Abstract
The COVID-19 pandemic has touched the lives of adolescents around the world. This short-term longitudinal, observational study followed 1,334 adolescents (11–17 yo) to investigate whether social-ecological resilience relates to intra- and inter-personal resources and/or the caregiver relationship relates to changes in internalizing symptoms during five stressful weeks of COVID-19 lockdown in Perú. In this work, we contextualize social-ecological resilience in relation to culturally-relevant personal and caregiver resources that youth can use to adapt to stressful situations. We found that adolescents who reported higher levels of personal, caregiver, and overall resilience had lower levels of anxiety and depressive symptoms at week six. We also find that personal, caregiver, and overall resilience moderated the change in anxiety symptoms from week 6 to week 11 of lockdown in 2020. Our findings underscore the importance of social-ecological resilience related to both intra/interpersonal resources and the caregiver relationship for minimizing the harmful impacts of COVID-19 on adolescent internalizing symptoms.
Keywords: Resilience, Adolescence, Anxiety, Depression, LMICs, COVID-19 pandemic
Introduction
Adolescents under Lockdown
The COVID-19 pandemic and associated lockdowns constitute extreme, prolonged stressors of uncertain duration and unprecedented magnitude for adolescents around the world. Lockdown measures in response to COVID-19 have impacted adolescents through school closures, the need to stay at home with family, and separation from peers and friends. Although the pandemic is global in scale, it has affected different communities and countries in different ways. In Perú, a very stringent lockdown was put in place for the first 100 days of the pandemic (Alvarez-Risco et al., 2020; Presidency of the Council of Ministers, 2020a, b; Dyer, 2020). Unlike many other countries, children and adolescents were prohibited from leaving the house and seeing their friends, or other members of the family. Stringent lockdowns in Perú were enforced by military personnel who were patrolling the streets (Presidency of the Council of Ministers, 2020a, b). Perú also has suffered a high number of case counts and deaths as well as significant economic ramifications (Munayco et al., 2020; Peruvian Health Ministry, 2020).
While young people might not be as physically affected by the COVID-19 virus (Zare-Zardini et al., 2020), adolescents may be particularly vulnerable to experiencing adverse mental health effects of the lockdown. Adolescence is an important period of social cognitive development characterized by developing mentalizing abilities, exploration of identity, peer integration, romantic interests and increasing independence and autonomy (Nelson et al., 2016). The combination of a global public health crisis, economic recession, sudden isolation, and remote instruction due to COVID-19 can compromise opportunities for face-to-face social interaction, general sociability, relationships, and, in turn, adolescent well-being (Golberstein et al., 2020; Loades et al., 2020). These effects may be exacerbated by or due, in part, to vulnerability to mental health problems during this period of development (Pfeifer & Allen, 2021). For example, mood and anxiety disorders – two of the most common mental health disorders – typically emerge in mid- to late-adolescence (Kessler et al., 2007b; Solmi et al., 2022). During adolescence, girls display higher rates of depression and anxiety than boys and older adolescents have higher rates of depression and anxiety than their younger counterparts (Ghandour et al., 2019; Kessler et al., 2007a; Patton et al., 2014; Thapar et al., 2012). Furthermore, recent data suggests that COVID-19-related lockdowns and school closures may contribute to anxiety and depression in adolescence (Barendse et al., 2021; Smirni et al., 2020).
To contextualize the potential effect of these lockdown orders on the well-being of Peruvian adolescents, we can consider several theoretical and empirical perspectives. Developmentally, adolescence is a time of reorientation away from parents towards peers (Nelson et al., 2016) and a period of social and identity exploration during which, along with a drive for connectedness with peers, there is a high desire for expanding autonomy (Fuligni, 2019). Yet adolescence encompasses a broad age range (Sawyer et al., 2018), and is not a monolith; thus, adolescents in different developmental stages will likely have different needs and may be differentially impacted by the lockdown. For example, it is possible that older adolescents might more accurately comprehend the magnitude of the lockdown, but, they may also have more autonomy in online social communication – allowing them to more effectively communicate with friends through digital means. While older adolescents may be more vulnerable to mental health problems, they might also be better able to draw on resources to make them resilient in the face of adversity. Thus, it is important to investigate differences across the adolescent age range both in terms of vulnerability to internalizing symptoms during lockdown, as well as potentially differential sources of resilience for younger compared to older adolescents.
Social-ecological Resilience
Researchers have called for more longitudinal research on risk and resilience in adolescents particularly amidst the stressful COVID-19 lockdown (Dvorsky et al., 2021). Due to the global nature of the pandemic, it is important to have a contextualized approach that takes into account the “cultural and national ecologies” of youth development (Hussong et al., 2021). Measures of resilience have often focused on the identification of personal characteristics that allow individuals to overcome, and even thrive, in the face of stressors and adversity (Guazzelli Williamson et al., 2021; Dulin et al., 2018; Connor & Davidson, 2003). However, this approach might overlook important cultural and contextual factors that are related to positive coping under conditions of adversity (Ungar, 2006, 2018; Guazzelli Williamson et al., 2021; Dulin et al., 2018). Social-ecological resilience refers to culturally-relevant personal and caregiver resources that youth can use to adapt to stressful situations. Personal resilience refers to intrapersonal and interpersonal resources to cope with a stressor (Resilience Research Centre, 2018). Caregiver resilience pertains to “characteristics associated with the important relationships shared with either primary caregiver or a partner or a family” including the degree to which adolescents feel connected to a parent or caregiver, receive support from family during difficult times and feel a sense of security when with family (Resilience Research Centre, 2018). Shifting away from individual traits that might be protective in the face of adversity, the social-ecological model emphasizes the individual’s ability to navigate towards resources in their environment and negotiate for these resources to be provided (Ungar, 2008). The abilities to navigate and negotiate for psychological, social, cultural and physical resources will also be affected by individual maturation of physical and cognitive processes (Ungar, 2012). In shifting the focus away from individual traits towards systemic and dynamic processes, this project seeks to use a social-ecological resilience framework to expand upon previously reported concepts of adolescent development which are largely decontextualized from sociocultural factors (Ungar, 2008).
While intra/interpersonal sources of resilience – including social support, peer relationships, autonomy, and education – typically become increasingly important across adolescence, lockdown may uniquely challenge these dynamics due to limited peer contact, online education, and increased interactions with caregivers. Research suggests that caregivers play an important role in protecting against adverse mental health outcomes in adolescents, particularly in relation to anxiety and depression (Butterfield et al., 2021).
Cultural contextual factors may also offer protection from adversity. Due to a collectivistic culture for example, Peruvian cultural norms and values might have protective effects in coping with physical isolation in spite of a stringent lockdown, high case and death count, and an economic recession. While this is not a cross-cultural study that would allow us to dissect this question, here we take a first step in enriching and diversifying existing literature on the topic by investigating a large sample of low- to middle-class youth in secondary schools in Perú who did have access to continued remote instruction.
The Present Study
In this short-term longitudinal study, we investigated internalizing symptoms and social-ecological resilience among Peruvian adolescents from low- to middle-income urban settings during a critical five week period of intense COVID-19 lockdown. We pre-registered the hypotheses that social-ecological resilience would temper potential increases in depressive and anxiety symptoms. We also predicted that this effect would be stronger among girls compared to boys. We further pre-registered our plans to conduct exploratory analyses to examine the potentially moderating role of caregiver and personal sources of resilience – and moderation of resilience’s impact by school grade level and sex.
The goals of the present study were to 1) investigate whether there were differential rates of anxiety and depression among adolescents between the ages of 11 and 17 during early stages of a very stringent lockdown, and 2) assess whether different sources of resilience were differentially protective against anxiety or depression in a population of secondary school students in Perú.
Methods
Participants
A detailed account of the protocol of the larger study from which this subsample was extracted is described elsewhere (Magis-Weinberg et al., 2021). Data were collected starting from the sixth week of lockdown in Perú, in April 2020, to the 11th week of lockdown, in May 2020 (see Fig. 1 for timeline). Notably, this five week period captured the peak of the initial COVID-19 stressor as it coincided with the strictest days of lockdown in Perú–the first 100 days of lockdown–in which the country declared a nation-wide state of emergency. Students continued to have access to remote instruction during this time. Participants came from 63 Innova Schools across Perú. Innova is a “network of private schools designed to support students of emerging middle-class families in Latin America” (Magis-Weinberg et al., 2021; Wente et al., 2019). While we did not collect socioeconomic status (SES) data for individual participants, at a school network level, 70% of students are in the third (middle) SES quintile for Perú and 29% are in the second SES quintile. We did not collect data on race/ethnicity at an individual level. However, our sample generally reflects the ethnic/racial breakdown of Peruvian youth, oversampling from the mestizo population. According to the Peruvian National Institute on Statistics and Informatics in 2015, 57% of the Peruvian population self-identified as mestizo, 20% as quechua, 5% as white, 2% as aymara, 2% as black, 1% as native, 8% doesn’t know and 5% as other (Instituto Nacional de Estadística e Informática, 2017). The schools have fewer indigenous or White students than the general population given the focus of Innova Schools on low and middle income students, and the fact that racial identification and SES are very intertwined in Latin America (Telles & Paschel, 2014). Thus, the sample presented here consists of low- and middle-income students attending the Innova Schools in Perú who continued to receive remote instruction during the pandemic.
