Abstract
Objectives
The COVID-19 pandemic has brought significant changes to family life, society and essential health and other services. A rapid review of evidence was conducted to examine emerging evidence on the effects of the pandemic on three components of nurturing care, including responsive caregiving, early learning, and safety and security.
Design
Two academic databases, organisational websites and reference lists were searched for original studies published between 1 January and 25 October 2020. A single reviewer completed the study selection and data extraction with verification by a second reviewer.
Interventions
We included studies with a complete methodology and reporting on quantitative or qualitative evidence related to nurturing care during the pandemic.
Primary and secondary outcome measures
Studies reporting on outcomes related to responsive caregiving, early learning, and safety and security were included.
Results
The search yielded 4410 citations in total, and 112 studies from over 30 countries met our eligibility criteria. The early evidence base is weighted towards studies in high-income countries, studies related to caregiver mental health and those using quantitative survey designs. Studies reveal issues of concern related to increases in parent and caregiver stress and mental health difficulties during the pandemic, which was linked to harsher and less warm or responsive parenting in some studies. A relatively large number of studies examined child safety and security and indicate a reduction in maltreatment referrals. Lastly, studies suggest that fathers’ engagement in caregiving increased during the early phase of the pandemic, children’s outdoor play and physical activity decreased (while screen time increased), and emergency room visits for child injuries decreased.
Conclusion
The results highlight key evidence gaps (ie, breastfeeding support and opportunities for early learning) and suggest the need for increased support and evidence-based interventions to ensure young children and other caregivers are supported and protected during the pandemic.
Keywords: COVID-19, Child protection, Community child health, Depression & mood disorders
Strengths and limitations of this study.
This examines families’ and children’s well-being during the COVID-19 pandemic from a holistic, multisectoral lens and highlights how education, health, and child protection all have a role in improving support for families so that the pandemic does not break the provision of nurturing care and wipe out decades of progress, especially for vulnerable families and children.
The review includes evidence from more than 30 countries, including low/middle-income contexts. As with other pandemic features, results show that not all families are affected equally: financially vulnerable families are much more likely to experience negative ramifications. The pandemic is also disproportionately affecting parents and other caregivers with young children, particularly mothers, those with pre-existing mental health difficulties and those caring for children with disabilities.
Future research is needed on studies related to nurturing care during the pandemic from low/middle-income countries, topics focused on issues related to opportunities for early learning, and those that use qualitative or mixed methods research designs. There is also a need for robust evaluations of parenting and other interventions to support families and children during emergencies that demand physical distancing measures and movement restrictions.
Introduction
Early childhood development is universally endorsed in the 2030 Sustainable Development Goals. The WHO, UNICEF and World Bank Group launched the Nurturing Care Framework in 2018 and advocate for optimal child development and multisectoral interventions that support families and reach very young children. The most formative experiences of young children come from nurturing care received from parents, other family members, caregivers and community-based services. Nurturing care is characterised by a stable environment that promotes children’s health and nutrition, responsive caregiving and early learning opportunities, and protection from safety risks and maltreatment. Families need support to provide nurturing care for young children, including material and financial resources, national policies such as paid parental leave, and provision of community-based services in health, nutrition, education, and child and social protection (for further details, see https://nurturing-care.org).
The COVID-19 pandemic has brought significant changes to family life, society and essential health and other services. Starting from March 2020, large-scale physical distancing measures and movement restrictions (ie, school closures, day-care closures, stay-at-home orders, lockdowns) lead widespread and sudden disruption across every continent. Early on the pandemic, global stakeholders raised concerns that critical components of nurturing care may be harmed, and child development was at risk due, in part, to reduced access to essential healthcare services, deteriorating economic circumstances, and caregiver stress and mental health—risks that were particularly pronounced in low/middle-income countries and among vulnerable populations.1 2
This rapid evidence review captures the emerging evidence during the first 7 months following COVID-19 being declared a pandemic in March 2020. It consolidates early evidence on the effects of the pandemic on three components of nurturing care: responsive caregiving, early learning opportunities, and child safety and protection from violence and neglect.3 Indeed, evidence from past epidemics and pandemics shows that public health emergencies were associated with increased caregiver social isolation and stress,4 disruption to family routines,5 traumatic stress among caregivers,6 family conflict and anxiety,7 early termination of breast feeding,8 and reduced play among children and engagement in team-based sports.9 The current review did not examine child health and nutrition—the other two components of nurturing care—because reviews have already been published in these areas. The current evidence synthesis was explored through different outcomes that are critical for nurturing care and child development. Responsive caregiving includes the good mental health of parents and caregivers, warm and responsive parent–child relationships, breastfeeding support to promote emotional bonds and attachment, and fathers’ engagement in caregiving. Early learning includes access to formal and home-based learning, parent–child reading and other early learning activities, and safe play spaces. Children’s safety and security include protecting children against injury, neglect and abuse, including child protection and referral services for suspected maltreatment. The review findings can help identify and conceptualise priority issues for early years’ policy and programming during health emergencies and identify the literature gaps where future studies are required.
Methods
We employed abbreviated systematic review methods to generate evidence in a short time (ie, 8 weeks). A single reviewer completed the study selection and data extraction with verification by a second reviewer, and we omitted formal quality assessments of the included studies. The population of interest is young children (birth–8 years old) and their caregivers, including birth parents, adoptive parents and caregivers. Studies involving children up to 18 years old and their caregivers are included if the studies had results for children under 8 years old. Published quantitative or qualitative studies that document their full methodology are included. Preprints and grey literature are included to ensure representativeness and reflect the rapidly evolving nature of COVID-19 pandemic impact evidence. Studies were published between 1 January 2020 and 25 October 2020.
As outlined in table 1, we focused on studies that reported outcomes related to responsive caregiving, access to and opportunities for early learning, and children’s safety and security during the pandemic. We searched two databases (ie, PubMed and ERIC) based on a search strategy developed and pilot tested in collaboration with a research team and librarian skilled in systematic review processes. Also, the review team manually searched the websites of more than 80 multilateral and bilateral organisations, internal NGOs (non-governmental organisations) and the grey literature. Lastly, we screened the reference lists of the included studies for further relevant citations. We restricted the search to English, French, Spanish and Portuguese papers because these were the research team’s languages. Identified records were exported and managed on Zotero. After removing duplicates, the titles and abstracts of the remaining records were screened against the eligibility criteria, followed by full-text screening. Next, we extracted data from the studies using a standardised form, with a second reviewer assessing for completeness and accuracy. Data extracted included, but were not limited to, investigators/authors, year of publication, setting, context, details of the methods and data collection, participants, outcomes, results and conclusions. Data extraction was guided by the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist items. The preliminary stages of the synthesis involved organising the extracted data by itemising the data into thematic areas and tabulating the results to systematically identify patterns within and between studies and variations across studies. Finally, because of the heterogeneity of the available primary studies, we synthesised the results narratively in the report (see online supplemental file 1 for the full search strategy).
