Immunization is well recognized as one of modern medicine’s greatest success stories. Beyond safe water no other intervention has had such a major impact on mortality reduction and population growth [1]. Immunization is underlined as one of the most important measures for improving global health, impacting on countries efforts to achieve 14 of the 17 Sustainable Development Goals [2]. The COVID-19 pandemic has further emphasized the importance and value of having effective vaccines to decrease morbidity and mortality in globally raging viral outbreaks [3]. However, vaccines are only of value if target groups, and individuals, can easily access vaccines and accept to be immunized. Given the critical role vaccines play in control of vaccine preventable infections including the COVID-19 pandemic, much attention has been drawn to COVID-19 vaccine acceptance concerns in many countries [4], [5]. However, even prior to the pandemic, the World Health Organization (WHO) had named vaccine hesitancy as one of the 10 threats to global health [6].
Vaccination decision-making is complex with multiple factors influencing an individual’s decision to accept or not accept a vaccine in a timely fashion. The Strategic Advisory Group of Experts (SAGE) on immunization of WHO defined vaccine hesitancy in 2014 as the “delay in acceptance or refusal of vaccines despite availability of vaccination services. Vaccine hesitancy is complex and context-specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience and confidence” [7]. Vaccine hesitancy and acceptance is very multidimensional with many influencing factors including ease of access, not just demand or individual determinants [8].
All too often white papers, reports, and advice on addressing vaccine hesitancy have focused outward from public health, health systems and government policy perspective not on the needs, barriers, and enablers from each person’s, group’s or community’s perspectives. To help organize thinking and increase understanding of complex areas, health systems and public health propose definitions and models as simplified ways to present challenging areas. Advantages of such models include heightening the attention to complexity, emphasizing a wider range factor groupings that might otherwise easily be overlooked and adding support for higher ordered broadened thinking when designing and implementing targeted interventions to address the problem. Among the disadvantages are that the models may narrow the thinking by homing in on only a few factor categories thus limiting the breadth and scope of the proposed interventions. The plan may completely miss major factor area not included in the model.
To help immunization programs consider the broad range of factors that can influence vaccine hesitancy, SAGE in 2014 presented three overlapping categories – the 3C’s: (“as trust in (i) the effectiveness and safety of vaccines; (ii) the system that delivers them, including the reliability and competence of the health services and health professionals and (iii) the motivations of policy-makers who decide on the needed vaccines”); complacency (“when perceived risks of vaccine-preventable diseases are seen as low, vaccination not deemed a necessary and other life/health responsibilities are seen as more important”) and convenience (“when physical availability, affordability and willingness-to-pay, geographical accessibility, ability to understand (language and health literacy) and appeal of immunization services affect uptake”) [7].
Much attention has been paid to confidence with development of assessment measures [9] such that the term vaccine confidence has come to sometimes be used as a synonym for vaccine hesitancy [10]. In 2016, a broader taxonomy for the determinant factors of vaccine uptake, the 5 A’s, was proposed encompassing the dimensions of Access, Affordability, Awareness, Acceptance, Activation [11] . In 2018, based upon both empirical and theoretical work, the 3C’s model was readjusted, emphasizing the importance of more than confidence, and emerging as the 5C’s model. confidence, complacency, constraints (adjustment of the term convenience to now include both structural and psychological barriers), calculation (preference for deliberation) and collective responsibility (communal orientation). [12].
In 2014 to obtain a more global assessment of vaccine hesitancy, two questions based upon the SAGE definition were added to the WHO/UNICEF annual Joint Reporting Form in which countries provide yearly details and outcomes of their immunization programs. Review of these data over several years found differences in the reported major vaccine hesitancy factors between countries and between WHO regions [13]. While the SAGE definition did appear to be understood, the hesitancy reasons cited were many and varied with some more focused on community issues, others on systems and health providers. Even the most frequently reported category, risk- benefit (scientific evidence e.g., vaccine safety concerns), accounted for less than one quarter of all reasons cited. Another important observation was the lack of validated surveys useful for assessing hesitancy especially in low- and middle-income countries [13]. This led WHO, UNICEF and partners to form a working group focused on the behavioral and social drivers of vaccine uptake. They were charged with developing and validating survey tools that could be used in high-, middle-, and low-income countries to assess vaccine hesitancy [14], [15]. The tools and report will be available in 2022. This working group developed a Behavioral and Social Drivers framework with four components: Thinking and Feeling (perceived disease risk, vaccine confidence), Social processes (social norms, provider recommendation), Motivation (intention to get recommended vaccines) and Practical issues (availability, affordability, ease of access, service quality, respect from provider) [16].
