Abstract
Background
Cardiac amyloidosis (CA) is an under-diagnosed disease presenting as a restrictive cardiomyopathy with high morbidity and mortality. Wild-type transthyretin amyloid cardiomyopathy (ATTR-CM) is mostly seen in elderly patients, with increasing prevalence as life expectancy is growing. New diagnostic imaging techniques and treatments allow for a better prognosis, but lack of clinical awareness delays timely diagnosis and appropriate management. Our purpose was to investigate the knowledge of clinicians regarding ATTR-CM and to assess the availability of imaging resources in the Latin-American region.
Methods and Results
Two online surveys were distributed among clinicians and nuclear medicine professionals, respectively: one asking about awareness of CA in different clinical scenarios, and the other about the availability of diagnostic resources and studies performed. 406 responses were received for the first survey and 82 for the second, representing 17 and 14 countries, respectively. A significant lack of awareness was identified among clinicians, although appropriate diagnostic resources are generally available. Survey data showed that very few patients are evaluated for ATTR-CM in most Latin-American countries.
Conclusions
The surveys demonstrated the need for educational programs and other measures to increase clinical awareness and early detection of CA, so patients receive timely treatment and management of the disease.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12350-022-03005-5.
Keywords: Amyloid heart disease, statistical analysis, molecular imaging
Introduction
Cardiac amyloidosis (CA) is an under-diagnosed disease caused by extracellular deposition of abnormal proteins in the myocardium and presenting clinically as a restrictive cardiomyopathy (CM) associated with high morbility and mortality.1,2 There are two main types of CA, according to the precursor protein:3 one type (AL-CM) is caused by misfolded monoclonal immunoglobulin light chains from an abnormal clonal proliferation of plasma cells; the second type, ATTR-CM) is caused by transthyretin (TTR), a liver-synthesized protein normally involved in the transportation of the hormone thyroxine and retinol-binding protein. Although with similarities in clinical findings, generally presenting with heart failure with preserved ejection fraction (HFpEF), both types have substantially different prognosis and treatment approaches.4 Clinical interest in CA, particularly in ATTR wild type, has increased due to several factors: prevalence of the disease has been demonstrated to be higher than previously thought;5 conventional treatment for heart failure is poorly tolerated by these patients;6 novel imaging techniques allow accurate noninvasive diagnosis of ATTR-CM without the need for endomyocardial biopsy;7,8 and specific therapies have been recently developed and made available.9 Additionally, since life expectancy has increased during the last decades in most regions of the world, including Latin America (LATAM),10 an expanding incidence of this condition is predictable.
Because therapy for ATTR-CM seems most effective when administered before reaching an advanced stage of the disease,11,12 early identification of affected individuals is essential; however, misdiagnosis or delayed diagnosis is still common.13 In order to facilitate management in accordance to current strategies, awareness of the clinical cardiologist about the disease—including advances in diagnosis and treatment—is crucial. In this regard, we have recently created an international working group on CA (AMILO-LATAM) composed by cardiac imaging specialists from different Latin-American countries, aiming to identify potential needs in technical resources, training, and education. To our knowledge, there are no reliable data on the prevalence and/or incidence of CA in the region, and local guidelines or recommendations for its clinical management are scarce.14 Our group has set up three main goals: (1) to investigate the prevalence of the disease and the awareness about its management; (2) to disseminate knowledge among clinicians and imaging specialists through educational activities; and (3) to encourage the establishment of registries, guidelines and protocols to facilitate evidence-based management. As a first step, we aimed to assess the degree of knowledge and interest of clinicians by surveying healthcare professionals in the region. We also conducted a second survey among various nuclear medicine (NM) departments in order to investigate the availability of imaging equipment, radiopharmaceuticals, and experience in use. Accessibility of other diagnostic tools needed to complete diagnosis was also investigated, including trans-thoracic echocardiography (TTE) with echo-strain imaging (ESI), cardiac magnetic resonance (CMR) with parametric mapping (PM), and light-chains quantification (LCQ).
Methods
Two different surveys were designed to be administered at one time as a cross-sectional, observational study to gain insights on CA regarding knowledge of the disease and availability of diagnostic tools. Anonymous questionnaires were managed via Google Forms, a survey administration software available as a web application included as part of the free, web-based Google Docs Editor.15 The application allows users to create and edit surveys online, and the information is automatically entered into a spreadsheet for tabulation and statistical analysis.
