Abstract
Objectives
This study evaluated the differences in clinical outcomes of COVID-19 infection between ethnic minorities and the White ethnic group in the UK.
Study design
Systematic review and meta-analysis.
Methods
This study included adult residents in the UK with confirmed COVID-19 infection. The outcomes evaluated in this study were mortality, intensive care unit (ICU) admission and invasive mechanical ventilation (IMV). Outcome data were compared between individuals from ethnic minority groups and individuals from a White ethnic background. MEDLINE, Embase, Cochrane, medRxiv and PROSPERO were searched for articles published between May 2020 and April 2021. The risk of bias was evaluated using the Newcastle–Ottawa Scale checklist. PROSPERO ID: CRD42021248117.
Results
Fourteen studies (767,177 participants) were included in the current review. In the adjusted analysis, the pooled odds ratio (OR) for mortality following COVID-19 infection was higher for Black (OR 1.83, 95% confidence interval [CI]: 1.21–2.76, number of studies [k] = 6), Asian (OR 1.16, 95% CI: 0.85–1.57, k = 6) and Mixed and Other (MO) ethnic groups (OR 1.12, 95% CI: 1.04–1.20, k = 5) compared with the White ethnic group. The adjusted and unadjusted ORs of ICU admission for many of the ethnic minority groups were more than double the OR values for the White ethnic group (Black ethnic group = OR 2.32, 95% CI: 1.73–3.11, k = 5; Asian ethnic group = OR 2.34, 95% CI: 1.89–2.90, k = 5; and MO ethnic group = OR 2.26, 95% CI: 1.64–3.11, k = 4). In the adjusted analysis for IMV, the ORs were similarly significantly raised in ethnic minority groups compared with the White ethnic group (Black ethic group = OR 2.03, 95% CI: 1.80–2.29, k = 3; Asian ethnic group = OR 1.84, 95% CI: 1.20–2.80, k = 3; and MO ethnic group = OR 2.09, 95% CI: 1.35–3.22, k = 3).
Conclusion
This review found that in the UK, Black, Asian and MO ethnic groups experienced increased COVID-19–related disease severity and mortality compared with the White ethnic group majority.
Keywords: COVID-19, UK, Ethnic minorities, Mortality, Ethnic
Introduction
In the UK, as a result of the COVID-19 pandemic between March 2020 and June 2021, there were 152,490 deaths (192 deaths/100,000 population), 471,045 hospital admissions and 471,7811 confirmed cases (7062 cases per 100,000 population).1 There are growing concerns in the UK that individuals belonging to many, if not all, ethnic minorities have been disproportionately impacted by COVID-19.2, 3, 4
A systematic review conducted between December 2019 and August 2020 found that Asian people had a higher risk of intensive care unit (ICU) admissions and death.5 However, another review of COVID-19 patients did not find that ethnicity was associated with the most severe outcomes.6 This present study was adapted from the systematic reviews by Sze et al.,5 and Raharja et al.,6 and builds on the work of these two earlier studies.5 , 6 Since the demographics, socio-economic issues, healthcare policies and systems of each country are unique, a UK-centric review was needed to investigate whether UK ethnic minority groups faced a greater risk of adverse outcomes from COVID-19.
To reduce the impact of COVID-19 on the population, pandemic-related research was prioritised and classified as urgent public health research by the National Institute for Health Research (NIHR).7 Following the government's call and support for research in this area, numerous studies were conducted; however, there were no published systematic review and meta-analysis studies on the impact of COVID-19 on ethnic minorities in the UK. Therefore, an up-to-date systematic review of UK-based studies was urgently needed to quantify the health inequalities faced by ethnic minority groups with regard to COVID-19. This research aimed to assess the clinical outcomes of COVID-19 in ethnic minority groups in the UK.
Methods
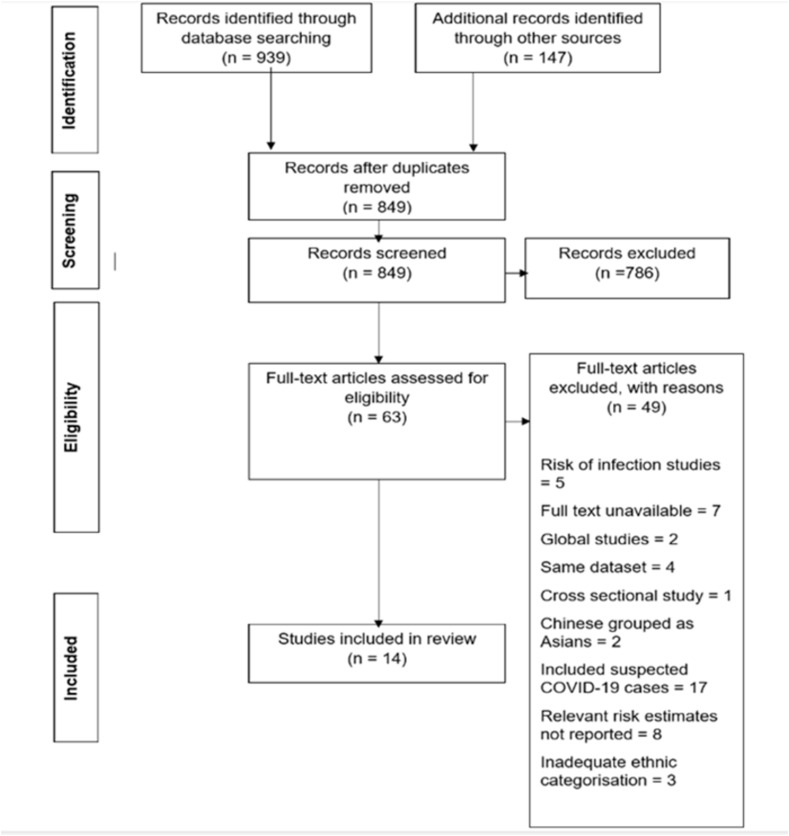
The current review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria.8 The PRISMA checklist is available in the Supplementary Material (see file S1 in the Appendix). The protocol was registered with PROSPERO international prospective register of systematic reviews with the ID. CRD42021248117.9
Information sources
The reference lists of previous reviews were searched for relevant studies published between January 2020 and August 2020.5 , 6 The database searches (Ovid MEDLINE, Ovid Embase, Ovid Cochrane, medRxiv and PROSPERO) were restricted to 1 year from May 2020 to April 2021.
Search strategy
The Population, Exposure, Comparator and Outcomes (PECO) framework was used to formulate the criteria for study selection. The target sample included the adult population (aged ≥18 years) in the UK with a confirmed positive COVID-19 result using reverse transcriptase–polymerase chain reaction (RT-PCR) tests. The ethnic categorisation into White, Black, Asian and Mixed and Other (MO) groups was based on the UK Census categories in 2001.10 The Census 2001 categorisation was used because it is used by the National Health Service (NHS). However, it is important to note that there is no separate group for the Chinese ethnic group in the Asian category. The South Asian and East Asian ethnic groups differ in terms of mortality; thus, combining these two ethnic groups may limit some results.11
All-cause mortality and ICU admission rates were assessed as the primary outcomes, with invasive mechanical ventilation (IMV) as a secondary outcome. The measures of effect for the outcomes were hazard ratio (HR), risk ratio (RR), odds ratio (OR) or standardised mortality ratio.
