Abstract
Maternal depression is associated with cognitive, emotional, and behavioral problems in offspring, but the substantial heterogeneity of depression precludes a full understanding of these associations. Variation in course of depression, characterized by severity or chronicity, may be related differentially to children’s development. The current meta-analytic review examined the relations of these characteristics of maternal depression to children’s developmental outcomes. Twenty-nine studies were identified and reviewed; the majority (93%) of studies reported a negative association between some aspect of maternal depression and children’s adjustment. Separate meta-analyses revealed significant effect sizes for severity (Fisher’s z = −.243) and chronicity (adjusted Fisher’s z = −.337) of maternal depression and children’s cognitive or behavioral functioning. Findings are synthesized across features of maternal depression; methodological limitations within the empirical literature are discussed, and recommendations for future research are suggested.
Keywords: maternal depression, severity, chronicity, child functioning
A reliable and robust risk factor for psychopathology in children and adolescents is the extent of psychopathology in their parents (e.g., Beardslee et al., 2011). In particular, depression in mothers has been linked with a myriad of problems in offspring throughout their development (Goodman et al., 2011). Depression, however, is quite heterogeneous regarding several characteristics such as its severity and chronicity; much less is known about which aspects of maternal depression are associated with which child outcomes and about the relative strength of these relations.
Heterogeneity of Depression
Depressive episodes can vary in intensity (i.e., severity) and duration and recurrence (i.e., chronicity), and often have been examined in tandem (e.g., Hammen et al., 2003, Netsi et al., 2018). This heterogeneity and variability might partially explain inconsistent findings regarding the relation between maternal depression and offspring functioning (e.g., Cents et al., 2013; Dawson et al., 2003). Both severity and chronicity of maternal depression have been associated significantly with cognitive deficits and with psychopathology in offspring (e.g., Brennan et al. 2000; Deave et al., 2008; Kim-Cohen, et al., 2005; Rouse & Goodman, 2014).
Functioning in Offspring of Depressed Mothers
Much existing research on the relation between maternal depression and offspring outcomes has focused on two aspects of child development – cognitive functioning and emotional or behavioral functioning. There are direct links between maternal psychopathology and fetal growth as early as mid-pregnancy (for a review, see Van den Bergh et al., 2005) and negative associations have been found between maternal depression and offspring outcomes throughout the lifespan (Goodman et al., 2011; Klein et al., 2005). Maternal depression has been linked with emotional problems (e.g., depression and anxiety), behavioral problems, and social and cognitive impairment in offspring (Gentile, 2017). The current review of the extant literature of maternal depression focused on two commonly studied domains of functioning – cognitive, and emotional or behavioral.
Maternal depression might be associated somewhat differently with specific facets of cognitive, emotional, and behavioral functioning. For example, O’Connor and colleagues (2017) showed that prior severity/chronicity of maternal depression predicted both internalizing and externalizing symptoms in children when controlling for current maternal depressive symptoms at each time point, but that chronicity, apart from severity, also predicted rate of change in youth externalizing symptoms over time. O’Connor et al. recommended that studies of maternal depression in relation to child functioning should explore severity and chronicity of parents’ depression and should consider them separately in relation to various child outcomes. Given the high comorbidity among youth cognitive, emotional, and behavioral outcomes (Riglin et al., 2014), the current review examined the links between maternal depression chronicity and severity and child functioning in two central domains – cognitive, and emotional and behavioral.
Methods
This review was conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (Moher et al., 2009). We conducted a systematic search and review of studies relevant to severity and chronicity of maternal depression. Some studies included information about more than one of these characteristics. We included empirical studies that (a) provided longitudinal, retrospective, or multiple cross-sectional assessments of maternal depression over time, and (b) measured some aspect of cognitive or emotional/behavioral functioning in offspring. We included studies that provided prospective (e.g., maternal depression measured continuously, or for ≥ 3 discrete measures during the child’s life) or retrospective data, whereby at least three prior episodes or three instances of elevated symptoms of maternal depression were assessed at one time point.
We identified articles published between 1983 and 2021 using Google Scholar, PsycINFO, and Pubmed, applying the initial search terms maternal OR mother, depression OR depressive, child* OR offspring, AND severity OR chronicity OR perinatal OR postpartum OR development OR behavior OR cognitive OR psychological OR emotional OR behavioral OR disorder OR programming, eliminating duplicates and inaccurate returns and expanding as necessary. All search returns were downloaded directly into spreadsheets. We evaluated potentially relevant articles using the following inclusion criteria: (a) assessment of maternal depression longitudinally, as described above, (b) measurement of an aspect of child functioning at the final time point, and (c) examination of the relation between a characteristic of maternal depression and child outcome(s). Additionally, we examined the reference lists of relevant articles for other empirical studies and performed a forward reference search of relevant empirical and review articles using Google Scholar. All spreadsheets of potentially relevant articles were coded by two independent raters with 92% reliability; eligibility was determined by consensus, and relevant data were extracted by the first author. This study was not preregistered and did not generate new human data requiring review by the Institutional Review Board.
Inclusion criteria required that studies present some measure of effect size (e.g., Pearson correlation coefficient, odds ratio, or two-group t-test). Ultimately, 29 studies published between 1995 and 2021 met inclusion criteria for this meta-analysis. Eleven studies examined the relation between severity of maternal depression and child outcomes, and 18 studies examined the link between chronicity and child outcomes, with five of these 29 studies reporting outcomes in relation to both severity and chronicity.
Data Analysis Plan
For studies that reported more than one child outcome (e.g., language development, IQ) within one outcome category (e.g., cognitive development), we calculated pooled effect sizes and standard error values. We adjusted effect directions as needed to appropriately reflect child outcomes across measures. For example, if chronicity of maternal depression and child problem behaviors were correlated positively r = .50, and chronicity and secure child attachment were correlated negatively r = −.50, the direction of the first correlation was reversed (e.g., r = .50 converted to r = −.50), such that both correlations represented the association between chronicity and problematic child outcomes.
As risk for transmission of psychopathology may have developmental components and studies of several developmental stages were included in the analyses, average age (in months) of offspring at the time of outcome assessment participants was tested as a moderator.
Quantitative analyses were performed with Comprehensive Meta-Analysis Version 3 (Borenstein et al., 2015), which yielded Fisher’s Z-values and confidence intervals of effect sizes to assess statistical significance. Models were set to “random effects,” as effect size distributions were heterogenous. Homogeneity of weighted effect sizes were examined with I2 and Q-tests. An estimate of between study variance (Tau squared) was used as a measure of heterogeneity. Because studies of several developmental stages were included in the analyses, we used average age (in months) of offspring at the time of outcome assessment as a moderator in meta-regression analyses.
A common concern when interpreting meta-analytic models is publication bias – studies that report significant effect sizes are more likely to be submitted to and published in journals than are those that report nonsignificant or even modest significant effects. We examined funnel plots for each meta-analytic model visually and by calculating Egger’s tests for detection of funnel plot asymmetry (Egger et al., 1997). Potential publication bias was addressed using trim and fill analysis.
