Abstract
Introduction:
Homework assignments are considered key components of behavioral treatments for bulimia nervosa (BN), but little is known about whether homework compliance predicts BN symptom improvement. The present study is the first to examine whether session-by-session change in homework compliance predicts session-by-session changes in BN symptoms during behavioral treatment.
Method:
Patients with BN-spectrum eating disorders (n=42) received 20 sessions of behavioral treatment. Each session, their clinicians completed surveys assessing compliance with self-monitoring, behavioral, and written homework assignments and BN symptom frequency during the previous week.
Results:
Significant between-persons effects of self-monitoring and behavioral homework compliance were identified, such that patients with greater compliance in the past week experienced greater reductions in binge eating and purging the following week. There were significant within-persons effects of self-monitoring compliance on binge eating and behavioral homework compliance on restrictive eating, binge eating, and purging, such that greater than one’s usual compliance predicted greater improvements in BN symptoms the following week. No significant effects of written homework compliance were identified.
Conclusion:
Compliance with self-monitoring and behavioral homework predict improvements in BN symptoms during behavioral treatment. These findings reinforce the importance of self-monitoring and behavioral homework compliance as drivers of change during treatment for BN.
Keywords: behavioral treatment, bulimia nervosa, homework, self-monitoring
Introduction and Aims
Bulimia nervosa (BN) spectrum disorders are eating disorders characterized by recurrent engagement in binge eating (characterized by consumption of objectively-large amounts of food accompanied by a subjective sense of loss of control) and inappropriate compensatory behaviors (e.g., self-induced vomiting, laxative or diuretic misuse, driven or compelled exercise, or fasting) driven by concerns about body weight or shape (American Psychiatric Association, 2013). BN spectrum disorders impacts as many as 1.0% of people in the United States and is associated with significant psychosocial impairment (Hudson, Hiripi, Pope, & Kessler, 2007). Although behavioral treatment approaches (i.e., Cognitive-Behavior Therapy and third-wave behavioral treatments) have the strongest empirical support for the treatment of BN spectrum disorders, as many as 70% of individuals with these disorders who undergo a full course of treatment remain symptomatic (Linardon, 2018). Further understanding of the components of behavioral treatments for BN spectrum disorders that promote reduction of symptomsis acutely needed.
Out-of-session assignments, often referred to as ‘homework’ (HW), have been emphasized as key components of behavioral treatments (BTs) for BN spectrum disorders (Cooper & Fairburn, 2010; Delinsky & Wilson, 2010; Thackwray, Smith, Bodfish, & Meyers, 1993; Wilson, Fairburn, Agras, Walsh, & Kraemer, 2002). The completion of HW assignments is presumed to assist individuals in acquiring and utilizing therapeutic skills and strategies. Specifically, HW facilitates generalization of skills taught in treatment to individuals’ daily lives, thereby disrupting patterns of eating disorder symptomatology (Kazantzis, Deane, & Ronan, 2000; Kazantzis et al., 2016) and improving treatment outcome (Spielmans et al., 2013; Wilson et al., 2002). BTs for BN spectrum disorders largely utilize three types of homework: 1) self-monitoring of eating and disordered eating behaviors designed to increase awareness of these behaviors and provide data about their antecedents and consequences, 2) behavioral assignments designed to practice treatment skills in daily life, and 3) written homework assignments designed to spur motivation for change (e.g. reflect on the pros and cons of changing eating behavior) and support behavioral skills use (e.g. brainstorming a list of alternative activities to use at home to manage urges) (Cooper & Fairburn, 2010; Fairburn et al., 2008; Wilson et al., 2002).
Many studies have investigated the link between HW compliance and outcome from BTs for various psychological disorders, but research evaluating the role of HW compliance in BTs for BN spectrum disorders is scarce. A handful of experimental studies have assessed the role of self-monitoring in promoting change in BN symptoms (Barakat et al., 2017; Hildebrandt & Latner, 2006; Latner & Wilson, 2002). For example, in two studies, adults with BN spectrum disorders filled out daily self-monitoring records indicating the food consumed and any episodes of binge eating for 7 days. This study found that daily self-monitoring for 7 days was associated with reductions in binge eating at the end of self-monitoring period (Hildebrandt & Latner, 2006; Latner & Wilson, 2002). In another study, during brief online guided self-help CBT program, self-monitoring was found to be linked to imrpovements in binge eating and eating disorder pathology at post-treatment (Barakat et al., 2017). To date, only one study has examined the role of all three types of HW assigned in in a full BT treatment protocol for BN spectrum disorders. Parker, Clark and Juarascio (Unpublished results) examined participant’s average compliance with self-monitoring HW, behavioral HW, and written HW, over the course of BTs for BN. They found that greater average compliance with behavioral HW (and not with self-monitoring and written HW) during treatment was associated with cessation of binge eating and compensatory behaviors within one month post-treatment (Parker, Clark, & Juarascio, Unpublished results). These results lend preliminary support to the positive relationship between HW compliance and post-treatment BN symptom improvement.
Research has yet to assess whether, during treatment, high HW compliance precedes or follows improvement in BN symptoms which limits understanding of the therapeutic role of HW compliance in promoting reductions in BN symptoms during treatment. HW compliance is expected to have relatively immediate effects on symptom change. For example, individuals who are more compliant with regular eating (a behavioral HW assignment involving eating every 3–4 hours) may be less likely to binge eat due to a decrease in dietary restriction. Alternatively, reductions in BN symptoms may enable a individual to engage in difficult HW assignments. Specifically, an individual experiencing a reduction in binge eating may be better able to regularly eat. Therefore, testing the weekly prospective associations among HW compliance and BN symptoms could clarify whether HW is a driver of change in BN symptoms. Moreover, clarifying whether HW compliance in a given week temporally precedes and predicts symptom improvement in the following week, or vice versa, can guide how the assignment of HW is used to promote, or maintain, specific types of therapeutic change. If greater compliance with behavioral HW is found to precede weekly reductions in behavioral BN symptoms (e.g., binge eating and purging) a therapist may assign specific behavioral assignments to a individual who is struggling to stop self-induced vomiting. Thus, elucidating if compliance with HW temporally precedes changes in BN symptoms and/or if symptom improvements foster greater compliance with HW, could inform treatment planning and implementation.
It is also important to understand the differential roles of overall degree of homework compliance (i.e., between-persons compliance) and greater than one’s usual HW compliance (i.e. within-person compliance) in predicting change in BN symptoms. If individuals who have poorer overall compliance with HW during a given week experience lesser reductions in binge eating frequency the following week, compared to patients who are more compliant, a therapist may devote subsequent session time to addressing barriers to HW implementation. Additionally, if a specific individual who generally demonstrates average compliance with HW assignments, experiences a plateau or increase in binge eating during treatment, a therapist may encourage greater than usual compliance with that week’s HW to promote reductions in binge eating the following week. Disentangling the associations among between- and within-person HW compliance and change in BN symptoms may elucidate how to more effectively harness HW assignments to promote BN symptom change during treatment.
