Abstract
Introduction
The Coronavirus disease (COVID-19) pandemic has significantly altered the provision of rehabilitation services, especially pulmonary rehabilitation (PR). Our objective was to assess the provision of PR services in Latin America 18 months after the COVID-19 pandemic was declared.
Methods
A cross-sectional study that included professionals dedicated to PR in centres in Latin America was applied. Responses to an online questionnaire were collected from May to September 2021. The following data were included for the analysis: demographic data, evaluation strategies, program structure, PR intervention in post-COVID-19 patients, and perception of strategies therapies for the care of post-COVID-19 patients. The questionnaire was distributed in Spanish and Portuguese languages.
Results
Responses were received from 196 PR centres. Exercise tolerance was predominantly measured with the six-minute walk test. Less than 50% of the institutions evaluate quality of life, physical qualities, symptoms, and lung function. Most of the programmes have physiotherapists (90.8%), as well as pulmonologists (60%), and psychologists (35%), among other professionals.
Conclusion
PR services in Latin America have adapted in their way to the requirements of the pandemic, and most continued to provide face-to-face services. It was identified that the application of the programs is heterogeneous both in evaluations and interventions.
Keywords: Pulmonary rehabilitation, Latin America, post-COVID-19, survey
Introduction
Rehabilitation is an essential component in healthcare and management, helping to improve functional capacity, prevent both acute and chronic diseases and promote health and wellbeing. 1 According to the World Health Organisation (WHO) 2 the rehabilitation services benefit society, individuals, communities, and contribute in economic aspects of the countries, contributing to their social development.3,4
The world is currently experiencing a major health crisis due to the ongoing Coronavirus Disease 19 (COVID-19) pandemic, which has affected global healthcare across the board. Among the services that have been affected, research reports detail that at the beginning of the pandemic, hospitals are being forced to convert PR units and health teams into units of respiratory management for COVID-19 patients, wich caused an impact on the opportunity and changes in care compared to pre-pandemic periods, both in people with chronic lung diseases and in post-COVID patients. 4
In recent months, the scientific literature has used the term ‘long COVID’ to describe the disease in people who have recovered from COVID-19 but still have very long-lasting symptoms and signs after infection. WHO defines it as a condition that “occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis”. 5 Post-discharge sequelae and their impact on health-related quality of life (HRQoL) are not fully understood. Among the most reported symptoms of long COVID are fatigue and dyspnoea, which play an essential role in limiting activities of daily living and the ability to exercise. 6
According to 2016 data, Latin America has a high percentage of mortality due to poor quality of care. 7 Based on which, countries or regions with lower levels of quality of care have been projected to have higher mortality rates from COVID-19. 8 In the Latin American region, failures of health systems to prevent and control chronic diseases adequately are likely to result in a higher percentage of the population at risk of developing complications related to COVID-19 and long COVID. In addition to the targeted response, public health emergencies present significant challenges for health systems to meet the essential health needs of the population, and gaps in quality of care tend to be wider. 9
In recent years, policies have been implemented to considerably increase care for chronic non-communicable diseases and rehabilitation centres in different Latin American countries, particularly in the respiratory area. 10 In 2016, the Pan American Health Organization, in conjunction with the WHO, published a study on the economic dimensions of chronic non-communicable diseases, reinforcing the importance of access to rehabilitation services to improve equity in health promotion. 11 However, the increase in the need for services, such as emergency and critical care, redeployed rehabilitation services personnel. Additionally, the changes in health policies that promoted self-isolation for health reasons led to the suspension and/or limitation of the operation of the rehabilitation services at the time of prioritising care, which has negatively impacted patients with disabilities, chronic respiratory diseases, but also those with acute illnesses or serious trauma not related to COVID-19 due to the lack of health resources. 4
Fortunately, the start of vaccination has allowed a return to relative normality, and rehabilitation centres have started caring for respiratory patients, but not without facing a series of challenges of this new type of patient and health conditions. Due to the above, the objective of this study was to assess the provision of PR services in Latin America 18 months after the COVID-19 pandemic was declared.
Methods
Study design
Cross-sectional observational study included professionals representing PR centres from all Latin American countries. Responses to an online questionnaire disseminated between May and September 2021 were collected (Supplementary Material 1). Participants were invited using the registry of the Latin American Thoracic Association (ALAT); also by mass dissemination using official social networks of the association (Facebook, Twitter, Instagram). The study was approved by the ALAT respiratory care committee and by the institutional ethics committee with registry IYECDO-1372.
