Abstract
Introduction. Musculoskeletal disorders (MSD) remain a substantial burden to society and to workplaces worldwide. Evidence-based practice approaches may be helpful; however, current research evidence is not consistently strong. Workplaces must address MSD regardless of the state of the research evidence. The study objective was to describe workplace MSD prevention practices experiences and perspectives of workers, managers, and occupational health and safety practitioners. Methods. This descriptive study used a convenience sample from Newfoundland and Labrador workplaces. Data were collected via survey and interviews. The survey data was analyzed using descriptive statistics and the interview data was analyzed using thematic analysis. Results. Results were examined from 645 survey respondents and 17 interviewees. Survey findings revealed that about half of respondents reported MSD policies existed in their workplace. Many MSD practices (such as ergonomics and force reduction) were considered available by most respondents. Over fifty percent of respondents received some training on MSD. The person most often endorsed as responsible to support workers with MSD was a manager. Interview findings showed that MSD prevention practices related to awareness, training, and hazard reduction are considered important and effective. Facilitators of MSD prevention include practices that are proactive and customized and increase knowledge about MSD prevention. Barriers concerning lack of resources and poor implementation were consistently mentioned. Conclusions. Evidence from current practices may help workplaces reduce MSD burden. However, with only about fifty percent of respondents reporting that MSD policies exist in the workplace, further work to address MSD is required. Future research should examine workplace practices as an important source of evidence. OHS professionals can use the study findings and adapt it to their context(s) to guide their design and implementation of MSD prevention practices. Improved MSD prevention practices and interventions can lead to decreases in MSD in workplaces across all industrial sectors.
Keywords: evidence-based practice, musculoskeletal disorders, occupational health and safety programs, workplace practices, injury prevention
What do we already know about this topic?
Evaluations of workplace practices are rare in the literature but can be useful for evidence-based approaches to prevention.
How does your research contribute to the field?
This research describes workplace practices for the prevention of MSD; the results can be applied to support an evidence-based approach to MSD prevention.
What are your research’s implications towards theory, practice or policy?
Occupational Health and Safety professionals/practitioners and workplace managers/supervisors can use the study findings and adapt it to their context(s) to guide their design and implementation of evidence-based MSD prevention practices.
Introduction
Workers from all jurisdictions and industrial sectors experience musculoskeletal disorders (MSD) including low back pain, neck and upper extremity pain and disorders. MSD are challenging for workplaces to address due to the variety and interconnectedness of the hazards linked with these disorders. High quality epidemiological investigations have identified a broad range of physical, psychological, psychosocial, and organizational risk factors for MSDs.1-5 MSD are a substantial burden to society and to workplaces because of lost productivity, reduced performance, and lost time claims.6-10 Research has shown that low back pain is the leading cause of disability among non-communicable diseases in both developed and developing countries and consistently ranks in the top 3 causes globally 11 and that MSD are pervasive in multimorbidity. 12 Work-related MSDs account for 29% of all US workplace injuries. 3 Work-related musculoskeletal disorders are also a consistent and sizeable problem for many Canadian provinces, comprising between 40 to 68% of all lost time claims for the past 2 decades.13-17
One way to address MSD in workplaces is through an evidence-based practice (EBP) approach. EBP evolved from the evidence-based medicine model, defined as the: ‘. . . use of current best evidence in making decisions . . . integrating individual expertise with the best available external evidence from systematic research’. 18 Optimal EBP employs the knowledge and experience of practitioners along with the most up-to-date evidence from the scientific literature contextualized to the situation of the client (worker, etc.) to determine prevention solutions. 18
Occupational health and safety (OHS) practitioners need to make decisions about MSD prevention practices and programs in the context of their specific workplaces. While OHS practitioners are encouraged to, and often engage in, EBP,19-22 decisions about MSD must be made regardless of the availability of scientific evidence to guide practice.
Over the past decade, a series of systematic reviews has contributed a substantial body of research evidence addressing MSD prevention.21,23-30 Across these reviews, many different workplace-based prevention interventions were studied. Overall, there is evidence that interventions to address MSD hazards such as modified equipment, adjustable workstation elements, work breaks, stress management programs, etc., are effective in reducing relevant MSD outcomes (e.g. pain and work ability). Increasing research evidence also shows the effectiveness of exercise programs such as strengthening and stretching.21,24,26-28 However, there is inconsistent evidence about the effectiveness of MSD prevention training programs currently reported in the research literature.25,29,31
As these various systematic reviews show, there is some scientific evidence about workplace-based MSD prevention interventions. However, few studies have focused on workplace practices.32-35 Available studies are heterogeneous, focusing on different types of practices, different methods for ascertaining the practices, and different implementation elements. For example, workplace practices relevant for sustainable return to work (RTW) after MSD were examined through a qualitative case study approach33,34 with the overall finding that while RTW practices were consistent with local regulations, they were diverse both within and across organizations. Findings from another study 35 focused broadly on OHS and implementation practices (also relevant to MSD) determined that many of the implementation components found in practice have not been rigorously evaluated. Given the diversity in implementation practice and the lack of evidence in context, more research on workplace MSD practices is required.
The objective of this research was to examine and describe workplace MSD prevention practices from the experiences and perspectives of workers, managers, and OHS practitioners.
Methods
This is a descriptive study, using a survey and interviews of current workplace MSD prevention practices and experiences related to MSD prevention. The descriptive approach employed was informed by Qualitative Description 36 as this allows for comprehensive descriptions about who is doing what 37 in the workplace. Informed by a stakeholder advisory committee, this research employed a web-based survey and semi-structured interviews with workers and OHS personnel in workplaces in the Canadian province of Newfoundland and Labrador (NL). The research protocol was approved by the University of Toronto Research Ethics Board.
Stakeholder advisory Committee
We established a stakeholder advisory committee comprised of 9 key stakeholders from public and private sectors in NL with expertise in OHS. These included OHS professionals, ergonomists, physiotherapists and allied health professionals, policy advisors, and industry leaders. Early in the project, the committee aided the research team in developing survey items and interview guides and in recruiting survey participants through their respective networks. In later project stages, we asked for committee feedback on preliminary findings and development of practical messages for dissemination.
Study Sample
Our study employed a convenience sampling approach. The sample consisted of participants who identified as workers with MSD experience (those who did not manage others or have OHS responsibilities) and those that identified as having direct experience with MSD prevention or managing or providing support to those with, or at risk for, MSD (e.g. OHS practitioners, health and safety personnel, and managers/supervisors). We recruited from workplaces across NL.