Results
Publication Bias
Visual examination of funnel plots showed an apparently symmetrical distribution of effect sizes in severity analyses and was confirmed with results of Egger’s tests (p = .489). The funnel plot for chronicity effect sizes, however, appeared skewed and analysis could not rule out the potential for an effect of publication bias (p < .05). Therefore, the trim and fill procedure was used to generate an adjusted effect size for the chronicity analysis.
Severity of Maternal Depression and Children’s Outcomes
We conducted a meta-analysis of effect sizes of seven studies that tested differences between offspring of severely depressed mothers versus offspring of less severely depressed mothers (comparison groups varied from minimal depressive symptoms to moderate severity of depression), and four studies that tested the relations between maternal depression severity and child outcomes directly (e.g. correlations between continuous symptom measures of maternal depression and offspring problem behaviors). Analyses revealed a significant effect (Fishers’ z = −.247, 95% CI [−.389 −.106], Plot 1) for the relation between severity and child outcomes, indicating that more severe maternal depression was significantly associated with more negative cognitive and psychological outcomes in offspring.
Plot 1.
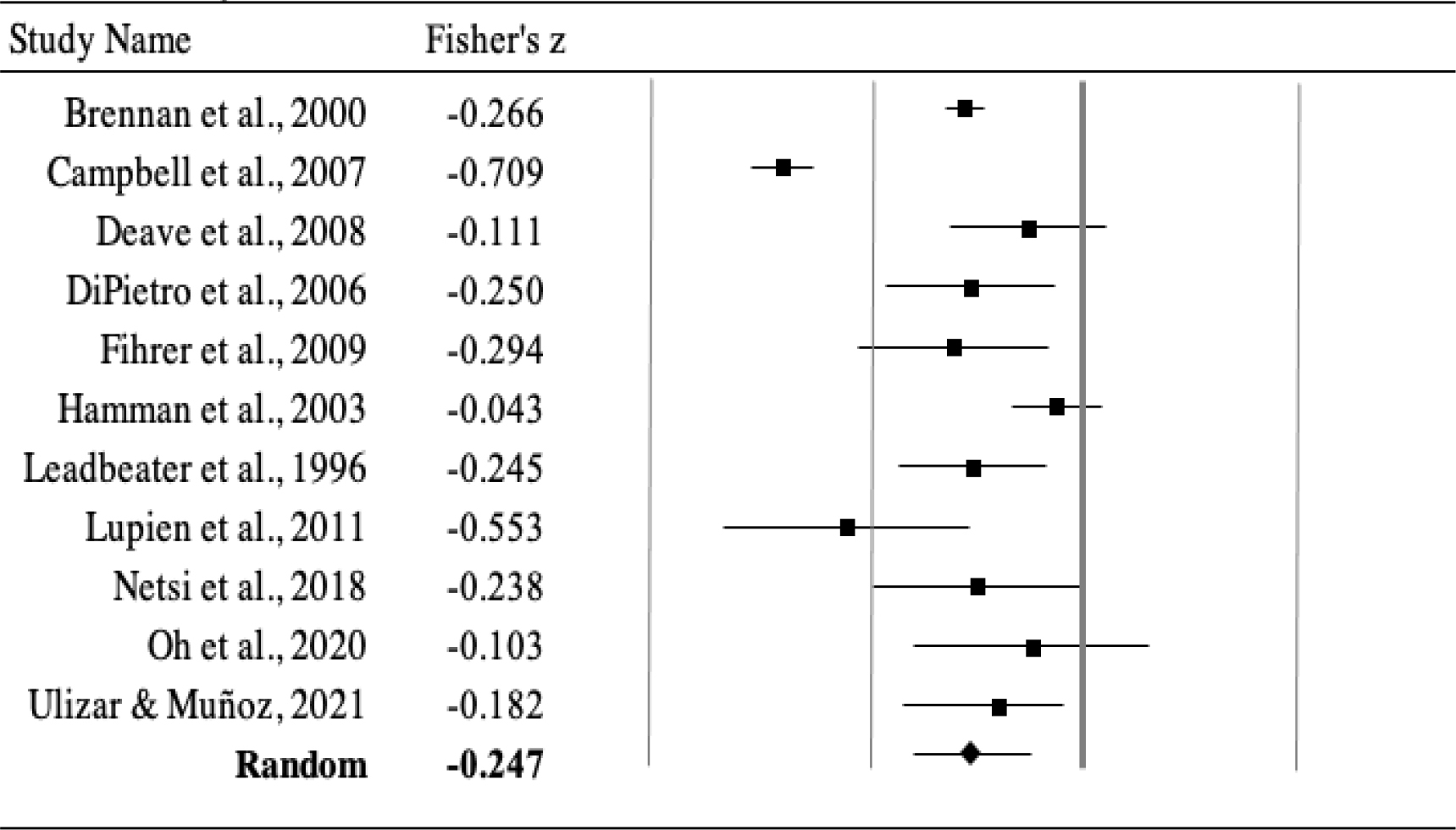
Severity
Notably, five studies (Brennan et al., 2000; Campbell et al., 2007; Fihrer et al., 2009; Leadbeater et al., 1996; Oh et al., 2020) used similar methodology, finding significant relations between maternal depression severity (assessed with questionnaires) and offspring emotional and behavioral symptoms as measured with the Child Behavior Checklist (CBCL; Achenbach et al., 2014). For example, in a sample of adolescent mothers and their young children, Leadbeater et al. (1996) found that more severe maternal depression when children were age one significantly predicted higher levels of children’s behavior problems on the CBCL at child age five.
We conducted a meta-regression analysis of the severity studies to test whether the relation between severity of parental depression and offspring outcomes varied as a function of child age. Here we used age as a continuous variable (i.e., mean age of sample in months). Results showed that age was not a significant moderator, Z = .37, p = .71.
Chronicity of Maternal Depression and Child Outcomes
The meta-analysis revealed a significant negative association (adjusted Fishers’ z = −.337, 95% CI [−.418, −.251]), indicating a statistically significant relation between chronicity of maternal depression and child functioning. Plot 2 presents results from this model. Most studies revealed that more chronic depression in mothers was associated with worse functioning in offspring. This pattern was found for infant outcomes, including fewer positive interactions and less frequent use of self-regulation strategies (Campbell et al., 1995; Deave et al., 2008; Granat et al., 2017).
Plot 2.
