Summary
Background
Screen time has increased as a result of the COVID-19 pandemic, and several correlates have been associated with these increases. These changes, however, have not been aggregated. It was the aim of this review to (a) aggregate changes in screen time in adults and children, and (b) report on variables in relation to screen time during the COVID-19 pandemic.
Methods
A systematic review of major databases was undertaken for studies published from inception to 06/12/2021, using a pre-published protocol (PROSPERO ID: CRD42021261422). Studies reporting (a) screen time pre-versus-during the pandemic, (b) screen time percentage change, or (c) correlates of screen time during the pandemic were included. A random effects meta-analysis was undertaken with subgroup analysis by age group and type of screen time.
Findings
After review, 89 studies (n = 204,734; median age=20·6; median female=53·3%) were included. The majority of studies were cross-sectional. With regards to total screen time, primary aged children (6–10 years) reported largest increases (1·4 hrs/day; 95%CI 1·1–1·7), followed by adults (>18 years; 1·0 hrs/day; 95%CI 0·7–1·2), adolescents (11–17 years; 0·9 hrs/day; 95%CI 0·3–1·5), and young children (0–5 years; 0·6 hrs/day 95%CI 0·3–0·9 hrs/day). For leisure screen time (non-work/non-academic), primary aged children reported largest increases (1·0 hrs/day 95%CI 0·8–1·3), followed by adults (0·7hr/day 95%CI 0·3–1·2), young children (0·6 hrs/day; 95%CI 0·4–0·8), with adolescents reporting the lowest increase (0·5 hrs/day 95%CI 0·3–0·7). Several correlates were associated with reported increases in screen time, including adverse dietary behaviours, sleep, mental health, parental health, and eye health.
Interpretation
Pooled evidence suggest that primary aged children reported the highest increase in both total and leisure screen time during COVID-19. It is recommended that screen time should be reduced in favour of non-sedentary activities. This study has the potential to inform public health policy and future guidance regarding screen time, and to inform future research in this area.
Funding
No funding was received for this study.
Keywords: Covid-19, Screentime, Children, Adults, Review
Research in context.
Evidence before this study
Sedentary behaviour has increased because of the COVID-19 pandemic. It was the aim of this review to pool and report on increases in screen time during the COVID-19 pandemic, and review associations between screen time and correlates. Pubmed, Embase, Scopus, PSYCInfo, ERIC, Child development and adolescent studies, Web of Science and Opengrey were searched using terms relating to “screen time”, “digital screen time”, “sedentary behaviour”, “sitting time” and COVID-19 from inception to 6/12/2021.
Added value of this study
This review found that all age groups increased their total screentime. Primary aged children (6–10 years) reported largest increases, followed by adults (>18 years), adolescents (11–17years), and young children 0–5 years). Leisure screen time also increased in all aged groups, with primary aged children reporting the largest increases, followed by adults, young children, and adolescents. Several correlates were associated with reported increases in screen time, including adverse dietary behaviours, sleep, mental health, and eye health.
Implications of all the available evidence
This review provides evidence that screen time should be reduced wherever possible to negate potential adverse outcomes, and, instead, non-sedentary activities should be promoted.
Alt-text: Unlabelled box
Introduction
In March 2020, the World Health Organization (WHO) declared the COVID-19 outbreak a global pandemic, and as of 19th January 2022, over 325,000,000 confirmed cases have been diagnosed in more than 130 countries and areas, resulting in approximately 5500,000 deaths.1 Since the beginning of 2020, more than 100 countries have enforced some kind of social distancing measures to reduce the rate of COVID-19 transmission, commonly called ‘lockdown’.2 The severity of lockdown has varied from country to country, even region to region, with some countries limiting the distance people could travel from their homes, and some banning any unnecessary outdoor activity.2 These lockdowns have undoubtedly impacted the way in which people work, travel, and spend recreational time. For example, a systematic review reported in the initial phases (in the year 2020) of the pandemic, the majority of adults and children had increased time in sedentary behaviours, defined as any waking behaviour with an energy expenditure of ≤ 1·5 Metabolic Equivalents (METs) whilst in a sitting or reclining posture,3 with concurrent decreases in physical activity,4 although the study did not stratify the type of sedentary behaviour. One type of sedentary activity that has increased substantially during the pandemic is screen time – adults who are now working from home are increasingly using online platforms for work meetings, and children in a number of countries have been taking part in their educational classes online,5 with an estimated 1.37 billion children being at home in March 2020.6 To date, however, these changes in screen time have not been aggregated, which is likely due to a paucity of homogeneous data. On the other hand, several correlates have already been associated with increases in screen time in adults and children independently, including unfavourable dietary choices (such as positive associations between screen time and increases in alcohol and sweetened foods consumption),7,9 adverse physical and mental health (headaches, anxiety, and poor mental health outcomes related to problematic smartphone use, (such as anxiety, insomnia, increased perceived stress, poor educational attainment and decreased overall quality of life),10, 11, 12 and eye related correlates (such as dry eye syndrome, heavy eyelids, and increased myopia).13, 14, 15, 16 Furthermore, a systematic review has reported consistent associations between smartphone and/or tablet use and several measures of sleep outcomes in children, including significant associations between device use and poor sleep quality, quantity, and excessive daytime sleepiness.17 Despite these negative associations, however, problematic screen time behaviours are not consistently reported in studies measuring screen time, with authors arguing that problematic screen time and screen time should be measured concurrently using well established tools, such as the Smartphone Addiction Scale.18,19 In view of these reported associations between screen time and various negative outcomes, it is important to understand the effect that COVID-19 pandemic has had on screen time behaviours and how this has impacted on different correlates. To date, these changes in screen time during the pandemic and correlates have not been systematically reviewed and discussed. It was therefore the aim of this review to:
-
1.
Aggregate and report on the changes in screen time in adults and children independently.
-
2.
Report on all correlates that have been measured in relation to screen time during the COVID-19 pandemic.
This study has the potential to inform public health policy and guidance regarding screen time, and to inform future research in this area.
Methods
Protocol and registration
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines,20 and has been registered with the international prospective register of systematic reviews (PROSPERO protocol ID CRD42021261422). Note that there were no deviations from the published protocol.
Search strategy
Databases were searched from inception to 06/12/2021 including Pubmed; Embase; Scopus; OpenGrey; Psycinfo; ERIC; Child Development and Adolescent Studies; and Web of Science, using the following search terms:
(screen time OR sedentary behaviour OR digital screen time OR sitting time OR screen-time OR gaming OR television OR smartphone OR computer time)
AND
(SARSCoV-2 OR 2019-nCoV OR COVID-19 OR coronavirus OR COVID19 OR coronavirus 19)
No other limiters were applied.
Results of searches were imported in a bibliographic database, with duplicates removed automatically. Titles and abstracts of the remaining studies were independently screened for inclusion by two authors (MT; EI). Following title and abstract screening, the full texts of all potentially eligible papers were reviewed independently by two reviewers (MT,EI) before making a final decision on eligibility, with a senior reviewer (SP) mediating any disputes. The following section describes the inclusion and exclusion criteria:
Population
All types of population (e.g., age, country) were considered, using any study design.
Intervention(s)/exposure(s)
All studies that reported pre vs during screen time usage during COVID-19, or studies that reported associations between any outcome and screen time during COVID-19.
Comparator(s)/control(s)
In studies that measured pre vs during COVID-19 screen time usage, the pre COVID-19 screen time data must have been collected prior to November 2019. Furthermore, all data were stratified into two group: adults (>18yrs), and children (<18yrs). Children were also stratified into three sub-groups were available: adolescents (11–17years), primary aged children (6–10years), and young children (<5 years).
Outcomes
Studies had to report one or more of the following:
-
-
Mean screen time (in either hours or minutes/week) prior to and during the COVID-19 pandemic
-
-
Percentage change (in terms of increased, remained the same, or decreased) screen time during the COVID-19 pandemic
-
-
Associations between any outcome and screen time during the COVID-19 pandemic.
Exclusion criteria:
-
1.
Written in languages other than English, Italian, French, or Spanish
-
2.
Not been through the peer-review process (for example, pre-prints).
Data extraction
Data were extracted by two reviewers (MT & RD) and included: first author; study title; publication date; country; study type; outcome type; outcome effect size; sample size; and participant characteristics.
Risk of bias assessment
Risk of bias was assessed by two independent researchers (MT; EI) using the Newcastle Ottawa Scale (NOS) for cross-sectional studies.21,22 There are 3 parts in which studies are assessed and stars awarded: (i) selection (max. 5 stars) - representativeness of the sample, sample size, non-respondents, and ascertainment of the exposure (risk factor); (ii) comparability (max. 2 stars) - participants in different outcome groups are comparable; (iii) outcome (max. 3 stars)- assessment of outcome, and statistical test. Scores can range from 0 to 10 stars, with higher scores indicating better quality research. Any discrepancies over the final risk of bias verdict were solved by consensus, with involvement of a third review author (SP) where necessary.
Statistical analysis
To aggregate screen time changes pre vs during COVID-19, a random-effects meta-analysis was conducted using the DerSimonian and Laird method, with studies weighted according the inverse variance, using Comprehensive Meta-Analysis.23 The meta-analysis was conducted using the following steps:
-
(1)
Pre and during COVID-19 screen time (hrs/wk.), standard deviations were imputed, and means differences with standard errors were calculated. Note all analyses were stratified as adults (>18) and children (<18). Children were further stratified into three groups: (a) Adolescents (age 11–17); (b) children (age 6–10); and (c) young children (age 0–5). Note that only studies of the same study design were pooled.
-
(2)
Heterogeneity between studies was assessed using the I² statistic,24 with 0–50% being considered low, 51–75% moderate, and >75% being considered high heterogeneity. If pooled results showed high heterogeneity, sub-group analysis was used to find the potential sources.
-
(3)
Publication bias was assessed with a visual inspection of funnel plots and with the Egger bias test.25 As per the recommendations by Fu et al.26 and Sterne et al.,27 these tests were only conducted if the number of studies in each analysis exceeded ten. If significant publication bias (Egger's p=<0.05) was present, a trim-and-fill analysis was conducted.28
-
(4)
Furthermore, sensitivity analyses were conducted to assess the robustness of analyses through the one study removed method.
Mean percent changes in screen time (increased, remain constant, and decreased) and SDs were also calculated using a random effects model, with studies weighted based on the inverse of the variance.
Due to anticipated heterogeneity in measurement types, all associations were aggregated in a narrative synthesis.
Certainty of evidence
To ascertain the certainty of the evidence, the Grading of Recommendations, Assessment, Development and Evaluations29 (GRADE) framework was used.
Role of the funding source
No funding was received for this study. All authors confirm that they had full access to all the data in the study and accept responsibility to submit for publication.
Results
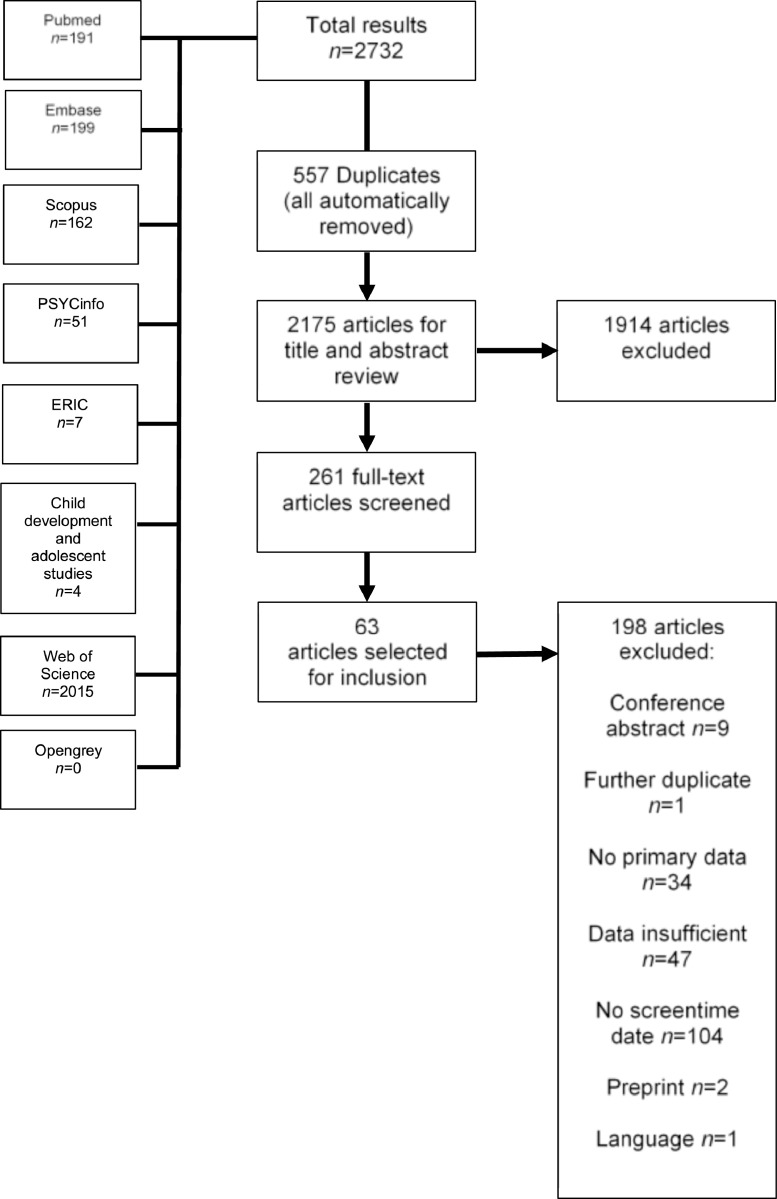
The initial search yielded 7283 results, of which 1403 were removed as duplicates, leaving 5880 articles to be screened at the title and abstract level. Of these, 408 were selected for full text screening. After the full text assessment, 89 articles were selected for inclusion (total n 204,734; median age=20·6; median percentage female=53·3%). All but one of the included studies were cross-sectional in study design, with the one study being longitudinal. The full PRISMA diagram is shown in Figure 1. Of these, 46 studies included data regarding adults,7,8,10,13,14,30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70 and 46 studies included children.9,11,15,42,66,69,71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92,92, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109 Furthermore, 32 studies34,38,43,46,46, 47, 48, 49,51,52,55, 56, 57,65,68,70, 71, 72, 73,75,79,89,90,92, 93, 94, 95,98,100, 101, 102,108 reported pre and during COVID-19 screen time data (and were included in the meta-analysis), 22 studies32,35,37,39,42, 45,54,56,59,61,66,67,77,78, 80,82,84,85,87,96,97,104 reported percentage change in screen time use during the pandemic, and 53 studies reported associations between several correlates and screen time use. Full descriptive characteristics are shown in Table 1. The mean NOS score was 6·4 (SD=0·9; range 4–8; see Supplementary Table 1 for full scoring information).