The Royal Society of Canada (RSC) Task Force on COVID-19 subgroup on Vaccine Acceptance was charged with reporting on how to enhance COVID-19 vaccine acceptance in Canada. They reviewed these frameworks in terms of scope and ability to help programs and policy makers envision constructive ways to achieve high COVID-19 vaccine acceptance [17]. A sensitive underbelly of the previous models is that in trying to simplify complex realities important factors may have been missed or overlooked.
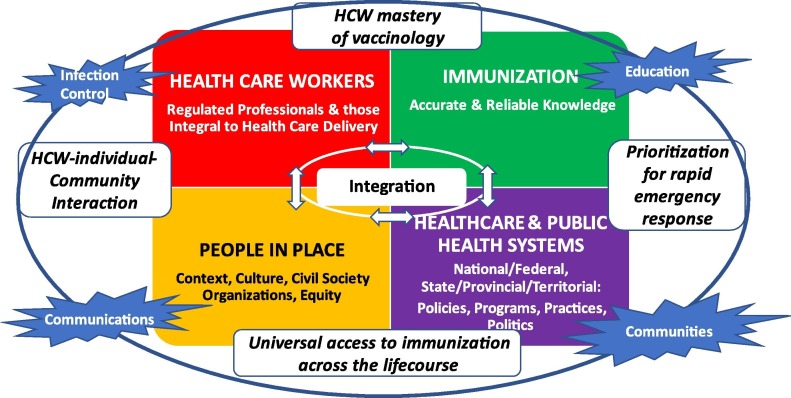
After discussion and review, the RSC subgroup noted that two core elements raised in the Immunization Agenda 2030 – a global strategy: to leave no one behind and immunization across the life course [17] – were not well covered in these models. Furthermore, the legal, regulatory, political, infection control, communication and marked impact of mis/disinformation information on vaccine acceptance in many countries were not highlighted [8]. These models tended to overlook the complex interactions and the influences that culture, politics, historical context, and civil society actions have on an individual’s vaccine acceptance decision and on the community’s valuing of immunization. Vaccine equity has also been raised by the WHO as a global issue [18] and by individual countries as issues within their own country in certain communities [19]. Structural racism, discrimination and imbalance in power, and access to resources are key factors in vaccine acceptance but are rarely covered in these models or are lumped in large meta-categories that are hard to turn into an action. Bearing these gaps in mind, the RSC COVID-19 Vaccine Acceptance subgroup developed a more comprehensive framework that emphasizes complexity, the interconnectivity, and the diversity of factor categories with a focus on COVID-19 vaccine acceptance [8]. The Figure presented is an adapted version of the RSC framework that is applicable to Canada and beyond for both COVID-19 vaccines and for routine vaccines across the life course (see Fig. 1 ).
Fig. 1.
Adapted* Royal Society of Canada Vaccine Uptake Framework for Canada and Beyond. *Adapted from Reference 8 MacDonald NE et al. FACETS 2021; 6:1184–1246.
This Adapted RSC Vaccine Uptake Framework is centered on four major factor domains that influence vaccine uptake including trust in vaccines (people & communities; health care workers (HCW); accurate and reliable immunization knowledge; and the health care system and public health programs). None of the factor domains should be considered in isolation; each impacts on all of the others and all are influenced by the four overarching theme areas (education, infection control, extent of collaborations and communications about the vaccine preventable disease, and the specific vaccine or vaccines) and by the four additional concepts (HCW mastery of vaccinology, HCW individual and community interaction – past and present including political and historical contexts, universal vaccine access across the life course and prioritization for rapid emergency response) to be considered tangentially across the domines and themes. The Adapted RSC Framework visually illustrates complexity, and thus emphasizes that strategies to address vaccine acceptance gaps need to be multifactorial, tailored to fit the individual, the community, the context, the resources and be evidence based [20], [21]. In the Table, for each of the four domains examples of issues are provided with examples of needed actions (see Table 1 ).