Survey
The survey was designed by a committee of experts who incorporated the preliminary questions. The construction of the questions was based on the ATS/ERS recommendation guidelines for pulmonary rehabilitation. 12 Subsequently, and after an additional review, they were sent to five independent reviewers selected for their experience in the area of PR and the management of patients with post-COVID-19. After receiving the recommendations, the final version was obtained, which had five sections and a total of 31 questions (Supplementary Material 1). We follow the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) recommendations for preparing online questionnaires. 13
The sections included were: Demographic data of PR programmes, evaluation and intervention strategies, programme structure, PR in post-COVID-19 patients, and perception of therapeutic strategies for the care of post-COVID-19 patients. The questionnaire was distributed in Spanish and Portuguese, and, according to the responses obtained, the results were filtered by PR centres, and the first response obtained was selected, eliminating repeated centres. The first page of the questionnaire contained informed consent.
The survey was designed with an ‘open survey’ system. The participants' responses were stored with a NUMID number on an encrypted server. Therefore, there was no incentive for the participants.
Statistical analysis
The analysis of the data obtained with the survey was carried out with GraphPad Prism version 9.0 (GraphPad Software, San Diego, CA, USA), the variables were placed in categories which are presented in frequencies and percentages.
Results
Demographics of PR programmes
During the evaluation period, responses were received in total from 196 PR centres from 14 countries; of these 196, 15 responses from centres that had already responded to the survey were excluded; the countries from which the greatest data participation was obtained were Chile, Argentina, Colombia, Mexico and Ecuador (Table 1). Most of the responses were provided by physiotherapists, representing 65.7%, followed by respiratory therapists (18.2%) and physicians (14.4%).
Table 1.
Distribution of responses by country.
| Countries | n (%) |
|---|---|
| Chile | 39 (21.5) |
| Argentina | 38 (21) |
| Colombia | 34 (18.8) |
| México | 24 (13.3) |
| Ecuador | 15 (8.3) |
| Perú | 10 (5.5) |
| Brazil | 5 (2.8) |
| Costa Rica | 4 (2.2) |
| El Salvador | 4 (2.2) |
| Bolivia | 3 (1.7) |
| Venezuela | 2 (1.1) |
| Cuba | 1 (0.6) |
| Guatemala | 1 (0.6) |
| Uruguay | 1 (0.6) |
| The profession of the person who answered the survey | |
| Physiotherapist | 119 (65.7) |
| Respiratory therapist | 33 (18.2) |
| Physician | 26 (14.4) |
| Speech therapist | 2 (1.1) |
| Occupational therapist | 1 (0.6) |
Evaluation and intervention strategies for PR programmes
Regarding the evaluations carried out at the beginning and the end of the PR intervention, most programmes review the medical history, measure vital signs at rest and with effort (heart rate, oxygen saturation, and respiratory rate), and apply dyspnea scales. Regarding effort tolerance evaluations, the six-minute walk test (6MWT) is the most used (69.4%), both at the beginning and end of the programmes. More than half of those who responded to the survey report that they carry out an evaluation of the strength of the upper and lower limbs before and after PR.
In both pre-assessment and post-PR assessments, less than 50% of the institutions perform HRQoL, physical qualities, symptoms and spirometry assessments to assess lung function (Table 2).
Table 2.
Distribution of evaluation activities.
| Top 10 evaluation activities | Start n (%) | End n (%) |
|---|---|---|
| Review of clinical history | 192 (98) | 145 (74) |
| Taking vital signs at rest and with effort | 191 (97.4) | 174 (88.8) |
| Dyspnoea scales | 167 (85.2) | 153 (78.1) |
| Six-minute walk test | 136 (69.4) | 134 (68.4) |
| Upper extremity strength assessment | 120 (61.2) | 107 (54.6) |
| Lower extremity strength assessment | 112 (57.1) | 96 (49) |
| Muscle fatigue scales | 108 (55.1) | 99 (50.5) |
| Quality of life survey | 87 (44.4) | 75 (38.3) |
| Evaluation of physical qualities | 86 (43.9) | 88 (44.9) |
| Spirometry | 85 (43.4) | 81 (41.3) |
Strength training using dumbbells or free weights is the most used muscle training strategy (74%), followed by respiratory muscle training (69.9%). Among the tools used for aerobic training, the cycle ergometer is the most used by 69.9% of the centres surveyed, followed by treadmill training (54.1%) and circuit training (35.7%). Within the adjuvant strategies, respiratory physiotherapy (76.5%) and self-care education (76%) are the most applied, while only 21.9% and 16.8% have occupational therapy and speech therapy services, respectively.
