Abstract
Background
Caregivers of cancer patients commonly experience depressive symptoms due to the heavy burden of caregiving responsibility.
Objective
This meta-analysis examined the prevalence of depression among caregivers of cancer patients.
Methods
We included 85 studies covering 23,317 participants published between 2001 and 2021 (25 countries) that reported the prevalence of depression among caregivers of cancer patients. We examined the pooled prevalence of depression and hypothesized moderators, including year, age, sex, geographic regions, percentage of spousal caregivers, depression measures, and cancer stage.
Results
All 85 effect sizes included 6,077 caregivers of patients with depression. The weighted average prevalence of depression was 25.14% (95% CI, 21.42–29.27%) among caregivers. The prevalence rates were moderated by geographic region, patients' cancer stage, and measures for depression. The prevalence rates also varied among the different measures assessing depression. The prevalence rate decreased with the mean age of the caregivers and the percentage of spousal caregivers.
Conclusions
This study revealed a high prevalence of depression among caregivers of cancer patients. The prevalence rates also varied with the study design, demographics of caregivers, and patients' medical information. These findings highlight that psychological support and intervention may be crucial for patients and their caregivers in clinical practice.
Keywords: meta-analysis for depression among caregivers depression, caregivers, cancer patients, prevalence, meta-analysis, depression
Introduction
Day-to-day caregiving responsibilities are a heavy burden for caregivers of patients suffering from life-threatening illnesses, such as cancer. Additionally, caregivers must contend with their fear and distress regarding their loved ones' health and prognosis. In the past two decades, a growing body of research has documented elevated levels of psychological distress among caregivers. Previous studies suggested that routinely caregiving to a close family member with cancer may negatively affect physical and mental health (1, 2). A wide range of psychosocial, physical, and economic factors contribute to family caregivers' burden throughout the patient's illness, from diagnosis to possible death (3). Several studies have found that a high proportion of family caregivers suffer from depressive symptoms (4, 5). Caregivers' depressive symptoms are also associated with worse quality of life, physical well-being, and less leisure time (4). Depressive symptoms can also compromise caregivers' ability to effectively maintain their role (e.g., providing day-to-day care and satisfying the psychological needs of patients). Thus, investigating the prevalence of depression among caregivers is crucial for enhancing their well-being and improving the quality of caregiving.
In previous studies, the depression prevalence rates among caregivers of cancer patients had significant variance, ranging from 2.6 to 82.2% (6). A community study showed that caregivers of cancer patients scored significantly higher for depression than the UK adult general population. Almost 25% of all caregivers are evaluated as having moderate, severe, or even highly severe depression (7). A meta-analysis included 30 studies with 21,149 participants to estimate the depression prevalence in caregivers of cancer patients; the pooled depression prevalence rate was 42.3% (6). The meta-analysis also identified several factors associated with depressive symptoms, primarily related to caregiver characteristics, such as caregiving burden, spousal caregiving, sex of the caregiver, and caregiver's age. In another meta-analysis that included 58 studies with 9,262 parents of children with cancer, the pooled prevalence of depression was 28.0%, with high heterogeneity. The depression prevalence was also higher than in parents of children without cancer (8).
The heterogeneity of the depression prevalence rates among caregivers may also depend on other moderators, such as geographic regions, depression measurements, and patients' cancer stage. In Denmark, a nationwide population-based cohort study (N = 2,865) found that 17.2% of the family caregivers reported moderate-to-severe pre-loss depressive symptoms (9). In another nationally representative survey among caregivers of cancer patients in Korea, the prevalence rate of moderate-to-severe depression was 41.8% (10). Additionally, assessment tools for depression may account for divergent prevalence rates. In a previous meta-analysis, the pooled prevalence rates estimated with different measures ranged from 3.35% (with diagnostic criteria of depression in the DSM-IV) to 50.82% (with the Center for Epidemiological Studies Depression [CESD]). A meta-analysis examined the prevalence of anxiety, depression, and post-traumatic stress disorder (PTSD) among caregivers of children with cancer. The high heterogeneity was not explained by the caregiver's sex or child's cancer phase but was likely due to significant methodological differences in measurement tools and defined thresholds among the three psychiatric disorders (8). Furthermore, patients' medical information, such as the stage of cancer, may also affect the prevalence of depression in their caregivers. Several studies have found that the cancer stage can significantly explain variations in the severity of depressive symptoms (11–13). Contrastingly, a recent Asian study found no association between patients' cancer stage and caregivers' depression (14). Considering that the characteristics of caregivers and study design may highly impact the prevalence of depression in caregivers of patients with cancer, a more comprehensive meta-analysis is urgently needed.
Even among caregivers of patients with other illnesses, depression is a common experience and the caregivers' characteristics and methodology moderate the depression prevalence rates. In a meta-analysis examining the prevalence of mental health disorders among caregivers of patients with Alzheimer's disease, the pooled prevalence of depression among caregivers was 34.0%. The meta-analysis also revealed that the odds of depression were 2.51 times higher in spousal caregivers (15). A meta-analysis investigated the association between subjective caregiver burden and depressive symptoms among the caregivers of older relatives. They found that care for patients with illness and the sampling method accounted for 45.0% of the heterogeneity. Sex, mean age of caregivers, and percentage of spouses of caregivers did not contribute to the meta-regression model (16). A recent meta-analysis examining the prevalence of depression among informal caregivers of people with dementia revealed that depression prevalence differed according to the instrument used to assess depression, with interviews based on diagnostic criteria yielding the lowest pooled prevalence estimate (17). Due to the impact of these factors on the prevalence of depression in caregivers, it is necessary to conduct a meta-analysis to re-examine the moderators of depression prevalence in caregivers.
Therefore, there is a need to examine the depression prevalence in caregivers of cancer patients and their corresponding moderators. Our primary aim was to determine the pooled prevalence rates of depression among caregivers worldwide. Moderators of interest included 1) characteristics of study: year of publication, geographic regions (i.e., Eastern vs. Western sample), and measures of depressive symptoms; 2) demographics of caregivers (i.e., mean age of caregivers, proportion of male caregivers, and percentage of spousal caregivers); and 3) patients' medical information (i.e., cancer stage).
Methods
Search Strategy
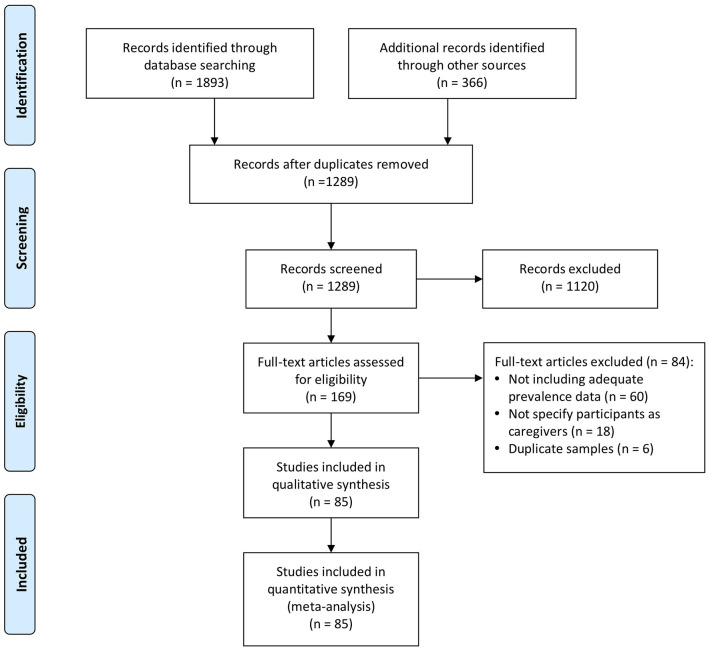
PubMed and PsycINFO were searched using the following search terms with combinations (Caregiver OR Carer OR Relatives [tw] OR Famil* OR Spouse [tw] OR Parent [tw]) AND (Cancer OR Oncology OR Tumor) AND (Depression) AND (Epidemiology OR Prevalence). Reference lists from related articles were included in other relevant studies. Articles published in English that explored depression in caregivers of cancer patients were initially included. Studies involving caregivers who cared for illnesses other than cancer (e.g., rare diseases or dementia) were excluded. Studies were included if they reported the number or percentage of participants with depression assessed by diagnostic interviews based on various criteria. These included the Diagnostic and Statistical Manual of Mental Disorders (DSM), the International Classification of Disease (ICD), or validated self-report measures with specified clinical cutoffs. Two reviewers came to a consensus decision regarding each study wherein there was ambiguity regarding inclusion. Figure 1 shows the flow diagram of the literature search. The original articles included in the identification phase were published between 1972 and 2021. When more than one study reported the same sample, we chose the effect size associated with the most recent and complete data from a given study. The search was updated in August 2021.