Interventional studies, systematic reviews, observational studies, including case–control studies, and cohort studies were included in the current review. In addition, non–peer reviewed studies were also included as this is a rapidly evolving field. Conference abstracts, commentaries, cross-sectional studies, reports, editorials, non-systematic review articles, case reports, late-breaking abstracts, studies without a comparator group and papers whose full text was unavailable were excluded. Risk of infection only studies were also excluded. Studies were restricted to those in the English language. Studies from the same population, with similar outcomes, were reviewed and only one relevant study was included (the rest were excluded, as this may have created a duplication of data). Studies that grouped all ethnic minorities as one were also excluded.
Specialist librarians were asked to review the search strategy with the keywords COVID-19, ethnic minority and the UK. The search strategy was based on the search originally conducted by Sze et al.,5 and Public Health England (PHE) and was adapted for this review by the addition of ‘UK’ as a key term during the searches.2 The detailed search strategy for each database was provided in the research proposal.9 The search terms were tailored for each database and the searches were run separately for each database to enhance sensitivity. The defined search period was between May 2020 and April 2021.
Selection process
Two reviewers independently screened the titles and abstracts of the studies, and all non-relevant studies were excluded. Full texts of the remaining studies were retrieved and reviewed for inclusion in the study against the selection criteria. Any disagreements between the researchers were resolved through discussion.
Data collection process
One researcher (SS) extracted data from the eligible studies and assessed the risk of bias (ROB). Data extraction was checked by a second reviewer (IA). The authors of relevant studies were also contacted for clarity on missing data.
Quality assessment
The Newcastle–Ottawa Scale (NOS; see file S2 in the Appendix) was used to assess the ROB in the included studies.12 An NOS score <5 is defined as a high ROB, a score of 5–6 as a moderate ROB and a score of 7–9 is classed as a low ROB.13 One researcher (SS) carried out the quality assessment at the study and outcome level using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.14 Publication bias was not assessed as there were fewer studies in the adjusted analysis. The funnel plot may not detect publication bias when the number of studies is small.15
Data synthesis
The raw counts for the various outcome variables were used to calculate the RR and 95% confidence intervals (CIs). Studies that did not use the White ethnic group as a comparator group were excluded from the meta-analysis. As all the studies were observational designs, a DerSimonian-Laird random-effects meta-analysis (REM) was conducted for all outcomes. For rare outcomes, OR was assumed to be equal to RR, and RR was assumed to be equal to HR.5 , 6 Mortality in hospital-based studies was not a rare outcome; however, in population-based studies, mortality was a rare outcome. The studies that provided adjusted odds ratios (AORs) were pooled together in one group and those that provided adjusted hazard ratios (AHRs) were separately pooled together in another group (if the outcomes were not rare). Thus, adjustments were made, whilst extracting, for study characteristics of each included study.
In studies where raw data were missing, the authors were contacted to obtain this information. To include studies with missing data in the meta-analysis, the unadjusted HR/RR were combined using the inverse variance method. Using this method, the pooled risk estimates were calculated separately for each ethnic group and a summary statistic was provided.
The results were written in tabulated form and as forest plots. Excel and RevMan were used to analyse and tabulate the data. Origin 2021b was used to convert graphical data into tabulated form. The statistical heterogeneity was explored by calculating the I2 statistic using RevMan and by investigating the overlap of CIs in the forest plots. A subgroup analysis was conducted to explore differences in risk estimates across the subgroups.16 Studies based only on ICU patients, general hospital patients and the general population were analysed separately. A sensitivity analysis was conducted based on only peer-reviewed studies and a separate analysis was conducted based on studies with a low ROB.16
Results
The search on MEDLINE, Embase, medRxiv, Cochrane and PROSPERO yielded 939 studies on 14–15 April 2021. Fourteen studies were selected to be included in the systematic review as shown in Supplementary Fig. S1 and Table S1.
Study characteristics
The 14 studies included in the review had a total of 767,177 participants. The study characteristics are shown in Table 1 .17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 As all of the studies were observational, no adjustment was needed. Fourteen studies were included in the systematic review and 12 in the meta-analysis. Thirteen studies provided data on risks of mortality due to COVID-19 in the various ethnic groups, six on ICU admission and four on the requirement for IMV.
Table 1.
Study characteristics of included studies.
| Study ID | Study design | Population | Setting | Sample size | Outcomes | Confounders adjusted for | Comorbidities |
|---|---|---|---|---|---|---|---|
| Alaa17 | Cohort | Data from ‘COVID-19 Hospitalisation in England Surveillance System’ (CHESS)a database, which included COVID-19 cases admitted to hospitals | Hospital | 6068 | Mortality | None | Asthma, diabetes mellitus (DM), hypertension (HTN), kidney and liver diseases, cardiovascular disease (CVD), respiratory illness, immunosuppressive states |
| Apea18 | Cohort | COVID-19 positive cases admitted to East London hospitals | Hospital | 1737 | Mortality, IMV | Age, sex, deprivation, body mass index (BMI), DM, HTN, chronic kidney disease (CKD) | DM, CKD, HTN, ischemic heart disease (IHD), CVD, cerebrovascular accident (CVA), chronic obstructive lung disease (COPD), liver disease, cancer, acquired immunodeficiency syndrome (AIDS), Charlson comorbidity index |
| Batty19 | Cohort | Participants of the UK Biobank cohort study | Community | 448,664 | Mortality | Age, sex, socio-economic status, lifestyle factors, comorbidities | CVD, DM, chronic bronchitis, HTN, mental illnesses |
| Ferrando-Vivas20 | Cohort | COVID-19 cases from the Intensive Care National Audit & Research Centre (ICNARC) database, of ICU admitted cases | ICU | 9990 | Mortality | Age, sex, deprivation, BMI, prior dependency, immunocompromised state, sedated for first 24 h, various clinical variables | Immunocompromised state |
| Field29 | Cohort | COVID-19 positive cases admitted to a London hospital | Hospital | 500 | Mortality | None | None |
| Gopal Rao21 | Cohort | COVID-19 cases tested in London hospitals | Hospital | 1901 | Mortality, ICU admission, IMV | Age, sex, deprivation, area of residence | None |
| Mahida27 | Case-control | Patients admitted to an ICU of a Birmingham hospital | ICU | 140 | ICU admission | None | HTN, obesity, IHD, DM, asthma, COPD, CVA, CKD, cancer |
| Perez-Guzman22 | Cohort | COVID-19 positive cases admitted to a London hospital | Hospital | 559 | Mortality, ICU admission, IMV | Age, sex, comorbidity, deprivation, admission NEWS-2 score | HTN, DM, IHD, heart failure, stroke, CKD, dementia, previous deep venous thrombosis/pulmonary embolism, atrial fibrillation (AF), COPD, liver disease, cancer, AIDS |
| Perkin28 | Case-control | COVID-19 and non-COVID-19 cases admitted to a London hospital | Hospital | 573 | Mortality | Age | DM, HTN, IHD |
| Russell30 | Cohort | COVID-19 positive cancer patients from a London hospital | Hospital | 156 | Mortality | None | Cancer, HTN, chronic steroid use, DM, lung disease, liver disease, CVD, frailty |
| Sapey23 | Cohort | COVID-19 cases admitted to Birmingham hospital Trust | Hospital | 2169 | Mortality, ICU admission | Age, sex, deprivation, comorbidities | Count of morbidities used; HTN, CVA, AF, IHD, DM, asthma, COPD, interstitial lung disease, CKD, malignancy, dementia, obesity |
| Singh24 | Cohort | Living population of Wolverhampton | Community and hospital | 228,632 | Mortality | Sex, age, deprivation, smoking, BMI, comorbidities, previous hospital admissions | DM, HTN, chronic heart, lung, kidney, joint diseases, cancer, dementia, mental illnesses, learning difficulties, immunosuppressive states, palliative care |
| Thomson26 | Cohort | COVID-19 cases admitted to an ICU in London | ICU | 156 | Mortality | Age, BMI, lowest PaO2/FiO2 ratio (P/F) on first day of ICU, pH and PaCO2 at time of lowest P/F ratio | HTN, DM, hyperlipidaemia, IHD, chronic respiratory illnesses, CKD |
| Yates25 | Cohort | COVID-19 cases admitted to hospitals in the UK, International Severe Acute Respiratory and emerging Infections Consortium (ISARIC) data set | Hospital | 65,932 | Mortality, ICU admission, IMV | Age, sex, obesity, DM, chronic heart disease, CKD, chronic pulmonary disease, cancer | Chronic heart, kidney and lung diseases, DM, cancer |
This is a surveillance system set up by PHE to obtain data regarding COVID-19 cases.17
Quality of studies
The risk of bias (ROB) was low, average NOS score was 7.7. (ranging from 4 to 9). Nine studies had a low ROB score on the NOS, four studies had a moderate ROB score and one study had a high ROB as shown in Table S2. The low bias scores were largely due to studies that failed to adjust for confounding factors. Most studies were hospital based; thus, these populations are somewhat representative of the average COVID-19 patient in the community but did not necessarily reflect the wider community. Also, there might be bias introduced in hospital-based studies as people in some ethnic groups might be reluctant to seek medical advice.
