Abstract
Obesity is a multifactorial disease with both genetic and environmental components. The prevailing view is that obesity results from an imbalance between energy intake and expenditure caused by overeating and insufficient exercise. We describe another environmental element that can alter the balance between energy intake and energy expenditure: obesogens. Obesogens are a subset of environmental chemicals that act as endocrine disruptors affecting metabolic endpoints. The obesogen hypothesis posits that exposure to endocrine disruptors and other chemicals can alter the development and function of the adipose tissue, liver, pancreas, gastrointestinal tract, and brain, thus changing the set point for control of metabolism. Obesogens can determine how much food is needed to maintain homeostasis and thereby increase the susceptibility to obesity. The most sensitive time for obesogen action is in utero and early childhood, in part via epigenetic programming that can be transmitted to future generations. This review explores the evidence supporting the obesogen hypothesis and highlights knowledge gaps that have prevented widespread acceptance as a contributor to the obesity pandemic. Critically, the obesogen hypothesis changes the narrative from curing obesity to preventing obesity.
Keywords: Obesogen, Adipocyte differentiation, Weight gain, Obesity, Endocrine disruptor
1. Introduction
1.1. Obesity
Obesity is a chronic, relapsing condition characterized by excess body fat [1,2]. Obesity has increased worldwide in every country studied in the last 50 years and is now considered a global pandemic [3]. The number of overweight and obese people is currently greater than those underweight [4]. Obesity results from long-term energy imbalance characterized by a weight shift over height setpoint towards higher values. It is commonly defined by a Body Mass Index (BMI) above 30 kg/m2 in Western countries. The prevailing view is that the energy imbalance characterizing obesity is due to overeating and insufficient exercise. However, obesity is a multifactorial disease with many underlying intertwined causes, including genetics and environmental factors, including components of the exposome such as drugs, environmental chemicals, stress, and altered gut microbiome [2]. There is increasing attention on the impact of environmental chemicals called obesogens on the development of obesity.
This is the second of three reviews focusing on obesity. The first, Obesity I, developed an overview of obesity focusing on causes and mechanisms. Obesity III focuses on assays for defining a chemical as an obesogen or potential obesogen. This review, Obesity II, focuses on evidence supporting the obesogen hypothesis, known obesogens and their mechanisms of action. We then discuss knowledge gaps and experimental discrepancies that have hampered the acceptance of the obesogen hypothesis as an essential contributor to the obesity pandemic.
1.2. Endocrine disrupting chemicals (EDCs)
Many thousands of chemicals are used in commerce today, yet most health hazards have not been characterized. Chemical toxicants have several modes of action. These include specific or non-specific lethality, organ toxicity, genotoxicity, and mutagenicity through DNA sequence and structural alterations. They can also disrupt hormone levels or action, as with EDCs [5]. EDCs have an array of key characteristics, including the ability to interact with or activate hormone receptors, antagonize hormone receptors, alter hormone receptor expression, alter signal transduction in hormone-responsive cells, induce epigenetic modifications in hormone-producing or hormone-responsive cells, alter hormone synthesis, alter hormone transport across cell membranes, alter hormone distribution or circulating hormone levels [6].
The Endocrine Society outlined the toxicity of EDCs, including their effects on a variety of diseases, in 2015 [7]. Currently, about 1000 chemicals are designated as EDCs [8]. EDCs can mimic the actions of endogenous hormones, but their effects may not be as specific as hormones that bind to cognate receptors. The EDC bisphenol A (BPA), for example, binds to estrogen (ER), androgen (AR), thyroid (TR), and the peroxisome proliferator-activated receptor-gamma (PPARγ).
EDCs have two other characteristics that distinguish them from most other toxicants. Like endogenous hormones, they can act at very low concentrations, often lower than known environmental exposures. EDCs, like bona fide hormones, can elicit non-monotonic dose response profiles where the effects of low doses may differ from the effects of higher doses [9]. Such non-monotonic dose–response can be explained by the impact of EDCs on multiple receptor-mediated pathways, including antagonistic effects on some with different dose response profiles and effects on receptor number and turnover, extinguishing the response at high doses [10,11].
1.3. Obesogens
1.3.1. Definition
Obesogens are chemicals that elicit increased white adipose tissue mass (WAT) after exposure in vivo, reviewed in [12-15]. Potential obesogens are chemicals that can induce differentiation of adipocytes in vitro but have not yet been demonstrated to increase WAT accumulation in vivo. Obesogenic chemicals can act directly on adipose tissue physiology by modulating the commitment of stem cells, their differentiation into adipocytes, and the number size and triglyceride content of adipocytes.
1.3.2. Novelty
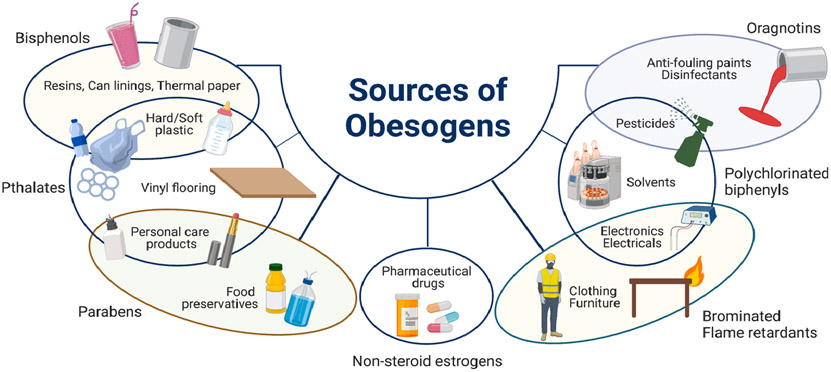
Exposure to obesogenic chemicals is an under-recognized and understudied factor in the obesity pandemic. Indeed, many chemicals known to be obesogenic in animal models have also been associated with increased obesity prevalence, BMI, and body weight in humans [13]. Research in this area has burgeoned, and numerous recent reviews have summarized aspects of obesogen research [e.g. [12,14,16-19]]. A history of the obesogen field was published [20]. Obesogens are prevalent in our environment and have been identified in dust, water, food contamination, processed foods (including food additives), food packaging, food and storage containers, cosmetics and personal care products, furniture and electronics, air pollution, and solvents, disinfectants, pesticides, sunscreens, plastics and plasticizers, nonnutritive sweeteners, some antidepressants and antidiabetic drugs, and common household products [7,18] (Fig. 1).
Fig. 1. Sources of obesogens.
This figure shows just some of the major classes of obesogens along with some sources of exposure. Exposure to obesogens occurs at home and work; via the air, water, food and skin contact.
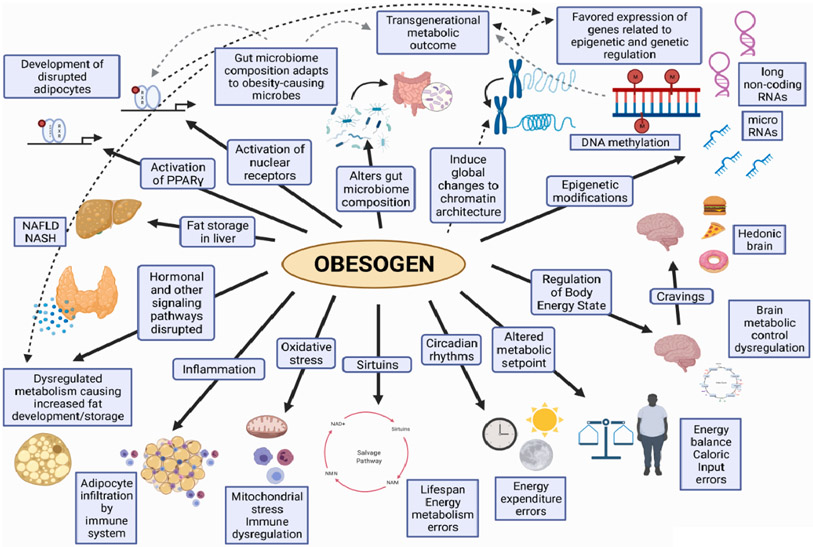
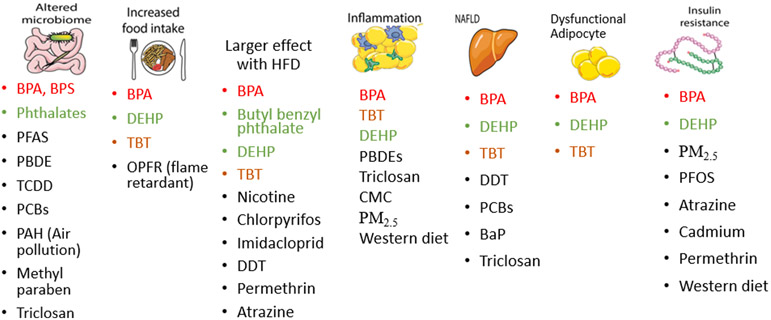
1.3.3. Metabolic disruption
Obesogens may have more diverse effects on metabolic health (e.g., type 2 diabetes (T2D), non-alcoholic fatty liver disease (NAFLD), insulin resistance) than just contributing directly to increased fat mass. For example, obesogens can modify the metabolic rate, gut microbiota composition, and hormonal control of eating behavior. Some obesogens also affect thyroid function, a key mediator of carbohydrate and lipid metabolism, fat oxidation, food intake and resting metabolic rate. Most obesogens are a subset of a larger class of chemicals termed metabolism disrupting chemicals (MDCs), not all of which are obesogens, reviewed in [13,20]. Considering the diverse pathways important for the development of obesity, it is noteworthy that some chemicals classified as obesogens are not EDCs because they don’t influence obesity via an endocrine mode of action. Below we summarize what is known about the mechanisms underlying obesogen action, discuss newly identified obesogens and potentially obesogenic chemicals, and propose essential areas for future research.
1.3.4. Timing of action
The Developmental Origins of Health and Disease (DOHaD) paradigm initially focused on altered nutrition during pregnancy and its effects on diseases, including obesity later in life [21]. It soon became apparent that there are sensitive windows of vulnerability for exposure to EDCs, including obesogens [22]. This increased sensitivity to obesogens, during development results from multiple interacting factors, including developmental plasticity of metabolic tissues and central control of feeding behaviors [23], epigenetic remodeling, an immature immune system, lack of DNA repair, and poor liver metabolism and partly developed blood–brain and blood-organ barriers. These factors allow chemicals to have longer half-lives and reach tissues normally unreachable [23]. Development is controlled by hormones and growth factors that determine which genes are turned on and off in a synchronized fashion leading to the development of normal tissues. EDCs, including obesogens, alter hormone action at critical times, leading to changes in epigenetic patterns and gene expression, resulting in increased susceptibility to metabolic diseases and obesity later in life.
1.3.5. Characteristics
Several important characteristics of obesogen action during development include:
Effects may be subtle epigenetic changes transmitted via the germline to future generations (transgenerational epigenetic inheritance). They might not be detectable without sensitive molecular approaches and/or apparent without a challenge or “second hit” later in life.
There is a latency between exposure and onset of disease, which may last from months to years to decades.
Since the disease susceptibility is likely due to epigenetic changes, the effects may not be reversible with current technologies.
It may be possible to measure epigenetic changes due to obesogen exposures at birth, but some changes will not become apparent until later in life.
Obesogen effects will often be sex specific.
Obesogen exposure can interact with genetics, nutrition, and other environmental stressors to alter disease incidence, susceptibility, or severity.
Pre-conception, pregnancy and early childhood are the most sensitive times for obesogens to affect tissue development leading to obesity later in life. However, obesogen exposure in adulthood can also cause changes leading to increased susceptibility to obesity. Indeed, exposures during adulthood can also interact with nutritional changes and other environmental factors to exacerbate susceptibility to obesity due to developmental exposures. There is scant evidence showing that the effects of obesogen exposure in adulthood can persist throughout life. In contrast, developmental exposures can elicit changes that persist over the lifespan and across generations.
2. Mechanisms underlying obesogen actions
Establishing a causal link between chemical exposure(s) and obesity requires the identification of its mechanism of action. Numerous studies have attempted to delineate these mechanisms and have identified general principles discussed below. They can be grouped into several classes representing different stages in the mechanisms of action. 1) Long-term mechanisms including epigenetic pathways accounting for intergenerational and transgenerational effects. 2) Proximal mechanisms which focus primarily on receptor targets. 3) Intermediate events such as inflammation, oxidative stress or specific intermediate proteins that link receptor regulation to longer-term effects. 4) Organ-dependent mechanisms highlight specific contributions of different critical organs and tissues such as the liver, fat, and the nervous system.
2.1. Epigenetic mechanisms
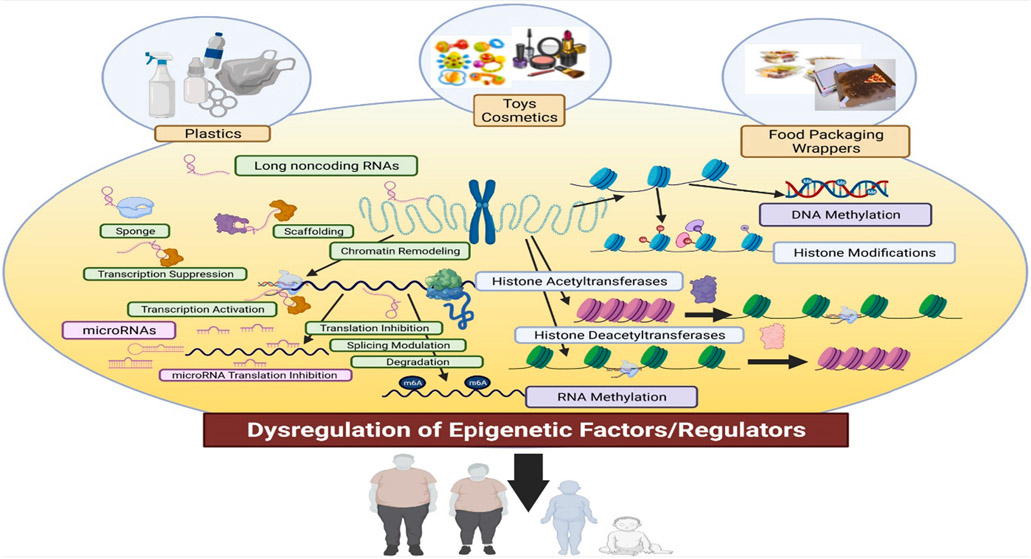
Epigenetics studies the heritable and persistent mechanisms that control gene expression changes without changing the DNA sequence. Five main types of these mechanisms are currently understood. One involves the DNA itself, e.g., DNA methylation; another requires interaction with the histone proteins around which the DNA is wound, e.g., histone methylation, a third involves non-coding RNAs (ncRNAs), a fourth involves modification of the RNA (e.g., RNA methylation) and a fifth involves higher-order chromatin structure[24-26] (Fig. 2). DNA methylation and histone modifications will be further discussed in the transgenerational mechanisms section. These changes influence the body’s epigenome, varying across multiple cell types and undergoing very specific, synchronized changes during a lifetime [27]. Early life environmental exposures can modify the epigenome and influence gene expression within current and future generations.
Fig. 2. Epigenetic regulation of obesity.
Chemicals shown are just representatives of all of the classes of chemicals that are obesogens, and that can act via alterations in epigenetic control of gene expression, especially when exposures occur during development when hormones and growth factors are controlling cell and tissue differentiation. The known epigenetic control systems are shown: DNA methylation, Histone modification, chromatin modeling, and a variety of noncoding RNAs.
Obesogens that act during development likely will modify epigenetic mechanisms as part of their mechanism of action. Different phthalates have been implicated in adipogenesis via alterations in epigenetic mechanisms, including effects of butyl benzyl phthalate (BBP) and diisobutyl phthalate (DiBP) [28,29]. Bisphenols, including bisphenol A, F and S, have promoted obesity via epigenetic mechanisms [30,31].
ncRNAs are transcribed from DNA but not translated into proteins. ncRNAs regulate gene expression at the transcriptional and post-transcriptional levels. They can comprise short ncRNAs (less than 30 nucleotides (nts)) and the long ncRNAs (greater than 200 nts). Micro-RNAs (miRNAs), short inhibitory RNAs (19–22 nts) and piwi-interacting RNAs (21-31nts) are considered short non-coding RNA [26]. ncRNAs regulate gene expression at the translational level, and recent evidence indicates their role in DNA methylation and histone modifications. ncRNAs have been linked with several diseases, including obesity [26,27,32,33]. Long ncRNAs (lncRNAs) play a significant regulatory role during development [34] and exhibit cell-type-specific expression [35,36].
Entries for disease-related lncRNAs in the lncRNA and Disease Database (lncRNADisease: https://www.cuilab.cn/lncrnadisease) have increased from 63 entries to over 2,900 experimentally verified entries in recent years [37]. Several lncRNAs are differentially expressed in fat or adipose tissues in obese individuals, and are associated with adipogenesis [38,39]. lncRNA RP11-20G13.3 was positively associated with leptin, high-sensitivity C-reactive protein (CRP), low-density lipoprotein (LDL) cholesterol, fasting insulin, waist-to-hip ratio, waist circumference, and BMI. Lower BMI, waist circumference, fasting insulin, and triglycerides were associated with higher expression levels of lncRNA GYG2P1 [40].
Although the link between obesity and ncRNAs is accepted, there is limited evidence for miRNA/lncRNA regulation of obesity. Tetrabromobisphenol A (TBBPA) induced miR-107 and miR-103, reduced Thy1 expression and promoted adipogenesis [41]. lncRNA, miRNA, and small nucleolar RNA were differentially expressed in human primary adipocytes exposed to low and high doses of bisphenols [30]. Finally, BBP exposure was linked to metabolic dysregulation and alterations in lncRNA H19 and its target miRNAs [29]. More data are required to substantiate these associations, and studies investigating the role of mi/lncRNA in mediating the impact of different EDCs on obesity are warranted.
2.2. Transgenerational inheritance of obesity
Transgenerational inheritance refers to the inheritance of a phenotype resulting from an environmental exposure to which the generation expressing the phenotype was not exposed [42]. Exposure of pregnant F0 female mammals during pregnancy to a chemical or environmental stressor (e.g., starvation) will directly affect the F1 generation, which were exposed in utero and the F2 generation, which were directly exposed as developing germ cells in the F1 embryos. The effects of direct exposures are termed multi- or intergenerational. The F3 generation was never exposed, and effects are considered transgenerational. Exposure of non-pregnant females or males directly affects only the F1 generation via the germ cells; thus, effects seen in F2 are transgenerational. Effects in nonmammalian vertebrates such as fish and invertebrates follow this pattern.
There is considerable experimental evidence supporting the transgenerational inheritance of obesity. Pregnant F0 mouse dams exposed to tributyltin (TBT) during pregnancy [43] or throughout pregnancy and lactation [44] produced descendants with increased WAT size with more and larger white adipocytes, particularly in males, through the F3 and F4 generations, respectively. Transgenerational effects of TBT were also apparent as altered metabolomic fingerprints in F3 and F4 males and females. Although females did not become obese, they had an altered metabolome indicating transgenerational effects [45]. This was accompanied by up-regulation of genes associated with lipid storage and transport, lipogenesis, and lipolysis, as well as fatty livers [43]. Studies with various chemicals have shown that the obese phenotype could be passed transgenerationally [46-49]. Rodents exposed to air pollution (fine particulate matter, PM2.5), dichlorodiphenyltrichloroethane (DDT), jet fuel (JP-8), BPA, di(2-ethylhexyl) phthalate (DEHP), and dibutyl phthalate (DBP) [31,46-48,50,51] exhibited an increased incidence of adult-onset obesity, together with numerous other pathologies. Starvation or stress of F0 C. elegans elicited altered metabolism on the F3 generation [52,53]. Multigenerational exposure to bisphenol S (BPS) in C.elegans promoted fat storage over four generations [54]. Long-term, high dose exposure of F0 Drosophila melanogaster to DEHP led to an increased bodyweight of the offspring [55]. Together, these studies indicated that obesogens exposure can lead to transgenerational inheritance of obesity.
Possible mechanisms that have been proposed for transgenerational inheritance in general and specifically for transgenerational inheritance of obesity include epigenetic mutations (epi-mutations) such as DNA methylation [42], the inheritance of histone methylation [56], histone retention [57,58], the transmission of small, non-coding RNAs (ncRNAs) in males [59] and altered higher-order chromatin structure [44]. Blocks of differentially methylated DNA denoted as iso-directional differentially methylated blocks (isoDMBs) were observed in F4 generation male mice after F0 TBT exposure. Regions, where the isoDMBs were undermethylated compared to controls, were enriched in metabolic genes such as leptin and less accessible than controls in F3 sperm and F4 sperm from the same animals [60]. Therefore, ancestral TBT exposure was proposed to result in heritable changes in higher-order chromatin structure, leading to increased expression of adipogenic and metabolic genes in WAT compared with controls [44,60]. Transgenerational reconstruction of altered higher-order chromatin structure offers an attractive unifying model for how disparate mechanisms such as DNA methylation, histone methylation, histone retention, and ncRNA expression might be coordinately regulated across the generations. However, more research is needed to delineate the mechanisms through which this occurs.
2.3. Receptor mechanisms
Obesogens have been shown to activate or antagonize the action of nuclear hormone receptors, which are ligand-modulated transcription factors that directly regulate the expression of genes involved in adipocyte differentiation, body weight, and metabolism.
2.3.1. Peroxisome proliferator-activated receptor gamma
The master regulator of adipogenesis is the peroxisome proliferator-activated receptor γ (PPARγ) [61]. There is strong evidence showing that activation of this receptor leads to obesity, the most striking examples being the thiazolidinedione drugs. A number of environmental substances that bind to this receptor display obesogenic effects. Plasticizers phthalates and BPA and its analogs, flame retardant chemicals, per and poly fluoroalkyl substances (PFAS) and TBT stimulate adipogenesis via the PPARγ pathway [45,62-65] covered in more detail below. The effects of obesogens mediated by PPARγ are not limited to adipose tissue. For example, TBT has been shown to promote hepatomegaly and liver triglyceride (TG) levels in zebrafish [66].
2.3.2. Retinoid X receptor
The retinoid X receptor (a.k.a., the 9-cis retinoic acid receptor, RXR) heterodimerizes with many nuclear receptors (NRs), including PPARγ, supporting a key role for RXR in adipogenesis [67]. Activation of RXR can promote both adipogenic differentiation and preadipocyte proliferation [68,69]. The obesogen TBT is a potent activator of RXR and a partial agonist for PPARγ leading to an increased number of adipocytes [70,71]. Adipocyte differentiation induced by RXR activation by TBT or other RXR activators (called rexinoids) appears to create functionally distinct adipocytes than those generated via PPAR [72-74] with decreased glucose uptake, adiponectin expression, and altered browning pathways. The activation of the RXR:PPARγ heterodimer by TBT, which has been proposed to be mediated primarily by RXR, leads to both lipid accumulation and induction of liver lipogenic genes of zebrafish [66].
2.3.3. Estrogens/estrogen receptors
Estrogens display complex effects on metabolism and obesity, depending partially on the timing of exposure. Estrogens act via ERα and ERβ nuclear receptors and membrane receptors [75]. Human adipose tissue contains both membrane and nuclear estrogen receptors [76]. They can impact metabolic health by inhibiting adipocyte lipogenesis and modulation of energy expenditure and food consumption via actions on the brain [77]. Estrogens promote preadipocyte proliferation and regulate adipocyte number [78,79], presumably mediated by insulin growth factor (IGF) 1 receptor (IGF1-R) and PPARγ [78]. During development, exposure to diethylstilbestrol (DES), a synthetic estrogen, is associated with an increased risk of obesity [80]. BPA and its analogs are obesogens that act at least partially via nuclear and membrane-associated estrogen receptors [81]. Indeed BPA inhibits adiponectin release from human adipose tissue explants and adipocytes at nanomolar concentrations, suggesting it acts via the membrane estrogen receptor [76].
2.3.4. Androgens/androgen receptor
Androgens play a key role in adipogenesis. They are considered anti-obesogenic [82,83] because decreased androgen action is associated with increased adiposity. A non-steroidal anti-androgen, flutamide promoted triglyceride accumulation in 3T3-L1 preadipocytes [69].
2.3.5. Glucocorticoid receptor
The glucocorticoid receptor (GR) has a role in lipid metabolism and adipocyte formation [84]. The GR agonist, dexamethasone, promotes triglyceride accumulation and pre-adipocyte proliferation in mesenchymal and pre-adipocyte models [69,85], while GR antagonists inhibit adipogenesis [86]. The fungicide tolylfluanid is an obesogen that functions via GR activation [87].
2.3.6. Thyroid receptors
The thyroid receptor (TR) is essential for maintaining lipid and carbohydrate metabolism, blood pressure, and body mass [88-90]. TR regulates basal metabolic rate and thermogenesis in brown adipose tissue (BAT) [91]. Receptor isoforms (α, β1, β2) play distinct roles with TRα primarily regulating thermogenesis, while TRβ primarily regulates cholesterol metabolism and lipogenesis [89]. TRβ also governs genes essential for pre-adipocyte proliferation and differentiation [89]. Bisphenols and PFAS are obesogens that can act via the TR in larval zebrafish [81].
2.3.7. Constitutive androstane receptor and pregnane X receptor
The constitutive androstane receptor (CAR) and pregnane X receptor (PXR) are related liver-enriched receptors that regulate xenobiotic metabolism as well as glucose and energy homeostasis, immune function, and lipid metabolism [92,93]. PXR acts by regulating PPARγ expression [93], while PPARα activation induces CAR expression [94]. Polychlorinated biphenyls (PCBs) act indirectly via CAR/PXR [95], as do some pesticides [96].
2.3.8. Farnesoid X receptor
The farnesoid X receptor (FXR, also known as the bile acid receptor) regulates bile acid synthesis and other bile acid-associated receptors[97-99]. It is expressed in mature adipocytes and differentiated 3T3-L1 cells [100]. FXR agonists increase adipocyte differentiation and enhance insulin-associated signaling [100,101]. The obesogens perfluorooctanoic acid (PFOA) and perfluorooctanesulfonic acid (PFOS) induce the expression of genes normally regulated by FXR [102].
2.3.9. Aryl hydrocarbon receptor
The aryl hydrocarbon receptor (AhR) is a member of the basic-helix-loop-helix (bHLH)–PER-ARNT-SIM (PAS) superfamily of transcriptional regulators [103]. It transduces signals in response to environmental cues [103].
AhR signaling in the deregulation of metabolism is observed in diet- and obesogen-induced obesity. AhR inhibition can prevent and reverse obesity. Activation of AhR in mesenchymal stem cells (MSC) by benzo [a]pyrene (BaP) inhibited terminal adipocyte differentiation by down-regulating PPARγ signaling and reducing expression of adipogenic genes [104]. Antagonism of AhR by alpha-naphthoflavone abrogated the AhR-mediated inhibition of adipogenesis [104]. PCBs can act as AhR agonists. Overall, the in vitro effects of AhR ligands on adipogenesis do not appear to be consistent and depend on the cellular system; however, these ligands can induce inflammatory cytokines and metabolic disruption [105] in vivo.
2.3.10. Other signaling pathways
Obesogens and EDCs may also act by disrupting non-hormonal signals such as receptor kinase pathways downstream of growth factor signaling, neurotransmitter signaling, developmental signaling processes, a concept known as “signal toxicity” [106]. This area is currently unexplored for EDCs but could encompass other possible pathways for obesogen action.
2.4. Organ-specific effects
2.4.1. Adipocytes
All obesogens either directly or indirectly increase adipose cell number and/or size. As described above, strong evidence exists to connect each of ten nuclear receptors with changes in adipocytes. Current literature on adipocytes focuses on using murine 3T3-L1 lines and human origin adipocytes or MSCs to examine the mechanism of adipocyte production in vitro. Replication and expansion of these data and techniques to obesogens in vivo would provide further insight into how obesogens promote obesity at the adipocyte level.
2.4.2. Liver
The liver is the principal organ for intermediary and xenobiotic metabolism and detoxification. Industrial chemical exposures are associated with several liver lesions. The most common histologic form of liver pathology is fatty liver disease (FLD) [107-109]. NAFLD is the hepatic manifestation of obesity and metabolic syndrome. Mortality from cardiovascular disease (CVD) is the leading cause of death in NAFLD patients.
Toxicant-associated steatohepatitis (TASH) was coined to describe FLD associated with insulin resistance in non-obese subjects with high-level occupational vinyl chloride exposures [110]. TASH was associated with other environmental chemical exposures, including persistent organic pollutants (POPs), volatile organic compounds, particulate matter, metals, BPA, fungicides, glyphosate-based herbicides, and dinoseb [13,109,111,112]. Some exposures, such as 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD or dioxin) or high-dose vinyl chloride, are sufficient to cause hepatic steatosis. A urinary biomarker of vinyl chloride exposure was associated with increased pediatric NAFLD and adult liver fibrosis in residents living near a petrochemical complex in Taiwan [113,114]. Other exposures, such as ortho-substituted PCBs, compromise the liver exacerbating diet-induced FLD. Hepatic steatosis increases liver PCB levels, possibly increasing their hepatotoxicity [115]. Several prescription medications have also been implicated in the development of FLD [116].
In epidemiology studies and animal models, PCBs were associated with FLD [109]. PCBs were implicated in ligand-activation of hepatic xenobiotic receptors and intermediary metabolism (e.g., AhR, CAR or PXR) and appear to be competitive antagonists of the epidermal growth factor receptor (EGFR). The inhibition of phosphoprotein signaling downstream of the EGFR accounts for the indirect CAR activation associated with these compounds [95,117]. Epidermal growth factor (EGF) therapy improved hepatic inflammation and fibrosis in a mouse model of PCB-related steatohepatitis but paradoxically worsened hyperglycemia and dyslipidemia [118]. Further complicating matters, the induction of hepatic CAR, AhR, and PXR target genes by PCBs was recently shown to be partly dependent on the gut microbiome [119]. The increasingly complex mechanisms by which PCBs and TCDD exposures reprogram gene expression impacting NAFLD warrant further investigation.
PFAS were associated with NAFLD in human adults [120], pediatric populations [121,122], and a humanized PPARα mouse model. Developmental exposure to TBT was associated with increased liver steatosis and tumors in male, but not female, mice [123]. In vitro TBT exposures increased liver lipids in the human hepatic cell line, HepaRG [124]. Plasticizers BPA, BPS and DEHP have been associated with NAFLD in zebrafish models [125-127].
T2D is a primary clinical driver of NAFLD disease severity. Obesogens that worsen insulin resistance may increase NAFLD severity through this mechanism. However, the liver itself is an endocrine organ that releases hepatokines impacting hunger, systemic metabolism, and obesity-associated diseases. Recent experimental studies demonstrated associations between PCB or triclosan exposures and hepatokines (e.g., Fgf21, Igf1 and betatrophin) in FLD model systems [128,129]. Thus, NAFLD may be both an effect and a cause of the systemic endocrine disruption associated with environmental chemical exposures.
2.4.3. Skeletal muscle
Skeletal muscle plays a critical role in developing metabolic diseases, including obesity, since it consumes most of the glucose in the body and is an insulin-target organ. Therefore, any chronic disturbances in muscle cells may contribute to insulin resistance and subsequent obesity. Obesogens can affect glucose utilization in skeletal muscle. BPA alters insulin signal transduction glucose homeostasis in muscle cells in mice [130,131], and TBT reduces the expression of the insulin receptor and GLUT4 in skeletal muscle in mice [132].
2.4.4. Other mechanisms
In addition to activating receptors in adipose tissue, skeletal muscle and liver, obesogens can disrupt the function of other tissues and pathways which are not directly activated by specific hormone receptors but can lead to obesity.
2.4.5. Gut microbiome
The gut microbiota composition can be targeted by obesogens [133,134]. These include heavy metals, nanoparticles and numerous known obesogens: BPA (and to some extent other bisphenols), natural estrogens, phthalates, individual PCB congeners and their mixtures, polycyclic aromatic hydrocarbons (PAHs), PFAS, brominated flame retardants, pesticides, polychlorinated dibenzo-p-dioxins and dibenzofurans (PCDD/Fs) [133,134] and air pollution. These effects can be exacerbated when combined with excess nutrients, such as in a high-fat (Western) diet. Environmental chemical action on gut microbiota composition and the resulting dysbiosis might profoundly affect host metabolism, thus contributing to metabolic disruption to the onset of multiple metabolic diseases [133-135]. It was recently found that delta-valerobetaine derived from the microbiome is a diet-dependent obesogen correlated with VAT mass in humans. Delta-valerobetaine inhibited mitochondrial fatty acid oxidation [136]. Furthermore, alterations in the microbiome may alter the bioavailability of obesogens, although this requires a formal investigation.
2.4.6. Circadian rhythms
Environmental pollutants target regulators (e.g., REV-Erβ or PPAR) involved in the transcriptional-translational feedback loop that forms the circadian clock mechanism [137-139]. Exposure to these xenobiotics can lead to metabolic pathologies like obesity or NAFLD. TCDD was shown to disrupt circadian rhythmicity through AhR-dependent repression of hepatic clock regulators in mice, resulting in altered hepatic carbohydrate metabolism [137,140]. Tolylfluanid (TF) exposure to adult mice led to increased fat mass and body weight and altered circadian rhythms [141]. BPA can also disrupt circadian rhythms [142-145].
Further research is needed to explore the EDC and obesogen-related circadian clock disturbances and their potential role in intergenerational obesity. More recently, parental exposure of the medaka fish Oryzias melastigma to BaP [146] disrupted circadian rhythms, which were transferred across generations.
2.4.7. Inflammation
Numerous environmental chemicals disrupt innate immunity and promote inflammation, including PCBs, bisphenols, phthalates, flame retardants, herbicides, and fungicides [147-149]. Their effects on inflammation have been documented in vitro and in vivo. Their actions can also affect inflammatory reactions indirectly via alterations of the gut microbiome and/or disruption of the intestinal barrier [147,150,151]. The immune-disrupting effects of pollutants may disrupt innate immune system balance, which contributes to chronic inflammation both systemically and within individual organs involved in controlling energy metabolism.
2.4.8. Mitochondrial/Oxidative stress
Oxidative stress was proposed to contribute to obesity and obesity-related metabolic disorders [152]. WAT can contribute to proinflammatory states and oxidative stress depending on its location. Excess WAT can increase the concentration of free fatty acids (FFAs) in serum, leading to dysregulation of glucose metabolism and accumulation of energy substrates like glucose and fatty acid (FA). WAT accumulation in the liver and muscles can trigger mitochondrial and peroxisomal oxidation, increasing reactive oxygen species (ROS) [152]. Mitochondria are a primary site of producing reactive species through the electron transport chain (ETC) due to their essential role in the oxidative phosphorylation pathway of ATP synthesis [153]. The physiological production of mitochondrial ROS (mtROS) is counterbalanced by anti-oxidant enzymes, including catalase and glutathione peroxidase [153]. This balance can be altered under pathological situations or exposure to environmental toxicants, leading to increased mtROS production [154,155]. Steatotic HepaRG human hepatocytes exposed to a mixture of BaP/ethanol at low doses show increased mtROS production and decreased complex I, II and IV activity likely via AhR activation [156]. Obesogens such as arsenic, atrazine, BPA, BBP, cadmium (Cd), chlorpyrifos, DEHP, PFOA, PFOS, TCDD and TBT were reported to target mitochondria resulting in altered mitochondrial bioenergetics, mass and excessive ROS production, causing cell death and insulin resistance [155]. Changes in mitochondrial epigenetics (e.g., mtDNA methylation) could be important in inducing mitochondrial dysfunction and related oxidative stress [157].
2.4.9. Sirtuins
Sirtuins (SIRTs) are a conserved family of proteins present in most species that function as energy sensors and transcriptional effectors by controlling histone acetylation [158,159]. SIRTs constitute a major biological link between energy status and epigenetic regulation. SIRTs are expressed in tissues involved in metabolic regulation, such as the liver, skeletal muscle and adipose tissue. SIRT1 is a critical physiological regulator mediating metabolism, oxidative stress, and apoptosis [160]. SIRT3 functions in the mitochondria to regulate energy metabolism and insulin secretion [161,162]. SIRT1 and SIRT2 stimulate lipolysis in WAT during fasting. SIRT3 stimulates thermogenesis in brown adipose tissue [162]. Hepatic SIRT1 and SIRT3 activity are decreased in animal models fed a high-fat diet (HFD) for extended periods that develop FLD [158,163]. BBP lowered SIRT1 and SIRT3 and elicited protein hyperacetylation in cell adipogenesis and fatty liver models in vitro [164,165]. Mitochondrial biogenesis regulators PGC-1α, NRF-1, and NRF-2, were also decreased in both models. Thus, obesogens can increase adipogenesis and metabolic dysregulation by altering critical epigenetic regulators like SIRTs.
2.5. Feeding behavior and food addiction
Several studies demonstrated that developmental exposures to obesogens, particularly BPA, influenced the dopaminergic reward system and the impulsivity network of the cortex [166]. BPA exposure in children was associated with hyperactivity and attention deficit hyperactivity disorder (ADHD) [167], which involves the same neurological circuits. Still, this study did not consider binge eating and/or food addiction. A recent cross-sectional study of obese patients found that serum concentrations of bisphenol A bis(2,3-dihydroxy propyl) ether (BADGE.2H20) were positively associated with the incidence of binge eating disorder [168]. Because brain regions associated with the dopaminergic reward system express obesogen targets [169-171], future studies on the relationship between obesogen exposure, binge eating disorders, and food addiction in animal models would be valuable.
3. Evidence supporting the obesogen concept
About 50 chemicals and classes of chemicals are classified as obesogens. See recent reviews [12,15,17,172], including a systematic review and meta-analysis [173] and an assessment of obesogens among the youth of Latino or Hispanic origin in the United States and Latin America [174]. This section describes obesogens with the most experimental support and robust evidence for effects on obesity. The chemicals detailed below have in vitro, animal dose–response, and mechanistic data, together with supporting human data. Experiments in animal models can show cause and effect, linking a chemical to increased adipogenesis and obesity. Table 1 integrates the evidence for obesogens. In assessing the weight of evidence for a chemical being an obesogen, we considered the following factors:
Table 1.
This table summarizes the main findings of the in vitro (in stem cells, adipocytes, or hepatocytes), in vivo (in rodents or zebrafish), and epidemiological studies (including meta-analyses) discussed in the text relating to adiposity, lipids, or fatty liver. Reviews are not included unless they are meta-analyses, and birthweight results are not included.
| In vitro | In vivo | Epidemiological | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adipocytes, stem cells | Hepatic cells | Rodents or zebrafish | Humans | |||||||
| Differentiation, proliferation, adipogenesis, dysfunction |
Fatty liver, lipids |
Adiposity, adipocyte dysfunction | Dys-lipidemia | Fatty liver | Neurological, food, energy, microbiome |
Adiposity | Dys-lipidemia | Fatty liver | Neurological, food, energy, microbiome |
|
| OBESOGENS | ||||||||||
| Maternal or paternal smoking, nicotine | ↑D[195,197-200] | ↑D[201] | ↑D[201] | ↑D[193,197,198] | ↑D[191,203,205-209,214] ↑C[208] |
↑D[194,203] | ||||
| BPA | ↑[30,44,76,87,222,225,226,229,459,699] ↓[267] |
↑[223,224] | ↑D[44,238,239,241,245,706,735] ↑D,T[31,48,51] ↑A[125,235,246] ↓A[696] |
↑D[238,706] ↑A[232,694,696,703] |
↑D[125] ↑A[125,230-232,235,702] |
↑D[239,243-245,677] ↔D[241]↑A[736] |
↑D[251,252,254] ↓D[257] ↔D[208,255,256,295]↑C[255,257] ↔C[208,252] ↑A[248-250,737] |
↔D[254] | ||
| BPS | ↑[30,226,699] | ↔[224] | ↑D[233] ↑D + A[247] |
↑D[233] ↑D + A[247] |
↑D[126] | ↔ D + A[247] | ↑ | |||
|
Air pollution: particulate matter, traffic,
ozone |
↑D[316,328] ↑D,T[50] ↑A [306,309,310,321,323,325,335] ↑P[328] |
↑D[328] ↑A{[318,321,336] |
↑D[317] ↑A[319,320,329,330,336] |
↑A[335] | ↑D[342,344] ↔D[208,342,350] ↑C[208,338,340,345,348] ↔C[352] ↑A[354,356,357] ↑↓A[355] |
↔C[352] ↑A[346,347,353,356,717] |
↑C[311,332] | |||
| Air pollution: B [a] P, PAHs, diesel exhaust | ↑[313] | ↑[156,190,315] | ↑D[314,322]↑A[313] | ↑A[315] | ↑D[156,314,322] ↑A[315] |
↑D[339,343] | ||||
| Phthalates | ↑[28,87,164,267-271,274,286,459] ↔[265] ↓[266] |
↑[124,280,281] | ↑D[265,283,284,286,287 ]↑D,T[48] ↑A[263,268,269,284,285] |
↑D[286] | ↑D[278] ↑A[279]; |
↑A[275,276,284] | ↑D[289,291,293,295] ↓D[253,255,290,296,299] ↑↓D[292,297] ↔D[208] ↑C[299] ↓C[255] ↔C[208,272] ↑A[249,737] ↑↓A[272] ↔P[738] |
↑D[291] | ||
| PBDEs | ↑[407] | ↑D[412] | ↔D[208] ↓C[208] ↑↓A[478] |
|||||||
| OPFRs (e.g., triphenyl phosphate) | ↑D[142] ↔D[376] |
↑↓D[445] ↑P[445] |
↑D[445] | |||||||
| DDT/DDE | ↑[452,454-458] | ↑D[460] ↑D,T[46,49] |
↑D[460] | ↑D[253,461,475-477,479-483,491,492,739] ↑D,T[484] ↔D[208,485,486,490,493] ↓C[208] ↔C[463] ↑A[463,464,466-468,473,474,478] ↔ A[469] ↓P[554] |
↔D[482] ↑A[474] |
|||||
| PFAS | ↑[65,523 524] | ↑[102,525]↑↓ [124] |
↑D[526,534] ↔A[534] ↓A[533] |
↑D[527] ↑A[528,530-532] |
↓A[533] | ↑D[487,488,490,558-560] ↔D[208,487,562,563] ↑C[541,546] ↓C[490,540] ↔C[208] ↑A[535,536,544,545] ↑P[551-555] |
↑C[541-543] ↑A[537,538,557] |
↑D[122] ↑C[121] ↑A [120,541] |
||
| PCBs | ↑[105,452,459] ↑↓[501] |
↑A[501] | ↑A[501] | ↑A[95,118,129,149,686] | ↑A[119] | ↑D[253,476,488,491] ↓D[481] ↔D[208,480,482,485,490,492,739] ↑↓C[463] ↓C[208,490] ↑A[464,474] ↓A[471] ↑↓A[463,467,468,473] ↔A[469,478] |
↑D[739] ↔D[482] ↑C[489] ↑A[464,474] |
|||
| TBT | ↑[70,73,74,267,368-371,382,384,407] | ↑[124,372] | ↑D[123,142,376,382] ↑D,T[43,44] ↔A[387] |
↑D[382] | ↑D[66,123,382] ↑D,T[43] ↑A[385,386] |
↑A[383,386,387] | ↑D[388] | |||
|
Non-nutritive
Sweeteners |
↑[570,573] | ↑D[570,578] ↑A[571,577] |
↑D[578] ↑A [572] |
↑D[570] | ↑A[576] ↔A[575] |
|||||
| Glyphosate | ↓ | ↑D,T[653] | ||||||||
| Chlorpyrifos | ↑[580] | ↑D[583,589] ↑D + A[584] ↑A[581,582,585] |
↑A[588] | ↑D[583] ↑D + A[584] ↑A[582,585,587] |
||||||
| Neonicotinoid pesticides | ↑[590,592] | ↑A[591,592] | ||||||||
| Permethrin | ↑[594,596] | ↑A[594] | ↑A[594] | |||||||
| Parabens | ↑[459,614,615] | ↑D[616] | ↑D[616] | ↑D[616,740] | ||||||
| Tween-80 | ↑A[618] | ↑A[618] | ||||||||
| CMC | ↑A[618] | ↑A[618] | ||||||||
| 3-BHA | ↑[620] | ↑A[619] | ||||||||
| MSG | ↓[621] | ↑A[622] | ||||||||
| Tolyfluanid | ↑[87] | ↑A[141] ↑↓A[599] |
||||||||
| DOSS | ↑[626] | ↑D[627] | ||||||||
| Cadmium | ↓[634] | ↑D[188,632] | ↑D[632] ↑A[189] |
↑D[632] ↑A[189] |
↑D[188] ↓D[480] ↓C[463] ↓A[463,636] ↔A[635] |
|||||
| Arsenic | ↓, [638,639] | ↑D[640,641] ↓A[642] |
↓A[642] | ↔A[642] | ↔D,C[208] | |||||
| DBTs | ↑[371,364] | ↑D[364] | ↔D[388] | |||||||
| Fructose, HFCS | ↑A[703] | ↑A[703] | ↑C[610] | ↑C[610] | ||||||
| βHCH | ↑D[253] ↔D[485,492] ↑A[464,471,478] |
|||||||||
| HCB | ↑D[253,482,490,739] ↔D[208,480,485,491,492] ↓C[208,463,490] ↑A[464,467,468] ↑↓A[463] ↔A[469,478] |
↔D[482] ↑A[464,474] |
||||||||
| Triflumizole | ↑[670] | ↑D[670] | ||||||||
| Atrazine | ↑A[676] | |||||||||
| POP mixtures | ↑A[453] | ↑A[723] | ||||||||
| Mixtures, misc. | ↑D,T[48] | |||||||||
| TBBPA, TCBPA | ↑[41,228] | ↑D[142,234] ↑A[235] |
↑A[235] | |||||||
| TCDD, TCDF, dioxin | ↑↓[501] ↑[105] |
↑A[502] | ↑[137] | ↔D[480] ↑A[463,473] |
||||||
| Oil, gas, hydrocarbons, petrochemicals | ↑[646,647] | ↑D[649] ↑D,T[47] |
↑↓D[649]} | ↑C[113] A[114] |
||||||
| POTENTIAL OBESOGENS | ||||||||||
| Triclosan | ↑A[125] | ↑D,A[125] ↑A[128] |
||||||||
| BPAF | ↑[227] | |||||||||
| PF | ↑[30,226,699] | |||||||||
| Diazinon | ↑[655] | |||||||||
|
Alkylphenols, alcohols, and
their ethoxylates |
↑[660,662] | ↑[662] | ||||||||
| BADGE | [664] | |||||||||
| BPA-Glucuronide | ↑[665] | |||||||||
|
Strobilurin
pesticides |
↑[656], | |||||||||
| Endrin | ↑[87] | |||||||||
| DBP | ↑[656] | ↑A[288] | ↑A[288] | |||||||
| DiBP | ↑[656] | ↑C[294] | ||||||||
A = adult exposure; C = childhood/adolescent exposure; D = developmental/early life exposure; D + A = developmental plus adult exposure; P = exposure during pregnancy; T = transgenerational effects. ↑ positive or increased effect/association, or increased obesogenic effect linked to the exposure.
↓ negative or inverse effect/association, or decreased obesogenic effect linked to the exposure.
↔ no effect or statistically significant association.
Multiple arrows show various effects/associations.
Abbreviations: 3-BHA = 3-tert-butyl-4-hydroxyanisole; B[a]P = benzo [a] pyrene; BADGE = bisphenol A diglycidyl ether; BHA =; BPA = bisphenol A; BPAF = bisphenol AF; BPF = bisphenol F; BPS = bisphenol S; CMC = carboxymethylcellulose; DBT = dibutyltin; DDT = dichlorodiphenyltrichloroethane; DDE = dichlorodiphenyldichloroethylene; DES = diethylstilbestrol; DOSS = dicotyl sodium sulfoscuccinate; HCB = hexachlorobenzene; HCH = hexachlorocyclohexane; HFCS = high fructose corn syrup; MSG = monosodium glutamate; OPFR = organophosphate flame retardants; PAH = polyaromatic hydrocarbon; PBDE = polybrominated diphenyl ether; PCB = polychlorinated biphenyl; PFAS = per- and poly-fluorinated alkyl substances; POP = persistent organic pollutant; TBBPA = tetrabromobisphenol A; TBT = Tributyltin; TCBPA = tetrachlorobisphenol A; TCDD = 2,3,7,8-tetrachlorodibenzo-p-dioxin; TCDF = 2,3,7,8-tetrachlorodibenzofuran, DBP-dibutylphthalate, DiBP-diisobutyl phthalate.
Positive studies were given more weight than negative studies.
Studies confirmed on repetition were given more weight than single studies.
It is expected that not all animal studies will agree due to different timing and routes of exposure, range of doses tested, the timing and sensitivity of endpoints assessed, and the genetic background of the model. Similarly, epidemiology studies are not all expected to agree due to differences in exposures, exposure assessments, demographics and endpoints evaluated.
Animal model studies can prove cause and effect.
Unless there are data to the contrary, it is assumed that animal data will extrapolate to humans.
Developmental exposure to obesogens will likely be more impactful than adult exposures.
It is expected that the effects of obesogens will be sexually dimorphic.
There may be non-monotonic dose responses, which should be considered physiologically and endocrinologically plausible.
For non-persistent obesogens, it is difficult to accurately assess actual exposures in human epidemiology studies unless there are multiple measurements across the assessment period. Single measures may lead to erroneous results. Multiple other confounders make it more complicated to assess the impacts of epidemiology studies.
Longitudinal birth cohort studies are more sensitive and likely to find an association between exposure and obesity than cross-sectional studies.
4. The most relevant obesogens
This section discusses the most relevant obesogens and the evidence supporting their impact on obesity. Such evidence includes data linking obesogen exposure to the formation of adipocytes in vitro and weight gain in animal and human studies.
4.1. Pharmaceuticals
It is well-known that some drugs have the side effect of causing weight gain. These data provide strong proof-of-concept for the obesogen hypothesis and establish causal links between chemical exposure and weight gain. Most examples of drug-induced obesity derive from adult rather than developmental exposure.
Antidepressants are used in the management of moderate to severe depression. Long-term use of antidepressants was associated with increased abdominal adiposity and weight gain [175,176]. It remains unclear whether these effects are secondary to the hypercortisolemia of stress and depression. These effects also appear drug-specific [177]. The selective serotonin reuptake inhibitors (SSRIs), sertraline and escitalopram, were associated with weight gain/increased body mass, whereas fluoxetine use was associated with weight loss [177]. The tricyclic antidepressant amitriptyline and the serotonin-receptor antagonist Trazadone were associated with weight gain [178]. Second-generation or “atypical” antipsychotic drugs often used in severe depression are also associated with weight gain, leading to metabolic syndrome or T2D [179,180]. The mechanisms by which antidepressants can alter weight have not been fully elucidated; however, SSRI exposure was shown to cause abnormal hepatic lipid homeostasis [181] and dysregulated glucose and lipid metabolism in adipose tissue [182].
Some anti-diabetic drugs, including thiazolidinediones like rosiglitazone (ROSI), pioglitazone, and sulfonylureas, can also lead to weight gain [183]. ROSI likely stimulates weight gain because of its action as a PPARγ agonist: activation of the PPARγ pathway results in the differentiation of precursors into adipocytes[61]. Beta-blockers used to control blood pressure [184] and corticosteroids used to treat inflammation can also cause weight gain [185].
DES is an estrogenic drug used to prevent miscarriages from the 1940s through the 1970s. In a mouse model, perinatal exposure to low but not high doses of DES resulted in obesity in the female-specific offspring as adults. Increased weight gain and visceral WAT began at puberty, and by adulthood, the mice weighed about three times the weight of controls [186]. Prenatal exposure to DES in humans resulted in a slight increase in adult obesity in the offspring [80].
