Abstract
Particulate matter with aerodynamic diameter no larger than 2.5 μm (PM2.5) has been linked to cardiovascular diseases (CVDs) but evidence for vulnerability by sex remains unclear. We performed systematic review and meta-analysis to synthesize the state of scientific evidence on whether cardiovascular risks from PM2.5 differ for men compared to women. The databases Pubmed, Scopus, Embase, and GreenFILE were searched for studies published Jan. 1995 to Feb. 2020. Observational studies conducting subgroup analysis by sex for impacts of short-term or long-term exposure to PM2.5 on target CVDs were included. Data were independently extracted in duplicate and pooled with random-effects meta-regression. Risk ratios (RRs) for long-term exposure and percent changes in outcomes for short-term exposure were calculated per 10 μg/m3 PM2.5 increase. Quality of evidence of risk differences by sex was rated following Grading of Recommendations Assessment, Development and Evaluation (GRADE). A total of 12,502 articles were screened, with 61 meeting inclusion criteria. An additional 32 studies were added from citation chaining. RRs of all CVD mortality for long-term PM2.5 for men and women were the same (1.14; 95% CI: 1.09, 1.22) indicating no statistically different risks. Men and women did not have statistically different risks of daily CVD mortality, hospitalizations from all CVD, ischemic heart disease, cardiac arrest, acute myocardial infarction, and heart failure from short-term PM2.5 exposure (difference in % change in risk per 10 μg/m3 PM2.5: 0.04 (95% CI, −0.42 to 0.51); −0.05 (−0.47 to 0.38); 0.17 (−0.90, 1.24); 1.42 (−1.06, 3.97); 1.33 (−0.05, 2.73); and −0.48 (−1.94, 1.01), respectively). Analysis using GRADE found low or very low quality of evidence for sex differences for PM2.5-CVD risks. In conclusion, this meta-analysis and quality of evidence assessment of current observational studies found very limited evidence of the effect modification by sex for effects of PM2.5 on CVD outcomes in adults, which can inform clinical approaches and policies.
Keywords: Cardiovascular outcomes, hospitalization, meta-analysis, mortality, particulate matter, sex, systematic review
1. Introduction
Cardiovascular diseases (CVDs) are a leading cause of death globally and CVD mortality reached 18.6 million worldwide in 2019 (Roth et al 2020). Epidemiological studies have reported adverse impacts of short-term or long-term exposure to particulate matter with aerodynamic diameter ≤2.5 μm (PM2.5) on cardiovascular outcomes including total CVDs (Karimi and Samadi 2019), ischemic heart disease (Alexeeff et al 2021b)(Lim et al 2020), cardiac arrest (CA) (Zhao et al 2017a). Some human trials have suggested the potential of reduced blood pressure and increased heart rate variability with reduced exposure to airborne particles (Faridi et al 2022). These findings imply that preventing effects of fine particulate matter is crucial to reducing disease burden from CVDs.
Previous studies showed that PM2.5’s effects on human health differ among subpopulations (Gold and Mittleman 2013a), and estimating risks for subpopulations is an important facet of epidemiological studies. Findings are inconsistent regarding whether sex influences vulnerability to PM2.5-CVDs risks (Gold and Mittleman 2013a). Disproportionate risks between men and women may relate to biological susceptibility and/or nonbiological factors such as different exposure level due to socioeconomic status and occupation (Sacks et al 2011) and gendered behaviors (Clougherty 2010). Proportionally smaller airways and greater airway reactivity of women than men may be a potential reason for differences by sex (Sacks et al 2011). A comprehensive systematic review of epidemiological literature examining effect modifications by sex for the associations between short-term and long-term exposure to ambient PM2.5 on CVDs has not been previously reported, to the best of our knowledge. This means that information is needed to understand if policies to mitigate exposure to PM2.5 can be expected to benefit men and women similarly. Identifying effect modification by sex for cardiovascular effects of PM2.5 is important to develop clinical approaches and policy interventions for outdoor air pollution in subpopulations at risk. Such findings also can inform studies of biological mechanism.
Men and women may have different vulnerability to health effects of PM2.5 due to different lung size and growth, gas absorption, and airway response rates. Women’s higher vulnerability to cardiovascular risks from exposure to particulate matter (PM) has been suggested by some previous narrative review studies (Hamanaka and Mutlu 2018, Tibuakuu et al 2018). A meta-analysis showed higher risks in women than men for coronary heart disease mortality risks from long-term PM2.5 exposure (Zhao et al 2017b). Another meta-analysis suggested higher out-of-hospital CA risks from PM2.5 in men than women (Zhao et al 2017a). Although several review studies addressed the vulnerability by sex for PM-CVD associations, they have some limitations in comprehensively reviewing the study results and evaluating the quality of evidence. Narrative reviews can be prone to selective bias in searching and reviewing literature. Although systematic reviews combine research findings based on their structured inclusion criteria, there is a limitation in comparing vulnerability by sex across various CVDs. Furthermore, quality of evidence for vulnerability by sex is often omitted in existing systematic reviews. Therefore, there is a need for systematic review that can provide comprehensive summary of evidence investigating the body of studies for each CVD that have been studied in relation to vulnerability by sex to cardiovascular effects of PM2.5, reviewing sex vulnerability across CVDs, and evaluating the quality of the evidence.
In this review research, we focused on PM2.5 than PM in other size ranges as PM2.5 has been the focus as a target for regulation and epidemiological study (Gold and Mittleman 2013b). For example, PM2.5 is regulated through the National Ambient Air Quality Standards (NAAQS) in the United States because of well-established knowledge of the cardiovascular and respiratory effects of PM2.5 from epidemiologic evidence (Bell et al 2007) and the World Health Organization (WHO) provides health-based guidelines for PM2.5. Smaller particles are thought to be more harmful to health than larger particles as PM2.5 is able to penetrate to the deepest parts of the lungs and gain access to other organs (Schraufnagel 2020, Yin et al 2020), although other size fractions are also harmful including larger PM (PM10) and particles smaller than PM2.5. We systematically reviewed observational studies to determine if vulnerability differs by sex (men or women) for associations between short-term and long-term PM2.5 exposure and cardiovascular outcomes in adults. Meta-regression analysis was performed to quantitatively combine risks and compare the size of risks between men and women for each studied CVD. Findings can assist researchers, decision-makers, and health professionals by identifying quality of evidence for effect modification by sex. Systematic reviews and meta-analysis can identify, assess, and summarize a large body of literature to provide a comprehensive interpretation of the scientific evidence (Higgins and Thompson 2002, Higgins et al 2022, Van Houwelingen et al 2002, MacKenzie et al 2012, Gopalakrishnan and Ganeshkumar 2013).
2. Methods
2.1. Literature search
We conducted literature searches in the databases Medline/Pubmed, Embase, GreenFILE, and Scopus for English-language papers published between Jan. 1995 and Feb. 2020. Details of the protocol were registered on PROSPERO (Heo et al 2020). Librarians searched each database using controlled vocabulary (eTable 4). Grey literature (i.e., non-peer reviewed) was excluded. We screened references of eligible studies that remained after full-text review and relevant systematic review studies found in the screening process. During the peer-review process, additional reference examinations (i.e., forward citation chaining) was applied using the ‘citationchaser’ program (Haddaway et al 2021) for the studies published during the period between Mar. 2020 and Dec. 2021.
2.2. Study selection and data extraction
This research is reported in accordance with the MOOSE Checklist for Meta-analyses of Observational Studies (eTable 5). We targeted cardiac disease, ischemic heart disease, heart failure (HF), heart attack, CA, arterial occlusive disease, myocardial ischemia, angina, emboli, arrhythmia, tachycardia, thrombosis, atrial fibrillation, and cardiac-related death. “Total cardiovascular disease” was included as an outcome. As we targeted clinical cardiovascular endpoint, pathological mechanisms (e.g., atherosclerosis, blood pressure, hypertension, cholesterol related disease) and cardiovascular abnormalities were excluded. Cerebrovascular diseases (e.g., stroke) were excluded as they are diseases affecting blood flow and blood vessels specifically in the brain.
We screened publications identified by the database searches based on our inclusion/exclusion criteria of the PICOS Worksheet (eTable 6). Two screeners in 4 teams screened an equally divided number of references. To be included, each reference required agreement from the 2-person screening team; a third screener resolved disagreements. Included studies fulfilled the following inclusion criteria of PICOS; the study: 1) addressed adults (as defined in each study); 2) examined short-term or long-term exposure to ambient PM2.5; 3) addressed risks estimations of PM2.5 and cardiovascular morbidity/mortality modified by sex (studies focusing on one sex group (e.g., only women) were also included); 4) included at least one of the target CVDs; and 5) was a population-based observational studies. Exclusion criteria were: 1) study population of only children; 2) PM2.5 exposure estimated by personal sampler; 3) results not reported specifically by sex, for at least one group; 4) studies of global disease burdens or disease mapping; 5) non-research publication types of commentary, brief article without detailed texts on methodologies, or systematic review; and 6) studies of PM2.5 exposure during wildfire, smog episodes, or Asian dust storms due to heterogeneous study characteristics.
We conducted full-text review and labeled 1 primary exclusion reason for each excluded study, although multiple conditions may apply. Data from each eligible study were independently extracted in duplication using a pre-generated data extraction form. Information collected included author, publication year, study location, duration, sample size, study design, exposure methods, period of exposure (i.e., short-term vs. long-term), type of CVD, International Classification of Diseases (ICD) code(s), type of statistical models for effect modifications (e.g., stratification, interaction terms), average PM2.5 concentration for the study, increment of pollution used for presentation of estimates of associations (e.g., 10 μg/m3), risk estimates (e.g., relative risks (RRs), 95% confidence intervals (CIs)), lag period (if applicable), and confounders analyzed. We extracted risk estimates by sex for each study. When exact data were unavailable from an article, we contacted the original authors twice and studies without responses from the original authors were excluded.
2.3. Data synthesis
We included both single-city and multicity studies. Risk estimates for men and women were pooled using random-effect meta-regression analysis. Meta-regression analyses were applied to CVDs with risk estimates from >5 studies. Meta-regression analysis was separately applied to long-term exposure and short-term exposure studies. A categorical variable of sex indicating risk estimates for men or women was applied as a moderator in meta-regression analysis. For example, sex-specific log-scaled risk ratios (e.g., LogRRmen, LogRRwomen) for long-term PM2.5 exposure for a standardized increment (i.e., 10 μg/m³) was referred by the moderator variable of sex in the meta-analysis. Pooled risk ratios for long-term PM2.5 exposure were calculated separately for men and women. The difference in the risks of long-term exposure between men and women was calculated as the ratio of the RRs (O’Keeffe et al 2018) using the exponential coefficient of the moderator variable referring to sex groups for the log RRs in men and women. We combined results for hospitalization and emergency room (ER) visits together for short-term PM2.5 exposure. Sex-specific pooled risks of mortality and hospitalization/ER visits in relation to short-term exposure were presented as percent change per 10 μg/m3 increase in PM2.5. The pooled risk difference between men and women was calculated by the coefficient (β) of the moderator variable referring to sex groups for the percent change in outcomes of short-term exposure studies (i.e., 100[exp(10β)−1). Studies with a study time period <1 year for health data were excluded. Heterogeneity of included studies was examined by standard I2 test applying the restricted maximum likelihood (REML) method. We determined the extent of between study heterogeneity with the following cut-offs based on suggestions from Grading of Recommendations, Assessment, Development and Evaluations (GRADE) guidelines adopted by the World Health Organization (WHO) (Schünemann et al 2013): <30% (low), 30-49% (moderate), 50-79% (substantial), and >80% (considerable).
We conducted assessment of risk of bias (RoB) for included studies using the OHAT Risk of Bias Rating Tool for Human and Animal Studies (Office of Health Assessment and Translation 2019). For each criterion of OHAT (i.e., selection bias, confounding bias, attrition/exclusion bias, detection bias, selective reporting bias), each study was rated using 4 scores: +2 (definitely low risk of selective reporting bias), +1 (probably low risk of bias), −1 (probably high risk of bias), or −2 (definitely high risk of bias). In rating selection bias, we evaluated if a given study had dissimilarity in terms of age, health status, and observation period for exposure and health outcomes. For confounding bias, we listed well-known confounders and co-exposures from previous literature and experts’ opinions and evaluated if they were properly addressed in each study. For attribution/exclusion bias, we evaluated if there was direct evidence from the article that exclusion of subjects from analyses was adequately addressed or the reasons of exclusion were reported. Validity of exposure and outcome measurements used in each study was evaluated regarding detection bias. Lastly, to rate selective bias, we evaluated if each article reported their results for all health outcomes with their protocols and research methodologies outlined. The RoB assessment of each study was conducted by the same investigators who extracted data and any disagreement was resolved by the leading author. Overall risk of bias was rated separately for each outcome across studies.