Mortality
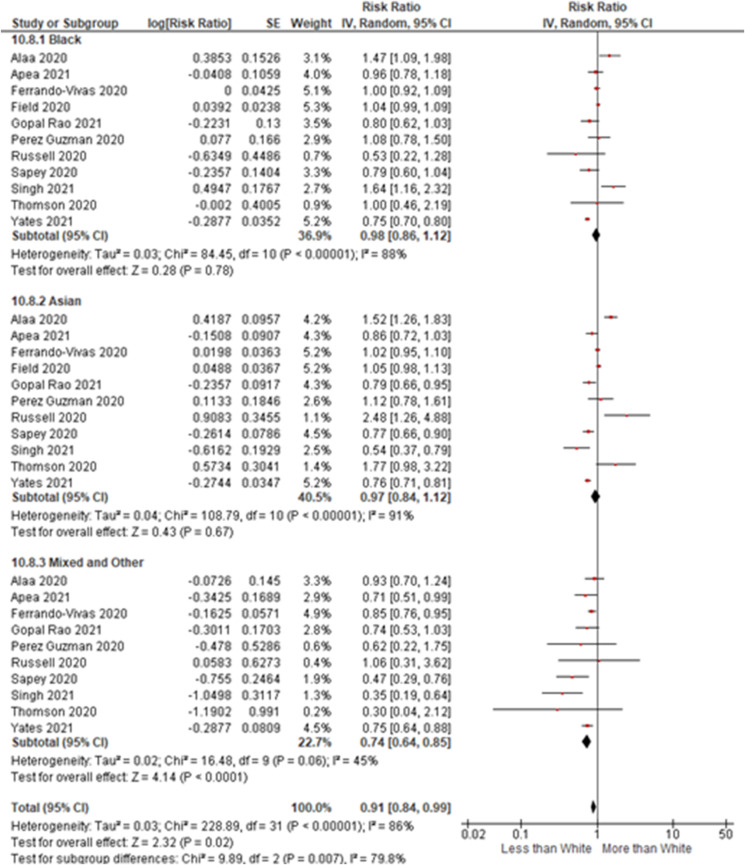
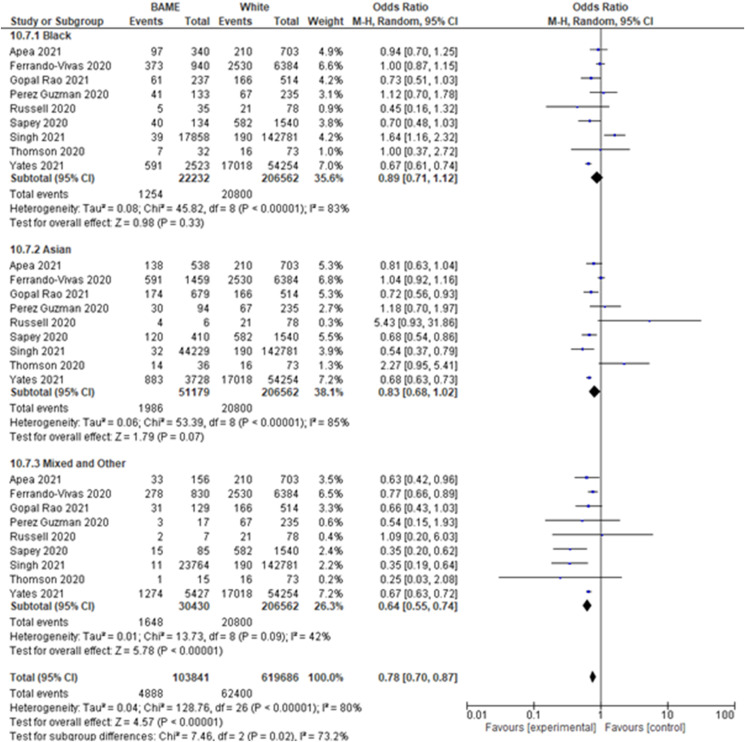
The unadjusted OR, RR, AOR and AHR are shown in Fig. S2, Fig. 1, Fig. 2 , and Fig. S3. As seen in Fig. S2, 20,800/206,562 White individuals died due to COVID-19 compared with 1254/22,232 Black individuals, 1986/51,179 Asian individuals and 1648/30,430 MO individuals.
Fig. 1.
Forest plot of unadjusted RR for the mortality outcome. REM, inverse variance method.