4.2. Smoking/Nicotine
Global tobacco use is the second leading cause of disease; more than 30 diseases and conditions are caused by smoking, including obesity in smokers and those exposed to tobacco smoke [187]. Cigarettes contain nicotine, and it is this chemical that leads to dependence. Nicotine binds to receptors, including dopamine, leading to positive stimulation and smoking reinforcement. Nicotine, Cd, and BaP are among the chemicals in smoke that have been linked with obesity. The extensive data linking maternal smoking to obesity in the offspring provides strong proof of principle that an environmental chemical can be an obesogen.
4.2.1. Zebrafish studies
Developmental exposure to Cd increases lipid deposition in juvenile zebrafish [188]. Embryo and adult zebrafish exposed to Cd for four weeks showed severe hyperlipidemia and fatty liver changes, showing that Cd promotes increased adiposity and development of fatty liver [189]. Zebrafish larvae fed a HFD to induce obesity, then co-exposed to BaP and ethanol developed steatohepatitis. Therefore, HFD-induced obesity acted as a first hit to sensitize the system, and BaP/ethanol exposure provided a second hit that promoted the development of steatohepatitis and inflammation [190].
4.2.2. Rodent studies
Cigarette smoke contains more than 7000 chemicals, but most animal studies have focused on the effects of nicotine exposure to understand how fetal exposure to cigarette smoke can increase adiposity and obesity risk [191]. Mechanisms underlying how early-life exposure to nicotine or cigarette smoke elicits obesity in animals are varied and include increased energy intake, reduced energy expenditure, and effects on adipose tissue development and function. Nicotine increases oxidative stress, hepatocellular apoptosis, and hepatic lipogenesis, exacerbating hepatic steatosis triggered by HFD in rats [192]. Early-life exposure to cigarette smoke resulted in hyperphagia and an increased preference for a HFD in rats [193]. These results parallel those reported in humans following prenatal exposure to cigarette smoke [194]. Nicotine-altered hypothalamic neuropeptides are important for appetite control in animal studies [195-197] and may function similarly in humans. Early-life exposure to nicotine also affected energy expenditure [198], perhaps by “whitening” of BAT that reduced BAT activity [195,199,200]. Prenatal nicotine exposure also led to elevated expression of adipogenic markers in WAT and increased storage of lipids in both WAT and peripheral tissues in rats [191,198,199,201]. This effect is central to developing obesity and insulin resistance [202].
4.2.3. Human studies
Epidemiological data strongly support a positive and probable causal association between maternal smoking and increased risk of obesity or overweight in offspring. Increased body fat and fat mass have also been reported in children born to women who smoke [203-205]. A meta-analysis based on 39 studies of 236,687 children reported an increased risk of obesity in children born to mothers who smoked during pregnancy (pooled OR 1.55) [206]. Analysis of over 200,000 singleton births from 28 birth cohorts reported an increased risk of childhood overweight (OR 1.42). This effect was not altered by reducing the number of cigarettes smoked during pregnancy [207].
When 77 different prenatal exposures, including indoor and outdoor air pollutants, built environment, green spaces, tobacco smoking, and biomarkers of chemical pollutants were examined in the Human Early Life Exposome study (HELIX) (N = 1,301 mother–child pairs from 6 longitudinal birth cohorts in Europe), maternal smoking was the only factor associated with higher child BMI [208]. Another study correlated epidemiological data to results obtained in the zebrafish larval model in which Cd exposure increased adiposity, demonstrating that Cd can act as an obesogen [188]. These data supported the observations that maternal smoking during pregnancy is a risk factor for obesity in offspring. A recent study quantitated the dose–response between smoking and obesity and found a linear relationship between maternal smoking (1–15 cigarettes per day with no further increase after 15 cigarettes) and offspring obesity with no sex differences observed [209].
4.2.4. Passive smoking/ secondhand smoke /environmental tobacco smoking
Less is known about the association between passive or secondhand exposure to tobacco smoke and obesity. A recent meta-analysis of eleven studies evaluated potential associations between secondhand smoke (SHS) and the risk of increased BMI and waist circumference [210]. SHS was associated with a higher BMI overall (0.58 kg/m2). There was a stronger association between SHS and BMI in adults (1.31 kg/m2) than in children (0.47 kg/m2) or teenagers (0.54 kg/m2). No significant associations were shown in the elderly. Some evidence links paternal smoking with childhood overweight (OR 1.21) [207], but this association is less consistent across studies [211]. A systematic review revealed that SHS exposure during pregnancy was associated with higher BMI or overweight in children in 4 of 7 studies [212]. Contrasting results were observed between high and low GNI (gross national income per capita) countries, with SHS exposure associated with higher BMI in high GNI countries and lower BMI in low GNI countries.
4.2.5. Integration and summary of evidence
Active smoking during pregnancy provides robust evidence for obesogens and the obesogen hypothesis. Population attributable risk of obesity from maternal smoking was estimated at 5.5% in the US and up to 10% in areas with higher smoking rates [213]. Therefore, avoiding smoking during pregnancy has substantial benefits in preventing offspring obesity and reducing other harmful effects on mothers and children. Exposure to SHS during pregnancy increases the risk of overweight in the offspring, although the effect is smaller and less consistent [214].
4.3. Bisphenol A and analogs
BPA is widely used in plastics and epoxy resins. Free BPA is also an additive (plasticizer) in a wide variety of plastics (e.g., polyvinyl chloride (PVC)), in other products for everyday use, in many food contact materials and as a developer coating the surface of thermal papers from which it is readily released [215]. BPA is among the highest production-volume chemicals detected in ecosystems, human fluids, and tissues. BPA has received increased public attention due to its harmful effects on development, reproduction, metabolism, cardiovascular, and immune systems. BPA was classified as a substance of very high concern, and its use is prohibited or restricted in some products, but such restrictions differ considerably within and between countries.
Twenty-four BPA analogs exist, including BPS, bisphenol F (BPF), bisphenol B (BPB), bisphenol E (BPE), and bisphenol AF (BPAF). Some of these are used as BPA replacements, but due to their structural and functional similarity to BPA, these are likely to have similar health impacts [216-218]. Tolerable Daily Intakes (TDI) for BPA have been elaborated (for example, the European Food Safety Authority fixed BPA TDI to 4 μg/kg bw/day). Modified guidance values derived from human biomonitoring data are under development for BPA in general and occupational populations [219-221].
4.3.1. In vitro studies
BPA, BPS, and BPF induce adipocyte differentiation. In vitro studies using the mouse 3T3-L1, preadipocytes showed that BPA treatment resulted in transient effects on methylation of the PPARγ promoter and lipid accumulation [222]. GR may also participate in BPA response in 3T3-L1 cells [87]. In vitro studies in human hepatic HepG2 cells showed that low concentrations of BPA promoted lipid accumulation in hepatic cells, mitochondrial dysfunction, alterations in lipid metabolism, and inflammation [223]. Unlike BPA, BPS did not induce metabolic abnormalities in hepatocyte cell lines [224]. The ability of bisphenols to bind to many NRs can explain the pro-adipogenic effects associated with BPA, BPF, BPS and BPAF in the murine 3T3-L1 cell line and human preadipocytes [225-228].
BPA also induced inflammatory responses, lipogenesis, and decreased adipocyte insulin sensitivity [225,229], indicating that it produces a dysfunctional adipocyte in vitro. The induction of proinflammatory cytokines such as TNFα and IL6 in adipocytes and reduced expression of the anti-inflammatory hormone adiponectin caused inflammation in cultured human adipocyte explants [76].
4.3.2. Zebrafish studies
Chronic exposure to BPA induced a dysregulation in lipid metabolism-related genes, leading to liver steatosis in juvenile zebrafish. BPA exposure induced NAFLD and promoted the progression of hepatic inflammation, leading to a more severe pathological stage of NAFLD [125]. In adult fish, chronic and acute BPA exposures, altered gene expression signatures associated with NAFLD, indicating lipid metabolism disturbance that could promote lipid accumulation in the liver, hence steatosis [230-232]. Similarly, long-term exposure to BPS increased fat accumulation in the liver, thereby favoring the risk of NAFLD onset and promoting simple steatosis to nonalcoholic steatohepatitis (NASH) via endoplasmic reticulum stress [126]. Exposure to environmentally-relevant doses of BPS and BPF caused adverse effects similar to BPA regarding metabolism disruption [216], including disruption of triglyceride metabolism [233].
Two halogenated-BPAs, TBBPA and tetrachlorobisphenol A (TCBPA), commonly used as flame retardants, elicited lipid accumulation in zebrafish larvae and late-onset weight gain in juvenile zebrafish by activating PPARγ [234]. Exposure to environmentally-relevant levels of BPA or TBBA in zebrafish led to hyperphagia and obesity in adult fish. Also, they activated the cannabinoid receptor CB1, which could be part of the mechanism leading to obesity [235]. Lastly, exposure to BPA, BPF or BPS in zebrafish confirmed the alterations of estrogen, androgen, and thyroid hormone disruption observed in vitro [81,236].
4.3.3. Rodent studies
Ingested BPA passes from the gut through the mesenteric vessels directly to the liver, where extensive first-pass phase II conjugation occurs, resulting in hydrophilic BPA conjugates (primarily BPA-glucuronide and BPA-sulfate) that are selectively excreted into the urine. Fetal and postnatal exposure to BPA permanently disrupted metabolic systems regulating body weight. After the fetal-neonatal period of organogenesis, BPA was shown to disrupt homeostatic systems required to maintain normal body weight, including long-term consequences for pregnant female mice exposed to BPA [237].
A systematic review and meta-analyses performed on 61 rodent (rats and mice) studies reported the obesogenic effects of BPA on fat or body weight, triglycerides, and free fatty acid [238]. Globally, a positive association was found between early-life exposures to BPA and WAT weight, triglyceride or FFA levels, and a negative association with body weight. These associations depended on the animal strain, sex, frequency, route, dose, and exposure window. Fetal exposure to low but not high doses of BPA caused increased body weight, food intake, the number of adipocytes and altered leptin, adiponectin, glucose and insulin regulation [239]. Developmental exposure of CD-1 mice to a low dose (25μg/kg/day) of BPA increased the body weight of both male and female offspring. The addition of BPA during the peri-pubertal period augmented prenatal exposure in females [240]. Prenatal exposure to a low dose of BPA increased adult body weight associated with a 3-fold increase in parametrial WAT and adipocyte hypertrophy in female Sprague-Dawley rats. They also exhibited increased expression of lipogenic genes: PPARγ, C/EBPα, lipoprotein lipase (LPL), sterol regulatory element-binding protein (SREBP-1C), fatty acid synthase (FAS), and stearoyl-CoA desaturase 1 (SCD-1) [241,242].
Developmental BPA exposure elicited weight gain from increased food intake in specific animal models by reducing the number of satiety neurons and increasing the number of appetite neurons in the brain [243]. Developmental BPA exposure via the maternal diet can also influence the hypothalamic melanocortin neurocircuitry that controls feeding behavior in CD-1 mice [244]. BPA-exposed mice were more insensitive to leptin’s effects on pro-opiomelanocortin (POMC) expression than controls. They exhibited a reduction in POMC innervation of the paraventricular nucleus (PVN), rescued by postnatal leptin administration in females. BPA-exposed males and females were resistant to the effects of leptin injection on body weight [244]. Prenatal exposure of rats to BPA impaired glucose tolerance, increased food intake, increased body weight and led to changes in hypothalamic signals controlling food intake [245].
BPA-induced inflammation may be an essential part of the underlying mechanism of BPA action. BPA exposure in adolescent C57BL/6J mice resulted in the release of proinflammatory cytokines, chronic lowgrade inflammation, and increased body weight and fat [147,246]. F1 and F2 offspring of female mice exposed to BPA from preconception until weaning had increased pancreatic inflammation, body weight, and body fat in adulthood [31].
BPS potentiates high-fat-induced obesity in mice [247], and BPF may be associated with a decreased bodyweight in rats, reviewed in [236]. The obesogenic effects of BPA analogs in animals need further investigation because these data are scarce compared to BPA.
4.3.4. Human studies
A meta-analysis [248] identified 15 cross-sectional BPA studies, 12 found a significant association between BPA levels and obesity in adults. One prospective study, conducted in women only, showed that elevated BPA levels were linked to an increased future weight gain [249]. A second prospective study detected associations between elevated BPA and future abdominal obesity in both sexes [250].
Prenatal BPA exposure was associated with increased central adiposity in girls between ages 2 to 6 in a large birth cohort study [251] and increased body fat at age 7 in girls [252], but not boys. Others did not find associations between prenatal exposure to BPA spot urine samples in the first and third trimester and increased BMI in children ages 7 in a birth cohort [253]. BPA concentration, measured with a single spot urine sample in the first trimester in a birth cohort study, was not related to adiposity in the offspring, but higher levels of BPA measured at four years were associated with child adiposity at that time [254]. Two smaller birth cohort studies using a spot urine sample for BPA showed no association with adiposity [255,256]. The epidemiological evidence for an obesogenic effect of BPA in birth cohort studies and childhood obesity is inconsistent, as another study found reduced BMI [257].
Several factors can explain these divergent data from epidemiological studies on BPA exposures. Most have assessed BPA exposure in urine or serum using a single measure of BPA that cannot reflect the multiple exposures and fluctuating levels of BPA resulting from its short half-life in humans (~6 h) [258]. BMI or body weight are imprecise measures of obesity, particularly in children. Prospective longitudinal studies using multiple BPA level evaluations and improved exposure assessments are required to better assess exposure to short-lived chemicals and improve coherence between human and experimental data [259].
4.3.5. Integration and summary of evidence
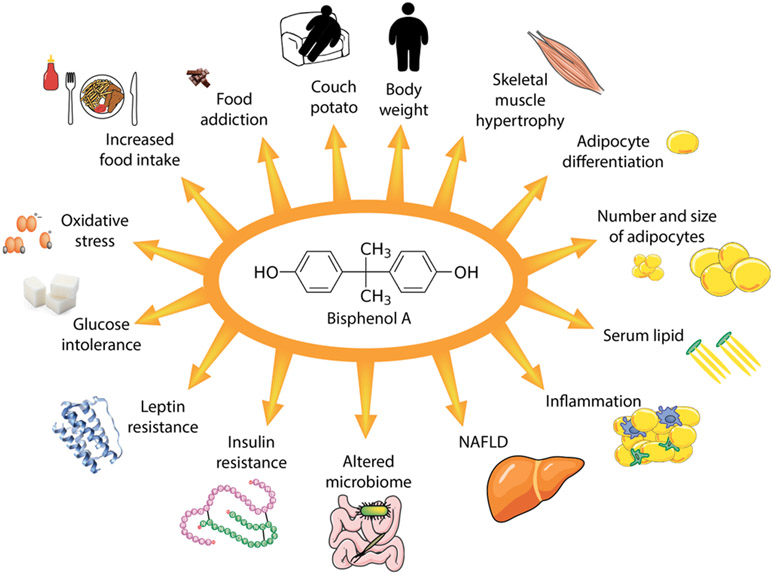
BPA stimulated the differentiation of adipocytes in vitro and increased food intake, body weight, and adipose tissue in vivo in multiple rodent studies. BPA also disrupted rodents’ immune function, gastrointestinal tract microbiome, liver, pancreatic β cell function, and the hypothalamic regulation of food intake (Fig. 3). Some birth cohort studies also indicated that BPA acts as an obesogen. However, the evidence is inconsistent. BPA studies have provided several important concepts and tools to the obesogen field: impact on metabolic tissues, regulation of appetite and satiety in the central nervous system (CNS), low dose and non-monotonic dose-responses, impact on epigenetic interaction with diets, the multiplicity of target receptors and mechanisms and potential relevance of computational studies. The overall integration of BPA data indicates it is an obesogen, and its use and regulation should consider these findings.
Fig. 3. BPA regulation of obesity.
BPA is an obesogen. The actions of BPA are the most detailed and comprehensive of all obesogens and this figure indicates the multiple sites and mechanisms whereby it was shown to act to stimulate weight gain from in vitro and animal model experiments.
4.4. Phthalates
Phthalates (diesters of phthalic acid) are a class of high-production volume chemicals that consist of 1,2-diester benzene rings where alkyl chains differ one from the next. About 25 phthalate esters are currently in use [260], and some metabolites are also active. High molecular weight (long-chain) phthalates include DEHP, diisononyl phthalate (DiNP), diisodecyl phthalate (DiDP), di-propylheptyl phthalates (DPHP), and di-n-octylphthalate (DOP). Long-chain phthalates are used as plasticizers in plastic consumer goods, PVC-based household products, packaging materials, and medical devices. Phthalate plasticizers are used to increase plastic durability, flexibility, longevity, and transparency. Phthalates are not bound to the background plastic matrix and can readily migrate into the environment. Short-chain phthalates are used as additives in personal care products and the production of varnishes and coatings. Common low molecular weight (short-chain) phthalates include dimethyl phthalate (DMP), diethyl phthalate (DEP), DBP, and DiBP.
Human exposures occur directly (oral and tropical) or indirectly (environmental) via air, food and water, air, dust, plastic products, cosmetics, and consumer products via inhalation, ingestion, or dermal contact. Phthalates are also found in plastics used in neonatal intensive care units [261]. Phthalates are metabolized and excreted via urine, sweat, and feces. Some phthalate metabolites are more active than the parent components. Epidemiological studies reported the detection of metabolites of phthalates in body fluids [262].
4.4.1. In vitro studies
BBP and DiBP are potent activators of adipocyte differentiation in the 3T3-L1 preadipocyte cell line, but only BBP activated PPARγ and induced adipogenesis in MSCs [28,164,263]). DEHP did not induce adipogenesis in 3T3-L1 cells in some studies [264,265] or the human cell culture model, SGBS [266], but did induce adipogenesis in the MSC-like cell line C3H10T1/2 [267]. DEHP exposure in 3T3-L1 cells was shown to enhance adipocyte proliferation, decrease lipid content, increase basal and insulin-stimulated glucose uptake while downregulating PPARγ expression, with increased PI3K signaling pathway [268]. These data indicate that DEHP exposure leads to a dysfunctional adipocyte with reduced lipids, reduced lipid droplet size, decreased adiponectin and insulin resistance, perhaps via activation of different pathways than the most common PPARγ pathway [268]. Like the actions of TBT, DEHP exposure in bone marrow MSCs increased adipogenesis at the expense of osteoblastogenesis [269]. One human DEHP metabolite, mono ethylhexyl phthalate (MEHP), activated PPARγ and stimulated adipogenesis in 3T3-L1 pre-adipocytes [270-273]. MEHP also induced early transcriptomic and metabolic alterations in human adipocytes differentiated in vitro, resulting in adipocyte differentiation and glyceroneogenesis [274]. Thus, differences in reported adipogenesis by DEHP could result from insufficient metabolizing capability in some cell lines.
BBP exposure may lead to metabolic dysregulation by altering epigenetic regulators such as lncRNA H19 and its target, miRNA-103/107. BBP induced adipogenesis in C3H10T1/2 cells via an epigenetic pathway [29]. BBP also acts through PPARγ to increase histone 3 lysine 9 acetylation while decreasing histone 3 lysine 9 dimethylation and tipping the epigenomic balance toward adipogenesis [28].
4.4.2. Zebrafish studies
Exposure to low doses of DEHP modulated the expression of liver genes related to fatty acid metabolism inducing NAFLD in zebrafish [127]. Long-term exposure to DEHP disrupted the gastrointestinal microbiome and expression of genes related to lipid metabolism, increasing fat storage in adult zebrafish [275,276]. Developmental exposure to MEHP disrupted pancreatic organogenesis in zebrafish that could lead to metabolic dysfunction [277]. DEHP has also been shown to induce the pathological progression of liver steatosis upon co-exposure with ethanol in zebrafish larvae induced to be steatotic by HFD [278]. In vitro and in vivo studies agree that DEHP exposure can promote hepatocyte lipid accumulation, disrupt redox prompting oxidative stress, and elicit de novo lipogenesis via SREBP1c activation [279-281]. Bis(2-ethylhexyl)-2,3,4,5-tetrabromophthalate (TBPH) and its metabolite, mono-(2-ethyhexyl)-tetrabromophthalate (TBMEHP) were shown to alter lipid metabolism of early larval stages of zebrafish via demethylation of PPARγ promotor DNA [282].
4.4.3. Rodent models
A systematic review examined 31 rodent studies that analyzed the effects of DEHP on obesity [283]. Study results differed, but developmental exposure of rodents to DEHP was significantly associated with increased fat weight. Exposure to DEHP for eight weeks in C3H/N mice caused increased food intake, body weight and visceral WAT in both sexes [284]. Similar results were reported in another C3H/N study after five weeks of exposure to DEHP. Increased expression of neuropeptide Y (NPY) and Agouti-related peptide (AgRP) and decreased POMC, critical genes involved in regulating food intake and body weight was proposed to explain increased food intake [285]. Treatment of 1296S, obesity-resistant mice with DEHP for ten weeks elicited weight and WAT gain in females, along with an increased expression of ERα in adipose tissue [268].
Developmental and lactational DEHP exposure in mice also increased weight in both sexes at weaning that continued to postnatal day (PND) 84 [284]. Experiments using the C57BL/6J strain showed weight gain only in males [286]. Long-Evans rat dams were exposed during pregnancy and lactation to a phthalate mixture (200 or 1000 μg/kg/day) that mimicked the urinary phthalate profiles of pregnant women in Champaign-Urbana, Illinois (35% DEP, 21% DEHP, 15% DBP, 15% DiNP, 8% DiBP, and 5% BBP), together with control or HFD [287]. HFD increased body weight and adipocyte size, and gene expression in females at 90 days of age. In males, HFD or 200 μg/kg/day of the phthalate mixture, but not both, increased body weight with no effect on adipocyte size. BBP exposure significantly increased the body weight of adult C57BL6 mice fed a HFD for 16 weeks due to increased liver and adipose tissue in both sexes [263]. Adult exposure to DBP for 13 weeks resulted in increased body weight gain and serum cholesterol in rats [288].
4.4.4. Human studies
Phthalates have short half-lives (~12–18 h) and do not accumulate in adipose tissue. A systematic review and meta-analysis examined 18 studies linking phthalate exposure to obesity [248]. Fifteen cross-sectional studies with ten studies in adult populations showed an overall relationship between phthalates and different measurements of obesity. A prospective study in adult women associated high phthalate levels with weight gain over the next ten years [249].
Several prospective birth cohort studies showed an association of maternal phthalate metabolites with weight gain. In utero exposures to monoethyl phthalate (MEP), BBP and the sum of DEHP monoester metabolites were associated with increased BMI, waist circumference and percent body fat in children aged 5 and 12 years [289]. In a pooled analysis of three birth cohorts, prenatal urinary concentrations of the DEHP metabolite mono-3-carboxypropyl phthalate (MCPP) were associated with increased weight among 4–7-year-old children [290]. In a birth cohort study, DEHP exposure inferred from metabolite measurements in the infant’s first urine was positively associated with increased weight at three months [291]. Prenatal exposure to a mixture of five metabolites of high molecular weight phthalates, measured twice during pregnancy, was associated with lower early weight gain in infancy and lower BMI at 4–7 years of age in boys, but with higher infant weight gain and childhood BMI in girls [292]. A metabolite of DEP, measured once during pregnancy, was associated with offspring BMI at five years of age in the EDEN mother–child cohort study [293]. DEHP, DiBP, DEP, and di-n-butyl phthalate (DNBP) exposure measured in a cross-sectional study in adolescents were associated with abdominal obesity and waist circumference [294].
Overall, the data associating in utero phthalate exposure with weight gain in the offspring were inconsistent. Several studies reported no significant associations or inverse associations. Maternal first-trimester phthalate acid levels but not DEHP or DOP concentrations increased childhood adiposity at ten years [295]. In the U.S., levels of non-DEHP phthalates in the womb were associated with a lower BMI, smaller waist circumference, and lower fat mass in boys at age 5–7 [296]. There was no association in girls or with DEHP metabolite levels. Prenatal phthalate exposures, measured once during the third trimester in a New York birth cohort, were not associated with increased body fat among children 4–9 years of age [297]. Prenatal exposure to 11 phthalate metabolites, measured twice during pregnancy, showed that urinary concentrations of MEP monocarboxy-isonyl phthalate were consistently associated with increased BMI z-score and childhood adiposity at 5 years of age [298]. Mono(2-ethyl-5-carboxypentyl) phthalate (MECPP) was inversely related to the risk of child obesity [253]. In a birth cohort study that used repeated phthalate measurements during gestation, infancy, and childhood, results showed no association between the sum of DEHP metabolites and child adiposity at eight years or no association between urinary MEP metabolite concentrations at 5 and 8 years of age with adiposity at 8 years [299].
4.4.5. Integration and summary of evidence
The in vitro zebrafish and rodent studies present compelling evidence that the long-chain phthalates DEHP and DBP are obesogens. However, many of the phthalates that humans are exposed to have not been adequately studied, especially the low molecular weight phthalates found in personal care products and new phthalates like 1,2-cyclo-hexane dicarboxylic acid diisononyl ester (DINCH). Exposure levels are usually inferred by measuring urinary phthalate metabolites. Single measurements cannot accurately assess long-term or continual exposure due to a short phthalate half-life. Many epidemiological studies suffer from an inadequate exposure assessment, lack of evaluation of current phthalates, and lack of sensitive endpoints outside of body weight and BMI. Phthalate cross-sectional studies are of limited value. The mechanism underlying how many phthalates act alone or in mixtures is unclear.
4.5. Air pollution
Ambient air pollution is a significant global environmental health risk factor contributing substantially to the worldwide burden of disease [300,301]. Ambient air pollution levels increased significantly over the past three decades [302]. PM2.5 refers to atmospheric particulate matter (PM) with a diameter of less than 2.5 μm. Although annual average PM2.5 and ozone concentrations continue to decrease in high-income countries, most of the world population lives in areas where air quality guidelines are routinely exceeded [300].
4.5.1. Rodent studies
Several mechanisms have been proposed to contribute to air pollutants’ obesogenic and diabetogenic effects. Studies have focused on the impact of ozone, nitrogen oxides, black carbon, and proinflammatory effects of PM, as well as the metabolic effects of gases and other major PM constituents, such as PAHs or transient metals [303]. The effects of PM and their constituents may be linked with endothelial dysfunction and insulin resistance [304], oxidative stress, inflammation, increased leptin levels and interference with the endocrine system [304-311]. Chronic exposure of mice to the PAH, BaP caused obesity [312-314]. Exposure to diesel exhaust, which contains large quantities of PAHs, can also cause mitochondrial dysfunction and lipid accumulation in liver cells, in vitro and in vivo [315]. Early-life exposure to PM leads to subsequent insulin resistance, adiposity, and inflammation in mice [316]. Prenatal exposure of rats to PM2.5 predisposed the progeny to multiple long-term metabolic defects, although this may not lead to obesity in adults [317]. PM2.5 exposure induced impaired glucose tolerance, insulin resistance or lipid metabolism disorders in mice [318]. Liver glucose and lipid metabolism were altered in mice exposed to PM2.5 [319]. Changes in cellular lipid profiles were linked with adverse metabolic effects observed after PM exposure [320]. PM in ambient air promoted adipose tissue growth in experimental animals [321]. PM may interact with other obesogenic factors to induce inflammation, oxidative stress or T2D in experimental animals [322-324]. PM has a higher impact in animals with a genetic predisposition to T2D [325].
The pro-inflammatory effects of PM [326] may be the principal cause of their impact on obesity and T2D development. PM exposure elicited pulmonary and systemic inflammation, contributing to metabolic syndrome and cardiopulmonary disease [327]. Exposure to polluted air increased systemic oxidative stress and inflammation in various tissues [328]. It may exaggerate inflammation within adipose tissue and promote insulin resistance in mouse models [304,306,329]. Induction of inflammation is a common effect of various types of PM, regardless of their origin [308]. Systemic inflammation and oxidative stress could trigger changes observed in numerous organs, including vasculature, liver, skeletal muscles, and white and brown adipose tissues [330,331].
The gut microbiome represents another potential target of air pollutants. Both PM and PAHs alter gut microbial composition to favor bacterial taxa linked with obesity and diabetes in experimental animals. However, only a few studies have been carried out in humans [303,332].
Numerous components of PM, in particular PAHs, are ligands of AhR [333] and may disrupt the physiological role(s) of AhR in regulating epithelial barrier integrity [334]. In addition to the above mechanisms, air pollution also impacts physical activity, affects hypothalamic inflammation, the hypothalamic–pituitary-adrenal axis or acts via epigenetic mechanisms in animal models [335-337].
4.5.2. Human studies
Ambient air pollution contributed to children’s increased obesity and abdominal adiposity [338]. Traffic air pollution is positively associated with BMI growth in children [339-341]. There is limited evidence that prenatal exposure to PM can lead to obesogenic effects in infants [342]; however, early-life exposure to air pollution may increase the risk for overweight and obesity later in life [343-345]. Air pollution exposure impacted lipid levels in young adults, particularly those with obesity [346] and altered FA metabolism [347]. Systematic evaluation of several distinct birth cohorts indicated that air pollution contributed to childhood obesity [208], and a similar finding was reported in another large-scale study [348]. A recent meta-analysis and systematic literature review evaluated whether air pollution exposure was associated with childhood obesity [349]. They reported that PM2.5, PM10, PM2.5 absorbance, and NO2 significantly increased the risk of obesity in children (OR 1.06, 1.07, 1.23, and 1.10, respectively). In contrast, other studies suggested that the association of traffic-related pollution, including prenatal exposure, with child overweight is weak or nonexistent [350-352].
Other studies pointed to the potential role of ambient air pollution or traffic-related air pollution in specific adult populations. It was proposed that older adults will be more sensitive to obesogenic and adipogenic effects of PM [353-355]. Sex, age, or a genetic susceptibility to higher BMI may sensitize individuals during long-term exposure to ambient air pollutants, increasing the risk of obesity. In individuals exposed to increased PM levels, a higher risk for metabolic syndrome, waist circumference, hypertriglyceridemia, and hyperglycemia were observed [356]. More extensive longitudinal studies, with finer analysis of air pollution composition, are needed to investigate further links between air pollution and overweight/obesity [357].
4.5.3. Integration and summary of evidence
Mechanistic and epidemiological studies associated chronic exposure to ambient air pollution with increased obesity (particularly during childhood from exposure in utero) and an elevated risk for T2D. Evidence strongly suggests that air pollution is an obesogen that can contribute to these effects. The functional links between air pollution and metabolic disease, potentially contributing to obesity and severe consequences in adult life (including an increased risk of T2D), certainly deserves more attention. This could be particularly relevant for vulnerable populations, such as those with pre-existing metabolic dysfunctions [358].
4.6. Tributyltin
TBT is a well-characterized obesogen [reviewed in [18]]. TBT and other organotins are widely used in industry and to a lesser extent in agriculture. Humans are exposed to TBT via the diet since TBT continues to contaminate seafood due to its ongoing, albeit diminishing, use in marine shipping applications [359]. TBT is also used as a fungicide in paper mills and industrial water systems [reviewed in [360]]. The related organotin, triphenyl tin (TPhT), is used as a fungicide on potatoes, sugar beets, beans, and pecans (among others) and as a miticide on certain food crops, including stone fruits and nuts, presenting additional opportunities for human exposure [361]. Perhaps most notably, TBT is present as a contaminant of dibutyltin (DBT) used at up to 3% w/w in PVC plastics. House dust contains organotins, and these are likely to be dermal and inhalation hazards for humans [362,363].
4.6.1. Dibutyltin
DBT is found in PVC plastics and leaches into drinking water from PVC pipes. It is also the primary breakdown product of TBT. In mice, developmental exposure to DBT resulted in increased adipose tissue and insulin resistance [364]. It also stimulated adipogenesis in 3T3-L1 cells and human and mouse MSCs via a PPARγ-dependent pathway [364,365].
4.6.2. In vitro studies
TBT is a high-affinity activator of the nuclear receptors PPARγ and its heterodimeric partner, RXR, at nanomolar levels in vitro [70,71]. X-ray crystallographic analysis showed that TBT binds to RXR as a covalent adduct to cysteine 432 of helix 11 in the RXRα protein [366]. TBT can also bind to the PXR and may modulate the affinity of RXR-PXR heterodimer for transcriptional coactivators [367]. TBT induced differentiation of mouse 3T3-L1 preadipocytes into mature white adipocytes [70,71,368], and this differentiation was blocked by co-treatment with a PPARγ antagonist [369]. Human and mouse MSCs were also induced to differentiate into white adipocytes via a PPARγ-dependent pathway after exposure to nanomolar (nM) levels of TBT [369,370], as was the mouse MSC-like cell line C3H/10 T1/2 [267]. Prenatal TBT exposure shifted the fate of adipose-derived and bone marrow-derived MSCs preferentially toward the adipose lineage and away from the bone lineage in exposed mice [370] and mouse MSCs, in vitro [371] via an RXR-dependent pathway. Finally, the human liver cell lines, HepaRG and HepG2, responded to nM levels of TBT by increasing lipid content via activation of PPARγ [372].
4.6.3. Zebrafish studies
Zebrafish larvae treated with nM concentrations of TBT exhibited increased adiposity in both short-term and chronic exposures [373-375]. TBT modulated the transcription of key lipid regulating factors and enzymes involved in adipogenesis, lipogenesis, glucocorticoid metabolism, and growth and development [66,376]. TBT exposure also increased body weight and food intake in goldfish [377] and adiposity in salmon and medaka [378,379]. While TBT activates mammalian PPARγ, its zebrafish ortholog was unresponsive to TBT, perhaps due to a specific mutational remodeling of the ligand-binding pocket [380]. Since TBT binds avidly to RXR [366], TBT may induce fat accumulation via RXR homodimers or by activating the RXR side of the RXR-PPARγ heterodimer. A zebrafish study using TBT and selective antagonists of various nuclear receptors suggested that TBT may promote triacylglycerol storage in adipocytes via RXR-dependent pathways independently of PPARs [381].
4.6.4. Rodent studies
TBT was the first chemical designated an obesogen in vivo [382]. Prenatal or perinatal exposure to TBT in mice led to increased body fat in the offspring [43,44,382] and predisposition of the MSCs to produce adipocytes when cultured ex vivo [370]. TBT induced obesity in mice in both sexes irrespective of the age at treatment [383-386]. Similar effects were observed in rats [386]. As noted earlier, exposure to low doses of TBT throughout pregnancy or pregnancy and lactation led to transgenerational predisposition to obesity in the male offspring to at least the F4 generation [43,44].
In addition to its direct effect on adipogenesis, TBT is also toxic to the liver and interferes with the control of metabolism via effects on the brain. When adult rats were exposed to TBT for 54 days, males exhibited increased body weight and fat mass while females showed increased food intake. Females had an increase in NPY while males showed depressed brain POMC, AgRP and cocaine and amphetamine-regulated transcript (CART) mRNA expression, indicating specific actions on the control of feeding behavior [386]. Another adult feeding study of TBT in male mice showed no weight gain but reduced NPY and Y1-related β-galactosidase activity in the hypothalamic circuit controlling food intake [387]. Therefore, the effects of TBT on the control of feeding behavior are not clear.
4.6.5. Human studies
There are few epidemiological studies of TBT exposures and their effects, despite the strength of the animal literature. A single longitudinal Finnish cohort study revealed a linear association between placental TBT levels and infant weight gain, although TBT was undetectable in the blood [388]. Although the National Health and Nutrition Examination Survey (NHANES) data are cross-sectional and, therefore, unsuitable for inferring causality, a recent analysis of NHANES data identified a significant link between elevated urinary total tin levels and diabetes [389]. In this population, exposure to tin was ubiquitous [390]. However, in a small cohort (55 individuals) of Danish women, significant levels of TBT were not identified in a study conducted by the National Toxicology Program (NTP) [391]. Significantly, it was recently shown that plastic specimen containers of the type universally used in such studies were strong binders of TBT and other organotins, markedly reducing organotin recovery during analysis [392]. Therefore, previous studies of organotin levels in human specimens, including the NTP study, probably substantially underestimated TBT levels because they used plastic blood and specimen containers during processing and analysis.
4.6.6. Integration and summary of evidence
The obesogenic effects of TBT exposure are well-supported via in vitro, zebrafish, and rodent assays. TBT stimulates the differentiation of preadipocytes to adipocytes and alters the brain feeding centers and liver lipogenesis. The lack of longitudinal human data precludes a definitive assessment of the obesogenic effects of organotins in humans, but evidence from other studies is substantial. Therefore, the obesogenic effects of TBT exposure are well-supported in the literature [18].
4.7. Flame retardants
Flame retardants such as polybrominated diphenyl ethers (PBDE) and organophosphate flame retardants (OPFR) are classes of EDCs. To meet government fire safety regulations, flame retardants were added to products assuming that this would reduce combustibility. These products include furniture, clothing, toys, electronics, plastics, and other household and workplace furnishings. Flame retardants are not chemically bound to the fabric, plastic, or materials and may be volatile. They are found in house dust, food, water and the air of offices, airplanes, and other workplace environments [393-396]. There are 209 PBDEs, and most are persistent, bioaccumulative, and neurotoxic. Evaluation of PBDE safety led to a phase-out in Europe and the USA [397]. Five to ten years after the phase-out, PBDEs were detected in human samples (placental and breast milk) at concentrations from 1 to 60 ng/g lipid [398,399] compared to standard safety levels set at 0.1–7 mg/kg/day. BDEs have been primarily replaced by OPFRs, which have shorter half-lives of hours to days [400].
OPFRs are organic esters of phosphoric acid containing alkyl chains or aryl groups. While the use of PBDEs is declining, OPFR use is increasing, and they may exhibit similar toxicity [401]. Human body burdens of OPFRs and their metabolites are increasing, with some metabolites found at levels 15 times higher in 2014–15 than in 2002–03 [402-404]. Since there are many different PBDEs and OPFRs, most assays assess the effects of representative chemicals like PBDE-47 or PBDE-97 or triphenylphosphate (TPhP). OPFR metabolites are detectable in human urine, breast milk, and blood samples [405]. TPhP, tricresyl phosphate (TCP), and tris (1,3-dichlor-2-propyl) phosphate (TDCPP) are found in household dust at median concentrations of ~1–6 μg/g dust and are accidentally ingested by pregnant people and their developing infants [406].
4.8. PBDEs
4.8.1. in vitro studies
Exposure of 3T3-L1 adipocytes to PBDE-47 and PBDE-99 induced adipogenesis in a dose-dependent manner (2.5–30 μM) [407,408] and induced expression of PPARγ via demethylation of CpG sites in the PPARγ promoter [408,409]. This induction led to leptin and glucose-6-phosphatase catalytic subunit expression and disruption of adipocyte glucose homeostasis in vivo [409]. Furthermore, PBDE-47 altered purine and glutathione metabolism in 3T3-L1 cells and elevated mitochondrial respiration and glycolysis, leading to reactive oxidative stress [410]. PBDE-47 also activated Akt signaling via thyroid hormone signaling in pancreatic β-cells to augment glucose-stimulated insulin secretion [411].
4.8.2. Rodent studies
Many rodent studies reported that perinatal PBDE exposures altered adult offspring’s growth, body weight, adiposity, and glucose and insulin homeostasis. PBDE-47 exposure at 0.1 and 1.0 mg/kg, the no observed adverse effect level ((NOAEL) is 0.7 mg/kg), from pre-mating until weaning increased body weight in male offspring. It was hypothesized that PBDE-47 exposure induced a malnutrition-like state in dams, leading to subsequent weight gain susceptibility in male pups [412]. Exposure to a low dose of PBDE-47 (0.2 mg/kg/day) induced greater pup and juvenile growth and body weight in rats potentially through augmenting IGF-1 signaling in male pups [413]. In mice, perinatal exposure to the same dose of PBDE-47 altered xenobiotic and lipid metabolic genes in gonadal adipose tissue in young male offspring [414]. In male mice, PBDE-47 exposure exacerbated the response to diet-induced obesity with hepatic steatosis and perturbation to the gut microbiome [415].
Adult PBDE exposures also influenced metabolic processes in rodent models at doses that were within the upper range of exposure or exceeded human exposures. Adult exposures to low doses of PBDEs (0.5 or 10 μg/kg/day drinking water) exacerbated the response to diet-induced obesity by inducing hyperglycemia and disrupting insulin action in skeletal muscle [416]. Adult exposure to PBDE-47 (1 mg/kg, 6 d/week, 8 weeks) induced hyperglycemia in male rats, which correlated with increased hepatic expression of genes involved in glucose mobilization in a diet-induced obesity model [417]. PBDE exposure may also target the gut microbiome because short-term oral dosing of PBDE-47 or PBDE-99 altered metabolites of branched-chained and aromatic amino acids and populations of twenty-three bacterial taxa in the gut [418]. These studies indicate that chronic, intermittent, or short-term exposure to doses relevant to human exposures can disrupt metabolic processes and exacerbate metabolic disruption associated with obesity.
4.8.3. Human studies
Numerous studies have examined the relationships between PBDE body burdens or perinatal exposures and metabolic outcomes and disease states. In women from the United Kingdom, the body burdens of hexabromocyclododecane (HBCDD) were weakly correlated with higher body weights [419]. In women from an indigenous Canadian population (Cree), positive correlations were found between elevated fasting glucose levels and plasma PBDE-47 concentrations [420]. A study of adult women from the California-based CHAMACOS study found that serum concentrations of PBDE-153 were associated with lower BMI over the subsequent 1–3 years.
Prenatal PBDE exposure was associated positively and negatively with BMI in childhood depending upon the sex of the subject, location of the study, and the specific PBDE studied. In a longitudinal birth cohort study of PBDE exposure in children from a Latin American population in California, maternal serum PBDE concentrations were associated with higher BMI in boys but lower BMI in girls at age seven years [421]. This is expected as the effects of environmental chemical exposures tend to be sex-specific. However, in a study in China, PBDE-153 and PBDE-154 levels were associated with lower BMI and waist circumference in children at 8 years of age [422]. Similarly, maternal PBDE (99, 100, 153, 154, 209) levels from colostrum taken up to 96 hr postpartum were not associated with child BMI and obesity risk at age 7 years [253]. In the Health Outcomes and Measures of the Environment Cohort, prenatal and perinatal exposures to PBDE-153 (50–200 ng/g lipid) were negatively correlated with BMI, waist circumference, and percent body fat up to 8 years of age [423]. These results suggest limited evidence that perinatal exposures to PBDEs can alter metabolic processes in children. Different results may stem from the various ages of children at the time of weight or adiposity assessment, as well as differences in the specific PBDE examined and range of exposure in each population and other cooccurring chemical exposures.
4.8.4. Integration and summary of evidence
The in vitro and animal models, supported by limited human studies, indicate that the PBDEs tested are obesogens. Since PBDEs are now banned, their effects on obesity should decrease as their levels gradually decline.
4.9. Organophosphate flame retardants (OPFRs)
4.9.1. In vitro studies
TPhP (1–50 μM) induced adipocyte proliferation and differentiation while increasing PPAR and CCAAT/enhancer protein (C/EBP) transcripts levels [424]. The OPFR 2-ethylhexyl diphenyl phosphate (EHDPHP) altered the expression of genes involved in the cell cycle, immune response, and glucose and lipid homeostasis. In a similar study using human HepG2 cells, TPhP, trTCP, and TDCPP increased intracellular triglyceride and total cholesterol deposition through modulation of fatty acid β-oxidation by altering the signaling of PPARγ and SREBP2 [425]. TPhP decreased mitochondrial oxygen consumption and ATP content, supporting findings in the adult and perinatal exposure studies [426,427]. TPhP also created adipocytes with different properties than ROSI, including failure to induce beige adipocyte differentiation, differences in the proteome, reduced mitochondrial biogenesis, differences in cytoskeletal and other proteins involved in lipid and glucose homeostasis [428].
4.9.2. Zebrafish and chicken studies
Both adult and developmental exposures to OPFRs impact metabolic processes in non-mammalian models. In zebrafish, exposure to TPhP at environmentally relevant concentrations induced many hepatic metabolic and transcriptional changes, including glucose and lactate metabolism and PPAR signaling [429]. In developing chickens, TDCPP induced CYP3A37 and CYP2H1 expression, cholestatic liver and biliary fibrosis, disrupted lipid and steroid metabolism, increased circulating bile acid, decreased plasma cholesterol and altered PPARγ expression [430].
4.9.3. Rodent studies
OPFRs pose a similar, if not higher, risk for metabolic disruption than PBDEs due to their prevalence in manufactured products. OPFR exposure increased glucose, triglyceride, and cholesterol levels together with the hepatic expression of genes involved in glucose metabolism [431], increased serum triacylglycerol, LDL and very low-density lipoprotein (VLDL) concentrations by inhibiting carboxylesterase (Ces) enzymes in the liver [432] and increased total serum cholesterol and high-density lipoprotein (HDL) cholesterol in both sexes in mice [433]. At doses approaching human exposures, an OPFR mixture of TPhP, TDCPP, and TCP (1 mg/kg each) impacted energy homeostasis, hypothalamic and hepatic gene expression, and hypothalamic neuronal excitability in adult mice. A 4-week oral administration of the OPFR mixture increased hypothalamic and hepatic gene expression and body weight gain, potentially via ERα [434]. Exposure to the same OPFRs disrupted food and fluid intake, reduced leptin and insulin production, increased fasting glucose levels, suppressed locomotor activity and metabolic rates [435], and produced fatter, heavier male mice on a HFD with no effect on female adiposity. Adult exposure to the same OPFR mixture induced hyperexcitability in POMC neurons via increasing excitatory presynaptic inputs in female but not male mice. OPFR exposure also increased the excitability in NPY/AgRP neurons in female mice, partly through inhibiting the M–current, the potassium current that controls firing frequency. NPY/AgRP neurons in females were also more sensitive to the hunger hormone ghrelin after exposure to OPFRs [427]. Collectively, these data suggest that adult exposures to OPFRs in rodents at concentrations exceeding non-occupational daily human exposures may disrupt energy homeostasis through nutrient- and hormonally sensitive circuits that control homeostasis, especially in males.
There is a growing body of research on the perinatal effects of OPFR exposure on offspring metabolism in rats and mice. Perinatal exposure to EHDPHP in male mice increased body weight when the males were fed a low-fat diet [436]. In a study using a commercial mixture of OPFRs and brominated flame retardants, Firemaster® 550, perinatal exposure (1 mg/kg/d) increased body weight and decreased glucose clearance in female rat offspring [437]. Conversely, perinatal exposure in Wistar rats to a mixture of OPFRs or a mixture of new brominated flame retardants (2-ethylhexyl-2,3,4,5-tetrabromobenzoate (EH-TBB) and TBPH reduced body weights in male offspring from postnatal days 64 to 250 [438]. In female offspring, juvenile body weight was lower in the exposed groups, with normalization occurring by postnatal day 49.
Perinatal exposure to TPhP in CD-1 mice fed a HFD increased body weight and adiposity, liver weight, and lipogenesis gene expression [415,439,440]. Maternal exposure to a mixture of TPhP, TDCPP, and TCP in C57Bl/6J mice, did not affect body weight or adiposity on a low or HFD. However, the OPFR mixture interacted with the HFD to increase fasting glucose in females and altered glucose and insulin resistance in male offspring [441]. Thus, maternal exposure to some OPFRs programs the liver and adipose tissue in a sex and animal model manner, changing their response to an obesogenic diet and altering adult energy homeostasis.
4.9.4. Human studies
Since the phase-out of PBDEs, body burdens of OPFRs in humans have increased to levels higher than PBDEs [401,404]. Limited data associated OPFR exposure with metabolic outcomes. Using US NHANES data and samples, OPFR metabolites including tris(2-chloroethyl) phosphate (TCEP) and TDCPP were associated with metabolic syndrome in adult men, and OPFR mixtures were associated with metabolic syndrome, hyperglycemia, and central obesity [442]. Another study using NHANES data found greater odds for being overweight among children with high concentrations of bis(2-chloroethyl) phosphate (BCEP) but lower BMI associated with higher concentrations of dibutyl phosphate (DBUP) [443].
The only two birth cohort studies that examined prenatal OPFRs found that in utero exposures resulted in weight gain in the offspring. Maternal urinary concentrations of bis(1,3-dichloro-2-propyl) phosphate (BDCPP) during pregnancy were associated with a greater infant ponderal index at birth [444]. Additionally, a pilot study (n = 56) found a positive association between BDCPP and increasing infant length and weight in males only [445].
4.9.5. Integration and summary of evidence
Both former flame retardants (PBDEs) and their newer replacement compounds (OPFRs) are obesogens, depending on the animal model, dose, exposure window, sex of the animal, and metabolic outcome examined. While the epidemiology studies are limited, the results are consistent that all OPFRs tested are obesogenic and or metabolically disruptive in adults and offspring from in utero exposure.
4.10. Pesticides/DDT
While numerous classes of pesticides have been implicated as potential obesogens, including the organochlorine, organophosphate, and pyrethroid classes, the data tend to be inconsistent [446,447]. The most widely studied pesticide analyzed were organochlorines dichlorodiphenyldichloroethylene (DDE), DDT and their metabolites, including dichlorodiphenyldichloroethane (DDD) (p,p′-DDE/p,p′-DDD and p,p′-DDT), hexachlorobenzene (HCB) and β-hexachlorocyclohexane (βHCH) [13,447,448]. DDT is an obesogenic pesticide with the most data. While its use was banned in the United States in the early 1970s, DDT is still used in India and Africa for malarial vector control [449,450]. Technical DDT is a persistent organic pesticide mixture of three isoforms, p,p′-DDT o,p’-DDT and p,p’-DDD. DDT is metabolized to the bioaccumulative DDE, which is highly lipophilic and persistent in the environment and food chain [451]. Thus, exposure to DDT via environmental or occupational contact and DDE via consuming contaminated foods remains a relevant concern worldwide.
4.10.1. In vitro studies
Human preadipocytes treated with DDE for 48 h were induced to proliferate [452]. DDE exposure increased the differentiation of murine 3T3-L1 preadipocytes to mature adipocytes [453-455]. DDT exposure also induced adipogenesis in 3T3-L1 preadipocytes and MSCs [456,457]. These in vitro pro-adipogenic effects of DDE and DDT were associated with upregulation of key mediators of adipogenesis, including C/EBP-α, FAS, sterol response element-binding factor-1, and PPARγ [454,456]. DDE exposure increased fatty acid uptake in 3T3-L1 adipocytes and increased the expression and/or release of adipokines (adiponectin, leptin, and resistin) in 3T3-L1 adipocytes MSCs [457-459]. However, DDE/DDT did not induce adipogenesis in all studies [458,459].
4.10.2. Rodent studies
Perinatal exposure to DDT in mice increased body and fat mass restricted to female offspring and attributed to decreased energy expenditure and reduced thermogenesis [460]. Exposure of rats to DDT (25 mg/kg or 50 mg/kg) on days 8–14 of gestation produced significant obesity in both males and females in the F3 generation from low dose dams and F3 males from high dose dams [46]. Numerous in vivo studies examined alterations in systemic lipid metabolism as an index of obesogenic potential. A systematic review determined that the most consistent index of DDT/DDE-induced alterations in systemic lipid metabolism were alterations in hepatic lipid metabolism. The predominance of studies indicated that exposure to DDT/DDE increased hepatic cholesterol, triacylglycerol, total lipids, and liver weight in experimental rodent models [461].
4.10.3. Human studies
Because DDT was widely used, it was studied in birth cohorts and cross-sectional studies across the globe. DDT is highly lipophilic; therefore, it was frequently screened in the lipid portion of serum, placenta, and adipose tissue, considered the main reservoir for DDT accumulation [462]. Cross-sectional studies in adults frequently reported positive associations of DDT/DDE body burden with obesity estimates, such as BMI [463-465], waist circumference [466], visceral and subcutaneous adipose tissue depots [467], and total fat mass [468]. Opposite or null findings were reported in some cross-sectional studies. Serum DDT/DDE levels were not associated with BMI in Tunisians [469], fat mass percentages of the trunk, leg, and whole body in the NHANES (U.S.) population [470] or BMI, waist circumference, fat mass percentage, or total and subcutaneous abdominal adipose tissue in obese Belgians [471]. Cross-sectional associations of DDT with obesity may depend on the timing of exposure and age of the population, with negative associations during the exposure stage eventually turning positive after 2–3 half-lives [472].
