Abstract
We examine how trust shapes compliance with public health restrictions during the COVID- 19 pandemic in Uganda. We use an endorsement experiment embedded in a mobile phone survey to show that messages from government officials generate more support for public health restrictions than messages from religious authorities, traditional leaders, or international NGOs. We further show that compliance with these restrictions is strongly positively correlated with trust in government, but only weakly correlated with trust in local authorities or other citizens. We use measures of trust from both before and during the pandemic to rule out the possibility that trust is a function of the pandemic itself. The relationship between trust and compliance is especially strong for the Ministry of Health and—more surprisingly—the police. We conclude that trust is crucial for encouraging compliance but note that it may be difficult to sustain, particularly in settings where governments and police forces have reputations for repression.
Keywords: COVID-19 pandemic, Trust in government, Uganda, Survey experiments, Policing, Public health
The COVID-19 pandemic has laid bare the crucial role that trust plays in generating and sustaining compliance with public health directives during times of crisis. It has also brought into stark relief the many “varieties” of trust that shape behavior when public health is at stake. Citizens are expected to trust public health authorities to diagnose public health threats accurately and recommend policies to mitigate them effectively. They are expected to trust elected officials to enact those policies quickly and faithfully, and trust law enforcement agencies to enforce them equitably. They are expected to trust the safety and efficacy of treatments and vaccines, many of which are developed by the private sector (e.g. pharmaceutical companies). Especially in lower income countries, citizens are also expected to trust international NGOs and foreign aid agencies that are involved in disseminating vaccines and treatments to the public.
Trust in these various institutions matters because it increases the likelihood that citizens will take actions that are costly and disruptive for them as individuals, but necessary for public health (Kahan, 2003). Especially in the early stages of the COVID-19 pandemic, when access to testing was limited and treatments and vaccines had not yet been developed, compliance with social distancing policies, masking, and other public health measures was crucial for reducing the transmission of the virus (Haug et al., 2020; Kraemer et al., 2020). Because these policies imposed tight constraints on citizens’ social and economic lives, compliance was imperfect, and some degree of resistance was likely unavoidable. But the consequences of non-compliance were often severe, and refusal to adhere to COVID-19 public health restrictions has been linked to spikes in caseloads in countries around the world (Flaxman et al., 2020; Yilmazkuday, 2021).
A small but growing body of research has documented the importance of trust as a predictor of compliance during previous public health emergencies, especially the 2013–16 Ebola epidemic in West Africa (Blair et al., 2017; Tsai et al., 2020) and the 2018–19 Ebola crisis in the Democratic Republic of Congo (Vinck et al., 2019). Others have demonstrated the importance of trust during the COVID-19 pandemic (Bargain and Aminjonov 2020). These studies have taught us much about the relationship between trust and compliance with public health measures. But most have operationalized trust in rather coarse ways, ignoring potentially significant variation in the types of agencies and authorities that citizens do and do not trust, and the types of public health messages they do and do not find persuasive (for exceptions focused on Guinea and Malawi, respectively, see Arriola and Grossman, 2020; Kao et al., 2021).
We argue that trust is important at four distinct but interrelated stages of pandemic response, which we call diagnosis, regulation, promulgation, and enforcement. Various governmental and non-governmental actors are responsible for each of these steps. First, public health officials and international NGOs must diagnose the causes and transmission pathways of a new public health threat. Next, government officials must pass new regulations to contain the threat. A variety of state and non-state actors—including government officials, religious authorities, local civil society leaders, and the media—then must promulgate information about the threat and the new regulations. Finally, government institutions—most commonly the police—must enforce these new regulations to ensure compliance. Citizens may express varying levels of trust in these distinct actors and institutions, with potentially important implications for their willingness to comply with public health restrictions. But most existing studies use measures of trust that are too broad to capture these subtle but crucial distinctions. Moreover, existing studies typically overlook the importance of trust in institutions that are only tangentially involved in public health in high-income countries, but that serve as the primary (and sometimes only) enforcers of public health restrictions in many low-income countries—in particular, the police.
We extend the existing literature by asking two interrelated questions. First, which authorities are most effective in persuading citizens to accept costly and disruptive restrictions on their behavior during public health emergencies? Are messages from local religious leaders more effective than messages from international NGOs? Are messages from traditional (or “customary”) authorities more persuasive than messages from the government? Second and related, of the varieties of trust described above, which is most important in generating actual compliance with public health restrictions? In the context of low-income countries where reliable information is often hard to come by, is trust in public health authorities more important than trust in government as a whole? Is trust in the police more important than trust in other community members?
We answer these questions through interconnected observational and experimental studies in Uganda. Using an endorsement experiment embedded in a mobile phone survey conducted during the pandemic, we first show that messages from government officials are more effective at generating support for public health restrictions than messages from religious authorities, traditional leaders, or international NGOs. We then show that compliance with these restrictions is strongly positively correlated with trust in government, but only weakly (and in some cases negatively) correlated with trust in local authorities or other citizens. One key advantage of our study is that we employ measures of trust collected before the onset of the pandemic, demonstrating that pre-pandemic levels of trust—in addition to measures of trust from during the pandemic—help explain variation in individuals' compliance with costly measures to contain the virus's spread.
The correlation between compliance and trust in government does not appear to be an artifact of misinformation or misunderstanding of the virus among less trusting respondents: if anything, respondents who express less trust in government are more knowledgeable about COVID-19. This echoes similar findings from research on the Ebola epidemic in Liberia (Blair et al., 2017). The correlation also does not appear to be an artifact of social desirability bias: using a pair of list experiments, we show that respondents do not overreport compliance with public health restrictions in the context of the survey. Disaggregating these results further, we show that while trust in all government agencies is positively correlated with compliance, the relationship appears to be especially strong for trust in the Ministry of Health and—perhaps more surprisingly—the police. This latter result may reflect the pivotal (yet controversial) role that the police have played in enforcing social distancing policies in Uganda and other African countries, often resulting in human rights abuses (Aborisade, 2021; Grasse et al., 2021). However, as a recent study of community policing in six low-income countries—including Uganda—suggests, it is far from easy to build trust in state institutions where it is lacking (Blair et al., 2021). We conclude that trust is crucial but sticky, and that changing it may require more intensive interventions before a crisis strikes (Haim et al., 2021).