In the current study, we examined the prospective association between HW compliance and change in BN symptoms, and vice versa, by utilizing session-by-session measurements of both of these constructs over the course of treatment. Identifying when compliance with HW is likely to decreases or increases can be used to inform clinical decisions about when additional support and guidance on maintaining compliance with HW assignments should be provided. To understand how and when during treatment HW compliance changes, as a preliminary aim we assessed the trajectory of session-by-session change in compliance with three types of HW (self-monitoring, behavioral HW, and written HW) during BT for BN. The primary aim of the study was to determine the prospective relationships among weekly HW compliance and BN symptoms (e.g., binge eating, compensatory behaviors, dietary restriction). We hypothesized that: 1) greater weekly between-persons HW compliance would predict reductions in BN symptoms the following week; 2) greater weekly reductions in between-persons BN symptoms would predict greater HW compliance the following week; 3) greater weekly within-person HW compliance would predict greater reductions in BN symptoms the following week; and 4) greater weekly reductions in within-person BN symptoms would predict greater HW compliance the following week.
Method
Participants and procedures
The sample included 42 adults (MeanAge = 32.06, MeanBMI = 26.18, 88.10% female; see Table 1 for demographics and baseline BN spectrum eating disorder symptoms by treatment condition) experiencing 12 or more objectively- or subjectively-large binge eating episodes and 12 or more compensatory behaviors (including purging behaviors, driven exercise, and/or other extreme weight control behaviors) over the previous three months (American Psychiatric Association, 2013), who participated in a pilot randomized controlled trial (PI: Juarascio; K23 MH105680; (Juarascio et al., 2021) evaluating the feasibility, acceptability, and preliminary efficacy of a novel mindfulness and acceptance-based behavioral treatment (MABT) compared to the focused version of CBT-E for BN (Fairburn, 2008). Two patient included in the parent trial had BMI < 18.5 kg/m2 and were excluded from the present analysis to maintain homogeneity of the sample.
Table 1.
Demographic characteristics and baseline eating disorder symptoms by treatment condition.
| MABT (N = 25) | CBT (N = 17) | |
|---|---|---|
| % (N) | % (N) | |
| Sex | Female: 88.0% (22) Male: 12.0% (3) |
Female: 88.2% (15) Male: 11.8% (2) |
| Race/Ethnicity | Asian/Pacific Islander: 8.0% (2) Black/African American: 8.0% (2) Caribbean/Haitian: 4.0% (1) Latinx/Hispanic: 4.0% (1) White: 76.0% (19) |
Asian/Pacific Islander: 5.9% (1) Black/African American: 5.9% (1) Caribbean/Haitian: 0.0% (0) Latinx/Hispanic: 29.4% (5) White: 58.8% (10) |
| Mean (SD) | Mean (SD) | |
| Age | 29.80 (11.19) | 34.76 (14.61) |
| BMI (kg/m2) | 25.31 (5.64) | 28.11 (5.92) |
| Baseline Past Month Binge Episodes | 25.72 (16.11) | 28.41 (19.16) |
| Baseline Past Month Total Compensatory Behaviors | 29.80 (20.09) | 37.29 (29.29) |
| Baseline Past Month Vomiting Episodes | 14.28 (16.05) | 19.12 (26.08) |
| Baseline Past Month Laxative Misuse Episodes | 2.40 (7.25) | 2.35 (4.34) |
| Baseline Past Month Diuretics Misuse Episodes | 0.36 (1.60) | 2.06 (6.90) |
| Baseline Past Month Days with Driven Exercise | 9.56 (10.62) | 10.24 (11.58) |
| Baseline EDE Global Score | 3.28 (1.15) | 3.52 (0.89) |
Note: The groups did not significantly differ in any of the demographic or eating disorder symptom variables depicted above.
Patient were recruited from the community and provided informed consent. Eligible patient (N=42), were randomized to receive 20 sessions of manualized CBT (n=17) or MABT (n=25). Demographic characteristics of study patient is shown in Table 1. In both treatment conditions, patient received eight twice-weekly sessions, nine weekly sessions, and three biweekly sessions over the course of five months. Both treatments assigned three types of homework (self-monitoring, behavioral HW, and written HW) in similar amounts. MABT and CBT were delivered to all patient based on standardized manuals, which included standard weekly homework assignments (see (Juarascio et al., 2021) for more information about the treatments). Self-monitoring homework was initially assigned in session 2 and was assigned as a daily assignment throughout treatment in both conditions. Behavioral assignments were initially assigned in session 3 and completed daily throughout treatment. Written homework assignments were initially assigned in session 1 and assigned at 16 sessions in MABT and were initially assigned in session 4 and assigned at 9 sessions in CBT. Written homework varied from a one-time worksheet to daily tracking of triggering situations or behaviors across a given week of treatment (see Supplemental Table 1 for more information about HW assignments). We first ran all analysis with treatment condition as a predictor and found similar results for each of the study aims for both treatment groups. Thus, we decided to collapse the data across both treatment conditions. Increasing the sample size provided greater power to generate more reliable estimates for present study aims. 12 paprticipants discontinued treatment during the study. On average, patient who dropped out of treatment completed 16 sessions. The most common reason for treatment discontinuation was being too busy in personal life to prioritize treatment. Three patient were removed from the study at session 8, 9 and 12 for the following reasons: co-morbid substance abuse interfering in treatment engagement, boundary violation with the therapist and active suicidal ideation during treatment. The treatments were highly manualized and delivered individually by a trained graduate student clinician. The study included 14 clinicians who received ongoing weekly training and supervision by the principal investigator, a licensed psychologist. The study was approved by the University Institutional Review Board.
Measures
Demographics.
Patient self-reported their demographics at the baseline assessment.
Weekly compliance with self-monitoring.
Self-monitoring was assigned at all sessions after the first session (i.e., intake session). Compliance with self-monitoring was rated by the therapist on a 1–4 scale based on the percentage of monitoring forms completed (1= Completed 0–25%, 2= Completed 26–50%, 3= Completed 51–75%, 4= Completed 76–100%).
Weekly compliance with behavioral assignments.
Behavioral HW (e.g., regular eating, urge surfing) was assigned every session after session three. Compliance with behavioral HW was rated by the therapist on a scale of 1–4 (1= Did not attempt; 2= Poor- participant did not achieve the specified goal in terms of intensity or frequency; 3= Average- participant met the behavioral goal, but did not surpass; 4= Excellent - participant went above and beyond to challenge him/herself).