Adult longitudinal studies results were more consistent. In an adult cohort study in Sweden, serum p,ṕ-DDE was associated with both greater waist circumference (cross-sectional study) and a 5-year incident abdominal obesity (longitudinal study) [473]. Serum p,p′-DDT and p,p′-DDE concentrations from U.S. adults prospectively correlated with increased BMI 18 years later and showed a non-monotonic dose–response pattern [474].
A positive association was found in a Japanese population between estimated postnatal p,p’-DDE levels and BMI z-score at 42 months of age, mostly in girls [475]. Positive associations of maternal DDT/DDE exposure with rapid growth/obesity during infancy were reported in the INMA birth cohort (Spain) [253,476] and LIFE Child cohort (Germany). Positive prospective associations of maternal DDT/DDE exposure levels and obesity measures were reported in a diversity of locations worldwide, e.g., South Africa [477], United States [478,479] Belgian girls but not boys [480], seven pooled European birth cohorts [481] and Greece [482].
A 2017 systematic review identified seven prospective epidemiological studies reporting positive associations between exposure to p,p’-DDE and adiposity measured by BMI z-score [461]. Perhaps the most interesting data comes from the Child Health and Development Cohort where perinatal exposures to o,p’-DDT in the 1960s were positively associated with a higher risk of overweight and obesity in their daughters during their mid-life [483]. A recent report from this cohort showed that grandmother exposure to DDT could have increased obesity in current young adult women and their granddaughters [484].
Other studies reported no association between maternal exposure to persistent organochlorines including DDT and child obesity, including populations from the United States [485], Mexico [486], pooled cohorts from Ukraine, Greenland and Poland and Sweden [487], a Norwegian and Swedish population [488], and Korean children [489]. In a Faroese mother–child cohort, maternal exposure to persistent pollutants was linked to increased BMI z-scores and/or overweight risk at ages 18 months and/or five years, although the associations were unclear for DDT/DDE [490]. Several factors could explain these findings, including the above-mentioned differential exposure levels since null associations were more likely to be reported in populations with higher exposure levels [485] unaccounted effect modifiers such as smoking [491] or prepregnancy BMI [492]. Exposure estimations based on one spot sample may bias results toward the null because they may not reflect pre-and post-natal exposures [493].
In assessing the long-term implications of low-dose DDE/DDT exposures, it is crucial to consider potential co-exposure to other chemicals with similar physicochemical properties and possible mechanisms of action, such as other organochlorine pesticides and certain PCBs. These usually show moderate-to-high correlations [494] that add residual confounding and mask individual effects [495]. Concentrations of DDT and its metabolites will likely vary significantly in different countries due to variations in its use and when it was banned. Levels measured in countries with less use and where measurements were made more recently will tend to be lower and result in minimal differences across quartiles of concentrations making associations with obesity challenging to assess.
4.10.4. Integration and summary of evidence
A 2017 systematic review of in vitro, animal and epidemiological data on DDT exposures and obesity concluded the evidence indicated that DDT was “presumed” to be obesogenic for humans [461]. The in vitro and animal data strongly support DDT as an obesogen. Based on the number of positive prospective human studies, DDT is highly likely to be a human obesogen. Animal and human studies showed obesogenic transmission across generations. Thus, a POP banned almost 50 years ago is still playing a role in the current obesity pandemic, which indicates the need for caution with other chemical exposures that can cause multigenerational effects.
4.11. Dioxin and PCBs
The polychlorodibenzo-p-dioxins and dibenzofurans (PCDD/PCDFs), commonly grouped as dioxins, are byproducts released during the combustion of organic compounds or the manufacture of organochlorine chemicals. PCBs were used in electric transformers and capacitors because of their resistance to temperature and pressure. Polychlorinated dioxins, dibenzofurans and coplanar dioxin-like (dl) PCBs share similar structures and toxicity as they bind to the AhR and activate xenobiotic metabolism enzymes [105]. They are prototypical POPs that persist for many years and adversely affect humans and ecosystems. The Stockholm Convention banned their use and production in 2001, but they are still detectable in ecosystems and biological matrices. They are stored in adipose tissue and released during weight loss. Since there are 209 PCBs, studies usually focus on a specific PCB or a standard mixture of PCBs. Whereas dl-PCBs with a coplanar molecular structure may act like dioxins, i.e., activate AhR, so-called non-dioxin-like (non-dl) PCBs with a non-coplanar structure have different toxic modes of action. Thus, the effects of mixtures of different PCBs will depend on the relative contribution of both groups to their composition.
4.11.1. In vitro studies
TCDD is a prototypical AhR agonist with a high binding affinity. It displays anti-adipogenic effects with decreased expression of C/EBPβ, PPARγ2, key adipogenic factors or aP2 and GLUT4, decreased glucose uptake or LPL activity in 3T3-L1 cells, C3H10T1/2 cells and primary rat adipocytes [496-498]. The effects of PCBs on adipogenesis in vitro are congener-specific. PCB 126, a dl-PCB that activates the AhR, displays complex responses. It is anti-adipogenic in human preadipocytes [499] and blocks beiging in human preadipocytes. This can disrupt energy homeostasis and indirectly promote the development of obesity and diabetes [500]. PCB 126 stimulate the release of adipokines from 3T3-L1 adipocytes and hMADS cells [105,500]. Contradictory results were observed with another dl-PCB, PCB 77, which displayed pro-adipogenic effects in 3T3-L1 cells at low concentration and anti-adipogenic effects at higher concentrations [501]. The non-dl-PCBs (PCB 101, 138, 153 and 118) promoted adipogenesis in 3T3-L1 cells, reviewed in [15]. The effects of non-dl-PCBs on adipogenesis could be partly related to their ability to activate pathways other than AhR involved in controlling metabolic functions. Overall, the in vitro effects of AhR ligands on adipogenesis do not appear to be consistent and depend on the cellular system.
4.11.2. Rodent studies
TCDD-like compounds affect metabolic homeostasis and host-microbiome interactions. Metabolomic analysis of mice treated with 2,3,7,8-tetrachlorodibenzofuran (TCDF), an environmental AhR ligand with a similar potency to TCDD, revealed significant metabolic dysfunction in gluconeogenesis, glycogenolysis, and lipogenesis [502]. The gut microbiota composition is altered in AhR knockout mice [503]. Dietary AhR ligands may shape gut microbiota’s composition and proper functioning, suggesting that TCDD may alter both microbiome composition and host-microbiota interactions [504].
Initial studies associated exposure to high doses (25–200 μg/kg) of TCDD with hypoglycemia, hypoinsulinemia due to β-cell apoptosis and hypophagia, leading to the wasting syndrome reviewed in [505]. Lower doses (10 μg/kg) altered serum lipid concentrations by reducing the liver and adipose fatty acid synthesis rates and the activity of liver gluconeogenic enzymes [506,507]. However, opposite results were observed using PCB 77, another dl-PCB. PCB-77 increased body mass in wild-type C57BL/6 mice but not in Ahr−/− mice [501]. Kynurenine (KYN), an AhR agonist produced due to tryptophan metabolism, caused weight gain, fatty liver and hyperglycemia in mice fed a low-fat diet [508]. Exposure of female mice to TCDD during lactation and pregnancy increased their susceptibility to HFD-induced obesity and diabetes [509]. TCDD is also obesogenic in adult mice fed a HFD [510]. Therefore, TCDD-like compounds may impact in vivo obesity depending on the doses used and the type of diet [511].
Lastly, PCB153 is an obesogen that exacerbated hepatic steatosis, altered adipocytokine expression and disrupted hepatic lipid metabolism in adult mice but only when administered with a HFD [111]. This study also supports a model in which the liver is where AhR signaling is important in obesity.
4.11.3. Human studies
Epidemiological data from cohorts with accidental (Vietnam war veterans, residents near Seveso) or occupational (farmers) exposures to high doses of dioxin or POPs reported an increased risk for diabetes and impaired glucose metabolism and insulin signaling, reviewed in [512-514], in line with data from rodent studies. However, there are no clear data associating TCDD exposures to an increased risk of obesity. Other AhR agonists, such as PCBs, were associated with increased body weight, BMI, fat mass or waist circumference in some epidemiological studies, reviewed in [515,516]. A 2020 meta-analysis found that eleven cross-sectional studies reported positive associations between chlorinated POPs and obesity, while seven reported negative relationships [248]. One study reported a positive relationship for less chlorinated PCBs and negative relationship for highly chlorinated PCBs [468]. Additional studies were less consistent. There are many explanations for these contradictory results, including differences in the populations studied, co-exposure with other POPs such as organochlorine pesticides, differences in the levels of exposure, etc. Overall, the data from cross-sectional studies of PCBs are inconclusive.
4.11.4. Integration and summary of evidence
Human, rodent, and in vitro studies indicated that the evidence favoring pro-adipogenic effects associated with dioxins and PCBs is currently weak. This does not mean that these compounds do not exhibit obesogenic effects under certain circumstances, for example, when combined with HFD. It is likely that the effects of these compounds are dose-dependent. Dioxins, furans, and some PCBs act through AhR activation, other PCBs have different modes of action, and their effects should be explored in more detail. A confounding factor is the possible co-exposure with other chlorinated POPs such as organochlorine pesticides. While the obesogenic effects of dioxins and PCBs is not clear, their inflammatory and metabolic effects are much more consistent. Thus, in obese individuals, exposure to these contaminants may increase the likelihood of obesity-related metabolic and pathogenic effects.
4.12. Per-and polyfluroalkyl substances (PFAS)
PFAS are a large group (>5000) of unregulated synthetic chemical compounds with multiple fluorine atoms attached to an alkyl chain. PFAS includes PFOA, PFOS, and GenX are widely used in industrial applications and consumer products [517]. Uses include food packaging, coatings for cookware, furniture, manufacturing and processing facilities, airports, and military installations that use firefighting foams. PFAS were detected in air, soil, and water, including drinking water [518]. The strong carbon–fluorine bond makes PFAS highly resistant to degradation; thus, they are called “forever chemicals” with half-lives in humans of months to years [519]. PFAS can cross the placenta and be detectable in fetal tissues and umbilical cord blood [520-522]. PFAS can bioaccumulate in food chains and humans.
4.12.1. In vitro studies
PFOA can induce differentiation in 3T3-L1 preadipocytes by activating PPARγ and demethylating the PPARγ promoter, upregulating PPARγ protein expression [65]. The PFOS substitute, perfluorobutane sulfonic acid (PFBS), stimulated adipocyte differentiation and increased PPARγ and MER/ERK-dependent signaling pathways [523]. Another study showed only modest effects of PFOA and PFOS on adipogenesis in 3T3-L1 cells [407]; however, this study did not show an effect of BPA, which should have been positive. PFOA, PFOS, perfluoronanoic acid (PFNA), and perfluorhexanesulfonic acid (PFHxS) increased cell number, decreased cell size, increased total lipid, and upregulated expression of adipogenic genes in 3T3-L1 cells [524].
PFOA and PFOS robustly activated PPARα, PPARγ, PXR and CAR. In contrast, they marginally activated LXR and FXR as measured by upregulation of target gene expression in rat and human hepatocytes [102]. PFOS treatment of HepG2 cells increased triglyceride levels and decreased phosphorylated Akt, eventually leading to insulin resistance [525]. These studies indicate several potential roles of PFOA and PFOS in obesity.
4.12.2. Zebrafish studies
When zebrafish embryos were exposed to PFOS developmentally, lauric (C12:0) and myristic (C14:0) saturated fatty acids were increased at four days post-fertilization (dpf), and expression levels of all three PPAR genes were reduced [526]. The incidence of aberrant islet morphologies, principal islet areas, and adiposity were increased in 15 dpf larvae and 30 dpf juvenile fish. In utero exposure to PFOS provoked hepatic lipid droplet accumulation in zebrafish [527].
4.12.3. Rodent studies
In agreement with in vitro studies, there are consistent data showing upregulation of PPARα-target genes by PFAS, such as those involved in fatty acid, glucose or glycogen metabolism peroxisome, cholesterol, or bile acid biosynthesis [528,529]. However, PFAS-associated adipogenic effects were rare. In mice, PFOS or PFOA exacerbated total and liver lipid content induced by HFD [530,531]. PFOS or PFOA alone decreased liver-free fatty acid content, total cholesterol and triglycerides in mice and rats [531,532]. This lipid-lowering effect is consistent with PPARα activation. Exposure of adult mice to PFOA or PFOS reduced WAT due to reduced food intake and is dependent on recruitment of brown adipose tissue mediated thermogenesis [533]. Developmental exposure to PFOA increased serum leptin and insulin and increased weight in mid-life in mice [534].
4.12.4. Human studies
Cross-sectional and longitudinal studies examined associations between PFAS and body weight or adiposity in adults. In cross-sectional studies, serum or plasma concentrations of PFAS in adults were associated with greater adiposity and higher prevalence of overweight [535], metabolic syndrome [536,537], and diabetes [538]. Studies in children and adolescents produced variable results regarding the cross-sectional associations between serum or plasma PFAS concentrations and obesity in children: some have reported lower adiposity with certain PFAS [539,540]. Others reported a greater prevalence of obesity [541]. Two metabolome-wide association studies in children showed PFAS correlated with altered metabolic pathways, including lipids and amino acids [542,543]. Another study showed that people with the highest levels of PFAS in their blood had lower resting metabolic rates and regained weight faster after dieting than those with the lowest PFAS levels [544].
A prospective study of adults at elevated risk for diabetes found that plasma PFAS concentrations at baseline were associated with greater weight gain during the subsequent nine years of follow-up; however, no effects were observed in a subset of participants randomized to a lifestyle intervention program to prevent diabetes [545]. A longitudinal study of children and adolescents found that plasma PFOS concentrations at age 9 correlated with a greater BMI, skinfold thickness, and waist circumference at age 15 [546].
Low birth weight is the most consistent outcome reported from gestational PFOA exposures in humans. A systematic review of infants born to mothers with higher pregnancy serum concentrations of PFOA linked exposure with lower birth weight [547] or that PFOA or PFOS exposure led to low birth weight [548] and lowered adiposity at birth [549,550]. Low birth weight is associated with increased weight gain later in life.
Multiple studies reported that certain PFAS measured in maternal blood during pregnancy were associated with greater gestational weight gain [551-555]. Gestational weight gain is associated with greater infant adiposity at birth [556]. Plasma concentrations of PFOA were associated with impaired glucose metabolism and lipid oxidation among overweight and obese young adults in California [557].
Multiple epidemiologic studies reported that prenatal concentrations of PFOA or PFOS were associated with greater weight and adiposity among children aged 5–9 [487,488,558,559], young adults [560] and children overweight at age 5 [488]. Maternal plasma perfluoroundecanoic acid (PFDA), but not PFNA, was associated with greater adiposity in offspring at 4–8 years [561]. A meta-analysis of the human cohort data reported a statistically significant risk ratio of childhood obesity of 1.25, comparing higher to lower early life PFOA exposures [559]. In contrast, others reported null or inverse associations [490,562,563]. Higher PFAS levels were not associated with increased offspring BMI at 5 years in a Swedish cohort, whereas lower levels were [488]. This non-monotonic dose relationship between PFOA levels and BMI was confirmed in a different study [558].
4.12.5. Integration and summary of evidence
The in vitro, zebrafish, and rodent data, indicate that PFOA and PFOS are obesogens. While not wholly consistent, the human data support PFOA and PFOS as obesogens. Only a few of the thousands of PFAS have been examined; therefore, more data are needed to understand the role of PFAS in obesity.
4.13. Additional obesogens of concern
This section contains a description of chemicals designated as obesogens based on data from multiple laboratories and sources (in vitro, zebrafish, rodents, humans). There are data gaps that limit the conclusions drawn.
4.13.1. Non-nutritive sweeteners
Sweeteners can taste much sweeter than sugar and contain few calories [564]. The broad range of sweeteners can be separated into nutritive and non-nutritive groups (Fig. 4). Artificial sweeteners are manufactured and used more frequently in the food industry than natural sweeteners due to their cost-effectiveness [565]. Examples include aspartame, neotame, saccharin, sucralose, acesulfame potassium, and cyclamate [564]. Natural sweeteners can be produced from various sources, including plant saps, honey, fruit and vegetable sugars, as well as steviol glycosides, fructose, xylitol, erythritol, and yacon (Smallanthus sonchifolius) syrup are often touted as “healthier” due to their lower glycemic index [564].
Fig. 4. Classification of nutritive and non-nutritive sweeteners.
There are a variety of nutritive and non-nutritive sweeteners. This classification scheme shows the different categories and where each nutritive and non-nutritive fall to help in understanding their chemical backbone and chemistry.
Non-nutritive sweeteners (NNS) have replaced, and reduced sucrose intake as obesity became more prevalent. NNS are marketed as healthier alternatives [566]. Still, their links to adverse health effects such as reproductive and neurological disorders, cancer, gut microbiota changes, and metabolic syndrome have raised questions about the safety of NNS [567-569]. Aspartame, sucralose, and saccharin have been linked to metabolic syndrome. While they are obesogens, they may not be acting via an endocrine mechanism.
4.13.2. Aspartame and sucralose
A triangulated study of aspartame and sucralose consumption/exposure in a human cohort, in vivo mouse study, and in vitro cell analysis (3T3-L1 adipocytes) presented evidence that maternal NNS consumption during pregnancy may program obesity risk in offspring through effects on adiposity and adipocyte differentiation [570]. Sucralose exposure at early stages of differentiation in 3T3-L1 preadipocytes caused increased lipid accumulation and expression of adipocyte differentiation genes (e.g., C/EBPα, FABP4 and FAS). Pregnant C57BL6J mice exposed to aspartame and sucralose at doses relevant to human consumption gave birth to offspring that developed elevated body weight, adiposity, and insulin resistance. This was especially evident in males, which exhibited body fat increases of 47% (aspartame) and 15% (sucralose). Lastly, children born to 2298 mothers who regularly consumed beverages containing aspartame and sucralose had elevated BMI at three years of age [570]. Together, these studies indicated that certain artificial sweeteners consumed during pregnancy may increase obesity risk in offspring via effects on adipogenesis through key adipocyte differentiation genes. These studies used doses of aspartame and sucralose relevant to human consumption in North America yet below the acceptable daily intake (ADI) established by the Food and Drug Administration (FDA) [570]. These findings may be less relevant to European populations because the recommended ADI established by the European Food Safety Authority (EFSA) is below the study concentrations.
4.13.3. Sucralose
Sucralose reduced food consumption but increased body weight in 21-day-old CD1 mice, and it was hypothesized that the intensity of sucralose sweetness increased preference for sweet-tasting food, leading to weight gain. Sucralose also reduced the secretion of appetiteregulating gut hormones such as gastric inhibitory polypeptide (GIP) [571]. Another study demonstrated changes in the intestinal microbiome resulting in glucose intolerance after sucralose treatment [572]. Exposure of MSCs to sucralose promoted an acute inflammatory response by increasing adipogenesis and ROS concentration [573]. Consequently, sucralose may impact the endocrine system and increase the risk of obesity and T2D even at doses below the recommended ADI.
An in vivo study using male Sprague Dawley rats demonstrated that sucralose may provoke disturbances in the thyroid axis activity [574]. As the thyroid axis is required for regulating development, growth, and energy metabolism, its disruption may increase the risk of obesity.
Clinical studies found that sucralose may increase insulin resistance. A randomized clinical trial reported that sucralose consumption increased insulin resistance after only two weeks of exposure and without the need for continued exposure [575]. The dose of sucralose used in this trial was 15% of the recommended ADI set by the Joint FAO/WHO Expert Committee on Food Additives (JECFA). This study raised concerns about consuming sucralose even for short periods and below the set ADI consumption level, but the follow-up was soon after dosing termination. Further research involving a more extended study period and post-intervention period will be needed to obtain additional results regarding clinical significance. Sucralose consumption with carbohydrates impaired glucose metabolism and reduced insulin sensitivity, leading to diabetes. However, the sample size of healthy adults was limited (n = 45) and performed within a narrow age range (20–45 years old) [576]. Thus, further studies are needed to substantiate this finding.
4.13.4. Saccharin
The body weight of adult male rats treated with 5 mg/kg of saccharin increased by 59% and 67% after 60 and 120 days of exposure, respectively [577]. It is thought that saccharin and other artificial sweeteners increase food intake and ghrelin receptor expression in the hypothalamus, leading to overeating [578].
4.14. Agricultural chemicals
The role of agrochemicals (including pesticides) in obesity has recently been reviewed [448].
4.14.1. Chlorpyrifos
Chlorpyrifos is an organophosphate insecticide with significant human exposure because it is widely used on various field crops across the globe [579]. Chlorpyrifos and two of its metabolites enhanced the storage of lipids and the number of differentiated 3T3L-1 preadipocytes [580]. These effects occurred via upregulation of PPARγ and C/EBPα providing a possible mechanism for the obesogenic effects.
Adult rats receiving 5 mg/kg/day chlorpyrifos for two months weighed more and had increased weight of the perinephric fat pads [581]. Adult mice expressing the human ApoE3 gene, but not the ApoE3 or 4 gene, ate more and had increased body weight and high leptin levels after exposure to chlorpyrifos for 13 weeks [582]. In a related set of experiments, the interaction of genotype (APOE4 gene), sex, and HFD on weight gain stimulated by postnatal exposure to chlorpyrifos were assessed [583]. Only males in the chlorpyrifos-treated group exposed to the HFD gained more weight than the control HFD group. Male APOE3 and APOE4 mice were exposed to chlorpyrifos (1 mg/kg/day) on postnatal days 10–15 and again at five months of age. Only APOE4 mice had increased weight in adulthood, but both APOE3 and APOE4 mice exposed to chlorpyrifos had increased food intake. NPY expression was increased in APOE4 mice [584]. Chlorpyrifos exposed adult rats and mice (C57Bl/J6 and CD-1) exhibited an increased body weight and alterations in the gut microbiome composition [585-587]. When chlorpyrifos was administered to male Wistar rats at various ages (2mo,10mo, and 20mo) for 45 days, the older animals were more sensitive to the metabolic effects [588]. Developmental exposure to chlorpyrifos from (gestational day (GD)7 to PND 21) resulted in weight gain only in males in adulthood with a non-monotonic dose–response [589]. These laboratory data using different animal models indicate that chlorpyrifos is an obesogen and may act via alterations in the gut microbiome and food intake.
4.14.2. Neonicotinoids
The neonicotinoid insecticide imidacloprid induces 3T3L-1 preadipocytes to differentiate into adipocytes [590]. In addition, in an adult mouse (C57B1/6J) model, the effects of a HFD-induced weight gain and adiposity were enhanced by imidacloprid exposure for 12 weeks [591,592]. Gestational exposure to imidacloprid induced hyperglycemia, insulin resistance and dyslipidemia in female offspring; however, the body or adipose tissue weight was not examined [593].
4.14.3. Permethrin
Permethrin is a pyrethroid insecticide. Exposure of adult C57B1/6J mice to permethrin at 50, 500, and 5000 μg/kg/day resulted in increased body weight, fat mass and insulin resistance but only on a HFD [594]. Permethrin also increased adipogenesis in an in vitro model and changes in intracellular calcium levels [595,596].
4.14.4. Tolylfluanid
TF is a phenylsulfamide used as a fungicide in agriculture and as a booster biocide in marine paints. TF has been shown to promote adipogenesis in the 3T3-L1 cell line, presumably through the activation of GR signaling [87]. Primary murine and human adipose tissue exposed to TF ex vivo exhibited insulin resistance arising from a specific down-regulation of insulin receptor substrate-1 mediated by activation of GR signaling [597]. In male C57BL/6 mice exposed to TF via their diet for 12 weeks below the observed no adverse effect levels, the fungicide increased weight gain and fat mass while inducing insulin resistance, glucose intolerance, and disrupting circadian rhythms. WAT from these mice showed an increase in GR-dependent gene expression [141]. Another adult study using a transgenic mouse model and the same concentration of TF as the developmental study above did not show any weight gain in the offspring [598]]. Intriguingly, the effects of TF may depend on the macronutrient content of the diet, with the fungicide promoting visceral WAT accumulation when adult mice were fed a high sucrose diet but not a HFD [599].
Developmental exposure to TF, at a dose of 67 mg/kg/day via the diet, similar to the dose used in the adult study [141], resulted in lower birth weight, reduced weaning weight and reduced adiposity in adult female offspring with no change in males [600]. It is likely that the dose given during pregnancy, while the same as given to adults, was too high and thus was toxic to the developing fetus. No epidemiological studies are available to ascertain the effects of TF in humans; however, these data indicate that TF is an obesogen.
4.15. Western diet
The Western diet, characterized by nutrient-poor, ultra-processed foods (containing additives, colorants, and fructose), high fat, low fiber and high in refined carbohydrates and sugar, is strongly associated with obesity and related metabolic diseases [601]. Ultra-processed food consumption correlates with BMI in the US and many European countries [602]. The Western diet can induce obesity by compromising pancreatic β-cell function, increasing FFA in blood and creating insulin resistance [603]. The Western diet can alter the microbiome and stimulate gut-induced inflammation, leading to altered metabolism and obesity [601]. Processed foods also contain many chemicals that have not been tested for their obesogenic effects, including some known obesogens like BPA and phthalates, pesticides, and fructose [604]. Adult mice fed a HFD for six weeks gained weight. When they were changed to standard chow, they showed anxiety and enhanced motivation for sucrose and high-fat foods suggesting that the diet had stimulated the food addiction parts of their brains [605]. A diet high in saturated fat and low in fruits and vegetables can select against a gut microbiome associated with lean body mass. It was proposed that excess consumption of the Western diet sustains increased levels of KYN. A low-fat diet containing KYN induced AhR activity in mice, causing weight gain, fatty liver, and hyperglycemia [508,606]. In addition to its nutritional deficiencies, the Western diet is also obesogenic because it contains numerous actual obesogens, including pesticides on fruits and vegetables and BPA, phthalates and PFAS from packaging. Preservatives, emulsifiers, and additives found in processed foods that could be contributing to the obesogenic properties of the Western diet are described below.
4.15.1. Fructose
Added sugars or sugar-sweetened beverages are associated with insulin resistance, NAFLD, visceral obesity, and metabolic syndrome, reviewed in [607]. Sucrose is composed of equal parts glucose and fructose. However, the obesogenic effects of sugar are primarily driven by fructose and not glucose [608]. Fructose is metabolized mainly in the liver and is a mediator of NAFLD [609]. Fructose excess overwhelms the capacity of hepatic mitochondria, and the excess is converted into liver fat, driving insulin resistance [610]. Fructose does not shut off the hunger hormone ghrelin, so the brain does not respond appropriately to satiety signals [602,611]. Fructose is also addictive. Fructose, especially consumed during development and early childhood, causes weight gain [612]; thus, fructose can be characterized as an obesogen.
4.15.2. Methyl and butylparaben
Parabens are widely used as preservatives in foods, personal care products and cosmetics due to their antimicrobial and antifungal properties and are found in urine samples of the general population [613]. Parabens promoted adipogenesis in 3T3-L1 cells [614] and MSCs [615]. Exposure of mice to butylparaben (BP) in the range of human exposure levels, in utero and during breastfeeding, resulted in increased body weight, higher fat mass, lowered lean mass, and increased adipocyte size in female but not male offspring. Increased weight correlated with increased weekly feed intake, low levels of POMC RNA, and down-regulation of the leptin receptor. This suggested an effect on adipocytes and the brain satiety center resulting in increased food intake [616]. Rats exposed to BP from birth to adulthood exhibited changes in gut microbiota during adolescence, but the effect was lost in adulthood [617]. A birth cohort study indicated that BP exposure led to overweight in early childhood [616]. These in vitro, animal and epidemiology studies show that parabens are obesogens.
4.15.3. Tween 80®/Carboxymethylcellulose
The food additives (emulsifying agents) Tween 80® and carboxymethylcellulose (CMC) are likely obesogens due to their effects on the microbiome. Exposure of adult mice to CMC or Tween 80® (1%) for 12 weeks led to increased body weight and fat pad weight, increased food intake, increased fasting blood glucose, low-grade inflammation, and altered microbiota. Indeed, an altered microbiota is necessary and sufficient for the emulsifier-induced metabolic effects, as indicated by germ-free mice and fecal transplants [618]. These data should be expanded and repeated because of the ubiquitous nature of human exposures to these compounds.
4.15.4. 3-tert-butyl-4-hydroxyanisole
3-tert-butyl-4-hydroxyanisole (3-BHA) is widely used as an antioxidant in foods. 18-week exposure of adult mice to 3-BHA resulted in a non-monotonic increase in weight gain, increased fat pad weight, lipid accumulation via transcriptional regulation of adipogenesis, and lipid metabolism [619]. 3-BHA also stimulated adipogenesis 3T3-L1 preadipocytes by regulating upstream events of the PPARγ signaling pathway [620].
4.15.5. Monosodium glutamate
Monosodium glutamate (MSG) is a flavor enhancer used worldwide. Multiple animal studies provided causal and mechanistic evidence that parenteral MSG intake caused increased abdominal fat, dyslipidemia, total body weight gain, hyperphagia and T2D by affecting the hypothalamic feeding center [622-623]. MSG increased glucagon-like peptide-1 (GLP-1) secretion from the pGIP/neo: STC-1 cell line indicating a possible action on the gastrointestinal (GI) tract in addition to its effects on the brain [625]. It is challenging to show similar results in humans because there is no control population due to the ubiquitous presence of MSG in foods. MSG is an obesogen.
4.15.6. Dioctyl sodium sulfosuccinate
Dioctyl sodium sulfosuccinate (DOSS) is a food emulsifier and stool softener that is a putative obesogen due to its ability to induce adipogenesis in the 3T3-L1 preadipocyte model and activate PPARγ [626]. DOSS was administered orally during pregnancy in a rodent model; the adult male (but not female) offspring had increased body mass, visceral fat mass, decreased plasma adiponectin, glucose intolerance, increased leptin, and inflammatory response [627]. These findings indicate that DOSS should be examined for obesogenic properties in humans due to its ubiquitous presence in processed foods.
4.16. Cadmium
Cd is a metal that activates estrogen signaling pathways [628]. Cd actions on metabolism have been reviewed [629,630]. Exposure occurs through dietary sources, smoking, and air pollution. Cd has a long half-life reaching 45 years in humans [631]. Developmental exposure of mice to a concentration equivalent to the geometric mean for Cd levels in US women resulted in weight gain only in females starting after puberty [632]. Female offspring also had increased perigonadal fat pad weight at 90 and 120 days and increased total triglycerides, glucose intolerance, insulin resistance, and hepatic steatosis with no change in food intake. Cd also impaired glucose metabolism leading to increased lipolysis and insulin resistance in rodents and humans, reviewed in [633].
Cd did not stimulate 3T3-L1 differentiation [634], suggesting it does not act directly on adipocytes. Cd exposure during pregnancy in humans led to an increased risk of obesity in the offspring, which was recapitulated in a zebrafish model [188]. Another cohort study of 470 participants found that maternal urinary Cd concentrations during the first and third trimesters of pregnancy were not associated with child BMI z-scores at age 7 years [253]. An exploratory study on 111 pregnant Arab-Bedouin women did not find an association of urinary Cd concentrations with obesity onset two years or six years after exposure assessment [635]. A study in an adult cohort from Southern Spain showed an inverse cross-sectional association of adipose tissue Cd concentrations with obesity [636]. More studies are needed to clarify the role of Cd in obesity.
4.17. Arsenic
Arsenic is a contaminant in drinking water for millions of people worldwide. It is a known carcinogen and diabetogen [637]. Exposure of 3T3-L1 preadipocytes to inorganic arsenic (iAS) decreased adipogenesis which correlated with upregulation of CHOP10 and inhibition of C/EBP transcriptional activity [638]. iAS inhibited PPARγ and C/EBP expression [639]. Exposure of pregnant CD-1 mice to iAS (sodium arsenite) at the US Environmental Protection Agency (EPA) drinking water standard of 10 ppb resulted in increased body weight, body fat content, glucose intolerance and increased levels of leptin and insulin in females [640] and male offspring [641]. Adult male C57BL/6J mice given 50 mg/L via drinking water did not gain weight but improved insulin resistance on an HFD [642]. iAS suppressed HFD-induced obesity in young C57BL/6 mice and produced glucose intolerance [643]. These differences are likely the result of using outbred (CD-1) vs. inbred (C57Bl/6) mice that differed in arsenic sensitivity. Urinary arsenic is negatively associated with BMI in a cross-sectional study of adolescents in Taiwan [644]. While the results from the two separate CD-1 mice experiments indicate that iAS can be an obesogen, mechanistic data are lacking, and the relationship between iAS and obesity requires further study [645].
4.18. A mixture of unconventional oil and gas industry chemicals
A mixture of 23 commonly used unconventional oil and gas industry chemicals and water samples stimulated adipogenesis in 3T3-L1 preadipocytes via PPARγ-dependent and independent mechanisms [646]. Similarly, organic chemicals extracted from oil sands process water stimulated lipid accumulation in 3T3-L1 cells, and several compounds were isolated and shown to bind to PPARγ [647]. Gestational exposure to this mixture at realistic environmental concentrations increased body weights in male and female mouse pups through early adulthood [648,649]. A subsequent study reported altered energy expenditure, reduced activity, and reduced ability to respond to a high fat, high sugar diet challenge following gestational and lactational exposure to this same mixture [649].
4.19. Potential obesogens
We classify chemicals as potential obesogens if there are only in vitro data or a single unsubstantiated in vivo study. Recent reviews provided a list of over 50 chemicals that induced adipocyte differentiation in in vitro assays, thereby providing evidence of their potential as obesogens [17,448]. The following chemicals are considered potential obesogens.
4.19.1. Glyphosate
Glyphosate is the most used herbicide globally, focusing on corn, soy and canola [650]. Glyphosate was negative in 3T3-L1 adipogenic assays [651,652]. Interestingly, three different formulations of commercial glyphosate, in addition to glyphosate itself, inhibited adipocyte proliferation and differentiation from 3T3-L1 cells [652]. There are also no animal studies focusing on developmental exposure and weight gain in the offspring. An intriguing study exposed pregnant rats to 25 mg/kg/day during days 8–14 of gestation [653]. The offspring were then bred within the lineage to generate F2 offspring and bread to generate the F3 progeny. About 40% of the males and females of the F2 and F3 had abdominal obesity and increased adipocyte size revealing transgenerational inheritance. Interestingly, the F1 offspring did not show these effects. These results need verification before glyphosate can be designated as an obesogen.
4.19.2. Diazinon
Diazinon is a widely used organophosphate insecticide. It was banned for residential use in the USA in 2004 but is still detectable in workers and fruits and vegetables [654]. Diazinon (1–100 μM) caused the induction and differentiation of adipogenesis and induced expression of PPARγ and adiponectin in the 3T3-L1 preadipocyte cell line [655]. Diazinon is thus a potential obesogen.
4.19.3. Endrin
Endrin, a chlorinated insecticide, induces adipocyte lipid accumulation in 3T3-L1 preadipocytes via the GR signaling activity [87].
4.19.4. Strobilurin pesticides
The strobilurin pesticides pyraclostrobin, azoxystrobin, fluoxastrobin, and trifloxystrobin promoted triglyceride accumulation and preadipocyte proliferation in 3T3-L1 cells. A follow-up study on pyraclostrobin described differentiation-independent triglyceride accumulation through a presumed mitochondrial dysfunction mechanism [656].
4.19.5. House dust extracts
House dust extracts contain many chemicals identified as EDCs, including phthalates, PFAS and flame-retardants [657]. Approximately 90% of indoor house dust extracts collected from separate human cohorts in central North Carolina promoted significant triglyceride accumulation and/or proliferation in 3T3-L1 cells, indicating obesogenic activity from the chemicals in the dust [656]. Mechanistic assessments suggested that the adipogenic activities of house dust are not correlated with PPARγ agonism and that activity is instead mediated, at least in part, through TRβ antagonism [658].
4.19.6. Alkylphenols and alcohols
Alkylphenols and alcohols are used to produce non-ionic ethoxylated surfactants found in emulsifiers, household cleaners and other consumer products [659]. Alkylphenols, alcohols, and ethoxylates at concentrations from 0.1 to 10 μM promoted adipocyte differentiation and triglyceride accumulation in murine 3T3-L1 cells and two separate human mesenchymal stem cells (hMSC) lines. This adipogenic effect depended on the ethoxylate chain lengths, with the medium-chain ethoxylates having the more significant impact in all three models [660]. These effects appeared to occur through a PPARγ-independent mechanism. Recent research demonstrated obesogenic effects of nonylphenol and its ethoxylates in developmentally exposed zebrafish, with exposed zebrafish exhibiting increased body weights and adiposity relative to controls [661]. Another widely-used surfactant, 4-hexylphenol, promoted adipocyte differentiation and lipid accumulation in 3T3-L1 cells and stimulated oleic acid uptake in HepG2 liver cells [662].
4.19.7. Bisphenol A diglycidyl ether and BPA glucuronide
Bisphenol A diglycidyl ether (BADGE) is used to manufacture epoxy resins, paint, and the coating of food containers. It migrates from containers into the products and is thereby ingested [663]. It does not break down into BPA and thus is not a source of BPA. BADGE-induced adipogenesis in hMSCs and 3T3-L1 preadipocytes [664].
BPA-glucuronide is the primary metabolite of BPA and is considered biologically inactive. However, 3T3-L1 cells and primary human preadipocytes treated with BPA-glucuronide exhibit increased lipid accumulation, adipogenic gene and protein expression. These effects appeared to be mediated at least in part through ER signaling [665].
4.19.8. Triclosan
Triclosan is an antimicrobial used in household and personal care products [666]. Triclosan exposure to zebrafish induced NAFLD and hepatic inflammation [125]. Exposure of mice to triclosan and HFD resulted in a dysfunctional microbiome with lower Bacteriodetes and higher Firmicutes, like that found in NASH patients [128]. A meta-analysis of seven birth cohort studies that measured maternal triclosan did not find effects on neonatal birth weight [667]. Childhood triclosan exposure did not affect BMI [655] in three studies. An NHANES cross-sectional human study showed an association between triclosan exposure and BMI [668]. Another cross-sectional study showed triclosan and triclocarban were associated with an increased risk of childhood obesity [669]. Thus, the data are inconclusive; therefore, triclosan can only be classified as a potential obesogen.
4.19.9. Triflumizole
Triflumizole, an imidazole fungicide, induces adipogenesis in 3T3-L1 cells and human MSCs and increases adipose tissue weight after prenatal exposure in a mouse model [670]. It is a known PPARγ activator which provides a possible mechanism for its obesogen activity [670].
4.20. Atrazine
Atrazine is a triazine herbicide. Chronic administration of atrazine in an adult rat model resulted in decreased basal metabolic rate, increased body weight and insulin resistance: a HFD exacerbated the insulin resistance and obesity [671].
5. Obesogens and human obesity
The sections above summarized data supporting the role of obesogens in the development and maintenance of obesity. Animal studies demonstrated causal relationships between obesogen exposures and WAT gain, and in vitro studies have revealed some causal mechanisms. Prospective epidemiological studies showing similar results substantiate a causal link between obesogen exposure and human obesity. Human and animal studies also showed that in utero and early life exposures were the most sensitive times for exposure because this irreversibly altered programming of various parts of the metabolic system, increasing susceptibility for weight gain. The developmental effects of some obesogen exposures persist across generations. Adult obesogen exposure can cause weight gain. This section integrates the above data to present a more cohesive picture of obesogen actions and effects. Fig. 6 presents an overview of the sites and mechanisms known for obesogens. We highlight examples of how data on sites and mechanisms of obesogen actions in animal studies mimic aspects of the etiology of obesity in humans, which were described in the companion review, Obesity I. Some data presented above are repeated in this section to integrate and highlight the effects of obesogens on specific human pathways.
Fig. 6. Composite of sites and mechanisms of obesogens.
Obesogens, as described in the text, can act via a variety of mechanisms and act on a variety of tissues. Some mechanisms are direct, such as receptor mechanisms and epigenetic changes and some, such as sirtuins, oxidative stress, inflammation, circadian rhythms, alterations in food intake and food addiction, and increase in number and size of fat cells, can result from the initial mechanisms. Obesogens have both direct and indirect actions on several tissues like liver, pancreas, muscle, gut microbiome, and brain. Thus, obesogens can disrupt all the sites and tissues known to be involved in control of metabolism.
Humans maintain their weight for long periods despite changes in their diet. The ability to maintain weight results from a bodyweight setpoint, a physiological value around which normal weight fluctuates. Humans have a hard time losing weight, and it is difficult to maintain weight loss. Obese people have only a 15% annual chance of losing 5% of their total weight without surgery, and 83–87% of those who successfully lose large amounts of weight regain it within a few years [672,673]. It is harder to maintain a normal weight today than 30 years ago [674]. The reasons for this change over recent decades are multifactorial, but developmental programming of metabolism resulting in an altered setpoint for weight maintenance is probably responsible. The actions of TBT mimic this human situation. Offspring of pregnant mice given TBT in utero had increased fat later in life. Four generations after the TBT exposure, male mice were resistant to fat loss compared with controls, and these animals were extremely sensitive to a HFD [44]. HFD led to rapid weight gain in the TBT animals compared to controls, and when dietary fat content was reduced, the TBT group males lost less weight than controls. Thus, TBT exposure paralleled the human situation where it is easier to gain weight on a HFD and harder to lose that weight.
Obese individuals prefer high fat and high sugar foods, have a higher desire and anticipation for food, will work harder for food, tend to be emotional eaters with increased eating in response to anxiety, depression and mood swings and get a greater reward from food intake than non-obese individuals [675]. Developmental exposures to BPA can influence the dopaminergic reward system and the impulsivity network of the cortex [166]. BPA exposure in children was associated with hyperactivity and ADHD [167], which involve the same neurological circuits [171]. Serum concentrations of BADGE.2H(2)0 were positively associated with the incidence of binge eating disorder in a cross-sectional study of obese patients [168].
Several examples of effects of obesogens in rodents that mimic the human situation are shown in (Fig. 5).
Fig. 5. Multiple actions of obesogens.
Obesogens in addition to increasing the number and size of adipocytes also affect other tissues and process. Several of the main effects of obesogens are shown here. These are not all of the tissues and processes affected but show the broad effects of obesogenic chemicals. The chemicals shown have been reported to have that effect but that does not mean that other chemicals may not also have those effects. For example, the three chemicals shown are the only ones that have been examined for their effects on pathways and genes in adipocytes. It may be that other obesogens will also stimulate the production of dysfunctional adipocytes. Colors are only to highlight the same chemical across multiple mechanisms.
Food intake is controlled by appetite and satiety neurons in the brain. Developmental exposure to BPA resulted in weight gain due to increased food intake in some animal models along with changes in the appetite and satiety neurons in the brain: a reduction in the number of satiety neurons and an increase in the appetite neurons. BPA-exposed mice were insensitive to leptin’s effects on POMC expression exhibited reduced POMC innervation of the PVN compared to controls. This was rescued in females by postnatal administration of leptin [244]. BPA-exposed males and females were resistant to the effects of post-leptin injection on body weight [244]. Examination of the mechanism for increased food intake after exposure to DEHP in adult mice revealed an increase in NPY and AgRP genes and a decreased expression of POMC, key genes involved in regulating food intake and body weight [285]. Male adult rats exposed to TBT for 54 days exhibited increased body weight and fat mass with depressed brain POMC, AgRP and CART mRNA levels. Females had increased food intake, which was correlated with increased NPY, indicating specific actions on controlling feeding behavior [386]. OPFR exposures also altered brain controls of feeding behavior [427]. These results are directly applicable to the human situation of overeating.
Overeating with a focus on the role of HFD is often noted as a cause of obesity. Imidacloprid is a neonicotinoid pesticide that promotes HFD induced obesity [591]. HFD caused weight gain in a mouse model of prenatal nicotine exposure [198], an adult model of chlorpyrifos exposure [585], developmental exposure to permethrin [594], atrazine [676], DDT [460], and BBP [263].
Epidemiology and animal studies found that exposure to obesogens during development can result in early weight gain that persists throughout life. In some cases, weight gain did not occur until puberty or later in life. Developmental exposure to the synthetic estrogen DES caused weight gain in mice, but not until after the animal received a second hit - increased estrogen exposure at puberty. Developmental exposure to DES reprogrammed the estrogen pathways, sensitizing the animals to estrogens. At puberty, adipocytes with estrogen receptors increased fat uptake, leading to obesity in the adult mouse. These animals weighed up to 90 g compared to 30 g for controls [672].
Reduced exercise is often highlighted as a mechanism for weight gain, which is mimicked in animals. Exposure to either BPA or nicotine caused reduced activity and diminished energy expenditure. Mice exposed to BPA in utero slept more, moved less, walked more slowly, and expended less energy [677]. Similarly, developmental exposure to DDT decreased energy expenditure by lowering core body temperature and oxygen consumption [460]. HFD exaggerated these DDT effects.
Obesity in humans is sexually dimorphic, being more prevalent in females resulting at least partially from sensitivity to estrogens [678]. Obesogen action can also be sexually dimorphic, as shown by TBT and chlorpyrifos, which cause obesity only in males and DDT and Cd, which cause obesity only in females.
Obesogens can target the gut microbiome directly [133,134], and obesogen exposures have been shown to affect the gut microbiota composition leading to obesity. These include heavy metals, air pollution, nanoparticles and numerous known obesogens: BPS (and to some extent other bisphenols), natural estrogens, phthalates, individual PCB congeners and their mixtures PAHs, PFAS, brominated flame retardants, pesticides, TCCD and dibenzofurans [133,134].
Obesity is often associated with higher insulin levels and resistance [679]. Exposure to BPA, DEHP, PM2.5, PFOS, atrazine, Cd, permethrin and the Western diet are associated with insulin resistance.
Many obese individuals have impaired leptin signaling, leading to resistance [680]. Exposure to BPA, PM2.5, some OPFRs, PFOA, chlorpyrifos, Cd, and BP can lead to altered leptin signaling.
A key human study linked obesogen exposure and weight gain. A two-year randomized clinical trial that compared four diets showed that individuals lost about the same weight on any of the diets in the first six months and gained back about the same amount of weight over the ensuing 18 months. Critically, levels of PFAS were measured in the participants. Subjects with the highest levels of PFAS regained more weight than those with the lowest PFAS levels. This effect was associated with decreased resting metabolic rate during weight loss and reduced increase during weight gain [544] and provided further human support for the obesogen hypothesis.
There are two main areas where there are animal data but a lack of human data. Animal studies showed that DDT, TBT, BPA and a mixture of BPA and phthalates elicit transgenerational epigenetic inheritance. Recent results from a long-running human epidemiology study linked a grandmother’s DDT exposure during pregnancy to an increased incidence of obesity in the young adult granddaughters [484], indicating that obesogens can cause multigenerational effects in humans.
In all studies where adipocytes were examined in detail, BPA, TBT, phthalates and TPhP induced dysfunctional adipocytes, which could increase other metabolic diseases if this occurred in humans. There are no data in humans examining the functionality of adipocytes in normal vs. obese individuals.
6. Intervention and prevention strategies
Mitigation of the impact of obesogens on obesity risk and complications due to the diversity of chemicals linked to disease development will require a variety of approaches [681]. These approaches include interventions to reduce exposures, antagonizing the adverse effects of obesogens, facilitating obesogen excretion, and eliminating stressors that amplify obesogen-mediated metabolic disruption. Central to these efforts it is necessary to identify chemicals that promote obesity then reduce their exposure. We must develop and deploy new public policies to address metabolic threats posed by obesogens [682].
It is crucial to develop in vitro and in silico test systems that reliably predict obesogen action in vivo. Identifying key characteristics of obesogens coupled with the development of sophisticated new testing methods can aid in developing tiered testing frameworks that can validate integrated approaches to testing and assessment (IATA). While essential, these identification methodologies are insufficient without in vivo and human cohort follow-up followed by regulatory action. Obesity is a significant risk factor for various critical diseases that impose substantial morbidity and mortality, including cancer, musculoskeletal disorders, metabolic dysfunctions, and cardiovascular diseases, which collectively justify such a classification. Therefore, the identification and classification of obesogens as substances of great concern should be considered by regulatory agencies. To date, the European Chemicals Agency (ECHA) considers carcinogenic, mutagens, and reprotoxic agents as of very high concern, along with very persistent substances. EDCs were included (https://www.echa.europa.eu/candidate-list-table) and, based on this review, obesogens should be considered a separate category.
Reducing exposures to obesogens is fundamental to any successful intervention effort. Exposure reduction strategies must be large-scale and involve regulatory action to identify and eliminate toxicants that increase the population-level metabolic disease risk. Behavioral modification informed by knowledge of obesogenic chemicals and the sources of exposures, as well as individual efforts to minimize engagement can reduce their obesogen levels. Short-term intervention studies showed that lowering known sources of common obesogen successfully reduced levels of BPA, phthalates, parabens, and triclosan [683,684]. Individual reduction of obesogen levels is predicated on knowledge of the sources of that exposure and an absence of unexpected exposures arising from contamination [685]. While individual action is essential, it may be insufficient to improve population-level health. Regulatory action, including product labeling, will be needed to reduce societal risk.
Where the mechanism of metabolic toxicity is known for an obesogen, interventions could be targeted to address that specific pathway to mitigate the consequences of exposure. For example, animal studies showed that the antioxidant N-acetylcysteine may attenuate arsenicand PCB-induced metabolic dysfunction [686,687]. As we learn more about mechanisms of obesogen action, the feasibility of tailoring interventions to these pathways will improve. However, a persistent challenge to overcome is that most individuals are exposed to multiple toxicants with metabolism-disrupting capacity that may operate through various mechanisms that may themselves interact in unpredictable ways.
Interventions to facilitate the active elimination of obesogens or inhibit their effects may be beneficial for reducing their health impacts. The role of nutrition in reducing the toxicity of chemical exposures was reviewed [688], as was the use of antioxidants to counteract inflammation caused by PCBs [689] and antioxidants in reducing BPA toxicity [690]. Others reviewed the role of polyphenols against the effects of numerous EDCs [691].
A randomized controlled trial found that vitamin C supplementation (1000 mg/day for two months) reduced PCB and DDT/DDE (but not PBDE) levels in California women [692]. The diuretic hydrochlorothiazide and the sodium-glucose co-transporter-2 inhibitor dapagliflozin increased the excretion of urinary phthalate metabolites [693].
In rodents, several substances were protective against the various metabolic effects of BPA and other EDCs. For example, grape seed extract, resveratrol, or vitamin E reversed some BPA-induced increases in blood pressure, total cholesterol, LDL cholesterol, body fat, leptin, adiponectin, insulin, and glycemia in rats [694]. Nigella sativa oil and thymoquinone helped reduce many of the metabolic disruptions caused by BPA in rats [695], as did lycopene [696] and Korean red ginseng in mice [697]. Curcumin inhibited adipogenesis induced by BBP in 3T3-L1 cells [698], and the food supplement Potentilla rugulosa Nakai extract suppressed the BPA-, BPS-, and BPF-mediated induction of adipogenesis in 3T3-L1 cells [699]. The flavonoid icariin alleviated BPA-induced disrupted intestinal barrier function in mice [700]. Probiotics almost eliminated the metabolic toxicity of a mixture of phthalates and BPA in rats [701].
Crocin, a component of saffron, is protective against BPA-induced liver toxicity in rats [702]. Melatonin partly counteracted the metabolic changes to rat liver caused by fructose and BPA (separately and together) [703]. The herbal medicine Asparagus officinalis extract protected against kidney and liver damage induced by BPA in rats [704]. In liver cells, curcumin reduced the effects of BPA-triggered insulin resistance [705]. Some substances are also protective against the effects of BPA during development. Magnesium lithospermate B, an active compound of danshen/red sage, protected rat offspring against metabolic effects of BPA in utero [706].
