Abstract
Objectives
Despite increases in global health actors and funding levels, health inequities persist. We empirically tested whether global health governance (GHG) operates under the rational actor model (RAM) and characterised GHG power dynamics.
Design
We collected approximately 75 000 tweets of 20 key global health actors, between 2016 and 2020, using Twitter API. We generated priorities from tweets collected using topic modelling. Priorities from tweets were compared with stated priorities from content analyses of policy documents and with revealed priorities from network analyses of development assistance for health funding data. Comparing priorities derived from Twitter, policy documents and funding data, we can test whether GHG operates under RAM and characterise power dynamics in GHG.
Participants
20 global health actors were identified based on a consensus of three peer-reviewed articles mapping global health networks. All tweets of each actor were collected in 3-month intervals from November 2016 to May 2020. Policy documents and developmental assistance for health (DAH) financial data for each actor were collected for the same period.
Results
We find all 20 actors and the global health system collectively fulfil the three conditions of RAM based on stated and revealed priorities. We also find compulsory and institutional power asymmetries in GHG. Funding organisations have compulsory power over channels of DAH and implementing institutions they directly fund. Funding organisations also have transitive influence over implementing institutions receiving DAH funding.
Conclusions
We find that there is a correlation between the priorities of large funders and the priorities of health actors. This correlation in conjunction with GHG operating under the RAM and the asymmetric power held by funders raises issues. GHG under the RAM grants large funders majority of the power to determine global health priorities and ultimately influencing outcomes while implementing organisations, especially those that work closest with populations, have little to limited influence in priority-setting.
Keywords: Health policy, international health services, public health, information technology, rationing
Strengths and limitations of this study.
This study uses an alternative methodology of using Twitter data in understanding global health governance and priority setting.
This study triangulates findings from multiple data sources to test the rational actor model and to characterise power asymmetries in global health governance.
Because the scope of this study is from 2016 to 2020, the findings may not be fully representative of global health governance during the COVID-19 pandemic.
Only the key 20 actors of the hundreds of global health actors today were included in the study.
Introduction
The turn of the 21st century introduced an unprecedented volume of new public and private actors in global health accompanied by stratospheric levels of funding.1 While some argue that this multiplicity of new actors promotes cooperation, what persists is a politically fragmented network of actors with competing priorities and preferences.2–4 Academics studying the complex network of global health actors have described it as a ‘congested’ and ‘chaotic’ network that causes inefficiencies in the practice and delivery of global health programmes and aid.5
Inequities in global health have increasingly been attributed to the actions of transnational actors with varying degrees of power and divergent interests.6 While more actors have entered global health with ostensible benevolent purposes, health inequities and inefficiencies in delivery still exist today. Fierce competition among donor priorities and requirements overwhelms the institutional capacities of recipient countries,7 8 disrupts national health planning,9 delays the delivery of aid10 and creates duplications and resource waste.11 12 Paradoxically, despite the exponential increases in global health actors and funding, preventable global health inequities have persisted.
Researchers have presented at least two arguments attempting to understand this paradox through the lens of economics, politics and power. First, global health governance (GHG) has been theorised as operating under the rational actor model (RAM) where ‘each actor has its own set of goals and objectives, and these actors take actions based on analysis of the costs and benefits of various available options’.13 Under RAM, each actor acts on their own set of explicit and implicit goals. Explicit goals come in the form of mission statements, bylaws and other founding documents. Implicit goals are priorities revealed from past decisions and behaviours. It is theorised that under RAM, prioritisation in GHG is based on the aggregation of individual explicit and implicit objectives.
Second, the Lancet-University of Oslo Commission on Global Governance for Health (2014) argues that ‘power asymmetry and global social norms limit the range of choice and constrain action on health inequity’.6 The actions of powerful global health actors in pursuit of their own interests ‘are not designed to harm health but can have negative side effects’ that may have contributed to the persistence of inequities.6 The lack of power of global health beneficiaries and smaller health actors, and the outsized wielded power of large global health funders may also have contributed to the slow rate of reduction in global health inequities.
The argument that GHG operates under the RAM and the Commission on Global Governance for Health’s argument about power asymmetry are mainly theoretical ideas about the behaviours of global health actors founded on a collection of studies within specific nations and regions or global and domestic institutions. What is necessary is empirical evidence at the global level that can confirm, deny or recharacterise these characterisations of how global health currently operates. Empirical evidence at the global level addresses doubts of how decisions are currently made in global health and can guide GHG towards addressing the world’s inequities in health.
We aim to empirically test the following research questions at the global level: (1) does GHG operate under the RAM? and (2) how can we characterise power dynamics in GHG?
We hypothesise that GHG operates under RAM and that there are power asymmetries in GHG that limit the range of health priorities. We analysed empirical evidence from Twitter, funding data and policy documents at the global level to test whether GHG operates under RAM and to characterise the power dynamics in GHG.
Methods
We test if GHG operates under the RAM and characterise the power dynamics in GHG through the lens of global health priority setting. All global health actors have certain preferences for health issues and act in alignment with these priorities.
Priorities can either be stated or revealed. Stated priorities are those preferences explicitly stated in a health actor’s founding documents, websites and annual reports. The mission statements and the health areas each actor explicitly mention in their official documents and websites are stated priorities. Revealed priorities are preferences that are gleaned from records of past behaviours and choices. Past health funding allocations and accounts of implemented programmes and policies are revealed priorities. Revealed priorities may or may not be aligned with stated priorities.
We use evidence for both stated and revealed priorities from 2016 to 2020 to test our research questions.
Study sample
We identified 20 key global health actors based on a consensus among three past studies that mapped the global health network using quantitative and qualitative methodologies.4 14 15 As shown in table 1, the key global health actors were categorised based on their nature of work in global health. Global health actors were either funding organisations, channels of developmental assistance for health (DAH) or implementing institutions. While most actors fall into multiple categories in practice, for the integrity of this analysis, organisations were limited to only one category based on the nature of their main line of work.
Table 1.