1. Theoretical framework
Recent studies have documented the myriad ways that trust in government has shaped citizens’ willingness to comply with public health directives during the COVID-19 pandemic (Lalot et al., 2022; Pagliaro et al., 2021). In the US, for example, one study finds that counties with high trust in government decreased their mobility significantly more than counties with low trust after lock-downs were imposed (Brodeur et al., 2020). In the UK, another study demonstrates that citizens who expressed greater trust in government were more likely to comply with government-imposed social distancing policies (Moxham-Hall and Strang 2020). Trust has been shown to correlate with COVID-19 mortality and other important outcomes as well. For example, one study finds that trust in government is negatively correlated with COVID-19 deaths across 25 European countries (Oksanen et al., 2020). While in some settings (e.g. the US) this correlation is mediated by partisanship (Goldstein and Wiedemann 2021; Grossman et al., 2020), overall, the relationship between trust and compliance is clear. These studies complement and extend an existing literature focused on the relationship between trust and compliance during earlier epidemics, including Ebola (Blair et al., 2017; Dhillon and Kelly 2015; Tsai et al., 2020; Van der Windt and Voors, 2020), HIV/AIDS (Dionne and Poulin, 2013), and H1N1 (Freimuth et al., 2014).
Most existing studies characterize the relationship between trust in government and compliance with public health guidelines as simple and straightforward. We argue, instead, that trust may shape citizens’ behavior at four distinct but interrelated links in a more complex causal chain consisting of diagnosis, regulation, promulgation, and enforcement. At the first link in the chain, the nature of a given public health threat must be diagnosed, and mechanisms for curtailing it must be identified. This role is typically played by public health officials (e.g. a Ministry of Health), supported in many cases by international or multinational NGOs (e.g. the World Health Organization). At the second link, regulations must be passed to codify and systematize measures for containing the threat.
This role is usually played by government officials at all levels—not just the central government, but state, district, and municipal government officials (e.g. mayors) as well. At the third link in the chain, information about these regulations must be promulgated to the public. This role tends to be more widely shared. In highly religious communities, for example, priests, imams, and other religious leaders may encourage their congregations to abide by public health laws by canceling services or encouraging congregants to worship in private. In rural areas of low-income countries, where information and communication technologies may be unreliable or inaccessible, local leaders, chiefs, and other traditional or “customary” authorities may communicate information to ensure that citizens are aware of new public health regulations (Dionne, 2017; Van der Windt and Voors, 2020). Finally, at the fourth link in the chain, compliance with these regulations must be enforced, and non-compliance must be punished. This role falls most obviously on the police, who can use or threaten coercion to induce compliance. Less obviously but potentially equally important, other community members can engender compliance through social sanctions (e.g. naming and shaming).
Trust may be critical at each link in this chain. If citizens do not trust public health authorities to accurately diagnose a given public health threat and propose effective mechanisms to mitigate it, they may refuse to comply with subsequent public health regulations even if they trust the government officials responsible for enacting them. Conversely, if citizens do not trust government officials to pass laws that faithfully adhere to public health authorities’ recommendations, they may circumvent any new restrictions on their behavior, even if they trust the recommendations on which those restrictions are (ostensibly) based. If citizens do not trust local leaders to disseminate information about public health laws accurately, then they may ignore the information they receive, even if they trust the government officials responsible for passing public health laws in the first place. Finally, if citizens do not trust the police or other community members to enforce public health restrictions fairly, they may choose to comply only when their behavior is easily observable, even if they trust the information they receive about the restrictions being imposed and the government officials responsible for imposing them.
To fix ideas, consider the example of face masks, which have been repeatedly shown to be effective for limiting the transmission of COVID-19 (Chu, Derek K., et al., 2020). Despite this record of effectiveness, many citizens around the world resisted (and continue to resist) wearing face masks, even before the availability of vaccines. Some did so because they did not trust public health authorities and their claims about the efficacy of face masks; others resisted because they did not trust the government officials responsible for passing laws mandating the use of face masks in public (Taylor and Asmundson, 2021). Some resisted because they did not trust the actors responsible for disseminating information about mask mandates. In the US, for example, some analysts have attributed low levels of masking in Orthodox Jewish neighborhoods in part to the lack of trusted, Yiddish-speaking contact tracers who could disseminate information about masks’ effectiveness (Armus, 2020). Finally, some citizens resisted because they distrusted the institutions responsible for enforcing mask mandates. Again in the US, some Black Americans refused to wear face masks because they believed doing so would invite harassment by the police (McFarling, 2020; Taylor, 2020).
Most studies of trust and compliance during the COVID-19 pandemic focus on aggregate, highly generalized measures of trust in government (Bargain and Aminjonov 2020) or other citizens (Goldstein and Wiedemann 2021). We argue that this approach may obscure theoretically and empirically significant variation in citizens’ attitudes towards different individuals and institutions. Variation of this sort may have especially important implications for compliance in settings where different authorities at different levels of government enact conflicting policies, and where those policies attract opposition or support from conflicting civil or religious groups. In Brazil, for example, state governors and city mayors imposed restrictions on public gatherings that would have forced many churches to close, at least temporarily. Church leaders resisted these measures, encouraging their congregations to gather in person. The Brazilian Supreme Court sided with the governors and mayors; President Jair Bolsonaro sided with the church (Pooler, 2021; Dunn and Laterzo, 2021). Similar clashes over policy emerged in many countries. Under these conditions, the magnitude and even the direction of the correlation between trust and compliance may depend crucially on the object of that trust—a possibility that existing scholars generally have not explored (Devine et al., 2021).
2. Setting
Our study focuses on Uganda, an electoral authoritarian regime that has been ruled by the same party (the National Resistance Movement, or NRM) and president (Yoweri Museveni) since 1986. Uganda is an instructive setting for our study due to its similarities with many other low-income countries. Uganda is in the mid-range of the World Bank's ranking of low-income countries in terms of economic development (as captured by GDP per capita) and human development (as captured by HDI). Authoritarian regimes that hold periodic elections like the one in Uganda are common throughout the Global South, and are the modal regime type in sub-Saharan Africa (Weghorst, 2022). As with any study of a single country, we cannot know for certain how far our results will travel. Nonetheless, these similarities suggest that lessons learned in Uganda may be generalizable to other African countries, and potentially to other developing countries as well.
The Ugandan government's reliance on international NGOs and domestic non-state actors to respond to past public health crises highlights the importance of examining citizens' attitudes towards these actors. For example, Youde (2007) argues that one reason why Uganda was more effective than South Africa at battling HIV/AIDS was the high value that Museveni and the NRM placed on interdependence and connections with Western states. Others have highlighted the critical role that local NGOs (Kaleeba et al., 1997) and donor relations played in Uganda relative to South Africa (Parkhurst and Lush, 2004). Uganda's effective response to the HIV/AIDS epidemic appears to have bolstered the state's legitimacy both domestically and internationally (Parkhurst, 2005). However, examining Uganda's level of preparedness in responding to an Ebola outbreak in 2019, Schmidt-Sane et al. (2020) suggest that lingering distrust in political authorities negatively affected (distrusting) communities' responses.
