 2 groups was not statistically significant (OR: 6.48; 95% CI: [0.77, 54.4] I2: 0%) with 18.8% in MISS group and 2.2% in open group.
Figure 7.
Overall complication (a) and reoperation rate (b).
Discussion
Traditional open techniques are considered the gold standard for the surgical management of scoliosis, though as minimally invasive spine surgery is becoming more widely practiced it is being increasingly applied to pediatric deformity correction.15-20 This meta-analysis was conducted to evaluate the differences in outcomes between open and MIS deformity correction and found that MISS is associated with less blood loss but longer operative times compared to traditional open fusion for AIS, while demonstrating similar outcomes in terms of curve correction, postoperative pain, LOS, and complications/reoperations.
MISS is emerging as a feasible tool in deformity correction, particularly in adult populations. The technique has found applications in adult degenerative scoliosis, demonstrating excellent short- and long-term radiographic and patient reported outcomes.21-24 More recently, several studies have demonstrated similar success in the treatment of AIS with minimally invasive techniques.8,9,12,14-16 Theoretical advantages include reduced soft tissue trauma, decreased blood loss, less postoperative pain, shorter hospital LOS, and fewer infections. 16 However, it is unclear if the limited exposure associated with MIS techniques limits the ability to perform an adequate correction. To our knowledge, this is the first meta-analysis to examine MISS and traditional open approaches in the surgical management of AIS. Here we demonstrate that MISS was associated with less blood loss (240 mL) compared to open surgery. We further found no differences in curve correction, postoperative pain, hospital LOS, or complications and reoperations. While there appear to be certain benefits associated with the MISS approach, this analysis did show that operative times were longer when compared to traditional open surgery, with MISS taking ∼85 minutes longer on average to perform.
A critical factor that supports the use of MISS is the reduction in intraoperative blood loss and the corresponding decreased need for intra- and postoperative blood transfusion. Managing blood loss has been a focus of deformity surgery, as it has important implications on patient outcome thought to be associated with reducing the use of allogeneic blood products, which can increase the risk for postoperative infection25,26 As a result, many efforts have been put forth to study pharmacologic agents to help limit blood loss during these procedures.27-31 In the pediatric and adolescent population these effects may be even more pronounced, as smaller overall body size increases the percentage of blood volume loss during posterior fusion. 32 Regarding transfusion requirements in the current study, the data was incompletely reported among the 4 included studies which precluded meaningful analysis. Sawarhi et al noted that 11 of 15 patients in the open group required transfusion (7 intraoperative, 4 postoperative; 73.3%) versus 1 patient in the MISS group (postoperative; 14.3%), while Zhu et al reported that 3 of 30 patients in the open group (10%) required transfusion versus none in the MIS group. Our results are consistent with the findings of prior studies, with MIS techniques demonstrating significantly less blood loss than open procedures.
In addition to blood loss, another commonly cited benefit of the MIS approach is reduced hospital LOS, as patients undergoing MIS procedures tend to show quicker recover and earlier hospital discharge. 14 While the results of our meta-analysis showed a lower mean length of stay for the MIS cohort by 1 day, this difference was not statistically significant. The data is based on the results of only 3 studies, with 2 studies (Urbanski, Miyanji) reporting reduced LOS for the MIS group and 1 study (Sarwahi et al 2016) reporting longer LOS for the MIS cohort. Sarwahi et al. may represent an outlier since the reported LOS in this study (8 and 9 days for the open and MIS cohorts, respectively) is substantially longer than what is reported in the literature.
