Abstract
Structural and social determinants of health (SSDoH) are environmental conditions in which individuals are born, live, learn, work, play, worship, and age that affect health, functioning, and quality-of-life outcomes across the life course. Growing evidence suggests that SSDoH can help to explain heterogeneity in outcomes in Alzheimer’s disease and Alzheimer’s disease and related dementias (AD/ADRD) research and clinical practice. The National Institute on Aging has prioritized collecting SSDoH data to elucidate disease mechanisms and aid discovery of disease-modifying treatments. However, a major nexus of AD/ADRD research, the national network of Alzheimer’s Disease Research Centers (ADRCs), collects few SSDoH data. We describe a framework for feasibly gathering and modeling SSDoH data across ADRCs. We lay out key constructs, their measures, and empirical evidence for their importance in elucidating disease and prevention mechanisms. Toward a goal of translation, the framework proposes a modular structure with a core set of measures and options for adjunctive modules. We describe considerations for measuring SSDoH in existing geographically and culturally diverse research cohorts. We also outline a rationale for universal implementation of a set of SSDoH measures and juxtapose the approach with alternatives aimed at collecting SSDoH data.
Keywords: SSDOH, Alzheimer’s, Measurement, Social determinants of health
Structural and social determinants of health (SSDoH) are environmental conditions where individuals are born, live, learn, work, play, worship, and age that affect health, functioning, and quality-of-life outcomes across the life span. SSDoH can affect an individual’s risk for Alzheimer’s disease and Alzheimer’s disease and related dementias (AD/ADRD), likelihood to receive a diagnosis, and prognosis (Centers for Disease Control and Prevention, 2020; Hill et al., 2015). Growing evidence demonstrates that SSDoH explains heterogeneity in cognitive, functional, biomarker, and interventional outcomes in AD/ADRD research and clinical practice (Centers for Disease Control and Prevention, 2020; Hill et al., 2015). The ability to characterize and study SSDoH in AD/ADRD is crucial for advancing scientific understanding and developing interventions to improve health outcomes.
Social determinants include aspects of the social and physical environments. Structural determinants refer to social processes, systems, and policy. In practice, social determinants comprise an individual’s microsystem and mesosystem, and structural factors comprise the exosystem and macrosystem (Vélez-Agosto et al., 2017). Though there is substantial overlap between structural and social determinants, the distinction is useful for informing actionability, which is an essential element of achieving the overall goal of improving health outcomes in AD/ADRD. For example, individuals can decide whether or not to seek health care, but their receipt of quality health care is dependent upon system-level factors, like insurance, availability of hospitals, knowledge and skill of care providers, and availability of evidence-based treatments. Furthermore, an individual’s decision to seek health care is informed by structural and social determinants such as symptom recognition, cultural practices, and past experiences. This conceptual distinction facilitates a pipeline of translation from research to practice and policy that ensures impact, not simply intent. Knowledge of social determinants may help inform clinical interventions, while knowledge of structural determinants often informs public policies and practices.
The National Institute on Aging (NIA) has prioritized funding for the collection and study of SSDoH data in order to elucidate disease mechanisms and aid discovery of disease-modifying treatments. Efforts are underway to enhance collection of SSDoH data in NIA-funded Alzheimer’s Disease Research Centers (ADRCs). Informed by NIA’s diversity and disparities framework (Hill et al., 2015)—including target domains and special populations—we propose a framework for feasibly gathering and modeling SSDoH data across ADRCs, which support a large portion of AD/ADRD research in the United States and often serve as a model for programs in the field. Our proposed approach unifies routine collection across a national network of research centers to leverage shared resources, advance discovery of interventions that improve community and individual outcomes, and develop wide sociocultural representation of research samples.
A Unifying Framework to Measure SSDoH
We used a multidisciplinary approach to develop a framework for assessing SSDoH relevant to AD/ADRD with a primary goal to harmonize a set of evidence-based measures. Mechanisms of action in our framework are informed by Fundamental Cause Theory, Ecological Systems Theory (EST), and the NIA Health Disparities Framework (Bronfenbrenner, 1992; Hill et al., 2015; Phelan et al., 2010). Fundamental Cause Theory holds that social conditions are fundamental causes of health inequalities. EST operationalizes dimensions of social conditions (micro-, meso-, macro-, chrono levels) that alone and together act as determinants in health outcomes and health care disparities. The NIA’s Health Disparities Framework provides a landscape for pursuing opportunities for innovative solutions to health disparities research related to aging and AD/ADRD.
The SSDoH domains in our framework are based on Healthy People 2030 (Office of Disease Prevention and Health Promotion, n.d.). Through a review of extant research and scholarship on brain health and aging, we identified seven specific SSDoH domains that appear foundational to AD/ADRD. Measures of these seven core domains from across four ADRCs, which volunteered to contribute and serve geographically and sociodemographically divergent populations, were cataloged and, where feasible, harmonized (Table 1). Additional information is available in Supplementary Table 1.
Table 1.