Whether and how this lingering distrust has shaped compliance during the COVID-19 pandemic remains an open question. Early in the pandemic, the Ugandan central government oversaw the implementation of public health directives in partnership with district governments, which are the highest tier of government below the national level. On March 24, 2020, three days after the pandemic was formally announced in Uganda, the government published a comprehensive set of regulations to control the transmission of the virus (The Public Health Control of COVID-19 Rules, 2020). These rules specified the responsibilities of government officials and health and medical practitioners, and also imposed a set of restrictions on individual behavior punishable by law. These included a duty to report COVID-19 cases to the authorities (article 3) and a ban on attending large public gatherings such as bars and movie theaters (article 9b), churches and mosques (article 9c), wedding parties, vigils, and funerals (article 9e), and political rallies and cultural conferences (article 9f). The regulations also mandated quarantines for anyone with direct contact with COVID-19 patients. On May 4, Museveni announced a mask mandate and extended a lockdown that had already been in place since April 1 (Reuters, 2020; XinhuaNet, 2020).
The Uganda Police Force (UPF) has been actively involved in enforcing these policies, and has in some cases engaged in excessive force to punish non-compliance. UPF officers have also used the pandemic as a pretext to suppress protests by opposition politicians and their supporters, including, most notably, the musician-turned-activist Bobi Wine (Burke and Okiror 2020). The police have justified these abuses as necessary to contain the transmission of the virus, but in many cases their actions have disproportionately targeted critics of the ruling party (Okiror and Burke 2020). This is part of a more general pattern in which Museveni and the NRM deploy the UPF to harass, intimidate, imprison, and in some cases kill members of the opposition (Curtice and Behlendorf, 2021). Some UPF officers also helped distribute food aid, at least early in the crisis.
Other actors and institutions also played a key role in educating the public about ways to reduce the risk of COVID-19 transmission. These include Local Council chairpersons (LC1s), traditional leaders, religious authorities, and local and international NGOs. Following the government's guidelines, several traditional leaders—most notably the Kabaka (king) of the Buganda Kingdom, Ronald Muwenda Mutebi II—issued public statements about the importance of respecting social distancing measures and mask mandates (The Independent, 2020).
Top clerics of various Christian denominations also issued proclamations banning church gatherings across the country (Isiko, 2020). These efforts by traditional and religious leaders continued as the pandemic progressed. In March 2021, for example, the Archbishop of the Church of Uganda, Dr. Stephen Kaziimba Mugalu, appealed to leaders at all levels to help debunk fears and misconceptions about the AstraZeneca vaccine and to encourage their followers to get vaccinated (The Independent, 2021). Whether these messages have been effective remains an open question.
3. Research design
3.1. Sample
To test which authorities are most effective in generating support for public health restrictions, we use both experimental and observational data from an original panel survey conducted both before and during the pandemic in Uganda. Our sample includes 2587 respondents across 288 villages spanning 13 districts and all four regions of Uganda—north, central, east, and west. (Uganda is divided into 134 districts; our survey covers Mbarara, Lira, Mbale, Gulu, Mityana, Kamuli, Jinja, Tororo, Iganga, Kabale, Rakai, Arua, and Ntungamo.) We selected these districts in coordination with the government to ensure equal representation of Uganda's four regions in an unrelated community policing study completed prior to the onset of the pandemic. The 13 study districts look roughly similar to other districts in Uganda based on 2014 census data, as shown in Table B.1. The districts in our sample have slightly higher average population, age, and education but are similar on other dimensions.
We randomly sampled six male and six female respondents in each village to participate in a survey in June and July 2018 (baseline), for a total of 3456 respondents. These same respondents were resurveyed between July and September 2020 (endline). Both survey rounds were administered by Innovations for Poverty Action (IPA), Uganda. The baseline survey was conducted in person; the endline was implemented during the pandemic amidst the government's recently imposed restrictions on travel and public gatherings, and was therefore conducted by mobile phone in order to mitigate any potential risks to the health of our enumerators and respondents. Further details on these surveys and sample composition can be found in the appendix..
Given the upheaval of the pandemic, and the change in survey method, it is perhaps unsurprising that we observed an attrition rate of roughly 35% between baseline and endline. Of the 3456 respondents interviewed at baseline, 2245 could be reached to complete the mobile phone survey at endline. Differences produced by this attrition rate are shown in Table A.2 in the appendix. Compared to the baseline respondents lost to attrition, endline respondents are more likely to be married and have children, have more education, and have higher employment and income. Baseline measures of trust are typically more balanced but we also see that the endline sample is somewhat less trusting of the district government, the central government, and the police.
3.2. Endorsement experiment
Our mobile phone survey included an endorsement experiment that allows us to test whether respondents’ support for public health guidelines varies with the identity of the authority with whom those guidelines are associated. Respondents were randomly assigned to hear two messages attributed to one of four authorities: the government, international NGOs, traditional leaders, or religious authorities. Importantly, attrition between baseline and endline cannot bias our analysis of the endorsement experiment, as treatment assignment was randomized at the individual level at endline only. The two messages included endorsements of two policies: a ban on public gatherings and a recommendation that citizens maintain six feet of social distance while interacting with anyone other than family members. Respondents were randomly assigned to the same condition (and thus the same endorser) in both experiments.
They were then asked how much they support each of the two policies on a 5-point scale. Specifically, they were asked, first, “[Government/International NGOs/Traditional leaders/Religious leaders] say there can be no large public gatherings and no church or mosque at this time. Do you disagree or agree with this rule?” And second, “[Government/International NGOs/Traditional leaders/Religious leaders] say we should maintain a distance of 2 m between people outside of the same household. Do you disagree or agree with this suggestion?”
3.3. Observational design
The survey also included modules of questions on trust in a variety of state and non-state actors, knowledge of COVID-19, perceptions of public health restrictions, and compliance with those restrictions. We use these modules to test the observational relationship between compliance and different “varieties” of trust, and between trust and knowledge of COVID-19. To measure knowledge of COVID-19, respondents were asked a series of simple factual questions about who can contract the virus, whether there is a “cure,” and the symptoms of infection. To measure public health compliance, respondents were asked seven questions about their behavior over the preceding seven days, including avoiding large public gatherings and wearing masks.
3.4. List experiments
To address potential social desirability concerns, we also administered two list experiments designed to measure violations of Uganda's mask mandate and its ban on attending religious services outside the home. Respondents were randomly assigned to the same condition, treatment or control, for both experiments. In the first experiment, respondents were asked whether they had engaged in each of four activities in the last seven days. The list included three non-sensitive items (“You went for a stroll outside the house;” “You asked a relative for a small loan; ” “You sent someone mobile money”) and one sensitive item (“You walked around the village without a face mask”).