Despite the observed advantages of MIS approaches, several important concerns must be acknowledged. Longer operative times have been consistently reported with the adoption of MIS techniques, with all included studies in our analysis noting longer OR times in the MIS cohort. Prolonged surgical times are of particular import as not only is using an operating room costly, but maintaining a patient under anesthesia for extended periods of time may have deleterious effects on perioperative morbidity. Among other possible confounders contributing to increased OR time is the use of intraoperative navigation. In this series, apart from the cohort reported by Miyanji which utilized direct visualization for the placement of pedicle screws, the remaining studies reported navigation-assisted pedicle screw placement utilizing the O-arm in the MIS cohorts. Sarwahi and Zhu report pedicle screw accuracy based on postoperative CT scan in the MIS vs open cohorts (Sarwahi et al. 90.7% vs 90.8%; Zhu et al. 93.8% vs 95.5%, respectively) noting no significant differences in accuracy of screw placement based on technique. While the literature largely supports the accuracy of navigated pedicle screw placement, less clear is the effect it may have on increasing operative times.33-35 Notably in the study by Miyanji et al the operative times were significantly longer for the MIS cohort (MIS 444 minutes vs open 350 minutes) despite using direct visualization and freehand technique. This suggests that the prolonged operative time seen in the MIS cohort is a result of the adoption and application of a new technique rather than a result of the modality used for pedicle screw placement. Given the recent adoption of MIS techniques for deformity correction, this may reflect a steep learning curve, with operative time improving with experience.21,22 Radiation exposure is an additional concern with the use of MIS techniques. While total radiation exposure has been shown to increase with the use of navigation compared to free-hand placement of pedicle screws, Urbanski et al reported no difference in radiation between MIS and open approaches. 32 Radiation exposure may therefore be more dependent upon surgeon technique/preference and less related to approach type. Use of a protective barrier, the distance and positioning of the surgeon in relation to the radiation source, and use of navigation-assisted technology to minimize persistent and cumulative radiation exposure to surgeon and staff are important factors in decreasing intraoperative radiation. 36 A final consideration in MIS deformity correction is the achievement of fusion, as reduced bony exposure may limit preparation of the fusion bed, theoretically leading to lower fusion rates. In order to optimize fusion, several authors describe the importance of direct visualization of the facet joints, enabling osteotomy/decortication (Sarwahi, Miyanji), with 1 group ultimately reporting that all MIS cases went on to solid fusion based on CT imaging (Sarwahi).
The overall complication profile and reoperation rate is important aspect of any surgical procedure, particularly 1 in the early stages of adoption. A comparable complication rate was found between both approaches in the 2 studies where they were reported, though low overall numbers preclude a meaningful comparison. The most commonly reported complications in both groups were instrumentation-related, surgical site infection or wound dehiscence, and anemia.12,14,15,16
Finally, as with any surgical procedure and technique, appropriate patient selection is paramount. Though minimally invasive surgery has many benefits, by definition there is less soft tissue dissection and exposure and therefore it may not be suitable for more severe deformities. As this is a relatively novel technique, there is no consensus on the characteristics which make a patient appropriate for MISS. Sarwahi et al. limited their indications to patients with less severe (<70 degrees) and flexible (>50% flexibility on bending films) curves. Others have focused on a narrow population of patients with Lenke type 5C curves (Urbanski, Zhu). Urbanski et al. note that early adoption of MIS may be most appropriate in patients with flexible curves and wide pedicles, making type 5C curves requiring fusion only in the lumbar and lower thoracic spine ideal initial candidates. This is supported by the finding that MISS techniques achieved less correction by percentage versus open techniques in a subgroup analysis of Lenke types 1-4. Whether these indications can be extended to include more severe and less flexible curves is unclear based on the findings of the current study.
There are several limitations associated with this study. First, as a meta-analysis, it is limited by the primary data that was reported by the included studies. These studies were all retrospective in nature and therefore could introduce selection bias with underlying differences in those undergoing MIS versus open techniques. Furthermore, the included studies are small and heterogeneous, with 2 studies focused on a narrow population of Lenke type 5C curves and 2 other studies inclusive of more curve types. We attempted to limit this drawback and further evaluate the Lenke 5C curves, where MIS techniques appear to be most applicable, by performing subgroup analysis of these patients where possible. Third, as this is an emerging technique, our study is limited to the relatively early and perhaps varied experience of several surgeons, and results may change as these surgeons gain more experience and adopt new or refined techniques. Finally, there are important variables about which we are not able to report given the lack of data, including radiation exposure and fusion rate. Further research is needed to bolster the current findings and better understand the differences between these approaches.