Structural and Social Determinants of Health Measures by Collection at Select Alzheimer’s Disease Research Centers
| EST, domains, and measures | Construct assessed | UW-M | Rush | UPenn | WUSTL |
|---|---|---|---|---|---|
| Microsystem | |||||
| Social stressors and perceived stress | |||||
| Adverse Childhood Experiences Scales | Childhood stressors | ✓ | ✓ | ✓ | |
| Perceived Stress Scale | Subjective stress | ✓ | ✓ | ✓ | ✓ |
| Everyday Discrimination Scale | Lifetime stressors | ✓ | ✓ | ✓ | |
| Social Readjustment Rating Scale | Adulthood stressors | ✓ | ✓ | ✓ | |
| Minority Aging Research Study (MARS) | Childhood stressors | ✓ | ✓ | ✓ | |
| Social support | |||||
| Lubben Social Network Scale | Social support | ✓ | ✓ | ||
| Multidimensional Scale of Perceived Social Support | ✓ | ✓ | |||
| Education and health literacy | |||||
| MARS | Educational experiences | ✓ | ✓ | ✓ | |
| Calgary Charter on Health Literacy Scale | Health literacy | ✓ | ✓ | ||
| Health Literacy | Health and financial literacy | ✓ | |||
| Modified UDS A-1 Subject Demographic | Years of education | ✓ | ✓ | ||
| Health and Retirement Study | Maternal years of education | ✓ | |||
| Occupation | |||||
| Modified UDS A-1 Subject Demographic | Occupation | ✓ | ✓ | ✓ | ✓ |
| Occupational Cognitive Response Score | Occupation cognition | ✓ | |||
| Exosystem | |||||
| Social positioning | |||||
| Modified UDS A-1 Subject Demographic | Occupation, education | ✓ | ✓ | ✓ | ✓ |
| Socioeconomic Status and Strain (SES) | SES | ✓ | ✓ | ✓ | |
| MacArthur Scale of Subjective Social Status (MacArthur SSS Scale) | Social positioning | ✓ | ✓ | ✓ | |
| Social/built environment/neighborhood | |||||
| Modified Life-course Sociodemographic Neighborhood Exposures Questionnaire | Neighborhood strengths | ✓ | ✓ | ||
| Area Deprivation Index | Neighborhood stressors | ✓ | ✓ | ✓ | ✓ |
| Macrosystem | |||||
| Social identity | |||||
| Sexual Orientation and Gender Identity (SOGI) | SOGI | ✓ | ✓ | ✓ | ✓ |
| Modified UDS A-1 Subject Demographics | Age, race, ethnicity | ✓ | ✓ | ✓ | ✓ |
| Modified Home Language Survey | Language | ✓ | |||
| Washington Group Short Set on Functioning | Disability | ✓ | |||
| Modified Brief Multidimensional Measure of Religiousness/Spirituality | Religion | ✓ | |||
| National Health Interview Survey | Childhood learning disability | ✓ |
Note: UW-M = University of Wisconsin–Madison; Rush = Rush University; UPenn = University of Pennsylvania; WUSTL = Washington University in St. Louis; EST = Ecological Systems Theory.
Core Battery of SSDoH Measures
In this section, we describe seven core conceptual domains for SSDoH in AD/ADRD, pursuant to EST. We include the constructs’ theoretical underpinnings, validated measures, and empirical evidence that supports their potential value for elucidating AD/ADRD mechanisms.
Microsystem
Social stressors and perceived stress
Social stressors—financial insecurity and strain, discrimination, caregiving, mental and physical conditions, managing health conditions, and other factors—can contribute to perceived stress (Alzheimer’s Association, 2021; Peavy et al., 2012), which correlates with cognitive function (Shields et al., 2017) and can compromise participation in brain health behaviors (Senn et al., 2014). Life course stressors and community-specific stressors, such as discrimination, are associated with cognitive function and partially explain racial disparities in AD/ADRD outcomes (Zuelsdorff et al., 2020). Measuring stressors from early childhood can help elucidate critical and sensitive periods for stress in brain health and AD/ADRD outcomes (Lee et al., 2003) and contextual factors elevating exposure to stress and stressors (Hannum et al., 2009).
Social support
Social support can buffer stress, facilitate research participation and health behaviors, moderate genetic and environmental vulnerabilities, and promote well-being for older persons (Ozbay et al., 2007), all of which may directly and indirectly influence brain health and AD/ADRD outcomes. Social networks—which include friends, family and peers, and colleagues—have distinct distributions across sociocultural groups and the life course that can influence health outcomes (Lin, 1999). Minoritized populations, for example, often report smaller networks but less social isolation than White populations, while older adults report that narrowing of social networks is often associated with better emotional well-being (English & Carstensen, 2014).
Education and health literacy
Studies show fewer years of education correlate with higher risk and incidence of Alzheimer’s diagnosis and differences in brain structure (Hill et al., 2015). Quality of education correlates with cognitive performance (Chin et al., 2012), varies geographically in the United States (Hanushek & Yilmaz, 2011), and corresponds to mid- and late-life health determinants such as health literacy and other behaviors (James et al., 2012). Maternal years of education is a useful measure of life course and transgenerational social class. Nuanced education measures enable the mapping of geographic variability and complex life course mechanisms to AD/ADRD outcomes.
Occupation
Manual labor, such as goods production, may increase the likelihood of dementia diagnosis (Qiu et al., 2003), while other occupations may exert protective effects against dementia outcomes (Stern et al., 1994). Occupational conditions can also serve as barriers to health care access, health behaviors, and research participation. Structural factors, like segregation and other racialized education exposures, also contribute to disparities in occupation type (Marquez et al., 2010), retirement, physical stress, and other factors that may differentially influence AD/ADRD outcomes.
Mesosystem
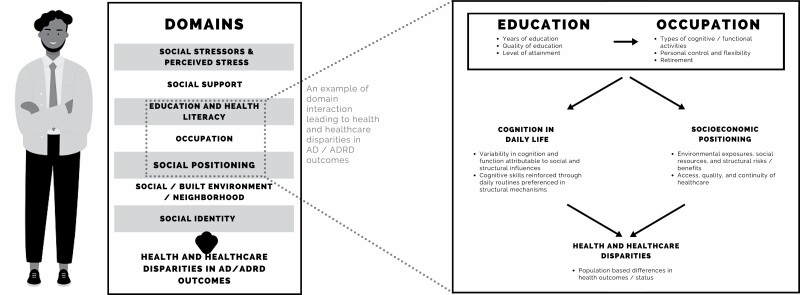
The combination of domains within the microsystem represents the mesosystem. SSDoH domains are often interconnected and may convey multiple influences relevant to aging and AD/ADRD. Furthermore, these influences may interact across EST systems. For example, as depicted in Figure 1, low education (Microsystem) may act as a social determinant of neurodiversity in daily life that can increase one’s risk for cognitive decline while also influencing socioeconomic position (Exosystem), which is known to convey structural risks associated with disparities in health outcomes and health care inequalities.