For the second experiment, respondents were again asked whether they had engaged in each of four activities in the last seven days, including three non-sensitive items (“You were asked by a relative for a large loan;” “You had to skip some meals;” “You spoke about coronavirus with a friend or family member”) and one sensitive item (“You attended church or mosque service”). Respondents were asked to report the number of activities they had engaged in without specifying which ones, thus allowing them to report any non-compliance indirectly.
4. Results
4.1. Endorsement experiment
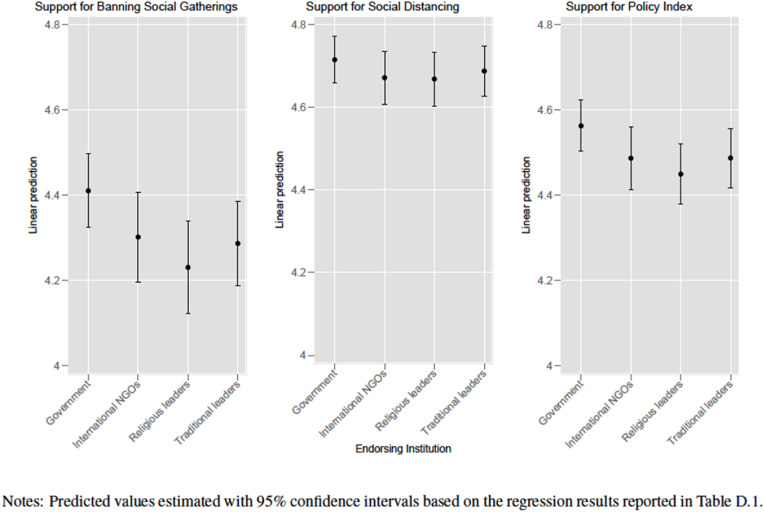
Our endorsement experiment is designed to address whether some authorities are more effective than others at convincing citizens to adhere to restrictions during public health crises. Fig. 1 plots predicted values and 95% confidence intervals based on the regression results reported in Table D.1. The dependent variables in panels 1 and 2 are 5-point Likert scales measuring support for the government's ban on public gatherings (panel 1) and its recommendations for social distancing outside the home (panel 2). The dependent variable in panel 3 is a mean index of support for the two policies. We regress each dependent variable on dummies indicating endorsement by international NGOs, religious authorities, and traditional leaders; the base category is endorsement by the government. Standard errors are clustered at the village level. We do not include any control variables, though our results are substantively similar if we do.
Fig. 1.
Endorsement Experiment. Notes: Predicted values estimated with 95% confidence intervals based on the regression results reported in Table D.1.
On average, we find that respondents expressed greater support for the ban on public gatherings when it was endorsed by the government than when it was endorsed by any of the other three authorities (panel 1). The differences between the government's endorsement and those of religious leaders and traditional leaders are statistically significant at the 95% confidence level. As we show in Figure D.1, predicted levels of support for the ban are not statistically distinguishable across the three non-governmental treatment groups. A similar but weaker pattern holds for social distancing guidelines (panel 2), though in this case our treatment effect estimates are not statistically different from one another at conventional thresholds. This could be due in part to ceiling effects, since overall support for social distancing was higher than support for the ban on gatherings. The ban on gatherings is also arguably more onerous than the guidelines on social distancing, especially in a rural setting; it could be that government endorsement is especially important for public health restrictions that severely curtail citizens' activities. Respondents also expressed greater support for the two policies combined when they were endorsed by the government, rather than by international NGOs, traditional leaders, or religious authorities (panel 3). Finally, it appears these differences are indeed driven by the endorsement and not imbalance in characteristics across experimental conditions. Table D.2 shows that the treatment conditions are well-balanced across demographic categories, partisanship, and trust.
4.2. Observational analysis
Our endorsement experiment suggests that government officials are more effective at generating support for public health restrictions than other domestic (e.g. traditional leaders and religious authorities) or foreign (e.g. international NGOs) actors, even in an autocracy in which citizens may have cause to distrust the government. Is trust in government also important for ensuring actual compliance with these public health policies? Is it more important than trust in more localized (and less overtly politicized) authorities? Is it more important than trust in other citizens—i.e. “social trust?” As we discuss in our theoretical framework, even within the government, a variety of different actors and agencies are responsible for enacting and enforcing public health restrictions. Which “variety” of trust is most important for promoting compliance? Observational analysis of our mobile phone survey data allows us to answer these questions.
We measure compliance with a standardized summary index (following Anderson (2008)) comprising seven items, scaled such that larger values indicate greater compliance: 1) number of days spent at home without leaving; 2) number of times attending church or mosque; 3) number of times going to a restaurant, bar, or cafe; 4) number of times attending a community meeting; 5) number of times attending large social gatherings like weddings, funerals, or parties; 6) frequency practicing social distancing; and 7) frequency of using a mask when in public. These measures are positively correlated (Cronbach's alpha = 0.36). The summary index maximizes the amount of information it captures by using a weighted mean of the standardized outcomes, where the weights are the inverse of the covariance matrix.
We measure trust in government with a standardized additive index comprising trust in government institutions. Our in-person baseline survey included questions about four government institutions: trust in the central government, district government, subcounty (or LC3) government, and the police (Cronbach's alpha = 0.65). In our follow-up mobile phone survey we included questions about trust in the central government, the Ministry of Health, the district government, and the police (Cronbach's alpha = 0.70). As we show in Table D.3 in the appendix, there is a positive correlation between these different varieties of trust, but they are not so highly correlated as to suggest that they are simply proxies for the same underlying phenomenon. We also measure trust in other members of the community and trust in the village head (referred to in Uganda as LC1 chairperson). These are potentially important local forms of trust that are less directly related to trust in government, both theoretically and—as we show in Table D.3—empirically.
Table 1 presents results from a series of OLS regressions where the dependent variable is our compliance index. The key independent variables of interest are 1) trust in government, 2) trust in the LC1 chairperson, and 3) trust in other community members. The top panel uses baseline measures of these trust variables, while the bottom panel uses endline measures from our mobile phone survey. While these are correlations rather than relationships of cause and effect, we include a host of covariates and village fixed effects to mitigate confounding. Covariates include information on respondents’ gender, age, education, and average monthly income over the last 3 months as measured at baseline (i.e. pre-pandemic). To facilitate comparison, all continuous and categorical variables (including our three measures of trust) are standardized such that a one unit increase is equivalent to a shift of one standard deviation on that variable.
Table 1.