Conclusion
For surgeons with the appropriate training, MISS appears to be a safe and effective alternative to open posterior fusion in the surgical treatment of AIS, particularly for patients with Lenke 5C curves. While MISS has emerged as a feasible option for the surgical management of AIS, further research is warranted to compare these 2 approaches.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Qureshi reports other from Cervical Spine Research Society, personal fees from Stryker K2M, other from Simplify Medical, Inc., other from Avaz Surgical, other from International Society for the Advancement of Spine Surgery, other from North American Spine Society, other from LifeLink.com Inc., other from Association of Bone and Joint Surgeons, other from Society of Lateral Access Surgery, personal fees from Globus Medical, Inc., personal fees from Paradigm Spine, other from Society of Minimally Invasive Spine Surgery, other from Minimally Invasive Spine Study Group, personal fees from RTI Surgical Inc., other from Spinal Simplicity, LLC, personal fees from AMOpportunities, other from Contemporary Spine Surgery, other from Annals of Translational Medicine, personal fees from Healthgrades, other from The American Orthopaedic Association, other from Vital 5, outside the submitted work
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Yoji Ogura, MD, PhD  https://orcid.org/0000-0003-2007-6881
https://orcid.org/0000-0003-2007-6881
Sheeraz A. Qureshi, MD, MBA  https://orcid.org/0000-0002-7177-1756
https://orcid.org/0000-0002-7177-1756
References
- 1.Yaman O, Dalbayrak S. Idiopathic scoliosis. Turk Neurosurg. 2014;24(5):646–657. doi:10.5137/1019-5149.JTN.8838-13.0 [DOI] [PubMed] [Google Scholar]
- 2.Konieczny MR, Senyurt H, Krauspe R. Epidemiology of adolescent idiopathic scoliosis. J Chil Orthop. 2013;7(1):3–9. 10.1007/s11832-012-0457-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sud A, Tsirikos AI. Current concepts and controversies on adolescent idiopathic scoliosis: part I. Indian J Orthop. 2013;47(2):117–128. doi: 10.4103/0019-5413.108875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sud A, Tsirikos AI. “Current concepts and controversies on adolescent idiopathic scoliosis: part I”. Indian J Orthop. 2013;47(2):117–128. doi:10.4103/0019-5413.108875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shakil H, Iqbal ZA, Al-Ghadir AH. Scoliosis: review of types of curves, etiological theories and conservative treatment. J Back Musculoskelet Rehabil. 2014;27(2):111–115. doi:10.3233/bmr-130438 [DOI] [PubMed] [Google Scholar]
- 6.Janicki JA, Alman B. “Scoliosis: review of diagnosis and treatment.” Paediatrics Child Health. 2007;12(9):771–776. doi:10.1093/pch/12.9.771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lenke LG, Betz RR, Bridwell KH, et al. Intraobserver and interobserver reliability of the classification of thoracic adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1998;80(8):1097–1106. [DOI] [PubMed] [Google Scholar]
- 8.Sarwahi V, Horn JJ, Kulkarni PM, et al. Minimally invasive surgery in patients with adolescent idiopathic scoliosis. Clin Spine Surg. 2016;29(8):331–340. doi:10.1097/bsd.0000000000000106 [DOI] [PubMed] [Google Scholar]
- 9.Zhu W, Sun W, Xu L, et al. Minimally invasive scoliosis surgery assisted by O-arm navigation for Lenke Type 5C adolescent idiopathic scoliosis: a comparison with standard open approach spinal instrumentation. J Neurosurg Pediatr. 2017;19(4):472–478. doi:10.3171/2016.11.peds16412 [DOI] [PubMed] [Google Scholar]
- 10.Ovadia D. Classification of adolescent idiopathic scoliosis (AIS). J Chil Orthop. 2013;7(1):25–28. doi:10.1007/s11832-012-0459-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maruyama T, Takeshita K. Surgical treatment of scoliosis: a review of techniques currently applied. Scoliosis. 2008;3(1). doi:10.1186/1748-7161-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sarwahi V, Wollowick AL, Sugarman EP, Horn JJ, Gambassi M, Amaral TD. “Minimally invasive scoliosis surgery: an innovative technique in patients with adolescent idiopathic scoliosis.” Scoliosis. 2011;6:16. doi:10.1186/1748-7161-6-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaikumar S, Kim DH, Kam AC. History of minimally invasive spine surgery. Neurosurgery. 2002;51:S1–14. Doi:10.1097/00006123-200211002-00003 [PubMed] [Google Scholar]
- 14.De Bodman C, Miyanji F, Borner B, Zambelli PY, Racloz G, Dayer R. Minimally invasive surgery for adolescent idiopathic scoliosis. Bone Joint J. 2017;99-B(12):1651–1657. doi:10.1302/0301-620x.99b12.bjj-2017-0022.r2 [DOI] [PubMed] [Google Scholar]
- 15.Yang JH, Chang D, Suh SW, et al. Safety and effectiveness of minimally invasive scoliosis surgery for adolescent idiopathic scoliosis: a retrospective case series of 84 patients. Eur Spine J. 2020;29:761–769. 10.1007/s00586-019-06172-1 [DOI] [PubMed] [Google Scholar]
