Abstract
Objectives
To support workforce deficits and rising demand for medicines, independent prescribing (IP) by nurses, pharmacists and allied health professionals is a key component of workforce transformation in UK healthcare. This systematic review of qualitative research studies used a thematic synthesis approach to explore stakeholders’ views on IP in primary care and identify barriers and facilitators influencing implementation.
Setting
UK primary/community care.
Participants
Inclusion criteria were UK qualitative studies of any design, published in the English language. Six electronic databases were searched between January 2010 and September 2021, supplemented by reference list searching. Papers were screened, selected and quality-appraised using the Quality Assessment Tool for Studies with Diverse Designs. Study data were extracted to a bespoke table and two reviewers used NVivo software to code study findings. An inductive thematic synthesis was undertaken to identify descriptive themes and interpret these into higher order analytical themes. The Diffusion of Innovations and Consolidated Framework for Implementation Research were guiding theoretical anchors.
Primary and secondary outcome measures
N/A.
Results
Twenty-three articles addressing nurse, pharmacist and physiotherapist IP were included. Synthesis identified barriers and facilitators in four key stages of implementation: (1) ‘Preparation’, (2) ‘Training’, (3) ‘Transition’ and 4) ‘Sustainment’. Enhancement, substitution and role-specific implementation models reflected three main ways that the IP role was used in primary care.
Conclusions
In order to address global deficits, there is increasing need to optimise use of IP capability. Although the number of independent prescribers continues to grow, numerous barriers to implementation persist. A more coordinated and targeted approach is key to overcoming barriers identified in the four stages of implementation and would help ensure that IP is recognised as an effective approach to help alleviate workforce shortfalls in the UK, and around the world.
PROSPERO registration number
CRD42019124400.
Keywords: PRIMARY CARE, Health policy, Organisational development
Strengths and limitations of this study.
Adopting a qualitative synthesis facilitated contextual understanding into the implementation of non-medical independent prescribing (IP) in primary care settings in the UK.
Higher order analytical themes were identified that offer in-depth interpretation of non-medical IP implementation in UK primary care.
The theoretical lens improved understanding of the generalisability of factors known to facilitate non-medical IP in UK primary care.
Grey literature was excluded from the synthesis.
Introduction
Equitable access to primary care improves health outcomes, lowers costs and enhances patient experience.1 2 Global workforce deficits3–5 and the rising prevalence of long-term conditions,6 7 multimorbidity8–10 and COVID-1911 have severely threatened primary care sustainability.12–15 Medicines use in global priorities including diabetes and cardiovascular diseases is increasing, with worldwide drug therapy days rising in 2019 to 1.8 trillion and an average of 234 days per person/year.16 With one in four adults in UK primary care taking five or more medicines daily,17 the workforce implications for meeting prescribing needs are profound.
Mobilising primary care to improve workforce and service sustainability is a global challenge.5 18 As in other countries,19 20 primary care in the four devolved UK nations (ie, England, Scotland, Wales and Northern Ireland) has undergone significant restructuring and reorganisation.21–24 In England, for example, the 2019 National Health Service (NHS) long-term plan amalgamated general practitioner (GP) practices into primary care networks (PCN), covering populations of 30 000–50 000.25 Pooling resources to achieve government targets26 with the promise of extra non-medical staff (eg, advanced/specialist clinical pharmacists, dieticians, paramedics and physiotherapists), PCNs were expected to offer additional hours within broader service options.27 While the impact of the new 2021/2022 Health and Care Bill on primary care workforce transformation in England remains uncertain,28 the diverse skills of the non-medical advanced practice workforce including prescribing capability are likely to remain important for addressing UK primary care prescribing and medicines optimisation needs.29–31
In line with global movements to enhance the skills of non-medical healthcare professionals, over 90 000 UK nurses, pharmacists, optometrists, radiographers, physiotherapists, podiatrists, dieticians and paramedics32 under serial legislative changes33–36 and with accredited additional training37–39 are authorised to prescribe using supplementary and/or independent forms. Although UK legislation restricts dieticians and diagnostic radiographers to supplementary prescribing, as reported by professions with dual supplementary/independent prescribing (IP) rights (eg, nurses, pharmacists, physiotherapists, podiatrists) IP is more workable40 41 and has largely superseded supplementary prescribing in many UK non-doctor led primary and community care services.42–44 Enabling the autonomous initial assessment and ongoing management of patient prescribing and medicines optimisation needs, IP increases practitioner autonomy/expertise,29 45–47 enhances clinical outcomes compared with doctor-led care29 and results in high service-user satisfaction.48 Across contemporary primary care settings in the UK and internationally IP is an increasingly essential component of service re-design.45 49–54
Despite its many benefits, the UK adoption rates for IP vary,55 56 with medical opposition to prescribing roles,57 58 training course drop-out,46 delayed prescribing onset59 60 and role underuse reported.61–64 Difficulties with implementation are frequently cited.43 46 59 65–67 Several UK68 69 and international systematic54 70–72 and literature reviews,73 74 have focused on implementation barriers and/or facilitators. However, these have been profession-specific,54 70–72 74 have included international models with varying legislative/jurisdictional levels of prescribing autonomy54 70–72 and/or have addressed prescribing in heterogenous care settings.54 68 69 74 None have synthesised qualitative studies in all IP eligible professions in UK primary care. Considering IP enhances workforce skills and builds capacity for service redesign and improved sustainability,42 75–77 identifying and understanding the challenges to its implementation is ever pressing.78 79
Aim
This qualitative meta-synthesis aimed to identify barriers and facilitators that influence implementation of IP in UK primary care.
Theoretical perspective
This review is broadly informed by the Diffusion of Innovations theory80 81 and the Consolidated Framework for Implementation Research82 83 which provided theoretical anchors for identifying contextual factors likely to influence implementation.84–89
Methods
This qualitative meta-synthesis is reported following the Enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) guidelines90 which incorporates elements of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.91 Thematic qualitative meta-synthesis92 93 permits synthesis of context-embodied research and is a suitable method for identifying factors influencing implementation.94–96 The review was registered in PROSPERO.97
Search strategy
A systematic search of UK literature on primary and community care IP was undertaken in January 2021 and updated in September 2021. Barriers/facilitators to healthcare innovations are conceptually well established98–102 and thus grey literature was excluded. Search terms were developed according to the Sample, Phenomenon of Interest, Design, Evaluation, Research Type (SPIDER) tool103 and tested based on truncations of words related to prescribing, community/primary care and UK non-medical healthcare professions with IP authority (eg, nurses, pharmacists, optometrists, physiotherapists, podiatrists, paramedics and radiographers). Wild card and Boolean Search Operators were used. Qualitative search terms were not included104 105; all citations were screened for qualitative methodology. Search strings (see online supplemental file 1 examples) were adapted for six electronic databases (EBSCO - MEDLINE, CINAHL, OVID – Embase, ProQuest - British Nursing Index, Nursing & Allied Health, Web of Science). The 2010 inception search date reflected major UK coalition governmental change and the introduction of landmark legislative reforms106–109 that decentralised UK primary/community care commissioning.110 Inclusion criteria applied to study selection are shown in table 1. Retrieved citations were downloaded to EndNote V.X9 and duplicates removed.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|
|
|
|
|
|
|
|
|
|
|
|
|
IP, independent prescribing.
bmjopen-2021-052227supp001.pdf (33.7KB, pdf)
Screening and eligibility
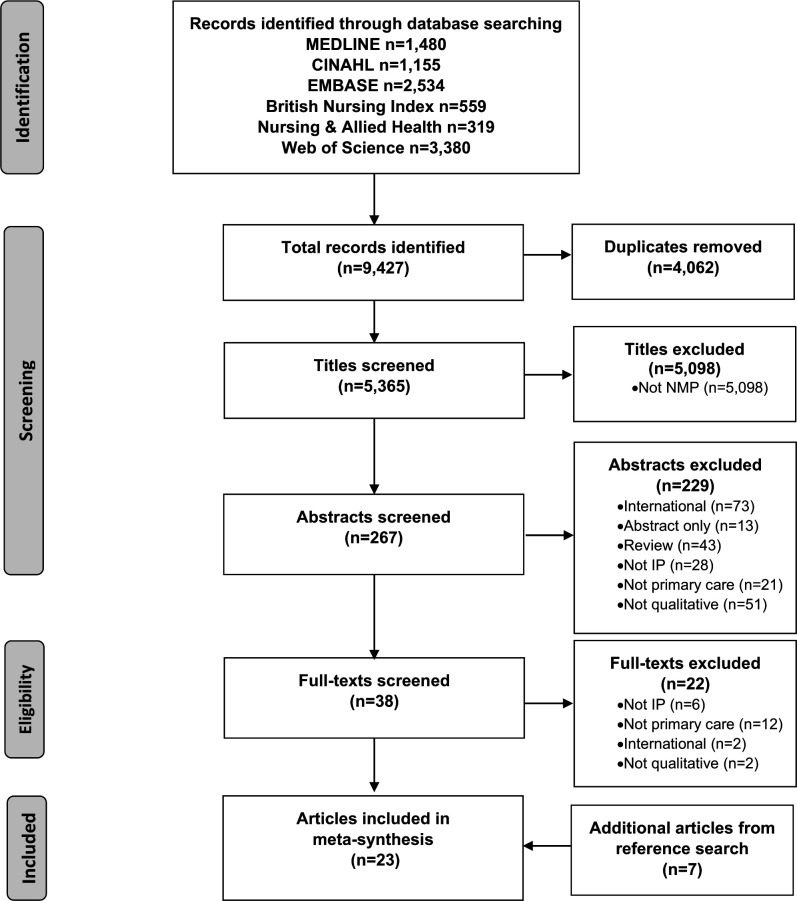
Two reviewers (JE and NC) independently assessed all titles and abstracts against the inclusion criteria and the full-text versions of papers deemed potentially relevant were obtained and reviewed. Papers found not to meet the criteria during screening were excluded with reasons recorded as shown in the PRISMA table (figure 1). Reference list hand searching supplemented database searching.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses depicting study selection, screening, eligibility for inclusion and synthesis (adapted from Page et al).91 IP, independent prescribing; NMP, non-medical prescribing.