Table 2.
Meta-analytic changes in any type of screen time in hrs/day, stratified between adults and children.
| Population | n studies(k outcomes) | n participants | Pooled screen time change(95%CI) | p-value | I2 | Eggers's bias(p-value) | Trim and fill adjustment(95%CI; n studies trimmed) | |
|---|---|---|---|---|---|---|---|---|
| Total screen time | Adults | 13 (33) |
30,514 | 0·96 (0·70–1·22) |
<0·001 | 99·80 | 0·10 (1·00) |
NA |
| Adolescents | 8 (21) |
6495 | 0·91 (0·32–1·50) |
0·003 | 99·96 | −4·56 (0·80) |
NA | |
| Primary aged children | 11 (21) |
5566 | 1·39 (1·10–1·69) |
<0·001 | 99·76 | 3·24 (0·69) |
NA | |
| Young children | 7 (25) |
5991 | 0·59 (0·29–0·91) |
<0·001 | 99·91 | −32·17 (<0·001) |
0·70 (0·43–0·97; 4 studies) |
|
| Leisure screen time | Adults | 7 (15) |
22,921 | 0·72 (0·29–1·15) |
0·001 | 99·89 | −3·36 (0·84) |
NA |
| Adolescents | 3 (10) |
2102 | 0·48 (0·29–0·67) |
<0·001 | 98·14 | 11·02 (0·04) |
0·61 (0·31–0·90; 2 studies) |
|
| Primary aged children | 6 (10) |
2202 | 1·04 (0·77–1·30) |
<0·001 | 99·03 | 15·78 (<0·001) |
1·12 (0·70–1·54; 1 study) |
|
| Young children | 3 (8) |
1767 | 0·61 (0·40–0·82) |
<0·001 | 98·78 | NA | NA | |
Figure 1.
PRISMA flow diagram of study selection.
Caption: PRISMA flow diagram showing the process of study selection. ERIC= Education Resources Information Centre.
Table 1.
Descriptive characteristics of included studies.
| Author(s) | Country | Study design | Population type | Mean age (SD) | Age range | Percent female | Total n | Type of screen-time | Screen time reporting type | Risk of bias score |
|---|---|---|---|---|---|---|---|---|---|---|
| Abdulsalam et al.30 | Saudi Arabia | Cross-sectional | Adults | NR | 18–59 | 68% | 472 | Overall screen time | Online survey; self-report | 4 |
| Abid et al.71 | Tunisia |
Cross-sectional | Children | 8·7 (3·3) |
5–12 | 48% | 100 | Diurnal screen time; nocturnal screen time; global screen time | Online survey; self-report | 8 |
| Aguilar-Farias et al.72 | Chile | Cross-sectional | Children | 3·1 (1·4) |
1–5 | 49% | 3157 | Overall screen time | Online survey; self-report | 7 |
| Agurto et al.31 | Peru | Cross-sectional | Adults | NR | NR | NR | 201 | Sitting or lying in front of a screen | Online survey; self-report | 7 |
| Alomari et al.32 | Jordan | Cross-sectional | Adults | 33·7 (11·3) |
18–72 | 70% | 1844 | Use of electronic screens; social media use; television use | Online survey; self-report | 7 |
| Alves et al.11 | USA | Cross-sectional | Children (overweight or obese) | 11·7 (1·2) | NR | 57% | 30 | Leisure screen time | Telephone or video calls; parental self-report | 7 |
| Children (healthy weight) | 11·9 (1·2) | NR | 68% | 34 | Leisure screen time | 7 | ||||
| Balsam14 | Saudi Arabia | Cross-sectional | Adults | 33·4 (12·2) |
18–81 | 72% | 1939 | Smartphone usage; daily digital device usage | Online survey; self-report | 5 |
| Beck et al.73 | USA | Cross-sectional | Children | NR | 4–12 | 55% | 145 | Non-academic screen time | Survey; parental report | 7 |
| Bird et al.33 | UK | Cross-sectional | Adults | NR | 18–85 | 80% | 392 | Overall screen time | Online survey; self-report | 4 |
| Branquinho et al.34 | Portugal | Cross-sectional | Adults | 48.5 (14.3) |
NR | 67.7% | 5746 | TV use; mobile phone use; social networking; gaming | Online survey; self-report | 6 |
| Breidokiene et al.74 | Lithuania | Cross-sectional | Children | 9.7 (1.9) |
6–14 | 52.9% | 306 | Screentime for leisure; screen time for education | Online survey; parental report | 6 |
| Brzek et al.75 | Poland | Cross-sectional | Children | NR | 3–5 | NR | 1311 | TV use; tablet time; PC time; mobile time | Online survey; parental report | 6 |
| Cachon-Zagalaz et al.76 | Spain | Cross-sectional | Children | 6·2 (3·4) |
0–12 | 50% | 837 | Daily use of digital screens | Online survey; self-report | 7 |
| Cahal et al.77 | Israel | Cross-sectional | Children | 6·2 (4·7) |
0–18 | 38% | 445 | Overall screen time | Online survey; self-report | 7 |
| Chambonniere et al.78 | France | Cross-sectional | Children | NR | 6–10 | 46% | 1588 | Overall screen time | Online survey; self-report | 7 |
| Children | NR | 11–17 | 61% | 4903 | Overall screen time | 7 | ||||
| Cheikh Ismail et al.35 | UAE | Cross-sectional | Adults | NR | NR | 76% | 1012 | Screen time for entertainment | Online survey; self-report | 6 |
| Chen et al.79 | China | Longitudinal | Children | 10.3 (0.8) |
NR | 50.5% | 535 | Smartphone use | Online survey; self-report | 7 |
| Conroy et al.36 | USA | Cross-sectional | Adults | 43 (13) |
NR | 79% | 834 | Screentime before bed | Online survey; self-report | 5 |
| Constandt et al.110 | France | Cross-sectional | Adults | NR | NR | 51.2% | 4005 | Overall screen time | Online survey; self-report | 6 |
| Coyne et al.38 | Canada | Cross-sectional | Adults | 39.2 (15.1) |
21–77 | 87% | 64 | Recreational screen time | Online survey; self-report | 7 |
| de Sa et al.80 | Brazil | Cross-sectional | Children | NR | 0–12 | NR | 816 | Playful screen time | Online survey; parental report | 6 |
| Donati et al.81 | Italy | Cross-sectional | Children | 11.1 (NR) |
NR | 27% | 554 | Gaming | Online survey; parental and child report (not stratified) | 5 |
| Dragun et al.39 | Croatia | Cross-sectional | Adults (international medical students) | 22 (6) |
NR | 63% | 59 | Computer/table use time; television watching time; mobile use time | Online survey; self-report | 7 |
| Adults (domestic medical students) | 23 (6) |
NR | 78% | 148 | Computer/table use time; television watching time; mobile use time | 4 | ||||
| Dubuc et al.82 | Canada | Cross-sectional | Children | NR | NR | 53.3% | 2661 | Recreational screen time | Online survey; self-report | 7 |
| Farah et al.83 | Israel | Cross-sectional | Children | 2 (0·6) |
1–3 | 47% | NR | Screen exposure | Online survey; parental report | 6 |
| Fillon et al.84 | France | Cross-sectional | Children | NR | 1–6 | 49.7% | 348 | Overall screen time | Online survey; parental report | 5 |
| Fraser et al.40(p19) | USA | Cross-sectional | Adults (college students) | NR | NR | 70% | 74 | TV use; social media; gaming | Online survey; self-report | 7 |
| Ganne et al.41 | India | Cross-sectional | Adults | 23.4 (8.2) |
18–79 | 48.9% | 941 | Overall screen time | Online survey; self-report | 6 |
| Garcia et al.85 | USA | Cross-sectional | Children with autism | NR | NR | 11% | 9 | Overall screen time; weekday screen time | Online survey; self-report | 6 |
| Genin et al.42 | France | Cross-sectional | Children | NR | 6–10 | NR | 1588 | Overall screen time | Online survey; self-report | 8 |
| Children | NR | 11–17 | NR | 4903 | Overall screen time | 7 | ||||
| Adults | NR | 18–64 | NR | 15,226 | Overall screen time | 7 | ||||
| Adults | NR | 65+ | NR | 1178 | Overall screen time | 6 | ||||
| Giannini et al.86 | Brazil | Cross-sectional | Children | 15.3 (1.8) |
12–18 | 57.7% | 208 | Overall screen time | Online survey; self-report | 7 |
| Gornika et al.7 | Poland | Cross-sectional | Adults | NR | NR | 89.8% | 2381 | Overall screen time | Online survey; self-report | 7 |
| Guo et al.87(p19) | China | Cross-sectional | Children (primary, secondary, and high school students) | Median=13 (IQR=10–16) |
NR | 49.9% | 10,416 | Overall screen time | Online survey; self-report | 7 |
| Hadianfard et al.88 | Iran | Cross-sectional | Children | NR | 12–16 | 49.4% | 510 | Overall screen time | Online survey; self-report | 7 |
| Hashem et al.9 | Egypt | Cross-sectional | Children | NR | 4–16 | 47% | 765 | Electronics and screen use; mobile extra screen time; television extra screen time; laptop extra screen time | Online survey; self-report | 6 |
| Helbach and Stahlmann43 | Germany | Cross-sectional | Adults | 22.4 (2) |
18–26 | 76% | 884 | Smartphone use; TV use; PC/computer/tablet use | Online survey; self-report | 8 |
| Hodes et al.44 | South Africa | Cross-sectional | Adults | 20·5 (1·5) |
18–25 | NR | 244 | Objectively measured smartphone use | iPhone screen time data shared via screenshots | 6 |
| Hu et al.45 | China | Cross-sectional | Adults | NR | 18–60 | 48% | 1033 | Leisure screen time; overall screen use | Online survey; self-report | 7 |
| Hyunshik et al.89 | Japan | Cross-sectional | Children | 4.8 (0.3) |
3–5 | 47.8% | 290 | Overall screen time | Online survey; parental report | 6 |
| Jáuregui et al.90 | Mexico | Cross-sectional | Children | 3.3 (NR) |
1–5 | 47.2% | 631 | Overall screen time | Online survey; parental report | 6 |
| Jia et al.46 | China | Cross-sectional | Adults (undergraduate students) | 20.6 (1.8) |
NR | 70% | 7024 | Overall screen time | Online survey; self-report | 6 |
| Adults (graduate students) | 24.6 (3.5) |
NR | 71% | 234 | Overall screen time | Online survey; self-report | 7 | |||
| Kim et al.91 | South Korea | Cross-sectional | Children | 9.2 (1.4) |
7–12 | 43.8% | 217 | TV time; tablet time; smartphone time | Online survey; parental report | 6 |
| Koohsari et al.47 | Japan | Cross-sectional | Adults | NR | NR | NR | 1086 | Television time; PC use during workday; PC use sitting time | Online survey; self-report | 6 |
| Kowalsky et al.48 | USA | Cross-sectional | Adults | 22.1 (4.9) |
NR | 73% | 189 | TV/computer/phone use | Online survey; self-report | 5 |
| Lawrence et al.49 | USA | Cross-sectional | Adults (social care students) | 29 (10) |
NR | 93% | 88 | Overall screen time | Online survey; self-report | 7 |
| Le et al.50 | USA | Cross-sectional | Adtuls (healthcare workers) | NR | 25–64 | 51% | 74 | Overall screen time | Online survey; self-report | 7 |
| Lim et al.92 | Singapore | Cross-sectional | Children | Median 8 (IQR 6–11) | NR | NR | 593 | Non-academic screen time | Online survey; parental report | 7 |
| Liu et al.a111 | China | Cross-sectional | Children | NR | NR | 48% | 3405 | e-learning screen use | Online survey; self-report | 6 |
| Lui et al. b15 | China | Cross-sectional | Children | NR | NR | 48% | 3831 | Non-academic screen time | Online survey; self-report | 6 |
| Lopez-Gil et al.93 | Spain | Cross-sectional | Children | NR | 3–17 | 50% | 604 | Sedentary screen-based pursuits | Online survey; parental report | 6 |
| Brazil | Children | 3–17 | 44% | 495 | 5 | |||||
| Ma et al.94 | China | Cross-sectional | Children | 8.9 (0.7) |
8–10 | 47.6 | 208 | Digital screen time(not including online education) | Online survey; self and parental report | 6 |