Case studies and small human trials showed potential utility for the non-absorbable fat olestra [707], the bile acid sequestrant cholestyramine [708], and fermented brown rice [709]. Olestra was successfully used to increase POP elimination in people exposed to high levels of POPs [707,710]. Human and animal studies suggest a potential benefit of dietary fiber, particularly fermentable fibers [711]. Approaches focused on interrupting the enterohepatic circulation of persistent obesogens may be productive when coupled with weight loss, which liberates these toxicants from fat.
The adverse metabolic effects of some obesogens can be amplified or unmasked by deleterious diets, such as high fat and Western diets. Healthier diets may mitigate the metabolic impacts of obesogens. However, more studies are required to demonstrate mitigating effects of healthful diets on obesogen-induced metabolic disruption, including the potential ameliorating effects of diets known to confer metabolic benefits such as the “Mediterranean Diet.” Specific dietary components may protect against obesogen-induced dysfunctions, such as sulforaphane from Brassica vegetables and resveratrol. Ensuring adequate intake and avoiding micronutrient deficiencies that inhibit obesogen absorption/action or amplify obesogen effects, respectively, are also critical [681]. Indeed, resveratrol butyrate esters reduced weight gain, lipid accumulation, increased leptin levels, and the harmful effects on the microbiome resulting from developmental exposure to BPA in female rats [712].
Human intervention trials aimed to examine the effects of environmental chemical exposures on metabolism are needed. For example, in a crossover experiment, researchers gave low, “presumed safe” levels of BPA to adult men and non-pregnant women, and their glucose-stimulated insulin response was affected [713]. In a randomized, double-blind crossover study, college students dosed with BPA had immediate changes in insulin, glucose, and c-peptide (a marker of β cell function) levels [714]. In a randomized crossover trial, elderly adults who consumed two beverages from cans containing BPA had significantly higher systolic blood pressure two hours later than when they drank beverages out of glass [715]; these changes were linked to epigenetic effects [716].
There have been human intervention trials on air pollution. Twenty-five healthy adults living in rural Michigan were moved to an urban location for 4–5 h over five days. Higher PM2.5 exposures were associated with increased insulin resistance [305]. In a blinded crossover study, ozone exposure during exercise increased stress hormone levels and affected lipid metabolism [717]. A randomized, double-blind crossover trial exposed healthy college students to either filtered or unfiltered, “normal” air in dorm rooms in Shanghai, China. Within nine days of exposure, significant differences were observed in insulin resistance, glucose levels, lipids, blood pressure, and fatty acids, among other metabolic markers [718].
A cluster-randomized 40-day organic diet crossover trial reduced children’s body burden levels of pesticides, reduced BMI, and lowered oxidative stress and inflammation markers. Since caloric intake was also lower during the organic diet, this association may not be due to the organic diet but to calorie intake [719]. This important area of new research needs to be expanded because it can provide the evidence necessary for both acceptance and counteracting the action of obesogens.
Interventions using drugs or diets should be cautiously evaluated to balance potential benefits with possible risks related to the drugs or the diets. If the dietary intervention has already been shown to have other metabolic benefits, the positive preventive effects on obesogens will constitute an additional benefit. If drugs display toxicity, the advantages and risks should be cautiously weighed.
7. Future directions
7.1. General needs for the obesogen field (BOX 1)
Box 1. General Recommendations for the Obesogen Field.
Develop a low cost readily available personal biomonitoring kit to assess exposures to EDCs.
Update guideline-based testing protocols.
Improve messaging to public and physicians.
Improve coordination between researchers using model systems (in vitro, animal, and computational) and human researchers.
Improve communication and coordination between obesogen researchers and basic scientists and clinicians.
Work with national and international organizations to assess evidence for specific chemicals as obesogens and develop lists of obesogenic chemicals.
Change the narrative to a focus on prevention rather than treatment.
This section describes points that must be improved in vitro, in vivo and epidemiological studies commonly used in obesogen fields, the new methods necessary, and which data are needed to move the field of obesogens and obesity forward. It implies the necessity to have validated testing methods to identify missing obesogens.
A low-cost, easy-to-use (e.g., $100) personal biomonitoring kit that can measure many EDCs and obesogens with interpretable results would be valuable for consumers and clinicians. Empowering people with the knowledge of which chemicals they have in their bodies that could be causing or contributing to diseases could influence their behavior stimulating action by clinicians and policymakers to reduce exposures. It could also promote measures to reduce exposures at a personal and family level. It is critical to expedite studies on the interpretation of these biomonitoring levels by defining robust guidance values based on solid human and experimental work.
The obesogen field suffers from poor communication to the community about the importance of reducing exposures to obesogens. There also needs to be improved coordination and collaboration between animal and human researchers, particularly among obesogen researchers and basic and clinical researchers working on obesity and metabolic disorders. Improved cooperation could break down scientific silos and lead to joint research projects that could answer questions about the role of obesogens in the obesity pandemic.
Finally, although it should be self-evident, prevention is the best way to reduce or eliminate the obesity pandemic. Prevention saves lives and money while costing far less than any drug therapy or surgical intervention.
7.2. In vitro, animal models: Data gaps/needs (BOX 2)
Box 2. In Vitro, Animal Model Recommendations.
Use human in vitro cells to define both commitment and differentiation into adipocytes.
Determine which obesogens stimulate the development of dysfunctional adipocytes.
Use human in vitro systems to assess insulin sensitivity and resistance.
Work towards 3D cultures and organ-on-chip technologies.
Use human models to investigate mechanisms of action of obesogens.
Measure different fat depots, liver, pancreas, brain, and GI as well as hormones, bioactive molecules, lipid levels, immune cells, and inflammation.
Assess epigenetic changes as biomarkers of exposure, effect, and prediction modeling.
Assess the interaction of obesogens with diet.
Assess the effects of obesogens on weight loss and fasting.
Assess the effects of human relevant chemical mixtures.
Assess the effects of exposures across multiple windows of sensitivity including transgenerational inheritance.
Assess exposures across the lifespan as well as during sensitive windows.
Many experiments in rats and mice focused on exposure to an environmental chemical in utero and examining obesity in their offspring over their lifespan. This makes sense because gestation and early childhood in humans is the most sensitive exposure window. However, preconception, puberty, menopause, and old age are also times when hormone levels are changing and where there may be increased sensitivity to environmental exposures. Adults are also responsive to obesogens, albeit usually at higher levels. Since the goal is to mimic the human situation in animal models, studies should focus on exposure during multiple windows, including before conception, in utero and adulthood and even from in utero and across the lifespan.
Animal models must include enough animals of both sexes from multiple strains to detect phenotypes and examine sex differences. At least 4–5 doses of chemical should be used to allow detection of non-monotonic dose responses. Levels of chemicals and metabolites should be measured in blood and urine. Tests should include concentrations in the range of human exposures or a broad range of doses if human exposures are not well-established. Toxicokinetic modeling should be employed to assess achieved doses in the target tissues. Many overlapping endpoints across the lifespan should be evaluated. In addition to body weight, critical endpoints include body composition (fat vs. lean), weights of individual fat depots to assess potential differential effects on subcutaneous or visceral type adipose tissues and gene expression assays of fat pads. Activity, feeding behavior, possible binge eating and addiction, the gut microbiome, liver fat and effects on all critical systems and tissues that control metabolism should be examined [15]. Examining the interaction between chemical exposures and diet, including high fat and high sugar diets, will help extrapolate the data to humans. It will be constructive to assess the effects of obesogen exposure on weight loss over time and weight loss during fasting. Since humans are exposed to mixtures of chemicals, it will be important to develop sensitive methods to evaluate the effects of mixtures, particularly mixtures of chemicals based on reported human levels.
Few studies explicitly studied feeding behaviors (size, duration, frequency), meal patterns (hourly/diurnal ingestive cycles), or hypothalamic-hindbrain circuits after perinatal obesogen exposure. Most studies focused on cumulative total food intake over a short (few days) or long-term (~6 months) period with a subsequent examination of the hypothalamic expression of neuropeptides involved in food intake. Additional data on how obesogens affect the feeding response to peripheral peptides (leptin, ghrelin, cholecystokinin, etc.) or fasting-induced refeeding are needed.
As testing increases, more putative obesogens will be found. Therefore, more testing should be a priority. A combination of in vitro assays and in silico screening that are curated to validate the results will be needed to prioritize chemicals for in vivo testing. It would be advantageous to develop key characteristics (KCs) of obesogens, similar to the KCs established for EDCs [6] and reproductive toxicants [720,721]. Updated guideline-based protocols with more relevant and sensitive endpoints to define which chemicals are obesogens are also needed. This would necessitate changes to the FDA and EPA guidelines for industry testing of chemicals, but such improved regulatory testing could keep harmful obesogens off the market. Since some obesogens and EDCs can act transgenerationally, testing protocols should account for and be sensitive to such effects. Chemicals should be administered to pregnant dams in each generation and across lifespans and generations to mimic the human situation to assess potentially cumulative transgenerational effects.
7.3. Human epidemiology: Data gaps/needs (BOX 3)
Box 3. Recommendations for the Epidemiology Field.
Improve the capacity for measuring chemicals exposures.
Standardize biomarker collection and exposure assessment techniques.
Continue to assess the health of offspring of birth cohort studies across the lifespan.
Assess the interaction of nutrition with obesogen exposures.
Assess multiple overlapping endpoints that match those measured in animal models.
Use birth cohorts to study the effects of developmental exposure on nutrition-induced weight gain and fasting and weight loss in children and adults.
Use prospective studies in adults to define the effects of earlier exposure on nutrition-induced weight gain and fasting and weight loss in adults.
Coordinate with clinicians and basic scientists to develop protocols to assess the obesogen hypothesis.
A key aspect of epidemiology studies is accurate exposure assessment. Many potential obesogens have short half-lives. Epidemiology studies pose a problem because single spot urine is inadequate for precise exposure assessment [722]. Since inadequate exposure assessment is probably the main reason for the inconsistency among epidemiology studies, improving it will be critical for moving the field forward. Developing protocols with repeated biospecimens is one way forward [259].
Another improvement in epidemiological studies on obesogens would be studying the effects of contaminant mixtures in mother–child dyad cohort studies and studies conducted in adult populations [723]. Few epidemiological studies investigated the obesogenic effects of mixtures from different chemical families. While a sample size of hundreds could be enough for single compounds, larger sample sizes are needed to assess mixture effects with sufficient power.
Multiple obesogen exposures studies face statistical and methodological challenges that need to be considered in future studies, as reviewed in [724-726]. Potential limitations are related to misclassification of exposures with high within-person variability (e.g., for the short half-life chemicals such as BPA), reverse causality due to pharmacokinetic factors (e.g., different routes of exposure affecting the rate of excretion), or inability of the biomarker to represent exposure during the relevant period. In addition to these challenges, consideration should be given to isolating the potential effects of one obesogen exposure from another when exposures are correlated due to common sources, and statistical challenges exist (such as missing data and exposure below the detection level). Future studies should examine interactions between obesogens based on common biological pathways related to obesity, rather than purely on statistical considerations [725].
Another challenge is to minimize the amount of blood needed for chemical analyses. It would be helpful to measure multiple obesogens in 225 μl of plasma, which is commonly available in modern biobanking of blood. Since very few epidemiological studies with thousands of subjects are initiated with the primary aim to study obesogens, it is essential to use existing biobanks in already established cohort studies. Improved standardization of sample collection, storage, and laboratory protocols will be helpful. Having access to biobanks and a single laboratory or a network of laboratories consistent in protocol and equipment for sample analyses will allow for greater comparability across studies on a global level. Such an approach was developed in the HBM4EU project [728].
Ectopic fat distribution inside the abdomen or in the liver is more harmful than subcutaneous adipose tissue; therefore, it is important to use objective, minimally invasive methods to measure the different fat depots in humans. We must not rely solely on BMI to measure obesity outcomes when more sophisticated evaluation of fat distribution and anthropometrics could be achieved by measuring waist diameter, CT scanning or magnetic resonance imaging (MRI). Since such imaging is expensive, it is crucial to partner with studies where such measurements have already been performed or are planned [467]. It is also essential to assess the interaction of chemical exposures with diets and the effects of sex and genetics.
Improved interactions, coordination and collaborations between epidemiologists and animal researchers will improve future progress. Controlled experimental studies with animals can show causal relationships and indicate sites, mechanisms, and endpoints to measure in epidemiological studies. Some of the same endpoints should be measured in human and animal studies. Developing a battery of overlapping endpoints (physiology, endocrinology, epigenetics, metabolomics) that can be assessed in animal and human studies is warranted. Many human studies focus on fasting and the effectiveness of various diets. These studies should include assessing obesogen exposures both in utero and in adulthood to associate obesogen exposures with susceptibility to gaining and losing weight and their effects on fasting weight loss.
If birth cohort studies could relate in utero exposures to offspring sensitivity to weight gain and problems with weight loss, such data could convince clinicians and regulators to assess exposures and reduce exposures to improve metabolic health.
Longitudinal, birth cohort studies need to focus on birth and early childhood, but it is imperative to follow the subjects into adulthood; lifelong studies are required.
Another issue in epidemiological studies is publication bias; studies with statistically significant results are more likely to be published than non-significant ones [729]. This problem might be solved by preregistration of protocols for observational studies (as is commonly done for clinical trials), facilitating incorporating all results into meta-analyses [730].
While all the above suggestions will help move the obesogen field forward, perhaps the greatest need is more birth cohort studies to assess the effects of developmental exposures on weight gain and loss. Many cohort studies showed that developmental exposure to a specific chemical was associated with weight gain in childhood through the teen years. Participants could be re-evaluated at their current ages, separated into low and high exposures in utero and then placed on controlled diets for a limited time. The question is whether the participants with the highest level of chemicals in utero gain or lose weight (particularly fat) differently from those with the lowest exposures? Participants could then be placed on a low-calorie regimen for two weeks, and weight loss/body composition measured to assess whether developmental obesogen exposure impacts weight/fat loss. It is unethical to deliberately treat humans with toxic chemicals; therefore, this approach could be the next best experimental design. Similar strategies could be developed for current exposures, singly and as mixtures.
8. Clinical implications and a path forward
Despite burgeoning knowledge regarding obesogens, translating these data into clinical practice is essentially non-existent. Addressing this knowledge gap among physicians and policymakers could bring novel tools and approaches to stem the tide of obesity. This is critical because the current clinical management of obese patients is woefully inadequate. Pharmacological management of obesity has improved with new medications and drug formulations. However, current treatments are often insufficient. As many as 55–65% of patients failed to achieve even 5% weight loss in clinical trials [723,724]. Although weight loss medications are underutilized in clinical care [731], the modest efficacy of currently available therapies suggests that pharmacological treatments will be insufficient to alleviate obesity. While metabolic surgery can be highly effective, the surgical and post-surgical risks of these procedures, together with their high cost and the scale of the obesity pandemic, make it clear that surgery cannot solve this significant health threat. The emergence of pediatric obesity with its attendant lifetime of adverse health effects further complicates clinical management because this population has few treatment options. Weight-loss interventions become less efficacious over time, leading to weight regain. This underscores the challenges of treating obesity using our current approaches [721] and indicates that new approaches are needed, including addressing all obesity risk factors including obesogenic chemicals in the environment.
Focusing on prevention is a timely and essential component of any public health approach to stopping the obesity pandemic. Over the last decade, evolution in medical thought has recognized the importance of the social (or structural) determinants of health - conditions in which people live their lives that affect health risks and outcomes. These include neighborhood and built environments but clinical guidelines considering “environments” often neglect chemical exposures [732]. This is beginning to change, and evidence presented in this and our companion reviews, Obesity I and III, indicates that such exposures should be explicitly considered. Appropriate interventions at the individual and policy levels should be developed to reduce exposures to obesogenic chemicals.
Recognizing and addressing environmental drivers of disease risk may be especially salient in combatting obesity. The predominant cultural belief that obesity is a personal failing runs directly counter to the tenets of the social determinants of health [733]. Internalizing these beliefs across society and healthcare systems results in poorer clinical outcomes [733]. Once medical practice appreciates the environmental drivers of obesity risk better, clinicians will be empowered to change the self-defeating personal responsibility narrative and focus on disrupting the obesity-promoting mechanisms discussed here. This can improve societal health while working in the best interests of individual patients.
It will be incumbent upon clinicians to counsel patients to reduce obesogenic threats to their lives and confront that medical care can lead to obesogen exposure [261]. Patients do not recognize the potential for medications and medical devices to be a source of obesogen and EDC exposure. Publications documenting the exposures of infants in neonatal intensive care units to BPA and phthalates from medical equipment have not led to changes in the design or use of medical equipment that releases these chemicals [734]. Clinicians must advocate for more knowledge and transparency about these hidden threats. Ethical obligations as healthcare providers require clinicians to act in the patient’s best interests by maximizing benefits, minimizing risks, and empowering patients to make informed decisions about their health. The cryptic nature of healthcare-associated EDC exposures violates these promises and must be addressed.
Meeting the needs of patients suffering from obesity requires a multipronged approach to treat those who are obese while preventing others from becoming obese. This undoubtedly includes attention to diet, physical activity, and underlying genetic risks. However, a successful approach should also address other factors that amplify obesity risk, including obesogenic environmental exposures. Various interventions can reduce and mitigate exposures for individual patients [681]. But physicians must also leave their exam rooms and advocate for public policy that eliminates exposure to obesogenic chemicals across society. Our failures to address the obesity pandemic are evident. New approaches that incorporate environmental health into clinical practice and public policy can improve this dismal performance by translating emerging science into improved health and well-being for everyone.
9. Conclusions
Genetic and environmental factors play roles in the obesity pandemic. Obesity is multifactorial; no known genetic or environmental factors alone can cause the global obesity pandemic. A persistent key question is what percent of obesity is due to genetics, stress, overnutrition, lack of exercise, viruses, drugs or obesogens? It is virtually impossible to answer that question for any contributing factors because they likely all work together with different effects depending on the balance of factors. Genetic background and overnutrition play a significant role; we can see the impact of high sugar and high fat and highly processed diets on obesity. However, it is difficult to determine the exact effects of obesogens on obesity because each chemical is different, people are different, and exposures vary regionally and globally. Importantly, exposures of interest may have occurred years, decades, or generations earlier.
What data support a role for obesogens in the obesity pandemic? Are the data sufficient to warrant a focus on reducing exposures to reduce the scope of obesity? In vitro data can indicate a chemical is a potential obesogen. Animal data can reveal causal relationships between exposure and later weight gain, increased adiposity, and obesity. In vitro and animal data also indicate which tissues, hormones and pathways are altered by obesogens. Birth cohort studies provide robust human data linking exposures during development to weight gain and obesity later in life. We cannot run actual “clinical trials” where exposure to obesogens and their effects are monitored over time. Thus, we focus on assessing the strength of the data for each obesogen. When there are multiple studies in vitro, in animals, and in humans, which exist for multiple obesogens, it must be concluded that a chemical is an obesogen that probably impacts human weight gain. We must inform the public, clinicians, and policymakers to reduce their exposures to these chemicals to improve individual health and reduce the societal burden of disease.
Like the classification of carcinogens, it will be helpful to identify different classes of obesogens for both research and regulatory purposes. This review puts forward two categories: obesogens and potential obesogens. We now propose to divide obesogens into Class 1 and Class 2 to aid researchers and regulatory agencies in determining the status of data and research needs. We describe these classes and suggest preventive actions in Table 2.
Table 2.
Categorization of obesogens according to data. Obesogens are divided into two classes, class I and II depending on the extent of data. These categories indicate the status of regulations and the need for further testing. Chemicals with only in vitro data are designated as potential obesogens.
| Obesogen | Obesogen | Potential Obesogens |
|
|---|---|---|---|
| Class 1 | Class 2 | ||
| Epidemiological evidence | Medium to strong | Weak or absent | absent |
| Animal evidence | Strong | Medium to strong | Usually absent |
| In vitro evidence | Strong | Strong | Medium to strong |
| In silico predictions | Not required | Helpful | May be present |
| Regulatory action | To be banned | To be Regulated | Suspect list |
| Research | As a model | Priority: human studies | Priority: experimental and human studies |
| examples | Smoking, (nicotine) |
TBT | BPS BPF, BPAF |
| BPA | Non-nutritive sweeteners | Glyphosate | |
| Air Pollution (PAH, PM2.5) | BBP | DiBP | |
| Fructose | Endrin | ||
| Phthalates (DEHP) | Chlorpyrifos | House Dust | |
| PBDE | Atrazine | Diazinon | |
| OPFRs (TPhP) | Neonicotinoids | Alkylphenols | |
| DDT | Permethrin | BADGE | |
| PFOA, PFOS | Methyl and butyl Paraben |
BPA Glucuronide | |
| PCBs | Tween 80® | Trifloxystrobin | |
| MSG | Carboxymethylcellulose | Praclostrobin | |
| 3-BHA | Azoxystrobin | ||
| TBBPA, TCBPA | Triclosan | ||
| Tolyfluanid | |||
| DOSS | |||
| Cadmium | |||
| Arsenic | |||
| DBT | |||
| βHCH | |||
| Triflumizole | |||
| TCDD, TCDF | |||
| Oil, gas | |||
| “fracking” mixture | |||
| PFAS | |||
| HCB | |||
| βBCH | |||
| TBBPA, TCBPA |
We propose that Class 1 obesogens with significant in vitro, animal model, and human data should be banned or exposure significantly reduced. Class 2 obesogens require further data, and we hope the discussion presented above will stimulate research to obtain the needed information. Potential obesogens need further testing as soon as possible to determine if they are obesogens and require regulatory action.
In summary, the focus in the obesity field has been to reduce obesity via medicines, surgery, or diets. These interventions have not been efficacious as most people fail to lose weight, and even those who successfully lose substantial amounts of weight regain it. A better approach would be to prevent obesity from occurring in the first place. BOX 4 summarizes our current thinking: An alternative hypothesis for obesity. A significant advantage of the obesogen hypothesis is that obesity results from an endocrine disorder and is thus amenable to a focus on prevention. To the extent that obesogens result in weight gain, reducing exposures should prevent that weight gain. We know that developmental windows (in utero and early childhood) are the most sensitive periods for obesogen action. This review provides a list of chemicals that can increase our susceptibility to overweight and obesity. We know how to reduce exposure to these chemicals. Improved biomonitoring can give “early warnings” that exposure has occurred even before the illness is noted, which can be used to develop prevention policies. Therefore, we know what to do and when to do it. What remains is to change the narrative and focus from just intervention to prevention.
Box 4. An Alternative Hypothesis for Obesity.
The conventional wisdom is that obesity is an energy balance disorder, caused merely by the consumption of more calories than are expended. By this logic, combating the obesity epidemic requires that obese and overweight individuals learn to eat less and exercise more, and that our environment changes to facilitate those specific behaviors.
This focus on dieting and increased exercise has not impacted the global obesity epidemic because it does not address the underlying cause of the increased eating and lack of exercise.
We propose an alternative hypothesis that focuses on the mechanism(s) responsible for the altered eating behavior. This alternative hypothesis states that obesity is a growth disorder, in effect, caused by hormonal/enzymatic defects triggered by exposures to environmental chemicals and specific foods in our diet.
The environmental chemicals (obesogens) and specific foods in our diet alter the setpoint for gaining weight, e.g., how much food it takes to increase weight and how much dieting it takes to lose weight by virtue of their effects on the hormonal control of metabolism.
By this logic, combating the obesity epidemic requires that individuals reduce exposures to environmental chemicals and specific foods during sensitive times when the adipose-GI-muscle-pancreatic regulatory system is set up and regulated.
It is not the number but type of calories
It is not intervention but prevention!
Funding.
Alison Holloway, Canadian Institutes of Health Research, PTF155981.
Christopher D. Kassotis, NIH, R00 ES030405.
Trey Howell, NIH, R15ES026790, R21ES030786.
Helene Le Mentic, European Union Horizon 2020 Research and Innovation Program, Oberon #825712.
Troy Roepke, NIH, R01MH123544,P30ES005022, USDA/NIFA NJ6195.
Robert Sargis, NIH, R01ES028879, R21ES030884,P30ES027792.
Craig R. Tomlinson, P30NCI23108, NCCC Pruty Pilot Award.
Jan Vondracek, Czech Science Foundation #21–00533s, Institute of Biophysics of the Czech Academy of Science, RVO-68081707, European Union Horizon 2020 Research and Innovation Program, Oberon #825712.
Juan P. Arrebola, Ramony Cajal Program RYC-2016–20155.
Patrick Babin, European Union Horizon 2020 Research and Innovation Program, Oberon #825712.
Mathew Cave, NIH, R35ES028373, R01ES032189, T32ES011564, P42ES023716, P30ES030283, R21ES031510.
Saurabh Chatterjee, NIH, P20GM103641, P01ES028942, P01AT003961, DoD-IIRFA W81XWH1810374.
David Collier, NIH, P30ES025128.
Lisa Connolly, European Union Horizon 2020 Research and Innovation Program, PROTECTD #722634.
Xavier Coumoul, European Union Horizon 2020 Research and Innovation Program, Oberon #825712.
Bruce Blumberg, NIH R01ES023316, R01ES03113.
Abbreviations:
- 3-BHA
3-tert-butyl-4-hydroxyanisole
- ADHD
attention deficit hyperactivity disorder
- ADI
acceptable daily intake
- AgRP
Agouti-related peptide
- AhR
aryl hydrocarbon receptor
- AR
androgen receptor
- BADGE
bisphenol A diglycidyl ether
- BADGE.2H(2)0
bisphenol A bis(2,3-dihydroxy propyl) ether
- BaP
benzo [a] pyrene
- BAT
brown adipose tissue
- BBP
butyl benzyl phthalate
- BCEP
bis(2-chloroethyl) phosphate
- BDCPP
bis(1,3-dichloro-2-propyl) phosphate
- bHLH
basic-helix-loop-helix
- BMI
body mass index
- BP
butylparaben
- BPA
bisphenol A
- BPAF
bisphenol AF
- BPB
bisphenol B
- BPE
bisphenol E
- BPF
bisphenol F
- BPS
bisphenol S
- CAR
constitutive androstane receptor
- CART
cocaine- and amphetamine regulated transcript
- CB
cannabinoid receptor
- Cd
cadmium
- C/EBP
CCAAT/enhancer-binding protein
- Ces
carboxylesterase
- CMC
carboxymethylcellulose
- CNS
central nervous system
- CRP
C-reactive protein
- CVD
cardiovascular disease
- DBP
di-n-butyl phthalate
- DBT
dibutyltin
- DBUP
dibutyl phosphate
- DDD
dichlorodiphenyldichloroethane
- DDE
dichlorodiphenyldichloroethylene
- DDT
dichlorodiphenyltrichloroethane
- DEHP
di(2-ethylhexyl) phthalate
- DEP
diethyl phthalate
- DES
diethylstilbestrol
- DiBP
diisobutyl phthalate
- DiDP
diisodecyl phthalate
- DINCH
1,2-cyclohexane dicarboxylic acid diisononyl ester
- DiNP
diisononyl phthalate
- dl
dioxin-like
- DMP
dimethyl phthalate
- DOHaD
Developmental Origins of Health and Disease
- DOP
di-n-octyl phthalate
- DOSS
dicotyl sodium sulfoscuccinate
- dpf
days post-fertilization
- DPHP
di-propylheptyl phthalate
- ECHA
European Chemicals Agency
- EDC
endocrine disrupting chemical
- EFSA
European Food Safety Authority
- EGF
epidermal growth factor
- EGFR
epidermal growth factor receptor
- EHDPHP
2-ethylhexyl diphenyl phosphate
- EH-TBB
2-ethylhexyl-2,3,4,5-tetrabromobenzoate
- EPA
Environmental Protection Agency
- ER
estrogen receptor
- ETC
electron transport chain
- FA
fatty acid
- FAS
fatty acid synthase
- FDA
Food and Drug Administration
- FFA
free fatty acid
- FLD
fatty liver disease
- FXR
farnesoid X receptor
- GD
gestational day
- GI
gastrointestinal
- GIP
gastric inhibitory polypeptide
- GNI
gross national income
- GR
glucocorticoid receptor
- HBCDD
hexabromocyclododecane
- HCB
hexachlorobenzene
- HCH
hexachlorocyclohexane
- HDL
high-density lipoprotein
- HELIX
Human Early Life Exposome
- HFCS
high fructose corn syrup
- HFD
high-fat diet
- hMSC
human mesenchymal stem cell
- IATA
integrated approaches to testing and assessment
- IGF
insulin growth factor
- IGF1R
insulin growth factor 1 receptor
- iAS
inorganic arsenic
- isoDMBs
iso-directional differentially methylated blocks
- JECFA
Joint FAO/WHO Expert Committee on Food Additives
- JP-8
jet fuel
- KCs
key characteristics
- KYN
kynurenine
- LDL
low-density lipoprotein
- lncRNA
long-coding RNA
- LPL
ipoprotein lipase
- LXR
liver X receptor
- MCPP
mono-3-carboxypropyl phthalate
- MDC
metabolism disrupting chemical
- MECPP
mono(2-ethyl-5-carboxypentyl) phthalate
- MEHP
monoethylhexyl phthalate
- MEP
monoethyl phthalate
- MiRNA
microRNA
- MRI
magnetic resonance imaging
- MSC
mesenchymal stem cell
- MSG
monosodium glutamate
- mtROS
mitochondrial reactive oxygen species
- NAFLD
non-alcoholic fatty liver disease
- NASH
non-alcoholic steatohepatitis
- ncRNAs
noncoding RNAs
- NHANES
National Health and Nutrition Examination Survey
- NNS
non-nutritive sweeteners
- NOAEL
no observed adverse effect level
- non-dl
non-dioxin-like
- NPY
neuropeptide Y
- NR
nuclear receptor
- NTP
National Toxicology Program
- OPFR
organophosphate flame retardant
- PAH
polycyclic aromatic hydrocarbon
- PAS
PER-ARNT-SIM
- PBDE
polybrominated diphenyl ether
- PCB
polychlorinated biphenyl
- PCDD/F
polychlorinated dibenzo-p-dioxins and dibenzofurans
- PFAS
per- and poly-fluorinated alkyl substances
- PFBS
perfluorobutane sulfonic acid
- PFDA
perfluoroundecanoic acid
- PFNA
perfluorononanoic acid
- PFOA
perfluorooctanoic acid
- PFOS
perfluorooctanesulfonic acid
- PFHxS
perfluorohexanesulfonic acid
- PM
particulate matter
- PM2.5
fine particulate matter under 2.5 μm in width
- PM10
coarse particulate matter under 10 μm in width
- PND
postnatal day
- POMC
pro-opiomelanocortin
- POP
persistent organic pollutant
- PPAR
peroxisome proliferation activated receptor
- PVC
polyvinyl chloride
- PVN
paraventricular nucleus
- PXR
pregnane X receptor
- ROS
reactive oxygen species
- ROSI
rosiglitazone
- RXR
retinoid X receptor
- SCD
stearoyl-CoA desaturase
- SHS
secondhand smoke
- SIRTs
sirtuins
- SREBP
sterol regulatory element-binding protein
- SSRI
selective serotonin reuptake inhibitor
- T2D
type 2 diabetes
- TASH
toxicant-associated steatohepatitis
- TBBPA
tetrabromobisphenol A
- TBMEHP
mono-(2-ethyhexyl)tetrabromophthalate
- TBPH
bis(2-ethylhexyl)-2,3,4,5-tetrabromophthalate
- TBT
tributyltin
- TCBPA
tetrachlorobisphenol A
- TCDD
2,3,7,8-tetrachlorodibenzo-p-dioxin
- TCDF
2,3,7,8-tetrachlorodibenzofuran
- TCEP
tris(2-chloroethyl) phosphate
- TCP
tricresyl phosphate
- TDCPP
tris(l,3-dichloro-2-propyl) phosphate
- TDI
Tolerable Daily Intake
- TF
tolyfluanid
- TG
triglyceride
- TPhP
triphenyl phosphate
- TPhT
triphenyltin
- TR
thyroid receptor
- VLDL
veey low density lipoprotein
- VT
delta valerobetaine
- WAT
white adipose tissue
References
- [1].Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, Abraham JP, Abu-Rmeileh NM, Achoki T, AlBuhairan FS, Alemu ZA, Alfonso R, Ali MK, Ali R, Guzman NA, Ammar W, Anwari P, Banerjee A, Barquera S, Basu S, Bennett DA, Bhutta Z, Blore J, Cabral N, Nonato IC, Chang JC, Chowdhury R, Courville KJ, Criqui MH, Cundiff DK, Dabhadkar KC, Dandona L, Davis A, Dayama A, Dharmaratne SD, Ding EL, Durrani AM, Esteghamati A, Farzadfar F, Fay DF, Feigin VL, Flaxman A, Forouzanfar MH, Goto A, Green MA, Gupta R, Hafezi-Nejad N, Hankey GJ, Harewood HC, Havmoeller R, Hay S, Hernandez L, Husseini A, Idrisov BT, Ikeda N, Islami F, Jahangir E, Jassal SK, Jee SH, Jeffreys M, Jonas JB, Kabagambe EK, Khalifa SE, Kengne AP, Khader YS, Khang YH, Kim D, Kimokoti RW, Kinge JM, Kokubo Y, Kosen S, Kwan G, Lai T, Leinsalu M, Li Y, Liang X, Liu S, Logroscino G, Lotufo PA, Lu Y, Ma J, Mainoo NK, Mensah GA, Merriman TR, Mokdad AH, Moschandreas J, Naghavi M, Naheed A, Nand D, Narayan KM, Nelson EL, Neuhouser ML, Nisar MI, Ohkubo T, Oti SO, Pedroza A, Prabhakaran D, Roy N, Sampson U, Seo H, Sepanlou SG, Shibuya K, Shiri R, Shiue I, Singh GM, Singh JA, Skirbekk V, Stapelberg NJ, Sturua L, Sykes BL, Tobias M, Tran BX, Trasande L, Toyoshima H, van de Vijver S, Vasankari TJ, Veerman JL, Velasquez-Melendez G, Vlassov VV, Vollset SE, Vos T, Wang C, Wang X, Weiderpass E, Werdecker A, Wright JL, Yang YC, Yatsuya H, Yoon J, Yoon SJ, Zhao Y, Zhou M, Zhu S, Lopez AD, Murray CJ, Gakidou E, Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013, Lancet 384 (9945) (2014) 766–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM, Leibel RL, Obesity Pathogenesis: An Endocrine Society Scientific Statement, Endocr. Rev 38 (4) (2017) 267–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Blüher M, Obesity: global epidemiology and pathogenesis, Nat. Rev. Endocrinol 15 (5) (2019) 288–298. [DOI] [PubMed] [Google Scholar]
- [4].Williams EP, Mesidor M, Winters K, Dubbert PM, Wyatt SB, Overweight and Obesity: Prevalence, Consequences, and Causes of a Growing Public Health Problem, Current obesity reports 4 (3) (2015) 363–370. [DOI] [PubMed] [Google Scholar]
- [5].Zoeller RT, Brown TR, Doan LL, Gore AC, Skakkebaek NE, Soto AM, Endocrine-disrupting chemicals and public health protection: a statement of principles from the Endocrine Society, Endocrinology 153 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].La Merrill MA, Vandenberg LN, Smith MT, Goodson W, Browne P, Patisaul HB, Guyton KZ, Kortenkamp A, Cogliano VJ, Woodruff TJ, Rieswijk L, Sone H, Korach KS, Gore AC, Zeise L, Zoeller RT, Consensus on the key characteristics of endocrine-disrupting chemicals as a basis for hazard identification, Nat. Rev. Endocrinol 16 (1) (2020) 45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, Toppari J, Zoeller RT, Executive Summary to EDC-2: The Endocrine Society’s Second Scientific Statement on Endocrine-Disrupting Chemicals, Endocr. Rev 36 (6) (2015) E1–E150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Godfray HCJ, Stephens AEA, Jepson PD, Jobling S, Johnson AC, Matthiessen P, Sumpter JP, Tyler CR, McLean AR, A restatement of the natural science evidence base on the effects of endocrine disrupting chemicals on wildlife, Proceedings. Biological sciences 286 (1897) (2019) 20182416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs DR, Lee DH, Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses, Endocr. Rev 33 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Villar-Pazos S, Martinez-Pinna J, Castellano-Munoz M, Alonso-Magdalena P, Marroqui L, Quesada I, Gustafsson JA, Nadal A, Molecular mechanisms involved in the non-monotonic effect of bisphenol-a on ca2+ entry in mouse pancreatic beta-cells, Sci. Rep 7 (1) (2017) 11770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].vom Saal FS, Vandenberg LN, Update on the Health Effects of Bisphenol A: Overwhelming Evidence of Harm, Endocrinology 162 (3) (2021) 1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Heindel JJ, Blumberg B, Environmental Obesogens: Mechanisms and Controversies, Annu. Rev. Pharmacol. Toxicol 59 (2019) 89–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Heindel JJ, Blumberg B, Cave M, Machtinger R, Mantovani A, Mendez MA, Nadal A, Palanza P, Panzica G, Sargis R, Vandenberg LN, vom Saal FS, Metabolism disrupting chemicals and metabolic disorders, Reprod. Toxicol 68 (2017) 3–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Darbre PD, Endocrine Disruptors and Obesity, Current obesity reports (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Veiga-Lopez A, Pu Y, Gingrich J, Padmanabhan V, Obesogenic Endocrine Disrupting Chemicals: Identifying Knowledge Gaps, Trends in endocrinology and metabolism: TEM 29 (9) (2018) 607–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Chamorro-Garcia R, Blumberg B, Current Research Approaches and Challenges in the Obesogen Field, Front Endocrinol (Lausanne) 10 (2019) 167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Amato AA, Wheeler HB, Blumberg B, Obesity and endocrine-disrupting chemicals, Endocr Connect 10 (2) (2021) R87–R105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Egusquiza RJ, Blumberg B, Environmental Obesogens and Their Impact on Susceptibility to Obesity: New Mechanisms and Chemicals, Endocrinology 161 (3) (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Papalou O, Kandaraki EA, Papadakis G, Diamanti-Kandarakis E, Endocrine Disrupting Chemicals: An Occult Mediator of Metabolic Disease, Front Endocrinol (Lausanne) 10 (2019) 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Heindel JJ, History of the Obesogen Field: Looking Back to Look Forward, Front. Endocrinol 10 (14) (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hanson MA, Gluckman PD, Early Developmental Conditioning of Later Health and Disease, Physiology or Pathophysiology? (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Heindel JJ, Balbus J, Birnbaum L, Brune-Drisse MN, Grandjean P, Gray K, Landrigan PJ, Sly PD, Suk W, Cory Slechta D, Thompson C, Hanson M, Developmental Origins of Health and Disease: Integrating Environmental Influences, Endocrinology 156(10) (2015) 3416–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Heindel JJ, Role of exposure to environmental chemicals in the developmental basis of reproductive disease and dysfunction, Semin Reprod Med 24 (3) (2006) 168–177. [DOI] [PubMed] [Google Scholar]
- [24].Stel J, Legler J, The Role of Epigenetics in the Latent Effects of Early Life Exposure to Obesogenic Endocrine Disrupting Chemicals, Endocrinology (2015) en20151434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Martinez-Jimenez CP, Sandoval J, Epigenetic crosstalk: a molecular language in human metabolic disorders, Frontiers in bioscience (Scholar edition) 7 (2015) 46–57. [DOI] [PubMed] [Google Scholar]
- [26].Statello L, Guo CJ, Chen LL, Huarte M, Gene regulation by long non-coding RNAs and its biological functions, Nat. Rev. Mol. Cell Biol 22 (2) (2021) 96–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Romano G, Veneziano D, Nigita G, Nana-Sinkam SP, RNA Methylation in ncRNA: Classes, Detection, and Molecular Associations, Front Genet 9 (2018) 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Sonkar R, Powell CA, Choudhury M, Benzyl butyl phthalate induces epigenetic stress to enhance adipogenesis in mesenchymal stem cells, Mol. Cell. Endocrinol 431 (2016) 109–122. [DOI] [PubMed] [Google Scholar]
- [29].Zhang J, Choudhury M, Benzyl Butyl Phthalate Induced Early lncRNA H19 Regulation in C3H10T1/2 Stem Cell Line, Chem. Res. Toxicol 34 (1) (2021) 54–62. [DOI] [PubMed] [Google Scholar]
- [30].Verbanck M, Canouil M, Leloire A, Dhennin V, Coumoul X, Yengo L, Froguel P, Poulain-Godefroy O, Low-dose exposure to bisphenols A, F and S of human primary adipocyte impacts coding and non-coding RNA profiles, PLoS ONE 12 (6) (2017), e0179583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Susiarjo M, Xin F, Bansal A, Stefaniak M, Li C, Simmons RA, Bartolomei MS, Bisphenol A exposure disrupts metabolic health across multiple generations in the mouse, Endocrinology (2015) en20142027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Joh RI, Palmieri CM, Hill IT, Motamedi M, Regulation of histone methylation by noncoding RNAs, BBA 1839 (12) (2014) 1385–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Squillaro T, Peluso G, Galderisi U, Di Bernardo G, Long non-coding RNAs in regulation of adipogenesis and adipose tissue function, Elife 9 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Rinn JL, Kertesz M, Wang JK, Squazzo SL, Xu X, Brugmann SA, Goodnough LH, Helms JA, Farnham PJ, Segal E, Chang HY, Functional demarcation of active and silent chromatin domains in human HOX loci by noncoding RNAs, Cell 129 (7) (2007) 1311–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Mercer TR, Dinger ME, Sunkin SM, Mehler MF, Mattick JS, Specific expression of long noncoding RNAs in the mouse brain, PNAS 105 (2) (2008) 716–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Clemson CM, Hutchinson JN, Sara SA, Ensminger AW, Fox AH, Chess A, Lawrence JB, An architectural role for a nuclear noncoding RNA: NEAT1 RNA is essential for the structure of paraspeckles, Mol. Cell 33 (6) (2009) 717–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Chen G, Wang Z, Wang D, Qiu C, Liu M, Chen X, Zhang Q, Yan G, Cui Q, LncRNADisease: a database for long-non-coding RNA-associated diseases, Nucleic acids research 41(Database issue) (2013) D983–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Sun L, Goff LA, Trapnell C, Alexander R, Lo KA, Hacisuleyman E, Sauvageau M, Tazon-Vega B, Kelley DR, Hendrickson DG, Yuan B, Kellis M, Lodish HF, Rinn JL, Long noncoding RNAs regulate adipogenesis, PNAS 110 (9) (2013) 3387–3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Zhao XY, Li S, Wang GX, Yu Q, Lin JD, A long noncoding RNA transcriptional regulatory circuit drives thermogenic adipocyte differentiation, Mol. Cell 55 (3) (2014) 372–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Wijesinghe SN, Nicholson T, Tsintzas K, Jones SW, Involvements of long noncoding RNAs in obesity-associated inflammatory diseases, Obes. Rev 22 (4) (2021), e13156. [DOI] [PubMed] [Google Scholar]
- [41].Woeller CF, Flores E, Pollock SJ, Phipps RP, Editor’s Highlight: Thy1 (CD90) Expression is Reduced by the Environmental Chemical Tetrabromobisphenol-A to Promote Adipogenesis Through Induction of microRNA-103, Toxicological sciences : an official journal of the Society of Toxicology 157 (2) (2017) 305–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Skinner MK, Environmental Epigenetics and a Unified Theory of the Molecular Aspects of Evolution: A Neo-Lamarckian Concept that Facilitates Neo-Darwinian Evolution, Genome biology and evolution 7 (5) (2015) 1296–1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Chamorro-Garcia R, Sahu M, Abbey RJ, Laude J, Pham N, Blumberg B, Transgenerational inheritance of increased fat depot size, stem cell reprogramming, and hepatic steatosis elicited by prenatal exposure to the obesogen tributyltin in mice, Environ. Health Perspect 121 (3) (2013) 359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Chamorro-Garcia R, Diaz-Castillo C, Shoucri BM, Kach H, Leavitt R, Shioda T, Blumberg B, Ancestral perinatal obesogen exposure results in a transgenerational thrifty phenotype in mice, Nat. Commun 8 (1) (2017) 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Chamorro-García R, Poupin N, Tremblay-Franco M, Canlet C, Egusquiza R, Gautier R, Jouanin I, Shoucri BM, Blumberg B, Zalko D, Transgenerational metabolomic fingerprints in mice ancestrally exposed to the obesogen TBT, Environ. Int 157 (2021), 106822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Skinner MK, Manikkam M, Tracey R, Guerrero-Bosagna C, Haque M, Nilsson EE, Ancestral dichlorodiphenyltrichloroethane (DDT) exposure promotes epigenetic transgenerational inheritance of obesity, BMC Med 11 (2013) 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Tracey R, Manikkam M, Guerrero-Bosagna C, Skinner MK, Hydrocarbons (jet fuel JP-8) induce epigenetic transgenerational inheritance of obesity, reproductive disease and sperm epimutations, Reprod. Toxicol 36 (2013) 104–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Manikkam M, Tracey R, Guerrero-Bosagna C, Skinner MK, Plastics derived endocrine disruptors (BPA, DEHP and DBP) induce epigenetic transgenerational inheritance of obesity, reproductive disease and sperm epimutations, PLoS ONE 8 (1) (2013), e55387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].King SE, Nilsson E, Beck D, Skinner MK, Adipocyte epigenetic alterations and potential therapeutic targets in transgenerationally inherited lean and obese phenotypes following ancestral exposures, Adipocyte 8 (1) (2019) 362–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Xu Y, Wang W, Chen M, Zhou J, Huang X, Tao S, Pan B, Li Z, Xie X, Li W, Kan H, Ying Z, Developmental programming of obesity by maternal exposure to concentrated ambient PM(2.5) is maternally transmitted into the third generation in a mouse model, Part. Fibre Toxicol 16 (1) (2019) 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Bansal A, Li C, Xin F, Duemler A, Li W, Rashid C, Bartolomei MS, Simmons RA, Transgenerational effects of maternal bisphenol: a exposure on offspring metabolic health, Journal of developmental origins of health and disease 10 (2) (2019) 164–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Rechavi O, Houri-Ze’evi L, Anava S, Goh WSS, Kerk SY, Hannon GJ, Hobert O, Starvation-induced transgenerational inheritance of small RNAs in C. elegans, Cell 158 (2) (2014) 277–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Tauffenberger A, Parker JA, Heritable transmission of stress resistance by high dietary glucose in Caenorhabditis elegans, PLoS Genet. 10 (5) (2014), e1004346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Zhou X, Li J, Zhang X, Zhang C, Bai J, Zhao Y, Zhu Y, Zhang J, Xiao X, Bisphenol S promotes fat storage in multiple generations of Caenorhabditis elegans in a daf-16/nhr-49 dependent manner, Comp. Biochem. Physiol. C: Toxicol. Pharmacol 109175 (2021). [DOI] [PubMed] [Google Scholar]