Two questionnaires were presented to potential participants; one (Appendix A) focused on awareness of CA, and the other (Appendix B) about availability and use of imaging and laboratory diagnostic tools. Potential participants in each survey were selected according to their professional profiles. There were 10 questions in the first survey, and 5 in the other; a missed-answer automatic reminder prompted participants about unfinished questionnaires in real time, so incomplete forms were not submitted to the system. Data were checked for duplications, but for the sake of confidentiality, the IP addresses were not verified, and e-mail addresses were not recorded, although there was a voluntary entry for the latter. No participant names were gathered from the survey, and potential identifying information was analyzed separately and not made public. To encourage participation, multiple reminders were sent periodically, but no incentive was provided other than contributing to a research project. The surveys were in Spanish, with a Portuguese version for Brazil.
Surveys were distributed to physicians in 21 countries between May 30th and July 21st, 2021, and responses were accepted until July 24th. Links to the surveys were distributed by e-mail, Whatsapp, Facebook, and Twitter. To reach participants, personal databases of the authors were used, together with a request for recipients to forward the survey to their own contacts, and so on. No institutional databases were used for this purpose, and none of the participants knew about the survey in advance. The invitation headline stated that each survey was directed solely to those involved in clinical practice or medical imaging, respectively. It was understood that, by proceeding with the survey, responders implied their informed consent to participate in the study. Descriptive statistics were calculated using Microsoft Excel 2016.
Results
The total number of persons the survey actually reached is not known, since recipients were asked to forward the link to their own contacts. We estimate the number of survey recipients to be a few thousand, but we were unable to calculate the response rate with reasonable accuracy. Full results of the surveys are included in appendices A and B.
Survey 1: Awareness of Clinicians About CA
A total of 406 surveys were collected from participants in 98 cities in 17 Latin-American countries (Table 1). The countries with the highest number of responses were Mexico (156 ) and Argentina (71), which together account for 55% of the total number of participants. No responses were obtained from professionals in 3 countries.
Table 1.
Latin-American countries represented in Survey 1 (N = 17)
| Country | No. responses | % |
|---|---|---|
| Mexico | 156 | 38.4 |
| Argentina | 71 | 17.5 |
| Uruguay | 30 | 7.4 |
| Dominican Rep. | 22 | 5.4 |
| Peru | 20 | 4.9 |
| Chile | 19 | 4.7 |
| Brazil | 17 | 4.2 |
| Guatemala | 17 | 4.2 |
| Colombia | 16 | 3.9 |
| Cuba | 15 | 3.7 |
| Ecuador | 6 | 1.5 |
| El Salvador | 6 | 1.5 |
| Bolivia | 4 | 1 |
| Paraguay | 4 | 1 |
| Honduras | 1 | 0.2 |
| Panama | 1 | 0.2 |
| Venezuela | 1 | 0.2 |
| TOTAL | 406 | 100 |
Practice setting
Of the physicians who answered the survey, 83% (N = 337) work in a single workplace, while 17% (N = 69) work in at least 2 different institutions or sites. Of those who practice exclusively in a single place, 43% are associated with a non-academic high complexity hospital, followed by 22% in a university hospital, and 22% in a private office, while 13% work in a low complexity clinic. Since some doctors work in various sites, taking each one of these as an individual response, data were obtained from up to 482 different institutions/workplaces. When considering all work centers, high complexity hospitals were the most frequent (39%) responders, followed by private offices (26%).
Medical speciality
The majority of respondents were cardiologists (65%), followed by general practitioners/family doctors (17%), others (12%), and internists (6%) (Fig. 1). The group of “others” consisted of 15 different specialties. Among these, a small subgroup of cardiac imaging specialists made up of echocardiographers, nuclear cardiologists, and radiologists which represent 5.6% of total respondents. These imaging professionals were involved in office-based clinical practice as well.
Figure 1.
