Abstract
Background:
Myocardial infarction (MI) with non-obstructive coronary arteries (MINOCA) represents ~6% of all acute MI. Myocarditis is a diagnosis that may be identified by cardiac magnetic resonance (CMR) imaging in patients with a provisional diagnosis of MINOCA. The aim of the study was to determine the prevalence of myocarditis among patients presenting with MINOCA in relation to the angiographic severity of non-obstructive coronary artery disease (CAD).
Methods:
We performed a systematic review to identify studies reporting the results of CMR findings in MINOCA patients with non-obstructive CAD or normal coronary arteries. Study-level and individual patient-data meta-analyses were performed using fixed and random effects methods.
Results:
27 articles were included with 2,921 MINOCA patients; CMR findings were reported in 2,866 (98.1%). Myocarditis prevalence was 34.5% (95% CI 27.2%-42.2%) overall and was numerically higher in studies that defined MINOCA as MI with angiographically normal coronaries compared with a definition that permitted non-obstructive CAD (45.9% vs. 32.3%, p=0.16). In a meta-analysis of individual patient data from 9 of the 27 studies, the pooled prevalence of CMR-confirmed myocarditis was greater in patients with angiographically normal coronary arteries than those with non-obstructive CAD (51% [95% CI 47-56%] vs. 23% [18-27%], p<0.001). Men and younger MINOCA patients were more likely to have myocarditis. Angiographically normal coronaries were associated with increased odds of myocarditis after adjustment for age and sex (aOR 2.30, 95% 1.12-4.71; p=0.023).
Conclusion:
Patients with a provisional diagnosis of MINOCA are more likely to have CMR findings consistent with myocarditis if they have angiographically normal coronary arteries.
Keywords: Myocarditis, Myocardial Infarction, Cardiac Magnetic Resonance Imaging
Condensed Abstract:
Myocarditis may be identified by cardiac magnetic resonance (CMR) imaging in patients with a provisional diagnosis of myocardial infarction with non-obstructive coronary arteries (MINOCA). We performed a systematic review of 27 studies with 2,921 patients with provisional MINOCA diagnoses. Myocarditis prevalence was 34.5% overall. In a meta-analysis of individual patient data from 9 of the 27 studies, the pooled prevalence of CMR-confirmed myocarditis was greater in patients with angiographically normal coronary arteries than those with non-obstructive CAD (51% [95% CI 47-56%] vs. 23% [18-27%], p<0.001). Men and younger MINOCA patients were more likely to have myocarditis.
Background:
Myocardial infarction with nonobstructive coronary arteries (MINOCA) represents approximately 6% of all acute myocardial infarctions (MI) and more often affects women and younger patients.1–5 MINOCA is a working diagnosis with a variety of potential underlying etiologies including coronary artery spasm, occult plaque rupture/erosion, coronary thrombosis and thrombolysis, coronary embolism, and coronary dissection.2,5 Alternative diagnoses in patients with suspected MINOCA include myocarditis and takotsubo syndrome.2 It is recommended that patients with a provisional diagnosis of MINOCA undergo a complete diagnostic workup including cardiac magnetic resonance imaging (CMR) where available, to identify the etiology of the MI presentation.2,5 CMR is a highly sensitive and specific imaging modality that can reliably identify myocarditis.6,7 Studies reporting the frequency of myocarditis in patients presenting with MINOCA are small and heterogeneous, with prevalence of myocarditis reported to be between 4% and 75% by CMR.8–21 This wide range may be related to demographics of enrolled participants, variations in the definition of MINOCA, as well as the timing of CMR after the initial presentation. The contemporary definition of MINOCA requires a clinical presentation consistent with the Universal Definition of MI and non-obstructive coronary arteries with <50% diameter stenosis in all major epicardial coronary vessels by coronary angiography.2,3 However, some studies have used a <30% diameter stenosis cutoff or restricted the analysis to MI patients with angiographically normal coronary arteries. The aim of this systematic review was to clarify the prevalence of myocarditis by CMR among patients presenting with MINOCA overall and stratified according to coronary angiographic findings.