Figure 1.
PRISMA flow diagram of the review process.
Study Selection
All studies included in this study met the criteria described by the participants, intervention, comparison, outcome, and study design (PICOS). Participants (P): informal caregivers of cancer patients; Intervention (I): not applicable; Comparison (C): not applicable; Outcomes (O): reported data for depression as defined by self-reported scales with well-validated cutoff values, self-reported medical history, or diagnostic interviews; and Study design (S): all included articles were epidemiological surveys or empirical studies with prevalence data for depression. Data on the depression prevalence in cancer patient caregivers, sample demographic data, country variables, percentage of spousal caregivers, assessment tools, the cutoff point of assessment tools, and patients' medical information were coded. The meta-analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) (18).
Meta-Analysis
We used the metaphor and metaviz package in R to meta-analyze the data (19, 20). The prevalence rates were transformed using logit transformation to normalize the data distribution with inverse variance weighting (21). A random-effects model was used to estimate the average weighted prevalence of depression. We also calculated the depression prevalence rates for each geographic region separately. Cochran's Q statistic was used to assess whether the prevalence rates were homogeneous across samples. The estimates' heterogeneity across studies was examined using I2 index (21). I2 values above 50 and 75% indicate heterogeneity and high heterogeneity, respectively (22). Mixed-effects meta-regression was used to test whether the depression prevalence changed across regions or other design predictors. Meta-regression analyses were then performed to identify moderators that explained the heterogeneity of prevalence.
Results
The search netted 85 studies from 25 different countries, conducted between 2001 and 2021, covering 6,077 cases of depression, with 23,317 participants (5, 9, 10, 14, 23–103). Table 1 lists all studies included in the analyses. There are 85 effect sizes obtained from these 85 studies, which were all on informal caregivers.
Table 1.
Studies included in meta-analysis.
| First Author | Year of Publication | Prevalence | Total N | Location |
Region (East/West) |
Measures for depression |
|---|---|---|---|---|---|---|
| Applebaum | 2020 | 14.00% | 14 | US | W | HADS |
| Areia | 2018 | 68.80% | 112 | Portugal | W | Other |
| Baudry | 2019 | 15.00% | 364 | France | W | HADS |
| Bonafede | 2020 | 32.98% | 94 | Italy | W | BDI |
| Bradley | 2004 | 25.90% | 174 | US | W | SCID |
| Burns | 2021 | 48.65% | 74 | Russia | W | DASS-21 |
| Carey | 2017 | 21.00% | 989 | Australia | W | DASS-21 |
| Corà | 2012 | 45.00% | 20 | Italy | W | BDI |
| Costa-Requena | 2012 | 77.40% | 159 | Spain | W | HADS |
| Doubova | 2016 | 6.80% | 826 | Mexico | W | HADS |
| Duckworth | 2020 | 39.00% | 58 | US | W | CESD |
| Fancourt | 2019 | 11.50% | 62 | UK | W | HADS |
| Fasse | 2015 | 25.00% | 60 | France | W | BDI |
| Fenix | 2006 | 28.00% | 175 | US | W | SCID |
| Fletcher | 2008 | 12.20% | 60 | US | W | CESD |
| Goren | 2014 | 16.00% | 1,713 | European | W | Self-reported diagnosis |
| Gough | 2009 | 12.26% | 106 | Australia | W | HADS |
| Grov | 2005 | 23.96% | 96 | Norway | W | HADS |
| Gupta | 2021 | 28.60% | 904 | US | W | PHQ |
| Haj Mohammad | 2015 | 2.00% | 47 | Netherland | W | HADS |
| Haley | 2001 | 52.50% | 40 | US | W | CESD |
| Han | 2013 | 47.20% | 301 | China | E | CESD |
| Haun | 2014 | 27.00% | 189 | Germany | W | PHQ |
| He | 2020 | 25.50% | 98 | China | E | Other |
| Heckel | 2015 | 30.00% | 150 | Australia | W | CESD |
| Hyde | 2018 | 9.00% | 427 | Australia | W | HADS |
| Jamani | 2018 | 14.80% | 849 | Canada | W | Self-reported diagnosis |
| Janda | 2017 | 14.00% | 84 | Australia | W | HADS |
| Janda | 2008 | 10.30% | 70 | Australia | W | HADS |
| Jassem | 2015 | 17.80% | 107 | European | W | Self-reported diagnosis |
| Kang | 2021 | 24.38% | 159 | South Korea | E | PHQ |
| Katende | 2017 | 26.00% | 119 | Uganda | W | HADS |
| Kehoe | 2019 | 18.90% | 414 | US | W | PHQ |
| Kim | 2014 | 20.00% | 60 | US | W | CESD |
| Kim | 2008 | 24.60% | 314 | US | W | CESD |
| Kim | 2005 | 30.00% | 120 | US | W | CESD |
| Kleijn | 2020 | 29.70% | 64 | Netherland | W | HADS |
| Krähenbühl | 2007 | 21.60% | 109 | Germany | W | Other |
| Lambert | 2013 | 5.20% | 436 | Australia | W | HADS |
| Langenberg | 2019 | 7.00% | 61 | Netherland | W | HADS |
| Lee | 2017 | 14.69% | 143 | Taiwan | E | SCID |
| Lee | 2013 | 17.00% | 106 | Taiwan | E | HADS |
| Leroy | 2016 | 45.00% | 60 | France | W | HADS |
| Lin | 2020 | 31.53% | 555 | China | E | HADS |
| Ling | 2013 | 60.00% | 217 | Taiwan | E | CESD |
| Lutfi | 2019 | 72.00% | 250 | Iraq | E | BDI |
| Malpert | 2015 | 3.10% | 127 | US | W | Other |
| Mazanec | 2017 | 25.00% | 12 | US | W | Other |
| Mazzotti | 2012 | 52.98% | 151 | Italy | W | HADS |
| Mekonnen | 2020 | 23.30% | 275 | Ethiopia | W | BDI |
| Moser | 2013 | 32.84% | 137 | Switzerland | W | HADS |
| Nielsen | 2017 | 17.20% | 2,865 | Denmark | W | BDI |
| Nik Jaafar | 2014 | 33.90% | 130 | Malaysia | E | DASS-21 |
| Oberoi | 2016 | 11.00% | 196 | Australia | W | HADS |
| Oechsle | 2019 | 39.00% | 232 | Germany | W | PHQ |
| Oechsle | 2013 | 21.21% | 33 | Germany | W | PHQ |
| Papastavrou | 2009 | 66.40% | 130 | Greek | W | CESD |
| Park | 2018 | 88.00% | 100 | South Korea | E | HADS |
| Park | 2013 | 41.81% | 897 | South Korea | E | HADS |
| Pawl | 2013 | 28.00% | 126 | US | W | CESD |
| Price | 2009 | 5.10% | 373 | Australia | W | HADS |
| Rhee | 2008 | 66.80% | 310 | South Korea | E | BDI |
| Rumpold | 2017 | 17.90% | 80 | Austria | W | HADS |
| Rumpold | 2015 | 21.30% | 345 | Austria | W | HADS |
| Sacher | 2018 | 31.00% | 45 | Germany | W | CESD |
| Sahadevan | 2019 | 18.00% | 384 | India | E | Other |
| Schellekens | 2016 | 7.10% | 98 | Netherland | W | SCID |
| Shaffer | 2017 | 22.80% | 491 | US | W | CESD |
| Simpson | 2015 | 9.80% | 51 | Australia | W | HADS |
| Stenberg | 2014 | 24.30% | 278 | Norway | W | CESD |
| Sterba | 2017 | 37.00% | 72 | US | W | CESD |
| Stieb | 2018 | 20.00% | 50 | Germany | W | HADS |
| Tang | 2021 | 52.10% | 309 | Taiwan | E | CESD |
| Tang | 2013 | 54.90% | 193 | Taiwan | E | CESD |
| Toledano-Toledano | 2021 | 45.70% | 330 | Mexico | W | BDI |
| Trevino | 2018 | 4.10% | 540 | US | W | SCID |
| Vanderwerker | 2005 | 4.50% | 200 | US | W | SCID |
| Virtue | 2014 | 18.00% | 215 | US | W | SCID |
| Waldman | 2021 | 6.20% | 193 | US | W | HADS |
| Wang | 2016 | 28.20% | 117 | China | E | BDI |
| Wen | 2021 | 79.60% | 661 | Taiwan | E | CESD |
| Williams | 2014 | 21.30% | 150 | US | W | CESD |
| Yang | 2021 | 8.90% | 191 | China | E | HADS |
| Yang | 2012 | 63.50% | 312 | China | E | CESD |
| Yu | 2017 | 21.00% | 309 | China | E | HADS |
E, Eastern country; W, Western country; CESD, Center of Epidemiological Studies Depression Scale; HADS, Hospital Anxiety and Depression Scale; BDI, Beck Depression Inventory; DASS-21, Depression Anxiety Stress Scale; PHQ, Patient Health Questionnaire; SCID, Structured Clinical Interview for DSM.