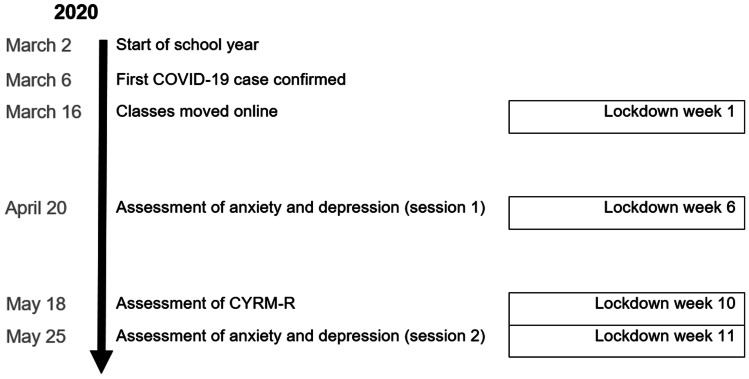
Fig. 1.
Study timeline expressed in weeks of lockdown. Data was collected on the sixth, tenth and eleventh weeks of lockdown. There are no baseline measurements before the lockdown
Questionnaires were delivered remotely via Qualtrics as part of a six-week digital citizenship intervention consisting of a curriculum designed to promote well-being and healthy technology use during the COVID-19 lockdown (Magis-Weinberg et al., 2021). Participants provided demographic information as well as self-report surveys of internalizing symptoms, resilience, and digital media use. Parents were notified of the digital citizenship intervention ahead of time by the schools and were allowed to remove their children from the study at any time. The University of California, Berkeley’s human subjects committee granted ethics approval for this study. Passive consent was obtained from parents, and verbal passive assent was obtained from students (i.e. teachers reminded students that they only needed to click on the Qualtrics link if they wanted to participate). All study questions with the exception of demographics could be skipped and students were informed that they could stop at any point. Following data cleaning and processing from a sample of 1398 participants, the final sample consisted of 1334 students (58.2% girls) between sixth and 11th grade. Included participants were an average of 13.54 years old (range = 10.92–17.41).
Measures
All measures were administered in Spanish. A detailed description of all measures and English translations can be found in the Open Science Framework (https://osf.io/nzp2w/).
Depressive symptoms were assessed via the Patient Health Questionnaire-2 (PHQ-2; Kroenke et al., 2003) twice (during weeks six and 11). This two-item questionnaire asked participants to respond to items asking how often, over the last two weeks, participants had “little interest or pleasure in doing things” and been “feeling down, depressed or hopeless.” Responses to each item were recorded on a four-point Likert scale, ranging from “not at all” to “nearly every day”. Item responses were summed to produce a raw score, ranging from zero to six, with a score of three indicating that a diagnosis of major depressive disorder is likely. In our sample, Spearman Brown’s reliability was 0.51. The PHQ-2 has been used in studies around the world including in studies of health and well-being during the COVID-19 pandemic (Gelaye et al., 2016; Kroenke et al., 2003; Löwe et al., 2005; Nelson et al., 2020). A meta-analysis comprised of samples of adolescents and adults has found the pooled sensitivity of the PHQ-2 to be 0.76 (95% CI = 0.68–0.82) and its specificity to be 0.87 (95% CI–0.82–0.90) (Manea et al., 2016).
Anxiety symptoms were assessed via the four-item Patient-Reported Outcomes Measurement Information System Short Form v1.0–Anxiety 4a (PROMIS; Pilkonis et al., 2011) twice (during weeks six and 11). The PROMIS is a four-item self-report scale in which subjects report on their anxious moods and behaviors over the past seven days on a five-point scale (ranging from one for “never” to five for “always”). In our sample, Cronbach’s alpha was 0.66. The PROMIS anxiety measure is a common, well-validated screener that has been shown to be sensitive to change in anxiety symptoms (Pilkonis et al., 2011; Schalet et al., 2016). In a racially/ethnically diverse sample, the PROMIS-anxiety has displayed a Chronbach’s alpha of 0.97 (Teresi et al., 2016). Symptom levels, including normal, mild, moderate and severe levels, were calculated in accordance with the thresholds provided by the PROMIS handbook (https://www.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points).
Social-ecological resilience was assessed during week 10 via the 17-item Rasch-validated Revised Child and Youth Resilience Measure (CYRM-R) consisting of two subscales (personal resilience and caregiver resilience) (Jefferies et al., 2019). Caregiver resilience “relates to characteristics associated with the important relationships shared with either primary caregiver or a partner or a family” (Jefferies et al., 2019). These include a sense of security when with family, getting support from family when experiencing difficulties and feeling connected to a parent or caregiver. Personal resilience refers to intrapersonal and interpersonal resources to cope with a stressor. These include aspects of sociability and likability and features including the opportunity to demonstrate one’s capability, the value of education to an individual, and one’s attachment to their cultural or family heritage. The CYRM-R is a measure of social-ecological resilience that recognizes two main dimensions in an individual’s social ecology for adjusting to adversity (Jefferies et al., 2019).
The CYRM-R is an appropriate measure across multiple contexts and cultures and contains items obtained from the International Resilience Project which includes data from 11 countries across five continents (Jefferies et al., 2019). Other versions of the CYRM have been used in Spanish with youth in Chile (Caqueo-Urízar et al., 2021, CYRM-12) and in Spain (Llistosella et al., 2019, CYRM-32) where the Cronbach’s alpha’s was 0.88. In our sample, Cronbach’s alpha for overall resilience was 0.88, Cronbach’s alpha for personal resilience was 0.83, and Cronbach’s alpha for caregiver resilience was 0.78.
Data Analyses
Pre-registered hypotheses and detailed analyses can be found in the Open Science Framework (https://osf.io/c8n65/).
Data Processing
Individuals who selected the same answer for every CYRM-R item were excluded. Individuals who answered at least seven of the ten items on CYRM-R personal resilience subscale and who answered five out of seven items on the CYRM-R caregiver resilience subscale were included in the analysis. If participants only answered seven, eight, or nine of the ten CYRM-R items in the personal resilience subscale or five or six items of the seven in the caregiver resilience subscale, their scores were imputed by calculating an average CYRM-R score based on the questions that they did answer. Outliers on the CYRM-R were winsorized to 1% above the next highest or 1% below the next lowest value.
Individuals who did not complete both items on the PHQ-2, or the four items on the PROMIS scale, were excluded from analyses of the time point (week six or 11) where their data were missing. Mixed effects models allowed us to retain participants with complete PROMIS or PHQ-2 responses for just one time point (even if they did not fill out anxious and depressive symptoms at both weeks six and 11). Apart from descriptive analyses where thresholded cutoffs of depression and anxiety were explored, depressive and anxiety symptoms were used as continuous measures in all models testing our hypotheses.
Descriptive Analysis
All data analyses were conducted in R 4.0.2 (R Core Team, 2020) using apaTables to calculate mean and standard deviations and bivariate correlations between variables (Stanley & Spence, 2018) and compareGroups for group comparisons (Subirana et al., 2014).
Hypothesis Testing
Using linear mixed effects models, we investigated whether youth-reported ratings of resilience moderated the change in subjective youth-ratings of depressive and anxiety symptoms from week six to week 11, and whether grade or gender interacted with this relationship. Further, we explored whether this relationship differed for personal or caregiver resilience.
We tested our hypothesis using a mixed effects model comparison approach pre-registered at the Open Science Framework (Guazzelli Williamson et al., 2020). Two series of mixed-effects models were conducted in parallel, following the same steps, one with anxiety symptoms as the outcome variable and the other with depressive symptoms as the outcome variable. To account for longitudinal effects such as changes between week six and 11, time point was included as a fixed effect in all models. Gender and school grade were included to test for differences in anxiety and depressive symptoms among groups. To test whether the magnitude or change of anxiety and depressive symptoms was moderated by resilience we tested for CYRM-R (total, personal, and caregiver (separately)) and time point interactions. Finally, we tested for three-way interactions between sex or grade, CYRM-R, and time point (see Table 1). Resilience scores were mean centered.
Table 1.
