Abstract
Objectives
This study examined children’s perspectives about returning to in-person school following lockdown due to the pandemic and about mask-wearing in class, as well as the mental health of children and parents during the pandemic.
Methods
This cross-sectional study was part of a 2-day school simulation exercise that randomized students to different masking recommendations. Parent-report of mental health and post-simulation child-report of COVID-19-related anxiety and mask-wearing were analyzed using descriptive and multiple regression analyses. Semi-structured focus groups were conducted with older students to supplement questionnaire data.
Results
Of 190 students in this study, 31% were in grade 4 or lower 95% looked forward to returning to in-person school. Greater child anxiety about COVID-19 was predicted by increased parent/caregiver anxiety (β=0.67; P<0.001), and lower parental educational attainment (β=1.86; P<0.002). Older students were more likely than younger students to report that mask-wearing interfered with their abilities to interact with peers (χ2(1)=31.16; P<0.001) and understand the teacher (χ2(1)=13.97; P<0.001). Students in the group that did not require masks were more likely than students in the masking group to report worries about contracting COVID-19 at school (χ2(1)=10.07; P<0.05), and anticipated difficulty wearing a mask (χ2(1)=18.95; P<0.001).
Conclusions
For children anxious about COVID-19, parental anxiety and education about COVID-19 may be targets for intervention. Future research should examine the impact of prolonged implementation of public health mitigation strategies in school on academic achievement and children’s mental health.
Keywords: Children, COVID-19, Masks, Mental health, School reopening
The coronavirus disease 2019 (COVID-19) pandemic has evoked unprecedented changes, eliciting mental health concerns for school-aged youth (1–3). Disease-containment measures during previous pandemics, such as quarantine, were associated with increased likelihood of post-traumatic stress disorder among parents and children (4). Early research from the pandemic has demonstrated worsened mental health among children, presumably as a result of diminished social and physical contact with others (5–8). Concerns regarding harms from school closures also include disruption to daily routines, including regular physical activity, sleeping schedules, and eating schedules, as well as from the suspension of school-based nutrition and mental health services, with children from low-income households and racial/ethnic minority groups reportedly disproportionately affected (1,9–11).
To mitigate viral spread within schools, several health and safety measures, including the use of non-medical masks, have been recommended in schools. Canadian guidelines included the use of medical or cloth masks in schools for students in grade 1 and above, as well as teachers’ masks (12,13). Minimal research has explored the psychological, social, and communication consequences of mask-wearing in schools (14). Extant research has suggested, however, that although masks may be effective in reducing viral spread among children, they may also impair face recognition, verbal and non-verbal communication, and emotion signalling between teacher and student (14). Our study sought to examine the experiences and perspectives of school-aged children about returning to school in September 2020 during the COVID-19 pandemic and about wearing masks in the classroom. Given indications of worsened anxiety and depression among children and adolescents following the onset of the pandemic (15), we also explored variables predicting worsening mental health symptoms.
METHODS
Procedure
This cross-sectional study was part of a 2-day school simulation during August of 2020 in Toronto, Canada, evaluating the implementation of health and safety measures in schools. At this time, no vaccines were authorized for use, and daily case counts in Toronto ranged from approximately 10 to 20 per day. The study was registered with full protocol on ClinicialTrials.net (#NCT04531254) and approved by the Hospital for Sick Children Research Ethics Board.
At the start of day 1, participants (parents or children) completed a pre-simulation questionnaire about underlying health conditions (e.g., diabetes, asthma, inflammation), medications, allergies, and safety requirements, as well as parent and child concerns regarding COVID-19, public health measures for school reopening, and child mental health symptoms during the pandemic. Children were then randomized using computer-generated allocation assignment, stratified by age and sex, to either a Mask condition, where students always wore masks (except when eating/drinking) or No-Mask condition, where students did not wear masks (grade 4 and lower) or only wore masks when unable to maintain physical distance (>2 m) (grade 5 and above). There were two classrooms (i.e., a Mask classroom and a No-Mask classroom) for each grade level (JK/SK, grades 1/2, 3/4, 5/6, 7/8, 9/10, 11/12), resulting in 14 classes in total. In all classes, teachers always wore masks and were provided optional face shields. Students and teachers completed the school simulation in their respective classrooms over 2 full days. These simulated school days were structured like typical school days, in which teachers instructed on standardized curriculum, children completed independent and group activities, and on-site breaks were taken for recess and lunch. At the end of day 2, students completed a self-report post-simulation questionnaire (all students) and semi-structured focus groups (grade 5 and above) about their experiences.