Methods:
We performed a comprehensive structured systematic review of the literature to identify studies reporting the results of CMR findings in patients with MI and non-obstructive or normal coronary arteries. In collaboration with a librarian with systematic review expertise, we searched PubMed/MEDLINE, Ovid EMBASE, Ovid Cochrane CENTRAL, and Web of Science databases through October 18th, 2018. We created a search strategy using keywords and appropriate subject headings for our main concepts: acute coronary syndrome or myocardial infarction, non-obstructive or normal coronary arteries, and magnetic resonance imaging. Studies were eligible for inclusion if they were published as full-text, English-language manuscripts that included original data on the prevalence of myocarditis as determined by CMR among patients with a provisional diagnosis of MI with non-obstructive coronary arteries (now termed MINOCA). We excluded abstracts from scientific conferences, articles that did not report CMR findings in all patients, studies that included patients without MI or did not specify a consistent definition of non-obstructive coronary artery disease (CAD) (such as definitions of MINOCA that required the “absence of a culprit lesion” or without a discrete threshold specified for maximum stenosis severity), and manuscripts that did not report the prevalence of myocarditis by CMR. Manuscripts that focused exclusively on patients with suspected takotsubo syndrome were also excluded from analysis. The initial search yielded 1,337 unique manuscripts eligible for screening (Figure 1). Two reviewers independently conducted review of titles and abstracts, with conflicts resolved through adjudication by a third reviewer. This resulted in the exclusion of 1,214 records. A full-text review of the remaining 123 studies excluded an additional 100 studies that did not meet study eligibility criteria. Four additional references that met study eligibility criteria but were not returned during the database query were identified through expert review. All 27 studies were evaluated using the Newcastle-Ottawa Quality Assessment Scale, an instrument recommended by the Cochrane Collaborative Group for the assessment of quality of nonrandomized observational studies.22 The definition of MINOCA and the frequency of CMR findings in patients with MINOCA were recorded for each eligible study. Myocarditis was defined according to non-ischemic regional distribution of late gadolinium enhancement alone in 15 studies and Lake Louise Consensus Criteria (non-ischemic late gadolinium enhancement with edema on T-2 weighted images) in 12 studies.6
