Abstract
Background
Ultrasound-guided percutaneous renal biopsy (PCRB) is a commonly used technique to obtain renal tissue for histopathological diagnosis in children and adolescents. The objectives of this study include determining the indications for renal biopsy, documenting the safety and efficacy of ultrasound-guided PCRB, and documenting its complications along with histopathological findings in children.
Methodology
The Ethical Review Committee approved this cross-sectional study. Data of all children with either nephrotic or nephritic syndrome from January 2017 to September 2020 (at The Kidney Center Post Graduate Training Institute Karachi) who underwent ultrasound-guided PCRB were collected and analyzed. An ultrasonic examination was performed both before and after the biopsy.
Results
During the research period, 104 individuals underwent PCRB. The average age of the children biopsied was 7.44 ± 4.12 years (range = 1-17 years). The most prevalent reason for biopsy was nephrotic syndrome. Almost 94% of PCRBs were effective. Post-biopsy complications were detected in 16 cases, with peri-nephric hematoma being the most prevalent.
Conclusions
In children, ultrasound-guided PCRB can safely be performed under sedation in experienced hands with an automated biopsy gun needle. The use of real-time ultrasound guidance as well as the automated biopsy gun ensures good outcomes.
Keywords: hematuria, nephrotic syndrome, children, percutaneous, ultrasound-guided biopsy, renal biopsy
Introduction
Renal biopsy through the percutaneous approach was introduced decades ago. With time, the advances of automated biopsy needles and ultrasound guidance made it safer with great diagnostic yield in the treatment of children with renal disease [1,2]. Ultrasound-guided percutaneous renal biopsy (PCRB) with a biopsy gun has become an accepted procedure for the past many years, allowing the safe passage of the needle into the kidney to obtain tissue for histological diagnosis. It is minimally invasive and gives satisfactory diagnostic output [3,4].
The accurate localization of the lower pole of the kidney by ultrasound is essential for the success and safety of the biopsy procedure. Ultrasound guidance along with automated biopsy needles is intended for optimizing the efficacy and safety of the PCRB procedure. This results in considerable improvement in the general safety and complication rate of the procedure [1,3,5,6].
The primary complications faced after ultrasound-guided renal biopsy are hematuria and hematoma due to post-biopsy bleeding [7-9]. Nonetheless, most of the perirenal hematomas are not clinically significant and resolve spontaneously. The main concerns of the procedure are sufficient tissue for histopathological diagnosis and post-biopsy bleeding which are clinically important [10,11]. This study is undertaken to examine the feasibility and safety of this critical procedure in a pediatric population in a resource-poor setting.
Materials and methods
This cross-sectional study was conducted among children with a clinical diagnosis of nephrotic and nephritic syndrome from January 2017 to September 2020 at The Kidney Centre Post Graduate Training Institute Karachi (TKC-PGTI). Approval from the Ethical Review Committee was taken (No.69-RAD-102018). Data of all children who underwent ultrasound guided PCRB during the study period were collected and analyzed.
Renal biopsy was done from the lower pole of the left kidney by a trained pediatric nephrologist using an 18-gauge automated spring-loaded biopsy needle under ultrasound guidance of a senior radiologist and under general anesthesia in the operation theater.
Most children had nephrotic syndrome (with steroid resistance or dependence) or frequently relapsing nephrotic syndrome as a primary indication for biopsy. Biopsies were performed using an 18-gauge automated spring-loaded biopsy needle under ultrasound guidance (Figure 1).
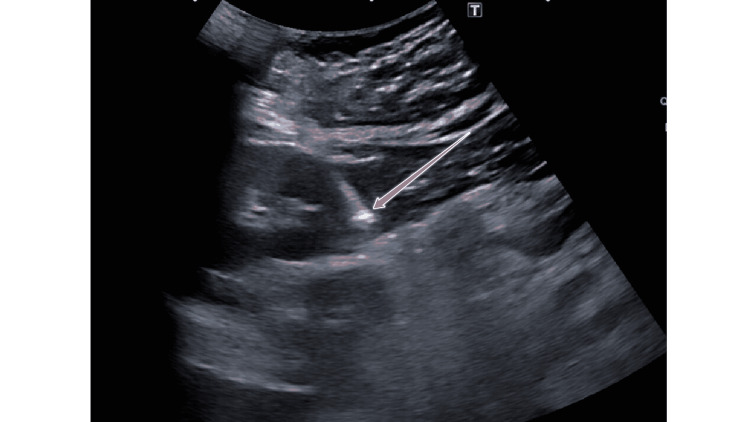
Figure 1. Percutaneous biopsy of the kidney under ultrasound guidance.