Summary of global health actors
| Nature of work in global health |
Organisational category | Twitter username | Global health actor | Number of Twitter followers (as of October 2021) |
| Channels of developmental assistance for health | Global Health Initiative | gavi | Gavi, the Vaccine Alliance | 153 000 |
| UNITAID | Unitaid | 17 200 | ||
| GlobalFund | Global Fund to Fight AIDS, Tuberculosis and Malaria | 240 100 | ||
| Multilateral Development Bank | WorldBank | World Bank | 3 500 000 | |
| United Nations System | WHO | WHO | 10 000 000 | |
| UNAIDS | Joint United Nations Programme on HIV/AIDS (UNAIDS) | 286 800 | ||
| UNFPA | United Nations Population Fund (UNFPA) | 260 800 | ||
| UNICEF | United Nations Children’s Fund (UNICEF) | 8 900 000 | ||
| Funding organisations | National Government | USAID | United States Agency for International Development (USAID) | 843 200 |
| DFID_UK* | United Kingdom Department for International Development (UK DFID)* | 1 000 000 | ||
| Philanthropic Organization | gatesfoundation | Bill and Melinda Gates Foundation | 2 100 000 | |
| Implementing institutions | Global CSO/NGO | MSF | Doctors Without Borders (MSF) | 165 100 |
| PATHtweets | PATH | 59 500 | ||
| SavetheChildren | Save the Children | 2 700 000 | ||
| Oxfam | Oxfam International | 836 300 | ||
| United Nations System | FAO | Food and Agriculture Organization (FAO) | 469 600 | |
| UNDP | United Nations Development Programme (UNDP) | 1 600 000 | ||
| National Government | CDCgov | Centers for Disease Control and Prevention (CDC) | 4 300 000 | |
| ECDC_EU | European Centre for Disease Prevention and Control (ECDC) | 90 600 | ||
| NIH | National Institutes of Health (NIH) | 1 400 000 |
Characteristics of the 20 global health actors analysed in this study.
*UK DFID is now the Foreign, Commonwealth and Development Office. During the time of the analysis, the UK’s agency for aid was known as DFID.
Patient and public involvement
Patients and the public were not involved in the development of the research questions and outcome measures.
Data sources
We analyse stated and revealed priorities of 20 key global health actors from three data sources—policy documents, DAH funding data and tweets. Table 2 summarises each data source, how they were collected, how they were analysed and what types of priorities can be derived.
Table 2.
Summary of data source, collection and analysis
| Data source | Data collection | Analysis | Type of priorities derived from source |
| Policy Documents | Manual collection of annual reports, policy documents and official communications from official websites of each global health actor | Manual content analysis | Stated |
| DAH Funding Data | Queried funding allocation data of each global health actor from the International Health Metrics and Evaluation (IHME) DAH Database | Descriptive statistics; network analysis | Revealed |
| Twitter Data | Collected all the tweets of each global health actor from November 2016 to May 2020 in 3 month intervals using the Twitter API | Natural language processing (topic modelling); network analysis | Revealed |
Description of how data are collected and analysed in the study.
DAH, developmental assistance for health.
Drawing stated priorities from policy documents
Stated priorities are obtained from a manual content analysis of policy documents, annual reports and official websites of global health actors.
Available policy documents, annual reports and relevant official communications from the websites of each global health actor between 2016 and 2020 were collected. Manual content analysis was conducted to evaluate the available policy documents for each global health actor and identify their respective stated priorities.
The stated priorities drawn from these documents were commonly obtained from official statements that fall under the following headings: ‘strategic priorities’, ‘programme priorities’, ‘strategic objectives’, ‘focus areas’, ‘strategic work areas’, ‘programme focus’, ‘Strategy 20XX-20XX’, ‘strategic goals’, ‘priority areas’, among others (online supplemental table S1 contains the stated priorities obtained from each actor).
bmjopen-2021-054470supp001.pdf (279.9KB, pdf)
Deriving revealed priorities from funding data
The first of two ways we derive revealed priorities is by using a network analysis and descriptive statistics of financial flows in DAH funding data.
Data from the Institute for Health Metrics and Evaluation’s (IHME) Developmental Assistance for Health Database were collected for 2019.16 The database includes approximately 800 000 transactions of health financing from funding organisations to channels of DAH and to implementing countries.
Descriptive statistics were conducted to determine the allocations of funding for each health area and geographic region for the 20 global health actors in 2019.
Network analysis is an analytic method that has proved to be useful in understanding relational dynamics across actors in global and public health.17 18 Network analysis was conducted to observe the funding relationships between global health actors. Gephi V.0.9.2 was used in constructing and analysing the network map. The network modelled in the study allows for a visualisation of the flows of global health funding in 2019. In the network map, nodes represent global health actors and lines or ‘edges’ indicate a flow of funding in global health. The Fruchterman-Reingold algorithm was used in modelling the network map. The algorithm ‘calculates the optimal layout so that nodes with less strength and less connections are placed further apart, and those with more and/or stronger connections are placed closer to each other’.19 The thickness of edges represents the amount of funding transferred between actors. The modelled network is discussed in the findings section.
Twitter data
The second way we derive revealed priorities is by using topic modelling in natural language processing (NLP) and conducting a network analysis of the global health actors’ tweets.