Weekly compliance with written assignments.
Written HW (e.g., reflect on the pros and cons of changing one’s behaviors, creating a list of binge trigger foods) was assigned starting session seven and continued until session nineteen. Compliance was only rated when written assignments were brought to the session. Compliance with written HW was rated by the therapist on a scale of 1–4 (1= Did not attempt; 2= Poor- Written assignment was attempted with little effort, partially completed and/or of low quality; 3= Average- Written assignment appeared to be done in an average way; 4= Excellent- Written assignment was 100% completed in a thoughtful manner).
Of note, at every session, physical self-montoring forms and written HW assignments (e.g., binge analysis worksheet) were collected by therapist to rate HW compliance. In addition, during HW review portion of every session, therapist asked targeted questions about completion of behvaioral assignment in the past week (e.g., Were there opportunities in past week to use urge management skills? How did you use urge management? On how many days in the past week did you use this skill?) to inform compliance ratings for behvavioral HW assignments. All compliance ratings were completed immediately following the session to prevent therapist recall bias. These measures were undertaken to improve reliability of therapist ratings of HW compliance.
Weekly BN symptoms.
In weekly post-session surveys, therapists reported patient’ frequency of binge eating (i.e., any eating episode where loss of control was experienced, regardless of the amount of food consumed), purging episodes (i.e., total number of vomiting, laxative and diuretics misuse episodes), and days of compulsive exercise by answering the following question: “During the past week, how many [episodes of behavior] did the participant report?” Therapists rated how often patient engaged in restrictive eating in the past week by rating the statement, “During the past week, participant deliberately limited his or her food intake to influence shape or weight,” on a scale from 0 (not at all) to 6 (all of the time). Therapists queried patient during therapy sessions and consulted self-monitoring records to determine the frequencies of these behaviors.
Statistical analyses
Missing session-by-session data on weekly compliance on three types of HW assignments and weekly BN symptoms were imputed with five iterations using Markov chain Monte Carlo (MCMC) method. Because weekly HW compliance was rated at every session, we only used ratings from sessions 2 (i.e., end of week 1), 4 (i.e., end of week 2), 6 (i.e., end of week 3), and 8 (i.e., end of week 4) during the twice-weekly phase to ensure that ratings were not double counted during the twice weekly period. For sessions 9–17 (weekly) and sessions 18–20 (biweekly), we used ratings from each session. For the preliminary aim, each type of HW assignment, the intercept, linear, and quadratic effects (growth parameters were centered at session number when a specific HW was assigned for the first time) were modeled. All models were estimated using full maximum likelihood estimation using all available data. Model-building procedures detailed by Singer and Willett (Singer & Willett, 2003) were utilized, and specification of random effects was based on the likelihood ratio test.
For primary aims 1 and 2, we employed linear mixed effects modeling to analyze individual change over time (Singer & Willett, 2003). We lagged the HW compliance ratings by a week for each type of HW assignments. We disaggregated the between-persons effects (participant’s mean HW compliance across all time points subtracted from the grand mean of all participant’s compliance during the entire treatment) and within-person effects (each participant’s mean compliance over all of the sessions subtracted from their compliance measured at each session) (Wang & Maxwell, 2015). Separate models were conducted that simultaneously included time-lagged between-persons effects modeled as random effects and within-person effects modeled as fixed effects for HW compliance with each of the assignments (i.e., self-monitoring, behavior and written HW) as predictors and each of the BN symptoms (i.e., days of restrictive eating, frequency of binge eating, purging and days of compulsive exercise) entered as outcomes. We included fixed and random effects of time in the model to control for general effects of time (i.e., detrending, (Wang & Maxwell, 2015)). Finally, BN symptoms in the previous week, HW compliance the following week and treatment condition were entered as covariates. To account for the dependence within the session-by-session data, first order autoregressive (AR[1]) structure was used. An unstructured covariance structure was chosen, which allowed intercept and slopes to correlate.
For primary aims 2 and 4, we lagged BN symptoms by a week (binge eating, purging, compulsive exercise and restrictive eating). We disaggregated the between-persons effects and within-person effects for BN symptoms. Separate models were conducted that simultaneously included time-lagged between-persons effects modeled as random effects and within-person effects modeled as fixed effects for BN symptoms with each of the Bn symptoms as predictors and each of HW assignment entered as outcomes. Fixed and random effects of time in the model to control for general effects of time were included. Finally, HW compliance in the previous week, BN symptoms the following week and treatment condition were entered as covariates. To account for the dependence within the session-by-session data, first order autoregressive (AR[1]) structure was used. An unstructured covariance structure was chosen, which allowed intercept and slopes to correlate.
Alpha was set at .01 to account for multiple comparisons. To make the results more easily interpretable, we also estimated pseudo-R2, i.e. the proportion of residual variance explained by the between- and within-person effects of changes in HW compliance (Singer & Willett, 2003). All statistical analyses were conducted using SPSS v.26 (SPSS, 2019).
Results
Trajectory of session-by-session change in HW compliance during treatment
Growth curves and analyses for compliance with each type of HW are shown in Figure 1 and Table 2. Significant negative linear and positive quadratic change was observed in self-monitoring ratings over time, such that initial compliance decreased more rapidly and then slowed somewhat over time. There was a significant positive linear (b = 0.07, SE = 0.03, p = 0.01) and non-significant quadratic change over time in compliance with behavioral HW, such that compliance with behavioral HW improved at a steady rate throughout treatment. For written HW compliance, a negative linear and non-significant quadratic change indicated a decline in compliance with written HW at a constant rate over time (b = −0.04, SE = 0.05, p = 0.04).