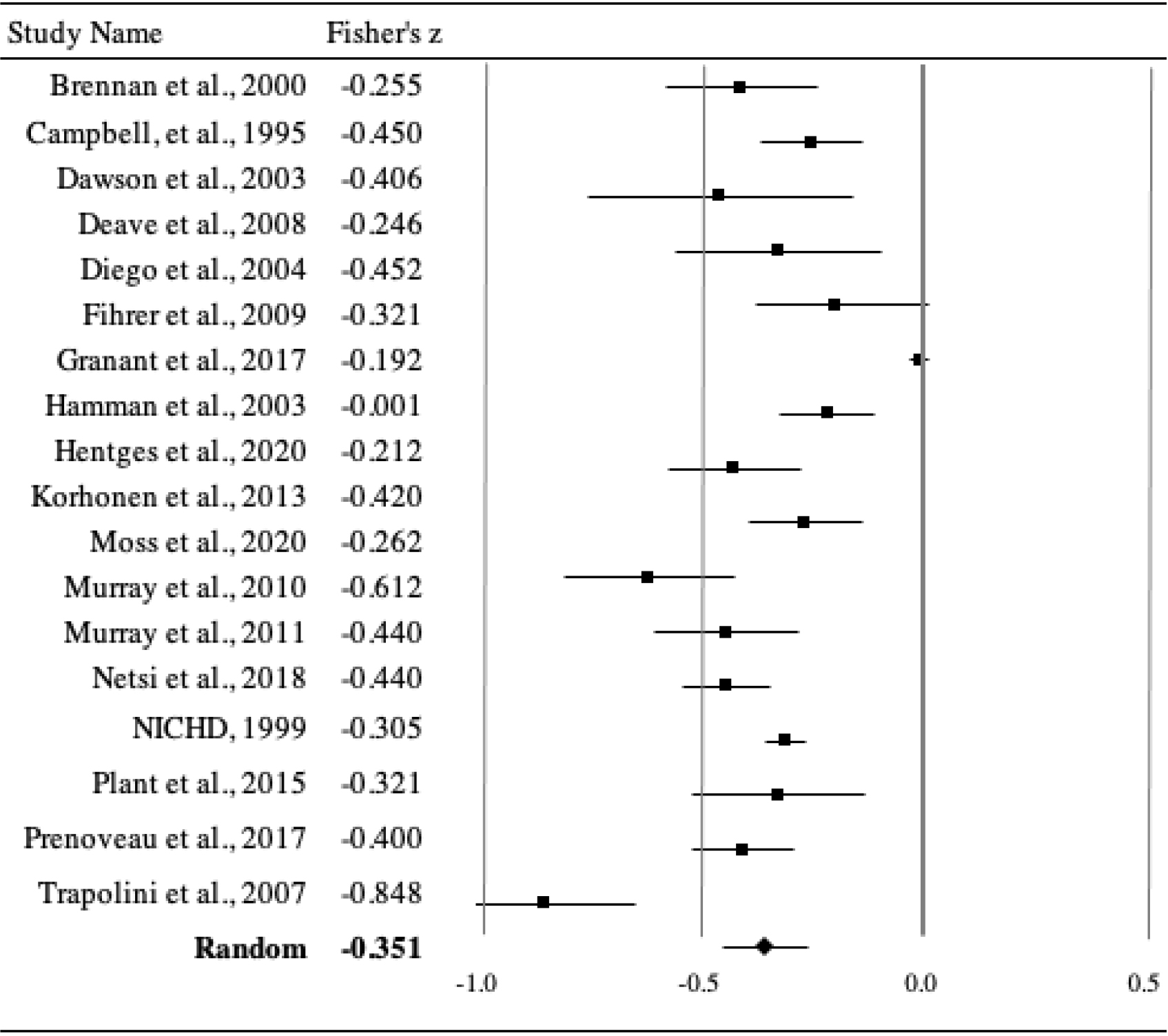
Chronicity
Several studies reported a significant positive relation between chronicity of maternal depression and offspring emotional and behavioral symptoms on the CBCL (Brennan et al., 2000; Dawson et al., 2003; NICHD Early Child Care Research Network, 1999; Prenoveau et al., 2017; Trapolini et al., 2007). For example, using latent Trait-State-Occasion modeling, Prenoveau et al. (2017) showed that persistent maternal depressive symptoms (EPDS administered at child ages of 3, 6, 10, 14, and 24 months) during the first two years postpartum, as compared to time-limited maternal depressive episodes occurring at a single time point, significantly predicted higher levels of problem behaviors and negative emotions in offspring at 24 months old.
Of note, chronicity has had several different definitions across studies. Whereas in some studies, chronicity was defined as having a high score on a self-report measure of depressive symptoms, sometimes at as few as two time points (e.g., Diego et al., 2004; Plant et al., 2015), other studies defined chronicity as measured across multiple time points (e.g., Brennan et al., 2000; Deave et al., 2008; NICHD, 1999; Prenoveau et al., 2017), and still others defined chronicity as a cumulative count of the number of months across a two-year period (e.g., Dawson et al., 2003; Murray et al., 2010). Despite these differences, results generally showed that more chronic maternal depression was associated with a greater likelihood of both lower cognitive and emotional/behavioral functioning as compared to less chronic depression in mothers.
In the meta-regression analysis testing age as a continuous variable (i.e., mean age of sample in months), we found that the relation between chronicity of parental depression and offspring outcomes was not significantly moderated by child age, Z = .13, p = .89.
Both Severity and Chronicity
Five studies examined the relations of both severity and chronicity to the same child outcomes, with three studies identifying significant relations between both severity and chronicity and child outcomes (Deave et al., 2008; Fihrer et al., 2009; Hammen et al.; 2003). Further, Netsi et al. (2018) defined chronicity as elevated EPDS scores at 2 and 8 months postpartum and examined severity dimensionally. They found that persistence of maternal depression, over and above the severity of mothers’ depressive symptoms, predicted increased odds of child behavior problems at age 3.5 years.
In a particularly compelling study, Brennan et al. (2000) reported that both the severity and chronicity of maternal depressive symptoms were related to more behavior problems and lower vocabulary scores in children. Moreover, the interaction of severity and chronicity of maternal depressive symptoms was significantly predicted higher levels of child behavior problems, but not vocabulary scores. Further analysis of the interaction revealed that children whose mothers had experienced both chronic and severe depressive symptoms had significantly more behavior problems than children of mothers who had experienced either severity or chronicity or neither. Brennan and colleagues concluded that the combination of severity and chronicity appears to be especially potent in relation to child behavior outcome.
Discussion
Several interesting findings emerged from this review regarding the connections between aspects of maternal depression and child functioning. We focused on two characteristics of maternal depression – severity and chronicity – in relation to salient domains of child development – cognitive and emotional or behavioral functioning. The meta-analyses quantified the strength of the associations between both severity and chronicity and child functioning, yielding significant effect sizes for both.
That more severe maternal depression was associated with more deleterious child functioning is not surprising. Indeed, mothers in the throes of a severe depression might become increasingly impaired. That is, as the intensity of symptoms escalates, mothers might find it increasingly difficult to interact positively with their children (e.g., problems attending, less enjoyment of shared activities, negative affect or negative cognitive style), which then might result in fewer or more maladaptive mother-child interactions and heightened distress and dysfunction in the child (e.g., Dunning et al., 2021).
More severe maternal depression might be categorically distinct from less severe depression, such that different mechanisms underlie risk to offspring of parents at the more severe end of the continuum. For example, more severe depression might reflect greater heritability, more environmental (e.g., family) stress, or both (e.g., Goodman & Gotlib, 1999). Indeed, severity of depression likely reflects an additive or interactive combination of genes and environmental vulnerability (Weissman, 2020).
