Abstract
Introduction:
Injury is a major health problem worldwide and a leading cause of death and disability. Disability caused by traumatic injury is often severe and long-lasting. Injuries place a large burden on societies and individuals in the community, both in cost and lost quality of life. Progress in developing effective injury prevention programs in developing countries is hindered by the lack of basic epidemiological injury data regarding the prevalence of traumatic injuries. The aim of this research was to describe the epidemiological characteristics of injury in all hospitals in Georgia.
Methods:
The database of the National Center for Disease Control and Public Health of Georgia for 2018, which includes all hospital admissions, was used to identify injury cases treated in hospitals. Cases were included based on the S and T diagnosis coded of ICD-10.
Results:
A total of 25103 adult patients were admitted for an injury, of whom 14798 (59%) were males and 10305 (41%) were females, between the ages of 18 and 108 years old. The highest prevalence was among the age group 25–44 years old (n=8654; 34%), followed by 45–64 years old (n=6852; 27%). The main mechanism of injury was falls (n=13932; 55%) and exposure to mechanical forces (n=2701; 11%). Over 1,50% (n=379) of injuries resulted in death after hospitalization. The median hospital length of stay (LOS) was 2 days. There was a significant association between age, mechanism of injury, type of injury, performed surgical interventions, and longer LOS.
Conclusion:
Injuries are prevalent throughout the life course and cause substantial hospitalization time. This research can help focus prevention efforts can focus on the demographic and injury causes that are most prevalent.
Keywords: Injury, Epidemiological characteristics, Injury date, Prevention, Georgia
Introduction
Traumatic injuries account for significant global burden of disease, causing 9% of all deaths worldwide and substantial short- and long-term disability. Almost 16,000 people die from injuries worldwide every day. Injuries occur across all age and income groups, and their incidence varies significantly between countries. Injury rates are disproportionately high in low- and middle -income countries (LMICs) [1–6]. However, despite the fact that more than 90% of injury related deaths occur in LMICs, most of the research comes from high- income countries [1,4,7,8]. In spite of the overall impact and importance of the topic, emerging economies such as Georgia experience high injury rates yet have little research addressing incidence, characteristics, risk factors, and prevention strategies [7].
Georgia is a country in the Caucasus region of Eurasia. Located at the crossroads of western Asia and eastern Europe, Georgia has a total population 3 713 800 of which 691 300 (18,61%) is pediatric (0–14 years), 2 492 300 (67,11%) adult (15–64), and 530 200 (14,28%) elderly (65 years and over) [9]. The country is divided into the capital city Tbilisi and eleven regions (two of which, Abkhazia and South Ossetia, are now politically beyond the jurisdiction of the central authorities of Georgia). Traumatic injuries are the fourth leading cause of death in Georgia [7]. According to the National Center for Disease Control and Public Health of Georgia (NCDC), the incidence of injuries in Georgia per 100,000 population in 2018 year was 3042.3 [10].
Basic epidemiological studies which provide information about the prevalence of injury, injury characteristics, age and sex distribution can create meaningful information for planning, developing and implementing injury prevention strategies [2,11,12]. We aimed to study and describe the injury characteristics and outcome of injuries in our settings, to understand the basis for establishment of prevention measures and strategies. Therefore, the study was conducted with the goal of providing the baseline data to policy makers and other stakeholders to help guide future research, policy and funding agendas.
Materials and Methods
This was a retrospective, descriptive study of injured patients of aged 18 and above admitted to all private and public hospitals in Georgia. Data comes from a total of 152 hospitals in the country, of which almost half (70) are located in the capital and provide service for the people of Tbilisi (population of 1 158700 in 2018), as well as being available for referral for different regions of Georgia (total population 3 729600 in 2018). The data reported in this manuscript were extracted from the official database of the National Center for Disease Control and Public Health of Georgia (NCDC). Injuries were identified using ICD-10 classifications using the class XIX (S and T codes) and class XX for the type of injury (V-Y codes). The National database is based on the principle of double coding, where a class XIX code describing the nature of the injury is added to a class XX code describing its cause. Injury external causes are presented as appendix to ICD – 10 for external cause classification. For codes S and T it is obligatory to use codes of external causes. ICD-10, with the external causes classification, is the general informational cluster for the international mortality reporting and is widely used for the classification of hospitalized injuries [13]. The study period was from January 1, 2018 to December 31, 2018.
The data included in the present manuscript is the following: patient’s demographic data, type of injury, and outcome of treatment (ie post-operative complications, length of hospital stay and case fatality proportion). Injury mechanisms were defined according to ICD-10 as follows: transport accidents (V01–V99); falls (W00–W19); exposure to mechanical forces (W20–W64); exposure to fire/burn/radiation/air temperature and pressure (W85–W99, X00–X09, X10–X19, X76–X77, Y26–Y27); poisoning/toxic effects (X40–X49, X60–X69, X85–X90, Y10–Y19); unspecified injuries (X58–X59, X84, Y09, Y34). Since we studied the initial injury-related hospitalizations, we have not considered the following Y codes: “Complications of medical and surgical care” (Y40–Y84) and “Sequelae of external causes of morbidity and mortality”(Y85–Y89). Other mechanisms were combined as a category “other specified”.
Injuries were classified into 10 categories by their anatomical location: injuries to the head, thorax/neck, abdomen and pelvis including lower back and genitals, upper extremities, lower extremities, burns/corrosions, multiple, poisoning/toxic effects, complications and other/unspecified. Multiple injuries were defined as injuries to two or more body sites. The primary outcome measure was the length of stay (LOS) for injury-related hospitalizations, which was defined as short LOS (1–2 days) and long LOS (3 and more days). The geographical area of admission to the hospital was classified into two groups: capital and regions. This study was exempt from the requirement of informed consent owing to the retrospective study design. Data on all injuries are presented as absolute numbers and proportions. Data were reviewed in 2020.
Statistical data analyses was done using SPSS software version 23.0. Characteristics of the injured individual and the injury were examined. Differences in categorical variables were tested with chi-square tests of independence. Multiple logistic regression models were built with backward elimination to assess predictors of length of stay. The dependent variable was length of stay dichotomized into three days and less and more than three days. The full model included demographic and clinically important characteristics of patients, including injured region of the body and type of injury. Variables with p value <0,05 were retained in the final model. Statistical significance was considered for p < 0.05. The OR index was used to determine the relationship between variables. Effect estimates were presented for the model with the best fit, and results from the three significant models were also included.
Results
Study sample
During the period under study, a total of 25 103 injury related hospitalizations were identified. Males comprised 59% (14 798) and females comprised 41% (10 305) of patients, giving a male to female ratio of 1.4:1. The age of patients ranged from 18 to 108 years with a median and mode of 47 and 26 years, respectively. The modal age group was 25–44 years, accounting for 8654 (34%) patients; followed by 45–64 years, accounting for 6852 (27%) patients and 65+ years, accounting for 6477 (26%) patients. Chi-square test results show that males tended to be more injured than females.
Overall, 51% of hospitalizations in the sample occurred in Tbilisi, the capital. The most common mode of arrival to the hospital was by private/public transport (64%). One third of patients (33%) arrived via emergency medical service (EMS) ground ambulances. Patients transported by EMS were mostly 65 and more years old or over (35%). Unintentional injuries accounted for 86% of all hospital admissions for injuries, and they were predominant in all age groups. Intentional injury was reported in 2% of patients (assault and intentional self-harm), the most prevalent in the age groups 25–44 years and 45–44 years (54% and 21% respectively). Among injury-related hospitalized patients 379 deaths occurred and the in-hospital mortality proportion was 1,5% (Table 1).