Fit statistics and model comparisons for the linear mixed effects models predicting anxiety and depressive symptoms
| Anxiety symptoms (outcome) |
Depressive symptoms (outcome) | ||||
|---|---|---|---|---|---|
| Models | AIC | χ2 (p) | AIC | χ2 (p) | |
| CYRM-R total (sex main effects and interaction) | |||||
|
Baseline Overall resilience is a main effect but not a moderator of change in internalizing symptoms |
CYRM-R + time point + sex + (1|ID) | 13666 | - | 9121.8★ | - |
|
Hypothesis 1 Overall resilience moderates change in internalizing symptoms |
CYRM-R * time point + sex + (1|ID) | 13660 |
8.02 (p < 0.005)** |
9123.0 |
0.83 (p = 0.362) |
|
Hypothesis 2 Moderation is influenced by sex |
CYRM-R * time point * sex + (1|ID) | 13647★ |
19.02 (p < 0.001)*** |
9122.7 |
6.33 (p = 0.097) |
| CYRM-R total (grade main effects and interaction) | |||||
|
Hypothesis 3 Overall resilience does not moderate change in internalizing symptoms |
CYRM-R + time point + grade + sex + (1|ID) | 13656 | - | 9113.5★ | - |
|
Hypothesis 3a Overall resilience moderates change in internalizing symptoms |
CYRM-R * time point + grade + sex + (1|ID) | 13650★ |
8.04 (p < 0.005)** |
9114.7 | 0.81 (p = 0.368) |
|
Hypothesis 3b Moderation is influenced by grade |
CYRM-R * time point * grade + sex + (1|ID) | 13658 |
22.58 (p = 0.094) |
9123.4 |
21.24 (p = 0.129) |
| CYRM-R personal (grade main effects and interaction) | |||||
|
Hypothesis 4a Personal resilience does not moderate change in internalizing symptoms |
CYRM-R_personal + time point + sex r + grade + (1|ID) | 13656 | - | 9137.1★ | - |
|
Hypothesis 4b Personal resilience moderates change in internalizing symptoms |
CYRM-R_personal * time point + sex + grade + (1|ID) | 13653★ |
4.22 (p = 0.040)* |
9139.1 |
0.01 (p = 0.929) |
|
Hypothesis 4c Moderation is influenced by grade |
CYRM-R_personal * time point * grade + sex + (1|ID) | 13656 |
19.48 (p = 0.370) |
9150.2 |
18.85 (p = 0.221) |
| CYRM-R caregiver (grade main effects and interaction) | |||||
|
Hypothesis 4d Caregiver resilience does not moderate change in internalizing symptoms |
CYRM-R_caregiver + time point + sex + grade + (1|ID) | 13662 | - | 9121.6★ | - |
|
Hypothesis 4e Caregiver resilience moderates change in internalizing symptoms |
CYRM-R_caregiver * time point + sex + grade + (1|ID) | 13654★ |
9.59 (p = 0.002)** |
9120.9 |
2.69 (p = 0.101) |
|
Hypothesis 4f Moderation is influenced by grade |
CYRM-R_caregiver * time point * grade + sex + (1|ID) | 13653 |
24.95 (p = 0.060) |
9130.7 |
20.23 (p = 0.163) |
Preferred models (in bold) were selected based on AIC values by sequentially comparing nested models. Chi-squared likelihood ratio tests were performed on nested models (i.e., each model was compared to the next simplest model) to determine a chi-squared and p-value. Models with interaction effects also included a main effect for these factors. Models of depressive and anxiety symptoms were run separately
★ indicates winning models, * indicates p < 0.05, ** p < 0.01, *** p < 0.001
All models were fitted with full information maximum likelihood estimation. Model fitting was performed using R (R Core Team, 2020) and package lme4 (Bates et al., 2020). The best fitting model was determined using chi-squared likelihood ratio tests comparing nested models (i.e., each model was compared to the next simplest model) as indicated in Table 1.
Results
Descriptive Data
Anxiety Symptoms
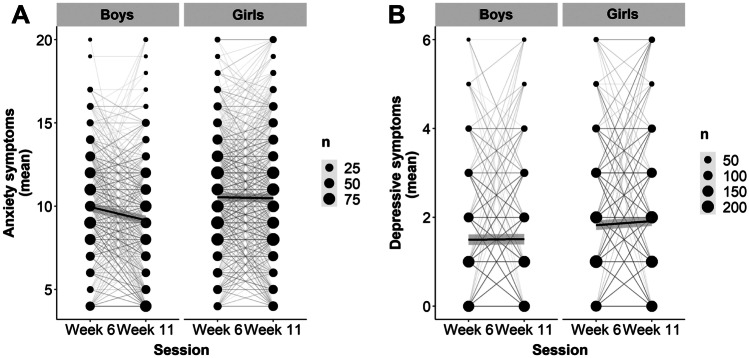
At week six, 40.5% of adolescents indicated moderate levels of self-reported anxiety symptoms and 6.7% indicated severe levels of anxiety symptoms. At week six, anxiety symptoms were also significantly higher among girls compared to boys (Table 2) (b = 0.59; SE = 0.1848, t(1329) = 3.215, p = 0.001). There were grade differences in anxiety symptoms (Table 3): pairwise comparisons revealed 11th graders had higher levels of anxiety symptoms compared to sixth graders (b = -1.03, SE = 0.36, t(1325) = -2.88, p = 0.047), seventh graders (b = -1.41, SE = 0.36, t(1325) = -3.96, p < 0.001), eighth graders (b = -1.12, SE = 0.37, t(1325) = -3.08, p = 0.026) and ninth graders (b = -1.26, SE = 0.39, t(1325) = -3.25, p = 0.015). For boys, anxiety symptoms decreased by week 11 (b = -0.78, SE = 0.21, t(2651) = -3.78, p < 0.001) while for girls anxiety symptoms remained stable (b = -0.07, SE = 0.18, t(2651) = -0.37, p = 0.983; Figure 2).
Table 2.
Summary descriptives table by sex
| Boys | Girls |
t test (df) |
p | |
|---|---|---|---|---|
| N = 557 | N = 777 | |||
| grade: | ||||
| 6 | 127 (22.8%) | 167 (21.5%) | ||
| 7 | 137 (24.6%) | 165 (21.2%) | ||
| 8 | 102 (18.3%) | 156 (20.1%) | ||
| 9 | 78 (14.0%) | 105 (13.5%) | ||
| 10 | 70 (12.6%) | 105 (13.5%) | ||
| 11 | 43 (7.72%) | 79 (10.2%) | ||
| anxiety symptoms | 9.95 (3.16) | 10.5 (3.44) | t(1329) = 3.22 | 0.001 |
| depressive symptoms | 1.49 (1.38) | 1.82 (1.46) | t(1321) = 4.13 | < 0.001 |
| caregiver resilience | 3.72 (0.58) | 3.72 (0.64) | t(1332) = 0.11 | 0.910 |
| personal resilience | 3.83 (0.60) | 3.91 (0.61) | t(1332) = 2.51 | 0.0122 |
| overall resilience | 3.77 (0.54) | 3.82 (0.57) | t(1332) = 1.46 | 0.144 |
Table 3.
Summary descriptives table by school grade
| 6 | 7 | 8 | 9 | 10 | 11 | F test (df) | p | |
|---|---|---|---|---|---|---|---|---|
| N = 294 | N = 302 | N = 258 | N = 183 | N = 175 | N = 122 | |||
| sex: | ||||||||
| boys | 127 (43.2%) | 137 (45.4%) | 102 (39.5%) | 78 (42.6%) | 70 (40.0%) | 43 (35.2%) | ||
| girls | 167 (56.8%) | 165 (54.6%) | 156 (60.5%) | 105 (57.4%) | 105 (60.0%) | 79 (64.8%) | ||
| age (years) | 11.6 (0.47) | 12.60 (0.48) | 13.50 (0.48) | 14.50 (0.49) | 15.40 (0.53) | 16.50 (0.49) | < 0.001 | |
| anxiety symptoms | 10.3 (3.37) | 9.92 (3.11) | 10.20 (3.33) | 10.10 (3.22) | 10.60 (3.32) | 11.30 (3.79) | F(5, 1325) = 3.63 | 0.003 |
| depressive symptoms | 1.56 (1.38) | 1.63 (1.42) | 1.74 (1.47) | 1.61 (1.36) | 1.81 (1.41) | 1.94 (1.61) | F(5, 1317) = 1.78 | 0.113 |
| caregiver resilience | 3.80 (0.69) | 3.72 (0.61) | 3.64 (0.59) | 3.73 (0.61) | 3.72 (0.57) | 3.69 (0.53) | F(5, 2662) = 3.93 | 0.082 |
| personal resilience | 3.87 (0.69) | 3.84 (0.60) | 3.82 (0.59) | 3.92 (0.60) | 3.94 (0.57) | 3.92 (0.51) | F(5, 2662) = 2.58 | 0.245 |
| overall resilience | 3.84 (0.64) | 3.78 (0.56) | 3.73 (0.54) | 3.82 (0.55) | 3.83 (0.52) | 3.80 (0.47) | F(5, 2662) = 2.53 | 0.278 |
Grade refers to school grade at week six
Fig. 2.
Plot of individual trajectories of symptoms of anxiety (A) and depression (B) by sex. The black line depicts the mean level of anxiety or depression symptoms by sex. Size of each dot represents the number of participants who endorsed each score
Depressive Symptoms
At week six, 25% of students’ self-reported depressive symptoms met the screening threshold for major depressive disorder. Also at week six, girls had significantly higher levels of depressive symptoms compared to boys (Table 2) (b = 0.33, SE = 0.08, t(1321) = 4.13, p < 0.001), but depressive symptoms did not differ significantly by grade (Table 3). Depressive symptoms were stable between week six and week 11 for boys (b = -0.01, SE = 0.09, t(2639) = -0.15, p = 0.999) and girls (b = 0.09, SE = 0.07, t(2639) = 1.22, p = 0.612, Figure 2).
Resilience
Overall resilience (b = 0.05, SE = 0.03, t(1332) = 1.46, p = 0.144) and caregiver resilience (b < 0.01, SE = 0.03, t(1332) = 0.11, p = 0.910) were not significantly higher for girls compared to boys, but personal resilience was higher for girls compared to boys (b = 0.08, SE = 0.03, t(1332) = 2.51, p = 0.0122).