The stakeholder advisory committee (described above) assisted in identifying a variety of appropriate workplace and OHS personnel to contact for participation. The research team also contacted NL workplaces directly using information publicly available on the internet. Participants were recruited via email through existing distribution lists provided by stakeholders and the research organization. Additional participants were recruited through a snowball method. The recruitment period was between July 2019 to February 2020.
Data Collection
Web-based survey
Potential participants were sent an invitation email to participate in a web-based survey and to provide consent before participating. Email reminders at 2, 4 and 8 weeks were used to increase the response rate. 38 The survey included a brief section on context and demographics (including questions on sector, company size, respondent job title and tenure), a section on MSD experiences and practices/interventions at the workplace (including questions on who is responsible for support, practice implementation steps, and policy), and a section on implementation experiences (including questions about facilitators and barriers, and program sustainability). Survey participants were also asked if they were interested in participating in an interview.
Interviews
To collect more in-depth data on workplace experiences around MSD prevention programs/practices, we conducted 45- to 60-minute semi-structured interviews to explore and focus on experiences with implementation of MSD prevention programs and practices at workplaces, gaps in existing programs, and improvements. Participants who agreed to be contacted, and provided informed consent, were interviewed by telephone. Interviews were transcribed for analysis.
Data Analysis
Survey data were analyzed descriptively using counts and frequencies indicating endorsement of items along with simple descriptive statistics where applicable. Data analysis was performed using SAS v9.3 (SAS Institute, Cary, NC, USA).
Interviews were coded using a preliminary coding list developed by the research team to capture MSD prevention practices and key barriers and facilitators in accordance with the research objectives. Following an iterative coding process, interview data were independently reviewed, analyzed for content, and organized into intermediary matrices. 39 Team members met to discuss any differences in coding and to refine identified themes. This allowed researchers to descriptively analyze the content that emerged from the data. The interviews and survey data underwent separate analysis, but results were considered together to support/or contrast findings.
Results
Study Participant Characteristics
There were 792 survey respondents. Of these, 645 (85%) completed 30% or more of the survey and were used in the analysis (30% completion was chosen as it corresponds to where in the survey respondents identify as either worker or as a manager/OHS professional).
Survey respondents (n = 645) were predominantly from NL (96%), with the remaining respondents from other Canadian provinces. A majority of respondents (60%) were 45 years of age or older, and most worked in workplaces with either 50-100 staff (42%) or 1-5 staff (40%). Most respondents reported they had worked at the workplace for more than 10 years (47%) with the greatest proportion having permanent full-time jobs (39%). Various sectors were represented in this sample with the largest proportion of respondents coming from construction, forestry, and healthcare (see Table 1).
Table 1.
Study participant characteristics a .
| Variable | Response Category | % Worker Respondents (n = 395, 61%) | % Mgr/OHS Respondents (n = 250, 39%) |
|---|---|---|---|
| Age category | 18–34 | 17.0 | 14.8 |
| 35–44 | 23.3 | 25.2 | |
| 45 or above | 59.2 | 60.0 | |
| Sex | Male | 59.2 | 49.6 |
| Female | 40.2 | 50.4 | |
| Tenure in organization | <1 year | 14.2 | 12.8 |
| 1–5 years | 30.6 | 26.4 | |
| 6–10 years | 18.0 | 18.0 | |
| >10 years | 36.5 | 42.8 | |
| Organization size | 1–5 staff | 40.0 | 39.6 |
| 6–50 staff | 8.9 | 9.6 | |
| 50–100 staff | 42.5 | 40.8 | |
| 100+ staff | 7.6 | 10.0 | |
| Employment status | Contract part time | 6.1 | 2.0 |
| Contract full time | 10.4 | 9.6 | |
| Permanent part time | 8.1 | 7.6 | |
| Permanent full time | 66.8 | 76.8 | |
| Other | 7.8 | 4.0 | |
| Employment role | Staff/employee | 33.2 | 12.4 |
| Manager/supervisor/human resources | 5.8 | 37.2 | |
| OHS personnel/disability management | 5.1 | 20.8 | |
| Union/labour representative | 27.3 | 12.8 | |
| Other | 2.0 | 1.2 | |
| Tenure in role | <1 year | 13.7 | 13.1 |
| 1–5 years | 36.2 | 30.8 | |
| 6–10 years | 18.5 | 24.4 | |
| >10 years | 30.6 | 31.2 | |
| Sectorik | Construction | 19.2 | 13.2 |
| Forestry | 10.1 | 9.6 | |
| Health care and social assistance | 8.4 | 11.6 | |
| Professional, scientific and technical services | 6.6 | 4.8 | |
| Finance/insurance/real estate | 5.8 | 6.8 | |
| Educational services | 4.8 | 6.0 | |
| Utilities | 3.8 | 5.2 | |
| Transportation and warehousing | 3.3 | 3.2 | |
| Retail | 3.0 | 2.8 | |
| Manufacturing | 1.8 | 4.0 | |
| Food/accommodation | 2.5 | 1.2 | |
| Other b | 17.7 | 18.4 | |
| Province c | Newfoundland and labrador | 95.2 | 96.4 |
| Other provinces | 4.8 | 3.6 |
All but 1 interview participant also completed the survey, characteristics described separately in text.
Includes responses entered as ‘other’ and combines sectors where the size was too small to report.
The survey was targeted to Newfoundland and Labrador workplaces but there were also respondents from other provinces as they may live in Newfoundland and Labrador but work outside of the province.
Sixty-one percent of respondents identified as a worker with MSD experience, the remaining 39% identified as a manager or OHS practitioner with experience managing or providing support to others with MSD (Table 1).
Seventeen interviews were conducted with participants who identified as having experience with MSD, either as workers, managers, or OHS practitioners. One interview was excluded from analysis due to incomplete data. All interview participants were from NL, 44% were male and 56% were in the ‘45 or above’ age range. Fifty-six percent identified as managers or OHS personnel and 44% were workers from various industrial sectors.
Results describing workplace MSD prevention practices are presented first. Second, we present MSD prevention experiences from the perspective of workers, managers, and OHS practitioners including MSD training experiences, responsibility for MSD prevention, program, and practice implementation, as well as identified facilitators and barriers to preventing MSD. We note that interviews consistently provided rich descriptions of experiences related to MSD and provided additional context to the survey responses. Identified themes are listed and described in each section with accompanying illustrative quotes to provide an example of content coded under each theme.