Using the Twitter API, we collected all the tweets of each global health actor by username from November 2016 to May 2020 in 3 month intervals. This means that all the tweets of each global health actor were collected for each day in the months of February, May, August, and November for each year. An interval of 3 months was decided for two reasons. First, a variation in the issues, topics, and themes that global health actors’ tweet can be observed in 3 month intervals. Initial small sample testing indicates that collecting all the tweets of every month for each actor yields redundancy in issues and topics observed. Redundancy is eliminated in 3 month intervals. Second, it also allows for efficient usage of the data request limits of the Twitter API. As Twitter limits the number of tweets one can collect from the Twitter API, this interval is an efficient way of collecting data for the timeframe. A total of 74 241 tweets were collected from 2016 to 2020 for the 20 global health actors. Online supplemental tables S2 and S3 describe the tweets collected.
bmjopen-2021-054470supp002.pdf (15.8KB, pdf)
bmjopen-2021-054470supp003.pdf (23.4KB, pdf)
Using Twitter as a data source plays an important role in analysing GHG. In the academic area of communications studies, researchers suggest that there are two forms of utility that motivate actors to post content on Twitter. First, intrinsic utility assumes that a user receives inherent satisfaction from posting content on Twitter.20 While global health actors do not necessarily receive the same “inherent satisfaction” as individual Twitter users, global health actors acquire more intrinsic utility as their communications reach a greater number of users. Second, image-related utility assumes that the perceptions of others,21 22 and seeking status are strong motivators for posting content.23 24 As global health actors operate best with high public approval, posting content on Twitter can improve public perception. Twitter is the ideal platform for global health actors to simultaneously share their work to a greater number of individuals and to improve their public perception.
Because Twitter limits each post to 280 characters, the platform promotes short, frequent, and straightforward manners of communication. The tweets of global health actors are regular ways of communicating their work, preferences, and priorities to the public.25–28 The tweets of global health actors act as an archive, a record of historical preferences, priorities, goals, and implemented programmes.29
We consider tweets equally to funding data as they both reveal priorities through documentation of past decisions, preferences, and goals. Funding data is a record of priorities in the form of financial flows and transactions towards certain global health issues. Twitter is a record of priorities in the form of programmes, policies, and opinions deemed important and necessary to communicate with the world. Because of their archival nature, both funding data and tweets reveal priorities through complementing records of decisions.
While tweets can represent both stated and revealed priorities, for this study, we use tweets to represent revealed priorities. Since this study analyses tweets in aggregation, our findings reveal the top themes discussed by each actor from 2016 to 2020. We do not analyse each tweet at an individual level, tweets are considered revealed priorities and not stated priorities.
Obtaining revealed priorities from Twitter data
NLP is a subfield in artificial intelligence, computer science, and linguistics at the intersection of the human language and computers. NLP uses computers to process and analyse large quantities of human language data. We use NLP to analyse the tweets of the global health actors for two reasons. First, NLP allows for the efficient analysis of tens of thousands of rows of text data that could not be done manually.30–32 Second, NLP allows for topic modelling, an algorithm that generates lists of words frequently used together.33–35 These lists of words correspond to themes, topics, or issues that can be used to identify the top 10 priorities of each global health actor. The results are then used in a network analysis that visualises where actors converge or diverge in global health priorities.
As seen in table 3, ten topics were generated using the Latent Dirichlet Allocation (LDA) topic model for each global health actor’s tweets to reveal their priorities from 2016 to 2020. LDA is a generative probabilistic modelling method where words in a corpus of text that are frequently used together are categorised into topics.36 This follows the assumption that documents, or in this case Twitter profiles, can be broken down into multiple topics that are identified by certain combinations of words.
Table 3.
Revealed priorities from Twitter topic modelling
| United States | United Kingdom | Gates Foundation | WHO | World Bank | UNAIDS | UNFPA | UNICEF | Unitaid | Gavi |
| Africa | Africa | Africa | Africa | Africa | Access | Africa | Africa | Access | Africa |
| Children | Agriculture | Breastfeeding | Breastfeeding | Agriculture | Africa | Child Marriage | Breastfeeding | Cancer | Cancer |
| Education | Children | Children | Children | Children | Discrimination | Children | Children | Children | Children |
| Food Security | Development | Education | Ebola | Climate Change | HIV/AIDS | Family Planning | Climate Change | Hepatitis | Cholera |
| HIV/AIDS | Ebola | HIV/AIDS | HIV/AIDS | Food Security | Human Rights | FGM | Ebola | HIV/AIDS | Ebola |
| Humanitarian Aid | Education | Malaria | Malaria | Humanitarian Aid | Innovation | Human Rights | Education | Malaria | Measles |
| Mothers | Food Security | Mothers | Measles | Poverty | Prevention | Humanitarian Aid | Human Rights | Testing | Pneumonia |
| South America | HIV/AIDS | Polio | Mothers | Sanitation | Testing | Nutrition | Online | Treatment | Polio |
| Water | Humanitarian Aid | Sanitation | Polio | Water | Treatment | Violence | Violence | Tuberculosis | Poverty |
| Women | Water | Women | Women | Women | Women | Women | Water | Vaccines | Vaccines |
| Global Fund | CDC | EU CDC | NIH | FAO | UNDP | MSF | PATH | Save the Children | Oxfam |
| Africa | Children | Ebola | Africa | Africa | Africa | Africa | Access | Africa | Africa |
| Children | Diarrhea | Hepatitis | Cancer | Agriculture | Children | Children | Africa | Children | Climate Change |
| Cholera | E.Coli | HIV/AIDS | Funding | Biodiversity | Climate Change | Cholera | Breastfeeding | Donations | Ebola |
| Ebola | Influenza | Influenza | Heart Disease | Climate Change | Education | Ebola | Cancer | Education | Food Security |
| HIV/AIDS | Measles | Measles | HIV/AIDS | Families | FGM | HIV/AIDS | Children | Food Security | Humanitarian Aid |
| Malaria | Prevention | Outbreaks | News | Farmers | Food Security | Humanitarian Aid | Ebola | Humanitarian Aid | Malaria |
| Pneumonia | Vaccines | Report | Rare Disease | Fisheries | HIV/AIDS | Refugees | Innovation | Pneumonia | Pneumonia |
| Polio | Water | Surveillance | Research | Food Security | Malaria | Treatment | Malaria | Refugees | Refugees |
| Tuberculosis | Women | Tuberculosis | Stress | Forests | Water | Tuberculosis | Pneumonia | Schools | Water |
| Women | Zika | West Nile | Veterans | Water | Women | Violence | Vaccines | Water | Women |
Ten revealed priorities of each of the 20 global health actors based on their tweets from 2016 to 2020. Priorities are alphabetically arranged. Red indicates funding organisations. Blue indicates channels of DAH. Grey indicates implementing institution.