Table 1.
Patients demographics according to age group
| Demographic characteristics | Age groups | |||||
|---|---|---|---|---|---|---|
| 18–24 | 25–44 | 45–64 | 65 + | Total: | p value | |
| N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Sex | ||||||
| Male | 2185(70) | 6322(73) | 4089(60) | 2202(34) | 14798(59) | < 0.001 |
| Female | 933(30) | 2333(27) | 2761(40) | 4277(66) | 10304(41) | |
| Area | ||||||
| Capital | 1755(56) | 4651(54) | 3298(48) | 3048(47) | 12752(51) | < 0.001 |
| Region | 1365(44) | 4001(46) | 3554(52) | 3431(53) | 12351(49) | |
| Mode of Arrival | ||||||
| Walk-in | 2025(65) | 5773(67) | 4381(64) | 3926(61) | 16105(64) | < 0.001 |
| Ambulance | 1017(33) | 2630(30) | 2282(33) | 2381(37) | 8310(33) | |
| Referral from a medical facility | 54(2) | 172(2) | 139(2) | 139(2) | 504(2) | |
| Unknown | 24(1) | 77(1) | 50(1) | 33(1) | 184(1) | |
| Intent | ||||||
| Unintentional | 2647(85) | 7206(83) | 5903(86) | 5832(91) | 21618(86) | < 0.001 |
| Assault | 45(1) | 145(2) | 57(1) | 18(0) | 265(1) | |
| Intentional self-harm | 46(1) | 124(1) | 62(1) | 26(0) | 258(1) | |
| Undetermined intent and other | 381(12) | 1179(14) | 830(12) | 571(9) | 2961(12) | |
| Outcome | ||||||
| Completed treatment | 2931(94) | 8029(93) | 6368(93) | 5945(92) | 23273(93) | < 0.001 |
| Referral | 118(4) | 383(4) | 287(4) | 247(4) | 1035(4) | |
| Death | 15(0) | 66(1) | 94(1) | 204(3) | 379(1) | |
| Discontinued treatment | 55(2) | 174(2) | 103(1) | 83(1) | 415(2) | |
Etiology of injury
Among all age groups, the predominant mechanism of injury was falls (n=13932, 55%), followed by exposure to mechanical forces (n=2701, 11%), poisoning (n=2733, 11%) and road traffic injuries (n=2556, 10%). Most cases of falls were among those 65+ years old (n=4821, 35%), followed by the group of 45–64 years old (n=3954, 28%) and the group of 25–44 years old (n=3785, 27%). Falls were also the predominant cause of injury among all age groups, reaching the highest proportion in the age group 65+ years (n=4821, 74%). Falls were the leading cause of injury-related hospitalizations both among women (n=6550, 64%) and among men (n=7382, 50%). The leading cause in fall-related hospitalization in all age categories was fall on same level.
Generally, the second through fifth leading mechanisms of injury were similar for all age groups and included road traffic injuries (RTI), poisoning, and exposure to mechanical forces, but the order of these mechanisms differed between the groups based on the age of hospitalized patients. Following falls, for patients 18 – 24 years old the next most frequent mechanisms for hospitalizations were road traffic injuries (n=487, 16%), poisoning (n=431, 14%) and exposure to mechanical forces (n=385, 12%); For patients 25 – 44 years old the order was poisoning (n=1289, 15%), exposure to mechanical forces (n=1215, 14%) and road traffic injuries (n=1069, 12%); and, for those aged 45 – 64 the order was exposure to mechanical forces (n=766, 11%), poisoning (n=688, 10%) and road traffic injuries (n=641, 9%). For the most elderly age group, 65 years of and above, the order was road traffic injuries (n=359, 6%), exposure to mechanical forces (n=335, 5%) and poisoning (n=325, 5%) for patients over 65 years old.
Patients hospitalized following transportation injuries were predominantly male, with a sex ratio of 1.87:1. Car occupants were the most affected by road traffic injuries, accounting for almost half (n=1050, 41%) of all road traffic accidents-related hospitalizations. This proportion was more than three times higher that of road traffic injuries among pedestrians (n=305, 12%). Most of the hospitalizations related to road traffic injuries occurred in the region compared to the capital (57% vs 43%).
Exposure to mechanical forces more commonly affected males than females, with a sex ratio of 3.6:1. The vast majority of cases (n=2295, 86%) were the impact of inanimate mechanical forces. 6% of exposure of inanimate mechanical forces were associated with sharp objects including a knife (n = 132) and 2% were due to a gunshot (n = 57). The majority of people harmed by sharp objects and gunshots were males (n=115, 87%; n=55, 96%). The most of sharp objects (n=59, 45%) and gunshot (n=35, 61%) injuries occurred in a 25–44 years age group. The proportion of poisoning-related hospitalization was higher in male, with a sex ratio of 1.7:1. Poisoning was most common in the age group 25–44 years (n=1289, 47%). Poisoning by drugs, medicaments and biological substances was the leading cause of poisoning associated hospitalizations in all age groups.
Injury characteristics
The head, lower extremities and upper extremities were the most common body regions injured accounted for 32% (n=8100), 23% (n=5804) and 16% (4026) of cases, respectively (Table 3). However, in male patients, the first most common injury location was the head (n=5049, 34%), followed by injuries to the upper extremities (n=2630, 18%) and lower extremities (n=2487, 17%). In females, the first most common injury location was the lower extremities (n=3317, 32%), followed by the head (n=3048, 30%) and upper extremities (n=1393, 14%). There were several differences between patient age groups patients regarding the injured body regions ratios. The proportion of head injuries was the highest in the youngest group and decreased with increasing age (18–24, 43%; 25–44, 36%; 45–64, 31%; 65+, 24%). However, the proportion of lower extremity injuries was the lowest in the oldest group of patients and increased with age up to age 65 (18–24, 8%; 25–44, 12%; 45–64, 22%; 65+, 46%). Fractures (n=8433, 34%) and intracranial injuries (n=7025, 28%) were the most common types of injuries, respectively. The third most common type of injury for both males (n=1521, 10%) and females (n=870, 8%) was toxic effects of substance chiefly nonmedicinal as to source (Table 2).
Table 3.