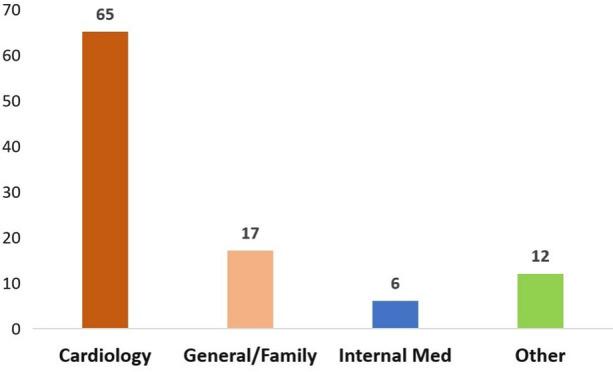
Percentage of responders according to medical specialty (N = 406)
Degree of knowledge about CA
When asked about the degree of knowledge that participants think they have about CA, there were 3 options to choose from. The most frequent response (47%) was “intermediate degree of knowledge—probably insufficient,” followed by 33% that considered themselves to have “adequate knowledge” and 20% who say they have “little knowledge” (Figure 2). Among specialtists (cardiologists, general/family doctors, internists, and other specialties), less than half indicated an “adequate knowledge” of the disease. Forty-eight percent of cardiologists consider themselves to have an intermediate degree of knowledge, while 43% indicated adequate, and 9% little knowledge. Meanwhile, 64% of internists claim to have an intermediate degree of knowledge, 18% adequate, and 18% little knowledge. General practitioners declare predominantly a low degree of knowledge (56%), followed by intermediate degree (44%), and no one indicated an adequate knowledge. Among physicians from other specialties, the main response was intermediate knowledge with 41%, followed by adequate with 33%, and low knowledge with 26%. Of this group, imaging professionals (N = 78) including echocardiograpy, radiology, and NM specialists, were the only subgroup where a majority indicated they had adequate knowledge (54%), followed by intermediate (42%) and low knowledge (4%).
Figure 2.
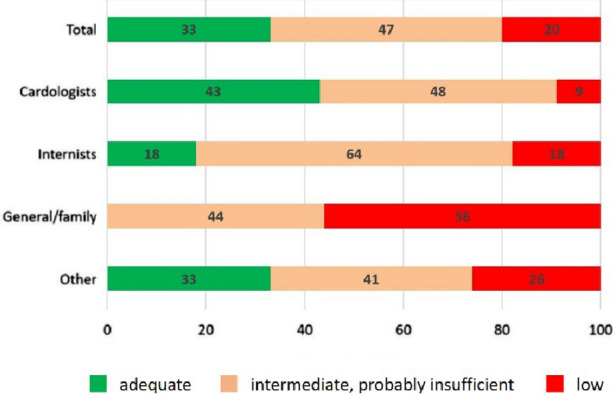
Degree of knowledge about CA considering total responses and by specialty (expressed in % of total for each category)
Prevalence of CA in the elderly
The majority of participants (74%) believe that the prevalence of CA in older adults is low, although higher than perceived; only 15% believe, it is high, and 11% very low. Separating responders by specialty, differences in opinions are observed, with general practitioners being those who most believe that the prevalence in the elderly is high (45%), followed by cardiologists (18%), internists (9%), and other specialists (6%); among the latter group, 20% of imaging specialists consider a high prevalence of CA in this population.
Importance of reaching diagnosis
A large majority of responders (93%) believe that reaching a diagnosis in patients with suspected CA is important because it can change the therapeutic strategy. Among those few physicians who minimize the real importance of diagnosis because no therapy is available, general practitioners and internists were most likely to respond.
Investigation of CA in elderly patients with HFpEF
Fifty-three percent of responders think that CA should always be investigated in elderly patients with HFpEF, 43% believe that only sometimes, and 4% rarely. Among the few physicians who considered that CA should rarely be sought in this group of patients, 86% were cardiologists (2% specializing in cardiac imaging), 7% internists, and 7% had other specialties.
Investigation of CA in elderly patients with LVH and discordant ECG
Seventy-three percent of physicians responded that CA should be investigated; whenever, LVH (detected by TTE) with a discordant ECG is present, while 24% consider this only sometimes, and the remaining 3% believe it should rarely be considered.