The prescription of exercise intensity is carried out mainly with subjective symptom scales (Borg Scale) (78.1%), exercise response with vital signs (71.4%) and heart rate equations (66.8%); peak (21.4%) and estimated (36.2%) oxygen consumption are used marginally (Table 3).
Table 3.
Distribution of intervention activities.
| Intervention strategies | n (%) |
|---|---|
| Strength/endurance training using free weights | 145 (74) |
| Respiratory muscle training | 137 (69.9) |
| Cycleorgometer | 137 (69.9) |
| Strength training using apparatus | 115 (58.7) |
| Treadmill walk | 106 (54.1) |
| Community walk | 84 (42.9) |
| Circuit training | 70 (35.7) |
| Water training | 11 (5.6) |
| Nordic walk | 8 (4.1) |
| Nordic platform | 7 (3.6) |
| Coadjuvant interventions | |
| Respiratory physiotherapy | 150 (76.5) |
| Self-care education | 149 (76) |
| Flexibility exercises | 131 (66.8) |
| Energy conservation techniques | 120 (61.2) |
| Nutritional support | 86 (43.9) |
| Smoking cessation | 83 (42.4) |
| Psychosocial support | 68 (34.7) |
| Occupational therapy | 43 (21.9) |
| Speech therapy | 33 (16.8) |
| Methods for prescribing intensity | |
| Effort perception with Borg scale | 153 (78.1) |
| Use of vital signs | 140 (71.4) |
| Calculated maximum heart rate | 131 (66.8) |
| Estimated oxygen consumption | 71 (36.2) |
| Peak oxygen consumption | 42 (21.4) |
PR programme structure
Table 4 shows the characteristics of the programmes, which, in 90.8%, have a physiotherapist and 59.2% have a pulmonologist. Professionals such as dietitians and medical specialists such as cardiologists, internists, and physiatrists participate in less than 40% of PR centres in Latin America. Patients attend PR mainly on an outpatient basis (74.5%), with a duration of the programme ranging mostly between four and 8 weeks (40.3%). The most used training frequency is three sessions a week (40.8%). Regarding the session duration, the centres mostly reported duration of between 40 and 60 min (44.9%). Only 13% of the programmes reported that the sessions lasted more than 60 min. More than half carry out controls after discharge from PR (58.2%); of these, 30.1% are followed up to 3 months, 12.8% up to 6 months, 3.6% up to one year, and 11.7% until functional recovery of the patients., 49.5% of the centres that reported post-PR controls said they did it face-to-face.
Table 4.
Administrative characteristics of the programmes.
| Professional | n (%) |
|---|---|
| Physiotherapist | 178 (90.8) |
| Pulmonologist | 116 (59.2) |
| Psychologist | 68 (34.7) |
| General practitioner | 64 (32.7) |
| Nutritionist | 60 (30.6) |
| Cardiologist | 48 (24.5) |
| Internal medicine | 46 (23.5) |
| Physiatrist | 44 (22.4) |
| Type of assistance | |
| Outpatient | 146 (74.5) |
| Home-based | 81 (41.3) |
| Inpatient | 75 (38.3) |
| Telerehabilitation | 73 (37.2) |
| Community-based | 9 (4.6) |
| Physician in charge of referring patients | |
| Pulmonologist | 131 (66.8) |
| General practitioner | 107 (54.6) |
| Physiatrist | 60 (30.6) |
| Autoreferred | 40 (20.4) |
| Duration | |
| <4 weeks | 21 (11.6) |
| >4 and <8 weeks | 73 (40.3) |
| >8 and <12 weeks | 50 (27.6) |
| >12 weeks | 27 (14.9) |
| Number of PR sessions per day | |
| 1–5 | 60 (33.1) |
| 6–10 | 45 (24.9) |
| 10–15 | 18 (9.9) |
| 15–20 | 24 (13.3) |
| >20 | 34 (18.8) |
| Frequency of supervised sessions (per week) | |
| 1 | 19 (10.5) |
| 2 | 57 (31.4) |
| 3 | 74 (40.8) |
| >3 | 31 (17.1) |
| Follow-up post-PR | |
| No | 82 (41.8) |
| Until 3 months post-discharge | 59 (30.1) |
| Until 6 months post-discharge | 25 (12.8) |
| Until 12 months post-discharge | 7 (3.6) |
| Undefined | 23 (11.7) |
| Follow-up system post-PR | |
| Face-to-face | 90 (49.5) |
| Telephone | 67 (32.7) |
| Telemedicine | 49 (25) |
Perception of therapeutic strategies of post-COVID-19 patients
Since the WHO’s declaration of the pandemic in March 2020, 56 centres did not continue with face-to-face care during confinement, with a suspension that mostly lasted 6 months (32.6%), and 14.6% between 1 and 3 months. However, 42% of those surveyed responded that non-COVID-19 patients continued with the same adherence prior to the health emergency. The availability of personnel and biosafety requirements were the ones that mainly caused adjustments in service times (Table 5).