Figure 1:
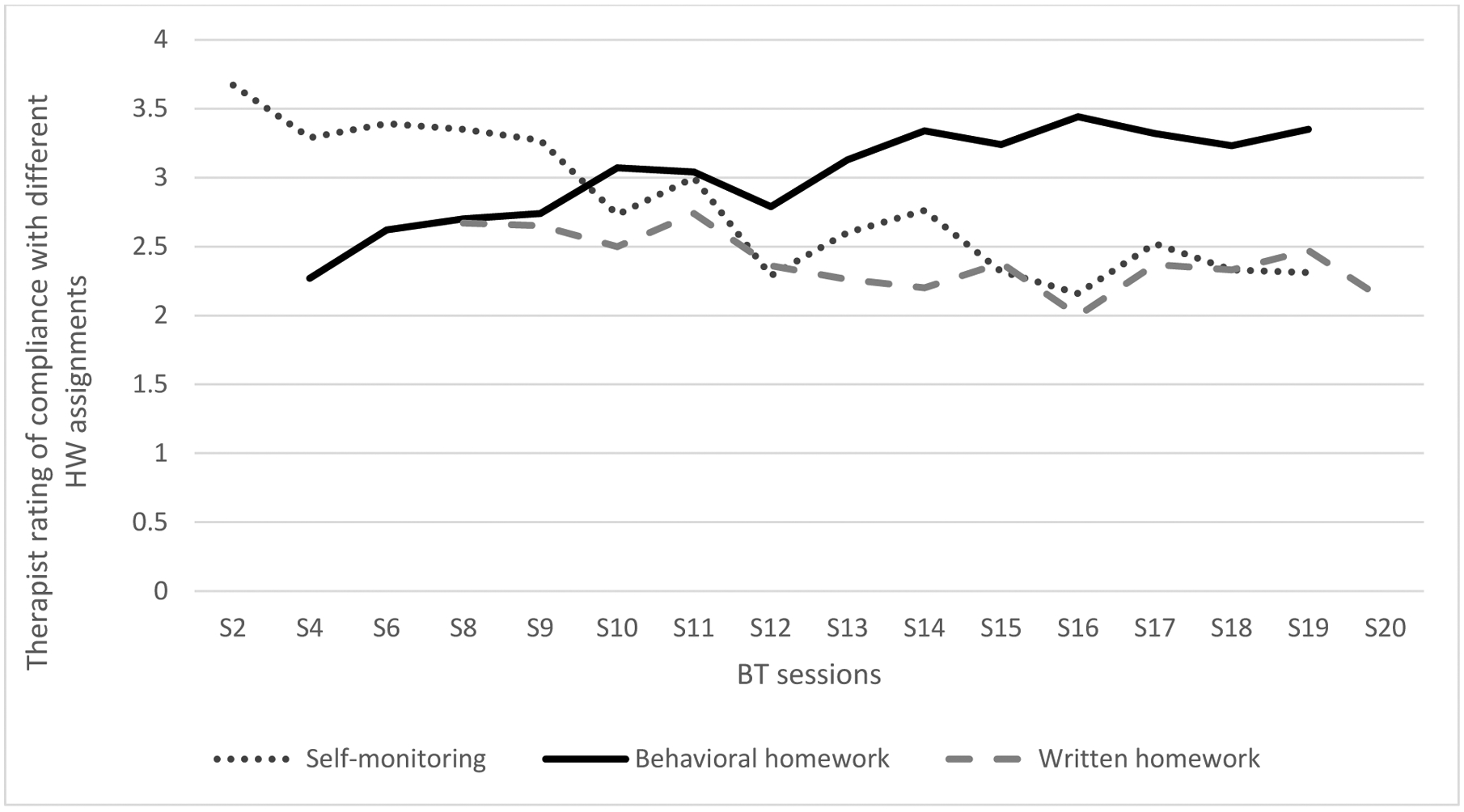
Trajectory of change in average weekly compliance with three types of HW assignments during the course of BTs for BN across all study patient.
Table 2:
Growth curve analysis for HW compliance in BT for BN
| Homework assignment | b | S.E | t | p | |
|---|---|---|---|---|---|
| Self-monitoring | Intercept | 5.59 | 0.16 | 33.35 | <0.001** |
| Linear | −0.21 | 0.05 | 4.15 | <0.001** | |
| Quadratic | 0.01 | 0.01 | −5.49 | <0.001** | |
| Behavior homework | Intercept | 2.75 | 0.08 | 33.10 | <0.001** |
| Linear | 0.07 | 0.03 | 2.90 | 0.01* | |
| Quadratic | −0.02 | 0.01 | −1.80 | 0.08 | |
| Written homework | Intercept | 3.48 | 0.10 | 34.36 | <0.001** |
| Linear | −0.04 | 0.05 | −0.70 | 0.04 | |
| Quadratic | 0.001 | 0.01 | 0.46 | 0.65 |
Note:
designates p-value at the 0.01 significance level;
designates p-values at the <0.001 significance level
Prospective association between weekly between-persons HW compliance and change in BN symptoms
Significant between-persons effects of self-monitoring compliance on binge eating (γ = −1.09, p < 0.01) and purging (γ = −1.05, p = 0.01) were detected, such that patient with greater self-monitoring compliance in previous week experienced greater reductions in binge eating and purging in the following week (see Table 3). Significant between-persons behavioral HW compliance on restrictive eating (γ = −1.05, p < 0.01), binge eating (γ = −1.07, p < 0.01) and purging (γ = −1.01, p < 0.01) were detected, such that patient with greater behavioral HW compliance in the previous week experienced greater reductions in binge eating and purging in the following week. Higher between-persons compliance with written HW in a given week did not prospectively predict improvements in BN symptoms (all ps > 0.01).
Table 3:
Prospective association of weekly compliance with different types of HW assignments and change in BN symptoms.
| Weekly between-persons HW compliance | BN symptoms in the following week | γ | S.E. | p | Pseudo-R2 |
|---|---|---|---|---|---|
| Self-monitoring | Binge Eating | −1.09 | 0.06 | < 0.001** | 0.24 |
| Purging | −1.05 | 0.10 | 0.01* | 0.29 | |
| Compulsive Exercise | 0.99 | 0.04 | 0.11 | 0.15 | |
| Restrictive Eating | 0.99 | 1.35 | 0.33 | 0.07 | |
| Behavioral HW | Binge Eating | −1.07 | 0.09 | <0.001** | 0.26 |
| Purging | −1.01 | 0.12 | <0.001** | 0.26 | |
| Compulsive Exercise | 0.85 | 0.08 | 0.55 | 0.03 | |
| Restrictive Eating | −1.05 | 0.09 | <0.001** | 0.20 | |
| Written HW | Binge Eating | −0.04 | 0.08 | 0.73 | 0.21 |
| Purging | 0.05 | 0.08 | 0.56 | 0.14 | |
| Compulsive Exercise | −0.01 | 0.06 | 0.82 | 0.12 | |
| Restrictive Eating | 0.79 | 0.15 | 0.64 | 0.12 | |
| Weekly within-person HW compliance | BN symptoms in following week | γ | S.E. | p | Pseudo-R2 |
| Self-monitoring | Binge Eating | −1.09 | 0.06 | 0.01* | 0.21 |
| Purging | −0.71 | 0.49 | 0.09 | 0.09 | |
| Compulsive Exercise | 1.04 | 0.13 | 0.22 | 0.11 | |
| Restrictive Eating | 0.68 | 0.22 | 0.59 | 0.13 | |
| Behavioral HW | Binge Eating | −1.08 | 0.10 | <0.001** | 0.27 |
| Purging | −1.12 | 0.07 | 0.01* | 0.27 | |
| Compulsive Exercise | 1.07 | 0.28 | 0.75 | 0.11 | |
| Restrictive Eating | −1.76 | 0.17 | <0.001** | 0.28 | |
| Written HW | Binge Eating | 0.07 | 0.18 | 0.39 | 0.09 |
| Purging | −0.05 | 0.24 | 0.21 | 0.07 | |
| Compulsive Exercise | −0.02 | 0.26 | 0.71 | 0.05 | |
| Restrictive Eating | 0.38 | 1.60 | 0.81 | 0.10 |
Note:
designates p-value at the 0.01 significance level;
designates p-values at the <0.001 significance level
Prospective association between weekly between-persons change in BN symptoms and HW compliance
Greater between-persons effects of BN symptoms in a given week did not prospectively predict self-monitoring compliance in the following week (all ps > 0.01) (see Table 4). Significant between-persons effects of improvements in binge eating (γ = −1.88, p < 0.01) on behavioral HW compliance were detected, such that patient who endorsed reduction in binge eating frequency in any given week demonstarted greater compliance with behvaioral HW in the following week. Higher between-persons improvements in BN symptoms in a given week did not prospectively predict compliance with written HW in the following week (all ps > 0.01).