Table 1.
The three components of nurturing care3 during COVID-19 investigated in the rapid review
| Components of nurturing care | Types of outcomes included in the review |
|
Responsive caregiving This is about the ability of the parent/caregiver to notice, understand and respond to their child’s signals in a timely and appropriate manner, and is considered the foundational component because responsive caregivers are better able to support the other components of nurturing care. |
|
|
Opportunities for early learning This is about any opportunity for a young child to interact with a person, place or object in their environment, and recognises that every interaction (positive or negative) or absence of an interaction contributes to the child’s brain development and laying the foundation for later learning. |
|
|
Safety and security This is about safe and secure environments for children and their families. It addresses physical dangers, emotional stress, environmental risks, and access to food and water. |
|
bmjopen-2021-050417supp001.pdf (107KB, pdf)
Patient and public involvement
No patient was involved. Advisory group members and service-user researchers provided input into the research reporting and interpreted results after review completion. These individuals brought their personal experience of the topic under review. They helped ensure that the review provides clear and relevant information for those involved in health and child development programming. The consultation and group discussion provided a check on the credibility of the synthesis, developing review implications and identifying evidence gaps. Stakeholders, including the public and health professionals, will be informed of the results through an online and publicly accessible research brief suitable for a non-specialist audience.
Results
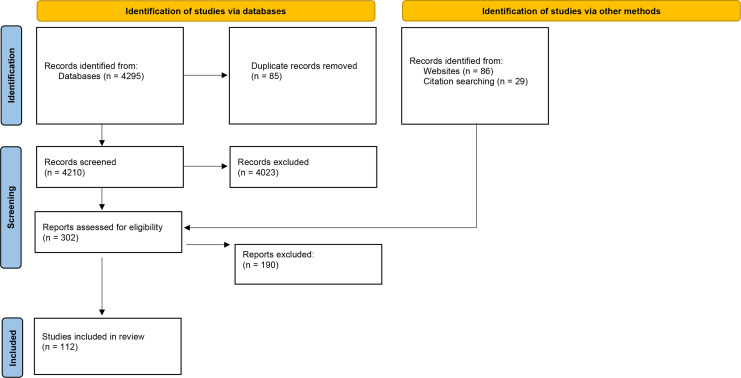
The initial search yielded 4295 papers from the database search, 86 publications through the organisational website search and 29 additional papers identified through reference lists. After the title, abstract and full-text review, 112 publications were included in the review. Excluded items were primarily irrelevant to the components of nurturing care and the population under review. The PRISMA flow diagram in figure 1 provides an overview of the study selection process.
Figure 1.
PRISMA diagram. PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analyses.
The findings show that 89 of the 112 studies (79%) were conducted in high-income countries. In contrast, research from low/middle-income countries was far more limited during the earlier period of the pandemic. We identified relevant studies from the following low/middle-income countries: Bangladesh, Brazil, Cambodia, China, Ethiopia, India, Iran, Mexico, Nigeria and Turkey. In total, 53% of the papers focused predominantly on issues related to responsive caregiving. The most common topics under this theme related to parent and caregiver stress, burnout, depression and anxiety during the COVID-19 pandemic. In total, 32% of the studies examined children’s safety and security, including child abuse and neglect referrals to child protection services and emergency department visits for child injuries. Lastly, only 19% of studies focused on early learning and play during the COVID-19 pandemic, including screen time among children, outdoor play and physical activities and home-based learning. Furthermore, results indicate that 85% were quantitative studies (primarily cross-sectional surveys). In contrast, only 8% were qualitative studies, and 7% were mixed methods designs. Thus, the early evidence base is weighted towards studies in high-income countries, studies related to caregiver mental health and those using quantitative survey designs. In contrast, there are relatively fewer studies from low/middle-income countries, topics focused on issues related to opportunities for early learning during the pandemic, and those that use qualitative or mixed methods research designs. Key findings of included studies are synthesised in the following sections. A summary of each study can be found in the online supplemental file 2.
bmjopen-2021-050417supp002.pdf (585.5KB, pdf)
Responsive caregiving: parent and caregiver stress and mental health
The review indicates that caregivers’ and primarily mothers’ mental health has been among the most researched topics related to nurturing care during the early stages of the pandemic, with more than 30 studies across various geographical and demographic contexts examining the implications of the COVID-19 pandemic on parent and caregiver stress, burnout, depression and anxiety.10–45 The presented evidence indicates that the pandemic has been detrimental to caregiver stress and mental health, particularly for parents and other caregivers of young children and mothers,14 16 30 31 33 being single,30 economically vulnerable families14 27 42 and those with pre-existing mental health issues.14 42 In addition, studies suggest that parents and caregivers of children with disabilities showed a heightened prevalence of depressive symptoms, anxiety and stress during the pandemic.11 18 30 43 While this evidence base is heterogeneous, with variations in the data, context and methodology, the findings generally reveal that the pandemic and its related containment measures was associated with increases in caregiver stress and poor mental health.
For example, a study of 192 Italian mothers found that 29% of mothers who had given birth during COVID-19 physical distancing measures and movement restrictions had an Edinburgh Postnatal Depression Scale (EPDS) global score above the cut-off score of >12, compared with only 12% in the control group who had given birth during the same period the year before COVID-19.45 Likewise, a study of 651 Finnish parents of children (aged 5–8 years old) found that 26% met the clinical EPDS cut-off score for potential depression during the pandemic, compared with 15% among the same sample of parents with data collected between 2014 and 2019.33
While the literature identified multiple and often overlapping COVID-19-related stressors that adversely affected parents’ mental health, economic insecurity stands out as one of the most consistent sources of parent and caregiver stress.12 24 25 28 42 46–49 For example, using data from 2174 Bangladeshi mothers with children aged 0–5 years old, Hamadani et al25 found that 96% of respondents experienced a reduction in paid work during COVID-19 physical distancing measures and movement restrictions, with average monthly family income falling from US$212 to US$59; and food insecurity increasing by more than 50%. Self-reported maternal depressive symptoms, as measured by the Centre for Epidemiologic Studies-Depression Scale, increased dramatically during the COVID-19 period compared with before the pandemic; and nearly 70% of the sample reported that their anxiety had risen during the COVID-19 physical distancing measures and movement restrictions. A US study of 561 parents and other caregivers of young children (aged 2–7 years old)—who were hourly workers—found that most respondents reported a loss of household income (69%) and job loss (60%), which linked with increased anxiety, depression, anger and irritability, as well as worse sleep quality among caregivers.24 The results indicate that parents’ and children’s well-being was strongly associated with the number of crisis-related hardships.