Table 5.
Modifications in PR programmes after the pandemic.
| Continuation of care during confinement | n (%) |
|---|---|
| Yes | 125 (69.1) |
| No | 56 (30.9) |
| Adherence of non-COVID-19 patients | |
| Similar | 76 (42) |
| >50% of patients continue | 34 (18.8) |
| <50% of patients continue | 71 (39.2) |
| Causes of change in attending time | |
| Number of patients | 21 (11.6) |
| Staff available | 59 (32.6) |
| Severity of patients | 7 (3.9) |
| Biosecurity requirements | 30 (16.6) |
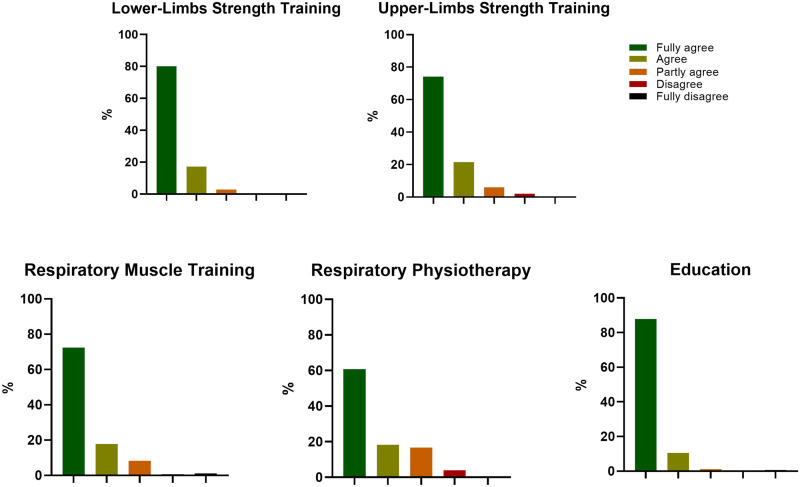
Figure 1 shows that the centres mostly agree with strategies such as upper limb training, in which 74% of the participants state that they agree, 80% of those surveyed state that they agree with the training of lower limbs, and 72.4% with respiratory muscles for post-COVID-19 patients. In addition, coadjuvant strategies such as respiratory physiotherapy techniques and education also obtained high approval (60.8 and 87.8%, respectively), where more than half of those surveyed agreed to use these strategies in patients who had SARS-CoV-2 infection.
Figure 1.
Perception of therapeutic strategies for the care of post-COVID-19 patients.
Discussion
Eighteen months after the declaration of the pandemic, according to the results obtained, the activity of RP programs in Latin America has been gradually resumed; more than half of the programs that suspended their service resumed activities in a maximum period of 6 months, this is partly due to the need for rehabilitation not only from post-COVID-19 patients but also from other diseases; however, we do not know if the activities carried out are in completely regular operation. Due to the high epidemiological impact that has occurred in Latin America, 14 all pulmonary rehabilitation programs surveyed have received COVID-19 patients, having to make the necessary adjustments to sustain the services despite the difficulties of this period of time. Despite recommendations for PR implementation, these programmes in Latin America are heterogeneous, both in the evaluation and in the intervention in post-COVID-19 patients. Nevertheless, through ALAT, it was possible to disseminate and format a diagnosis on PR in Latin America.