Quality assessment
In keeping with the scope of a qualitative meta-synthesis,111 112 studies were not excluded on the basis of quality assessment.92 113 Methodological appraisal of individual papers was undertaken using the Quality Assessment Tool for Studies with Diverse Designs (QATSDD),114 which has demonstrated validity and test–retest reliability for assessing the reporting and methodological transparency of diverse study designs.115 The tool uses a 4-point scoring system for assessment of qualitative studies (14 questions) and mixed methods studies (16 questions), resulting in total possible scores of 42 and 48, respectively.114 Scoring was undertaken by one reviewer (JE) and any uncertainties were discussed and resolved with a second reviewer (NC). Online supplemental file 2 provides a detailed breakdown of questions and the grading of study manuscripts.
bmjopen-2021-052227supp002.pdf (41.4KB, pdf)
Data extraction
Study data were extracted by one author (JE) to a bespoke table adapted from recommended templates.116 This collated contextual and methodological information, data on barriers and/or facilitators and main findings and was piloted on five index studies to ensure consistency and usability. Data extraction was recursive and involved repeated review/update between ensuing analysis stages.117
Data analysis and synthesis
The aim of thematic analysis was to develop a coherent synthesis of barriers and facilitators that influenced IP across stages of the implementation continuum.118–120 Data analysis followed a four stage, iterative process described by Thomas and Harden121 (table 2). Qualitative ‘data’ referred to participant quotations, (sub)themes, explanations, hypotheses or new theory, observational excerpts and author interpretations.122 Barriers were defined as ‘any obstacle (material or immaterial) impeding adoption, implementation and/or sustainability of IP’123 124 and facilitators were defined as ‘any obstacle (material or immaterial) enhancing adoption, implementation and/or sustainability of IP’.123 124
Table 2.
Stages of analysis
| Stage 1 | In-depth reading and familiarisation with individual papers, data extraction. |
| Stage 2 | Inductive line-by-line coding of highest quality, index papers (n=5) to develop a set of ‘open codes’ by two independent reviewers (JE and NC). |
| Stage 3 | Codes discussed/agreed, grouped into descriptive themes using NVivo189; codebook applied to all papers, and expanded/modified by identifying new codes/themes and/or merging/renaming existing codes/themes.190 |
| Stage 4 | Descriptive themes organised into higher order analytical themes and matrix charted with corresponding indicative quotes. |
Rigour within the analytical process
To ensure analytical rigour, two independent reviewers (JE and NC) initially performed inductive line-by-line data coding from five highest quality index papers (stage 2). Each reviewer produced sets of open data codes which were compared and discussed. If different codes and/or different interpretations were assigned to a concept, these were discussed and revised. Disagreements were resolved by a third reviewer (MC). Data codes were subsequently grouped into descriptive themes, creating a codebook for application to all papers (stage 3). To identify possible contradictory cases and clarify thematic commonalities within studies,125 a matrix of participant quotes was charted to constituent themes (see online supplemental file 3).126
bmjopen-2021-052227supp003.pdf (151.6KB, pdf)
Patient and public involvement
The review was conducted as part of a PhD exploring paramedic IP in UK primary care, for which a University service user/carers group was instrumental in informing study design and methods. However, as the systematic review focused on implementation challenges and not patient-related outcomes, the group was not involved in design or conduct.
Results
Out of 5365 original articles identified 23 met inclusion criteria127–150 (see figure 1, PRISMA table).
Study characteristics and quality assessment
Table 3 summaries the study characteristics and quality assessment scores of included articles. Studies were undertaken in England,129 132 133 136 138 140 141 143 146–150 Scotland127 128 130 139 or across devolved UK nations.131 134 135 142 144 The representation of independent prescribers from Wales131 134 and Northern Ireland142 144 was limited. Sixteen studies used qualitative methods,127 130 131 133 135–140 144–150 six used mixed methods128 129 132 134 141 142 and one employed a qualitative survey.143
Table 3.
Characteristics of included studies (n=23) and key barriers and facilitators
| Author(s), year | Country, setting | Study focus, participants | Barriers | Facilitators | QATSDD score |
| Afseth and Paterson (2017)127 | Scotland. HEI. | Views on prescribing training. 6 NIP trainees, 6 DMPs. |
1, 2, 3 | 4, 5, 6, 7, 8 | 67% |
| Boreham et al (2013)128 | Scotland. | Views on prescribing training. 87 NIP trainees, 10 HEI leads. |
1, 2, 3, 8, 9 | 4, 5, 9, 10, 11 | 67% |
| Bowskill et al (2014)129 | England. HEI. | Views on prescribing training 6 IP trainees, 3 IPs (unspecified professions). |
1, 3, 9 | 12 | 60% |
| Brodie et al (2014)130 | Scotland. Gen-P, Comm. | Views on prescribing role. 4 NIPs, 4 PIPs. |
8, 13, 14, 15, 16, 17, 18, 19 | 9, 10, 20, 21, 22, 23, 24 | 38% |
| Carter et al (2021)131 | England, Scotland, Wales. Gen-P, Comm pharmacy. | Factors influencing prescribing and role of practice pharmacists on evidence based prescribing. 6 GPs, 6 NIPs, 6 PIPs, 12 key informants. |
25, 26, 27 | 9, 11, 24, 28, 29, 30, 31, 32, 61 | 78% |
| Cole and Gillett (2015)132 | England. Comm pall care. | Prescribing practices. 6 NIPs. |
2, 3, 15, 26, 27, 33, 34, 35, 36, 37, 38 | 21, 28, 30, 37, 61 | 29% |
| Courtenay et al (2010)133 | England. Gen-P, Comm clinics. | Patient experiences/views of nurse prescribing. 41 patients. |
10, 11, 22, 39 | 50% | |
| Courtenay et al (2017)134 | England, Scotland, Wales. Gen-P, Comm clinics. | Patient experiences/views of nurse and pharmacist antibiotic prescribing for respiratory tract infection. 16 NIPs, 1 PIP, 22 patients. |
27 | 22, 23, 39, 40, 41 | 67% |
| Courtenay et al (2019)135 | UK (unspecified countries). Gene-P, OOH, IC. | Factors influencing antibiotic prescribing for respiratory tract infection. 17 NIPs, 4 PIPs. |
18, 27, 38, 42, 43 | 6, 10, 11, 22, 23, 24, 28, 29, 32, 39, 40, 41, 44, 57 | 78% |
| Cousins and Donnell (2012)136 | England. Gen-P. | Views on prescribing role. 6 NIPs. |
3, 16, 18, 27, 34, 35, 37, 42, 45 | 6, 9, 10, 20, 24, 28, 61 | 59% |
| Daughtry and Hayter (2010)137 | England. Gen-P. | Experiences of prescribing role. 8 practice NIPs. |
3, 6, 18, 27, 29, 35, 62 | 5, 8, 9, 10, 11, 24, 28, 29, 30, 44, 46, 47, 57, 61 | 36% |
| Dhalivaal et al (2011)138 | England. Gen-P. | Patient views on nurse prescribing. 15 patients. |
22, 39 | 43% | |
| Downer and Shepherd (2010)139 | Scotland. Comm. | Views on prescribing role. 8 district NIPs. |
3, 15, 17, 18, 35, 37, 38, 45, 48, 49, 62 | 3, 9, 10, 30, 44, 57, 61 | 48% |
| Herklots et al (2015)140 | England. Comm. | Experiences of prescribing. 7 community matron IPs. |
3, 15, 16, 18, 35, 38, 48, 49, 62 | 6, 7, 10, 11, 12, 22, 29, 47, 57, 61 | 43% |
| Holden et al (2019)141 | England. | Medicines optimisation practices. 20 physio non-IPs, 1 physio-IP. |
3, 13, 36, 42, 45, 50, 51 | 10, 21 | 75% |
| Inch et al (2019)142 | England, Scotland, Northern Ireland. Elderly residential care. |
Feasibility of implementation. 2 P non-IPs, 4 PIPs, 6 GPs, 16 care home staff, 2 patients, 3 relatives, 1 dietician non-IP. |
3, 49 | 10, 21, 22, 23, 52 | 54% |
| Kelly et al (2010)143 | England. Gen-P. | Barriers to adoption of IP. 31 practice NIPs, 120 N non-IPs. |
1, 2, 3, 9, 13, 35, 36, 42, 45, 50, 51, 53, 54, 55 | 33% | |
| Lane et al (2020)144 | England, Scotland, Northern Ireland. Elderly residential care |
Barriers and facilitators to prescribing. 27 P non-IPs, 29 GPs, 12 care home staff, 7 patients, 7 relatives. |
3, 35, 43, 48, 49 | 6, 7, 8, 10, 11, 21, 22, 39, 46, 52, 56 | 78% |
| Latham and Nyatanga (2018a, b)145 146 | England. Comm pall care. | Views on prescribing role. 6 NIPs. |
3, 15, 18, 27, 35, 36, 38, 49, 50, 60 | 7, 8, 10, 11, 12, 20, 21, 22, 30, 44, 52, 57, 61 | 71% |
| Maddox et al (2016)147 | England. Gen-P, Comm, Nursing homes, Comm pharmacy. | Barriers and facilitators to prescribing. 25 NIPs, 5 PIPs. |
3, 15, 16, 26, 27, 29, 35, 37, 42, 48, 62 | 6, 7, 10, 12, 24, 29, 30, 42, 47, 57, 61 | 71% |
| Stenner et al (2011)148 | England. Gen-P, Comm clinics. | Patient views on nurse prescribing. 41 patients. |
11, 22, 23, 29, 39 | 55% | |
| Weiss et al (2016)149 | England. Gen-P. | Views on prescribing role. 7 NIPs, 7 PIPs, 7 GPs. |
3, 6, 17, 25, 35, 45, 49, 51, 56, 58, 59, 63 | 3, 6, 8, 11, 12, 22, 24, 29, 39, 44, 46, 47, 63 | 52% |
| Williams et al (2018)150 | England. OOH/unscheduled care. |
Factors influencing nurse and GP antibiotic prescribing for respiratory tract infection. 15 NIPs, 15 GPs. |
15, 16, 18, 26, 27, 34, 49, 59 | 6, 12, 22, 23, 24, 28, 32, 41 | 76% |
Barriers: 1=Lack of backfill/protected/study time, 2=Lack of DMP role clarity/supervision/availability, 3=Lack of medical/managerial support/leadership, 14=Lack of national IP incentives/policy initiatives, 15=Lack of clinical record/IT access, 16=Lack of CPD/supervision, 17=IP role isolation, 18=Time/workload constraints, 19=Lack of IP strategy, 25=Lack of interprofessional collaboration/communication networks, 26=Unclear/absent clinical protocols/guidelines, 27=Inappropriate patient/team pressure for prescribing, 33=Lack of local policies for IP, 34=Lack of governance/accountability structures, 35=Lack of team understanding of IP, 36=Lack of clinical/service advantage of IP, 37=Lack of peer support/mentoring, 38=Lack of prescribing confidence/competence, 42=Fear of responsibility/accountability/error, 43=Lack of practitioner specialist skills, 45=Lack of professional/personal adoption incentive, 48=Poor/absent physician relationships, 49=Lack of IP role clarity, 50=Expedient medicines pathways, 51=Prescribing considered outside professional practice scope, 53=Lack of course information, 54=Inconsistent selection policies, 55=Lack of workforce planning, 58=Formulary restrictions, 59=Lack of service user acceptance, 60=Delayed registration post qualification, 62=Lack of medical supervision, 63=Employment model.