Death during hospitalization
| Death | Age groups | p value | |||
|---|---|---|---|---|---|
| 18–24 | 25–44 | 45–64 | 65 + | ||
| Sex | |||||
| Male | 13(0.6) | 57(0.9) | 76(1.9) | 105(4.8) | < 0.001 |
| Female | 2(0.2) | 9(0.4) | 18(0.7) | 99(2.3) | |
| Mechanism | |||||
| Transport accident (V01–V99) | 6(1.2) | 20(1.9) | 27(4.2) | 34(9.5) | < 0.001 |
| Fall (W00–W19) | 4(0.3) | 18(0.5) | 40(1.0) | 128(2.7) | |
| Exposure to mechanical forces (W20–W64) | 1(0.3) | 8(0.7) | 5(0.7) | 6(1.8) | |
| Poisoning (X40–X49; X60–X69; X85–X90; Y10–Y19) | 1(0.2) | 7(0.5) | 6(0.9) | 9(2.8) | |
| Fire/burn/radiation/air temperature and pressure (W85–W99; X00–X09; X10–X19; X76–X77; Y26) | 1(0.7) | 8(1.8) | 6(2.2) | 15(7.9) | |
| Other /unspecified (W65–W84; X20–X29; X30–X39; X50–X57; X91–X99; X58–X59; X84; Y34) | 2(0.9) | 5(1.3) | 10(3.4) | 12(4.7) | |
| Injured body region | |||||
| Head (S00–S09) | 5(0.4) | 16(0.5) | 38(1.8) | 64(4.1) | < 0.001 |
| Upper extremities (S40–S69) | 0(0) | 1(0.7) | 1(0.8) | 3(0.4) | |
| Lower extremities (S70–S99) | 0(0) | 2(0.2) | 2(0.1) | 57(1.9) | |
| Multiple (T00–T07) | 6(6.2) | 19(6.6) | 19(8.1) | 26(17.9) | |
| Abdomen and pelvis including lower back and genitals (S30–S39 | 1(1.0) | 3(1.0) | 4(1.9) | 9(9.5) | |
| Burns and corrosions (T20–T32) | 1(0.7) | 9(2.0) | 8(2.9) | 15(7.6) | |
| Thorax/neck (S10–S29) | 1(1.2) | 7(2.6) | 8(2.8) | 5(2.8) | |
| Other/unspecified (T66–T78) | 0(0.3) | 2(1.8) | 7(5.2) | 15(10.9) | |
| Mode of injury | |||||
| Intracranial injury | 5(0.4) | 14(0.5) | 35(1.9) | 61(4.4) | < 0.001 |
| Fracture | 0(0) | 5(0.3) | 6(0.3) | 67(1.8) | |
| Burns and corrosions | 1(0.7) | 9(2.0) | 8(2.9) | 15(7.6) | |
| Open wound | 1(0.7) | 3(0.6) | 1(0.4) | 0(0) | |
| Toxic effects/poisoning | 1(0.3) | 7(1.0) | 7(2.8) | 10(4.4) | |
| Injury muscles, tendons, blood vessels, nerves and spinal cord | 0(0) | 3(0.5) | 2(0.6) | 1(0.9) | |
| Internal organs | 1(1.2) | 3(1.2) | 7(3.9) | 11(10.7) | |
| Superficial injury | 0(0) | 1(0.6) | 2(2.3) | 3(4.1) | |
| Other/unspecified | 6(4.3) | 21(5.5) | 26(8.9) | 39(16.2) | |
| Total | 15(0.5) | 66(0.8) | 94(1.4) | 204(3.2) | |
Table 2.
Distribution of injury characteristics according to age group
| Injury characteristics | Age groups | ||||
|---|---|---|---|---|---|
| 18–24 | 25–44 | 45–64 | 65 + | p value | |
| n (%) | n (%) | n (%) | n (%) | ||
| Mechanism of injury | |||||
| Fall (W00–W19) | 1370 (44) | 3785(44) | 3954(58) | 4821 (74) | < 0.001 |
| on same level | 682(50) | 1852(49) | 2047(52) | 2714(56) | |
| from one level to another | 240(18) | 691(18) | 642(16) | 497(10) | |
| into water | 6(0) | 2(0) | 2(0) | 0(0) | |
| unspecified fall | 442(32) | 1240(33) | 1263(32) | 1610(33) | |
| Exposure to mechanical forces (W20–W64) | 386(12) | 1215(14) | 766(11) | 335(5) | |
| inanimate | 324(84) | 1022(84) | 661(86) | 292(87) | |
| animate | 62(16) | 193(16) | 105(14) | 43(13) | |
| Poisoning (X40–X49; X60–X69; X85–X90; Y10–Y19) | 431 (14) | 1289(15) | 688(10) | 325(5) | < 0.001 |
| by drugs, medicaments and biological substances | 282(65) | 755(59) | 418(61) | 238(73) | |
| by alcohol | 84(19) | 377(29) | 173(25) | 21(6) | |
| by chemicals and noxious substances | 65(15) | 157(12) | 97(14) | 66(20) | |
| Transport accident (V01–V99) | 487(16) | 1069(12) | 641(9) | 359(6) | < 0.001 |
| pedestrian | 44(9) | 99(9) | 95(15) | 67(19) | |
| pedal cyclist | 14(3) | 19(2) | 7(1) | 4(1) | |
| motorcycle, three-wheeled motor vehicle rider/occupant | 22(5) | 24(2) | 8(1) | 2(1) | |
| car occupant | 183(38) | 473(44) | 270(42) | 124(35) | |
| other land transport occupant | 43(9) | 125(12) | 85(13) | 58(16) | |
| other and unspecified transport | 181(37) | 329(31) | 176(27) | 104(29) | |
| Fire/burn/radiation/air temperature and pressure (W85–W99; X00–X09; X10–X19; X76–X77; Y26) | 154(5) | 447(5) | 269(4) | 191(3) | |
| Other specified (W65–W84; X20–X29; X30–X39; X50–X57; X91–X99) | 215(7) | 585(7) | 363(5) | 274(4) | |
| Unspecified (X58–X59; X84; Y34) | 77(2) | 262(3) | 171(2) | 172(3) | |
| Mode of injury | |||||
| Intracranial injury | 1141(37) | 2664(31) | 1850(27) | 1371(21) | < 0.001 |
| Fracture | 543(17) | 1837(21) | 2420(35) | 3633(56) | |
| Toxic effects of substance | 384(12) | 1147(13) | 605(9) | 256(4) | |
| Open wound | 151(5) | 456(5) | 263(4) | 143(2) | |
| Injury muscles, tendons, blood vessels, nerves and spinal cord | 226(7) | 641(7) | 354(5) | 112(2) | |
| Internal organs | 86(3) | 252(3) | 190(3) | 103(2) | |
| Burns and corrosions | 151(5) | 445(5) | 273(4) | 197(3) | |
| Poisoning | 113(4) | 322(4) | 141(2) | 97(1) | |
| Dislocation, sprain and strain of joint and ligaments | 94(3) | 174(2) | 152(2) | 110(2) | |
| Superficial injury | 61(2) | 171(2) | 88(1) | 73(1) | |
| Other/unspecified | 170(5) | 543(6) | 516(7) | 384(5) | |
| Injured body region | |||||
| Head (S00–S09) | 1336(43) | 3124(36) | 2103(31) | 1538(24) | < 0.001 |
| Upper extremities (S40–S69) | 516(17) | 1453(17) | 1277(19) | 780(12) | |
| Toxic effects of substances chiefly nonmedicinal as to source (T51–T65) | 384(12) | 1147(13) | 606(9) | 256(4) | |
| Lower extremities (S70–S99) | 265(8) | 1074(12) | 1490(22) | 2975(46) | |
| Multiple (T00–T07) | 96(3) | 287(3) | 234(3) | 145(2) | |
| Abdomen and pelvis including lower back and genitals (S30–S39) | 104(3) | 313(4) | 216(3) | 95(1) | |
| Burns and corrosions (T20–T32) | 151(5) | 445(5) | 273(4) | 197(3) | |
| Poisoning by, adverse effect of and underdosing of drugs, medicaments and biological substances (T36–T50) | 114(4) | 324(4) | 141(2) | 97(1) | |
| Thorax/neck (S10–S29) | 85(3) | 268(3) | 290(4) | 177(3) | |
| Other/unspecified (T66–T78) | 69(2) | 217(3) | 222(3) | 219(3) | |
| TOTAL | 3120(12) | 8652(34) | 6852(27) | 6479(26) | 25103 |
Single injuries occurred in 97% (n=24340) of patients while 3% (n=762) patients had multiple injury diagnoses. The main mechanism of multiple injuries was road traffic (n=366, 48%), followed by falls (n=287, 38%) and exposure to mechanical forces (n=56, 7%). The majority of multiple injuries (n=553, 73%) occurred in male patients. Multiple injuries were most common in the age group 25–44 years (n = 287, 38%).