Models
We explored two main questions: whether different sources of resilience (overall, personal, and caregiver) moderated the change in anxiety and depressive symptoms, and whether sex or grade interacted with the moderation.
Anxiety Symptoms
Comparisons of the models outlined in Table 1 revealed four winning models (in parentheses we indicate the hypothesis that won). Overall resilience, personal resilience, and caregiver resilience moderated the change in anxiety symptoms. Overall resilience interacted with sex (Hypothesis 2), but not with grade (Hypothesis 3a). Subscales (i.e., personal and caregiver resilience) did not interact with grade (Hypothesis 4b, Hypothesis 4e).
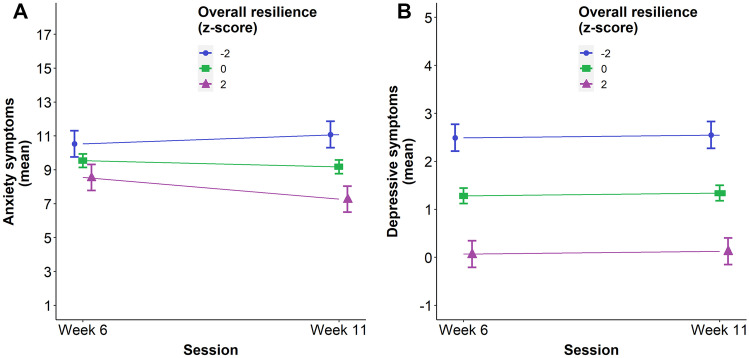
Participants with higher overall resilience, personal resilience, and caregiver resilience had lower levels of anxiety symptoms at week six (Table 4). In addition, participants with higher levels of resilience reported greater decreases in anxiety symptoms (Table 4, Fig. 2A). The change was similar for all grades (Fig. 3).
Table 4.
Parameter estimates for the best fitting models with anxiety symptoms as an outcome
| Hypothesis 2 | Hypothesis 3a | Hypothesis 4b | Hypothesis 4e | |
|---|---|---|---|---|
| Intercept | 9.94 *** | 9.54 *** | 9.50 *** | 9.57 *** |
| [9.66, 10.23] | [9.14, 9.94] | [9.10, 9.90] | [9.17, 9.98] | |
| Overall Resilience | -0.14 | -0.28 ** | ||
| [-0.43, 0.16] | [-0.46, -0.09] | |||
| Time Point | -0.80 *** | -0.36 *** | -0.36 *** | -0.36 *** |
| [-1.08, -0.53] | [-0.54, -0.18] | [-0.54, -0.18] | [-0.54, -0.18] | |
| Sex | 0.61 ** | 0.95 *** | 0.97 *** | 0.92 *** |
| [0.24, 0.99] | [0.63, 1.28] | [0.65, 1.30] | [0.60, 1.25] | |
| Overall Resilience: Time Point | -0.25 | -0.26 ** | ||
| [-0.54, 0.03] | [-0.44, -0.08] | |||
| Overall Resilience: Sex | -0.22 | |||
| [-0.59, 0.16] | ||||
| Time Point: Sex | 0.76 *** | |||
| [0.40, 1.12] | ||||
| Overall Resilience: Time Point: Sex | -0.03 | |||
| [-0.40, 0.33] | ||||
| 7th grade | -0.04 | -0.02 | -0.05 | |
| [-0.53, 0.44] | [-0.51, 0.46] | [-0.53, 0.44] | ||
| 8th grade | 0.13 | 0.17 | 0.12 | |
| [-0.37, 0.64] | [-0.33, 0.68] | [-0.39, 0.63] | ||
| 9th grade | 0.10 | 0.14 | 0.07 | |
| [-0.46, 0.66] | [-0.42, 0.70] | [-0.49, 0.63] | ||
| 10th grade | 0.41 | 0.46 | 0.37 | |
| [-0.15, 0.98] | [-0.10, 1.03] | [-0.19, 0.94] | ||
| 11th grade | 1.26 *** | 1.31 *** | 1.22 *** | |
| [0.62, 1.89] | [0.67, 1.94] | [0.58, 1.86] | ||
| Personal Resilience | -0.31 ** | |||
| [-0.49, -0.12] | ||||
| Personal Resilience: Time Point | -0.19 * | |||
| [-0.37, -0.01] | ||||
| Caregiver Resilience | -0.21 * | |||
| [-0.39, -0.02] | ||||
| Caregiver Resilience: Time Point | -0.28 ** | |||
| [-0.46, -0.10] | ||||
| N | 2655 | 2655 | 2655 | 2655 |
| N (id) | 1334 | 1334 | 1334 | 1334 |
| R2 (fixed) | 0.04 | 0.05 | 0.04 | 0.04 |
| R2 (total) | 0.56 | 0.56 | 0.56 | 0.56 |
Girls and 6th grade students are reference levels, Hypothesis 3a incorporates overall resilience as a predictor, Hypothesis 4b incorporates personal resilience as a predictor, Hypothesis 4e incorporates caregiver resilience as a predictor. All continuous predictors are Girlsmean-centered and scaled by 1 standard deviation. Standard errors are heteroskedasticity robust. Asterisks indicate significance at p < 0.05 (*), p < 0.01 (**) and p < 0.001 (***). Refer to Table 1 for details on each model
Fig. 3.
(Color online) Plot of simple slopes of symptoms of anxiety (left) and depression (right) by overall resilience. Error bars represent SE
Depressive Symptoms
Depressive symptoms did not change significantly from week six to week 11 in our sample. Neither overall resilience nor the resilience subscales significantly moderated change in depression symptoms. Comparisons of the models outlined in Table 1 revealed four winning models (in parentheses we indicate the hypothesis that won). Overall resilience, personal resilience, and caregiver resilience did not moderate the change in depressive symptoms (Hypothesis 3 baseline, Hypothesis 4a, Hypothesis 4d), and we did not find an interaction with sex (Baseline) or grade (Hypothesis 3 Baseline). Similarly, subscales did not interact with grade (Hypothesis 4a, Hypothesis 4d).
There were significant main effects for overall resilience, personal resilience, and caregiver resilience on depressive symptoms, but, unlike the analyses of anxiety symptoms, overall resilience, personal resilience, and caregiver resilience did not significantly moderate change in depressive symptoms (Table 5, Fig. 3).
Table 5.
Parameter estimates for the best fitting models with depressive symptoms as an outcome
| Baseline | Hypothesis 3 Baseline | Hypothesis 4a | Hypothesis 4d | |
|---|---|---|---|---|
| Intercept | 1.46 *** | 1.28 *** | 1.25 *** | 1.31 *** |
| [1.35, 1.56] | [1.12, 1.44] | [1.08, 1.41] | [1.15, 1.47] | |
| Time Point | 0.06 | 0.06 | 0.06 | 0.06 |
| [-0.02, 0.14] | [-0.02, 0.14] | [-0.02, 0.14] | [-0.02, 0.14] | |
| Sex | 0.39 *** | 0.38 *** | 0.39 *** | 0.36 *** |
| [0.26, 0.53] | [0.25, 0.51] | [0.26, 0.53] | [0.23, 0.49] | |
| 7th grade | 0.14 | 0.16 | 0.13 | |
| [-0.05, 0.33] | [-0.03, 0.35] | [-0.06, 0.33] | ||
| 8th grade | 0.27 ** | 0.30 ** | 0.25 * | |
| [0.07, 0.46] | [0.10, 0.51] | [0.05, 0.45] | ||
| 9th grade | 0.14 | 0.17 | 0.11 | |
| [-0.08, 0.36] | [-0.05, 0.39] | [-0.11, 0.33] | ||
| 10th grade | 0.28 * | 0.31 ** | 0.24 * | |
| [0.05, 0.50] | [0.09, 0.54] | [0.01, 0.46] | ||
| 11th grade | 0.50 *** | 0.54 *** | 0.46 *** | |
| [0.25, 0.75] | [0.29, 0.79] | [0.21, 0.71] | ||
| Overall Resilience | -0.34 *** | -0.34 *** | ||
| [-0.41, -0.28] | [-0.40, -0.28] | |||
| Personal Resilience | -0.30 *** | |||
| [-0.36, -0.24] | ||||
| Caregiver Resilience | -0.33 *** | |||
| [-0.39, -0.26] | ||||
| N | 2643 | 2643 | 2643 | 2643 |
| N (id) | 1333 | 1333 | 1333 | 1333 |
| R2 (fixed) | 0.07 | 0.08 | 0.07 | 0.07 |
| R2 (total) | 0.45 | 0.45 | 0.45 | 0.45 |
Girls and 6th grade students are reference levels, Hypothesis 3 baseline incorporates overall resilience as a predictor, Hypothesis 4a incorporates personal resilience as a predictor, Hypothesis 4d incorporates caregiver resilience as a predictor. All continuous predictors are mean-centered and scaled by 1 standard deviation. Standard errors are heteroskedasticity robust.Asterisks indicate significance at p < 0.05 (*), p < 0.01 (**) and p < 0.001 (***). Refer to Table 1 for details on each model
Discussion
We investigated internalizing symptoms and social-ecological resilience in a large sample of low- and middle-income adolescents in Perú during the early and intense stages of the COVID-19 pandemic lockdowns. During the sixth week of lockdown, we found higher levels of anxiety symptoms for girls and for adolescents from higher school grades. Anxiety symptoms decreased for boys and remained stable for girls, while depressive symptoms did not change significantly across time for boys or girls from week six to week 11. Overall resilience, as well as caregiver and personal resilience alone, were associated with lower levels of anxiety and depression in week six and moderated change in anxiety symptoms, but not depressive symptoms, in week 11.