- [55].Chen MY, Liu HP, Cheng J, Chiang SY, Liao WP, Lin WY, Transgenerational impact of DEHP on body weight of Drosophila, Chemosphere 221 (2019) 493–499. [DOI] [PubMed] [Google Scholar]
- [56].Camacho J, Truong L, Kurt Z, Chen YW, Morselli M, Gutierrez G, Pellegrini M, Yang X, Allard P, The Memory of Environmental Chemical Exposure in C. elegans Is Dependent on the Jumonji Demethylases jmjd-2 and jmjd-3/utx-1, Cell reports 23 (8) (2018) 2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Ben Maamar M, Nilsson E, Sadler-Riggleman I, Beck D, McCarrey JR, Skinner MK, Developmental origins of transgenerational sperm DNA methylation epimutations following ancestral DDT exposure, Dev. Biol 445 (2) (2018) 280–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Skinner MK, Ben Maamar M, Sadler-Riggleman I, Beck D, Nilsson E, McBirney M, Klukovich R, Xie Y, Tang C, Yan W, Alterations in sperm DNA methylation, non-coding RNA and histone retention associate with DDT-induced epigenetic transgenerational inheritance of disease, Epigenetics Chromatin 11 (1) (2018) 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Carone BR, Fauquier L, Habib N, Shea JM, Hart CE, Li R, Bock C, Li C, Gu H, Zamore PD, Meissner A, Weng Z, Hofmann HA, Friedman N, Rando OJ, Paternally induced transgenerational environmental reprogramming of metabolic gene expression in mammals, Cell 143 (7) (2010) 1084–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Diaz-Castillo C, Chamorro-Garcia R, Shioda T, Blumberg B, Transgenerational Self-Reconstruction of Disrupted Chromatin Organization After Exposure To An Environmental Stressor in Mice, Sci. Rep 9 (1) (2019) 13057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Shao X, Wang M, Wei X, Deng S, Fu N, Peng Q, Jiang Y, Ye L, Xie J, Lin Y, Peroxisome Proliferator-Activated Receptor-γ: Master Regulator of Adipogenesis and Obesity, Curr. Stem Cell Res. Ther 11 (3) (2016) 282–289. [DOI] [PubMed] [Google Scholar]
- [62].Gao P, Wang L, Yang N, Wen J, Zhao M, Su G, Zhang J, Weng D, Peroxisome proliferator-activated receptor gamma (PPARγ) activation and metabolism disturbance induced by bisphenol A and its replacement analog bisphenol S using in vitro macrophages and in vivo mouse models, Environ. Int 134 (2020), 105328. [DOI] [PubMed] [Google Scholar]
- [63].Hoepner LA, Bisphenol a: A narrative review of prenatal exposure effects on adipogenesis and childhood obesity via peroxisome proliferator-activated receptor gamma, Environ. Res 173 (2019) 54–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Wen Q, Xie X, Zhao C, Ren Q, Zhang X, Wei D, Emanuelli B, Du Y, The brominated flame retardant PBDE 99 promotes adipogenesis via regulating mitotic clonal expansion and PPARgamma expression, The Science of the total environment 670 (2019) 67–77. [DOI] [PubMed] [Google Scholar]
- [65].Ma Y, Yang J, Wan Y, Peng Y, Ding S, Li Y, Xu B, Chen X, Xia W, Ke Y, Xu S, Low-level perfluorooctanoic acid enhances 3T3–L1 preadipocyte differentiation via altering peroxisome proliferator activated receptor gamma expression and its promoter DNA methylation, Journal of applied toxicology : JAT 38 (3) (2018) 398–407. [DOI] [PubMed] [Google Scholar]
- [66].Lyssimachou A, Santos JG, André A, Soares J, Lima D, Guimarães L, Almeida CMR, Teixeira C, Castro LFC, Santos MM, The Mammalian “Obesogen” Tributyltin Targets Hepatic Triglyceride Accumulation and the Transcriptional Regulation of Lipid Metabolism in the Liver and Brain of Zebrafish, PLoS ONE 10 (12) (2015) e0143911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Rosen ED, Sarraf P, Troy AE, Bradwin G, Moore K, Milstone DS, Spiegelman BM, Mortensen RM, PPAR gamma is required for the differentiation of adipose tissue in vivo and in vitro, Mol. Cell 4 (4) (1999) 611–617. [DOI] [PubMed] [Google Scholar]
- [68].Tontonoz P, Singer S, Forman BM, Sarraf P, Fletcher JA, Fletcher CD, Brun RP, Mueller E, Altiok S, Oppenheim H, Evans RM, Spiegelman BM, Terminal differentiation of human liposarcoma cells induced by ligands for peroxisome proliferator-activated receptor gamma and the retinoid X receptor, PNAS 94 (1) (1997) 237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Kassotis CD, Masse L, Kim S, Schlezinger JJ, Webster TF, Stapleton HM, Characterization of adipogenic chemicals in three different cell culture systems: implications for reproducibility based on cell source and handling, Sci. Rep 7 (2017) 42104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Kanayama T, Kobayashi N, Mamiya S, Nakanishi T, Nishikawa J, Organotin compounds promote adipocyte differentiation as agonists of the peroxisome proliferator-activated receptor [gamma]/retinoid X receptor pathway, Mol. Pharmacol 67 (2005) 766–774. [DOI] [PubMed] [Google Scholar]
- [71].Grun F, Blumberg B, Environmental obesogens: organotins and endocrine disruption via nuclear receptor signaling, Endocrinology 147 (6 Suppl) (2006) S50–S55. [DOI] [PubMed] [Google Scholar]
- [72].Shoucri BM, Hung VT, Chamorro-Garcia R, Shioda T, Blumberg B, Retinoid X receptor activation during adipogenesis of female mesenchymal stem cells programs a dysfunctional adipocyte, Endocrinology (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Kim S, Li A, Monti S, Schlezinger JJ, Tributyltin induces a transcriptional response without a brite adipocyte signature in adipocyte models, Arch. Toxicol 92 (9) (2018) 2859–2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Regnier SM, El-Hashani E, Kamau W, Zhang X, Massad NL, Sargis RM, Tributyltin differentially promotes development of a phenotypically distinct adipocyte, Obesity (Silver Spring) 23 (9) (2015) 1864–1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Fuentes N, Silveyra P, Estrogen receptor signaling mechanisms, Adv Protein Chem Struct Biol 116 (2019) 135–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Hugo ER, Brandebourg TD, Woo JG, Loftus J, Alexander JW, Ben-Jonathan N, Bisphenol A at environmentally relevant doses inhibits adiponectin release from human adipose tissue explants and adipocytes, Environ. Health Perspect 116 (12) (2008) 1642–1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Cooke PS, Naaz A, Role of estrogens in adipocyte development and function, Exp Biol Med (Maywood) 229 (11) (2004) 1127–1135. [DOI] [PubMed] [Google Scholar]
- [78].Dieudonne MN, Pecquery R, Leneveu MC, Giudicelli Y, Opposite effects of androgens and estrogens on adipogenesis in rat preadipocytes: evidence for sex and site-related specificities and possible involvement of insulin-like growth factor 1 receptor and peroxisome proliferator-activated receptor gamma2, Endocrinology 141 (2) (2000) 649–656. [DOI] [PubMed] [Google Scholar]
- [79].Roncari DA, Van RL, Promotion of human adipocyte precursor replication by 17beta-estradiol in culture, J Clin Invest 62 (3) (1978) 503–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Hatch EE, Troisi R, Palmer JR, Wise LA, Titus L, Strohsnitter WC, Ricker W, Hyer M, Hoover RN, Prenatal diethylstilbestrol exposure and risk of obesity in adult women, J Dev Orig Health Dis 6 (3) (2015) 201–207. [DOI] [PubMed] [Google Scholar]
- [81].Lee S, Kim C, Shin H, Kho Y, Choi K, Comparison of thyroid hormone disruption potentials by bisphenols A, S, F, and Z in embryo-larval zebrafish, Chemosphere 221 (2019) 115–123. [DOI] [PubMed] [Google Scholar]
- [82].Blouin K, Boivin A, Tchernof A, Androgens and body fat distribution, J. Steroid Biochem. Mol. Biol 108 (3–5) (2008) 272–280. [DOI] [PubMed] [Google Scholar]
- [83].O’Reilly MW, House PJ, Tomlinson JW, Understanding androgen action in adipose tissue, J. Steroid Biochem. Mol. Biol 143 (2014) 277–284. [DOI] [PubMed] [Google Scholar]
- [84].John K, Marino JS, Sanchez ER, Hinds TD Jr., The glucocorticoid receptor: cause of or cure for obesity?, American journal of physiology, Endocrinology and metabolism 310 (4) (2016) E249–E257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Contador D, Ezquer F, Espinosa M, Arango-Rodriguez M, Puebla C, Sobrevia L, Conget P, Dexamethasone and rosiglitazone are sufficient and necessary for producing functional adipocytes from mesenchymal stem cells, Exp Biol Med (Maywood) 240 (9) (2015) 1235–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Asada M, Rauch A, Shimizu H, Maruyama H, Miyaki S, Shibamori M, Kawasome H, Ishiyama H, Tuckermann J, Asahara H, DNA binding-dependent glucocorticoid receptor activity promotes adipogenesis via Kruppel-like factor 15 gene expression, Lab. Invest 91 (2) (2011) 203–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Sargis RM, Johnson DN, Choudhury RA, Brady MJ, Environmental Endocrine Disruptors Promote Adipogenesis in the 3T3-L1 Cell Line through Glucocorticoid Receptor Activation, Obesity (Silver Spring, Md.) 18 (7) (2010) 1283–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Iwen KA, Schroder E, Brabant G, Thyroid hormones and the metabolic syndrome, European thyroid journal 2 (2) (2013) 83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Obregon MJ, Thyroid hormone and adipocyte differentiation, Thyroid 18 (2) (2008) 185–195. [DOI] [PubMed] [Google Scholar]
- [90].Shulman AI, Mangelsdorf DJ, Retinoid x receptor heterodimers in the metabolic syndrome, The New England journal of medicine 353 (6) (2005) 604–615. [DOI] [PubMed] [Google Scholar]
- [91].Mullur R, Liu YY, Brent GA, Thyroid hormone regulation of metabolism, Physiol. Rev 94 (2) (2014) 355–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Gao J, Xie W, Targeting xenobiotic receptors PXR and CAR for metabolic diseases, Trends Pharmacol. Sci 33 (10) (2012) 552–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Moreau A, Vilarem MJ, Maurel P, Pascussi JM, Xenoreceptors CAR and PXR activation and consequences on lipid metabolism, glucose homeostasis, and inflammatory response, Mol. Pharm 5 (1) (2008) 35–41. [DOI] [PubMed] [Google Scholar]
- [94].Saito K, Kobayashi K, Mizuno Y, Fukuchi Y, Furihata T, Chiba K, Peroxisome proliferator-activated receptor alpha (PPARalpha) agonists induce constitutive androstane receptor (CAR) and cytochrome P450 2B in rat primary hepatocytes, Drug Metab. Pharmacokinet 25 (1) (2010) 108–111. [DOI] [PubMed] [Google Scholar]
- [95].Hardesty JE, Wahlang B, Falkner KC, Shi H, Jin J, Wilkey D, Merchant M, Watson C, Prough RA, Cave MC, Hepatic signalling disruption by pollutant Polychlorinated biphenyls in steatohepatitis, Cell. Signal 53 (2019) 132–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Lukowicz C, Ellero-Simatos S, Régnier M, Polizzi A, Lasserre F, Montagner A, Lippi Y, Jamin EL, Martin J-F, Naylies C, Canlet C, Debrauwer L, Bertrand-Michel J, Al Saati T, Théodorou V, Loiseau N, Mselli-Lakhal L, Guillou H, Gamet-Payrastre L, Metabolic Effects of a Chronic Dietary Exposure to a Low-Dose Pesticide Cocktail in Mice: Sexual Dimorphism and Role of the Constitutive Androstane Receptor, Environ. Health Perspect 126 (6) (2018) 067007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Wang H, Chen J, Hollister K, Sowers LC, Forman BM, Endogenous bile acids are ligands for the nuclear receptor FXR/BAR, Mol. Cell 3 (5) (1999) 543–553. [DOI] [PubMed] [Google Scholar]
- [98].Jiao Y, Lu Y, Li XY, Farnesoid X receptor: a master regulator of hepatic triglyceride and glucose homeostasis, Acta Pharmacol. Sin 36 (1) (2015) 44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Prawitt J, Caron S, Staels B, How to modulate FXR activity to treat the Metabolic Syndrome, Drug Discov Today: Disease Mechanisms 6 (1–4) (2009) e55–e64. [Google Scholar]
- [100].Rizzo G, Disante M, Mencarelli A, Renga B, Gioiello A, Pellicciari R, Fiorucci S, The farnesoid X receptor promotes adipocyte differentiation and regulates adipose cell function in vivo, Mol. Pharmacol 70 (4) (2006) 1164–1173. [DOI] [PubMed] [Google Scholar]
- [101].Cariou B, van Harmelen K, Duran-Sandoval D, van Dijk TH, Grefhorst A, Abdelkarim M, Caron S, Torpier G, Fruchart JC, Gonzalez FJ, Kuipers F, Staels B, The farnesoid X receptor modulates adiposity and peripheral insulin sensitivity in mice, J. Biol. Chem 281 (16) (2006) 11039–11049. [DOI] [PubMed] [Google Scholar]
- [102].Bjork JA, Butenhoff JL, Wallace KB, Multiplicity of nuclear receptor activation by PFOA and PFOS in primary human and rodent hepatocytes, Toxicology 288 (1–3) (2011) 8–17. [DOI] [PubMed] [Google Scholar]
- [103].McIntosh BE, Hogenesch JB, Bradfield CA, Mammalian Per-Arnt-Sim proteins in environmental adaptation, Annu. Rev. Physiol 72 (2010) 625–645. [DOI] [PubMed] [Google Scholar]
- [104].Rathore K, Cekanova M, Effects of environmental carcinogen benzo(a)pyrene on canine adipose-derived mesenchymal stem cells, Res. Vet. Sci 103 (2015) 34–43. [DOI] [PubMed] [Google Scholar]
- [105].Kim MJ, Pelloux V, Guyot E, Tordjman J, Bui L-C, Chevallier A, Forest C, Benelli C, Clément K, Barouki R, Inflammatory Pathway Genes belong to Major Targets of Persistent Organic Pollutants in Adipose Cells, Environ. Health Perspect (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Kanno J, Introduction to the concept of signal toxicity, J Toxicol Sci 41(Special) (2016) SP105–SP109. [DOI] [PubMed] [Google Scholar]
- [107].e.e.e. European Association for the Study of the Liver. Electronic address, C. Clinical Practice Guideline Panel, m. Panel, E.G.B. representative, EASL Clinical Practice Guideline: Occupational liver diseases, J Hepatol 71(5) (2019) 1022–1037. [DOI] [PubMed] [Google Scholar]
- [108].Wahlang B, Beier JI, Clair HB, Bellis-Jones HJ, Falkner KC, McClain CJ, Cave MC, Toxicant-associated Steatohepatitis, Toxicol. Pathol 41 (2) (2013) 343–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Wahlang B, Jin J, Beier JI, Hardesty JE, Daly EF, Schnegelberger RD, Falkner KC, Prough RA, Kirpich IA, Cave MC, Mechanisms of Environmental Contributions to Fatty Liver Disease, Current environmental health reports 6 (3) (2019) 80–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Cave M, Falkner KC, Ray M, Joshi-Barve S, Brock G, Khan R, Bon Homme M, McClain CJ, Toxicant-associated steatohepatitis in vinyl chloride workers, Hepatology 51 (2) (2010) 474–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Wahlang B, Falkner KC, Gregory B, Ansert D, Young D, Conklin DJ, Bhatnagar A, McClain CJ, Cave M, Polychlorinated biphenyl 153 is a diet-dependent obesogen that worsens nonalcoholic fatty liver disease in male C57BL6/J mice, The Journal of Nutritional Biochemistry 24 (9) (2013) 1587–1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Foulds CE, Trevino LS, York B, Walker CL, Endocrine-disrupting chemicals and fatty liver disease, Nat Rev Endocrinol advance online publication (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Wang CW, Chuang HY, Liao KW, Yu ML, Dai CY, Chang WT, Tsai CH, Chiang HC, Huang PC, Urinary thiodiglycolic acid is associated with increased risk of non-alcoholic fatty liver disease in children living near a petrochemical complex, Environ. Int 131 (2019), 104978. [DOI] [PubMed] [Google Scholar]
- [114].Yuan TH, Chen JL, Shie RH, Yeh YP, Chen YH, Chan CC, Liver fibrosis associated with potential vinyl chloride and ethylene dichloride exposure from the petrochemical industry, The Science of the total environment 739 (2020), 139920. [DOI] [PubMed] [Google Scholar]
- [115].Li X, Zhang C, Wang K, Lehmler HJ, Fatty liver and impaired hepatic metabolism alter the congener-specific distribution of polychlorinated biphenyls (PCBs) in mice with a liver-specific deletion of cytochrome P450 reductase, Environmental pollution (Barking, Essex : 1987) 266(Pt 1) (2020) 115233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Allard J, Le Guillou D, Begriche K, Fromenty B, Drug-induced liver injury in obesity and nonalcoholic fatty liver disease, Adv. Pharmacol 85 (2019) 75–107. [DOI] [PubMed] [Google Scholar]
- [117].Hardesty JE, Al-Eryani L, Wahlang B, Falkner KC, Shi H, Jin J, Vivace BJ, Ceresa BP, Prough RA, Cave MC, Epidermal Growth Factor Receptor Signaling Disruption by Endocrine and Metabolic Disrupting Chemicals, Toxicological sciences : an official journal of the Society of Toxicology 162 (2) (2018) 622–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Hardesty JE, Wahlang B, Prough RA, Head KZ, Wilkey D, Merchant M, Shi H, Jin J, Cave MC, Effect of Epidermal Growth Factor Treatment and Polychlorinated Biphenyl Exposure in a Dietary-Exposure Mouse Model of Steatohepatitis, Environ. Health Perspect 129 (3) (2021) 37010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Lim JJ, Li X, Lehmler HJ, Wang D, Gu H, Cui JY, Gut Microbiome Critically Impacts PCB-induced Changes in Metabolic Fingerprints and the Hepatic Transcriptome in Mice, Toxicological sciences : an official journal of the Society of Toxicology 177 (1) (2020) 168–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Bassler J, Ducatman A, Elliott M, Wen S, Wahlang B, Barnett J, Cave MC, Environmental perfluoroalkyl acid exposures are associated with liver disease characterized by apoptosis and altered serum adipocytokines, Environmental pollution (Barking, Essex 247 (2019) (1987) 1055–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Jin R, McConnell R, Catherine C, Xu S, Walker DI, Stratakis N, Jones DP, Miller GW, Peng C, Conti DV, Vos MB, Chatzi L, Perfluoroalkyl substances and severity of nonalcoholic fatty liver in Children: An untargeted metabolomics approach, Environ. Int 134 (2020), 105220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Stratakis N, D VC, Jin R, Margetaki K, Valvi D, Siskos AP, Maitre L, Garcia E, Varo N, Zhao Y, Roumeliotaki T, Vafeiadi M, Urquiza J, Fernandez-Barres S, Heude B, Basagana X, Casas M, Fossati S, Grazuleviciene R, Andrusaityte S, Uppal K, McEachan RRC, Papadopoulou E, Robinson O, Haug LS, Wright J, Vos MB, Keun HC, Vrijheid M, Berhane KT, McConnell R, Chatzi L, Prenatal Exposure to Perfluoroalkyl Substances Associated With Increased Susceptibility to Liver Injury in Children, Hepatology 72(5) (2020) 1758–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Katz TA, Grimm SL, Kaushal A, Dong J, Trevino LS, Jangid RK, Gaitan AV, Bertocchio JP, Guan Y, Robertson MJ, Cabrera RM, Finegold MJ, Foulds CE, Coarfa C, Walker CL, Hepatic Tumor Formation in Adult Mice Developmentally Exposed to Organotin, Environ. Health Perspect 128 (1) (2020) 17010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Franco ME, Fernandez-Luna MT, Ramirez AJ, Lavado R, Metabolomic-based assessment reveals dysregulation of lipid profiles in human liver cells exposed to environmental obesogens, Toxicol. Appl. Pharmacol 398 (2020), 115009. [DOI] [PubMed] [Google Scholar]
- [125].Sun L, Ling Y, Jiang J, Wang D, Wang J, Li J, Wang X, Wang H, Differential mechanisms regarding triclosan vs. bisphenol A and fluorene-9-bisphenol induced zebrafish lipid-metabolism disorders by RNA-Seq, Chemosphere 251 (2020), 126318. [DOI] [PubMed] [Google Scholar]
- [126].Qin J, Ru S, Wang W, Hao L, Ru Y, Wang J, Zhang X, Long-term bisphenol S exposure aggravates non-alcoholic fatty liver by regulating lipid metabolism and inducing endoplasmic reticulum stress response with activation of unfolded protein response in male zebrafish, Environ. Pollut 263 (2020), 114535. [DOI] [PubMed] [Google Scholar]
- [127].Huff M, da Silveira WA, Carnevali O, Renaud L, Hardiman G, Systems Analysis of the Liver Transcriptome in Adult Male Zebrafish Exposed to the Plasticizer (2-Ethylhexyl) Phthalate (DEHP), Sci. Rep 8 (1) (2018) 2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [128].Yueh MF, He F, Chen C, Vu C, Tripathi A, Knight R, Karin M, Chen S, Tukey RH, Triclosan leads to dysregulation of the metabolic regulator FGF21 exacerbating high fat diet-induced nonalcoholic fatty liver disease, PNAS 117 (49) (2020) 31259–31266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [129].Shi H, Jan J, Hardesty JE, Falkner KC, Prough RA, Balamurugan AN, Mokshagundam SP, Chari ST, Cave MC, Polychlorinated biphenyl exposures differentially regulate hepatic metabolism and pancreatic function: Implications for nonalcoholic steatohepatitis and diabetes, Toxicol. Appl. Pharmacol 363 (2019) 22–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130].Go GY, Lee SJ, Jo A, Lee JR, Kang JS, Yang M, Bae GU, Bisphenol A and estradiol impede myoblast differentiation through down-regulating Akt signaling pathway, Toxicol. Lett 292 (2018) 12–19. [DOI] [PubMed] [Google Scholar]
- [131].Mullainadhan V, Viswanathan MP, Karundevi B, Effect of Bisphenol-A (BPA) on insulin signal transduction and GLUT4 translocation in gastrocnemius muscle of adult male albino rat, Int. J. Biochem. Cell Biol 90 (2017) 38–47. [DOI] [PubMed] [Google Scholar]
- [132].Li B, Guo J, Xi Z, Xu J, Zuo Z, Wang C, Tributyltin in male mice disrupts glucose homeostasis as well as recovery after exposure: mechanism analysis, Arch. Toxicol 91 (10) (2017) 3261–3269. [DOI] [PubMed] [Google Scholar]
- [133].Chiu K, Warner G, Nowak RA, Flaws JA, Mei W, The Impact of Environmental Chemicals on the Gut Microbiome, Toxicological sciences : an official journal of the Society of Toxicology (176(2)) (2020) 253–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134].Rosenfeld CS, Gut Dysbiosis in Animals Due to Environmental Chemical Exposures, Front. Cell. Infect. Microbiol 7 (2017) 396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Claus SP, Guillou H, Ellero-Simatos S, The gut microbiota: a major player in the toxicity of environmental pollutants? npj Biofilms Microbiomes 2 (2016) 16003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Liu KH, Owens JA, Saeedi B, Cohen CE, Bellissimo MP, Naudin C, Darby T, Druzak S, Maner-Smith K, Orr M, Hu X, Fernandes J, Camacho MC, Hunter-Chang S, VanInsberghe D, Ma C, Ganesh T, Yeligar SM, Uppal K, Go Y-M, Alvarez JA, Vos MB, Ziegler TR, Woodworth MH, Kraft CS, Jones RM, Ortlund E, Neish AS, Jones DP, Microbial metabolite delta-valerobetaine is a diet-dependent obesogen, Nature Metabolism 3 (12) (2021) 1694–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Fader KA, Nault R, Doskey CM, Fling RR, Zacharewski TR, 2,3,7,8-Tetrachlorodibenzo-p-dioxin abolishes circadian regulation of hepatic metabolic activity in mice, Sci. Rep 9 (1) (2019) 6514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Jin Y, Zeng Z, Wu Y, Zhang S, Fu Z, Oral Exposure of Mice to Carbendazim Induces Hepatic Lipid Metabolism Disorder and Gut Microbiota Dysbiosis, Toxicological sciences : an official journal of the Society of Toxicology 147 (1) (2015) 116–126. [DOI] [PubMed] [Google Scholar]
- [139].Wang C, Xu C-X, Krager SL, Bottum KM, Liao D-F, Tischkau SA, Aryl Hydrocarbon Receptor Deficiency Enhances Insulin Sensitivity and Reduces PPAR-α Pathway Activity in Mice, Environ. Health Perspect 119 (12) (2011) 1739–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Wang C, Zhang ZM, Xu CX, Tischkau SA, Interplay between Dioxin-mediated signaling and circadian clock: a possible determinant in metabolic homeostasis, Int. J. Mol. Sci 15 (7) (2014) 11700–11712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Regnier SM, Kirkley AG, Ye H, El-Hashani E, Zhang X, Neel BA, Kamau W, Thomas CC, Williams AK, Hayes ET, Massad NL, Johnson DN, Huang L, Zhang C, Sargis RM, Dietary exposure to the endocrine disruptor tolylfluanid promotes global metabolic dysfunction in male mice, Endocrinology 156 (3) (2015) 896–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [142].Kopp R, Martínez IO, Legradi J, Legler J, Exposure to endocrine disrupting chemicals perturbs lipid metabolism and circadian rhythms, J Environ Sci (China) 62 (2017) 133–137. [DOI] [PubMed] [Google Scholar]
- [143].Loganathan N, Salehi A, Chalmers JA, Belsham DD, Bisphenol A Alters Bmal1, Per2, and Rev-Erba mRNA and Requires Bmal1 to Increase Neuropeptide Y Expression in Hypothalamic Neurons, Endocrinology 160 (1) (2019) 181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Bottalico LN, Weljie AM, Cross-species physiological interactions of endocrine disrupting chemicals with the circadian clock, Gen. Comp. Endocrinol 301 (2021), 113650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [145].Nesan D, Feighan KM, Antle MC, Kurrasch DM, Gestational low-dose BPA exposure impacts suprachiasmatic nucleus neurogenesis and circadian activity with transgenerational effects, Sci. Adv 7 (22) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Yin X, Liu Y, Zeb R, Chen F, Chen H, Wang KJ, The intergenerational toxic effects on offspring of medaka fish Oryzias melastigma from parental benzo[a] pyrene exposure via interference of the circadian rhythm, Environmental pollution (Barking, Essex 267 (2020) (1987), 115437. [DOI] [PubMed] [Google Scholar]
- [147].Bansal A, Henao-Mejia J, Simmons RA, Immune System: An Emerging Player in Mediating Effects of Endocrine Disruptors on Metabolic Health, Endocrinology 159 (1) (2018) 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [148].Thompson PA, Khatami M, Baglole CJ, Sun J, Harris SA, Moon EY, Al-Mulla F, Al-Temaimi R, Brown DG, Colacci A, Mondello C, Raju J, Ryan EP, Woodrick J, Scovassi AI, Singh N, Vaccari M, Roy R, Forte S, Memeo L, Salem HK, Amedei A, Hamid RA, Lowe L, Guarnieri T, Bisson WH, Environmental immune disruptors, inflammation and cancer risk, Carcinogenesis 36 (Suppl 1) (2015) S232–S253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [149].Petriello MC, Brandon JA, Hoffman J, Wang C, Tripathi H, Abdel-Latif A, Ye X, Li X, Yang L, Lee E, Soman S, Barney J, Wahlang B, Hennig B, Morris AJ, Dioxin-like PCB 126 Increases Systemic Inflammation and Accelerates Atherosclerosis in Lean LDL Receptor-Deficient Mice, Toxicological sciences : an official journal of the Society of Toxicology 162 (2) (2018) 548–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Snedeker SM, Hay AG, Do interactions between gut ecology and environmental chemicals contribute to obesity and diabetes? Environ. Health Perspect 120 (3) (2012) 332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [151].Winer DA, Winer S, Dranse HJ, Lam TK, Immunologic impact of the intestine in metabolic disease, J Clin Invest 127 (1) (2017) 33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Čolak E, Pap D, The role of oxidative stress in the development of obesity and obesity-related metabolic disorders, Journal of Medical Biochemistry 40 (1) (2021) 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].Li X, Fang P, Mai J, Choi ET, Wang H, Yang X-F, Targeting mitochondrial reactive oxygen species as novel therapy for inflammatory diseases and cancers, Journal of Hematology & Oncology 6 (1) (2013) 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Javadov S, Kozlov AV, Camara AKS, Mitochondria in Health and Diseases, Cells 9 (5) (2020) 1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Marroqui L, Tuduri E, Alonso-Magdalena P, Quesada I, Nadal A, Dos Santos RS, Mitochondria as target of endocrine-disrupting chemicals: implications for type 2 diabetes, The Journal of endocrinology 239 (2) (2018) R27–R45. [DOI] [PubMed] [Google Scholar]
- [156].Bucher S, Le Guillou D, Allard J, Pinon G, Begriche K, Tête A, Sergent O, Lagadic-Gossmann D, Fromenty B, Possible Involvement of Mitochondrial Dysfunction and Oxidative Stress in a Cellular Model of NAFLD Progression Induced by Benzo[a]pyrene/Ethanol CoExposure, Oxid. Med. Cell. Longevity 2018 (2018) 4396403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [157].Zhou Z, Goodrich JM, Strakovsky RS, Mitochondrial Epigenetics and Environmental Health: Making a Case for Endocrine Disrupting Chemicals, Toxicol. Sci 178 (1) (2020) 16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Suter MA, Chen A, Burdine MS, Choudhury M, Harris RA, Lane RH, Friedman JE, Grove KL, Tackett AJ, Aagaard KM, A maternal high-fat diet modulates fetal SIRT1 histone and protein deacetylase activity in nonhuman primates, FASEB journal : official publication of the Federation of American Societies for Experimental Biology 26 (12) (2012) 5106–5114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159].Kratz EM, Sołkiewicz K, Kubis-Kubiak A, Piwowar A, Sirtuins as Important Factors in Pathological States and the Role of Their Molecular Activity Modulators, Int. J. Mol. Sci 22 (2) (2021) 630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [160].Imai S, Armstrong CM, Kaeberlein M, Guarente L, Transcriptional silencing and longevity protein Sir2 is an NAD-dependent histone deacetylase, Nature 403 (6771) (2000) 795–800. [DOI] [PubMed] [Google Scholar]
- [161].Chalkiadaki A, Guarente L, Sirtuins mediate mammalian metabolic responses to nutrient availability, Nat. Rev. Endocrinol 8 (5) (2012) 287–296. [DOI] [PubMed] [Google Scholar]
- [162].Kurylowicz A, In Search of New Therapeutic Targets in Obesity Treatment: Sirtuins, Int. J. Mol. Sci 17 (4) (2016) 572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Kendrick AA, Choudhury M, Rahman SM, McCurdy CE, Friederich M, Van Hove JL, Watson PA, Birdsey N, Bao J, Gius D, Sack MN, Jing E, Kahn CR, Friedman JE, Jonscher KR, Fatty liver is associated with reduced SIRT3 activity and mitochondrial protein hyperacetylation, Biochem. J 433 (3) (2011) 505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [164].Zhang J, Choudhury M, The plasticizer BBP selectively inhibits epigenetic regulator sirtuin during differentiation of C3H10T1/2 stem cell line, Toxicol. In Vitro 39 (2017) 75–83. [DOI] [PubMed] [Google Scholar]
- [165].Zhang J, Ali HI, Bedi YS, Choudhury M, The plasticizer BBP selectively inhibits epigenetic regulator sirtuins, Toxicology 338 (2015) 130–141. [DOI] [PubMed] [Google Scholar]
- [166].Adriani W, Della Seta D, Dessi-Fulgheri F, Farabollini F, Laviola G, Altered profiles of spontaneous novelty seeking, impulsive behavior, and response to D-amphetamine in rats perinatally exposed to Bisphenol A, Environ. Health Perspect 111 (4) (2003) 395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Rodríguez-Carrillo A, Mustieles V, Pérez-Lobato R, Molina-Molina JM, Reina-Pérez I, Vela-Soria F, Rubio S, Olea N, Fernández MF, Bisphenol A and cognitive function in school-age boys: Is BPA predominantly related to behavior? NeuroToxicology 74 (March) (2019) 162–171. [DOI] [PubMed] [Google Scholar]
- [168].Leyrolle Q, Cserjesi R, Mulders MDGH, Zamariola G, Hiel S, Gianfrancesco MA, Rodriguez J, Portheault D, Amadieu C, Leclercq S, Bindels LB, Neyrinck AM, Cani PD, Karkkainen O, Haninheva K, Lanthier N, Trefois P, Paquot N, Cnop M, Thissen JP, Klein O, Luminet O, Delzenne NM, Specific gut microbial, biological, and psychiatric profiling related to binge eating disorders: A cross-sectional study in obese patients, Clinical Nutrition 85 (2020) 162–169. [DOI] [PubMed] [Google Scholar]
- [169].Krentzel AA, Willett JA, Johnson AG, Meitzen J, Estrogen receptor alpha, G-protein coupled estrogen receptor 1, and aromatase: Developmental, sex, and region-specific differences across the rat caudate–putamen, nucleus accumbens core and shell, Journal of Comparative Neurology 529 (4) (2021) 786–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [170].Wise LM, Hernández-Saavedra D, Boas SM, Pan YX, Juraska JM, Perinatal High-Fat Diet and Bisphenol A: Effects on Behavior and Gene Expression in the Medial Prefrontal Cortex, Dev. Neurosci 41 (1–2) (2019) 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171].Fowler N, Russell N, Sisk CL, Johnson AW, Klump KL, The Binge Eating-Prone/Binge Eating-Resistant Animal Model: A Valuable Tool for Examining Neurobiological Underpinnings of Binge Eating, in: Avena NM, Avena NM (Eds.), Animal Models of Eating Disorders, New York, NY, 2021, pp. 7–24. [Google Scholar]
- [172].Griffin MD, Pereira SR, DeBari MK, Abbott RD, Mechanisms of action, chemical characteristics, and model systems of obesogens, BMC Biomed Eng 2 (2020) 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Ribeiro CM, Beserra BTS, Silva NG, Lima CL, Rocha PRS, Coelho MS, Neves F.d.A.R., Amato AA, Exposure to endocrine-disrupting chemicals and anthropometric measures of obesity: a systematic review and meta-analysis, BMJ Open 10(6) (2020) e033509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [174].Perng W, Cantoral A, Soria-Contreras DC, Betanzos-Robledo L, Kordas K, Liu Y, Mora AM, Corvalan C, Pereira A, Cardoso MA, Chavarro JE, Breton CV, Meeker JD, Harley KG, Eskenazi B, Peterson KE, Tellez-Rojo MM, Exposure to obesogenic endocrine disrupting chemicals and obesity among youth of Latino or Hispanic origin in the United States and Latin America: A lifecourse perspective, Obes Rev 22 Suppl 3(Suppl 3) (2021) e13245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [175].De Long NE, Stepita RA, Taylor VH, Holloway AC, Major depressive disorder and diabetes: does serotonin bridge the gap? Curr. Diabetes Rev 11 (2) (2015) 71–78. [DOI] [PubMed] [Google Scholar]
- [176].Verhaegen AA, Van Gaal LF, Drug-induced obesity and its metabolic consequences: a review with a focus on mechanisms and possible therapeutic options, J. Endocrinol. Invest (2017). [DOI] [PubMed] [Google Scholar]
- [177].Solmi M, Fornaro M, Ostinelli EG, Zangani C, Croatto G, Monaco F, Krinitski D, Fusar-Poli P, Correll CU, Safety of 80 antidepressants, antipsychotics, anti-attention-deficit/hyperactivity medications and mood stabilizers in children and adolescents with psychiatric disorders: a large scale systematic meta-review of 78 adverse effects, World Psychiatry 19 (2) (2020) 214–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [178].Himmerich H, Minkwitz J, Kirkby KC, Weight Gain and Metabolic Changes During Treatment with Antipsychotics and Antidepressants, Endocr. Metab. Immune Disord. Drug Targets 15 (4) (2015) 252–260. [DOI] [PubMed] [Google Scholar]
- [179].De Hert M, Dobbelaere M, Sheridan EM, Cohen D, Correll CU, Metabolic and endocrine adverse effects of second-generation antipsychotics in children and adolescents: A systematic review of randomized, placebo controlled trials and guidelines for clinical practice, European psychiatry : the journal of the Association of European Psychiatrists 26 (3) (2011) 144–158. [DOI] [PubMed] [Google Scholar]
- [180].Martínez-Ortega JM, Funes-Godoy S, Díaz-Atienza F, Gutiérrez-Rojas L, Pérez-Costillas L, Gurpegui M, Weight gain and increase of body mass index among children and adolescents treated with antipsychotics: a critical review, Eur. Child Adolesc. Psychiatry 22 (8) (2013) 457–479. [DOI] [PubMed] [Google Scholar]
- [181].Pan SJ, Tan YL, Yao SW, Xin Y, Yang X, Liu J, Xiong J, Fluoxetine induces lipid metabolism abnormalities by acting on the liver in patients and mice with depression, Acta Pharmacol. Sin 39 (9) (2018) 1463–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [182].Flechtner-Mors M, Jenkinson CP, Alt A, Adler G, Ditschuneit HH, Metabolism in adipose tissue in response to citalopram and trimipramine treatment–an in situ microdialysis study, J. Psychiatr. Res 42 (7) (2008) 578–586. [DOI] [PubMed] [Google Scholar]
- [183].Medici V, McClave SA, Miller KR, Common Medications Which Lead to Unintended Alterations in Weight Gain or Organ Lipotoxicity, Curr. Gastroenterol. Rep 18 (1) (2016) 2. [DOI] [PubMed] [Google Scholar]
- [184].Coats AJS, Beta-blockers, hypertension, and weight gain: the farmer, the chicken, and the egg, Hong Kong Med J 26 (1) (2020) 6–7. [DOI] [PubMed] [Google Scholar]
- [185].Christ-Crain M, Kola B, Lolli F, Fekete C, Seboek D, Wittmann G, Feltrin D, Igreja SC, Ajodha S, Harvey-White J, Kunos G, Muller B, Pralong F, Aubert G, Arnaldi G, Giacchetti G, Boscaro M, Grossman AB, Korbonits M, AMP-activated protein kinase mediates glucocorticoid-induced metabolic changes: a novel mechanism in Cushing’s syndrome, FASEB journal : official publication of the Federation of American Societies for Experimental Biology 22 (6) (2008) 1672–1683. [DOI] [PubMed] [Google Scholar]
- [186].Newbold RR, Padilla-Banks E, Jefferson WN, Environmental estrogens and obesity, Mol. Cell. Endocrinol 304 (1–2) (2009) 84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [187].Mackenbach JP, Damhuis RA, Been JV, The effects of smoking on health: growth of knowledge reveals even grimmer picture, Ned. Tijdschr. Geneeskd 160 (2017) D869. [PubMed] [Google Scholar]
- [188].Green AJ, Hoyo C, Mattingly CJ, Luo Y, Tzeng J-Y, Murphy SK, Buchwalter DB, Planchart A, Cadmium exposure increases the risk of juvenile obesity: a human and zebrafish comparative study, International Journal of Obesity 42 (7) (2018) 1285–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [189].Kim J-Y, Kim S-J, Bae MA, Kim J-R, Cho K-H, Cadmium exposure exacerbates severe hyperlipidemia and fatty liver changes in zebrafish via impairment of high-density lipoproteins functionality, Toxicology in Vitro 47 (2018) 249–258 %U https://linkinghub.elsevier.com/retrieve/pii/S0887233317303582. [DOI] [PubMed] [Google Scholar]
- [190].Bucher S, Tête A, Podechard N, Liamin M, Le Guillou D, Chevanne M, Coulouarn C, Imran M, Gallais I, Fernier M, Hamdaoui Q, Robin M-A, Sergent O, Fromenty B, Lagadic-Gossmann D, Co-exposure to benzo[a]pyrene and ethanol induces a pathological progression of liver steatosis in vitro and in vivo, Sci. Rep 8 (1) (2018) 5963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [191].Behl M, Rao D, Aagaard K, Davidson TL, Levin ED, Slotkin TA, Srinivasan S, Wallinga D, White MF, Walker VR, Thayer KA, Holloway AC, Evaluation of the association between maternal smoking, childhood obesity, and metabolic disorders: a national toxicology program workshop review, Environ. Health Perspect 121 (2) (2013) 170–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [192].Sinha-Hikim AP, Sinha-Hikim I, Friedman TC, Connection of Nicotine to Diet-Induced Obesity and Non-Alcoholic Fatty Liver Disease: Cellular and Mechanistic Insights, Front. Endocrinol 8 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [193].Pinheiro CR, Moura EG, Manhães AC, Fraga MC, Claudio-Neto S, Younes-Rapozo V, Santos-Silva AP, Lotufo BM, Oliveira E, Lisboa PC, Maternal nicotine exposure during lactation alters food preference, anxiety-like behavior and the brain dopaminergic reward system in the adult rat offspring, Physiol. Behav 149 (2015) 131–141. [DOI] [PubMed] [Google Scholar]
- [194].Lee KW, Abrahamowicz M, Leonard GT, Richer L, Perron M, Veillette S, Reischl E, Bouchard L, Gaudet D, Paus T, Pausova Z, Prenatal exposure to cigarette smoke interacts with OPRM1 to modulate dietary preference for fat, J. Psychiatry Neurosci 40 (1) (2015) 38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [195].Chen HJ, Li GL, Zhang WX, Fan J, Hu L, Zhang L, Zhang J, Yan YE, Maternal nicotine exposure during pregnancy and lactation induces brown adipose tissue whitening in female offspring, Toxicol. Appl. Pharmacol 409 (2020), 115298. [DOI] [PubMed] [Google Scholar]
- [196].Huang LZ, Winzer-Serhan UH, Nicotine regulates mRNA expression of feeding peptides in the arcuate nucleus in neonatal rat pups, Dev Neurobiol 67 (3) (2007) 363–377. [DOI] [PubMed] [Google Scholar]
- [197].Younes-Rapozo V, Moura EG, Manhães AC, Pinheiro CR, Santos-Silva AP, de Oliveira E, Lisboa PC, Maternal nicotine exposure during lactation alters hypothalamic neuropeptides expression in the adult rat progeny, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 58 (2013) 158–168. [DOI] [PubMed] [Google Scholar]
- [198].Somm E, Schwitzgebel VM, Vauthay DM, Camm EJ, Chen CY, Giacobino JP, Sizonenko SV, Aubert ML, Huppi PS, Prenatal nicotine exposure alters early pancreatic islet and adipose tissue development with consequences on the control of body weight and glucose metabolism later in life, Endocrinology 149 (12) (2008) 6289–6299. [DOI] [PubMed] [Google Scholar]
- [199].Fan J, Ping J, Zhang WX, Rao YS, Liu HX, Zhang J, Yan YE, Prenatal and lactation nicotine exposure affects morphology and function of brown adipose tissue in male rat offspring, Ultrastruct. Pathol 40 (5) (2016) 288–295. [DOI] [PubMed] [Google Scholar]
- [200].Peixoto TC, Moura EG, Soares PN, Bertasso IM, Pietrobon CB, Caramez FAH, Miranda RA, Oliveira E, Manhães AC, Lisboa PC, Nicotine exposure during breastfeeding reduces sympathetic activity in brown adipose tissue and increases in white adipose tissue in adult rats: Sex-related differences, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 140 (2020), 111328. [DOI] [PubMed] [Google Scholar]
- [201].Ma N, Nicholson CJ, Wong M, Holloway AC, Hardy DB, Fetal and neonatal exposure to nicotine leads to augmented hepatic and circulating triglycerides in adult male offspring due to increased expression of fatty acid synthase, Toxicol. Appl. Pharmacol 275 (1) (2014) 1–11. [DOI] [PubMed] [Google Scholar]
- [202].Blüher M, Adipose tissue dysfunction contributes to obesity related metabolic diseases, Best practice & research, Clinical endocrinology & metabolism 27 (2) (2013) 163–177. [DOI] [PubMed] [Google Scholar]
- [203].Cameron JD, Doucet É, Adamo KB, Walker M, Tirelli A, Barnes JD, Hafizi K, Murray M, Goldfield GS, Effects of prenatal exposure to cigarettes on anthropometrics, energy intake, energy expenditure, and screen time in children, Physiol. Behav 194 (2018) 394–400. [DOI] [PubMed] [Google Scholar]
- [204].Moschonis G, Kaliora AC, Karatzi K, Michaletos A, Lambrinou CP, Karachaliou AK, Chrousos GP, Lionis C, Manios Y, Perinatal, sociodemographic and lifestyle correlates of increased total and visceral fat mass levels in schoolchildren in Greece: the Healthy Growth Study, Public Health Nutr. 20 (4) (2017) 660–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Oken E, Levitan EB, Gillman MW, Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis, International journal of obesity (2005) 32(2) (2008) 201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [206].Rayfield S, Plugge E, Systematic review and meta-analysis of the association between maternal smoking in pregnancy and childhood overweight and obesity, J. Epidemiol. Community Health 71 (2) (2017) 162–173. [DOI] [PubMed] [Google Scholar]
- [207].Philips EM, Santos S, Trasande L, Aurrekoetxea JJ, Barros H, von Berg A, Bergström A, Bird PK, Brescianini S, Ní Chaoimh C, Charles MA, Chatzi L, Chevrier C, Chrousos GP, Costet N, Criswell R, Crozier S, Eggesbø M, Fantini MP, Farchi S, Forastiere F, van Gelder MMHJ, Georgiu V, Godfrey KM, Gori D, Hanke W, Heude B, Hryhorczuk D, Iñiguez C, Inskip H, Karvonen AM, Kenny LC, Kull I, Lawlor DA, Lehmann I, Magnus P, Manios Y, Melén E, Mommers M, Morgen CS, Moschonis G, Murray D, Nohr EA, Nybo Andersen AM, Oken E, Oostvogels AJJM, Papadopoulou E, Pekkanen J, Pizzi C, Polanska K, Porta D, Richiardi L, Rifas-Shiman SL, Roeleveld N, Rusconi F, Santos AC, Sørensen TIA, Standl M, Stoltenberg C, Sunyer J, Thiering E, Thijs C, Torrent M, Vrijkotte TGM, Wright J, Zvinchuk O, Gaillard R, Jaddoe VWV, Changes in parental smoking during pregnancy and risks of adverse birth outcomes and childhood overweight in Europe and North America: An individual participant data meta-analysis of 229,000 singleton births, PLoS Med. 17 (8) (2020), e1003182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [208].Vrijheid M, Fossati S, Maitre L, Marquez S, Roumeliotaki T, Agier L, Andrusaityte S, Cadiou S, Casas M, de Castro M, Dedele A, Donaire-Gonzalez D, Grazuleviciene R, Haug LS, McEachan R, Meltzer HM, Papadopouplou E, Robinson O, Sakhi AK, Siroux V, Sunyer J, Schwarze PE, Tamayo-Uria I, Urquiza J, Vafeiadi M, Valentin A, Warembourg C, Wright J, Nieuwenhuijsen MJ, Thomsen C, Basagana X, Slama R, Chatzi L, Early-Life Environmental Exposures and Childhood Obesity: An Exposome-Wide Approach, Environ. Health Perspect 128 (6) (2020) 67009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [209].Albers L, Sobotzki C, Kuß O, Ajslev T, Batista RF, Bettiol H, Brabin B, Buka SL, Cardoso VC, Clifton VL, Devereux G, Gilman SE, Grzeskowiak LE, Heinrich J, Hummel S, Jacobsen GW, Jones G, Koshy G, Morgen CS, Oken E, Paus T, Pausova Z, Rifas-Shiman SL, Sharma AJ, da Silva AA, Sørensen TI, Thiering E, Turner S, Vik T, von Kries R, Maternal smoking during pregnancy and offspring overweight: is there a dose-response relationship? An individual patient data meta-analysis, International journal of obesity (2005) 42(7) (2018) 1249–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [210].Chen HJ, Li GL, Sun A, Peng DS, Zhang WX, Yan YE, Age Differences in the Relationship between Secondhand Smoke Exposure and Risk of Metabolic Syndrome: A Meta-Analysis, Int. J. Environ. Res. Public Health 16 (8) (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [211].Oldereid NB, Wennerholm UB, Pinborg A, Loft A, Laivuori H, Petzold M, Romundstad LB, Söderström-Anttila V, Bergh C, The effect of paternal factors on perinatal and paediatric outcomes: a systematic review and meta-analysis, Human reproduction update 24 (3) (2018) 320–389. [DOI] [PubMed] [Google Scholar]
- [212].Nadhiroh SR, Djokosujono K, Utari DM, The association between secondhand smoke exposure and growth outcomes of children: A systematic literature review, Tob Induc Dis 18 (2020) 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [213].Chaiton M, Holloway A, Population attributable risk of smoking during pregnancy on obesity in offspring, Can. J. Public Health 107 (3) (2016), e336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [214].Harris HR, Willett WC, Michels KB, Parental smoking during pregnancy and risk of overweight and obesity in the daughter, International journal of obesity (2005) 37(10) (2013) 1356–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [215].Pérez-Bermejo M, Mas-Pérez I, Murillo-Llorente MT, The Role of the Bisphenol A in Diabetes and Obesity, Biomedicines 9 (6) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [216].Qiu W, Liu S, Yang F, Dong P, Yang M, Wong M, Zheng C, Metabolism disruption analysis of zebrafish larvae in response to BPA and BPA analogs based on RNA-Seq technique, Ecotoxicol. Environ. Saf 174 (2019) 181–188. [DOI] [PubMed] [Google Scholar]
- [217].Ji Z, Liu J, Sakkiah S, Guo W, Hong H, BPA Replacement Compounds: Current Status and Perspectives, ACS Sustainable Chem. Eng 9 (6) (2021) 2433–2446. [Google Scholar]
- [218].Mesnage R, Phedonos A, Arno M, Balu S, Corton JC, Antoniou MN, Editor’s Highlight: Transcriptome Profiling Reveals Bisphenol A Alternatives Activate Estrogen Receptor Alpha in Human Breast Cancer Cells, Toxicological sciences : an official journal of the Society of Toxicology 158 (2) (2017) 431–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [219].Ougier E, Zeman F, Antignac JP, Rousselle C, Lange R, Kolossa-Gehring M, Apel P, Human biomonitoring initiative (HBM4EU): Human biomonitoring guidance values (HBM-GVs) derived for bisphenol A, Environ. Int 154 (2021), 106563. [DOI] [PubMed] [Google Scholar]
- [220].Bousoumah R, Leso V, Iavicoli I, Huuskonen P, Viegas S, Porras SP, Santonen T, Frery N, Robert A, Ndaw S, Biomonitoring of occupational exposure to bisphenol A, bisphenol S and bisphenol F: A systematic review, The Science of the total environment 783 (2021), 146905. [DOI] [PubMed] [Google Scholar]