Participants
Participants were children (aged 3 to 17 years) who had attended a structured learning environment (kindergarten to grade 12) during the academic year 2019 to 2020. Children were excluded if they had tested positive for COVID-19 or travelled outside of Canada within 14 days of the simulation, had symptoms of COVID-19 on simulation days, or required classroom resources beyond what one teacher could provide. Snowball and convenience sampling methods were implemented, with school principals in the Greater Toronto Area approaching participants through email and community notices. The general public was recruited through media and news releases. Interested students and families were directed to a website and webinar containing study information. Following webinars, families indicated their willingness to participate in the study via an online form and were subsequently contacted by a research team member for eligibility screening and consent.
Measures
Anxiety about COVID-19 and child mental health during the pandemic were assessed using items from the international CRISIS questionnaire (16) (see Supplementary Tables S1 and S2), which measures impact of the pandemic so that it can be compared across cultures and previous research of the impact of the pandemic on children’s mental health (8,17).
Anxiety about COVID-19.
Parental anxiety about COVID-19 was determined using a three-item scale enquiring about parental concerns regarding infection (Cronbach α=0.72; Supplementary Table S1), scored on five-point Likert scales. Child anxiety about COVID-19 was determined using a parallel three-item scale inquiring about concerns regarding infection (Cronbach α=0.79; Supplementary Table S1).
Child mental health during COVID-19.
Parents reported on their child’s mental health and changes in mental health during the pandemic on five-point Likert scales across five domains: mood, anxiety, irritability, difficulty concentrating, and fidgeting (Supplementary Tables S2a and S2b).
Attitudes toward school reopening and public health measures.
At the end of day 2, students completed a four-item (grade 4 and lower) or eight-item (grade 5 and above) questionnaire about their attitudes regarding returning to school and public health measures (Supplementary Table S3), using five-point ‘Faces’ (grade 4 and below) or standard (grade 5 and above) Likert scales. Questionnaires were pilot tested by non-participant public school students and teachers for readability, clarity, comprehension, and completeness prior to administration.
Student focus groups.
Semi-structured, 45-minute focus groups were conducted and audio-recorded with each class of students in grade 5 and above to obtain feedback on their experiences during the simulation experiment and with public health protocols. This occurred at the end of the second day of school and was facilitated by research staff trained in qualitative methods. A script was prepared based on the research team’s clinical and qualitative expertise, consisting of open-ended questions to promote rich, descriptive, and synergistic responses (18).
Data analysis
Group differences were determined using Mann–Whitney U test for dimensional measures, and Pearson’s chi-square or Fisher’s exact tests for categorical measures. Multiple linear and logistic regression analyses were conducted to examine associations between baseline and post-simulation responses for continuous (e.g., anxiety about COVID-19) and dichotomous (e.g., attitudes toward school reopening, mental health change) variables, respectively. We included annual household income (greater than $50,000), race/ethnicity (White and non-White), school system (private or public), and highest parental educational level (elementary/high school, or university/college graduate or higher) in models as covariates based on previous knowledge and univariable pre-screening (5). We regrouped responses to mental health change items for each of the five domains for analysis. We combined responses of ‘a lot worse’ and ‘a little worse’ into ‘worse’ and ‘a little better’ and ‘a lot better’ into ‘improved’. As child anxiety was measured using an ordinal Likert rating scale, linear and logistic regression results were examined and found to be comparable. Only cases with complete data on variables of interest were included. Data were analyzed using SPSS (version 20) (19).
Audio-recordings of focus groups were transcribed verbatim and de-identified for thematic analysis using a qualitative descriptive approach. Transcripts were read and analyzed by multiple team members. Deductive thematic analysis was utilized, and codes were developed through a line-by-line review of all transcripts using NVivo (20). Codes emerging repeatedly in the transcript were noted and comparatively analyzed by multiple team members for consistency. Themes were discussed with six educators to support data interpretation and rigour.
RESULTS
The study initially included 190 students (aged 3.1 to 17.1 years), of whom 59 (31%) were in grade 4 and below. In the previous academic year, 58 (31%) students were in high school. Most children identified as White (49%) and attended public school (58%). Demographic characteristics of students assigned to Mask and No-Mask groups are summarized in Table 1.