2.4. Quality of evidence
Grading evidence is a transparent and systematic process of assessing the quality of evidence for the research topic available in a body of literature. We determined quality of evidence for effect modification by sex according to the criteria of GRADE guidelines, which are established tools presenting a standardized process for grading evidence. Quality of evidence reflects the degree of confidence about findings for effect modification by sex for PM2.5 associations with each CVD outcome. Quality of evidence (or strength of evidence) is categorized as high, moderate, low, or very low. The process initially assigns each observational study a quality of evidence as ‘low’. Quality of evidence are downgraded one or two levels based on five downgrading criteria (inconsistency, publication bias, imprecision, indirectness, and risk of bias) (Schünemann et al 2013) and upgraded if 1) the estimated effect is very large (e.g., RR >2), 2) an exposure-response gradient is clear, or 3) potential residual biases would increase the effect, while no effect was observed from the current data combination. We upgraded quality of evidence by one level if it was likely that differences in exposure levels by sex were not addressed in included studies but would affect the effect modification by sex. Publication bias was examined using funnel plot of exposure-outcome combinations.
Based on the GRADE process, the extent of each criterion was categorized as ‘not serious’, ‘serious’, or ‘very serious’. Inconsistency of the included studies was assessed by the direction of point estimates (i.e., RR, % change), overlap of confidence intervals, and statistical criterion of meta-regression analysis (i.e., I2). Indirectness was rated for the following aspects: studies targeted representative samples of the population; studies measured exposure level to PM2.5 using the same measuring systems between the exposed and comparison groups; and studies used appropriate endpoints of target CVDs rather than surrogates to identify study samples. Regarding imprecision, we judged if the confidence intervals of risk differences between men and women span the null (i.e., 1 for RR, 0 for % changes) and if so, rated down for imprecision. We considered the imprecision as more ‘serious’ when both of the separate risk estimates for each sex group were not significant. Asymmetry of funnel plots of meta-regression analysis were constructed for assessment of publication bias. Quality of evidence is not rated across all CVDs but rated for each CVD outcome by exposure period (i.e., long-term, short-term) and health outcome. The GRADE guideline suggests to upgrade quality of evidence when considering all potential unmeasured bias in studies is expected to result in true effect size, assuming that having unmeasured bias in a rigorous observational study would result in an underestimate/overestimate of an effect of the exposure of interest. We judged if studies have accurately measured differences in exposure levels of PM2.5 between sex groups.
3. Results
3.1. Study characteristics of the included studies
A total of 12,502 unique articles were initially identified and screened by the search (Figure 1). After title and abstract screening, 645 studies remained for full-text review. Studies for CVD outcomes with ≤5 identified studies (n=47) and studies with methodological approaches not satisfying inclusion criteria (n=7) were excluded. During the full-text review process, we found 2 additional eligible studies for our systematic review through examining references cited in the included studies. Further, we added 30 studies to our analysis by performing forward citation chaining on the published papers from the time the paper search was completed to the peer-review period of this research (2020-2021). As a result, 93 studies were eligible for meta-analysis. Summaries of each included study are shown in eTables 1 and 2. The most applied study design was time-series analysis (n=41, 44.1%), mathematically equivalent to case-crossover design (n=25, 26.9%), which enabled quantitative synthesis of risk for short-term exposure to PM2.5 (eTable 2). Cohort study design was applied in 24 studies (25.8%).
Figure 1.
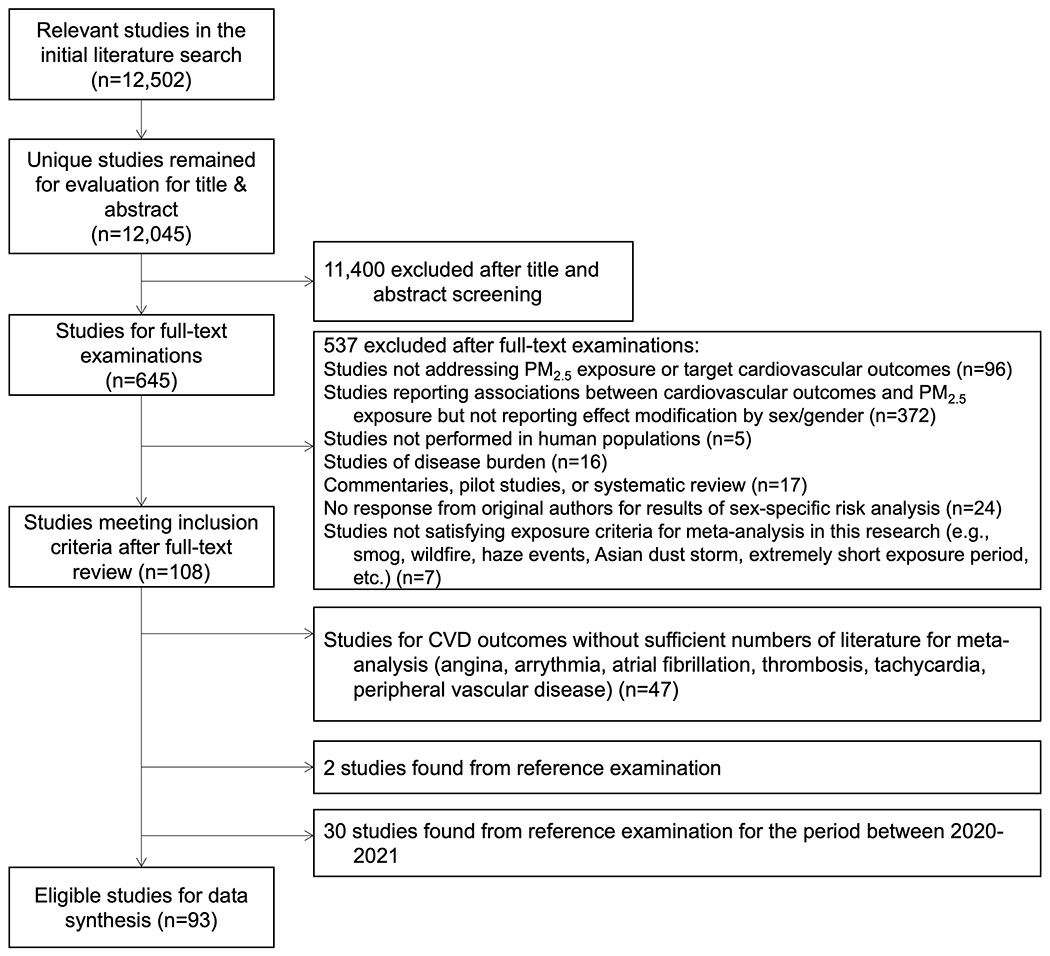
Flow chart of identified studies for systematic review and meta-analysis.
Two studies (2.2%) applied multiple designs including time-series and time-stratified case-crossover analyses. All CVD mortality was examined in 44 studies (41.5%) (25 studies for long-term exposure, 19 studies for short-term exposure) (Alexeeff et al 2021a, Beelen et al 2014, Berger et al 2018, Cesaroni et al 2013, Byun et al 2019, Chen et al 2018, Cheng et al 2019, Chi et al 2016, Dabass et al 2016, Dong et al 2020, Franklin et al 2007, Guiqin et al 2020, Hayes et al 2019, Hvidtfeldt et al 2019, Hystad et al 2020, Kim et al 2019, Kuźma et al 2020, Li et al 2018a, Liao et al 2021, Liang et al 2020, Lim et al 2020, Lin et al 2017, Lipsett et al 2011, Liu et al 2019, Luo et al 2016, Ma et al 2011, Miller et al 2007, Pinault et al 2016, 2018, Pope et al 2015, Qu et al 2018, Shi et al 2021, So et al 2020, Thurston et al 2016, Villeneuve et al 2015, Wang et al 2020a, Weichenthal et al 2014, Wu et al 2018, Yin et al 2017, Yu et al 2020, 2019, Zhang et al 2021b, Zhou et al 2021, 2022). All CVD hospitalization/ER visits were studied in 26 studies (28.0%) (Bell et al 2015, Chen et al 2021, 2020, Cox et al 2017, deSouza et al 2021, Gu et al 2020, Heo and Bell 2019, Hwang et al 2017, Gu et al 2020, Khan et al 2019, Lanzinger et al 2016, Liu et al 2020b, Michikawa et al 2015, Milojevic et al 2014, Motesaddi Zarandi et al 2022, Nayebare et al 2019, Ren et al 2021, Rodopoulou et al 2015, Su et al 2016, Vahedian et al 2017, Wang et al 2021, 2020b, Xu et al 2017b, Yang et al 2016, Yao et al 2019, Zhang et al 2021a, 2018, Zheng et al 2018). Hospitalization/ER visits from IHD and CA were studied in 11 (10.4%) (Bell et al 2015, Haikerwal et al 2015, Heo and Bell 2019, Liu et al 2020a, Milojevic et al 2014, Motesaddi Zarandi et al 2022, Pope et al 2006, Ren et al 2021, Xu et al 2017a, Ye et al 2016, Zheng et al 2018) and 10 (9.4%) studies (Dennekamp et al 2010, Haikerwal et al 2015, Kang et al 2016, Kojima et al 2020, Pradeau et al 2015, Silverman et al 2010, Straney et al 2014, Sullivan 2003, Wichmann et al 2013, Zhao et al 2020), respectively. AMI hospitalization/ER visits were examined in 8 studies (7.5%) (Bell et al 2015, Heo and Bell 2019, Milojevic et al 2014, Rich et al 2010, Sullivan et al 2005, Yu et al 2018, Weichenthal et al 2016, Zheng et al 2020) and HF hospitalization/ER visits were examined in 7 studies (6.6%) (Bell et al 2015, Haley et al 2009, Heo and Bell 2019, Li et al 2018b, Milojevic et al 2014, Pope III et al 2008, Zheng et al 2018). The period of 5 – 9 years was the most common study time period (n=25, 38.7%). One cohort study had a study period under 5 years (Shi et al 2021). Time-series analysis or case-crossover designs had study time periods under 20 years. The most studied countries were China (n=35, 37.6%) and the United States (n=26, 28.0%). Nine studies (9.7%) were conducted in Europe. Averages of PM2.5 concentrations from multiple monitoring stations were used in 48 studies (51.6%). Monitoring data from a single monitoring site was used in 11 studies (11.8%). Most studies were based on all ages but some targeted a narrower age range (e.g., ≥65, 50-64, 50-71 years) (eTable 1).
3.2. Meta-regression analysis and RoB assessment
For long-term exposure, pooled risk estimates by sex were assessed for all CVD mortality (Figure 2). For short-term exposure, sex-specific risk estimates were pooled for all CVD mortality, all CVD hospitalization/ER visits, IHD hospitalization/ER visits, CA hospitalization/ER visits, AMI hospitalization/ER visits, and HF hospitalization/ER visits (Figures 3 to 8). Numeric results of pooled risks are shown in eTable 3.
Figure 2.
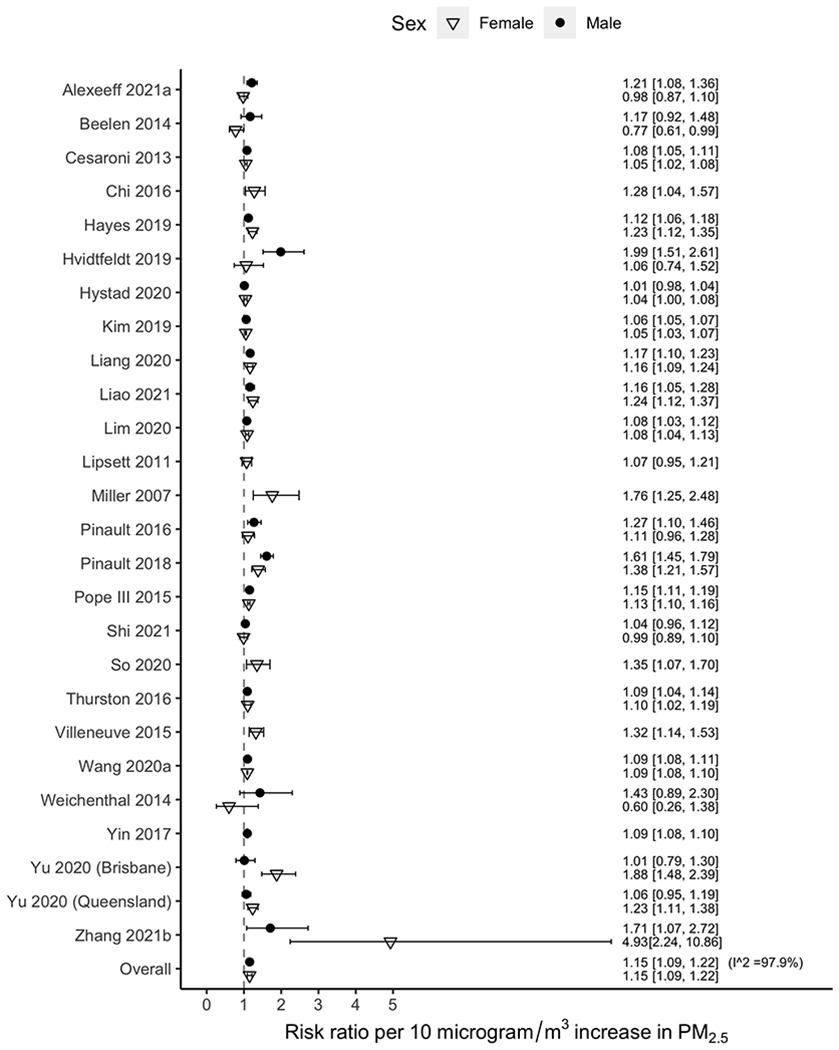
Risk ratio of all cardiovascular disease mortality for a 10 μg/m3 increase in PM2.5 concentration for the included studies in a meta-analysis, by sex. Horizontal lines represent 95% confidence intervals.