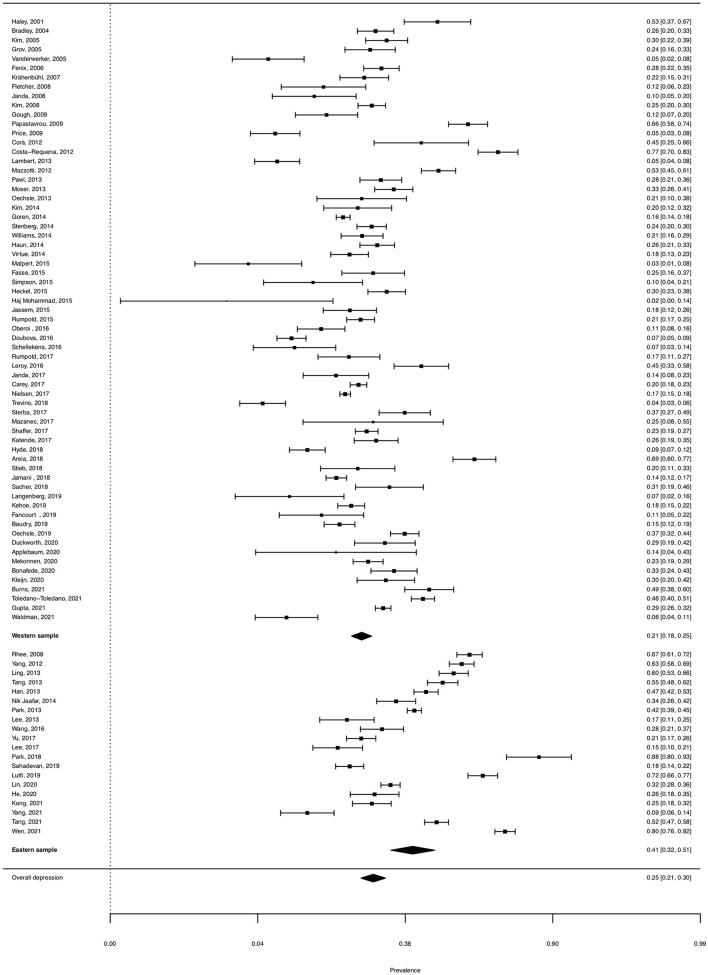
Funnel plot and Egger's test indicated no publication bias (t = −0.66, df = 83, p = 0.508, Figure 2). The pooled prevalence of clinical depression was 25.14% (95% CI, 21.42–29.27%). There was significant heterogeneity between the studies (QE = 3249.96, df = 84, p < 0.0001; H2 = 38.69, I2 = 97.42%). Forest plots of the estimated depression prevalence by study are shown in Figure 3.
Figure 2.
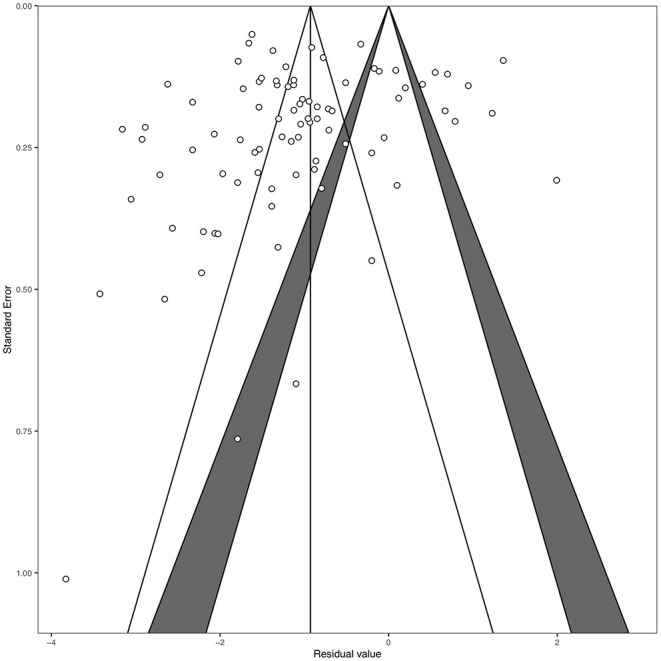
Funnel plot for prevalence of depression among caregivers of cancer patient.
Figure 3.
Forest plot for prevalence of depression among caregivers of cancer patient.
Meta-Regression Analyses
Table 2 shows depression prevalence and the effect of hypothesized moderators. The depression prevalence significantly decreases with the mean age of the caregivers (β = −0.037, p = 0.007). The prevalence of depression significantly decreases with the percentage of spousal caregivers (β = −1.753, p = 0.007). The pooled prevalence is 41.09% for the Eastern sample and 21.19% for the Western sample. The prevalence rate of the studies conducted in the Eastern countries is significantly higher (β = −0.969, p < 0.001) than the prevalence rate in Western countries. The year of publication (β = −0.002, p = 0.925) and proportion of male caregivers (β = 0.152, p = 0.864) did not significantly explain the variance in the depression prevalence.
Table 2.
Clinical depression prevalence by geographic region and measures.
| Subgroups | Categories | k | Prevalence (%) | 95% CI (%) | I2 | Q | p-valuea |
|---|---|---|---|---|---|---|---|
| Clinical depression | 85 | 25.14 | 21.42 – 29.27 | 97.42% | 3249.96 | <0.001 | |
| Geographic region | Eastern sample | 20 | 41.09 | 31.65 – 51.25 | 97.92% | 913.77 | <0.001 |
| Western sample | 65 | 21.19 | 18.21 – 24.52 | 95.13% | 1314.39 | <0.001 | |
| Patient stage of cancer | Non-advanced cancer | 55 | 22.14 | 18.31 – 26.52 | 96.85% | 1713.41 | <0.001 |
| Advanced cancer | 12 | 18.83 | 9.66 – 33.48 | 98.52% | 742.04 | <0.001 | |
| Terminal or palliative stage | 18 | 41.64 | 30.05 – 54.24 | 97.73% | 748.94 | <0.001 | |
| Measures | SCID | 7 | 12.12 | 6.61 – 21.17 | 94.03% | 100.43 | <0.001 |
| CESD | 20 | 38.46 | 29.31 – 48.50 | 97.10% | 655.51 | <0.001 | |
| HADS | 31 | 18.79 | 13.65 – 25.28 | 96.74% | 920.30 | <0.001 | |
| BDI | 9 | 38.32 | 22.58 – 56.96 | 98.67% | 602.31 | <0.001 | |
| DASS-21 | 3 | 32.71 | 18.24 – 51.44 | 94.56% | 36.79 | <0.001 | |
| PHQ | 6 | 26.19 | 20.92 – 32.25 | 84.00% | 31.24 | <0.001 | |
| Other self-reported tools | 6 | 22.75 | 10.23 – 43.24 | 95.73% | 117.22 | <0.001 | |
| Self-reported diagnosis | 3 | 15.57 | 14.24 – 17.00 | 0.00% | 1.55 | 0.450 |
SCID, Structured Clinical Interview for DSM; CESD, Center of Epidemiological Studies Depression Scale; HADS, Hospital Anxiety and Depression Scale; BDI, Beck Depression Inventory; DASS-21, Depression Anxiety Stress Scale- 21-itens; PHQ, Patient Health Questionnaire. The “a” indicates the p-value stands the significant heterogeneity.