Figure 1.
Aspects of individuals’ identities, biology, and lived experiences capture structural and social determinants of health that interact to influence aging and Alzheimer’s disease and related dementias (ADRD) outcomes.
Exosystem
Social positioning
Social positioning includes socioeconomic position and social status. The Centers for Disease Control and Prevention (2019) defines socioeconomic position as the amount of money, power, and resources a person has. Educational attainment and occupation contribute to socioeconomic status (Figure 1). Lower or diminished socioeconomic status—which impedes access to stable, safe housing, healthy food, and quality health care—contributes to health care disparities and risk of dementia diagnosis (Hill et al., 2015). Moreover, childhood socioeconomic effects influence cognition across the life course and, in later life, AD/ADRD outcomes (Greenfield & Moorman, 2019). Social status—the relative rank that an individual holds in a social hierarchy—can affect mental and physical outcomes and one’s ability to access social resources (Amir et al., 2019). Social positioning alone and in combination with other SSDoH can have powerful effects on health outcomes (Hill et al., 2015).
Social/built environment/neighborhood
Neighborhood and built environment factors can influence cognitive function and AD/ADRD outcomes (Besser et al., 2019). Participants’ approximate (buffered) home residences—childhood and adulthood—can be linked with publicly available, longitudinal neighborhood data to provide rich characterizations of individuals’ local environments across the life course. Participant self-report measures can aid in gathering data on how individuals engage their local environments (Mendes de Leon et al., 2009).
Macrosystem
Social identity
Aspects of identity are central to SSDoH and warrant study in AD/ADRD. They include self-report of age, race, ethnicity, religion, language, disability, sexual orientation (Flatt et al., 2021; Stites et al., 2021), sex, and gender (Stites, 2020). Personal characteristics—being older, female, and African American—can have concurrent roles as markers of AD/ADRD risk (Alzheimer’s Association, 2021). The intersections between sociocultural and biologic attributions have tremendous implications for stigma and discrimination persons face in living with dementia (Stites et al., 2018). They do not dictate AD/ADRD risk but rather correspond with SSDoH and other experiences that convey elevated risks. They also influence racial, ethnic, and sex/gender disparities in health care and AD/ADRD outcomes (Cabin & Stites, 2021; Sternthal et al., 2011).
Uniform and standardized approaches to classify individuals by sociocultural characteristics can aid resource sharing and translation of SSDoH research into policy and practice interventions. National Institutes of Health (NIH, 2015) offer standards for collection of race and ethnicity data. These federal classifications of race and ethnicity are exceedingly broad in order to facilitate data sharing across large geopolitical areas and guide population-level policy. More discrete groupings may be advantageous to facilitate the study of within-group heterogeneity. Measures of self-reported sex, sexual orientation, and gender identity are also available (Flatt et al., 2021). Disability status should also be assessed as those living with impairments can experience distress and anxiety from social factors—that is, discrimination, prejudice, and exclusion—that impede their social and political participation (Trani et al., 2016).
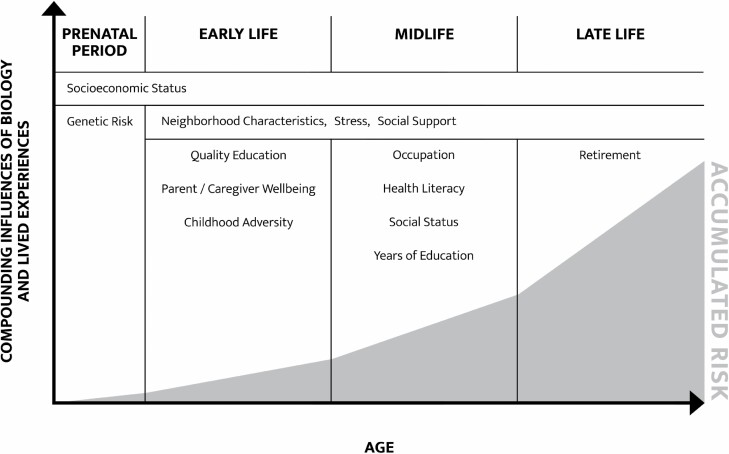
Chronosystem
Our framework subsumes a life course perspective, which recognizes that events and exposures compound over the lifetime (Figure 2) and have outsized impacts on health during critical and sensitive periods from the prenatal period and through later life. Thus, several SSDoH domains warrant repeated measurement along the life course. In prior sections, we outline opportunities to consider effects of specific life stages—that is, retirement and age-related social network narrowing—and the life course—that is, cumulative effects of subjective stress and life course stressors—in SSDoH domains.
Figure 2.
Individuals’ lived experiences and biology have cumulative effects over the life course.
SSDoH Assessment Modules
Our framework uses a modular structure to augment the core battery with population-specific SSDoH measures, which are conceptualized to operate like the SSDoH in the core battery. A module contains SSDoH for a population subgroup, as defined by specific demographic features or sociocultural experiences, and compliments the core set of universal SSDoH. Selection and implementation of modules are expected to reflect a center’s local community and thereby research cohort.
