Abstract
Objectives
Disability in the United States has not improved in recent decades. Comparing temporal trends in disability prevalence across different income groups, both within and between the United States and England, would inform public policy aimed at reducing disparities in disability.
Methods
Using the Health and Retirement Study and the English Longitudinal Study of Ageing, we estimated annual percent change from 2002 to 2016 in disability among community-dwelling adults (197,021 person-years of observations). Disability was defined based on self-report of limitations with 5 instrumental activities of daily living and 6 activities of daily living. We examined the trends by age and income quintile and adjusted for individual-level sociodemographic status and survey design.
Results
The adjusted annual percent change (AAPC) in disability prevalence declined significantly in both countries for ages 75 and older during 2002–2016. For ages 55–64 and 65–74, disability prevalence was unchanged in the United States but declined in England. Both countries experienced a widening gap in disability between low- and high-income adults among the younger age groups. For example, for those ages 55–64 in each country, there was no significant improvement in disability for the low-income group but a significant improvement for the high-income group (AAPC = −3.60; 95% confidence interval [CI; −6.57, −0.63] for the United States; AAPC = −6.06; 95% CI [−8.77, −3.35] for England).
Discussion
Improvements in disability were more widespread in England than in the United States between 2002 and 2016. In both countries, the disparity in disability between low- and high-income adults widened for middle-aged adults. Policies targeted at preventing disability among low-income adults should be a priority in both countries.
Keywords: ADL limitation, Disability trend, Health disparity, IADL limitation, U.S.–England comparison
More than 40% of adults aged 65 and older in the United States have a disability that limits vision, hearing, mobility, or independent living (CDC, 2018). Long-standing favorable trends of declining rates of disability among older adults have stalled or reversed in recent decades in the United States, raising concerns for increasing needs of long-term care among the growing population of older adults (Chen & Sloan, 2015; Choi & Schoeni, 2017; Freedman et al., 2013; Martin et al., 2010). About 8.3 million people in the United States used long-term care services in 2016 (Sengupta et al., 2018). Medicaid financed the largest portion of paid long-term care with $158 billion in 2015 (National Center for Health Statistics (U.S.), 2019), and many unpaid family caregivers also provide a significant amount of daily care, valued at $470 billion in 2017 (Reinhard et al., 2019). Separate from the impact on future long-term care needs, increasing rates of disability would have a profound impact on broader aspects of health and well-being of older adults and their families. The coronavirus disease 2019 pandemic has brought even greater challenges for persons with disability and their families with high risks for low psychological well-being and poor quality of life (Steptoe & Di Gessa, 2021). Determining population trends and assessing differential trends in disability are important to inform public policy and interventions to prevent or reduce disability.
Socioeconomic and environmental factors are likely to affect physiological health and hence physical functioning and disability, but those factors may also have a direct effect on disability which is independent of the effect on underlying physical capacity (Verbrugge & Jette, 1994). Some evidence suggests that economic hardship may have contributed to the recent concerning trends in disability among middle-aged adults in the United States (Choi et al., 2016; Zajacova & Montez, 2018), which is likely to be more pronounced among the lower-income families. There is evidence on differential trends in disability by income groups among adults ages 55–64 in the United States with more favorable trend for higher-income group versus lower-income group over the last decades (Tipirneni et al., 2020).
Comparing disability trends in the United States with those in other countries may provide important context and perspectives for further investigation of significant factors contributing to the population trend. While there are many studies showing substantial health disparities across economic groups in the United States and other high-income countries (Chetty et al., 2016; Choi et al., 2020; Emanuel et al., 2021; Jivraj, 2020; Kinge et al., 2019; Makaroun et al., 2017; Marmot, 2020; Zaninotto et al., 2020), there are few studies that compare population trends in disability across economic groups in the United States with other high-income countries.
While increasing income inequality has been observed in high-income countries other than the United States, it has been more dramatic in the United States during recent decades (Chetty et al., 2016; World Inequality Database (WID), n.d.). The public safety net, including public health care and social welfare, is more limited in the United States than other high-income countries (Banks et al., 2006; Case & Deaton, 2020; Schneider et al., 2021) which may have contributed to the U.S. health disadvantage in recent decades (Avendano & Kawachi, 2014). Adults in the United States may have experienced difficulties with carrying out daily tasks relatively more in recent years because of lack of means (e.g., assistive equipment, transportation, finance to buy services for delivery) to facilitate their daily activities of living and may have perceived specific daily tasks more difficult due to social and economic stressors, especially during the financial crises.
This paper aims to fill the gap in comparing differences in population trends in disability in the United States and England. The primary age group of interest is 55–64, preretirement ages, because of its implications for the labor market and future long-term care burden; many recent studies provided evidence that the health of working-age adults in the United States is worsening (National Academies of Sciences, Engineering, and Medicine, 2021; Woolf & Aron, 2013). We also examine trends for adults 65 and older to provide more comparisons and context for the trend in disability among those 55–64. The United States and England have relatively similar culture, language, and economic systems and experience increasing inequality, but they have quite different health care and social welfare systems (Banks et al., 2006; Case & Deaton, 2020). We hypothesize that the concerning population trend in disability among working-age adults—no improvement or even worsening disability—persists in the United States even after controlling for sociodemographic changes but not in England. We also hypothesize that, given the increasing economic inequality, both countries experience a widening gap in disability between low- and high-income groups.
Method
Data and Sample
The Health and Retirement Study (HRS) is a biennial longitudinal survey of approximately 20,000 Americans over the age of 50 that started in 1992. The HRS collects extensive health information as well as sociodemographic characteristics (Sonnega et al., 2014). We mainly used the RAND HRS which provides a cleaned, user-friendly data set covering a large range of topics (Bugliari et al., 2021). The HRS was approved by the University of Michigan Institutional Review Board. The English Longitudinal Study of Ageing (ELSA) is a biennial longitudinal household survey of English adults aged 50 years or older that began data collection in 2002 including detailed health and sociodemographic measures. The ELSA was developed with the goal of using methods and survey questions that are comparable to the HRS to facilitate cross-national comparisons(NatCen Social Research, 2020). Ethical approval for all the ELSA waves was granted by the National Health Service Research Ethics Committees under the National Research and Ethics Service.
We used the Gateway to Global Aging Data which provides a harmonized version of ELSA data sets with variables comparable to the RAND HRS.