PR is based on an interdisciplinary and comprehensive intervention that includes aerobic and resistance training and adjuvant interventions such as education, management of nutritional aspects, or psychology, which all contribute to improving HRQoL. 12 Less than 50% of PR programmes assess HRQoL, which is a crucial aspect to consider according to different clinical recommendations,15,16 being one of the most affected factors in subjects hospitalised for COVID-19.17,18 Several studies have used generic and specific questionnaires, among which the 36-item Short-Form Health Survey (SF36), the Euro Qol-5 dimension (EQ-5D) and the St George’s Respiratory Questionnaire (SGRQ) stand out.18,19
Several of these questionnaires are available free of charge for use in these patients and can also be applied self-directed. Also, it is necessary to discuss that the quality of life is significantly affected in patients with other chronic lung diseases, such as chronic obstructive pulmonary disease (COPD), 20 asthma, 21 interstitial lung disease (ILD) 22 and pulmonary hypertension. 23 This situation must be considered by the programs so that in the future, with the results obtained in the evaluations, intervention strategies are established according to the needs of the patients.
In contrast, the low rate of performing spirometry is an expected result given that the recommendations for their evaluation are ideally two or 3 months after hospital discharge in post-COVID patients due to the effects of inflammation and post-viral oedema, this could affect the result of this test. Also, several centres do not have the equipment or trained personnel to carry out the tests.24,25
Concerning the evaluation of patients, only half of the PR programmes evaluate fatigue, despite being the most prevalent symptom in post-COVID-19 patients. 6 This symptom, and dyspnoea, are two of the main outcomes of interest to the patient (PROMs) 26 and should be used to complement the results of other evaluations used in PR programmes, such as exercise tests. 27 However, and clarifying that it was not an objective of this paper to measure the use of spirometry in other chronic lung diseases, its use is scarce, especially considering that spirometry is a diagnostic test in COPD and asthma, its inclusion is imperative, within the initial evaluation protocols.
In this sense, the evaluation of fatigue and dyspnoea should be considered, since their assessment does not involve additional time, and the results can be effectively used to monitor and evaluate the results obtained, especially since these symptoms are prevalent in various stages of COVID-19, from active disease, but also in immediate evaluations after overcoming the infection, and even months later. 28 Likewise, in other pathologies such, dyspnea and fatigue are very frequent and relevant symptoms, which have been shown to improve with PR intervention, not only in COPD, 29 but also in asthma, ILD, as others, 12 a situation that requires Latin American programs to pay attention to this and make the corresponding assessments.
Regarding the structure of PR programmes, although the recommendations propose an interdisciplinary model, 30 this does not happen in Latin America. Only 40% of the programmes had nutrition and psychosocial support, and 21.9% had occupational therapy and 16.8% included speech therapy. Undoubtedly, in order to achieve the greatest possible effect, the programmes must have this multidisciplinary team, increasing the participation of all professionals (particularly occupational therapists and speech therapists). This would allow to comprehensively rehabilitate those patients who remain with disorders due to prolonged intubation or tracheostomy and those whose activities of daily living are significantly limited.4,31
The clinical guidelines recommend interdisciplinary interventions, where personnel other than those in charge of pharmacological prescription and training are included. This is why the shortage of associated professionals could reduce the quality of the interventions; especially considering that patients with post-COVID-19 suffer from residual anxiety and depression32,33 and nutritional disorders. 34
According to the results obtained, in Latin America, the two main ways of prescribing exercise are through the Borg scale and % of predicted maximum heart rate (HR). Both forms have the advantage of being simple tools to apply, allowing their use in low-resource PR programmes.35,36 In the case of the Borg scale, its use has been recommended by clinical guidelines.37,38 On the other hand, the scenario is different in HR, a tool that should be used with caution, both in general patients and particularly in post-COVID-19 patients, who have been shown to present alterations in the autonomic nervous system. 39 It has been shown that the values of the HR at rest and during exertion are high and also could be higher in patients that have cardiometabolic comorbidities in which they use drugs that attenuate the heart rate response to exertion, so their interpretation may be affected, 40 therefore, its use must be evaluated individually patient by patient.
The low use of tests such as the 6MWT and the cardiopulmonary exercise test is striking; evaluations have been widely used in the literature and allow predetermining training loads objectively. 41 In addition, there is little use of tests such as the sit-to-stand test, which has been highly recommended in post-COVID-19 patients.42–44 This information reflects that there is potentially little training in the rehabilitation services, considering that exercise capacity measures are essential for the evaluation of PR programmes.
During the pandemic, there has been a significant increase in telerehabilitation programmes. 45 These have been shown to provide the same benefit as an outpatient programme and a more significant effect when compared to no intervention. 46 However, in Latin America, our data show that face-to-face rehabilitation is still the main form of rehabilitation and that telerehabilitation programmes are approximately half. However, although this number continues to be low, it is probably higher than what existed before the pandemic, although reports of programmes of this type are almost non-existent.