Table 4:
Prospective association of weekly change in BN symptoms and compliance with different types of HW assignments.
| Weekly between-persons BN symptoms | Weekly HW compliance | γ | S.E. | p | Pseudo-R2 |
|---|---|---|---|---|---|
| Binge Eating | Self-monitoring | −0.09 | 0.34 | 0.99 | 0.01 |
| Behavioral HW | −1.88 | 0.10 | 0.01* | 0.26 | |
| Written HW | 0.02 | 0.14 | 0.61 | 0.05 | |
| Purging | Self-monitoring | 0.07 | 0.09 | 0.91 | 0.02 |
| Behavioral HW | −0.68 | 0.11 | 0.10 | 0.12 | |
| Written HW | 0.05 | 0.45 | 0.65 | 0.03 | |
| Compulsive Exercise | Self-monitoring | 0.04 | 0.28 | 0.83 | 0.01 |
| Behavioral HW | 0.25 | 0.38 | 0.36 | 0.09 | |
| Written HW | −0.08 | 0.36 | 0.89 | 0.02 | |
| Restrictive Eating | Self-monitoring | 0.04 | 0.18 | 0.98 | 0.01 |
| Behavioral HW | 0.11 | 0.12 | 0.16 | 0.04 | |
| Written HW | 0.01 | 0.26 | 0.99 | 0.01 | |
| Weekly within-person BN symptoms | Weekly HW compliance | γ | S.E. | p | Pseudo-R2 |
| Binge Eating | Self-monitoring | −1.21 | 0.13 | 0.01* | 0.22 |
| Behavioral HW | −1.00 | 0.12 | 0.01* | 0.28 | |
| Written HW | 0.14 | 0.63 | 0.28 | 0.09 | |
| Purging | Self-monitoring | −0.18 | 0.20 | 0.32 | 0.02 |
| Behavioral HW | −0.02 | 0.17 | 0.51 | 0.07 | |
| Written HW | 0.11 | 0.22 | 0.31 | 0.01 | |
| Compulsive Exercise | Self-monitoring | 0.08 | 0.21 | 0.31 | 0.06 |
| Behavioral HW | −0.12 | 0.14 | 0.26 | 0.09 | |
| Written HW | −0.01 | 0.26 | 0.35 | 0.06 | |
| Restrictive Eating | Self-monitoring | −0.61 | 0.43 | 0.56 | 0.03 |
| Behavioral HW | −1.00 | 0.12 | 0.01* | 0.23 | |
| Written HW | 0.11 | 0.53 | 0.51 | 0.03 |
Prospective association between weekly within-person HW compliance and change in BN symptoms
There was a significant within-person effect of self-monitoring compliance on binge eating, such that greater than one’s usual self-monitoring in previous week significantly predicted reductions in binge eating (γ = −1.09, p < 0.01) the following week (see Table 3). The pseudo-R2 for within-person self-monitoring compliance was 21%, suggesting that approximately 21% of the change in binge eating the following week stems from greater than one’s usual self-monitoring compliance in the previous week. Greater weekly within-person behavioral HW compliance in previous week significantly prospectively predicted improvements in restrictive eating (γ = −1.76, p < 0.01), binge eating (γ = −1.08, p < 0.01), and purging (γ = −1.12, p = 0.01). Greater weekly within-person behavioral HW compliance in the previous week explained 27%, 27%, and 28% of the reductions in binge eating, purging, and restrictive eating the following week, respectively. Greater weekly within-person written HW compliance during a given week did not prospectively predict improvements in BN symptoms in following week.
Prospective association between weekly within-persons change in BN symptoms and HW compliance
Significant within-person effect of improvements in binge eating on self-monitoring compliance were observed, such that lower than one’s usual frequency of binge eating in previous week significantly predicted greater self-monitoring compliance (γ = −1.21, p < 0.01) the following week (see Table 4). The pseudo-R2 for within-person self-monitoring compliance was 22%, suggesting that approximately 22% of the improvement in self-monitoring compliance in any given week is explained by lower than one’s usual frequency of binge eating in the previous week. Greater within-person improvements in restrictive eating (γ = −1.12, p < 0.01), binge eating (γ = −1.00, p < 0.01) in previous week significantly prospectively predicted behavioral HW compliance in the following week. Greater weekly within-person improvements in restrictive eating and binge eating in the previous week accounted for 23% and 28% improvement in behavioral HW compliance, respectively. Greater weekly within-person improvements in BN symptoms during a given week did not prospectively predict written HW compliance in following week.
Discussion
Although researchers have speculated that HW compliance may contribute to improvements in bulimic symptoms (Spielmans et al., 2013; Wilson et al., 2002), this study is the first to investigate whether HW compliance prospectively predicts change in eating disorder symptoms on session-by-session basis during BTs for BN spectrum disorders.
The study aimed to preliminarily examine the trajectories of change in HW assignment compliance during BTs for BN spectrum disorders. The following overall trajectories were observed: self-monitoring compliance declined over mid-to-late phases of treatment, behavioral HW compliance increased throughout treatment, and written HW compliance decreased throughout treatment. These trajectories may be related to the changing nature of session content across BTs for BN spectrum disorders—for instance, the decline pattern in self-monitoring may be indicative of the mid-to-late treatment phase refocusing of self-monitoring on potentially anxiety-provoking constructs (e.g., self-monitoring triggers for BE). Similarly, increased behavioral compliance over time may be related to patient building self-efficacy by repeatedly gathering successful experiences implementing behavioral skills (e.g., regular eating over time), encouraging further HW compliance(Hildebrandt & Latner, 2006; Latner & Wilson, 2002; Wilson et al., 2002). Written HW compliance decreased throughout treatment, likely because these assignments are time intensive; especially when paired with self-monitoring. However, this finding should be interpreted with caution given that therapists had room to flexibly assign HW (e.g., emphasize use of written HW).