Our study sample included community-dwelling adults aged 55 and older from both the HRS and ELSA in each biennial survey 2002–2016. For both the HRS and ELSA, nursing home residents were not included in the initial study sample but those who transitioned to a nursing home in subsequent years continued to be followed. The sample weight is not available for nursing home residents in the ELSA, and hence cannot provide nationally representative estimates for the population including nursing home residents (NatCen Social Research, 2020). With the refreshment samples from the HRS and ELSA and applying cross-sectional weights, the study sample is nationally representative of the age group (55 and older) in a given survey year. There were 29,088 persons and 131,764 person-year observations from the HRS, and 14,939 persons and 65,257 person-year observations from the ELSA.
Measures
We examined harmonized measures (Phillips et al., 2017) of disability based on limitations in instrumental activities of daily living (IADLs) or activities of daily living (ADLs). IADLs include using the telephone, managing money, taking medication, shopping, or preparing meals (Supplementary Table 1). ADLs include walking across a room, dressing, bathing, eating, getting in/out bed, or using the toilet (Supplementary Table 1). Limitations in IADLs and ADLs reflect different aspects and domains of disability, but may be combined with or without hierarchical relations depending on the study population and focus (Kempen & Suurmeijer, 1990; Spector & Fleishman, 1998). We created a sum score of IADL/ADL limitations (i.e., the number of activities with difficulty) and subsequently two dichotomized measures of IADL/ADL limitations (at least one IADL/ADL, three or more IADL/ADLs). The distribution of the number of IADL or ADL limitations is summarized in Supplementary Figure 1. After confirming that these measures provided similar results, we used the dichotomized measure of having a limitation with at least one IADL/ADL as the primary measure of disability. There were fewer than 5% missing values in this primary disability measure in the HRS and fewer than 1% in the ELSA. We used an indicator of having a limitation with at least three IADL/ADLs as the secondary outcome. We also used separate measures of having a limitation with at least one IADL and a limitation with at least one ADL to check if trends in disability were substantively consistent between IADLs and ADLs.
Besides the country indicator (United States vs England), we used age group (55–64, 65–74; 75 and older) and income quintile as stratification variables. Both income and wealth variables can be considered as important economic stratification variables, but each has a unique context and implication for public policy. We use income as the primary economic stratification variable rather than wealth because we believe income reflects the day-to-day financial situation of middle-aged adults better than wealth. We created a measure of income quintiles based on a harmonized household income by specifying it within each country, year, and age after the adjustment with the 2012 consumer price index (OECD, n.d.) and household size. The harmonized income variables are the sum of income from all financial items, but they are collected as before-tax for HRS and after-tax for ELSA (Beaumaster et al., 2018). Because we are using relative income position defined within each country, this discrepancy is unlikely to affect the trend estimates by income quintiles.
We were also interested in the disability trend, independent of changes in demographic characteristics over time. More specifically, we included in the multivariable analyses age (years), gender (female indicator), foreign-born status (outside the United States for HRS, outside the United Kingdom for ELSA), race (White vs others), household size (number of people living in the household), marital status (partnered, separated/divorced, widowed, never married), and the number of biological or adopted children (0, 1, 2, 3+). We also controlled for differences in survey design including refreshment sample indicator, interview month, and proximity interview indicator, which may affect estimates of disability trends within and between countries. There were fewer than 1% missing values in these covariates in both the HRS and ELSA.
For an auxiliary analysis examining the potential influence of education and health behaviors, we included measures of education, a three-tier harmonized scale based on the simplified International Standard Classification of Education 1997 (ISCED 97) (less than secondary, upper secondary and vocational training, and tertiary; OECD, 1999; Phillips et al., 2017), smoking status (never, former, or current), and body mass index (BMI) category (<25, 25–30, ≥30). BMI values were calculated based on weights and heights that were self-reported for HRS and directly measured by nurses for ELSA.
Statistical Analysis
We first summarized means or percentages of sociodemographic and health behavior covariates for each study period (pooled over 2002–2016) and calculated unadjusted annual percent change (APC) from 2002 to 2016, for each age group. We then estimated the unadjusted prevalence of disability for each year with 95% confidence intervals (CIs) and APC in disability from 2002 to 2016.
To estimate an adjusted percent change over time in disability, we conducted multivariable logistic regressions. We included in the models a continuous variable of survey year and adjustment variables of sociodemographic characteristics and survey aspects. Based on the estimates, we first calculated adjusted risk ratio based on the data for all eight survey waves covering 14 years and then calculated adjusted annual percent change (AAPC): 100 * ln(Adjusted Risk Ratio2016 vs 2002)/14 for dichotomized disability outcomes.
To assess the change in disability over time by income, we first estimated the unadjusted prevalence of disability at each quintile of the income distribution in the United States and England, for each year and for 2002–2008 and 2010–2016. We also estimated unadjusted APC from 2002 to 2016 (using all eight waves). To estimate the AAPC in disability, we included as explanatory variables the indicator variables for each country-specific income quintile, the indicator for the HRS sample, an interaction between the indicator variables for each income quintile and an indicator for the HRS sample, and sociodemographic and survey aspect covariates.
We performed auxiliary and sensitivity analyses. First, we estimated the disability trend using separate measures of any IADL limitation and any ADL limitation. Second, we tested whether education and health behaviors contributed to the trends in disability. Third, we examined whether the estimates of trends in disability were influenced by the sample restriction of excluding nursing home populations. For this, we used an unweighted sample because population weights for those living in a nursing home were not available for ELSA. Fourth, we employed a multiple-imputation technique to impute missing values for covariates using chained equations with 10 replications. All analyses were conducted using STATA 15. For all estimates, standard errors were adjusted, and cross-sectional population weights were applied, according to the complex survey design of the HRS and ELSA.
Results
There were significant changes from 2002 to 2016 in many sociodemographic and health behavior variables in the United States and England (Table 1). The share of women decreased in both countries for those 75 and older. The percentage of foreign-born among those 55–64 and 75 and older increased in both countries. The percentage of those who have a spouse or partner decreased among those 55–64 while it increased among those 75 and older in both countries. The rate of those who never married increased in all age groups in the United States but only among ages 55–64 in England. The share of adults without a child has increased significantly among those 55–64 and 65–74 but decreased among the 75 and older in both countries.
Table 1.