Numerous studies found that parent and caregiver stress, depression and anxiety during the COVID-19 pandemic were associated with reduced responsive caregiving, including, for example, lower parent–child closeness and more avoidant or harsher parenting attitudes and behaviours.10 13 16 27 28 32 37 38 41 42 48 For example, a New Zealand study found that parents of young children (aged 4–5 years old) who experienced more significant depressive symptoms and perceived stress during COVID-19 physical distancing measures and movement restrictions reported harsher parenting and less warm/responsive parenting, as measured by the Parenting Styles and Dimensions Questionnaire; and parent–child relationships were also of lower quality.32 In addition, a US study of low-income families with preschool-aged children found that parental job loss and income loss during the pandemic were strongly associated with parents’ depressive symptoms, stress, diminished sense of hope and negative parent–child interactions, including losing their temper or yelling at their child.27 However, parents who lost their job but did not experience corresponding household income decline (perhaps due to economic stimulus relief and other social protection measures) were more likely to report enjoying spending time with their child during the COVID-19 pandemic and engaging in positive parent–child interactions, such as playing with or hugging their child, compared with those who experienced a decline in household income. The authors suggest that efforts to support families’ economic security may help address parents’ and other caregivers’ mental health needs and reduce adverse parenting risks during the pandemic. Studies also noted more couple conflict50 and increased substance use51 among parents and caregivers experiencing stress and anxiety during the pandemic. One study found mothers rarely used mental health services during the COVID-19 pandemic due to various barriers, such as a lack of time or energy, service cost, not believing they needed such services and uncertainty on access.14
Studies found that partner support and cooperative co-parenting,13 14 20 32 and moderate physical exercise17 29 were associated with better mental health and coping among parents and caregivers during the pandemic. Lastly, some studies point towards mixed and potentially positive impacts of the COVID-19 restrictions on deepening family ties, improving couples’ relationships, and developing new family hobbies or activities.13 22 46 52–54 However, such positive benefits were typically found among parents and caregivers of older children (ie, adolescents) and families with several protective factors, including financial stability, comfortable and safe homes, enough food to eat, good health and healthy couple relationships.22 46 Unfortunately, few studies from the early pandemic discussed potential interventions to support parents and other caregivers with COVID-19-related stress, anxiety, and mental health issues or ways to protect parents’ capacity for responsive caregiving, signalling a significant gap in the evidence.
Responsive caregiving: breastfeeding support
Five studies related to breastfeeding support during the pandemic indicate reduced breastfeeding support and care.55–59 For example, over a quarter of respondents in a national UK study struggled to access breastfeeding support during the pandemic, and some stopped breast feeding before they intended to.55 Among the women who stopped breast feeding during the pandemic, the most common reason was the lack of breastfeeding support and face-to-face help with practical issues, such as latching. Some valued digital consultations for lactation support were made available. In contrast, others reported feeling violated and described how they felt discomfort recording their infant trying to latch onto the breast.59 Some breastfeeding women said positive benefits during COVID-19 physical distancing measures and movement restrictions, including having more time to focus on breast feeding, fewer visitors, more privacy and more support from fathers.58 Notably, we did not find studies on breastfeeding support in low/middle-income countries during this early pandemic period. Also, there was an absence of studies related to skin-to-skin contact and social support during labour, other components that are important for early bonding.
Responsive caregiving: fathers’ engagement in childcare
In total, eight studies reported that fathers took on more childcare responsibilities during the COVID-19 pandemic.60–67 For example, a survey of 1536 Australian parents of children (aged 0–16 years old) reported that fathers averaged 2.21 daily hours on active childcare before the pandemic, and this average increased to 3.64 hours during the pandemic, thereby narrowing the childcare gap between mothers and fathers.62 Therefore, the evidence suggests that increases in fathers’ time at home during COVID-19 may have, at least temporarily, reduced gender gaps in childcare division. However, mothers continued to carry the burden of extra childcare and household responsibilities.68 Furthermore, gendered employment patterns were exacerbated during the pandemic.60 67 69–71 Mothers were more likely than fathers to lose their jobs during the crisis, spend less time on paid work and be interrupted during work hours, principally by childcare. We did not find studies with an explicit focus on parents and other caregivers of infants and young children and how they have negotiated childcare responsibilities and household work during the pandemic, which may be more time-consuming and demanding than for parents of school-aged children and adolescents. There was also a lack of studies discussing male caregivers’ perspectives and caregiving experiences during the pandemic.
Opportunities for early learning
Evidence on home-based early learning during the COVID-19 pandemic is limited. What is available indicates that children in early childhood or pre-primary education often did not have contact with teachers or access to remote early learning during school closure.66 72 73 For example, a study of Ethiopian parents and caregivers of young children found that only 10% of children who enrolled in pre-primary schooling had been in contact with teachers or school principals during school closures.73 In this study, half of parents and caregivers reported supporting educational or learning activities for pre-primary children, with significant differences by household wealth and across regions. Children living in rural or remote areas had significant disadvantages regarding access to electricity, technologies, and children’s books or learning materials. Other studies provide evidence of frustration and negative attitudes among caregivers about distance learning benefits and values, especially for preschool-aged children.74–76 Some studies report that home-based learning is challenging for young children for various reasons, including limited learning materials and technological barriers.77 78 Children looked after by grandparents faced challenges due to little awareness about online technologies.77 Some studies find that parents engaged more in adult–child reading and other learning activities during the pandemic,66 73 while others reported they engaged less than before.72 Parents who met the criteria for probable major or severe depression and parenting stress during the pandemic were less likely to perceive being prepared to educate their child at home.79 Ultimately, the number of studies related to formal or informal opportunities for early learning was scarce during the first months of the pandemic, marking a critical evidence gap.
Early learning: play and physical activity during COVID-19
Nine studies reported that COVID-19 restrictions, such as the closure of schools and playgrounds, the cancellation of sports and activity classes, and reduced social interactions with peers, were linked to reduced outdoor play and physical activity and more sedentary behaviour among children.72 80–88 In some studies, parents noted concerns about the lack of social interaction, sedentary behaviour and limited physical activity during COVID-19 school closures.21 79 80 A study of parents of children (aged 2–4 years) reported that almost half of the children spent no time playing with another child in their household during COVID-19 physical distancing measures and movement restrictions.21 One study found that nearly 9 out of 10 Canadian parents reported increased screen time since the beginning of the pandemic among young children aged 18 months old to 5 years old.81 More than half of the parents in this study reported that children’s physical activity decreased during the pandemic, citing challenges due to the lack of indoor space and the variety of available toys. Another study found a dramatic decline in children’s outdoor physical activity and much higher screen time use (average of 5 hours/day) during the initial period of the COVID-19 outbreak, compared with before the restrictions.83 Play indoors did not seem to replace active play outdoors, resulting in a net decline in children’s play-based activities. Cities and areas with the highest number of COVID-19 cases, and thus most stringent restrictions, had the most significant drop in children’s outdoor play.84 Living in houses (as opposed to apartments) was correlated with increased outdoor activities.86 Notably, despite an urgent need, we did not find studies on the implementation or evaluation of training programmes for families to improve play interactions, home routines, and capacity to communicate with children during home quarantine or physical distancing measures.