| Majumdar et al.51 | India | Cross-sectional | Adults (office workers) | 33·1 (7·1) |
NR | 18% | 203 | Cell phone use; desktop/laptop use; television use | Online survey; self-report | 5 |
| Adults (students) | 22·1 (1·7) |
NR | 61% | 325 | 7 | |||||
| McArthur et al.95 | Canada | Cross-sectional | Children | 9·9 (0·8) |
8–9·5 | 48% | 1333 | Screen time reported by child; screen time reported by mother | Online survey; parental report | 6 |
| McCormack et al.96 | Canada | Cross-sectional | Children | 10.8 (4) |
NR | 45.1% | 328 | Use of screen based devices; TV use; gaming | Online survey; self-report | 7 |
| Meyer et al.10 | USA | Cross-sectional | Adults | NR | NR | NR | 1540 | Overall screen time | Online survey; self-report | 7 |
| Mitra et al.97 | Canada | Cross-sectional | Children | NR | 5–11 | NR | 693 | Overall screen time | Online survey; parental report | 7 |
| Children | NR | 12–17 | NR | 779 | Overall screen time | 8 | ||||
| Mohan et al.98 | India | Cross-sectional | Children | 13 (2·5) |
10–18 | 54% | 261 | Overall screen time | Online survey; parental and self-report | 7 |
| Mon-Lopez et al.52 | Spain | Cross-sectional | Adults | 39.7 (13.6) |
NR | 50% | 120 | Overall screen time | Online survey; self-report | 4 |
| Nassar et al.99 | Egypt | Cross-sectional | Children (soccer players) | NR | 9–11 | 0% | 74 | Overall screen time | Online survey; self-report | 6 |
| Nathan et al.100 | Australia | Cross-sectional | Children | 6.9 (1.7) |
5–9 | 45.9% | 157 | Leisure screen time | Online survey; self-report | 5 |
| Oswald et al.53 | Australia | Cross-sectional | Adults | 21·2 (1·9) |
18–24 | 55% | 55 | Overall screen time | Online survey; self-report | 7 |
| Pavithra and Sundar13 | India | Cross-sectional | Adults (engineering students) | NR | NR | 54% | 396 | Overall screen time | Online survey; self-report | 7 |
| Peddie et al.101 | New Zealand | Cross-sectional | Children (adolescent boys) | 16.6 (0.7) |
15–18 | 0% | 109 | Overall screen time | Online survey; self-report | 7 |
| Robbins et al.54 | USA | Cross-sectional | Adults (elderly adults) | NR | 65+ | NR | 3122 | TV time | Online survey; self-report | 6 |
| Rodriguez-Larrad et al.55 | Spain | Cross-sectional | Adults | 22·8 (5·3) |
18–54 | 65% | 13,754 | Leisure screen time; study screen time | Online survey; self-report | 6 |
| Sallie et al.56 | International cohort | Cross-sectional | Adults | 28.9 (12.5) |
18–90 | 24.2% | 771 | Online gaming | Online survey; self-report | 7 |
| 859 | Porn viewing | 6 | ||||||||
| Sanudo et al.70 | Spain | Cross-sectional | Adults | 22·6 (3·4) |
NR | 45% | 20 | Overall screen time | Phone usage data; objectively measured | 8 |
| Saxena et al.57 | India | Cross-sectional | Adults (college students) | 20·4 (1·4) |
18–24 | 50% | 60 | Overall screen time | Online survey; self-report | 5 |
| Schmidt et al.102 | Germany | Cross-sectional | Children | NR | 4–17 | NR | 1711 | Television use; gaming time; recreational internet use; recreational screen time | Online survey; self-report | 6 |
| Sewall et al.58 | USA | Cross-sectional | Adults | 24·5 (5·1) |
18–35 | 57% | 384 | Objectively measured screen time | iPhone screen time data shared via screenshots | 7 |
| Sikorska et al.103 | International cohort | Cross-sectional | Children | NR | 11–16 | 65.7% | 370 | Online gaming; internet browsing; TV use; social media | Online survey; self-report | 7 |
| Siste et al.104 | Indonesia | Cross-sectional | Children | 17.4 (2.2) |
NR | 78.7% | 2932 | Internet duration | Online survey; self-report | 6 |
| Spence et al.59 | UK | Cross-sectional | Adults | NR | NR | 51% | 1521 | Overall screen time; screen time for work/school; screen time for leisure | Online survey; self-report | 6 |
| Stieger et al.60 | Austria | Cross-sectional | Adults | 31 (14·5) |
NR | 56% | 286 | Overall screen time | App-collected; self-report | 7 |
| Stokes et al.105 | Australia | Cross-sectional | Children | 10.6 (3.1) |
5–17 | 23.6% | 213 | TV use; social media use; gaming | Online survey; self-report | 7 |
| Suka et al.61 | Japan | Cross-sectional | Adults | NR | 25–64 | NR | 8000 | Television use; digital media exposure | Online survey; self-report | 6 |
| Szwarcwald et al.106 | Brazil | Cross-sectional | Children | NR | 12–17 | 50% | 9470 | Overall screen time | Online survey; self-report | 6 |
| Tan et al.62 | Malaysia | Cross-sectional | Adults (university students) | 22 (2.3) |
18–27 | 74.2% | 186 | Sedentary screen time | Online survey; self-report | 6 |
| Tebar et al.8 | Brazil | Cross-sectional | Adults | 37·9 (13·3) |
NR | 59% | 1896 | Television use; cell phone use; computer time | Online survey; self-report | 4 |
| Werneck et al.64 | Brazil | Cross-sectional | Adults | NR | NR | 53% | 33,862 | Television use; computer/tablet use | Online survey; self-report | 8 |
| Windiani et al.107 | Indonesia | Cross-sectional | Children | Median 16 | 15–18 | 49% | 204 | Overall screen time | Online survey; self-report | 7 |
| Woodruff et al.65 | Canada | Cross-sectional | Adults | 36·2 (13·1) |
18–77 | 80% | 80 | Screen related sedentary behaviour | Online survey; self-report | 7 |
| Wunsch et al.108 | Germany | Cross-sectional | Children | NR | 4–17 | NR | 1686 | Overall screen time | Online survey; self-report | 7 |
| Xiao et al.109 | China | Cross-sectional | Children | NR | NR | 49% | 1680 | Online study time; other screen time | Online survey; self-report | 7 |
| Yang et al.66† | China | Cross-sectional | Adults (graduate students) | 24·6 (3·5) |
NR | 71% | 234 | Overall screen time | Online survey; self-report | 7 |
| Adults (undergraduate students) | 20·6 (1·6) |
NR | 70% | 7024 | Overall screen time | 5 | ||||
| Children (high school students) | 17·5 (1·2) |
NR | 76% | 2824 | Overall screen time | 7 | ||||
| Zajacova et al.67 | Canada | Cross-sectional | Adults | NR | NR | 51% | 4319 | Internet time; television time | Online survey; self-report | 4 |
| Zarco-Alpeunte et al.63 | Spain | Cross-sectional | Adults | NR | 18–55 | NR | 886 | TV use; online sexual activities; video games; social networks; online shopping; instant messaging | Online survey; self-report | 6 |
| Zhang et al.68 | China | Cross-sectional | Adults (pregnant women) | 29 (4) |
NR | 100% | 1794 | Overall screen time | Online survey; self-report | 6 |
| Zhou et al.69† | China | Cross-sectional | Adults (graduate students) | 24·6 (3·5) |
NR | 71% | 234 | Overall screen time | Online survey; self-report | 6 |
| Adults (undergraduate students) | 20·6 (1·6) |
NR | 70% | 7024 | Overall screen time | 7 | ||||
| Children (high school students) | 17·5 (1·2) |
NR | 76% | 2824 | Overall screen time | 7 |
Yang et al. and Zhou et al. used the same sample, with data reported in different formats.
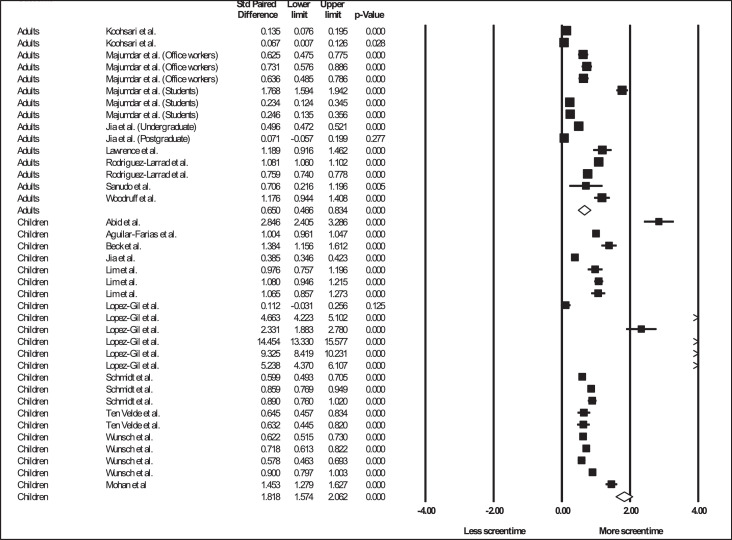
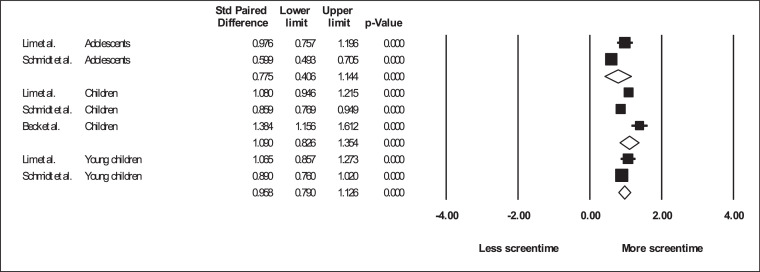
Meta-analytic changes in screen time
There were 133 outcomes yielded from 32 studies in the meta-analysis. Regarding total screen time (see Figure 2), adults reported increases of 0·96 hrs/day (95%CI 0·70–1·22 hrs/day; I2=99·80; k = 33), adolescents 0·91 hrs/day (95%CI 0·32–1·50; I2=99·96; k = 21), primary aged children 1·39 hrs/day (95%CI 1·1–1·69; I2=99·76; k = 21), and young children 0·59 hrs/day (95%CI 0·29–0·91; I2=99·91; k = 25). The analysis of total screen time in young children showed significant publication bias (Egger's p=<0.001). Subsequent trim and fill analysis yielded a significant increase of 0·70 hrs/day (95%CI 0·43–0·97), with four studies trimmed to the right of the mean. The magnitude or direction of results were not influenced by the removal of any one study. Because all analyses had high heterogeneity, all these results were classified as of ‘very low’ certainty according to the GRADE criteria.
Figure 2.
Forest plot showing pooled changes in any type of screentime from before the COVID-19 pandemic, stratified by adults or children.
Caption: Units=hrs/day; Error bars= 95% confidence interval; Solid boxes = individual study point estimates; Clear box = Pooled point estimates.
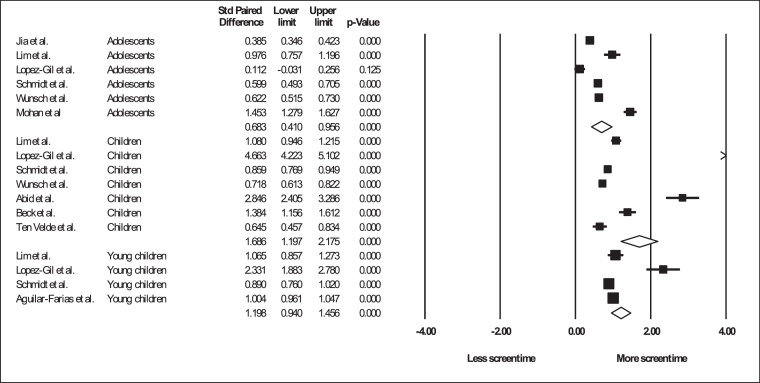
In studies that reported changes in leisure screen time (non-work/non-academic; see Figure 3), adults reported increases of 0·72 hrs/day (95%CI 0·29–1·15 hrs/day; I2=99·89; k = 15), adolescents 0·48 hrs/day (95%CI 0·29–0·67; I2=98·14; k = 10), primary aged children 1·04 hrs/day (95%CI 0·77–1·30; I2=99·03; k = 10), and young children 0·61 hrs/day (95%CI 0·40–0·82; I2=98·78; k = 8). The analysis of leisure screen time in adolescents and primary aged children showed significant publication bias (Egger's p = 0.04 and <0.001, respectively), with the subsequent trim and fill analyses yielding respective significant increase of 0·61 hrs/day (95%CI 0·31–0·90; two studies removed) and 1·12 hrs/day (95%CI 0·70–1·54; one study removed), with all studies trimmed to the right of the mean. The magnitude or direction of results were not influenced by the removal of any one study. Due to the study design (all included studies were cross-sectional) and high heterogeneity, all these results were classified as ‘very low’ certainty according to the GRADE criteria.
Figure 3.
Forest plot showing pooled changes in any type of screentime from before the COVID-19 pandemic in children, stratified by age group.
Caption: Units=hrs/day; Error bars= 95% confidence interval; Solid boxes = individual study point estimates; Clear box = Pooled point estimates.
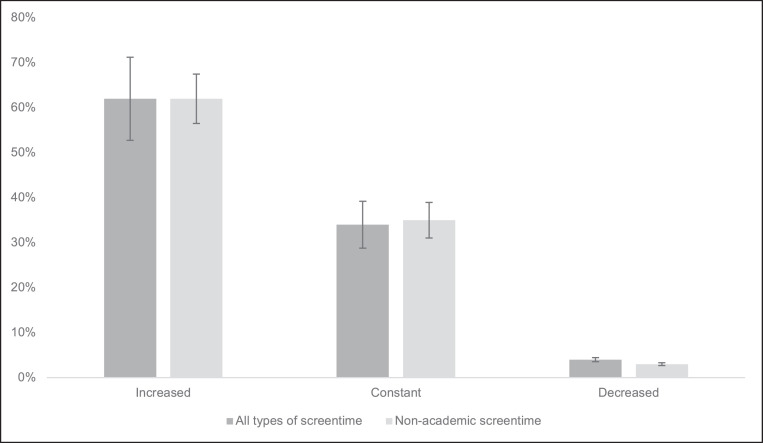
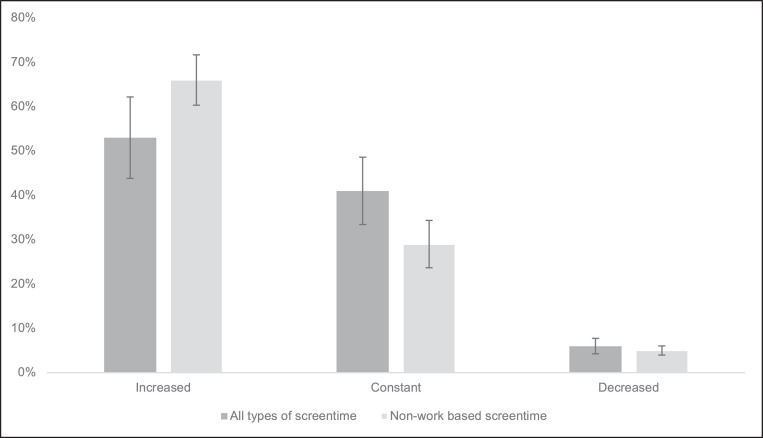
Percent changes in screen time
As shown in Table 3 and Figure 4, the random effects model yielded 51% (95%CI 44–58) of adults reporting an increase in total screen time, 39% (95% CI 33–46) no change, and 7% (95% CI 5–9) a decrease. Regarding leisure screen time (non-academic or non-work related), 52% (95% CI 38–66) of adults reported an increase, 38% (95% CI 27–51) reported no change, and 7% (95% CI 5–9) reported a decrease. In children, 67% (95% CI 60–74) reported an increase in total screen time, 27% (95% CI 21–33) reported no change, and 4% (95% CI 3–6) reported a decrease. Regarding leisure (non-academic or non-work related) screen time, 59% (95% CI 50–69) of children reported an increase, 30% (95% CI 24–35) reported no change, and 9% (95% CI 6–14) reported a decrease (see Figure 5). Stratification of children into age-groups was not possible due to a paucity of data.