CDC, Centers for Disease Control and Prevention; DAH, developmental assistance for health; ECDC, European Centre for Disease Prevention and Control; FGM, Female Genital Mutilation; MSF, Médecins Sans Frontières; NIH, National Institutes of Health; UNAIDS, United States Agency for International Development; UNDP, United Nations Development Programme; UNICEF, United Nations Children’s Fund.
Additionally, we model a network map from the priorities generated using the LDA topic model also using the Fruchterman-Reingold algorithm. This network map visualises the similarities in priorities between the 20 actors. Data used for this network map can be found in online supplemental table S4. This network map is compared with the network map generated using financial data from IHME in the findings section. This comparison between network maps can illustrate if priorities from tweets and from financial data are aligned. Further details on LDA and network maps can be found in online supplemental methods.
bmjopen-2021-054470supp004.pdf (23.1KB, pdf)
bmjopen-2021-054470supp006.pdf (256.6KB, pdf)
Testing if GHG operates under the RAM
By combining evidence for stated and revealed priorities of 20 key global health actors, we can determine if GHG operates under the RAM.
The RAM in international cooperation is categorised as the ‘linchpin of foreign policy decision-making’.37 This approach is rooted in expected utility theory in microeconomics introduced by von Neumann and Morgenstern in the 1940s and subsequent theories of rationality.38
RAM is most useful in explanations of economic behaviour if the three conditions of the rationality assumption are fulfilled.37 First, it is assumed that an actor’s goal is predetermined before intentionally acting to achieve it.37 Second, actors are assumed to ‘display consistent preferences as manifested in the ability to rank the preferences in transitive order’.37 Third, actors are assumed to maximise utility while choosing an alternative that provides the highest amount of net personal benefit.37
‘Rational’ in this case does not simply mean a dispassionate calculation of costs and benefits. In the case of global health actors, acting rationally means weighing both economic and political factors and acting according to the three assumptions of RAM.
‘To maximise utility’ in this study refers to maximising the net personal benefits, however, defined by the health actor. It can be defined as financial benefits, ethical benefits such as equity, or, however, else the health actor defines their utility.
GHG operates under RAM if each of the 20 global health actors and the global health system collectively fulfil the three assumptions of predetermined goal, rank order preferences and benefit maximisation.
To test the first assumption of predetermined goal, we determine the stated priorities of each global health actor from policy documents. We test whether there exist explicit statements on goals and priorities and note what health areas or issues are the stated priorities of each global health actor.
To test the second assumption of consistent rank order preferences, we compare revealed priorities from DAH funding data and revealed priorities from tweets. From the funding data, we can determine rank-order preferences based on which health issues are allocated the most funding in 2019. From tweets, we can determine rank-order preferences based on the top 10 topics each global health actor tweeted about from 2016 to 2020. If there is consistency in rank-order preferences between the revealed priorities from funding data and revealed priorities from tweets, then the second assumption is fulfilled.
To test the third assumption of benefit maximisation, we compare the stated and revealed priorities from all three data sources. The priorities that are consistent across stated priorities from policy documents and revealed priorities from funding data and from tweets are revealed to be the priority that the global health actor determines to be benefit maximising. An alignment of a preference across the three different sources can lead us to believe with some certainty that it is the actor’s benefit-maximising preference. While indirect, we believe that this method of determining benefit-maximising preference is the best method given the available data.
We also test the three assumptions at the global health system level. Predetermined goals are obtained from stated priorities from collective stated commitments to global health based on Sustainable Development Goal 3 (SDG3) of ‘good health and well-being’ as all 20 of the actors in this study have stated commitments to this goal. Consistent rank-order preferences are derived from the alignment between aggregated DAH funding allocations of all global health actors and the most common topics generated from tweets across all global health actors. The consistent preferences across stated and revealed priorities are inferred to be the global health systems’ benefit-maximising preference.
If each global health actor and the global health system collectively fulfil the three assumptions, then GHG operates under the RAM.
Characterising power dynamics in GHG
We use the following typology of power when characterising power dynamics in GHG. ‘Power is exercised everywhere in global health although its presence may be more apparent in some instances than others’,39 one global health researcher notes. The power concept in global health does not stray far from Robert Dahl’s (1957) definition in his seminal study where he describes ‘A has power over B to the extent that he can get B to do something B would not otherwise do’.40 One way to categorise power is through the four types introduced by Barnett and Duvall41, each manifesting in different manners in global health.41 Online supplemental table S5 summarises Barnett and Duvall’s four types of power. First, compulsory power is defined as ‘direct control of one actor over the conditions of existence or the actions of another’.41 In global health, compulsory power can be seen in how donor countries dictate the conditions in low and middle-income countries (LMICs) through development aid.42 Second, institutional power is ‘the control actors exercise indirectly over others through diffuse relations of interactions’.41 High-income countries control funding allocations for LMICs through institutional power via their contributions to multilateral organisations. Third, structural power refers to the ‘constitution of subjects’ capacities in direct structural relation to one another’.41 The structural and historical disempowerment of indigenous populations has resulted in their disproportionate outcomes in health.43 44 Fourth, ‘productive power works through diffuse constitutive relations to produce the situated social capacities of actors’.40 Research institutions funded by high-income countries direct what health issues are studied and addressed.45
bmjopen-2021-054470supp005.pdf (52.6KB, pdf)
To characterise the power dynamics in GHG, we analyse the interplay of stated and revealed priorities between funding organisations, channels of DAH and implementing organisations. Particularly, we identify which global health actors have the most influence in setting global health priorities. The global health actors which have the most priorities aligned with the stated and revealed priorities of the global health system are determined to have the most influence and power in priority-setting.
Discussion
GHG operates under RAM
As seen in online supplemental table S1, we find that each of the 20 key global health actors fulfils the three assumptions of the RAM. Each actor has a predetermined goal stated in policy documents, annual reports and official websites. Each actor has consistent rank-order preferences as observed in the alignment of order of preferences in DAH funding data and top identified topics from tweets. Consistent, top-ranking preferences across policy documents, funding data and tweets are the alternatives that maximise benefits for each global health actor based on their predetermined goal.