Facilitators: 4=DMP role clarity/good DMP supervision, 5=Interprofessional training model, 6=IP role clarity, 7=Established physician relationships, 8=Medical/managerial support/leadership, 9=Professional/personal adoption incentive, 10=Clinical/service advantage of IP, 11=Interprofessional collaboration/communication networks, 12=Peer support/mentoring, 13=Lack of course funding, 20=Prescribing integral to advanced practice, 21=Identified service pathways gaps, 22=Practitioner specialist skills, 23=Consultation time, 24=CPD/supervision, 28=Clinical/professional protocols/guidelines, 29=Prescribing confidence/competence, 30=Exposure to prescribing opportunity, 31=Adequate formulary, 32=National incentives/policy initiatives for prescribing, 39=Service user acceptance of IP, 40=Governance/accountability structures, 41=Audit/feedback on prescribing practice, 44=Good interprofessional relationships, 46=Stakeholder consultation, 47=Team understanding of IP, 52=Clinical record/IT access, 56=Employment model, 57=Medical supervision, 61=Delineated scope of prescribing competence.
Comm, community; CPD, continued professional development; DMPs, designated medical practitioners; Gen-P, general practice; GPs, general practitioners; HEI, higher educational institute; IC, integrated care; IP, independent prescribing; IT, information technology; NIP, nurse IP; N non-IPs, nurse non-IPs; OOH, out of hours; pall, palliative; physio-IP, physiotherapist IP; physio non-IPs, physiotherapist non-IP; PIPs, pharmacist IP; QATSDD, Quality Assessment Tool for Studies with Diverse Designs.
Fifteen studies addressed nurse IP,127–129 132–134 136–140 143 146 148 150 seven included pharmacists130 131 135 142 144 147 149 and one study focused on physiotherapists.141 Where indicated, studies were conducted pre-2011,128 129 133 137–139 143 147–149 between 2011–2015127 130 132 134 145 146 150 or between 2016–2019.131 135 142 144
All studies reported results from primary care IP implementation; in general practice,136–138 143 community domiciliary/residential care132 139 140 142 144 146 150 or mixed general practice/community settings.127–131 133–135 141 147 148 Participants included nurse/pharmacist prescribers,130 132 134–137 139 140 146 147 149 150 nurse/physiotherapist non-prescribers,141 143 nurse non-medical prescriber trainees and educational staff,127–129 service-users133 134 138 148 and multidisciplinary team members.142 144 149 150 Studies explored training,127–129 IP roles,130 136 137 139 146 149 patient acceptance,133 138 148 prescribing/medicines optimisation practices,131 132 134 140 141 150 implementation feasibility142 and barriers and/or facilitators.135 143 144 147
The methodological quality of included studies (see table 3 summary) was average, with a QATSDD mean score 25 (range 13–36), mainly due to seven low scoring studies.130 132 137–140 143 Common methodological weaknesses were: lack of explicit theoretical framework,130 132 137 138 140 143 limited/absent rationale for choice of analytical methods130 132 137–140 143 and lack of reliability assessment for analytical processes.130 132 137–140 143 Methodological strengths of higher scoring studies were: statement of aims/objectives in main body of report,128 131 134 135 141 145 150 description of data collection procedures128 131 135 141 144 145 147 and fit between research question and method of analysis.128 134 135 141 144 145 147 150 Notably studies providing richer contextual descriptions,131 135 144 146 147 150 and/or using implementation theory135 144 explored barriers and/or facilitators in greater depth.
Identification of barriers and facilitators and key stages of implementation
Implementation of IP in primary care was found to be complex and influenced by a myriad of organisational service, team and individual stakeholder level barriers and facilitators. Informed by descriptive/data themes, these fell into four major analytical themes, each of which is presented as a key stage in the implementation process as follows:
Analytical theme 1: Preparation—organisational readiness for implementation
Analytical theme 2: Training—optimising practitioner readiness for IP
Analytical theme 3: Transition—ensuring early prescribing support
Analytical theme 4: Sustainment—maximising and developing IP.
Table 4 provides an overview of analytical themes, associated descriptive/data themes and summative findings. Examples of indicative quotations making up these themes are presented in online supplemental file 3. Factors presented within themes acted as barriers and/or facilitators to implementation, for example, poor managerial support was a barrier, while proactive managerial support and leadership facilitated implementation. It is acknowledged that barriers and facilitators overlap some themes and in some cases are interdependent. For example, lack of mentoring relationships with doctors limited opportunity for informal support, which in turn prevented prescribing competence development and risked loss of prescriber confidence.140 147 Therefore, to avoid duplication of findings, barriers and facilitators are presented within the themes deemed most appropriate, yet their presence and influence is acknowledged elsewhere. Given that the majority of data were derived from studies conducted in England or mixed geographical settings, it was not possible to deduce differences in barriers and facilitators across the devolved UK nations.
Table 4.
Analytical themes and subthemes from included studies, with summative findings
| Analytical theme | Descriptive theme | Data theme | Summative findings |
| Analytical theme 1: Preparation—organisational readiness for implementation | Theme 1.1: Clarifying need and advantage of independent prescribing | Clarifying clinical/service need for independent prescribing |
|
| Establishing service pathway gaps | |||
| Role clarity | |||
| Theme 1.2: Managerial leadership and support | Role of managers | ||
| Recognising value | |||
| Culture | |||
| Theme 1.3: Interprofessional environment | Inter-professional relationships | ||
| Communication & collaboration | |||
| Analytical theme 2: Training—optimising practitioner readiness for independent prescribing | Theme 2.1: Selecting the right practitioners | Selection |
|
| Skills and aptitudes | |||
| Motivation and commitment | |||
| Theme 2.2: Preparing and supporting practitioners during training | Expectations of training |
|
|
| Study leave | |||
| Designated Medical Practitioners | |||
| Analytical theme 3: Transition—ensuring early prescribing support |
Theme 3.1: Transition as a point of vulnerability | Self-confidence |
|
| Theme 3.2: Nurturing confidence and competence | Minimum competence | ||
| Experience and exposure | |||
| Theme 3.3: Transition support needs | Informal and formal support systems | ||
| Analytical theme 4: Sustainment—maximising and developing independent prescribing | Theme 4.1: Service delivery | Impact on workload |
|
| Theme 4.2: Supporting role development | Role/service expansion | ||
| Continued professional development | |||
| Evaluation and reflection |
CPD, continued professional development; DMPs, designated medical practitioners; GPs, general practitioners; IP, independent prescribing; NMP, non-medical prescribing.
Analytical theme 1: preparation—organisational readiness for implementation
This analytical theme refers to barriers and facilitators influential to the planning phase of implementation which related to the service need and relative advantage of implementing IP, the need for consistent managerial leadership and an interprofessional environment that was conducive to team implementation.
Descriptive theme 1.1: clarifying need and advantage of implementing independent prescribing
Identifying shortfalls in existing medicines pathways and how IP could fill service gaps were key steps in this stage. Studies described a highly qualified, specialist nursing and pharmacy workforce delivering unscheduled, scheduled and out-of-hours services130 132–137 139 140 142 144 146 148–150 who routinely made autonomous clinical decisions necessitating prescribing and medicines optimisation skills.127 133–135 140 146 148 150 IP held tangible advantage over former methods of accessing prescribed medicines which involved request, referral and/or the counter-signing of prescriptions by doctors. Subject to GP workload132 142 144 and constrained availability,140 142 144 146 these methods were labour intensive,140–142 144 146 inefficient136 140 141 146 and burdened services and patients through the need for additional healthcare contacts.133 137 139 141 142 146 148 By removing the need for doctor input, IP improved responsiveness with respect to medicines,133 135 139 140 142 144 146 148 enhanced care quality130 142 146 and helped prevent adverse outcomes.140
Lack of team clarity and transparency on IP role intentions were persistent barriers to implementation.137 139 140 142 144 146 147 149 Poor team understanding of IP could limit integration,149 and promote role ambiguity149 or misuse.130 136 140 147 Consultative team stakeholder processes facilitated clarification of current medicines pathways bottle necks,144 helped cement clinical advantage of IP144 and encouraged a collective understanding of implementation.142 144 149 Conversely, if existing medicines pathways were perceived to be expedient and IP held limited advantage, adoption was less likely.141 143
Descriptive theme 1.2: managerial leadership and support
Lack of managerial leadership and support were highly cited barriers to implementation that persisted across the review decade. Nurse/pharmacist prescribers reported stage specific and ongoing funding,128 141 143 training129 130 132 136 137 139 140 147 and infrastructural needs130 132 139 140 146 147 that extended across the IP implementation trajectory. Managerial support was, however, frequently reported to diminish post-adoption128–130 132 136 137 139–141 143 146 147 and many practitioners believed managers lacked knowledge about IP130 136 137 141 143 or misunderstood its potential for improving service quality.130 143 Nurses/pharmacists ascribed high value to IP for improving service efficiency135 136 139 140 146 147 and skill utilisation,130 132 136 140 perceiving it extended clinical knowledge beyond prescribing,130 132 140 146 enhanced clinical confidence130 137 139 140 146 and job satisfaction,136 139 146 and facilitated team education.130 142 149 They perceived themselves a unique workforce resource with potential for better mobilisation in under-resourced areas (eg, mental health).130 However, there was a perception that management lacked appreciation of primary care workforce aspirations for IP143 and overlooked its scope.130 141 143 Better recognition and commitment were considered essential for leveraging and driving IP services forward.130
Ensuring teams understood IP and its role within care delivery mitigated subsequent barriers136 137 140 149 and was critical for implementation success.137 139 140 142 144 146 147 149 Doctors, receptionists,136 137 149 dispensing pharmacists146 149 and peer colleagues139 146 147 149 all played supervisory and/or infrastructural roles in IP implementation and understanding the need for this input was essential. While staff clarity on their roles in relation to IP positively influenced willingness to provide enabling supports such as clinical administration,136 149 record access144 and clinical supervision/pharmaceutical advice140 146 lack of team understanding of IP was a barrier that was cited repeatedly across the review decade.132 136 137 139 140 143 144 146 147 149
Descriptive theme 1.3: Interprofessional environment
Respectful, trusting interprofessional relationships promoted an appreciation of different professional skill sets,149 helped ratify the purpose of IP127 149 and built team confidence in the prescribing competence of nurses and pharmacists.127 140 Good relationships facilitated information transfer,140 promoted supervision provision,147 149 shared learning127 and team working.149 Acceptance and positive attitudes towards IP as a shared skill were facilitative to implementation142 144 149 and mitigated the likelihood of ‘turf wars’ emerging if IP roles was perceived to encroach on professional territories.149 While many nurses/pharmacists reported positive relationships with doctors,137 139 140 146 149 others described jurisdictional tensions over prescribing authority.137 143 149 Building trust for IP where relationships were weak took time,142 and given the important supervisory role of doctors in IP,130 132 136 139 140 146 147 consideration of their strength in adoption planning is pertinent. Good communication networks were more likely where established relationships and positive attitudes towards IP prevailed,140 149 and were important for imparting information to teams about IP,136 142 144 for developing supervision and peer support140 146 and promoting teamwork.144 149
Analytical theme 2: training—optimising practitioner readiness for independent prescribing
This analytical theme refers to the extent to which organisations select and prepare the right practitioners for IP training, as well as how they support and maximise students’ learning experiences.