Safety and security: child protection from violence and neglect
Thirteen studies across seven countries, mainly using publicly available administrative data, suggest that referrals of potential abuse, neglect and maltreatment to child protective services were substantially lower during the COVID-19 pandemic than before COVID-19 measures were put in place.89–101 Thus, evidence indicates that COVID-19 has reduced child maltreatment referrals. For example, a study based on data from January 2015 to May 2020 for New York City’s Administration for Children’s Services reports there were 29% fewer allegations of child maltreatment for March 2020—when school closures first began—compared with previous years.96 In addition, education personnel and other mandated reporters reported substantially fewer child maltreatment allegations, including childcare personnel and medical health personnel during this time. Non-mandated reporters, including family members and neighbours, also made fewer referrals, which may be linked to social distancing and limited contact between children and those outside their households. Bullinger et al found in the USA that while emergency calls for domestic crimes rose in March and April 2020, calls for potential child abuse fell, potentially due to the lessened visibility of child victims than adults.90 91 Furthermore, surveys of child protection workers similarly reported decreased referrals and more difficulty identifying children and families in need during COVID-19 large-scale physical distancing measures and movement restrictions.99 102 103 These changes do not reflect an actual reduction in the incidence or prevalence of maltreatment. Instead, the decrease in referrals is likely due to the given physical distancing measures and movement restrictions that preclude children from having in-person contact with educators and other mandated reporters.
Two studies indicate a striking rise in child abuse-related injuries among babies and toddlers during the pandemic.104 105 Comparing cases of children’s head trauma caused by suspected abuse, there were 10 cases at an urban medical facility in the UK over the March–April 2020 period, representing an increase of 1493% compared with the previous 3 years preceding the onset of the COVID-19 pandemic.105 Although alarming, it is important to consider that COVID-19 has led to significant healthcare delivery changes. Many centres have diverted non-COVID-19-related health emergencies to specific healthcare facilities, which may account for increased abuse of head trauma at institutions. One study found that COVID-19 job loss among parents and caregivers was significantly associated with psychological maltreatment, including verbal threats, belittling and ridiculing, with more significant effects for younger children.106
Safety and security: child injuries
Nine studies from eight countries reported a significant reduction in emergency department presentations and operations for injuries among children during government-imposed physical distancing measures and movement restrictions, primarily related to admissions and operations for sporting-related injuries and those that occur on playground bans on sports and access to playgrounds.107–115 Thus, data on emergency department visits and injuries suggest that children’s environments shifted during COVID-19 school closures and movement restrictions and presented different child safety threats. For example, a study based on data from a large acute paediatric hospital in London, UK found that the prevalence of referrals for child injuries was reduced by nearly two-thirds from 17 March to 28 April 2020 during COVID-19 physical distancing measures and movement restrictions, compared with the same period in 2019.111 In contrast, some centres found a relative increase in child injuries during the pandemic, including bicycle injuries,107 109 burn injuries,116 ingestions and poisonings,108 and electrical injuries.114 The general demographic of those presenting with injuries also changed during the pandemic compared with before the pandemic, with a significantly younger median age.111 113 115 Parents and other caregivers may have treated more minor injuries at home or, in some cases, may have avoided seeking medical attention due to the concern of contracting COVID-19 in hospital facilities. Physical distancing measures, including a ban on sports and children’s use of playgrounds during the COVID-19 pandemic lockdowns, are likely linked to the overall reduction in child injuries seen through emergency room admissions. At the same time, there may have been a shift in care-seeking behaviour, with parents and caregivers being more anxious about attending the hospital due to the risk to themselves and the child contracting COVID-19.
Discussion and conclusion
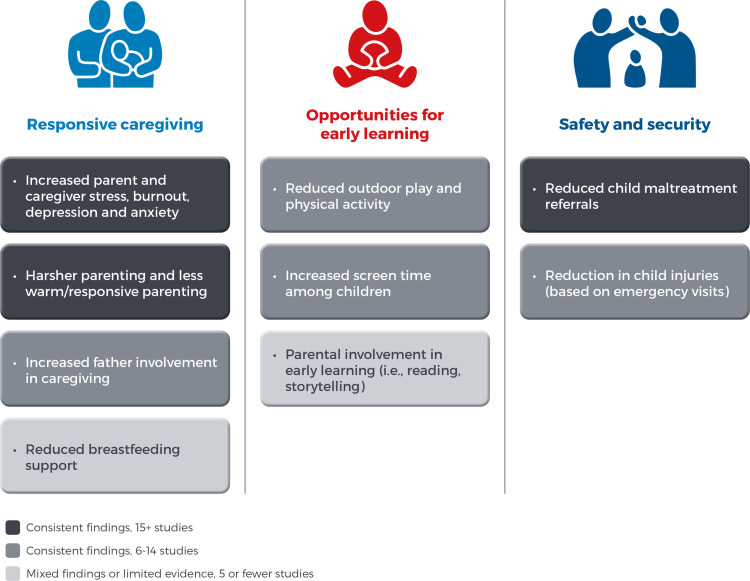
Emerging evidence from the COVID-19 pandemic, mainly drawn from parents and other caregivers’ surveys, shows striking similarities in how essential components of nurturing care—responsive caregiving, support for young children’s learning, and children’s safety and security—have been disrupted. As shown in figure 2, many studies were devoted to examining mental health during the early pandemic period and reveal issues of concern related to increases in parent and caregiver stress and mental health difficulties, which was linked to harsher and less warm or responsive parenting in some studies. Also, there was a relatively large number of studies (ie, more than 15) examined child protection during the pandemic and consistent results show a reduction in maltreatment referrals, suggesting that traditional mechanisms for responding to potential child neglect and maltreatment may not be as effective during school closures and large-scale physical distancing measures. Furthermore, there are consistent results across studies to suggest that fathers’ engagement in caregiving increased during the early phase of the pandemic, children’s outdoor play and physical activity decreased (while screen time increased), and emergency room visits for child injuries decreased. In contrast to the above, there were far more limited studies, and some inconsistent findings, related to opportunities for early learning and support for breast feeding.
Figure 2.
Key review findings on nurturing care during the COVID-19 pandemic.
The papers point towards at least four implications. First, there remains a substantial unmet need to expand and diversify research studies on social protection during health emergencies to ensure that families meet their essential income needs and food and housing security, which may reduce parenting stress and reduce the risk of harsh and non-responsive parenting. Second, improving studies on access to and use of mental health and psychosocial support services to reduce parenting stress and harsh parenting are needed. Third, evaluations of interventions to promote early learning and play, which are scalable and appropriate during physical distancing measures and movement restrictions, are needed. Lastly, more research is needed on child protection systems that can help educators and other mandated reporters to identify signs of child abuse and neglect specific during school closures.