For the different measures, the pooled prevalence was 38.46% for the Center of Epidemiological Studies Depression Scale (CESD), 18.79% for the Hospital Anxiety and Depression Scale (HADS), 38.32% for the Beck Depression Inventory (BDI), and 32.71% for the Depression Anxiety Stress Scale (DASS-21). Further, 26.19% for the Patient Health Questionnaire (PHQ), 12.12% for the Structured Clinical Interview for DSM (SCID), 22.75% for other self-reported tools (i.e., other validated instruments for assessing depression), and 15.57% for self-reported diagnosis (i.e., the respondents' self-reports about whether they had been diagnosed with depression). Additionally, the pooled prevalence rate was significantly higher in studies using CESD (β = 1.514, p < 0.001) and BDI (β = 1.510, p = 0.002) than in SCID. In terms of caring for cancer patients, the depression prevalence was 22.14% for caring for patients with non-advanced cancer, 18.83% for caring for those with advanced cancer, and 41.64% for caring for those with terminal or palliative stage cancer. The depression prevalence was significantly lower in studies involving caregivers caring for non-advanced cancer (β = −0.930, p < 0.001) and advanced cancer (β = −1.107, p = 0.004) than in studies involving caregivers caring for terminal or palliative cancer stages.
Discussion
To the best of our knowledge, this is the first meta-analysis to examine geographical regions, caregiver characteristics, and patients' cancer stage as moderators of the depression prevalence among cancer patient caregivers. We extended previous studies on the depression prevalence in caregivers (6) to evaluate 85 prevalence rates based on studies from 25 countries from 2001 to 2021. Our primary findings showed that the pooled depression prevalence rate was 25.14% among cancer patient caregivers. Only one meta-analysis investigated the depression prevalence in cancer patient caregivers and found that the pooled depression prevalence was 42.30% (6). This difference could be because the previous meta-analysis did not use “prevalence” or “epidemiology” as keywords in the literature search stage. Instead, they included studies evaluating the depression prevalence based on self-reported measures with loosened cutoff points. Additionally, the current meta-analysis included almost three times as many studies and may have provided a more accurate prevalence estimate. Considering moderators for depression prevalence, the pooled prevalence rate estimated from the Eastern sample was significantly higher than that estimated in the Western sample. Furthermore, the depression prevalence rate was higher in studies involving caregivers caring for patients with terminal or palliative cancer than in studies involving caregivers caring for patients with non-advanced and advanced cancer. The current meta-analysis also revealed that the depression prevalence rates differed according to the measures used to assess it. In addition, the prevalence rates of depression significantly decreased with the mean age of caregivers and percentage of spousal caregivers.
The pooled prevalence of depression among caregivers found in the current meta-analysis was lower than that found in caregivers caring for other illnesses. For example, prevalence studies have shown that depressive symptoms in caregivers of older relatives are 40.2% for those caring for stroke survivors (104) and 34.0% for caregivers of people living with AD (15). Moreover, a meta-analysis examined the prevalence of depression among caregivers of individuals with dementia. They found that the pooled depression prevalence was 31.24% (17). Compared to the general adult population, several studies have directly compared the prevalence of depressive symptoms between caregivers and community-dwelling adults. For example, a UK study found that caregivers scored considerably higher for depression compared to the adult general population sample, with almost 25% of all caregivers being moderately, severely, or even highly severely depressed (7). Additionally, a meta-analysis evaluated the depression prevalence in communities in 30 countries between 1994 and 2014. They found that the depression prevalence among adults in the community was 12.9% (105). Further, it was lower than the pooled prevalence in the present study in the general population. This implies that caregivers experience more physical problems and psychological burdens. Our findings demonstrate that cancer patient caregivers may need long-lasting interventions compared to the general adult population.
The significantly high heterogeneity in depression prevalence can be explained by several moderators. First, geographic regions may account for the heterogeneity in the prevalence rates of depression. The pooled prevalence rate estimated from the Eastern sample was significantly higher than that estimated in the Western sample. Second, the heterogeneity was partially explained by the instruments used to measure depression, with studies using diagnostic interviews of depression yielding lower pooled prevalence estimates. Most of the studies included in the current meta-analysis used self-report tools to estimate the prevalence of depression. Mental health care specialists should keep in mind that the prevalence rates of depression among caregivers may depend highly on the assessment tools they used. This is also consistent with the findings from previous meta-analyses focused on the depression prevalence among caregivers (6, 17). The discrepancy in depression prevalence rates evaluated from studies using self-report instruments and from studies using diagnostic interviews should be considered by mental health professionals working with caregivers. Additionally, heterogeneity was explained by the patients' cancer stage. The prevalence rate of depression was higher among studies involving caregivers caring for patients with terminal or palliative cancer than those involving caregivers caring for patients with non-advanced and advanced cancer.
The current meta-analysis showed that caregivers in Eastern countries had a higher depression prevalence than caregivers in Western countries. Such cultural discrepancies were not examined in any previous meta-analysis of cancer patient caregivers. Further, a previous study found that cancer patient caregivers in Asia reported a significantly lower quality of life than caregivers in Western countries (106). They suggested that this may have been influenced by filial piety and obligatory care. A study investigating the caregiving burden among Asian caregivers of dementia patients identified a unique dimension described as “worry about caregiving performance” (107). When caring for patients with cancer, it is essential to recognize that caregivers' cultural roots or social norms may determine their beliefs about caring for them and the burden they received. Considering the relationship between caregivers and patients, we found that the prevalence of depression decreased as the percentage of spousal caregivers increased. A previous study also found that adult–child caregivers reported higher scores on the depression scale than spousal caregivers (108). Other studies also found low levels of depression among spousal caregivers of cancer patients (109, 110). Additionally, spousal caregivers reported feelings of loneliness and loss (111). Non-spousal caregivers reported a higher depression and perceived burden rate than other caregivers. Nevertheless, this finding could have been attributed to sex and cultural differences (112).
In line with previous meta-analyses examining depression prevalence among caregivers (6, 16, 17), the current meta-analysis found that the depression prevalence rates differed according to the measures used to assess depression. In this study, studies using SCID reported a significantly lower prevalence of depression than those using the CESD and BDI. In addition, consistent with our findings, a previous meta-analysis of caregivers of cancer patients also found that the prevalence of depression evaluated with diagnostic interviews yielded the lowest pooled prevalence estimate (6). Another meta-analysis revealed that the depression prevalence estimates differed according to the measures used. They found that two studies that used diagnostic criteria reported the lowest prevalence rate, and those using the BDI reported the highest prevalence estimate (17). Divergent prevalence rates were discovered in caregivers and the general population. A meta-analysis examined the depression prevalence in community samples and found that most studies using self-report instruments were significantly higher than those using interview-based assessment tools (105). The differences in the assessment tools could explain the heterogeneous prevalence rates for depression and the cutoffs used.
Our results revealed that depression among cancer patient caregivers is highest in studies with caregivers of patients with terminal cancer or the palliative stage, compared to those caring for non-advanced or advanced cancer. Several empirical studies have found that the patients' cancer stage is associated with depressive symptoms and quality of life among caregivers (62, 63, 106). The impending death of a close family is not unexpected (113). As caregivers often have to deal with role changes and new caregiving tasks, they can experience caregiver burden, which has been shown to influence depression (114). Recently, a systematic review investigated the associations between pre-loss grief and post-loss adjustment among caregivers of patients with terminal cancer. They found that high levels of pre-loss grief and low levels of perceived preparedness for death were associated with prolonged grief and more depressive symptoms (115). In the terminal or palliative stage, the depressive symptoms of caregivers may overlap with anticipatory grief and move from curing the patient's illness toward facing the patient's death soon.
Several methodological limitations should be noted. First, some factors were not reported in sufficient detail to be included as moderators, such as duration of caregiving and time since diagnosis. Future studies should consider the impact of such factors that may affect the prevalence of depression. Second, our search strategy may have also neglected some studies that reported the proportion of depression but did not use the word “prevalence” or “epidemiology” in the abstract. These strategies may avoid enhancing heterogeneity but may also omit potential prevalence data. Third, although the current study tried to use a rigorous database searching strategy, which is essential for systematic review, it may still have ignored potential studies which only include other alternative terms. Furthermore, future meta-analyses focused on caregivers of cancer patients and other mental health conditions are also urgently needed.