Internalizing Symptoms
School-grade Differences in Internalizing Symptoms
Compared to younger adolescents, older adolescents reported higher rates of symptoms of anxiety, but not depression, in the early stages of the COVID-19 pandemic. The positive association between anxiety and grade aligns with the general developmental pattern, observed in studies before the pandemic, of increased internalizing symptoms with age throughout adolescence (Ghandour et al., 2019; Kessler et al., 2005; 2007b; Merikangas et al., 2010; Thapar et al., 2012). Internalizing problems during adolescence could be intensified during a period of lockdown given the disruption to normal routine and increased stress. Indeed, cross-sectional evidence suggests that awareness of COVID-19 is associated with anxiety and depression among adolescents, with girls and older adolescents at highest risk (Zhou et al., 2020). An international collaboration (Barendse et al., 2021) reported that anxiety symptoms decreased in younger but not older adolescents from before to during the first six months of the pandemic. Taken together, these studies and ours suggest that older adolescents and girls may be particularly vulnerable to anxiety symptoms during lockdown. In this study, we used grade instead of age to index development to better capture the socio-ecological environment in the educational context. For example, given that the school year in Perú had just begun when the schools were forced to close, 7th graders (regardless of age) had just started to meet schoolmates and build networks. Similarly, 11th graders (regardless of age) had particular concerns about graduation. Future research should seek to better characterize these potentially differential impacts of pandemic lockdowns across developmental stages.
Although we do not have data on this sample from before the COVID-19 pandemic, at week six, symptoms of both anxiety and depression appear to be elevated. Forty percent of the sample reported moderate levels of anxiety, and an additional six percent of adolescents reported severe anxiety. One in every four students met screening criteria for a major depressive disorder. The rates of anxiety and depression in our sample were substantially higher than both the 2017 nationally representative averages from the World Health Organization (World Health Organization, 2017) and results from a 2018 survey of Peruvian adults (Hernández-Vásquez et al., 2020). However, our findings align with prevalence rates in samples of adolescents from Latin America and Perú from 2020 (United Nations Children's Fund UNICEF, 2021) and 2021 (Barendse et al., 2021).
Sex Differences in Internalizing Symptoms
Girls reported higher levels of anxiety and depressive symptoms than boys. While we originally expected that girls would have a higher prevalence of internalizing symptoms, one departure from our pre-registered analysis was that we did not consider an interaction between sex and time point. When analyzing the data, however, we realized that girls and boys had different trajectories. For girls, anxiety and depressive symptoms did not change significantly between week six and week 11 of lockdown. For boys, we observe a decrease in anxiety symptoms with time, with stable depressive symptoms. These sex differences in trajectories of internalizing problems during our five week study likely reflect pre-existing sex differences in internalizing symptoms that are amplified during adolescence (Lewinsohn et al., 1998; Martel, 2013; Salk et al., 2017) and periods of high stress. In line with these findings, many studies during COVID-19 report evidence of this sex disparity (Barendse et al., 2021; Craig et al., 2020; Halldorsdottir et al., 2021; Qi et al., 2020). This increased vulnerability to internalizing problems could be due in part to sex differences in the cognitive or affective experience of coping with stressors. Indeed, in a large study of 12,232 low-income adolescents from six countries in Asia Pacific (Bangladesh, India, Indonesia, Myanmar, Philippines, and Vietnam), girls felt more isolated, unsafe, and stressed and worried about education and household income in May–June of 2020 (Wang et al., 2021).
In a short time frame of five weeks, different trajectories of internalizing symptoms emerged between sexes. It will be important to investigate the medium- to long-term effects of the pandemic on internalizing symptom trajectories and whether these differ for boys and girls. Additionally, while girls reported higher baseline rates of personal resilience compared to boys, it is possible that it may take higher levels of personal resilience to buffer the pre-existing vulnerability to mental health that girls face (as well as structural difficulties associated with occupying an often lower social status position). Indeed, significant interactions between sex and social status as well as resilience and social status have been found for health-related behaviors in Hispanic American late adolescents (Guazzelli Williamson et al., 2020).
Social-ecological Resilience
In contrast with factors of resilience related to internal strengths such as optimism or problem-solving ability (Ko & Chang, 2019; Marx et al., 2017), here we have investigated the role of social-ecological resilience in resources related to family, community and opportunities for growth (Ungar, 2012) during the stress of the COVID-19 pandemic. Social-ecological resilience is a globally-developed measure that incorporates cultural considerations. This was important in our work with a population in Perú that is often not represented in the research literature.
Associations at “Baseline” (Week Six)
During week six of a stringent lockdown, social-ecological resilience was associated with lower anxiety and depressive symptoms in our sample. This aligns with evidence that psychological resilience, specifically social-ecological resilience, may serve as a protective factor against internalizing symptoms in the face of adversity. For example, previous research has found higher levels of psychological resilience to be associated with lower levels of anxiety in samples around the world (Beutel et al., 2010; Charney, 2003; Jefferies et al., 2021). Of note, our week six (“baseline”) measurements occurred after the pandemic had already started: students had been under strict lockdown measures for six weeks. This should frame our week six results as reflective of an adaptation to an already adverse environment characterized not only by disruptions of school and family routines but also by concerning news and uncertainty around COVID-19. As such, we expect that adolescents were already relying more heavily on psychological and ecological resources to cope and adapt, and that those endorsing higher sources of resilience would have lower internalizing symptoms.
Moderation Analyses
The main aim for this study was to investigate whether the change in depressive and anxious symptoms at the individual level was moderated by an individual’s psychological resilience during the early stages of the COVID-19 pandemic. As we predicted, we found that overall resilience, personal resilience and caregiver resilience moderated the change in anxiety symptoms. However, counter to our predictions, we did not observe a moderation of depressive symptoms (which we discuss further below).
The Importance of Personal and Caregiver Resilience in Moderating Anxiety Symptoms Across Adolescence
We further investigated the stability of personal and caregiver resilience across grades and the role of the CYRM-R resilience subscales (personal vs. caregiver) in predicting change in depressive and anxious symptoms and grade effects on this relationship. Our rationale for looking at the subscales separately was to explore developmental effects. For example, as adolescence is a developmental period of increasing autonomy and independence (Daddis, 2011; Dahl et al., 2018; Nelson et al., 2016) one might expect that caregivers would play a more critical role earlier in adolescence while personal resilience may be more impactful among older adolescents. However, in line with Jefferies et al. (2019), there were also no significant grade differences in overall resilience, caregiver resilience, and personal resilience (Jefferies et al., 2019) and we did not find evidence for an interaction between grade and resilience subscales. The stability of the role of caregiver and personal sources of social-ecological resilience across adolescents in our sample aligns with a longitudinal study of adolescents between ages 14 and 17 where no changes were found in individual sources of resilience from friendship or family sources over time (Fritz et al., 2019). Our findings suggest that both caregiver and personal resilience play an important role in moderating anxiety symptoms across adolescence. Moreover, caregivers may play an important protective role throughout adolescence, regardless of developmental stage (Collins & Laursen, 2006; Reed et al., 1996). Parent and caregiver influence during adolescence has been observed in sleep hygiene (Peltz et al., 2020), motivation and achievement (Kriegbaum et al., 2016), substance use and peer influence (Wood et al., 2004), and changes in anxiety and depression (Butterfield et al., 2021). Maternal warmth has also been found to attenuate anxiety and depression in adolescents with high-risk for mental health (Butterfield et al., 2021). In another study of four low to middle income countries, “strong parent–child relationships emerged as a significant protective factor” against anxiety and depression for young people in Perú during the COVID-19 pandemic (Porter et al., 2021). Overall, our findings suggest that both personal and caregiver sources of resilience remain important for mental health, particularly symptoms of anxiety, throughout adolescence.
While we do not present comparisons to other countries in this study, caregiver relationships may be particularly important in Perú due to a strong cultural emphasis on familial relationships (Child Trends, 2013; Social Trends Institute, 2017). Across countries, caregiver resilience has been demonstrated as the most important driver of adolescent resilience in stressful contexts (Höltge et al., 2021). Future studies should continue exploring the role of personal versus caregiver resilience as caregiver relationships may be particularly important during COVID-19 due to increased time at home and increased contact with caregivers as a result of lockdown.
Personal Versus Caregiver Resilience: The Influence of Sex
In line with previous developmental research on social-ecological resilience, girls reported slightly higher personal resilience than boys (Jefferies et al., 2019). However, we did not find previously reported sex differences on caregiver resilience (Jefferies et al., 2019) boys and girls in our sample reported similar scores. The lack of sex differences observed for the caregiver subscale in our sample may reflect cultural differences between our Peruvian sample and the Canadian sample where previous gender differences were reported. It is also possible that proximity to caregivers as a result of lockdown may eradicate gender differences in caregiver subscale scores.