We present, as illustrative cases, four modules for populations defined as Latin, Black and African American, refugee and immigrant, and Native American and indigenous. These populations are among those identified by NIH as having priority for health disparities research and warranting particular attention to promote productive and healthy aging (Hill et al., 2015). While they have divergent lived experiences, themes of unique cultural values, social and economic adversity, and access to social capital and structural resources are common SSDoH across populations. The goal of presenting these priority populations is to demonstrate consideration of SSDoH in specific groups and highlight commensurate measures (Supplementary Table 2), based on the expert opinion of AD/ADRD researchers conducting studies with these groups.
Latin Populations
Latino/a/x or Hispanic refers to people born, or with ancestors, from Latin American countries or from Spanish-speaking countries, respectively. In the United States, the number of Latinos with AD/ADRD is expected to increase (Alzheimer’s Association, 2021). Compared to older non-Latino Whites, older Latinos have a higher risk and prevalence of AD/ADRD (Chin et al., 2011).
Cultural heritage or country of origin can be useful for capturing community-specific stress in Latino populations. For example, one study found that Mexicans had higher levels of immigration and acculturative stress compared to Cuban or Dominican immigrants in the United States (Cervantes et al., 2019). In another study of diverse Latinos, more acculturative stress was associated with poorer performance on cognitive measures (Muñoz et al., 2021).
Cultural values of familismo, marianismo, fatalismo, and machismo influence behaviors relevant to AD/ADRD. Familismo, as measured for example by Sabogal’s Familism Scale (Campos et al., 2019), is the “strong identification and attachment of individuals with their families (nuclear and extended) and solidarity among members of the same family” (Sabogal et al., 1987). Familismo and marianismo—a traditional Latin American view of femininity—may aid in conceptualizing participation in caregiving and the medical establishment. In contrast, machismo—a traditional Latin American view of masculinity—may be informative in understanding how to reduce AD/ADRD risk (Moreira et al., 2018). Fatalismo—the belief that all events are predetermined and humans are powerless to change them—underlies the salience of religiosity and spirituality in Latin communities (Moreira et al., 2018) and may convey resilience factors with important roles in the AD/ADRD patient and caregiver experiences.
Immigrant and Refugee Communities
Immigrants depart their countries of origin for mostly negative reasons. Economic migrants seek better financial opportunities, asylees seek international protection from dangers in their home country, and refugees seek resettlement fleeing violence/conflict, political, religious, or ethnic persecution. For decades, the United States has led the world in the number of immigrants (Connor & Manuel Krugstad, 2018), with over three million refugees resettled nationally. Refugees and internally displaced people face multiple disadvantages, placing them at risk for poor AD/ADRD outcomes.
The refugee experience is, broadly, composed of an emergency relocation and a resettlement phase. The first particularly affects children who are a third of the world population but represent half of the global refugee population. The childhood refugee experience is characterized by stress, anxiety, depression, and trauma, which are all AD/ADRD risk factors (Donley et al., 2018; Livingston et al., 2020). Capturing these childhood sequalae may aid understanding of life course effects in AD/ADRD. Measuring multidimensional poverty (Alkire & Foster, 2011) and deprivation and trauma exposure (Mollica et al., 1992) allow characterizing SSDoH in immigrant and refugee populations in childhood and adulthood.
Upon resettlement, refugees endure acculturation pressures while often being perceived as burdens on social systems and as market competitors (Alemi & Stempel, 2018). Refugees contend with limited access to quality health care, overstretched economic resources, and employment barriers (Kerwin & Nicholson, 2021). Stresses of displacement and relocation are magnified by loneliness, isolation, and erosion of traditional values (Alemi et al., 2014). Refugees may also be living with injuries and disabilities acquired during emigration, which compound vulnerabilities to emotional, physical, and sexual violence (Kett & Trani, 2010).
Native American and Indigenous Populations
Indigenous people of North America (INA) continue to experience the long-term effects of colonialism. Stresses of colonialism manifest themselves in multiple social pathologies and physical disease. Physiological stress processes and unhealthy behaviors as self-treatment of stresses arising from a life of vulnerability contribute to cardiovascular and cardiometabolic dysfunction (Jackson et al., 2010) as well as elevate the risk for developing type 2 diabetes and its comorbidities. Social adversities experienced in adolescence, such as exposure to peer, community, and collective violence, also elevate the risk of behavioral and physical health impairments later in life (El Mhamdi et al., 2019). Over time, these conditions can increase the risk of vascular lesions in the brain culminating in impaired cognition (El Mhamdi et al., 2019).
Cultural values and perspectives are essential SSDoH in INA populations, shaping opportunities for early detection, research enrollment and participation, and helping with family caregiver coping. Hallucinations may be interpreted as positive events wherein the affected person is considered to be communicating with the “other side” before death, thereby proving the existence of an afterlife (Henderson & Henderson, 2002). Medical perspectives that suggest that dementia limits one’s experience of life are incompatible with some INA cultural concepts that interpret dementia progression as a life-expanding experience (Jacklin et al., 2015).
Past personal and community experiences with institutionalized medicine can be key indicators of prior cultural traumas and barriers to care as individuals age. Optimal communications between providers and care receivers are facilitated by shared cultural understandings of affected persons and their social network (Jacklin & Pitawanakwat, 2019). Measures of health and health care communication may be useful in INA populations.