Outcome
Among this patient sample with injuries severe enough to require hospital admission, 93% (n=23273) recovered and were released home, 4% (n=1035) were referred to another hospital or facility for follow-up care, 1.6% (n=415) discontinued treatment, and 1.5% (n=379) of patients died.
The large majority of reported referrals were received from the regions (93%) outside the capital Tbilisi. High proportion of patients transferred to other hospitals came from mountainous regions of the country: Racha (n=55, 95%), Samegrelo-Zemo Svaneti (n=716, 20%) and Samtskhe-Javakheti (n=465, 19%).
Intracranial injuries and fractures accounted for 45% of such referrals.
The main cause of fatal injury by mechanism was road traffic injury (n=87, 3.40%) followed by fire/burn (n=30, 2.83%) and fall (n=190, 1.36%). The highest death proportion from road traffic crashes occured in the age group 65 + years (n=34, 9.5%), followed by 45–64 years (n=27, 4.2%), 25–44 years (n=20, 1.9%) and 18–24 years (n=6, 1.2%). Unlike the majority of injuries, the majority of fatal road traffic injuries occurred outside in the capital in more rural regions (2.1% vs 1.3%). Motor vehicle occupants (n=36, 1.41%) ranked first amongst the fatal types, followed by pedestrians (n=20, 0.78%). A higher proportion of motor vehicle occupant injuries resulted in death in the non-capital regions (1.2% died) compared with those within the capital (0.28% died). In contrast, a higher proportion of pedestrian injuries resulted in death in the capital (0.58%) than the regions (0.28%).
The highest fire/burn and fall related death case fatalities were among those ages 65+ years (7.8% and 2.7%, respectively). Among all deaths, 9.19% (n=70) were due to multiple injuries, followed by burns and corrosions (n=33, 3.10%) and injuries of abdomen and pelvis including lower back and genitals (n=17, 2.34%). Most deaths were among the age group of 65+ years (n=204, 3.15%), followed by 45–64 years (n=94, 1.37%), 25–44 years (n=66, 0.76%), and 18–24 years (n=15, 0.48%). There were gender differences in hospital mortality. It was higher for males than for females in all age groups: 18–24 years (0.6% vs 0.2%), 25–44 years (0.9% vs 0.4%), 44–64 years (1.9% vs 0.7%) and 65 + years (4.8% vs 2.3%) (Table 3). About 26% of deaths occurred within 24 hours from arrival at a hospital, and about half of deaths (48%) occurred within the first five days of hospitalization (Figure 2).
Figure 2.
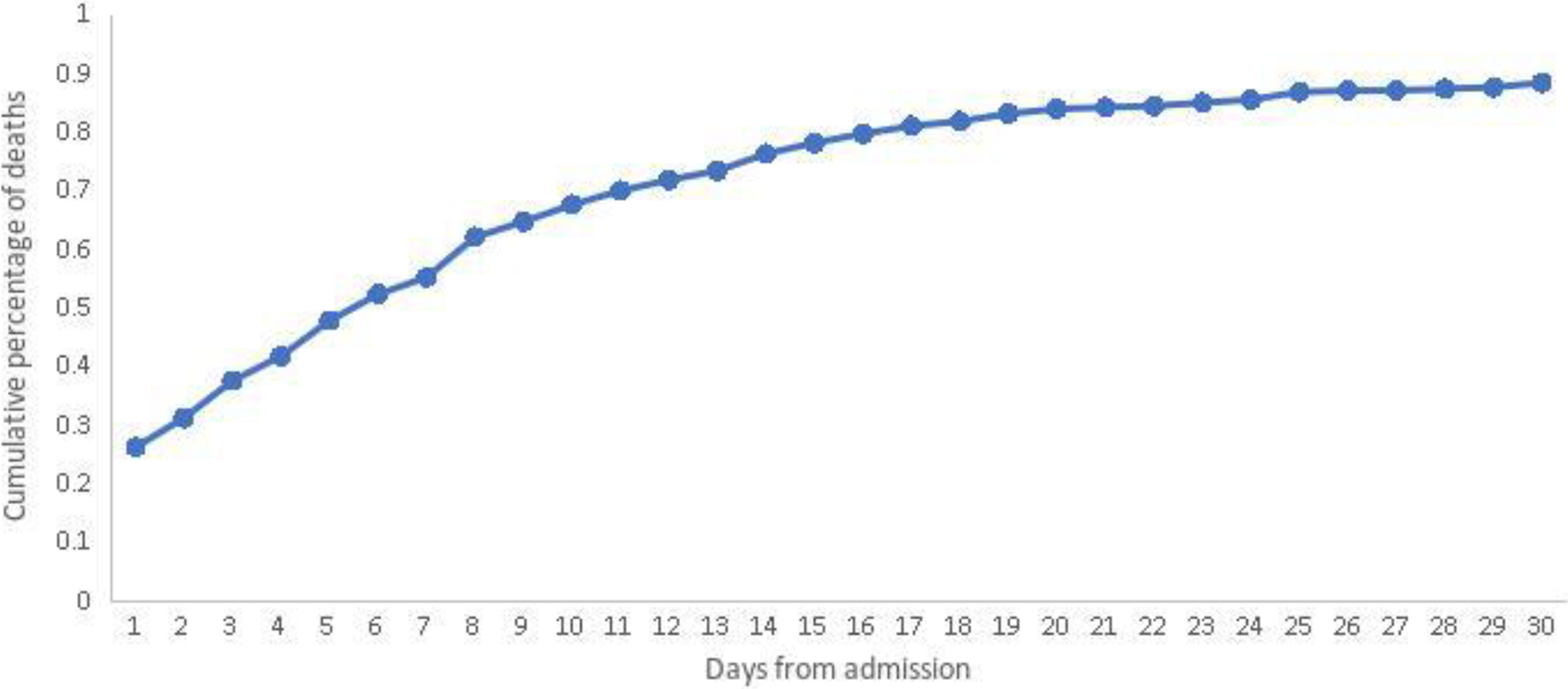
Cumulative distribution of death from hospital admission
The median LOS was 2 days, the modal length of stay one day, and the range was from 1 to 263 days. In general, 57% (n=14294) of all injured patients were treated in less than 3 days. The oldest age group (65+) made up the highest proportion of those staying three days or more (64%) compared with less than 3 days (36%). There were differences in the longer LOS between male and female depending on the age group. The duration of LOS in females increased with age (19% in age group 18–24 years, 20% in age group 25–44 years, 38% in age group 45–64 years and 68% in age group 65 + years) in contrast to male where it decreased with increasing age (81% in age group 18–24 years, 80% in age group 25–44 years, 62% in age group 45–64 years and 32% in age group 65 + years) (Figure 1).
Figure 1.