A report of case studies of programme implementation to support nurturing care during COVID-19 illustrates several examples of how organisations in various contexts have adapted to support nurturing care efforts during COVID-19.117 For instance, programmes have organised emergency food delivery services for vulnerable families. Others have developed new training materials for frontline workers that integrate both mental health and nurturing care components. Gaps in the evidence base remain, with a lack of studies in low/middle-income countries and an urgent need for action-oriented implementation studies—those that go beyond identifying trends and begin to pinpoint ‘what works’ to effectively promote and protect nurturing care during health emergencies such as COVID-19.
Footnotes
Collaborators: The authors are grateful to the support and collaboration provided by Vanessa Cavallera, Bernadette Daelmans and Tarun Dua from the World Health Organization, Geneva, Switzerland.
Contributors: KP is responsible for the overall content as the guarantor and coordinated the review, screened citations and full-text articles, abstracted data, interpreted the results and wrote the manuscript. RL-W and RH screened citations and full-text articles, abstracted data and edited the manuscript. KH helped conceptualise the research, interpreted the results and edited the manuscript. CO coordinated the review, obtained the funding and edited the manuscript. All authors approved the final version to be published.
Funding: Lego Foundation funded this work (grant number 1226.001).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not applicable.
References
- 1.Cluver L, Lachman JM, Sherr L, et al. Parenting in a time of COVID-19. Lancet 2020;395:e64. 10.1016/S0140-6736(20)30736-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoshikawa H, Wuermli AJ, Britto PR, et al. Effects of the global coronavirus Disease-2019 pandemic on early childhood development: short- and long-term risks and mitigating program and policy actions. J Pediatr 2020;223:188–93. 10.1016/j.jpeds.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNICEF, World Bank, World Health Organization . Nurturing care for early childhood development a framework for helping children survive and thrive to transform health and human potential. Geneva: World Health Organization, 2018. https://www.who.int/maternal_child_adolescent/documents/nurturing-care-early-childhood-development/en [Google Scholar]
- 4.Chow MYK, Morrow AM, Booy R, et al. Impact of children's influenza-like illnesses on parental quality of life: a qualitative study. J Paediatr Child Health 2013;49:664–70. 10.1111/jpc.12261 [DOI] [PubMed] [Google Scholar]
- 5.Effler PV, Carcione D, Giele C, et al. Household responses to pandemic (H1N1) 2009-related school closures, Perth, Western Australia. Emerg Infect Dis 2010;16:205–11. 10.3201/eid1602.091372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sprang G, Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep 2013;7:105–10. 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- 7.Green E, Chase RM, Zayzay J, et al. The impact of the 2014 Ebola virus disease outbreak in Liberia on parent preferences for harsh discipline practices: a quasi-experimental, pre-post design. Glob Ment Health 2018;5:e1. 10.1017/gmh.2017.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kodish SR, Bio F, Oemcke R, et al. A qualitative study to understand how Ebola virus disease affected nutrition in Sierra Leone-A food value-chain framework for improving future response strategies. PLoS Negl Trop Dis 2019;13:e0007645. 10.1371/journal.pntd.0007645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plan Internationa . Ebola: beyond the health emergency. plan international, 2015. Available: https://plan-international.org/publications/ebola-beyond-health%C2%A0emergency
- 10.Adıbelli D, Sümen A. The effect of the coronavirus (COVID-19) pandemic on health-related quality of life in children. Child Youth Serv Rev 2020;119:105595. 10.1016/j.childyouth.2020.105595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asbury K, Fox L, Deniz E, et al. How is COVID-19 affecting the mental health of children with special educational needs and disabilities and their families? J Autism Dev Disord 2021;51:1772–80. 10.1007/s10803-020-04577-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asia-Pacific Regional Network for Early Childhood . Perspectives on the impact of COVID-19 on young children and early childhood development in the Asia-Pacific region, 2020. [Google Scholar]
- 13.Brown SM, Doom JR, Lechuga-Peña S, et al. Stress and parenting during the global COVID-19 pandemic. Child Abuse Negl 2020;110:104699. 10.1016/j.chiabu.2020.104699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cameron EE, Joyce KM, Delaquis CP, et al. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J Affect Disord 2020;276:765–74. 10.1016/j.jad.2020.07.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ceulemans M, Hompes T, Foulon V. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic: a call for action. Int J Gynaecol Obstet 2020;151:146–7. 10.1002/ijgo.13295 [DOI] [PubMed] [Google Scholar]
- 16.Chung G, Lanier P, Wong PYJ. Mediating effects of parental stress on harsh parenting and parent-child relationship during coronavirus (COVID-19) pandemic in Singapore. J Fam Violence 2020:1–12. 10.1007/s10896-020-00200-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davenport MH, Meyer S, Meah VL, et al. Moms are not OK: COVID-19 and maternal mental health. Front Glob Womens Health 2020;1:1. 10.3389/fgwh.2020.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dhiman S, Sahu PK, Reed WR, et al. Impact of COVID-19 outbreak on mental health and perceived strain among caregivers tending children with special needs. Res Dev Disabil 2020;107:103790. 10.1016/j.ridd.2020.103790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Giorgio E, Di Riso D, Mioni G, et al. The interplay between mothers' and children behavioral and psychological factors during COVID-19: an Italian study. Eur Child Adolesc Psychiatry 2021;30:1401–12. 10.1007/s00787-020-01631-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dib S, Rougeaux E, Vázquez-Vázquez A, et al. Maternal mental health and coping during the COVID-19 lockdown in the UK: data from the COVID-19 new Mum study. Int J Gynaecol Obstet 2020;151:407–14. 10.1002/ijgo.13397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dodd H, Westbrook J, Lawrence P. Co-SPYCE report one: findings from 1728 parents/carers of 2-4 year olds on stress, child activities, child worries and need for support. 10, 2020. [Google Scholar]