Table 1.
Demographic characteristics of participants randomly assigned to the ‘mask’ and ‘no-mask’ groups
| Mask | No-Mask | |||
|---|---|---|---|---|
| N | % | n | % | |
| Gender | ||||
| Male | 47 | 47 | 41 | 51 |
| Female | 52 | 53 | 40 | 49 |
| Trans or non-binary gender | 0 | 0 | 0 | 0 |
| School system | ||||
| Public | 59 | 60 | 53 | 63 |
| Private | 40 | 40 | 31 | 37 |
| Educational setting | ||||
| ‘Regular’ English | 74 | 75 | 64 | 76 |
| ‘Regular’ French | 12 | 12 | 12 | 14 |
| Regular with support | 6 | 6 | 2 | 2 |
| Full-time or part-time special education | 4 | 4 | 2 | 2 |
| Full-time gifted | 2 | 2 | 3 | 4 |
| Attended homeschool or full-time online school | 0 | 0 | 0 | 0 |
| Attended a residential placement and did not live at home | 0 | 0 | 0 | 0 |
| None of these | 1 | 1 | 1 | 1 |
| Race/ethnicity | ||||
| Asian | 17 | 18 | 11 | 13 |
| Black | 9 | 9 | 6 | 7 |
| Indian-Caribbean | 1 | 1 | 3 | 3 |
| Indigenous/Aboriginal | 0 | 0 | 0 | 0 |
| Latin/Central/South American | 1 | 1 | 2 | 2 |
| Middle Eastern | 3 | 3 | 0 | 0 |
| White | 53 | 55 | 42 | 52 |
| Mixed heritage | 12 | 12 | 12 | 15 |
| Other(s) | 0 | 0 | 6 | 7 |
| Do not know | 0 | 0 | 0 | 0 |
| Prefer not to answer | 1 | 1 | 1 | 1 |
| Income | ||||
| Equal or less than $49,000 | 9 | 9 | 4 | 9 |
| $50,000–99,999 | 5 | 8 | 9 | 11 |
| $100,000–199,999 | 18 | 19 | 21 | 26 |
| Equal to or more than $200,000 | 52 | 54 | 37 | 46 |
| Choose not to answer | 13 | 13 | 10 | 11 |
School system and educational setting were both reported for the previous academic year
Five participants withdrew after randomization. In pre-simulation questionnaires, these participants did not differ significantly from those who remained in the study on any pre-simulation variables of interest. An additional five participants were excluded due to missing data for all variables of interest, resulting in a final sample of 180 students to be included in the analyses.
Children’s anxiety about COVID-19
Greater child anxiety about COVID-19 was associated with increased parent/caregiver anxiety about COVID-19 (B=0.67; P<0.001) and lower level of parent education (B=–1.81; P=0.002) (Table 2). Child anxiety about contracting COVID-19 at school was positively associated with parent/caregiver anxiety about COVID-19, irrespective of mask use (B=0.063; P=0.020). Greater parental anxiety about COVID-19 was associated with the presence of food insecurity (B=0.020; P=0.035).
Table 2.
Child anxiety about COVID-19
| Child anxiety about COVID-19 | ||||||
|---|---|---|---|---|---|---|
| B | SE | t | P | 95% CI | ||
| Lower | Upper | |||||
| Intercept | 1.59 | 0.88 | 1.81 | 0.07 | –0.13 | 3.33 |