- 16.Miyanji F, Samdani A. Minimally invasive surgery for AIS: an early prospective comparison with standard open posterior surgery. J Spine. 2013. doi:10.4172/2165-7939.s5-001 [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. [DOI] [PubMed] [Google Scholar]
- 18.Wells G, Shea B, OO’Connell D, et al. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Department of Epidemiology and Community Medicine, University of Ottawa; 2004. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [Google Scholar]
- 19.Modi HN, Suh S, Hong J, Song SH, Yang JH. Intraoperative blood loss during different stages of scoliosis surgery: a prospective study. Scoliosis. 2010;5:16. 10.1186/1748-7161-5-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sarwahi V, Amaral T, Wendolowski S, et al. Minimally invasive scoliosis surgery: a novel technique in patients with neuromuscular scoliosis. Biomed Res Int. 2015;2015:481945. doi:10.1155/2015/481945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech. 2008;21(7):459–467. [DOI] [PubMed] [Google Scholar]
- 22.Anand N, Rosemann R, Khalsa B, Baron EM. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus. 2010;28(3):E6. [DOI] [PubMed] [Google Scholar]
- 23.Othman YA, Alhammoud A, Aldahamsheh O, Vaishnav AS, Gang CH, Qureshi SA. Minimally invasive spine lumbar surgery in obese patients: a systematic review and meta-analysis. HSS J. 2020;16(2):168–176. 10.1007/s11420-019-09735-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Than KD, Mummaneni PV, Bridges KJ, et al. Complication rates associated with open versus percutaneous pedicle screw instrumentation among patients undergoing minimally invasive interbody fusion for adult spinal deformity. Neurosurg Focus. 2017;43(6):E7. doi:10.3171/2017.8.FOCUS17479 [DOI] [PubMed] [Google Scholar]
- 25.Schwarzkopf R, Chung C, Park JJ, Walsh M, Spivak JM, Steiger D. Effects of perioperative blood product use on surgical site infection following thoracic and lumbar spinal surgery. Spine (Phila Pa 1976). 2010;35(3):340–346. [DOI] [PubMed] [Google Scholar]
- 26.Shen J, Liang J, Yu H, Qiu G, Xue X, Li Z. Risk factors for delayed infections after spinal fusion and instrumentation in patients with scoliosis. Clinical article. J Neurosurg Spine. 2014;21(4):648–652. [DOI] [PubMed] [Google Scholar]
- 27.Wang M, Zheng XF, Jiang LS. Efficacy and safety of antifibrinolytic agents in reducing perioperative blood loss and transfusion requirements in scoliosis surgery: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0137886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sethna NF, Zurakowski D, Brustowicz RM, Bacsik J, Sullivan LJ, Shapiro F. Efficacy of tranexamic acid on surgical bleeding in spine surgery: a meta-analysis.[Spine J. 2015] Tranexamic acid reduces intraoperative blood loss in pediatric patients undergoing scoliosis surgery. Anesthesiology. 2005;102(4):727–732. [DOI] [PubMed] [Google Scholar]
- 29.Neilipovitz DT, Murto K, Hall L, Barrowman NJ, Splinter WM. A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg. 2001;93(1):82–87. [DOI] [PubMed] [Google Scholar]
- 30.Verma K, Errico T, Diefenbach C, et al. The relative efficacy of antifibrinolytics in adolescent idiopathic scoliosis: a prospective randomized trial. J Bone Joint Surg Am. 2014;96(10):e80. [DOI] [PubMed] [Google Scholar]
- 31.Jones KE, Butler EK, Barrack T, et al. Tranexamic acid reduced the percent of total blood volume lost during adolescent idiopathic scoliosis surgery. Int J Spine Surg. 2017;11(4):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jain A, Sponseller PD, Newton PO, et al. Harms study group. J Bone Joint Surg Am. 2015;97(6):507–511. [DOI] [PubMed] [Google Scholar]
- 33.Mason A, Paulsen R, Babuska JM, et al. The accuracy of pedicle screw placement using intraoperative image guidance systems. J Neurosurg Spine. 2014;20(2):196–203. doi:10.3171/2013.11.SPINE13413 [DOI] [PubMed] [Google Scholar]
- 34.Tajsic T, Patel K, Farmer R, Mannion RJ, Trivedi RA. Spinal navigation for minimally invasive thoracic and lumbosacral spine fixation: implications for radiation exposure, operative time, and accuracy of pedicle screw placement. Eur Spine J. 2018;27(8):1918–1924. [DOI] [PubMed] [Google Scholar]
- 35.Ling JM, Dinesh SK, Pang BC, et al. Routine spinal navigation for thoraco–lumbar pedicle screw insertion using the O-Arm three-dimensional imaging sys- tem improves placement accuracy. J Clin Neurosci. 2014;21(3):493–498. [DOI] [PubMed] [Google Scholar]
- 36.Yu E, Khan SN. Does less invasive spine surgery result in increased radiation exposure? A systematic review. Clin Orthop Relat Res. 2014;472(6):1738–1748. doi:10.1007/s11999-014-3503-3 [DOI] [PMC free article] [PubMed] [Google Scholar]