Summary Statistics of Sociodemographic and Health Behavior Covariates in the United States and England and Annual Percentage Change (APC) in Each Covariate From 2002 to 2016, by Age Group
| Age 55–64 | Age 65–74 | Age 75 and older | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HRS (United States) N = 48,372 |
ELSA (England) N = 25,238 |
HRS (United States) N = 43,651 |
ELSA (England) N = 22,674 |
HRS (United States) N = 39,741 |
ELSA (England) N = 17,345 |
|||||||
| Mean or % | APC | Mean or % | APC | Mean or % | APC | Mean or % | APC | Mean or % | APC | Mean or % | APC | |
| Age, mean | 59.2 | 0.04** | 59.2 | 0.05*** | 69.1 | −0.03*** | 69.2 | −0.03*** | 81.6 | 0.08*** | 81.2 | 0.04*** |
| Female, % | 52.0 | −0.14 | 50.9 | 0.01 | 53.7 | −0.12 | 52.3 | −0.17 | 60.0 | −0.38*** | 59.1 | −0.60*** |
| Foreign-born status, % | 10.4 | 3.09** | 10.1 | 6.78*** | 9.6 | −0.76 | 8.1 | 0.36 | 9.4 | 2.80*** | 6.6 | 2.15** |
| White, % | 81.5 | −0.71*** | 95.0 | −0.45*** | 86.1 | −0.26** | 96.9 | 0.03 | 89.0 | −0.20** | 98.1 | −0.11*** |
| Household size, % | ||||||||||||
| 1 person | 18.5 | 1.15* | 15.4 | 0.46 | 23.5 | 0.57 | 24.1 | −1.74*** | 38.7 | −0.99*** | 45.7 | −1.38*** |
| 2 persons | 49.9 | −0.70** | 57.6 | −1.17*** | 58.1 | −0.17 | 65.8 | 0.49*** | 47.8 | 0.42* | 48.5 | 0.94*** |
| 3+ persons | 31.6 | 0.44 | 27.0 | 2.21*** | 18.4 | −0.19 | 10.2 | 0.94 | 13.4 | 1.39** | 5.8 | 2.85*** |
| Marital status, % | ||||||||||||
| 1. With spouse | 71.4 | −0.49** | 77.3 | −0.46*** | 68.0 | 0.00 | 71.7 | 0.66*** | 47.9 | 0.46* | 47.7 | 1.57*** |
| 2. Separated/divorced | 16.6 | 0.27 | 12.0 | 2.46*** | 13.2 | 2.24*** | 9.7 | 2.02*** | 7.3 | 4.72*** | 4.9 | 7.24*** |
| 3. Widowed | 5.3 | −3.10*** | 4.5 | −4.46*** | 14.5 | −3.22*** | 14.2 | −4.23*** | 41.6 | −1.69*** | 42.7 | −2.31*** |
| 4. Never married | 6.7 | 7.50*** | 6.1 | 4.21*** | 4.2 | 4.52*** | 4.4 | −1.77** | 3.2 | 4.75*** | 4.7 | −2.84*** |
| N of children, % | ||||||||||||
| None | 13.4 | 4.00*** | 19.3 | 3.26*** | 9.2 | 4.06*** | 14.1 | 0.98* | 8.9 | −2.39*** | 13.7 | −3.37*** |
| 1 child | 14.8 | 1.99*** | 22.6 | 2.13*** | 10.7 | 3.71*** | 16.9 | 0.62 | 10.8 | −3.82*** | 18.9 | −3.12*** |
| 2 children | 35.4 | 0.31 | 36.7 | −1.11*** | 30.9 | 2.61*** | 38.3 | 0.89*** | 26.6 | 0.03 | 34.2 | 1.40*** |
| 3 children | 36.4 | −2.52*** | 21.4 | −3.35*** | 49.3 | −3.10*** | 30.7 | −1.92*** | 53.7 | 1.16*** | 33.1 | 1.67*** |
| Education (ISCED), % | ||||||||||||
| 1. Less than secondary | 11.6 | −3.94*** | 32.3 | −2.55*** | 17.6 | −5.16*** | 45.6 | −3.58*** | 25.0 | −3.61*** | 60.9 | −2.10*** |
| 2. Upper secondary and vocational training | 58.3 | −0.16 | 50.1 | 0.94*** | 58.0 | 0.04 | 42.1 | 2.27*** | 55.9 | 0.62*** | 31.5 | 3.23*** |
| 3. Tertiary | 30.2 | 1.86*** | 17.6 | 1.91*** | 24.5 | 3.76*** | 12.3 | 5.26*** | 19.1 | 2.94*** | 7.6 | 3.01*** |
| Smoking status, % | ||||||||||||
| 0. Never smoke | 43.5 | 1.29*** | 37.6 | 1.25*** | 40.4 | 0.83** | 35.4 | −0.79*** | 46.7 | −0.19 | 35.4 | −0.22 |
| 1. Former smoker | 38.2 | −0.75** | 44.1 | −0.09 | 47.3 | −0.38 | 51.9 | 1.23*** | 48.0 | 0.33* | 57.2 | 0.54*** |
| 2. Current smoker | 18.3 | −1.46** | 18.4 | −2.38*** | 12.3 | −1.20* | 12.7 | −2.85*** | 5.2 | −1.31 | 7.4 | −3.13*** |
| BMI status, % | ||||||||||||
| 1. Underweight/normal | 25.8 | −0.99** | 26.0 | 0.07 | 28.0 | −2.14*** | 25.5 | −0.27 | 42.9 | −1.90*** | 32.4 | −1.19*** |
| 2. Overweight | 37.4 | −0.72** | 39.6 | −0.65** | 38.9 | −0.40 | 42.2 | −0.15 | 37.6 | 0.52* | 40.0 | 0.76*** |
| 3. Obese | 36.8 | 1.45*** | 34.4 | 0.69** | 33.1 | 2.34*** | 32.4 | 0.41 | 19.5 | 3.24*** | 27.7 | 0.27 |
Notes: BMI = body mass index; ELSA = English Longitudinal Study of Ageing; HRS = Health and Retirement Study. The analysis sample includes community-dwelling adults. Estimates on the mean value and percentages were based on the pooled data from 2002 to 2016. 95% confidence intervals are provided in parenthesis. p Value was based on the t test of whether the APC estimate was equal to zero.
*p < .05. **p < .01. ***p < .001.
A greater share of adults had tertiary education in more recent years in both countries. There was a decreasing trend in the share of current smokers in both countries for all age groups. The percentage of whom were obese increased for all age groups in the United States but for those 55–64 and 65–74 in England.