Black and African American Populations
Nomenclature associated with Black/African American populations has shifted over time. For the current analysis, we refer to Black populations as those existing globally and characterized by an intersecting set of skin tone, facial features, and hair textures, while African American communities are comprised of Blacks with ancestry within the United States. As such, Blacks/African Americans represent one of the most diverse groups in the United States, with widely varying geographic locations of birth within and outside of the United States, national migratory patterns, sexual orientation and gender identity, faith-based practices, and socioeconomic status—all lending an intersectional lens to lived experiences affected by racism and discrimination within the United States and globally (Tamir et al., 2021). Despite this diversity, Black/African American populations are connected in their universal experiences related to structural and social adversity, that is, systemic racism. Hence, SSDoH assessment in Black/African American communities must incorporate these lived and diverse experiences; how they affect access to and quality of resources such as employment, education, housing, and health care; and link to chronic diseases of aging, including AD/ADRD and their risk factors (Thornton et al., 2016). These experiences are interwoven with elevated risk for AD/ADRD burden experienced by Black/African American communities as well as the deleterious health impacts of dementia caregiver stress and burden largely experienced by Black/African American women (Alzheimer’s Association, 2021).
Measuring SSDoH offers a seminal step to engaging with Black/African American communities to eradicate AD/ADRD and decrease AD/ADRD risk. It requires addressing the historical and current impact of systemic and structural racism and discrimination on the cognitive health of Black/African American communities (Chin et al., 2011; Hill et al., 2015). As such, key foci of SSDoH measures are the real and perceived impacts of racism and discrimination and their direct links to cognitive and healthy aging for Black/African Americans communities, which include persons living with dementia, persons at elevated risk for AD/ADRD, and their caregivers (Alzheimer’s Association, 2021).
Modes of Data Collection
The SSDoH modular framework is adaptable, aimed at meeting the needs of geographically and culturally diverse AD/ADRD research cohorts. Pilot testing is underway to assure the battery operates equitably across administration modalities (in-person, telephone, or mobile phone, and self-administered online). Initial administration of the core battery requires ~30–40 min, with follow-up administrations shorter in duration. The battery can be completed over multiple self-administered sessions (Supplementary Table 3). Many items can be completed by a spouse or other research partner if proxy responses are needed. Moreover, modules can be added or changed based on organizational priorities.
Rationale for Universal Implementation of SSDoH Measures
We juxtapose our rationale for universal implementation of an SSDoH battery with an alternative of implementing measures via investigator-initiated grants. As evidence grows about the importance of distal and proximal social determinants for brain and cognition trajectories in later life, some individual investigators have initiated collection of SSDoH data within their affiliate ADRC cohorts. We argue that, while investigator-initiated data collection may continue to be ideal for local community samples and other specialized data, standardized collection of foundational SSDoH measures provides crucial benefits to the AD/ADRD field and the public it serves. Measures highlighted in our framework are not a comprehensive set of SSDoH measures that shape ADRD-relevant exposures; many additional data may complement these modules.
Universal collection of a battery that captures core domains ensures that participant data can be harmonized across ADRCs. This maximizes statistical power to explore risk, resilience, and potential interventions in underrepresented populations who experience disproportionate burdens of dementia. Universal collection also facilitates both early career and senior investigators with expertise in SSDoH leveraging such data to readily and consistently prioritize underserved populations, regardless of the physical location of their employment and/or their affiliated ADRCs.
Conclusion and Recommendations
While study of SSDoH in AD/ADRD research is gaining momentum, significant work remains, emphasized by three reasons. First, consideration of SSDoH may help mitigate disparities in groups that are disproportionately burdened by AD/ADRD. Second, the focus on biology and behavior alone, without consideration of social and structural influences, places causes of disparity and onuses of risk reduction unilaterally on individuals without any recognition of the contributions of systems. Last, SSDoH exert influences essential to developing intervention models that are accessible and applicable to many populations.
In an effort to advance and expand this work, we propose a framework for gathering foundational data on SSDoH relevant to AD/ADRD. The framework is a mechanism to elevate cultural awareness of the needs of diverse communities at greatest risk for AD/ADRD and probable cumulative effects of SSDoH on cognition and brain health. Similarities and divergences of SSDoH across populations underscore opportunities for natural synergies in assessment and collaboration among ADRCs.
Broadly, research on SSDoH has been gaining momentum over the last two decades, but investigation of SSDoH in older populations, and in cognitive aging particularly, has not experienced the same growth. Developing this area of research requires addressing gaps in key SSDoH measures. Many gaps remain in the sparse availability of SSDoH measures to capture, as examples, disability, language, and INA lived experiences. Measures are an essential early step to facilitate researchers’ ability to identify, characterize, and track SSDoH as they shape AD/ADRD outcomes.
Collecting SSDoH is a necessary initial step; however, ultimately, identifying and building relationships with community organizations will facilitate health equity in aging by addressing and eliminating harmful SSDoH. To do this, community-partnered and community-informed processes are needed to elucidate the needs of community members and prioritize aspects of cognitive aging (Chin et al., 2011). Both community-engaged research (CER) and patient-centered outcomes research (PCOR) approaches acknowledge the potential lack of trustworthiness that may exist for researchers and their institutions but also encourage mutually beneficial and bidirectional relationships built upon trust to determine a shared purpose for research, one that is both scientifically and community relevant (Gilmore-Bykovskyi et al., 2019).
Encouraging implementation of CER and PCOR that employ mixed methods will aid in robust examination of lived experiences, biological processes, biomarkers, and other mechanisms related to AD/ADRD and cognitive aging while also making tangible advances in building socioculturally diverse research samples, community trust and engagement, and interdisciplinary scientific communities in aging and AD/ADRD research (Gilmore-Bykovskyi et al., 2019; Glover et al., 2019). This framework offers an initial step toward these broader goals.
Supplementary Material
Acknowledgments
The authors thank Kristin Harkins for her persistence and attention to detail in the preparation of this manuscript. The authors also thank Nina Miller for the contribution of her graphic design skills.