Figure 1.
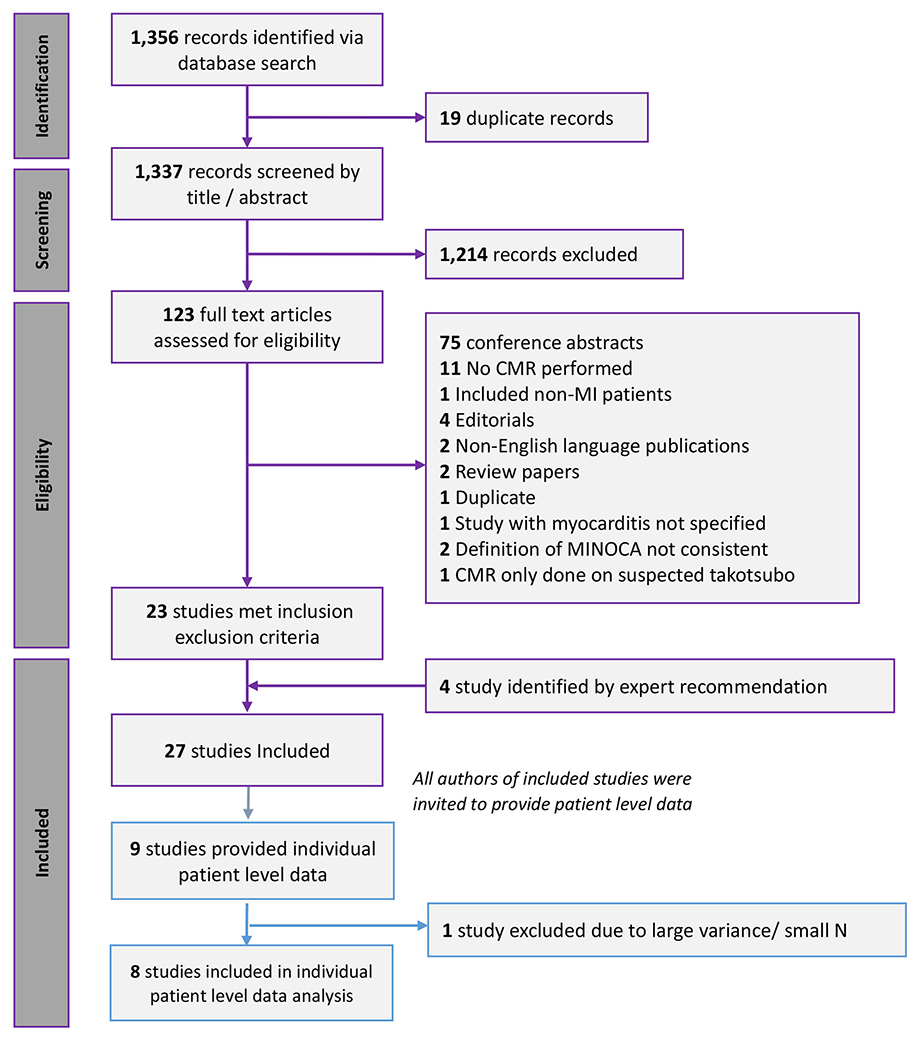
PRISMA flow diagram of study selection process
To complement study-level meta-analyses, corresponding authors of all eligible studies were contacted and invited to contribute de-identified data to an individual patient level meta-analysis. Nine authors responded and contributed de-identified data.
Pooled prevalence of myocarditis and its 95% confidence intervals (CIs) was estimated from meta-analysis, using either fixed-effects or random-effects models, depending on the degree of statistical heterogeneity present. Heterogeneity in the study estimates were assessed using I2 statistics. For the Higgins I2 test, statistical significance was set at 50% or greater. Study-level CMR data from the 27 publications were pooled and analyzed using random effects meta-analysis models to estimate the prevalence of myocarditis overall and within subgroups based on coronary angiographic findings. The prevalence of myocarditis was also estimated using fixed effects models of individual patient data. The association between sex, age, angiographic findings, and myocarditis was assessed using random effects meta-analysis of individual patient data. The relationship between non-obstructive CAD and a CMR-confirmed diagnosis of myocarditis was adjusted for age and sex. Publication bias was tested using Egger’s test of asymmetry and visual inspection of a Funnel plot. A sensitivity analysis was performed excluding studies with small sample sizes and large variances to determine consistency of the general findings. All analyses were performed using STATA (version 15, College Station, TX, USA). All data used in this meta-analysis were de-identified and observational, and New York University School of Medicine institutional board review was not required for the meta-analysis. Each individual study received ethics committee/institutional review board approval at the time of recruitment.
Results
A total of 27 publications met the study inclusion criteria and were included in the systematic review (Figure 1, Supplemental Table 1). Of these, 5 studies defined the study cohort as MI with angiographically normal coronary arteries (0% angiographic diameter stenosis), 2 defined the study cohort based on MI with <30% diameter stenosis, and 20 studies defined the study cohort based on MI with <50% diameter stenosis in all coronary arteries. These 27 studies reported CMR findings in 2,866 of the 2,921 MINOCA patients (98.1%). Lack of CMR completion was most commonly secondary to patient refusal, claustrophobia or lack of availability of CMR.