Correlates of public health compliance.
| Top Panel: Baseline Measures of Trust | ||||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Trust in Government (Index) | 0.07* | 0.06* | ||
| (0.03) | (0.03) | |||
| Trust LC1 | 0.03 | 0.01 | ||
| (0.02) | (0.03) | |||
| Trust People in Community | 0.04 | 0.02 | ||
| (0.03) | (0.03) | |||
| Female | 0.27*** | 0.28*** | 0.29*** | 0.27*** |
| (0.05) | (0.05) | (0.05) | (0.05) | |
| Age | 0.04 | 0.04+ | 0.04 | 0.04 |
| (0.03) | (0.03) | (0.03) | (0.03) | |
| Education | −0.00 | −0.00 | −0.00 | −0.00 |
| (0.03) | (0.03) | (0.03) | (0.03) | |
| Income | −0.01 | −0.00 | −0.00 | −0.00 |
| (0.04) | (0.04) | (0.04) | (0.04) | |
| Constant | −0.66*** | −0.57*** | −0.62*** | −0.63*** |
| (0.05) | (0.08) | (0.05) | (0.08) | |
| Village Fixed Effects | YES | YES | YES | YES |
| Observations | 1905 | 1905 | 1905 | 1905 |
| Bottom Panel: Follow-up Measures of Trust | ||||
| (5) |
(6) |
(7) |
(8) |
|
| Trust in Govt (Index) | 0.10*** | 0.09** | ||
| (0.03) | (0.03) | |||
| Trust LC1 | 0.05+ | 0.01 | ||
| (0.03) | (0.03) | |||
| Trust People in Community | 0.05* | 0.03 | ||
| (0.03) | (0.03) | |||
| Female | 0.25*** | 0.29*** | 0.29*** | 0.26*** |
| (0.05) | (0.05) | (0.05) | (0.05) | |
| Age | 0.04 | 0.04+ | 0.04 | 0.04 |
| (0.03) | (0.03) | (0.03) | (0.03) | |
| Education | 0.00 | −0.00 | −0.00 | 0.00 |
| (0.03) | (0.03) | (0.03) | (0.03) | |
| Income | 0.00 | −0.01 | −0.00 | 0.00 |
| (0.04) | (0.04) | (0.04) | (0.04) | |
| Constant | −0.72*** | −0.69*** | −0.72*** | −0.76*** |
| (0.05) | (0.05) | (0.06) | (0.06) | |
| Village Fixed Effects | YES | YES | YES | YES |
| Observations | 1905 | 1905 | 1905 | 1905 |
Notes: OLS regression models with S.E.‘s clustered at the village level (in parentheses). DV: Index of public health compliance.
+p < 0.10, *p < 0.05, **p < 0.01, ***p < 0.001.
As in the endorsement experiment, we find that trust in government is consistently positively correlated with compliance with public health restrictions. Across all models, the point estimate on trust in government is about twice the size of the point estimates on trust in the village head (LC1 chairperson) or trust in other community members. At baseline, these more local varieties of trust appear to have little to no relationship with compliance, though the correlation becomes positive and weakly statistically significant at endline.
In contrast, trust in government remains strongly positively correlated with compliance even after accounting for demographics, village fixed effects, and the other types of trust. It remains robust to specifications that account for NRM partisanship (Table D.4), those that exclude control variables (see Table D.6), and those that cluster standard errors at the district level (Table D.8). While noting that our measure of NRM support was gathered after the onset of the pandemic, this result is important given that NRM support is key to understanding citizens' perceptions of government in Uganda, where the ruling party systematically favors its own loyalists over supporters of the opposition. Our results suggest that trust in government still helps explain public health compliance even when conditioning on this key predictor of citizens’ perceptions.
Table 1 tests the relationship between compliance and trust in government broadly defined. But as noted above, the state is not a unitary actor, and perceptions of different government institutions may vary in ways that are consequential for compliance with public health measures. It is also possible that specific government agencies may vary in their importance for promoting compliance with public health restrictions. To explore this possibility, in Table 2 we disaggregate our index of trust in government into its constituent parts. At baseline, we use measures of trust in the central government, the district government, the LC3 government, and the UPF. At endline, we use measures of trust in the central government, the Ministry of Health, the district government, and the UPF. While these four measures are moderately positively correlated with one another in both survey waves, there is enough variation in perceptions that we can generate at least suggestive evidence about the relative importance of different varieties of trust for explaining public health compliance.
Table 2.
Disaggregating trust in the state.
| Top Panel: Baseline Measures of Trust | |||||
|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | |
| Trust Central Govt | 0.05+ | 0.03 | |||
| (0.03) | (0.03) | ||||
| Trust Police | 0.06* | 0.05+ | |||
| (0.03) | (0.03) | ||||
| Trust District Govt | 0.03 | 0.00 | |||
| (0.02) | (0.03) | ||||
| Trust in LC3 Govt | 0.04 | 0.02 | |||
| (0.03) | (0.03) | ||||
| Constant | −0.65*** | −0.65*** | −0.66*** | −0.66*** | −0.66*** |
| (0.05) | (0.05) | (0.05) | (0.05) | (0.05) | |
| Demographic Controls | YES | YES | YES | YES | YES |
| Village FE | YES | YES | YES | YES | YES |
| Observations | 1905 | 1905 | 1905 | 1905 | 1905 |
| Bottom Panel: Follow-up Measures of Trust | |||||
| (6) |
(7) |
(8) |
(9) |
(10) |
|
| Trust Central Govt | 0.07* | 0.02 | |||
| (0.03) | (0.03) | ||||
| Trust Police | 0.08** | 0.05 | |||
| (0.03) | (0.03) | ||||
| Trust District Govt | 0.05+ | 0.02 | |||
| (0.03) | (0.03) | ||||
| Trust MoH | 0.08** | 0.05+ | |||
| (0.03) | (0.03) | ||||
| Constant | −0.69*** | −0.62*** | −0.72*** | −0.68*** | −0.69*** |
| (0.05) | (0.05) | (0.06) | (0.05) | (0.07) | |
| Demographic Controls | YES | YES | YES | YES | YES |
| Village FE | YES | YES | YES | YES | YES |
| Observations | 1905 | 1905 | 1905 | 1905 | 1905 |
Notes: OLS regression models with S.E. clustered at the village level (in parentheses). Each model includes covariates for gender, age, education, and average monthly income levels at baseline.
DV: Index of public health compliance.
+p < 0.10, *p < 0.05, **p < 0.01, ***p < 0.001.
We find that the most consistent correlates of compliance are trust in the police and the Ministry of Health. As shown in Table 2 , trust in the police is statistically significantly correlated with compliance even when controlling for other types of trust in government (column 5). Meanwhile, trust in the central, district, and LC3 governments are only weakly correlated with compliance. The point estimates for these variables are small across baseline specifications, and are typically not statistically significant. Using endline measures, trust in the Ministry of Health and the UPF are more strongly positively correlated with compliance (both statistically significant at the 99% confidence level), with larger point estimates. (We note, however, that contemporaneous measures of trust may suffer from “post-treatment” bias in that trust in the government may be affected by the government's pandemic response.)