The sonographic image of the right kidney shows the position of the biopsy needle (arrow) after firing. The entire intraparenchymal portion of the needle is located within the renal cortex, avoiding the renal medulla and more centrally located blood vessels.
All procedures were performed in the operation theater under aseptic measures and general anesthesia along with subcutaneous local anesthesia. All children underwent standard pre-biopsy evaluation including coagulation profile (prothrombin time and partial thromboplastin time), renal function tests (blood urea, creatinine, and electrolytes), and full blood count and ultrasonography for confirmation of both kidneys and exclusion of any congenital anomaly. Blood tests for hepatitis B and C infection were also carried out in all cases. Blood tests for autoimmune markers were done in selected cases.
Post-biopsy, all patients were kept in hospital for at least 24 hours with monitoring of vitals and gross hematuria. Post-biopsy ultrasound was done after six hours for evidence of hematoma or perirenal collection. In case of complication, a follow-up ultrasound was done at 24 hours. The perirenal hematoma or collection was small in all cases and did not warrant intervention. In case of no complication, the ultrasound was repeated a few weeks later. Data were analyzed using Statistical Package for the Social Sciences version 21 (IBM Corp., Armonk, NY, USA), and descriptive statistics were applied.
The abstract of this study was previously presented at the European Congress of Radiology 2019.
Results
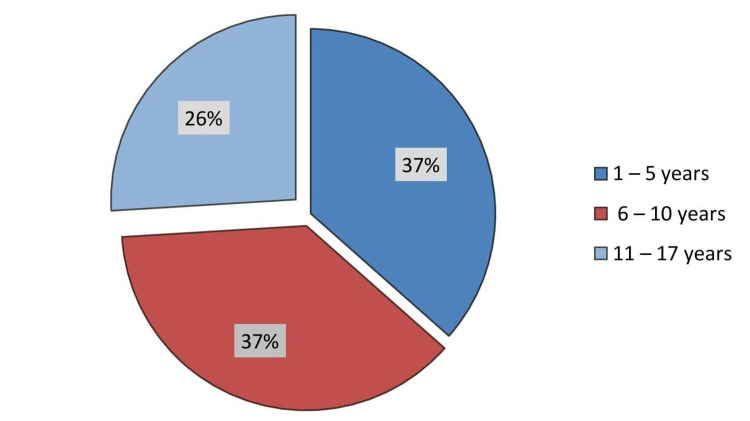
A total of 104 patients underwent PCRBs during the study period. The mean age of the children biopsied was 7.44 ± 4.12 years (range = 1-17 years) with an almost equal male-to-female ratio (Figure 2).
Figure 2. Age distribution of patients.
The pie chart shows the age distribution of children undergoing percutaneous renal biopsy.
The most common indication was primary nephrotic syndrome (95.5%). Among nephrotic syndrome, steroid-sensitive nephrotic syndrome was the most common indication for biopsy (n = 54, 51.9%), followed by steroid-dependent nephrotic syndrome (n = 29, 27.8%) and the frequently relapsing type (n = 13, 12.5%). Biopsy for lupus nephritis and rapidly progressing glomerulonephritis/nephritic syndrome was also indicted in two separate cases. Other indications (n = 4, 3.84%) for biopsy included Henoch-Schönlein Purpura and post-infectious glomerulonephritis in two cases each (Table 1).
Table 1. Clinical indications of patients who underwent percutaneous renal biopsy.
| Clinical diagnosis | Number |
| Steroid-sensitive nephrotic syndrome | 54 |
| Steroid-dependent nephrotic syndrome | 29 |
| Frequently relapsing nephrotic syndrome | 13 |
| Lupus nephritis | 2 |
| Rapidly progressing glomerulonephritis/nephritic syndrome | 2 |
| Henoch-Schönlein purpura | 2 |
| Post-infectious glomerulonephritis | 2 |
| Total | 104 |
Adequate renal tissues were obtained in 98 patients with a success rate of 94%. In the majority of the patients (80%), two core tissue specimens were obtained (Figure 2). Most children (n = 88, 84.62%) underwent a single post-biopsy complication while only two cases showed four (1.92%) post-biopsy complications. An inadequate sample with scanty glomeruli was obtained in six cases.