Figure 6.
Percent changes in screentime in children
Caption: Error bars show 95% confidence intervals.
Table 3.
Pooled changes in screen time over the COVID-19 pandemic reported as percentages.
| n studies(k outcomes) | n participants | Increased(95% CI) | No change(95% CI) | Decrease(95% CI) | ||
|---|---|---|---|---|---|---|
| Total screen time | Adults | 13 (26) |
59,405 | 50·8% (44·0–57·6%) |
39·0% (32·9–45·5%) |
7·0% (5·1–9·4%) |
| Children | 12 (21) |
34,467 | 67·3% (59·8–74%) |
26·8% (21·1–33·3%) |
4·0% (2·7–6·0%) |
|
| Leisure screen time (non-work/non-academic) | Adults | 4 (6) |
6733 | 52·4% (38·3–66·2%) |
38·0% (26·8–50·5%) |
6·7% (4·8–9·3%) |
| Children | 3 (6) |
3805 | 59·4% (49·6–68·5%) |
29·5% (24·2–35·3%) |
9·0% (5·7–13·9%) |
|
Figure 4.
Forest plot showing pooled changes in leisure screentime from before the COVID-19 pandemic in children, stratified by age group.
Caption: Units=hrs/day; Error bars= 95% confidence interval; Solid boxes = individual study point estimates; Clear box = Pooled point estimates.
Figure 5.
Percent changes in screentime in adults.
Caption: Error bars show 95% confidence intervals.
Associations between screen time and multiple correlates
Adults
In adults, 30 studies7,8,10,13,14,30,31,33,36,40,41,43, 44, 45,47,49,50,52, 53, 54,57,58,60, 61, 62, 63, 64,66,68,69 reported 109 outcomes across the following areas: diet and smoking, eye health, mental health, fatigue, general health, physical activity, and weight gain/BMI (see Supplementary Table 2).
Diet and smoking
Three studies7,8,62 (yielding 29 independent outcomes) reported correlates in relation to diet and smoking, of which 35% (10/29) were statistically significant.
In outcomes that were related to overall screen time, 50% (2/4) of the outcomes yielded significant outcomes. The significant outcomes included a negative association between increases in screen time and a ‘constant diet’ during COVID (OR=0·68; 95%CI 0·56–0·82),8 and increases in screen time was reported to be associated with ‘unhealthy dietary changes’ (OR=1·54 95%CI 1·21–1·96).8 Non-significant associations were found between increases in screen time and ‘pro-healthy’ dietary changes, or ‘self-regulation around eating’.7
Regarding TV time, 43% (3/7) outcomes were statistically significant, including a significant negative correlation between TV time and self-regulation around eating (r= −0·24; p = 0·01),62 positive associations between increased TV use and increased desire to drink (OR=1·46 95%CI 1·12–1·89),8 and increases in sweetened food consumption (OR=1·53 95%CI 1·12–1·89).8 Non-significant findings included increased TV use and alcohol consumption, increased desire to smoke, and increases in smoking.
In outcomes that measured gaming, 50% (1/2) of univariate correlations were statistically significant. The significant association was a negative correlation between the use of gaming consoles and self-regulation around eating (r= −0·15; p = 0·04),62 and the non-significant association was ‘gaming on a computer’ and self-regulation around eating (r= −0·06; p=NR).62
Regarding cell phone use, 17% (1/6) of outcomes yielded significant associations, with increases in cell phone use being significantly associated with the consumption of sweetened foods (OR=1·78 95%CI 1·18–2·67).8 Increases in cell phone use was not significantly associated with alcohol consumption, increased desire to drink alcohol, increased in smoking or the desire to smoke more.
In outcomes that measured computer-based screen time (including internet use), 33% (3/9) of outcomes were significant. Of these significant outcomes, increases in computer time was negatively associated with alcohol (OR=0·68; 95%CI 0·53–0·86), and sweetened foods (OR=0·78; 95%CI 0·62–0·98)8 consumption. Furthermore, internet use for self-directed learning was found to be positively associated with self-regulation around eating in univariate analyses (r = 0·17; p = 0·02).62
Eye health
Three studies13,14,41 (yielding 17 independent outcomes) examined associations between screen time and eye health, 88% (15/17) being statistically significant. Regarding the type of screen time, all studies examined increases in total screen time. All three studies that measured dry eye syndrome found significant positive associations (increased screen time OR=66·7 95%CI 20·4–218·3; <6 hrs/day with >6 hrs/day as the reference group; OR 0·51 95%CI 0·39–0·67; x2=39.2 p=<0.001).13,14,41 The remaining associations measured symptoms of digital eye strain,14 and found significant associations between less than 6 hrs/day of screen time (with >6 hrs/day as the reference group) and tearing (OR=0·72 95%CI 0·54–0·96); eye strain (OR=0·51 95%CI 0·41–0·64); eye dryness (OR=0·62 95%CI 0·49–0·79); heavy eyelids (OR=0·68 95%CI 0·51–0·91); eye redness (OR=0·60 95%CI 0·44–0·81); eye itchiness (OR=0·53 95%CI 0·40–0·69); burning sensations in the eye (OR=0·59 95%CI 0·45–0·76); sensitivity to bright light (OR=0·58 95%CI 0·43–0·79); difficulty focussing (OR=0·70 95%CI 0·55–0·90); eye pain (OR=0·56 95%CI 0·41–0·75); foreign body sensation in the eye (OR=0·69 95%CI 0·49–0·98); and excessive blinking (OR=0·68 95%CI 0·52–0·87).14 Neither diplopia and blurred vision were associated with increases in screentime.14
Mental health
A total of twenty studies10,14,33,36,40,44,45,47,49,50,52, 53, 54,58,60,63,64,66,68,69 (yielding 68 independent outcomes) examined associations between screen time and mental health outcomes, with 46% (31/68) outcomes yielding significant results.
Seventeen outcomes measured screen time and anxiety, with 47% (8/17) of outcomes being statistically significant. Regarding increases in overall screen time, several nominal categories of screen time were associated with anxiety (with less than 2 hrs/day as the reference variable) with higher levels of screen time showing higher odds ratios: 5–6 hrs/day (OR=1·76 95%CI 1·20–2·58), 7–8 hrs/day (OR=1·98 95%CI 1·29–3·03), and more than 8 hrs/day (OR=2·22 95% 1·45–3·40), however 3–4 hrs/day was not significant.68 This is in agreement with two other studies who also found significant positive associations between overall screen time and anxiety (β=1·34; p = 0·00310 and β=0·93; p = 0·0449). Conversely, both studies that measured screen time objectively (using smartphone data) yielded no significant associations.44,58 Furthermore, Le et al.50 found no significant associations between screen time and anxiety. Increases in TV use was associated with anxiety about COVID-19 (prevalence ratio=1·4 95% CI 1·2–1·6), and overall anxiety in people with (OR=1·58; p=<0.05), and without depression (OR=1·73; p=<0.05).64 Concurrently, decreases in TV use yielded non-significant associations with anxiety about COVID-19,54 and anxiety in people with and without depression.64
Depression was measured in eight outcomes, with 63% (5/8) being significant, including increasing TV use and ‘depression about COVID-19′ (prevalence ratio=1·3 95%CI 1·1–1·5), with a concurrent non-significant association between decreases in TV use and ‘depression about COVID-19′.54 Overall screen time yielded conflicting results, with two studies10,69 reporting positive associations with depression (OR=1·54 95%CI 1·03–2·30; β=1·92; p=<0·001), another68 reporting that increases in screen time yield negative (protective) associations with depressive symptoms (OR=0·54 95%CI 0·43–0·65), and others yielding no significant results.49,58
Loneliness was examined in 15 outcomes, with 47% (7/15) of outcomes yielding significant results. Of the significant outcomes, overall screen time was reported to be associated with onliness in one study (β =0·34; p=<0·001).10 Social loneliness was associated with social media use (β of direct effect=0·54; p=<0·001; β of indirect effect= −0·01; p=<0·05),66 and internet gaming use (β of direct effect=0·43; p=<0·001; β of indirect effect was not significant).66 Emotional loneliness was associated with social media use (β of direct effect=0·52; p=<0·001; β indirect effect was not significant), and internet gaming use (β of direct effect=0·44; p=<0·001; β of indirect effect was not significant).66 Increases in TV use were also reported to be significantly associated with loneliness in people without depression (OR=1·59; p=<0.05), whereas this result was not significant in people with depression.64 The same study also found non-significant associations between decreases (and no changes) in screen time and loneliness in people with and without depression.64
Two studies36,50 examined mood changes and screen time, with both studies yielding non-significant results.
Regarding other aspects of mental health, studies report conflicting results. TV time (β=0·16; p=<0·001), online shopping (β=0·16; p=<0·01), and online sexual activities (β=0·13; p=<0·05) were all correlated with the impact of COVID-19 lockdowns on overall mental health, whereas total screen time, video gaming, social media use and instant messaging were non-significant.33,63 Positive affect was significantly negatively correlated with instant messaging (β=−0·1; p=<0·01) and TV use (β= −0·09; p=<0·05), but not significantly associated with online sexual activities, video games, social media use, or online shopping.63 Negative affect was significantly negatively associated with social media use (β= −0·08; p=<0·05), and positively associated with online shopping (β= 0·15; p=<0·05), but not with video games or instant messaging.63 Furthermore, increases in screen time were negatively associated with overall wellbeing in one study (ICC r= −0·31 p=<0·001),60 but not in others.45 ‘Struggling’ versus ‘flourishing’ mental health was associated with increases and decreases in screen time (RR=2·20; p=<0·05 and RR=23·85; p=<0·05 respectively), indicating widely conflicting results.53 Headaches were reported to be negatively associated with less than 6 hrs/day of screen time (OR=0·55; p=<0.001), and boredom was consistently associated with increases in social media use (β of direct effect=0·46; p=<0·001; β of indirect effect=0·03; p=<0·05) and internet gaming (β of direct effect=0·39; p=<0·001; β of indirect effect=0·04; p=<0·05).66
The remaining outcomes were non-significant, including leisure screen time and subjective wellbeing,45 increasing screen time and ‘languishing’ versus ‘flourishing’ mental health,53 and overall mental health.33 Furthermore, increases in instant messaging, social media use, and video games were all not significantly associated with COVID-19 related overall mental health.63
Sleep/fatigue
Two studies47,50 yielded 14 independent outcomes regarding sleep/fatigue and concentration, all of which were not significant.
General health
One study61 examined screen time and general health, with two outcomes. Of these 50% (1/2) were significant. Digital media exposure was significantly associated with general health (OR=1·14 95%CI 1·03–1·27), and TV use was not.61
Physical activity
Three studies30,43,47 yielding 10 independent outcomes reported associations between screen time and physical activity, with 50% (5/10) being significant. Associations between overall screen time and physical activity consistently yielded significant results (β= −0·08; p=<0·001; One study30 did not report an effect size, but reported that they had a significant association).30,43 Conflicting results were found regarding TV use and physical activity, with one study reporting significant associations (β= −0·15; p=<0·01),43 and another showing no significant associations.47 Significant associations were found between gaming (β= −0·21; p = 0·04),43 and social media use (β= −0·06; p = 0·04),43 but not smartphone use,43 or PC/computer/tablet use.43,47
Weight gain/BMI
There were two studies,31,57 each reporting one outcome each, regarding weight gain. One study found that time spent lying in front of a screen was significantly higher in people who had gained weight during COVID-19, compared to people whose weight had stayed consistent or lost weight (X2 NR; p = 0·002),31 with the other study reporting no differences between overall screen time and BMI.57
Children
In children, 24 studies9,11,15,66,72,74,76,79, 81,83,86,88,90, 91, 92,95,98,99,103,105, 106, 107,109,111 reported 181 outcomes across the following areas: diet, eye health, mental health, physical activity, parental health, physiology, sleep, and problematic behaviours (see Supplementary Table 3).
Diet
One study9 with 35 independent outcomes examined associations between screen time and diet, with 54% of outcomes (19/35) yielding significant results. ‘Extra mobile screen time’ was significantly associated with increases in: appetite (r = 0·13; p=<0·001), sweets and unhealthy food consumption (r = 0·07; p = 0·04), not caring about eating fruit and vegetables (r = 0·09; p = 0·01), late snacking at night (r = 0·16; p=<0·001), and decreases in regular protein intake (r = 0·11; p = 0·003). Non-significant associations included decreases in (or loss of) appetite, and frequently snacking between meals.
Extra TV time was significantly associated with increases in: frequent snacks between meals (r = 0·08; p = 0·04), late snacks at night (r = 0·09; p = 0·01), and decreases in (or loss of) appetite (r = 0·07; p=<0·05). Increases in appetite, not caring about eating fruits and vegetables, and decreases in protein intake were all not significantly associated with extra TV time.
‘Extra laptop screen time’ was positively associated with: not caring about eating fruit and vegetables (r = 0·10; p = 0·005), frequent snacking in between means (r = 0·20; p=<0·001), appetite (r = 0·16; p=<0·001), and negatively associated (a protective effect) with loss of appetite (r=−0·14; p=<0·001). Conversely, increases in sweets and unhealthy foods, decreases in protein intake, and snaking during the night were all not associated with extra laptop screen time.
Increases in ‘video gaming’ were associated with increases in appetite (r = 0·12; p=<0·001), and late snacking during the night (r = 0·09; p = 0·02). Non-significant findings included decreases (or loss of): appetite, protein intake, increases in sweets and unhealthy foods, not caring about eating fruits and vegetables, and frequent snacking between meals.
Remote learning was negatively associated (a protective effect) with increases in snacking in between meals (r=−0·08; p = 0·02), and positively associated with decreases in appetite (r = 0·11; p = 0·002), and decreases in regular protein intake (r = 0·07; p = 0·04). Non-significant associations included increases in appetite and consumption of sweets or unhealthy foods.
Eye health
Three studies15,98,111 reported six independent outcomes between screen time and eye health, with 83% (5/6) being statistically significant. Several types of screen time were significantly associated with myopic symptoms, including overall screen time (OR=1·26 95%CI 1·21–1·31), computer time (with TV time as the reference; OR=1·81 95%CI 1·05–3·12), smartphone use (with TV time as the reference; OR=2·02 95%CI 1·19–3·43), with multiple devices (with TV time as the reference) being non-significant.15 The progression of myopic symptoms was also associated with e-learning screen use (OR=1·07 95%CI 1·06–1·09).111 Furthermore, significant associations were found between digital device usage and digital eye strain (OR=3·6 95%CI 1·7–7·6).