Musculoskeletal Disorders Prevention Practices
Survey findings: MSD policies and practices for preventing MSD
Over 40% of workers and over 50% of managers/OHS replied that their workplace had MSD policies in place. Furthermore, around a third of workers and nearly half of managers/OHS indicated that MSD policies and processes were reviewed and updated regularly.
Workers and managers/OHS generally agreed on the overall availability of workplace MSD prevention practices except for flexible work hours/location and exercise (Table 2). There were also disagreements in reporting between worker and manager/OHS responses on availability of practices related to ‘adequate staffing’, whether ‘workers were heard’, and if ‘timely information was provided’.
Table 2.
Survey respondent agreement or disagreement about available MSD practices in their workplace.
| MSD Practice | Respondent | Response (%) |
|||
|---|---|---|---|---|---|
| Agree | Disagree | N/A | Do Not Know | ||
| Safe tools: Safe tools and/or equipment are provided to do job tasks | Worker | 67.6 | 12.4 | 1.3 | 3.3 |
| Manager/OHS | 75.6 | 3.6 | 4.4 | 0.4 | |
| Rest breaks: Adequate rest breaks and recovery time are provided to complete job tasks | Worker | 63.3 | 16.5 | 2.5 | 2.8 |
| Manager/OHS | 72.8 | 8.0 | 2.4 | 0.8 | |
| Force: Efforts are made to reduce excessive force requirements (e.g. heavy lifting, lowering, carrying, push/pull, gripping) of job tasks | Worker | 61.0 | 17.7 | 2.8 | 3.5 |
| Manager/OHS | 74.0 | 5.6 | 3.2 | 1.2 | |
| PPE: Personal protective equipment is available and encouraged (e.g. wrist supports/splints, anti-vibration gloves, knee pads, shock-absorbing insoles) | Worker | 58.0 | 12.7 | 9.1 | 4.8 |
| Manager/OHS | 68.4 | 6.4 | 8.8 | 0.4 | |
| Modified tools: Tools and/or equipment are modified when needed for doing job tasks | Worker | 52.4 | 19.7 | 4.1 | 8.1 |
| Manager/OHS | 63.6 | 8.8 | 8.0 | 3.2 | |
| Ergonomics: Ergonomics strategies are used to improve workstation design | Worker | 49.1 | 21.3 | 5.3 | 8.9 |
| Manager/OHS | 66.4 | 12.4 | 2.4 | 2.4 | |
| Task flexibility: Workers have flexibility in prioritizing job tasks to complete their work (i.e. tasks can be done in an order of their choosing) | Worker | 48.9 | 25.1 | 3.0 | 7.3 |
| Manager/OHS | 54.4 | 19.6 | 6.0 | 4.0 | |
| Feedback: Worker feedback is used to improve the organization of the job tasks | Worker | 48.4 | 20.3 | 3.3 | 13.2 |
| Manager/OHS | 63.6 | 12.0 | 2.8 | 4.8 | |
| Temperature: Efforts are made to reduce exposure to extreme temperatures (i.e. too hot or too cold) | Worker | 46.8 | 18.2 | 15.7 | 4.3 |
| Manager/OHS | 58.0 | 3.2 | 21.2 | 1.2 | |
| Staffing: Efforts are made to make sure there are adequate staffing levels to complete job tasks | Worker | 45.8 | 32.2 | 3.8 | 3.0 |
| Manager/OHS | 68.0 | 12.0 | 2.0 | 2.0 | |
| Worker heard/involved: When workers approach the workplace representative about MSD hazards, they feel heard and supported | Worker | 42.0 | 15.7 | 3.5 | 23.5 |
| Manager/OHS | 74.0 | 2.8 | 5.2 | 2.4 | |
| Timely information: When workers approach the workplace representative about MSD hazards, they are told how the workplace can take action in a timely manner | Worker | 41.5 | 13.2 | 4.3 | 26.1 |
| Manager/OHS | 76.0 | 4.4 | 1.6 | 2.0 | |
| Vibration: Efforts are made to reduce exposure to vibration (hand-arm and/or whole-body vibration) of job tasks | Worker | 37.2 | 16.7 | 22.8 | 7.8 |
| Manager/OHS | 46.4 | 5.2 | 26.8 | 5.6 | |
| Flexible hours/work location: Workers are able to work from home, or have flexible working hours to complete their work | Worker | 19.7 | 35.2 | 24.8 | 4.8 |
| Manager/OHS | 24.0 | 30.8 | 24.8 | 4.4 | |
| Exercise: Workers have access to a workplace-based resistance or strength training exercise program | Worker | 16.7 | 48.1 | 9.1 | 10.6 |
| Manager/OHS | 25.2 | 40.0 | 11.6 | 6.8 | |
| No programs: No supports, resources and/or programs are available to prevent or respond to MSD hazards | WorkerManager/OHS | 19.511.2 | 34.248.0 | 7.111.6 | 21.810.0 |
In general, both workers and managers/OHS agreed organizational policies and practices related to MSD prevention happen between 60 and 100% of the time at their workplace (Table 3).
Table 3.
Survey respondents report of the percentage time that MSD prevention organizational policies and practices take place.
| Organizational Performance Practice | Respondent | Percentage of Time Each
Practice Takes Place |
|
|---|---|---|---|
| 0–60% | 60–100% | ||
| Workers and supervisors have information needed to work safely | Worker | 20.8 | 54.2 |
| Manager/OHS | 10.0 | 62.0 | |
| Workplace considers safety at least as important as production and quality | Worker | 24.6 | 50.4 |
| Manager/OHS | 19.2 | 52.8 | |
| Formal safety audits occur regularly | Worker | 29.0 | 45.1 |
| Manager/OHS | 20.8 | 50.8 | |
| Everyone at this workplace values safety improvement | Worker | 21.0 | 54.5 |
| Manager/OHS | 18.4 | 53.4 | |
| Those in charge of safety have the authority to make changes | Worker | 25.4 | 49.6 |
| Manager/OHS | 18.8 | 53.2 | |
| Everyone has tools/equipment needed to work safely | Worker | 26.8 | 47.8 |
| Manager/OHS | 13.2 | 58.4 | |
| Employees are always involved in health and safety decisions | Worker | 31.1 | 43.8 |
| Manager/OHS | 24.8 | 47.2 | |
| Those who act safely receive positive recognition | WorkerManager/OHS | 39.831.6 | 35.240.4 |
Interview Findings: Musculoskeletal Disorders Prevention Practice Themes
Participants were asked to describe specific types of workplace MSD prevention programs and practices that they found useful. Three themes of MSD prevention practices emerged in our analyses: 1) awareness; 2) training; and 3) hazard identification/solutions. Briefly, the interviews provided perspectives about the need for awareness and training approaches for MSD as well as the importance of hazard identification and solution practices for prevention. These were considered 3 key elements of workplace MSD prevention practice and are elaborated below.