Trends in Disability in the United States and England
The unadjusted trends in disability prevalence (Table 2) show a decrease for all age groups in England (APC = −2.24 for ages 55–64, −1.93 for ages 65–74, −0.96 for ages 75 and older) but only for those 75 and older in the United States (APC = −0.59 for ages 75 and older). Among those 55–64, disability prevalence was lower in the United States versus England in 2002 (15.8% vs 18.2%; p value = .01), but higher in the United States in 2016 (16.3% vs England 13.4%; p value = .02). Among those 65–74, disability prevalence was lower in the United States versus England in 2002 (19.1% vs 24.4%; p value < .001) but similar in 2016.
Table 2.
Unadjusted Disability Prevalence and Annual Percent Change (APC) Over 2002–2016 in the United States and England by Age Group
| Ages 55–64 | Ages 65–74 | Ages 75 and older | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HRS (N = 48,372) | ELSA (N = 25,238) | HRS (N = 43,651) | ELSA (N = 22,674) | HRS (N = 48,372) | ELSA (N=25,238) | ||||
| Year | % of disability (95% CI) | % of disability (95% CI) | HRS vs ELSA p Value |
% of disability (95% CI) | % of disability (95% CI) | HRS vs ELSA p Value |
% of disability (95% CI) | % of disability (95% CI) | HRS vs ELSA p Value |
| 2002 | 15.8 (14.3, 17.3) | 18.2 (17.0, 19.4) | .01 | 19.1 (17.6, 20.6) | 24.4 (23.0, 25.7) | <.001 | 39.7 (37.7, 41.7) | 42.6 (40.7, 44.5) | .04 |
| 2004 | 16.4 (15.1, 17.8) | 18.0 (16.7, 19.4) | .10 | 19.5 (18.1, 20.9) | 24.4 (22.7, 26.1) | <.001 | 38.6 (36.8, 40.5) | 43.8 (41.4, 46.1) | <.001 |
| 2006 | 17.5 (16.0, 19.1) | 17.7 (16.3, 19.2) | .86 | 20.1 (18.7, 21.5) | 23.2 (21.4, 25.0) | .01 | 41.2 (39.2, 43.3) | 41.7 (39.4, 44.1) | .76 |
| 2008 | 15.9 (14.5, 17.3) | 15.7 (14.4, 16.9) | .82 | 19.5 (17.9, 21.1) | 22.8 (21.2, 24.5) | .004 | 39.5 (37.9, 41.1) | 43.9 (41.5, 46.3) | .003 |
| 2010 | 18.1 (16.6, 19.6) | 14.9 (13.7, 16.2) | .002 | 19.7 (18.0, 21.3) | 21.4 (19.8, 23.0) | .13 | 40.2 (38.5, 41.9) | 43.1 (40.9, 45.4) | .04 |
| 2012 | 16.3 (14.7, 17.9) | 15.1 (13.7, 16.5) | .28 | 19.6 (18.1, 21.0) | 20.8 (19.2, 22.4) | .26 | 37.3 (35.8, 38.9) | 39.8 (37.6, 42.0) | .07 |
| 2014 | 17.1 (15.5, 18.7) | 14.6 (13.0, 16.2) | .04 | 19.7 (18.1, 21.3) | 19.0 (17.4, 20.5) | .50 | 37.9 (36.1, 39.7) | 37.8 (35.6, 40.0) | .96 |
| 2016 | 16.3 (14.8, 17.9) | 13.4 (11.4, 15.3) | .02 | 18.0 (16.4, 19.7) | 19.3 (17.6, 20.9) | .30 | 36.6 (34.8, 38.4) | 37.7 (35.4, 39.9) | .46 |
| APC from 2002–2016 (95% CI) | 0.12 (−0.83, 1.07) | −2.24 (−2.98, −1.5) | <.001 | −0.31 (−1.03, 0.40) | −1.93 (−2.47, −1.38) | <.001 | −0.59 (−1.09, −0.08) | −0.96 (−1.37, −0.55) | .25 |
Notes: ADL = activity of daily living; CI = confidence interval; ELSA = English Longitudinal Study of Ageing; HRS = Health and Retirement Study; IADL = instrumental activity of daily living. The analysis sample includes community-dwelling adults. Disability was defined as having at least one IADL/ADL limitation. p Values were based on t test of whether the percentages of disability in a given year and the estimates of annual percentage changes are equal between HRS and ELSA.
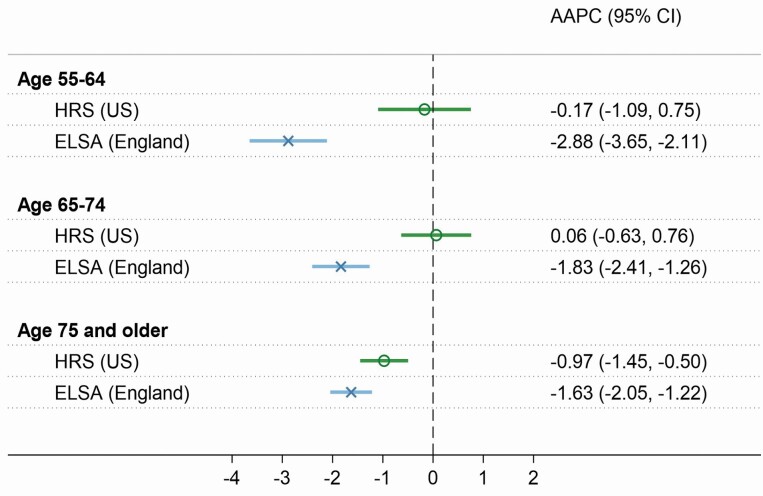
The overall trends are consistent after controlling for sociodemographic characteristics and survey design aspects (Figure 1). In England, the estimate on AAPC suggests a significant decrease in disability, especially for the younger age groups: AAPC = −2.88 (95% CI = −3.65, −2.11) for ages 55–64; −1.83 (95% CI = −2.41, −1.26) for ages 65–74; and −1.63 (95% CI = −2.05, −1.22) for 75 and older. On the contrary, in the United States, there was no decline in disability for the younger age groups (55–64 and 65–74), but there was a decline for the oldest group (−0.97 [95% CI = −1.45, −0.50] for 75 and older).
Figure 1.