When combining all endline measures of trust (column 10), the Ministry of Health variable remains statistically significant at the 90% confidence level (p ≤ 0.08), while the police variable falls just outside that level (p ≤ 0.14). These results remain similar when examining alternative specifications with NRM support as a covariate (see Table D.5), with no control variables (see Table D.7), and with standard errors clustered at the district level (see Table D.9). The UPF and the Ministry of Health have been at the forefront of the government's response to COVID-19, though with different roles. In the language of our theoretical framework, the Ministry of Health has led efforts to diagnose the nature of the crisis and the restrictions needed to reduce its transmission, while the UPF has assumed responsibility for enforcing those restrictions (sometimes with excessive force). Our results suggest that trust in these two institutions may be especially important for generating compliance.
4.3. Ruling out alternative explanations
Our survey also allows us to probe two possible alternative explanations for the results above. First, it is possible that respondents who express higher levels of trust in government are simply more knowledgeable about COVID-19 and ways to avoid contracting it. In this case, trust in government may be spuriously correlated with compliance. We explore this possibility by regressing two indices of knowledge about COVID-19 on our measures of trust. The first index is the sum of respondents’ correct answers to a series of three simple true/false questions about the virus; the second is the number of COVID-19 symptoms that respondents were able to identify. As we show in Tables D.10 and D.11 in the appendix, respondents who expressed higher levels of trust in government knew as much or less about COVID-19 than those who expressed lower levels of trust. In most cases, trust is not significantly related to knowledge about COVID-19. While not conclusive, these results suggest that the positive correlation between compliance and trust in government is unlikely to reflect a simple informational channel.
Second, it is possible that the correlation between compliance and trust is an artifact of social desirability bias, especially if more trusting respondents are prone to over-reporting their compliance with government-imposed public health restrictions. To probe this possibility, we use two list experiments that should mitigate social desirability concerns by allowing respondents to report non-compliance indirectly (Tourangeau and Yan, 2007). Table D.12 in the appendix reports results from the first list experiment, which includes a sensitive item for “walking around the village without a mask.” We find that an estimated 51% of respondents reported walking around the village without a mask in the last seven days. This is in line with our estimate from a direct question in which 47% of respondents said they wore a mask “every time they left the home” in the past seven days (compared to 26% saying “most of the time,” 14% “sometimes,” and 13% “not at all”).
Table D.13 in the appendix reports results from our second list experiment, which includes a sensitive item for “attending church or mosque service.” Based on the list experiment, we estimate that approximately 5% of respondents attended a religious service in the past week. Again, this is close to our direct question estimate in which 4.68% of respondents reported attending church or mosque at least once in the last seven days. While we cannot conclusively test whether the gap between our direct and indirect estimates of compliance is larger for more trusting respondents, taken together, our results in Tables D.12 and D.13 suggest that our direct questions are capturing the prevalence of non-compliance relatively accurately, and that social desirability bias is therefore unlikely to explain the correlation between compliance and trust in government in our observational analyses. We also acknowledge that the list experiment cannot confirm that respondents answered all other questions free of social desirability bias.
5. Discussion
In this study, we examine the role of trust in shaping citizens' compliance with public health restrictions in an electoral autocracy. Our study is motivated by the idea that citizens’ responses to public health emergencies are shaped by their trust in multiple state and non-state institutions, not just the government in general. We extend existing research by distinguishing between multiple potential targets of trust, and by assessing whether some of these targets are more important than others in generating support for, and compliance with, costly and disruptive public health policies. We answer these questions in the context of the COVID-19 pandemic in Uganda. Through interconnected experimental and observational studies, we show that (1) endorsements by the government are more effective in generating support for public health restrictions than endorsements by traditional leaders, religious authorities, or international NGOs; (2) trust in government is strongly positively correlated with compliance with these restrictions, while trust in local authorities and other citizens is not; (3) the correlation between compliance and trust in government is unlikely to be a function of differential knowledge of COVID-19 among more and less trusting individuals, and is also unlikely to be an artifact of social desirability bias; and (4) trust in the Ministry of Health and trust in the police appear to be especially important predictors of compliance.
Taken together, our results suggest that the relationship between trust and compliance during public health crises is complex and multifaceted. Our theory posits that individuals’ trust matters at several links along a complicated causal chain of pandemic response, including diagnosis, regulation, promulgation, and enforcement. One of the empirical advantages of our study is that we examine how trust in multiple state and non-state actors correlates with compliance with public health restrictions. Another empirical advantage is that the panel structure of our data allows us to explore how varying levels of trust measured both before and during the pandemic relate to public health compliance.
Our study has several limitations, however. First, we consider just a subset of actors that matter for the theoretical process we describe. The initial waves of our survey were conducted before the pandemic began and we did not anticipate needing other measures of trust. Our endline mobile phone survey conducted during the pandemic needed to be short, and so we focused on the set of authorities we thought would be most relevant in Uganda. There are other types of trust we did not measure. Future work could explore the potential mechanisms that explain why trust in each of these institutions matters at each link in pandemic response.
Second, the endorsement experiment lacks a pure control. We designed the endorsements based on real policies that were in effect at the time of the survey, and real messages that Ugandan authorities were already transmitting to citizens. One of our concerns was that it would be impossible to create a “pure” control condition, since respondents very likely would have associated the endorsements with a particular actor—most likely the central government. To the extent that respondents associated the endorsements with the government even in the absence of a pure control, they may have interpreted endorsements by the other actors as representing a combined endorsement (e.g. by the government and also traditional leaders). In this case, the fact that we find a treatment effect from the government endorsement is telling, since a government endorsement may have been implicit in the other endorsements as well, biasing us towards the null.
Third, our study does not explicitly test the causal pathways that explain why trust matters at each stage in pandemic response for each government actor. We suspect there are two possible mechanisms that link trust and compliance across the chain of diagnosis, regulation, promulgation, and enforcement. First, people may be more likely to believe that public health restrictions are appropriate and necessary when they trust the actors responsible for recommending, legislating, disseminating, and enforcing them. Second, individuals who trust the actors involved in diagnosis, regulation, promulgation, and enforcement may be less likely to believe conspiracy theories about the intentions of those actors. We do not explicitly measure these pathways. Importantly, however, we do show that our results are unlikely to be driven either by an informational mechanism or by social desirability bias.
A robust and important finding in our study is the correlation between compliance and trust in the police and the Ministry of Health. The latter result is perhaps unsurprising: as in most other countries, the Ministry of Health in Uganda plays a key role in diagnosing the nature of public health crises and recommending measures to contain them. The former result is perhaps more surprising; indeed, research on the COVID-19 pandemic (and previous epidemics) has largely ignored the relationship between compliance and trust in the actors who are specifically tasked with enforcing compliance.