Awareness
Most workers and manager/OHS participants considered awareness a key element of MSD prevention. It was noted that both workers and managers could benefit from increased awareness of MSD, however awareness activities described were most often directed to workers.
Quote: ‘I do think workplaces are all trying to prevent MSDs, but if employees don’t know enough about them, they cannot know what to do to prevent them.’ (EMP02)
Descriptions of awareness practices included informal and formal communication between manager/OHS and workers. ‘Toolbox talks’ were frequently mentioned by participants either as formal with planned regular occurrences or informal as ‘toolbox chats’ or ‘worker safety huddles’. Both formal and informal toolbox talks were considered an effective way to increase awareness of MSD.
Quote: ‘[toolbox talks are] To communicate new ideas and make safety a priority in the workplace.’ [Commonly occurred weekly, during lunch breaks and usually on a health &; safety topic related to their current work] ‘They are full of information for them [owners] and our employees. I can’t tell you how much I take back to employees through Toolbox Talks. They keep issues fresh in mind among workers.’ MGR06
In contrast, posters and other passive approaches were believed to play a role but were not considered as effective as direct communication. Posters and bulletin boards served as reminders but required regular updating to be most effective.
Quote: ‘[The posters] have not been changed in a long time. Most people just read them once and forget about it. If you ask them what’s on them, they probably can’t tell you. But it does give you a visual and if you take a minute to read it, it gives you a kick in the pants.’ EMP07
Training
Training was consistently identified as an important element of MSD prevention by both worker and manager/OHS participants. Formal and informal types of training, including full courses, online sessions, and webinars, as well as one-on-one training for specific tasks such as manual materials handling, were described. Participants noted that training should be ‘user-friendly’ but also cover MSD prevention topics in-depth. Engaging trainees with hands-on, practical examples relevant to their work and tasks was also noted as an important element of effective training.
Quote: ‘Training courses need to be user-friendly, packaged in a way so learners fully understand what MSDs are and how to identify risks in the workplace – it all comes back to the education and training. A lot of people just don’t have the knowledge.’ OHS14
Manager/OHS participants often delivered training and noted the need for it to be evidence-based and regularly reviewed with updated content. Workers also noted that training should be up-to-date and delivered regularly (not just at orientation).
Hazard Identification/Solutions
The most common MSD prevention programs and practices described by interviewees were related to the identification of or solutions for MSD hazards. Workers shared specific workplace hazards for MSD they experienced and the solutions they felt were effective. Manager/OHS interviewees tended to reflect on hazards across multiple jobs or tasks as well as task-specific hazards. Both groups mentioned hazards can change over time and that identifying them early was a priority.
Both worker and manager/OHS interviewees described physical hazards in their jobs and workplaces as addressed through ergonomics programs often providing examples of solutions implemented. In fact, ergonomics programs were sometimes noted as synonymous with MSD prevention.
Quote: ‘Very few people from an employee standpoint would understand the term MSD. But if I use the term ergonomics, that term is probably used enough now that people have at least heard it. They might not fully understand what the science is, but at least they have heard it, and they know it means adjusting their workstation or chair, they at least know some sort of adjustment is being made or needs to be made.’ OHS01
Workload was also a concern and a perceived cause of MSD, however workers and managers/OHS had different perspectives on the role that workload had on prevention practice. Some workers remarked that ‘ergonomics’ were not always an issue/concern for their job instead they felt that workload or pace of work imposed on them often led to MSD. Some workers described MSD risk in terms of perceived workload.
Quote: ‘Workload contributes and is a barrier to preventing MSDs. [The only thing that prevents prevention is the high workload. Using poor practices to get the work done.]’ EMP10
In contrast, some manager/OHS interviewees described workload MSD issues as being related to workers being too rushed and/or not in control due to their own decisions.
Quote: ‘Even though there are different programs and approaches in place to make people aware of the potential for injury, at the end of the day it’s the workers themselves in trying to get the job done that may influence if they get hurt or not. Sometimes human nature is to do what you can to save time but it can come back and nip them in the butt.’ (OHS16)
Regardless of the work environment, both worker and management/OHS participants consistently noted that individualized assessments and solutions were more effective than generic or one-size-fits-all approaches.
Quote: ‘They don’t live in my world. They don’t do my work.’ EMP13
Musculoskeletal disorders prevention experiences
Survey findings
Musculoskeletal disorders training and knowledge
Fifty-five percent of workers indicated receiving some training on MSD. The largest proportions of worker respondents reported receiving training that was half a day or less (15.7%) or 1 day long (11.4%). Training for workers was most often delivered in-person by their own organization (24.6%) or from an external source (16%) with seventeen percent receiving a certificate. A majority (87%) of worker respondents felt they were ‘somewhat’ or ‘very knowledgeable’ about MSD.
Two thirds (67.6%) of manager/OHS respondents reported they had some training to support workers with MSD. Many manager/OHS respondents received a full day of MSD training (29%) with the rest of the respondents evenly distributed across less than half-day, half day, 2–3 days, or more than 5 days long training. MSD training was most often delivered in-person from an external organization (43.2%) and 41% reported receiving a certificate. Over 90% of manager/OHS respondents indicated they were ‘somewhat’ or ‘very knowledgeable’ about MSD.
Who is Responsible to Support Workers with MSD?