As hypothesized, patient who engaged in greater overall self-monitoring in previous week relative to others had greater reductions in binge eating and purging in the following week. However, greater than one’s usual self-monitoring in the previous week predicted improvement only in binge eating in the following week. These findings are consistent with previous research demonstrating that self-monitoring is a powerful driver of reductions in binge eating (Hildebrandt & Latner, 2006; Latner & Wilson, 2002). Our results also suggest that greater overall levels of self-monitoring may be needed to reduce purging. Interestingly, both greater overall and greater than one’s usual self-monitoring compliance did not prospectively predict improvements in restrictive eating and compulsive exercise. Further research is needed to examine the functional role of restrictive eating and compulsive exercise, and to determine how self-monitoring intervenes to disrupt or facilitate those functional processes (e.g., it may be that restrictive eating and compulsive exercise could function as perceived ways of maintaining control over eating, shape, or weight, and self-monitoring these behaviors may reinforce control attempts (Dalle Grave, Di Pauli, Sartirana, Calugi, & Shafran, 2007; Mond & Calogero, 2009; Shafran, Fairburn, Nelson, & Robinson, 2003)
Consistent with our hypothesis, within-person reductions in binge eating frequency prospectively predicted improvements in self-monitoring compliance. Given that self-monitoring makes an individual aware of factors that could trigger a binge (Fairburn, 2008), it may be possible that greater reductions in binge eating frequency may have motivated an patient to engage in greater self-monitoring and learn about factors to prevent future binge eating. While we are limited in the ability to test this hypothesis, future research should explore factors (e.g., motivation, desire to learn about binge triggers) that may explain the prospective association between improvements in binge eating and self-monitoring compliance.
As hypothesized, both greater overall compliance and greater than one’s usual compliance with behavioral HW in the previous week were associated with greater improvements in restrictive eating, binge eating and purging in the following week. (Kazantzis et al., 2000; Kazantzis et al., 2016). Although previous research demonstrates links between certain behavioral skills (e.g., regular eating) and improvements in BN spectrum disorders (Fairburn, Agras, Walsh, Wilson, & Stice, 2004; Le Grange et al., 2012), our findings provide additional evidence that dedicating more effort and resources to behavioral skill use pays off in the short term (i.e., on session-by-session basis). Unexpectedly, both greater overall and greater than one’s usual behavioral HW compliance did not prospectively predict improvements in compulsive exercise. These results indicate a need for further examination of the maintenance factors for compulsive exercise (e.g., overvaluation of shape/weight) and how extant BTs’ behavioral assignments could better target those target maintenance factors.
Consistent with our hypothesis, both greater overall improvement in restrictive eating and lower than one’s usual restrictive eating significantly prospective predicted improvements in behavioral HW compliance. One plausible explanation for this finding could be that reduction in restrictive eating may improve overall energy levels and facilitate better engagement in behvaioral HW. For example, going for long periods without eating may produce energy deficit and take away from an individual’s ability to engage in behvaioral assignments (e.g., deliberately engaging in other domains of self-evaluation). Future research should examine factors potential factors (e.g., energy levels, mood stability) that may explain the role of improvement in restrictive eating and behvaioral HW compliance. As expected, lower than one’s usual frequency of binge eating significantly prospective predicted improvements in behavioral HW compliance. Reduction in binge eating may serve to improve behavioral HW compliance through several pathways (e.g., greater motivation to overcome binge eating and sense of self-efficacy etc). Future research should examine the role of potential factors that may contribute to improvement in behvaioral HW compliance.
Contrary to our hypothesis, greater overall and greater than one’s usual compliance with written HW in a given week did not prospectively predict reductions in any BN symptom the following week. Importantly, these findings do not necessarily mean that written HW serves no role improving BN symptoms. Indeed, these findings highlight relevant issues of measurement in the present study; for example, self-monitoring, behavioral, and written HW are not always mutually exclusive (e.g., written HW may facilitate or serve as a precursor to behavioral HW completion, detailed self-monitoring HW that includes pre-planning of skill use or extensive context/comments shares features of written HW). Future research examining specific types of written HW in isolation and how written HW is related to other HW types will be needed to better understand the clinical utility of written HW in this treatment context. Given the present study’s findings regarding the contributions of behavioral HW, it’s possible that written HW is beneficial insofar as itfacilitates practice of behavioral skills (i.e., completing a written worksheet on problem-solving prospectively predicts symptom reduction only when words on the page are translated into behavior that brings problem-solving practice to fruition.
Limitations of the study include a relatively small and mostly Caucasian female sample. Some results were likely impacted by floor effects of the specific eating disorder symptomatology in the current sample (e.g., absence of observed effect of any type of HW compliance in prospectively predicting change in compulsive exercise may partly be due to low weekly frequency of compulsive exercise across the sample, see Table 1). Future research should therefore attempt to replicate our findings in larger, more demographically- and clinically-diverse samples (Westra, Dozois, & Marcus, 2007). As this study was a secondary analysis of a larger clinical trial, a control group in which no HW was assigned was not included. Well-controlled experimental studies testing the independent and combined impact of compliance with three types of HW assignments on clinical outcomes (e.g., using a MOST design (Manasse, Clark, Juarascio, & Forman, 2019) are needed to further understand the role of HW compliance in improving BN spectrum disorders. Further, factors that may interfere with an inidvidual’s HW compliance, such as motivation, cost/resources, and competing priorities (Chakrabarti, 2014; Gatt et al., 2014), were not captured in this study. Thus, future studies that aim to replicate these findings may assess the role of factors that may interfere in HW compliance to inform the assignment of HW during treatment. For example, if competing priorities is found to be a barrier to HW compliance, smaller and more manageable HW may be assigned in session. We did not examine potential moderating variables (e.g., therapist competence) that may influence HW compliance (Westra et al., 2007). While study therapists were adherent to a manualized version of BT, there was room for flexibility and individual differences in HW assignment. Due to various patient characteristics, treatment circumstances, or provider biases/preferences, specific implementation of HW may have differed (e.g., prioritizing one HW assignment over another), and these details were not captured in our data collection. Additionally, HW compliance may have varied by therapist due to differing therapist skills in reinforcing HW compliance (e.g., providing a rationale for the assignment(s), clearly assigning and tailoring the homework to the patient’s problems as discussed in the session, and seeking reactions to the assignment and trouble shooting for problems that might prevent compliance). Future research should explore moderators of the relationship between HW compliance and BN symptomatology and also consider identifying therapeutic processes and therapist characteristics that promote weekly HW compliance (Jensen et al., 2020). The present study did not assess for inter-rater reliability of HW compliance ratings completed by therapists. While measures were undertaken to prevent variability in therapist ratings of HW compliance (e.g., operationalizing HW compliance, collecting self-monitoring forms as objective dat to inform self-monitoring compliance ratings), there could still be potential for variability in therapist ratings of HW compliance. Future studies should have well trained independent assessors rate the HW compliance ratings by therapist to establish reliability of therapist ratings. While measures were undertaken to increase therapist’s confidence that HW assignement was completed in the previous week (e.g., using physical paperwork to rate self monitoring and written HW, and asking targeted questions to assess for compliance with behavioral HW), there remains a possibility that patient overreported HW completion. Additionally, patient self-reported BN symptoms and may have underreported them. Although, research has shown high correlation between self-reporting and clinician rating of eating disorder symptoms (Wilfley, Schwartz, Spurrell, & Fairburn, 1997), future research should that aims to replicate these findings may utilize more objective methods of data collection on both HW compliance and BN symptoms (e.g., passive sensors (Smith et al., 2019). Importantly, while the present study provides support for the utility of self-monitoring HW and behavioral HW in BTs for BN, we are unable to draw conclusions as to why HW works. Future study using observational or experimental designs to elucidate the underlying functional models at play (e.g., how self-monitoring HW interrupts habitual patterns of behavior, how behavioral HW positively or negatively reinforces desired behavior change) is critical to understanding how HW compliance contributes to improved BN symptoms in the short- and long-term.