Table 1.
The 4 Adapted RSC Framework domains with examples of problems and suggested actions to address.
| Framework domains | Problems | Examples of needed actions |
|---|---|---|
| Health Care Workers: health professionals and other workers integral for care delivery | Contradictory advice from HCW leads to confusion HCW are role model but may be unwilling to be vaccinated themselves |
All HCW involved in immunization, even if indirectly, trained on effective vaccine acceptance strategies, steps to make immunization a more positive experience including immunization pain mitigation All health care workers have access to education about vaccines and immunization best practices that have been co-developed and tailored to fit their needs and vaccine acceptance issues are addressed using evidence-based strategies (e.g., motivational interviewing techniques) |
| People in Place | Negative past history with distrust in health system, government Barriers in access to services |
Active community engagement, recruitment of community leaders and civil society organizations to co-create programs to fit peoples’ needs Access to vaccination be facilitated through mobile clinics, transportation to vaccination sites and help provided for booking appointments |
| Health Care System & Public Health Governments: local, regional, national | Immunization acceptance influenced by program options, government regulations, laws and politics | Programs and policies that support infection control practices at immunization sites; optimize data collection on coverage (who is not immunized); behavioural and social determinants (why not immunized), community outreach and collaboration; and surveillance – epidemiology of VPD, AEFIs, vaccine supply. All need. government support-funding, +/-legislation, education, etc. Health care system, public health and all levels government work together to support effective immunization strategies to increase vaccine acceptance across the life course All jurisdictions recognize immunization as a legally enforceable right by publicly recommending vaccinations in public health or equivalent statutes, and remove barriers that inhibit equitable access. |
| Immunization: accurate reliable knowledge | HCW, the public, community leaders, politicians all need accurate reliable immunization knowledge and ability to recognize and overcome mis/disinformation | Ongoing monitoring in social media to identify rumors and mis/disinformation about vaccines and tailored communication intervention to address that use tools that reach target audience Education on immunization starts in primary school including the scientific method, importance of critical thinking, logic and awareness of strategies used to sell mis/disinformation. The general public, communities, HCW and politicians all need fireproofing to decrease the effect of mis/disinformation on vaccine acceptance |
One of the areas highlighted in the Adapted Framework in the Healthcare and Public Health domain is politics. National/federal, provincial/state, and territorial politics, practices and programs can much affect vaccine decision making. For example, healthcare in Canada is under provincial jurisdiction. Provincial political leaders took different stances on COVID-19 management, vaccine rollout and other COVID-19 control measures. Thus, it should come as no surprise that the rates of COVID-19 vaccine acceptance and COVID-19 deaths have differed across the country [22]. Around the globe one can readily find examples of politics affecting vaccine acceptance [23]. In the United States, the Kaiser Family Foundation tracking of state vaccine acceptance rates has shown major differences along political partisan support lines [24]. However, one needs to be careful about raising prominence of one aspect of one domain as being the critical element in vaccine uptake. Many factors from other domains and themes also had impact. For example, historical mistrust of government amongst indigenous, black, and new immigrant communities and poor ease of access lead to lower uptake rates compared to neighboring communities with differing backgrounds [8].
Concern in many different communities about acquiring COVID-19 while waiting to be immunized with a COVID-19 vaccine led to guidance on infection prevention and control for such settings [25] and infection control being included as a theme in the Framework again emphasizing the complexity and need for broad multifactorial integrative program development thinking. This is not a new concern. Worry about contracting a vaccine preventable disease while waiting to be immunized has been raised in past measles catch up programs during measles outbreaks and in Ebola outbreaks but has not been attended to in the earlier vaccine hesitancy models.
The infodemic has added emphasis to the importance of the accurate and reliable immunization knowledge domain. Social media mis/disinformation has eroded trust in immunization programs, polices and national regulatory agencies [26]. Mis/disinformation has impacted vaccine decisions amongst individuals, groups, health care workers and politicians. But to address this, we need to understand why these discourses resonate and are trusted by some. Where people are at is critical in how susceptible they are to mis/disinformation [27]. When trying to address this complex issue of vaccine uptake amid the infodemic not only do the factors in the People in Place domain need to be considered but also factors in the other domains as well as the roles of three of the theme areas- communication, education, and collaboration.