- [221].Hines CJ, Jackson MV, Deddens JA, Clark JC, Ye X, Christianson AL, Meadows JW, Calafat AM, Urinary Bisphenol A (BPA) Concentrations among Workers in Industries that Manufacture and Use BPA in the USA, Ann Work Expo Health 61 (2) (2017) 164–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [222].Longo M, Zatterale F, Naderi J, Nigro C, Oriente F, Formisano P, Miele C, Beguinot F, Low-dose Bisphenol-A Promotes Epigenetic Changes at Ppargamma Promoter in Adipose Precursor Cells, Nutrients 12 (11) (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [223].Huc L, Lemarié A, Guéraud F, Héliès-Toussaint C, Low concentrations of bisphenol A induce lipid accumulation mediated by the production of reactive oxygen species in the mitochondria of HepG2 cells, Toxicol. In Vitro 26 (5) (2012) 709–717. [DOI] [PubMed] [Google Scholar]
- [224].Peyre L, Rouimi P, de Sousa G, Héliès-Toussaint C, Carré B, Barcellini S, Chagnon M-C, Rahmani R, Comparative study of bisphenol A and its analogue bisphenol S on human hepatic cells: A focus on their potential involvement in nonalcoholic fatty liver disease, Food Chem. Toxicol 70 (2014) 9–18. [DOI] [PubMed] [Google Scholar]
- [225].Boucher JG, Husain M, Rowan-Carroll A, Williams A, Yauk CL, Atlas E, Identification of mechanisms of action of bisphenol a-induced human preadipocyte differentiation by transcriptional profiling, Obesity (Silver Spring) 22 (11) (2014) 2333–2343. [DOI] [PubMed] [Google Scholar]
- [226].Martinez MA, Blanco J, Rovira J, Kumar V, Domingo JL, Schuhmacher M, Bisphenol A analogues (BPS and BPF) present a greater obesogenic capacity in 3T3-L1 cell line, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 140 (2020), 111298. [DOI] [PubMed] [Google Scholar]
- [227].Skledar DG, Carino A, Trontelj J, Troberg J, Distrutti E, Marchiano S, Tomasic T, Zega A, Finel M, Fiorucci S, Masic LP, Endocrine activities and adipogenic effects of bisphenol AF and its main metabolite, Chemosphere 215 (2019) 870–880. [DOI] [PubMed] [Google Scholar]
- [228].Riu A, Grimaldi M, le Maire A, Bey G, Phillips K, Boulahtouf A, Perdu E, Zalko D, Bourguet W, Balaguer P, Peroxisome proliferator-activated receptor gamma is a target for halogenated analogs of bisphenol A, Environ. Health Perspect 119 (9) (2011) 1227–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [229].Ariemma F, D’Esposito V, Liguoro D, Oriente F, Cabaro S, Liotti A, Cimmino I, Longo M, Beguinot F, Formisano P, Valentino R, Low-Dose bisphenol-A impairs adipogenesis and generates dysfunctional 3T3-L1 adipocytes, PLoS ONE 11 (3) (2016) 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [230].Martella A, Silvestri C, Maradonna F, Gioacchini G, Allarà M, Radaelli G, Overby DR, Di Marzo V, Carnevali O, Bisphenol A Induces Fatty Liver by an Endocannabinoid-Mediated Positive Feedback Loop, Endocrinology 157 (5) (2016) 1751–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [231].Renaud L, Silveira W.A.d., Hazard ES, Simpson J, Falcinelli S, Chung D, Carnevali O, Hardiman G, The Plasticizer Bisphenol A Perturbs the Hepatic Epigenome: A Systems Level Analysis of the miRNome, Genes 8(10) (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [232].Santangeli S, Notarstefano V, Maradonna F, Giorgini E, Gioacchini G, Forner-Piquer I, Habibi HR, Carnevali O, Effects of diethylene glycol dibenzoate and Bisphenol A on the lipid metabolism of Danio rerio, Sci. Total Environ 636 (2018) 641–655. [DOI] [PubMed] [Google Scholar]
- [233].Wang W, Zhang X, Wang Z, Qin J, Wang W, Tian H, Ru S, Bisphenol S induces obesogenic effects through deregulating lipid metabolism in zebrafish (Danio rerio) larvae, Chemosphere 199 (2018) 286–296. [DOI] [PubMed] [Google Scholar]
- [234].Riu A, McCollum CW, Pinto CL, Grimaldi M, Hillenweck A, Perdu E, Zalko D, Bernard L, Laudet V, Balaguer P, Bondesson M, Gustafsson J-A, Halogenated Bisphenol-A Analogs Act as Obesogens in Zebrafish Larvae (Danio rerio), Toxicol. Sci (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [235].Tian S, Yan S, Meng Z, Huang S, Sun W, Jia M, Teng M, Zhou Z, Zhu W, New insights into bisphenols induced obesity in zebrafish (Danio rerio): Activation of cannabinoid receptor CB1, J. Hazard. Mater 418 (2021), 126100. [DOI] [PubMed] [Google Scholar]
- [236].Rochester JR, Bolden AL, Bisphenol S and F: A Systematic Review and Comparison of the Hormonal Activity of Bisphenol A Substitutes, Environ. Health Perspect 123 (7) (2015) 643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [237].Alonso-Magdalena P, Garcia-Arevalo M, Quesada I, Nadal A, Bisphenol-A treatment during pregnancy in mice: a new window of susceptibility for the development of diabetes in mothers later in life, Endocrinology 156 (5) (2015) 1659–1670. [DOI] [PubMed] [Google Scholar]
- [238].Wassenaar PNH, Trasande L, Legler J, Systematic Review and Meta-Analysis of Early-Life Exposure to Bisphenol A and Obesity-Related Outcomes in Rodents, Environ. Health Perspect 125 (10) (2017), 106001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [239].Angle BM, Do RP, Ponzi D, Stahlhut RW, Drury BE, Nagel SC, Welshons WV, Besch-Williford CL, Palanza P, Parmigiani S, vom Saal FS, Taylor JA, Metabolic disruption in male mice due to fetal exposure to low but not high doses of bisphenol A (BPA): Evidence for effects on body weight, food intake, adipocytes, leptin, adiponectin, insulin and glucose regulation, Reprod. Toxicol 42 (2013) 256–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [240].Rubin BS, Paranjpe M, DaFonte T, Schaeberle C, Soto AM, Obin M, Greenberg AS, Perinatal BPA exposure alters body weight and composition in a dose specific and sex specific manner: The addition of peripubertal exposure exacerbates adverse effects in female mice, Reprod. Toxicol 68 (2017) 130–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [241].Somm E, Schwitzgebel VM, Toulotte A, Cederroth CR, Combescure C, Nef S, Aubert ML, Huppi PS, Perinatal exposure to bisphenol a alters early adipogenesis in the rat, Environ. Health Perspect 117 (10) (2009) 1549–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [242].Rubin BS, Soto AM, Bisphenol A: Perinatal exposure and body weight, Mol. Cell. Endocrinol 304 (1–2) (2009) 55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [243].Desai M, Ferrini MG, Han G, Jellyman JK, Ross MG, In vivo maternal and in vitro BPA exposure effects on hypothalamic neurogenesis and appetite regulators, Environ. Res 164 (2018) 45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [244].MacKay H, Patterson ZR, Abizaid A, Perinatal Exposure to Low-Dose Bisphenol-A Disrupts the Structural and Functional Development of the Hypothalamic Feeding Circuitry, Endocrinology 158 (4) (2017) 768–777. [DOI] [PubMed] [Google Scholar]
- [245].Stoker C, Andreoli MF, Kass L, Bosquiazzo VL, Rossetti MF, Canesini G, Luque EH, Ramos JG, Perinatal exposure to bisphenol A (BPA) impairs neuroendocrine mechanisms regulating food intake and kisspetin system in adult male rats, Evidences of metabolic disruptor hypothesis, Mol Cell Endocrinol 499 (2020), 110614. [DOI] [PubMed] [Google Scholar]
- [246].Yang M, Chen M, Wang J, Xu M, Sun J, Ding L, Lv X, Ma Q, Bi Y, Liu R, Hong J, Ning G, Bisphenol A promotes adiposity and inflammation in a nonmonotonic dose-response way in five-week old male and female C57BL/6J mice fed a low-calorie diet, Endocrinology (2016) en20151926. [DOI] [PubMed] [Google Scholar]
- [247].Ivry Del Moral L, Le Corre L, Poirier H, Niot I, Truntzer T, Merlin JF, Rouimi P, Besnard P, Rahmani R, Chagnon MC, Obesogen effects after perinatal exposure of 4,4’-sulfonyldiphenol (Bisphenol S) in C57BL/6 mice, Toxicology 357–358 (2016) 11–20. [DOI] [PubMed] [Google Scholar]
- [248].Ribeiro CM, Beserra BTS, Silva NG, Lima CL, Rocha PRS, Coelho MS, Neves FAR, Amato AA, Exposure to endocrine-disrupting chemicals and anthropometric measures of obesity: a systematic review and meta-analysis, BMJ Open 10 (6) (2020), e033509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [249].Song Y, Hauser R, Hu FB, Franke AA, Liu S, Sun Q, Urinary concentrations of bisphenol A and phthalate metabolites and weight change: a prospective investigation in US women, International journal of obesity (2005) 38(12) (2014) 1532–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [250].Hao M, Ding L, Xuan L, Wang T, Li M, Zhao Z, Lu J, Xu Y, Chen Y, Wang W, Bi Y, Xu M, Ning G, Urinary bisphenol A concentration and the risk of central obesity in Chinese adults: A prospective study, J. Diabetes 10 (6) (2018) 442–448. [DOI] [PubMed] [Google Scholar]
- [251].Braun JM, Li N, Arbuckle TE, Dodds L, Massarelli I, Fraser WD, Lanphear BP, Muckle G, Association between gestational urinary bisphenol a concentrations and adiposity in young children: The MIREC study, Environ. Res 172 (2019) 454–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [252].Hoepner LA, Whyatt RM, Widen EM, Hassoun A, Oberfield SE, Mueller NT, Diaz D, Calafat AM, Perera FP, Rundle AG, Bisphenol A and Adiposity in an Inner-City Birth Cohort, Environ. Health Perspect 124 (10) (2016) 1644–1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [253].Agay-Shay K, Martinez D, Valvi D, Garcia-Esteban R, Basagana X, Robinson O, Casas M, Sunyer J, Vrijheid M, Exposure to Endocrine-Disrupting Chemicals during Pregnancy and Weight at 7 Years of Age: A Multi-pollutant Approach, Environ. Health Perspect 123 (10) (2015) 1030–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [254].Vafeiadi M, Roumeliotaki T, Myridakis A, Chalkiadaki G, Fthenou E, Dermitzaki E, Karachaliou M, Sarri K, Vassilaki M, Stephanou EG, Kogevinas M, Chatzi L, Association of early life exposure to bisphenol A with obesity and cardiometabolic traits in childhood, Environ. Res 146 (2016) 379–387. [DOI] [PubMed] [Google Scholar]
- [255].Yang TC, Peterson KE, Meeker JD, Sánchez BN, Zhang Z, Cantoral A, Solano M, Tellez-Rojo MM, Bisphenol A and phthalates in utero and in childhood: association with child BMI z-score and adiposity, Environ. Res 156 (2017) 326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [256].Buckley JP, Herring AH, Wolff MS, Calafat AM, Engel SM, Prenatal exposure to environmental phenols and childhood fat mass in the Mount Sinai Children’s Environmental Health Study, Environ. Int 91 (2016) 350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [257].Harley KG, Aguilar Schall R, Chevrier J, Tyler K, Aguirre H, Bradman A, Holland NT, Lustig RH, Calafat AM, Eskenazi B, Prenatal and postnatal bisphenol A exposure and body mass index in childhood in the CHAMACOS cohort, Environ Health Perspect 121(4) (2013) 514–20, 520e1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [258].Ryan KK, Haller AM, Sorrell JE, Woods SC, Jandacek RJ, Seeley RJ, Perinatal exposure to bisphenol-A and the development of metabolic syndrome in CD-1 mice, Endocrinology 151 (6) (2010) 2603–2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [259].Rolland M, Lyon-Caen S, Sakhi AK, Pin I, Sabaredzovic A, Thomsen C, Slama R, Philippat C, Exposure to phenols during pregnancy and the first year of life in a new type of couple-child cohort relying on repeated urine biospecimens, Environ. Int 139 (2020), 105678. [DOI] [PubMed] [Google Scholar]
- [260].Petersen JH, Breindahl T, Plasticizers in total diet samples, baby food and infant formulae, Food Addit. Contam 17 (2) (2000) 133–141. [DOI] [PubMed] [Google Scholar]
- [261].Genco M, Anderson-Shaw L, Sargis RM, Unwitting Accomplices: Endocrine Disruptors Confounding Clinical Care, The Journal of clinical endocrinology and metabolism 105 (10) (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [262].Bowman JD, Choudhury M, Phthalates in neonatal health: friend or foe? J Dev Orig Health Dis 7 (6) (2016) 652–664. [DOI] [PubMed] [Google Scholar]
- [263].Zhang J, Powell CA, Kay MK, Park MH, Meruvu S, Sonkar R, Choudhury M, A moderate physiological dose of benzyl butyl phthalate exacerbates the high fat diet-induced diabesity in male mice, Toxicol. Res (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [264].Rajagopal G, Bhaskaran RS, Karundevi B, Developmental exposure to DEHP alters hepatic glucose uptake and transcriptional regulation of GLUT2 in rat male offspring, Toxicology 413 (2019) 56–64. [DOI] [PubMed] [Google Scholar]
- [265].Hao C, Cheng X, Guo J, Xia H, Ma X, Perinatal exposure to diethyl-hexylphthalate induces obesity in mice, Front Biosci (Elite Ed) 5 (2013) 725–733. [DOI] [PubMed] [Google Scholar]
- [266].Schaedlich K, Gebauer S, Hunger L, Beier L-S, Koch HM, Wabitsch M, Fischer B, Ernst J, DEHP deregulates adipokine levels and impairs fatty acid storage in human SGBS-adipocytes, Sci. Rep 8 (1) (2018) 3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [267].Biemann R, Navarrete Santos A, Navarrete Santos A, Riemann D, Knelangen J, Bluher M, Koch H, Fischer B, Endocrine disrupting chemicals affect the adipogenic differentiation of mesenchymal stem cells in distinct ontogenetic windows, Biochem. Biophys. Res. Commun 417 (2) (2012) 747–752. [DOI] [PubMed] [Google Scholar]
- [268].Klöting N, Hesselbarth N, Gericke M, Kunath A, Biemann R, Chakaroun R, Kosacka J, Kovacs P, Kern M, Stumvoll M, Fischer B, Rolle-Kampczyk U, Feltens R, Otto W, Wissenbach DK, von Bergen M, Blüher M, Di-(2-Ethylhexyl)-Phthalate (DEHP) Causes Impaired Adipocyte Function and Alters Serum Metabolites, PLoS ONE 10 (12) (2015), e0143190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [269].Chiu CY, Sun SC, Chiang CK, Wang CC, Chan DC, Chen HJ, Liu SH, Yang RS, Plasticizer di(2-ethylhexyl)phthalate interferes with osteoblastogenesis and adipogenesis in a mouse model, Journal of orthopaedic research : official publication of the Orthopaedic Research Society 36 (4) (2018) 1124–1134. [DOI] [PubMed] [Google Scholar]
- [270].Feige JN, Gelman L, Rossi D, Zoete V, Metivier R, Tudor C, Anghel SI, Grosdidier A, Lathion C, Engelborghs Y, Michielin O, Wahli W, Desvergne B, The endocrine disruptor monoethyl-hexyl-phthalate is a selective peroxisome proliferator-activated receptor gamma modulator that promotes adipogenesis, J. Biol. Chem 282 (26) (2007) 19152–19166. [DOI] [PubMed] [Google Scholar]
- [271].Hurst CH, Waxman DJ, Activation of PPARalpha and PPARgamma by environmental phthalate monoesters, Toxicological sciences : an official journal of the Society of Toxicology 74 (2) (2003) 297–308. [DOI] [PubMed] [Google Scholar]
- [272].Hatch EE, Association of urinary phthalate metabolite concentrations with body mass index and waist circumference: a cross-sectional study of NHANES data, 1999–2002, Environ. Health 7 (2008) 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [273].Desvergne B, Feige JN, Casals-Casas C, PPAR-mediated activity of phthalates: A link to the obesity epidemic? Mol. Cell. Endocrinol 304 (1–2) (2009) 43–48. [DOI] [PubMed] [Google Scholar]
- [274].Ellero-Simatos S, Claus SP, Benelli C, Forest C, Letourneur F, Cagnard N, Beaune PH, de Waziers I, Combined Transcriptomic–1H NMR Metabonomic Study Reveals That Monoethylhexyl Phthalate Stimulates Adipogenesis and Glyceroneogenesis in Human Adipocytes, J. Proteome Res 10 (12) (2011) 5493–5502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [275].Buerger AN, Schmidt J, Chase A, Paixao C, Patel TN, Brumback BA, Kane AS, Martyniuk CJ, Bisesi JH, Examining the responses of the zebrafish (Danio rerio) gastrointestinal system to the suspected obesogen diethylhexyl phthalate, Environmental Pollution (Barking, Essex 245 (2019) (1987) 1086–1094. [DOI] [PubMed] [Google Scholar]
- [276].Buerger AN, Dillon DT, Schmidt J, Yang T, Zubcevic J, Martyniuk CJ, Bisesi JH, Gastrointestinal dysbiosis following diethylhexyl phthalate exposure in zebrafish (Danio rerio): Altered microbial diversity, functionality, and network connectivity, Environmental Pollution (Barking, Essex: 1987) 265(Pt B) (2020) 114496. [DOI] [PubMed] [Google Scholar]
- [277].Jacobs HM, Sant KE, Basnet A, Williams LM, Moss JB, Timme-Laragy AR, Embryonic exposure to Mono(2-ethylhexyl) phthalate (MEHP) disrupts pancreatic organogenesis in zebrafish (Danio rerio), Chemosphere 195 (2018) 498–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [278].Tête A, Gallais I, Imran M, Legoff L, Martin-Chouly C, Sparfel L, Bescher M, Sergent O, Podechard N, Lagadic-Gossmann D, MEHP/ethanol co-exposure favors the death of steatotic hepatocytes, possibly through CYP4A and ADH involvement, Food Chem. Toxicol 146 (2020), 111798. [DOI] [PubMed] [Google Scholar]
- [279].Chen H, Zhang W, Rui B-B, Yang S-M, Xu W-P, Wei W, Di(2-ethylhexyl) phthalate exacerbates non-alcoholic fatty liver in rats and its potential mechanisms, Environ. Toxicol. Pharmacol 42 (2016) 38–44. [DOI] [PubMed] [Google Scholar]
- [280].Zhang W, Shen X-Y, Zhang W-W, Chen H, Xu W-P, Wei W, The effects of di 2-ethyl hexyl phthalate (DEHP) on cellular lipid accumulation in HepG2 cells and its potential mechanisms in the molecular level, Toxicol. Mech. Methods 27 (4) (2017) 245–252. [DOI] [PubMed] [Google Scholar]
- [281].Zhang Y, Wang S, Zhao T, Yang L, Guo S, Shi Y, Zhang X, Zhou L, Ye L, Mono-2-ethylhexyl phthalate (MEHP) promoted lipid accumulation via JAK2/STAT5 and aggravated oxidative stress in BRL-3A cells, Ecotoxicol. Environ. Saf 184 (2019), 109611. [DOI] [PubMed] [Google Scholar]
- [282].Guo W, Han J, Wu S, Shi X, Wang Q, Zhou B, Bis(2-ethylhexyl)-2,3,4,5-tetrabromophthalate Affects Lipid Metabolism in Zebrafish Larvae via DNA Methylation Modification, Environ. Sci. Technol 54 (1) (2020) 355–363. [DOI] [PubMed] [Google Scholar]
- [283].Wassenaar PNH, Legler J, Systematic review and meta-analysis of early life exposure to di(2-ethylhexyl) phthalate and obesity related outcomes in rodents, Chemosphere 188 (2017) 174–181. [DOI] [PubMed] [Google Scholar]
- [284].Schmidt J-S, Schaedlich K, Fiandanese N, Pocar P, Fischer B, Effects of di(2-ethylhexyl) phthalate (DEHP) on female fertility and adipogenesis in C3H/N mice, Environ. Health Perspect 120 (8) (2012) 1123–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [285].Lv Z, Cheng J, Huang S, Zhang Y, Wu S, Qiu Y, Geng Y, Zhang Q, Huang G, Ma Q, Xie X, Zhou S, Wu T, Ke Y, DEHP induces obesity and hypothyroidism through both central and peripheral pathways in C3H/He mice, Obesity (Silver Spring) 24 (2) (2016) 368–378. [DOI] [PubMed] [Google Scholar]
- [286].Hao C, Cheng X, Xia H, Ma X, The endocrine disruptor mono-(2-ethylhexyl) phthalate promotes adipocyte differentiation and induces obesity in mice, Biosci. Rep 32 (6) (2012) 619–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [287].Moody L, Kougias D, Jung PM, Digan I, Hong A, Gorski A, Chen H, Juraska J, Pan Y-X, Perinatal phthalate and high-fat diet exposure induce sex-specific changes in adipocyte size and DNA methylation, The Journal of nutritional biochemistry 65 (2019) 15–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [288].Majeed KA, Ur Rehman H, Yousaf MS, Zaneb H, Rabbani I, Tahir SK, Rashid MA, Sub-chronic exposure to low concentration of dibutyl phthalate affects anthropometric parameters and markers of obesity in rats, Environ. Sci. Pollut. Res. Int 24 (32) (2017) 25462–25467. [DOI] [PubMed] [Google Scholar]
- [289].Harley KG, Berger K, Rauch S, Kogut K, Claus Henn B, Calafat AM, Huen K, Eskenazi B, Holland N, Association of prenatal urinary phthalate metabolite concentrations and childhood BMI and obesity, Pediatr. Res 82 (3) (2017) 405–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [290].Buckley JP, Engel SM, Braun JM, Whyatt RM, Daniels JL, Mendez MA, Richardson DB, Xu Y, Calafat AM, Wolff MS, Lanphear BP, Herring AH, Rundle AG, Prenatal Phthalate Exposures and Body Mass Index Among 4- to 7-Year-old Children: A Pooled Analysis, Epidemiology (Cambridge, Mass.) 27 (3) (2016) 449–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [291].Kim JH, Park H, Lee J, Cho G, Choi S, Choi G, Kim SY, Eun S-H, Suh E, Kim SK, Kim H-J, Kim G-H, Lee JJ, Kim YD, Eom S, Kim S, Moon H-B, Park J, Choi K, Kim S, Kim S, Association of diethylhexyl phthalate with obesity-related markers and body mass change from birth to 3 months of age, J. Epidemiol. Community Health 70 (5) (2016) 466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [292].Valvi D, Casas M, Romaguera D, Monfort N, Ventura R, Martinez D, Sunyer J, Vrijheid M, Prenatal Phthalate Exposure and Childhood Growth and Blood Pressure: Evidence from the Spanish INMA-Sabadell Birth Cohort Study, Environ. Health Perspect 123 (10) (2015) 1022–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [293].Botton J, Philippat C, Calafat AM, Carles S, Charles M-A, Slama R, E.m.-c.c.s. g. the, Phthalate pregnancy exposure and male offspring growth from the intrauterine period to five years of age, Environ. Res 151 (2016) 601–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [294].Hou JW, Lin CL, Tsai YA, Chang CH, Liao KW, Yu CJ, Yang W, Lee MJ, Huang PC, Sun CW, Wang YH, Lin FR, Wu WC, Lee MC, Pan WH, Chen BH, Wu MT, Chen CC, Wang SL, Lee CC, Hsiung CA, Chen ML, The effects of phthalate and nonylphenol exposure on body size and secondary sexual characteristics during puberty, Int. J. Hyg. Environ. Health 218 (7) (2015) 603–615. [DOI] [PubMed] [Google Scholar]
- [295].Sol CM, Santos S, Duijts L, Asimakopoulos AG, Martinez-Moral M-P, Kannan K, Philips EM, Trasande L, Jaddoe VWV, Fetal exposure to phthalates and bisphenols and childhood general and organ fat, A population-based prospective cohort study, International Journal of Obesity 44 (11) (2020) 2225–2235. [DOI] [PubMed] [Google Scholar]
- [296].Maresca MM, Hoepner LA, Hassoun A, Oberfield SE, Mooney SJ, Calafat AM, Ramirez J, Freyer G, Perera FP, Whyatt RM, Rundle AG, Prenatal Exposure to Phthalates and Childhood Body Size in an Urban Cohort, Environ. Health Perspect 124 (4) (2016) 514–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [297].Buckley JP, Engel SM, Mendez MA, Richardson DB, Daniels JL, Calafat AM, Wolff MS, Herring AH, Prenatal Phthalate Exposures and Childhood Fat Mass in a New York City Cohort, Environ. Health Perspect 124 (4) (2016) 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [298].Berger K, Hyland C, Ames JL, Mora AM, Huen K, Eskenazi B, Holland N, Harley KG, Prenatal Exposure to Mixtures of Phthalates, Parabens, and Other Phenols and Obesity in Five-Year-Olds in the CHAMACOS Cohort, Int. J. Environ. Res. Public Health 18 (4) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [299].Shoaff J, Papandonatos GD, Calafat AM, Ye X, Chen A, Lanphear BP, Yolton K, Braun JM, Early-Life Phthalate Exposure and Adiposity at 8 Years of Age, Environ. Health Perspect 125 (9) (2017), 097008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [300].Brauer M, Freedman G, Frostad J, van Donkelaar A, Martin RV, Dentener F, van Dingenen R, Estep K, Amini H, Apte JS, Balakrishnan K, Barregard L, Broday D, Feigin V, Ghosh S, Hopke PK, Knibbs LD, Kokubo Y, Liu Y, Ma S, Morawska L, Sangrador JL, Shaddick G, Anderson HR, Vos T, Forouzanfar MH, Burnett RT, Cohen A, Ambient Air Pollution Exposure Estimation for the Global Burden of Disease 2013, Environ. Sci. Technol 50 (1) (2016) 79–88. [DOI] [PubMed] [Google Scholar]
- [301].G.B.D.R.F. Collaborators, Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017, Lancet 392(10159) (2018) 1923–1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [302].Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K, Balakrishnan K, Brunekreef B, Dandona L, Dandona R, Feigin V, Freedman G, Hubbell B, Jobling A, Kan H, Knibbs L, Liu Y, Martin R, Morawska L, Pope CA 3rd, Shin H, Straif K, Shaddick G, Thomas M, van Dingenen R, van Donkelaar A, Vos T, Murray CJL, Forouzanfar MH, Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015, Lancet 389 (10082) (2017) 1907–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [303].Bailey MJ, Naik NN, Wild LE, Patterson WB, Alderete TL, Exposure to air pollutants and the gut microbiota: a potential link between exposure, obesity, and type 2 diabetes, Gut Microbes 11 (5) (2020) 1188–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [304].Rajagopalan S, Brook RD, Air pollution and type 2 diabetes: mechanistic insights, Diabetes 61 (12) (2012) 3037–3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [305].Brook RD, Xu X, Bard RL, Dvonch JT, Morishita M, Kaciroti N, Sun Q, Harkema J, Rajagopalan S, Reduced metabolic insulin sensitivity following subacute exposures to low levels of ambient fine particulate matter air pollution, The Science of the total environment 448 (2013) 66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [306].Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, Cai Y, Ostrowski MC, Lu B, Parthasarathy S, Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity, Circulation 119 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [307].Wang Y, Eliot MN, Kuchel GA, Schwartz J, Coull BA, Mittleman MA, Lipsitz LA, Wellenius GA, Long-term exposure to ambient air pollution and serum leptin in older adults: results from the MOBILIZE Boston study, J. Occup. Environ. Med 56 (9) (2014) e73–e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [308].Wu W, Jin Y, Carlsten C, Inflammatory health effects of indoor and outdoor particulate matter, J. Allergy Clin. Immunol 141 (3) (2018) 833–844. [DOI] [PubMed] [Google Scholar]
- [309].Xu Z, Xu X, Zhong M, Hotchkiss IP, Lewandowski RP, Wagner JG, Bramble LA, Yang Y, Wang A, Harkema JR, Lippmann M, Rajagopalan S, Chen LC, Sun Q, Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues, Part. Fibre Toxicol 8 (2011) 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [310].Haberzettl P, O’Toole TE, Bhatnagar A, Conklin DJ, Exposure to Fine Particulate Air Pollution Causes Vascular Insulin Resistance by Inducing Pulmonary Oxidative Stress, Environ. Health Perspect 124 (12) (2016) 1830–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [311].Calderon-Garciduenas L, Franco-Lira M, D’Angiulli A, Rodriguez-Diaz J, Blaurock-Busch E, Busch Y, Chao CK, Thompson C, Mukherjee PS, Torres-Jardon R, Perry G, Mexico City normal weight children exposed to high concentrations of ambient PM2.5 show high blood leptin and endothelin-1, vitamin D deficiency, and food reward hormone dysregulation versus low pollution controls. Relevance for obesity and Alzheimer disease, Environ. Res 140 (2015) 579–592. [DOI] [PubMed] [Google Scholar]
- [312].Irigaray P, Newby JA, Lacomme S, Belpomme D, Overweight/obesity and cancer genesis: more than a biological link, Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie 61 (10) (2007) 665–678. [DOI] [PubMed] [Google Scholar]
- [313].Irigaray P, Ogier V, Jacquenet S, Notet V, Sibille P, Mejean L, Bihain BE, Yen FT, Benzo[a]pyrene impairs beta-adrenergic stimulation of adipose tissue lipolysis and causes weight gain in mice, A novel molecular mechanism of toxicity for a common food pollutant, The FEBS journal 273 (7) (2006) 1362–1372. [DOI] [PubMed] [Google Scholar]
- [314].Ortiz L, Nakamura B, Li X, Blumberg B, Luderer U, In utero exposure to benzo [a]pyrene increases adiposity and causes hepatic steatosis in female mice, and glutathione deficiency is protective, Toxicol. Lett 223 (2) (2013) 260–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [315].Yin F, Gupta R, Vergnes L, Driscoll WS, Ricks J, Ramanathan G, Stewart JA, Shih DM, Faull KF, Beaven SW, Lusis AJ, Reue K, Rosenfeld ME, Araujo JA, Diesel Exhaust Induces Mitochondrial Dysfunction, Hyperlipidemia, and Liver Steatosis, Arterioscler. Thromb. Vasc. Biol 39 (9) (2019) 1776–1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [316].Xu X, Yavar Z, Verdin M, Ying Z, Mihai G, Kampfrath T, Wang A, Zhong M, Lippmann M, Chen LC, Rajagopalan S, Sun Q, Effect of early particulate air pollution exposure on obesity in mice: role of p47phox, Arterioscler. Thromb. Vasc. Biol 30 (12) (2010) 2518–2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [317].Wu G, Brown J, Zamora ML, Miller A, Satterfield MC, Meininger CJ, Steinhauser CB, Johnson GA, Burghardt RC, Bazer FW, Li Y, Johnson NM, Molina MJ, Zhang R, Adverse organogenesis and predisposed long-term metabolic syndrome from prenatal exposure to fine particulate matter, PNAS 116 (24) (2019) 11590–11595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [318].Pan K, Jiang S, Du X, Zeng X, Zhang J, Song L, Zhou J, Kan H, Sun Q, Xie Y, Zhao J, AMPK activation attenuates inflammatory response to reduce ambient PM2.5-induced metabolic disorders in healthy and diabetic mice, Ecotoxicol. Environ. Saf 179 (2019) 290–300. [DOI] [PubMed] [Google Scholar]
- [319].Reyes-Caballero H, Rao X, Sun Q, Warmoes MO, Lin P, Sussan TE, Park B, Fan TW, Maiseyeu A, Rajagopalan S, Girnun GD, Biswal S, Air pollution-derived particulate matter dysregulates hepatic Krebs cycle, glucose and lipid metabolism in mice, Sci. Rep 9 (1) (2019) 17423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [320].Li R, Wang Y, Hou B, Lam SM, Zhang W, Chen R, Shui G, Sun Q, Qiang G, Liu C, Lipidomics insight into chronic exposure to ambient air pollution in mice, Environmental pollution (Barking, Essex 262 (2020) (1987), 114668. [DOI] [PubMed] [Google Scholar]
- [321].Jiang M, Li D, Piao J, Li J, Sun H, Chen L, Chen S, Pi J, Zhang R, Chen R, Leng S, Chen W, Zheng Y, Real-ambient exposure to air pollution exaggerates excessive growth of adipose tissue modulated by Nrf2 signal, The Science of the total environment 730 (2020), 138652. [DOI] [PubMed] [Google Scholar]
- [322].Bolton JL, Smith SH, Huff NC, Gilmour MI, Foster WM, Auten RL, Bilbo SD, Prenatal air pollution exposure induces neuroinflammation and predisposes offspring to weight gain in adulthood in a sex-specific manner, FASEB J. (2012). [DOI] [PubMed] [Google Scholar]
- [323].Goettems-Fiorin PB, Grochanke BS, Baldissera FG, Dos Santos AB, Homem de Bittencourt PI Jr., Ludwig MS, Rhoden CR, Heck TG, Fine particulate matter potentiates type 2 diabetes development in high-fat diet-treated mice: stress response and extracellular to intracellular HSP70 ratio analysis, J Physiol Biochem 72(4) (2016) 643–656. [DOI] [PubMed] [Google Scholar]
- [324].Pardo M, Kuperman Y, Levin L, Rudich A, Haim Y, Schauer JJ, Chen A, Rudich Y, Exposure to air pollution interacts with obesogenic nutrition to induce tissue-specific response patterns, Environmental pollution (Barking, Essex 239 (2018) (1987) 532–543. [DOI] [PubMed] [Google Scholar]
- [325].Liu C, Bai Y, Xu X, Sun L, Wang A, Wang TY, Maurya SK, Periasamy M, Morishita M, Harkema J, Ying Z, Sun Q, Rajagopalan S, Exaggerated effects of particulate matter air pollution in genetic type II diabetes mellitus, Part. Fibre Toxicol 11 (2014) 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [326].Tang H, Cheng Z, Li N, Mao S, Ma R, He H, Niu Z, Chen X, Xiang H, The short- and long-term associations of particulate matter with inflammation and blood coagulation markers: A meta-analysis, Environmental pollution (Barking, Essex 267 (2020) (1987), 115630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [327].Clementi EA, Talusan A, Vaidyanathan S, Veerappan A, Mikhail M, Ostrofsky D, Crowley G, Kim JS, Kwon S, Nolan A, Metabolic Syndrome and Air Pollution: A Narrative Review of Their Cardiopulmonary Effects, Toxics 7 (1) (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [328].Wei Y, Zhang JJ, Li Z, Gow A, Chung KF, Hu M, Sun Z, Zeng L, Zhu T, Jia G, Li X, Duarte M, Tang X, Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: findings from a natural experiment in Beijing, FASEB journal : official publication of the Federation of American Societies for Experimental Biology 30 (6) (2016) 2115–2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [329].Liu C, Xu X, Bai Y, Wang TY, Rao X, Wang A, Sun L, Ying Z, Gushchina L, Maiseyeu A, Morishita M, Sun Q, Harkema JR, Rajagopalan S, Air pollution-mediated susceptibility to inflammation and insulin resistance: influence of CCR2 pathways in mice, Environ. Health Perspect 122 (1) (2014) 17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [330].Xu MX, Ge CX, Qin YT, Gu TT, Lou DS, Li Q, Hu LF, Feng J, Huang P, Tan J, Prolonged PM2.5 exposure elevates risk of oxidative stress-driven nonalcoholic fatty liver disease by triggering increase of dyslipidemia, Free Radic Biol Med 130 (2019) 542–556. [DOI] [PubMed] [Google Scholar]
- [331].Liu C, Ying Z, Harkema J, Sun Q, Rajagopalan S, Epidemiological and experimental links between air pollution and type 2 diabetes, Toxicol. Pathol 41 (2) (2013) 361–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [332].Alderete TL, Jones RB, Chen Z, Kim JS, Habre R, Lurmann F, Gilliland FD, Goran MI, Exposure to traffic-related air pollution and the composition of the gut microbiota in overweight and obese adolescents, Environ. Res 161 (2018) 472–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [333].Andrysík Z, Vondráček J, Marvanová S, Ciganek M, Neča J, Pěnčíková K, Mahadevan B, Topinka J, Baird WM, Kozubík A, Machala M, Activation of the aryl hydrocarbon receptor is the major toxic mode of action of an organic extract of a reference urban dust particulate matter mixture: the role of polycyclic aromatic hydrocarbons, Mutat. Res 714 (1–2) (2011) 53–62. [DOI] [PubMed] [Google Scholar]
- [334].Metidji A, Omenetti S, Crotta S, Li Y, Nye E, Ross E, Li V, Maradana MR, Schiering C, Stockinger B, The Environmental Sensor AHR Protects from Inflammatory Damage by Maintaining Intestinal Stem Cell Homeostasis and Barrier Integrity, Immunity 49(2) (2018) 353–362 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [335].Campolim CM, Weissmann L, Ferreira CKO, Zordao OP, Dornellas APS, de Castro G, Zanotto TM, Boico VF, Quaresma PGF, Lima RPA, Donato J Jr., Veras MM, Saldiva PHN, Kim YB, Prada PO, Short-term exposure to air pollution (PM2.5) induces hypothalamic inflammation, and long-term leads to leptin resistance and obesity via Tlr4/Ikbke in mice, Sci. Rep 10 (1) (2020) 10160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [336].Li R, Sun Q, Lam SM, Chen R, Zhu J, Gu W, Zhang L, Tian H, Zhang K, Chen LC, Sun Q, Shui G, Liu C, Sex-dependent effects of ambient PM2.5 pollution on insulin sensitivity and hepatic lipid metabolism in mice, Part. Fibre Toxicol 17 (1) (2020) 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [337].Seo MY, Kim SH, Park MJ, Air pollution and childhood obesity, Clin Exp Pediatr 63 (10) (2020) 382–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [338].Alderete TL, Habre R, Toledo-Corral CM, Berhane K, Chen Z, Lurmann FW, Weigensberg MJ, Goran MI, Gilliland FD, Longitudinal Associations Between Ambient Air Pollution With Insulin Sensitivity, beta-Cell Function, and Adiposity in Los Angeles Latino Children, Diabetes 66 (7) (2017) 1789–1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [339].Rundle A, Hoepner L, Hassoun A, Oberfield S, Freyer G, Holmes D, Reyes M, Quinn J, Camann D, Perera F, Whyatt R, Association of childhood obesity with maternal exposure to ambient air polycyclic aromatic hydrocarbons during pregnancy, Am. J. Epidemiol 175 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [340].Jerrett M, McConnell R, Wolch J, Chang R, Lam C, Dunton G, Gilliland F, Lurmann F, Islam T, Berhane K, Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis, Environ Health 13 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [341].McConnell R, Gilliland FD, Goran M, Allayee H, Hricko A, Mittelman S, Does near-roadway air pollution contribute to childhood obesity? Pediatric obesity (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [342].Starling AP, Moore BF, Thomas DSK, Peel JL, Zhang W, Adgate JL, Magzamen S, Martenies SE, Allshouse WB, Dabelea D, Prenatal exposure to traffic and ambient air pollution and infant weight and adiposity: The Healthy Start study, Environ. Res 182 (2020), 109130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [343].Rundle AG, Gallagher D, Herbstman JB, Goldsmith J, Holmes D, Hassoun A, Oberfield S, Miller RL, Andrews H, Widen EM, Hoepner LA, Perera F, Prenatal exposure to airborne polycyclic aromatic hydrocarbons and childhood growth trajectories from age 5–14 years, Environ. Res 177 (2019) 108595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [344].Kim JS, Alderete TL, Chen Z, Lurmann F, Rappaport E, Habre R, Berhane K, Gilliland FD, Longitudinal associations of in utero and early life near-roadway air pollution with trajectories of childhood body mass index, Environmental Health 17 (1) (2018) 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [345].de Bont J, Casas M, Barrera-Gomez J, Cirach M, Rivas I, Valvi D, Alvarez M, Dadvand P, Sunyer J, Vrijheid M, Ambient air pollution and overweight and obesity in school-aged children in Barcelona, Spain, Environ. Int 125 (2019) 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [346].Kim JS, Chen Z, Alderete TL, Toledo-Corral C, Lurmann F, Berhane K, Gilliland FD, Associations of air pollution, obesity and cardiometabolic health in young adults: The Meta-AIR study, Environ. Int 133 (Pt A) (2019), 105180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [347].Chen Z, Newgard CB, Kim JS, O II, Alderete TL, Thomas DC, Berhane K, Breton C, Chatzi L, Bastain TM, McConnell R, Avol E, Lurmann F, Muehlbauer MJ, Hauser ER, Gilliland FD, Near-roadway air pollution exposure and altered fatty acid oxidation among adolescents and young adults - The interplay with obesity, Environ Int 130 (2019) 104935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [348].Guo Q, Xue T, Jia C, Wang B, Cao S, Zhao X, Zhang Q, Zhao L, Zhang JJ, Duan X, Association between exposure to fine particulate matter and obesity in children: A national representative cross-sectional study in China, Environ. Int 143 (2020), 105950. [DOI] [PubMed] [Google Scholar]
- [349].Parasin N, Amnuaylojaroen T, Saokaew S, Effect of Air Pollution on Obesity in Children, A Systematic Review and Meta-Analysis, Children (Basel) 8 (5) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [350].Frondelius K, Oudin A, Malmqvist E, Traffic-Related Air Pollution and Child BMI-A Study of Prenatal Exposure to Nitrogen Oxides and Body Mass Index in Children at the Age of Four Years in Malmo, Sweden, Int. J. Environ. Res. Public Health 15 (10) (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [351].Wang Z, Zhao L, Huang Q, Hong A, Yu C, Xiao Q, Zou B, Ji S, Zhang L, Zou K, Ning Y, Zhang J, Jia P, Traffic-related environmental factors and childhood obesity: A systematic review and meta-analysis, Obes. Rev (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [352].Fioravanti S, Cesaroni G, Badaloni C, Michelozzi P, Forastiere F, Porta D, Traffic-related air pollution and childhood obesity in an Italian birth cohort, Environ. Res 160 (2018). [DOI] [PubMed] [Google Scholar]
- [353].Zhang K, Wang H, He W, Chen G, Lu P, Xu R, Yu P, Ye T, Guo S, Li S, Xie Y, Hao Z, Wang H, Guo Y, The association between ambient air pollution and blood lipids: A longitudinal study in Shijiazhuang, China, The Science of the total environment 752 (2021), 141648. [DOI] [PubMed] [Google Scholar]
- [354].Zhang N, Wang L, Zhang M, Nazroo J, Air quality and obesity at older ages in China: The role of duration, severity and pollutants, PLoS ONE 14 (12) (2019), e0226279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [355].Zhang X, Zhao H, Chow WH, Bixby M, Durand C, Markham C, Zhang K, Population-Based Study of Traffic-Related Air Pollution and Obesity in Mexican Americans, Obesity (Silver Spring) 28 (2) (2020) 412–420. [DOI] [PubMed] [Google Scholar]
- [356].Lee S, Park H, Kim S, Lee EK, Lee J, Hong YS, Ha E, Fine particulate matter and incidence of metabolic syndrome in non-CVD patients: A nationwide population-based cohort study, Int. J. Hyg. Environ. Health 222 (3) (2019) 533–540. [DOI] [PubMed] [Google Scholar]
- [357].Huang S, Zhang X, Huang J, Lu X, Liu F, Gu D, Ambient air pollution and body weight status in adults: A systematic review and meta-analysis, Environmental pollution (Barking, Essex : 1987) 265(Pt A) (2020) 114999. [DOI] [PubMed] [Google Scholar]
- [358].Wolf K, Popp A, Schneider A, Breitner S, Hampel R, Rathmann W, Herder C, Roden M, Koenig W, Meisinger C, Peters A, K.O.-S. Group, Association Between Long-term Exposure to Air Pollution and Biomarkers Related to Insulin Resistance, Subclinical Inflammation, and Adipokines, Diabetes 65 (11) (2016) 3314–3326. [DOI] [PubMed] [Google Scholar]
- [359].Mattos Y, Stotz WB, Romero MS, Bravo M, Fillmann G, Castro IB, Butyltin contamination in Northern Chilean coast: Is there a potential risk for consumers? The Science of the total environment 595 (2017) 209–217. [DOI] [PubMed] [Google Scholar]
- [360].Lagadic L, Katsiadaki I, Biever R, Guiney PD, Karouna-Renier N, Schwarz T, Meador JP, Tributyltin: Advancing the Science on Assessing Endocrine Disruption with an Unconventional Endocrine-Disrupting Compound, Rev. Environ. Contam. Toxicol 245 (2018) 65–127. [DOI] [PubMed] [Google Scholar]
- [361].Golub M, Doherty J, Triphenyltin as a potential human endocrine disruptor, J. Toxicol. Environ. Health B. Crit. Rev 7 (2004) 281–295. [DOI] [PubMed] [Google Scholar]
- [362].Fromme H, Mattulat A, Lahrz T, Ruden H, Occurrence of organotin compounds in house dust in Berlin (Germany), Chemosphere 58 (10) (2005) 1377–1383. [DOI] [PubMed] [Google Scholar]
- [363].Kannan K, Takahashi S, Fujiwara N, Mizukawa H, Tanabe S, Organotin compounds, including butyltins and octyltins, in house dust from Albany, New York, USA, Arch Environ Contam Toxicol 58 (4) (2010) 901–907. [DOI] [PubMed] [Google Scholar]
- [364].Chamorro-García R, Shoucri BM, Willner S, Käch H, Janesick A, Blumberg B, Effects of Perinatal Exposure to Dibutyltin Chloride on Fat and Glucose Metabolism in Mice, and Molecular Mechanisms, in Vitro, Environ. Health Perspect 126 (5) (2018), 057006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [365].Milton FA, Lacerda MG, Sinoti SBP, Mesquita PG, Prakasan D, Coelho MS, de Lima CL, Martini AG, Pazzine GT, Borin MF, Amato AA, Neves FAR, Dibutyltin Compounds Effects on PPARγ/RXRα Activity, Adipogenesis, and Inflammation in Mammalians Cells, Frontiers in pharmacology 8 (2017) 507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [366].le Maire A, Grimaldi M, Roecklin D, Dagnino S, Vivat-Hannah V, Balaguer P, Bourguet W, Activation of RXR-PPAR heterodimers by organotin environmental endocrine disruptors, EMBO Rep. 10 (4) (2009) 367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [367].Delfosse V, Huet T, Harrus D, Granell M, Bourguet M, Gardia-Parège C, Chiavarina B, Grimaldi M, Le Mével S, Blanc P, Huang D, Gruszczyk J, Demeneix B, Cianférani S, Fini JB, Balaguer P, Bourguet W, Mechanistic insights into the synergistic activation of the RXR-PXR heterodimer by endocrine disruptor mixtures, PNAS 118 (1) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [368].Inadera H, Shimomura A, Environmental chemical tributyltin augments adipocyte differentiation, Toxicol. Lett 159 (3) (2005) 226–234. [DOI] [PubMed] [Google Scholar]
- [369].Li X, Ycaza J, Blumberg B, The environmental obesogen tributyltin chloride acts via peroxisome proliferator activated receptor gamma to induce adipogenesis in murine 3T3-L1 preadipocytes, The Journal of Steroid Biochemistry and Molecular Biology 127 (1–2) (2011) 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [370].Kirchner S, Kieu T, Chow C, Casey S, Blumberg B, Prenatal exposure to the environmental obesogen tributyltin predisposes multipotent stem cells to become adipocytes, Molecular endocrinology (Baltimore, Md.) 24 (3) (2010) 526–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [371].Yanik SC, Baker AH, Mann KK, Schlezinger JJ, Organotins are potent activators of PPARgamma and adipocyte differentiation in bone marrow multipotent mesenchymal stromal cells, Toxicological sciences : an official journal of the Society of Toxicology 122 (2) (2011) 476–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [372].Stossi F, Dandekar RD, Johnson H, Lavere P, Foulds CE, Mancini MG, Mancini MA, Tributyltin chloride (TBT) induces RXRA down-regulation and lipid accumulation in human liver cells, PLoS ONE 14 (11) (2019) e0224405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [373].Flynn EJ, Trent CM, Rawls JF, Ontogeny and nutritional control of adipogenesis in zebrafish (Danio rerio), J. Lipid Res 50 (8) (2009) 1641–1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [374].Imrie D, Sadler KC, White adipose tissue development in zebrafish is regulated by both developmental time and fish size, Dev. Dyn 239 (11) (2010) 3013–3023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [375].Tingaud-Sequeira A, Ouadah N, Babin PJ, Zebrafish obesogenic test: a tool for screening molecules that target adiposity, J. Lipid Res 52 (9) (2011) 1765–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [376].den Broeder MJ, Moester MJB, Kamstra JH, Cenijn PH, Davidoiu V, Kamminga LM, Ariese F, de Boer JF, Legler J, Altered Adipogenesis in Zebrafish Larvae Following High Fat Diet and Chemical Exposure Is Visualised by Stimulated Raman Scattering Microscopy, Int. J. Mol. Sci 18 (4) (2017) 894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [377].Zhang J, Sun P, Yang F, Kong T, Zhang R, Tributyltin disrupts feeding and energy metabolism in the goldfish (Carassius auratus), Chemosphere 152 (2016) 221–228. [DOI] [PubMed] [Google Scholar]
- [378].Meador JP, Sommers FC, Cooper KA, Yanagida G, Tributyltin and the obesogen metabolic syndrome in a salmonid, Environ. Res 111 (1) (2011) 50–56. [DOI] [PubMed] [Google Scholar]
- [379].Chen K, Iwasaki N, Qiu X, Xu H, Takai Y, Tashiro K, Shimasaki Y, Oshima Y, Obesogenic and developmental effects of TBT on the gene expression of juvenile Japanese medaka (Oryzias latipes), Aquatic toxicology (Amsterdam, Netherlands) 237 (2021), 105907. [DOI] [PubMed] [Google Scholar]
- [380].Capitão AMF, Lopes-Marques MS, Ishii Y, Ruivo R, Fonseca ESS, Páscoa I, Jorge RP, Barbosa MAG, Hiromori Y, Miyagi T, Nakanishi T, Santos MM, Castro LFC, Evolutionary Exploitation of Vertebrate Peroxisome Proliferator-Activated Receptor γ by Organotins, Environ. Sci. Technol 52 (23) (2018) 13951–13959. [DOI] [PubMed] [Google Scholar]
- [381].Ouadah-Boussouf N, Babin PJ, Pharmacological evaluation of the mechanisms involved in increased adiposity in zebrafish triggered by the environmental contaminant tributyltin, Toxicol. Appl. Pharmacol 294 (2016) 32–42. [DOI] [PubMed] [Google Scholar]
- [382].Grun F, Endocrine-disrupting organotin compounds are potent inducers of adipogenesis in vertebrates, Mol. Endocrinol 20 (2006) 2141–2155. [DOI] [PubMed] [Google Scholar]
- [383].Bo E, Viglietti-Panzica C, Panzica GC, Acute exposure to tributyltin induces c-fos activation in the hypothalamic arcuate nucleus of adult male mice, Neurotoxicology 32 (2) (2011) 277–280. [DOI] [PubMed] [Google Scholar]
- [384].Penza M, Jeremic M, Marrazzo E, Maggi A, Ciana P, Rando G, Grigolato PG, Di Lorenzo D, The environmental chemical tributyltin chloride (TBT) shows both estrogenic and adipogenic activities in mice which might depend on the exposure dose, Toxicol. Appl. Pharmacol 255 (1) (2011) 65–75. [DOI] [PubMed] [Google Scholar]
- [385].Zuo Z, Chen S, Wu T, Zhang J, Su Y, Chen Y, Wang C, Tributyltin causes obesity and hepatic steatosis in male mice, Environ. Toxicol 26 (1) (2011) 79–85. [DOI] [PubMed] [Google Scholar]
- [386].He K, Zhang J, Chen Z, Effect of tributyltin on the food intake and brain neuropeptide expression in rats, Endokrynol Pol 65 (6) (2014) 485–490. [DOI] [PubMed] [Google Scholar]
- [387].Bo E, Farinetti A, Marraudino M, Sterchele D, Eva C, Gotti S, Panzica G, Adult exposure to tributyltin affects hypothalamic neuropeptide Y, Y1 receptor distribution, and circulating leptin in mice, Andrology 4 (4) (2016) 723–734. [DOI] [PubMed] [Google Scholar]
- [388].Rantakokko P, Main KM, Wohlfart-Veje C, Kiviranta H, Airaksinen R, Vartiainen T, Skakkebaek NE, Toppari J, Virtanen HE, Association of placenta organotin concentrations with growth and ponderal index in 110 newborn boys from Finland during the first 18 months of life: a cohort study, Environ Health 13 (1) (2014) 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [389].Liu B, Sun Y, Lehmler HJ, Bao W, Association between urinary tin concentration and diabetes in nationally representative sample of US adults, J. Diabetes 10 (12) (2018) 977–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [390].Lehmler HJ, Gadogbe M, Liu B, Bao W, Environmental tin exposure in a nationally representative sample of U.S. adults and children: The National Health and Nutrition Examination Survey 2011–2014, Environmental pollution (Barking, Essex 240 (2018) (1987) 599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [391].National Toxicology Program (NTP), NTP research report on organotin and total tin levels in Danish women of reproductive age., NTP Research Report Series, National Toxicology Program. Research Report 2, Research Triangle Park, NC, 2016. [PubMed] [Google Scholar]
- [392].Gadogbe M, Bao W, Wels BR, Dai SY, Santillan DA, Santillan MK, Lehmler HJ, Levels of tin and organotin compounds in human urine samples from Iowa, United States, Journal of environmental science and health, Part A, Toxic/hazardous substances & environmental engineering 54 (9) (2019) 884–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [393].Xue J, Zartarian V, Moya J, Freeman N, Beamer P, Black K, Tulve N, Shalat S, A meta-analysis of children’s hand-to-mouth frequency data for estimating nondietary ingestion exposure, Risk analysis : an official publication of the Society for Risk Analysis 27 (2) (2007) 411–420. [DOI] [PubMed] [Google Scholar]