| Parent anxiety about COVID-19 | 0.67 | 0.73 | 9.12 | <0.001 | 0.052 | .081 |
| Food insecurity | 0.38 | 0.72 | 2.03 | 0.07 | –1.04 | 1.80 |
| Family income∗ | 0.84 | 0.64 | 1.30 | 0.19 | –0.43 | 2.08 |
| Race/ethnicity† | 0.21 | 0.31 | 0.68 | 0.50 | –0.41 | 0.83 |
| School system‡ | –0.25 | 0.31 | –0.79 | 0.433 | –0.87 | 0.37 |
| Parental education§ | –1.81 | 0.64 | 3.01 | 0.002 | 0.65 | 3.10 |
Family income less than $50,000;
White European and White North American vs. not white;
Private vs. public school system;
University/college education vs High school or lower
Attitudes toward school reopening and public health measures
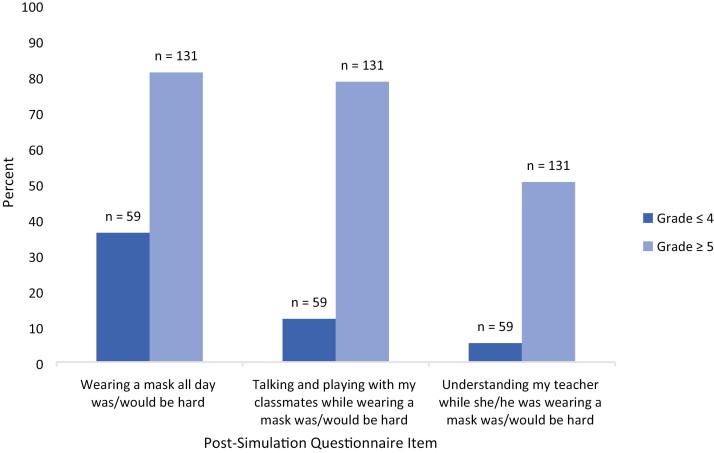
Nearly all (95%) children reported looking forward to school, irrespective of grade (P=0.21) or mask use (P=0.32), supported by participant responses: ‘I kind of stepped into the classroom, saw how far away the desks were, it felt pretty safe. […] I’m excited to go back to school’. Children’s appraisal of mask use in post-simulation questionnaires varied by both grade and experience (Figures 1 and 2). Children in grade 5 and above were more likely than children in grade 4 and below to report that it was/would be hard to: wear a mask at school, (χ2(1)=11.98; P=0.001), talk or play with classmates while wearing a mask, (χ2(1)=31.16; P<0.001), and understand the teacher while wearing a mask, (χ2(1)=13.97; P<0.001).
Figure 1.
Post-simulation questionnaire responses by grade group.
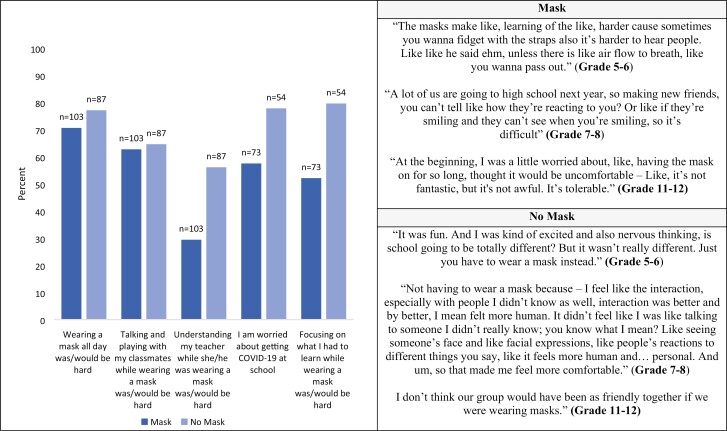
Figure 2.
Post-simulation questionnaire responses by ‘mask’ or ‘no-mask’ groups.
Post-simulation, No-Mask-group children were more likely than Mask-group children to report being worried about contracting COVID-19 at school (χ2(1)=10.07; P=0.007), and to report that it was/would be hard to: wear a mask at school, (χ2(1)=18.95; P<0.001), talk or play with classmates while wearing a mask, (χ2(1)=6.33; P=0.042), focus on learning while wearing a mask, (χ2(1)=11.76; P=0.003), and understand the teacher while he/she is wearing a mask (χ2(1)=18.95; P<0.001). In post-simulation focus groups, the No-Mask group again noted anticipated difficulties of mask-wearing during school. Some participants in the Mask group also reported similar concerns: ‘…[when] making new friends, you can’t tell like how they’re reacting to you? […] It’s difficult’; ‘The masks make like, learning of the like, harder […] You wanna fidget with the straps, also it’s harder to hear people’.
There were no associations between parent or child anxiety about COVID-19 and attitudes about mask-wearing or returning to school (all P values >0.73).