Next study to be indicated in patients with a suspicious TTE
In patients with a suspicious TTE, 331 participants (81%) chose only one study to be performed next as a response, 47 (12%) combined 2 options, 16 (4%) marked all 3 options (CMR, NM, and LCQ), and 12 (3%) none of them. The most chosen single method as the next study option was CMR (43%), followed by NM (38%), and LCQ (16%), while 3% believed none of those tests should be needed (Figure 3). Given the option of combining methods, CMR + NM was the choice for 41%, followed by NM + LCQ with 36%, while the least popular choice was CMR + LCQ, with 23%.
Figure 3.
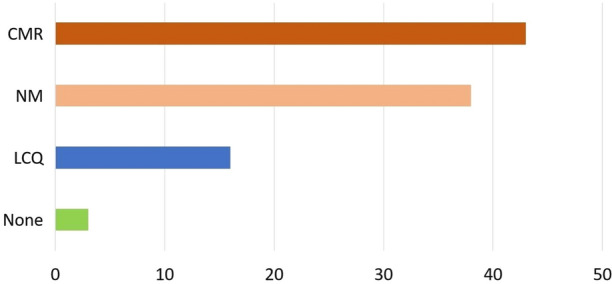
Distribution of responses (%) for the single most appropriate test to be performed after CA is suspected by TTE results
Nuclear scans for CA requested during the previous year
Sixty-five percent (N = 266) of surveyed physicians had not ordered a single nuclear scan during the year prior to the survey (Figure 4). Of the remaining 35% who had requested the procedure, the vast majority (27%) had ordered 1–5 studies, and only 4% more than 10. Having requested a technetium-99m pyrophosphate (PYP) scan was directly related to a higher degree of knowledge on the subject.
Figure 4.
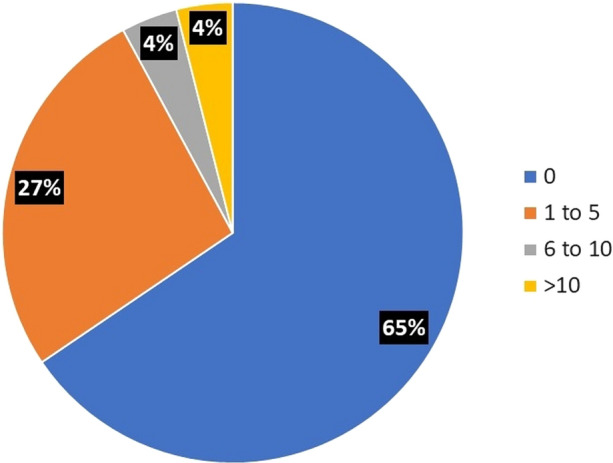
NM scans requested during the previous year, expressed as percentage of total responding physicians across all categories
Usefulness of disseminating more information about CA
Finally, 98% of participants declared that disseminating more information about CA among clinicians would be useful, indicating that a significant gap of knowledge is generally perceived.
Survey 2: Availability of diagnostic modalities and expertise
Surveys were collected from 14 countries, with a total of 82 NM centers in 45 different cities (Table 2). Countries with the highest number of responding centers were Brazil (17), Mexico (15), Argentina (13), and Colombia (12), with others including 5 centers or less. No responses were received from centers in 6 countries.
Table 2.
Latin-American countries represented in Survey 2 (N = 14)
| Country | No. responses | % |
|---|---|---|
| Brazil | 17 | 20.7 |
| Mexico | 15 | 18.3 |
| Argentina | 13 | 15.9 |
| Colombia | 12 | 14.6 |
| Chile | 5 | 6.1 |
| Peru | 4 | 4.9 |
| Uruguay | 4 | 4.9 |
| Ecuador | 3 | 3.7 |
| El Salvador | 2 | 2.4 |
| Panama | 2 | 2.4 |
| Dominican Rep. | 2 | 2.4 |
| Cuba | 1 | 1.2 |
| Paraguay | 1 | 1.2 |
| Venezuela | 1 | 1.2 |
| TOTAL | 82 | 100 |
Type of installation
Of the responding centers, 50 (61%) are located in non-academic high complexity hospitals, 26% are private imaging facilities, 8% are in low complexity hospitals, and only 5% belong to a university hospital.