Overall, this study suggests that emphasizing HW assignments during BTs for BN spectrum eating disorders appears to be valuable. Clinical implications may include indication that patients should be strongly encouraged to engage in HW (especially behavioral assignments) in their day-to-day life. Resources abound with potential HW tasks and their associated necessary materials that can be adapted to individual patients’ needs, symptoms, and goals, including eating disorder-specific HW such as food diary self-monitoring templates (Fairburn et al., 2008)), imagery rescripting exercises (Waller, Turner, Tatham, Mountford, & Wade, 2019), exposure-based behavioral experiments (Waller et al., 2019) and mealtime strategies for parents/caregivers (Muhlheim, 2018). Though further research is necessary to understand the role of HW in eating disorders treatment, results from the present study are aligned with research on HW in BTs for other disorders (e.g., (Wheaton & Chen, 2021), suggesting that clinicians can speak confidently about the importance of HW adherence as an intervention generally speaking. Recent scholarship has highlighted the importance of clinician behavior in improving HW compliance (e.g., (Bunnell et al., 2021; Dobson, 2021), and denote the session time and clinician effort required to meaningfully develop, assign, and review HW (Dobson, 2021). Clinician actions such as delivering treatment with HW as an integral aspect of session structure may be recommended (e.g., confirming specific HW at the end of each session and prompting patients to write down the home practice tasks, including explicit HW review during each session to provide therapeutic accountability and reinforce the significance of HW completion) (Fairburn, 2008; Waller et al., 2019). Psychoeducation on the therapeutic process arguably should incorporate the message that “what you put into it is what you get out of it” and regard HW as a fundamental or essential part of fully completing treatment (Fairburn, 2008; Waller et al., 2019). The therapeutic stance can be firm (see description of “the five-minute session” by Waller and colleagues (Waller et al., 2007; Waller et al., 2019) and regard HW non-completion as a type of therapy-interfering behavior (Chapman & Rosenthal, 2016) or barrier to change (Fairburn, 2008). Clinicians can validate patients’ challenges in this area and acknowledge that HW can be difficult and provoke distress; incorporating additional strategies (e.g., distress tolerance skills) may therefore be beneficial (Fairburn, 2008; Waller et al., 2019). Techniques such as employing and reviewing routine outcome monitoring (Lambert, Whipple, & Kleinstäuber, 2018), using adjunctive mobile phone applications (Tang & Kreindler, 2017), and ensuring that HW assignments are congruent with patients’ session takeaways (Jensen et al., 2020) can further reinforce and support HW engagement on a session-by-session basis.
Supplementary Material
Clinical Implications:
Emphasizing homework compliance during behavioral treatment for bulimia is valuable
Self-monitoring compliance predicts reductions in binge eating and purging
Behavioral homework compliance predicts reduced binge eating, purging, restriction
Written homework should be assigned sparingly in behavioral treatment for bulimia
Acknowledgements
Funding:
This study was funded by a grant for the National Institute of Mental Health (grant number redacted).
Footnotes
Declaration of Interest: None.
Declarations: The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the Uniformed Services University of the Health Sciences (USUHS), or the U.S. Department of Defense.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. [Google Scholar]
- Barakat S, Maguire S, Surgenor L, Donnelly B, Miceska B, Fromholtz K, … Touyz S (2017). The role of regular eating and self-monitoring in the treatment of bulimia nervosa: a pilot study of an online guided self-help CBT program. Behavioral Sciences, 7(3), 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunnell BE, Nemeth LS, Lenert LA, Kazantzis N, Deblinger E, Higgins KA, & Ruggiero KJ (2021). Barriers Associated with the Implementation of Homework in Youth Mental Health Treatment and Potential Mobile Health Solutions. Cognitive Therapy & Research, 45(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarti S (2014). What’s in a name? Compliance, adherence and concordance in chronic psychiatric disorders. World journal of psychiatry, 4(2), 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman AL, & Rosenthal MZ (2016). Managing therapy-interfering behavior: Strategies from dialectical behavior therapy: American Psychological Association. [Google Scholar]
- Cooper Z, & Fairburn CG (2010). Cognitive behavior therapy for bulimia nervosa. The treatment of eating disorders: A clinical handbook, 243–270. [Google Scholar]
- Dalle Grave R, Di Pauli D, Sartirana M, Calugi S, & Shafran R (2007). The interpretation of symptoms of starvation/severe dietary restraint in eating disorder patients. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 12(3), 108–113. [DOI] [PubMed] [Google Scholar]
- Delinsky SS, & Wilson GT (2010). Cognitive behavior therapy with body image exposure for bulimia nervosa: A case example. Cognitive and Behavioral Practice, 17(3), 270–277. [Google Scholar]
- Dobson KS (2021). A Commentary on the Science and Practice of Homework in Cognitive Behavioral Therapy. Cognitive Therapy and Research, 1–7.34177004 [Google Scholar]
- Fairburn C, Cooper Z, Shafran R, Bohn K, Hawker D, Murphy R, & Straebler S (2008). Enhanced cognitive behavior therapy for eating disorders: the core protocol. Cognitive behavior therapy and eating disorders, 47–193. [Google Scholar]
- Fairburn CG (2008). Cognitive behavior therapy and eating disorders. New York, NY, US: Guilford Press. [Google Scholar]
- Fairburn CG, Agras WS, Walsh BT, Wilson GT, & Stice E (2004). Prediction of outcome in bulimia nervosa by early change in treatment. American Journal of Psychiatry, 161(12), 2322–2324. [DOI] [PubMed] [Google Scholar]