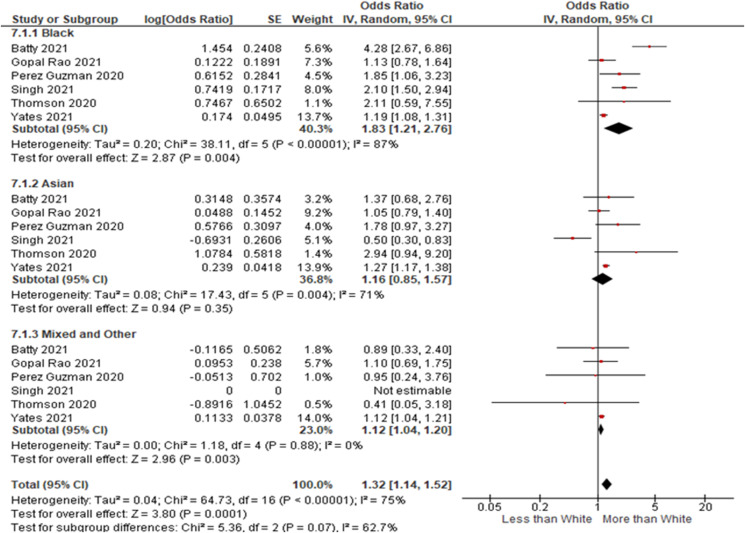
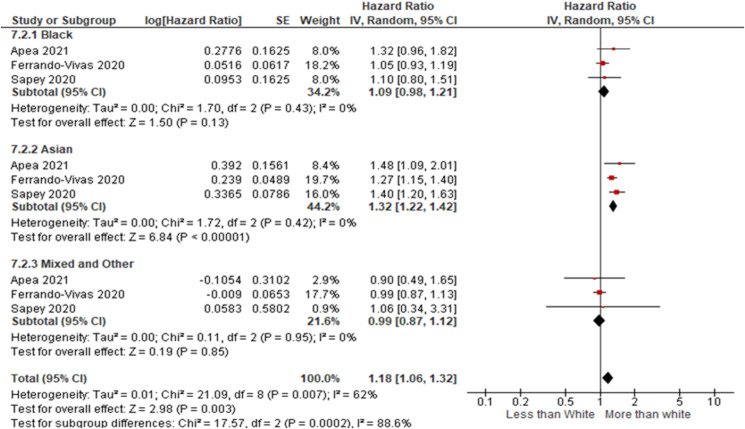
Fig. 2.
Forest plot of AOR, REM, for the mortality outcome.
In the unadjusted analysis, the risk of death was similar in Black and Asian populations (Black ethnic group = OR 0.89, 95% CI: 0.71–1.12, I2 = 83%, number of studies [k] = 9; Asian ethnic group = OR 0.83, 95% CI: 0.68–1.02, I2 = 85%, k = 9), but significantly reduced in the MO ethnic group (OR 0.64, 95% CI: 0.55–0.74, I2 = 42%, k = 9) as shown in Fig. 1.
The adjusted mortality risk was significantly higher for the Asian group (OR 1.32, 95% CI: 1.22–1.42, I2 = 0%, k = 3) but not for the Black or MO ethnic groups. The odds of dying from COVID-19 were significantly increased for the Black and MO ethnic minority groups compared with the White ethnic group in the adjusted analysis (Black ethnic group = AOR 1.83, 95% CI: 1.21–2.76, I2 = 87%, k = 6 and MO ethnic group = AOR 1.12, 95% CI: 1.04–1.20, I2 = 0%, k = 5), but not for the Asian ethnic group. All the studies in the adjusted analysis were low ROB studies.
In the sensitivity analysis, with only published studies, the increased odds of mortality in the Black and MO ethnic groups were maintained (Black ethnic group = AOR 1.48, 95% CI: 1.10–1.99 and MO ethnic group = AOR 1.12, 95% CI: 1.04–1.20) as shown in Table S3.
The odds of increased mortality for Black, Asian and MO ethnicities were greater in subgroup analysis with only hospital-based studies (Black ethnic group = AOR 1.22, 95% CI 1.07–1.38, I2 = 6%, k = 4; Asian ethnic group = AOR 1.28, 95% CI 1.04–1.57, I2 = 40%, k = 4; and MO ethnic group = AOR 1.12, 95% CI 1.04–1.20, I2 = 0%, k = 4). This subgroup had low heterogeneity and showed statistically significant results (see Table S4).
In the adjusted analysis of only population-based studies, the likelihood of dying from COVID-19 for the Black ethnic group was almost three times higher than for the White ethnic group (AOR 2.94, 95% CI: 1.46–5.90), but with a larger CI. However, the likelihood of mortality was not increased for the Asian group.
Perkin et al.28 found that adjusted odds of mortality due to COVID-19 were increased for all ethnic minority groups (Asian ethnic group = AOR 3.62, 95% CI 1.84–7.11; Black ethnic group = AOR 2.91, 95% CI 1.43–5.91; Other ethnic group = AOR 3.01, 95% CI 1.61–5.64) compared with hospital deaths in 2019.
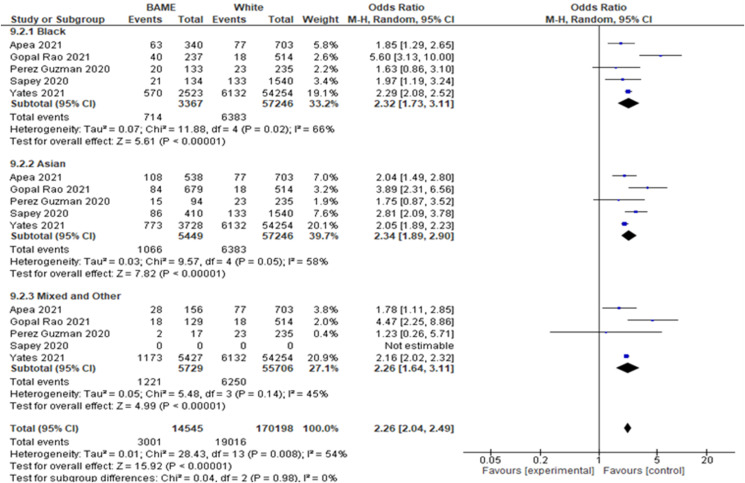
ICU admission
Six studies provided data about ICU admissions for various ethnic groups. Five of these studies were suitable for aggregating the raw outcomes and for pooling the unadjusted risk estimates. These studies included a total of 71,791 participants who were admitted to ICU in the UK. In total, 80% of these ICU admissions were White, 5% were Black, 9.5% were Asian and 8% were MO.
The unadjusted and adjusted analyses for ICU admission are shown in Fig. 3 and Fig. S4. From Fig. S4, it can be seen that 11% of White individuals were admitted to ICU with COVID-19 compared with 21% of Black, 20% of Asian and 21% MO individuals. In the adjusted and unadjusted analysis, the likelihood of ICU admission was more than double for patients in the Black, Asian and MO ethnic minority groups than the White ethnic group. The unadjusted OR for the Black ethnic group was 2.32 (95% CI: 1.73–3.11, I2 = 66%, k = 5), for the Asian ethnic group was 2.34 (95% CI: 1.89–2.90, I2 = 58%, k = 5) and for the MO ethnic group was 2.26 (95% CI: 1.64–3.11, I2 = 45%, k = 4).
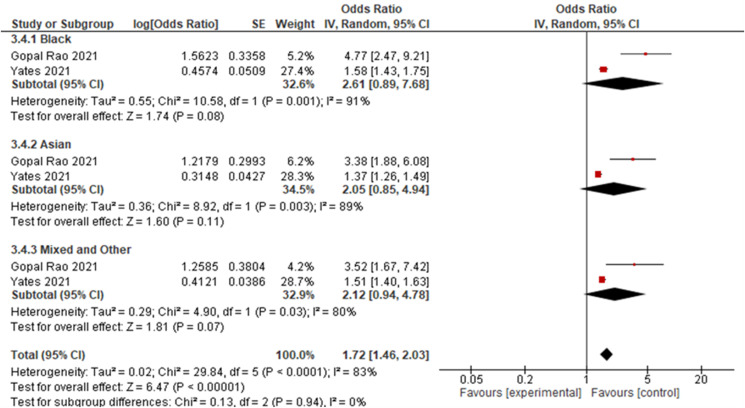
Fig. 3.