Understanding the importance of citizens' trust in the police during public health crises is especially important because the extant literature suggests that distrust is “sticky,” perhaps especially in a setting where the government in general—and the police in particular—has a reputation for repression. This stickiness is evident in Uganda, where a recent community policing program failed to improve citizens’ trust in the police (Blair et al., 2021)—though it is of course possible that a more intensive intervention might have yielded a larger and more sustained improvement in police-community relations. Other recent studies similarly point to the difficulties of building trust in widely distrusted police forces in the Global South (Blair et al., 2019; Blair et al., 2021). Further exploration of the important but underappreciated link between policing and public health in low-income countries strikes us a fruitful avenue for future research.
Finally, while our study highlights the importance of fostering trust in “normal” times so the government can rely on that trust to generate compliance in times of crisis, it is important to note that governments can bolster or erode trust in the ways they respond to crises as well. For example, if the police enforce public health restrictions by abusing human rights, then trust in the police may decline, which may have the paradoxical effect of decreasing compliance and making enforcement even more costly. This risk is especially salient given the tendency of governments throughout the developing world to rely on their police forces to enforce compliance during public health (and other) emergencies (Grasse et al., 2021).
Acknowledgements
This study was approved by the University of Pennsylvania's Institutional Review Board authorization #10077896, Mildmay Research Ethics Committee (MUREC) #00404–2020, and the Uganda National Council for Science and Technology #SS465ES. Funding for this project was provided by the UK Foreign, Commonwealth Development Office, awarded through Innovation for Poverty Action's Peace Recovery Program, and by the UK Foreign, Commonwealth Development Office, awarded through the Abdul Latif Jameel Poverty Action Lab (J-PAL) Crime and Violence Initiative (CVI-1382). Data collection was implemented by Innovations for Poverty Action, Uganda. Special thanks to Vianney Mbonigaba and Allan Claudio Katimbo Katurebe for their excellent work in helping us implement the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.115045.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Aborisade Richard A. Accounts of unlawful use of force and misconduct of the Nigerian Police in the enforcement of COVID-19 measures. J. Police Crim. Psychol. 2021;36(3):450–462. doi: 10.1007/s11896-021-09431-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson Michael. Multiple inference and gender differences in the effects of early intervention: a reevaluation of the Abecedarian, perry preschool, and early training projects. J. Am. Stat. Assoc. 2008;103(484) [Google Scholar]
- Armus Teo. 2020. Brooklyn's Orthodox Jews Burn Masks in Violent Protests as New York Cracks Down on Rising Coronavirus Cases. Washington Post October 8. [Google Scholar]
- Arriola Leonardo R., Grossman Allison Namias. Ethnic marginalization and (Non)Compliance in public health emergencies. J. Polit. Forthcoming. 2020 doi: 10.1086/710784. [DOI] [Google Scholar]
- Bargain Olivier, Aminjonov Ulugbek. Trust and compliance to public health policies in times of COVID-19. J. Publ. Econ. 2020;192:104316. doi: 10.1016/j.jpubeco.2020.104316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair Graime, et al. Community policing does not build citizen trust in police or reduce crime in the Global South. Science. 2021;374(6571) doi: 10.1126/science.abd3446. [DOI] [PubMed] [Google Scholar]
- Blair Robert A., Morse Benjamin S., Tsai Lily L. Public health and public trust: survey evidence from the Ebola Virus Disease epidemic in Liberia. Soc. Sci. Med. 2017;172:89–97. doi: 10.1016/j.socscimed.2016.11.016. [DOI] [PubMed] [Google Scholar]
- Blair Robert, Karim Sabrina M., Morse Benjamin S. Establishing the rule of law in weak and war-torn states: evidence from a field experiment with the Liberian national police. Am. Polit. Sci. Rev. 2019;113(3):641–657. [Google Scholar]
- Brodeur Abel, Grigoryeva Idaliya, Kattan Lamis. Stay-at-Home orders, social distancing and trust. 2020. http://ftp.iza.org/dp13234.pdf IZA Discussion Paper No. 13234. URL: [DOI] [PMC free article] [PubMed]
- Burke Jason, Okiror Samuel. Violent clashes in Uganda after pop star politician detained. Guardian. 2020 https://www.theguardian.com/world/2020/nov/18/violent-clashes-in-uganda-after-pop- star-politician-detained November 18. URL. [Google Scholar]
- Chu Derek K., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic Review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtice Travis B., Behlendorf Brandon. Street-level repression: protest, policing, and dissent in Uganda. J. Conflict Resolut. 2021;65(1):166–194. [Google Scholar]
- Devine Daniel, Gaskell Jennifer, Jennings Will, Stoker Gerry. Trust and the coro- navirus pandemic: what are the consequences of and for trust? An early Review of the literature. Polit. Stud. Rev. 2021;19(2):274–285. doi: 10.1177/1478929920948684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhillon Ranu S., Daniel Kelly J. Community trust and the Ebola endgame. N. Engl. J. Med. 2015;373(9):787–789. doi: 10.1056/NEJMp1508413. [DOI] [PubMed] [Google Scholar]
- Dionne Kim Yi. Cambridge University Press; 2017. Doomed Interventions: the Failure of Global Responses to AIDS in Africa. [Google Scholar]
- Dionne Kim Yi, Poulin Michelle. Ethnic identity, region and attitudes towards male circumcision in a high HIV-prevalence country. Global Publ. Health. 2013;8(5):607–618. doi: 10.1080/17441692.2013.790988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn Claire, Laterzo Isabel. State-level citizen response to COVID-19 containment measures in Brazil and Mexico. J. Polit. Lat Am. 2021;13(3):328–357. [Google Scholar]
- Flaxman Seth, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- Freimuth Vicki S., Musa Don, Hilyard Karen, Quinn Sandra Crouse, Kim Kevin. Trust during the early stages of the 2009 H1N1 pandemic. J. Health Commun. 2014;19(3):321–339. doi: 10.1080/10810730.2013.811323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein Daniel A.N., Johannes Wiedemann. Who do you trust? The Consequences of Partisanship and Trust for Public Responsiveness to COVID-19 Orders. Perspect. Polit. Forthcoming. 2021 [Google Scholar]
- Grasse Donald, Pavlik Melissa, Matfess Hilary, Curtice Travis B. Opportunistic repression: civilian targeting by the state in response to COVID-19. Int. Secur. 2021;46(2):130–165. [Google Scholar]
- Grossman Guy, Kim Soojong, Rexer Jonah M., Thirumurthy Harsha. Political partisanship influences behavioral responses to governors' recommendations for COVID-19 prevention in the United States. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117(39):24144–24153. doi: 10.1073/pnas.2007835117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haim Dotan, Ravanilla Nico, Sexton Renard. Sustained government engagement improves subsequent pandemic risk reporting in conflict zones. Am. Polit. Sci. Rev. 2021;115(2):717–724. [Google Scholar]
- Haug Nils, et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Human Behav. 2020;4(12):1303–1312. doi: 10.1038/s41562-020-01009-0. [DOI] [PubMed] [Google Scholar]
- Isiko Alexander Paul. Religious construction of disease: an exploratory appraisal of religious responses to the COVID-19 pandemic in Uganda. J. Afr. Stud. Dev. 2020;12(3):77–96. [Google Scholar]
- Kahan Dan M. The logic of reciprocity: trust, collective action, and law. Mich. Law Rev. 2003;102(1):71–103. [Google Scholar]
- Kaleeba Noerine, et al. Participatory evaluation of counselling, medical and social services of the AIDS Support Organization (TASO) in Uganda. AIDS Care. 1997;9(1):13–26. doi: 10.1080/09540129750125307. [DOI] [PubMed] [Google Scholar]
- Kao Kristen, et al. The ABCs of Covid-19 prevention in Malawi: authority, benefits, and costs of compli- ance. World Dev. 2021;137:105167. doi: 10.1016/j.worlddev.2020.105167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer Moritz U.G., et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalot Fanny, Maria S Heering, Rullo Marika, Travaglino Giovanni A., Abrams Dominic. The dangers of distrustful complacency: low concern and low political trust combine to un- dermine compliance with governmental restrictions in the emerging Covid-19 pandemic. Group Process. Intergr. Relat. 2022;25(1):106–121. [Google Scholar]
- McFarling Usha Lee. ’Which death do they choose?’: many Black men fear wearing a mask more than the coronavirus. STAT June. 2020;3 [Google Scholar]
- Moxham-Hall Vivienne, Strang Lucy. Public opinion and trust in government during a public health crisis. 2020. https://www.kcl.ac.uk/news/public-opinion-and-trust-in-government-during-a-public-health-crisis Accessed 25 March 2022.