- Gatt L, Jan S, Mondraty N, Horsfield S, Hart S, Russell J, … Essue B (2014). The household economic burden of eating disorders and adherence to treatment in Australia. BMC psychiatry, 14(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildebrandt T, & Latner J (2006). Effect of self‐monitoring on binge eating: treatment response or ‘binge drift’? European Eating Disorders Review: The Professional Journal of the Eating Disorders Association, 14(1), 17–22. [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr., & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry, 61(3), 348–358. doi: 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen A, Fee C, Miles AL, Beckner VL, Owen D, & Persons JB (2020). Congruence of patient takeaways and homework assignment content predicts homework compliance in psychotherapy. Behavior Therapy, 51(3), 424–433. [DOI] [PubMed] [Google Scholar]
- Juarascio AS, Parker MN, Hunt R, Murray HB, Presseller EK, & Manasse SM (2021). Mindfulness and acceptance‐based behavioral treatment for bulimia‐spectrum disorders: A pilot feasibility randomized trial. International Journal of Eating Disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazantzis N, Deane FP, & Ronan KR (2000). Homework assignments in cognitive and behavioral therapy: A meta‐analysis. Clinical Psychology: Science and Practice, 7(2), 189–202. [Google Scholar]
- Kazantzis N, Whittington C, Zelencich L, Kyrios M, Norton PJ, & Hofmann SG (2016). Quantity and quality of homework compliance: a meta-analysis of relations with outcome in cognitive behavior therapy. Behavior Therapy, 47(5), 755–772. [DOI] [PubMed] [Google Scholar]
- Lambert MJ, Whipple JL, & Kleinstäuber M (2018). Collecting and delivering progress feedback: A meta-analysis of routine outcome monitoring. Psychotherapy, 55(4), 520. [DOI] [PubMed] [Google Scholar]
- Latner JD, & Wilson GT (2002). Self-monitoring and the assessment of binge eating. Behavior Therapy, 33(3), 465–477. [Google Scholar]
- Le Grange D, Lock J, Agras WS, Moye A, Bryson SW, Jo B, & Kraemer HC (2012). Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behaviour research and therapy, 50(2), 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J (2018). Meta-analysis of the effects of cognitive-behavioral therapy on the core eating disorder maintaining mechanisms: implications for mechanisms of therapeutic change. Cogn Behav Ther, 47(2), 107–125. doi: 10.1080/16506073.2018.1427785 [DOI] [PubMed] [Google Scholar]
- Manasse SM, Clark KE, Juarascio AS, & Forman EM (2019). Developing more efficient, effective, and disseminable treatments for eating disorders: an overview of the multiphase optimization strategy. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 24(6), 983–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond JM, & Calogero RM (2009). Excessive exercise in eating disorder patients and in healthy women. Australian & New Zealand Journal of Psychiatry, 43(3), 227–234. [DOI] [PubMed] [Google Scholar]
- Muhlheim L (2018). When your teen has an eating disorder: Practical strategies to help your teen recover from anorexia, bulimia, and binge eating: New Harbinger Publications. [Google Scholar]
- Parker MN, Clark KE, & Juarascio AS (Unpublished results). Homework compliance is related to outcomes from behavioral treatment for bulimia nervosa.
- Shafran R, Fairburn C, Nelson L, & Robinson P (2003). The interpretation of symptoms of severe dietary restraint. Behaviour research and therapy, 41(8), 887–894. [DOI] [PubMed] [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence: Oxford university press. [Google Scholar]
- Smith KE, Mason TB, Juarascio A, Schaefer LM, Crosby RD, Engel SG, & Wonderlich SA (2019). Moving beyond self‐report data collection in the natural environment: A review of the past and future directions for ambulatory assessment in eating disorders. International Journal of Eating Disorders, 52(10), 1157–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielmans GI, Benish SG, Marin C, Bowman WM, Menster M, & Wheeler AJ (2013). Specificity of psychological treatments for bulimia nervosa and binge eating disorder? A meta-analysis of direct comparisons. Clinical psychology review, 33(3), 460–469. [DOI] [PubMed] [Google Scholar]
- SPSS, I. (2019). IBM SPSS statistics for Windows, version 26.0. Armonk, NY: IBM Corp., 440. [Google Scholar]
- Tang W, & Kreindler D (2017). Supporting homework compliance in cognitive behavioural therapy: essential features of mobile apps. JMIR mental health, 4(2), e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thackwray DE, Smith MC, Bodfish JW, & Meyers AW (1993). A comparison of behavioral and cognitive-behavioral interventions for bulimia nervosa. Journal of consulting and clinical psychology, 61(4), 639. [DOI] [PubMed] [Google Scholar]
- Waller G, Cordery H, Corstorphine E, Hinrichsen H, Lawson R, Mountford V, & Russell K (2007). Cognitive behavioral therapy for eating disorders: A comprehensive treatment guide: Cambridge University Press. [Google Scholar]
- Waller G, Turner H, Tatham M, Mountford V, & Wade T (2019). Brief cognitive behavioural therapy for non-underweight patients. In: London, UK: Taylor and Francis Ltd. [Google Scholar]
- Wang LP, & Maxwell SE (2015). On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychological methods, 20(1), 63. [DOI] [PubMed] [Google Scholar]
- Westra HA, Dozois DJ, & Marcus M (2007). Expectancy, homework compliance, and initial change in cognitive-behavioral therapy for anxiety. Journal of consulting and clinical psychology, 75(3), 363. [DOI] [PubMed] [Google Scholar]
- Wheaton MG, & Chen SR (2021). Homework completion in treating obsessive–compulsive disorder with exposure and ritual prevention: A review of the empirical literature. Cognitive Therapy and Research, 45(2), 236–249. [Google Scholar]
- Wilfley DE, Schwartz MB, Spurrell EB, & Fairburn CG (1997). Assessing the specific psychopathology of binge eating disorder patients: Interview or self-report? Behaviour research and therapy, 35(12), 1151–1159. [PubMed] [Google Scholar]
- Wilson GT, Fairburn CC, Agras WS, Walsh BT, & Kraemer H (2002). Cognitive-behavioral therapy for bulimia nervosa: Time course and mechanisms of change. Journal of consulting and clinical psychology, 70(2), 267. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