- [394].Hoffman K, Butt CM, Chen A, Limkakeng AT, Stapleton HM, High Exposure to Organophosphate Flame Retardants in Infants: Associations with Baby Products, Environ. Sci. Technol 49 (24) (2015) 14554–14559. [DOI] [PubMed] [Google Scholar]
- [395].Wong KH, Durrani TS, Exposures to Endocrine Disrupting Chemicals in Consumer Products-A Guide for Pediatricians, Curr Probl Pediatr Adolesc Health Care 47 (5) (2017) 107–118. [DOI] [PubMed] [Google Scholar]
- [396].Percy Z, La Guardia MJ, Xu Y, Hale RC, Dietrich KN, Lanphear BP, Yolton K, Vuong AM, Cecil KM, Braun JM, Xie C, Chen A, Concentrations and loadings of organophosphate and replacement brominated flame retardants in house dust from the home study during the PBDE phase-out, Chemosphere 239 (2020), 124701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [397].Zota AR, Linderholm L, Park JS, Petreas M, Guo T, Privalsky ML, Zoeller RT, Woodruff TJ, Temporal comparison of PBDEs, OH-PBDEs, PCBs, and OH-PCBs in the serum of second trimester pregnant women recruited from San Francisco General Hospital, California, Environ. Sci. Technol 47 (20) (2013) 11776–11784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [398].Adgent MA, Hoffman K, Goldman BD, Sjödin A, Daniels JL, Brominated flame retardants in breast milk and behavioural and cognitive development at 36 months, Paediatr. Perinat. Epidemiol 28 (1) (2014) 48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [399].Leonetti C, Butt CM, Hoffman K, Hammel SC, Miranda ML, Stapleton HM, Brominated flame retardants in placental tissues: associations with infant sex and thyroid hormone endpoints, Environ Health 15 (1) (2016) 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [400].van der Veen I, de Boer J, Phosphorus flame retardants: Properties, production, environmental occurrence, toxicity and analysis, Chemosphere 88 (10) (2012) 1119–1153. [DOI] [PubMed] [Google Scholar]
- [401].Blum A, Behl M, Birnbaum LS, Diamond ML, Phillips A, Singla V, Sipes NS, Stapleton HM, Venier M, Organophosphate Ester Flame Retardants: Are They a Regrettable Substitution for Polybrominated Diphenyl Ethers? Environ. Sci. Technol. Lett 6 (11) (2019) 638–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [402].Meeker JD, Cooper EM, Stapleton HM, Hauser R, Urinary metabolites of organophosphate flame retardants: temporal variability and correlations with house dust concentrations, Environ. Health Perspect 121 (5) (2013) 580–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [403].Dishaw LV, Macaulay LJ, Roberts SC, Stapleton HM, Exposures, mechanisms, and impacts of endocrine-active flame retardants, Curr. Opin. Pharmacol 19 (2014) 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [404].Hoffman K, Butt CM, Webster TF, Preston EV, Hammel SC, Makey C, Lorenzo AM, Cooper EM, Carignan C, Meeker JD, Hauser R, Soubry A, Murphy SK, Price TM, Hoyo C, Mendelsohn E, Congleton J, Daniels JL, Stapleton HM, Temporal Trends in Exposure to Organophosphate Flame Retardants in the United States, Environ. Sci. Technol. Lett 4 (3) (2017) 112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [405].Hoffman K, Daniels JL, Stapleton HM, Urinary metabolites of organophosphate flame retardants and their variability in pregnant women, Environ. Int 63 (2014) 169–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [406].Carignan CC, McClean MD, Cooper EM, Watkins DJ, Fraser AJ, Heiger-Bernays W, Stapleton HM, Webster TF, Predictors of tris(1,3-dichloro-2-propyl) phosphate metabolite in the urine of office workers, Environ. Int 55 (2013) 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [407].Bastos Sales L, Kamstra JH, Cenijn PH, van Rijt LS, Hamers T, Legler J, Effects of endocrine disrupting chemicals on in vitro global DNA methylation and adipocyte differentiation, Toxicol. In Vitro 27 (6) (2013) 1634–1643. [DOI] [PubMed] [Google Scholar]
- [408].Wen Q, Xie X, Zhao C, Ren Q, Zhang X, Wei D, Emanuelli B, Du Y, The brominated flame retardant PBDE 99 promotes adipogenesis via regulating mitotic clonal expansion and PPARγ expression, Sci. Total Environ 670 (2019) 67–77. [DOI] [PubMed] [Google Scholar]
- [409].Kamstra JH, Hruba E, Blumberg B, Janesick A, Mandrup S, Hamers T, Legler J, Transcriptional and epigenetic mechanisms underlying enhanced in vitro adipocyte differentiation by the brominated flame retardant BDE-47, Environ. Sci. Technol 48 (7) (2014) 4110–4119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [410].Yang C, Wong CM, Wei J, Chung ACK, Cai Z, The brominated flame retardant BDE 47 upregulates purine metabolism and mitochondrial respiration to promote adipocyte differentiation, Sci. Total Environ 644 (2018) 1312–1322. [DOI] [PubMed] [Google Scholar]
- [411].Karandrea S, Yin H, Liang X, Heart EA, BDE-47 and BDE-85 stimulate insulin secretion in INS-1 832/13 pancreatic β-cells through the thyroid receptor and Akt, Environ. Toxicol. Pharmacol 56 (May) (2017) 29–34. [DOI] [PubMed] [Google Scholar]
- [412].Gao H, Li P, Liu L, Yang K, Xiao B, Zhou G, Tian Z, Luo C, Xia T, Dong L, Zhao Q, Wang A, Zhang S, Perigestational low-dose BDE-47 exposure alters maternal serum metabolome and results in sex-specific weight gain in adult offspring, Chemosphere 233 (2019) 174–182. [DOI] [PubMed] [Google Scholar]
- [413].Suvorov A, Battista MC, Takser L, Perinatal exposure to low-dose 2,2’,4,4’-tetrabromodiphenyl ether affects growth in rat offspring: what is the role of IGF-1? Toxicology 260 (1–3) (2009) 126–131. [DOI] [PubMed] [Google Scholar]
- [414].Abrha A, Suvorov A, Transcriptomic Analysis of Gonadal Adipose Tissue in Male Mice Exposed Perinatally to 2,2’,4,4’-Tetrabromodiphenyl Ether (BDE-47), Toxics 6 (2) (2018) 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [415].Wang D, Zhu W, Chen L, Yan J, Teng M, Zhou Z, Neonatal triphenyl phosphate and its metabolite diphenyl phosphate exposure induce sex- and dose-dependent metabolic disruptions in adult mice, Environ. Pollut 237 (2018) 10–17. [DOI] [PubMed] [Google Scholar]
- [416].Yanagisawa R, Koike E, Win-Shwe TT, Takano H, Decabromodiphenyl ether exacerbates hyperglycemia in diet-induced obese mice, Toxicology 412 (November 2018) (2019) 12–18. [DOI] [PubMed] [Google Scholar]
- [417].Zhang Z, Li S, Liu L, Wang L, Xiao X, Sun Z, Wang X, Wang C, Wang M, Li L, Xu Q, Gao W, Wang SL, Environmental exposure to BDE47 is associated with increased diabetes prevalence: Evidence from community-based case-control studies and an animal experiment, Sci. Rep 6 (May) (2016) 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [418].Scoville DK, Li CY, Wang D, Dempsey JL, Raftery D, Mani S, Gu H, Cui JY, Polybrominated diphenyl ethers and gut microbiome modulate metabolic syndrome-related aqueous metabolites in mice, Drug Metab. Dispos 47 (8) (2019) 928–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [419].Drage DS, Heffernan AL, Cunningham TK, Aylward LL, Mueller JF, Sathyapalan T, Atkin SL, Serum measures of hexabromocyclododecane (HBCDD) and polyborminated diphenyl ethers (PBDEs) in reproductive-aged women in the United Kingdom, Environ. Res 177 (July) (2019) 108631. [DOI] [PubMed] [Google Scholar]
- [420].Cordier S, Anassour-Laouan-Sidi E, Lemire M, Costet N, Lucas M, Ayotte P, Association between exposure to persistent organic pollutants and mercury, and glucose metabolism in two Canadian Indigenous populations, Environ. Res 184 (February) (2020). [DOI] [PubMed] [Google Scholar]
- [421].Erkin-Cakmak A, Harley KG, Chevrier J, Bradman A, Kogut K, Huen K, Eskenazi B, In utero and childhood polybrominated diphenyl ether exposures and body mass at age 7 years: the CHAMACOS study, Environ. Health Perspect 123 (6) (2015) 636–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [422].Guo J, Miao W, Wu C, Zhang J, Qi X, Yu H, Chang X, Zhang Y, Zhou Z, Umbilical cord serum PBDE concentrations and child adiposity measures at 7 years, Ecotoxicol. Environ. Saf 203 (July) (2020) 111009. [DOI] [PubMed] [Google Scholar]
- [423].Vuong AM, Braun JM, Wang Z, Yolton K, Xie C, Sjodin A, Webster GM, Lanphear BP, Chen A, Exposure to polybrominated diphenyl ethers (PBDEs) during childhood and adiposity measures at age 8years, Environ. Int 123 (2019) 148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [424].Cano-Sancho G, Smith A, La Merrill MA, Triphenyl phosphate enhances adipogenic differentiation, glucose uptake and lipolysis via endocrine and noradrenergic mechanisms, Toxicol. In Vitro 40 (2017) 280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [425].Hao Z, Zhang Z, Lu D, Ding B, Shu L, Zhang Q, Wang C, Organophosphorus Flame Retardants Impair Intracellular Lipid Metabolic Function in Human Hepatocellular Cells, Chem. Res. Toxicol 32 (6) (2019) 1250–1258. [DOI] [PubMed] [Google Scholar]
- [426].Walley SN, Roepke TA, Perinatal exposure to endocrine disrupting compounds and the control of feeding behavior — An overview, Hormones and Behavior 101 (November 2017) (2018) 22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [427].Vail GM, Roepke TA, Organophosphate Flame Retardants Excite Arcuate Melanocortin Circuitry and Increase Neuronal Sensitivity to Ghrelin in Adult Mice, Endocrinology 161 (11) (2020) 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [428].Kim S, Rabhi N, Blum BC, Hekman R, Wynne K, Emili A, Farmer S, Schlezinger JJ, Triphenyl phosphate is a selective PPARγ modulator that does not induce brite adipogenesis in vitro and in vivo, Arch. Toxicol 94 (9) (2020) 3087–3103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [429].Du Z, Zhang Y, Wang G, Peng J, Wang Z, Gao S, TPhP exposure disturbs carbohydrate metabolism, lipid metabolism, and the DNA damage repair system in zebrafish liver, Sci. Rep 6 (February) (2016) 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [430].Farhat A, Buick JK, Williams A, Yauk CL, O’Brien JM, Crump D, Williams KL, Chiu S, Kennedy SW, Tris(1,3-dichloro-2-propyl) phosphate perturbs the expression of genes involved in immune response and lipid and steroid metabolism in chicken embryos, Toxicol. Appl. Pharmacol 275 (2) (2014) 104–112. [DOI] [PubMed] [Google Scholar]
- [431].Wang C, Le Y, Lu D, Zhao M, Dou X, Zhang Q, Triphenyl phosphate causes a sexually dimorphic metabolism dysfunction associated with disordered adiponectin receptors in pubertal mice, J. Hazard. Mater 388 (2020) 121732. [DOI] [PubMed] [Google Scholar]
- [432].Morris PJ, Medina-Cleghorn D, Heslin A, King SM, Orr J, Mulvihill MM, Krauss RM, Nomura DK, Organophosphorus flame retardants inhibit specific liver carboxylesterases and cause serum hypertriglyceridemia, ACS Chem. Biol 9 (5) (2014) 1097–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [433].Wade MG, Kawata A, Rigden M, Caldwell D, Holloway AC, Toxicity of Flame Retardant Isopropylated Triphenyl Phosphate: Liver, Adrenal, and Metabolic Effects, International journal of toxicology 38 (4) (2019) 279–290. [DOI] [PubMed] [Google Scholar]
- [434].Krumm EA, Patel VJ, Tillery TS, Yasrebi A, Shen J, Guo GL, Marco SM, Buckley BT, Roepke TA, Organophosphate Flame-Retardants Alter Adult Mouse Homeostasis and Gene Expression in a Sex-Dependent Manner Potentially Through Interactions With ERα, Toxicol. Sci 162 (1) (2018) 212–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [435].Vail GM, Walley SN, Yasrebi A, Maeng A, Conde K, Roepke TA, The interactions of diet-induced obesity and organophosphate flame retardant exposure on energy homeostasis in adult male and female mice, Journal of Toxicology and Environmental Health, Part A 83 (11–12) (2020) 438–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [436].Yan S, Wang D, Teng M, Meng Z, Yan J, Li R, Jia M, Tian S, Zhou Z, Zhu W, Perinatal exposure to 2-Ethylhexyl Diphenyl Phosphate (EHDPHP) affected the metabolic homeostasis of male mouse offspring: Unexpected findings help to explain dose- and diet-specific phenomena, Journal of hazardous materials 388 (September 2019) (2020) 122034–122034. [DOI] [PubMed] [Google Scholar]
- [437].Patisaul HB, Roberts SC, Mabrey N, McCaffrey KA, Gear RB, Braun J, Belcher SM, Stapleton HM, Accumulation and endocrine disrupting effects of the flame retardant mixture Firemaster(R) 550 in rats: an exploratory assessment, J. Biochem. Mol. Toxicol 27 (2) (2013) 124–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [438].Witchey SK, Al Samara L, Horman BM, Stapleton HM, Patisaul HB, Perinatal exposure to FireMaster® 550 (FM550), brominated or organophosphate flame retardants produces sex and compound specific effects on adult Wistar rat socioemotional behavior, Hormones and Behavior 126(September) (2020) 104853–104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [439].Wang D, Yan S, Yan J, Teng M, Meng Z, Li R, Zhou Z, Zhu W, Effects of triphenyl phosphate exposure during fetal development on obesity and metabolic dysfunctions in adult mice: Impaired lipid metabolism and intestinal dysbiosis, Environ. Pollut 246 (2019) 630–638. [DOI] [PubMed] [Google Scholar]
- [440].Philbrook NA, Restivo VE, Belanger CL, Winn LM, Gestational triphenyl phosphate exposure in C57Bl/6 mice perturbs expression of insulin-like growth factor signaling genes in maternal and fetal liver, Birth defects research 110 (6) (2018) 483–494. [DOI] [PubMed] [Google Scholar]
- [441].Walley SN, Krumm EA, Yasrebi A, Kwiecinski J, Wright V, Baker C, Roepke TA, Maternal organophosphate flame-retardant exposure alters offspring energy and glucose homeostasis in a sexually dimorphic manner in mice, J. Appl. Toxicol (2020) 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [442].Luo D, Liu W, Tao Y, Wang L, Yu M, Hu L, Zhou A, Covaci A, Xia W, Li Y, Xu S, Mei S, Prenatal Exposure to Organophosphate Flame Retardants and the Risk of Low Birth Weight: A Nested Case-Control Study in China, Environ. Sci. Technol 54 (6) (2020) 3375–3385. [DOI] [PubMed] [Google Scholar]
- [443].Boyle M, Buckley JP, Quirós-Alcalá L, Associations between urinary organophosphate ester metabolites and measures of adiposity among U.S. children and adults: NHANES 2013–2014, Environment International 127(March) (2019) 754–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [444].Kuiper JR, Stapleton HM, Wills-Karp M, Wang X, Burd I, Buckley JP, Predictors and reproducibility of urinary organophosphate ester metabolite concentrations during pregnancy and associations with birth outcomes in an urban population, Environmental health : a global access science source 19 (1) (2020) 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [445].Crawford KA, Hawley N, Calafat AM, Jayatilaka NK, Froehlich RJ, Has P, Gallagher LG, Savitz DA, Braun JM, Werner EF, Romano ME, Maternal urinary concentrations of organophosphate ester metabolites: associations with gestational weight gain, early life anthropometry, and infant eating behaviors among mothers-infant pairs in Rhode Island, Environmental health : a global access science source 19 (1) (2020) 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [446].Pinos H, Carrillo B, Merchán A, Biosca-Brull J, Pérez-Fernández C, Colomina MT, Sánchez-Santed F, Martín-Sánchez F, Collado P, Arias JL, Conejo NM, Relationship between Prenatal or Postnatal Exposure to Pesticides and Obesity: A Systematic Review, Int. J. Environ. Res. Public Health 18 (13) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [447].Heindel JJ, Skalla LA, Joubert BR, Dilworth CH, Gray KA, Review of developmental origins of health and disease publications in environmental epidemiology, Reprod. Toxicol 68 (2017) 34–48. [DOI] [PubMed] [Google Scholar]
- [448].Ren XM, Kuo Y, Blumberg B, Agrochemicals and obesity, Mol. Cell. Endocrinol 515 (2020), 110926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [449].van den Berg H, Global status of DDT and its alternatives for use in vector control to prevent disease, Environ. Health Perspect 117 (11) (2009) 1656–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [450].Enayati A, Hemingway J, Malaria management: past, present, and future, Annu. Rev. Entomol 55 (2010) 569–591. [DOI] [PubMed] [Google Scholar]
- [451].A.f.T.S.a.D.R. (ATSDR), Toxicological profile for DDT, DDE, and DDD, in: D.o.H.a.H. Services; (Ed.) Atlanta, GA, 2002. [Google Scholar]
- [452].Chapados NA, Casimiro C, Robidoux MA, Haman F, Batal M, Blais JM, Imbeault P, Increased proliferative effect of organochlorine compounds on human preadipocytes, Mol. Cell. Biochem 365 (1–2) (2012) 275–278. [DOI] [PubMed] [Google Scholar]
- [453].Ibrahim MM, Fjaere E, Lock EJ, Naville D, Amlund H, Meugnier E, Le Magueresse Battistoni B, Froyland L, Madsen L, Jessen N, Lund S, Vidal H, Ruzzin J, Chronic consumption of farmed salmon containing persistent organic pollutants causes insulin resistance and obesity in mice, PLoS ONE 6 (9) (2011), e25170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [454].Mangum LH, Howell GE 3rd, Chambers JE, Exposure to p, p’-DDE enhances differentiation of 3T3-L1 preadipocytes in a model of sub-optimal differentiation, Toxicol. Lett 238 (2) (2015) 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [455].Kim J, Sun Q, Yue Y, Yoon KS, Whang KY, Marshall Clark J, Park Y, 4,4’-Dichlorodiphenyltrichloroethane (DDT) and 4,4’-dichlorodiphenyldichloroethylene (DDE) promote adipogenesis in 3T3-L1 adipocyte cell culture, Pestic. Biochem. Physiol 131 (2016) 40–45. [DOI] [PubMed] [Google Scholar]
- [456].Moreno-Aliaga MJ, Matsumura F, Effects of 1,1,1-trichloro-2,2-bis(p-chlorophenyl)-ethane (p, p’-DDT) on 3T3-L1 and 3T3-F442A adipocyte differentiation, Biochem. Pharmacol 63 (5) (2002) 997–1007. [DOI] [PubMed] [Google Scholar]
- [457].Strong AL, Shi Z, Strong MJ, Miller DF, Rusch DB, Buechlein AM, Flemington EK, McLachlan JA, Nephew KP, Burow ME, Bunnell BA, Effects of the endocrine-disrupting chemical DDT on self-renewal and differentiation of human mesenchymal stem cells, Environ. Health Perspect 123 (1) (2015) 42–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [458].Howell G 3rd, Mangum L, Exposure to bioaccumulative organochlorine compounds alters adipogenesis, fatty acid uptake, and adipokine production in NIH3T3-L1 cells, Toxicol. In Vitro 25 (1) (2011) 394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [459].Taxvig C, Dreisig K, Boberg J, Nellemann C, Schelde AB, Pedersen D, Boergesen M, Mandrup S, Vinggaard AM, Differential effects of environmental chemicals and food contaminants on adipogenesis, biomarker release and PPARgamma activation, Mol. Cell. Endocrinol 361 (1–2) (2012) 106–115. [DOI] [PubMed] [Google Scholar]
- [460].La Merrill M, Karey E, Moshier E, Lindtner C, La Frano MR, Newman JW, Buettner C, Perinatal exposure of mice to the pesticide DDT impairs energy expenditure and metabolism in adult female offspring, PLoS ONE 9 (7) (2014), e103337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [461].Cano-Sancho G, Salmon AG, La Merrill MA, Association between Exposure to p, p’-DDT and Its Metabolite p, p’-DDE with Obesity: Integrated Systematic Review and Meta-Analysis, Environ. Health Perspect 125 (9) (2017), 096002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [462].Mustieles V, Arrebola JP, How polluted is your fat? What the study of adipose tissue can contribute to environmental epidemiology, J Epidemiol Community Health 74 (5) (2020) 401–407. [DOI] [PubMed] [Google Scholar]
- [463].Dhooge W, Den Hond E, Koppen G, Bruckers L, Nelen V, Van De Mieroop E, Bilau M, Croes K, Baeyens W, Schoeters G, Van Larebeke N, Internal exposure to pollutants and body size in Flemish adolescents and adults: associations and dose-response relationships, Environ. Int 36 (4) (2010) 330–337. [DOI] [PubMed] [Google Scholar]
- [464].Arrebola JP, Ocana-Riola R, Arrebola-Moreno AL, Fernandez-Rodriguez M, Martin-Olmedo P, Fernandez MF, Olea N, Associations of accumulated exposure to persistent organic pollutants with serum lipids and obesity in an adult cohort from Southern Spain, Environmental pollution (Barking, Essex 195 (2014) (1987) 9–15. [DOI] [PubMed] [Google Scholar]
- [465].Arrebola JP, Cuellar M, Claure E, Quevedo M, Antelo SR, Mutch E, Ramirez E, Fernandez MF, Olea N, Mercado LA, Concentrations of organochlorine pesticides and polychlorinated biphenyls in human serum and adipose tissue from Bolivia, Environ. Res 112 (2012) 40–47. [DOI] [PubMed] [Google Scholar]
- [466].Elobeid MA, Padilla MA, Brock DW, Ruden DM, Allison DB, Endocrine disruptors and obesity: an examination of selected persistent organic pollutants in the NHANES 1999–2002 data, Int. J. Environ. Res. Public Health 7 (7) (2010) 2988–3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [467].Roos V, Ronn M, Salihovic S, Lind L, van Bavel B, Kullberg J, Johansson L, Ahlstrom H, Lind PM, Circulating levels of persistent organic pollutants in relation to visceral and subcutaneous adipose tissue by abdominal MRI, Obesity (Silver Spring) 21 (2) (2013) 413–418. [DOI] [PubMed] [Google Scholar]
- [468].Ronn M, Lind L, van Bavel B, Salihovic S, Michaelsson K, Lind PM, Circulating levels of persistent organic pollutants associate in divergent ways to fat mass measured by DXA in humans, Chemosphere 85 (3) (2011) 335–343. [DOI] [PubMed] [Google Scholar]
- [469].Ben Hassine S, Hammami B, Ben Ameur W, El Megdiche Y, Barhoumi B, El Abidi R, Driss MR, Concentrations of organochlorine pesticides and polychlorinated biphenyls in human serum and their relation with age, gender, and BMI for the general population of Bizerte, Tunisia, Environ. Sci. Pollut. Res. Int 21 (10) (2014) 6303–6313. [DOI] [PubMed] [Google Scholar]
- [470].Zong G, Grandjean P, Wu H, Sun Q, Circulating persistent organic pollutants and body fat distribution: Evidence from NHANES 1999–2004, Obesity (Silver Spring) 23 (9) (2015) 1903–1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [471].Dirinck E, Jorens PG, Covaci A, Geens T, Roosens L, Neels H, Mertens I, Van Gaal L, Obesity and persistent organic pollutants: possible obesogenic effect of organochlorine pesticides and polychlorinated biphenyls, Obesity (Silver Spring) 19 (4) (2011) 709–714. [DOI] [PubMed] [Google Scholar]
- [472].Wolff MS, Anderson HA, Britton JA, Rothman N, Pharmacokinetic variability and modern epidemiology–the example of dichlorodiphenyltrichloroethane, body mass index, and birth cohort, Cancer Epidemiol Biomarkers Prev 16 (10) (2007) 1925–1930. [DOI] [PubMed] [Google Scholar]
- [473].Lee DH, Lind L, Jacobs DR Jr., Salihovic S, van Bavel B, Lind PM, Associations of persistent organic pollutants with abdominal obesity in the elderly: The Prospective Investigation of the Vasculature in Uppsala Seniors (PIVUS) study, Environ. Int 40 (2012) 170–178. [DOI] [PubMed] [Google Scholar]
- [474].Lee DH, Steffes MW, Sjodin A, Jones RS, Needham LL, Jacobs DR Jr., Low dose organochlorine pesticides and polychlorinated biphenyls predict obesity, dyslipidemia, and insulin resistance among people free of diabetes, PLoS ONE 6 (1) (2011), e15977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [475].Plouffe L, Bosson-Rieutort D, Madaniyazi L, Iwai-Shimada M, Nakai K, Tatsuta N, Nakayama SF, Verner M-A, Estimated postnatal p, p’-DDT and p, p’-DDE levels and body mass index at 42 months of age in a longitudinal study of Japanese children, Environmental Health 19 (1) (2020) 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [476].Valvi D, Mendez MA, Martinez D, Grimalt JO, Torrent M, Sunyer J, Vrijheid M, Prenatal concentrations of polychlorinated biphenyls, DDE, and DDT and overweight in children: a prospective birth cohort study, Environ. Health Perspect 120 (3) (2012) 451–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [477].Coker E, Chevrier J, Rauch S, Bradman A, Obida M, Crause M, Bornman R, Eskenazi B, Association between prenatal exposure to multiple insecticides and child body weight and body composition in the VHEMBE South African birth cohort, Environ. Int 113 (2018) 122–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [478].Warner M, Rauch S, Coker ES, Harley K, Kogut K, Sjödin A, Eskenazi B, Obesity in relation to serum persistent organic pollutant concentrations in CHAMACOS women, Environmental Epidemiology 2 (4) (2018) e032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [479].Heggeseth B, Harley K, Warner M, Jewell N, Eskenazi B, Detecting Associations between Early-Life DDT Exposures and Childhood Growth Patterns: A Novel Statistical Approach, PLoS ONE 10 (6) (2015) e0131443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [480].Delvaux I, Van Cauwenberghe J, Den Hond E, Schoeters G, Govarts E, Nelen V, Baeyens W, Van Larebeke N, Sioen I, Prenatal exposure to environmental contaminants and body composition at age 7–9 years, Environ. Res 132 (2014) 24–32. [DOI] [PubMed] [Google Scholar]
- [481].Iszatt N, Stigum H, Verner M-A, White RA, Govarts E, Murinova LP, Schoeters G, Trnovec T, Legler J, Pelé F, Botton J, Chevrier C, Wittsiepe J, Ranft U, Vandentorren S, Kasper-Sonnenberg M, Klümper C, Weisglas-Kuperus N, Polder A, Eggesbø M, Obelix, Prenatal and Postnatal Exposure to Persistent Organic Pollutants and Infant Growth: A Pooled Analysis of Seven European Birth Cohorts, Environ. Health Perspect 123 (7) (2015) 730–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [482].Vafeiadi M, Georgiou V, Chalkiadaki G, Rantakokko P, Kiviranta H, Karachaliou M, Fthenou E, Venihaki M, Sarri K, Vassilaki M, Kyrtopoulos SA, Oken E, Kogevinas M, Chatzi L, Association of Prenatal Exposure to Persistent Organic Pollutants with Obesity and Cardiometabolic Traits in Early Childhood: The Rhea Mother-Child Cohort (Crete, Greece), Environ. Health Perspect 123 (10) (2015) 1015–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [483].La Merrill MA, Krigbaum NY, Cirillo PM, Cohn BA, Association between maternal exposure to the pesticide dichlorodiphenyltrichloroethane (DDT) and risk of obesity in middle age, International journal of obesity (2005) 44(8) (2020) 1723–1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [484].Cirillo PM, La Merrill MA, Krigbaum NY, Cohn BA, Grandmaternal Perinatal Serum DDT in Relation to Granddaughter Early Menarche and Adult Obesity: Three Generations in the Child Health and Development Studies Cohort, Cancer Epidemiol. Biomark. Prev 8 (2021) 1480–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [485].Cupul-Uicab LA, Klebanoff MA, Brock JW, Longnecker MP, Prenatal Exposure to Persistent Organochlorines and Childhood Obesity in the U.S. Collaborative Perinatal Project, Environ. Health Perspect 121 (9) (2013) 1103–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [486].Garced S, Torres-Sanchez L, Cebrian ME, Claudio L, Lopez-Carrillo L, Prenatal dichlorodiphenyldichloroethylene (DDE) exposure and child growth during the first year of life, Environ. Res 113 (2012) 58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [487].Hoyer BB, Ramlau-Hansen CH, Vrijheid M, Valvi D, Pedersen HS, Zviezdai V, Jonsson BA, Lindh CH, Bonde JP, Toft G, Anthropometry in 5- to 9-Year-Old Greenlandic and Ukrainian Children in Relation to Prenatal Exposure to Perfluorinated Alkyl Substances, Environ. Health Perspect 123 (8) (2015) 841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [488].Lauritzen HB, Larose TL, Oien T, Sandanger TM, Odland JO, van de Bor M, Jacobsen GW, Prenatal exposure to persistent organic pollutants and child overweight/obesity at 5-year follow-up: a prospective cohort study, Environ Health 17 (1) (2018) 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [489].Lee HA, Park SH, Hong YS, Ha EH, Park H, The Effect of Exposure to Persistent Organic Pollutants on Metabolic Health among KOREAN Children during a 1-Year Follow-Up, Int. J. Environ. Res. Public Health 13 (3) (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [490].Karlsen M, Grandjean P, Weihe P, Steuerwald U, Oulhote Y, Valvi D, Early-life exposures to persistent organic pollutants in relation to overweight in preschool children, Reprod. Toxicol 68 (2017) 145–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [491].Verhulst SL, Nelen V, Hond ED, Koppen G, Beunckens C, Vael C, Schoeters G, Desager K, Intrauterine exposure to environmental pollutants and body mass index during the first 3 years of life, Environ. Health Perspect 117 (1) (2009) 122–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [492].Mendez MA, Garcia-Esteban R, Guxens M, Vrijheid M, Kogevinas M, Goni F, Fochs S, Sunyer J, Prenatal organochlorine compound exposure, rapid weight gain, and overweight in infancy, Environ. Health Perspect 119 (2) (2011) 272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [493].Jusko TA, Koepsell TD, Baker RJ, Greenfield TA, Willman EJ, Charles MJ, Teplin SW, Checkoway H, Hertz-Picciotto I, Maternal DDT exposures in relation to fetal and 5-year growth, Epidemiology (Cambridge, Mass.) 17 (6) (2006) 692–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [494].Artacho-Cordón F, Fernández-Rodríguez M, Garde C, Salamanca E, Iribarne-Durán LM, Torné P, Expósito J, Papay-Ramírez L, Fernández MF, Olea N, Arrebola JP, Serum and adipose tissue as matrices for assessment of exposure to persistent organic pollutants in breast cancer patients, Environ. Res 142 (2015) 633–643. [DOI] [PubMed] [Google Scholar]
- [495].Karmaus W, Zhu X, Maternal concentration of polychlorinated biphenyls and dichlorodiphenyl dichlorethylene and birth weight in Michigan fish eaters: a cohort study, Environ Health 3 (1) (2004) 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [496].Brodie AE, Azarenko VA, Hu CY, Inhibition of increases of transcription factor mRNAs during differentiation of primary rat adipocytes by in vivo 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) treatment, Toxicol. Lett 90 (2–3) (1997) 91–95. [DOI] [PubMed] [Google Scholar]
- [497].Cimafranca MA, Hanlon PR, Jefcoate CR, TCDD administration after the pro-adipogenic differentiation stimulus inhibits PPARgamma through a MEK-dependent process but less effectively suppresses adipogenesis, Toxicol. Appl. Pharmacol 196 (1) (2004) 156–168. [DOI] [PubMed] [Google Scholar]
- [498].Nagashima H, Matsumura F, 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD)-induced down-regulation of glucose transporting activities in mouse 3T3-L1 preadipocyte, Journal of environmental science and health, Part. B, Pesticides, food contaminants, and agricultural wastes 37 (1) (2002) 1–14. [DOI] [PubMed] [Google Scholar]
- [499].Gadupudi G, Gourronc FA, Ludewig G, Robertson LW, Klingelhutz AJ, PCB126 inhibits adipogenesis of human preadipocytes, Toxicol. In Vitro 29 (1) (2015) 132–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [500].Gourronc FA, Perdew GH, Robertson LW, Klingelhutz AJ, PCB126 blocks the thermogenic beiging response of adipocytes, Environ. Sci. Pollut. Res. Int 27 (9) (2020) 8897–8904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [501].Arsenescu V, Arsenescu RI, King V, Swanson H, Cassis LA, Polychlorinated Biphenyl-77 Induces Adipocyte Differentiation and Proinflammatory Adipokines and Promotes Obesity and Atherosclerosis, Environ. Health Perspect 116 (6) (2008) 761–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [502].Zhang L, Hatzakis E, Nichols RG, Hao R, Correll J, Smith PB, Chiaro CR, Perdew GH, Patterson AD, Metabolomics Reveals that Aryl Hydrocarbon Receptor Activation by Environmental Chemicals Induces Systemic Metabolic Dysfunction in Mice, Environ. Sci. Technol 49 (13) (2015) 8067–8077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [503].Korecka A, Dona A, Lahiri S, Tett AJ, Al-Asmakh M, Braniste V, D’Arienzo R, Abbaspour A, Reichardt N, Fujii-Kuriyama Y, Rafter J, Narbad A, Holmes E, Nicholson J, Arulampalam V, Pettersson S, Bidirectional communication between the Aryl hydrocarbon Receptor (AhR) and the microbiome tunes host metabolism, npj Biofilms Microbiomes 2 (2016) 16014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [504].Brawner KM, Yeramilli VA, Duck LW, Van Der Pol W, Smythies LE, Morrow CD, Elson CO, Martin CA, Depletion of dietary aryl hydrocarbon receptor ligands alters microbiota composition and function, Sci. Rep 9 (1) (2019) 14724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [505].Girer NG, Tomlinson CR, Elferink CJ, The Aryl Hydrocarbon Receptor in Energy Balance: The Road from Dioxin-Induced Wasting Syndrome to Combating Obesity with Ahr Ligands, Int. J. Mol. Sci 22 (1) (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [506].Duval C, Teixeira-Clerc F, Leblanc AF, Touch S, Emond C, Guerre-Millo M, Lotersztajn S, Barouki R, Aggerbeck M, Coumoul X, Chronic Exposure to Low Doses of Dioxin Promotes Liver Fibrosis Development in the C57BL/6J Diet-Induced Obesity Mouse Model, Environ. Health Perspect 125 (3) (2017) 428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [507].Weber LW, Lebofsky M, Stahl BU, Gorski JR, Muzi G, Rozman K, Reduced activities of key enzymes of gluconeogenesis as possible cause of acute toxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) in rats, Toxicology 66 (2) (1991) 133–144. [DOI] [PubMed] [Google Scholar]
- [508].Rojas IY, Moyer BJ, Ringelberg CS, Wilkins OM, Pooler DB, Ness DB, Coker S, Tosteson TD, Lewis LD, Chamberlin MD, Tomlinson C, Kynurenine-Induced Aryl Hydrocarbon Receptor Signaling in Mice Causes Body Mass Gain, Liver Steatosis, and Hyperglycemia, Obesity (Silver Spring) 29 (2) (2021) 337–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [509].Hoyeck MP, Merhi RC, Blair HL, Spencer CD, Payant MA, Martin Alfonso DI, Zhang M, Matteo G, Chee MJ, Bruin JE, Female mice exposed to low doses of dioxin during pregnancy and lactation have increased susceptibility to diet-induced obesity and diabetes, Molecular metabolism 42 (2020), 101104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [510].Brulport A, Le Corre L, Chagnon M-C, Chronic exposure of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) induces an obesogenic effect in C57BL/6J mice fed a high fat diet, Toxicology 390 (2017) 43–52. [DOI] [PubMed] [Google Scholar]
- [511].Merrill ML, Kuruvilla BS, Pomp D, Birnbaum LS, Threadgill DW, Dietary Fat Alters Body Composition, Mammary Development, and Cytochrome P450 Induction after Maternal TCDD Exposure in DBA/2J Mice with Low-Responsive Aryl Hydrocarbon Receptors, Environ. Health Perspect 117 (9) (2009) 1414–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [512].Eskenazi B, Warner M, Brambilla P, Signorini S, Ames J, Mocarelli P, The Seveso accident: A look at 40 years of health research and beyond, Environ. Int 121 (Pt 1) (2018) 71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [513].Goodman M, Narayan KM, Flanders D, Chang ET, Adami HO, Boffetta P, Mandel JS, Dose-response relationship between serum 2,3,7,8-tetrachlorodibenzo-p-dioxin and diabetes mellitus: a meta-analysis, Am. J. Epidemiol 181 (6) (2015) 374–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [514].Taylor KW, Novak RF, Anderson HA, Birnbaum LS, Blystone C, Devito M, Jacobs D, Köhrle J, Lee DH, Rylander L, Rignell-Hydbom A, Tornero-Velez R, Turyk ME, Boyles AL, Thayer KA, Lind L, Evaluation of the association between persistent organic pollutants (POPs) and diabetes in epidemiological studies: a national toxicology program workshop review, Environ. Health Perspect 121 (7) (2013) 774–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [515].de Cock M, van de Bor M, Obesogenic effects of endocrine disruptors, what do we know from animal and human studies? Environ. Int 70 (2014) 15–24. [DOI] [PubMed] [Google Scholar]
- [516].Tang-Péronard JL, Andersen HR, Jensen TK, Heitmann BL, Endocrine-disrupting chemicals and obesity development in humans: A review, Obes. Rev 12 (8) (2011) 622–636. [DOI] [PubMed] [Google Scholar]
- [517].De Silva AO, Armitage JM, Bruton TA, Dassuncao C, Heiger-Bernays W, Hu XC, Kärrman A, Kelly B, Ng C, Robuck A, Sun M, Webster TF, Sunderland EM, PFAS Exposure Pathways for Humans and Wildlife: A Synthesis of Current Knowledge and Key Gaps in Understanding, Environ. Toxicol. Chem 40 (3) (2021) 631–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [518].Blake BE, Fenton SE, Early life exposure to per- and polyfluoroalkyl substances (PFAS) and latent health outcomes: A review including the placenta as a target tissue and possible driver of peri- and postnatal effects, Toxicology 443 (2020) 152565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [519].Fromme H, Tittlemier SA, Völkel W, Wilhelm M, Twardella D, Perfluorinated compounds–exposure assessment for the general population in Western countries, Int. J. Hyg. Environ. Health 212 (3) (2009) 239–270. [DOI] [PubMed] [Google Scholar]
- [520].Inoue K, Okada F, Ito R, Kato S, Sasaki S, Nakajima S, Uno A, Saijo Y, Sata F, Yoshimura Y, Kishi R, Nakazawa H, Perfluorooctane sulfonate (PFOS) and related perfluorinated compounds in human maternal and cord blood samples: assessment of PFOS exposure in a susceptible population during pregnancy, Environ. Health Perspect 112 (11) (2004) 1204–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [521].Gützkow KB, Haug LS, Thomsen C, Sabaredzovic A, Becher G, Brunborg G, Placental transfer of perfluorinated compounds is selective–a Norwegian Mother and Child sub-cohort study, Int. J. Hyg. Environ. Health 215 (2) (2012) 216–219. [DOI] [PubMed] [Google Scholar]
- [522].Fisher M, Arbuckle TE, Liang CL, LeBlanc A, Gaudreau E, Foster WG, Haines D, Davis K, Fraser WD, Concentrations of persistent organic pollutants in maternal and cord blood from the maternal-infant research on environmental chemicals (MIREC) cohort study, Environ Health 15 (1) (2016) 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [523].Qi W, Clark JM, Timme-Laragy AR, Park Y, Perfluorobutanesulfonic acid (PFBS) potentiates adipogenesis of 3T3-L1 adipocytes, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 120 (2018) 340–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [524].Watkins AM, Wood CR, Lin MT, Abbott BD, The effects of perfluorinated chemicals on adipocyte differentiation in vitro, Mol. Cell. Endocrinol 400 (2015) 90–101. [DOI] [PubMed] [Google Scholar]
- [525].Qiu T, Chen M, Sun X, Cao J, Feng C, Li D, Wu W, Jiang L, Yao X, Perfluorooctane sulfonate-induced insulin resistance is mediated by protein kinase B pathway, Biochem. Biophys. Res. Commun 477 (4) (2016) 781–785. [DOI] [PubMed] [Google Scholar]
- [526].Sant KE, Annunziato K, Conlin S, Teicher G, Chen P, Venezia O, Downes GB, Park Y, Timme-Laragy AR, Developmental exposures to perfluorooctanesulfonic acid (PFOS) impact embryonic nutrition, pancreatic morphology, and adiposity in the zebrafish, Danio rerio, Environmental pollution (Barking, Essex 275 (2021) (1987), 116644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [527].Du Y, Shi X, Liu C, Yu K, Zhou B, Chronic effects of water-borne PFOS exposure on growth, survival and hepatotoxicity in zebrafish: a partial life-cycle test, Chemosphere 74 (5) (2009) 723–729. [DOI] [PubMed] [Google Scholar]
- [528].Rosen MB, Abbott BD, Wolf DC, Corton JC, Wood CR, Schmid JE, Das KP, Zehr RD, Blair ET, Lau C, Gene profiling in the livers of wild-type and PPARalpha-null mice exposed to perfluorooctanoic acid, Toxicol. Pathol 36 (4) (2008) 592–607. [DOI] [PubMed] [Google Scholar]
- [529].Rosen MB, Schmid JE, Das KP, Wood CR, Zehr RD, Lau C, Gene expression profiling in the liver and lung of perfluorooctane sulfonate-exposed mouse fetuses: comparison to changes induced by exposure to perfluorooctanoic acid, Reprod. Toxicol 27 (3–4) (2009) 278–288. [DOI] [PubMed] [Google Scholar]
- [530].Kudo N, Kawashima Y, Fish oil-feeding prevents perfluorooctanoic acid-induced fatty liver in mice, Toxicol. Appl. Pharmacol 145 (2) (1997) 285–293. [DOI] [PubMed] [Google Scholar]
- [531].Marques E, Pfohl M, Auclair A, Jamwal R, Barlock BJ, Sammoura FM, Goedken M, Akhlaghi F, Slitt AL, Perfluorooctanesulfonic acid (PFOS) administration shifts the hepatic proteome and augments dietary outcomes related to hepatic steatosis in mice, Toxicol. Appl. Pharmacol 408 (2020), 115250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [532].Wang L, Wang Y, Liang Y, Li J, Liu Y, Zhang J, Zhang A, Fu J, Jiang G, PFOS induced lipid metabolism disturbances in BALB/c mice through inhibition of low density lipoproteins excretion, Sci. Rep 4 (2014) 4582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [533].Shabalina IG, Kramarova TV, Mattsson CL, Petrovic N, Rahman Qazi M, Csikasz RI, Chang SC, Butenhoff J, DePierre JW, Cannon B, Nedergaard J, The Environmental Pollutants Perfluorooctane Sulfonate and Perfluorooctanoic Acid Upregulate Uncoupling Protein 1 (UCP1) in Brown-Fat Mitochondria Through a UCP1-Dependent Reduction in Food Intake, Toxicological sciences : an official journal of the Society of, Toxicology 146 (2) (2015) 334–343. [DOI] [PubMed] [Google Scholar]
- [534].Hines EP, White SS, Stanko JP, Gibbs-Flournoy EA, Lau C, Fenton SE, Phenotypic dichotomy following developmental exposure to perfluorooctanoic acid (PFOA) in female CD-1 mice: Low doses induce elevated serum leptin and insulin, and overweight in mid-life, Mol. Cell. Endocrinol 304 (1–2) (2009) 97–105. [DOI] [PubMed] [Google Scholar]
- [535].Tian YP, Zeng XW, Bloom MS, Lin S, Wang SQ, Yim SHL, Yang M, Chu C, Gurram N, Hu LW, Liu KK, Yang BY, Feng D, Liu RQ, Nian M, Dong GH, Isomers of perfluoroalkyl substances and overweight status among Chinese by sex status: Isomers of C8 Health Project in China, Environ. Int 124 (2019) 130–138. [DOI] [PubMed] [Google Scholar]
- [536].Chen A, Jandarov R, Zhou L, Calafat AM, Zhang G, Urbina EM, Sarac J, Augustin DH, Caric T, Bockor L, Petranovic MZ, Novokmet N, Missoni S, Rudan P, Deka R, Association of perfluoroalkyl substances exposure with cardiometabolic traits in an island population of the eastern Adriatic coast of Croatia, The Science of the total environment 683 (2019) 29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [537].Christensen KY, Raymond M, Meiman J, Perfluoroalkyl substances and metabolic syndrome, Int. J. Hyg. Environ. Health 222 (1) (2019) 147–153. [DOI] [PubMed] [Google Scholar]
- [538].He X, Liu Y, Xu B, Gu L, Tang W, PFOA is associated with diabetes and metabolic alteration in US men: National Health and Nutrition Examination Survey 2003–2012, The Science of the total environment 625 (2018) 566–574. [DOI] [PubMed] [Google Scholar]
- [539].Harris MH, Rifas-Shiman SL, Calafat AM, Ye X, Mora AM, Webster TF, Oken E, Sagiv SK, Predictors of Per- and Polyfluoroalkyl Substance (PFAS) Plasma Concentrations in 6–10 Year Old American Children, Environ. Sci. Technol 51 (9) (2017) 5193–5204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [540].Scinicariello F, Buser MC, Abadin HG, Attanasio R, Perfluoroalkyl substances and anthropomorphic measures in children (ages 3–11 years), NHANES 2013–2014, Environ. Res 186 (2020), 109518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [541].Averina M, Brox J, Huber S, Furberg AS, Exposure to perfluoroalkyl substances (PFAS) and dyslipidemia, hypertension and obesity in adolescents, Environ Res, The Fit Futures study, 2021, p. 110740. [DOI] [PubMed] [Google Scholar]
- [542].Kingsley SL, Walker DI, Calafat AM, Chen A, Papandonatos GD, Xu Y, Jones DP, Lanphear BP, Pennell KD, Braun JM, Metabolomics of childhood exposure to perfluoroalkyl substances: a cross-sectional study, Metabolomics : Official journal of the Metabolomic Society 15 (7) (2019) 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [543].Alderete TL, Jin R, Walker DI, Valvi D, Chen Z, Jones DP, Peng C, Gilliland FD, Berhane K, Conti DV, Goran MI, Chatzi L, Perfluoroalkyl substances, metabolomic profiling, and alterations in glucose homeostasis among overweight and obese Hispanic children: A proof-of-concept analysis, Environ. Int 126 (2019) 445–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [544].Liu G, Dhana K, Furtado JD, Rood J, Zong G, Liang L, Qi L, Bray GA, DeJonge L, Coull B, Grandjean P, Sun Q, Perfluoroalkyl substances and changes in body weight and resting metabolic rate in response to weight-loss diets: A prospective study, PLoS Med. 15 (2) (2018), e1002502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [545].Cardenas A, Hauser R, Gold DR, Kleinman KP, Hivert MF, Fleisch AF, Lin PD, Calafat AM, Webster TF, Horton ES, Oken E, Association of Perfluoroalkyl and Polyfluoroalkyl Substances With Adiposity, JAMA network open 1 (4) (2018), e181493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [546].Domazet SL, Grontved A, Timmermann AG, Nielsen F, Jensen TK, Longitudinal Associations of Exposure to Perfluoroalkylated Substances in Childhood and Adolescence and Indicators of Adiposity and Glucose Metabolism 6 and 12 Years Later: The European Youth Heart Study, Diabetes Care 39 (10) (2016) 1745–1751. [DOI] [PubMed] [Google Scholar]
- [547].Johnson PI, Sutton P, Atchley DS, Koustas E, Lam J, Sen S, Robinson KA, Axelrad DA, Woodruff TJ, The Navigation Guide - evidence-based medicine meets environmental health: systematic review of human evidence for PFOA effects on fetal growth, Environ. Health Perspect 122 (10) (2014) 1028–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [548].Cao T, Qu A, Li Z, Wang W, Liu R, Wang X, Nie Y, Sun S, Zhang X, Liu X, The relationship between maternal perfluoroalkylated substances exposure and low birth weight of offspring: a systematic review and meta-analysis, Environ. Sci. Pollut. Res. Int (2021). [DOI] [PubMed] [Google Scholar]
- [549].Starling AP, Adgate JL, Hamman RF, Kechris K, Calafat AM, Ye X, Dabelea D, Perfluoroalkyl Substances during Pregnancy and Offspring Weight and Adiposity at Birth: Examining Mediation by Maternal Fasting Glucose in the Healthy Start Study, Environ. Health Perspect 125 (6) (2017), 067016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [550].Kobayashi S, Azumi K, Goudarzi H, Araki A, Miyashita C, Kobayashi S, Itoh S, Sasaki S, Ishizuka M, Nakazawa H, Ikeno T, Kishi R, Effects of prenatal perfluoroalkyl acid exposure on cord blood IGF2/H19 methylation and ponderal index: The Hokkaido Study, J. Eposure Sci. Environ. Epidemiol 27 (3) (2017) 251–259. [DOI] [PubMed] [Google Scholar]
- [551].Mitro SD, Sagiv SK, Rifas-Shiman SL, Calafat AM, Fleisch AF, Jaacks LM, Williams PL, Oken E, James-Todd TM, Per- and Polyfluoroalkyl Substance Exposure, Gestational Weight Gain, and Postpartum Weight Changes in Project Viva, Obesity (Silver Spring) 28 (10) (2020) 1984–1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [552].Romano ME, Gallagher LG, Eliot MN, Calafat AM, Chen A, Yolton K, Lanphear B, Braun JM, Per- and polyfluoroalkyl substance mixtures and gestational weight gain among mothers in the Health Outcomes and Measures of the Environment study, Int. J. Hyg. Environ. Health 231 (2021), 113660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [553].Marks KJ, Jeddy Z, Flanders WD, Northstone K, Fraser A, Calafat AM, Kato K, Hartman TJ, Maternal serum concentrations of perfluoroalkyl substances during pregnancy and gestational weight gain: The Avon Longitudinal Study of Parents and Children, Reprod. Toxicol 90 (2019) 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [554].Jaacks LM, Boyd Barr D, Sundaram R, Grewal J, Zhang C, Buck Louis GM, Pre-Pregnancy Maternal Exposure to Persistent Organic Pollutants and Gestational Weight Gain: A Prospective Cohort Study, Int. J. Environ. Res. Public Health 13 (9) (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [555].Ashley-Martin J, Dodds L, Arbuckle TE, Morisset AS, Fisher M, Bouchard MF, Shapiro GD, Ettinger AS, Monnier P, Dallaire R, Taback S, Fraser W, Maternal and Neonatal Levels of Perfluoroalkyl Substances in Relation to Gestational Weight Gain, Int. J. Environ. Res. Public Health 13 (1) (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [556].Starling AP, Brinton JT, Glueck DH, Shapiro AL, Harrod CS, Lynch AM, Siega-Riz AM, Dabelea D, Associations of maternal BMI and gestational weight gain with neonatal adiposity in the Healthy Start study, Am. J. Clin. Nutr 101 (2) (2015) 302–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [557].Chen Z, Yang T, Walker DI, Thomas DC, Qiu C, Chatzi L, Alderete TL, Kim JS, Conti DV, Breton CV, Liang D, Hauser ER, Jones DP, Gilliland FD, Dysregulated lipid and fatty acid metabolism link perfluoroalkyl substances exposure and impaired glucose metabolism in young adults, Environ. Int 145 (2020), 106091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [558].Braun JM, Chen A, Romano ME, Calafat AM, Webster GM, Yolton K, Lanphear BP, Prenatal perfluoroalkyl substance exposure and child adiposity at 8 years of age: The HOME study, Obesity (Silver Spring) 24 (1) (2016) 231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [559].Liu P, Yang F, Wang Y, Yuan Z, Perfluorooctanoic Acid (PFOA) Exposure in Early Life Increases Risk of Childhood Adiposity: A Meta-Analysis of Prospective Cohort Studies, Int. J. Environ. Res. Public Health 15 (10) (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [560].Halldorsson TI, Rytter D, Haug LS, Bech BH, Danielsen I, Becher G, Henriksen TB, Olsen SF, Prenatal Exposure to Perfluorooctanoate and Risk of Overweight at 20 Years of Age: A Prospective Cohort Study, Environ. Health Perspect (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [561].Bloom MS, Commodore S, Ferguson PL, Neelon B, Pearce JL, Baumer A, Newman RB, Grobman W, Tita A, Roberts J, Skupski D, Palomares K, Nageotte M, Kannan K, Zhang C, Wapner R, Vena JE, Hunt KJ, Association between gestational PFAS exposure and Children’s adiposity in a diverse population, Environ. Res 203 (2022), 111820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [562].Barry V, Darrow LA, Klein M, Winquist A, Steenland K, Early life perfluorooctanoic acid (PFOA) exposure and overweight and obesity risk in adulthood in a community with elevated exposure, Environ. Res 132 (2014) 62–69. [DOI] [PubMed] [Google Scholar]