Our study has limitations. One of them is that we cannot know precisely how representative our data is concerning all PR centres in Latin America. However, we believe that it is high since we obtained 196 responses. In a recent study supported by ALAT, a census of pulmonary rehabilitation centres was carried out prior to the pandemic, and 217 were detected. 10 Therefore, the survey that we sent was answered by 196 centres, corresponding to 90% of the places. However, we believe that there may be a bias in the initial information since there may be PR centres that ALAT does not register for two reasons: (1) that the professionals are not affiliated with ALAT, or (2) Centres that were opened after the pandemic, given the number of patients who have been left with sequelae.
Conclusions
In conclusion, due to the pandemic, and after 18 months of its course, negative impacts were observed in PR centres in Latin America, the closure of programs temporarily, the intensification of biosafety measures, changes in the levels of adherence of patients with other pathologies were presented. Despite the existence of recommendations and guidelines for the implementation of PR programmes, their implementation in Latin America is heterogeneous, both considering the evaluation aspects of post-COVID-19 patients and the aspects of the execution of the PR intervention. Therefore, we recommend that regional scientific societies, such as ALAT, should adopt dissemination and incentive programmes in association with national societies to promote and disseminate clinical and scientific aspects of the importance of PR.
Supplemental Material
Supplemental Material sj-pdf-1-crd-10.1177_14799731221104102 for Provision of pulmonary rehabilitation in Latin America 18 months after the COVID-19 pandemic: A survey of the Latin American Thoracic Association by Vicente Benavides-Cordoba, Marisol Barros-Poblete, Rodolfo P Vieira, Guillermo Mazzucco, Guilherme Fregonezi and Rodrigo Torres-Castro in Chronic Respiratory Disease
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Marisol Barros-Poblete https://orcid.org/0000-0002-3288-5363
Rodrigo Torres-Castro https://orcid.org/0000-0001-7974-4333
References
- 1.Ilyas A, Naiz A, Abualait T, et al. The impact of COVID-19 pandemic on rehabilitation services in a tertiary care hospital in the eastern region of Saudi Arabia: a single-center study. Cureus 2021; 13: e18303–e18303. DOI: 10.7759/cureus.18303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mills J-A, Cieza A, Short SD, et al. Development and validation of the WHO rehabilitation competency framework: a mixed methods study. Arch Phys Med Rehabil 2021; 102: 1113–1123. DOI: 10.1016/J.APMR.2020.10.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . World report on disability 2011, 2011. [PubMed] [Google Scholar]
- 4.Rivera-Lillo G, Torres-Castro R, Fregonezi G, et al. Challenge for rehabilitation after hospitalization for COVID-19. Arch Phys Med Rehabil 2020; 101: 1470–1471. DOI: 10.1016/J.APMR.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soriano JB, Ancochea J. On the new post COVID-19 condition. Archivos de Bronconeumología (English Edition) 2021; 57: 735–736. DOI: 10.1016/J.ARBRES.2021.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanchez-Ramirez DC, Normand K, Zhaoyun Y, et al. Long-term impact of COVID-19: a systematic review of the literature and meta-analysis. Biomedicines 2021; 9: 900. DOI: 10.3390/biomedicines9080900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kruk ME, Gage AD, Joseph NT, et al. Mortality due to low-quality health systems in the universal health coverage era: a systematic analysis of amenable deaths in 137 countries. The Lancet 2018; 392: 2203–2212. DOI: 10.1016/S0140-6736(18)31668-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirby T. South America prepares for the impact of COVID-19. The Lancet Respir Med 2020; 8: 551–552. DOI: 10.1016/S2213-2600(20)30218-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ezequiel GE, Jafet A, Hugo A, et al. The COVID-19 pandemic: a call to action for health systems in Latin America to strengthen quality of care. Int J Qual Heal Care J Int Soc Qual Heal Care 2021; 33. DOI: 10.1093/INTQHC/MZAA062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barreto GZ, Ivanaga IT, Chiavegato L, et al. Perspective of pulmonary rehabilitation centers in Latin America. COPD: J Chronic Obstructive Pulm Dis 2021; 18: 401–405. DOI: 10.1080/15412555.2021.1934822 [DOI] [PubMed] [Google Scholar]
- 11.Economic dimensions of non-communicable disease in Latin America and the Caribbean. disease control priorities. 3. ed. Companion Volume n.d. https://iris.paho.org/handle/10665.2/28501 (accessed 10 December 2021).