Forest plot of ICU admission outcome, pooled AOR, REM.
In the pooled AOR, the results were not statistically significant for the ethnic minorities as the lower CI crossed the line of no effect as shown in Fig. 3. However, the results indicated a strong association (OR twice as high) between ethnicity and ICU admission outcome. The pooled AOR for the Black ethnic group was 2.61 (95% CI: 0.89–7.68, I2 = 91%, k = 2), for the Asian ethnic group was 2.05 (95% CI: 0.85–4.94, I2 = 89%, k = 2) and for the MO ethnic group was 2.12 (95% CI: 0.94–4.78, I2 = 80%, k = 2).
One study, which was not included in the meta-analysis, compared patients admitted to the ICU with COVID-19 with patients admitted to the ICU with community-acquired pneumonia (non-COVID controls).27 The study found that the cases with COVID-19 had statistically significantly fewer White (P = 0.012) and more Asian patients (P = 0.002).27
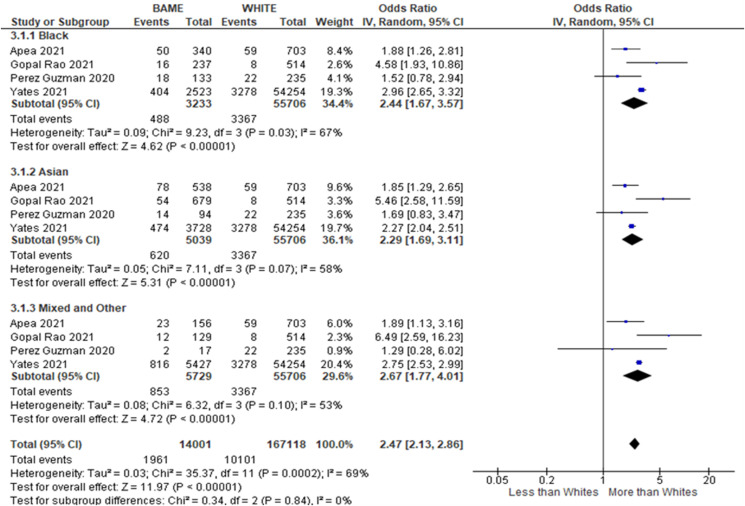
Invasive mechanical ventilation
Four cohort studies reported ethnicity data about the need for IMV for COVID-19-hospitalised patients in the UK. From a total of 69,707 patients, 80% were White, 5% were Black, 7% were Asian and 8% were from the MO ethnic group. In the unadjusted analysis, the odds of an individual in the Black, Asian or MO ethnic groups requiring IMV were twice as high than an individual in the White ethnic group (Black ethnic group = OR 2.44, 95% CI: 1.67–3.57, I2 = 67%, k = 4; Asian ethnic group = OR 2.29, 95% CI: 1.69–3.11, I2 = 58%, k = 4; and MO ethnic group = OR 2.67, 95% CI: 1.77–4.01, I2 = 53%, k = 4) [see Fig. S5]. In Fig. S5, it can be seen that 6% of White patients required IMV compared with 15% of Black patients, 12% of Asian patients and 15% of MO patients.
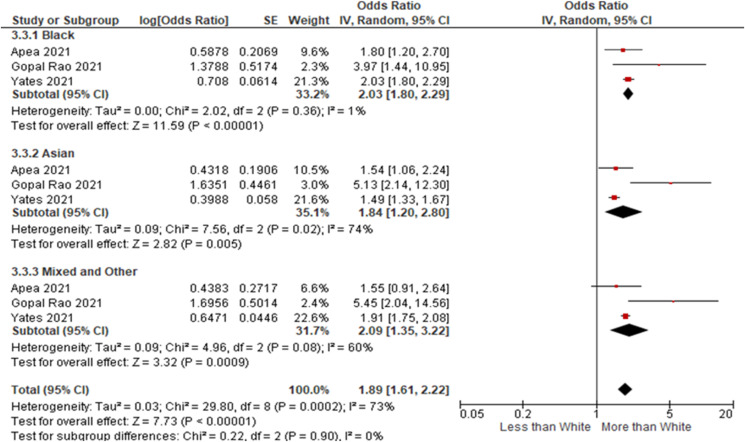
After adjusting for confounders, the likelihood of requiring IMV remained high for the Black, Asian and MO ethnic groups, indicating that other factors may have been putting them at increased risk of IMV. The AOR for the Black ethnic group was 2.03 (95% CI: 1.80–2.29, I2 = 1%, k = 3), AOR for the Asian ethnic group was 1.84 (95% CI: 1.20–2.80, I2 = 74%, k = 3) and AOR for the MO ethnic group was 2.09 (95% CI: 1.35–3.22, I2 = 60%, k = 3) as shown in Fig. 4 .
Fig. 4.
Forest plot of the IMV outcome, pooled adjusted OR, REM.
Studies included in the IMV requirement and ICU admission analyses were all published hospital-based studies and were classified as having a low ROB; thus, so further sensitivity analyses were not conducted. The heterogeneity was high for most of the outcomes.
Quality of evidence assessment
As the best evidence for risk factors is usually obtained from observational studies, the evidence in this review had high ratings as advised by Foroutan et al. (for prognostic studies).31 The overall GRADE assessment indicated a high level of confidence for all outcomes, except for the mortality outcomes in the Asian ethnic group, which was moderate and was downrated due to inconsistency, as shown in the summary of findings in Table S5.
Discussion
There was heterogeneity in the study populations, settings, methodology and statistical analyses of the included studies. However, the meta-analysis was conducted since this degree of heterogeneity had been reported by other reviews and the results of the analysis would be beneficial.
The results indicate greater COVID-19 disease severity in the Black, Asian and MO ethnic groups, necessitating ICU admission and IMV provision. Overall, the current results suggest that ethnicity is a risk factor for worse prognosis in ethnic minority populations and they experience increased disease severity. Several studies and data from the Office for National Statistics (ONS) and the Intensive Care National Audit and Research Centre (ICNARC) also validate this finding of the worst COVID-19 outcomes for ethnic minorities in the UK.2 , 5 , 31 , 33, 34, 35, 36 In the UK, in the national publications, all ethnic groups, apart from the White British, are considered as ethnic minorities, including White minorities, such as Irish traveller groups, Gypsy, Roma and any other White background.37
Some reviews on the topic of ethnicity and COVID-19 outcomes have combined data from all over the world.5 , 6 However, the results from these studies cannot be extrapolated to the UK as the healthcare systems, health inequality issues and ethnic make-up vary from country to country. A more recent review has attempted to address this issue by analysing the COVID-19 data regionally, but they did not include any data on ICU admissions nor conduct any adjusted analysis on mortality in Europe.38 Agyemang et al.38 concluded that hospitalised patients from ethnic minority groups did not experience worse COVID-19 outcomes except for increased mortality in Brazil.