- Okiror Samuel, Burke Jason. Bobi wine charged with covid rule breach after Uganda protests. Guardian. 2020 https://www.theguardian.com/world/2020/nov/20/bobi-wine-charged-with-covid-rule-breach-after-uganda-protests November 20. [Google Scholar]
- Oksanen Atte, Kaakinen Markus, Latikka Rita, Savolainen Iina, Savela Nina, Aki Koivula. Regulation and trust: 3-month follow-up study on COVID-19 mortality in 25 European countries. JMIR Public Health Surveillance. 2020;6(2) doi: 10.2196/19218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagliaro Stefano, et al. Trust predicts COVID-19 prescribed and discretionary behavioral intentions in 23 countries. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0248334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkhurst Justin O. The response to HIV/AIDS and the construction of national legitimacy: lessons from Uganda. Dev. Change. 2005;36(3):571–590. [Google Scholar]
- Parkhurst Justin O., Lush Louisiana. The political environment of HIV: lessons from a comparison of Uganda and South Africa. Soc. Sci. Med. 2004;59(9):1913–1924. doi: 10.1016/j.socscimed.2004.02.026. [DOI] [PubMed] [Google Scholar]
- Pooler Michael. 2021. Churches Become a Covid Battleground in Brazil.https://www.ft.com/content/4f9c81f7-adb5-4b08-a7e7-527f6b912050 Financial Times May 3. URL: [Google Scholar]
- Reuters Uganda extends coronavirus lockdown for three more weeks. Reuters. 2020 https://www.reuters.com/article/health-coronavirus-uganda/uganda-extends-coronavirus-lockdown-for-three-more-weeks-idUSL5N2C24SS April 14. URL. [Google Scholar]
- Schmidt-Sane, et al. Challenges to Ebola preparedness during an ongoing outbreak: an analysis of borderland livelihoods and trust in Uganda. PLoS One. 2020;15(3) doi: 10.1371/journal.pone.0230683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor Derrick Bryson. 2020. For Black Men, Fear That Masks Will Invite Racial Profiling. The New York Times April 14. [Google Scholar]
- Taylor Steven, Asmundson Gordon J.G. Negative attitudes about facemasks during the COVID-19 pandemic: the dual importance of perceived ineffectiveness and psychological reactance. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Independent Observe all covid-19 SOPs while celebrating christmas - Kabaka Mutebi. Independent. 2020 https://www.independent.co.ug/observe-all-covid-19-sops-while-celebrating-christmas-kabaka-mutebi/ December 24. [Google Scholar]
- The Independent Archbishop Kaziimba rallies Ugandans to embrace covid-19 vaccine. Independent. 2021 https://www.independent.co.ug/archbishop-kaziimba-rallies-ugandans-to-embrace-covid-19-vaccine/ March 30. URL. [Google Scholar]
- The Public Health Control of COVID-19 Rules . 2020. The Uganda Gazette No. 19, Volume CXIII, Statutory Instruments No. 52. [Google Scholar]
- Tourangeau Roger, Yan Ting. Sensitive questions in surveys. Psychol. Bull. 2007;133(5):859–883. doi: 10.1037/0033-2909.133.5.859. [DOI] [PubMed] [Google Scholar]
- Tsai Lily L., Morse Benjamin S., Blair Robert A. Building credibility and cooperation in low-trust settings: persuasion and source accountability in Liberia during the 2014–2015 Ebola crisis. Comp. Polit. Stud. 2020;53(10–11):1582–1618. [Google Scholar]
- Van der Windt Peter, Voors Maarten. Traditional leaders and the 2014–2015 Ebola epidemic. J. Polit. 2020;82(4):1607–1611. [Google Scholar]
- Vinck Patrick, Pham Phuong N., Bindu Kenedy K., Bedford Juliet, Eric J., Nilles Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in north Kivu, DR Congo: a population-based survey. Lancet Infect. Dis. 2019;19(5):529–536. doi: 10.1016/S1473-3099(19)30063-5. [DOI] [PubMed] [Google Scholar]
- Weghorst Keith. Cambridge University Press; 2022. Activist Origins of Political Ambition: Opposition Candidacy in Africa's Electoral Authoritarian Regimes. [Google Scholar]
- XinhuaNet Uganda enforces mandatory wearing of face masks. XinhuaNet. 2020 http://www.xinhuanet.com/english/2020-05/07/c139035998.htm May 6. URL: [Google Scholar]
- Yilmazkuday Hakan. Stay-at-Home works to fight against COVID-19: international evidence from google mobility data. J. Hum. Behav. Soc. Environ. 2021;31(1–4):210–220. [Google Scholar]
- Youde Jeremy. Ideology's role in AIDS policies in Uganda and South Africa. Global Health Governance. 2007;1(1) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.