Adjusted annual percent change (AAPC) in disability from 2002 to 2016 in the United States and England, by age group. Note: Control variables included sociodemographic characteristics (age, gender, foreign-born status, race, household size, marital status, number of children) and survey design aspects (refreshment sample indicator, interview month, proxy interview indicator). Disability was defined as having at least one IADL/ADL limitation. ADL = activity of daily living; CI = confidence interval; ELSA = English Longitudinal Study of Ageing; HRS = Health and Retirement Study; IADL = instrumental activity of daily living.
Results for the secondary disability outcome measure of having three or more limitations (Supplementary Figure 2) are generally consistent with the results from the primary measure, showing a significant improvement in disability in England for all age groups from 2002 to 2016; for the United States there was no improvement for any age group, and disability even worsened among ages 65–74. Results from the sensitivity analysis of estimating trend for IADL limitation and ADL limitation separately (Supplementary Figure 3) are also consistent with the results from the primary analyses. Trends in disability are not sensitive to the inclusion of nursing home population (Supplementary Figure 4).
Additional controls for education and health behaviors did not change the disability trend, in general (Supplementary Figure 5). However, the null disability trend in the United States changed to positive for those 65–74 (APC = 0.81 [95% CI = 0.13, 1.50]), suggesting that, without improvement in education, disability would have significantly worsened between 2002 and 2016 for those 65–74.
Differences in Disability Trend Across Income Groups in the United States and England
Table 3 summarizes the unadjusted prevalence of disability separately for 2002–2008 and 2010–2016 and APC from 2002 to 2016 for each income quintile groups. There is a substantial gap in the prevalence of disability between low-income adults (Q1: the bottom 20% of the income distribution) and high-income adults (Q5: the top 20% of the income distribution) in both countries, especially among those in the younger age groups. However, disability among the lowest income group was substantially higher in the United States versus England for all age groups (see Supplementary Figure 6 for each year). Among ages 55–64, for example, the average prevalence of disability for 2010–2016 was 37.9% (95% CI 35.5–40.3) in the United States compared to 28.7% (95% CI 26.5–30.9) in England. There was a decline in disability from 2002 to 2016 in broader income groups in England versus the United States; for ages 55–64, disability declined significantly for most income groups (Q2 through Q5) in England, but only for higher-income groups (Q4 and Q5) in the United States.
Table 3.
Unadjusted Average Prevalence (%) of Disability During 2002–2008 and 2010–2016 and Annual Percent Change (APC) From 2002 to 2016 in the United States and England by Income and Age Group
| HRS (United States) | ELSA (England) | |||||
|---|---|---|---|---|---|---|
| 2002–2008 | 2010–2016 | APC from 2002 to 2016 | 2002–2008 | 2010–2016 | APC from 2002 to 2016 | |
| % of disability (95% CI) | % of disability (95% CI) | APC (95% CI) | % of disability (95% CI) | % of disability (95% CI) | APC (95% CI) | |
| Among ages 55–64 | ||||||
| Q1: 0–20th percentile of the income distribution | 35.7 (33.7, 37.6) | 37.9 (35.5, 40.3) | 0.72 (−0.12, 1.57) | 27.5 (25.8, 29.1) | 28.7 (26.5, 30.9) | 0.44 (−0.72, 1.60) |
| Q2: 20–40th | 20.0 (18.1, 21.9) | 22.1 (20.3, 23.9) | 0.77 (−0.44, 1.98) | 22.7 (21.2, 24.3) | 18.7 (16.8, 20.5) | −2.53 (−3.91, −1.16) |
| Q3: 40–60th | 11.8 (10.4, 13.2) | 12.9 (11.6, 14.2) | 0.28 (−1.39, 1.95) | 17.2 (15.9, 18.6) | 12.9 (11.2, 14.6) | −3.80 (−5.66, −1.94) |
| Q4: 60–80th | 8.7 (7.7, 9.7) | 7.2 (6.1, 8.2) | −2.07 (−3.82, −0.32) | 11.8 (10.7, 12.9) | 7.8 (6.6, 9.0) | −5.31 (−7.34, −3.29) |
| Q5: 80–100th | 5.7 (4.6, 6.7) | 4.5 (3.6, 5.4) | −3.66 (−6.64, −0.68) | 7.9 (7.0, 8.8) | 5.1 (4.1, 6.1) | −5.90 (−8.60, −3.21) |
| Among ages 65–74 | ||||||
| Q1: 0–20th percentile of the income distribution | 35.1 (33.5, 36.6) | 34.4 (31.9, 37.0) | −0.03 (−0.95, 0.89) | 26.6 (24.9, 28.3) | 24.8 (22.8, 26.9) | −0.50 (−1.60, 0.61) |
| Q2: 20–40th | 22.0 (20.1, 23.9) | 22.7 (20.6, 24.8) | 0.39 (−0.92, 1.71) | 26.1 (24.3, 27.8) | 24.8 (22.8, 26.8) | −0.26 (−1.41, 0.89) |
| Q3: 40–60th | 17.1 (15.7, 18.5) | 15.9 (14.2, 17.5) | −0.72 (−1.94, 0.51) | 26.8 (25.1, 28.5) | 21.9 (20.1, 23.7) | −3.30 (−4.45, −2.15) |
| Q4: 60–80th | 12.9 (11.5, 14.3) | 13.1 (11.7, 14.5) | −0.47 (−1.95, 1.01) | 23.1 (21.5, 24.7) | 17.6 (15.9, 19.2) | −2.83 (−4.07, −1.59) |
| Q5: 80–100th | 10.0 (8.7, 11.3) | 9.4 (7.8, 10.9) | −1.82 (−3.85, 0.20) | 16.5 (15.1, 18.0) | 11.9 (10.6, 13.2) | −3.91 (−5.41, −2.41) |
| Among ages 75 and older | ||||||
| Q1: 0–20th percentile of the income distribution | 54.1 (51.6, 56.5) | 51.8 (49.5, 54.2) | −0.70 (−1.34, −0.06) | 40.6 (38.2, 43.0) | 40.7 (38.1, 43.2) | −0.37 (−1.31, 0.58) |
| Q2: 20–40th | 42.9 (40.2, 45.5) | 40.0 (37.8, 42.2) | −0.82 (−1.73, 0.10) | 38.2 (35.9, 40.4) | 40.6 (38.0, 43.1) | 0.94 (0.03, 1.86) |
| Q3: 40–60th | 37.3 (34.7, 39.9) | 35.4 (33.1, 37.8) | −0.56 (−1.59, 0.46) | 48.7 (46.4, 51.0) | 42.7 (40.2, 45.2) | −1.73 (−2.53, −0.93) |
| Q4: 60–80th | 32.5 (30.3, 34.7) | 32.4 (30.7, 34.0) | 0.09 (−0.85, 1.02) | 47.2 (44.9, 49.4) | 41.5 (39.0, 44.0) | −1.81 (−2.65, −0.97) |
| Q5: 80–100th | 31.1 (29.7, 32.6) | 29.5 (27.4, 31.6) | −0.78 (−1.80, 0.24) | 40.6 (38.3, 42.8) | 33.8 (31.3, 36.2) | −1.68 (−2.66, −0.70) |
Notes: ADL = activity of daily living; CI = confidence interval; ELSA = English Longitudinal Study of Ageing; HRS = Health and Retirement Study; IADL = instrumental activity of daily living. The analysis sample includes community-dwelling adults. Disability measure was an indicator of having at least one IADL/ADL limitation. Low income (Q1) was defined as the bottom 20% of the income distribution. High income (Q5) was defined as the top 20% of the income distribution. p Value was based on t test of whether the APC estimate was equal to zero.