Depressive symptoms in mothers were not associated with negative outcomes for children in every study, however. DiPietro et al. (2006) showed that low levels of maternal depression (as in low-risk, financially stable families with wanted pregnancies) were associated with more adaptive child outcomes as compared to offspring of mothers with no depression. This finding is consistent with the notion of inoculation or the “steeling effect” – that exposure to some mild levels of stress might prepare children optimally for dealing with subsequent adversity (e.g., Yan et al., 2014).
Chronicity of Maternal Depression and Offspring Functioning
Most studies showed that more chronic depression in mothers was associated with greater impairment in child functioning. With increased length of exposure to maternal depression, offspring might experience more instances of maternal modeling of negative affect, cognitions, and behaviors. In turn, this prolonged exposure to maladaptive thoughts and actions might confer susceptibility to similar depressive tendencies and other problem behaviors in offspring. Depressed parents display more negative parenting behaviors, which, in turn, are associated with more emotional and behavioral problems in offspring (Neece et al., 2012). Moreover, chronic life stress early in life is known to be associated with maladaptive outcomes such as over-activation of stress responsive-organs, more maladaptive lifestyles, and adverse cardiovascular events. Goodman and Halpern (2019) suggested that maternal depression may be one important vessel of such early life stress.
Child Functioning
Both severity and chronicity of maternal depression were significantly associated with poorer offspring cognitive functioning, which often is associated with more social and academic problems in general (e.g., Samuels et al., 2016). Deficits in child cognitive functioning may be one pathway through which maternal depression is linked to worse psychosocial functioning in children. Cognitive ability also may be an important predictor of responses to psychological treatments of depression, as interventions that require a higher level of cognitive skills might be less effective with individuals with lower cognitive functioning (Mohlman, & Gorman, 2005).
In one study that examined the interaction between severity and chronicity of maternal depression, Brennan et al. (2000) found that the interaction was significant for child behavior but not cognitive functioning. Brennan and colleagues suggested that this discrepancy might be due to two factors. First, generally there is a lower association between maternal depression and cognitive outcomes as compared to behavioral outcomes. Second, the outcomes differed in how they were assessed. Cognitive outcomes were measured with standardized tools, whereas behavioral problems were assessed by maternal report only, and therefore were more subjective and possibly affected by a negative reporting bias. Ultimately, the distinct risk profiles for different child outcomes should be examined in future studies of chronicity and severity of parents’ depression.
Methodological Concerns
Three methodological factors may have contributed to variability across studies: (a) heterogeneity of measurement, (b) failure to examine additive and interactive effects of severity and chronicity, (c) absence of control for symptoms of depression outside of targeted periods, and (d) lack of specificity in measures of child outcomes.
Studies in this review were quite heterogeneous in their conceptualizations and operationalizations of severity and chronicity of depression. Some studies used continuous measures of depressive symptoms (e.g., BDI-II), whereas some studies used categories (e.g., “mild” vs. “severe”) or different cut-off scores on dimensional measures; still other studies used novel descriptors, such as “course” or “pattern” (e.g., high-chronic, low-episodic) that combined characteristics. Ideally, severity would be assessed using a measure designed specifically to determine level of symptoms, such as the Hamilton Depression Rating Scale (Hamilton, 1960). Some investigators, however, have used continuous measures of the number and frequency of symptoms experienced (e.g., EPDS) or a rating of symptom severity on an 8-point scale (e.g., Prenoveau et al., 2017). Because of the heterogeneity of measures of depression and operationalizations of severity and chronicity in the literature, we included a broad representation of these constructs (i.e., severity, chronicity) in the current review.
A related concern is that definitions and measurement of severity and chronicity sometimes have overlapped, particularly when using dimensional, self-report measures at multiple points across time, thereby making it difficult to determine the unique contribution of each. Although few studies have examined how severity and chronicity separately and together predict child functioning, those that have done so (i.e., Brennan et al., 2000; Netsi et al., 2018; O’Connor et al., 2017) have yielded important results that provide a model for future investigations. Understanding the impact of both severity and chronicity, separately, additively, or multiplicatively, could help identify mechanisms of the intergenerational transmission of psychopathology and possible targets for intervention.
In addition, age of onset and recurrence of maternal depression should be examined. To study the prospective relation between maternal depression and child functioning, future studies should use longitudinal designs and comprehensive measures of parental depression to gather continuous data over time. Measurement of concurrent associations may aid in understanding longitudinal questions, as without collecting child outcome data simultaneously with maternal risk data, predictive analyses may be limited. For example, when depression is assessed prenatally and offspring outcomes are assessed in toddlerhood, the relative contribution of maternal depression during the post-natal versus infancy periods is ambiguous. Because earlier onset of depressive episodes is associated with a more recurrent and sometimes more severe course of depression (van Lang, Ferdinand, & Verhulst, 2007), mothers who experience their first episode as adolescents might be more vulnerable to a more extended course of depression, due to greater genetic or environmental risk. Thus, women with an early onset of depression might confer more risk to their children than mothers who experience their first episode later.
Finally, the definitions and measures of child outcomes also were quite heterogeneous, and many studies utilized general rather than specific measures of child functioning. Therefore, broad categories of cognitive and emotional/behavioral outcomes were the focus of the current review. As such, generalizing findings from disparate measures of children’s functioning needs to be done with caution. Thus, a uniform battery of psychometrically adequate measures of both mother and child characteristics should be used across studies.
Strengths, Limitations, and Future Directions
Strengths.
The primary strength of this meta-analytic review was that it addressed a notable gap in the literature regarding different aspects of maternal depression in relation to offspring functioning. Recent work has highlighted the importance of “multi-domain and longitudinal [studies] with respect to both mothers’ and offsprings’ function,” (p. 7; Gotlib et al., 2020) and a “greater consideration of the variability within depression” (p. 20; Goodman, 2020). The current review consolidated and synthesized the heterogeneous extant literature in response to these suggestions and provided information about the strength of the associations reported.
Other strengths of this review were the inclusion of heterogeneous measures of various descriptors of maternal depression. Recent work has called for examination of comprehensive, longitudinal data to address both predictor and outcome variables associated with different developmental periods (Goodman et al., 2011; Prenoveau et al., 2017) and to further understand risks associated with severity and chronicity of maternal depression (Allen et al., 2019). To provide a more complete understanding of the various facets of maternal depression, future studies should continue to incorporate prospective and retrospective data and analyses (Granat et al., 2017).
A final strength of this review was its breadth. Studies of maternal depression have emphasized the importance of replicating findings with diverse samples. Moreover, maternal depression should be assessed repeatedly, beginning during critical prenatal months and throughout the children’s development. In addition, measures of children’s outcomes occurring across multiple developmental stages from infancy to young adulthood are needed (Priel et al., 2019).
Limitations.
Limitations of the current review provide directions for future research. First, this review focused on depression only, rather than other common psychopathologies (e.g., anxiety; substance use) or risk factors (e.g., stress, trauma). Our emphasis on depression, however, was justified because it is a particularly debilitating and common disorder (Meaney, 2018) associated with maladaptation in offspring. Second, as noted previously, many studies relied on maternal reports of both their own depression and children’s behaviors, which may have overestimated the correlations due to shared method variance. Whereas some studies did include paternal or teacher reports (e.g., Campbell et al., 2007; Fihrer et al., 2009), most did not.