Mental health
Eleven studies,11,72,74,79,83,86,91, 103,105,106,109 with 86 independent outcomes examined screen time and aspects of mental health, with 29% (25/86) being significant.
Nine outcomes examined anxiety and screen time in children, of which 67% (6/9) were significant. Leisure time screen time was significantly associated with state anxiety in children of both healthy weight (r = 0·28; p=<0·05) and children who were overweight or obese (r = 0·20; p=<0·001).11 Playing online games (r = 0·11; p=<0·05), internet browsing (r = 0·21; p=<0·01), TV use (r = 0·16; p=<0·01), and social media use (r = 0·23; p=<0·01) were all also significantly associated with anxiety.103 Increases in overall screen time, however, was not significantly associated with anxiety.86
All four outcomes examining depression and screen time in children yielded significant associations, including between depression and: playing online video games (r = 0·12; p=<0·05); internet browsing (r = 0·21; p=<0·01); TV use (r = 0·16; p=<0·01); and social media use (r = 0·23; p=<0·01).103 Conversely, no significant associations were found between sadness and screen time in any of the seven independent outcomes.72,86
A total of 23 outcomes examined associations between screen time and behavioural factors, with 53% (9/17) of negative behavioural factors being statistically significant. Regarding overall screen time, significant associations were found in the following outcomes: aggression (β= 0·12; 95% CI 0·04 - 0·19); irritability (β= 0·12; 95% CI 0·06 - 0·19); frustration (β= 0·13; 95% CI 0·06 - 0·19); and frequency of temper tantrums (β= 0·10; 95% CI 0·03 - 0·17). Conversely, being afraid and being restless were not significant.72 Increasing total screen time was not associated with anger in any outcome,86 but increases in screen time were associated with fear (p=<0.01).86 Online study time was reported to be associated with mood disturbances (r = 0·43; p=<0·05), whereas leisure screen time was not significant.109 Tablet and smartphone time were both significantly associated with overall behavioural problems (r = 0·22; p=<0·05 and r = 0·17; p=<0·05 respectively), whereas TV time was not.91 Regarding other behavioural factors, child sensitivity, calmness, and affection were not associated with overall screen time.72,86
Seven outcomes examined associations between screen time and stress, with 50% (4/8) being significant. One study found a significant association between overall screen time and stress in a multiple mediation analysis (effect size=0·18; p = 0·05).83 Gaming was reported to be associated with ‘COVID related worries’ (OR=1·6 95%CI 1·1- 2·3), whereas TV time and social media use were not.105 Social media use was reported to be associated with ‘COVID related stress’ (OR=2·1; p=<0·001), whereas TV use and gaming were not.103 Increasing smartphone use was also reported to be associated with psychological distress (r = 0·2; p=<0·01).79
Regarding other aspects of mental health, studies reported increased odds of ‘at least two mental health problems from frequent sadness, irritability, and/or sleep problems’ (OR=2·51 p=<0·001).106 Negative affect was associated with leisure screen time in children with a healthy weight (r = 0·38; p=<0·05), but not in children who were overweight or obese.11 Positive affect was not associated with screen time in children of all weight categories.11 Other studies reported children's emotional and psychological well- being negatively associated with internet browsing (emotional r=−0·16; p=<0·01; psychological r=−0·13; p=<0·05) and social media use (emotional r=−0·12; p=<0·05; psychological r=−0·10; p=<0·05), but not with playing online games or TV use.103 The same study reported that children's social wellbeing was negatively associated (a protective effect) with internet browsing (r=−0·11; p=<0·05), but not with social media use, playing online games or TV use.103 The same study also reported no associations between children's resilience and internet browsing, social media use, TV use or playing online games.103
Physical activity
Regarding physical activity, four studies11,74,76,90 yielded 10 independent outcomes, with 70% (7/10) of outcomes being statistically significant. Overall screen time was negatively associated with physical activity (β= −0·18; 95%CI −0·25; −0·11) in one study,90 with another study (defining screen time as ‘the daily use of digital screens’) yielded non-significant results.76 Leisure screen time was positively associated with sedentary time in both healthy (r = 0·41; p=<0·05) and overweight/obese (r = 0·71; p=<0·05) children, however moderate/vigorous physical activity was not significant in both healthy and overweight/obese children.11 Other studies reported significant negative associations between overall physical activity and leisure (r= −0·16; p=<0·01), and education (r= −0·21; p=<0·01) screen time.74
Parental correlates
Five studies74,83,95,96,109 with 25 independent outcomes examined children's screen time and parental correlates, with 36% (9/25) being significant.
Overall screen time (as reported by the child) was negatively associated with parental screen time rules (β= −3·20; 95%CI −5·30; −2·19) and positively associated with the pandemic's impact on resources (β= 2·06; 95%CI 0·57 - 3·54), however was not significantly associated with: maternal stress; difficult balancing homelife; job/income loss; or difficulty obtaining childcare.95 Overall child screen time (as reported by the mother) in the same study yielded conflicting results, being negatively associated with parental awareness of social media (β=−3·37; 95%CI −4·20; −2·54), parental screen time rules (β =−3·81; 95%CI −5·43; −2·19), and positively associated with maternal stress (β =0·21; 95%CI 0·12 - 0·30). The pandemic's ‘impact on resources’; difficult balancing homelife; job/income loss; and difficulty obtaining childcare were non-significant.95 Overall screen time was also found to be significantly associated with parental screen use (X2=0·17; p=<0·05), but not parental employment status.83
Parental anxiety was significantly associated only with child video gaming (OR=1·78 95%CI 1·02–3·11),96 and not with overall screen time83,96 or TV use.96 Conflicts with parents were also associated with both online (β=0·02; p=<0.05) and leisure based (β=0·06; p=<0.01) screen time.109 Parental stress was not associated with overall screentime,83 screen time for edication,74 or screen time for leisure.74
Weight gain/BMI
Two studies88,99 yielding four independent outcomes reported associations between physiology and screen time, with no significant findings reported between screen time and changes in BMI99 and several categorical weight variables.88
Sleep
Regarding sleep, five studies76,90, 91, 92,107 with seven independent outcomes were included, of which 86% (6/7) were significant.
Sleep duration yielded conflicting results, with one study reporting negative correlations between overall screen time and sleep duration (r=−0·40; p=<0·01),76 and another reporting positive associations (β = 0·003; 95% CI 0·001 - 0·005).90 Non-academic screen time was negatively associated with sleep duration (r=−0·41; p=<0·01).92
Overall screen time was also associated with increased odds of sleep disorders (OR=3·80 95%CI 1·09–13·1),107 and tablet (r = 0·17; p=<0·05) and smartphone time (r = 0·30; p=<0·001) were both associated with ‘sleep problems’ (TV time was not significantly associated with sleep problems).91
Problematic screen time behaviours
Two studies79,81 yielding four independent outcomes were found reporting associations between screen time and problematic screen time behaviours, all of which were statically significant. Gaming time was reported to be significantly associated with gaming disorder symptoms (r = 0·43; p=<0·001),81 and smartphone use was reported to be significantly associated with problematic smartphone use (r = 0·35; p=<0·01), problematic social media use (r = 0·29; p=<0·01), and problematic gaming (r = 0·25; p=<0·01).79
Discussion
This systematic review and meta-analysis, including 89 studies, examined the pooled reported changes in screen time from before the COVID-19 pandemic, and narratively examined correlates associated with screen time during the COVID-19 pandemic.
The results from the meta-analysis showed that all groups significantly increased both their total and leisure screen time. Children of primary age had the largest increase in both total and leisure screen time, followed by adults, with adolescents and young children yielding the smallest increase. Furthermore, 51% of adults and 67% of children reported increases in total screen time, and 52% of adults and 60% of children reported increases in leisure screen time. These results are in line with research showing increases in sedentary behaviours during the COVID-19 pandemic,4 although this study is the first to examine screen time independently. Although the increases in total screen time could be partially caused by increasing time in front of a screen for work or academic purposes (such as increases in online meetings and education), the increases in non-academic screen time in children are concerning. Indeed, it has been reported in pre-COVID-19 reviews that screen time is associated with several unfavourable outcomes, such as increased BMI, increased maternal depression, lower cognitive stimulation at home, decreased quality of life, lower self-esteem, and anxiety.112,113 A recent systematic review and meta-analysis has also concluded that smart device exposure may be associated with increased risk of myopia in children, indicating that increases in screen time during COVID may also lead to increased prevalence of myopia.16 Furthermore, a recent longitudinal study has reported that screen time at the age of 4 is negatively associated with mathematic and literacy grades at the age of 8,114 suggesting that screen time at a younger age could affect future academic achievement. Although the absolute screen time adults and children should adhere to are under debate and not universally agreed upon, there is a growing consensus that leisure screen time should be minimised in favour of physically active pursuits.115 Moreover, the UK Chief Medical Officer recommends that parents of children (of all ages) proactively consider if a child's screen time if affecting sleep, physical activity, and snacking.116
Several negative food behaviours were associated with increases in screen time in both adults and children. These included associations between increased screen time and ‘unhealthy diet changes’, and associations between increased computer, television, and cell phone use and increases in sweet food consumption. Further, increases in computer time for self-directed learning was found to be positively associated with eating related self-regulation while increases in TV time were found to be negatively correlated, and other types of screen time, including computer gaming and overall screen time, were not significantly associated. Importantly, there were more significant associations between increases in screen time in children than in adults, suggesting that appropriate interventions may benefit children more. This broadly concurs with pre-pandemic reviews showing sedentary behaviours (including screen time) are associated with less healthy diets, including lower fruit and vegetable consumption, higher energy dense drinks, fast foods and higher total energy intake in both adults and children.117,118 As the pandemic has resulted in increases in screen time, it is recommended that public health guidance on reduced screen time and healthy dietary behaviours during it be promoted, with a focus on targeting parents and children.
Alcohol use during the pandemic was shown to be negatively associated with increased computer time, however increased television use was associated with an increased desire to drink alcohol (but not with increased consumption). Although other reviews have reported increases in alcohol consumption during the pandemic,119 results from this study suggest that these increases are not associated with screen time. Longitudinal study is warranted to examine these behaviours. Furthermore, all correlates related to smoking (smoking and desire to smoke) were not significantly associated with any type of screen time use, indicating that COVID-19 screen time did not affect smoking habits.
This review found that several eye related correlates were associated with screen time. In adults, increases in screen time was consistently associated with dry eye syndrome, which broadly agrees with previous literature in both a COVID-19 and non-COVID-19 context.120,121 It was also found that more than 6 h of screen time/day was associated with several symptoms of digital eye strain, including tearing, eye strain, dryness, heavy eyelids, red eyes, eye itchiness, burning sensation in the eye, sensitivity of bright light, difficulty focussing, eye pain, the feeling of a foreign body in the eye, and excessive blinking. These results concur with pre-pandemic reviews that have found associations between dry eye syndrome and screen time.120 It has previously been reported that the possible mechanisms for this could be reduced blink rates, meibomian gland dysfunction, and corneal phototoxicity, most likely to be multifactorial,120and further study is warranted, especially longitudinal study to establish temporal relationships.
In children, increased screen time was significantly associated with myopia, with almost all associations being significant. Indeed, every stratified type of screen time significantly correlated with increases in myopia across multiple studies, with the exception of ‘multiple devices’. This is in agreement with a recent meta-analysis that reported associations between screen time and myopia,16 however other reviews have reported mixed results.122 Although the results from this review cannot determine temporal relationships due to the cross-sectional design of included studies, these results concur with longitudinal studies that have found that increased screen time may be a casual factor of myopia in children.123 It is recommended that children minimise screen time (particularly using screens where the child is very close to the screen, such as tablets and phones) use to potentially prevent dry eye and increased risk of myopia. As higher odds of myopia were found in increased smartphone devices, it is also recommended that any e-learning be conducted on a larger screen further away from the eyes, and not on a smartphone device (or similar), to negate these risks.
In adults, studies that measured overall screen time subjectively mostly found significant associations, however the two studies that objectively measured screen time found no significant associations. Regarding different types of screen time, one study found that TV time was associated with COVID-19 related anxiety, with other studies finding no association between TV time and overall anxiety. Due to these conflicting results, it is difficult to come to conclusions regarding screen time and anxiety. This is broadly in agreement with other systematic reviews examining sedentary behaviour (including screen time) and anxiety in adults.124 We agree with Teychenne, Costigan and Parker124 that large longitudinal studies are needed to comprehensively examine this possible association.
In children, there was a general consensus across included studies that overall screen time was not associated with anxiety, however this was not the case regarding stratified screen time. Indeed, studies reported associations between anxiety and leisure screen time, online gaming, internet browsing, TV and social media use, with no stratified type of screen time yielding non-significant results. This is in agreement with other large longitudinal studies that have found associations between screen time and anxiety in adolecents,125,126 however more research is needed in children of younger ages.
In adults, studies reported conflicting results, with different studies reporting significant associations between overall screen time and depression in both directions (e.g. one study showed a protective effect), with other studies reporting no association. The only stratified type of screen time was TV, which was found to be significantly associated. It is likely that these conflicting results are because of heterogeneity in populations, measurement tools, and statistical methodology. Although previous systematic reviews have reported positive associations between screen time and depression in adults, in one review the significance of results changed when stratifying according to gender (only females yielded a significant association).127 Furthermore, other studies have found that only moderate to severe depression is associated with screen time.128 It is therefore difficult to conclude whether depression is associated with screen time during the COVID-19 pandemic – further studies with heterogeneous measurement tools would be highly beneficial.
In contrast to adults, the studies that examined screen time and depression in children all found significant associations, suggesting a link between screen time and depression in children with a higher level of certainty. This is in agreement with previous literature that has concluded that screen time is associated with depression in children, with a significant (non-linear) dose response relationship.129 Although the direction of association is difficult to ascertain, it is recommended that parents monitor screen time usage in children to prevent or identify possible depressive symptoms.