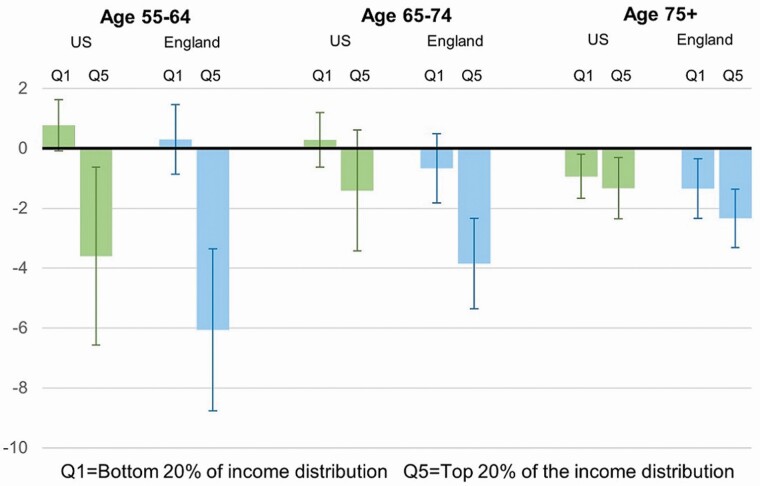
Figure 2 shows the adjusted estimates focusing on low (Q1) and high (Q5) income group, which suggests no significant change in disability from 2002 to 2016 in either country for the low-income group but a significant decline for those with high income for ages 55–64 in both countries. For example, the AAPC for the high-income (Q5) adults 55–64 were −3.60 (95% CI −6.57, −0.63) in the United States and −6.06 (95% CI −8.77, −3.35) in England (Figure 2). In both countries, among those at ages 75+, the adjusted prevalence of disability declined significantly in both low- and high-income groups. Estimates from all income groups are provided in Supplementary Figure 7.
Figure 2.
Adjusted annual percent change (AAPC) in disability from 2002 to 2016 in the United States and England, by income and age group. Note: Control variables included sociodemographic characteristics (age, gender, foreign-born status, race, household size, marital status, number of children) and survey design aspects (refreshment sample indicator, interview month, proxy interview indicator). Income quintile was defined as weighted income, which was adjusted by the square root of household size, divided into five groups within the study, year, and age. Disability measure was an indicator of having at least one IADL/ADL limitation. Results for all income quintile groups are summarized in Supplementary Figure 7. ADL = activity of daily living; IADL = instrumental activity of daily living.
The sensitivity analysis using imputed data (Supplementary Figure 8) are similar to the results above (Figure 2). Results from the secondary measure of disability suggest, among ages 55–64, the percent having three or more IADL/ADL limitations significantly increased among low-income adults in both countries (Supplementary Figures 9).
Discussion
Our findings from comparable nationally representative surveys in the United States and England highlight a number of important issues regarding population levels of disability and their change over time from 2002 to 2016. First, overall trends in disability were more favorable and widespread for England than the United States among middle-aged and young-old adults, with no decline in the United States but a significant decline in England. Second, disability among low-income adults in the United States was persistently and significantly higher than in England in all age groups during the study period. Third, both countries experienced a widening gap between low- and high-income adults among younger age groups (55–64 in the United States and 55–64 and 65–74 in England); disability in the lowest economic group has not improved, and, considering more severe disability, it may have even worsened.
Disability prevalence among middle-aged and young-old adults in the United States was lower than England at the beginning of the study period (2002) but similar to or even greater than England at the end of the study period (2016). The adverse trend might have been affected negatively for the United States as baby-boomer and younger cohorts with greater disability reaching middle ages and older ages. Without improvements in rates of disability among the younger cohorts, the declines in disability among older adults (75 and older) in recent decades may be muted or even reversed in the decades ahead, leading to a substantial increase in the total number of adults who need long-term care. In addition, those in the baby-boomer and younger cohorts have fewer available family caregivers because they are less likely to be married and more likely to have no child or fewer children than those in older cohorts. Rising rates of disability and a declining pool of family caregivers will create significant burdens on individuals, families, and public programs (National Center for Health Statistics (U.S.), 2019; Watts et al., 2020). We also suspect that economic hardship during the Great Recession may have contributed to the worse trends in the United States compared to England (Margerison-Zilko et al., 2016), especially for the working-age adults. Adults in the United States may have experienced difficulties with carrying out daily tasks relatively more due to social and economic stressors during financial crises.
Our findings highlight the widening gap in disability between low- and high-income adults in both countries, especially among middle-aged adults (those 55–64). For example, in England, all income groups except the bottom quintile experienced significant declines in disability among middle-aged adults. In the United States, only high-income groups (the top 40%) experienced this decline among middle-aged adults. Income inequality increased in both countries during the study period, although the increase was greater in the United States than in England (World Inequality Database (WID), n.d.). However, there may be differences in how economic inequality leads to disparities in health and disability in the United States and England, perhaps related to the generosity of the public safety net, access to the health care system, and other socioeconomic and built environmental factors.