- 12.Spruit MA, Singh SJ, Garvey C, et al. An official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013; 188: e13–e64. DOI: 10.1164/rccm.201309-1634st/suppl_file/executive_summary.pdf [DOI] [PubMed] [Google Scholar]
- 13.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 2004; 6: e34. DOI: 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ashktorab H, Pizuomo A, González NAF, et al. A comprehensive analysis of COVID-19 impact in Latin America. Res Sq 2021. DOI: 10.21203/RS.3.RS-141245/V1 [DOI] [Google Scholar]
- 15.Barker-Davies RM, O’Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med 2020; 54: 949–959. DOI: 10.1136/BJSPORTS-2020-102596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agostini F, Mangone M, Ruiu P, et al. Rehabilitation setting during and after Covid-19: an overview on recommendations. J Rehabil Med 2021; 53: jrm00141. DOI: 10.2340/16501977-2776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One 2020; 15: e0243882. DOI: 10.1371/journal.pone.0243882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poudel AN, Zhu S, Cooper N, et al. Impact of Covid-19 on health-related quality of life of patients: A structured review. PLoS One 2021; 16: e0259164–e0259164. DOI: 10.1371/journal.pone.0259164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo L, Lin J, Ying W, et al. Correlation study of short-term mental health in patients discharged after coronavirus disease 2019 (COVID-19) infection without comorbidities: a prospective study. Neuropsychiatr Dis Treat 2020; 16: 2661–2667. DOI: 10.2147/NDT.S278245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osadnik CR, Singh S. Pulmonary rehabilitation for obstructive lung disease. Respirology 2019; 24: 871–878. DOI: 10.1111/RESP.13569 [DOI] [PubMed] [Google Scholar]
- 21.de Albornoz SC, Chen G. Relationship between health-related quality of life and subjective wellbeing in asthma. J Psychosomatic Res 2021; 142: 110356. DOI: 10.1016/j.jpsychores.2021.110356 [DOI] [PubMed] [Google Scholar]
- 22.Kanjrawi AA, Mathers L, Webster S, et al. Nutritional status and quality of life in interstitial lung disease: a prospective cohort study. BMC Pulm Med 2021; 21: 51. DOI: 10.1186/S12890-021-01418-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarzynska K, Swiatoniowska-Lonc N, Dudek K, et al. Quality of life of patients with pulmonary arterial hypertension: a meta-analysis. Eur Rev Med Pharmacol Sci 2021; 25: 4983–4998. DOI: 10.26355/EURREV_202108_26455 [DOI] [PubMed] [Google Scholar]
- 24.George PM, Barratt SL, Condliffe R, et al. Respiratory follow-up of patients with COVID-19 pneumonia. Thorax 2020; 75: 1009–1016. DOI: 10.1136/thoraxjnl-2020-215314 [DOI] [PubMed] [Google Scholar]
- 25.Sibila O, Molina-Molina M, Valenzuela C, et al. Documento de consenso de la Sociedad Española de Neumología y Cirugía Torácica (SEPAR) para el seguimiento clínico post-COVID-19. Open Respir Arch 2020; 2: 278–283. DOI: 10.1016/J.OPRESP.2020.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wong AW, Shah AS, Johnston JC, et al. Patient-reported outcome measures after COVID-19: a prospective cohort study. Eur Respir J 2020; 56: 2003276. DOI: 10.1183/13993003.03276-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meys R, Stoffels AAF, Houben-Wilke S, et al. Association between patient-reported outcomes and exercise test outcomes in patients with COPD before and after pulmonary rehabilitation. Health Qual Life Outcomes 2020; 18: 300. DOI: 10.1186/S12955-020-01505-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goërtz YMJ, Van Herck M, Delbressine JM, et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Research 2020; 6: 00542. DOI: 10.1183/23120541.00542-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mccarthy B, Casey D, Devane D, et al. Pulmonary rehabilitation for chronic obstructive pulmonary disease. The Cochrane Database Systematic Reviews 2015; 2015: CD003793. DOI: 10.1002/14651858.CD003793.PUB3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parker AM, Brigham E, Connolly B, et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: a multidisciplinary model of care. The Lancet Respir Med 2021; 9: 1328–1341. DOI: 10.1016/S2213-2600(21)00385-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pizarro-Pennarolli C, Sánchez-Rojas C, Torres-Castro R, et al. Assessment of activities of daily living in patients post COVID-19: a systematic review. PeerJ 2021; 9: e11026. DOI: 10.7717/peerj.11026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mazza MG, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun 2020; 89: 594–600. DOI: 10.1016/J.BBI.2020.