Study Level Meta-Analysis
The pooled prevalence of CMR-defined myocarditis in patients with a provisional diagnosis of MINOCA was 34.5% (95% CI 27.2%-42.2%) overall and 34.9% (95% CI 27.8%-42.4%) among those MINOCA patients who underwent CMR in the 27 studies that met study eligibility criteria. 19/27 (70%) were prospective studies. The prevalence of myocarditis varied by study based on the maximum allowable diameter stenosis for a diagnosis of MINOCA. Overall, myocarditis prevalence was numerically greater when MINOCA was defined as MI with angiographically normal coronaries compared with a MINOCA definition that included non-obstructive coronary disease (<50% diameter stenosis) (45.9% [95% CI 28.8%-63.5%] vs. 32.3% [95% CI 24.6%-40.5%], test for heterogeneity between subgroups, p=0.16, I2), although this did not reach statistical significance (Figure 2). A high heterogeneity was observed in the analysis (I2 = 94.3%). A numerically greater prevalence of myocarditis was also observed in patients with angiographically normal coronary arteries after excluding 3 studies in which not all MINOCA patients had CMR (45.9% vs. 36.6%, test for heterogeneity between subgroups, p=0.33) (Supplemental Figure 1).
Figure 2: Proportion of myocarditis among patients and 95% confidence intervals with MINOCA based on the threshold angiographic diameter stenosis.
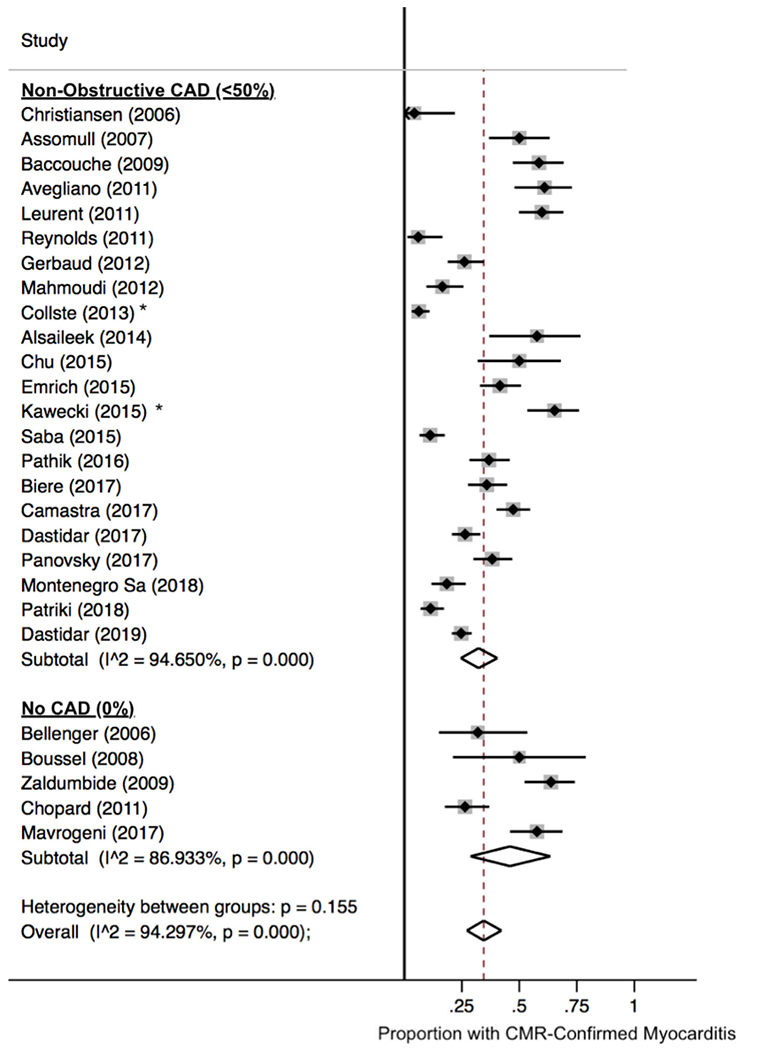
* Denotes studies that defined MINOCA based on <30% diameter stenosis by coronary angiography.