Our findings should be considered in the context of the potential limitations of the study. First, while the measures in the HRS and ELSA are comparable, the method used to elicit responses differed. For example, the HRS survey asks about each activity or physical movement one at a time, but the ELSA shows all items at the same time on a card and asks respondents to select relevant items (Supplementary Table 1). It is however not clear whether this difference in approach, which occurred consistently across all survey years, would affect the change in each measure over time. Second, the measures of disability are self-assessed and may be interpreted differently between countries due to different health expectations and reference groups (Molina, 2017). And, the operational definitions of disability used in this paper may have some limitations in clinical practice. Third, we used a measure of relative income position to assess inequality in the trend in disability. Income is an important economic measure reflecting day-to-day financial situation, but it may have limitation in capturing the full economic circumstance. We also considered a measure of relative wealth position (i.e., wealth quintile). Findings by wealth groups provided the trend patterns similar to the results by income groups although there are some differences in terms of statistical significance (Supplementary Figure 10). Fourth, our estimates on trends in disability were based on community-dwelling populations, which may not be generalized to the older adult population including nursing home populations. However, based on our sensitivity analysis (Supplementary Figure 4), it is unlikely to have any notable differences in the estimates due to the sample restriction of excluding nursing home populations.
In summary, trends in disability from 2002 to 2016 were more favorable in England than the United States, especially for middle-aged adults. However, there was an increasing disparity in disability between low- and high-income adults in both countries. Public policies aimed at facilitating the social and economic opportunity for the poor may contribute significantly to reversing the unfavorable disability trends in the United States and reducing the gap in disability between low- and high-income groups in both countries.
Supplementary Material
Contributor Information
HwaJung Choi, Department of Internal Medicine, School of Medicine, University of Michigan, Ann Arbor, Michigan, USA; Department of Health Management and Policy, School of Public Health, University of Michigan, Ann Arbor, Michigan, USA.
Robert F Schoeni, Institute for Social Research, University of Michigan, Ann Arbor, Michigan, USA; Gerald R. Ford School of Public Policy, University of Michigan, Ann Arbor, Michigan, USA.
Andrew Steptoe, Department of Behavioural Science and Health, University College London, London, UK.
Tsai-Chin Cho, Department of Epidemiology, School of Public Health, University of Michigan, Ann Arbor, Michigan, USA.
Kenneth M Langa, Department of Internal Medicine, School of Medicine, University of Michigan, Ann Arbor, Michigan, USA; Institute for Social Research, University of Michigan, Ann Arbor, Michigan, USA.
Funding
Funding for this research was provided by the National Institute on Aging (P30AG012846, R21AG054818, K01AG057820, R01AG053972, P30AG024824, U01AG009740). This paper was published as part of a supplement sponsored by the University of Michigan with support from the National Institute on Aging (P30AG012846).
Conflict of Interest
None declared.
Acknowledgments
An earlier version of this paper was presented at the 2020 Annual Meeting of the TRENDS Network, May 8. The views expressed are those of the authors alone and do not represent those of their employers or any funding agency.
References
- Avendano, M., & Kawachi, I. (2014). Why do Americans have shorter life expectancy and worse health than do people in other high-income countries?. Annual Review of Public Health, 35(1), 307–325. doi: 10.1146/annurev-publhealth-032013-182411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks, J., Marmot, M., Oldfield, Z., & Smith, J. P. (2006). Disease and disadvantage in the United States and in England. Journal of American Medical Association, 295(17), 2037–2045. doi: 10.1001/jama.295.17.2037 [DOI] [PubMed] [Google Scholar]
- Beaumaster, S., Chien, S., Crosswell, A., Lin, A., Phillips, D., Valev, M., Wilkens, J., Yonter, V., & Lee, J. (2018). Harmonized ELSA F 2002-2016.pdf. USC Center for Economic and Social Research. [Google Scholar]
- Bugliari, D., Carroll, J., Hayden, O., Hayes, J., Hurd, M., St. Clair, P., Karabatakis, A., Main, R., Marks, J., McCullough, C., Meijer, E., Moldoff, M., Pantoja, P., & Rohwedder, S. (2021). RAND HRS longitudinal file 2018 (V1) Documentation. RAND. [Google Scholar]
- Case, A., & Deaton, A. (2020). Deaths of despair and the future of capitalism. Princeton University Press. [Google Scholar]
- CDC (2018, November 26). Prevalence of disabilities and health care. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/disabilityandhealth/features/kf-adult-prevalence-disabilities.html [Google Scholar]
- Chen, Y., & Sloan, F. A. (2015). Explaining disability trends in the U.S. elderly and near-elderly population. Health Services Research, 50(5), 1528–1549. doi: 10.1111/1475-6773.12284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty, R., Stepner, M., Abraham, S., Lin, S., Scuderi, B., Turner, N., Bergeron, A., & Cutler, D. (2016). The association between income and life expectancy in the United States, 2001–2014. Journal of American Medical Association, 315(16), 1750–1766. doi: 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, H., & Schoeni, R. (2017). Health of Americans who must work longer to reach social security retirement age. Health Affairs, 36(10), 1815–1819. doi: 10.1377/hlthaff.2017.0217 [DOI] [PubMed] [Google Scholar]
- Choi, H., Schoeni, R., & Martin, L. (2016). Are functional and activity limitations becoming more prevalent among 55 to 69-year-olds in the United States?. PLoS One, 11(10), e0164565. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0164565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi, H., Steptoe, A., Heisler, M., Clarke, P., Schoeni, R. F., Jivraj, S., Cho, T.-C., & Langa, K. M. (2020). Comparison of health outcomes among high- and low-income adults aged 55 to 64 years in the US vs England. JAMA Internal Medicine, 180(9), 1185–1193. doi: 10.1001/jamainternmed.2020.2802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emanuel, E. J., Gudbranson, E., Van Parys, J., Gørtz, M., Helgeland, J., & Skinner, J. (2021). Comparing health outcomes of privileged US Citizens with those of average residents of other developed countries. JAMA Internal Medicine, 181(3), 339. doi: 10.1001/jamainternmed.2020.7484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., Spillman, B. C., Andreski, P. M., Cornman, J. C., Crimmins, E. M., Kramarow, E., Lubitz, J., Martin, L. G., Merkin, S. S., & Schoeni, R. F. (2013). Trends in late-life activity limitations in the United States: An update from five national surveys. Demography, 50(2), 661–671. doi: 10.1007/s13524-012-0167-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jivraj, S. (2020). Are self-reported health inequalities widening by income? An analysis of British pseudo birth cohorts born, 1920–1970. Journal of Epidemiology and Community Health, 74(3), 255–259. doi: 10.1136/jech-2019-213186 [DOI] [PubMed] [Google Scholar]