Social-ecological Resilience Did Not Moderate Change in Depressive Symptoms
Overall social-ecological, personal, and caregiver resilience were not associated with a change in depressive symptoms across the five-week period. This may be due, at least in part, to the fact that there was not a significant change in depressive symptoms between time points. There are several plausible explanations why we did not find a significant decrease in depressive symptoms during lockdown. First, stressors were already in place by the first time point analyzed in this study (the sixth week of lockdown in Perú). Additionally, these stressors (e.g., health implications of the virus and economic impacts and the lockdown) continued, and in many cases may have increased, across the five weeks in our study. There are also important methodological considerations which may have impacted this relationship including the relative proximity of the first and last time point (five weeks) and because our short measure of depressive symptoms was a two-question screener which may not have captured changes in depressive symptoms or expected sex differences with sufficient sensitivity. However, in a different subsample of students that used the 8-item PROMIS measure of depression, we found a similar pattern of no change in self-reported depressive symptoms between week six and week 11, and no interaction between time point and sex. Similarly to the current results, girls had higher overall levels of depressive symptoms (Magis-Weinberg, unpublished data). Taken together, these findings seem to indicate that levels of depressive symptoms were fairly stable in the first few weeks of lockdown. Additionally, rates of depression increase with age in adolescence (Ghandour et al., 2019; Kessler et al., 2007a; Patton et al., 2014; Thapar et al., 2012) and our sample composition included a higher proportion of younger than older adolescents. Follow up studies should incorporate more comprehensive measures of anxiety and depression.
Strengths and Limitations
Here, we included a large and diverse sample of Peruvian adolescents in low- and middle-income settings, a population that is underrepresented in the research literature. In addition, we include pre-registered analyses of longitudinal trajectories during the early stages of the pandemic. Despite these strengths, there are some limitations to be noted. First, we were limited to short self-reported measures for all variables due to time constraints. The PROMIS and PHQ-2 measures are designed as screeners in a “first-step” approach and are not intended to be used alone for diagnostic purposes. Thus, these results warrant follow up studies with more in-depth assessments of anxiety and depression. Similarly, our self-report measure of social-ecological resilience was based on youths’ perceptions and while an adolescent might be supported at home, they might not perceive that to be the case. Thus, future research should also study whether and why youth’s perceptions might differ from objective facets of resilience. Nevertheless, we show that youth’s perceptions of resilience and mental health matter, and do relate to change in anxiety symptoms across a highly stressful period of lockdown.
It should also be noted that our data collection coincided with the delivery of school curricula to promote well-being and healthy technology use during the COVID-19 lockdown. It is possible that this curricula had an impact on internalizing symptoms at our second time point (week 11), which limits our interpretation of social-ecological resilience as the only driver for attenuation of internalizing symptoms. However, given the brief, light-touch nature of the intervention, which provided general coping strategies for one hour once a week as part of a broader curriculum (e.g., short videos on mindfulness and gratitude exercises; (Magis-Weinberg et al., 2021)), it is unlikely that this would be enough to counteract the effects of such a large stressor like the COVID-19 pandemic. If anything, the inclusion of the curriculum suggests that our estimates of the impact of psychological resilience may be conservative.
Additionally, as our assessment schedule was determined by the needs and schedule of the schools we work with early on during the pandemic, only two timepoints of anxiety and depression were collected (week six and week 11) and resilience was collected during week 10, only one week prior to our second assessment of anxiety and depression. To truly understand the temporal nature of these influences throughout the pandemic, future research should include a greater number of timepoints with varying duration of time between data collection. As our study captures the initial period of the pandemic which coincided with a very strict lockdown, our data may reflect acute responses. In an effort to capture potential changes, accentuations, or cascading impacts of the stressors over time, future research should continue to gather data on adolescent well-being throughout the course of the pandemic (Masten & Motti-Stefanidi, 2020).
Finally, while our participants consisted of a large sample of low- to middle-income Peruvian youth, these results may not generalize to other countries, due to the potential for country-specific effects of resilience. Additionally, as this sample is composed of low- to middle-income students in a private school network, it is unclear to what extent these findings could be generalized to the larger adolescent population in Perú. Recent reports suggest that 18% of students in Latin America are not receiving any form of education, and thus protective effects of social-ecological resilience (which include value of education) may differ – and perhaps be particularly important – in these groups compared to students included in our study (all of whom continued to receive remote instruction throughout the pandemic) (UNICEF, 2021). Future research should include multiple time points to fully capture the long-term effects of the pandemic on adolescent depression and anxiety.
Conclusion
In a large sample of Peruvian students, we find that during the early and intense stages of the COVID-19 pandemic, rates of anxiety symptoms were higher among older adolescents and rates of anxiety and depressive symptoms were higher among girls. Social-ecological sources of resilience were associated with lower anxiety and depressive symptoms at week six of lockdown. In addition, overall social-ecological resilience as well as personal and caregiver resilience tempered the increase in anxiety symptoms between week six and week 11 of lockdown for both younger and older adolescents. This aligns with research emphasizing caregiver roles of continued protection against the development of anxiety and depression for adolescents of all ages. These findings underscore the importance of both personal and caregiver sources of resilience for interventions aimed at improving adolescent mental health during COVID-19 – perhaps especially in settings such as Perú where strong family values may contribute to the particularly important role of caregivers in social-ecological resilience.
Acknowledgements
The authors would like to thank adolescents and their families for their participation in the study, especially during a particularly challenging time in April and May 2020.
Authors' Contributions
VGW and LMW contributed to the conceptualization of the manuscript as well as running the analyses. MEAB ran data analyses and revised the manuscript. LMW and ELB developed the study protocol, identified surveys and collected data. VGW and LMW wrote the manuscript. JP and RED reviewed and revised the manuscript. All authors approved the final version of the manuscript.
Funding
This research was supported by funding from Carlos Rodriguez-Pastor and the Bezos Family Foundation.
Availability of Data and Material
Data are available by request.
Code Availability
Code available by request.
Compliance with Ethical Standards
Ethics Approval
The study was conducted in accordance with the American Psychological Association ethical standards and approval was granted by the Institutional Review Board at the University of California, Berkeley.
Consent to Participate
Participants’ parents gave passive informed consent for participation.
Consent for Publication
All listed authors have approved the manuscript for publication.
Conflicts of Interest/Competing Interests
Lucía Magis Weinberg and Estelle Berger collaborate with Innova Schools to inform curricula development and implementation. Other authors do not have conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alvarez-Risco A, Mejia CR, Delgado-Zegarra J, Del-Aguila-Arcentales S, Arce-Esquivel AA, Valladares-Garrido MJ, Rosas Del Portal M, Villegas LF, Curioso WH, Sekar MC, Yáñez JA. The Peru Approach against the COVID-19 Infodemic: Insights and Strategies. The American Journal of Tropical Medicine and Hygiene. 2020;103(2):583–586. doi: 10.4269/ajtmh.20-0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barendse, M., Flannery, J., Cavanagh, C., Aristizabal, M., Becker, S. P., Berger, E., Breaux, R., Campione-Barr, N., Church, J. A., Crone, E., Dahl, R., Dennis-Tiwary, T. A., Dvorsky, M., Dziura, S., Groep, S. van de, Ho, T., Killoren, S. E., Langberg, J., Larguinho, T., & Pfeifer, J. (2021). Longitudinal change in adolescent depression and anxiety symptoms from before to during the COVID-19 pandemic: An international collaborative of 12 samples. PsyArXiv. 10.31234/osf.io/hn7us
- Bates, D., Maechler, M., Bolker [aut, B., cre, Walker, S., Christensen, R. H. B., Singmann, H., Dai, B., Scheipl, F., Grothendieck, G., Green, P., Fox, J., Bauer, A., & simulate.formula), P. N. K. (shared copyright on. (2020). lme4: Linear Mixed-Effects Models using “Eigen” and S4 (1.1–26) [Computer software]. https://CRAN.R-project.org/package=lme4
- Beutel ME, Glaesmer H, Wiltink J, Marian H, Brähler E. Life satisfaction, anxiety, depression and resilience across the life span of men. The Aging Male. 2010;13(1):32–39. doi: 10.3109/13685530903296698. [DOI] [PubMed] [Google Scholar]
- Butterfield RD, Silk JS, Lee KH, Siegle GS, Dahl RE, Forbes EE, Ryan ND, Hooley JM, Ladouceur CD. Parents still matter! Parental warmth predicts adolescent brain function and anxiety and depressive symptoms 2 years later. Development and Psychopathology. 2021;33(1):226–239. doi: 10.1017/S0954579419001718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caqueo-Urízar A, Urzúa A, Escobar-Soler C, Flores J, Mena-Chamorro P, Villalonga-Olives E. Effects of Resilience and Acculturation Stress on Integration and Social Competence of Migrant Children and Adolescents in Northern Chile. International Journal of Environmental Research and Public Health. 2021;18(4):2156. doi: 10.3390/ijerph18042156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charney DS. The psychobiology of resilience and vulnerability to anxiety disorders: Implications for prevention and treatment. Dialogues in Clinical Neuroscience. 2003;5(3):207–221. doi: 10.31887/DCNS.2003.5.3/dcharney. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Child Trends. (2013). How Family Life Differs in Central and South America. Retrieved March 31, 2021 from https://www.childtrends.org/blog/how-family-life-differs-in-central-and-south-america
- Collins, W. A., & Laursen, B. (2006). Parent-Adolescent Relationships. In Close relationships: Functions, forms and processes (pp. 111–125). Psychology Press/Taylor & Francis (UK).