In conclusion, the prevalence of depression among caregivers of patients with cancer varied with the age of the caregivers and the percentage of spousal caregivers. The prevalence rates were also moderated by geographic region, patients' cancer stage, and measures for depression. This meta-analysis revealed that almost one-fourth of the caregivers of cancer patients experience depression. This highlights that psychological support may be necessary for cancer patients and their caregivers. Several sociodemographic and care-related risk factors impact caregivers' mental burden and quality of life. Therefore, it is crucial to move forward from a patient-centered approach to a family-centered approach to reduce the burden on family caregivers when facing the imminent death of a family member and prevent the deterioration of depressive symptoms.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author Contributions
Y-SL and Y-CP contributed to conception, design of the study, and organized the database. Y-CP performed the statistical analysis and wrote the first draft of the manuscript. Both authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This study was supported by grants from the Ministry of Science and Technology, Taiwan (MOST 107-2410-H-002-119-MY3).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Ms. Si-Yu Chen for providing excellent technical assistance.
References
- 1.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? a meta-analysis. Psychological Bulletin. (2003) 129:946–72. 10.1037/0033-2909.129.6.946 [DOI] [PubMed] [Google Scholar]
- 2.Song JI, Shin DW, Choi JY, Kang J, Baik YJ, Mo H, et al. Quality of life and mental health in family caregivers of patients with terminal cancer. Support Care Cancer. (2011) 19:1519–26. 10.1007/s00520-010-0977-8 [DOI] [PubMed] [Google Scholar]
- 3.Hudson P, Payne S. Family caregivers and palliative care: current status and agenda for the future. J Palliat Med. (2011) 14:864–9. 10.1089/jpm.2010.0413 [DOI] [PubMed] [Google Scholar]
- 4.Oechsle K, Ullrich A, Marx G, Benze G, Wowretzko F, Zhang Y, et al. Prevalence and predictors of distress, anxiety, depression, and quality of life in bereaved family caregivers of patients with advanced cancer. Am J Hosp Palliat Care. (2020) 37:201–13. 10.1177/1049909119872755 [DOI] [PubMed] [Google Scholar]
- 5.Fasse L, Flahault C, Brédart A, Dolbeault S, Sultan Describing S. Describing and understanding depression in spouses of cancer patients in palliative phase. Psycho-oncol. (2015) 24:1131–7. 10.1002/pon.3777 [DOI] [PubMed] [Google Scholar]
- 6.Geng HM, Chuang DM, Yang F, Yang Y, Liu WM, Liu LH, et al. Prevalence and determinants of depression in caregivers of cancer patients: a systematic review and meta-analysis. Medicine. (2018) 97:e11863. 10.1097/MD.0000000000011863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurtz ME, Kurtz JC, Given CW, Given BA. Depression and physical health among family caregivers of geriatric patients with cancer—a longitudinal view. Med Sci Monit. (2004) 10:Cr447–56. [PubMed] [Google Scholar]
- 8.van Warmerdam J, Zabih V, Kurdyak P, Sutradhar R, Nathan PC, Gupta S. Prevalence of anxiety, depression, and post–traumatic stress disorder in parents of children with cancer: a meta-analysis. Pediatr blood and cancer. (2019) 66:e27677. 10.1002/pbc.27677 [DOI] [PubMed] [Google Scholar]
- 9.Nielsen MK, Neergaard MA, Jensen AB, Vedsted P, Bro F, Guldin MB. Preloss grief in family caregivers during end–of–life cancer care: a nationwide population–based cohort study. Psycho-oncol. (2017) 26:2048–56. 10.1002/pon.4416 [DOI] [PubMed] [Google Scholar]
- 10.Park B, Kim SY, Shin J–Y, Sanson–Fisher RW, Shin DW, Cho J, et al. Prevalence and predictors of anxiety and depression among family caregivers of cancer patients: a nationwide survey of patient–family caregiver dyads in korea. Suppor Care Cancer. (2013) 21:2799–807. 10.1007/s00520-013-1852-1 [DOI] [PubMed] [Google Scholar]
- 11.Cameron JI, Franche RL, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. (2002) 94:521–7. 10.1002/cncr.10212 [DOI] [PubMed] [Google Scholar]
- 12.Given B, Wyatt G, Given C, Sherwood P, Gift A, DeVoss D, et al. Burden and depression among caregivers of patients with cancer at the end of life. Oncol Nurs Forum. (2004) 31:1105–17. 10.1188/04.ONF.1105-1117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. (2004) 170:1795–801. 10.1503/cmaj.1031205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sahadevan S, Namboodiri V. Depression in caregivers of patients with breast cancer: a cross–sectional study from a cancer research center in south india. Indian J Psychiatry. (2019) 61:277–82. 10.4103/psychiatry.IndianJPsychiatry_46_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sallim AB, Sayampanathan AA, Cuttilan A, Ho R. Prevalence of mental health disorders among caregivers of patients with alzheimer disease. J Am Med Dir Assoc. (2015) 16:1034–41. 10.1016/j.jamda.2015.09.007 [DOI] [PubMed] [Google Scholar]
- 16.del–Pino–Casado R, Rodríguez Cardosa M, López–Martínez C, Orgeta V. The association between subjective caregiver burden and depressive symptoms in carers of older relatives: a systematic review and meta-analysis. PLoS ONE. (2019) 14:e0217648. 10.1371/journal.pone.0217648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collins RN, Kishita N. Prevalence of depression and burden among informal care–givers of people with dementia: a meta-analysis. Ageing Soc. (2020) 40:2355–92. 10.1017/S0144686X19000527 [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the pRISMA statement. PLoS Med. (2009) 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kossmeier M, Tran US, Voracek M. Visual inference for the funnel plot in meta-analysis. Zeitschrift für Psychologie. (2019) 227:83–9. 10.1027/2151-2604/a000358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Viechtbauer W. Conducting meta-Analyses in r with the metafor package. J Stat Softw. (2010) 36:1–48. 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 21.Huedo–Medina TB, Sanchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: q statistic or i2 index? Psychol methods. (2006) 11:193–206. 10.1037/1082-989X.11.2.193 [DOI] [PubMed] [Google Scholar]
- 22.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 23.Applebaum AJ, Polacek LC, Walsh L, Reiner AS, Lynch K, Benvengo S, et al. The unique burden of rare cancer caregiving: caregivers of patients with erdheim-chester disease. Leuk Lymphoma. (2020) 61:1406–17. 10.1080/10428194.2020.1719090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Areia NP, Fonseca G, Major S, Relvas AP. Psychological morbidity in family caregivers of people living with terminal cancer: prevalence and predictors. Palliat Support Care. (2019) 17:286–93. 10.1017/S1478951518000044 [DOI] [PubMed] [Google Scholar]
- 25.Baudry AS, Vanlemmens L, Anota A, Cortot A, Piessen G, Christophe V. Profiles of caregivers most at risk of having unmet supportive care needs: recommendations for healthcare professionals in oncology. Eur J Oncol Nurs. (2019) 43:101669. 10.1016/j.ejon.2019.09.010 [DOI] [PubMed] [Google Scholar]
- 26.Bonafede M, Granieri A, Binazzi A, Mensi C, Grosso F, Santoro G, et al. Psychological distress after a diagnosis of malignant mesothelioma in a group of patients and caregivers at the national priority contaminated site of casale monferrato. Int J Environ Res Public Health. (2020) 17:4353. 10.3390/ijerph17124353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bradley EH, Prigerson H, Carlson MD, Cherlin E. Johnson-Hurzeler R, Kasl SV. Depression among surviving caregivers: does length of hospice enrollment matter? Am J Psychiatry. (2004) 161:2257–62. 10.1176/appi.ajp.161.12.2257 [DOI] [PubMed] [Google Scholar]