The likelihood of mortality for hospitalised COVID-19 patients was higher for the Black, Asian and MO ethnic groups than the White ethnic group in the adjusted analysis. This result is significant because it shows that after hospital admission, there are additional factors that increase the risk of mortality in ethnic minority patients. Thus, the difference in mortality cannot be attributed to differential access to healthcare facilities or increased risk of infection alone.
The odds of mortality due to COVID-19 for the general population were higher for the Black ethnic group than the White ethnic group, which is similar to findings from the ONS and Mathur.32 , 34 Increased prevalence of comorbidities and raised C-reactive protein (CRP) levels, a non-specific marker of inflammation, are possible causes of the greater severity of COVID-19 in Black and Asian individuals.
Obesity has also been identified as an important risk factor associated with morbidity and mortality due to COVID-19.25 , 45 , 46 It has been shown that individuals in the Black ethnic group with obesity experience the worst COVID-19 outcomes.25 Another study reported that the association between obesity and mortality was greater for non-White individuals (especially Black and South Asian people) compared to White individuals (P-value 0.002).46 In the UK, the highest rates of obesity have been observed in the Black population (68%), compared to the other ethnic groups (White 64% and Asian 60%), with an average obesity rate of 63% in adults.47
Diabetes mellitus and hypertension were three times more common in patients who died due to COVID-19.45 Hypertension is three to four times more prevalent in Black individuals in the UK than in the rest of the population.48 In the UK, diabetes mellitus is more prevalent in the South Asian ethnic group (six times more) and the Black ethnic group (three times more) than in the White ethnic group.49 Genetic predisposition, urbanisation, migration to Western countries and reduced physical activity are important causative factors of diabetes mellitus in South Asian populations.50
Black and Asian populations have raised CRP levels compared with White populations, putting them at an increased risk of severe COVID-19 infection.51 Raised CRP levels have been shown to be an important predictor of severe COVID-19 and are also a risk factor for diabetes mellitus and cardiovascular disease.50 , 52, 53, 54 One study observed that the median CRP levels in Black (181.5 mg/L) and Asian (146 mg/L) people were higher than in White people (136 mg/L) on presentation at a hospital for COVID-19–related symptoms.18 Lower socio-economic status is a risk factor for raised CRP levels and it has been hypothesised that stress may be a mediator in this.51 It has also been hypothesised that chronic inflammation, linked to insulin resistance, obesity, cardiovascular disease, stress and chronic infections, in the Black and other ethnic minority groups can trigger a ‘cytokine storm’, which is associated with the severe COVID-19.44 A cytokine storm is an abnormal dysregulated inflammatory response diagnosed by the presence of respiratory distress and hyperinflammation (raised CRP levels more than 100 mg/L or raised ferritin levels) in COVID-19 cases.55
This is the first meta-analysis that analyses IMV and ICU data from the UK. The odds of ICU admission in hospitalised patients are similar to findings from the ICNARC and the study by Mathur, which also found that the adjusted risk of ICU admission was raised two to three times for Black, Asian and MO ethnic groups (in the general population).34 , 36 Sze et al.5 only found increased odds of ICU admission for individuals in the Asian ethnic group; however, their analysis was limited by small numbers (n = 4439) compared to the current review, which included ICU data on 67,833 COVID-19 patients. Several studies have highlighted that COVID-19 cases presenting to UK hospitals tend to be individuals who are White, elderly and have more comorbidities (e.g. dementia and chronic obstructive pulmonary disease).22 , 23 , 28 , 56 In contrast, Black and Asian people tend to be younger and have fewer comorbidities, but have a higher prevalence of diabetes mellitus.22 , 23 , 28 Elderly White individuals are not good candidates for ICU admission or IMV; however, Black and Asian individuals may be more suitable for ICU admission, and this may be another reason why they have higher rates of ICU admission and IMV.23
Strengths
This is the first systematic review and meta-analysis conducted to assess the burden of COVID-19 faced by ethnic minorities in the UK. The strength of the research lies in its comprehensive analysis of relevant databases for published and preprint articles. Although the heterogeneity was quite high, this was to be expected with observational studies that had very large numbers of participants.32 The heterogeneity was explored by conducting subgroup and sensitivity analyses.
Limitations
A broad ethnic classification was used in this review. The Asian ethnic group included very diverse subgroups, each of which has now been shown to have different risk profiles. This review was limited to adults so the results cannot be generalised to children. The PCR test for COVID-19 has a high false-negative rate, which led to some cases being wrongly classified as non–COVID-19. As this review concentrated on UK-based studies, the results are less generalisable to other countries. It has been noted that many participants' ethnicities have been put down as ‘Other’ and this may have created erroneous results for the MO ethnic group.22 The representativeness of study populations is a limitation of the current review. The variables used for the adjustment differed greatly between studies, thus the amount and nature of adjustment could impact the results.
Policy implications
The results of the present study have urgent implications for formulating a COVID-19 response strategy (including vaccination provision) that protects ethnic minorities who are at most risk from the most severe COVID-19 outcomes and addresses long-standing health inequalities. Recommendations made by Marmot et al.39 to address the health inequalities should be adopted in full, including increased public health funding, investment in key areas, such as housing and employment, development of a national strategy to reduce health inequalities and setting targets to monitor government interventions.39, 40, 41, 42 Strategies to reduce the effects of COVID-19, such as health promotion efforts, should be targeted at high-risk communities. Clinical guidelines should be adapted to consider the health inequalities faced by ethnic minorities.43 The NICE guidance on excluding cases with cardiovascular disease, especially angina patients, from critical care disproportionately influences ethnic minorities as Asian and Black people are more prone to heart disease.43 The COVID-19 risk assessment of being employed in healthcare does not allow for the redeployment of staff based on ethnicity alone.43 As ethnicity has been shown to be associated with increased mortality, these workers should be given the choice of being redeployed in non–patient-facing roles.43
Implications of research
The current review needs to be upgraded to a living systematic review so that the changing pandemic risks can be identified in the various ethnicities as the pandemic progresses. There is a need for more epidemiological population-based studies to assess the true risk experienced by various ethnic groups with regard to the most severe COVID-19 clinical outcomes. The data set needs to be large enough to appreciate the risk in the various population subgroups. Ethnic minority-focused healthcare research concerning COVID-19 treatments can help to reduce health inequalities.44 Research should be conducted to assess why COVID-19 related health inequalities exist for some ethnic minorities.
Conclusion
It can be concluded that the Black, Asian and MO ethnic groups experience the most severe COVID-19 clinical outcomes in the UK. These findings are of immense public health importance and should be used to help formulate policy concerning COVID-19 and reducing socio-economic disparities.
Author statements
Acknowledgements
SA is a Research Associate in the National Institute for Health and Care Research, Applied Research Collaboration-Greater Manchester (NIHR200174). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, the United Kingdom Health Security Agency, the Department of Health and Social Care, or its partner organisations. The Librarians at the University of Manchester and Public Health England (PHE) helped to formulate the search strategy. Librarians from PHE also helped to find the full text of articles. SS would like to thank her family, especially her sister Hina Siddiq who funded her studies, Sarah Siddiq who edited this article and her children who put up with her whilst she worked on this paper.
Ethical approval
None required.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
None declared.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2022.05.019.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Fig. S1.
Fig. S2.
Fig. S3.
Fig. S4.
Fig. S5.