Another limitation of the current review was the variability of samples and depression assessment methods across studies. For example, whereas many studies utilized community samples and assessed depression using symptom level measures (e.g., Hentges et al., 2020), other studies included clinical samples and conducted diagnostic interviews (e.g. Klein et al., 2005). It is not clear to what extent the different assessment methods and measures contributed to discrepancies in the findings across studies.
Finally, another important limitation of this review and the more general literature on maternal depression is an absence of attention to potentially important contextual factors such as poverty or family functioning. Unfortunately, data examining these factors were not consistently available across the papers reviewed. Although some papers did explore context (NICHD Early Child Care Research Network, 1999), this was not done systematically across studies, thereby limiting our ability to quantify and interpret findings concisely. Studies of the relation between parental depression and children’s functioning should include conceptually driven and rigorously defined measures of a range of potential contextual influences.
Future Directions.
In summary, longitudinal studies of offspring of depressed mothers, beginning at birth or even before (Diego et al., 2009, Goodman, 2020), are necessary for a better understanding of the extent and nature of the potential effects of maternal depression on children’s development. Future research should explore moderators to clarify possible inconsistent associations between the different aspects of maternal depression and various child outcomes (Goodman et al., 2020). Potential moderators include the family environment and both stable (e.g., sex) and dynamic (e.g., age, SES) factors (Bagner et al., 2011; Goodman & Gotlib, 1999; Stein et al., 2014). For example, associations between maternal psychopathology and child outcomes have been found to vary by offspring sex (Sutherland & Brunwasser, 2018), although few articles (e.g., Wen et al., 2017) have provided the relevant data. Recent work has highlighted the importance of considering context such as family socio-economic status when examining the cross-generational transmission of psychopathology (Pelham et al., 2020).
Another important direction for future research is to identify mediators of the relation between maternal depression and children’s outcomes. Prior research has identified several likely biomarkers of maternal depression and has examined different biological pathways, including stress hormones and neurotransmitters (Gentile, 2017; Priel et al., 2019; Serati et al., 2016). as well as environmental pathways such as family income, maternal social behavior, parental monitoring and support, positive parenting, and level of parental conflict (Gotlib et al., 2020; Granat et al., 2017). In addition, the current review focused on mothers, but the mental health of other caretakers, such as fathers, also should be explored in relation to child outcomes. For example, having a highly supportive other caretaker may buffer children from some of the negative effects of the mother’s depression (Vakrat et al., 2018).
Maternal depression during the perinatal period may not have a direct link to maladaptive child outcomes, but rather may be a distal process that initiates a developmental cascade eventually resulting in poor outcomes in the children (Waters et al., 2014). This cascade might include dysfunctional parenting or abuse by parents (Plant et al., 2015) or dyadic factors (e.g., attachment, Campbell et al., 2004). Researchers also have called for the use of cross-lagged or bidirectional models to further elucidate the potential temporal, reciprocal, and transactional connections between mothers and offspring (Allen et al., 2019; Sutherland et al., 2019).
In summary, studying characteristics of maternal depression is relevant to understanding the relation between maternal depression and offspring adjustment, and ultimately may inform targeted preventive interventions (McDaid et al., 2019). For example, if at-risk offspring of depressed mothers can be identified early for intervention by evaluating the chronicity and severity of the mother’s depression, perhaps developmental cascades may be redirected and a pathway of risk curtailed or eliminated (Meaney, 2018).
Figure 1.
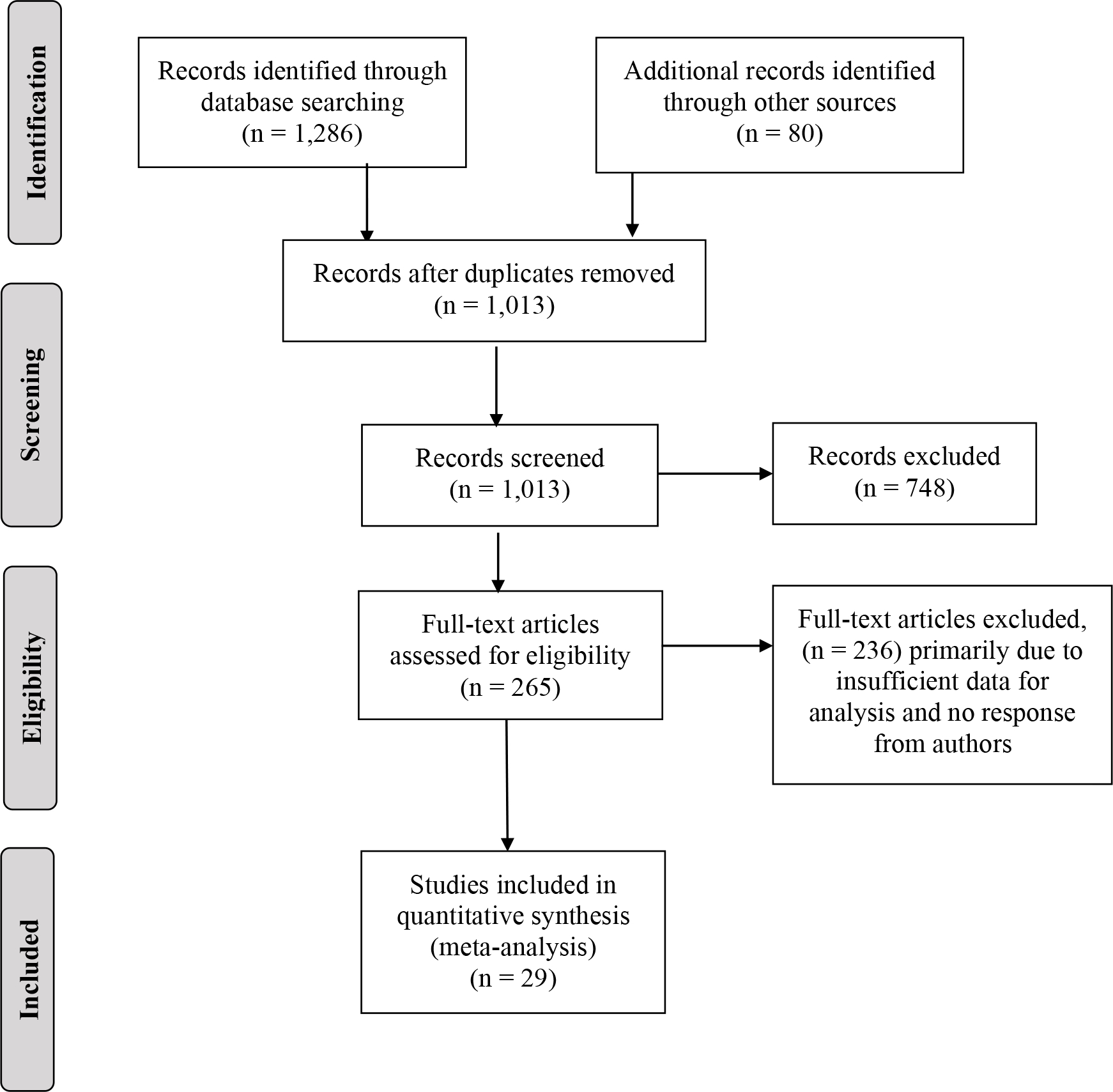
Prisma Flow Diagram.