Descriptive theme 2.1: selecting the right practitioners
Overall, strategic planning for IP workforce selection lacked scrutiny, and practitioner choice,128 130 136 expectation of improved job satisfaction,136 143 146 efficiency and patient benefit128 136 were the primary drivers for implementation across the review period. Training course drop out128 and failure to prescribe following training,130 132 suggest a need to ensure selection procedures match skills and capabilities to IP and increase the chances of organisational return on IP training investment. Synthesis identified essential skills130 133 135 136 138 146 148 150 and personal motivation128 130 as important considerations. Study demographic data indicated a clinically experienced workforce,130 136 137 146 147 with degree/higher degree educational and/or specialist skills attainment.128 133 140 148 Advanced physical assessment and clinical specialty skills not only suggested expertise and theoretical knowledge to underpin IP but were also recognised by patients as important contributors to care quality.133 138 148 Patients reported high levels of confidence in IP led care, with the caveat that prescribers demonstrated knowledge and expertise.133 138 148 Good interpersonal, communication, examination, history taking and diagnostic skills were key. These were mandatory for differential diagnosis133–135 148 150 and holistic management,136 146 150 for conferring practitioner prescribing/non-prescribing decisions134 135 150 and managing treatment concordance130 133 135 138 144 148 150 and patient expectations for medicines.134 135 150 Motivational deterrents to IP uptake that were identified by non-prescribing nurses143 and physiotherapists141 were being near retirement,143 a reluctance to undertake further advanced training,141 143 concerns about training rigour141 and a perception of effort/remuneration imbalance.141 143 Although IP job satisfaction and professional benefits were considered future adoption drivers143 lack of financial remuneration in particular disincentivised practice nurse143 and physiotherapy adoption.141
Descriptive theme 2.2: preparing and supporting practitioners during training
UK non-medical prescribing training programmes employ profession-specific or interprofessional models, delivering 26 days equivalent full-time education alongside a supervised learning in practice period.127 Given the onus for safe prescribing, programmes were reported by students and nurse/pharmacist prescribers to be academically rigorous.129 146 There was evidence however that students lacked key knowledge about generic training models,143 the learning expectations of different pedagogies,127 as well as course assessment and portfolio requirements.128 Expecting narrower, specialty specific rather than generic training was common.128 146 Students found the academic demands of training while continuing their usual clinical duties challenging indicating a need to better balance work, personal and academic commitments.127 129 The degree of allocated support time128 129 and the quality of mentoring during supervised practice learning127 were key influences on student learning experiences. Adequate study leave, protected time and backfill respectively optimised study time, reduced personal time encroachment and negated the need to absorb usual role duties while training.128 Despite organisational requirement to confirm study leave arrangements pre-training, primary care allocation was highly unstandardised, with some students entering training without a confirmed agreement.128 Prepared practice mentors with clarity on their role obligations in general provided a higher level of input to students,127 and good mentor–student relationships that continued post-training facilitated transition.132 Additional training buddying schemes helped students better manage the competing demands of training while working, although time constraints limited their uptake.129
Analytical theme 3: transition—ensuring early prescribing support
This analytical theme highlighted the importance of the post-qualification transition period in the development of prescribing confidence/competence and identified a high need for supervision and informal and formal support. Delineating the scope of prescribing competence facilitated early implementation.
Descriptive theme 3.1: transition as a point of vulnerability
Many nurses/pharmacists held vivid memories of anxiety and fear during their first IP encounters,137 139 140 146 147 reporting a diminution of self-confidence during the early transition period.135 137 139 140 146 147 This finding traversed the review decade and was unrelated to how prepared prescribers felt by training.137 146 Heightened awareness of the risks of error,147 the cautionary approach instilled by training137 147 and liability for personal accountability139 146 fuelled feelings. It was recognised that self-confidence and competence development were essential for prescribing137 147 and mitigated anxiety,146 but were highly dependent on exposure to prescribing opportunities,146 147 time137 147 and above all, the level of available support.127 132 139 146 147 Without a channel for accessing supervision, nurses/pharmacists could doubt competence, lose confidence and defer from prescribing.147 This led to a lack of competence development and underutilisation of IP147 and suggests that greater acknowledgement of transitional developmental needs is necessary.
Descriptive theme 3.2: nurturing competence and confidence
Establishing competence boundaries and recognising personal limitations were important enablers in transition.137 147 Nurse/pharmacist prescribers defined competence as the immediate clinical areas in which they had the knowledge and confidence to prescribe.136 137 139 140 147 149 Delineating individual scope of prescribing practice by restricting the range of medicines prescribed to circumscribed clinical areas136 140 146 149 in line with clinical guidelines and protocols137 encouraged the early development of competence.147 Alternatively, prescribing outside these boundaries,137 as in complex polypharmacy or comorbidity,132 140 was deemed risky, unsafe and unprofessional.136 147 149 Nurses/pharmacists reported that teams often failed to recognise their self-confidence issues related to competence,140 and exerted inappropriate expectations for IP.132 136 137 Recognising that as a new skill, development of prescribing competence was time and opportunity dependent137 146 147 several nurses expressed anxiety that prescribing skills would diminish during transition if not used.146
Descriptive theme 3.3: transition support needs
Reports of poor transition support pervaded the review decade130 132 135 136 139 140 146 147 and there was limited evidence of pre-emptive, formalised supervision provision.132 Nurses reported this absence as immediately impactful,139 especially in isolated roles and in services with few prescribers.130 147 While nurses and pharmacists desired structured and informal supervision,140 147 in all seven studies addressing this theme,130 132 136 139 140 146 147 most could only access a variable level of informal support. ‘Open door’ contemporaneous advice given by GPs was the primary source, although specialist doctors, peers and pharmacists were also consulted. Team receptiveness to providing this mentoring,147 its reliability135 139 and accessibility146 147 were key facilitators. Informal opportunities for discussion provided security147 and were valued.136 139 146 147 Exemplifying barrier interdependence, lack of mentoring relationships with doctors limited opportunity for informal support, prevented prescribing and limited competence with specific medicines or clinical conditions.147 In turn this necessitated re-engagement of GP referral for prescribing and culminated in inequitable patient medicines management.140 147 To address shortfalls in formal support provision, several prescribers set up local peer networks,132 136 140 however a strong desire for formalised mentorship was expressed.130 136 140 147
Analytical theme 4: sustainment—maximising and developing independent prescribing
This analytical theme describes barriers and facilitators within the descriptive subthemes of service delivery and supporting role development, which relate to how IP was used and maximised in primary care.
Descriptive theme 4.1: service delivery
Prescribers reported that IP promoted efficient, streamlined services.136 137 139 140 142 146 However, views on how it impacted individual practitioner workload differed.136 137 139 140 146 147 IP reportedly lengthened consultations,130 136 added administrative tasks139 146 and increased job-related stress.136 Undertaking in-depth holistic assessment to inform prescribing needs imposed time constraints,130 150 which were exacerbated in strict 10-minute clinical allocation systems.135 136 Additional time and experience could however be mitigating.135 150 Community IPs reported their main workload barriers as administrative and related to absent or incompatible electronic record and prescription generation systems.132 139 140 146 147 150 Seeking clinical information caused significant delays, in some cases causing IPs to revert to GP referral for prescribing needs.132 139 146 147 However, recent IT accessibility was suggested to mitigate retrieval problems.144
Attitudes towards role change because of IP also influenced perceptions about workload.136 137 Some prescribers perceived that GPs abdicated responsibility for prescribing following introduction of IP146 which increased workload and job demand.136 137 Prescribers negatively referred to this as work offloading,137 and were suspicious of underpinning financial motives.143 Alternatively, other prescribers viewed the benefits of IP at a broader service level and as an opportunity to reduce GP colleague workforce pressures.132 144 146 While GPs in one study stressed that their acceptance of pharmacist IP rested on whether it increased existing workload142 limited team member involvement within studies precluded synthesis of wider primary care workload impact of IP.