- 22.Evans S, Mikocka-Walus A, Klas A, et al. From “It Has Stopped Our Lives” to “Spending More Time Together Has Strengthened Bonds”: The Varied Experiences of Australian Families During COVID-19. Front Psychol 2020;11. 10.3389/fpsyg.2020.588667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farewell CV, Jewell J, Walls J, et al. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. J Prim Care Community Health 2020;11:2150132720944074. 10.1177/2150132720944074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gassman-Pines A, Ananat EO, Fitz-Henley J. COVID-19 and parent-child psychological well-being. Pediatrics 2020;146:e2020007294. 10.1542/peds.2020-007294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamadani JD, Hasan MI, Baldi AJ, et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health 2020;8:e1380–9. 10.1016/S2214-109X(20)30366-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hiraoka D, Tomoda A. Relationship between parenting stress and school closures due to the COVID-19 pandemic. Psychiatry Clin Neurosci 2020;74:497–8. 10.1111/pcn.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kalil A, Mayer S, Shah R. Impact of the COVID-19 crisis on family dynamics in Economically vulnerable households. University of Chicago: Harris School of Public Policy Studies, 2020. [Google Scholar]
- 28.Lee S, Ward K. Stress and parenting during the coronavirus pandemic. University of Michigan, 2020. [Google Scholar]
- 29.Limbers CA, McCollum C, Greenwood E. Physical activity moderates the association between parenting stress and quality of life in working mothers during the COVID-19 pandemic. Ment Health Phys Act 2020;19:100358. 10.1016/j.mhpa.2020.100358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marchetti D, Fontanesi L, Mazza C, et al. Parenting-Related exhaustion during the Italian COVID-19 Lockdown. J Pediatr Psychol 2020;45:1114–23. 10.1093/jpepsy/jsaa093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mazza C, Ricci E, Marchetti D, et al. How Personality Relates to Distress in Parents during the Covid-19 Lockdown: The Mediating Role of Child’s Emotional and Behavioral Difficulties and the Moderating Effect of Living with Other People. Int J Environ Res Public Health 2020;17:6236. 10.3390/ijerph17176236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McRae CS, Henderson AM, Low RS. Parents’ Distress and Poor Parenting during COVID-19: The Buffering Effects of Partner Support and Cooperative Coparenting, 2020. Available: https://psyarxiv.com/nxdsk/ [DOI] [PubMed]
- 33.Nolvi S, Karukivi M, Korja R. Parental depressive and anxiety symptoms as a response to the COVID-19 pandemic: a birth cohort follow-up study. PsyArXiv 2020. [Google Scholar]
- 34.Oskovi-Kaplan ZA, Buyuk GN, Ozgu-Erdinc AS, et al. The effect of COVID-19 pandemic and social restrictions on depression rates and maternal attachment in immediate postpartum women: a preliminary study. Psychiatr Q 2021;92:1–8. 10.1007/s11126-020-09843-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-Being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics 2020;146:e2020016824. 10.1542/peds.2020-016824 [DOI] [PubMed] [Google Scholar]
- 36.Peltz JS, Daks JS, Rogge RD. Mediators of the association between COVID-19-related stressors and parents’ psychological flexibility and inflexibility: The roles of perceived sleep quality and energy. J Contextual Behav Sci 2020;17:168–76. 10.1016/j.jcbs.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Romero E, López-Romero L, Domínguez-Álvarez B, et al. Testing the Effects of COVID-19 Confinement in Spanish Children: The Role of Parents’ Distress, Emotional Problems and Specific Parenting. Int J Environ Res Public Health 2020;17:6975. 10.3390/ijerph17196975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roos LE, Salisbury M, Penner-Goeke L. Supporting families to protect child health: parenting quality and household needs during the COVID-19 pandemic, 2020 [DOI] [PMC free article] [PubMed]
- 39.Russell BS, Hutchison M, Tambling R, et al. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent-child relationship. Child Psychiatry Hum Dev 2020;51:671–82. 10.1007/s10578-020-01037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spinelli M, Lionetti F, Pastore M. Parents’ Stress and Children’s Psychological Problems in Families Facing the COVID-19 Outbreak in Italy. Front Psychol 2020:11. 10.3389/fpsyg.2020.01713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Spinelli M, Lionetti F, Setti A, et al. Parenting stress during the COVID-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam Process 2021;60:639-653. 10.1111/famp.12601 [DOI] [PubMed] [Google Scholar]
- 42.Westrupp EM, Bennett C, Berkowitz T, et al. Child, parent, and family mental health and functioning in Australia during COVID-19: comparison to pre-pandemic data. Eur Child Adolesc Psychiatry 2021. 10.1007/s00787-021-01861-z. [Epub ahead of print: 21 Aug 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Willner P, Rose J, Stenfert Kroese B, Kroese BS, et al. Effect of the COVID-19 pandemic on the mental health of carers of people with intellectual disabilities. J Appl Res Intellect Disabil 2020;33:1523–33. 10.1111/jar.12811 [DOI] [PubMed] [Google Scholar]
- 44.Xu Y, Wu Q, Levkoff SE. Material hardship and parenting stress among grandparent kinship providers during the COVID-19 pandemic: The mediating role of grandparents’ mental health. Child Abuse Negl 2020. 10.1016/j.chiabu.2020.104700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zanardo V, Manghina V, Giliberti L, et al. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynaecol Obstet 2020;150:184–8. 10.1002/ijgo.13249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brandstetter S, Poulain T, Vogel M. The impact of the COVID-19 pandemic on families in Germany. medRxiv 2020. 10.1101/2020.10.05.20206805 [DOI] [Google Scholar]
- 47.Loperfido L, Burgess M. The hidden impact of COVID-10 on child Povery. London: Save the Children International, 2020. https://resourcecentre.savethechildren.net/node/18174/pdf/the_hidden_impact_of_covid-19_on_child_poverty.pdf [Google Scholar]
- 48.Ritz D, O’Hare G, Burgess M. The hidden impact of COVID-19 on child protection and wellbeing. London: Save the Children International, 2020. https://resourcecentre.savethechildren.net/node/18174/pdf/the_hidden_impact_of_covid-19_on_child_protection_and_wellbeing.pdf [Google Scholar]
- 49.Vision W. COVID-19 rapid impact assessment report, 2020. Available: https://www.wvi.org/sites/default/files/2020-07/Rapid%20Impact%20Assesment%20Report_Full%20Report.pdf
- 50.Chung G, Chan XW, Lanier P. Associations between Work-Family balance, parenting stress, and marital conflicts during COVID-19 pandemic in Singapore. Open Science Framework 2020. 10.31219/osf.io/nz9s8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Joyce KM, Cameron E, Slymka J. Changes in maternal substance use during the COVID-19 pandemic, 2020. Available: https://psyarxiv.com/htny8/ [PubMed]
- 52.Abdelrahman M, Al-Adwan D, Hasan Y. Impact of social distancing on the mental health of parents and children in Qatar. Int J Ment Health Addict 2021:1-12. 10.1007/s11469-021-00555-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chu KA, Schwartz C, Towner E, et al. Parenting under pressure: a mixed-methods investigation of the impact of COVID-19 on family life. J Affect Disord Rep 2021;5:100161. 10.1016/j.jadr.2021.100161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Günther-Bel C, Vilaregut A, Carratala E, et al. A Mixed-method study of individual, couple, and parental functioning during the State-regulated COVID-19 Lockdown in Spain. Fam Process 2020;59:1060–79. 10.1111/famp.12585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr 2021;17:e13088. 10.1111/mcn.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Das R. COVID-19 perinatal mental health and the digital pivot; 2020.