Table 1.
Characteristics of Articles included in the Review
| Study Name | N dyads | Maternal Depression Measure | Fisher’s z (SE) or Y/N sig. association | Offspring Measures |
|---|---|---|---|---|
|
| ||||
| Severity of Maternal Depression | ||||
| Cognitive functioning | ||||
| DiPietro et al., 2006 | 94 | POMS | −.250 (.105) | Bayley Scale - PDI, MDI |
| Brennan et al., 2000 | 4,953 | BDI | −.266 (.014) | PPVT-R |
| Urizar & Munoz, 2021 | 96 | CES-D | −.138(.121) | Mullen Early Learning |
| Campbell et al., 2007 | 1,261 | CES-D | −.709 (.039) | Woodcock Johnson-III |
| Deave et al., 2008 | 10,125 | EPDS | −.111 (.096) | DDST |
| Emotional/behavioral functioning | ||||
| Leadbeater et al., 1996 | 120 | BDI | −.245 (.092) | CBCL (Preschool) |
| Brennan et al., 2000 | 4,953 | BDI | −.266 (.014) | CBCL (Preschool) |
| Fihrer et al., 2009 | 75 | CES-D, CIDI Retrospective | −.294 (.118) | CBCL (School age) |
| Urizar & Munoz, 2021 | 96 | CES-D | −.368(.117) | Vineland Soc-Emo |
| Oh et al., 2020 | 688 | Kessler Depression | −.119(.038) | CBCL (School age) |
| Campbell et al., 2007 | 1,261 | CES-D | −.709 (.039) | CBCL (School age) |
| Hamman et al., 2003 | 816 | SCID, LIFE | −.043 (.055) | KSADS (MDE) |
| Netsi et al., 2018 | 7,917 | EPDS | −.238 (.129) | Rutter Total Problems |
| Klein et al., 2005 | 775 | SCID, LIFE | No | KSADS (MDE) |
| Hamman et al., 2003 | 816 | SCID, LIFE | −.043 (.055) | KSADS (nondepressive disorders) |
|
| ||||
| Chronicity of Maternal Depression | ||||
| Cognitive functioning | ||||
| Deave et al., 2008 | 10,125 | EPDS | −.246 (.059) | DDST |
| NICHD, 1999 | 1,215 | CES-D | −.164 (.025) | Reynell |
| Brennan et al., 2000 | 4,953 | DSSI | −.050 (.014) | PPVT-R |
| Murray et al., 2010 | 89 | EPDS, SADS | −.612 (.098) | General Certificate of Secondary Education |
| Emotional/behavioral functioning | ||||
| Campbell et al., 1995 | 140 | SADS | −.450 (.081) | coded interaction |
| Granat et al., 2017 | 215 | BDI | −.192 (.105) | coded infant self-regulation |
| Prenoveau et al., 2017 | 296 | EPDS | −.400 (.058) | CBCL (Preschool) |
| NICHD, 1999 | 1,215 | CES-D | −.305 (.024) | CBCL (Preschool) |
| Trapolini et al., 2007 | 92 | CES-D, CIDI Retrospective | −.907 (.106) | CBCL (Preschool) |
| Dawson et al., 2003 | 124 | SCID, LIFE | −.529 (.084) | CBCL (Preschool) |
| Brennan et al., 2000 | 4,953 | BDI | −.255 (.014) | CBCL (Preschool & School) |
| Korhonen et al., 2013 | 192 | EPDS | −.420 (.076) | CBCL (Preschool & School) |
| Netsi et al., 2018 | 7,917 | EPDS | −.440 (.050) | Rutter Total Problems |
| Moss et al., 2020 | 229 | CES-D | −.262(−.389) | Strengths and Difficulties |
| Murray et al., 2011 | 100 | SADS | −.440(−.083) | KSADS (MDE) |
| Hentges et al., 2020 | 338 | EPDS, CES-D | −.212(−.318) | BASC |
| Plant et al., 2015 | 103 | CIS, SADS Retrospective | −.321 (.100) | SCID (MDE) |
| Hamman et al., 2003 | 816 | SCID, LIFE | −.001 (.003) | KSADS (nondep. disorders) |
| Hamman et al., 2003 | 816 | SCID, LIFE | −.000 (.003) | KSADS (MDE) |
| Pawlby et al., 2011 | 120 | SADS, CIS Retrospective | No | CAPA conduct module |
Note: BDI = Beck Depression Inventory; BITSEA = Brief Infant-Toddler Social and Emotional Assessment; BSI = Brief Symptom Inventory; CBCL = Child Behavior Checklist; CES-D = Center for Epidemiologic Studies - Depression; CIDI = Composite International Diagnostic Interview; CIS = Clinical Interview Schedule; DAWBA = Development and Well-Being Assessment; DDST = Denver Developmental Screening Test; DSM = Diagnostic and Statistical Manual of Mental Disorders; DSSI = Delusions-Symptoms-States Inventory; EPDS = Edinburgh Postnatal Depression Scale; KSADS = Schedule for Affective Disorders and Schizophrenia for School-Age Children; LIFE = Longitudinal Interval Follow up Evaluation; MDI = Mental Development Index; PDI = Psychomotor Development Index; POMS = Profile of Mood States; SADS = Schedule for Affective Disorders and Schizophrenia; SCID = Structured Clinical Interview for DSM Disorders; WISC = Wechsler Intellectual Scale for Children.
Effect present for one gender only.