- 28.Burns MA, Aralova M, Ellis SJ, Aslanyan KS, Egorkina T, Wakefield CE. Pediatric Psycho-oncol in russia: caregiver mental health and sleep outcomes on the oncology wards. Psycho-oncol. (2021) 30:185–93. 10.1002/pon.5547 [DOI] [PubMed] [Google Scholar]
- 29.Carey M, Sanson–Fisher R, Paul C, Bradstock K, Williamson A, Campbell HS. Psychological morbidity among australian rural and urban support persons of haematological cancer survivors: results of a national study. Psycho-oncol. (2017) 26:1952–8. 10.1002/pon.4411 [DOI] [PubMed] [Google Scholar]
- 30.Corà A, Partinico M, Munafò M, Palomba D. Health risk factors in caregivers of terminal cancer patients: a pilot study. Cancer Nurs. (2012) 35:38–47. 10.1097/NCC.0b013e31820d0c23 [DOI] [PubMed] [Google Scholar]
- 31.Costa–Requena G, Cristófol R, Cañete J. Caregivers' morbidity in palliative care unit: predicting by gender, age, burden and self–esteem. Support Care Cancer. (2012) 20:1465–70. 10.1007/s00520-011-1233-6 [DOI] [PubMed] [Google Scholar]
- 32.Doubova SV. Infante–Castañeda C. Factors associated with quality of life of caregivers of mexican cancer patients. Qual Life Res. (2016) 25:2931–40. 10.1007/s11136-016-1322-6 [DOI] [PubMed] [Google Scholar]
- 33.Duckworth KE, McQuellon RP, Russell GB, Perry KC, Nightingale C, Shen P, et al. Caregiver quality of life before and after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Am Coll Surg. (2020) 230:679–87. 10.1016/j.jamcollsurg.2019.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fancourt D, Warran K, Finn S, Wiseman T. Psychosocial singing interventions for the mental health and well–being of family carers of patients with cancer: results from a longitudinal controlled study. BMJ Open. (2019) 9:e026995. 10.1136/bmjopen-2018-026995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fenix JB, Cherlin EJ, Prigerson HG, Johnson–Hurzeler R, Kasl SV, Bradley EH. Religiousness and major depression among bereaved family caregivers: a 13–month follow–up study. J Palliat Care. (2006) 22:286–92. 10.1177/082585970602200406 [DOI] [PubMed] [Google Scholar]
- 36.Fletcher BS, Paul SM, Dodd MJ, Schumacher K, West C, Cooper B, et al. Prevalence, severity, and impact of symptoms on female family caregivers of patients at the initiation of radiation therapy for prostate cancer. J Clin Oncol. (2008) 26:599–605. 10.1200/JCO.2007.12.2838 [DOI] [PubMed] [Google Scholar]
- 37.Goren A, Gilloteau I, Lees M, DaCosta Dibonaventura M. Quantifying the burden of informal caregiving for patients with cancer in europe. Support Care Cancer. (2014) 22:1637–46. 10.1007/s00520-014-2122-6 [DOI] [PubMed] [Google Scholar]
- 38.Gough K, Hudson P. Psychometric properties of the hospital anxiety and depression scale in family caregivers of palliative care patients. J Pain Symptom Manage. (2009) 37:797–806. 10.1016/j.jpainsymman.2008.04.012 [DOI] [PubMed] [Google Scholar]
- 39.Grov EK, Dahl AA, Moum T, Fosså SD. Anxiety, depression, and quality of life in caregivers of patients with cancer in late palliative phase. Ann Oncol. (2005) 16:1185–91. 10.1093/annonc/mdi210 [DOI] [PubMed] [Google Scholar]
- 40.Gupta V, Raj M, Hoodin F, Yahng L, Braun T, Choi SW. Electronic health record portal use by family caregivers of patients undergoing hematopoietic cell transplantation: united states national survey study. JMIR cancer. (2021) 7:e26509. 10.2196/26509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haj Mohammad N, Walter AW, van Oijen MG, Hulshof MC, Bergman JJ, Anderegg MC, et al. Burden of spousal caregivers of stage iI and iII esophageal cancer survivors 3 years after treatment with curative intent. Support Care Cancer. (2015) 23:3589–98. 10.1007/s00520-015-2727-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haley WE, LaMonde LA, Han B, Narramore S, Schonwetter R. Family caregiving in hospice: effects on psychological and health functioning among spousal caregivers of hospice patients with lung cancer or dementia. J Hosp. (2001) 15:1–18. 10.1300/J011v15n04_01 [DOI] [PubMed] [Google Scholar]
- 43.Han Y, Yuan J, Luo Z, Zhao J, Wu J, Liu R, et al. Determinants of hopelessness and depression among chinese hospitalized esophageal cancer patients and their family caregivers. Psycho-oncol. (2013) 22:2529–36. 10.1002/pon.3315 [DOI] [PubMed] [Google Scholar]
- 44.Haun MW, Sklenarova H, Brechtel A, Herzog W, Hartmann M. Distress in cancer patients and their caregivers and association with the caregivers' perception of dyadic communication. Oncol Res Treat. (2014) 37:384–8. 10.1159/000364885 [DOI] [PubMed] [Google Scholar]
- 45.He Y, Sun LY, Peng KW, Luo MJ, Deng L, Tang T, et al. Sleep quality, anxiety and depression in advanced lung cancer: patients and caregivers. BMJ Support Palliat Care. (2020) 10.1136/bmjspcare-2018-001684 [DOI] [Google Scholar]
- 46.Heckel L, Fennell KM, Reynolds J, Osborne RH, Chirgwin J, Botti M, et al. Unmet needs and depression among carers of people newly diagnosed with cancer. Eur J Cancer. (2015) 51:2049–57. 10.1016/j.ejca.2015.06.129 [DOI] [PubMed] [Google Scholar]
- 47.Hyde MK, Legg M, Occhipinti S, Lepore SJ, Ugalde A, Zajdlewicz L, et al. Predictors of long–term distress in female partners of men diagnosed with prostate cancer. Psycho-oncol. (2018) 27:946–54. 10.1002/pon.4617 [DOI] [PubMed] [Google Scholar]
- 48.Jamani K, Onstad LE, Bar M, Carpenter PA, Krakow EF, Salit RB, et al. Quality of life of caregivers of hematopoietic cell transplant recipients. Biol Blood Marrow Transplant. (2018) 24:2271–6. 10.1016/j.bbmt.2018.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Janda M, Neale RE, Klein K, O'Connell DL, Gooden H, Goldstein D, et al. Anxiety, depression and quality of life in people with pancreatic cancer and their carers. Pancreatol. (2017) 17:321–7. 10.1016/j.pan.2017.01.008 [DOI] [PubMed] [Google Scholar]
- 50.Janda M, Steginga S, Dunn J, Langbecker D, Walker D, Eakin E. Unmet supportive care needs and interest in services among patients with a brain tumour and their carers. Patient Educ Couns. (2008) 71:251–8. 10.1016/j.pec.2008.01.020 [DOI] [PubMed] [Google Scholar]
- 51.Jassem J, Penrod JR, Goren A, Gilloteau I. Caring for relatives with lung cancer in europe: an evaluation of caregivers' experience. Quality of Life Research. (2015) 24:2843–52. 10.1007/s11136-015-1028-1 [DOI] [PubMed] [Google Scholar]
- 52.Kang E, Keam B, Lee NR, Kang JH, Kim YJ, Shim HJ, et al. Impact of family caregivers' awareness of the prognosis on their quality of life/depression and those of patients with advanced cancer: a prospective cohort study. Support Care Cancer. (2021) 29:397–407. 10.1007/s00520-020-05489-8 [DOI] [PubMed] [Google Scholar]
- 53.Katende G, Nakimera Prevalence L. and correlates of anxiety and depression among family carers of cancer patients in a cancer care and treatment facility in Uganda: a cross–sectional study. Afr Health Sci. (2017) 17:868–76. 10.4314/ahs.v17i3.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kehoe LA, Xu H, Duberstein P, Loh KP, Culakova E, Canin B, et al. Quality of life of caregivers of older patients with advanced cancer. J Am Geriatr Soc. (2019) 67:969–77. 10.1111/jgs.15862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim D, Lee Y, Lee J, Nam JK, Chung Y. Development of korean smartphone addiction proneness scale for youth. PLoS ONE. (2014)9:e97920. 10.1371/journal.pone.0097920 [DOI] [Google Scholar]
- 56.Kim Y, Carver CS, Deci EL, Kasser T. Adult attachment and psychological well–being in cancer caregivers: the mediational role of spouses' motives for caregiving. Health Psychol. (2008) 27:S144–54. 10.1037/0278-6133.27.2(Suppl.).S144 [DOI] [PubMed] [Google Scholar]
- 57.Kim Y, Duberstein PR, Sörensen S, Larson MR. Levels of depressive symptoms in spouses of people with lung cancer: effects of personality, social support, caregiving burden. Psychosomatics. (2005) 46:123–30. 10.1176/appi.psy.46.2.123 [DOI] [PubMed] [Google Scholar]