Figure 3.
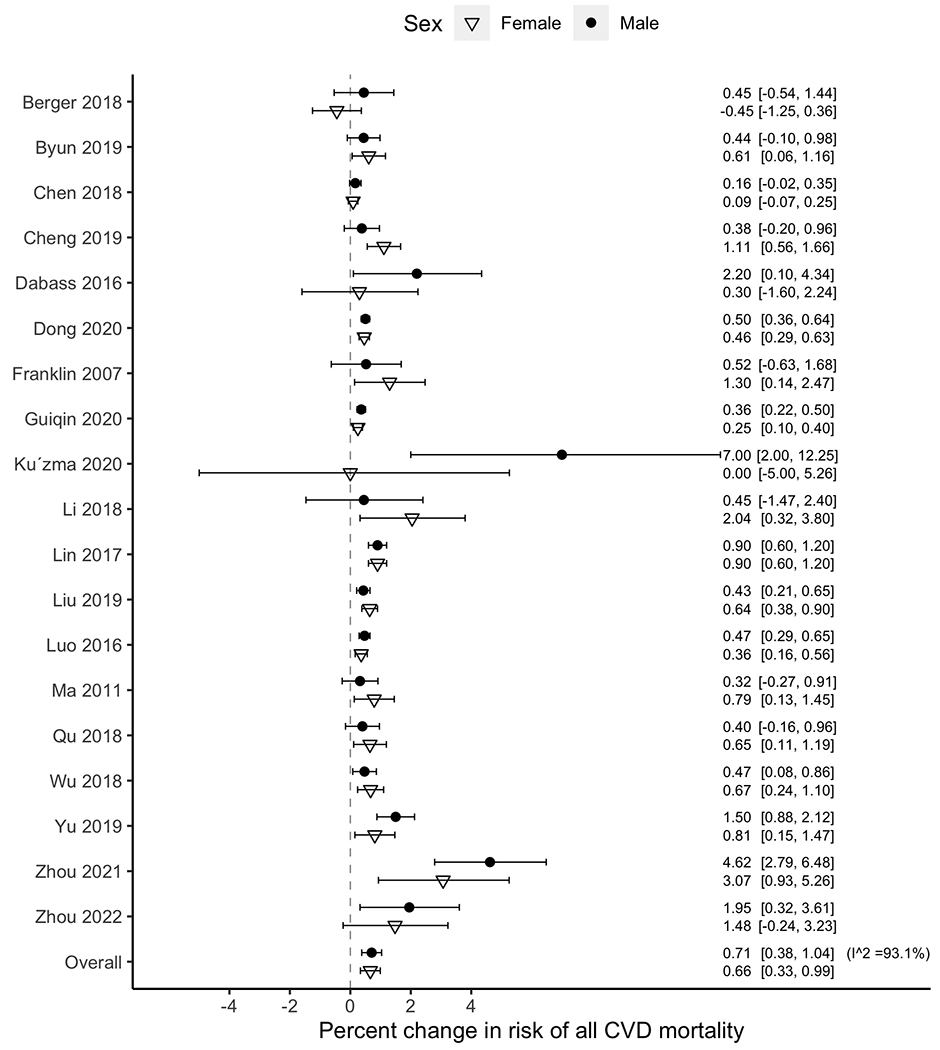
Percent changes in all CVD mortality for a 10 μg/m3 increase in PM2.5 (short-term) for the included studies in a meta-analysis, by sex. Horizontal lines represent 95% confidence intervals.
Figure 8.
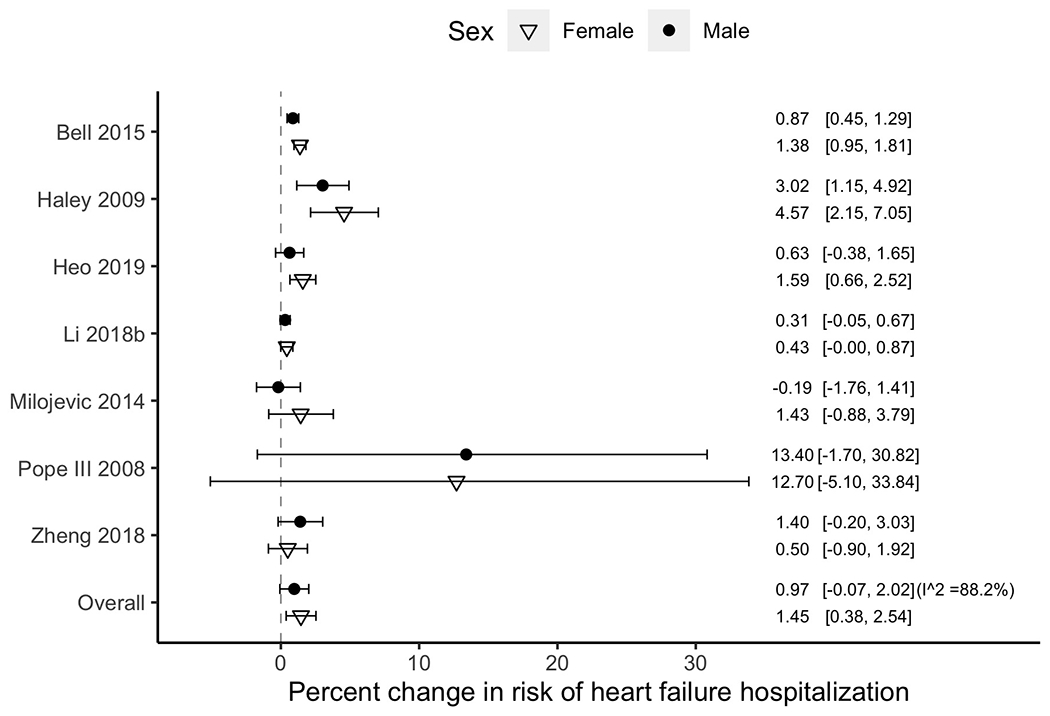
Percent changes in heart failure hospitalization for a 10 μg/m3 increase in PM2.5 (short-term) for the included studies in a meta-analysis, by sex. Horizontal lines represent 95% confidence intervals.
Long-term exposure
Results of meta-analysis for the risk ratio of all CVD mortality per 10 μg/m3 PM2.5 was 1.15 (95% CI, 1.09 to 1.22) for men and 1.15 (95% CI, 1.09 to 1.22) for women. The risk difference by sex (men vs. women) in risk ratio was 1.00 (95% CI, 0.93 to 1.08), indicating that the difference was null. Some studies reported risk estimates only for one sex group. We also applied a meta-regression analysis to compare the risks in men and women by only including the studies that reported risk estimates for both male and female groups. The results were robust to the main analysis. The risk difference between men and women increased to 1.03 (95% CI: 0.94 to 1.12) but the difference was not statistically significant (RR in men = 1.16, 95% CI: 1.09 to 1.23; RR in women = 1.13, 95% CI: 1.06 to 1.20; I2 = 85.8%). The results of RoB assessment are shown in eTable 7. Almost half of the included 25 studies showed ‘definitely low risk of bias’ for all the 5 domains of RoB assessment. Two studies showed ‘definitely high risk of bias’ for selection bias. Studies that were rated as ‘probably high risk of bias’ for any of the 5 domains were 11 out of 25 studies. Overall, RoB was rated as ‘probably high’ for selection bias and as ‘probably low’ for the other 4 domains of RoB assessment.
Short-term exposure
The percent change in mortality per 10 μg/m3 PM2.5 increase was 0.71 (95% CI, 0.38 to 1.04) for men and 0.66 (95% CI, 0.33 to 0.99) for women (Figure 3). The risk difference (men vs. women) was 0.04 (95% CI, −0.42 to 0.51), indicating no statistically significant difference (eTable 3). The percent change in all CVD hospitalization/ER visits per 10 μg/m3 PM2.5 was 0.53 (95% CI, 0.23 to 0.83) for men and 0.58 (95% CI, 0.28 to 0.88) for women (Figure 4); the risk difference between men and women was −0.05 (95% CI, −0.47 to 0.38). The percent change of IHD hospitalization/ER visits for men (0.66; 95% CI, −0.08 to 1.40) was higher than for women (0.49; 95% CI, −0.29 to 1.27) (Figure 5). For CA hospitalization/ER visits, the percent change for men (2.95; 95% CI, 1.22 to 4.71) was higher than for women (1.51, 95% CI: −0.32 to 3.37) (Figure 6). The percent change of AMI hospitalization/ER visits for men (1.02, 95% CI: 0.08 to 1.97) was higher than for women (−0.30, 95% CI: −1.30 to 0.70) (Figure 7). The percent change of HF hospitalization/ER visits was higher for women (1.45, 95% CI: 0.38 to 2.54) than for men (0.97, 95% CI: −0.07 to 2.02) (Figure 8). None of these differences in PM2.5-CVD risk by sex was statistically significant.
Figure 4.
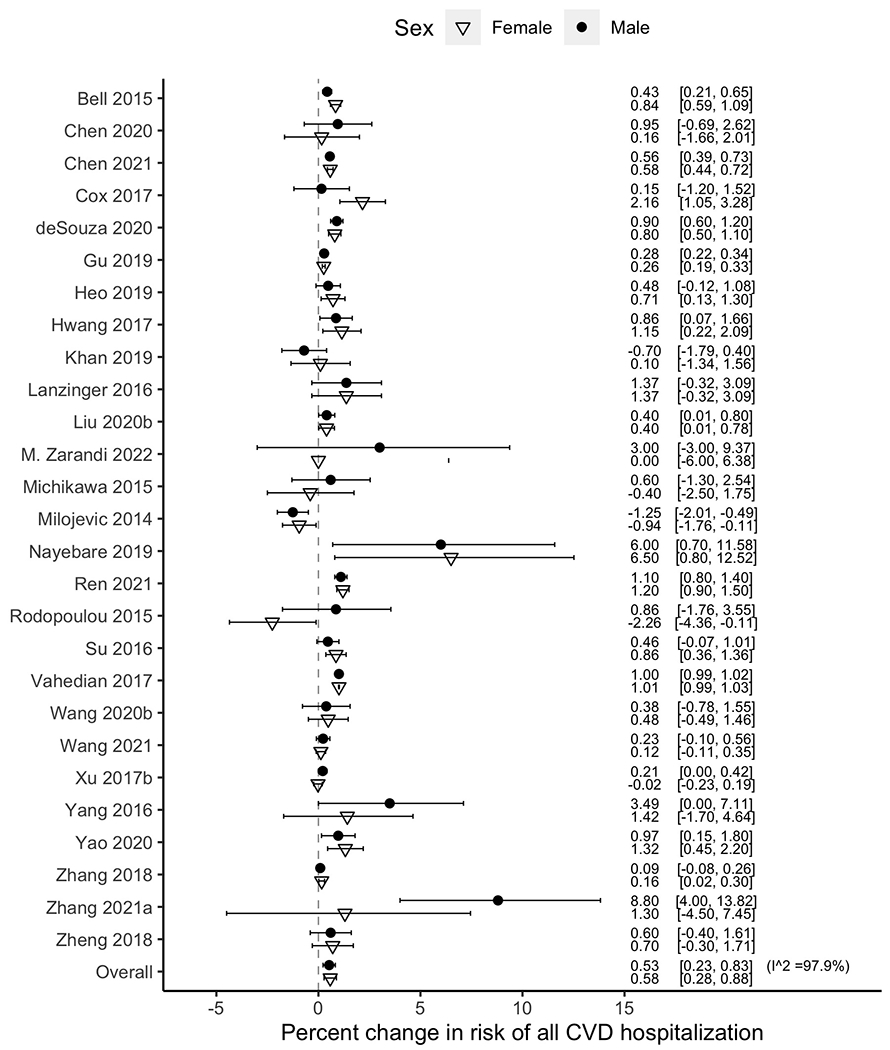
Percent changes in all cardiovascular hospitalization for a 10 μg/m3 increase in PM2.5 (short-term) for the included studies in a meta-analysis, by sex. Horizontal lines represent 95% confidence intervals.