As an example, US Agency for International Development (USAID)’s predetermined goal is ‘advancing American security and prosperity’ through providing aid in the health areas of child and maternal health, HIV/AIDS, malaria and tuberculosis as found on their official website.46 In 2019, 49% of aid from USAID supported HIV/AIDS, 22% supported child and maternal health and 7% to malaria.47 The topic modelling for USAID’s tweets shows that HIV/AIDS, child and maternal health and malaria are the top themes tweeted about by the organisation from 2016 to 2020 (see online supplemental table S1). USAID behaves under the RAM as their revealed priorities from past funding behaviour and from tweets align with their predetermined goal.
As shown in the last row of online supplemental table S1, we find that the global health system collectively fulfils the three assumptions of the RAM. The predetermined goal of the global health system can be found in the WHO constitution and the nine target areas for SDG3 on good health and well-being. All 20 global health actors have stated commitments to the WHO mission and the SDGs. The alignment of DAH funding allocations and most common health issues from Twitter reveal that in terms of rank order, HIV/AIDS, child health and maternal health are the top three priorities of the global health system collectively. To maximise benefits of the predetermined goal of ‘health for all’ and ‘SDG3: good health and well-being’, the global health system prioritises HIV/AIDS, child health and maternal health. Among all nine stated targets in SDG3, only these three issues are prioritised. Effectively, the six other stated targets in SDG3 are deprioritized and underfunded by the global health system.
As each global health actor and the global health system collectively fulfils the three assumptions, we find that GHG operates under the RAM. This finding demonstrates that each global health actor operates based on their rational self-interest and that the global health system pursues only some predetermined health priorities. Who determines which priorities are pursued by the global health system? The findings on power dynamics in GHG reveal the actors who determine global priorities.
Compulsory and institutional power asymmetries in GHG
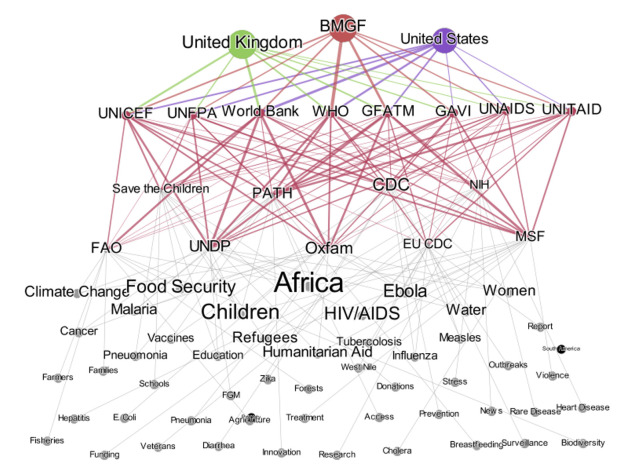
As demonstrated in the following network maps, we find that there is compulsory and institutional power asymmetry in GHG.
Compulsory power asymmetry can be found in how funding organisations strongly influence channels of DAH and implementing institutions based on their relationship. Channels of DAH and implementing institutions rely on funding organisations for resources to continue operating. We find that the top priorities of the three funding organisations in this study are also the priorities of channels of DAH and implementing institutions.
As seen in figure 1, HIV/AIDS is first priority of USAID, second priority of United Kingdom Department for International Development (UK-DFID) and second priority of the Bill and Melinda Gates Foundation (BMGF) based on the alignment of stated and revealed priorities. HIV/AIDS is a priority of four of eight channels of DAH and four of nine implementing institutions based on its presence in policy documents, DAH funding and tweets of each actor.
Figure 1.
Network Analysis of revealed priorities from tweets. Line thickness represents how many similar priorities one global health actor has with another. Font size of global health priorities represent the number of organisations have it as a priority. Data used found in online supplemental table 4. BMGF, Bill and Melinda Gates Foundation; CDC, Centers for Disease Control and Prevention; ECDC, European Centre for Disease Prevention and Control; NIH, National Institutes of Health; UNAIDS United States Agency for International Development; UNDP, United Nations Development Programme; UNFPA, United Nations Population Fund; UNICEF, United Nations Children’s Fund.
Figure 1 also demonstrates that maternal and child health is second priority of USAID, first priority of UK-DFID and first priority of BMGF based on the alignment stated and revealed priorities. Maternal and child health is a priority of six of eight channels of DAH and seven of nine implementing institutions based on its presence in policy documents, DAH funding and tweets of each actor.
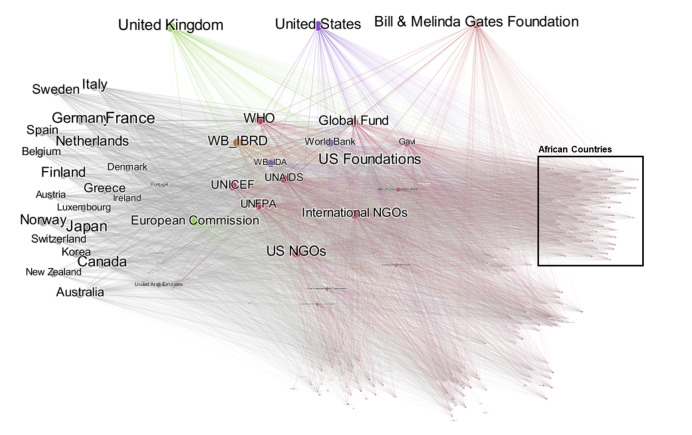
Following the flow of the funding in figure 2 and the similarities in tweets in figure 1, we can see that institutional power asymmetry can be found in how funding organisations strongly influence implementing institutions through outsized influence of channels of DAH that allocate funding to these implementing institutions. As some implementing institutions do not get direct funding from funding organisations, but through channels of DAH, their funding is controlled by channels of DAH. Because wealthy funding organisations influence the priorities of channels of DAH, transitively, funders have power over implementing institutions. Implementing institutions in turn align their priorities with the priorities of channels of DAH and transitively with the priorities of funding organisations.