- [563].Andersen CS, Fei C, Gamborg M, Nohr EA, Sorensen TI, Olsen J, Prenatal exposures to perfluorinated chemicals and anthropometry at 7 years of age, Am. J. Epidemiol 178 (6) (2013) 921–927. [DOI] [PubMed] [Google Scholar]
- [564].Mérillon JM, Ramawat KG , Sweeteners: Pharmacology, Biotechnology, and Applications, Switzerland: Springer; (2018). [Google Scholar]
- [565].Kumar NS, Sharma A, Kishore DK, K., Food Safety and Human Health, London: Academic Press; (2019). [Google Scholar]
- [566].Gardiner C, Wylie-Rossett J, Gidding SS, Steffen LM, Johnson RK, Reader D, Lichtenstein AH, Non-nutritive sweeteners: current use and health perspectives: a scientific statement from the American Heart association and the American Diabetes Association, Diabetes Care 35 (2012) 1798–1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [567].Moriconi E, Feraco A, Marzolla V, Infante M, Lombardo M, Fabbri A, Caprio M, ‘Neuroendocrine and Metabolic Effects of Low-Calorie and Non-Calorie Sweeteners, Front. Endocrinol 11 (2020) 444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [568].Liauchonak I, Qirri B, Dawoud F, Riat Y, Szewczuk MR, Non-nuitritive sweeteners and their implication on the development of metabolic syndrome, Nutrients 11 (2019) 644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [569].Rother KI, Conway EM, Sylvetsky AC, How non-nutritive sweeteners influence hormones and health, Trends Endocrinol. Metab 29 (7) (2018). [DOI] [PubMed] [Google Scholar]
- [570].Azad MB, Archibald A, Tomczyk MM, Head A, Cheung KG, Souza RJ, Becker AB, Mandhane PJ, Turvey SE, Moraes TJ, Sears MR, Subbarao P, Dolinsky VW, Nonnutritive sweetener consumption during pregnancy, adiposity, and adipocyte differentiation in offspring: evidence from humans, mice, and cells, International Journal of Obesity 44 (2020) 2137–2148. [DOI] [PubMed] [Google Scholar]
- [571].Rosales-Gomez CA, Martinez-Carrillo BE, Resendiz-Albor AA, Ramirez-Duran N, Valdes-Ramos R, Mondragon-Velasquez T, Escoto-Herrera JA, Chronic Consumption of Sweeteners and Its Effect on Glycaemia, Cytokines, Hormones, and Lymphocytes of GALT in CD1 Mice, Biomed Res. Int (2018) 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [572].Suez J, Korem T, Zeevi D, Zilberman-Schapira G, Thaiss CA, Maza O, Israeli D, Zmora N, Gilad S, Weinberger A, Kuperman Y, Harmelin A, Kolodkin-Gal I, Shapiro H, Halpern Z, Segal E, Elinav E, Artificial sweeteners induce glucose intolerance by altering the gut microbiota, Nature 514 (7521) (2014) 181–186. [DOI] [PubMed] [Google Scholar]
- [573].Kundu N, Domingues CC, Patel J, Aljishi M, Ahmadi N, Fakhri M, Sylvetsky AC, Sen S, Sucralose promotes accumulation of reactive oxygen species (ROS) and adipogenesis in mesenchymal stromal cells, Stem Cell Res. Ther 11 (1) (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [574].Palkowska-Gozdzik E, Bigos A, Rosolowska-Huszcz D, ‘Type of sweet flavour carrier affects thyroid axis activity in male rats’, Eur. J. Nutr 57 (2018) 773–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [575].Romo-Romo A, Aguilar-Salinas CA, Lopez-Carrasco MG, Guillen-Pineda LE, Brito-Cordova GX, Gomez-Diaz RA, Gomez-Perez FJ, Almeda-Valdes P, ‘Sucralose Consumption over 2 Weeks in Healthy Subjects Does Not Modify Fasting Plasma Concentrations of Appetite-Regulating Hormones: A Randomized Clinical Trial’, Journal of the Academy of, Nutrition and Dietetics 120 (8) (2020) 1295–1304. [DOI] [PubMed] [Google Scholar]
- [576].Dalenberg JR, Patel BP, Denis R, Vinke PC, Luquet S, Small DM, Short-Term Consumption of Sucralose with, but Not without, Carbohydrate Impairs Neural and Metabolic Sensitivity to Sugar in Humans, Cell Metab. 31 (2020) 493–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [577].Azeez OH, Alkass SY, Persike DS, Long-Term Saccharin Consumption and Increased Risk of Obesity, Diabetes, Hepatic Dysfunction, and Renal Impairment in Rats, Med. Lith 55 (10) (2019) 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [578].Y.J. Zhao X, Chen K, Song L, Sun B, Wei X, Effects of saccharin supplementation on body weight, sweet receptor mRNA expression and appetite signals regulation in post-weanling rats, Peptides 107 (2018) 32–38. [DOI] [PubMed] [Google Scholar]
- [579].Reiss R, Chang ET, Richardson RJ, Goodman M, A review of epidemiologic studies of low-level exposures to organophosphorus insecticides in non-occupational populations, Crit. Rev. Toxicol 45 (7) (2015) 531–641. [DOI] [PubMed] [Google Scholar]
- [580].Blanco J, Guardia-Escote L, Mulero M, Basaure P, Biosca-Brull J, Cabré M, Colomina MT, Domingo JL, Sánchez DJ, Obesogenic effects of chlorpyrifos and its metabolites during the differentiation of 3T3-L1 preadipocytes, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 137 (2020), 111171. [DOI] [PubMed] [Google Scholar]
- [581].Meggs WJ, Brewer KL, Weight gain associated with chronic exposure to chlorpyrifos in rats, J. Med. Toxicol 3 (3) (2007) 89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [582].Peris-Sampedro F, Cabré M, Basaure P, Reverte I, Domingo JL, Teresa Colomina M, Adulthood dietary exposure to a common pesticide leads to an obese-like phenotype and a diabetic profile in apoE3 mice, Environ. Res 142 (2015) 169–176. [DOI] [PubMed] [Google Scholar]
- [583].Guardia-Escote L, Blanco J, Basaure P, Biosca-Brull J, Verkaik-Schakel RN, Cabré M, Peris-Sampedro F, Pérez-Fernández C, Sánchez-Santed F, Plösch T, Domingo JL, Colomina MT, Sex and Exposure to Postnatal Chlorpyrifos Influence the Epigenetics of Feeding-Related Genes in a Transgenic APOE Mouse Model: Long-Term Implications on Body Weight after a High-Fat Diet, Int. J. Environ. Res. Public Health 18 (1) (2020) 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [584].Basaure P, Guardia-Escote L, Biosca-Brull J, Blanco J, Cabré M, Peris-Sampedro F, Sánchez-Santed F, Domingo JL, Colomina MT, Exposure to chlorpyrifos at different ages triggers APOE genotype-specific responses in social behavior, body weight and hypothalamic gene expression, Environ. Res 178 (2019), 108684. [DOI] [PubMed] [Google Scholar]
- [585].Fang B, Li JW, Zhang M, Ren FZ, Pang GF, Chronic chlorpyrifos exposure elicits diet-specific effects on metabolism and the gut microbiome in rats, Food Chem. Toxicol 111 (2018) 144–152. [DOI] [PubMed] [Google Scholar]
- [586].Liang Y, Zhan J, Liu D, Luo M, Han J, Liu X, Liu C, Cheng Z, Zhou Z, Wang P, Organophosphorus pesticide chlorpyrifos intake promotes obesity and insulin resistance through impacting gut and gut microbiota, Microbiome 7 (1) (2019) 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [587].Zhang Y, Jia Q, Hu C, Han M, Guo Q, Li S, Bo C, Zhang Y, Qi X, Sai L, Peng C, Effects of chlorpyrifos exposure on liver inflammation and intestinal flora structure in mice, Toxicol Res (Camb) 10 (1) (2021) 141–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [588].Samarghandian S, Foadoddin M, Zardast M, Mehrpour O, Sadighara P, Roshanravan B, Farkhondeh T, The impact of age-related sub-chronic exposure to chlorpyrifos on metabolic indexes in male rats, Environ. Sci. Pollut. Res. Int 27 (18) (2020) 22390–22399. [DOI] [PubMed] [Google Scholar]
- [589].Lassiter TL, Brimijoin S, Rats gain excess weight after developmental exposure to the organophosphorothionate pesticide, chlorpyrifos, Neurotoxicol. Teratol 30 (2) (2008) 125–130. [DOI] [PubMed] [Google Scholar]
- [590].Park Y, Kim Y, Kim J, Yoon KS, Clark J, Lee J, Imidacloprid, a neonicotinoid insecticide, potentiates adipogenesis in 3T3-L1 adipocytes, J. Agric. Food Chem 61 (1) (2013) 255–259. [DOI] [PubMed] [Google Scholar]
- [591].Sun Q, Xiao X, Kim Y, Kim D, Yoon KS, Clark JM, Park Y, Imidacloprid Promotes High Fat Diet-Induced Adiposity and Insulin Resistance in Male C57BL/6J Mice, J. Agric. Food. Chem 64 (49) (2016) 9293–9306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [592].Sun Q, Qi W, Xiao X, Yang SH, Kim D, Yoon KS, Clark JM, Park Y, Imidacloprid Promotes High Fat Diet-Induced Adiposity in Female C57BL/6J Mice and Enhances Adipogenesis in 3T3-L1 Adipocytes via the AMPKalpha-Mediated Pathway, J. Agric. Food Chem 65 (31) (2017) 6572–6581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [593].Ndonwi EN, Atogho-Tiedeu B, Lontchi-Yimagou E, Shinkafi TS, Nanfa D, Balti EV, Katte JC, Mbanya A, Matsha T, Mbanya JC, Shakir A, Sobngwi E, Metabolic effects of exposure to pesticides during gestation in female Wistar rats and their offspring: a risk factor for diabetes? Toxicological research 36 (3) (2020) 249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [594].Xiao X, Sun Q, Kim Y, Yang SH, Qi W, Kim D, Yoon KS, Clark JM, Park Y, Exposure to permethrin promotes high fat diet-induced weight gain and insulin resistance in male C57BL/6J mice, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 111 (2018) 405–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [595].Xiao X, Qi W, Clark JM, Park Y, Permethrin potentiates adipogenesis via intracellular calcium and endoplasmic reticulum stress-mediated mechanisms in 3T3-L1 adipocytes, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 109 (Pt 1) (2017) 123–129. [DOI] [PubMed] [Google Scholar]
- [596].Kim J, Park Y, Yoon KS, Clark JM, Park Y, Permethrin alters adipogenesis in 3T3-L1 adipocytes and causes insulin resistance in C2C12 myotubes, J. Biochem. Mol. Toxicol 28 (9) (2014) 418–424. [DOI] [PubMed] [Google Scholar]
- [597].Sargis RM, Neel BA, Brock CO, Lin Y, Hickey AT, Carlton DA, Brady MJ, The novel endocrine disruptor tolylfluanid impairs insulin signaling in primary rodent and human adipocytes through a reduction in insulin receptor substrate-1 levels, BBA 2012 (1822) 952–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [598].Chen Y, McCommis KS, Ferguson D, Hall AM, Harris CA, Finck BN, Inhibition of the Mitochondrial Pyruvate Carrier by Tolylfluanid, Endocrinology 159 (2) (2018) 609–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [599].Regnier SM, Kirkley AG, Ruiz D, Kamau W, Wu Q, Kannan K, Sargis RM, Diet-dependence of metabolic perturbations mediated by the endocrine disruptor tolylfluanid, Endocr Connect 7 (1) (2018) 159–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [600].Ruiz D, Regnier SM, Kirkley AG, Hara M, Haro F, Aldirawi H, Dybala MP, Sargis RM, Developmental exposure to the endocrine disruptor tolylfluanid induces sex-specific later-life metabolic dysfunction, Reprod. Toxicol 89 (2019) 74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [601].Zinöcker MK, Lindseth IA, The Western Diet-Microbiome-Host Interaction and Its Role in Metabolic Disease, Nutrients 10 (3) (2018) 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [602].Lustig RH, Ultraprocessed Food: Addictive, Toxic, and Ready for Regulation, Nutrients 12 (11) (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [603].Wong SK, Chin K-Y, Suhaimi FH, Fairus A, Ima-Nirwana S, Animal models of metabolic syndrome: a review, Nutrition & Metabolism 13 (1) (2016) 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [604].Simmons AL, Schlezinger JJ, Corkey BE, What Are We Putting in Our Food That Is Making Us Fat? Food Additives, Contaminants, and Other Putative Contributors to Obesity, Current obesity reports 3 (2) (2014) 273–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [605].Sharma S, Fernandes MF, Fulton S, Adaptations in brain reward circuitry underlie palatable food cravings and anxiety induced by high-fat diet withdrawal, International journal of obesity (2005) 37(9) (2013) 1183–91. [DOI] [PubMed] [Google Scholar]
- [606].Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, Griffin NW, Lombard V, Henrissat B, Bain JR, Muehlbauer MJ, Ilkayeva O, Semenkovich CF, Funai K, Hayashi DK, Lyle BJ, Martini MC, Ursell LK, Clemente JC, Van Treuren W, Walters WA, Knight R, Newgard CB, Heath AC, Gordon JI, Gut Microbiota from Twins Discordant for Obesity Modulate Metabolism in Mice, Science 341 (6150) (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [607].Stanhope KL, Sugar consumption, metabolic disease and obesity: The state of the controversy, Crit. Rev. Clin. Lab. Sci 53 (1) (2016) 52–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [608].Lustig RH, Fructose: metabolic, hedonic, and societal parallels with ethanol, J. Am. Diet. Assoc 110 (2010) 1307–1321. [DOI] [PubMed] [Google Scholar]
- [609].Muriel P, López-Sánchez P, Ramos-Tovar E, Fructose and the Liver, Int. J. Mol. Sci 22 (13) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [610].Schwarz JM, Noworolski SM, Erkin-Cakmak A, K. NJ, Wen MJ, Tai VW, Jones GM, Palii SP, Velasco-Alin M, Pan K, Patterson BW, Gugliucci A, Lustig RH, Mulligan K, Impact of dietary fructose restriction on liver fat, de novo lipogenesis, and insulin kinetics in children with obesity, Gastroenterology 153 (2017) 743–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [611].Bowen J, Noakes M, Clifton PM, Appetite hormones and energy intake in obese men after consumption of fructose, glucose and whey protein beverages, International journal of obesity (2005) 31(11) (2007) 1696–703. [DOI] [PubMed] [Google Scholar]
- [612].Goran MI, Dumke K, Bouret SG, Kayser B, Walker RW, Blumberg B, The obesogenic effect of high fructose exposure during early development, Nature reviews. Endocrinology 9 (8) (2013) 494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [613].Calafat AM, Ye X, Wong L-Y, Bishop AM, Needham LL, Urinary concentrations of four parabens in the U.S. population: NHANES 2005-2006, Environmental health perspectives 118(5) (2010) 679–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [614].Hu P, Chen X, Whitener RJ, Boder ET, Jones JO, Porollo A, Chen J, Zhao L, Effects of parabens on adipocyte differentiation, Toxicological sciences : an official journal of the Society of, Toxicology 131 (1) (2013) 56–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [615].Hu P, Overby H, Heal E, Wang S, Chen J, Shen C-L, Zhao L, Methylparaben and butylparaben alter multipotent mesenchymal stem cell fates towards adipocyte lineage, Toxicol. Appl. Pharmacol 329 (2017) 48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [616].Leppert B, Strunz S, Seiwert B, Schlittenbauer L, Schlichting R, Pfeiffer C, Roder S, Bauer M, Borte M, Stangl GI, Schoneberg T, Schulz A, Karkossa I, Rolle-Kampczyk UE, Thurmann L, von Bergen M, Escher BI, Junge KM, Reemtsma T, Lehmann I, Polte T, Maternal paraben exposure triggers childhood overweight development, Nat. Commun 11 (1) (2020) 561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [617].Hu J, Raikhel V, Gopalakrishnan K, Fernandez-Hernandez H, Lambertini L, Manservisi F, Falcioni L, Bua L, Belpoggi F, S LT, Chen J, Effect of postnatal low-dose exposure to environmental chemicals on the gut microbiome in a rodent model, Microbiome 4(1) (2016) 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [618].Chassaing B, Koren O, Goodrich JK, Poole AC, Srinivasan S, Ley RE, Gewirtz AT, Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome, Nature 519 (7541) (2015) 92–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [619].Sun Z, Tang Z, Yang X, Liu QS, Liang Y, Fiedler H, Zhang J, Zhou Q, Jiang G, Perturbation of 3-tert-butyl-4-hydroxyanisole in adipogenesis of male mice with normal and high fat diets, Sci. Total Environ 703 (2020), 135608. [DOI] [PubMed] [Google Scholar]
- [620].Sun Z, Yang X, Liu QS, Li C, Zhou Q, Fiedler H, Liao C, Zhang J, Jiang G, Butylated hydroxyanisole isomers induce distinct adipogenesis in 3T3-L1 cells, J. Hazard. Mater 379 (2019), 120794. [DOI] [PubMed] [Google Scholar]
- [621].Türküner MS, Özcan F, Monosodium glutamate restricts the adipogenic potential of 3T3 - L1 preadipocytes through mitotic clonal expansion, Cell Biology International 44 (3) (2020) 744–754. [DOI] [PubMed] [Google Scholar]
- [622].Olney JW, Brain lesions, obesity, and other disturbances in mice treated with monosodium glutamate, Science 164 (3880) (1969) 719–721. [DOI] [PubMed] [Google Scholar]
- [623].Chakraborty SP, Patho-physiological and toxicological aspects of monosodium glutamate, Toxicol. Mech. Methods 29 (6) (2019) 389–396. [DOI] [PubMed] [Google Scholar]
- [624].Hernández Bautista RJ, Mahmoud AM, Königsberg M, López Díaz Guerrero N.e., Obesity: Pathophysiology, monosodium glutamate-induced model and anti-obesity medicinal plants, Biomed. Pharmacother 111 (2019) 503–516. [DOI] [PubMed] [Google Scholar]
- [625].Shannon M, Green B, Willars G, Wilson J, Matthews N, Lamb J, Gillespie A, Connolly L, The endocrine disrupting potential of monosodium glutamate (MSG) on secretion of the glucagon-like peptide-1 (GLP-1) gut hormone and GLP-1 receptor interaction, Toxicol. Lett 265 (2017) 97–105. [DOI] [PubMed] [Google Scholar]
- [626].Temkin AM, Bowers RR, Magaletta ME, Holshouser S, Maggi A, Ciana P, Guillette LJ, Bowden JA, Kucklick JR, Baatz JE, Spyropoulos DD, Effects of Crude Oil/Dispersant Mixture and Dispersant Components on PPARγ Activity in Vitro and in Vivo: Identification of Dioctyl Sodium Sulfosuccinate (DOSS; CAS #577-11-7) as a Probable Obesogen, Environ. Health Perspect 124 (1) (2016) 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [627].Temkin AM, Bowers RR, Ulmer CZ, Penta K, Bowden JA, Nyland J, Baatz JE, Spyropoulos DD, Increased adiposity, inflammation, metabolic disruption and dyslipidemia in adult male offspring of DOSS treated C57BL/6 dams, Sci. Rep 9 (1) (2019) 1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [628].Stoica A, Katzenellenbogen BS, Martin MB, Activation of estrogen receptor-alpha by the heavy metal cadmium, Mol. Endocrinol 14 (4) (2000) 545–553. [DOI] [PubMed] [Google Scholar]
- [629].M.b. v, m.b. z, a. a, c. v, l. a, f. e, m. s,, The endocrine disruptor cadmium: a new player in the pathophysiology of metabolic diseases, J. Endocrinol. Invest 44 (7) (2021) 1363–1377. [DOI] [PubMed] [Google Scholar]
- [630].Bimonte VM, Besharat ZM, Antonioni A, Cella V, Lenzi A, Ferretti E, Migliaccio S, The endocrine disruptor cadmium: a new player in the pathophysiology of metabolic diseases, J. Endocrinol. Invest 44 (7) (2021) 1363–1377. [DOI] [PubMed] [Google Scholar]
- [631].Fransson MN, Barregard L, Sallsten G, Akerstrom M, Johanson G, Physiologically-Based Toxicokinetic Model for Cadmium Using Markov-Chain Monte Carlo Analysis of Concentrations in Blood, Urine, and Kidney Cortex from Living Kidney Donors, Toxicological Sciences 141 (2) (2014) 365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [632].Jackson TW, Ryherd GL, Scheibly CM, Sasser AL, Guillette TC, Belcher SM, Gestational Cd Exposure in the CD-1 Mouse Induces Sex-Specific Hepatic Insulin Insensitivity, Obesity, and Metabolic Syndrome in Adult Female Offspring, Toxicological Sciences 178 (2) (2020) 264–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [633].Buha A, Đukić-Cosić D, Ćurčić M, Bulat Z, Antonijević B, Moulis J-M, Goumenou M, Wallace D, Emerging Links between Cadmium Exposure and Insulin Resistance: Human, Animal, and Cell Study Data, Toxics 8 (3) (2020) 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [634].Lee EJ, Moon JY, Yoo BS, Cadmium inhibits the differentiation of 3T3-L1 preadipocyte through the C/EBPα and PPARγ pathways, Drug Chem. Toxicol 35 (2) (2012) 225–231. [DOI] [PubMed] [Google Scholar]
- [635].Karakis I, Baumfeld Y, Landau D, Gat R, Shemesh N, Yitshak-Sade M, Tirosh O, Sarov B, Novack L, Exposure to metals and morbidity at eight years follow-up in women of childbearing age, Sci. Rep (2021) 11429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [636].Echeverría R, Vrhovnik P, Salcedo-Bellido I, Iribarne-Durán LM, Fiket Ž, Dolenec M, Martin-Olmedo P, Olea N, Arrebola JP, Levels and determinants of adipose tissue cadmium concentrations in an adult cohort from Southern Spain, The Science of the total environment 670 (2019) 1028–1036. [DOI] [PubMed] [Google Scholar]
- [637].Kuivenhoven M, Mason K, Arsenic Toxicity, StatPearls, StatPearls Publishing. [PubMed] [Google Scholar]
- [638].Copyright © 2021, StatPearls Publishing LLC., Treasure Island (FL), 2021. [Google Scholar]
- [639].Hou Y, Xue P, Woods CG, Wang X, Fu J, Yarborough K, Qu W, Zhang Q, Andersen ME, Pi J, Association between arsenic suppression of adipogenesis and induction of CHOP10 via the endoplasmic reticulum stress response, Environ. Health Perspect 121 (2) (2013) 237–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [640].Wang ZX, Jiang CS, Liu L, Wang XH, Jin HJ, Wu Q, Chen Q, The role of Akt on arsenic trioxide suppression of 3T3-L1 preadipocyte differentiation, Cell Res. 15 (5) (2005) 379–386. [DOI] [PubMed] [Google Scholar]
- [641].Rodriguez KF, Ungewitter EK, Crespo-Mejias Y, Liu C, Nicol B, Kissling GE, Yao H-H-C, Effects of in Utero Exposure to Arsenic during the Second Half of Gestation on Reproductive End Points and Metabolic Parameters in Female CD-1 Mice, Environ. Health Perspect 124 (3) (2016) 336–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [642].Rodriguez KF, Mellouk N, Ungewitter EK, Nicol B, Liu C, Brown PR, Willson CJ, Yao HHC, In utero exposure to arsenite contributes to metabolic and reproductive dysfunction in male offspring of CD-1 mice, Reprod. Toxicol 95 (2020) 95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [643].Carmean CM, Kirkley AG, Landeche M, Ye H, Chellan B, Aldirawi H, Roberts AA, Parsons PJ, Sargis RM, Arsenic Exposure Decreases Adiposity During High-Fat Feeding, Obesity (Silver Spring) 28 (5) (2020) 932–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [644].Paul DS, Walton FS, Saunders RJ, Styblo M, Characterization of the impaired glucose homeostasis produced in C57BL/6 mice by chronic exposure to arsenic and high-fat diet, Environ. Health Perspect 119 (8) (2011) 1104–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [645].Su CT, Lin HC, Choy CS, Huang YK, Huang SR, Hsueh YM, The relationship between obesity, insulin and arsenic methylation capability in Taiwan adolescents, The Science of the total environment 414 (2012) 152–158. [DOI] [PubMed] [Google Scholar]
- [646].Eick SM, Steinmaus C, Arsenic and Obesity: a Review of Causation and Interaction, Current environmental health reports 7 (3) (2020) 343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [647].Kassotis CD, Nagel SC, Stapleton HM, Unconventional oil and gas chemicals and wastewater-impacted water samples promote adipogenesis via PPARγ-dependent and independent mechanisms in 3T3-L1 cells, The Science of the total environment 640–641 (2018) 1601–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [648].Peng H, Sun J, Alharbi HA, Jones PD, Giesy JP, Wiseman S, Peroxisome Proliferator-Activated Receptor γ is a Sensitive Target for Oil Sands Process-Affected Water: Effects on Adipogenesis and Identification of Ligands, Environ. Sci. Technol 50 (14) (2016) 7816–7824. [DOI] [PubMed] [Google Scholar]
- [649].Kassotis CD, Klemp KC, Vu DC, Lin CH, Meng CX, Besch-Williford CL, Pinatti L, Zoeller RT, Drobnis EZ, Balise VD, Isiguzo CJ, Williams MA, Tillitt DE, Nagel SC, Endocrine-Disrupting Activity of Hydraulic Fracturing Chemicals and Adverse Health Outcomes After Prenatal Exposure in Male Mice, Endocrinology 156 (12) (2015) 4458–4473. [DOI] [PubMed] [Google Scholar]
- [650].Balise VD, Cornelius-Green JN, Parmenter B, Baxter S, Kassotis CD, Rector RS, Thyfault JP, Paterlini S, Palanza P, Ruiz D, Sargis R, Nagel SC, Developmental Exposure to a Mixture of Unconventional Oil and Gas Chemicals Increased Risk-Taking Behavior, Activity and Energy Expenditure in Aged Female Mice After a Metabolic Challenge, Front Endocrinol (Lausanne) 10 (2019) 460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [651].Benbrook CM, Trends in glyphosate herbicide use in the United States and globally, Environ. Sci. Eur 28 (1) (2016) 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [652].Biserni M, Mesnage R, Ferro R, Wozniak E, Xenakis T, Mein CA, Antoniou MN, Quizalofop-p-Ethyl Induces Adipogenesis in 3T3-L1 Adipocytes, Toxicological sciences : an official journal of the Society of, Toxicology 170 (2) (2019) 452–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [653].Martini CN, Gabrielli M, Codesido MM, del Vila MC, Glyphosate-based herbicides with different adjuvants are more potent inhibitors of 3T3-L1 fibroblast proliferation and differentiation to adipocytes than glyphosate alone, Comp. Clin. Pathol 25 (3) (2016) 607–613. [Google Scholar]
- [654].Kubsad D, Nilsson EE, King SE, Sadler-Riggleman I, Beck D, Skinner MK, Assessment of Glyphosate Induced Epigenetic Transgenerational Inheritance of Pathologies and Sperm Epimutations: Generational Toxicology, Sci. Rep 9 (1) (2019) 6372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [655].Aggarwal V, Deng X, Tuli A, Goh KS, Diazinon-chemistry and environmental fate: a California perspective, Rev. Environ. Contam. Toxicol 223 (2013) 107–140. [DOI] [PubMed] [Google Scholar]
- [656].Smith A, Yu X, Yin L, Diazinon exposure activated transcriptional factors CCAAT-enhancer-binding proteins α (C/EBPα) and peroxisome proliferator-activated receptor γ (PPARγ) and induced adipogenesis in 3T3-L1 preadipocytes, Pestic. Biochem. Physiol 150 (2018) 48–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [657].Kassotis CD, Hoffman K, Stapleton HM, Characterization of Adipogenic Activity of House Dust Extracts and Semi-Volatile Indoor Contaminants in 3T3-L1 Cells, Environ. Sci. Technol 51 (15) (2017) 8735–8745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [658].Stapleton HM, Klosterhaus S, Eagle S, Fuh J, Meeker JD, Blum A, Webster TF, Detection of organophosphate flame retardants in furniture foam and U.S. house dust, Environ. Sci. Technol 43 (19) (2009) 7490–7495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [659].Kassotis CD, Hoffman K, Völker J, Pu Y, Veiga-Lopez A, Kim SM, Schlezinger JJ, Bovolin P, Cottone E, Saraceni A, Scandiffio R, Atlas E, Leingartner K, Krager S, Tischkau SA, Ermler S, Legler J, Chappell VA, Fenton SE, Mesmar F, Bondesson M, Fernández MF, Stapleton HM, Reproducibility of Adipogenic Responses to Metabolism Disrupting Chemicals in the 3T3-L1 Pre-adipocyte Model System: An Interlaboratory Study, Toxicology 461 (2021), 152900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [660].Ying G-G, Williams B, Kookana R, Environmental fate of alkylphenols and alkylphenol ethoxylates—a review, Environ. Int 28 (3) (2002) 215–226. [DOI] [PubMed] [Google Scholar]
- [661].Kassotis CD, Kollitz EM, Ferguson PL, Stapleton HM, Nonionic Ethoxylated Surfactants Induce Adipogenesis in 3T3-L1 Cells, Toxicological sciences : an official journal of the Society of, Toxicology 162 (1) (2018) 124–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [662].Kassotis CD, LeFauve MK, Chiang YT, Knuth MM, Schkoda S, Kullman SW, Nonylphenol Polyethoxylates Enhance Adipose Deposition in Developmentally Exposed Zebrafish, Toxics 10 (2) (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [663].Sun Z, Cao H, Liu QS, Liang Y, Fiedler H, Zhang J, Zhou Q, Jiang G, 4-Hexylphenol influences adipogenic differentiation and hepatic lipid accumulation in vitro, Environ. Pollut 268 (2021), 115635. [DOI] [PubMed] [Google Scholar]
- [664].Cao XL, Dufresne G, Clement G, Bélisle S, Robichaud A, Beraldin F, Levels of bisphenol A diglycidyl ether (BADGE) and bisphenol F diglycidyl ether (BFDGE) in canned liquid infant formula products in Canada and dietary intake estimates, J. AOAC Int 92 (6) (2009) 1780–1789. [PubMed] [Google Scholar]
- [665].Chamorro-García R, Kirchner S, Li X, Janesick A, Casey SC, Chow C, Blumberg B, Bisphenol A Diglycidyl Ether Induces Adipogenic Differentiation of Multipotent Stromal Stem Cells through a Peroxisome Proliferator-Activated Receptor Gamma-Independent Mechanism, Environ. Health Perspect 120 (7) (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [666].Boucher JG, Boudreau A, Ahmed S, Atlas E, In Vitro Effects of Bisphenol A β-D-Glucuronide (BPA-G) on Adipogenesis in Human and Murine Preadipocytes, Environ. Health Perspect 123 (12) (2015) 1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [667].Ginsberg GL, Balk SJ, Consumer products as sources of chemical exposures to children: case study of triclosan, Curr. Opin. Pediatr 28 (2) (2016) 235–242. [DOI] [PubMed] [Google Scholar]
- [668].Liu J, Chen D, Huang Y, Bigambo FM, Chen T, Wang X, Effect of Maternal Triclosan Exposure on Neonatal Birth Weight and Children Triclosan Exposure on Children’s BMI: A Meta-Analysis, Front. Public Health 9 (2021), 648196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [669].Lankester J, Patel C, Cullen MR, Ley C, Parsonnet J, Urinary triclosan is associated with elevated body mass index in NHANES, PLoS ONE 8 (11) (2013), e80057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [670].Han M, Wang Y, Tang C, Fang H, Yang D, Wu J, Wang H, Chen Y, Jiang Q, Association of triclosan and triclocarban in urine with obesity risk in Chinese school children, Environ. Int 157 (2021), 106846. [DOI] [PubMed] [Google Scholar]
- [671].Li X, Pham HT, Janesick AS, Blumberg B, Triflumizole Is an Obesogen in Mice that Acts through Peroxisome Proliferator Activated Receptor Gamma (PPARγ), Environ. Health Perspect 120 (12) (2012) 1720–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [672].Lim S, Ahn SY, Song IC, Chung MH, Jang HC, Park KS, Lee K-U, Pak YK, Lee HK, Chronic Exposure to the Herbicide, Atrazine, Causes Mitochondrial Dysfunction and Insulin Resistance, PLoS ONE 4 (4) (2009), e5186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [673].Fildes A, Charlton J, Rudisill C, Littlejohns P, Prevost AT, Gulliford MC, Probability of an Obese Person Attaining Normal Body Weight: Cohort Study Using Electronic Health Records, Am. J. Public Health 105 (9) (2015) e54–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [674].Fothergill E, Guo J, Howard L, Kerns JC, Knuth ND, Brychta R, Chen KY, Skarulis MC, Walter M, Walter PJ, Hall KD, Persistent metabolic adaptation 6 years after “The Biggest Loser” competition, Obesity (Silver Spring), 2016, p. n/a-n/a.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [675].Brown RE, Sharma AM, Ardern CI, Mirdamadi P, Mirdamadi P, Kuk JL, Secular differences in the association between caloric intake, macronutrient intake, and physical activity with obesity, Obesity research & clinical practice 10 (3) (2015) 243–255. [DOI] [PubMed] [Google Scholar]
- [676].Teixeira PJ, CarraÇa EV, Marques MM, Rutter H, Oppert J-M, De Bourdeaudhuij I, Lakerveld J, Brug J, Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators, BMC Medicine 13 (2015) 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [677].Newbold RR, Perinatal Exposure to Endocrine Disrupting Chemicals with Estrogenic Activity and the Development of Obesity, in: Lustig RH (Ed.), Obesity Before Birth, Springer US; 2011, pp. 367–382. [Google Scholar]
- [678].Johnson SA, Painter MS, Javurek AB, Ellersieck MR, Wiedmeyer CE, Thyfault JP, Rosenfeld CS, Sex-dependent effects of developmental exposure to bisphenol A and ethinyl estradiol on metabolic parameters and voluntary physical activity, J Dev Orig Health Dis (2015) 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [679].Hales CM, Carroll MD, Fryar CD, Ogden CL, Prevalence of Obesity Among Adults and Youth: United States, 2015-2016, NCHS data brief (288) (2017) 1–8. [PubMed] [Google Scholar]
- [680].Jiang X, Ma H, Wang Y, Liu Y, Early life factors and type 2 diabetes mellitus, J. Diabetes Research 2013 (2013), 485082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [681].Myers MG, Leibel RL, Seeley RJ, Schwartz MW, Obesity and Leptin Resistance: Distinguishing Cause from Effect, Trends in endocrinology and metabolism: TEM 21 (11) (2010) 643–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [682].Sargis RM, Heindel JJ, Padmanabhan V, Interventions to Address Environmental Metabolism-Disrupting Chemicals: Changing the Narrative to Empower Action to Restore Metabolic Health, Front. Endocrinol 10 (33) (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [683].Shaikh S, Jagai JS, Ashley C, Zhou S, Sargis RM, Underutilized and Under Threat: Environmental Policy as a Tool to Address Diabetes Risk, Curr Diab Rep 18 (5) (2018) 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [684].Harley KG, Kogut K, Madrigal DS, Cardenas M, Vera IA, Meza-Alfaro G, She J, Gavin Q, Zahedi R, Bradman A, Eskenazi B, Parra KL, Reducing Phthalate, Paraben, and Phenol Exposure from Personal Care Products in Adolescent Girls: Findings from the HERMOSA Intervention Study, Environ. Health Perspect 124 (10) (2016) 1600–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [685].Rudel RA, Gray JM, Engel CL, Rawsthorne TW, Dodson RE, Ackerman JM, Rizzo J, Nudelman JL, Brody JG, Food packaging and bisphenol A and bis(2-ethyhexyl) phthalate exposure: findings from a dietary intervention, Environ. Health Perspect 119 (7) (2011) 914–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [686].Sathyanarayana S, Alcedo G, Saelens BE, Zhou C, Dills RL, Yu J, Lanphear B, Unexpected results in a randomized dietary trial to reduce phthalate and bisphenol A exposures, J. Eposure Sci. Environ. Epidemiol 23 (4) (2013) 378–384. [DOI] [PubMed] [Google Scholar]
- [687].Lai IK, Dhakal K, Gadupudi GS, Li M, Ludewig G, Robertson LW, Olivier AK, N-acetylcysteine (NAC) diminishes the severity of PCB 126-induced fatty liver in male rodents, Toxicology 302 (1) (2012) 25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [688].Rezaei M, Khodayar MJ, Seydi E, Soheila A, Parsi IK, Acute, but not Chronic, Exposure to Arsenic Provokes Glucose Intolerance in Rats: Possible Roles for Oxidative Stress and the Adrenergic Pathway, Can J, Diabetes 41 (3) (2017) 273–280. [DOI] [PubMed] [Google Scholar]
- [689].Hennig B, Ormsbee L, McClain CJ, Watkins BA, Blumberg B, Bachas LG, Sanderson W, Thompson C, Suk WA, Nutrition Can Modulate the Toxicity of Environmental Pollutants: Implications in Risk Assessment and Human Health, Environ. Health Perspect 120 (6) (2012) 771–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [690].Gupta P, Thompson BL, Wahlang B, Jordan CT, Zach HJ, Hennig B, Dziubla T, The environmental pollutant, polychlorinated biphenyls, and cardiovascular disease: a potential target for antioxidant nanotherapeutics, Drug Deliv, Transl. Res (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [691].Amjad S, Rahman MS, Pang MG, Role of Antioxidants in Alleviating Bisphenol A Toxicity, Biomolecules 10 (8) (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [692].Zwierello W, Maruszewska A, Skorka-Majewicz M, Goschorska M, Baranowska-Bosiacka I, Dec K, Styburski D, Nowakowska A, Gutowska I, The influence of polyphenols on metabolic disorders caused by compounds released from plastics - Review, Chemosphere 240 (2019), 124901. [DOI] [PubMed] [Google Scholar]
- [693].Guo W, Huen K, Park JS, Petreas M, Crispo SS, Block G, Holland N, Vitamin C intervention may lower the levels of persistent organic pollutants in blood of healthy women - A pilot study, Food Chem. Toxicol 92 (2016) 197–204. [DOI] [PubMed] [Google Scholar]
- [694].Mengozzi A, Carli F, Guiducci L, Parolini F, Biancalana E, Gastaldelli A, Solini A, SGLT2 inhibitors and thiazide enhance excretion of DEHP toxic metabolites in subjects with type 2 diabetes: A randomized clinical trial, Environ. Res 192 (2021), 110316. [DOI] [PubMed] [Google Scholar]
- [695].Rameshrad M, Razavi BM, Imenshahidi M, Hosseinzadeh H, Vitis vinifera (grape) seed extract and resveratrol alleviate bisphenol-A-induced metabolic syndrome: Biochemical and molecular evidences, Phytother. Res (2019). [DOI] [PubMed] [Google Scholar]
- [696].Fadishei M, Ghasemzadeh RM, Imenshahidi M, Mohajeri A, Razavi BM, Hosseinzadeh H, Effects of Nigella sativa oil and thymoquinone against bisphenol A-induced metabolic disorder in rats, Phytother. Res 35 (4) (2020) 2005–2024. [DOI] [PubMed] [Google Scholar]
- [697].Elgawish RA, El-Beltagy MA, El-Sayed RM, Gaber AA, Abdelrazek HMA, Protective role of lycopene against metabolic disorders induced by chronic bisphenol A exposure in rats, Environ. Sci. Pollut. Res, Int, 2020. [DOI] [PubMed] [Google Scholar]
- [698].Park J, Choi K, Lee J, Jung JM, Lee Y, The Effect of Korean Red Ginseng on Bisphenol A-Induced Fatty Acid Composition and Lipid Metabolism-Related Gene Expression Changes, Am. J. Chin. Med 48 (8) (2020) 1841–1848. [DOI] [PubMed] [Google Scholar]
- [699].Sakuma S, Sumida M, Endoh Y, Kurita A, Yamaguchi A, Watanabe T, Kohda T, Tsukiyama Y, Fujimoto Y, Curcumin inhibits adipogenesis induced by benzyl butyl phthalate in 3T3-L1 cells, Toxicol. Appl. Pharmacol 329 (2017) 158–164. [DOI] [PubMed] [Google Scholar]
- [700].Choi SI, Lee JS, Lee S, Sim WS, Kim YC, Lee OH, Potentilla rugulosa Nakai Extract Attenuates Bisphenol A-, S- and F-Induced ROS Production and Differentiation of 3T3-L1 Preadipocytes in the Absence of Dexamethasone, Antioxidants, (Basel) 9 (2(2)) (2020) 3041–3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [701].Zhu K, Zhao Y, Yang Y, Bai Y, Zhao T, Icariin Alleviates Bisphenol A Induced Disruption of Intestinal Epithelial Barrier by Maintaining Redox Homeostasis In Vivo and In Vitro, ACS Omega 5 (32) (2020) 20399–20408. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [702].Baralić K, Živančević K, Jorgovanović D, Javorac D, Radovanović J, Gojković T, Djordjevic AB, Ćurčić M, Mandinić Z, Bulat Z, Antonijević B, Đukić-Cosić D, Probiotic reduced the impact of phthalates and bisphenol A mixture on type 2 diabetes mellitus development: merging bioinformatics with in vivo analysis, Food and chemical toxicology : an international journal published for the British Industrial Biological Research Association 112325 (2021). [DOI] [PubMed] [Google Scholar]
- [703].Vahdati HF, Mehri S, Abnous K, Birner-Gruenberger R, Hosseinzadeh H, Protective effect of crocin on BPA-induced liver toxicity in rats through inhibition of oxidative stress and downregulation of MAPK and MAPKAP signaling pathway and miRNA-122 expression, Food Chem. Toxicol 107 (Pt A) (2017) 395–405. [DOI] [PubMed] [Google Scholar]
- [704].Akcay NC, Omeroglu S, Dizakar SOA, Kavutcu M, Turkoglu I, Esmekaya MA, Peker TV, The effects of melatonin on possible damage that will occur on adipocytokines and liver tissue by coadministration of fructose and bisphenol a (BPA), Environ. Sci. Pollut. Res. Int (2020). [DOI] [PubMed] [Google Scholar]
- [705].Poormoosavi SM, Najafzadehvarzi H, Behmanesh MA, Amirgholami R, Protective effects of Asparagus officinalis extract against Bisphenol A-induced toxicity in Wistar rats, Toxicol. Rep 5 (2018) 427–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [706].Geng S, Wang S, Zhu W, Xie C, Li X, Wu J, Zhu J, Jiang Y, Yang X, Li Y, Chen Y, Wang X, Meng Y, Zhu M, Wu R, Huang C, Zhong C, Curcumin attenuates BPA-induced insulin resistance in HepG2 cells through suppression of JNK/p38 pathways, Toxicol. Lett 272 (2017) 75–83. [DOI] [PubMed] [Google Scholar]
- [707].Huang WC, Liao KY, Hsieh SK, Pan PH, Kuan YH, Liao SL, Chen CJ, Chen WY, Magnesium lithospermate B supplementation improved prenatal Bisphenol A exposure-induced metabolic abnormalities in male offspring, Environ. Toxicol (2021). [DOI] [PubMed] [Google Scholar]
- [708].Jandacek RJ, Heubi JE, Buckley DD, Khoury JC, Turner WE, Sjodin A, Olson JR, Shelton C, Helms K, Bailey TD, Carter S, Tso P, Pavuk M, Reduction of the body burden of PCBs and DDE by dietary intervention in a randomized trial, J. Nutr. Biochem 25 (4) (2014) 483–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [709].Iida T, Nakagawa R, Hirakawa H, Matsueda T, Morita K, Hamamura K, Nakayama J, Hori Y, Guo YL, Chang FM, et al. , Clinical trial of a combination of rice bran fiber and cholestyramine for promotion of fecal excretion of retained polychlorinated dibenzofuran and polychlorinated biphenyl in Yu-Cheng patients, Fukuoka Igaku Zasshi 86 (5) (1995) 226–233. [PubMed] [Google Scholar]
- [710].Takasuga T, Senthilkumar K, Takemori H, Ohi E, Tsuji H, Nagayama J, Impact of FEBRA (fermented brown rice with Aspergillus oryzae) intake and concentrations of PCDDs, PCDFs and PCBs in blood of humans from Japan, Chemosphere 57 (10) (2004) 1409–1426. [DOI] [PubMed] [Google Scholar]
- [711].Geusau A, Schmaldienst S, Derfler K, Papke O, Abraham K, Severe 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) intoxication: kinetics and trials to enhance elimination in two patients, Arch. Toxicol 76 (5–6) (2002) 316–325. [DOI] [PubMed] [Google Scholar]
- [712].Anderson JW, Baird P, Davis RH Jr., Ferreri S, Knudtson M, Koraym A, Waters V, Williams CL, Health benefits of dietary fiber, Nutr. Rev 67 (4) (2009) 188–205. [DOI] [PubMed] [Google Scholar]
- [713].Shih MK, Tain YL, Chen YW, Hsu WH, Yeh YT, Chang SKC, Liao JX, Hou CY, Resveratrol Butyrate Esters Inhibit Obesity Caused by Perinatal Exposure to Bisphenol A in Female Offspring Rats, Molecules (Basel, Switzerland) 26 (13) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [714].Stahlhut RW, Myers JP, Taylor JA, Nadal A, Dyer JA, vom Saal FS, Experimental BPA Exposure and Glucose-Stimulated Insulin Response in Adult Men and Women, J. Endocr. Soc 2 (10) (2018) 1173–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [715].Hagobian TA, Bird A, Stanelle S, Williams D, Schaffner A, Phelan S, Pilot Study on the Effect of Orally Administered Bisphenol A on Glucose and Insulin Response in Nonobese Adults, J. Endocr. Soc 3 (3) (2019) 643–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [716].Bae S, Hong YC, Exposure to bisphenol A from drinking canned beverages increases blood pressure: randomized crossover trial, Hypertension 65 (2) (2015) 313–319. [DOI] [PubMed] [Google Scholar]
- [717].Kim JH, Cho YH, Hong YC, MicroRNA expression in response to bisphenol A is associated with high blood pressure, Environ. Int 141 (2020), 105791. [DOI] [PubMed] [Google Scholar]
- [718].Miller DB, Ghio AJ, Karoly ED, Bell LN, Snow SJ, Madden MC, Soukup J, Cascio WE, Gilmour MI, Kodavanti UP, Ozone Exposure Increases Circulating Stress Hormones and Lipid Metabolites in Humans, Am. J. Respir. Crit. Care Med (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [719].Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, Chen J, Hao K, Kinney PL, Chen H, Kan H, Particulate Matter Exposure and Stress Hormone Levels: A Randomized, Double-Blind, Crossover Trial of Air Purification, Circulation 136 (7) (2017) 618–627. [DOI] [PubMed] [Google Scholar]
- [720].Makris KC, Konstantinou C, Andrianou XD, Charisiadis P, Kyriacou A, Gribble MO, Christophi CA, A cluster-randomized crossover trial of organic diet impact on biomarkers of exposure to pesticides and biomarkers of oxidative stress/inflammation in primary school children, PLoS ONE 14 (9) (2019), e0219420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [721].Luderer U, Eskenazi B, Hauser R, Korach KS, McHale CM, Moran F, Rieswijk L, Solomon G, Udagawa O, Zhang L, Zlatnik M, Zeise L, Smith MT, Proposed Key Characteristics of Female Reproductive Toxicants as an Approach for Organizing and Evaluating Mechanistic Data in Hazard Assessment, Environ. Health Perspect 127 (7) (2019) 75001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [722].Arzuaga X, Smith MT, Gibbons CF, Skakkebæk NE, Yost EE, Beverly BEJ, Hotchkiss AK, Hauser R, Pagani RL, Schrader SM, Zeise L, Prins GS, Proposed Key Characteristics of Male Reproductive Toxicants as an Approach for Organizing and Evaluating Mechanistic Evidence in Human Health Hazard Assessments, Environ. Health Perspect 127 (6) (2019) 65001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [723].Braun JM, Gray K, Challenges to studying the health effects of early life environmental chemical exposures on children’s health, PLoS Biol. 15 (12) (2017), e2002800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [724].Lind L, Salihovic S, Lampa E, Lind PM, Mixture effects of 30 environmental contaminants on incident metabolic syndrome-A prospective study, Environ. Int 107 (2017) 8–15. [DOI] [PubMed] [Google Scholar]
- [725].Taylor KW, Joubert BR, Braun JM, Dilworth C, Gennings C, Hauser R, Heindel JJ, Rider CV, Webster TF, Carlin DJ, Statistical Approaches for Assessing Health Effects of Environmental Chemical Mixtures in Epidemiology: Lessons from an Innovative Workshop, Environ. Health Perspect 124 (12) (2016) A227–A229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [726].Braun JM, Gennings C, Hauser R, Webster TF, What Can Epidemiological Studies Tell Us about the Impact of Chemical Mixtures on Human Health? Environ. Health Perspect 124 (1) (2016) A6–A9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [727].Lazarevic N, Barnett AG, Sly PD, Knibbs LD, Statistical Methodology in Studies of Prenatal Exposure to Mixtures of Endocrine-Disrupting Chemicals: A Review of Existing Approaches and New Alternatives, Environ. Health Perspect 127 (2) (2019) 26001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [728].Santos S, Maitre L, Warembourg C, Agier L, Richiardi L, Basagaña X, Vrijheid M, Applying the exposome concept in birth cohort research: a review of statistical approaches, Eur. J. Epidemiol 35 (3) (2020) 193–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [729].Esteban López M, Göen T, Mol H, Nübler S, Haji-Abbas-Zarrabi K, Koch HM, Kasper-Sonnenberg M, Dvorakova D, Hajslova J, Antignac JP, Vaccher V, Elbers I, Thomsen C, Vorkamp K, Pedraza-Díaz S, Kolossa-Gehring M, Castaño A, The European human biomonitoring platform - Design and implementation of a laboratory quality assurance/quality control (QA/QC) programme for selected priority chemicals, Int. J. Hyg. Environ. Health 234 (2021), 113740. [DOI] [PubMed] [Google Scholar]
- [730].Bonde JP, Flachs EM, Rimborg S, Glazer CH, Giwercman A, Ramlau-Hansen CH, Hougaard KS, Høyer BB, Hærvig KK, Petersen SB, Rylander L, Specht IO, Toft G, Bräuner EV, The epidemiologic evidence linking prenatal and postnatal exposure to endocrine disrupting chemicals with male reproductive disorders: a systematic review and meta-analysis, Human reproduction update 23 (1) (2016) 104–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [731].Williams RJ, Tse T, Harlan WR, Zarin DA, Registration of observational studies: is it time? CMAJ 182 (15) (2010) 1638–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [732].Kanj A, Levine D, Overcoming obesity: Weight-loss drugs are underused, Cleve Clin J Med 87 (10) (2020) 602–604. [DOI] [PubMed] [Google Scholar]
- [733].Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, Thornton PL, Haire-Joshu D, Social Determinants of Health and Diabetes: A Scientific Review, Diabetes Care 44 (1) (2020) 258–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [734].Alberga AS, Edache IY, Forhan M, Russell-Mayhew S, Weight bias and health care utilization: a scoping review, Prim Health Care Res Dev 20 (2019), e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [735].Calafat AM, Weuve J, Ye X, Jia LT, Hu H, Ringer S, Huttner K, Hauser R, Exposure to bisphenol A and other phenols in neonatal intensive care unit premature infants, Environ. Health Perspect 117 (4) (2009) 639–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [736].Rubin BS, Paranjpe M, DaFonte T, Schaeberle C, Soto AM, Obin M, Greenberg AS, Perinatal BPA exposure alters body weight and composition in a dose specific and sex specific manner: the addition of peripubertal exposure exacerbates adverse effects in female mice, Reprod. Toxicol (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [737].Lai KP, Chung YT, Li R, Wan HT, Wong CK, Bisphenol A alters gut microbiome: Comparative metagenomics analysis, Environmental pollution (Barking, Essex 218 (2016) (1987) 923–930. [DOI] [PubMed] [Google Scholar]
- [738].Zhang Y, Dong T, Hu W, Wang X, Xu B, Lin Z, Hofer T, Stefanoff P, Chen Y, Wang X, Xia Y, Association between exposure to a mixture of phenols, pesticides, and phthalates and obesity: Comparison of three statistical models, Environ. Int 123 (2019) 325–336. [DOI] [PubMed] [Google Scholar]
- [739].Philips EM, Santos S, Steegers EAP, Asimakopoulos AG, Kannan K, Trasande L, Jaddoe VWV, Maternal bisphenol and phthalate urine concentrations and weight gain during pregnancy, Environ. Int 135 (2020), 105342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [740].Güil-Oumrait N, Valvi D, Garcia-Esteban R, Guxens M, Sunyer J, Torrent M, Casas M, Vrijheid M, Prenatal exposure to persistent organic pollutants and markers of obesity and cardiometabolic risk in Spanish adolescents, Environ. Int 151 (2021), 106469. [DOI] [PMC free article] [PubMed] [Google Scholar]