Acknowledgments
This work was supported in part by a NIMH grant (R61MH115125) and training grant (T32MH018921)
References
- Achenbach TM, Rescorla LA, & Maruish ME (2014). The Achenbach system of empirically based assessment (ASEBA) for ages 1.5 to 18 years. The use of psychological testing for treatment planning and outcomes assessment, 2, 179–213. Routledge. [Google Scholar]
- Allen TA, Oshri A, Rogosch FA, Toth SL, & Cicchetti D (2019). Offspring personality mediates the association between maternal depression and childhood psychopathology. Journal of Abnormal Child Psychology, 47(2), 345–357. doi: 10.1007/s10802-018-0453-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR, & Jaccard J (2013). Disentangling the temporal relationship between parental depressive symptoms and early child behavior problems: A transactional framework. Journal of Clinical Child & Adolescent Psychology, 42(1), 78–90. doi: 10.1080/15374416.2012.715368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beardslee WR, Gladstone TR, & O’Connor EE (2011). Transmission and prevention of mood disorders among children of affectively ill parents: A review. Journal of the American Academy of Child & Adolescent Psychiatry, 50(11), 1098–1109. doi: 10.1016/j.jaac.2011.07.020 [DOI] [PubMed] [Google Scholar]
- Brennan PA, Hammen C, Andersen MJ, Bor W, Najman JM, & Williams GM (2000). Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology, 36(6), 759. doi: 10.1037//0012-1649.36.6.759 [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JP, & Rothstein H (2015). Regression in meta-analysis. Comprehensive meta-analysis manual. Biostat, Englwood, NJ. [Google Scholar]
- Campbell SB, Brownell CA, Hungerford A, Spieker SJ, Mohan R, & Blessing JS (2004). The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Development and Psychopathology, 16(2), 231–252. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Cohn JF, & Meyers T (1995). Depression in first-time mothers: mother-infant interaction. Developmental Psychology, 31(3), 349. doi: 10.1037/0012-1649.31.3 [DOI] [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, & Kirchner T (2007). Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology, 43(5), 1202–1215. doi: 10.1037/0012-1649.43.5.1202 [DOI] [PubMed] [Google Scholar]
- Cox JL, Chapman G, Murray D, & Jones P (1996). Validation of the Edinburgh Postnatal Depression Scale in non-postnatal women. Journal of Affective Disorders, 39(3), 185–189. doi: 10.1016/0165-0327(96)00008-0 [DOI] [PubMed] [Google Scholar]
- Dawson G, Ashman SB, Panagiotides H, Hessl D, Self J, Yamada E, & Embry L (2003). Preschool outcomes of children of depressed mothers: Role of maternal behavior, contextual risk, and children’s brain activity. Child Development, 74(4), 1158–1175. doi: 10.1111/1467-8624.00599 [DOI] [PubMed] [Google Scholar]
- Deave T, Heron J, Evans J, & Emond A (2008). The impact of maternal depression in pregnancy on early child development. British Journal of Obstetrics & Gynaecology, 115(8), 1043–1051. doi: 10.1111/j.1471-0528.2008.01752.x [DOI] [PubMed] [Google Scholar]
- Diego MA, Field T, Hernandez-Reif M, Cullen C, Schanberg S, & Kuhn C (2004). Prepartum, postpartum, and chronic depression effects on newborns. Psychiatry: Interpersonal and Biological Processes, 67(1), 63–80. doi: 10.1521/psyc.67.1.63.31251 [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Novak MF, Costigan KA, Atella LD, & Reusing SP (2006). Maternal psychological distress during pregnancy in relation to child development at age two. Child Development, 77(3), 573–587. doi: 10.1111/j.1467-8624.2006.00891.x [DOI] [PubMed] [Google Scholar]
- Dunning EE, McArthur BA, Abramson LY, & Alloy LB (2021). Linking maternal depression to adolescent internalizing symptoms: Transmission of cognitive vulnerabilities. Journal of Youth and Adolescence, 50(2), 324–335. doi: 10.1007/s10964-020-01342-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. Bmj, 315(7109), 629–634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fihrer I, McMahon CA, & Taylor AJ (2009). The impact of postnatal and concurrent maternal depression on child behaviour during the early school years. Journal of Affective Disorders, 119(1–3), 116–123. doi: 10.1016/j.jad.2009.03.001 [DOI] [PubMed] [Google Scholar]
- Gentile S (2017). Untreated depression during pregnancy: Short-and long-term effects in offspring. A systematic review. Neuroscience, 342, 154–166. doi: 10.1016/j.neuroscience.2015.09.001 [DOI] [PubMed] [Google Scholar]
- Goodman SH (2020). Intergenerational transmission of depression. Annual Review of Clinical Psychology, 16, 213–238. doi: 10.1146/annurev-clinpsy-071519-113915 [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Gotlib IH (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106(3), 458–490. doi: 10.1037/0033-295X.106.3.458 [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Halperin MS (2019). Perinatal depression as an early stress. In The Oxford Handbook of Stress and Mental Health (pp. 287–312). Oxford University Press. [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. doi: 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Goodman SH, Simon HFM, Shamblaw AL, & Kim CY (2020). Parenting as a mediator of associations between depression in mothers and children’s functioning: A systematic review and meta-analysis. Clinical Child and Family Psychology Review, 23, 427–460. 10.1007/s10567-020-00322-4 [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Goodman SH, & Humphreys KL (2020). Studying the intergenerational transmission of risk for depression: Current status and future directions. Current directions in psychological science, 29(2), 174–179. doi: 10.1177/0963721420901590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granat A, Gadassi R, Gilboa-Schechtman E, & Feldman R (2017). Maternal depression and anxiety, social synchrony, and infant regulation of negative and positive emotions. Emotion, 17(1), 11–27. doi: 10.1037/emo0000204 [DOI] [PubMed] [Google Scholar]
- Hamilton M (1960). A Rating Scale for Depression. Journal of Neurology, Neurosurgery and Psychiatry, 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, & Brennan PA (2003). Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry, 60(3), 253–258. doi: 10.1001/archpsyc.60.3.253 [DOI] [PubMed] [Google Scholar]
- Hentges RF, Graham SA, Fearon P, Tough S, & Madigan S (2020). The chronicity and timing of prenatal and antenatal maternal depression and anxiety on child outcomes at age 5. Depression and Anxiety, 37(6), 576–586. doi: 10.1002/da.23039 [DOI] [PubMed] [Google Scholar]
- Klein DN, Lewinsohn PM, Rohde P, Seeley JR, & Olino TM (2005). Psychopathology in the adolescent and young adult offspring of a community sample of mothers and fathers with major depression. Psychological Medicine, 35(3), 353–365. [DOI] [PubMed] [Google Scholar]
- Korhonen M, Luoma I, Salmelin R, & Tamminen T (2013). Maternal depressive symptoms: associations with adolescents’ internalizing and externalizing problems and social competence. Nordic Journal of Psychiatry, 68(5), 323–332. doi: 10.3109/08039488.2013.838804 [DOI] [PubMed] [Google Scholar]
- Leadbeater BJ, Bishop SJ, & Raver CC (1996). Quality of mother–toddler interactions, maternal depressive symptoms, and behavior problems in preschoolers of adolescent mothers. Developmental Psychology, 32(2), 280–288. doi: 10.1037/0012-1649.32.2.280 [DOI] [Google Scholar]
- McDaid D, Park AL, & Wahlbeck K (2019). The economic case for the prevention of mental illness. Annual Review of Public Health, 40, 373–389. doi: 10.1146/annurev-publhealth-040617-013629 [DOI] [PubMed] [Google Scholar]