Studies that examined mood changes yielded non-significant results in adults but showed several mood changes that were significantly associated with screen time in children. These significant associations, across several studies included increased aggression, irritability, frustration, temper tantrums, and mood disturbances. When stratified according to type of screen time, personal devices, such as mobile phones and tablets were associated with behavioural problems in children, whereas TV time was not. This concurs with a pre-pandemic umbrella review that found weak evidence for associations between poor mental health outcomes and screen time in children and adolescents.130 As with adults, it is currently unknown as to the mechanisms that drive these associations, and whether they are chronic or acute. For example, a review examining longitudinal studies found no longitudinal associations between increased screen time as a child and most long-term mental health conditions.131
In adults, most studies reported significant (direct whilst indirect were not significant) associations between several types of screen time (including overall screen time) and loneliness, however in one study this was only found in people without concurrent depression. This is in broad agreement with other pre-COVID studies that have found associations between screen time and loneliness, with some studies reporting that decreases in screen time (in particular social media use) can decrease loneliness.132
In children, several stress-related correlates were significantly associated with screen time, while others were not. Although a significant association was found between overall screen time and stress, this was found in only one study. Gaming related screen time was found to be associated with COVID-related worries, but not COVID-related stress. Social media use, on the other hand, was found to be associated with COVID-related stress, but not with COVID-related worries. Smartphone use was associated with psychological distress in one study. Lastly, TV time was not significantly associated with any form of stress in any study. Overall, the evidence is mixed, however previous studies have reported associations between screen time and stress in children.133 This could be because there were no more than one outcome examining the same correlate (except from TV use), and further research is warranted.
Other significant correlates of mental health in adults and children included several types of screen time being associated with general mental health and wellbeing, which concurs with several previous studies that have concluded similar results.127,133 Although when stratified according to type of screen time and type of mental health correlate, it is clear that several of the included studies agree with pre-COVID studies that increases in screen time are linked to negative mental health outcomes.127,133,134 It is therefore recommended that screen time be reduced wherever possible (for example, leisure time screen time) to negate these negative outcomes.
Overall screen time was consistently associated with decreases in physical activity in adults, however conflicting results were found regarding TV time. Furthermore, gaming and social media use were both found to correlate with physical activity, however smartphone use and PC/computer/tablet use were not. Weight gain was associated with time spent lying in front of a TV screen, yet in a different study overall BMI was not associated with overall screen time. Few previous studies have reported associations between screen time and physical activity levels, however studies have reported negative outcomes in adults with high screen time and low physical activity levels, including health related quality of life.135 Although screen time is generally classified as a sedentary behaviour, there are types of screen time that promote physical activity, including exergaming (a type physical activity that is technology-driven, and often includes an element of screen time), a type which has not been explicitly identified in this review. Indeed, exergaming has been shown to reduce anxiety levels and increase physical activity levels,136 and has been postulated as a potential source of physical activity during the COVID-19 pandemic, particularly in times of quarantine.137,138 Primary studies regarding the efficacy and accessibility of exergaming as an alternative to sedentary based screen time behaviours during the COVID-19 pandemic are warranted.
Significant associations between screen time and physical activity in children were conflicting, with some studies reporting negative associations between physical activity and overall, leisure, and education screen time, whereas other studies reported null results. The conflicting results could be due to several factors, including reporting biases and statistical methodology. Regarding sedentary behaviour, screen time was consistently associated in children, however changes in BMI and weight gain were not associated with screen time in any study. This concurs with much of the literature that has found similar associations, predominantly because screen time is usually conducted while in a sedentary position.130 It also agrees with previous reviews that have shown large increases in sedentary behaviour during the pandemic.4 Because several previous studies have found significant negative associations between screen time and physical activity in children of all ages, increases in physical activity and corresponding decreases in screen time being recommended.139, 140, 141
In adults, studies agreed that screen time was not associated with sleep or fatigue correlates, including sleep time. This is in conflict with pre-COVID studies that have found association between screen time and sleep time in adults.142 This conflict may be because people have been reported to experience sleep disturbances as a result of the COVID-19 pandemic.143
Conversely, in children, several studies agreed that increases in screen time were associated with sleep problems, including sleep duration and sleep disorders. The only exception to this appears to be TV time, which was not found to be associated with sleep problems. This is in broad agreement with much of the literature that reports disturbed sleep patterns with increases in screentime.17,18,130 All of these correlations, however, did not adjust for other known correlates of sleep disturbances, such as anxiety and depression.144 Further examination of potential mediating factors is warranted.
Several parental anxiety and parental stress correlates were associated with different types of screen time. Furthermore, conflicts with parents were significantly associated with increases in screen time, although these results should be treated with caution as several correlates were only measured in one study. This concurs with pre-pandemic reviews that have reported that parental stress is associated with child screentime.112,145 One possible reason for this finding is that COVID-related parental COVID-related stress is having a direct impact on child screen time – further longitudinal studies are required to establish temporal relationships.
There was a consensus across studies that screen time was associated with negative screen related behaviours, including problematic gaming and social media use. This is in agreement with the literature, and is a concerning finding because previous studies have reported that problematic screen use is associated with several negative mental health outcomes.12 Furthermore, it has been reported in a recent systematic review and meta-analysis that problematic smartphone behaviours are increasing globally,146 however the majority of included studies (as well as previous literature concerning screen time) did not include problematic usage in their studies.12 It is recommended, therefore, that both screen time and problematic screen time behaviours be monitored in children closely, and sedentary based leisure time screen time be reduced in favour of other activities that have been shown to have positive effects on mental and physical health, including physical activity and exergaming (especially if people are subject to further periods of restrictions).
Although this is the first review examining screen time changes during the COVID-19 pandemic in adults and children, the results of this review should be taken within its limitations. Firstly, there was high heterogeneity in the meta-analysis, which we could not fully explain. It is likely that differing methods of measuring screen time, and different populations, contributed to this. Furthermore, there was a large range in the quality of studies included, which may have added to the heterogeneity. Secondly, although several significant effect sizes were found spanning a wide variety of unfavourable outcomes, several non-significant findings were also found, possibly due to the heterogeneous nature of the included populations and the measures used. Thirdly, the methods of measuring screen time were highly heterogeneous, with some studies using self-report, others using parental report, and others using objective reports – future research should use either validated measures of screen time and/or problematic screen time use, or objective measures of screen time wherever possible. Lastly, although there were several correlates that concurred between studies, other significant correlates were based on one effect size from one study, and therefore the results of these should be treated with caution.
In conclusion, this review has found evidence that both overall and leisure screen time increased during the COVID-19 pandemic, with children of primary school age yielding the highest increases. Furthermore, several unfavourable correlates have been reported to be associated with increases in screen time in both adults and children, including several mental health correlates. In addition to the well-reported benefits of physical activity, it is recommended that leisure screen time should be reduced in favour of non-sedentary activities, including physical activity, especially in children. If, however, physical activity is difficult (for example, in periods of restrictions limiting the ability to go outdoors), screen related physical activity such as exergaming may yield favourable outcomes.
Data sharing statement
All data used in this research was gathered from already existing research. No original data was used for this study. Data extraction tables and figures are available from MT.
Contributors
Mike Trott: conceptualisation; literature search; figures; study design; data collection; data analysis; data interpretation; writing, Robin Driscoll: literature search; data collection; data analysis; writing, Enrico Iraldo: literature search; data collection; writing, Shahina Pardhan: conceptualisation; study design; writing; supervision.
Declaration of interests
None to report.
Funding
No funding was received for this study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101452.
Appendix. Supplementary materials
References
- 1.World Health Organization. WHO Coronovirus Didease (COVID-19) Dashboard. Accessed July 2, 2020. https://covid19.who.int
- 2.British Broadcasting Corporation. Coronavirus: the world in lockdown in maps and charts. Published 2020. Accessed August 12, 2020. https://www.bbc.co.uk/news/world-52103747
- 3.Tremblay M.S., LeBlanc A.G., Kho M.E., et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8(1):98. doi: 10.1186/1479-5868-8-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stockwell S., Trott M., Tully M., et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7(1) doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagata J.M., Magid H.S.A., Gabriel K.P. Screen time for children and adolescents during the COVID-19 pandemic. Obes Silver Spring Md. 2020 doi: 10.1002/oby.22917. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNSECO. 1.37 billion students now home as COVID-19 school closures expand, ministers scale up multimedia approaches to ensure learning continuity. Published 2021. Accessed January 12, 2022. https://en.unesco.org/news/137-billion-students-now-home-covid-19-school-closures-expand-ministers-scale-multimedia
- 7.Górnicka M., Drywień M.E., Zielinska M.A., Hamułka J. Dietary and lifestyle changes during COVID-19 and the subsequent lockdowns among Polish adults: a cross-sectional online survey PLifeCOVID-19 study. Nutrients. 2020;12(8):2324. doi: 10.3390/nu12082324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tebar W.R., Christofaro D.G., Diniz T.A., et al. Increased screen time is associated with alcohol desire and sweetened foods consumption during the COVID-19 pandemic. Front Nutr. 2021;8:78. doi: 10.3389/fnut.2021.630586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hashem S.A., El Refay A.S., Mostafa H.H., Kamel I.H., Sherif L.S. Impact of coronavirus disease-19 lockdown on egyptian children and adolescents: dietary pattern changes health risk. Open Access Maced J Med Sci. 2020;8(T1):561–569. [Google Scholar]
- 10.Meyer J., McDowell C., Lansing J., et al. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int J Environ Res Public Health. 2020;17(18) doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alves JM, Yunker AG, DeFendis A, Xiang AH, Page KA. BMI status and associations between affect, physical activity and anxiety among US children during COVID-19. Pediatr Obes. Published online 2021:e12786. [DOI] [PMC free article] [PubMed]
- 12.Sohn S.Y., Rees P., Wildridge B., Kalk N.J., Carter B. Prevalence of problematic smartphone usage and associated mental health outcomes amongst children and young people: a systematic review, meta-analysis and GRADE of the evidence. BMC Psychiatry. 2019;19(1):356. doi: 10.1186/s12888-019-2350-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pavithra S., Sundar M.D. Assessment of dry eye symptoms and quality of sleep in engineering students during the COVID-19 pandemic. Int J Res Pharm Sci. 2020;11(Special Issue 1) [Google Scholar]
- 14.Alabdulkader B. Effect of digital device use during COVID-19 on digital eye strain. Clin Exp Optom. 2021:1–7. doi: 10.1080/08164622.2021.1878843. Published online. [DOI] [PubMed] [Google Scholar]
- 15.Liu J., Li B., Sun Y., Chen Q., Dang J. Adolescent vision health during the outbreak of COVID-19: association between digital screen use and myopia progression. Front Pediatr. 2021;9:472. doi: 10.3389/fped.2021.662984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Foreman J., Salim A.T., Praveen A., et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit Health. 2021;3(12):e806–e818. doi: 10.1016/S2589-7500(21)00135-7. [DOI] [PubMed] [Google Scholar]
- 17.Carter B., Rees P., Hale L., Bhattacharjee D., Paradkar M.S. Association between portable screen-based media device access or use and sleep outcomes: a systematic review and meta-analysis. JAMA Pediatr. 2016;170(12):1202–1208. doi: 10.1001/jamapediatrics.2016.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sohn S.Y., Krasnoff L., Rees P., Kalk N.J., Carter B. The association between smartphone addiction and sleep: a UK cross-sectional study of young adults. Front Psychiatry. 2021;12:176. doi: 10.3389/fpsyt.2021.629407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kwon M., Lee J.Y., Won W.Y., et al. Development and validation of a smartphone addiction scale (SAS) PloS One. 2013;8(2):e56936. doi: 10.1371/journal.pone.0056936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wells G.A., Shea B., O'connell D., et al. Ottawa Hospital Research Institute; Ottawa (ON): 2009. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Published online 2009. [Google Scholar]
- 22.Modesti P.A., Reboldi G., Cappuccio F.P., et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One. 2016;11(1) doi: 10.1371/journal.pone.0147601. e0147601-e0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borenstein M., Hedges L., Higgins J., Rothstein H. Biostat; 2013. Comprehensive Meta Analysis. [Google Scholar]