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Craig, S., Ames, M. E., Bondi, B. C., & Pepler, D. J. (2020). Canadian Adolescents’ Mental Health and Substance Use during the COVID-19 Pandemic: Associations with COVID-19 Stressors. PsyArXiv. 10.31234/osf.io/kprd9
- Daddis C. Desire for increased autonomy and adolescents’ perceptions of peer autonomy: “Everyone else can; why can’t I?”. Child Development. 2011;82(4):1310–1326. doi: 10.1111/j.1467-8624.2011.01587.x. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Allen NB, Wilbrecht L, Suleiman AB. Importance of investing in adolescence from a developmental science perspective. Nature. 2018;554(7693):441–450. doi: 10.1038/nature25770. [DOI] [PubMed] [Google Scholar]
- Dulin AJ, Dale SK, Earnshaw VA, Fava JL, Mugavero MJ, Napravnik S, Hogan JW, Carey MP, Howe CJ. Resilience and HIV: A review of the definition and study of resilience. AIDS Care. 2018;30(sup5):S6–S17. doi: 10.1080/09540121.2018.1515470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorsky MR, Breaux R, Becker SP. Finding ordinary magic in extraordinary times: Child and adolescent resilience during the COVID-19 pandemic. European Child & Adolescent Psychiatry. 2021;30(11):1829–1831. doi: 10.1007/s00787-020-01583-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer, O. (2020). Covid-19 hot spots appear across Latin America. BMJ, 369, m2182. 10.1136/bmj.m2182 [DOI] [PubMed]
- Fritz J, Stochl J, Fried EI, Goodyer IM, van Borkulo CD, Wilkinson PO, van Harmelen A-L. Unravelling the complex nature of resilience factors and their changes between early and later adolescence. BMC Medicine. 2019;17(1):203. doi: 10.1186/s12916-019-1430-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni AJ. The Need to Contribute During Adolescence. Perspectives on Psychological Science. 2019;14(3):331–343. doi: 10.1177/1745691618805437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B, Wilson I, Berhane HY, Deyessa N, Bahretibeb Y, Wondimagegn D, ShibreKelkile T, Berhane Y, Fann JR, Williams MA. Diagnostic validity of the Patient Health Questionnaire-2 (PHQ-2) among Ethiopian adults. Comprehensive Psychiatry. 2016;70:216–221. doi: 10.1016/j.comppsych.2016.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghandour RM, Sherman LJ, Vladutiu CJ, Ali MM, Lynch SE, Bitsko RH, Blumberg SJ. Prevalence and Treatment of Depression, Anxiety, and Conduct Problems in US Children. The Journal of Pediatrics. 2019;206:256–267. doi: 10.1016/j.jpeds.2018.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E, Wen H, Miller BF. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatrics. 2020;174(9):819. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Guazzelli Williamson, V., Barendse, M., Pfeifer, J. H., & Magis-Weinberg, L. (2020). Psychological Resilience and Depression/Anxiety among Peruvian Adolescents During COVID-19. Open Science Framework. 10.17605/OSF.IO/7FGEH
- Halldorsdottir, T., Thorisdottir, I. E., Meyers, C. C., Asgeirsdottir, B. B., Kristjansson, A. L., Valdimarsdottir, H. B., Allegrante, J. P., & Sigfusdottir, I. D. (2021). Adolescent well‐being amid the Covid‐19 pandemic: Are girls struggling more than boys? JCPP Advances, 1(2). 10.1002/jcv2.12027 [DOI] [PMC free article] [PubMed]
- Hernández-Vásquez A, Vargas-Fernández R, Bendezu-Quispe G, Grendas LN. Depression in the Peruvian population and its associated factors: Analysis of a national health survey. Journal of Affective Disorders. 2020;273:291–297. doi: 10.1016/j.jad.2020.03.100. [DOI] [PubMed] [Google Scholar]
- Höltge J, Theron L, Cowden RG, Govender K, Maximo SI, Carranza JS, Kapoor B, Tomar A, van Rensburg A, Lu S, Hu H, Cavioni V, Agliati A, Grazzani I, Smedema Y, Kaur G, Hurlington KG, Sanders J, Munford R, Ungar M. A Cross-Country Network Analysis of Adolescent Resilience. Journal of Adolescent Health. 2021;68(3):580–588. doi: 10.1016/j.jadohealth.2020.07.010. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Benner AD, Erdem G, Lansford JE, Makila LM, Petrie RC, SRA COVID-19 Response Team Adolescence Amid a Pandemic: Short- and Long-Term Implications. Journal of Research on Adolescence: THe Official Journal of the Society for Research on Adolescence. 2021;31(3):820–835. doi: 10.1111/jora.12671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Estadística e Informática. (2017). Dinámicas Étnicas en el Perú: Hacia una Caracterización y Tipología para el diseño de Políticas Públicas. https://www.inei.gob.pe/
- Jefferies P, Höltge J, Ungar M. Social Anxiety and Resilience: Associations Vary by Country and Sex. Adversity and Resilience Science. 2021;2(1):51–62. doi: 10.1007/s42844-020-00026-2. [DOI] [Google Scholar]
- Jefferies P, McGarrigle L, Ungar M. The CYRM-R: A Rasch-Validated Revision of the Child and Youth Resilience Measure. Journal of Evidence-Based Social Work. 2019;16(1):70–92. doi: 10.1080/23761407.2018.1548403. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry. 2007;20(4):359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Angermeyer M, Anthony JC, de Graaf R, Demyttenaere K, Gasquet I, de Girolamo G, Gluzman S, Gureje O, Haro JM, Kawakami N, Karam A, Levinson D, Medina Mora ME, Oakley Browne MA, Posada-Villa J, Stein DJ, Adley Tsang CH, Aguilar-Gaxiola S, Alonso J, Ustün TB. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 2007;6(3):168–176. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Ko C-YA, Chang Y. Investigating the Relationships Among Resilience, Social Anxiety, and Procrastination in a Sample of College Students. Psychological Reports. 2019;122(1):231–245. doi: 10.1177/0033294118755111. [DOI] [PubMed] [Google Scholar]
- Kriegbaum K, Villarreal B, Wu V, Heckhausen J. Parents Still Matter: Patterns of Shared Agency With Parents Predict College Students’ Academic Motivation and Achievement. Motivation Science. 2016;2:97–115. doi: 10.1037/mot0000033. [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Guazzelli Williamson, V., Lee, A. M., Miller, D., Huo, T., Maner, J. K., & Cardel, M. (2021). Psychological Resilience, Experimentally Manipulated Social Status, and Dietary Intake among Adolescents. Nutrients, 13(3), 806. 10.3390/nu13030806 [DOI] [PMC free article] [PubMed]
- Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, Allen NB. Gender differences in anxiety disorders and anxiety symptoms in adolescents. Journal of Abnormal Psychology. 1998;107(1):109–117. doi: 10.1037/0021-843X.107.1.109. [DOI] [PubMed] [Google Scholar]
- Llistosella M, Gutiérrez-Rosado T, Rodríguez-Rey R, Liebenberg L, Bejarano Á, Gómez-Benito J, Limonero JT. Adaptation and Psychometric Properties of the Spanish Version of Child and Youth Resilience Measure (CYRM-32) Frontiers in Psychology. 2019;10:1410. doi: 10.3389/fpsyg.2019.01410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Linney C, McManus MN, Borwick C, Crawley E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. Journal of the American Academy of Child and Adolescent Psychiatry. 2020;59(11):1218–1239.e3. doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) Journal of Psychosomatic Research. 2005;58(2):163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Magis-Weinberg L, Berger E, Gys C, Dahl R. Study Protocol: Transitions, a school based intervention to promote digital citizenship in low- and middle income secondary school students in Perú. OSF Preprints; 2021. [Google Scholar]
- Manea L, Gilbody S, Hewitt C, North A, Plummer F, Richardson R, Thombs BD, Williams B, McMillan D. Identifying depression with the PHQ-2: A diagnostic meta-analysis. Journal of Affective Disorders. 2016;203:382–395. doi: 10.1016/j.jad.2016.06.003. [DOI] [PubMed] [Google Scholar]
- Martel MM. Sexual selection and sex differences in the prevalence of childhood externalizing and adolescent internalizing disorders. Psychological Bulletin. 2013;139(6):1221–1259. doi: 10.1037/a0032247. [DOI] [PubMed] [Google Scholar]
- Marx M, Young SY, Harvey J, Rosenstein D, Seedat S. An Examination of Differences in Psychological Resilience between Social Anxiety Disorder and Posttraumatic Stress Disorder in the Context of Early Childhood Trauma. Frontiers in Psychology. 2017 doi: 10.3389/fpsyg.2017.02058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS, Motti-Stefanidi F. Multisystem Resilience for Children and Youth in Disaster: Reflections in the Context of COVID-19. Adversity and Resilience Science. 2020;1(2):95–106. doi: 10.1007/s42844-020-00010-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas, K. R., He, J. -P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., & Swendsen, J. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication--AdolescentSupplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49(10), 980–989. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed]