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deng J, Zhou F, Hou W, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID‐19 patients: a meta‐analysis. Ann New York Acad Sci 2021; 1486: 90–111. DOI: 10.1111/nyas.14506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mechanick JI, Carbone S, Dickerson RN, et al. Clinical nutrition research and the COVID‐19 pandemic: a scoping review of the ASPEN COVID‐19 task force on nutrition research. J Parenter Enteral Nutr 2021; 45: 13–31. DOI: 10.1002/JPEN.2036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Colberg SR, Swain DP, Vinik AI. Use of heart rate reserve and rating of perceived exertion to prescribe exercise intensity in diabetic autonomic neuropathy. Diabetes Care 2003; 26: 986–990. DOI: 10.2337/DIACARE.26.4.986 [DOI] [PubMed] [Google Scholar]
- 36.Shariat A, Cleland JA, Danaee M, et al. Borg CR-10 scale as a new approach to monitoring office exercise training. Work 2018; 60: 549–554, DOI: 10.3233/WOR-182762 [DOI] [PubMed] [Google Scholar]
- 37.Natalucci V, Carnevale Pellino V, Barbieri E, et al. Is it important to perform physical activity during coronavirus pandemic (COVID-19)? Driving action for a correct exercise plan. Front Public Health 2020; 8: 602020. DOI: 10.3389/FPUBH.2020.602020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng Y-Y, Chen C-M, Huang W-C, et al. Rehabilitation programs for patients with COronaVIrus Disease 2019: consensus statements of Taiwan Academy of Cardiovascular and Pulmonary Rehabilitation. J Formos Med Assoc 2021; 120: 83–92. DOI: 10.1016/j.jfma.2020.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dani M, Dirksen A, Taraborrelli P, et al. Autonomic dysfunction in 'long COVID': rationale, physiology and management strategies. Clin Med 2021; 21: e63–e67. DOI: 10.7861/clinmed.2020-0896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh MK, Mobeen A, Chandra A, et al. A meta-analysis of comorbidities in COVID-19: which diseases increase the susceptibility of SARS-CoV-2 infection? Comput Biology Medicine 2021; 130: 104219. DOI: 10.1016/J.COMPBIOMED.2021.104219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Curci C, Pisano F, Bonacci E, et al. Early rehabilitation in post-acute COVID-19 patients: data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur Journal Physical Rehabilitation Medicine 2020; 56: 633–641. DOI: 10.23736/S1973-9087.20.06339-X [DOI] [PubMed] [Google Scholar]
- 42.Paneroni M, Simonelli C, Saleri M, et al. Muscle strength and physical performance in patients without previous disabilities recovering from COVID-19 pneumonia. Am J Phys Med Rehabil 2021; 100: 105–109. DOI: 10.1097/PHM.0000000000001641 [DOI] [PubMed] [Google Scholar]
- 43.Núñez-Cortés R, Rivera-Lillo G, Arias-Campoverde M, et al. Use of sit-to-stand test to assess the physical capacity and exertional desaturation in patients post COVID-19. Chron Respir Dis 2021; 18: 1–7. DOI: 10.1177/1479973121999205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arbillaga-Etxarri A, Lista-Paz A, Alcaraz-Serrano V, et al. Fisioterapia respiratoria post-COVID-19: algoritmo de decisión terapéutica. Open Respir Arch 2022; 4: 100139, DOI: 10.1016/j.opresp.2021.100139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bickton FM, Chisati E, Rylance J, et al. An improvised pulmonary telerehabilitation program for postacute COVID-19 patients would be feasible and acceptable in a low-resource setting. Am J Phys Med Rehabil 2021; 100: 209–212. DOI: 10.1097/PHM.0000000000001666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seron P, Oliveros MJ, Gutierrez-Arias R, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Therapy 2021; 101: pzab053. DOI: 10.1093/ptj/pzab053 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material sj-pdf-1-crd-10.1177_14799731221104102 for Provision of pulmonary rehabilitation in Latin America 18 months after the COVID-19 pandemic: A survey of the Latin American Thoracic Association by Vicente Benavides-Cordoba, Marisol Barros-Poblete, Rodolfo P Vieira, Guillermo Mazzucco, Guilherme Fregonezi and Rodrigo Torres-Castro in Chronic Respiratory Disease