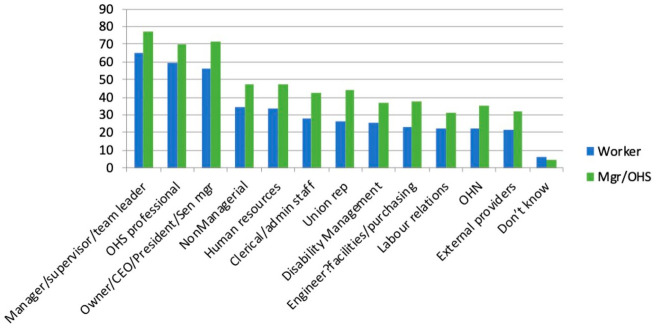
Figure 1 shows who, according to workers and managers/OHS, was responsible for workplace MSD prevention. Worker respondents reported turning most often to their direct manager (65.3%), an OHS professional (59.2%), or senior management (including Owner/CEO/President) (55.9%) for MSD issues. Manager/OHS respondents mirrored the worker responses with most endorsing a direct manager (76.8%), senior management (including Owner/CEO/President) (71.2%) and OHS professional (70.0%). Few workers or managers/OHS (6.1% and 4.4% respectively) indicated that they did not know who was responsible (see Figure 1).
Figure 1.
Percentage of workers and manager/OHS that endorsed who is responsible for MSD prevention at their workplace.
Implementation of Musculoskeletal Disorders Prevention Practices
When asked about the implementation of MSD prevention practices, between 30 and 40% of managers/OHS indicated there was a clear implementation plan, sufficient resources, and that prevention strategies were evaluated. While 30% of workers said their workplaces had an MSD prevention implementation plan, between 30 and 34% of workers answered they did not know if their workplace had enough resources or if MSD implementation plans were evaluated.
Interview Findings: Musculoskeletal Disorders Experiences
In this section we discuss 3 themes specific to participant experiences related to MSD prevention in the workplace and 3 themes related to barriers and facilitators to MSD prevention that emerged from the interviews. While survey data captured opinions on training, responsibility for MSD prevention, and prevention practices in place, interview data revealed valuable perspectives on the importance of MSD knowledge, the need for proactive strategies, and customized support to address MSD. Interviewees also identified barriers and facilitators in terms of communication, resources, and implementation. The themes are described in detail below.
Knowledge and Recognition
Participants consistently mentioned that knowledge about MSD and their impacts was lacking. Participants reported a need for knowledge about MSD risk factors, the nature of MSD injuries, and effective measures that could be taken to reduce risks.
Quote: ‘Everyone always thinks that to address MSDs, employees should change their seat or their desk. But how many construction employees sit at a desk? There is no recognition in understanding, for example, that the hammer a carpenter is using needs to be held at the right grip, or a drill should not be held in a certain way. That little bit of extra knowledge or recognition would be helpful in preventing MSDs . . .’ OHS01
To increase knowledge about MSD risk factors, some participants remarked that additional training and awareness was required for both workers and managers. Participants also acknowledged seeing improvements over time in the level of recognition and knowledge about MSD overall.
Quote: ‘People are getting better – attitudes to safety, including MSD, are becoming more open and understanding, they are looking for information about prevention education.’ OHS14
Informal sharing of knowledge was considered important to increase MSD risk factor recognition and identification of potential solutions. Both worker and manager/OHS interviewees considered sharing knowledge and information via reminders and updates about MSD as important. Many workers also mentioned sharing MSD knowledge based on their own experiences with co-workers. Informal methods of sharing knowledge and increasing awareness extended to ‘round-table’ meetings, toolbox talks, ‘buddy systems’, and leading by example, where supervisors exhibit safe practices.
Workers often felt they required updated information via formal training. Managers/OHS emphasized the need for training, but many also recognized the important role of informal communication to assist with putting policies into practice. Participants remarked that having written MSD policies in place was important, but information about those policies is also needs to be provided to the workplace broadly.
Quote: ‘. . . once a document is written, [the] employer will spend some time letting everyone know it exists, e.g., putting up posters across the workplace.’ OSH04
Further, while workers noted policies were in place, there was little follow-up to ensure actions related to prevention were taking place.
Quote: We have written guidelines for work practices. We have many policies, ‘policies galore.’ But the onus is on the employee to read it. Nobody goes around to make sure people are actually following safe ergonomic practices, the onus is on the employee. EMP02
Importance of Being Proactive
Workers and manager/OHS interviewees spoke of the need to be proactive in MSD prevention. Worker engagement and involvement with MSD prevention was emphasized as necessary and important in making MSD prevention more proactive.
Manager/OHS interviewees remarked that practices related to early reporting of injuries (including near misses) and hazards are key to injury prevention.
Quote: ‘We stress early reporting. Having dealt with lots of injured employees, if you catch it early enough, you can make the appropriate changes. So we stress early reporting as an organization. If there’s something even minor – tell your supervisor and then it gets dealt with from that level on. If you have even the slightest issue, lets deal with it early on because it becomes a major issue . . . I don’t think we’ve had a single person who has gone off with any MSD issue in the company.’ OHS01
However, workers often felt their workplace was reactive and hazards were not being identified to prevent MSD. They commented that regular equipment, worksite, and workstation checks by OHS professionals were key strategies in MSD prevention but should happen with regularity.
Manager/OHS interviewees also commented about their need to be responsive to worker feedback not only to encourage early reporting, but also to facilitate regular observations, and assessments. Workers reported that ‘open-door’ policies where workers felt comfortable discussing MSD hazards and programs were most helpful and part of a positive workplace culture. Manager/OHS interviewees supported this view and added that senior management support was also key in moving MSD prevention from ‘reactive’ to ‘proactive’, with positive results.
Quote: ‘The engineers and designers put their expertise into design, but human factors are not taken into consideration. The people themselves [who then work with it] then go, “hey, we didn’t have any input into this. We didn’t say put that desk there and even the process, we didn’t have a say” Then they are dealing with issues after the fact. Individuals should be involved in the planning and design process [during construction or renovation], not just supervisors and designers. Even just asking for their ideas at the design stage.’ OHS17
Customized and Updated Accommodations
Workers strongly endorsed the need for customized or individualized assessments and solutions (adjustments or equipment) for effective MSD prevention. They raised concerns about generic approaches potentially causing or exacerbating MSD injuries.
Quote: ‘[My] station was set up and [I] was supplied with the standard prevention tools but they actually contributed to the injury. But, there are going to be individual differences that have to be acknowledged. An ergonomic keyboard does not mean that there will not be an MSD.’ EMP10
Workers also expressed concerns about the time it took to receive an effective, individualized solution to identified issues. Oftentimes workers mentioned trying multiple solutions before finding 1 they considered helpful.