None of the factors highlighted above fit well in the earlier models. For immunization programs, health care systems, and ministries of health, the easier more straightforward path has been to overlook and/or ignore them when trying to determine how to strengthen vaccine acceptance. The earlier models support focusing on a few factors and ignoring the complexity. Sadly, with COVID-19, vaccine hesitancy has often been oversimplified to being a problem of adherence to counterculture/ non-mainstream views, without consideration of its multifactorial nature. Some influencing factors may have historically legitimate origins such as disrespect, colonization, and poverty. Too often, authorities talk about “the vaccine hesitancy problem” or “trust issues” without a reflection on how the programs are delivered and other key underlying impactful factors.
Broader and more expansive thinking about vaccine uptake is needed if we are to achieve high COVID-19 vaccine and routine immunization coverage. Even using terms like vaccine hesitancy and vaccine acceptance maybe stopping broader more integrated thinking. Health care systems, public health and especially governments should not hide behind vaccine hesitancy as being unfixable [28]. While oversimplified or narrowly focused views of barriers to immunization have led to truncated approaches to interventions with limited or no impact on vaccine uptake; multifactorial interventions can make a difference. There are no simple solutions. All aspects of the Adapted RSC Framework must be considered, especially for peoples and communities with low uptake. Community engagement and co-creation of immunization programs that fit their needs do work. The Adapted RSC Framework is a steppingstone to prod broader more comprehensive thinking on vaccine uptake. Given that the Immunization Agenda 2030 approved by the World Health assembly in 2020 emphasizes immunization across the life course and leaving no one behind, we must address vaccine hesitancy in all its guises, regularly adapting and revising our programs and be ready to readapt as the needs, concerns, contexts of our communities change and/or vaccines and science evolves.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Rodrigues C.R., Plotkin S.A. Impact of vaccines; health, economic and social perspectives. Front Microbiol. 2020;11:1526. doi: 10.3389/fmicb.2020.01526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gavi The Vaccine Alliance. Immunization and the sustainable development goals. Gavi The Vaccine Alliance. [Online] September 2019. [cited: October 29, 2021]. <https://www.gavi.org/sites/default/files/document/2019/Immunisation%20and%20the%20SDGs%20%281%29.pdf>.
- 3.Moghadas SM, Vilches TN, Zhang K, Wells CR, Shoukat A, Singer BH, et al. The impact of vaccination on COVID-19 outbreaks in the United States. Clin Infect Diseases 2021;online ahead of print. [DOI] [PMC free article] [PubMed]
- 4.Piltch-Loeb R., Harriman N.W., Healey J., Bonetti M., Toffolutti V., Testa M.A., et al. COVID-19 vaccine concerns about safety, effectiveness, and policies in the United States, Canada, Sweden, and Italy among Unvaccinated Individuals. Vaccines. 2021;9:1138. doi: 10.3390/vaccines9101138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nehal K.R., Steendam L.M., Campos Ponce M., van der Hoeven M., Smit G.S.A. Worldwide vaccination willingness for COVID-19: a systematic review and meta-analysis. Vaccines (Basel) 2021;9:1071. doi: 10.3390/vaccines9101071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Ten threats to global health 2019. World Health Organization; 2019. <https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019>.
- 7.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 8.MacDonald N.E., Comeau J., Dubé È., Graham J., Greenwood M., Harmon S., et al. Royal society of Canada COVID-19 report: Enhancing COVID-19 vaccine acceptance in Canada. FACETS. 2021;6:1184–1246. [Google Scholar]
- 9.Larson H.J., de Figueiredo A., Xiahong Z., Schulz W.S., Verger P., Johnston I.G., et al. Global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dudley M.Z., Privor-Dumm L., Dubé È., MacDonald N.E. Words matter: Vaccine hesitancy, vaccine demand, vaccine confidence, herd immunity and mandatory vaccination. Vaccine. 2020;38(4):709–711. doi: 10.1016/j.vaccine.2019.11.056. [DOI] [PubMed] [Google Scholar]
- 11.Thomson A., Robinson K., Vallée-Tourangeau G. The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34(8):1018–1024. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 12.Betsch C., Schmid P., Heinemeier D., Korn Holtmann C., Bohm R. Beyond confidence: development of a measure assessing thethe 5C psychological antecedents of vaccination. PLoS ONE. 2018;13:e0208601. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lane S., MacDonald N.E., Marti M., Dumolard L. Vaccine hesitancy around the globe: analysis of three years of WHO/UNICEF joint reporting form data-2015–2017. Vaccine. 2018;36(26):3861–3867. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meeting of the strategic advisory group of experts on immunization, 22–24 March 2021: conclusions and recommendations. World Health Organization, Strategic Group of Experts on Immunization. 22, June 4, 2021, Weekly Epidemiology Record, vol. 96. p. 197–216.