Impact of COVID-19 pandemic on child mental health
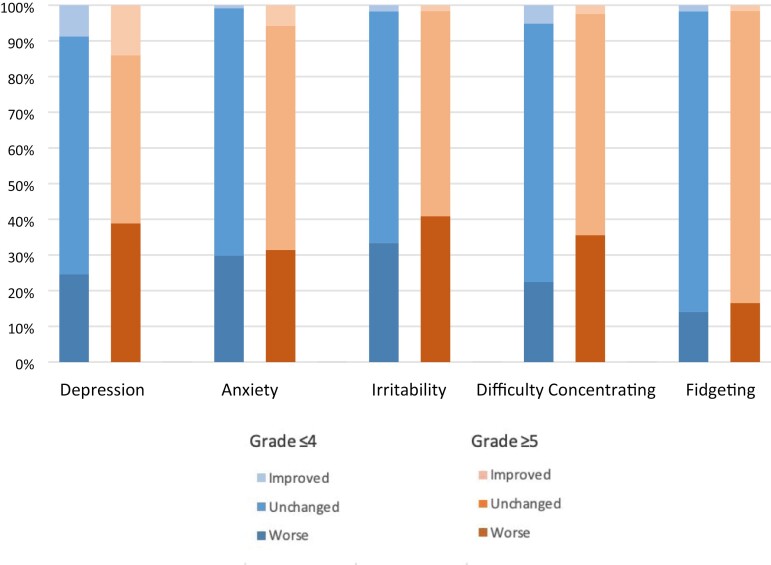
A total of 114/180 (63%) participants in the study reported worsened mental health in at least one domain during the pandemic (Supplementary Table S2b). Of the 114 participants who reported worsened mental health, 30 (26%), 27 (24%), and 57 (50%) reported deterioration in one, two, or three domains, respectively. Figure 3 shows the impact of the COVID-19 pandemic on child mental health, by domain.
Figure 3.
Mental health change during the COVID-19 pandemic by grade group.
Change in family financial circumstance during COVID-19, indicated by receiving government subsidies during COVID-19, was related to worsened child anxiety, (χ2(1)=4.79; P=0.029), mood (χ2(1)=11.55; P=0.001) and hyperactivity (χ2(1)=15.36; P<0.001). In addition, children with a pre-existing underlying medical condition were more likely to experience increased anxiety during the pandemic (χ2(1)=4.11; P=0.04).
Of mental health domains, child anxiety about COVID-19 was only associated with greater difficulty concentrating (B=0.04; P=0.008). Parent anxiety about COVID-19 was not associated with deterioration in any child mental health domain (all P values >0.13). Worsened mental health during the pandemic (deterioration in at least one domain) was not associated with post-simulation attitudes toward school reopening and public health measures (all P values >0.28).
DISCUSSION
This study found that parental anxiety and lower parental education were associated with child anxiety about COVID-19. Despite anticipated or experienced difficulties of wearing masks in class, nearly all children in this study looked forward to returning to school. Older and No-Mask-group children were more likely than younger and Mask-group children to report expected or experienced difficulties with mask-wearing. The majority of children reported worsened mental health during the pandemic in at least one of five domains, associated with factors such as pre-existing medical concerns.
Greater anxiety about COVID-19 was associated with lower parental educational attainment and food insecurity, both of which are potential indicators of socioeconomic disadvantage, and also associated with greater parental anxiety. Pre-COVID-19 studies have suggested that socioeconomic disadvantage is disruptive to families by increasing parental psychological distress and anxiety about the future, leading to negative child psychological outcomes (21,22). Given our findings, future work may consider the specific role of parental education in child anxiety associated with socioeconomic disadvantage. In addition, a recent study identified that anxiety about financial hardships during COVID-19 was higher among adults with children at home than among those without (23), suggesting that baseline anxiety levels among lower-income parents may be elevated during COVID-19 compared with higher-income parents, and that these effects may generalize to include anxiety about COVID-19. Our findings are also consistent with pre-COVID research demonstrating the importance of parental anxiety in precipitating or perpetuating anxiety among children (24). The addition of parental anxiety management to cognitive behavioural therapy (CBT) for children is more efficacious than CBT alone for children with anxiety disorders, particularly when increased parental anxiety is present (25). This suggests that parental anxiety may be a key target for child anxiety interventions during the pandemic and that COVID-19-specific education and support, particularly for families struggling financially, may be important to the well-being of children.