Funding
This work was supported by grants from the National Institute on Aging (NIA; P30AG012836-25-S2, P30AG010124, U24AG058556, P30AG10161, P30AG062715). S.D.S. is supported by the Alzheimer’s Association (AARF-17-528934) and the NIA (K23AG065442). G.B. is supported by the NIA (R01AG068183, R01AG067428, R01AG056466) and by the BrightFocus Foundation (A2021142S). D.M.-H. is supported by the Alzheimer’s Association (AACSF-19-617940) and NIA (K23AG065499). M.Z. is supported by the NIA (R03AG063303, R03AG063304) and the Alzheimer’s Association (AARF-18-562958).
Conflict of Interest
None declared.
References
- Alemi, Q., James, S., Cruz, R., Zepeda, V., & Racadio, M. (2014). Psychological distress in Afghan refugees: A mixed-method systematic review. Journal of Immigrant and Minority Health, 16(6), 1247–1261. doi: 10.1007/s10903-013-9861-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alemi, Q., & Stempel, C. (2018). Discrimination and distress among Afghan refugees in northern California: The moderating role of pre- and post-migration factors. PLoS One, 13(5), e0196822. doi: 10.1371/journal.pone.0196822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkire, S., & Foster, J. (2011). Counting and multidimensional poverty measurement. Journal of Public Economics, 95(7–8), 476–487. doi: 10.1016/j.jpubeco.2010.11.006 [DOI] [Google Scholar]
- Alzheimer’s Association . (2021). Facts and figures. https://www.alz.org/alzheimers-dementia/facts-figures
- Amir, D., Valeggia, C., Srinivasan, M., Sugiyama, L. S., & Dunham, Y. (2019). Measuring subjective social status in children of diverse societies. PLoS One, 14(12), e0226550. doi: 10.1371/journal.pone.0226550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Besser, L., Galvin, J. E., Rodriguez, D., Seeman, T., Kukull, W., Rapp, S. R., & Smith, J. (2019). Associations between neighborhood built environment and cognition vary by apolipoprotein E genotype: Multi-Ethnic Study of Atherosclerosis. Health & Place, 60, 102188. doi: 10.1016/j.healthplace.2019.102188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner, U. (1992). Ecological systems theory. In R. Vasta (Ed.), Six theories of child development: Revised formulations and current issues (pp. 187–249). Jessica Kingsley Publishers. [Google Scholar]
- Cabin, W., & Stites, S. D. (2021). Mental health issues in older adults: Social determinants and modalities of service delivery. In Jurkowski E. T. & Guest M. A. (Eds.), Social determinants of healthy aging: A public health perspective. American Public Health Association. [Google Scholar]
- Campos, B., Roesch, S. C., Gonzalez, P., Hooker, E. D., Castañeda, S. F., Giachello, A. L., Perreira, K. M., & Gallo, L. C. (2019). Measurement properties of Sabogal’s familism scale: Findings from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study. Journal of Latina/o Psychology, 7(4), 257–272. doi: 10.1037/lat0000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2019, December 19). Questions frequently asked about social determinants of health. https://www.cdc.gov/nchhstp/socialdeterminants/faq.html
- Centers for Disease Control and Prevention . (2020, December 31). Social determinants of health and Alzheimer’s disease and related dementias. https://www.cdc.gov/aging/disparities/social-determinants-alzheimers.html
- Cervantes, R. C., Gattamorta, K. A., & Berger-Cardoso, J. (2019). Examining difference in immigration stress, acculturation stress and mental health outcomes in six Hispanic/Latino nativity and regional groups. Journal of Immigrant and Minority Health, 21(1), 14–20. doi: 10.1007/s10903-018-0714-9 [DOI] [PubMed] [Google Scholar]
- Chin, A. L., Negash, S., & Hamilton, R. (2011). Diversity and disparity in dementia: The impact of ethnoracial differences in Alzheimer disease. Alzheimer Disease and Associated Disorders, 25(3), 187–195. doi: 10.1097/WAD.0b013e318211c6c9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin, A. L., Negash, S., Xie, S., Arnold, S. E., & Hamilton, R. (2012). Quality, and not just quantity, of education accounts for differences in psychometric performance between African Americans and white non-Hispanics with Alzheimer’s disease. Journal of the International Neuropsychological Society, 18(2), 277–285. doi: 10.1017/S1355617711001688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor, P., & Manuel Krugstad, J. (2018). For the first time, U.S. resettles fewer refugees than the rest of the world. Pew Research Center. https://www.pewresearch.org/fact-tank/2018/07/05/for-the-first-time-u-s-resettles-fewer-refugees-than-the-rest-of-the-world/ [Google Scholar]
- Donley, G. A. R., Lönnroos, E., Tuomainen, T. P., & Kauhanen, J. (2018). Association of childhood stress with late-life dementia and Alzheimer’s disease: The KIHD study. European Journal of Public Health, 28(6), 1069–1073. doi: 10.1093/eurpub/cky134 [DOI] [PubMed] [Google Scholar]
- El Mhamdi, S., Lemieux, A., Abroug, H., Ben Salah, A., Bouanene, I., Ben Salem, K., & al’Absi, M. (2019). Childhood exposure to violence is associated with risk for mental disorders and adult’s weight status: A community-based study in Tunisia. Journal of Public Health (Oxford, England), 41(3), 502–510. doi: 10.1093/pubmed/fdy149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English, T., & Carstensen, L. L. (2014). Selective narrowing of social networks across adulthood is associated with improved emotional experience in daily life. International Journal of Behavioral Development, 38(2), 195–202. doi: 10.1177/0165025413515404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flatt, J. D., Cicero, E. C., Kittle, K. R., & Brennan-Ing, M. (2021). Recommendations for advancing research with sexual and gender minority older adults. The Journals of Gerontology: Series B, gbab127. doi: 10.1093/geronb/gbab127 [DOI] [PubMed] [Google Scholar]