Almost 94% of the PCRBs were rendered successful. Post-biopsy complications were observed in 16 cases, and perinephric hematoma (12.50%) was the most common post-biopsy complication, followed by gross hematuria (7.77%) (Table 2).
Table 2. Complications of percutaneous renal biopsy.
| Complications | Number |
| Perinephric hematoma | 13 |
| Renal hematoma | 1 |
| Gross hematuria | 8 |
| Blood clot/Urine retention | 4 |
| Total | 26 |
We observed 13 perinephric hematomas and eight gross hematuria cases, which subsided in three days. However, two post-biopsy gross hematuria complications extended more than three days. None of our patients developed arteriovenous fistula on follow-up Doppler scans. The most commonly diagnosed disease was minimal change disease, followed by focal segmental glomerulosclerosis (Table 3).
Table 3. Histopathological diagnosis of patients who underwent percutaneous renal biopsy.
| Histopathology | Number |
| Minimal change disease | 42 |
| Focal segmental glomerulosclerosis | 33 |
| Membranous glomerular disease | 9 |
| Membranoproliferative glomerulonephritis | 3 |
| Lupus nephritis | 3 |
| Tubulointerstitial nephritis | 3 |
| Henoch-Schönlein purpura/Immunoglobulin A nephropathy | 3 |
| Post-infectious glomerulonephritis | 2 |
| Failed | 6 |
| Total | 104 |
Discussion
Ultrasound-guided PCRB is a recognized and effective diagnostic technique in children and adolescents for many years. Even though there is an abatement in the complication rates and improvement in safety with the use of ultrasound guidance, these procedures have few procedural complications and should not be done without attentiveness and care. The spectrum of complications includes small perirenal and renal hematomas, hemorrhage that may lead to obstruction of the urinary tract, or arteriovenous fistulas. Subcapsular renal hematomas that cause compression over the kidney require primal disclosure by early post-biopsy ultrasound (within 4-24 hours). It has a crucial role in prognosis. The risk of hematuria is increased if the post-biopsy hematoma has a width of 2 cm or more. As reported by the literature and established by different definitions, the complication rate varies between 0% and 45% [1,2,11,12]. A study from Nigeria performed PCRB in 24 patients, of whom complications occurred in two (8.3%) patients. One patient had vague abdominal pain over the biopsy site, while the second had a persistent, painless gross hematuria. The study reported no procedure-related deaths or complications requiring surgical intervention. The authors of the study obtained adequate tissue in 20 patients [1]. Franke et al. reported 99% efficacy of PCRB with no lethal complications. Only three of their patients received a blood transfusion but none of the patients required interventional treatment. The complication rate was 4.1% in their study which is similar to ours [11]. The complication rate should not be above 5% as per the standard of the British Association of Pediatric Nephrology (BAPN). In our study, the complication rate observed is 4.1%, fulfilling the standards of BAPN. No significant difference was seen in the incidence of complications between males and females. Similarly, no statistical difference was seen in the incidence of complications between inpatients and outpatients. Biopsies were followed with ultrasound using a prospective and strict protocol for follow-up examinations, including Doppler ultrasound.
Various sizes and types of needles have been used by different authors to minimize bleeding complications [4,5,12-15]. We used 18-gauge Tru-cut needles with exact positioning of the needles under ultrasound guidance and found that they were safe and effective with no major complications.
In most of our patients, two passes of the needle acquired an adequate sample for histopathology, with only a few requiring three or more passes with a maximum of five passes in one obese patient. We faced a little difficulty with obese patients and those with edema.
Limitations
Our sample size was relatively small and only represented a single center. Our study was a retrospective one, with the inherent limitations of retrospective studies.