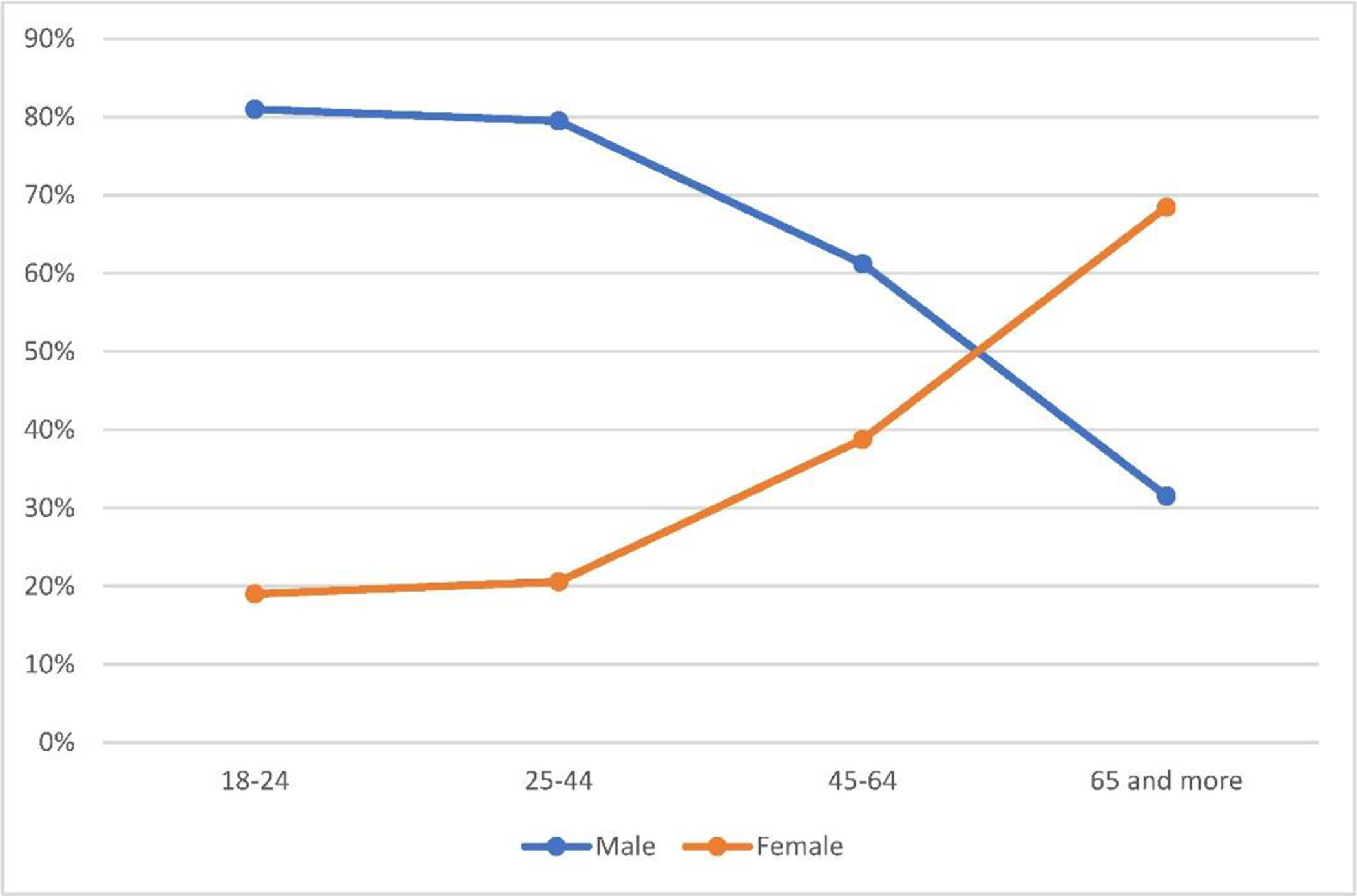
Distribution of longer LOS by gender and age group.
LOS was longer in fall-related patients (51% vs 49). Low extremities, abdomen/pelvis including lower back and genitals, thorax/neck and multiple injuries required the longer length of stay, with 76% vs 24%, 72% vs 28%, 66% vs 34% and 61% vs 39%, respectively. Fatal outcomes were twice as common in patients with longer LOS; 69% vs 31%). %). All gunshot-related and the majority of sharp objects-related injuries (89% vs 11%) required a long LOS. Moreover, the patients who were under surgical procedures were more prone to a longer LOS (66% vs 34%) (Table 4).
Table 4.
Length of stay (LOS) of injured patients
| Variables | Hospital length of stay (d) | OR (95% CI) | p value | |
|---|---|---|---|---|
| <3 (n=14932) | ≥3 (n=11404) | |||
| N (%) | N (%) | |||
| Age | ||||
| 18–24 | 2303(74) | 817(26) | 0.43(0.39 – 0.46) | <0.001 |
| 25–44 | 5887(68) | 2765(32) | 0.49(0.47 – 0.52) | |
| 45–64 | 3773(55) | 3079(45) | 1.11(1.05 – 1.18) | |
| 65+ | 2339(36) | 4140(64) | 3.18(3.0 – 3.37) | |
| Sex | ||||
| Male | 8722(59) | 6076(41) | 0.82(0.78 – 0.87) | <0.001 |
| Female | 5579(54) | 4725(46) | 1.22(1.16 – 1.28) | |
| Mechanism of injury | ||||
| Fall | 6883(49) | 7047(51) | 2.02 (1.92 −2.13) | <0.001 |
| Exposure to mechanical forces | 1774(66) | 928(34) | 0.66(0.61 – 0.72) | |
| Gunshot | 0 (0) | 57 (100) | - | |
| RTI* | 1331(52) | 1225(48) | 1.25(1.15 – 1.35) | |
| Poisoning | 2135(78) | 598(22) | 0.33(0.3 – 0.37) | |
| Fire/burn/radiation /air temperature and pressure | 731(69) | 330(31) | 0.58(0.51 – 0.67) | |
| Other specified | 998(69) | 439(31) | 0.61(0.55 – 0.68) | |
| Unspecified | 447(66) | 235(34) | 2.1(1.87 – 2.35) | |
| RTI | ||||
| Pedestrian | 127(42) | 178(58) | 1.61(1.26 – 2.05) | <0.001 |
| Car occupant | 594(57) | 456(43) | 0.74(0.63 – 0.86) | |
| Pedal cyclist | 26(59) | 18(41) | 0.75(0.41 – 1.37) | |
| Motorcycle rider/occupant of three-wheeled motor vehicle | 23(41) | 33(59) | 1.57(0.92 – 2.7) | |
| Occupant of bus, heavy transport vehicle, pick-up truck or van | 202(65) | 109(35) | 0.55(0.43 – 0.7) | |
| Other and unspecified transport accidents | 359(45) | 431(55) | 1.47(1.24 – 1.74) | |
| Type of injury | ||||
| Intracranial injury | 5201(74) | 1825(26) | 0.36(0.33 – 0.38) | <0.001 |
| Fracture | 2537(30) | 5896(70) | 5.57(5.26 – 5.9) | |
| Toxic effects | 1944(81) | 448(19) | 0.28(0.25 – 0.31) | |
| Open wound | 804(79) | 209(21) | 0.33(0.28 −0.39) | |
| Injury muscles, tendons, blood vessels, nerves and spinal cord | 852(64) | 481(36) | 0.74(0.66 – 0.83) | |
| Internal organs | 73(12) | 558(88) | 10.62(8.31 – 13.57 | |
| Burns and corrosions | 741(70) | 325(30) | 0.57(0.5 – 0.65) | |
| Poisoning | 451(67) | 222(33) | 0.64(0.55 – 0.76) | |
| Dislocation, sprain and strain of joint and ligaments | 427(81) | 103(19) | 0.31(0.25 – 0.39) | |
| Superficial injury | 340(87) | 53(13) | 0.20(0.15 – 0.27) | |
| Other/unspecified | 931(58) | 682(42) | 0.99(0.9 – 1.1) | |
| Injured body region | ||||
| Head | 5906(73) | 2195(27) | 0.36(0.34 – 0.38) | <0.001 |
| Upper extremities | 2561(64) | 1465(36) | 0.72(0.67 – 0.77) | |
| Toxic effects of substances chiefly nonmedicinal as to source | 1945(81) | 448(19) | 0.27(0.25 – 0.31) | |
| Lower extremities | 1367(24) | 4437(76) | 6.6(6.16 – 7.06) | |
| Multiple | 295(39) | 467(61) | 2.15(1.85 – 2.49) | |
| Abdomen and pelvis including lower back and genitals | 202(28) | 526(72) | 3.57(3.03 – 4.21) | |
| Thorax/neck | 279(34) | 541(66) | 2.7(2.33 – 3.13) | |
| Other/unspecified | 1292(72) | 501(28) | 0.61(0.57 – 0.67) | |
| Surgery | ||||
| Yes | 3412(36) | 6065(64) | 4.13(3.92 – 4.35) | <0.001 |
| No | 10887(70) | 4737(30) | 0.24(0.23 – 0.26) | |
| Outcome | ||||
| Alive | 14182(57) | 10541(43) | 0.34(0.27 – 0.42) | <0.001 |
| Death | 119(31) | 260(69) | 2.94(2.36 – 3.66) | |
RTI: Road traffic injury.