Figure 5.
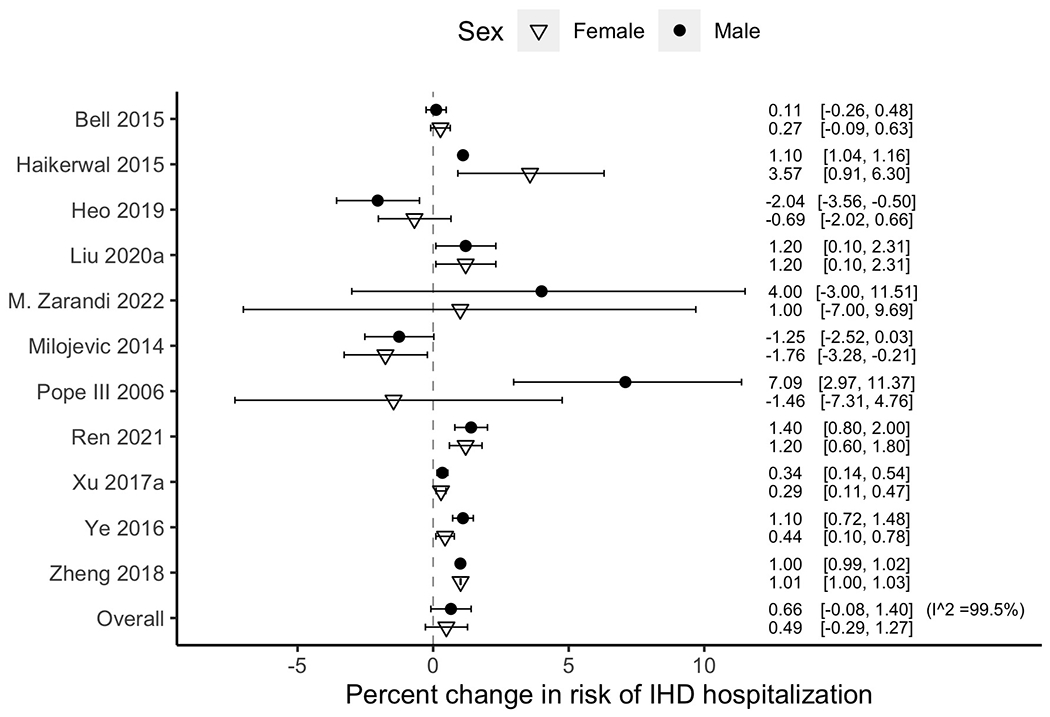
Percent changes in ischemic heart disease hospitalization for a 10 μg/m3 increase in PM2.5 (short-term) for the included studies in a meta-analysis, by sex. Horizontal lines represent 95% confidence intervals.
Figure 6.
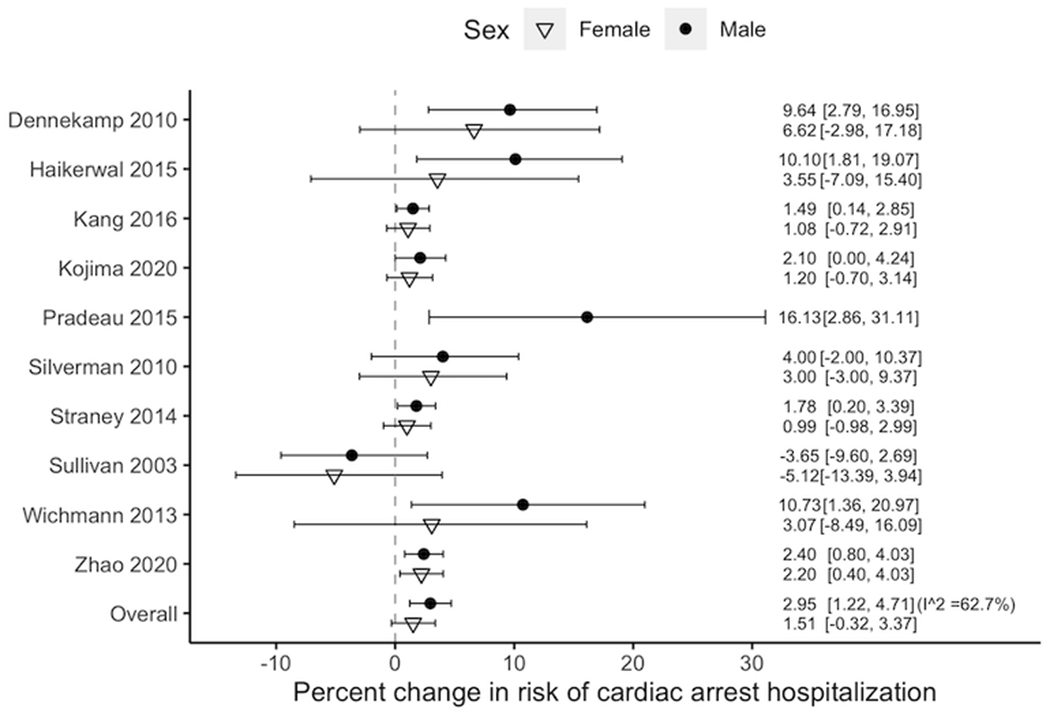
Percent changes in cardiac arrest hospitalization for a 10 μg/m3 increase in PM2.5 (short-term) for the included studies in a meta-analysis, by sex. Horizontal lines represent 95% confidence intervals.
Figure 7.
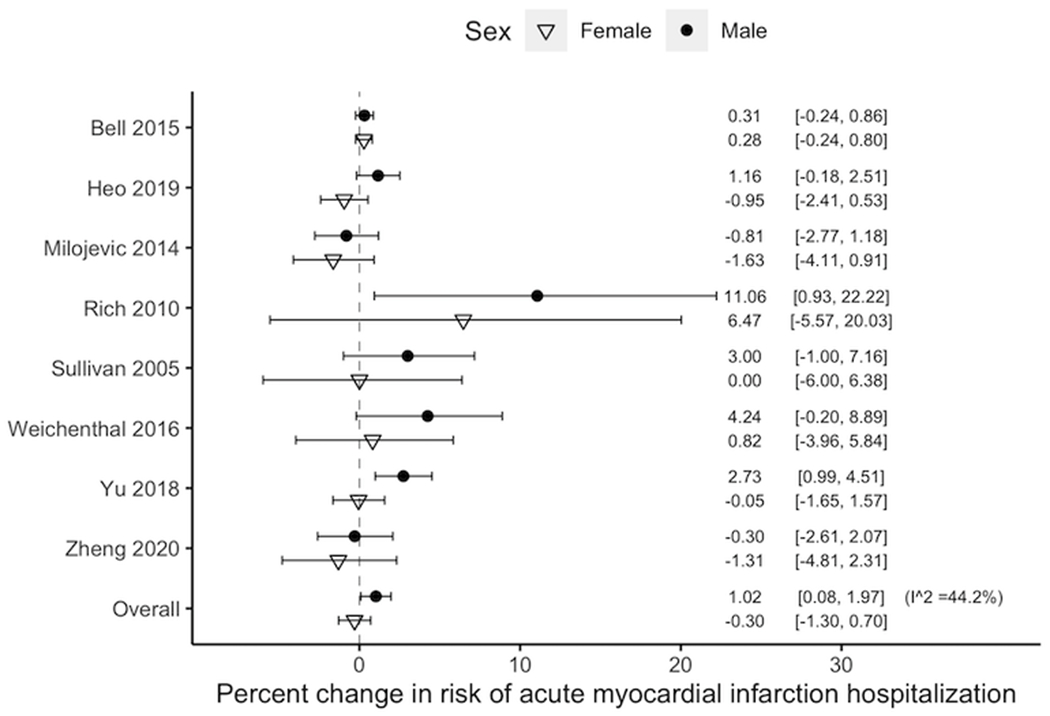
Percent changes in acute myocardial infarction hospitalization for a 10 μg/m3 increase in PM2.5 (short-term) for the included studies in a meta-analysis, by sex. Horizontal lines represent 95% confidence intervals.
The meta-regression model including the subset of studies that reported risks for both men and women for CA showed higher risk in men (% increase in men = 2.42, 95% CI: 1.12 to 3.74; % increase in women = 1.46, 95% CI: 0.08 to 2.87), but the difference was not statistically significant (0.94, 95% CI: −0.93 to 2.86).
Most studies were rated as ‘probably low risk’ or ‘definitely low risk’ of bias in the 5 domains of RoB assessment (eFigure 1). RoB assessment for each study is shown in eTables 7–13. Detailed assessment for each RoB domain is described below.
Selection bias:
We found that few studies had selection bias for study population (e.g., recruiting study participants from some select hospitals within a study region, restricted to a narrow age range for adults) (Ribeiro et al 2019, Rodopoulou et al 2015, Xu et al 2017b, Vahedian et al 2017) and were rated as ‘probably high risk of bias’. Studies where only one sex group was studied were rated as ‘definitely high risk of bias’ (Chi et al 2016, Miller et al 2007, So et al 2020, Villeneuve et al 2015, Pradeau et al 2015, Lipsett et al 2011, Yin et al 2017).
Confounding bias:
Cohort studies considered community-level socioeconomic status as well as several individual-level confounders (e.g., smoking, age, sex, BMI, etc.). Most time-series analysis and case-crossover studies adjusted for seasonality and temporal trend of mortality or morbidity for CVDs, weather, day of the week, and holidays resulting in a categorization of ‘probably low risk of bias’. Studies considering influenza epidemics were rated as ‘very low risk of bias’. A few studies did not control for the potential effects of weather (e.g., humidity, temperature) or holidays (Franklin et al 2007, Khan et al 2019, Haikerwal et al 2015, Milojevic et al 2014, Pradeau et al 2015) and were rated as ‘probably high risk of bias’.
Attrition/exclusion bias:
Many studies did not report the criteria for exclusion of study participants, which led to grading as ‘probably high’ risk of bias of attrition/exclusion bias for all CVD hospitalization/ER visits associated with short-term PM2.5 exposure and ‘probably low’ risk of bias for the other CVD outcomes associated with short-term PM2.5 exposure.
Detection bias:
CVDs were identified from population-representative medical or administrative records such as death certificate or hospitalization data, which reduces risk of poor detection of outcome. Exposure to air pollution was mostly based on community-level air pollution concentration rather than air pollution assessed with individual-level monitors. Studies using PM2.5 data from single monitoring site or multiple monitoring sites was rated as ‘probably low risk of bias’, whereas studies using modeling data were rated as ‘definitely low risk of bias’.
Selective reporting bias:
Due to the large volume of analysis considering complex lag structure as well as types of CVDs, we found some potential for selective reporting bias in the included studies. However, most studies provided results with sensitivity analysis.
3.3. Quality of evidence
The evidence profiles for quality of evidence are shown in eTable 3. Heterogeneity of effect estimates across studies was considered substantial or considerable in all cases. The quality of evidence for effect modification by sex was assessed as low for all CVD mortality associated with long-term PM2.5 exposure and all CVD mortality and hospitalization/ER visits associated with short-term PM2.5 exposure. Quality of evidence of effect modification by sex was very low for hospitalization/ER visits from IHD, CA, AMI, and HF associated with short-term PM2.5 exposure. Thus, our confidence in the effect modification by sex is limited. Detailed assessment for each upgrading/downgrading criterion is shown below.
Publication bias:
The funnel plot of all CVD mortality from long-term PM2.5 exposure showed asymmetry with an outlier on the lower left side (eFigure 2). This outlier was a cohort study (Weichenthal et al 2014) and no potential source of standard error of the risk estimates was identified. Also, this outlier would lead to a conservative bias towards the null for the mortality risk. Thus, the extent of publication bias was rated as ‘unlikely’.