Equipment
SPECT is available in 100% of the facilities (Table 3); 44% of them also have hybrid equipment (SPECT/CT). Mexico, Colombia, and Argentina reported having the most hybrid cameras. Only 7% (6 centers distributed in Brazil and Argentina) indicated they have dedicated CZT cameras.
Table 3.
Equipment availability among participating centers (N = 82)
| Equipment | N | % |
|---|---|---|
| SPECT | 82 | 100 |
| SPECT-CT | 36 | 44 |
| CZT | 6 | 7 |
Radiopharmaceuticals
Eighty-two percent of centers report using PYP for evaluation of CA. Of the rest, 10 centers use technetium-99m hydroxymethanediphosphonate (HMDP) and only 4 are using technetium-99m methylene diphosphonate (MDP) as the only bone-seeking agent (Table 3). Technetium-99m 2,3-dicarboxypropane-1,1-diphosphonate (DPD) is not available in the region.
Availability of diagnostic resources other than NM
Among the 82 responding centers, diagnostic methods for CA other than NM included 71 (86%) with access to TTE but only 49 (59%) to ESI; 63 centers (76%) have access to CMR, but only 35 (42%) to PM. LCQ is available in 57 centers (56%).
Nuclear scans for CA performed during the previous year
Thirty-nine percent of the centers performed 1 to 5 scans to search for CA in the previous year, 16% reported 6 to 10, 21% more than 10, and 24% none (Figure 5). The countries performing more scans (centers reporting >6 studies in the last year) were Brazil, Argentina, Chile, Colombia, and Mexico.
Figure 5.
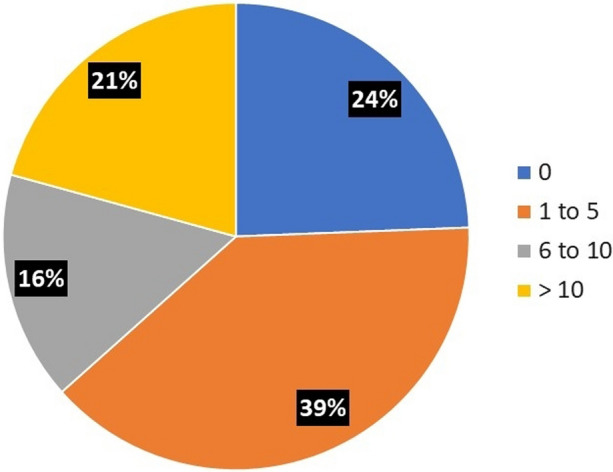
NM scans performed during the previous year, expressed as percentage of total responding centers
Discussion
The aim of the study was to investigate the current awareness and usage of novel clinical tools for the management of CA in Latin America through 2 different surveys, to identify potential needs in training, education and technology.
From the results, it is quite evident that the utilization of PYP scans for CA diagnosis in the region is not in accordance with expected prevalence of the disease. PYP is available in almost all responding centers and 100% have SPECT, but despite the accessibility of most necessary resources, 23% of the centers have not performed a single study to identify CA in the year prior to the survey, and most of the remaining ones report an average of one study per month, or less.
The surveys indicate enough qualified professionals in LATAM to carry out imaging studies for CA following current guidelines, as well as necessary tracers and equipment (PYP and SPECT), but some state-of-the-art technology (SPECT/CT, ESI, CMR with PM, and LCQ) is lacking in some areas. Only 39% of scans to search for CA are performed in high complexity hospitals, which could explain in part the limited accessibility to ESI and PM mapping in many centers.
Clinicians generally identify LVH and HFpEF as principal risk factors, but only 15% recognized advanced age as a possible red flag. Hence, they should be reminded that the disease is much more common in the elderly, so that age is not neglected as a risk factor. Although 80% of cardiologists consider themselves to have an intermediate degree of knowledge about CA, when asked what study they would perform next in a patient with a suspicious TTE, most chose CMR and only 38% mentioned NM. However, this should not be viewed as incorrect since some diagnostic algorithms start with typical imaging features on TTE and/or CMR. Although most physicians (93%) indicated awareness that novel treatments can modify the course of the disease, highlighting the importance of early and accurate diagnosis, only 4% had requested more than 10 PYP scans during the last year.