Conclusions
Ultrasound-guided PCRB is a safe approach for acquiring renal tissue for establishing the histopathological diagnosis in children. The use of real-time ultrasound guidance and an automated biopsy gun in experienced hands ensures good outcomes. It provides ample tissue for the diagnosis in more than 90% of the cases.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Ethical Review Committee, The Kidney Centre issued approval No.69-RAD-102018
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Out-patient percutaneous renal biopsy among children in Northern Nigeria: a single center experience. Obiagwu PN, Abdu A, Atanda AT. Ann Afr Med. 2014;13:169–173. doi: 10.4103/1596-3519.142286. [DOI] [PubMed] [Google Scholar]
- 2.Experience of renal biopsy in children with nephrotic syndrome. Nammalwar BR, Vijayakumar M, Prahlad N. Pediatr Nephrol. 2006;21:286–288. doi: 10.1007/s00467-005-2084-5. [DOI] [PubMed] [Google Scholar]
- 3.An overview on frequency of renal biopsy diagnosis in Brazil: clinical and pathological patterns based on 9,617 native kidney biopsies. Polito MG, de Moura LA, Kirsztajn GM. Nephrol Dial Transplant. 2010;25:490–496. doi: 10.1093/ndt/gfp355. [DOI] [PubMed] [Google Scholar]
- 4.Role of renal biopsy in managing pediatric renal diseases: a midterm analysis of a series at bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh. Roy RR, Al Mamun A, Shamsul Haque SM, Muinuddin G, Rahman MH. Saudi J Kidney Dis Transpl. 2017;28:125–132. doi: 10.4103/1319-2442.198164. [DOI] [PubMed] [Google Scholar]
- 5.Percutaneous renal biopsy in children: a 27-year experience. Feneberg R, Schaefer F, Zieger B, Waldherr R, Mehls O, Schärer K. Nephron. 1998;79:438–446. doi: 10.1159/000045090. [DOI] [PubMed] [Google Scholar]
- 6.Bleeding complications after transcutaneous kidney biopsy in patients with systemic amyloidosis: single-center experience in 101 patients. Soares SM, Fervenza FC, Lager DJ, Gertz MA, Cosio FG, Leung N. Am J Kidney Dis. 2008;52:1079–1083. doi: 10.1053/j.ajkd.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 7.Safety and complications of percutaneous kidney biopsies in 715 children and 8573 adults in Norway 1988-2010. Tøndel C, Vikse BE, Bostad L, Svarstad E. Clin J Am Soc Nephrol. 2012;7:1591–1597. doi: 10.2215/CJN.02150212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Renal biopsies in children: current practice and audit of outcomes. Hussain F, Mallik M, Marks SD, Watson AR. Nephrol Dial Transplant. 2010;25:485–489. doi: 10.1093/ndt/gfp434. [DOI] [PubMed] [Google Scholar]
- 9.Clinical risk factors associated with bleeding after native kidney biopsy. Shidham GB, Siddiqi N, Beres JA, Logan B, Nagaraja HN, Shidham SG, Piering WF. Nephrology (Carlton) 2005;10:305–310. doi: 10.1111/j.1440-1797.2005.00394.x. [DOI] [PubMed] [Google Scholar]
- 10.Yield and complications in percutaneous renal biopsy. A comparison between ultrasound-guided gun-biopsy and manual techniques in native and transplant kidneys. Nyman RS, Cappelen-Smith J, al Suhaibani H, Alfurayh O, Shakweer W, Akhtar M. Acta Radiol. 1997;38:431–436. doi: 10.1080/02841859709172096. [DOI] [PubMed] [Google Scholar]
- 11.Ultrasound-guided percutaneous renal biopsy in 295 children and adolescents: role of ultrasound and analysis of complications. Franke M, Kramarczyk A, Taylan C, Maintz D, Hoppe B, Koerber F. PLoS One. 2014;9:0. doi: 10.1371/journal.pone.0114737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Percutaneous renal biopsy of native kidneys: efficiency, safety and risk factors associated with major complications. Torres Muñoz A, Valdez-Ortiz R, González-Parra C, Espinoza-Dávila E, Morales-Buenrostro LE, Correa-Rotter R. Arch Med Sci. 2011;7:823–831. doi: 10.5114/aoms.2011.25557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Percutaneous ultrasound-guided renal biopsy in children: a single centre experience. Printza N, Bosdou J, Pantzaki A, Badouraki M, Kollios K, Ghogha C, Papachristou F. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306034/ Hippokratia. 2011;15:258–261. [PMC free article] [PubMed] [Google Scholar]
- 14.An approach to the paediatric renal biopsy. Sebire NJ. Curr Diagn Pathol. 2007;13:43–53. [Google Scholar]
- 15.Percutaneous ultrasound-guided renal biopsy in children: the need for renal biopsy in pediatric patients with persistent asymptomatic microscopic hematuria. Yu MC, Lee F, Huang WH, Hsueh S. Biomed J. 2014;37:391–397. doi: 10.4103/2319-4170.132878. [DOI] [PubMed] [Google Scholar]