Children in grade 5 and above were more likely than children in grade 4 and lower to report expected or experienced social, communication, and learning difficulties while wearing masks. To our knowledge, this is the first study to report children’s thoughts and feelings about mask-wearing in the classroom. Our findings are consistent with studies reporting that children experience social and communication difficulties when interacting with mask-wearing adult physicians (26–28). In post-simulation questionnaires, children in the Mask group were less likely than children in the No-Mask group to report worries about contracting COVID-19 at school, and to expect social and learning difficulties while wearing a mask at school, indicating that the reality of mask-wearing may be less problematic than children anticipate. Despite these group differences, however, focus group responses suggest that children in the Mask group also had significant concerns about wearing masks in class, and found that masks served as a barrier to communication, learning, and social connectivity (29). These findings highlight the importance of communication strategies that do not rely on facial expression in the classroom, including clear body language, dynamic storytelling, attention to humour and tone of voice, and of the value of teaching children to actively listen and articulating their thoughts and feelings clearly to be understood.
The majority of participants reported worsened mental health during the COVID-19 pandemic in one or more domains, consistent with extant literature suggesting increased depressive and anxiety symptoms among children in general, and exacerbation of mental health symptoms among children with physical health concerns, during COVID-19 (15,30–32). In this study, worsened mental health during the pandemic was not associated with post-simulation attitudes toward school reopening and masking, although these attitudes would be interesting to revisit following a longer period of classroom mask implementation.
Limitations
As the school simulation study lasted for 2 days, the mask-wearing period was brief relative to the reality of children returning to school in Fall 2020, and thereby limits extrapolation to the non-simulation experience. Socioeconomically disadvantaged families were under-represented in the study sample, potentially limiting generalizability of findings. These limitations likely serve to underestimate the effect sizes related to indicators of economic disadvantage observed in the current study. Finally, the cross-sectional study design limits inferences regarding directionality of the associations observed.
CONCLUSIONS
This study identifies parental anxiety as a potential target for intervention among children who are anxious about COVID-19, particularly in the presence of socioeconomic disadvantage. Moreover, our findings underscore the importance of incorporating teaching and communication strategies that do not rely on facial expression in the classroom and while at school, and of exploring other public health mitigation strategies that do not obscure facial expression, such as transparent face shields or maintaining social distancing during instruction. Paediatricians and child health care providers may play a key role in educating anxious parents about the impact of their anxiety on their child’s mental health (MH), educating families about COVID-19, and connecting anxious parents with MH resources. Future research, including longitudinal evaluation, should examine the impacts of prolonged implementation of these strategies in schools on academic achievement and children’s mental health outcomes.
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to thank the following Hospital for Sick Children research assistants for their contribution to this work: Marlena Colasanto, Victoria A. Gudzak, Maria Isabel T. Suarez, and R. J. Williams. The authors would also like to thank Melissa Jones for her input as a representative of the Research Family Advisory Committee at The Hospital for Sick Children. The authors thank Nicole Lee for providing critical review and feedback on the manuscript.
MANUSCRIPT FUNDING
This work was supported by the SickKids Foundation, Ministry of Health/Ontario Together COVID-19 Rapid Research Fund, and Miner’s Lamp Innovation Fund in Prevention and Early Detection of Severe Mental Illness at the University of Toronto.
POTENTIAL CONFLICTS OF INTEREST
DJK reports grants from CIHR, the Garry Hurvitz Centre for Brain & Mental Health, and Brain and Behaviour Research Foundation, outside the context of this study. DJK is also a guest editor for this supplemental issue. Another editor oversaw peer review of this manuscript. RI reports samples from Canada Strong Masks.
There are no other disclosures. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
SUPPLEMENT FUNDING
This article is part of a special supplement on the impact of the COVID-19 pandemic on children and youth. Production of this supplement was made possible through a financial contribution from the Public Health Agency of Canada. The views expressed herein do not necessarily represent the views of the Public Health Agency of Canada.