- 58.Kleijn G, Lissenberg–Witte BI, Bohlmeijer ET, Willemsen V, Becker–Commissaris A, Eeltink CM, et al. A randomized controlled trial on the efficacy of life review therapy targeting incurably ill cancer patients: do their informal caregivers benefit? Support Care Cancer. (2021) 29:1257–64. 10.1007/s00520-020-05592-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Krähenbühl A, Zwahlen D, Knuth A, Schnyder U, Jenewein J, Kuhn C, et al. [Prevalence of anxiety and depression in cancer outpatients and their spouses]. Praxis. (2007) 96:973–9. 10.1024/1661-8157.96.24.973 [DOI] [PubMed] [Google Scholar]
- 60.Lambert SD, Girgis A, Lecathelinais C, Stacey F. Walking a mile in their shoes: anxiety and depression among partners and caregivers of cancer survivors at 6 and 12 months post–diagnosis. Support Care Cancer. (2013) 21:75–85. 10.1007/s00520-012-1495-7 [DOI] [PubMed] [Google Scholar]
- 61.Langenberg S, Reyners AKL, Wymenga ANM, Sieling GCM, Veldhoven CMM, van Herpen CML, et al. Caregivers of patients receiving long–term treatment with a tyrosine kinase inhibitor (TKI) for gastrointestinal stromal tumour (GIST): a cross–sectional assessment of their distress and burden. Acta Oncol. (2019) 58:191–9. 10.1080/0284186X.2018.1518592 [DOI] [PubMed] [Google Scholar]
- 62.Lee CY, Lee Y, Wang LJ, Chien CY, Fang FM, Lin PY. Depression, anxiety, quality of life, and predictors of depressive disorders in caregivers of patients with head and neck cancer: a 6–month follow–up study. J Psychosom Res. (2017) 100:29–34. 10.1016/j.jpsychores.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 63.Lee YH, Liao YC, Liao WY, Shun SC, Liu YC, Chan JC, et al. Anxiety, depression and related factors in family caregivers of newly diagnosed lung cancer patients before first treatment. Psycho-oncol. (2013) 22:2617–23. 10.1002/pon.3328 [DOI] [PubMed] [Google Scholar]
- 64.Leroy T, Fournier E, Penel N, Christophe V. Crossed views of burden and emotional distress of cancer patients and family caregivers during palliative care. Psycho-oncol. (2016) 25:1278–85. 10.1002/pon.4056 [DOI] [PubMed] [Google Scholar]
- 65.Lin Y, Hu C, Xu Y, Zhao J, Li Q. The mutual impact and moderating factors of quality of life between advanced cancer patients and their family caregivers. Support Care Cancer. (2020) 28:5251–62. 10.1007/s00520-020-05351-x [DOI] [PubMed] [Google Scholar]
- 66.Ling SF, Chen ML, Li CY, Chang WC, Shen WC, Tang ST. Trajectory and influencing factors of depressive symptoms in family caregivers before and after the death of terminally ill patients with cancer. Oncol Nurs Forum. (2013) 40:E32–40. 10.1188/13.ONF.E32-E40 [DOI] [PubMed] [Google Scholar]
- 67.Lutfi NM, Al Lami F. Prevalence and determinants of depression among caregivers of children with leukaemia in Iraq. EMHJ. (2019) 25:385–93. 10.26719/emhj.19.005 [DOI] [PubMed] [Google Scholar]
- 68.Malpert AV, Kimberg C, Luxton J, Mullins LL, Pui CH, Hudson MM, et al. Emotional distress in parents of long–term survivors of childhood acute lymphoblastic leukemia. Psycho-oncol. (2015) 24:1116–23. 10.1002/pon.3732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mazanec SR, Miano S, Baer L, Campagnaro EL, Sattar A, Daly BJ, et al. family–centered intervention for the transition to living with multiple myeloma as a chronic illness: a pilot study. Appl Nurs Res. (2017) 35:86–9. 10.1016/j.apnr.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 70.Mazzotti E, Sebastiani C, Antonini Cappellini GC, Marchetti P. Predictors of mood disorders in cancer patients' caregivers. Support Care Cancer. (2013) 21:643–7. 10.1007/s00520-012-1663-9 [DOI] [PubMed] [Google Scholar]
- 71.Mekonnen H, Gebreyohannis GT, Cherie Depression A. and associated factors among parents of children diagnosed with cancer at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Psycho-oncol. (2020) 29:1141–7. 10.1002/pon.5389 [DOI] [PubMed] [Google Scholar]
- 72.Moser MT, Künzler A, Nussbeck F, Bargetzi M, Znoj HJ. Higher emotional distress in female partners of cancer patients: prevalence and patient–partner interdependencies in a 3–year cohort. Psycho-oncol. (2013) 22:2693–701. 10.1002/pon.3331 [DOI] [PubMed] [Google Scholar]
- 73.Nik Jaafar NR, Selamat Din SH, Mohamed Saini S, Ahmad SN, Midin M, Sidi H, et al. Clinical depression while caring for loved ones with breast cancer. Compr Psychiatry. (2014) 55(Suppl. 1):S52–9. 10.1016/j.comppsych.2013.03.003 [DOI] [PubMed] [Google Scholar]
- 74.Oberoi DV, White V, Jefford M, Giles GG, Bolton D, Davis I, et al. Caregivers' information needs and their ‘experiences of care' during treatment are associated with elevated anxiety and depression: a cross–sectional study of the caregivers of renal cancer survivors. Support Care Cancer. (2016) 24:4177–86. 10.1007/s00520-016-3245-8 [DOI] [PubMed] [Google Scholar]
- 75.Oechsle K, Ullrich A, Marx G, Benze G, Heine J, Dickel LM, et al. Psychological burden in family caregivers of patients with advanced cancer at initiation of specialist inpatient palliative care. BMC Palliat Care. (2019) 18:102. 10.1186/s12904-019-0469-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Oechsle K, Goerth K, Bokemeyer C, Mehnert Anxiety A. and depression in caregivers of terminally ill cancer patients: impact on their perspective of the patients' symptom burden. J Palliat Med. (2013) 16:1095–101. 10.1089/jpm.2013.0038 [DOI] [PubMed] [Google Scholar]
- 77.Papastavrou E, Charalambous A, Tsangari H. Exploring the other side of cancer care: the informal caregiver. Eur J Oncol Nurs. (2009) 13:128–36. 10.1016/j.ejon.2009.02.003 [DOI] [PubMed] [Google Scholar]
- 78.Park YY, Jeong YJ, Lee J, Moon N, Bang I, Kim H, et al. The influence of family adaptability and cohesion on anxiety and depression of terminally ill cancer patients. Support Care Cancer. (2018) 26:313–21. 10.1007/s00520-017-3912-4 [DOI] [PubMed] [Google Scholar]
- 79.Pawl JD, Lee SY, Clark PC, Sherwood PR. Sleep loss and its effects on health of family caregivers of individuals with primary malignant brain tumors. Res Nurs Health. (2013) 36:386–99. 10.1002/nur.21545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Price MA, Butow PN, Costa DS, King MT, Aldridge LJ, Fardell JE, et al. Prevalence and predictors of anxiety and depression in women with invasive ovarian cancer and their caregivers. Med J Aust. (2010) 193:S52–7. 10.5694/j.1326-5377.2010.tb03929.x [DOI] [PubMed] [Google Scholar]
- 81.Rhee YS, Yun YH, Park S, Shin DO, Lee KM, Yoo HJ, et al. Depression in family caregivers of cancer patients: the feeling of burden as a predictor of depression. J Clin Oncol. (2008) 26:5890–5. 10.1200/JCO.2007.15.3957 [DOI] [PubMed] [Google Scholar]
- 82.Rumpold T, Schur S, Amering M, Ebert–Vogel A, Kirchheiner K, Masel E, et al. Hope as determinant for psychiatric morbidity in family caregivers of advanced cancer patients. Psycho-oncol. (2017) 26:672–8. 10.1002/pon.4205 [DOI] [PubMed] [Google Scholar]
- 83.Rumpold T, Schur S, Amering M, Kirchheiner K, Masel EK, Watzke H, et al. Informal caregivers of advanced–stage cancer patients: every second is at risk for psychiatric morbidity. Support Care Cancer. (2016) 24:1975–82. 10.1007/s00520-015-2987-z [DOI] [PubMed] [Google Scholar]
- 84.Sacher M, Meixensberger J, Krupp W. Interaction of quality of life, mood and depression of patients and their informal caregivers after surgical treatment of high–grade glioma: a prospective study. J Neuro-oncol. (2018) 140:367–75. 10.1007/s11060-018-2962-x [DOI] [PubMed] [Google Scholar]
- 85.Schellekens MPJ, van den Hurk DGM, Prins JB, Molema J, van der Drift MA, Speckens AEM. The suitability of the hospital anxiety and depression scale, distress thermometer and other instruments to screen for psychiatric disorders in both lung cancer patients and their partners. J Affect Disord. (2016) 203:176–83. 10.1016/j.jad.2016.05.044 [DOI] [PubMed] [Google Scholar]