Figure 2.
Network analysis of revealed priorities from Funding for DAH (2019). Line thickness represents the amount of funding for health that was transferred between two actors. Font size represents the total amount of funding for health donated or received in 2019. DAH, developmental assistance for health; UNAIDS United States Agency for International Development; UNFPA, United Nations Population Fund; UNICEF, United Nations Children’s Fund.IBRD, International Bank for Reconstruction and DevelopmentNGO, Non-Governmental Organization
Both network analyses of revealed priorities from DAH funding data and from tweets show how there is asymmetric levels of power held by the USA, UK and the Gates Foundation. Figure 2 reveals how these three funding organisations are the largest funders of the Global Fund, WHO, World Bank, US Foundations, UN organisations and GAVI. The IHME DAH database reveals that 24% of all DAH funding was allocated to HIV/AIDS, 21% to child health and 12% to maternal health—the three top priorities of funding organisations.16 Only 14% was allocated to health system strengthening and 2% to non-communicable diseases.16
Figure 1 reveals how the most common topics generated across all global health actors include Africa, HIV/AIDS, child health, women health and infectious diseases. These are the same health issues highly prioritised by the USA, UK and Gates Foundation. Comparing figures 1 and 2, we find that these three funding organisations have outsized influence in priority setting because of how much DAH funding these three organisations have provided relative to other funders. We find that the priorities from 2016 to 2020 documented through the tweets of actors align with these funders’ priorities of HIV/AIDS, child health, maternal health, infectious disease and Africa. This outsized influence of global health funders limits the range of funded programmes and policies, especially making it difficult for smaller implementers to fund local programmes and policies that do not neatly align with the priorities of large funders.
Limitations
It is necessary to acknowledge the limitations of this study. First, we assume stated priorities match what is specified in organisational documents. It may be the case that some organisations communicate priorities differently from what is written in their foundational documents. Moreover, what is fundable may not necessarily be what is deemed important. Second, we assume that health funding is indeed spent on what it is ostensibly spent on when deriving revealed preferences from funding data, which may not always be true. Third, our scope is limited to examining 20 global health actors from 2016 to 2020. There are non-health actors and processes that likely influence health outcomes. Studying the stated and revealed priorities of non-health actors and processes such as foreign relations between nations and the influence of the private sector on health can improve the characterisation of current GHG. Fourth, tweets may only reveal priorities that the actor wants to communicate. As organisations have teams that plan communications, priorities derived from Twitter may be limited and not reveal all priorities. While what happens behind closed doors in GHG is unknowable, tweets can reveal some of the implicit priorities of actors. Fifth, we derived benefit-maximising preferences by identifying consistently top-ranking preferences across stated priorities from policy documents and revealed preferences from tweets and funding data. This manner of identifying benefit-maximising preferences is indirect and does not necessitate that it is indeed what the actor believes is a benefit-maximising preference. To be certain about what is benefit-maximising can only be done by directly asking health actors. However, even within organisations, there are inconsistencies about what members think are benefit-maximising. We acknowledge this indirect manner of deriving benefit-maximising priorities is a limitation.
Conclusion
We find empirical evidence at the global level showing that GHG operates under the RAM. Additionally, we find that at the global level, there is asymmetric compulsory and institutional power held by funding organisations, allowing global health priorities to be largely influenced by large funders. In the past years, these funders have been the USA, UK and the Gates Foundation.
We find that there is a correlation between the priorities of large funders and the priorities of channels of DAH and implementing institutions. This correlation in conjunction with GHG operating under the RAM and the asymmetric power held by funders raises issues. What is worrying is that GHG under the RAM grants large funders majority of the power to determine where GHG resources go, and ultimately influencing outcomes. Effectively, this limits the range of health issues that are adequately funded. Additionally, if outcomes are unfavourable, funding organisations do not have full accountability even if they have outsized influence in GHG priority setting. It is an issue that implementing organisations, especially smaller local organisations, who have the closest relationship with target populations, have little to no say in how resources are distributed in GHG under the RAM. GHG under the RAM can only lead to equitable health outcomes if and only if major funding organisations have a joint commitment towards the same goals of health equity and justice. If funders set priorities that are grounded on equity and justice, then it would be good for all actors to adhere to the RAM and seek funding by aligning their priorities with funder priorities. In this situation, all actors’ individual goals will be aligned with the funding organisations’ goals of equity and justice. These findings are aligned with current literature discussing how ‘philantrocapitalists’ and large funders have an outsized influence on global health agenda setting even without having an ethical framework for decision-making.48 49
Our article complements the current research on agenda setting in global health, which discusses how agenda setting is not purely a rational deliberation of evidence but the convergence of problems, solutions and political developments.50 This study attempts to deepen the understanding power’s manifestation and influence in agenda setting through the lens of stated and revealed priorities.
The priorities of funders of HIV/AIDS, child health and maternal health have been prioritised from 2016 to 2020. While we have seen improvements in these three areas, the existence of significant and severe preventable health inequalities demonstrates that this prioritisation architecture does not necessarily promote equity and justice in global health. Additionally, other core health issues such as horizontal health system improvements were not found to be prioritised, which may have affected the persistence of health inequities. We have empirical evidence supporting the arguments that current GHG operates under the RAM, and existing power asymmetries limit the range of choice for health policies and programmes that aim to reduce inequities.
Supplementary Material
Acknowledgments
We thank participants in the Harvard Law School Global Justice Workshop for helpful comments on an earlier version of this work.
Footnotes
Contributors: GFB and JJP made substantial contributions to the conception and design of the study. JJP supervised the research planning, analysis and execution and interpretation of data and analysis and GFB conducted the analyses. GFB prepared the manuscript draft with JJP’s critical input and revisions for important intellectual content. GFB and JJP approved the final manuscript version to be published. JJP obtained funding. GFB and JJP agree to be guarantors and accept full responsibility for the finished work and/or the conduct of the study.