References
- 1.GOV.UK. Guidance - coronavirus (COVID-19) statistics and analysis [Internet]. London: Cabinet Office; [updated 2021 June 26; cited 2021 June 26]. Available from: https://www.gov.uk/guidance/coronavirus-covid-19-statistics-and-analysis.
- 2.Public Health England . 2020. Beyond the data: understanding the impact of COVID-19 on BAME groups.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/892376/COVID_stakeholder_engagement_synthesis_beyond_the_data.pdf [Internet] [cited 20 April 2021] Available from: [Google Scholar]
- 3.Public Health England . 2020. Disparities in the risk and outcomes of COVID-19.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf [Internet] [cited 18 June 2021] Available from: [Google Scholar]
- 4.House of Commons . 2020. Unequal impact? Coronavirus and BAME people.https://committees.parliament.uk/publications/3965/documents/39887/default/ [Internet] [cited 2021 May 1] Available from: [Google Scholar]
- 5.Sze S., Pan D., Nevill C.R., Gray L.J., Martin C.A., Nazareth J., et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2020;29:100630. doi: 10.1016/j.eclinm.2020.100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raharja A., Tamara A., Kok L.T. Association between ethnicity and severe COVID-19 disease: a systematic review and meta-analysis. J Racial Ethn Health Disparities. 2020:12. doi: 10.1007/s40615-020-00921-5. Available at: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.UK Research and Innovation. COVID-19 and ethnicity: funding six new projects [Internet]. London: UK Research and Innovation; [updated 2021 Jan 28; cited 2021 March 1]. Available from: https://www.ukri.org/our-work/tackling-the-impact-of-covid-19/understanding-coronavirus-covid-19-and-epidemics/covid-19-and-ethnicity.
- 8.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting Items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siddiq S., Ahmed S. 2021. A systematic review of the health inequalities affecting the Black, Asian and other ethnic minority groups in the UK in comparison to the White ethnic population with respect to the clinical outcomes of COVID-19 infection. PROSPERO International prospective register of systematic reviews.https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021248117 [Internet] [cited 2021 June 24]; CRD42021248117. Available from: [Google Scholar]
- 10.GOV.UK. List of ethnic groups [Internet] London: Cabinet Office; no date [cited 2021 May 11]. Available from: https://www.ethnicity-facts-figures.service.gov.uk/style-guide/ethnic-groups.
- 11.Stanaway F., Noguchi N., Mathieu E., Khalatbari-Soltani S., Bhopal R. Mortality of ethnic minority groups in the UK: a systematic review protocol. Br Med J Open. 2020;10(6) doi: 10.1136/bmjopen-2019-034903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells G.A., Shea B., O'Connell D., Peterson J., Welch V., Losos M., et al. 2008. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses.http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm [10 June 2021]. Available from: [Google Scholar]
- 13.Luchini C., Stubbs B., Solmi M., Veronese N. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa Scale. World J Metaanal. 2017;5:80. doi: 10.13105/wjma.v5.i4.80. [DOI] [Google Scholar]
- 14.Guyatt G.H., Oxman A.D., Vist G.E., Kunz R., Falck-Ytter Y., Alonso-Coello P., et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sterne J.A.C., Sutton A.J., Ioannidis J.P.A., Terrin N., Jones D.R., Lau J., et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- 16.Page M.J., Moher D., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alaa A., Qian Z., Rashbass J., Benger J., Van Der Schaar M. Retrospective cohort study of admission timing and mortality following COVID-19 infection in England. BMJ Open. 2020;10:e042712. doi: 10.1136/bmjopen-2020-042712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Apea V.J., Wan Y.I., Dhairyawan R., Puthucheary Z.A., Pearse R.M., Orkin C.M., et al. Ethnicity and outcomes in patients hospitalised with COVID-19 infection in East London: an observational cohort study. BMJ Open. 2021;11:e042140. doi: 10.1136/bmjopen-2020-042140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Batty G.D., Gaye B., Gale C., Hamer M., Lassale C. Explaining ethnicity disparities in COVID-19 mortality: population-based, prospective cohort study. MedRxiv. 2021 doi: 10.1101/2021.02.07.21251079. [Preprint] [DOI] [Google Scholar]
- 20.Ferrando-Vivas P., Doidge J., Thomas K., Gould D.W., Mouncey P., Shankar-Hari M., et al. Prognostic factors for 30-day mortality in critically ill patients with Coronavirus disease 2019: an observational cohort study. Crit Care Med. 2021;49:102–111. doi: 10.1097/CCM.0000000000004740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gopal Rao G., Allen A., Papineni P., Wang L., Anderson C., McGregor A., et al. Cross-sectional observational study of epidemiology of COVID-19 and clinical outcomes of hospitalised patients in North West London during March and April 2020. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-044384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perez-Guzman P.N., Daunt A., Mukherjee S., Crook P., Forlano R., Kont M.D., et al. Clinical characteristics and predictors of outcomes of hospitalized patients with COVID-19 in a multi-ethnic London NHS Trust: a retrospective cohort study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sapey E., Gallier S., Mainey C., Nightingale P., McNulty D., Crothers H., et al. Ethnicity and risk of death in patients hospitalised for COVID-19 infection in the UK: an observational cohort study in an urban catchment area. BMJ Open Respir Res. 2020;7 doi: 10.1136/bmjresp-2020-000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh B.M., Bateman J., Viswanath A., Klaire V., Mahmud S., Nevill A., et al. Risk of COVID-19 hospital admission and COVID-19 mortality during the first COVID-19 wave with a special emphasis on ethnic minorities: an observational study of a single, deprived, multiethnic UK health economy. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-046556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yates T., Zaccardi F., Islam N., Razieh C., Gillies C.L., Lawson C.A., et al. Obesity, ethnicity and risk of critical care, mechanical ventilation and mortality in patients admitted to hospital with COVID-19: analysis of the ISARIC CCP-UK cohort. Obesity. 2021;29:1223–1230. doi: 10.1002/oby.23178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomson R.J., Hunter J., Dutton J., Schneider J., Khosravi M., Casement A., et al. Clinical characteristics and outcomes of critically ill patients with COVID-19 admitted to an intensive care unit in London: a prospective observational cohort study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0243710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahida R.Y., Chotalia M., Alderman J., Patel C., Hayden A., Desai R., et al. Characterisation and outcomes of ARDS secondary to pneumonia in patients with and without SARS-CoV-2: a single-centre experience. BMJ Open Respir Res. 2020;7:11. doi: 10.1136/bmjresp-2020-000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perkin M.R., Heap S., Crerar-Gilbert A., Albuquerque W., Haywood S., Avila Z., et al. Deaths in people from Black, Asian and minority ethnic communities from both COVID-19 and non-COVID causes in the first weeks of the pandemic in London: a hospital case note review. BMJ Open. 2020;10:e040638. doi: 10.1136/bmjopen-2020-040638. Available at: 10.1136/bmjopen-2020-040638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Field R.E., Afzal I., Dixon J., Patel V.R., Sarkar P., Marsh J.E. Cohort profile: preliminary experience of 500 COVID-19 positive cases at a South West London District General Hospital. MedRxiv. 2020 doi: 10.1101/2020.04.28.20075119. [Preprint] [DOI] [Google Scholar]