Multiple linear regression analysis with backward elimination was performed to assess the relationship between LOS as the dependent variable and other independent variables. The final model showed that statistically significant predictors LOS were age, gender, multiple injuries, injuries of abdomen and pelvis, of thorax/neck, of upper and lower extremities, burns, as well as fractures, internal organ and intracranial injuries (table 5, model 3). We further evaluated associations of injured body region and type of injury in separates models (Table 5, models 1 and 2). All of the above predictions proved to be statistically significant (Table 5).
Table 5.
Multiple linear regression analysis of predictors of length of stay
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β | t value | p value | β | t value | p value | β | t value | p value | |
| Age | 0.04 | 18.60 | <0.0001 | 0.04 | 18.90 | <0.0001 | 0.04 | 17.76 | <0.0001 |
| Gender | 0.65 | 7.69 | <0.0001 | 0.69 | 8.16 | <0.0001 | 0.70 | 8.39 | <0.0001 |
| Multiple injury | 5.09 | 22.36 | <0.0001 | 5.45 | 23.02 | <0.0001 | |||
| Abdomen and pelvis | 2.79 | 11.74 | <0.0001 | 1.80 | 6.15 | <0.0001 | |||
| Thorax/neck | 2.55 | 11.39 | <0.0001 | 1.83 | 7.05 | <0.0001 | |||
| Upper extremities | −0.40 | −3.55 | 0.0004 | −0.93 | −6.57 | <0.0001 | |||
| Lower extremities | 1.27 | 12.17 | <0.0001 | 0.41 | 2.72 | 0.007 | |||
| Burns | 2.19 | 10.94 | <0.0001 | 2.57 | 12.20 | <0.0001 | |||
| Fracture | 0.85 | 8.64 | <0.0001 | 1.55 | 12.46 | <0.0001 | |||
| Internal organ injury | 3.06 | 11.65 | <0.0001 | 1.95 | 5.91 | <0.0001 | |||
| Intracranial injury | −0.19 | −1.93 | 0.05 | 0.52 | 4.50 | <0.0001 | |||
| Model | R2=0.052, F=182.5, p<0.0001 | R2=0.028, F=150.5, p<0.0001 | R2=0.059, F=149.7, p<0.0001 | ||||||
Discussion
We examined all injury hospitalizations for the 2018 calendar year in Georgia. The results suggest that the majority of patients with injuries were men, and the greatest number of injuries was in the age group of 25–44 years old. The explanation for this predominance might be the types of exposures, behavioral factors, and environmental risks as they differ by age and gender. Identification of these specific causal factors was not possible in our study. The excess of injuries in males compared with females is described in previously published studies [14,15].
Most of the injuries were associated with falls, and their proportion among elderly patients was significantly higher than among other age groups. These results are in line with previous reports [16]. Elderly patients who suffered from falls had a longer length of stay as well as a higher case fatality proportion. These findings are consistent with previous literature and likely due to the functional impact of age on physical resilience, as well as comorbid conditions such as osteoporosis [(12,17)].
According to body region, the largest proportion of injuries were to the head. Scientific literature suggests that head injuries represent the most common cause of death and disability following trauma, especially in LMICs, and given their high death and disability propotions are an important priority for prevention [(18,19)]. As a cross sectional hospital based study in Nigeria suggests the similar findings to Georgia - 32% of all trauma deaths were attributable to severe head injury [18,20]. As well as findings of trauma care audit at a regional trauma center in South Africa shows that traumatic brain injuries were reason for 25% of hospital admissions [18,21].
Our data also underscore that a significant proportion of multiple injuries are associated with road traffic incidents. RTIs have been found to be the one of the most common cause of injury, following falls. The growing transportation infrastructure is the main contributor in the increasing number of fatalities from road traffic injuries in other LMICs as well [22]. Our research showed that more hospitalizations related to road traffic injuries occurred not in capital city but in the regions, that can be explained by the fact that many small towns and villages in Georgia are lack of safe road infrastructure and access to well-designed, modern roads [23].
In our study the sex ratio of RTI patients was 1.4:1, which was lower than ratios in China (1.61:1), Iran (2.2:1) and Romania (2:1) [24–26]. In current study a higher proportion of females was involved in RTIs as pedestrians and car occupants than as pedal cyclists and motorcycle riders. This is in line with findings of the early publication [27].
The findings from the current study indicated that the length of hospital stay significantly related on age, type of injury, mechanism of injury, and the performed surgical interventions. In our study, the multiple injury was determined by the most important independent predictor in the LOS model (β = 5.45). Our study found that hospitalizations associated with the lower extremities required longer LOS. The ratio of lower extremity injuries was almost twice as high in females compared to males (32% vs 17%). This may explain the longer LOS in women. Current research has found a significant relationship between older age and longer LOS which is consistent with the findings from other research that investigate factors affecting length of hospital stay among trauma patients [29]. We observed that patients who were under surgical interventions were more susceptible to stay in hospital for more than three days than those who did not undergo surgery. This is in agreement with other studies from developing countries [30–32]. In our study, survivors had a shorter LOS than those who did not survive, which is consistent with previous study in Canada but in contrast to studies from the developing countries [32–35]. The present study revealed that the LOS was higher in accidents involving pedestrians and motorcycles, compared with injuries in a car accident. Similar findings were reported in early studies in LMIC [30,35]. Moreover, LOS was found to be associated with gunshot and sharp objects, including knifes. These circumstances require future research to be focused on identifying gaps in our database.
In this study, 66% of recorded deaths were male patients, which agrees with previous studies describing that males are associated with an increased risk of death from injury [15,36–38]. The predominant age group was 65 + years (54%), similar results are shown in a previous study [24]. Intracranial injuries and fractures were responsible for majority of all deaths before discharge with 30% and 20% respectively. Brain injuries are also cited as the leading cause of death in other publications [38,39].
In the present study, the leading cause of injury-related deaths were RTIs, which is also observed in literature and previous studies [40]. Although road traffic deaths in Georgia have decreased by 13% since 2013, road safety remains a serious problem in the country [23]. In our study fire/burns were the second cause of fatal injuries. Which is in line with earlier study from LMIC [41]. The analysis of the study showed that future research and prevention should focus on injuries associated with RTIs and burns.