- 86.Shaffer KM, Kim Y, Carver CS, Cannady RS. Effects of caregiving status and changes in depressive symptoms on development of physical morbidity among long–term cancer caregivers. Health Psychol. (2017) 36:770–8. 10.1037/hea0000528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Simpson GK. Dall'Armi L, Roydhouse JK, Forstner D, Daher M, Simpson T, et al. Does resilience mediate carer distress after head and neck cancer? Cancer Nurs. (2015) 38:E30–6. 10.1097/NCC.0000000000000229 [DOI] [PubMed] [Google Scholar]
- 88.Stenberg U, Cvancarova M, Ekstedt M, Olsson M, Ruland C. Family caregivers of cancer patients: perceived burden and symptoms during the early phases of cancer treatment. Soc Work Health Care. (2014) 53:289–309. 10.1080/00981389.2013.873518 [DOI] [PubMed] [Google Scholar]
- 89.Sterba KR, Zapka J, Armeson KE, Shirai K, Buchanan A, Day TA, et al. Physical and emotional well–being and support in newly diagnosed head and neck cancer patient–caregiver dyads. J Psychosoc Oncol. (2017) 35:646–65. 10.1080/07347332.2017.1323817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stieb S, Fischbeck S, Wagner W, Appels J, Wiewrodt D. High psychosocial burden in relatives of malignant brain tumor patients. Clin Neurol Neurosurg. (2018) 170:1–6. 10.1016/j.clineuro.2018.04.023 [DOI] [PubMed] [Google Scholar]
- 91.Tang ST, Hsieh CH, Chou WC, Chang WC, Chen JS, Wen FH. Course of changes in emotional preparedness for death and its associations with caregiving outcomes for family caregivers of terminally ill cancer patients over their last year of life. J Pain Symptom Manage. (2021) 61:974–82. 10.1016/j.jpainsymman.2020.09.033 [DOI] [PubMed] [Google Scholar]
- 92.Tang ST, Chang WC, Chen JS, Wang HM, Shen WC Li CY, et al. Course and predictors of depressive symptoms among family caregivers of terminally ill cancer patients until their death. Psycho-oncol. (2013) 22:1312–8. 10.1002/pon.3141 [DOI] [PubMed] [Google Scholar]
- 93.Toledano–Toledano F, Luna D, Moral de la Rubia J, Martínez Valverde S, Bermúdez Morón CA, Salazar García M, et al. Psychosocial factors predicting resilience in family caregivers of children with cancer: a cross–sectional study. Int J Environ Res Public Health. (2021) 18:748. 10.3390/ijerph18020748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Trevino KM, Prigerson HG, Maciejewski PK. Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder. Psycho-oncol. (2018) 27:243–9. 10.1002/pon.4441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vanderwerker LC, Laff RE, Kadan–Lottick NS, McColl S, Prigerson HG. Psychiatric disorders and mental health service use among caregivers of advanced cancer patients. J Clin Oncol. (2005) 23:6899–907. 10.1200/JCO.2005.01.370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Virtue SM, Manne SL, Mee L, Bartell A, Sands S, Gajda TM, et al. Psychological distress and psychiatric diagnoses among primary caregivers of children undergoing hematopoietic stem cell transplant: an examination of prevalence, correlates, racial/ethnic differences. Gen Hosp Psychiatry. (2014) 36:620–6. 10.1016/j.genhosppsych.2014.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Waldman LP, Nelson AM, Jacobs JM, Gray TF, Clay M, Jagielo AD, et al. Anxiety and depression symptoms in caregivers prior to hematopoietic stem cell transplantation (HCT). Cell Ther Transplant. (2021) 27:517.e1–5. 10.1016/j.jtct.2021.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang LJ, Zhong WX Ji XD, Chen J. Depression, caregiver burden and social support among caregivers of retinoblastoma patients in china. Int J Nurs Pract. (2016) 22:478–85. 10.1111/ijn.12458 [DOI] [PubMed] [Google Scholar]
- 99.Wen FH, Chou WC, Hou MM, Su PJ, Shen WC, Chen JS, et al. Depressive–symptom trajectories from end–of–life caregiving through the first 2 bereavement years for family caregivers of advanced cancer patients. J Pain Symptom Manage. (2021) 2021:272–4. 10.1016/j.jpainsymman.2021.03.018 [DOI] [PubMed] [Google Scholar]
- 100.Williams AL, Dixon J, Feinn R, McCorkle R. Cancer family caregiver depression: are religion–related variables important? Psycho-oncol. (2015) 24:825–31. 10.1002/pon.3647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yang M, Ma F, Lan B, Cai J, Sun X, Xu B. Validity of distress thermometer for screening of anxiety and depression in family caregivers of chinese breast cancer patients receiving postoperative chemotherapy. Chin J Cancer Res. (2020) 32:476–84. 10.21147/j.issn.1000-9604.2020.04.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yang X, Wang L, He J, Ge C, Chang Y, Fu J, et al. Factors related to depressive symptoms among chinese caregivers of cancer patients. Psycho-oncol. (2012) 21:1063–70. 10.1002/pon.1999 [DOI] [PubMed] [Google Scholar]
- 103.Yu H, Li L, Liu C, Huang W, Zhou J, Fu W, et al. Factors associated with the quality of life of family caregivers for leukemia patients in china. Health Qual Life Outcomes. (2017) 15:55. 10.1186/s12955-017-0628-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Loh AZ, Tan JS, Zhang MW, Ho RC. The global prevalence of anxiety and depressive symptoms among caregivers of stroke survivors. J Am Med Dir Assoc. (2017) 18:111–6. 10.1016/j.jamda.2016.08.014 [DOI] [PubMed] [Google Scholar]
- 105.Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. (2018) 8:2861. 10.1038/s41598-018-21243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lim HA, Tan JY, Chua J, Yoong RK, Lim SE, Kua EH, et al. Quality of life of family caregivers of cancer patients in singapore and globally. Singapore Med J. (2017) 58:258–61. 10.11622/smedj.2016083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lim WS, Cheah WK, Ali N, Han HC, Anthony PV, Chan M, et al. Worry about performance: a unique dimension of caregiver burden. Int Psychogeriat. (2014) 26:677–86. 10.1017/S1041610213002445 [DOI] [PubMed] [Google Scholar]
- 108.Jones SB, Whitford HS, Bond MJ. Burden on informal caregivers of elderly cancer survivors: risk versus resilience. J Psychosoc Oncol. (2015) 33:178–98. 10.1080/07347332.2014.1002657 [DOI] [PubMed] [Google Scholar]
- 109.Goldzweig G, Baider L, Andritsch E, Pfeffer R, Rottenberg Y. A dialogue of depression and hope: elderly patients diagnosed with cancer and their spousal caregivers. JCE. (2017) 32:549–55. 10.1007/s13187-015-0975-0 [DOI] [PubMed] [Google Scholar]
- 110.Bachner YG, Karus DG, Raveis VH. Examining the social context in the caregiving experience: correlates of global self–esteem among adult daughter caregivers to an older parent with cancer. J Aging Health. (2009) 21:1016–39. 10.1177/0898264309344320 [DOI] [PubMed] [Google Scholar]
- 111.Beeson R, Loneliness A. and depression in spousal caregivers of those with Alzheimer's disease versus non–caregiving spouses. Arch Psychiatr Nurs. (2003) 17:135–43. 10.1016/S0883-9417(03)00057-8 [DOI] [PubMed] [Google Scholar]
- 112.Pinquart M, Sörensen S. Ethnic differences in stressors, resources, and psychological outcomes of family caregiving: a meta-analysis. Gerontologist. (2005) 45:90–106. 10.1093/geront/45.1.90 [DOI] [PubMed] [Google Scholar]
- 113.Caserta MS, Utz RL, Lund DA. Spousal bereavement following cancer death. Illn, Crisis Loss. (2013) 21:185–202. 10.2190/IL.21.3.b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Heckel L, Fennell KM, Reynolds J, Boltong A, Botti M, Osborne RH, et al. Efficacy of a telephone outcall program to reduce caregiver burden among caregivers of cancer patients [PROTECT]: a randomised controlled trial. BMC Cancer. (2018) 18:59. 10.1186/s12885-017-3961-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Treml J, Schmidt V, Nagl M, Kersting A. Pre–loss grief and preparedness for death among caregivers of terminally ill cancer patients: a systematic review. Soc Sci Med. (2021) 284:114240. 10.1016/j.socscimed.2021.114240 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.