Prevalence of CMR confirmed Myocardial Infarction
Twenty-six studies including 2,777 MINOCA patients with CMR data reported the frequency of CMR-confirmed myocardial infarction. The pooled prevalence of CMR findings of MI was 17.8% (95% CI 13.8-22.2%). Myocardial imaging by CMR was normal in 26.3% (95% CI 17.8-35.7%). There was no association between the study-level angiographic definition of MINOCA and the frequency of CMR-confirmed myocardial infarction (p=0.13) or normal CMR (p=0.47).
Meta-Analysis of Individual Patient Data
Authors of 9 studies contributed to a meta-analysis of individual patient data. Among 911 patients with a provisional diagnosis of MINOCA undergoing CMR, the pooled prevalence of myocarditis was greater in patients with angiographically normal coronary arteries than in patients with non-obstructive CAD (51% [95% CI 47-56%] vs. 23% [18-27%], p<0.001) and angiographically normal coronary arteries were associated with increased odds of myocarditis (OR 3.44, 95% CI 1.88-6.29, p<0.001, Supplemental Figure 2) compared to non-obstructive CAD. A sensitivity analysis was performed excluding one study from the analysis due to small sample sizes, low rates of myocarditis, and large variances. A funnel plot and Egger’s test (p=0.43) of the remaining studies were not suggestive of publication bias (Supplemental Figure 3). In these 8 studies (n=896 patients), the mean age of participants was 53.2 years and 53% were female. Angiographically normal coronaries were associated with increased odds of myocarditis (OR 3.26, 95% CI 1.77-6.01, p<0.001; Supplemental Figure 4). In a random effects meta-analysis of individual patient data from 7 studies that included men and women with suspected MINOCA (n=852 patients), female sex was associated with lower odds of myocarditis than male sex (OR 0.26, 95% CI 0.10-0.65, p=0.004). In the 7 studies that reported age (n=705), older age was also associated with a lower likelihood of myocarditis in MINOCA (OR 0.94 per year, 95% CI 0.93-0.95, p<0.001). Compared to individuals age <40 years with a provisional diagnosis of MINOCA, patients aged 40-49 (OR 0.28, 95% CI 0.18 - 0.45, p<0.001), 50-59 (OR 0.14, 95% CI 0.09 - 0.24, p<0.001), 60-69 (OR 0.17, 95% CI 0.10 - 0.28, p<0.001), and age 70+ years (OR 0.06, 95% CI 0.04 - 0.11, p<0.001) had lower odds of myocarditis (Supplemental Figure 5). In a multivariable model adjusted for age and sex, the finding of angiographically normal coronary arteries was independently associated with myocarditis (aOR 2.30, 95% 1.12-4.71; p=0.023; Table 1).
Table 1.
Characteristics independently associated with CMR-confirmed myocarditis in patients with a provisional diagnosis of MINOCA in a meta-analysis of individual patient data.
| Characteristic | OR (95% CI) | p-value |
|---|---|---|
| Angiographically Normal Coronaries | 2.30 (1.12-4.71) | 0.023 |
| Female Sex | 0.32 (0.16-0.63) | <0.001 |
| Older Age (per year) | 0.96 (0.95-0.97) | <0.001 |
Discussion:
This is the largest systematic review of CMR-confirmed myocarditis in MINOCA patients, and the first to report the relationship between CMR findings and angiographic severity of CAD in a study level and individual patient data meta-analysis. Myocarditis was identified in 34.5% of patients with MINOCA overall. This has significant clinical relevance, since the treatment of myocarditis differs substantially from that of ischemic mechanisms of MINOCA. In a prior meta-analysis, patients with myocarditis were younger, were more likely to be men, and had a low frequency of underlying cardiovascular risk factors, but the relationship between angiographic severity of CAD and the prevalence of myocarditis was not examined.10 In a meta-analysis of individual patient data, we found that angiographically normal coronary arteries were associated with three-fold increased odds of myocarditis. Younger patients and men were also more likely to have myocarditis, independent of angiographic findings. This is consistent with prior literature reporting that myocarditis is ~1.7 to 4-fold more common among men versus women and occurs at a median age of ~34 years23–25. In the study-level analysis, studies that defined MINOCA based on angiographically normal coronary arteries had a trend toward a higher prevalence of myocarditis by CMR imaging compared with studies that included MINOCA with non-obstructive CAD. This larger analysis was limited by the inclusion of some patients with angiographically normal coronary arteries in studies that defined MINOCA based on ≤50% angiographic stenosis. These results suggest that patient age, sex, and angiographic severity of CAD in patients with a provisional diagnosis of MINOCA significantly impact the pre-test probability of myocarditis by CMR.