- 57.Saunders B, Hogg S. Babies in Lockdown: listening to parent to build back better, 2020. Available: https://parentinfantfoundation.org.uk/our-work/campaigning/babies-in-lockdown/#fullreport
- 58.Spatz DL, Froh EB. Birth and breastfeeding in the hospital setting during the COVID-19 pandemic. MCN Am J Matern Child Nurs 2021;46:30–5. 10.1097/NMC.0000000000000672 [DOI] [PubMed] [Google Scholar]
- 59.Vazquez-Vazquez A, Dib S, Rougeaux E, et al. The impact of the Covid-19 lockdown on the experiences and feeding practices of new mothers in the UK: preliminary data from the COVID-19 new Mum study. Appetite 2021;156:104985. 10.1016/j.appet.2020.104985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Andrew A, Cattan S, Dias MC. How are mothers and fathers balancing work and family under lockdown?”. Inst Fisc Stud 2020. [Google Scholar]
- 61.Carlson DL, Petts R, Pepin J. Changes in Parents’ Domestic Labor During the COVID-19 Pandemic. SocArXiv 2020. 10.31235/osf.io/jy8fn [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Craig L, Churchill B. Dual‐earner parent couples’ work and care during COVID‐19. Gend Work Organ 2020:1–14. 10.1111/gwao.12497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Del Boca D, Oggero N, Profeta P, et al. Women's and men's work, housework and childcare, before and during COVID-19. Rev Econ Househ 2020;18:1001-1017. 10.1007/s11150-020-09502-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Farré L, Fawaz Y, González L. How the covid-19 lockdown affected gender inequality in paid and unpaid work in Spain, 2020. Available: https://www.iza.org/publications/dp/13434/how-the-covid-19-lockdown-affected-gender-inequality-in-paid-and-unpaid-work-in-spain
- 65.Lyttelton T, Zang E, Musick K. Gender differences in Telecommuting and implications for inequality at home and work. SSRN Electronic Journal 2020. 10.2139/ssrn.3645561 [DOI] [Google Scholar]
- 66.Mangiavacchi L, Piccoli L, Pieroni L. Fathers Matter: Intra-Household Responsibilities and Children’s Wellbeing During the Covid-19 Lockdown in Italy. Econ Hum Biol 2020. 10.2139/ssrn.3660266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zamarro G, Prados MJ. Gender differences in couples’ division of childcare, work and mental health during COVID-19. Rev Econ Househ 2021;19:11–40. 10.1007/s11150-020-09534-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hjálmsdóttir A, Bjarnadóttir VS. "I have turned into a foreman here at home." Families and work-life balance in times of Covid-19 in a gender equality paradise. Gend Work Organ 2020. 10.1111/gwao.12552. [Epub ahead of print: 19 09 2020] (Published Online First: 19 September 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Heggeness ML. Estimating the immediate impact of the COVID-19 shock on parental attachment to the labor market and the double bind of mothers. Rev Econ Househ 2020;18:1053-1078. 10.1007/s11150-020-09514-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Manzo LKC, Minello A, Mothers MA. Mothers, childcare duties, and remote working under COVID-19 lockdown in Italy: cultivating communities of care. Dialogues Hum Geogr 2020;10:120–3. 10.1177/2043820620934268 [DOI] [Google Scholar]
- 71.Qian Y, Fuller S. COVID-19 and the gender employment gap among parents of young children. Canadian Public Policy 2020;46:S89–101. 10.3138/cpp.2020-077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Barnett S, Jung K, Nores M, National Institute for Early Education Research . Young Children’s Home Learning and Preschool Participation Experiences During the Pandemic: NIEER 2020 Preschool Learning Activities Survey: Technical Report and Selected Findings, 2020. Available: http://nieer.org/wp-content/uploads/2020/08/NIEER-Tech-Rpt-July-2020-Young-Children%E2%80%99s-Home-Learning-and-Preschool-Participation-Experiences-During-the-Pandemic-AUG-2020-1.pdf
- 73.Kim J, Araya M, Ejigu C. The implications of COVID-19 on early learning continuity in Ethiopia: perspectives of parents and caregivers. REAL Centre, University of Cambridge, 2020. [Google Scholar]
- 74.Dong C, Cao S, Li H. Young children's online learning during COVID-19 pandemic: Chinese parents' beliefs and attitudes. Child Youth Serv Rev 2020;118:105440. 10.1016/j.childyouth.2020.105440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Briggs DC. COVID-19: The Effect of Lockdown on Children’s Remote Learning Experience – Parents’ Perspective. JESBS 2020:42–52. 10.9734/jesbs/2020/v33i930257 [DOI] [Google Scholar]
- 76.Grover S, Goyal SK, Mehra A, et al. A survey of parents of children attending the online classes during the ongoing COVID-19 pandemic. Indian J Pediatr 2021;88:280. 10.1007/s12098-020-03523-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dayal HC, Tiko L. When are we going to have the real school? A case study of early childhood education and care teachers’ experiences surrounding education during the COVID-19 pandemic. Australasian Journal of Early Childhood 2020;45:336–47. 10.1177/1836939120966085 [DOI] [Google Scholar]
- 78.World Vision . Rapid assessment of the impact of COVID-19 on child wellbeing in Cambodia, 2020. Available: https://www.wvi.org/sites/default/files/2020-06/Rapid%20assessment%20Covid%2019%20report-02June20.pdf
- 79.Lee SJ, Ward KP, Chang OD, et al. Parenting activities and the transition to home-based education during the COVID-19 pandemic. Child Youth Serv Rev 2021;122:105585. 10.1016/j.childyouth.2020.105585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Drouin M, McDaniel BT, Pater J, et al. How parents and their children used social media and technology at the beginning of the COVID-19 pandemic and associations with anxiety. Cyberpsychol Behav Soc Netw 2020;23:727–36. 10.1089/cyber.2020.0284 [DOI] [PubMed] [Google Scholar]
- 81.Carroll N, Sadowski A, Laila A, et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients 2020;12. 10.3390/nu12082352. [Epub ahead of print: 07 Aug 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020;20:1351. 10.1186/s12889-020-09429-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Moore SA, Faulkner G, Rhodes RE, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act 2020;17:85. 10.1186/s12966-020-00987-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.de Lannoy L, Rhodes RE, Moore SA, et al. Regional differences in access to the outdoors and outdoor play of Canadian children and youth during the COVID-19 outbreak. Can J Public Health 2020;111:988–94. 10.17269/s41997-020-00412-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis 2020;63:531–2. 10.1016/j.pcad.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mitra R, Moore SA, Gillespie M, et al. Healthy movement behaviours in children and youth during the COVID-19 pandemic: exploring the role of the neighbourhood environment. Health Place 2020;65:102418. 10.1016/j.healthplace.2020.102418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Idoiaga Mondragon N, Berasategi Sancho N, Dosil Santamaria M, et al. Struggling to breathe: a qualitative study of children's wellbeing during lockdown in Spain. Psychol Health 2021;36:179–94. 10.1080/08870446.2020.1804570 [DOI] [PubMed] [Google Scholar]