In Georgia prehospital triage and mobilization of emergency services is provided by the Emergency Response Center, which the public has access to through the nationwide number “112”. Calls to 112 service are free of charge from all fixed line and mobile networks. Emergency medical service is also free in the country [42]. Despite these circumstances in presents study majority were walk-in patients. There are several possible explanations why the less patients used Ambulance. First, injured people often practice self-medication because they do not take the injury seriously. Secondly, injured patients incorrectly assess their own state of health and need to visit a family doctor or get primary medical service in general.
Our research showed that the majority of referrals came from regions outside the capital Tbilisi. This can be explained by the fact that the health-care system of Georgia is characterized by an uneven geographical distribution of the health-care workforce. Many rural residents of Georgia have limited access to high quality health care. Most rural patients seek care at regional hospitals which often lack medical resource, creating a need for referral to tertiary hospitals. Although there is a large number of trained doctors and trauma care hospitals in the country, they are mainly concentrated in large cities. Therefore, further studies are needed to assess the overall picture of referral system in the country (42)(43). Therefore, further studies are needed to assess the overall picture of referral system in the country. The current study showed that standard national official databases are probably the best source for broad epidemiological studies of injury prevalence and incidence, and for monitoring trends. But it only contains information such as age, sex, type of injury, mechanism of injury, length of hospital stay, intent of injury, outcome, and does not contain information about injury severity, admission time, pre-hospital care, ED Assessment and Vital Signs. Thus, the current existent databases are incomplete sources of injury surveillance data, risk prediction, and health care quality assessment. Injury registers may be more useful in identifying populations at risk, implementing and evaluating prevention programs.
Strengths and Limitations
This is one of the most comprehensive study of traumatic injuries hospitalized in Georgia. We used standard coding mechanisms, so our data is comparable to similar reports from around the world. The results of our study can provide answers to the questions “who”, “when” and “which” receive injuries requiring inpatient treatment, but cannot answer in detail the questions “where”, “how” the injuries were received. These data are not sufficient evidence for planning effective prevention programs but can be helpful in prioritizing prevention approaches. Our study data contained limited information about what exactly caused the particular injury, under what circumstances it occurred, and what accompanying factors caused it. The database includes only hospitalization cases, so we do not know mortality proportion for patients before their admissions to hospitals. In other words, standardly recorded data provide insufficient information on factors whose elimination or change in action can prevent the occurrence of new injuries. This situation allows plan the work of the medical service, but does not allow the development of prevention programs.
One of the limitations of this study is that the multivariate model did not include injury scores such as AIS or ISS. Furthermore, the database does not provide information for assessment of a burden on the intensive care unit.
In Georgia, according to the international and national standards, the registration of injury data are implemented by several agencies: National Statistics Office of Georgia, LEPL of Ministry of Internally Displaced Persons from the Occupied Territories, Labour, Health and Social Affairs of Georgia – National Center for Disease Control and Public Health of Georgia, Ministry of Internal Affairs of Georgia. Statistical data of deaths caused by injury are reported by three different state departments, and these vary significantly [7]. Cases of death caused by injury are recorded in three databases separately and the numbers are never compared. Besides, these cases can be wrongly coded according to different morbidity, so it is very difficult to evaluate the real cases of death caused by injury. These findings represent the most accurate reporting of hospitalizations in Georgia.
Conclusions
Despite these limitations, the findings from our study provide baseline information about traumatic injury hospitalizations in Georgia. Our findings will be helpful to create a better understanding of the scope of the injuries and outcomes that are associated with traumatic injury hospitalizations so that intervention strategies can be developed to improve the quality of care and to direct an effort to prevent future injuries.
Highlights.
This is one of the first study to report injury epidemiology in Georgia.
The retrospective study includes injured patients of aged 18 and above admitted to all private and public hospitals in the country.
The length of hospital stay significantly related on age, type of injury, mechanism of injury, and the performed surgical interventions.
Acknowledgments
The work reported in this publication was funded by the NIH-Fogarty International Trauma Training Program iCREATE: Increasing Capacity for Research in Eastern Europe and INITIatE: International Collaboration to Increase Traumatic Brain Injury in Europe, both at the University of Iowa and the Cluj School of Public Health (National Institutes of Health, Fogarty International Center 2D43TW007261 and 5R21NS098850).
Abbreviations
- LMICs
Low and middle income countries
- NCDC
National Center for Disease Control and Public Health of Georgia
- LOS
Hospital length of stay
- SPSS
Statistical package for social sciences
- EMS
Emergency medical service
- RTI
Road traffic injury
- NIH
National Institutes of Health
- INITIatE
International Collaboration to Increase Traumatic Brain Injury Surveillance in Europe
- iCREATE
Increasing Capacity for Research in Eastern Europe
- WHO
World Health Organization
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Competing Interest
The authors report no conflicts of interest in this work.
Ethics and Consent Statements
The Georgian National Centre for Disease Control and Public Health Institutional Review Board approved the study protocol (IRB # 2018–04914.12.2018) in accordance with Georgian legislation and the ethical standards as stated in the Declaration of Helsinki. There is no Institutional Review Board at Tbilisi State University (TSU). The NCDC is a training base for TSU, Department of Public Health, and the consent for ongoing research is usually obtained from the NCDC Institutional Review Board. The NCDC Institutional Review Board was convinced by the protocol that the study has no risk to the study participants and approved observational research using NCDC database without requiring prior written consent, which is in line with “International Ethical Guidelines for Epidemiological Studies” prepared by the Council for International Organizations of Medical Sciences (CIOMS) in collaboration with the World Health Organization (WHO) CIOMS Geneva February 2008. The database did not allow identification of patients - it did not include personal information (name, surname, identification number, or details that could identify a person).
References
- 1.Hofman K, Primack A, Keusch G, Hrynkow S. Addressing the growing burden of trauma and injury in low- and middle-income countries. Am J Public Health. 2005;95(1):13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peden M (WHO). THE INJURY CHART BOOK A graphical overview of the global burden of injuries Department of Injuries and Violence Prevention Noncommunicable Diseases and Mental Health Cluster World Health Organization. Int Classif. 2002; [Google Scholar]
- 3.Organization WH. INJURIES VIOLENCE THE FACTS The magnitude and causes of injuries. 2014;20. [Google Scholar]
- 4.Rowe. 基因的改变NIH Public Access. Bone. 2008;23(1):1–7. [Google Scholar]
- 5.Boniface R, Museru L, Kiloloma O, Munthali V. Factors associated with road traffic injuries in Tanzania. Pan Afr Med J. 2016;23:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. Global Status Report. Glob Status Rep Road Saf. 2009;
- 7.National Center For Disease Control and Public Health Georgia. National Strategy for Prevention and Control of Injury and Violence (in Georgian). 2013.