Descriptive theme 4.2: supporting role development
Despite limited contextual detail on workforce planning,130 144 149 three broadly categorised ‘models’ of IP implementation were identified. The first ‘Enhancement’ model introduced IP to enhance the efficiency of existing nurse/pharmacist roles without changing the pattern of service provision, client group or condition complexity.137 139 140 147 149 The second ‘Substitution’ model adapted existing IP roles to directly substitute or replace GP services, which required some level of structural re-organisation of care and/or a change in core prescribing competence,130 139 142 144 146 (eg, substituting GPs in out-of-hours palliative care services and additionally managing non-cancer terminal illness146). The final, less frequently evidenced ‘Role specific’ model created new roles specifically for pharmacist prescribers, for which geriatric chronic disease and comorbidity management were new areas of competence, and in which pharmacists assumed a transfer of responsibility from GPs for care home medicines management.142 144 One study found that the specific models of employment/funding influenced how well IP roles were integrated,149 with direct GP practice employment as opposed to commissioned Primary Care Trust (PCT) funded roles creating greater sense of permanence, better role use and enhanced team involvement. This was assumed to result from improved relationships, trust and team building.142 144
A strategical top–down approach to implementation of IP was unclear from the reviewed studies, and overall an individual practitioner, bottom–up approach appeared to drive adoption. However, there was some evidence that where skill mix was recognised and valued within services,144 149 CPD was readily available149 and doctors provided leadership137 149 IP was used to greater extent for primary care redesign and service sustainability. Absent policy and national targets restrained IP resource allocation,130 while policy and national guidance was facilitative.142 144 Doctors also imposed constraints on IP by limiting clinical caseloads,137 147 restricting formularies132 149 or by retaining sole diagnostic prescribing responsibility for patients.130 144 For some prescribers, competence expansion was synonymous with crossing job descriptions and mandated formal negotiation with employers.147
Provision of CPD overall was inconsistent, untargeted to evolving learning needs,136 147 and prescribers identified pharmacology,139 statutory drug updates136 as key topics. Lack of confidence with heart failure,140 mental health conditions130 polypharmacy and off-label prescribing147 suggested CPD in comorbidities warranted further input. Trust provision included forums/meetings,136 140 commissioned training, national conference attendance139 149 and electronic journal resources.139 However, provision varied widely and with few prescribers reporting accessible CPD systems,136 140 there was agreement that improved implementation was necessary.130 136 139 140 147 150
With time and input to create support systems140 and enhance communication concerning role boundaries146 prescribers reported that IP integration improved. However, formal evaluation following implementation was rare,132 with only two studies135 150 identifying quality assurance activities such as audit and local/national data benchmarking in the context of antibiotic stewardship.
Discussion
The future of UK primary care is reliant on workforce expansion and introduction of new first-contact non-medical roles.27 151–154 Ensuring practitioners have the right skills to enable sustainable service development, at scale and pace is key.155 156 Recent reports of rising non-medical prescriber numbers in some regions of the UK30 79 157 suggest healthcare providers are recognising the value of prescribing for skill-mix and workforce transformation. Ensuring implementation is optimised, sustained and IP roles are maximised for service and patient benefit is essential.
This is the first meta-synthesis evaluating barriers and facilitators to the implementation of IP by non-medical healthcare professionals in primary care. Guided by theory and synthesising factors across a continuum of implementation provides a temporal dimension and insight into three primary ‘enhancement’, ‘substitution’, and ‘role specific’ models of implementation that previous UK systematic reviews lack.54 68 69 74 In its infancy in UK primary care non-medical prescribing research,135 144 158 159 implementation theory is likely to become increasingly important for informing implementation strategies as the governance arrangements for extended prescribing rights grow in complexity157 and the socio-political primary care landscape continues to change.160
From stakeholders’ experiences of implementing IP, barriers and facilitators were identified in four key analytical themes: ‘Preparation’, ‘Training’, ‘Transition’ and ‘Sustainment’. While some interdependence and overlap is acknowledged, these themes present a stage based road map of barriers and facilitators for consideration in future implementation.
In the theme ‘Preparation’, the importance of organisational readiness for implementing IP was reflected by a need for consistent managerial leadership/support, improved team understanding of prescribing role intentions and an interprofessional environment that supports novice prescribers. While nurses and pharmacists considered IP integral to advanced practice and essential to enhance workforce skill utilisation there was concern that it lacked strategic prominence in primary care. Accordingly, the ‘Training’ theme identified a need for improved managerial recognition of primary care workforce aspirations for IP along with a need to ensure skills and motivations matched those necessary for training. In line with national reports,43 46 55 the response to the non-medical prescribing agenda has been sluggish in some UK regions,59 with reforms to commissioning either marginalising59 or fragmenting its funding.110 161 Moreover, in common with national evaluations,43 59 162 163 this synthesis identified a continuing practitioner led implementation of IP with largely voluntary uptake. Contrary to secondary care,62 there was limited evidence142 144 for policy driven service design or targeted strategy embedding IP within career or service pathways. This suggests a disjointed approach to implementation that may reflect the rapidly changing policy and service context of UK primary care.164–166 However, with a third of the non-medical general practice workforce near retirement age,167 and succession of IP roles lacking guarantee,149 sustainability of non-medical prescribing capability is a key concern for future management of primary care patient medicines needs.168
Transition was identified as a key stage in implementation that warrants greater scrutiny and has resonance for professions such as paramedics who are new to prescribing. While its affective nature169 170 and need for bespoke support systems has been previously recognised,171 172 few studies have specifically sampled novice prescribers170 173 to ascertain optimal supervisory requirements.169 Despite extension of IP rights to optometrists, physiotherapists, radiographers, podiatrists and paramedics over the past 13 years, focus on implementation issues during transition within each profession has been limited.43 174 175 This is likely to be especially important for paramedics who, awarded IP rights in 2018 have not been subject to the supplementary prescribing lead in period that characterises other professions176 and who are historically less well established in the primary care workforce.177 178 Early data suggesting challenges around role isolation, team expectations of paramedic IP and lack of legislative parity for controlled drugs warrants further exploration to determine whether paramedics too, face similar barriers identified by this review.175 179
In common with other UK reviews,68 69 limited overall focus on long-term sustainability or strategy for implementation at either local, regional or national level was found. This was echoed by the dominance of the ‘enhancement’, as opposed to ‘role specific’ implementation models identified and may reflect the multiple changes made to policy,180 leadership181 and commissioning182 and the ongoing embedding of new governance structures within primary care.183 Of note, despite finding a need for more cohesive managerial support that extends across the entire implementation trajectory, minimal reference was made to the championing and change agent functions of non-medical prescribing leads.171 172 The Department of Health has long recommended implementation of non-medical prescribing under direction of a designated lead with strategic, operational and governance footholds.33 A lack of representation in recent regional research157 supports the tenet that many of these roles were not replaced in England following the abolition of primary care trusts.172 Successful implementation is more likely when champions are fully organisationally supported184 and provide sustained input to implementation activities.171 185 186 However, a lack of role infrastructure, clarity and designated time,157 172 along with the increasingly diverse non-medical prescribing workforce is challenging this important role. While other models of primary care workforce mentoring show promise,187 the repetition and frequency of barriers exposed by this synthesis over the review decade indicate urgent need for a more cohesive approach to supporting IP.
Strengths and limitations
This review strengthens the UK evidence base by identifying challenges to IP implementation in traditional and contemporary primary care contexts. Using comprehensive search strategies and robust analysis methods, it highlights factors during ‘Preparation’, ‘Training’, ‘Transition’ and ‘Sustainment’ stages and models of implementation which can be used by practitioners and policymakers to identify areas for improving implementation support.
Although limited to UK literature, the theoretical lens ensured focus on common factors known to facilitate implementation (eg, the need for leadership and championing) which are generalisable to any implementation context, either in the UK or internationally. We did not however include grey literature and although qualitative synthesis enabled rich description of elements perceived by stakeholders to influence implementation of IP in the UK, reviews that include quantitative literature in primary care are encouraged. Our focus on primary care excluded barriers and facilitators that may be unique to acute care and other settings. Moreover, as the non-medical prescribing agenda is disseminated across the NHS, it will be increasingly important to consider the theoretical basis for developing strategies to achieve more successful implementation of this complex innovation in different professions.67 119 188
Conclusion
Globally, healthcare systems are implementing strategies to address workforce deficits that enhance the skills of nurses, pharmacists and other non-medical healthcare professionals. Integral to advanced scope of practice, it is imperative that IP capability is optimised through successful implementation. This meta-synthesis has identified persistent barriers at the ‘Preparation’, ‘Training’, ‘Transition’ and ‘Sustainment’ stages of implementation. A more coordinated and targeted approach to overcome barriers identified in these stages is key to ensuring that IP is an effective approach to helping alleviate workforce shortfalls in the UK, and around the world.
Supplementary Material
Footnotes
Twitter: @666mellemel, @nmp_nicolacarey
Contributors: JE and NC conceived the study. JE obtained funding, oversaw all aspects of the project and contributed to all stages. JE drafted this paper. JE designed and executed all the searches, data extraction, coding and quality appraisal. NC contributed to all stages of the review, including data extraction and coding. MC and NC contributed to the evolving synthesis and formulation of conclusions. JE is the guarantor of the paper.