For short-term exposure to PM2.5, we rated publication bias as ‘unlikely’ for all CVD mortality, all CVD hospitalization, CA hospitalization, and IHD hospitalization based on the funnel plots from meta-regression analysis (eFigure 2). The funnel plot for AMI hospitalization for short-term PM2.5 exposure showed outliers on the lower right side, which were from one study (Rich et al 2010). Methodological issues for exposure assessment and patient ascertainment were not found among the included studies. The asymmetry of the funnel plot due to one study showing heterogeneity was not sufficient to conclude publication bias, which led to ‘not serious’ for grading publication bias for AMI. Asymmetry was found in the funnel plot of HF due to one study (Pope III et al 2008) showing high standard deviation for the risk estimates in men and women, but this was not likely associated with publication bias (‘not serious’ publication bias).
Inconsistency:
Sources of inconsistency of the included studies were different population, exposure (e.g., exposure range, co-exposure, composition of particulate matter), age range (e.g., variation in underlying health conditions), studied lag days, different exposure period (e.g., whole year, summer, or wildfire season), and difference definitions of CVDs (e.g., different ICD code range) in addition to differences in short-term and long-term exposure periods. Even though study designs differ across the observational studies, men and women were analyzed under the same analytical approach within each study. Although I2 from the meta-regression analysis indicated substantial or considerable heterogeneity of the studies, estimated risks from the included studies showed consistent directions (i.e., positive associations). The CIs were overlapping for all included studies. Overall, the substantial inconsistency among the studies was not sufficient to downgrade the strength of evidence except for IHD hospitalization/ER visits. The risk estimates of IHD hospitalization/ER visits showed inconsistent directions of risk (i.e., negative and positive impacts of PM2.5) with confidence intervals that did not overlap (see Figure 5). Heterogeneity of the included studies was extremely high (I2 = 99.5%).
Indirectness:
As this review targeted specific end points of cardiovascular diseases excluding surrogate conditions (e.g., blood pressure, serum lipids, coronary calcification), there are no or minimum indirectness of outcome measurements. Exposure to air pollution has been measured based on the community- or region-level air pollution level that would not lead to systematic misclassification among study regions or between sex groups. Thus, we determined that the indirectness would be very low in the included studies and would not be sufficient to downgrade the strength of evidence.
Imprecision:
The estimated risk difference between men and women was not objectively high and the confidence intervals were wide. The risk differences do not lead us to a conclusion that a certain sex group is more vulnerable to the risks of CVDs from PM2.5 exposure. We downgraded quality of evidence by one level for imprecision for all CVD outcomes. IHD, CA, AMI, and HF did not find statistically significant sex-specific risk estimates either for men or women, which lead to an additional downgrade of quality of evidence by one level.
Risk of bias:
Although there were some studies rated as ‘definitely high risk of bias’ for some RoB domains, most studies showed probably low risk of bias (eTables 7–13, eFigure 2). Overall, there were no serious limitations among the included studies and the evidence of risks and effect modification by sex mostly came from studies at low RoB.
Upgrading quality of evidence:
The included studies did not incorporate in the analysis fact that men and women may have different time-activity patterns (e.g., indoor vs. outdoor) or occupational exposures to PM2.5. Given the likelihood that residence-based pollutant exposure models (e.g., monitored PM2.5 exposure) may not represent exposure levels across subpopulations by sex and could lead to estimates that do not identify risk difference by sex, we upgraded the quality of evidence by one level (e.g., supporting the theory that there could be still a possibility that sex may modify the risks of CVDs from PM2.5 exposure).
4. Discussion
Our meta-analysis found that effect modification by sex differed by type of CVD outcome and exposure period. Women tended to show higher risks of hospitalization/ER visits from all CVD and HF associated with short-term PM2.5 exposure, whereas men showed higher hospitalization risks for all CVDs and specific sub-types of CVDs including IHD, CA, and AMI associated with short-term PM2.5 exposure and all CVD mortality associated with long-term PM2.5 exposure, although risks were not statistically different by sex.
We focused on PM2.5 as it is widely used as the key form in air pollution regulation, however datasets for particulate matter in non-industrialized countries may be more reliant on PM10 or total suspended particles rather than PM2.5. Review studies focusing on particulate matter with various size distributions may be helpful to represent the impact of particulate matter on CVDs globally. Due to the large volume of searched studies with a variety of CVDs of interest, we did not consider sizes of particulate matter other than PM2.5. We note that the results of insignificant effect modification by sex in our review may not apply to risks from PM10.
PM2.5 entering the lung through respiratory system can flow to the terminal bronchi and alveoli and access to the tissues or organs through blood circulation causing acute and chronic damages (Zhao et al 2021). Substantial studies have suggested mechanisms of cardiovascular effects of PM2.5. Oxidative stress from PM2.5 exposure could release pro-inflammatory cytokines, which can lead to inflammatory response, apoptosis, and activation of pathways for vascular damage repair (Zhang et al 2007, p 2, Lederer et al 2021). Reduced vascular permeability caused by inflammatory response and apoptosis from PM2.5 exposure can accumulate fat and cholesterol molecules in the vascular walls, which can reduce blood flow and oxygen supply (Zhao et al 2021). PM2.5 can reduce the vascular reparative capacity by affecting viability, migration, and formation of pro-inflammatory cytokines (e.g., Interleukin 8) and Tumor necrosis factor Alpha (Zhao et al 2021, Chen et al 2017). PM2.5 can break the balance of macrophages, which are important for immune system, and this can lead to the deterioration of CVD (Zhao et al 2021). A growing body of evidence suggests that PM2.5 can induce hypermethylation of several key gene promoters that affects the progression of heart diseases (Huang 2013).
Differences between gender (i.e., self-representation, socially derived roles and behaviors) and sex (biologic differences) are important to explore potential mechanisms of vulnerability to cardiovascular effects of PM2.5 (Clougherty 2010). Vulnerability by different lung size and growth, gas absorption, and airway response rates would be based on sex. Certain comorbid diseases affect women differently than men as well (Norris et al 2020). Gender-related factors would include education, socioeconomic status, social disparities, psychologic factors, and lifestyle (Pucci et al 2017). Differences in exposure by occupation may relate to both sex and gender. Many epidemiological studies have not distinguished between sex and gender because many datasets, especially databases for death or medical records, have information for sex only, and occupational and cultural gender roles may be interwound with persistent job classifications by sex (Clougherty 2010). We recognize that sex and gender are different and that multiple genders exist, but none of the included studies addressed differences between sex and gender. Most studies were based on sex although some studies used the wording “sex” and “gender” interchangeably, as is currently common in some countries. Several studies (Franklin et al 2007, Xu et al 2017b) used the wording “gender” comparing the results between men and women but discussed biological differences by sex for their comparisons between men and women. In this review, we use the term “sex” as many epidemiological studies of PM2.5 and CVDs depend on health databases providing information of biological sex while we investigate differences between men and women. A few recent studies suggested that the risk of CVDs may differ between sex and gender. For example, a cross-sectional study conducted in Canada and Australia found that female gender based on psychosocial and cultural gender had higher associations with risk factors for CVDs than did female sex (Azizi et al 2021). We recognize that sex and gender refer to different concepts, and that more genders than “male” and “female” exist, but cannot investigate this issue due to the available information in existing studies. Uncertainties remain for how PM2.5-CVD associations differ by sex and gender, which warrants future research. Also, future systematic reviews are needed on these topics when such epidemiological evidence becomes available.
Measurement errors from the use of monitor measurements have been noted among studies, and some topical reviews focusing on a specific country have recommended utilization of modeling data (e.g., satellite-derived) for PM2.5 exposure assessment (Miller and Xu 2018). However, using data from monitoring stations has the strength of use of measurements rather than estimates and might be “best practice”, particularly, in low-income or middle-income countries with limited data input for more complex exposure models. Exclusion of studies using certain exposure measurements approaches may lead to including research only from particular countries. About 71.0% of the studies included in our review used fixed monitoring station data. We suggest that research findings based on monitoring data should not be dismissed when the research question relates to vulnerability of subgroups and some regions of the world necessarily rely on such methods.
Some CVDs (e.g., thrombosis, atrial fibrillation) were excluded due to the small number of studies or absence of studies on our research question. We note that exclusion from our review does not indicate absence of relationships with PM2.5 or risk difference by sex. These CVDs warrant future investigation for effect modification by sex. Also, we did not apply GRADE to rate quality of evidence for effects from PM2.5 for those outcomes for which we did not conduct meta-analysis as our research was systematic review along with meta-analysis. GRADE provides transparent processes for explicit judgments for each factor that determines the quality of evidence for each outcome (Dijkers 2013). It is important to note that tools for rating risk of bias of each study are often used to select studies to pool the risk of an outcome based on the quality of studies, but GRADE offers process to present summary of findings across studies in systematic reviews. While a measure of the risk for each outcome is an important element of a summary of findings table in GRADE, they may not be available in the summary of findings for outcomes for which meta-analysis is not available (Guyatt et al 2013). Thus, we note that assessments of the quality of evidence based on the GRADE approaches are warranted for the omitted CVD outcomes in our review to understand the quality of evidence and develop evidence-based recommendations in guidelines as such studies become available. There has been disagreement on GRADE’s applications to observational studies. GRADE prioritizes randomized trials over observational studies for rating quality of evidence and lacks the ability to distinguish quality among reasonably well-supported evidence from various study designs of observational studies (Rehfuess and Akl 2013). Due to insufficient possibilities for upgrading quality of evidence for observational studies, some previous research started with a baseline of “moderate” rather than “low” quality (Orellano et al 2020). We consider that observational studies are critical components to understanding health effects of air pollution, given ethical limits to personal exposure studies and inherent limitations of toxicological studies, although all study designs contribute key evidence; thus, starting at “low quality” for quality of evidence based on GRADE may underestimate findings. Therefore, we considered that study characteristics related to generalizability but not quality in observational studies (e.g., studying specific age ranges or exposure period relying on existing environmental and health datasets, differences in population characteristics and pollution level) as criteria to downgrade quality of evidence.
A strength of this meta-analysis is that we assessed both long-term and short-term PM2.5 exposure on mortality and morbidity of various CVDs to identify effect modification by sex. Most previous systematic reviews focused solely on either short-term or long-term exposure. We also summarized quality of evidence, which is often omitted in existing systematic reviews. Further, our study provides the most up-to-date synthesis of evidence, which includes many studies not available when the previous reviews were conducted.
Our study also has several limitations. Focusing on English-written literature may have affected publication bias or focused findings on global north countries. Most studies identified were from China and the United States, indicating the need for additional research in additional locations. While the focus on English-language articles may have missed some articles in other locations, further studies are likely needed in other regions. In particular, summarizing evidence for developing countries that have been less studied is needed in future studies to understand the risk differences by sex for the associations between PM2.5 and CVDs. Clinical trials are very rare for our research question. The needs and challenges for randomized clinical trials have been discussed elsewhere (Brook et al 2018). A recent systematic review study evaluating the efficacy of wearing respirators for reducing the impacts of air pollution on blood pressure and heart rate variability identified only a small number of trials (Faridi et al 2022). Nonetheless, evidence from observational studies based on adequate and plausible study designs can reasonably support evidence-based decision making and inform individuals at risk. We focused on the closest lag from events of CVDs (i.e., lag0) when combining risk estimates across studies to avoid publication bias, and did not conduct risk synthesis for all analyzed lag periods. The potential resulting bias might be small as a previous meta-analysis combining risk at multiple lags for CA risk from PM2.5 suggested small differences between polled risks from different lags (Zhao et al 2017a). We could not examine whether observed risk difference by sex was attributable to biological susceptibility or to exposure or other differences as the included studies were only based on observational studies. Future research is needed to explore these suggestive findings and investigate causal mechanisms. Additional work is also needed on a wider range of variables related to potential differences in populations that may explain differences in health response to air pollution by sex, such as differences in smoking patterns and healthcare systems. There are factors for heterogeneity across the included studies such as study population, particle size, and exposure methods as we applied meta-analysis to provide an overarching risk estimation addressing the heterogeneity across populations, regions, and study designs. Further, research is needed on additional health endpoints and how health impacts from particulate matter may differ across various health responses. Also, review of studies on other size fractions of PM2.5, especially smaller particles (e.g., PM1) may be warranted as such studies become available. Exposure assessment based on monitoring stations was used in more than 70% the included studies in our review. The effect of applying different exposure methods on the pooled risk of the outcomes should be further investigated.
In summary, we did not find evidence that the impacts of PM2.5 on mortality, hospitalization, and ER visits from CVDs differ between men and women. The findings imply that the current scientific evidence does not provide support for different policies for preventing cardiovascular risks from PM2.5 exposure for men and women. However, several factors as discussed above (e.g., sex vs. gender, PM chemical composition) limit a full understanding of this issue. For instance, individual-level exposure has not been considered in the included studies in this review. Addressing individual-level exposure between men and women and other relevant factors in comparing PM2.5-CVD associations remains a challenge in future epidemiologic studies and policy recommendations.