- Meaney MJ (2018). Perinatal maternal depressive symptoms as an issue for population health. American Journal of Psychiatry, 175(11), 1084–1093. doi: 10.1176/appi.ajp.2018.17091031 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Prisma Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International Journal of Surgery, 89(9), 873–880. doi: 10.1016/j.ijsu.2010.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohlman J, & Gorman JM (2005). The role of executive functioning in CBT: A pilot study with anxious older adults. Behaviour Research and Therapy, 43(4), 447–465. doi: 10.1016/j.brat.2004.03.007 [DOI] [PubMed] [Google Scholar]
- Moss KM, Dobson AJ, & Mishra GD (2020). Testing the role of the timing and chronicity of maternal depressive symptoms in the associations with child behaviour and development. Paediatric and Perinatal Epidemiology, 34(6), 678–686. doi: 10.1111/ppe.12681 [DOI] [PubMed] [Google Scholar]
- Murray L, Arteche A, Fearon P, Halligan S, Croudace T, & Cooper P (2010). The effects of maternal postnatal depression and child sex on academic performance at age 16 years. Journal of Child Psychology and Psychiatry, 51(10), 1150–1159. doi: 10.1111/j.1469-7610.2010.02259.x [DOI] [PubMed] [Google Scholar]
- Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, & Cooper P (2011). Maternal postnatal depression and the development of depression in offspring up to 16 years of age. Journal of the American Academy of Child & Adolescent Psychiatry, 50(5), 460–470. doi: 10.1016/j.jaac.2011.02.001 [DOI] [PubMed] [Google Scholar]
- Neece CL, Green SA, & Baker BL (2012). Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities, 117(1), 48–66. doi: 10.1352/1944-7558-117.1.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, & Stein A (2018). Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry, 75(3), 247–253. doi: 10.1001/jamapsychiatry.2017.4363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. (1999). Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology, 35(5), 1297–1310. [DOI] [PubMed] [Google Scholar]
- O’Connor EE, Langer DA, & Tompson M C (2017). Maternal depression and youth internalizing symptomatology: Severity and chronicity of past depression and current maternal depression symptoms. Journal of Abnormal Child Psychology, 45, 557–568. doi: 10.1007/s10802-016-0185-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh Y, Joung YS, Baek JH, & Yoo N (2020). Maternal depression trajectories and child executive function over 9 years. Journal of Affective Disorders, 276, 646–652. doi: 10.1016/j.jad.2020.07.065 [DOI] [PubMed] [Google Scholar]
- Pawlby S, Hay D, Sharp, Waters C, & Pariante C (2011). Antenatal depression and offspring psychopathology: the influence of childhood maltreatment. BJP, 199(2), 106–112. doi: 10.1192/bjp.bp.110.087734 [DOI] [PubMed] [Google Scholar]
- Pelham III WE, West SG, Lemery-Chalfant K, Goodman SH, Wilson MN, Dishion TJ, & Shaw DS (2020). Depression in mothers and the externalizing and internalizing behavior of children: An attempt to go beyond association. Journal of Abnormal Psychology. doi: 10.1037/abn0000640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plant DT, Pariante CM, Sharp D, & Pawlby S (2015). Maternal depression during pregnancy and offspring depression in adulthood: role of child maltreatment. British Journal of Psychiatry, 207(3), 213–220. doi: 10.1192/bjp.bp.114.156620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prenoveau JM, Craske MG, West V, Giannakakis A, Zioga M, Lehtonen A, ... & Murray L (2017). Maternal postnatal depression and anxiety and their association with child emotional negativity and behavior problems at two years. Developmental Psychology, 53(1), 50–62. doi: 10.1037/dev0000221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priel A, Djalovski A, Zagoory-Sharon O, & Feldman R (2019). Maternal depression impacts child psychopathology across the first decade of life: Oxytocin and synchrony as markers of resilience. Journal of Child Psychology and Psychiatry, 60(1), 30–42. doi: 10.1111/jcpp.12880 [DOI] [PubMed] [Google Scholar]
- Riglin L, Petrides KV, Frederickson N, & Rice F (2014). The relationship between emotional problems and subsequent school attainment: A meta-analysis. Journal of Adolescence, 37(4), 335–346. doi: 10.1016/j.adolescence.2014.02.010 [DOI] [PubMed] [Google Scholar]
- Samuels WE, Tournaki N, Blackman S, & Zilinski C (2016). Executive functioning predicts academic achievement in middle school: A four-year longitudinal study. The Journal of Educational Research, 109(5), 478–490. doi: 10.1080/00220671.2014.979913 [DOI] [Google Scholar]
- Serati M, Redaelli M, Buoli M, & Altamura AC (2016). Perinatal major depression biomarkers: A systematic review. Journal of Affective Disorders, 193, 391–404. doi: 10.1016/j.jad.2016.01.027 [DOI] [PubMed] [Google Scholar]
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, ... & Pariante CM (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet, 384(9956), 1800–1819. doi: 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- Sutherland S, & Brunwasser SM (2018). Sex differences in vulnerability to prenatal stress: A review of the recent literature. Current Psychiatry Reports, 20(11), 102–114. doi: 10.1007/s11920-018-0961-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland S, Brunwasser SM, Nestor BA, McCauley E, Diamond G, Schloredt K, & Garber J (2019). Prospective relations between parents’ depressive symptoms and children’s attributional style. Journal of Clinical Child & Adolescent Psychology, 1–9. doi: 10.1080/15374416.2019.1567346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trapolini T, McMahon CA, & Ungerer JA (2007). The effect of maternal depression and marital adjustment on young children’s internalizing and externalizing behaviour problems. Child: Care, Health and Development, 33(6), 794–803. doi: 10.1111/j.1365-2214.2007.00739.x [DOI] [PubMed] [Google Scholar]
- Urizar GG, & Muñoz RF (2021). Role of maternal depression on child development: A prospective analysis from pregnancy to early childhood. Child Psychiatry & Human Development, 1–13. doi: 10.1007/s10578-021-01138-1 * [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vakrat A, Apter-Levy Y, & Feldman R (2018). Sensitive fathering buffers the effects of chronic maternal depression on child psychopathology. Child Psychiatry & Human Development, 49(5), 779–785. doi: 10.1007/s10578-018-0795-7 [DOI] [PubMed] [Google Scholar]
- Van den Bergh BR, Mulder EJ, Mennes M, & Glover V (2005). Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: Links and possible mechanisms, a review. Neuroscience & Biobehavioral Reviews, 29(2), 237–258. doi: 10.1016/j.neubiorev.2004.10.007 [DOI] [PubMed] [Google Scholar]
- van Lang ND, Ferdinand RF, & Verhulst FC (2007). Predictors of future depression in early and late adolescence. Journal of Affective Disorders, 97(1–3), 137–144. [DOI] [PubMed] [Google Scholar]
- Waters CS, Hay DF, Simmonds JR, & van Goozen SH (2014). Antenatal depression and children’s developmental outcomes: Potential mechanisms and treatment options. European Child & Adolescent Psychiatry, 23(10), 957–971. doi: 10.1007/s00787-014-0582-3 [DOI] [PubMed] [Google Scholar]
- Weissman MM (2020). Is Depression Nature or Nurture? Yes. American Journal of Psychiatry, 177(5), 376–37. doi: 10.1176/appi.ajp.2020.20020186 [DOI] [PubMed] [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, ... & Cerda G (2006). Remissions in maternal depression and child psychopathology: A STAR* D-child report. JAMA, 295(12), 1389–1398. doi: 10.1001/jama.295.12.1389 [DOI] [PubMed] [Google Scholar]
- Wen DJ, Soe NN, Sim LW, Sanmugam S, Kwek K, Chong YS, ... & Qiu A (2017). Infant frontal EEG asymmetry in relation with postnatal maternal depression and parenting behavior. Translational psychiatry, 7(3), e1057–e1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan Y, Fang F, Shijian C, Ye Z, Ke L, Kaiqing T, & He W (2014). The relationship between resilience, negative life events and depressive symptoms: steeling effect and sensitizing effect. Journal of Psychological Science, (6), 37–52. [Google Scholar]