Although—as expected—cardiologists seem to be among those best informed about CA, it is obvious that many still need further education about red flags, diagnostic methods, and treatment algorithms. Interestingly, in a recent study from Switzerland—a highly developed country with well-known reputation in medical sciences—similar findings were reported,16 suggesting that lack of awareness about CA is probably a global issue. Also, a web-based national survey in the U.S. showed high variability in PYP scintigraphy protocols for CA diagnosis, highlighting the need for standardization.17 Although this was not specifically addressed in our surveys, it can be hypothesized that it is probably also the case in LATAM, due to the variability in responses about the sequence of methods to be used.
Limitations
Among the limitations of this study, there is the absence of a previous sample design to achieve a more representative proportion of responders according to the population of their respective countries and their geographical distribution. This is only a partial view of the general situation, probably with high regional and local heterogeneity. Online surveys commonly suffer from at least two methodological limitations: the population to which they are distributed cannot be fully described, and respondents with biases may select themselves into the sample.18 Of note, Mexico is clearly over-represented and Brazil is under-represented in the first survey according to the size and population of those countries, while the second survey is more balanced. While the number of responses received allowed us to create a picture that can reasonably estimate the global situation in Latin America, a bias can be present with majority of responses coming from those with more interest in the disease. Finally, the disruption of clinical practice during the Covid-19 pandemic might have partially affected some responses, especially regarding the number of studies performed.
New Knowledge Gained
For the first time, a survey on the awareness of clinicians about CA and the availability of appropriate diagnostic tools have been conducted in Latin America, allowing an estimation of needs for education and technical resources to confront this disease of growing prevalence in the region.
Conclusions
Despite the abovementioned limitations, the results of our survey demonstrate a significant proportion of health professionals dealing with scarce information about CA in the Latin-American region. The clinical presentation of the disease is variable, and improved education of physicians is needed to ensure that CA is considered as a diagnosis. Early recognition of suggestive signs and symptoms (‘red flags’) and accurate diagnosis are crucial, since overall survival is low once advanced cardiac involvement is present. Furthermore, novel treatments have become available whose efficacy is highly dependent on a timely delivery. Thus, increased awareness of clinicians is needed to improve patient outcomes. On the other hand, imaging resources are reasonably available in the region, but specialists should be properly trained in the interpretation and reporting of different tests, so unnecessary costs associated with the diagnostic workup are avoided—which is especially important in areas with limited resources. As a consequence of the findings reported here, we intend to develop a series of actions towards achieving these educational goals, both at national and regional levels.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
The authors wish to thank Dr. Enrique Alexander Berríos Bárcenas for his help in database management and analysis, and Linda Giering, PhD for reviewing the manuscript and providing useful suggestions.
Appendix A
Survey 1
Awareness of clinicians about cardiac amyloidosis (CA)
| 1.- Describe your practice setting * | N | % |
|---|---|---|
| University hospital | 105 | 22 |
| Non-academic, high complexity hospital | 186 | 39 |
| Low complexity clinic | 64 | 13 |
| Private office | 127 | 26 |