- 15.World Health Organization, Department of Immunization, Vaccines and Biologicals (IVB). Strategic Advisory Group of Experts in Immunization 4–8 October 2021 meeting; background materials. [Online] 2021 [cited: October 28, 2021]. <https://terrance.who.int/mediacentre/data/sage/SAGE_eYB_Oct2021.pdf>.
- 16.—. Strategic advisory group of experts in immunization 4–8 October 2021 metting; background materials. Geneva: World Health Organization; 2021.
- 17.World Health Organization . World health Organization; Geneva: 2020. Immunization Agenda 2030: A global strategy to leave no one behind; pp. 1–60. [Google Scholar]
- 18.—. Vaccine Equity. World Health Organization. [Online] 2021 [cited: October 29, 2021]. <https://www.who.int/campaigns/vaccine-equity>.
- 19.Kamal A., Hodson A., Pearce J.M. A rapid systematic review of factors influencing COVID-19 vaccination uptake in minority ethnic groups in the UK. Vaccines (Basel) 2021;9:1121. doi: 10.3390/vaccines9101121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dube E., Ward J.K., Verger P., MacDonald N.E. Vaccine hesitancy, acceptance and anitvaccination: trends and future prospects for public health. Annu Rev Public Health. 2021;42:175–191. doi: 10.1146/annurev-publhealth-090419-102240. [DOI] [PubMed] [Google Scholar]
- 21.Dubé E., Bettinger J.A., Fisher W.A., Naus M., Mahmud S.M., Hilderman T. Vaccine acceptance, hesitancy and refusal in Canada: challenges and potential approaches. Can Comm Dis Rep. 2016;42:246–251. doi: 10.14745/ccdr.v42i12a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goverment of Canada. National Vaccination Coverage. COVID-19 vaccinaiton in Canada. [Online] February 13, 20 [cited: February 25, 2022]. <https://health-infobase.canada.ca/covid-19/vaccination-coverage/#a5>.
- 23.Gramacho W.G., Turgeon M. When politics collides with public health: COVID-19 vaccine country of origin and vaccination acceptance in Brazil. Vaccine. 2021;39(19):2608–2612. doi: 10.1016/j.vaccine.2021.03.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kates J, Tolbert J, Orgera K. The red/blue divide in COVID-19 vaccination rates. Kaiser Family Foundation CoronaVirus (COVID-19). [Online] September 14, 2021 [cited: February 25, 2022]. <https://www.kff.org/policy-watch/the-red-blue-divide-in-covid-19-vaccination-rates/>.
- 25.Commeau J. Royal Society of Canada; Ottawa: 2021. Keeping everyone safe: infection prevention and control in COVID-19 vaccine clinics; pp. 1–3. [Google Scholar]
- 26.Nahum A, Drekonja DM, Alpern JD. The erosion of public trust and SARS-CoV-2 vaccines-more action is needed. Open Forum Infect Dis 2021;8:ofaa657. [DOI] [PMC free article] [PubMed]
- 27.Scherer L.D., McPhetres J., Pennycook G., Kempe A., Allen L.A., Knoepke C.E., et al. Who is susceptible to online health misinformation? A test of four psychosocial hypotheses. Health Psychol. 2021;40:274–284. doi: 10.1037/hea0000978. [DOI] [PubMed] [Google Scholar]
- 28.Attwell K., Hannah A., Leask J. COVID-19: talk of ‘vaccine hesitancy’ lets governments off the hook. Nature. 2022;602(7898):574–577. doi: 10.1038/d41586-022-00495-8. [DOI] [PubMed] [Google Scholar]