- 88.Guerrero MD, Vanderloo LM, Rhodes RE, et al. Canadian children's and youth's adherence to the 24-h movement guidelines during the COVID-19 pandemic: a decision tree analysis. J Sport Health Sci 2020;9:313–21. 10.1016/j.jshs.2020.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barboza GE, Schiamberg LB, Pachl L. A spatiotemporal analysis of the impact of COVID-19 on child abuse and neglect in the city of Los Angeles, California. Child Abuse Negl 2021;116:104740. 10.1016/j.chiabu.2020.104740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bullinger LR, Carr JB, Packham A, UNICEF Innocenti library . COVID-19 and crime: effects of Stay-at-Home orders on domestic violence, 2020. Available: https://apackham.github.io/mywebsite/COVID_crime_webversion.pdf
- 91.Bullinger L, Boy A, Feely M. COVID-19 and alleged child maltreatment. Rochester, NY: Social Science Research Network, 2020. [Google Scholar]
- 92.Martins-Filho PR, Damascena NP, Lage RC, et al. Decrease in child abuse notifications during COVID-19 outbreak: a reason for worry or celebration? J Paediatr Child Health 2020;56:1980-1981. 10.1111/jpc.15213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Baron EJ, Goldstein EG, Wallace CT. Suffering in silence: how COVID-19 school closures inhibit the reporting of child maltreatment. J Public Econ 2020;190:104258. 10.1016/j.jpubeco.2020.104258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Garstang J, Debelle G, Anand I, et al. Effect of COVID-19 lockdown on child protection medical assessments: a retrospective observational study in Birmingham, UK. BMJ Open 2020;10:e042867. 10.1136/bmjopen-2020-042867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Whaling K, Sarkissian AD, Larez NA. Reduced child maltreatment prevention service case openings during COVID-19. in review, 2020. [Google Scholar]
- 96.Rapoport E, Reisert H, Schoeman E, et al. Reporting of child maltreatment during the SARS-CoV-2 pandemic in New York City from March to may 2020. Child Abuse Negl 2021;116:104719. 10.1016/j.chiabu.2020.104719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cabrera-Hernández F, Padilla-Romo M, University of Tennessee, Department of Economics . Hidden violence: how COVID-19 school closures reduced the reporting of child maltreatment, 2020. Available: https://ideas.repec.org/p/ten/wpaper/2020-02.html
- 98.Hansen AL. Child maltreatment reporting statistics during the Covid-19 pandemic: a Cursory analysis. Center for Health Law Policy and Bioethics Scholarship: UNICEF Innocenti Library:, 2020. https://digital.sandiego.edu/cgi/viewcontent.cgi?article=1080&context=law_chlb_research_scholarship [Google Scholar]
- 99.Toros K, Falch-Eriksen A. A child's right to protection during the COVID-19 crisis: an exploratory study of the child protective services of Estonia. Child Youth Serv Rev 2020;119:105568. 10.1016/j.childyouth.2020.105568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jentsch B, Schnock B. Child welfare in the midst of the coronavirus pandemic-Emerging evidence from Germany. Child Abuse Negl 2020;110:104716. 10.1016/j.chiabu.2020.104716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bhopal S, Buckland A, McCrone R, et al. Who has been missed? dramatic decrease in numbers of children seen for child protection assessments during the pandemic. Arch Dis Child 2021;106:e6. 10.1136/archdischild-2020-319783 [DOI] [PubMed] [Google Scholar]
- 102.Øverlien C. The COVID-19 pandemic and its impact on children in domestic violence refuges. Child Abuse Rev 2020:379–86. 10.1002/car.2650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tener D, Marmor A, Katz C, et al. How does COVID-19 impact intrafamilial child sexual abuse? comparison analysis of reports by practitioners in Israel and the US. Child Abuse Negl 2021;116:104779. 10.1016/j.chiabu.2020.104779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kovler ML, Ziegfeld S, Ryan LM, et al. Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the Covid-19 pandemic. Child Abuse Negl 2021;116:104756. 10.1016/j.chiabu.2020.104756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sidpra J, Abomeli D, Hameed B, et al. Rise in the incidence of abusive head trauma during the COVID-19 pandemic. Arch Dis Child 2021;106:e14. 10.1136/archdischild-2020-319872 [DOI] [PubMed] [Google Scholar]
- 106.Lawson M, Piel MH, Simon M. Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl 2020;110:104709. 10.1016/j.chiabu.2020.104709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? the epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop 2020;40:373–9. 10.1097/BPO.0000000000001600 [DOI] [PubMed] [Google Scholar]
- 108.Chaiyachati BH, Agawu A, Zorc JJ, et al. Trends in pediatric emergency department utilization after institution of coronavirus Disease-19 mandatory social distancing. J Pediatr 2020;226:274–7. 10.1016/j.jpeds.2020.07.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hamill JK, Sawyer MC. Reduction of childhood trauma during the COVID-19 level 4 lockdown in New Zealand. ANZ J Surg 2020;90:1242–3. 10.1111/ans.16108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nabian MH, Vosoughi F, Najafi F, et al. Epidemiological pattern of pediatric trauma in COVID-19 outbreak: data from a tertiary trauma center in Iran. Injury 2020;51:2811–5. 10.1016/j.injury.2020.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sugand K, Park C, Morgan C, et al. Impact of the COVID-19 pandemic on paediatric orthopaedic trauma workload in central London: a multi-centre longitudinal observational study over the “golden weeks”. Acta Orthop 2020;91:633–8. 10.1080/17453674.2020.1807092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Raitio A, Ahonen M, Jääskelä M, et al. Reduced number of pediatric orthopedic trauma requiring operative treatment during COVID-19 restrictions: a nationwide cohort study. Scand J Surg 2021;110:254-257. 10.1177/1457496920968014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Turgut A, Arlı H, Altundağ Ümit, et al. Effect of COVID-19 pandemic on the fracture demographics: data from a tertiary care hospital in turkey. Acta Orthop Traumatol Turc 2020;54:355–63. 10.5152/j.aott.2020.20209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Li H, Yu G, Duan H, et al. Changes in children's healthcare visits during coronavirus Disease-2019 pandemic in Hangzhou, China. J Pediatr 2020;224:146–9. 10.1016/j.jpeds.2020.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Verdoni F, Ricci M, Di grigoli C. Effect of the COVID-19 Outbreak on Pediatric Patients’ Admissions to the Emergency Department in an Italian Orthopedic Trauma Hub. Children 2021:1–8. doi:0.3390/children8080645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Williams FN, Chrisco L, Nizamani R, et al. COVID-19 related admissions to a regional burn center: the impact of shelter-in-place mandate. Burns Open 2020;4:158–9. 10.1016/j.burnso.2020.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hackett K, Proulx K, Alvarez A. Case studies of nurturing care initiatives during COVID-19 pandemic. Durham, NC: FHI360; 2021. https://www.fhi360.org/sites/default/files/media/documents/resource-lego-case-study-nurturing-care-report.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-050417supp001.pdf (107KB, pdf)
bmjopen-2021-050417supp002.pdf (585.5KB, pdf)
Data Availability Statement
Data are available upon reasonable request.