Funding: This work was supported by a University of Surrey Doctoral Scholarship 2018–2021 award (6522700).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. No additional data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Dugani S, Veillard J, Evans TG. Quality primary health care will drive the realization of universal health coverage. CMAJ 2018;190:E453–4. 10.1503/cmaj.180186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kluge H, Kelley E, Swaminathan S, et al. After Astana: building the economic case for increased investment in primary health care. Lancet 2018;392:2147–52. 10.1016/S0140-6736(18)32859-9 [DOI] [PubMed] [Google Scholar]
- 3.King's Fund . The health care workforce in England. Make or break? London: King’s Fund, 2018. [Google Scholar]
- 4.Stenberg K, Hanssen O, Bertram M, et al. Guide posts for investment in primary health care and projected resource needs in 67 low-income and middle-income countries: a modelling study. Lancet Glob Health 2019;7:e1500–10. 10.1016/S2214-109X(19)30416-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO . Operational framework for primary health care: transforming vision into action. Geneva: World Health Organization, 2020. [Google Scholar]
- 6.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 7.Stafford M, Steventon A, Thorlby R. Briefing: Understanding the health care needs of people with multiple health conditions. London: The Health Foundation, 2018. [Google Scholar]
- 8.Kingston A, Robinson L, Booth H, et al. Projections of multi-morbidity in the older population in England to 2035: estimates from the population ageing and care simulation (PACSim) model. Age Ageing 2018;47:374–80. 10.1093/ageing/afx201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith SM, Wallace E, O'Dowd T. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev 2016;4:CD006560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO . Multimorbidity: Technical Series on Safer Primary Care. Geneva: World Health Organization, 2016. [Google Scholar]
- 11.Lim J, Broughan J, Crowley D, et al. COVID-19's impact on primary care and related mitigation strategies: a scoping review. Eur J Gen Pract 2021;27:166–75. 10.1080/13814788.2021.1946681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenhalgh T, Knight M, A'Court C, et al. Management of post-acute covid-19 in primary care. BMJ 2020;370:m3026. 10.1136/bmj.m3026 [DOI] [PubMed] [Google Scholar]
- 13.Julia C, Saynac Y, Le Joubioux C, et al. Organising community primary care in the age of COVID-19: challenges in disadvantaged areas. Lancet Public Health 2020;5::e313. 10.1016/S2468-2667(20)30115-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pettigrew LM, Kumpunen S, Mays N. Primary care networks: the impact of covid-19 and the challenges ahead. BMJ 2020;370:m3353. 10.1136/bmj.m3353 [DOI] [PubMed] [Google Scholar]
- 15.Williams S, Tsiligianni I. COVID-19 poses novel challenges for global primary care. NPJ Prim Care Respir Med 2020;30:30. 10.1038/s41533-020-0187-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.IQVIA Institute for Human Data Science . Global medicine spending and usage trends: outlook to 2024. New York: IQVIA Institute for Human Data Science, 2020. [Google Scholar]
- 17.Avery A, Barber N, Ghaleb M. Investigating the Prevalence and Causes of Prescribing Errors in General Practice: The PRACtICe Study. General Medical Council, 2012. [Google Scholar]
- 18.WHO . Declaration of Astana. Global Conference on Primary Health Care: from Alma-Ata towards universal health coverage and the Sustainable Development Goals. Geneva: World Health Organization, 2018. [Google Scholar]
- 19.Osborn R, Moulds D, Schneider EC, et al. Primary care physicians in ten countries report challenges caring for patients with complex health needs. Health Aff 2015;34:2104–12. 10.1377/hlthaff.2015.1018 [DOI] [PubMed] [Google Scholar]
- 20.Rosen R, Parker H. New models of primary care: practical lessons from early implementers. London: Nuffield Trust, 2013. [Google Scholar]
- 21.Ham C, Heenan D, Longley M. Integrated care in Northern Ireland, Scotland and Wales. Lessons for England. London: The King’s Fund, 2013. [Google Scholar]
- 22.Mercer SW, Gillies J, Noble-Jones R. National Evaluation of New Models of Primary Care in Scotland. Glasgow: Scottish School of Primary Care, 2019. [Google Scholar]
- 23.NHS England . Integrating care. In: Next steps to building strong and effective integrated care systems across England. London: NHS England, 2020. [Google Scholar]
- 24.Welsh Government . Our plan for a primary care service for Wales up to March 201. 2015. NHS Wales, 8. [Google Scholar]
- 25.Morciano M, Checkland K, Hammond J, et al. Variability in size and characteristics of primary care networks in England: observational study. Br J Gen Pract 2020;70:e899–905. 10.3399/bjgp20X713441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Department of Health . The NHS Long Term Plan. London, UK: Department of Health, 2019. [Google Scholar]
- 27.Baird B, Beech J. Primary care networks explained. London: The King’s Fund, 2020. [Google Scholar]
- 28.UK Parliament . Health and care bill. London: House of Commons, 2021. [Google Scholar]
- 29.Weeks G, George J, Maclure K, et al. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst Rev 2016;11:CD011227. 10.1002/14651858.CD011227.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alghamdi SSA, Hodson K, Deslandes P, et al. Prescribing trends over time by non-medical independent prescribers in primary care settings across Wales (2011-2018): a secondary database analysis. BMJ Open 2020;10:e036379. 10.1136/bmjopen-2019-036379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Prescribing Centre . Non-medical prescribing by nurses, optometrists, pharmacists, physiotherapists, podiatrists and radiographers. A quick guide for commissioners. Liverpool, 2010. [Google Scholar]
- 32.Hogg D. Prescription, supply and administration of medicines by allied health professionals - where are we now and where are we going? Regional AHP Non-Medical Prescriber Forum. Taunton, 2019. [Google Scholar]
- 33.Department of Health . Improving patients' access to medicines: a guide to implementing nurse and pharmacist independent prescribing within the NHS in England. 2nd edn. Leeds, 2006. [Google Scholar]
- 34.Graham-Clarke E, Rushton A, Noblet T, et al. Non-medical prescribing in the United Kingdom National health service: a systematic policy review. PLoS One 2019;14:e0214630. 10.1371/journal.pone.0214630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.HM Government . The medicines for human use (prescribing) (miscellaneous amendments) order, 2006. [Google Scholar]
- 36.The National Health Service . Miscellaneous amendments relating to independent prescribing regulations. London, 2006. [Google Scholar]
- 37.General Pharmaceutical Council . Standards for the education and training of pharmacist independent prescribers. London, 2019. [Google Scholar]
- 38.Health and Care Professions Council . Standards for prescribing. London, 2019. [Google Scholar]
- 39.NMC . Standards for prescribing programmes, 2019. Available: https://www.nmc.org.uk/standards/standards-for-post-registration/standards-for-prescribers/standards-of-proficiency-for-nurse-and-midwife-prescribers/ [Accessed 12 Jan 2021].
- 40.Hales L, Lohan M, Jordan J. ‘It’s another way of standing outside the door’ supplementary prescribing and doctor–nurse partnerships. Soc Theory Health 2010;8:210–28. 10.1057/sth.2010.1 [DOI] [Google Scholar]
- 41.Hill DR, Conroy S, Brown RC, et al. Stakeholder views on pharmacist prescribing in addiction services in NHS Lanarkshire. J Subst Use 2014;19:56–67. 10.3109/14659891.2012.734540 [DOI] [Google Scholar]
- 42.Carey N, Stenner K, Courtenay M. An exploration of how nurse prescribing is being used for patients with respiratory conditions across the East of England. BMC Health Serv Res 2014;14:27. 10.1186/1472-6963-14-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carey N, Stenner K, Edwards J. Evaluation of physiotherapist and Podiatrist independent prescribing, mixing of medicines and prescribing of controlled drugs. Department of health policy research PR-R7-0513-11002. Guildford, UK: University of Surrey, 2017. [Google Scholar]
- 44.Courtenay M, Carey N, Stenner K. An overiew of non medical prescribing across one strategic health authority: a questionnaire survey. BMC Health Serv Res 2012;12:138. 10.1186/1472-6963-12-138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bhanbhro S, Drennan VM, Grant R, et al. Assessing the contribution of prescribing in primary care by nurses and professionals allied to medicine: a systematic review of literature. BMC Health Serv Res 2011;11:330. 10.1186/1472-6963-11-330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Latter S, Blenkinsopp A, Smith A. Evaluation of nurse and pharmacist independent prescribing. University of Southampton: Southampton, 2010. [Google Scholar]
- 47.Latter S, Smith A, Blenkinsopp A, et al. Are nurse and pharmacist independent prescribers making clinically appropriate prescribing decisions? an analysis of consultations. J Health Serv Res Policy 2012;17:149–56. 10.1258/JHSRP.2012.011090 [DOI] [PubMed] [Google Scholar]
- 48.Carey N, Edwards J, Otter S, et al. A comparative case study of prescribing and non-prescribing physiotherapists and podiatrists. BMC Health Serv Res 2020;20:1074. 10.1186/s12913-020-05918-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ecker S, Joshi R, Shanthosh J, et al. Non-Medical prescribing policies: a global scoping review. Health Policy 2020;124:721–6. 10.1016/j.healthpol.2020.04.015 [DOI] [PubMed] [Google Scholar]
- 50.Faruquee C, Guirguis L, Hughes C. Characterizing pharmacist prescribers in Alberta using cluster analysis. J Pharm Health Serv Res 2018;10. [Google Scholar]
- 51.Fong J, Cashin A, Buckley T. Models of prescribing, scope of practice, and medicines prescribed, a survey of nurse practitioners. J Adv Nurs 2020;76:2311–22. 10.1111/jan.14444 [DOI] [PubMed] [Google Scholar]
- 52.Kroezen M, van Dijk L, Groenewegen PP, et al. Nurse prescribing of medicines in Western European and Anglo-Saxon countries: a systematic review of the literature. BMC Health Serv Res 2011;11:127. 10.1186/1472-6963-11-127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ladd E, Schober M. Nurse prescribing from the global vantage point: the intersection between role and policy. Policy Polit Nurs Pract 2018;19:1–10. 10.1177/1527154418797726 [DOI] [PubMed] [Google Scholar]
- 54.Mills T, Patel N, Ryan K. Pharmacist non-medical prescribing in primary care. A systematic review of views, opinions, and attitudes. Int J Clin Pract 2021;75:e13827. 10.1111/ijcp.13827 [DOI] [PubMed] [Google Scholar]