Funding: This work was supported by the Health Equity and Policy Lab (HEPL) at the University of Pennsylvania. We acknowledge funding, in part, by the Vice Provost for Research University Research Foundation at the University of Pennsylvania.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Under the 'Content Redistribution' section of Twitter’s Developer Agreement and Policy, 'We restrict the redistribution of Twitter Content to third parties. If you provide Twitter Content to third parties, including downloadable datasets or via an API, you may only distribute Tweet IDs, Direct Message IDs, and/or User IDs.' Because the data collected using the Twitter API does not allow for redistribution under the Twitter Developer Agreement and Policy, tweets cannot be made publicly available. Only Tweet ID’s and User ID’s are allowed to be redistributed according to the Twitter policy. Please email jenpr@upenn.edu if you wish to receive a copy of the Tweet ID’s and User ID’s of the data and/or the code used in the study. The IHME DAH Database can be found at http://ghdx.healthdata.org/record/ihme-data/development-assistance-health-database-1990-2019.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study did not have any human or animal participants. Additionally, the study did not require ethical approval as the Twitter data used were already in the public domain.
References
- 1.Ng NY, Ruger JP. Global health governance at a crossroads. In: Global Health Governance : The Scholarly Journal for the New Health Security Paradigm. 3, 2011. [PMC free article] [PubMed] [Google Scholar]
- 2.Giaimo S, Groups I. Think tanks, and health care policy (1960s-Present). In: Guide to US. health and health care policy. Thousand Oaks, CA: SAGE Publications, 2014: 375–92. [Google Scholar]
- 3.Spicer N, Agyepong I, Ottersen T, et al. 'It's far too complicated': why fragmentation persists in global health. Global Health 2020;16:60. 10.1186/s12992-020-00592-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szlezák NA, Bloom BR, Jamison DT, et al. The global health system: actors, norms, and expectations in transition. PLoS Med 2010;7:e1000183. 10.1371/journal.pmed.1000183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Kingdom House of Lords . Chapter 3: international health: the institutional labyrinth. In: Select Committee on Intergovernmental organisations first report, 2008. [Google Scholar]
- 6.Ottersen OP, Dasgupta J, Blouin C, et al. The political origins of health inequity: prospects for change. The Lancet 2014;383:630–67. 10.1016/S0140-6736(13)62407-1 [DOI] [PubMed] [Google Scholar]
- 7.Walt G. Global cooperation in international public health. In: Merson M, Black R, Mills A, eds. International public health. Gaithersburg. Gaithersburg, Maryland: Aspen Publishers, 2001. [Google Scholar]
- 8.Mayhew SH, Walt G, Lush L, et al. Donor agencies' involvement in reproductive health: saying one thing and doing another? Int J Health Serv 2005;35:579-601. 10.2190/K46B-RRXJ-95M4-JDQU [DOI] [PubMed] [Google Scholar]
- 9.Burris S. Governance, Microgovernance and health. Temple Law Review 2004;77:335–62. [Google Scholar]
- 10.Brooks A, Cutts FT, Walt G. Policy study of factors influencing the adoption of new and underutilized vaccines in developing countries. Washington D.C 1999. [Google Scholar]
- 11.Travis P, Bennett S, Haines A, et al. Overcoming health-systems constraints to achieve the millennium development goals. The Lancet 2004;364:900–6. 10.1016/S0140-6736(04)16987-0 [DOI] [PubMed] [Google Scholar]
- 12.Hoffman SJ, Røttingen J-A. Dark sides of the proposed framework convention on global health’s many virtues: a systematic review and critical analysis. Health and Human Rights 2013;15:117–34. [PubMed] [Google Scholar]
- 13.Ruger JP. Global health governance as shared health governance. J Epidemiol Community Health 2012;66:653-61. 10.1136/jech.2009.101097 [DOI] [PubMed] [Google Scholar]
- 14.Frenk J, Moon S. Governance challenges in global health. NEJM 2013;368:936–42. 10.1056/NEJMra1109339 [DOI] [PubMed] [Google Scholar]
- 15.Hoffman SJ, Cole CB. Defining the global health system and systematically mapping its network of actors. Global Health 2018;14:38. 10.1186/s12992-018-0340-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Institute for Health Metrics and Evaluation (IHME) . Development assistance for health database 1990-2019. Institute for Health Metrics and Evaluation (IHME), 2020. [Google Scholar]
- 17.Lopreite M, Puliga M, Riccaboni M, et al. A social network analysis of the organizations focusing on tuberculosis, malaria and pneumonia. Soc Sci Med 2021;278:113940. 10.1016/j.socscimed.2021.113940 [DOI] [PubMed] [Google Scholar]
- 18.Quissell K, Berlan D, Shiffman J. Explaining global network emergence and nonemergence: comparing the processes of network formation for tuberculosis and pneumonia. Public Administration and Development 2018;38. [Google Scholar]
- 19.Hevey D. Network analysis: a brief overview and tutorial. Health Psychol Behav Med 2018;6:301-328. 10.1080/21642850.2018.1521283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68-78. 10.1037//0003-066x.55.1.68 [DOI] [PubMed] [Google Scholar]
- 21.Donelle L, Booth RG. Health tweets: an exploration of health promotion on Twitter. Online J Issues Nurs 2012;17:4. [PubMed] [Google Scholar]
- 22.Park H, Rodgers S, Stemmle J. Analyzing health organizations' use of Twitter for promoting health literacy. J Health Commun 2013;18:410-25. 10.1080/10810730.2012.727956 [DOI] [PubMed] [Google Scholar]
- 23.Glazer A. Konrad K. a signaling explanation for charity. American Economic Review 1996;86:1019–28. [Google Scholar]