Quote: ‘Proper workstations are very important . . . I finally received my new chair in [late] 2018 and I’m starting to reap the benefits, feeling better, but not my best – it took 5-6 years too long.’ EMP12
Workers who received customized accommodations related to equipment, workstation adjustments or modified duties felt their workplaces were responsive and noted they felt better quickly once the solution was implemented.
Some manager/OHS interviewees described customizing what they provided as a matter of course, recognizing the need to adapt solutions to their situation. They noted that they would go beyond the generic MSD prevention programs/practices often in place to solve a problem, customizing their training, awareness activities, and MSD prevention programs within their environments.
Quote: ‘If not geared to the environment, the uptake is not as good.’ OHS03
Perceived Facilitators and Barriers
Facilitators and barriers to MSD prevention identified by both workers and manager/OHS interviewees can be described as either-or depending on the language used. For example, resources can be seen as a barrier if they are too few, or a facilitator if they are sufficient. We present the predominant characterization as described by participants below. We note there were barriers described which were related to lack of knowledge about MSD as well as a lack of customization or tailoring of solutions. Since those themes are described above, we focus on standalone themes regarding facilitators and barriers in this section.
Facilitator – Communication
Communication was consistently noted as a key facilitator for MSD prevention. Both workers and manager/OHS interviewees discussed the benefits of clear, open, and frequent communication in all aspects of hazard identification, training, and awareness activities. Communication was also noted as important for conveying policy and program information to workers, as well as for workers to provide feedback and for reporting hazards and injuries without repercussions.
Quote: ‘Communication. It is very important for every workplace to communicate to their employees how important it is for them to work safe because they (employees) are an investment the company is making.’ EMP07
Workers reported that when the workplace had good levels of communication, they felt valued and that their employer exhibited genuine concerns for workers’ health status as well as concern for the hazards in the workplace. Manager/OHS interviewees also noted communication between all parties was essential for MSD prevention.
Quote: ‘Clear communication with employees without repercussions’ [is a key facilitator]; ‘Just open communications. We make sure workers’ voices are heard.’ OHS16
Barrier – Lack of Resources
Most participants commented on lack of resources as a barrier to MSD prevention. Workers identified resources were lacking for new or appropriate equipment, and in trained staff to address adjustments or workflow. Often, workers noted insufficient resources led to delays in necessary changes to avoid MSD injury.
Quote: ‘It is the job of the OHS manager to oversee all this and make sure risks for MSDs are recognized and people are made aware, but he is not doing it. One person can’t deal with a staff of [hundreds], get the information and reminders out to everyone and do his job full-time. He needs to collaborate with HR and see if they can do something together.’ EMP02
A lack of devoted resources was also recognized by Manager/OHS interviewees as a barrier to MSD prevention. This as a particular challenge when multiple workers’ concerns/hazards were identified.
Quote: ‘Managers/OHS do not have enough resources, and have too much on their plate, to successfully manage staff. Not enough support from upper level management or from employees you are managing in order to close that gap.’ OHS05
Barrier- Poor Implementation
Some manager/OHS interviewees raised concerns about MSD prevention program implementation. Poor MSD program implementation is reflected in more reactive or retroactive approaches rather preventing MSD. Some noted that the lack of proper implementation meant the full potential of expensive equipment solutions was not being realized. In effect, this vocal minority referred to MSD policies as only on paper and not put into practice.
Quote: MSD program is largely theoretic and prescriptive in nature, these ‘best practices’ are recommendations - but not implemented effectively, or at all. It is a checklist. All ingredients are there but the MSD program is a ‘sinking ship in terms of practice, it’s just not being implemented. It’s a checkbox for people to say that it’s done, but that doesn’t mean it is successfully done.’ OHS05
Discussion
This study aimed to describe current MSD practices and experiences related to MSD prevention using a survey and in-depth interviews. While there are descriptions of specific interventions that could be implemented into practice to address MSD from research and systematic reviews in the peer-reviewed literature, along with descriptions of how workplaces should tackle MSD from OHS professionals, there is little description of MSD prevention practices in workplaces. As noted in the introduction, this study helps to fill a gap by revealing workplace MSD prevention practices beyond intervention studies from the scientific literature. Our results suggest that to adopt an EBP approach, OHS professionals should include knowledge from current research or scientific evidence 18 but should also be aware of current workplace MSD practices. OHS researchers should also have a better understanding of workplace practices and consider research to examine and evaluate interventions that are consistent with workplace practices.
Our results from surveys and interviews revealed a variety of MSD practices are being employed. There was general agreement that organizational policies and practices relevant for MSD were in place in NL workplaces. However, there was less agreement that MSD prevention practices were well implemented. We found 3 categories of MSD prevention practices that were considered important and effective in NL workplaces: awareness, training, and MSD hazard identification and solutions. Our interview findings supported the survey results about the availability of MSD practices. In addition, we found themes related to knowledge and recognition, proactive approaches, and customization around MSD prevention practices. Key barriers and facilitators related to resources, implementation, and communication were linked to the success of MSD prevention practices.
Awareness programs and practices, both formal and informal, were described as necessary and effective particularly when updated regularly. We note that not all the current workplace practices are supported by available research evidence. There appears to be little research in the scientific literature on awareness interventions for MSD prevention. While there is a lack of research evidence, it does not mean that awareness programs and practices are not effective.
Training programs and practices for MSD were consistently noted as helpful, by both workers and managers/OHS. Training, especially when it is engaging, regularly reviewed and updated, was considered effective and an important element of MSD prevention. The research evidence for the effectiveness of MSD prevention training is not strong, with many studies reporting no evidence of effect from training.25,29,31 It is possible that the training interventions studied were not well implemented or that the follow-up times were short and therefore MSD outcomes did not change.
Workplaces were engaged in MSD prevention practices related to hazard reduction including personal protective equipment (PPE), proper tools, ergonomics, and rest breaks. MSD hazard identification/solutions were reported as key MSD prevention programs and practices by study participants. Specifically, ergonomics programs were judged to be necessary and effective for MSD prevention. The literature consistently recognizes MSD hazard solutions (such as modified equipment, adjustable workstation elements, work breaks) to be effective for MSD prevention.21,23-30 Participants also noted that workload issues play a role in MSD and should be addressed. Regardless of the type of hazards addressed, individualized solutions were felt to be more effective than general/generic or one-size-fits-all programs for MSD prevention.