- 30.Russell B., Moss C., Papa S., Irshad S., Ross P., Spicer J., et al. Factors affecting COVID-19 outcomes in cancer patients: a first report from Guy's Cancer Center in London. Front Oncol. 2020;10 doi: 10.3389/fonc.2020.01279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Foroutan F., Guyatt G., Zuk V., Vandvik P.O., Alba A.C., Mustafa R., et al. GRADE guidelines 28: use of GRADE for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol. 2020;121:62–70. doi: 10.1016/j.jclinepi.2019.12.023. [DOI] [PubMed] [Google Scholar]
- 32.Office for National Statistics . Office for National Statistics; London: 2020. Coronavirus (COVID-19) related deaths by ethnic group, England and Wales: 2 March 2020 to 15 May 2020.https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbyethnicgroupenglandandwales/2march2020to15may2020 [Internet] [updated 2020 June 19; cited 2021 July 6]. Available from: [Google Scholar]
- 33.Nafilyan V., Islam N., Mathur R., Ayoubkhani D., Banerjee A., Glickman M., et al. Ethnic differences in COVID-19 mortality during the first two waves of the Coronavirus pandemic: a nationwide cohort study of 29 million adults in England. Eur J Epidemiol. 2021:1–13. doi: 10.1007/s10654-021-00765-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mathur R., Rentsch C.T., Morton C.E., Hulme W.J., Schultze A., Mackenna B., et al. Ethnic differences in SARS-CoV-2 infection and COVID-19-related hospitalisation, intensive care unit admission, and death in 17 million adults in England: an observational cohort study using the OpenSAFELY platform. Lancet. 2021;397:1711–1724. doi: 10.1016/s0140-6736(21)00634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.King's Fund . 2021. Deaths from Covid-19 (coronavirus): how are they counted and what do they show?https://www.kingsfund.org.uk/publications/deaths-covid-19 [Internet] [cited 2021 June 12 ] Available from: [Google Scholar]
- 36.Intensive Care National Audit and Research . 2021. ICNARC report on COVID-19 in critical care: England, Wales and Northern Ireland 3 June 2021.https://www.icnarc.org/our-audit/audits/cmp/reports [Internet] [cited 2021 June 16] Available from: [Google Scholar]
- 37.GOV.UK. Writing about ethnicity [Internet] London: Cabinet Office; updated Dec 2021 [cited 2022 March 11]. Available from: https://www.ethnicity-facts-figures.service.gov.uk/style-guide/writing-about-ethnicity.
- 38.Agyemang C., Richters A., Jolani S., Hendriks S., Zalpuri S., Yu E., et al. Ethnic minority status as social determinant for COVID-19 infection, hospitalisation, severity, ICU admission and deaths in the early phase of the pandemic: a meta-analysis. BMJ Global Health. 2021;6:e007433. doi: 10.1136/bmjgh-2021-007433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marmot M., Allen J., Goldblatt P., Herd E., Morrison J. Institute of Health Equity; London: 2020. Build back fairer: the COVID-19 Marmot review. The pandemic, socioeconomic and health inequalities in England.https://www.health.org.uk/publications/build-back-fairer-the-covid-19-marmot-review [Online]. Available at: [Google Scholar]
- 40.Griffin S. Covid-19: failure to control pandemic and inequalities made England worst affected in Europe, says report. Br Med J. 2020;371 doi: 10.1136/bmj.m4842. [DOI] [PubMed] [Google Scholar]
- 41.Iacobucci G. Marmot 10 years on: austerity has damaged nation's health, say experts. Br Med J. 2020:m747. doi: 10.1136/bmj.m747. [DOI] [PubMed] [Google Scholar]
- 42.Marmot M., Allen J., Boyce T., Goldblatt P., Morrison J. 2020. Health equity in England: the Marmot review 10 years on. London: Institute of Health Equity.https://www.health.org.uk/publications/reports/the-marmot-review-10-years-on [Online]. Available at: [Google Scholar]
- 43.Paton A. Fairness, ethnicity, and COVID-19 ethics: a discussion of how the focus on fairness in ethical guidance during the pandemic discriminates against people from ethnic minority backgrounds. J Bioeth Inq. 2020;17(4):595–600. doi: 10.1007/s11673-020-09999-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vepa A., Bae J.P., Ahmed F., Pareek M., Khunti K. COVID-19 and ethnicity: a novel pathophysiological role for inflammation. Diabetes Metabol Syndr Clin Res Rev. 2020;14(5):1043–1051. doi: 10.1016/j.dsx.2020.06.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raleigh V. King's Fund; London: 2021. Deaths from Covid-19 (coronavirus): how are they counted and what do they show?https://www.kingsfund.org.uk/publications/deaths-covid-19 [Online]. Available at: [Google Scholar]
- 46.Sattar N., Ho F.K., Gill J.M., Ghouri N., Gray S.R., Celis-Morales C.A., et al. BMI and future risk for COVID-19 infection and death across sex, age and ethnicity: preliminary findings from UK biobank. Diabetes Metabol Syndr Clin Res Rev. 2020;14(5):1149–1151. doi: 10.1016/j.dsx.2020.06.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.GOV.UK . 2021. Ethnicity facts and figures: Overweight adults.https://www.ethnicity-facts-figures.service.gov.uk/health/diet-and-exercise/overweight-adults/latest Available at: [Google Scholar]
- 48.Schofield P., Saka O., Ashworth M. Ethnic differences in blood pressure monitoring and control in south east London. Br J Gen Pract. 2011;61(585):e190–e196. doi: 10.3399/bjgp11x567126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Raleigh V., Holmes J. The King's Fund; London, UK: 2021. The health of people from ethnic minority groups in England.https://www.kingsfund.org.uk/publications/health-people-ethnic-minority-groups-england [Online]. Available at: [Google Scholar]
- 50.Shah A., Kanaya A.M. Diabetes and associated complications in the South Asian population. Curr Cardiol Rep. 2014;16(5) doi: 10.1007/s11886-014-0476-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nazmi A., Victora C.G. Socioeconomic and racial/ethnic differentials of C-reactive protein levels: a systematic review of population-based studies. Biomed Cent Public Health. 2007;7(1):212. doi: 10.1186/1471-2458-7-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ali N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J Med Virol. 2020;92(11):2409–2411. doi: 10.1002/jmv.26097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manson J.J., Crooks C., Naja M., Ledlie A., Goulden B., Liddle T., et al. COVID-19-associated hyperinflammation and escalation of patient care: a retrospective longitudinal cohort study. Lancet Rheumatol. 2020;2(10):e594–e602. doi: 10.1016/s2665-9913(20)30275-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stringer D., Braude P., Myint P.K., Evans L., Collins J.T., Verduri A., et al. The role of C-reactive protein as a prognostic marker in COVID-19. Int J Epidemiol. 2021;50(2):420–429. doi: 10.1093/ije/dyab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cron R.Q. COVID-19 cytokine storm: targeting the appropriate cytokine. Lancet Rheumatol. 2021;3(4):e236–e237. doi: 10.1016/s2665-9913(21)00011-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Harrison E.M., Docherty A.B., Barr B., Buchan I., Carson G., Drake T.M., et al. Ethnicity and outcomes from COVID-19: the ISARIC CCP-UK prospective observational cohort study of hospitalised patients. SSRN Electron J. 2020 doi: 10.2139/ssrn.3618215. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.