- 24.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 25.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta analysis detected by a simple, graphical test. BMJ. 1997 doi: 10.1136/bmj.315.7109.629. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fu R., Gartlehner G., Grant M., et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective health care program. J Clin Epidemiol. 2011;64(11):1187–1197. doi: 10.1016/j.jclinepi.2010.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Sterne J.A., Egger M., Moher D. Addressing reporting biases. Cochrane Handb Syst Rev Interv Cochrane Book Ser. 2008:297–333. Published online. [Google Scholar]
- 28.Duval S., Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000 doi: 10.1111/j.0006-341X.2000.00455.x. Published online. [DOI] [PubMed] [Google Scholar]
- 29.Guyatt G.H., Oxman A.D., Vist G.E., et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abdulsalam N.M., Khateeb N.A., Aljerbi S.S., et al. Assessment of dietary habits and physical activity changes during the full COVID-19 curfew period and its effect on weight among adults in Jeddah, Saudi Arabia. Int J Environ Res Public Health. 2021;18(16):8580. doi: 10.3390/ijerph18168580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agurto H.S., Alcantara-Diaz A.L., Espinet-Coll E., Toro-Huamanchumo C.J. Eating habits, lifestyle behaviors and stress during the COVID-19 pandemic quarantine among Peruvian adults. PeerJ. 2021;9:e11431. doi: 10.7717/peerj.11431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alomari M.A., Khabour O.F., Alzoubi K.H. Changes in physical activity and sedentary behavior amid confinement: the bksq-covid-19 project. Risk Manag Healthc Policy. 2020;13:1757. doi: 10.2147/RMHP.S268320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bird J.M., Karageorghis C.I., Hamer M. Relationships among behavioural regulations, physical activity, and mental health pre-and during COVID–19 UK lockdown. Psychol Sport Exerc. 2021;55 doi: 10.1016/j.psychsport.2021.101945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Branquinho C., Paiva T., Guedes F., Gaspar T., Tomé G., Gaspar de Matos M. Health risk behaviors before and during COVID-19 and gender differences. J Community Psychol. 2021 doi: 10.1002/jcop.22705. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ismail L.C., Osaili T.M., Mohamad M.N., et al. Assessment of eating habits and lifestyle during the coronavirus 2019 pandemic in the Middle East and North Africa region: a cross-sectional study. Br J Nutr. 2021;126(5):757–766. doi: 10.1017/S0007114520004547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conroy D.A., Hadler N.L., Cho E., et al. The effects of COVID-19 stay-at-home order on sleep, health, and working patterns: a survey study of US health care workers. J Clin Sleep Med. 2021;17(2):185–191. doi: 10.5664/jcsm.8808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Constandt B., Thibaut E., De Bosscher V., Scheerder J., Ricour M., Willem A. Exercising in times of lockdown: an analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int J Environ Res Public Health. 2020;17(11):4144. doi: 10.3390/ijerph17114144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coyne P., Staffell Z., Woodruff S.J. Recreational screen time use among a small sample of canadians during the first six months of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(23):12664. doi: 10.3390/ijerph182312664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dragun R., Veček N.N., Marendić M., et al. Have lifestyle habits and psychological well-being changed among adolescents and medical students due to COVID-19 lockdown in Croatia? Nutrients. 2021;13(1):97. doi: 10.3390/nu13010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fraser A.M., Stockdale L.A., Bryce C.I., Alexander B.L. College students’ media habits, concern for themselves and others, and mental health in the era of COVID-19. Psychol Pop Media. 2021 Published online. [Google Scholar]
- 41.Ganne P., Najeeb S., Chaitanya G., Sharma A., Krishnappa N.C. Digital eye strain epidemic amid COVID-19 pandemic–a cross-sectional survey. Ophthalmic Epidemiol. 2021;28(4):285–292. doi: 10.1080/09286586.2020.1862243. [DOI] [PubMed] [Google Scholar]
- 42.Genin P.M., Lambert C., Larras B., et al. How did the COVID-19 confinement period affect our physical activity level and sedentary behaviors? Methodology and first results from the french national ONAPS survey. J Phys Act Health. 2021;18(3):296–303. doi: 10.1123/jpah.2020-0449. [DOI] [PubMed] [Google Scholar]
- 43.Helbach J., Stahlmann K. Changes in digital media use and physical activity in german young adults under the Covid-19 pandemic-a cross-sectional study. J Sports Sci Med. 2021;20(4):642–654. doi: 10.52082/jssm.2021.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hodes L.N., Thomas K.G. Smartphone screen time: inaccuracy of self-reports and influence of psychological and contextual factors. Comput Hum Behav. 2021;115 [Google Scholar]
- 45.Hu Z., Lin X., Kaminga A.C., Xu H. Impact of the COVID-19 epidemic on lifestyle behaviors and their association with subjective well-being among the general population in mainland China: cross-sectional study. J Med Internet Res. 2020;22(8) doi: 10.2196/21176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jia P., Zhang L., Yu W., et al. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: the COVID-19 Impact on Lifestyle Change Survey (COINLICS) Int J Obes. 2021;45(3):695–699. doi: 10.1038/s41366-020-00710-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koohsari M.J., Nakaya T., McCormack G.R., Shibata A., Ishii K., Oka K. Changes in workers’ sedentary and physical activity behaviors in response to the COVID-19 pandemic and their relationships with fatigue: longitudinal online study. JMIR Public Health Surveill. 2021;7(3):e26293. doi: 10.2196/26293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kowalsky R.J., Farney T.M., Kline C.E., Hinojosa J.N., Creasy S.A. The impact of the covid-19 pandemic on lifestyle behaviors in US college students. J Am Coll Health. 2021:1–6. doi: 10.1080/07448481.2021.1923505. Published online. [DOI] [PubMed] [Google Scholar]
- 49.Lawrence S.A., Garcia J., Stewart C., Rodriguez C. The mental and behavioral health impact of COVID-19 stay at home orders on social work students. Soc Work Educ. 2021:1–15. Published online. [Google Scholar]
- 50.Le C., Khalid Z., Avramut C., Lam A., Ragina N., Zyzanski S. Psychological effects of screen time in health care workers during the COVID-19 pandemic. Prim Care Companion CNS Disord. 2021;23(5) doi: 10.4088/PCC.21m02959. 0-0. [DOI] [PubMed] [Google Scholar]
- 51.Majumdar P., Biswas A., Sahu S. COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol Int. 2020;37(8):1191–1200. doi: 10.1080/07420528.2020.1786107. [DOI] [PubMed] [Google Scholar]
- 52.Mon-López D., Bernardez-Vilaboa R., Fernandez-Balbuena A.A., Sillero-Quintana M. The influence of COVID-19 isolation on physical activity habits and its relationship with convergence insufficiency. Int J Environ Res Public Health. 2020;17(20):7406. doi: 10.3390/ijerph17207406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Oswald T.K., Rumbold A.R., Kedzior S.G., Kohler M., Moore V.M. Mental health of young australians during the COVID-19 pandemic: exploring the roles of employment precarity, screen time, and contact with nature. Int J Environ Res Public Health. 2021;18(11):5630. doi: 10.3390/ijerph18115630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Robbins R., Weaver M.D., Czeisler M.É., Barger L.K., Quan S.F., Czeisler C.A. Associations between changes in daily behaviors and self-reported feelings of depression and anxiety about the COVID-19 pandemic among older adults. J Gerontol B Psychol Sci Soc Sci. June 22, 2021:gbab110. doi: 10.1093/geronb/gbab110. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rodríguez-Larrad A., Mañas A., Labayen I., et al. Impact of COVID-19 confinement on physical activity and sedentary behaviour in Spanish University Students: role of gender. Int J Environ Res Public Health. 2021;18(2):369. doi: 10.3390/ijerph18020369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sallie S.N., Ritou V.J.E., Bowden-Jones H., Voon V. Assessing online gaming and pornography consumption patterns during COVID-19 isolation using an online survey: highlighting distinct avenues of problematic internet behavior. Addict Behav. 2021;123 doi: 10.1016/j.addbeh.2021.107044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saxena R., Parmar N., Kaur P., Allen T. Effect of screen-time on sleep pattern and dietary habits among college-going students in COVID-19 pandemic. Indian J Community Health. 2021;33(1) [Google Scholar]
- 58.Sewall C.J., Goldstein T.R., Rosen D. Objectively measured digital technology use during the COVID-19 pandemic: impact on depression, anxiety, and suicidal ideation among young adults. J Affect Disord. 2021;288:145–147. doi: 10.1016/j.jad.2021.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Spence J.C., Rhodes R.E., McCurdy A., Mangan A., Hopkins D., Mummery W.K. Determinants of physical activity among adults in the United Kingdom during the COVID-19 pandemic: the DUK-COVID study. Br J Health Psychol. 2021;26(2):588–605. doi: 10.1111/bjhp.12497. [DOI] [PubMed] [Google Scholar]
- 60.Stieger S., Lewetz D., Swami V. Emotional well-being under conditions of lockdown: an experience sampling study in Austria during the COVID-19 pandemic. J Happiness Stud. 2021:1–18. doi: 10.1007/s10902-020-00337-2. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Suka M., Yamauchi T., Yanagisawa H. Changes in health status, workload, and lifestyle after starting the COVID-19 pandemic: a web-based survey of Japanese men and women. Environ Health Prev Med. 2021;26(1):1–11. doi: 10.1186/s12199-021-00957-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tan S.T., Tan S.S., Tan C.X. Screen time-based sedentary behaviour, eating regulation and weight status of university students during the COVID-19 lockdown. Nutr Food Sci. 2021 doi: 10.3390/ijerph18137125. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zarco-Alpuente A., Ballester-Arnal R., Billieux J., et al. Problematic internet use prior to and during the COVID-19 pandemic. Cyberpsychology J Psychosoc Res Cyberspace. 2021;15(4) [Google Scholar]
- 64.Werneck A.O., Silva D.R., Malta D.C., et al. Associations of sedentary behaviours and incidence of unhealthy diet during the COVID-19 quarantine in Brazil. Public Health Nutr. 2021;24(3):422–426. doi: 10.1017/S1368980020004188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Woodruff S.J., Coyne P., St-Pierre E. Stress, physical activity, and screen-related sedentary behaviour within the first month of the COVID-19 pandemic. Appl Psychol Health Well-Being. 2021;13(2):454–468. doi: 10.1111/aphw.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang S, Guo B, Ao L, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes. 10.1111/cob.12416 [DOI] [PMC free article] [PubMed]
- 67.Zajacova A., Jehn A., Stackhouse M., Denice P., Ramos H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Can J Public Health. 2020;111(6):953–962. doi: 10.17269/s41997-020-00434-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang Y., Zhang Y., Deng R., et al. Association of sleep duration and screen time with anxiety of pregnant women during the COVID-19 pandemic. Front Psychol. 2021;12:1094. doi: 10.3389/fpsyg.2021.646368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhou H., Dai X., Lou L., Zhou C., Zhang W. Association of sedentary behavior and physical activity with depression in sport university students. Int J Environ Res Public Health. 2021;18(18):9881. doi: 10.3390/ijerph18189881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sañudo B., Fennell C., Sánchez-Oliver A.J. Objectively-assessed physical activity, sedentary behavior, smartphone use, and sleep patterns preand during-COVID-19 quarantine in young adults from Spain. Sustain Switz. 2020;12(15) doi: 10.3390/SU12155890. [DOI] [Google Scholar]
- 71.Abid R., Ammar A., Maaloul R., Souissi N., Hammouda O. Effect of COVID-19-related home confinement on sleep quality, screen time and physical activity in tunisian boys and girls: a survey. Int J Environ Res Public Health. 2021;18(6):3065. doi: 10.3390/ijerph18063065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aguilar-Farias N., Toledo-Vargas M., Miranda-Marquez S., et al. Sociodemographic predictors of changes in physical activity, screen time, and sleep among toddlers and preschoolers in chile during the covid-19 pandemic. Int J Environ Res Public Health. 2021;18(1):176. doi: 10.3390/ijerph18010176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beck A.L., Huang J.C., Lendzion L., Fernandez A., Martinez S. Impact of the COVID-19 pandemic on parents’ perception of health behaviors in children with overweight and obesity. Acad Pediatr. 2021 doi: 10.1016/j.acap.2021.05.015. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Breidokienė R., Jusienė R., Urbonas V., Praninskienė R., Girdzijauskienė S. Vol. 9. Multidisciplinary Digital Publishing Institute; 2021. p. 756. (Sedentary Behavior among 6–14-Year-Old Children during the COVID-19 Lockdown and Its Relation to Physical and Mental Health). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brzęk A., Strauss M., Sanchis-Gomar F., Leischik R. Physical activity, screen time, sedentary and sleeping habits of polish preschoolers during the COVID-19 pandemic and WHO's recommendations: an observational cohort study. Int J Environ Res Public Health. 2021;18(21):11173. doi: 10.3390/ijerph182111173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cachón-Zagalaz J., Zagalaz-Sánchez M., Arufe-Giráldez V., Sanmiguel-Rodríguez A., González-Valero G. Physical activity and daily routine among children aged 0–12 during the COVID-19 pandemic in Spain. Int J Environ Res Public Health. 2021;18(2):703. doi: 10.3390/ijerph18020703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cahal M., Amirav I., Diamant N., Be'er M., Besor O., Lavie M. Real-time effects of COVID-19 pandemic lockdown on pediatric respiratory patients. Pediatr Pulmonol. 2021;56(6):1401–1408. doi: 10.1002/ppul.25310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chambonniere C., Lambert C., Fearnbach N., et al. Effect of the COVID-19 lockdown on physical activity and sedentary behaviors in french children and adolescents: new results from the ONAPS national survey. Eur J Integr Med. 2021;43 doi: 10.1016/j.eujim.2021.101308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen I.H., Chen C.Y., Pakpour A.H., et al. Problematic internet-related behaviors mediate the associations between levels of internet engagement and distress among schoolchildren during COVID-19 lockdown: a longitudinal structural equation modeling study. J Behav Addict. 2021;10(1):135–148. doi: 10.1556/2006.2021.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sá C dos SC de, Pombo A., Luz C., Rodrigues L.P., Cordovil R. Covid-19 social isolation in brazil: effects on the physical activity routine of families with children. Rev Paul Pediatr. 2020:39. doi: 10.1590/1984-0462/2021/39/2020159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Donati M.A., Guido C.A., De Meo G., et al. Gaming among children and Adolescents during the COVID-19 lockdown: the role of parents in time spent on video games and gaming disorder symptoms. Int J Environ Res Public Health. 2021;18(12):6642. doi: 10.3390/ijerph18126642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dubuc M.M., Berrigan F., Goudreault M., Beaudoin S., Turcotte S. COVID-19 impact on adolescent 24h movement behaviors. Int J Environ Res Public Health. 2021;18(17):9256. doi: 10.3390/ijerph18179256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Farah R., Zivan M., Niv L., Havron N., Hutton J., Horowitz-Kraus T. High screen use by children aged 12-36 months during the first COVID-19 lockdown was associated with parental stress and screen use. Acta Paediatr. 2021 doi: 10.1111/apa.15979. Published online. [DOI] [PubMed] [Google Scholar]
- 84.Fillon A., Lambert C., Tardieu M., et al. Impact of the COVID-19 confinement on movement behaviors among French young children: the ONAPS national survey. Minerva Pediatr. 2021 doi: 10.23736/S2724-5276.21.06194-2. Published online. [DOI] [PubMed] [Google Scholar]