We also note that exercise (stretching or strengthening) was not widely adopted by workplaces in our study. This is despite growing research evidence suggesting effectiveness for MSD prevention.24,26-28,40,41
Based on the experiences of workplace personnel, our findings suggest that MSD programs and practices were more successful if there were good levels of knowledge and recognition about MSD prevention in the workplace. Proactive approaches as well as customized and updated programs and practices were also considered to contribute to effective MSD prevention. Key facilitators were linked to good levels of communication and having tailored and responsive solutions to MSD prevention, whereas key barriers centred on a lack of sufficient resources and knowledge about MSD, as well as poor implementation of MSD programs and practices.
The concerns about implementation of programs and practices suggest more research is required in this area. For example, additional research on implementation would aid in understanding how workplaces can be more proactive in MSD prevention. The identified broader strategies for MSD prevention overlap with other implementation concepts previously reported, including awareness, current workplace needs (tailored and updated), and resources. 35 Although research supporting overall implementation practices exists, the research designs and rigor were considered lacking in these studies. 35 Further research about how MSD practices are implemented in workplaces is necessary.
Strengths and Limitations
This study has a number of strengths. We engaged with a stakeholder advisory committee to guide our research approach from the type of questions we asked through to the framing of the practical messages from our results. This integrated knowledge transfer approach can aid in the dissemination of research to workplace knowledge users. 42 In addition, we collected data from a sample of workers from different workplaces, including those who manage others or provide OHS expertise. Our approach resulted in rich descriptions of workplace practices and experiences.
One limitation of this study was our use of a convenience sample. It would be useful to explore workplace practices in a broader sample of respondents with equal representation of sectors and organization sizes. However, reaching workers, managers, and OHS personnel in workplaces is challenging. Therefore, we recruited from known networks and through our stakeholder advisory committee (and their networks) and encouraged potential participants to forward the survey to others who may be interested. While we were unable to determine our response rate, our sample represented those who reported experience with MSD in multiple industrial sectors. Additional research including individuals who had left the labour market due to MSD, or who are working in more precarious jobs, would complement our findings.
Conclusions
This research described current MSD workplace practices and experiences with MSD prevention. Our study finding that 40% of workers and just over 50% of managers/OHS reported that their workplace had MSD policies suggests that further work to develop and include policies (and practices) for this burdensome disorder must still be done. Our findings suggest that workplaces and OHS professionals should consider implementing i) awareness programs/practices, ii) training programs/activities, and iii) MSD hazard identification/solution programs/practices for MSD prevention. These programs and practices can be enhanced by being well implemented and responsive to workplace needs. OHS professionals and workplaces should address key implementation elements related to proactivity, customization, and supporting MSD knowledge and recognition. In addition, good communication, implementation, and sufficient resources are paramount. While these barriers and facilitators are commonly reported, they remain important to address to ensure that MSD prevention is effective in workplaces. Future high-quality research on well implemented and feasible MSD prevention practices would be useful for workplaces and OHS professionals.
Acknowledgments
We would like to thank the stakeholder advisory committee from Newfoundland and Labrador for their support during this project.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the WorkplaceNL (Research Initiatives Program).
Ethical approval: The research protocol (#00034907) was approved by the University of Toronto Research Ethics Board.
ORCID iD: Dwayne Van Eerd  https://orcid.org/0000-0002-5672-0168
https://orcid.org/0000-0002-5672-0168
References
- 1. Hagberg M, Silverstein B, Wells R. Work related Musculoskeletal Disorders (WMSDs): A reference Book for Prevention. Taylor & Francis; 1995. [Google Scholar]
- 2. National Research Council. Musculoskeletal Disorders in the Workplace: Low Back and Upper Extremities. National Academic Press; 2001. [PubMed] [Google Scholar]
- 3. Silverstein B, Evanoff B. Musculoskeletal Disorders. In: Levy BS, Wegman DH, Baron SL, eds Occupational and environmental health: recognizing and preventing disease and injury. Oxford University Press; 2011:335-365. [Google Scholar]
- 4. Wells R, Van Eerd D, Hägg G. Mechanical exposure concepts using force as the agent. Scand J Work Environ Health. 2004;30(3):179-190. doi: 10.5271/sjweh.778. [DOI] [PubMed] [Google Scholar]
- 5. Sluiter JK, Rest KM, Frings-Dresen MH. Criteria document for evaluating the work-relatedness of upper-extremity musculoskeletal disorders. Scand J Work Environ Health. 2001;1:27-102. [PubMed] [Google Scholar]
- 6. Hoy D, Geere JA, Davatchi F, Meggitt B, Barrero LH. A time for action: opportunities for preventing the growing burden and disability from musculoskeletal conditions in low-and middle-income countries. Best Pract Res Clin Rheumatol. 2014;28(3):377-393. doi: 10.1016/j.berh.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 7. Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197-2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 8. Tornqvist EW, Hagberg M, Hagman M, Risberg EH, Toomingas A. The influence of working conditions and individual factors on the incidence of neck and upper limb symptoms among professional computer users. Int Arch Occup Environ Health. 2009;82(6):689-702. [DOI] [PubMed] [Google Scholar]
- 9. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163-2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Walker-Bone K, Palmer KT, Reading I, Coggon D, Cooper C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Care Res (Hoboken). 2004;51(4):642-651. doi: 10.1002/art.20535. [DOI] [PubMed] [Google Scholar]