Large cohort studies have reported that MI with angiographically normal coronaries represents 47-76% of all MINOCA cases.26–29 Patients with angiographically normal arteries and MI tend to be younger, more often female and have fewer underlying cardiovascular comorbidities compared to patients who develop MINOCA in the setting of mild-to-moderate atherosclerosis.26,29 Though intracoronary imaging may reveal more atherosclerosis than is evident on angiography, available evidence suggests that plaque rupture is less likely when the arteries appear angiographically normal.11,30 The relationship between prognosis after MINOCA and the presence of any atherosclerosis on angiography has been variable in prior studies.12,26,28,31,32 Given the demographic, mechanistic and, in some studies, prognostic differences reported between MINOCA patients with and without any angiographic evidence of CAD, additional investigation is necessary to clarify whether diagnostic pathways and management strategies for MINOCA patients should differ based on degree of CAD discovered at the time of coronary angiography.
Limitations:
This systematic review is based on the published literature reporting CMR findings in MINOCA and may be subject to publication bias and referral bias for CMR. It is possible that patients without angiographic evidence of atherosclerosis were more likely to be referred for CMR. All included studies were observational and many were retrospective. However, after excluding studies in which CMR was not performed in all patients with MINOCA, the study results were remarkably consistent. Individual patient-level data for all included studies were not available for meta-analysis and patient-level analysis was necessarily limited to a smaller sample for this reason. We were unable to independently confirm diagnoses of MINOCA, the severity of CAD, or CMR findings. CMR protocols varied by site, and variable use of T2-weighted imaging or T1 mapping, for example, could theoretically have impacted the results. In addition, sensitivity for myocarditis may increase in patients with higher troponin levels; troponin results were not consistently reported across studies and thus we were unable to correlate the prevalence of myocarditis with troponin levels.
Conclusions:
Myocarditis was identified on CMR in 35% of patients with suspected MINOCA in this systematic review. Angiographically normal coronary arteries were associated with greater than two-fold increased odds of CMR-confirmed myocarditis. Men and younger MINOCA patients were also more likely to have CMR-confirmed myocarditis.
Supplementary Material
Perspectives:
Clinical Competency in Medical Knowledge:
Myocarditis can mimic acute myocardial infarction with non-obstructive coronary arteries (MINOCA) and diagnosis can be confirmed on CMR. The overall prevalence of myocarditis is ~35%.
Clinical Competency in Medical Knowledge 2:
Myocarditis is more frequent among MINOCA patients with angiographically normal coronaries compared to non-obstructive CAD. Myocarditis is also more common among men, and younger MINOCA patients.
Translational Outlook1:
Future prospective studies are needed to determine the best diagnostic strategies and treatments for patients presenting with a provisional diagnosis of MINOCA.
Sponsor / Funding:
Dr. Smilowitz was supported by an NYU CTSA grant, UL1 TR001445 and KL2 TR001446, from the National Center for Advancing Translational Sciences, National Institutes of Health. Dr. Hausvater was supported by a grant from the American Heart Association. Dr. Panovsky was supported by project no. LQ1605 from the National Program of Sustainability II (MEYS CR). Dr. Selvanayagam was supported by research grants from Biotronik, Bayer, Sanofi, Actelion. Dr. Reynolds was supported by the Doris Duke Charitable Foundation (CSDA 2006066)
Conflict of Interest Disclosures:
Dr. Selvanagayam is a consultant for Sanofi, Faraday, Recardio. Dr. Reynolds has received in kind support for an unrelated research study in MINOCA from Abbott Vascular.