- Kempen, G. I. J. M., & Suurmeijer, T. P. B. M. (1990). The development of a hierarchical polychotomous ADL-IADL scale for noninstitutionalized elders. The Gerontologist, 30(4), 497–502. doi: 10.1093/geront/30.4.497 [DOI] [PubMed] [Google Scholar]
- Kinge, J. M., Modalsli, J. H., Øverland, S., Gjessing, H. K., Tollånes, M. C., Knudsen, A. K., Skirbekk, V., Strand, B. H., Håberg, S. E., & Vollset, S. E. (2019). Association of household income with life expectancy and cause-specific mortality in Norway, 2005–015. Journal of American Medical Association, 321(19), 1916–1925. doi: 10.1001/jama.2019.4329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makaroun, L. K., Brown, R. T., Diaz-Ramirez, L. G., Ahalt, C., Boscardin, W. J., Lang-Brown, S., & Lee, S. (2017). Wealth-associated disparities in death and disability in the United States and England. JAMA Internal Medicine, 177(12), 1745. doi: 10.1001/jamainternmed.2017.3903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margerison-Zilko, C., Goldman-Mellor, S., Falconi, A., & Downing, J. (2016). Health impacts of the great recession: A critical review. Current Epidemiology Reports, 3(1), 81–91. doi: 10.1007/s40471-016-0068-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot, M. (2020). Health equity in England: The Marmot review 10 years on. BMJ, 368, m693. doi: 10.1136/bmj.m693 [DOI] [PubMed] [Google Scholar]
- Martin, L. G., Schoeni, R. F., & Andreski, P. M. (2010). Trends in health of older adults in the United States: Past, present, future. Demography, 47(1), S17–S40. doi: 10.1353/dem.2010.0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina, T. (2017). Adjusting for heterogeneous response thresholds in cross-country comparisons of self-reported health. The Journal of the Economics of Ageing, 10, 1–20. doi: 10.1016/j.jeoa.2017.08.002 [DOI] [Google Scholar]
- NatCen Social Research. (2020). ELSA: User guide to the main interview datasets—Waves 1 to 9.https://www.ucl.ac.uk/epidemiology-health-care/sites/epidemiology-health-care/files/5050_elsa_waves_1-9_interviewer_data_user_guide_v1.pdf
- National Academies of Sciences, Engineering, and Medicine (Ed.). (2021). High and rising mortality rates among working-age adults. National Academies Press. [PubMed] [Google Scholar]
- National Center for Health Statistics (U.S.) (Ed.). (2019). Long-term care providers and services users in the United States, 2015–2016. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Google Scholar]
- OECD . (n.d.). OECD data—Inflation (CPI). The OECD. http://data.oecd.org/price/inflation-cpi.htm
- OECD . (1999). Classifying educational programmes—Manual for ISCED-97 implementation in OECD countries. OECD. [Google Scholar]
- Phillips, D., Lin, Y.-C., Wight, J., Chien, S., & Lee, J. (2017). Harmonized ELSA version E.https://www.ucl.ac.uk/epidemiology-health-care/sites/epidemiology-health-care/files/5050_harmonized_elsa_e.pdf
- Reinhard, S. C., Feinberg, L. F., Houser, A., Choula, R., & Evans, M. (2019). Valuing the invaluable: 2019 update: Charting a Path Forward. AARP Public Policy Institute. doi: 10.26419/ppi.00082.001 [DOI] [Google Scholar]
- Schneider, E. C., Shah, A., Doty, M. M., Tikkanen, R., Fields, K., & Williams, R. D., II. (2021). Mirror, Mirror 2021—Reflecting poorly: Health care in the U.S. compared to other high-income countries. The Commonwealth Fund. doi: 10.26099/01dv-h208 [DOI]
- Sengupta, M., Harris-Kojetin, L., Lendon, J., Caffrey, C., Rome, V., & Valverde, R. (2018). National and state estimates of long-term care services users: 2016 National Study of Long-term Care Providers. Innovation in Aging, 2(Suppl. 1), 474. doi: 10.1093/geroni/igy023.1772 [DOI] [PubMed] [Google Scholar]
- Sonnega, A., Faul, J. D., Ofstedal, M. B., Langa, K. M., Phillips, J. W., & Weir, D. R. (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. doi: 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spector, W. D., & Fleishman, J. A. (1998). Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 53B(1), S46–S57. doi: 10.1093/geronb/53B.1.S46 [DOI] [PubMed] [Google Scholar]
- Steptoe, A., & Di Gessa, G. (2021). Mental health and social interactions of older people with physical disabilities in England during the COVID-19 pandemic: A longitudinal cohort study. Lancet Public Health, 6(6), e365–e373. doi:10.1016/ S2468-2667(21)00069-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tipirneni, R., Karmakar, M., & Maust, D. T. (2021). Trends and disparities in functional impairment among US adults age 55–64, 2002 to 2016. Journal of General Internal Medicine, 36(12), 3903–3906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge, L. M., & Jette, A. M. (1994). The disablement process. Social Science & Medicine, 38(1), 1–14. doi: 10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Watts, M. O. (2020, February 4). Medicaid home and community-based services enrollment and spending—Issue brief—9294-02. KFF. https://www.kff.org/report-section/medicaid-home-and-community-based-services-enrollment-and-spending-issue-brief/ [Google Scholar]
- Woolf, S. H., & Aron, L. (2013). US health in international perspective: Shorter lives, poorer health. National Academies Press. [PubMed] [Google Scholar]
- World Inequality Database (WID). (n.d.). WID—World Inequality Database. https://wid.world/world/ [Google Scholar]
- Zajacova, A., & Montez, J. K. (2018). Explaining the increasing disability prevalence among mid-life US adults, 2002 to 2016. Social Science & Medicine, 211, 1–8. doi: 10.1016/j.socscimed.2018.05.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaninotto, P., Batty, G. D., Stenholm, S., Kawachi, I., Hyde, M., Goldberg, M., ... & Head, J. (2020). Socioeconomic inequalities in disability-free life expectancy in older people from England and the United States: A cross-national population-based study. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 75(5), 906–913. doi: 10.1093/gerona/glz266 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.