- Gilmore-Bykovskyi, A. L., Jin, Y., Gleason, C., Flowers-Benton, S., Block, L. M., Dilworth-Anderson, P., Barnes, L. L., Shah, M. N., & Zuelsdorff, M. (2019). Recruitment and retention of underrepresented populations in Alzheimer’s disease research: A systematic review. Alzheimer’s & Dementia (New York, N. Y.), 5, 751–770. doi: 10.1016/j.trci.2019.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover, C. M., CoCroft, S., James, B. D., & Barnes, L. L. (2019). Perceptions of risk factors for Alzheimer disease among community-dwelling, nondemented older African Americans. Alzheimer Disease and Associated Disorders, 33(3), 254–259. doi: 10.1097/WAD.0000000000000314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield, E. A., & Moorman, S. M. (2019). Childhood socioeconomic status and later life cognition: Evidence from the Wisconsin Longitudinal Study. Journal of Aging and Health, 31(9), 1589–1615. doi: 10.1177/0898264318783489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannum, E., Sargent, T., & Yu, S. (2009). Poverty, parental ill health and children’s access to schooling in rural Gansu, China. Provincial China, 1(2), 24–60. doi: 10.5130/pc.v1i2.1257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanushek, E. A., & Yilmaz, K. (2011). Urban education: Location and opportunity in the United States. In N. Brooks, K. Donaghy, & G.-J. Knaap (Eds.), The Oxford handbook of urban economics and planning (pp. 583–615). Oxford University Press. doi: 10.1093/oxfordhb/9780195380620.013.0027 [DOI] [Google Scholar]
- Henderson, J. N., & Henderson, L. C. (2002). Cultural construction of disease: A “supernormal” construct of dementia in an American Indian tribe. Journal of Cross-Cultural Gerontology, 17(3), 197–212. doi: 10.1023/a:1021268922685 [DOI] [PubMed] [Google Scholar]
- Hill, C. V., Pérez-Stable, E. J., Anderson, N. A., & Bernard, M. A. (2015). The National Institute on Aging health disparities research framework. Ethnicity & Disease, 25(3), 245–254. doi: 10.18865/ed.25.3.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacklin, K., Pace, J. E., & Warry, W. (2015). Informal dementia caregiving among indigenous communities in Ontario, Canada. Care Management Journals, 16(2), 106–120. doi: 10.1891/1521-0987.16.2.106 [DOI] [PubMed] [Google Scholar]
- Jacklin, K., & Pitawanakwat, K. (2019). ADI—The circle of life; indigenous knowledge about dementia in Canada. https://www.alzint.org/news/the-circle-of-life-indigenous-knowledge-about-dementia-in-canada/
- Jackson, J. S., Knight, K. M., & Rafferty, J. A. (2010). Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100(5), 933–939. doi: 10.2105/AJPH.2008.143446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James, B. D., Boyle, P. A., Bennett, J. S., & Bennett, D. A. (2012). The impact of health and financial literacy on decision making in community-based older adults. Gerontology, 58(6), 531–539. doi: 10.1159/000339094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerwin, D., & Nicholson, M. (2021). Charting a course to rebuild and strengthen the US Refugee Admissions Program (USRAP): Findings and recommendations from the Center for Migration Studies Refugee Resettlement Survey: 2020. Journal on Migration and Human Security, 9(1), 1–30. doi: 10.1177/2331502420985043 [DOI] [Google Scholar]
- Kett, M., & Trani, J.-F. (2010). Vulnerability and disability in Darfur | Forced Migration Review. https://www.fmreview.org/disability/kett-trani
- Lee, S., Kawachi, I., Berkman, L. F., & Grodstein, F. (2003). Education, other socioeconomic indicators, and cognitive function. American Journal of Epidemiology, 157(8), 712–720. doi: 10.1093/aje/kwg042 [DOI] [PubMed] [Google Scholar]
- Lin, N. (1999). Social networks and status attainment. Annual Review of Sociology, 25, 467–487. doi: 10.1146/annurev.soc.25.1.467 [DOI] [Google Scholar]
- Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., … Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet (London, England), 396(10248), 413–446. doi: 10.1016/S0140-6736(20)30367-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez, D. X., Neighbors, C. J., & Bustamante, E. E. (2010). Leisure time and occupational physical activity among racial or ethnic minorities. Medicine and Science in Sports and Exercise, 42(6), 1086–1093. doi: 10.1249/MSS.0b013e3181c5ec05 [DOI] [PubMed] [Google Scholar]
- Mendes de Leon, C. F., Cagney, K. A., Bienias, J. L., Barnes, L. L., Skarupski, K. A., Scherr, P. A., & Evans, D. A. (2009). Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults: A multilevel analysis. Journal of Aging and Health, 21(1), 155–171. doi: 10.1177/0898264308328650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollica, R. F., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. doi: 10.1097/00005053-199202000-00008 [DOI] [PubMed] [Google Scholar]
- Moreira, T., Hernandez, D. C., Scott, C. W., Murillo, R., Vaughan, E. M., & Johnston, C. A. (2018). Susto, Coraje, y Fatalismo: Cultural-bound beliefs and the treatment of diabetes among socioeconomically disadvantaged Hispanics. American Journal of Lifestyle Medicine, 12(1), 30–33. doi: 10.1177/1559827617736506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz, E., Gallo, L. C., Hua, S., Sliwinski, M. J., Kaplan, R., Lipton, R. B., González, H. M., Penedo, F. J., Tarraf, W., Daviglus, M. L., Llabre, M. M., & Isasi, C. R. (2021). Stress is associated with neurocognitive function in Hispanic/Latino adults: Results from HCHS/SOL Socio-Cultural Ancillary Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 76(4), 122–128. doi: 10.1093/geronb/gbz144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health . (2015). NOT-OD-15-089: Racial and ethnic categories and definitions for NIH diversity programs and for other reporting purposes. https://grants.nih.gov/grants/guide/notice-files/not-od-15-089.html