Abbreviations List:
- MI
Myocardial Infarction
- MINOCA
Myocardial infarction with non-obstructive coronary arteries
- CMR
cardiac magnetic resonance
- CAD
coronary artery disease
References:
- 1.Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131(10):861–870. [DOI] [PubMed] [Google Scholar]
- 2.Agewall S, Beltrame JF, Reynolds HR, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J. 2017;38(3):143–153. [DOI] [PubMed] [Google Scholar]
- 3.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2018. [DOI] [PubMed] [Google Scholar]
- 4.Smilowitz NR, Mahajan AM, Roe MT, et al. Mortality of Myocardial Infarction by Sex, Age, and Obstructive Coronary Artery Disease Status in the ACTION Registry-GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry-Get With the Guidelines). Circ Cardiovasc Qual Outcomes. 2017;10(12):e003443. [DOI] [PubMed] [Google Scholar]
- 5.Tamis-Holland JE, Jneid H, Reynolds HR, et al. Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association. Circulation. 2019:CIR0000000000000670. [DOI] [PubMed] [Google Scholar]
- 6.Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol. 2009;53(17):1475–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stillman AE, Oudkerk M, Bluemke D, et al. Assessment of acute myocardial infarction: current status and recommendations from the North American society for Cardiovascular Imaging and the European Society of Cardiac Radiology. The international journal of cardiovascular imaging. 2011;27(1):7–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monney PA, Sekhri N, Burchell T, et al. Acute myocarditis presenting as acute coronary syndrome: role of early cardiac magnetic resonance in its diagnosis. Heart. 2011;97(16):1312–1318. [DOI] [PubMed] [Google Scholar]
- 9.Christiansen JP, Edwards C, Sinclair T, et al. Detection of myocardial scar by contrast-enhanced cardiac magnetic resonance imaging in patients with troponin-positive chest pain and minimal angiographic coronary artery disease. Am J Cardiol. 2006;97(6):768–771. [DOI] [PubMed] [Google Scholar]
- 10.Tornvall P, Gerbaud E, Behaghel A, et al. Myocarditis or “true” infarction by cardiac magnetic resonance in patients with a clinical diagnosis of myocardial infarction without obstructive coronary disease: A meta-analysis of individual patient data. Atherosclerosis. 2015;241(1):87–91. [DOI] [PubMed] [Google Scholar]
- 11.Reynolds HR, Srichai MB, Iqbal SN, et al. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation. 2011;124(13):1414–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hausvater A, Pasupathy S, Tornvall P, et al. ST-segment elevation and cardiac magnetic resonance imaging findings in myocardial infarction with non-obstructive coronary arteries. Int J Cardiol. 2019;287:128–131. [DOI] [PubMed] [Google Scholar]
- 13.Assomull RG, Lyne JC, Keenan N, et al. The role of cardiovascular magnetic resonance in patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. Eur Heart J. 2007;28(10):1242–1249. [DOI] [PubMed] [Google Scholar]
- 14.Camastra GS, Sbarbati S, Danti M, et al. Cardiac magnetic resonance in patients with acute cardiac injury and unobstructed coronary arteries. World J Radiol. 2017;9(6):280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pathik B, Raman B, Mohd Amin NH, et al. Troponin-positive chest pain with unobstructed coronary arteries: incremental diagnostic value of cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging. 2016;17(10):1146–1152. [DOI] [PubMed] [Google Scholar]
- 16.Alsaileek A, Nasim M, Aljizeeri A, Alharthi M, Al-Mallah MH. The role of delayed contrast-enhanced cardiac magnetic resonance in differentiating myocarditis from myocardial infarction. European Heart Journal Supplements. 2014;16(B):B24–B28. [Google Scholar]
- 17.Gerbaud E, Harcaut E, Coste P, et al. Cardiac magnetic resonance imaging for the diagnosis of patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. International Journal of Cardiovascular Imaging. 2012;28(4):783–794. [DOI] [PubMed] [Google Scholar]