- 55.Courtenay M, Khanfer R, Harries-Huntly G, et al. Overview of the uptake and implementation of non-medical prescribing in Wales: a national survey. BMJ Open 2017;7:e015313. 10.1136/bmjopen-2016-015313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dobel-Ober D, Brimblecombe N. National survey of nurse prescribing in mental health services; a follow-up 6 years on. J Psychiatr Ment Health Nurs 2016;23:378–86. 10.1111/jpm.12329 [DOI] [PubMed] [Google Scholar]
- 57.Wilson N, Pope C, Roberts L, et al. Limited pharmaceuticalisation: a qualitative case study of physiotherapist prescribing practices in an NHS trust in England following the expansion of non-medical prescribing in the UK. Sociol Health Illn 2020;42:643–59. 10.1111/1467-9566.13050 [DOI] [PubMed] [Google Scholar]
- 58.Weiss MC. The rise of non-medical prescribing and medical dominance. Res Social Adm Pharm 2021;17:632–7. 10.1016/j.sapharm.2020.05.015 [DOI] [PubMed] [Google Scholar]
- 59.Coull A, Murray I, Turner-Halliday F, et al. The expansion of nurse prescribing in Scotland: an evaluation. Br J Community Nurs 2013;18:235–42. 10.12968/bjcn.2013.18.5.234 [DOI] [PubMed] [Google Scholar]
- 60.Drennan J, Naughton C, Allen D. Independent evaluation of the nurse and midwife prescribing initiative. Dublin: University College Dublin, 2009. [Google Scholar]
- 61.Casey M, Rohde D, Higgins A, et al. "Providing a complete episode of care": A survey of registered nurse and registered midwife prescribing behaviours and practices. J Clin Nurs 2020;29:152–62. 10.1111/jocn.15073 [DOI] [PubMed] [Google Scholar]
- 62.Fisher J, Kinnear M, Reid F, et al. What supports hospital pharmacist prescribing in Scotland? - A mixed methods, exploratory sequential study. Res Social Adm Pharm 2018;14:488–97. 10.1016/j.sapharm.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 63.Ross JD, Kettles AM. Mental health nurse independent prescribing: what are nurse prescribers' views of the barriers to implementation? J Psychiatr Ment Health Nurs 2012;19:916–32. 10.1111/j.1365-2850.2011.01872.x [DOI] [PubMed] [Google Scholar]
- 64.Stewart D, Maclure K, Newham R, et al. A cross-sectional survey of the pharmacy workforce in general practice in Scotland. Fam Pract 2020;37:206–12. 10.1093/fampra/cmz052 [DOI] [PubMed] [Google Scholar]
- 65.General Pharmaceutical Council . Prescribers survey report. London, 2016. [Google Scholar]
- 66.Stenner K, Carey N, Courtenay M. Implementing nurse prescribing: a case study in diabetes. J Adv Nurs 2010;66:522–31. 10.1111/j.1365-2648.2009.05212.x [DOI] [PubMed] [Google Scholar]
- 67.Stewart D, Jebara T, Cunningham S, et al. Future perspectives on nonmedical prescribing. Ther Adv Drug Saf 2017;8:183–97. 10.1177/2042098617693546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Graham-Clarke E, Rushton A, Noblet T, et al. Facilitators and barriers to non-medical prescribing - A systematic review and thematic synthesis. PLoS One 2018;13:e0196471. 10.1371/journal.pone.0196471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Noblet T, Marriott J, Graham-Clarke E, et al. Barriers to and facilitators of independent non-medical prescribing in clinical practice: a mixed-methods systematic review. J Physiother 2017;63:221–34. 10.1016/j.jphys.2017.09.001 [DOI] [PubMed] [Google Scholar]
- 70.Jebara T, Cunningham S, MacLure K, et al. Stakeholders' views and experiences of pharmacist prescribing: a systematic review. Br J Clin Pharmacol 2018;84:1883–905. 10.1111/bcp.13624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nuttall D. Nurse prescribing in primary care: a metasynthesis of the literature. Prim Health Care Res Dev 2018;19:7–22. 10.1017/S1463423617000500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhou M, Desborough J, Parkinson A, et al. Barriers to pharmacist prescribing: a scoping review comparing the UK, New Zealand, Canadian and Australian experiences. Int J Pharm Pract 2019;27:479–89. 10.1111/ijpp.12557 [DOI] [PubMed] [Google Scholar]
- 73.Edwards J, Coward M, Carey N. Paramedic independent prescribing in primary care: seven steps to success. J Prescr Pract 2020;2:292–9. [Google Scholar]
- 74.Magowan J. Barriers and enablers to nurse prescribing in primary care. J Prescr Pract 2020;2:142–6. [Google Scholar]
- 75.Carey N, Stenner K, Courtenay M. Stakeholder views on the impact of nurse prescribing on dermatology services. J Clin Nurs 2010;19:498–506. 10.1111/j.1365-2702.2009.02874.x [DOI] [PubMed] [Google Scholar]
- 76.Stewart F, Caldwell G, Cassells K, et al. Building capacity in primary care: the implementation of a novel 'Pharmacy First' scheme for the management of UTI, impetigo and COPD exacerbation. Prim Health Care Res Dev 2018;19:531–41. 10.1017/S1463423617000925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Maskrey M, Johnson CF, Cormack J, et al. Releasing GP capacity with pharmacy prescribing support and new ways of working: a prospective observational cohort study. Br J Gen Pract 2018;68:e735–42. 10.3399/bjgp18X699137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mann C, Anderson C, Waring J. “GP Pharmacy Transformation project” Community Pharmacist Independent Prescribers (CPIPs) working in patient facing roles in Primary Care. Independent Evaluation Report. Nottingham: University of Nottingham, NHS England, 2017. [Google Scholar]
- 79.Northamptonshire GP Forward View Programme . Primary care workforce strategy. Northampton: Corby Clinical Commissioning Group and Nene Clinical Commissioning Group, 2017. [Google Scholar]
- 80.Greenhalgh T, Robert G, Macfarlane F, et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581–629. 10.1111/j.0887-378X.2004.00325.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rogers E. Diffusion of innovations. 5th edn. New York, USA: The Free Press, 2003. [Google Scholar]
- 82.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009;4:50. 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lambert-Kerzner AC, Aasen DM, Overbey DM, et al. Use of the consolidated framework for implementation research to guide dissemination and implementation of new technologies in surgery. J Thorac Dis 2019;11:S487–99. 10.21037/jtd.2019.01.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chor KHB, Wisdom JP, Olin S-CS, et al. Measures for predictors of innovation adoption. Adm Policy Ment Health 2015;42:545–73. 10.1007/s10488-014-0551-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dearing JW, Cox JG. Diffusion of innovations theory, principles, and practice. Health Aff 2018;37:183–90. 10.1377/hlthaff.2017.1104 [DOI] [PubMed] [Google Scholar]
- 86.Dearing JW, Singhal A. New directions for diffusion of innovations research: Dissemination, implementation, and positive deviance. Hum Behav Emerg Technol 2020;2:307–13. [Google Scholar]
- 87.Breimaier HE, Heckemann B, Halfens RJG, et al. The consolidated framework for implementation research (CFIR): a useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital-based nursing practice. BMC Nurs 2015;14:43. 10.1186/s12912-015-0088-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.CFIR . Consolidated framework for implementation research. Ann Arbor: USA: CFIR Research Team-Center for Clinical Management Research, 2021. https://cfirguide.org/tools/ [Google Scholar]
- 89.Damschroder LJ, Reardon CM, Sperber N, et al. Implementation evaluation of the telephone lifestyle coaching (TLC) program: organizational factors associated with successful implementation. Transl Behav Med 2017;7:233–41. 10.1007/s13142-016-0424-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12:181. 10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Aguirre R, Bolton K. Qualitative interpretive meta-synthesis in social work research: Uncharted Territory. J Soc Work 2014;14:279–94. [Google Scholar]
- 93.Nye E, Melendez-Torres GJ, Origins BC. Methods and advances in qualitative meta-synthesis. Rev Educ 2016;4:57–79. [Google Scholar]
- 94.et alBooth A, Noyes J, Flemming K. Guidance on choosing qualitative evidence synthesis methods for use in health technology assessments of complex interventions (on-line, 2016. Available: http://www.integrate-hta.eu/downloads/ [Accessed 17 Dec 2021].
- 95.National Cancer Institute . Qualitative research in implementation science (QualRIS). USA: U.S. Department of Health and Human Sciences, National Institues of Health, 2019. [Google Scholar]
- 96.Michie S, Fixsen D, Grimshaw JM, et al. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement Sci 2009;4:40. 10.1186/1748-5908-4-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Edwards J, Coward M, Carey N. Barriers and facilitators to implementation of non-medical independent prescribing in primary care: a qualitative systematic review (CRD42019124400). York: PROSPERO, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bosch M, van der Weijden T, Wensing M, et al. Tailoring quality improvement interventions to identified barriers: a multiple case analysis. J Eval Clin Pract 2007;13:161–8. 10.1111/j.1365-2753.2006.00660.x [DOI] [PubMed] [Google Scholar]
- 99.Grol R, Wensing M. What drives change? barriers to and incentives for achieving evidence-based practice. Med J Aust 2004;180:S57–60. 10.5694/j.1326-5377.2004.tb05948.x [DOI] [PubMed] [Google Scholar]
- 100.Nilsson-Kajermo K, Bostrom A-M, Thompson DS. The BARRIERS scale - the barriers to research utilization scale: a systematic review. Implementation science: IS 2010;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shaw B, Cheater F, Baker R, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2005:CD005470. 10.1002/14651858.CD005470 [DOI] [PubMed] [Google Scholar]
- 102.WHO . How do we ensure that innovation in health service delivery and organization is implemented sustained and spread? Copenhagen: European Observatory on Health Systems and Policies, 2018. [Google Scholar]
- 103.Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res 2012;22:1435–43. 10.1177/1049732312452938 [DOI] [PubMed] [Google Scholar]
- 104.Rogers M, Bethel A, Abbott R. Locating qualitative studies in dementia on MEDLINE, EMBASE, CINAHL, and PsycINFO: a comparison of search strategies. Res Synth Methods 2018;9:579–86. 10.1002/jrsm.1280 [DOI] [PubMed] [Google Scholar]
- 105.Rosumeck S, Wagner M, Wallraf S, et al. A validation study revealed differences in design and performance of search filters for qualitative research in PsycINFO and CINAHL. J Clin Epidemiol 2020;128:101–8. 10.1016/j.jclinepi.2020.09.031 [DOI] [PubMed] [Google Scholar]
- 106.Department of Health . Equity and excellence: Liberating the NHS. London, UK: NHS, 2010. [Google Scholar]
- 107.HM Government . The Health and Social Care Act 2012. London: The Stationery Office, 2012. [Google Scholar]
- 108.NHS England . Five Year Forward View. London, 2014. [Google Scholar]
- 109.Vizard P, Obolenskaya P. The Coalition’s Record on Health: Policy, Spending and Outcomes 2010-2015. Social Policy in a Cold Climate: Working Paper. London, UK: The London School of Economics and Political Science, 2015. [Google Scholar]