- 11. Buchbinder R, Blyth FM, March LM, Brooks P, Woolf AD, Hoy DG. Placing the global burden of low back pain in context. Best Pract Res Clin Rheumatol. 2013;27(5):575-589. doi: 10.1016/j.berh.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 12. Duffield SJ, Ellis BM, Goodson N, et al. The contribution of musculoskeletal disorders in multimorbidity: Implications for practice and policy. Best Pract Res Clin Rheumatol. 2017;31(2):129-144. doi: 10.1016/j.berh.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 13. WorkSafeBC. WorkSafeBC 2019 statistics. WorkSafeBC, 2019. [Google Scholar]
- 14. WorkplaceNL. WorkplaceNL reports 2019 workplace injury rates. WorkplaceNL. 2020. https://workplacenl.ca/article/workplacenl-reports-2019-workplace-injury-rates/. [Google Scholar]
- 15. Workplace Safety and Insurance Board (WSIB). By the numbers: 2018 WSIB statistical report (Schedule 1). Workplace Safety and Insurance Board (WSIB), 2018. [Google Scholar]
- 16. Workers Compensation Board of Nova Scotia. Workers’ compensation board of nova scotia 2013 annual report. Workers’ Compensation Board of Nova Scotia, 2018. [Google Scholar]
- 17. Workers Compensation Board of Manitoba. Manitoba workplace injury and illness statistics 2000-2013. Workers Compensation Board of Manitoba, 2018. [Google Scholar]
- 18. Sackett DL, Rosenberg WM, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: What it is and what it isn’t. BMJ. 1996;312(7023):71. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bramberg EB, Nyman T, Kwak L, et al. Development of evidence-based practice in occupational health services in Sweden: A 3-year follow-up of attitudes, barriers and facilitators. Int Arch Occup Environ Health. 2017;90(4):335-348. doi: 10.1007/s00420-017-1200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Salazar MK. Evidence based practice: Relevance to occupational health nurses. AAOHN J. 2003;51(3):109-112. [PubMed] [Google Scholar]
- 21. Teufer B, Ebenberger A, Affengruber L, et al. Evidence-based occupational health and safety interventions: a comprehensive overview of reviews. BMJ Open. 2019;9(12):e032528. doi: 10.1136/bmjopen-2019-032528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Van Eerd D, Cardoso S, Irvin E, Saunders R, King T, Macdonald S. Occupational safety and health knowledge users’ perspectives about research use. Pol Pract Health Saf. 2018;16(1):4-19. doi: 10.1080/14773996.2017.1356544. [DOI] [Google Scholar]
- 23. Agarwal S, Steinmaus C, Harris-Adamson C. Sit-stand workstations and impact on low back discomfort: A systematic review and meta-analysis. Ergonomics. 2018;61(4):538-552. doi: 10.1080/00140139.2017.1402960. [DOI] [PubMed] [Google Scholar]
- 24. Chen X, Coombes BK, Sjogaard G, Jun D, O'Leary S, Johnston V. Workplace-based interventions for neck pain in office workers: Systematic review and meta-analysis. Phys Ther. 2018;98(1):40-62. doi: 10.1093/ptj/pzx101. [DOI] [PubMed] [Google Scholar]
- 25. Hogan DAM, Greiner BA, O'Sullivan L. The effect of manual handling training on achieving training transfer, employee’s behaviour change and subsequent reduction of work-related musculoskeletal disorders: A systematic review. Ergonomics. 2014;57(1):93-107. doi: 10.1080/00140139.2013.862307. [DOI] [PubMed] [Google Scholar]
- 26. Moreira-Silva I, Teixeira PM, Santos R, Abreu S, Moreira C, Mota J. The effects of workplace physical activity programs on musculoskeletal pain. Workplace Health Saf. 2016;64(5):210-222. doi: 10.1177/2165079916629688. [DOI] [PubMed] [Google Scholar]
- 27. Skamagki G, King A, Duncan M, Wahlin C. A systematic review on workplace interventions to manage chronic musculoskeletal conditions. Physiother Res Int. 2018;23(4):e1738. doi: 10.1002/pri.1738. [DOI] [PubMed] [Google Scholar]
- 28. Van Eerd D, Munhall C, Irvin E, et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: An update of the evidence. Occup Environ Med. 2016;73(1):62-70. doi: 10.1136/oemed-2015-102992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Van Hoof W, O'Sullivan K, O'Keeffe M, Verschueren S, O’Sullivan P, Dankaerts W. The efficacy of interventions for low back pain in nurses: A systematic review. Int J Nurs Stud. 2018;77:222-231. doi: 10.1016/j.ijnurstu.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 30. Waongenngarm P, Areerak K, Janwantanakul P. The effects of breaks on low back pain, discomfort, and work productivity in office workers: A systematic review of randomized and non-randomized controlled trials. [Review]. Appl Ergon. 2018;68:230-239. doi: 10.1016/j.apergo.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 31. Kuijer PP, Verbeek JH, Visser B, et al. An evidence-based multidisciplinary practice guideline to reduce the workload due to lifting for preventing work-related low back pain. Ann Occup Environ Med. 2014;26(1):16. doi: 10.1186/2052-4374-26-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dunet DO, Sparling PB, Hersey J, et al. A new evaluation tool to obtain practicebased evidence of worksite health promotion programs. Prev Chronic Dis. 2008;5(4):A118. [PMC free article] [PubMed] [Google Scholar]
- 33. Durand MJ, Nastasia I, Coutu MF, Bernier M. Practices of return-to-work coordinators working in large organizations. J Occup Rehabil. 2017;27(1):137-147. doi: 10.1007/s10926-016-9640-7. [DOI] [PubMed] [Google Scholar]
- 34. Nastasia I, Durand MJ, Coutu MF, Collinge C, Cibotaru A. Workplace practices for healthy and sustainable return to work. Report No R-1047 IRSST. 2019. [Google Scholar]
- 35. Rasmussen CDN, Højberg H, Bengtsen E, Jørgensen MB. Identifying knowledge gaps between practice and research for implementation components of sustainable interventions to improve the working environment: A rapid review. Appl Ergon. 2018;67:178-192. doi: 10.1016/j.apergo.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 36. Kim H, Sefcik JS, Bradway C. Characteristics of qualitative descriptive studies: A systematic review. Res Nurs Health. 2017;40(1):23-42. doi: 10.1002/nur.21768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334-340. doi: 10.1002/1098-240x(200008)23. [DOI] [PubMed] [Google Scholar]
- 38. Dillman DA. The design and administration of mail surveys. Annu Rev Sociol. 1991;17(1):225-249. doi: 10.1146/annurev.so.17.080191.001301. [DOI] [Google Scholar]
- 39. Guest G, MacQueen K, Namey E. Applied Thematic Analysis. Sage; 2012. [Google Scholar]
- 40. Hoosain M, de KS, Burger M. Workplace-based rehabilitation of upper limb conditions: A systematic review. J Occup Rehabil. 2019;29(1):175-193. doi: 10.1007/s10926-018-9777-7. [DOI] [PubMed] [Google Scholar]
- 41. Schaafsma FG, Whelan K, Van Der Beek AJ, vdE-L LC, Ojajarvi A, Verbeek JH. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev. 2013;8:CD001822. doi: 10.1002/14651858.CD001822.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Van Eerd D, Saunders R. Integrated knowledge transfer and exchange: An organizational approach for stakeholder engagement and communications. Scholarly and Research Communication. 2017:8(1). doi: 10.22230/src.2017v8n1a274. [DOI] [Google Scholar]