5. Conclusions
This meta-analysis summarized the current state of scientific evidence on whether PM2.5’s impact on CVDs differs for men and women. We pooled sex-specific PM2.5-CVDs risk estimates and assessed evidence of risk differences by sex. Overall, across the identified studies, differences in PM2.5-CVD risk were not statistically different by sex. There was low and very low quality of evidence that men or women were more vulnerable to effects of PM2.5 on CVD mortality or hospitalization/ER visits, which can inform policies and future work.
Supplementary Material
Acknowledgement
This publication was developed under Assistance Agreement No. RD83587101 awarded by the U.S. Environmental Protection Agency to Yale University. It has not been formally reviewed by EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the Agency. EPA does not endorse any products or commercial services mentioned in this publication. Research reported in this publication was also supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number R01MD012769 and the National Institute of Environmental Health Sciences of the National Institutes of Health under Award number R01ES026246. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Alexeeff SE, Deosaransingh K, Liao NS, Van Den Eeden SK, Schwartz J and Sidney S 2021a. Particulate matter and cardiovascular risk in adults with chronic obstructive pulmonary disease American Journal of Respiratory and Critical Care Medicine 204 159–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexeeff SE, Liao NS, Liu X, Van Den Eeden SK and Sidney S 2021b. Long-term PM2.5 exposure and risks of ischemic heart disease and stroke events: Review and meta-analysis Journal of the American Heart Association 10 1–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azizi Z, Gisinger T, Bender U, Deischinger C, Raparelli V, Norris CM, Kublickiene K, Herrero MT, El Emam K and Kautzky-Willer A 2021. Sex, Gender Factors and Cardiovascular Health in Canadian and Austrian Populations Canadian Journal of Cardiology [DOI] [PubMed] [Google Scholar]
- Beelen R, Stafoggia M, Raaschou-Nielsen O, Andersen ZJ, Xun WW, Katsouyanni K, Dimakopoulou K, Brunekreef B, Weinmayr G, Hoffmann B, Wolf K, Samoli E, Houthuijs D, Nieuwenhuijsen M, Oudin A, Forsberg B, Olsson D, Salomaa V, Lanki T, Yli-Tuomi T, Oftedal B, Aamodt G, Nafstad P, De Faire U, Pedersen NL, Östenson C-G, Fratiglioni L, Penell J, Korek M, Pyko A, Eriksen KT, Tjønneland A, Becker T, Eeftens M, Bots M, Meliefste K, Wang M, Bueno-de-Mesquita B, Sugiri D, Krämer U, Heinrich J, de Hoogh K, Key T, Peters A, Cyrys J, Concin H, Nagel G, Ineichen A, Schaffner E, Probst-Hensch N, Dratva J, Ducret-Stich R, Vilier A, Clavel-Chapelon F, Stempfelet M, Grioni S, Krogh V, Tsai M-Y, Marcon A, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Katsoulis M, Trichopoulou A, Vineis P and Hoek G 2014. Long-term Exposure to Air Pollution and Cardiovascular Mortality: An Analysis of 22 European Cohorts Epidemiology 25 368–78 [DOI] [PubMed] [Google Scholar]
- Bell ML, Dominici F, Ebisu K, Zeger SL and Samet JM 2007. Spatial and temporal variation in PM2. 5 chemical composition in the United States for health effects studies Environmental health perspectives 115 989–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Son J-Y, Peng RD, Wang Y and Dominici F 2015. Brief Report: Ambient PM2.5 and Risk of Hospital Admissions Epidemiology 26 575–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger K, Malig BJ, Hasheminassab S, Pearson DL, Sioutas C, Ostro B and Basu R 2018. Associations of Source-apportioned Fine Particles with Cause-specific Mortality in California Epidemiology 29 639–48 [DOI] [PubMed] [Google Scholar]
- Brook RD, Newby DE and Rajagopalan S 2018. Air Pollution and Cardiometabolic Disease: An Update and Call for Clinical Trials American Journal of Hypertension 31 1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byun G, Kim H, Choi Y and Lee J-T 2019. The difference in effect of ambient particles on mortality between days with and without yellow dust events: Using a larger dataset in Seoul, Korea from 1998 to 2015 Science of The Total Environment 691 819–26 [DOI] [PubMed] [Google Scholar]
- Cesaroni G, Badaloni C, Gariazzo C, Stafoggia M, Sozzi R, Davoli M and Forastiere F 2013. Long-Term Exposure to Urban Air Pollution and Mortality in a Cohort of More than a Million Adults in Rome Environmental Health Perspectives 121 324–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Chan A, Dominici F, Peng RD, Sabath B, Di Q, Schwartz J and Bell ML 2021. Do temporal trends of associations between short-term exposure to fine particulate matter (PM2.5) and risk of hospitalizations differ by sub-populations and urbanicity—a study of 968 US counties and the Medicare population Environmental Research 206 112271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C, Zhu P, Lan L, Zhou L, Liu R, Sun Q, Ban J, Wang W, Xu D and Li T 2018. Short-term exposures to PM2.5 and cause-specific mortality of cardiovascular health in China Environmental Research 161 188–94 [DOI] [PubMed] [Google Scholar]
- Chen R, Gao Q, Sun J, Yang H, Li Y, Kang F and Wu W 2020. Short-term effects of particulate matter exposure on emergency room visits for cardiovascular disease in Lanzhou, China: A time series analysis Environmental Science and Pollution Research 27 9327–35 [DOI] [PubMed] [Google Scholar]
- Chen S, Wu X, Hu J, Dai G, Rong A and Guo G 2017. PM2.5 exposure decreases viability, migration and angiogenesis in human umbilical vein endothelial cells and human microvascular endothelial cells Molecular medicine reports 16 2425–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H, Zhu F, Lei R, Shen C, Liu J, Yang M, Ding R and Cao J 2019. Associations of ambient PM2.5 and O3 with cardiovascular mortality: a time-series study in Hefei, China Int J Biometeorol 63 1437–47 [DOI] [PubMed] [Google Scholar]
- Chi G, Hajat A, Bird C, Cullen M, Griffin B, Miller K, Shih R, Stefanick M, Vedal S, Whitsel E and Kaufman J 2016. Individual and Neighborhood socioeconomic status and the association between air pollution and cardiovascular disease Environmental Health Perspectives 124 1840–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty JE 2010. A growing role for gender analysis in air pollution epidemiology Environmental health perspectives 118 167–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox L, Liu X, Shi L, Zu K and Goodman J 2017. Applying Nonparametric Methods to Analyses of Short-Term Fine Particulate Matter Exposure and Hospital Admissions for Cardiovascular Diseases among Older Adults IJERPH 14 1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabass A, Talbott EO, Bilonick RA, Rager JR, Venkat A, Marsh GM, Duan C and Xue T 2016. Using spatio-temporal modeling for exposure assessment in an investigation of fine particulate air pollution and cardiovascular mortality Environmental Research 151 564–72 [DOI] [PubMed] [Google Scholar]
- Dennekamp M, Akram M, Abramson MJ, Tonkin A, Sim MR, Fridman M and Erbas B 2010. Outdoor Air Pollution as a Trigger for Out-of-hospital Cardiac Arrests Epidemiology 21 494–500 [DOI] [PubMed] [Google Scholar]
- deSouza P, Braun D, Parks RM, Schwartz J, Dominici F and Kioumourtzoglou M-A 2021. Nationwide Study of Short-term Exposure to Fine Particulate Matter and Cardiovascular Hospitalizations Among Medicaid Enrollees Epidemiology 32 6–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijkers M 2013. Introducing GRADE: a systematic approach to rating evidence in systematic reviews and to guideline development KT Update 1 1–9 [Google Scholar]
- Dong Z, Wang H, Yin P, Wang L, Chen R, Fan W, Xu Y and Zhou M 2020. Time-weighted average of fine particulate matter exposure and cause-specific mortality in China: a nationwide analysis The Lancet Planetary Health 4 e343–51 [DOI] [PubMed] [Google Scholar]
- Faridi S, Brook RD, Yousefian F, Hassanvand MS, Nodehi RN, Shamsipour M, Rajagopalan S and Naddafi K 2022. Effects of respirators to reduce fine particulate matter exposures on blood pressure and heart rate variability: A systematic review and meta-analysis Environmental Pollution 119109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin M, Zeka A and Schwartz J 2007. Association between PM2.5 and all-cause and specific-cause mortality in 27 US communities Journal of Exposure Science and Environmental Epidemiology 17 279–87 [DOI] [PubMed] [Google Scholar]
- Gold DR and Mittleman MA 2013a. New insights into pollution and the cardiovascular system: 2010 to 2012 Circulation 127 1903–13 [DOI] [PubMed] [Google Scholar]
- Gold DR and Mittleman MA 2013b. New insights into pollution and the cardiovascular system: 2010 to 2012 Circulation 127 1903–13 [DOI] [PubMed] [Google Scholar]
- Gopalakrishnan S and Ganeshkumar P 2013. Systematic reviews and meta-analysis: understanding the best evidence in primary healthcare Journal of family medicine and primary care 2 9–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J, Shi Y, Zhu Y, Chen N, Wang H, Zhang Z and Chen T 2020. Ambient air pollution and cause-specific risk of hospital admission in China: A nationwide time-series study PLoS medicine 17 e1003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guiqin F, Xingqin A, Huayue L, Yaqin T and Pengpeng W 2020. Assessment of the Impact of PM2. 5 Exposure on the Daily Mortality of Circulatory System in Shijiazhuang, China Atmosphere 11 1018 [Google Scholar]
- Guyatt GH, Oxman AD, Santesso N, Helfand M, Vist G, Kunz R, Brozek J, Norris S, Meerpohl J and Djulbegovic B 2013. GRADE guidelines: 12. Preparing summary of findings tables—binary outcomes Journal of clinical epidemiology 66 158–72 [DOI] [PubMed] [Google Scholar]
- Haddaway NR, Grainger MJ and Gray CT 2021. citationchaser: An R package and Shiny app for forward and backward citations chasing in academic searching [DOI] [PubMed] [Google Scholar]
- Haikerwal A, Akram M, Monaco A Del, Smith K, Sim MR, Meyer M, Tonkin AM, Abramson MJ and Dennekamp M 2015. Impact of fine particulate matter (PM2.5) exposure during wildfires on cardiovascular health outcomes Journal of the American Heart Association 4 1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley VB, Talbot TO and Felton HD 2009. Surveillance of the short-term impact of fine particle air pollution on cardiovascular disease hospitalizations in New York State Environmental Health 8 1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamanaka RB and Mutlu GM 2018. Particulate Matter Air Pollution: Effects on the Cardiovascular System Frontiers in Endocrinology 9 1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes RB, Lim C, Zhang Y, Cromar K, Shao Y, Reynolds HR, Silverman DT, Jones RR, Park Y, Jerrett M, Ahn J and Thurston GD 2019. PM2.5 air pollution and cause-specific cardiovascular disease mortality International Journal of Epidemiology 49 25–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heo S and Bell ML 2019. The influence of green space on the short-term effects of particulate matter on hospitalization in the US for 2000–2013. Environmental research 174 61–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heo S, M B L, Speigelman D, Son J, Lim CC, Fong CK, Choi H, Ramirez R, Nyhan K, Dhillon KP, Prabhakaran D and KApoor S 2020. Systematic review on Effect Modification by gender or sex in Associations with PM2.5 and Cardiovascular outcomes in adults PROSPERO [Google Scholar]
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ and Welch VA (editors) 2022. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022) (Cochrane; ) Online: www.training.cochrane.org/handbook [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP and Thompson SG 2002. Quantifying heterogeneity in a meta-analysis Statistics in medicine 21 1539–58 [DOI] [PubMed] [Google Scholar]
- Huang Y-CT 2013. The role of in vitro gene expression profiling in particulate matter health research Journal of Toxicology and Environmental Health, Part B 16 381–94 [DOI] [PubMed] [Google Scholar]
- Hvidtfeldt UA, Sørensen M, Geels C, Ketzel M, Khan J, Tjønneland A, Overvad K, Brandt J and Raaschou-Nielsen O 2019. Long-term residential exposure to PM2.5, PM10, black carbon, NO2, and ozone and mortality in a Danish cohort Environment International 123 265–72 [DOI] [PubMed] [Google Scholar]