- 18.Biere L, Niro M, Pouliquen H, et al. Risk of ventricular arrhythmia in patients with myocardial infarction and non-obstructive coronary arteries and normal ejection fraction. World J Cardiol. 2017;9(3):268–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montenegro Sa F, Ruivo C, Santos LG, et al. Myocardial infarction with nonobstructive coronary arteries: a single-center retrospective study. Coron Artery Dis. 2018;29(6):511–515. [DOI] [PubMed] [Google Scholar]
- 20.Emrich T, Emrich K, Abegunewardene N, et al. Cardiac MR enables diagnosis in 90% of patients with acute chest pain, elevated biomarkers and unobstructed coronary arteries. Br J Radiol. 2015;88(1049):20150025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panovsky R, Borova J, Pleva M, et al. The unique value of cardiovascular magnetic resonance in patients with suspected acute coronary syndrome and culprit-free coronary angiograms. BMC Cardiovasc Disord. 2017;17(1):170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wells GSB OC D, Peterson J, Welch V, Losos M, Tugwell P The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000; http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 23.Ammirati E, Cipriani M, Moro C, et al. Clinical Presentation and Outcome in a Contemporary Cohort of Patients With Acute Myocarditis. Circulation. 2018;138(11):1088–1099. [DOI] [PubMed] [Google Scholar]
- 24.Caforio ALP, Calabrese F, Angelini A, et al. A prospective study of biopsy-proven myocarditis: prognostic relevance of clinical and aetiopathogenetic features at diagnosis. European Heart Journal. 2007;28(11):1326–1333. [DOI] [PubMed] [Google Scholar]
- 25.Anzini M, Merlo M, Sabbadini G, et al. Long-term evolution and prognostic stratification of biopsy-proven active myocarditis. Circulation. 2013;128(22):2384–2394. [DOI] [PubMed] [Google Scholar]
- 26.Alzuhairi KS, Sogaard P, Ravkilde J, et al. Long-term prognosis of patients with non-ST-segment elevation myocardial infarction according to coronary arteries atherosclerosis extent on coronary angiography: a historical cohort study. BMC Cardiovasc Disord. 2017;17(1):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larsen AI, Nilsen DW, Yu J, et al. Long-term prognosis of patients presenting with ST-segment elevation myocardial infarction with no significant coronary artery disease (from the HORIZONS-AMI trial). Am J Cardiol. 2013;111(5):643–648. [DOI] [PubMed] [Google Scholar]
- 28.Bugiardini R, Manfrini O, De Ferrari GM. Unanswered questions for management of acute coronary syndrome: risk stratification of patients with minimal disease or normal findings on coronary angiography. Arch Intern Med. 2006;166(13):1391–1395. [DOI] [PubMed] [Google Scholar]
- 29.Bainey KR, Welsh RC, Alemayehu W, et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA): Insights from the Alberta contemporary acute coronary syndrome patients invasive treatment strategies (COAPT) study. Int J Cardiol. 2018;264:12–17. [DOI] [PubMed] [Google Scholar]
- 30.Opolski MP, Spiewak M, Marczak M, et al. Mechanisms of Myocardial Infarction in Patients With Nonobstructive Coronary Artery Disease: Results From the Optical Coherence Tomography Study. JACC Cardiovascular imaging. 2018. [DOI] [PubMed] [Google Scholar]
- 31.Williams MJA, Barr PR, Lee M, Poppe KK, Kerr AJ. Outcome after myocardial infarction without obstructive coronary artery disease. Heart. 2019;105(7):524–530. [DOI] [PubMed] [Google Scholar]
- 32.Bainey KR, Welsh RC, Alemayehu W, et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA): Insights from the Alberta contemporary acute coronary syndrome patients invasive treatment strategies (COAPT) study. International journal of cardiology. 2018;264:12–17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