- 24.Harbaugh W. The prestige motive for making charitable transfers. American Economic Review 1998;88:227–82. [Google Scholar]
- 25.Fung IC-H, Jackson AM, Ahweyevu JO, et al. #Globalhealth Twitter Conversations on #Malaria, #HIV, #TB, #NCDS, and #NTDS: a Cross-Sectional Analysis. Ann Glob Health 2017;83:682-690. 10.1016/j.aogh.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 26.Goff DA, Kullar R, Laxminarayan R, et al. Twitter to engage, educate, and advocate for global antibiotic stewardship and antimicrobial resistance. Lancet Infect Dis 2019;19:229-231. 10.1016/S1473-3099(19)30058-1 [DOI] [PubMed] [Google Scholar]
- 27.Guidry JPD, Jin Y, Orr CA. Ebola on Instagram and Twitter: how health organizations address the health crisis in their social media engagement. Public Relations Review 2017;43. [Google Scholar]
- 28.Scanfeld D, Scanfeld V, Larson EL. Dissemination of health information through social networks: Twitter and antibiotics. Am J Infect Control 2010;38:182-8. 10.1016/j.ajic.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zamora A. Making room for big data: web Scraping and an affirmative right to access publicly available information online. Entrep Bus Law J 2019;12:203–28. [Google Scholar]
- 30.Alvarez-Melis D, Saveski M. Topic modeling in Twitter: aggregating Tweets by conversations. Tenth International AAAI Conference on Web and Social Media 2016. [Google Scholar]
- 31.Hong L, Davison BD. Empirical study of topic modeling in Twitter. Proceedings of the First Workshop on Social Media Analytics - SOMA ’10. New York, USA: ACM Press, 2010. [Google Scholar]
- 32.Yang S-H, Kolcz A, Schlaikjer A. Large-Scale high-precision topic modeling on Twitter. Proceedings of the 20th ACM SIGKDD international conference on Knowledge discovery and data mining - KDD ’14. New York, USA: ACM Press, 2014. [Google Scholar]
- 33.Bakshi RK, Kaur N, Kaur R. Opinion mining and sentiment analysis. 2016 3rd International Conference on Computing for Sustainable Global Development 2016:452–5. [Google Scholar]
- 34.Pak A, Paroubek P. Twitter as a corpus for sentiment analysis and opinion mining. LREc 2010;10:1320–6. [Google Scholar]
- 35.Saif H, He Y, Alani H. Semantic sentiment analysis of Twitter 2012.
- 36.Blei DM, AY N, Jordan MI. Latent Dirichlet allocation. J Mach Learn Res. 2003;3. [Google Scholar]
- 37.Mintz A, DeRouen K. The Rational Actor Model. In: Understanding Foreign Policy Decision Making. Cambridge: Cambridge University Press, 2010: 57–68. [Google Scholar]
- 38.MacDonald PK. Useful fiction or miracle maker: the competing epistemological foundations of rational choice theory. Am Polit Sci Rev 2003;97:551–65. 10.1017/S000305540300087X [DOI] [Google Scholar]
- 39.Shiffman J. Knowledge, moral claims and the exercise of power in global health. Int J Health Policy Manag 2014;3:297-9. 10.15171/ijhpm.2014.120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dahl RA. The concept of power. Behav Sci 2007;2:215. 10.1002/bs.3830020303 [DOI] [Google Scholar]
- 41.Barnett M, Duvall R. Power in international politics. Int Organ 2005;59. 10.1017/S0020818305050010 [DOI] [Google Scholar]
- 42.Shawar YR, Ruger JP. The politics of global health inequalities: approaches to studying the role of power. In: McInnes C, Lee K, Youde J, eds. The Oxford Handbook of global health politics. Oxford, 2020: 59–76. [Google Scholar]
- 43.Holmes SM. Structural vulnerability and hierarchies of ethnicity and citizenship on the farm. Med Anthropol 2011;30:425-49. 10.1080/01459740.2011.576728 [DOI] [PubMed] [Google Scholar]
- 44.Goldade K. “Health Is Hard Here” or “Health for All”? Medical Anthropology Quarterly 2009;23. [DOI] [PubMed] [Google Scholar]
- 45.Sridhar D. Who sets the global health research agenda? the challenge of multi-bi financing. PLoS Med 2012;9:e1001312. 10.1371/journal.pmed.1001312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Usaid.gov . Global health, 2021. Available: https://www.usaid.gov/global-health [Accessed 1 November 2021].
- 47.Usaid.gov . Health areas, 2021. Available: https://www.usaid.gov/global-health/health-areas [Accessed 1 November 2021].
- 48.Birn A-E. Philanthrocapitalism, past and present: The Rockefeller Foundation, the Gates Foundation, and the setting(s) of the international/global health agenda. Hypothesis 2014;12. 10.5779/hypothesis.v12i1.229 [DOI] [Google Scholar]
- 49.McGoey L. Philanthrocapitalism and its critics. Poetics 2012;40. [Google Scholar]
- 50.Shiffman J. Agenda Setting in Public Health Policy. In: International encyclopedia of public health, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-054470supp001.pdf (279.9KB, pdf)
bmjopen-2021-054470supp002.pdf (15.8KB, pdf)
bmjopen-2021-054470supp003.pdf (23.4KB, pdf)
bmjopen-2021-054470supp004.pdf (23.1KB, pdf)
bmjopen-2021-054470supp006.pdf (256.6KB, pdf)
bmjopen-2021-054470supp005.pdf (52.6KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Under the 'Content Redistribution' section of Twitter’s Developer Agreement and Policy, 'We restrict the redistribution of Twitter Content to third parties. If you provide Twitter Content to third parties, including downloadable datasets or via an API, you may only distribute Tweet IDs, Direct Message IDs, and/or User IDs.' Because the data collected using the Twitter API does not allow for redistribution under the Twitter Developer Agreement and Policy, tweets cannot be made publicly available. Only Tweet ID’s and User ID’s are allowed to be redistributed according to the Twitter policy. Please email jenpr@upenn.edu if you wish to receive a copy of the Tweet ID’s and User ID’s of the data and/or the code used in the study. The IHME DAH Database can be found at http://ghdx.healthdata.org/record/ihme-data/development-assistance-health-database-1990-2019.