- Hwang S-H, Lee JY, Yi S-M and Kim H 2017. Associations of particulate matter and its components with emergency room visits for cardiovascular and respiratory diseases ed Q Sun PLoS ONE 12 e0183224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hystad P, Larkin A, Rangarajan S, AlHabib KF, Avezum Á, Calik KBT, Chifamba J, Dans A, Diaz R and du Plessis J L 2020. Associations of outdoor fine particulate air pollution and cardiovascular disease in 157 436 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study The Lancet Planetary Health 4 e235–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S-H, Heo J, Oh I-Y, Kim J, Lim W-H, Cho Y, Choi E-K, Yi S-M, Do Shin S, Kim H and Oh S 2016. Ambient air pollution and out-of-hospital cardiac arrest International Journal of Cardiology 203 1086–92 [DOI] [PubMed] [Google Scholar]
- Karimi B and Samadi S 2019. Mortality and hospitalizations due to cardiovascular and respiratory diseases associated with air pollution in Iran: A systematic review and meta-analysis Atmospheric environment 198 438–47 [Google Scholar]
- Khan R, Konishi S, Ng CFS, Umezaki M, Kabir AF, Tasmin S and Watanabe C 2019. Association between short-term exposure to fine particulate matter and daily emergency room visits at a cardiovascular hospital in Dhaka, Bangladesh Science of the Total Environment 646 1030–6 [DOI] [PubMed] [Google Scholar]
- Kim I-S, Yang P-S, Lee J, Yu HT, Kim T-H, Uhm J-S, Kim J-Y, Pak H-N, Lee M-H and Joung B 2019. Long-term fine particulate matter exposure and cardiovascular mortality in the general population: a nationwide cohort study Journal of Cardiology 75 549–58 [DOI] [PubMed] [Google Scholar]
- Kojima S, Michikawa T, Matsui K, Ogawa H, Yamazaki S, Nitta H, Takami A, Ueda K, Tahara Y and Yonemoto N 2020. Association of fine particulate matter exposure with bystander-witnessed out-of-hospital cardiac arrest of cardiac origin in Japan JAMA network open 3 e203043–e203043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuźma Ł, Struniawski K, Pogorzelski S, Bachórzewska-Gajewska H and Dobrzycki S 2020. Gender Differences in Association between Air Pollution and Daily Mortality in the Capital of the Green Lungs of Poland–Population-Based Study with 2,953,000 Person-Years of Follow-Up Journal of clinical medicine 9 2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanzinger S, Schneider A, Breitner S, Stafoggia M, Erzen I, Dostal M, Pastorkova A, Bastian S, Cyrys J, Zscheppang A, Kolodnitska T and Peters A 2016. Ultrafine and Fine Particles and Hospital Admissions in Central Europe. Results from the UFIREG Study Am J Respir Crit Care Med 194 1233–41 [DOI] [PubMed] [Google Scholar]
- Lederer AM, Fredriksen PM, Nkeh-Chungag BN, Everson F, Strijdom H, De Boever P and Goswami N 2021. Cardiovascular effects of air pollution: current evidence from animal and human studies American Journal of Physiology-Heart and Circulatory Physiology 320 H1417–39 [DOI] [PubMed] [Google Scholar]
- Li D, Wang J, Zhang Z, Shen P, Zheng P, Jin M, Lu H, Lin H and Chen K 2018a. Association between short-term exposure to ambient air pollution and daily mortality: a time-series study in Eastern China Environmental Science and Pollution Research 25 16135–43 [DOI] [PubMed] [Google Scholar]
- Li M, Wu Y, Tian Y-H, Cao Y-Y, Song J, Huang Z, Wang X-W and Hu Y-H 2018b. Association between PM2.5 and daily hospital admissions for heart failure: a time-series analysis in Beijing International journal of environmental research and public health 15 2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang F, Liu F, Huang K, Yang X, Li J, Xiao Q, Chen J, Liu X, Cao J and Shen C 2020. Long-term exposure to fine particulate matter and cardiovascular disease in China Journal of the American College of Cardiology 75 707–17 [DOI] [PubMed] [Google Scholar]
- Liao NS, Sidney S, Deosaransingh K, Van Den Eeden SK, Schwartz J and Alexeeff SE 2021. Particulate air pollution and risk of cardiovascular events among adults with a history of stroke or acute myocardial infarction Journal of the American Heart Association 10 e019758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim Y-H, Oh J, Han C, Bae H-J, Kim S, Jang Y, Ha E and Hong Y-C 2020. Long-term exposure to moderate fine particulate matter concentrations and cause-specific mortality in an ageing society International Journal of Epidemiology 49 1792–801 [DOI] [PubMed] [Google Scholar]
- Lin H, Ratnapradipa K, Wang X, Zhang Y, Xu Y, Yao Z, Dong G, Liu T, Clark J, Dick R, Xiao J, Zeng W, Li X, Qian Z (Min) and Ma W 2017. Hourly peak concentration measuring the PM 2.5 -mortality association: Results from six cities in the Pearl River Delta study Atmospheric Environment 161 27–33 [Google Scholar]
- Lipsett MJ, Ostro BD, Reynolds P, Goldberg D, Hertz A, Jerrett M, Smith DF, Garcia C, Chang ET and Bernstein L 2011. Long-term exposure to air pollution and cardiorespiratory disease in the California teachers study cohort American Journal of Respiratory and Critical Care Medicine 184 828–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M, Xue X, Zhou B, Zhang Y, Sun B, Chen J and Li X 2019. Population susceptibility differences and effects of air pollution on cardiovascular mortality: epidemiological evidence from a time-series study Environ Sci Pollut Res 26 15943–52 [DOI] [PubMed] [Google Scholar]
- Liu S, Wang L, Zhou L, Li W, Pu X, Jiang J, Chen Y, Zhang L and Qiu H 2020a. Differential effects of fine and coarse particulate matter on hospitalizations for ischemic heart disease: A population-based time-series analysis in Southwestern China Atmospheric Environment 224 117366 [Google Scholar]
- Liu Y, Sun J, Gou Y, Sun X, Zhang D and Xue F 2020b. Analysis of short-term effects of air pollution on cardiovascular disease using Bayesian spatio-temporal models International journal of environmental research and public health 17 879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo K, Li W, Zhang R, Li R, Xu Q and Cao Y 2016. Ambient Fine Particulate Matter Exposure and Risk of Cardiovascular Mortality: Adjustment of the Meteorological Factors IJERPH 13 1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y, Chen R, Pan G, Xu X, Song W, Chen B and Kan H 2011. Fine particulate air pollution and daily mortality in Shenyang, China Science of The Total Environment 409 2473–7 [DOI] [PubMed] [Google Scholar]
- MacKenzie H, Dewey A, Drahota A, Kilburn S, Kalra P, Fogg C and Zachariah D 2012. Systematic reviews: what they are, why they are important, and how to get involved Journal of Clinical and Preventive Cardiology 1 193–202 [Google Scholar]
- Michikawa T, Ueda K, Takeuchi A, Kinoshita M, Hayashi H, Ichinose T and Nitta H 2015. Impact of short-term exposure to fine particulate matter on emergency ambulance dispatches in Japan J Epidemiol Community Health 69 86–91 [DOI] [PubMed] [Google Scholar]
- Miller K, Siscovick D, Sheppard L, Shepherd K, Sullivan J, Anderson G and Kaufman J 2007. Long-Term Exposure to Air Pollution and Incidence of Cardiovascular Events in Women New England Journal of Medicine 356 447–58 [DOI] [PubMed] [Google Scholar]
- Miller L and Xu X 2018. Ambient PM2.5 human health effects-findings in China and research directions Atmosphere 9 1–16 [Google Scholar]
- Milojevic A, Wilkinson P, Armstrong B, Bhaskaran K, Smeeth L and Hajat S 2014. Short-term effects of air pollution on a range of cardiovascular events in England and Wales: Case-crossover analysis of the MINAP database, hospital admissions and mortality Heart 100 1093–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motesaddi Zarandi S, Hadei M, Hashemi SS, Shahhosseini E, Hopke PK, Namvar Z and Shahsavani A 2022. Effects of ambient air pollutants on hospital admissions and deaths for cardiovascular diseases: a time series analysis in Tehran Environmental Science and Pollution Research 29 1–13 [DOI] [PubMed] [Google Scholar]
- Nayebare SR, Aburizaiza OS, Siddique A, Carpenter DO, Pope CA III, Mirza HM, Zeb J, Aburiziza AJ and Khwaja HA 2019. Fine particles exposure and cardiopulmonary morbidity in Jeddah: A time-series analysis Science of The Total Environment 647 1314–22 [DOI] [PubMed] [Google Scholar]
- Norris CM, Yip CY, Nerenberg KA, Clavel M-A, Pacheco C, Foulds HJ, Hardy M, Gonsalves CA, Jaffer S and Parry M 2020. State of the science in women’s cardiovascular disease: a Canadian perspective on the influence of sex and gender Journal of the American Heart Association 9 e015634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Health Assessment and Translation 2019. Handbook for Conducting a Literature-Based Health Assessment Using OHAT Approach for Systematic Review and Evidence Integration (National Institute of Environmental Health Sciences; ) [Google Scholar]
- O’Keeffe LM, Taylor G, Huxley RR, Mitchell P, Woodward M and Peters SA 2018. Smoking as a risk factor for lung cancer in women and men: a systematic review and meta-analysis BMJ open 8 e021611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orellano P, Reynoso J, Quaranta N, Bardach A, Ciapponi A, Investigaciones C De, Nicolás S, Tecnológica U, Conicet N and Nicolás S 2020. Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: Systematic review and meta -analysis Environment International 142 105876. [DOI] [PubMed] [Google Scholar]
- Pinault L, Brauer M, Crouse DL, Weichenthal S, Erickson A, van Donkelaar A, Martin RV, Charbonneau S, Hystad P, Brook JR, Tjepkema M, Christidis T, Ménard R, Robichaud A and Burnett RT 2018. Diabetes Status and Susceptibility to the Effects of PM2.5 Exposure on Cardiovascular Mortality in a National Canadian Cohort Epidemiology 29 784–94 [DOI] [PubMed] [Google Scholar]
- Pinault L, Tjepkema M, Crouse DL, Weichenthal S, van Donkelaar A, Martin RV, Brauer M, Chen H and Burnett RT 2016. Risk estimates of mortality attributed to low concentrations of ambient fine particulate matter in the Canadian community health survey cohort Environ Health 15 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope CA, Muhlestein JB, May HT, Renlund DG, Anderson JL and Horne BD 2006. Ischemic Heart Disease Events Triggered by Short-Term Exposure to Fine Particulate Air Pollution Circulation 114 2443–8 [DOI] [PubMed] [Google Scholar]
- Pope CA, Turner MC, Burnett RT, Jerrett M, Gapstur SM, Diver WR, Krewski D and Brook RD 2015. Relationships Between Fine Particulate Air Pollution, Cardiometabolic Disorders, and Cardiovascular Mortality Circ Res 116 108–15 [DOI] [PubMed] [Google Scholar]
- Pope CA III, Renlund DG, Kfoury AG, May HT and Horne BD 2008. Relation of heart failure hospitalization to exposure to fine particulate air pollution The American journal of cardiology 102 1230–4 [DOI] [PubMed] [Google Scholar]
- Pradeau C, Rondeau V, Lévèque E, Guernion PY, Tentillier E, Thicoip M and Brochard P 2015. Air pollution and activation of mobile medical team for out-of-hospital cardiac arrest American Journal of Emergency Medicine 33 367–72 [DOI] [PubMed] [Google Scholar]
- Pucci G, Alcidi R, Tap L, Battista F, Mattace-Raso F and Schillaci G 2017. Sex-and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: A review of the literature Pharmacological research 120 34–42 [DOI] [PubMed] [Google Scholar]