- Munayco CV, Tariq A, Rothenberg R, Soto-Cabezas GG, Reyes MF, Valle A, Rojas-Mezarina L, Cabezas C, Loayza M, Chowell G, Garro DC, Vasquez KM, Castro ES, Ordinola IS, Mimbela JM, Cornejo KM, Quijano FC, La Torre Rosillo L, Ibarguen LO, Ramos W. Early transmission dynamics of COVID-19 in a southern hemisphere setting: Lima-Peru: February 29th–March 30th, 2020. Infectious Disease Modelling. 2020;5:338–345. doi: 10.1016/j.idm.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson BW, Pettitt A, Flannery JE, Allen NB. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PLoS ONE. 2020;15(11):e0241990. doi: 10.1371/journal.pone.0241990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EE, Jarcho JM, Guyer AE. Social re-orientation and brain development: An expanded and updated view. Developmental Cognitive Neuroscience. 2016;17:118–127. doi: 10.1016/j.dcn.2015.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, Olsson CA, Moran P. The prognosis of common mental disorders in adolescents: A 14-year prospective cohort study. Lancet (London, England) 2014;383(9926):1404–1411. doi: 10.1016/S0140-6736(13)62116-9. [DOI] [PubMed] [Google Scholar]
- Peltz, J. S., Rogge, R. D., & Connolly, H. (2020). Parents still matter: The influence of parental enforcement of bedtime on adolescents’ depressive symptoms. Sleep, 43(5). 10.1093/sleep/zsz287 [DOI] [PubMed]
- Peruvian Health Ministry (2020). MINSA | Datos Abiertos Minsa y Gestión del Conocimiento en Covid-19. Accessed March 31, 2021, from https://www.minsa.gob.pe/datosabiertos/?op=22
- Pfeifer JH, Allen NB. Puberty Initiates Cascading Relationships Between Neurodevelopmental, Social, and Internalizing Processes Across Adolescence. Biological Psychiatry. 2021;89(2):99–108. doi: 10.1016/j.biopsych.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item Banks for Measuring Emotional Distress From the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, Anxiety, and Anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter C, Favara M, Hittmeyer A, Scott D, Sánchez Jiménez A, Ellanki R, Woldehanna T, Duc LT, Craske MG, Stein A. Impact of the COVID-19 pandemic on anxiety and depression symptoms of young people in the global south: Evidence from a four-country cohort study. British Medical Journal Open. 2021;11(4):e049653. doi: 10.1136/bmjopen-2021-049653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presidency of the Council of Ministers. (2020a). Decreto Supremo N° 044–2020-PCM. Retrieved October 15, 2021 from https://www.gob.pe/institucion/pcm/normas-legales/460472-044-2020-pcm
- Presidency of the Council of Ministers. (2020b). Decreto Supremo N° 116–-2020-PCM. Retrieved October 15, 2021 from https://www.gob.pe/institucion/pcm/normas-legales/738529-116-2020-pcm
- Qi, M., Zhou, S. J., Guo, Z. C., Zhang, L. G., Min, H. J., Li, X. M., & Chen, J. X. (2020). The Effect of Social Support on Mental Health in Chinese Adolescents During the Outbreak of COVID-19. Journal of Adolescent Health, 67(4). 10.1016/j.jadohealth.2020.07.001 [DOI] [PMC free article] [PubMed]
- R Core Team. (2020). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/
- Resilience Research Centre. (2018). CYRM and ARM user manual. Halifax, NS: Resilience Research Centre, Dalhousie University. Retrieved from http://www.resilienceresearch.org/
- Reed L, Moneta G, Richards MH, Holmbeck G, Duckett E. Changes in adolescents’ daily interactions with their families from ages 10 to 18: Disengagement and transformation. Developmental Psychology. 1996;32(4):744–754. doi: 10.1037/0012-1649.32.4.744. [DOI] [Google Scholar]
- Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin. 2017;143(8):783–822. doi: 10.1037/bul0000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. The Lancet Child & Adolescent Health. 2018;2(3):223–228. doi: 10.1016/S2352-4642(18)30022-1. [DOI] [PubMed] [Google Scholar]
- Schalet BD, Pilkonis PA, Yu L, Dodds N, Johnston KL, Yount S, Riley W, Cella D. Clinical validity of PROMIS Depression, Anxiety, and Anger across diverse clinical samples. Journal of Clinical Epidemiology. 2016;73:119–127. doi: 10.1016/j.jclinepi.2015.08.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smirni, P., Lavanco, G., & Smirni, D. (2020). Anxiety in Older Adolescents at the Time of COVID-19. Journal of Clinical Medicine, 9(10). 10.3390/jcm9103064 [DOI] [PMC free article] [PubMed]
- Social Trends Institute. (2017). The World Family Map 2017: Mapping Family Change and Child Well-being Outcomes | Social Trends Institute. Retrieved March 31, 2021, from https://www.socialtrendsinstitute.org/publications/family/the-world-family-map-2017-mapping-family-change-and-child-well-being-outcomes
- Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, Il Shin J, Kirkbride JB, Jones P, Kim JH, Kim JY, Carvalho AF, Seeman MV, Correll CU, Fusar-Poli P. Age at onset of mental disorders worldwide: Large-scale meta-analysis of 192 epidemiological studies. Molecular Psychiatry. 2022;27(1):281–295. doi: 10.1038/s41380-021-01161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley DJ, Spence JR. Reproducible Tables in Psychology Using the apaTables Package. Advances in Methods and Practices in Psychological Science. 2018;1(3):415–431. doi: 10.1177/2515245918773743. [DOI] [Google Scholar]
- Subirana, I., Sanz, H., & Vila, J. (2014). Building Bivariate Tables: The compareGroups Package for R. Journal of Statistical Software, 57(1), 1–16. 10.18637/jss.v057.i12
- Telles E, Paschel T. Who is black, white, or mixed race? How skin color, status, and nation shape racial classification in Latin America. AJS; American Journal of Sociology. 2014;120(3):864–907. doi: 10.1086/679252. [DOI] [PubMed] [Google Scholar]
- Teresi JA, Ocepek-Welikson K, Kleinman M, Ramirez M, Kim G. Measurement Equivalence of the Patient Reported Outcomes Measurement Information System® (PROMIS®) Anxiety Short Forms in Ethnically Diverse Groups. Psychological Test and Assessment Modeling. 2016;58(1):183–219. [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379(9820):1056–1067. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungar M. Nurturing Hidden Resilience in At-Risk Youth in Different Cultures. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2006;15(2):53–58. [PMC free article] [PubMed] [Google Scholar]
- Ungar M. Resilience across Cultures. The British Journal of Social Work. 2008;38(2):218–235. doi: 10.1093/bjsw/bcl343. [DOI] [Google Scholar]
- Ungar, M. (2018). Systemic resilience: Principles and processes for a science of change in contexts of adversity. Ecology and Society, 23(4). 10.5751/es-10385-230434
- Ungar, M. (Ed.). (2012). The social ecology of resilience: A handbook of theory and practice (pp. xv, 463). Springer Science + Business Media. 10.1007/978-1-4614-0586-3
- UNICEF. (2021). The impact of COVID-19 on the mental health of adolescents and youth. Retrieved March 31, 2021, from https://www.unicef.org/lac/en/impact-covid-19-mental-health-adolescents-and-youth
- United Nations Children’s Fund. (2021). The State of the World’s Children 2021: On My Mind – Promoting, protecting and caring for children’s mental health, UNICEF, New York, October 2021.
- Wang, J., Aaron, A., Baidya, A., Chan, C., Wetzler, E., Savage, K., Joseph, M., & Kang, Y. (2021). Gender differences in psychosocial status of adolescents during COVID-19: a six-country cross-sectional survey in Asia Pacific. BMC Public Health, 21(1), 2009. 10.1186/s12889-021-12098-5 [DOI] [PMC free article] [PubMed]
- Wente AO, Kimura K, Walker CM, Banerjee N, Flecha MF, MacDonald B, Lucas C, Gopnik A. Causal Learning Across Culture and Socioeconomic Status. Child Development. 2019;90(3):859–875. doi: 10.1111/cdev.12943. [DOI] [PubMed] [Google Scholar]
- Wood MD, Read JP, Mitchell RE, Brand NH. Do parents still matter? Parent and peer influences on alcohol involvement among recent high school graduates. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors. 2004;18(1):19–30. doi: 10.1037/0893-164X.18.1.19. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2017). Depression and Other Common Mental Disorders: Global Health Estimates. https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf
- Zare-Zardini H, Soltaninejad H, Ferdosian F, Hamidieh AA, Memarpoor-Yazdi M. Coronavirus Disease 2019 (COVID-19) in Children: Prevalence, Diagnosis, Clinical Symptoms, and Treatment. International Journal of General Medicine. 2020;13:477–482. doi: 10.2147/IJGM.S262098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S-J, Zhang L-G, Wang L-L, Guo Z-C, Wang J-Q, Chen J-C, Liu M, Chen X, Chen J-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child & Adolescent Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available by request.
Code available by request.