- 8.Wisborg T, Montshiwa TR, Mock C. Trauma research in low- and middle-income countries is urgently needed to strengthen the chain of survival. Scand J Trauma Resusc Emerg Med. 2011;19(October). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Statistics Office of Georgia. Demographic Situation in Georgia. 2018;138. [Google Scholar]
- 10.Yearbook S, Office NS, Str TD, Tel G. Tbilisi, 0180, saqarTvelo. [Google Scholar]
- 11.Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand. 2012;7(1):18–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehrpour SR, Nabian MH, Zanjani LO, Foroughmand-Araabi MH, Kamrani RS. Descriptive epidemiology of traumatic injuries in 18890 adults: A 5-year-study in a tertiary trauma center in Iran. Asian J Sports Med. 2015;6(1):4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. ICD-10: International Statistical Classification od Diseases and Related Health Problems. Radiol Manage. 2011;33(3):26.21793458 [Google Scholar]
- 14.Chandran A, Hyder AA, Peek-Asa C. The global burden of unintentional injuries and an agenda for progress. Epidemiol Rev. 2010;32(1):110–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharif-Alhoseini M, Zafarghandi M, Rahimi-Movaghar V, Heidari Z, Naghdi K, Bahrami S, et al. National trauma registry of Iran: A pilot phase at a Major Trauma Center in Tehran. Arch Iran Med. 2019;22(6):286–92. [PubMed] [Google Scholar]
- 16.Krieg H, Eller T, Kies L. Verbreitung und Ökologie der Vaucheria-Arten (Tribophyceae) des Elbe-Ästuars und der angrenzenden Küste. Helgoländer Meeresuntersuchungen. 1988;42(3–4):613–36. [Google Scholar]
- 17.Marinho BCG, Guerra LP, Drummond JB, Silva BC, Soares MMS. O ônus da osteoporose no Brasil. Arq Bras Endocrinol Metabol. 2014;58(5):434–43. [DOI] [PubMed] [Google Scholar]
- 18.Qureshi JS, Ohm R, Rajala H, Mabedi C, Sadr-Azodi O, Andrén-Sandberg Å, et al. Head injury triage in a sub Saharan African urban population. Int J Surg. 2013;11(3):265–9. [DOI] [PubMed] [Google Scholar]
- 19.Rubiano AM, Carney N, Chesnut R, Puyana JC. Global neurotrauma research challenges and opportunities. Nature. 2015;527(7578):S193–7. [DOI] [PubMed] [Google Scholar]
- 20.Solagberu BA. Spinal cord injuries in Ilorin, Nigeria. Vol. 21, West African journal of medicine. 2002. p. 230–2. [DOI] [PubMed] [Google Scholar]
- 21.Alexander T, Ch MBB. traumatic brain injury at a busy regional hospital in South Africa. Sajs. 2009;47(4):9–14. [PubMed] [Google Scholar]
- 22.Reich MR, Nantulya VM. The neglected epidemic: road traffic injuries in developing countries. (Education and debate). Br Med J. 2002;324(7346):1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nations U, Commission E, Africa FOR, Nations U, Commission E, Europe FOR. UNITED NATIONS ECONOMIC COMMISSION FOR AFRICA Road Safety Performance Review Georgia [Internet]. Layout and Printing at United Nations. 2018. Available from: http://www.unece.org [Google Scholar]
- 24.Zhang M, Guo M, Guo X, Gao L, Zhou J, Bai X, et al. Unintentional injuries: A profile of hospitalization and risk factors for in-hospital mortality in Beijing, China. Injury. 2019;50(3):663–70. [DOI] [PubMed] [Google Scholar]
- 25.Yadollahi M, Ghiassee A, Anvar M, Ghaem H, Farahmand M. Analysis of Shahid Rajaee hospital administrative data on injuries resulting from car accidents in Shiraz, Iran: 2011–2014 data. Chinese J Traumatol - English Ed [Internet]. 2017;20(1):27–33. Available from: 10.1016/j.cjtee.2015.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hatieganu PI, Sciences C, Prevention I, City I. and 2010. 2017;16(8):835–41. [Google Scholar]
- 27.Reith G, Lefering R, Wafaisade A, Hensel KO, Paffrath T, Bouillon B, et al. Injury pattern, outcome and characteristics of severely injured pedestrian. Scand J Trauma Resusc Emerg Med [Internet]. 2015;23(1):12–4. Available from: 10.1186/s13049-015-0137-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwarz C, Vallance M. Length of stay. Hosp Community Psychiatry. 1987;38(2):201. [DOI] [PubMed] [Google Scholar]
- 29.Kashkooe A, Yadollahi M, Pazhuheian F. What factors affect length of hospital stay among trauma patients? A single-center study, Southwestern Iran. Chinese J Traumatol - English Ed [Internet]. 2020;23(3):176–80. Available from: 10.1016/j.cjtee.2020.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mbanjumucyo G, George N, Kearney A, Karim N, Aluisio AR, Mutabazi Z, et al. Épidémiologie des blessures et leurs résultats chez les patients souffrant de traumatismes bénéficiant d’une prise en charge préhospitalière dans un hôpital universitaire tertiaire à Kigali, Rwanda. African J Emerg Med [Internet]. 2016;6(4):191–7. Available from: 10.1016/j.afjem.2016.10.001 [DOI] [Google Scholar]
- 31.C PL, G JM, D RM, M MD, M M, M JB, et al. Trauma admissions to the intensive care unit at a reference hospital in Northwestern Tanzania. Scand J Trauma Resusc Emerg Med [Internet]. 2011;19:61. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L560026476%5Cnhttp://dy3uq8jh2v.search.serialssolutions.com?sid=EMBASE&issn=17577241&id=doi:&atitle=Trauma+admissions+to+the+intensive+care+unit+at+a+reference+hospital+in+Northweste [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Byrick RJ, Caskennette GM. Audit of critical care: aims, uses, costs and limitations of a Canadian system. Can J Anaesth. 1992;39(3):260–9. [DOI] [PubMed] [Google Scholar]
- 33.Adenekan A, Faponle A. Trauma admissions to the ICU of a tertiary hospital in a low resource setting. African J Anaesth Intensive Care. 2010;9(2):5–9. [Google Scholar]
- 34.H-B H, S S, B L, Y MH, H M. Factors affecting hospital length of stay and hospital charges associated with road traffic-related injuries in Iran. BMC Health Serv Res [Internet]. 2013;13:281. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed11&NEWS=N&AN=23875993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Evans JA, van Wessem KJP, McDougall D, Lee KA, Lyons T, Balogh ZJ. Epidemiology of Traumatic Deaths: Comprehensive Population-Based Assessment. World J Surg [Internet]. 2009;34(1):158. Available from: 10.1007/s00268-009-0266-1 [DOI] [PubMed] [Google Scholar]
- 36.Liu T, Xie J, Yang F, Chen J, Li Z, Yi C, et al. The influence of sex on outcomes in trauma patients: a meta-analysis. Am J Surg. 2015. Nov;210(5):911–21. [DOI] [PubMed] [Google Scholar]
- 37.Trajano AD, Pereira BM, Fraga GP. Epidemiology of in-hospital trauma deaths in a Brazilian university hospital. BMC Emerg Med. 2014;14(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: An overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma - Inj Infect Crit Care. 2006;60(6 SUPPL.):3–11. [DOI] [PubMed] [Google Scholar]
- 39.Alexandrescu R, O’Brien SJ, Lecky FE. A review of injury epidemiology in the UK and Europe: Some methodological considerations in constructing rates. BMC Public Health. 2009;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akbari ME, Naghavi M, Soori H. Epidemiology of deaths from. 2006;12:382–90. [PubMed] [Google Scholar]
- 41.Burkadze E, Chikhladze N, Lobzhanidze G, Chkhaberidze N. Brain injuries: health care capacity and policy in Georgia. J Inj Violence Res. 2021;13(1):55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.FAO. Gender, agriculture and rural development in georgia. 2018. 86 p. [Google Scholar]
- 43.Rukhadze T An overview of the health care system in Georgia: expert recommendations in the context of predictive, preventive and personalised medicine. EPMA J. 2013;4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]