- Qu Y, Pan Y, Niu H, He Y, Li M, Li L, Liu J and Li B 2018. Short-term effects of fine particulate matter on non-accidental and circulatory diseases mortality: A time series study among the elder in Changchun ed Q Sun PLoS ONE 13 e0209793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehfuess EA and Akl EA 2013. Current experience with applying the GRADE approach to public health interventions: An empirical study BMC Public Health 13 1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Z, Liu X, Liu T, Chen D, Jiao K, Wang X, Suo J, Yang H, Liao J and Ma L 2021. Effect of ambient fine particulates (PM 2.5) on hospital admissions for respiratory and cardiovascular diseases in Wuhan, China Respiratory research 22 1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribeiro PC, Nascimento LFC, Almeida AA, Targa M dos S and Cesar ACG 2019. Fine particulate matter and ischemic heart diseases in relation to sex. An ecological time series study Sao Paulo Medical Journal 137 60–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich DQ, Kipen HM, Zhang J, Kamat L, Wilson AC, Kostis JB and Group (MIDAS 12) M I D A S S 2010. Triggering of transmural infarctions, but not nontransmural infarctions, by ambient fine particles Environmental health perspectives 118 1229–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodopoulou S, Samoli E, Chalbot MCG and Kavouras IG 2015. Air pollution and cardiovascular and respiratory emergency visits in Central Arkansas: A time-series analysis Science of the Total Environment 536 872–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ and Benziger CP 2020. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study Journal of the American College of Cardiology 76 2982–3021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks JD, Stanek LW, Luben TJ, Johns DO, Buckley BJ, Brown JS and Ross M 2011. Particulate matter–induced health effects: who is susceptible? Environmental health perspectives 119 446–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraufnagel DE 2020. The health effects of ultrafine particles Experimental & molecular medicine 52 311–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schünemann H, Brożek J, Guyatt G and Oxman A 2013. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. (Grading of Recommendations, Assessment, Development and Evaluation (GRADE) Working Group; ) [Google Scholar]
- Shi Y, Zhang L, Li W, Wang Q, Tian A, Peng K, Li Y and Li J 2021. Association between long-term exposure to ambient air pollution and clinical outcomes among patients with heart failure: Findings from the China PEACE Prospective Heart Failure Study Ecotoxicology and Environmental Safety 222 112517. [DOI] [PubMed] [Google Scholar]
- Silverman RA, Ito K, Freese J, Kaufman BJ, De Claro D, Braun J and Prezant DJ 2010. Association of Ambient Fine Particles With Out-of-Hospital Cardiac Arrests in New York City American Journal of Epidemiology 172 917–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- So R, Jørgensen JT, Lim Y-H, Mehta AJ, Amini H, Mortensen LH, Westendorp R, Ketzel M, Hertel O and Brandt J 2020. Long-term exposure to low levels of air pollution and mortality adjusting for road traffic noise: A Danish Nurse Cohort study Environment International 143 105983. [DOI] [PubMed] [Google Scholar]
- Straney L, Finn J, Dennekamp M, Bremner A, Tonkin A and Jacobs I 2014. Evaluating the impact of air pollution on the incidence of out-of-hospital cardiac arrest in the Perth Metropolitan Region: 2000–2010. J Epidemiol Community Health 68 6–12 [DOI] [PubMed] [Google Scholar]
- Su C, Breitner S, Schneider A, Liu L, Franck U, Peters A and Pan X 2016. Short-term effects of fine particulate air pollution on cardiovascular hospital emergency room visits: a time-series study in Beijing, China Int Arch Occup Environ Health 89 641–57 [DOI] [PubMed] [Google Scholar]
- Sullivan J 2003. Exposure to Ambient Fine Particulate Matter and Primary Cardiac Arrest among Persons With and Without Clinically Recognized Heart Disease American Journal of Epidemiology 157 501–9 [DOI] [PubMed] [Google Scholar]
- Sullivan J, Sheppard L, Schreuder A, Ishikawa N, Siscovick D and Kaufman J 2005. Relation between short-term fine-particulate matter exposure and onset of myocardial infarction Epidemiology 41–8 [DOI] [PubMed] [Google Scholar]
- Thurston GD, Ahn J, Cromar KR, Shao Y, Reynolds HR, Jerrett M, Lim CC, Shanley R, Park Y and Hayes RB 2016. Ambient Particulate Matter Air Pollution Exposure and Mortality in the NIH-AARP Diet and Health Cohort Environmental Health Perspectives 124 484–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibuakuu M, Michos ED, Navas-Acien A and Jones MR 2018. Air pollution and cardiovascular disease: a focus on vulnerable populations worldwide Current epidemiology reports 5 370–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahedian M, Khanjani N, Mirzaee M and Koolivand A 2017. Ambient air pollution and daily hospital admissions for cardiovascular diseases in Arak, Iran ARYA Atherosclerosis 13 117–34 [PMC free article] [PubMed] [Google Scholar]
- Van Houwelingen HC, Arends LR and Stijnen T 2002. Advanced methods in meta-analysis: multivariate approach and meta-regression Statistics in medicine 21 589–624 [DOI] [PubMed] [Google Scholar]
- Villeneuve PJ, Weichenthal SA, Crouse D, Miller AB, To T, Martin RV, van Donkelaar A, Wall C and Burnett RT 2015. Long-term Exposure to Fine Particulate Matter Air Pollution and Mortality Among Canadian Women. Epidemiology 26 536–45 [DOI] [PubMed] [Google Scholar]
- Wang B, Eum K-D, Kazemiparkouhi F, Li C, Manjourides J, Pavlu V and Suh H 2020a. The impact of long-term PM 2.5 exposure on specific causes of death: Exposure-response curves and effect modification among 53 million US Medicare beneficiaries Environmental Health 19 1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Leng M, Liu Y, Qian ZM, Zhang J, Li Z, Sun L, Qin L, Wang C and Howard SW 2021. Different sized particles associated with all-cause and cause-specific emergency ambulance calls: A multicity time-series analysis in China Science of The Total Environment 783 147060. [DOI] [PubMed] [Google Scholar]
- Wang X, Tian J, Li Z, Lai J, Huang X, He Y, Ye Z and Li G 2020b. Relationship between different particle size fractions and all-cause and cause-specific emergency ambulance dispatches Environmental Health 19 1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weichenthal S, Lavigne E, Evans G, Pollitt K and Burnett RT 2016 Ambient PM 2.5 and risk of emergency room visits for myocardial infarction: impact of regional PM 2.5 oxidative potential: a case-crossover study Environmental Health 15 1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weichenthal S, Villeneuve PJ, Burnett RT, van Donkelaar A, Martin RV, Jones RR, DellaValle CT, Sandler DP, Ward MH and Hoppin JA 2014. Long-term exposure to fine particulate matter: association with nonaccidental and cardiovascular mortality in the agricultural health study cohort Environmental health perspectives 122 609–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichmann J, Folke F, Torp-Pedersen C, Lippert F, Ketzel M, Ellermann T and Loft S 2013. Out-of-Hospital Cardiac Arrests and Outdoor Air Pollution Exposure in Copenhagen, Denmark ed H ten Cate PLoS ONE 8 e53684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu R, Zhong L, Huang X, Xu H, Liu S, Feng B, Wang T, Song X, Bai Y, Wu F, Wang X and Huang W 2018. Temporal variations in ambient particulate matter reduction associated short-term mortality risks in Guangzhou, China: A time-series analysis (2006–2016) Science of The Total Environment 645 491–8 [DOI] [PubMed] [Google Scholar]
- Xu A, Mu Z, Jiang B, Wang W, Yu H, Zhang L and Li J 2017a. Acute Effects of Particulate Air Pollution on Ischemic Heart Disease Hospitalizations in Shanghai, China IJERPH 14 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q, Wang S, Guo Y, Wang C, Huang F, Li X, Gao Q, Wu L, Tao L, Guo J, Wang W and Guo X 2017b. Acute exposure to fine particulate matter and cardiovascular hospital emergency room visits in Beijing, China Environmental Pollution 220 317–27 [DOI] [PubMed] [Google Scholar]
- Yang H-C, Chang S-H, Lu R and Liou D-M 2016. The effect of particulate matter size on cardiovascular health in Taipei Basin, Taiwan Computer Methods and Programs in Biomedicine 137 261–8 [DOI] [PubMed] [Google Scholar]
- Yao C, Wang Y, Williams C, Xu C, Kartsonaki C, Lin Y, Zhang P, Yin P and Lam KBH 2019. The association between high particulate matter pollution and daily cause-specific hospital admissions: a time-series study in Yichang, China Environ Sci Pollut Res 27 5240–50 [DOI] [PubMed] [Google Scholar]
- Ye X, Peng L, Kan H, Wang W, Geng F, Mu Z, Zhou J and Yang D 2016. Acute Effects of Particulate Air Pollution on the Incidence of Coronary Heart Disease in Shanghai, China ed S A Cormier PLoS ONE 11 e0151119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin P, Brauer M, Cohen A, Burnett RT, Liu J, Liu Y, Liang R, Wang W, Qi J and Wang L 2017. Long-term fine particulate matter exposure and nonaccidental and cause-specific mortality in a large national cohort of Chinese men Environmental health perspectives 125 117002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin P, Guo J, Wang L, Fan W, Lu F, Guo M, Moreno SB, Wang Y, Wang H and Zhou M 2020. Higher risk of cardiovascular disease associated with smaller size-fractioned particulate matter Environmental Science & Technology Letters 7 95–101 [Google Scholar]
- Yu W, Guo Y, Shi L and Li S 2020. The association between long-term exposure to low-level PM2. 5 and mortality in the state of Queensland, Australia: A modelling study with the difference-in-differences approach PLoS medicine 17 e1003141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y, Yao S, Dong H, Ji M, Chen Z, Li G, Yao X, Wang S-L and Zhang Z 2018. Short-term effects of ambient air pollutants and myocardial infarction in Changzhou, China Environmental Science and Pollution Research 25 22285–93 [DOI] [PubMed] [Google Scholar]
- Yu Y, Yao S, Dong H, Wang L, Wang C, Ji X, Ji M, Yao X and Zhang Z 2019. Association between short-term exposure to particulate matter air pollution and cause-specific mortality in Changzhou, China Environmental Research 170 7–15 [DOI] [PubMed] [Google Scholar]
- Zhang L, Ding L, Cheung TH, Dong M-Q, Chen J, Sewell AK, Liu X, Yates JR III and Han M 2007. Systematic identification of C. elegans miRISC proteins, miRNAs, and mRNA targets by their interactions with GW182 proteins AIN-1 and AIN-2 Molecular cell 28 598–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Wang S, Fan X and Ye X 2018. Temperature modulation of the health effects of particulate matter in Beijing, China Environ Sci Pollut Res 25 10857–66 [DOI] [PubMed] [Google Scholar]
- Zhang Y, Zhang L, Wei J, Liu L, Wang Y, Liu J, Zhou P, Wang L, Ding Z and Zhang Y 2021a. Size-specific particulate air pollution and hospitalization for cardiovascular diseases: A case-crossover study in Shenzhen, China Atmospheric Environment 251 118271 [Google Scholar]
- Zhang Z, Wang J, Kwong JC, Burnett RT, van Donkelaar A, Hystad P, Martin RV, Bai L, McLaughlin J and Chen H 2021b. Long-term exposure to air pollution and mortality in a prospective cohort: The Ontario Health Study Environment International 154 106570. [DOI] [PubMed] [Google Scholar]
- Zhao B, Johnston FH, Salimi F, Kurabayashi M and Negishi K 2020. Short-term exposure to ambient fine particulate matter and out-of-hospital cardiac arrest: a nationwide case-crossover study in Japan The Lancet Planetary Health 4 e15–23 [DOI] [PubMed] [Google Scholar]
- Zhao R, Chen S, Wang W, Huang J, Wang K, Liu L and Wei S 2017a. The impact of short-term exposure to air pollutants on the onset of out-of-hospital cardiac arrest: A systematic review and meta-analysis International Journal of Cardiology 226 110–7 [DOI] [PubMed] [Google Scholar]
- Zhao T, Qi W, Yang P, Yang L, Shi Y, Zhou L and Ye L 2021. Mechanisms of cardiovascular toxicity induced by PM2.5: a review Environmental Science and Pollution Research 1–19 [DOI] [PubMed] [Google Scholar]
- Zhao Y, Cheng Z, Lu Y, Chang X, Chan C, Bai Y, Zhang Y and Cheng N 2017b. PM10 and PM2.5 particles as main air pollutants contributing to rising risks of coronary heart disease: a systematic review Environmental Technology Reviews 6 174–85 [Google Scholar]
- Zheng M, Zhang Y, Feng W, Chen Y, Huan L, Ye S, Wu J, Huang J, Liao Y and Guo P 2020. Short-term exposure to ambient air pollution and acute myocardial infarction attack risk Journal of Public Health 28 367–74 [Google Scholar]
- Zheng P, Shen P, Ye Z, Zhang Z, Chai P, Li D, Jin M, Tang M-L, Lu H, Lin H, Wang J and Chen K 2018. Acute effect of fine and coarse particular matter on cardiovascular visits in Ningbo, China Environ Sci Pollut Res 25 33548–55 [DOI] [PubMed] [Google Scholar]
- Zhou H, Geng H, Dong C and Bai T 2021. The short-term harvesting effects of ambient particulate matter on mortality in Taiyuan elderly residents: A time-series analysis with a generalized additive distributed lag model Ecotoxicology and Environmental Safety 207 111235. [DOI] [PubMed] [Google Scholar]
- Zhou X, Wang C, Chen P, Chen Y, Yin L, Du W and Pu Y 2022. Time series analysis of short-term effects of particulate matter pollution on the circulatory system disease mortality risk in Lishui District, China Environmental Science and Pollution Research 1–10 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