REFERENCES
- 1. Golberstein E, Wen H, Miller BF.. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr 2020;174(9):819–20. [DOI] [PubMed] [Google Scholar]
- 2. Hoffman JA, Miller EA.. Addressing the consequences of school closure due to COVID-19 on children’s physical and mental well-being. World Med Heal Policy 2020;12(3):300–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Masonbrink AR, Hurley E.. Advocating for children during the COVID-19 school closures. Pediatrics 2020;146(3):e20201440. [DOI] [PubMed] [Google Scholar]
- 4. Sprang G, Silman M.. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep 2013;7(1):105–10. [DOI] [PubMed] [Google Scholar]
- 5. Duan L, Shao X, Wang Y, et al. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J Affect Disord 2020;275:112–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, Simoes-e-Silva AC.. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct 2020;51:101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry 2020;59(11):1218–39.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cost K, Crosbie J, Anagnostou E, et al. Mostly worse, occasionally better: Impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry 2021; 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brazendale K, Beets MW, Weaver RG, et al. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int J Behav Nutr Phys Act 2017;14(1):100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ali MM, West K, Teich JL, Lynch S, Mutter R, Dubenitz J.. Utilization of mental health services in educational setting by adolescents in the United States. J Sch Health 2019;89(5):393–401. [DOI] [PubMed] [Google Scholar]
- 11. Phelps C, Sperry LL.. Children and the COVID-19 pandemic. Psychol Trauma 2020;12(S1):73–5. [DOI] [PubMed] [Google Scholar]
- 12. Government of Canada. COVID-19 Guidance for Schools Kindergarten to Grade 12. 2020. https://www.toronto.ca/wp-content/uploads/2020/09/97d0-COVID-19-Guidance-for-Re-opening-Schools-JK-12.pdf. [Google Scholar]
- 13. Toronto District School Board. Mask and Face Covering Requirements for TDSB Students and Staff – Updated. 2020. https://www.tdsb.on.ca/Portals/0/docs/TDSBMaskGuidelinesUpdatedSeptember24.pdf. [Google Scholar]
- 14. Spitzer M. Masked education? The benefits and burdens of wearing face masks in schools during the current Corona pandemic. Trends Neurosci Educ 2020;20:100138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Racine N, Cooke JE, Eirich R, Korczak DJ, McArthur BA, Madigan S.. Child and adolescent mental illness during COVID-19: A rapid review. Psychiatry Res 2020;292:113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nikolaidis A, Paksarian D, Alexander L, et al. The coronavirus health and impact survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. medRxiv, doi: 10.1038/s41598-021-87270-3, August 27, 2020, preprint: not peer reviewed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Merikangas K, Stringaris A, Milham M, Kline NS.. The CoRonavIruS Health Impact Survey (CRISIS). 2021. https://github.com/nimh-comppsych/CRISIS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kitzinger J. Qualitative research: Introducing focus groups. BMJ 1995;311(7000):299. https://www.bmj.com/content/311/7000/299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.IBM Corp. IBM SPSS Statistics for Windows Version 20.0. Armonk, NY: IBM Corp, 2011. [Google Scholar]
- 20. Richards L. Using NVivo in Qualitative Research. Thousand Oaks, CA: Sage Publications, 1999. [Google Scholar]
- 21. Neppl TK, Senia JM, Donnellan MB.. Effects of economic hardship: Testing the family stress model over time. J Fam Psychol 2016;30(1):12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barnett MA. Economic disadvantage in complex family systems: Expansion of family stress models. Clin Child Fam Psychol Rev 2008;11(3):145–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mann FD, Krueger RF, Vohs KD.. Personal economic anxiety in response to COVID-19. Pers Individ Dif 2020;167:110233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Burstein M, Ginsburg GS, Tein JY.. Parental anxiety and child symptomatology: An examination of additive and interactive effects of parent psychopathology [corrected]. J Abnorm Child Psychol 2010;38(7):897–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cobham VE, Dadds MR, Spence SH.. The role of parental anxiety in the treatment of childhood anxiety. J Consult Clin Psychol 1998;66(6):893–905. [DOI] [PubMed] [Google Scholar]
- 26. Truong J, Jain S, Tan J, Keegan D, Matsui D, Rieder MJ.. Young children’s perceptions of physicians wearing standard precautions versus customary attire. Pediatr Emerg Care 2006;22(1):13–7. [DOI] [PubMed] [Google Scholar]
- 27. Crowe AML. Communication skills with children in paediatric anaesthesia: Challenges while wearing a face mask. BMJ Paediatr Open 2020;4(1):e000846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shack AR, Arkush L, Reingold S, Weiser G.. Masked paediatricians during the COVID-19 pandemic and communication with children. J Paediatr Child Health 2020;56(9):1475–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lin J, Pol S, Korczak DJ, et al. The impact of COVID-19 public health measures on in-person teachers instructing in-person: A mixed-methods study. J Can Acad Child Adolesc Psychiatry 2021. [PMC free article] [PubMed] [Google Scholar]
- 30. Hawke LD, Monga S, Korczak D, et al. Impacts of the COVID-19 pandemic on youth mental health among youth with physical health challenges. Early Interv Psychiatry 2021;15(5):1146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health 2020;16(57):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics 2020;146(4):e2020016824. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.