- 85.Garcia J.M., Lawrence S., Brazendale K., Leahy N., Fukuda D. Brief report: the impact of the COVID-19 pandemic on health behaviors in adolescents with Autism Spectrum Disorder. Disabil Health J. 2021;14(2) doi: 10.1016/j.dhjo.2020.101021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Giannini D.T., Tavares C.M., Takey M., et al. Adolescents emotional state and behavioral and dietary habit changes during isolation due to the COVID-19 pandemic. J Am Coll Nutr. 2021:1–9. doi: 10.1080/07315724.2021.1897899. Published online. [DOI] [PubMed] [Google Scholar]
- 87.feng Guo Y, qi Liao M, li Cai W, et al. Physical activity, screen exposure and sleep among students during the pandemic of COVID-19. Sci Rep. 2021;11(1):1–11. doi: 10.1038/s41598-021-88071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hadianfard A.M., Mozaffari-Khosravi H., Karandish M., Azhdari M. Physical activity and sedentary behaviors (screen time and homework) among overweight or obese adolescents: a cross-sectional observational study in Yazd, Iran. BMC Pediatr. 2021;21(1):421. doi: 10.1186/s12887-021-02892-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hyunshik K., Jiameng M., Sunkyoung L., Ying G. Change in Japanese children's 24-hour movement guidelines and mental health during the COVID-19 pandemic. Sci Rep. 2021;11(1):22972. doi: 10.1038/s41598-021-01803-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jáuregui A., Argumedo G., Medina C., Bonvecchio-Arenas A., Romero-Martínez M., Okely A.D. Factors associated with changes in movement behaviors in toddlers and preschoolers during the COVID-19 pandemic: a national cross-sectional study in Mexico. Prev Med Rep. 2021;24 doi: 10.1016/j.pmedr.2021.101552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kim S.J., Lee S., Han H., Jung J., Yang S.J., Shin Y. Parental mental health and children's behaviors and media usage during COVID-19-related school closures. J Korean Med Sci. 2021;36(25) doi: 10.3346/jkms.2021.36.e184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lim M.T.C., Ramamurthy M.B., Aishworiya R., et al. School closure during the coronavirus disease 2019 (COVID-19) pandemic–Impact on children's sleep. Sleep Med. 2021;78:108–114. doi: 10.1016/j.sleep.2020.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.López-Gil J.F., Tremblay M.S., Brazo-Sayavera J. Changes in healthy behaviors and meeting 24-h movement guidelines in Spanish and Brazilian preschoolers, children and adolescents during the COVID-19 lockdown. Children. 2021;8(2):83. doi: 10.3390/children8020083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ma D., Wei S., Li S.M., et al. Progression of myopia in a natural cohort of Chinese children during COVID-19 pandemic. Graefes Arch Clin Exp Ophthalmol. 2021;259(9):2813–2820. doi: 10.1007/s00417-021-05305-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.McArthur B.A., Racine N., Browne D., McDonald S., Tough S., Madigan S. Recreational Screen Time Before and During COVID-19 in school aged children. Acta Paediatr. 2021 doi: 10.1111/apa.15966. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.McCormack G.R., Doyle-Baker P.K., Petersen J.A., Ghoneim D. Parent anxiety and perceptions of their child's physical activity and sedentary behaviour during the COVID-19 pandemic in Canada. Prev Med Rep. 2020;20 doi: 10.1016/j.pmedr.2020.101275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mitra R., Moore S.A., Gillespie M., et al. Healthy movement behaviours in children and youth during the COVID-19 pandemic: exploring the role of the neighbourhood environment. Health Place. 2020;65 doi: 10.1016/j.healthplace.2020.102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mohan A., Sen P., Shah C., Jain E., Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: digital eye strain among kids (DESK study-1) Indian J Ophthalmol. 2021;69(1):140. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nassar M.F., Allam M.F., Shata M.O. Effect of COVID-19 lockdown on young Egyptian soccer players. Glob Pediatr Health. 2021;8 doi: 10.1177/2333794X211012980. 2333794×211012980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nathan A., George P., Ng M., et al. Impact of COVID-19 restrictions on western Australian children's physical activity and screen time. Int J Environ Res Public Health. 2021;18(5):2583. doi: 10.3390/ijerph18052583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Peddie M.C., Scott T., Haszard J.J. Using a 24h Activity Recall (STAR-24) to Describe Activity in Adolescent Boys in New Zealand: comparisons between a Sample Collected before, and a Sample Collected during the COVID-19 Lockdown. Int J Environ Res Public Health. 2021;18(15):8035. doi: 10.3390/ijerph18158035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Schmidt S.C., Anedda B., Burchartz A., et al. Physical activity and screen time of children and adolescents before and during the COVID-19 lockdown in Germany: a natural experiment. Sci Rep. 2020;10(1):1–12. doi: 10.1038/s41598-020-78438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sikorska I., Lipp N., Wróbel P., Wyra M. Adolescent mental health and activities in the period of social isolation caused by the COVID-19 pandemic. Postępy Psychiatr Neurol Adv Psychiatry Neurol. 2021;30(2) doi: 10.5114/ppn.2021.108472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Siste K., Hanafi E., Sen L.T., et al. Implications of COVID-19 and lockdown on internet addiction among adolescents: data from a developing country. Front Psychiatry. 2021:12. doi: 10.3389/fpsyt.2021.665675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sciberras E., Patel P., Stokes M.A., et al. Physical health, media use, and mental health in children and adolescents with ADHD during the COVID-19 pandemic in australia. J Atten Disord. 2020 doi: 10.1177/1087054720978549. Published online1087054720978549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Szwarcwald C.L., Malta D.C., Barros M.B., de A., et al. Associations of sociodemographic factors and health behaviors with the emotional well-being of adolescents during the COVID-19 Pandemic in Brazil. Int J Environ Res Public Health. 2021;18(11):6160. doi: 10.3390/ijerph18116160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Windiani I.G.A.T., Noviyani N.M.R., Adnyana I.G.A.N.S., Murti N.L.S.P., Soetjiningsih S. Prevalence of sleep disorders in adolescents and its relation with screen time during the COVID-19 Pandemic Era. Open Access Maced J Med Sci. 2021;9(B):297–300. [Google Scholar]
- 108.Wunsch K., Nigg C., Niessner C., et al. The impact of COVID-19 on the interrelation of physical activity, screen time and health-related quality of life in children and adolescents in germany: results of the motorik-modul study. Children. 2021;8(2):98. doi: 10.3390/children8020098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xiao S., Yan Z., Zhao L. Physical activity, screen time, and mood disturbance among chinese adolescents during COVID-19. J Psychosoc Nurs Ment Health Serv. 2021;59(4):14–20. doi: 10.3928/02793695-20201104-04. [DOI] [PubMed] [Google Scholar]
- 110.Constant A., Conserve D.F., Gallopel-Morvan K., Raude J. Socio-cognitive factors associated with lifestyle changes in response to the COVID-19 epidemic in the general population: results from a cross-sectional study in France. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.579460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Liu J., Li B., Chen Q., Dang J. Multidisciplinary Digital Publishing Institute; 2021. Student Health Implications of School Closures During the COVID-19 Pandemic: New Evidence on the Association of e-Learning, Outdoor Exercise, and Myopia; p. 500. Vol 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Duch H., Fisher E.M., Ensari I., Harrington A. Screen time use in children under 3 years old: a systematic review of correlates. Int J Behav Nutr Phys Act. 2013;10(1):102. doi: 10.1186/1479-5868-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Saunders T.J., Vallance J.K. Screen Time and Health Indicators Among Children and Youth: current Evidence, Limitations and Future Directions. Appl Health Econ Health Policy. 2017;15(3):323–331. doi: 10.1007/s40258-016-0289-3. [DOI] [PubMed] [Google Scholar]
- 114.Cerniglia L., Cimino S., Ammaniti M. What are the effects of screen time on emotion regulation and academic achievements? A three-wave longitudinal study on children from 4 to 8 years of age. J Early Child Res. 2021;19(2):145–160. [Google Scholar]
- 115.World Health Organization. To grow up healthy, children need to sit less and play more. To grow up healthy, children need to sit less and play more. Published 2019. Accessed September 9, 2021. https://www.who.int/news/item/24-04-2019-to-grow-up-healthy-children-need-to-sit-less-and-play-more
- 116.Davis S.C., Atherton F., Calderwood C., McBride M. United Kingdom Chief Medical Officers’ commentary on ‘Screen-based activities and children and young people's mental health and psychosocial wellbeing: a systematic map of reviews.’. Depart Health Social Care. 2019 http://eppi.ioe.ac.uk/cms/Default.aspx?tabid=3748 PublishedAccessed September 9, 2021. [Google Scholar]
- 117.Pearson N., Biddle S.J.H. Sedentary behavior and dietary intake in children, adolescents, and adults. A systematic review. Am J Prev Med. 2011;41(2):178–188. doi: 10.1016/j.amepre.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 118.Hobbs M., Pearson N., Foster P.J., Biddle S.J.H. Sedentary behaviour and diet across the lifespan: an updated systematic review. Br J Sports Med. 2015;49(18):1179–1188. doi: 10.1136/bjsports-2014-093754. [DOI] [PubMed] [Google Scholar]
- 119.Calina D., Hartung T., Mardare I., et al. COVID-19 pandemic and alcohol consumption: impacts and interconnections. Toxicol Rep. 2021;8:529–535. doi: 10.1016/j.toxrep.2021.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mehra D., Galor A. Digital Screen Use and Dry Eye: a Review. Asia-Pac J Ophthalmol. 2020;9(6) doi: 10.1097/APO.0000000000000328. https://journals.lww.com/apjoo/Fulltext/2020/12000/Digital_Screen_Use_and_Dry_Eye__A_Review.3.aspx [DOI] [PubMed] [Google Scholar]
- 121.Prescott C.R. Increased screen time and dry eye: another complication of COVID-19. Eye Contact Lens. 2021;47(8) doi: 10.1097/ICL.0000000000000820. 433-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lanca C., Saw S.M. The association between digital screen time and myopia: a systematic review. Ophthalmic Physiol Opt. 2020;40(2):216–229. doi: 10.1111/opo.12657. [DOI] [PubMed] [Google Scholar]
- 123.Yang G.Y., Huang L.H., Schmid K.L., et al. Associations between screen exposure in early life and myopia amongst Chinese preschoolers. Int J Environ Res Public Health. 2020;17(3):1056. doi: 10.3390/ijerph17031056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Teychenne M., Costigan S.A., Parker K. The association between sedentary behaviour and risk of anxiety: a systematic review. BMC Public Health. 2015;15(1):513. doi: 10.1186/s12889-015-1843-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Khouja J.N., Munafò M.R., Tilling K., et al. Is screen time associated with anxiety or depression in young people? Results from a UK birth cohort. BMC Public Health. 2019;19(1):82. doi: 10.1186/s12889-018-6321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Gunnell K.E., Flament M.F., Buchholz A., et al. Examining the bidirectional relationship between physical activity, screen time, and symptoms of anxiety and depression over time during adolescence. Prev Med. 2016;88:147–152. doi: 10.1016/j.ypmed.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 127.Wang X., Li Y., Fan H. The associations between screen time-based sedentary behavior and depression: a systematic review and meta-analysis. BMC Public Health. 2019;19(1):1524. doi: 10.1186/s12889-019-7904-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Madhav K.C., Sherchand S.P., Sherchan S. Association between screen time and depression among US adults. Prev Med Rep. 2017;8:67–71. doi: 10.1016/j.pmedr.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Liu M., Wu L., Yao S. Dose–response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br J Sports Med. 2016;50(20):1252. doi: 10.1136/bjsports-2015-095084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Stiglic N., Viner R.M. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. 2019;9(1) doi: 10.1136/bmjopen-2018-023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tang S., Werner-Seidler A., Torok M., Mackinnon A.J., Christensen H. The relationship between screen time and mental health in young people: a systematic review of longitudinal studies. Clin Psychol Rev. 2021 doi: 10.1016/j.cpr.2021.102021. Published online. [DOI] [PubMed] [Google Scholar]
- 132.Hunt M.G., Marx R., Lipson C., Young J. No more FOMO: limiting social media decreases loneliness and depression. J Soc Clin Psychol. 2018;37(10):751–768. [Google Scholar]
- 133.Neophytou E., Manwell L.A., Eikelboom R. Effects of Excessive Screen Time on Neurodevelopment, Learning, Memory, Mental Health, and Neurodegeneration: a Scoping Review. Int J Ment Health Addict. 2021;19(3):724–744. doi: 10.1007/s11469-019-00182-2. [DOI] [Google Scholar]
- 134.Stiglic N., Viner R.M. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. 2019;9(1) doi: 10.1136/bmjopen-2018-023191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Davies C.A., Vandelanotte C., Duncan M.J., van Uffelen J.G.Z. Associations of physical activity and screen-time on health related quality of life in adults. Prev Med. 2012;55(1):46–49. doi: 10.1016/j.ypmed.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 136.Viana R.B., Dankel S.J., Loenneke J.P., et al. The effects of exergames on anxiety levels: a systematic review and meta-analysis. Scand J Med Sci Sports. 2020;30(7):1100–1116. doi: 10.1111/sms.13654. [DOI] [PubMed] [Google Scholar]
- 137.Rüth M., Kaspar K. Educational and social exergaming: a perspective on physical, social, and educational benefits and pitfalls of exergaming at home during the COVID-19 pandemic and afterwards. Front Psychol. 2021;12:857. doi: 10.3389/fpsyg.2021.644036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Corregidor-Sánchez A.I., Polonio-López B., Martin-Conty J.L., et al. Exergames to prevent the secondary functional deterioration of older adults during hospitalization and isolation periods during the COVID-19 pandemic. Sustainability. 2021;13(14):7932. [Google Scholar]
- 139.Boone J.E., Gordon-Larsen P., Adair L.S., Popkin B.M. Screen time and physical activity during adolescence: longitudinal effects on obesity in young adulthood. Int J Behav Nutr Phys Act. 2007;4(1):1–10. doi: 10.1186/1479-5868-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Janssen X., Martin A., Hughes A.R., Hill C.M., Kotronoulas G., Hesketh K.R. Associations of screen time, sedentary time and physical activity with sleep in under 5s: a systematic review and meta-analysis. Sleep Med Rev. 2020;49 doi: 10.1016/j.smrv.2019.101226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Venetsanou F., Kambas A., Gourgoulis V., Yannakoulia M. Physical activity in pre-school children: trends over time and associations with body mass index and screen time. Ann Hum Biol. 2019;46(5):393–399. doi: 10.1080/03014460.2019.1659414. [DOI] [PubMed] [Google Scholar]
- 142.Lakerveld J., Mackenbach J.D., Horvath E., et al. The relation between sleep duration and sedentary behaviours in European adults. Obes Rev. 2016;17(S1):62–67. doi: 10.1111/obr.12381. [DOI] [PubMed] [Google Scholar]
- 143.Jahrami Haitham, BaHammam Ahmed S., Bragazzi Nicola Luigi, Saif Zahra, Faris MoezAlIslam, Vitiello Michael V. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 17(2):299–313. 10.5664/jcsm.8930 [DOI] [PMC free article] [PubMed]
- 144.Baddam S.K., Canapari C.A., Van Noordt S.J., Crowley M.J. Sleep disturbances in child and adolescent mental health disorders: a review of the variability of objective sleep markers. Med Sci. 2018;6(2):46. doi: 10.3390/medsci6020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Xu H., Wen L.M., Rissel C. Associations of parental influences with physical activity and screen time among young children: a systematic review. J Obes. 2015:2015. doi: 10.1155/2015/546925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Olson J.A., Sandra D.A., Colucci É.S., et al. Smartphone addiction is increasing across the world: a meta-analysis of 24 countries. Comput Hum Behav. 2022;129 doi: 10.1016/j.chb.2021.107138. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.