| Total of individual institutions/workplaces | 482 | 100 |
*More than one workplace allowed per participant
| 2.- What is your medical specialty? | N | % |
|---|---|---|
| Clinical cardiology | 265 | 65 |
| Internal medicine | 22 | 6 |
| General practice/family medicine | 70 | 17 |
| Other (describe) | 49 | 12 |
| Total | 406 | 100 |
| 3.- What do you think is your degree of knowledge about CA? | N | % |
|---|---|---|
| Very low | 80 | 20 |
| Intermediate—probably insufficient | 193 | 47 |
| Adequate | 133 | 33 |
| Total | 406 | 100 |
| 4.- What do you think is the prevalence of CA in the elderly population? | N | % |
|---|---|---|
| Extremely low | 47 | 11 |
| Low, but higher than usually perceived | 299 | 74 |
| High | 60 | 15 |
| Total | 406 | 100 |
| 5.- How important do you think is diagnosis in patients with suspected CA? |
N | % |
|---|---|---|
| Not much, since no specific therapy is available | 27 | 7 |
| Very much, since it can change management | 379 | 93 |
| Total | 406 | 100 |
| 6.- Do you believe CA should be investigated in elderly patients with HFpEF? | N | % |
|---|---|---|
| Always | 216 | 53 |
| Sometimes | 176 | 43 |
| Rarely | 14 | 4 |
| Total | 406 | 100 |
| 7.- Do you believe CA should be investigated in elderly patients with LVH and discordant ECG? | N | % |
|---|---|---|
| Always | 297 | 73 |
| Sometimes | 97 | 24 |
| Rarely | 12 | 3 |
| Total | 406 | 100 |
| 8.- In patients in whom CA is suspected by TTE, what study/studies would you indicate next? * | N | % |
|---|---|---|
| Nuclear Medicine (NM) | 130 | 38 |
| Cardiac Magnetic Resonance (CMR) | 148 | 43 |
| Light-Chains Quatification (LCQ) | 53 | 16 |
| None of the above | 9 | 3 |
| Total (as an individual method) | 340 | 100 |
*Results indicating more than one method not listed here
| 9.- How many NM scans for CA have you requested during the last year? | N | % |
|---|---|---|
| None | 266 | 65 |
| 1—5 | 108 | 27 |
| 6—10 | 16 | 4 |
| > 10 | 16 | 4 |
| Total | 406 | 100 |
| 10.- Would you consider it useful to disseminate more information about CA among clinicians? | N | % |
|---|---|---|
| Yes | 399 | 98 |
| No | 1 | 0.5 |
| Not sure | 6 | 1.5 |
| Total | 406 | 100 |
Appendix B
Survey 2
Availability and use of imaging and laboratory diagnostic tools for CA
| 1.- Where your NM medicine service operates | N | % |
|---|---|---|
| University hospital | 4 | 5 |
| Non-academic, high complexity hospital | 50 | 61 |
| Low complexity clinic | 7 | 8 |
| Private office | 21 | 26 |
| Total | 82 | 100 |
| 2.- Type of equipment * | N | % |
|---|---|---|
| SPECT camera | 82 | 66 |
| SPECT/CT | 36 | 29 |
| CZT camera | 6 | 5 |
| Total of individual type of equipment | 124 | 100 |
*Some centers with more than one type of equipment
| 3.- Availability of (Tc-99m) bone-seeking tracers | N | % |
|---|---|---|
| PYP | 68 | 83 |
| DPD | 0 | 0 |
| MDP | 4 | 5 |
| HMDP | 10 | 12 |
| Total | 82 | 100 |
| 4.- At your institution, there is accesibility of | N | %* |
|---|---|---|
| Trans-thoracic echocardiography (TTE) | 71 | 86 |
| TTE with echo-strain imaging (ESI) | 49 | 59 |
| Cardiac magnetic resonance (CMR) | 63 | 76 |
| CMR with parametric mapping (PM) | 35 | 42 |
| Light-chains quantification (LCQ) | 46 | 56 |
*Over a total of 82 centers
| 5.- How many CA scans have been performed at your institution during the last year? | N | % |
|---|---|---|
| None | 20 | 24 |
| 1—5 | 32 | 39 |
| 6—10 | 13 | 16 |
| > 10 | 17 | 21 |
| Total | 82 | 100 |
Author contributions
All authors have participated in (1) conception and design or analysis and interpretation of data, or both; (2) collecting data with subsequent data analysis; (3) drafting of the manuscript or revising it critically for intellectual content; and (4) final approval of the manuscript submitted.
Funding
The authors declare that no funding was allocated for this research.
Disclosures
The authors declare that they have no conflict of interest.
Footnotes
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Fernando Mut, Email: mut.fer@gmail.com.
Erick Alexanderson, Email: alexandersonerick@gmail.com.