- Office of Disease Prevention and Health Promotion (n.d.). Social determinants of health—Healthy people 2030. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
- Ozbay, F., Johnson, D. C., Dimoulas, E., Morgan, C. A., Charney, D., & Southwick, S. (2007). Social support and resilience to stress. Psychiatry, 4(5), 35–40. Unique Identifier number: 2007-07464-009. [PMC free article] [PubMed] [Google Scholar]
- Peavy, G. M., Jacobson, M. W., Salmon, D. P., Gamst, A. C., Patterson, T. L., Goldman, S., Mills, P. J., Khandrika, S., & Galasko, D. (2012). The influence of chronic stress on dementia-related diagnostic change in older adults. Alzheimer Disease and Associated Disorders, 26(3), 260–266. doi: 10.1097/WAD.0b013e3182389a9c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan, J., Link, B., & Tehranifar, P. (2010). Social conditions as fundamental causes of health inequalities. Robert Wood Johnson Foundation. https://www.rwjf.org/en/library/research/2010/11/executive-summary/social-conditions-as-fundamental-causes-of-health-inequalities.html [DOI] [PubMed] [Google Scholar]
- Qiu, C., Karp, A., von Strauss, E., Winblad, B., Fratiglioni, L., & Bellander, T. (2003). Lifetime principal occupation and risk of Alzheimer’s disease in the Kungsholmen project. American Journal of Industrial Medicine, 43(2), 204–211. doi: 10.1002/ajim.10159 [DOI] [PubMed] [Google Scholar]
- Sabogal, F., Marín, G., Otero-Sabogal, R., Marín, B. V., & Perez-Stable, E. J. (1987). Hispanic familism and acculturation: What changes and what doesn’t? Hispanic Journal of Behavioral Sciences, 9(4), 397–412. doi: 10.1177/07399863870094003 [DOI] [Google Scholar]
- Senn, T. E., Walsh, J. L., & Carey, M. P. (2014). The mediating roles of perceived stress and health behaviors in the relation between objective, subjective, and neighborhood socioeconomic status and perceived health. Annals of Behavioral Medicine, 48(2), 215–224. doi: 10.1007/s12160-014-9591-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields, G. S., Doty, D., Shields, R. H., Gower, G., Slavich, G. M., & Yonelinas, A. P. (2017). Recent life stress exposure is associated with poorer long-term memory, working memory, and self-reported memory. Stress (Amsterdam, Netherlands), 20(6), 598–607. doi: 10.1080/10253890.2017.1380620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern, Y., Gurland, B., Tatemichi, T. K., Tang, M. X., Wilder, D., & Mayeux, R. (1994). Influence of education and occupation on the incidence of Alzheimer’s disease. Journal of the American Medical Association, 271(13), 1004–1010. doi: 10.1001/jama.1994.03510370056032 [DOI] [PubMed] [Google Scholar]
- Sternthal, M. J., Slopen, N., & Williams, D. R. (2011). Racial disparities in health: How much does stress really matter? Du Bois Review, 8(1), 95–113. doi: 10.1017/S1742058X11000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stites, S. (2020). The CoGenT3 Study: Cognition and gender trends in three American Generations. Innovation in Aging, 4(Suppl. 1), 817. doi: 10.1093/geroni/igaa057.2975 [DOI] [Google Scholar]
- Stites, S. D., Cao, H., Harkins, K., & Flatt, J. D. (2021). Measuring sex and gender in aging and Alzheimer’s research: Results of a national survey. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi: 10.1093/geronb/gbab226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stites, S. D., Milne, R., & Karlawish, J. (2018). Advances in Alzheimer’s imaging are changing the experience of Alzheimer’s disease. Alzheimer’s & Dementia (Amsterdam, Netherlands), 10, 285–300. doi: 10.1016/j.dadm.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamir, C., Budiman, A., Noe-Bustamante, L., & Mora, L. (2021). Facts about the U.S. Black population. Pew Research Center’s Social & Demographic Trends Project. https://www.pewresearch.org/social-trends/fact-sheet/facts-about-the-us-black-population/ [Google Scholar]
- Thornton, R. L., Glover, C. M., Cené, C. W., Glik, D. C., Henderson, J. A., & Williams, D. R. (2016). Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Affairs (Project Hope), 35(8), 1416–1423. doi: 10.1377/hlthaff.2015.1357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trani, J. F., Ballard, E., & Peña, J. B. (2016). Stigma of persons with disabilities in Afghanistan: Examining the pathways from stereotyping to mental distress. Social Science & Medicine (1982), 153, 258–265. doi: 10.1016/j.socscimed.2016.02.024 [DOI] [PubMed] [Google Scholar]
- Vélez-Agosto, N. M., Soto-Crespo, J. G., Vizcarrondo-Oppenheimer, M., Vega-Molina, S., & García Coll, C. (2017). Bronfenbrenner’s bioecological theory revision: Moving culture from the macro into the Micro. Perspectives on Psychological Science, 12(5), 900–910. doi: 10.1177/1745691617704397 [DOI] [PubMed] [Google Scholar]
- Zuelsdorff, M., Okonkwo, O. C., Norton, D., Barnes, L. L., Graham, K. L., Clark, L. R., Wyman, M. F., Benton, S. F., Gee, A., Lambrou, N., Johnson, S. C., & Gleason, C. E. (2020). Stressful life events and racial disparities in cognition among middle-aged and older adults. Journal of Alzheimer’s Disease, 73(2), 671–682. doi: 10.3233/JAD-190439 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.