References
- 1.Martinez-Naharro A, Hawkins PN, Fontana M. Cardiac amyloidosis. Clin Med (Lond) 2018;18(Suppl 2):s30–s35. doi: 10.7861/clinmedicine.18-2-s30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ash S, Shorer E, Ramgobin D, Vo M, Gibbons J, Golamari R, et al. Cardiac amyloidosis—A review of current literature for the practicing physician. Clin Cardiol. 2021;44:322–331. doi: 10.1002/clc.23572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Picken MM. The pathology of amyloidosis in classification: A review. Acta Haematol. 2020;143:322–334. doi: 10.1159/000506696. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Pavia P, Rapezzi C, Adler Y, Arad M, Basso C, Brucato A, et al. Diagnosis and treatment of cardiac amyloidosis: A position statement of the ESC Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2021;42:1554–1568. doi: 10.1093/eurheartj/ehab072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mesquita ET, Jorge AJL, Souza CV, Jr, Andrade TR. Cardiac amyloidosis and its new clinical phenotype: Heart failure with preserved ejection fraction. Arq Bras Cardiol. 2017;109:71–80. doi: 10.5935/abc.20170079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oghina S, Bougouin W, Bézard M, Kharoubi M, Komajda M, Cohen-Solal A, et al. The impact of patients with cardiac amyloidosis in HFpEF trials. JACC Heart Fail. 2021;9:169–178. doi: 10.1016/j.jchf.2020.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Aljaroudi WA, Desai MY, Tang WH, Phelan D, Cerqueira MD, Jaber WA. Role of imaging in the diagnosis and management of patients with cardiac amyloidosis: State of the art review and focus on emerging nuclear techniques. J Nucl Cardiol. 2014;21:271–283. doi: 10.1007/s12350-013-9800-5. [DOI] [PubMed] [Google Scholar]
- 8.Dorbala S, Cuddy S, Falk RH. How to image cardiac amyloidosis: A practical approach. JACC Cardiovasc Imaging. 2020;13:1368–1383. doi: 10.1016/j.jcmg.2019.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macedo AVS, Schwartzmann PV, de Gusmão BM, Melo MDT, Coelho-Filho OR. Advances in the treatment of cardiac amyloidosis. Curr Treat Options Oncol. 2020;21:36. doi: 10.1007/s11864-020-00738-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gietel-Basten S, Saucedo SEG, Scherbov S. Prospective measures of aging for Central and South America. PLoS ONE. 2020;15:e0236280. doi: 10.1371/journal.pone.0236280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kittleson MM, Maurer MS, Ambardekar AV, Bullock-Palmer RP, Chang PP, Eisen Howard J, et al. Cardiac amyloidosis: Evolving diagnosis and management: A scientific statement from the American Heart Association. Circulation. 2020;142:e7–22. doi: 10.1161/CIR.0000000000000792. [DOI] [PubMed] [Google Scholar]
- 12.Witteles RM, Bokhari S, Damy T, Elliott PM, Falk RH, Fine NM, et al. Screening for transthyretin amyloid cardiomyopathy in everyday practice. JACC Heart Fail. 2019;7:709–716. doi: 10.1016/j.jchf.2019.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Lane T, Fontana M, Martinez-Naharro A, Quarta CC, Whelan CJ, Petrie A, et al. Natural history, quality of life, and outcome in cardiac transthyretin amyloidosis. Circulation. 2019;140:16–26. doi: 10.1161/CIRCULATIONAHA.118.038169. [DOI] [PubMed] [Google Scholar]
- 14.Simões MV, Fernandes F, Marcondes-Braga FG, Scheinberg P, de Barros CE, Rohde LE, et al. Posicionamento sobre Diagnóstico e Tratamento da Amiloidose Cardíaca – 2021. Arq Bras Cardiol. 2021;117:561–598. doi: 10.36660/abc.20210718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rayhan RU, Zheng Y, Uddin E, Timbol C, Adewuyi O, Baraniuk JN. Administer and collect medical questionnaires with Google documents: A simple, safe, and free system. Appl Med Inform. 2013;33:12–21. [PMC free article] [PubMed] [Google Scholar]
- 16.Mircsof D. Diagnosis of amyloidosis: A survey of current awareness and clinical challenges among cardiologists in Switzerland. Cardiol Ther. 2020;9:127–138. doi: 10.1007/s40119-019-00160-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harb SC, Haq M, Flood K, Guerrieri A, Passerell W, Jaber WA, Miller EJ. National patterns in imaging utilization for diagnosis of cardiac amyloidosis: A focus on Tc99m-pyrophosphate scintigraphy. J Nucl Cardiol. 2017;24:1094–1097. doi: 10.1007/s12350-016-0478-3. [DOI] [PubMed] [Google Scholar]
- 18.Andrade C. The limitations of online surveys. Indian J Psychol Med. 2020;42:575–576. doi: 10.1177/0253717620957496. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