- 110.Gadsby EW, Peckham S, Coleman A, et al. Commissioning for health improvement following the 2012 health and social care reforms in England: what has changed? BMC Public Health 2017;17:1–11. 10.1186/s12889-017-4122-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Miller T, Bonas S, Dixon-Woods M. Qualitative research on breastfeeding in the UK: a narrative review and methodological reflection. Evid Policy 2007;3:197–230. 10.1332/174426407781172162 [DOI] [Google Scholar]
- 112.Noyes J, Popay J. Directly observed therapy and tuberculosis: how can a systematic review of qualitative research contribute to improving services? A qualitative meta-synthesis. J Adv Nurs 2007;57:227–43. 10.1111/j.1365-2648.2006.04092.x [DOI] [PubMed] [Google Scholar]
- 113.Carroll C, Booth A, Lloyd-Jones M. Should we exclude inadequately reported studies from qualitative systematic reviews? an evaluation of sensitivity analyses in two case study reviews. Qual Health Res 2012;22:1425–34. 10.1177/1049732312452937 [DOI] [PubMed] [Google Scholar]
- 114.Sirriyeh R, Lawton R, Gardner P, et al. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract 2012;18:746–52. 10.1111/j.1365-2753.2011.01662.x [DOI] [PubMed] [Google Scholar]
- 115.Fenton L, Lauckner H, Gilbert R. The QATSDD critical appraisal tool: comments and critiques. J Eval Clin Pract 2015;21:1125–8. 10.1111/jep.12487 [DOI] [PubMed] [Google Scholar]
- 116.National Institute of Care and Health Excellence . Developing NICE guidelines: the manual. London, 2020. https://www.nice.org.uk/process/pmg20/chapter/reviewing-research-evidence [PubMed] [Google Scholar]
- 117.Noyes J, Booth A, Lewin S, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 6: how to assess relevance of the data. Implement Sci 2018;13:4. 10.1186/s13012-017-0693-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fixsen DL, Blase KA, Van Dyke MK. The stages of implementation. Implementation Practice & Science. Chapel Hill, NC: Active Implementation Research Network 2019:81–108. [Google Scholar]
- 119.Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci 2015;10:53. 10.1186/s13012-015-0242-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Saldana L. The stages of implementation completion for evidence-based practice: protocol for a mixed methods study. Implement Sci 2014;9:43. 10.1186/1748-5908-9-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:45. 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 123.Checkland K, Harrison S, Marshall M. Is the metaphor of 'barriers to change' useful in understanding implementation? Evidence from general medical practice. J Health Serv Res Policy 2007;12:95–100. 10.1258/135581907780279657 [DOI] [PubMed] [Google Scholar]
- 124.Hossain LN, Fernandez-Llimos F, Luckett T, et al. Qualitative meta-synthesis of barriers and facilitators that influence the implementation of community pharmacy services: perspectives of patients, nurses and general medical practitioners. BMJ Open 2017;7:e015471. 10.1136/bmjopen-2016-015471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Booth A, Carroll C, Ilott I, et al. Desperately seeking dissonance: identifying the disconfirming case in qualitative evidence synthesis. Qual Health Res 2013;23:126–41. 10.1177/1049732312466295 [DOI] [PubMed] [Google Scholar]
- 126.Bazeley P. Analysing qualitative data: More than 'identifying themes'. Malays J Qual Res 2009;2. [Google Scholar]
- 127.Afseth JD, Paterson RE. The views of non-medical prescribing students and medical mentors on interprofessional competency assessment - A qualitative exploration. Nurse Educ Today 2017;52:103–8. 10.1016/j.nedt.2017.02.022 [DOI] [PubMed] [Google Scholar]
- 128.Boreham N, Coull AF, Murray ID, et al. Education programmes preparing independent prescribers in Scotland: an evaluation. Nurse Educ Today 2013;33:321–6. 10.1016/j.nedt.2013.01.018 [DOI] [PubMed] [Google Scholar]
- 129.Bowskill D, Meade O, Lymn JS. Use and evaluation of a mentoring scheme to promote integration of non-medical prescribing in a clinical context. BMC Med Educ 2014;14:1–12. 10.1186/1472-6920-14-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Brodie L, Donaldson J, Watt S. Non-medical prescribers and benzodiazepines: a qualitative study. Nurse Prescribing 2014;12:353–9. 10.12968/npre.2014.12.7.353 [DOI] [Google Scholar]
- 131.Carter M, Chapman S, Watson MC. Multiplicity and complexity: a qualitative exploration of influences on prescribing in UK general practice. BMJ Open 2021;11:e041460. 10.1136/bmjopen-2020-041460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cole T, Gillett K. Are nurse prescribers issuing prescriptions in palliative care? Nurse Prescribing 2015;13:98–102. 10.12968/npre.2015.13.2.98 [DOI] [Google Scholar]
- 133.Courtenay M, Stenner K, Carey N. The views of patients with diabetes about nurse prescribing. Diabet Med 2010;27:1049–54. 10.1111/j.1464-5491.2010.03051.x [DOI] [PubMed] [Google Scholar]
- 134.Courtenay M, Rowbotham S, Lim R, et al. Antibiotics for acute respiratory tract infections: a mixed-methods study of patient experiences of non-medical prescriber management. BMJ Open 2017;7:e013515. 10.1136/bmjopen-2016-013515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Courtenay M, Rowbotham S, Lim R, et al. Examining influences on antibiotic prescribing by nurse and pharmacist prescribers: a qualitative study using the theoretical domains framework and COM-B. BMJ Open 2019;9:e029177. 10.1136/bmjopen-2019-029177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Cousins R, Donnell C. Nurse prescribing in general practice: a qualitative study of job satisfaction and work-related stress. Fam Pract 2012;29:223–7. 10.1093/fampra/cmr077 [DOI] [PubMed] [Google Scholar]
- 137.Daughtry J, Hayter M. A qualitative study of practice nurses‘ prescribing experiences. Practice Nursing 2010;21:310–4. 10.12968/pnur.2010.21.6.48329 [DOI] [Google Scholar]
- 138.Dhalivaal J. Patients’ perspectives on prescribing by nurses in general practice. Practice Nursing 2011;22:41–6. 10.12968/pnur.2011.22.1.41 [DOI] [Google Scholar]
- 139.Downer F, Shepherd CK. District nurses prescribing as nurse independent prescribers. Br J Community Nurs 2010;15:348–52. 10.12968/bjcn.2010.15.7.48774 [DOI] [PubMed] [Google Scholar]
- 140.Herklots A, Baileff A, Latter S. Community matrons' experience as independent prescribers. Br J Community Nurs 2015;20:217. 10.12968/bjcn.2015.20.5.217 [DOI] [PubMed] [Google Scholar]
- 141.Holden MA, Whittle R, Waterfield J, et al. A mixed methods exploration of physiotherapist's approaches to analgesic use among patients with hip osteoarthritis. Physiotherapy 2019;105:328–37. 10.1016/j.physio.2018.08.003 [DOI] [PubMed] [Google Scholar]
- 142.Inch J, Notman F, Bond CM, et al. The Care Home Independent Prescribing Pharmacist Study (CHIPPS)-a non-randomised feasibility study of independent pharmacist prescribing in care homes. Pilot Feasibility Stud 2019;5:89. 10.1186/s40814-019-0465-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kelly A, Neale J, Rollings R. Barriers to extended nurse prescribing among practice nurses. Community Pract 2010;83:21–4. [PubMed] [Google Scholar]
- 144.Lane K, Bond C, Wright D, et al. "Everyone needs to understand each other's systems": Stakeholder views on the acceptability and viability of a Pharmacist Independent Prescriber role in care homes for older people in the UK. Health Soc Care Community 2020;28:1479–87. 10.1111/hsc.12970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Latham K, Nyatanga B. Community palliative care clinical nurse specialists as independent prescribers: Part 1. Br J Community Nurs 2018;23:94–8. 10.12968/bjcn.2018.23.2.94 [DOI] [PubMed] [Google Scholar]
- 146.Latham K, Nyatanga B. Community palliative care clinical nurse specialists as independent prescribers: Part 2. Br J Community Nurs 2018;23:126–33. 10.12968/bjcn.2018.23.3.126 [DOI] [PubMed] [Google Scholar]
- 147.Maddox C, Halsall D, Hall J, et al. Factors influencing nurse and pharmacist willingness to take or not take responsibility for non-medical prescribing. Res Social Adm Pharm 2016;12:41–55. 10.1016/j.sapharm.2015.04.001 [DOI] [PubMed] [Google Scholar]
- 148.Stenner KL, Courtenay M, Carey N. Consultations between nurse prescribers and patients with diabetes in primary care: a qualitative study of patient views. Int J Nurs Stud 2011;48:37–46. 10.1016/j.ijnurstu.2010.06.006 [DOI] [PubMed] [Google Scholar]
- 149.Weiss MC, Platt J, Riley R. GPs, nurses and pharmacists as prescribers in primary care: an exploration using the social identity approach / Hausärzte/-innen, Diplomierte Pflegefachpersonen und Apotheker/-innen ALS Arzneimittelverschreiber/-innen: eine exploration MIT dem ansatz Der Sozialen Identität. Int J Health Prof 2016;3:153–64. [Google Scholar]
- 150.Williams SJ, Halls AV, Tonkin-Crine S, et al. General practitioner and nurse prescriber experiences of prescribing antibiotics for respiratory tract infections in UK primary care out-of-hours services (the unite study). J Antimicrob Chemother 2018;73:795–803. 10.1093/jac/dkx429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Health Education England . The future of primary care. Creating teams for tomorrow. London, UK: Primary Care Workforce Commission, 2015. [Google Scholar]
- 152.Health Education England . Elective Care High Impact Interventions: First Contact Practitioner for MSK Services. London: Health Education England, NHS Improvment, 2019. [Google Scholar]
- 153.NHS England . Building the workforce — the new deal for general practice. London: NHS England, Health Education England, 2015. [Google Scholar]
- 154.NHS England . General Practice Forward View. London: NHS England, 2016. [Google Scholar]
- 155.Beech J, Bottery S, Charlesworth A. Closing the gap. Key areas for action on the health and care workforce. London, UK: The Nuffield Trust, 2019. [Google Scholar]
- 156.Primary Care Workforce Commission . The future of primary care. Creating teams for tomorrow. In: Roland M, ed. Report by the primary care workforce Commission. London: Health Education England, 2015. [Google Scholar]
- 157.Jarmain S, Carey N. Exploring the roles and responsibilities of non-medical prescribing leads in the South West of England. J Prescr Pract 2020;2:546–54. 10.12968/jprp.2020.2.10.546 [DOI] [Google Scholar]
- 158.Lim R, Courtenay M, Deslandes R, et al. Theory-based electronic learning intervention to support appropriate antibiotic prescribing by nurse and pharmacist independent prescribers: an acceptability and feasibility experimental study using mixed methods. BMJ Open 2020;10:e036181. 10.1136/bmjopen-2019-036181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Reeve J, Britten N, Byng R, et al. Identifying enablers and barriers to individually tailored prescribing: a survey of healthcare professionals in the UK. BMC Fam Pract 2018;19:17. 10.1186/s12875-017-0705-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lau R, Stevenson F, Ong BN, et al. Achieving change in primary care--effectiveness of strategies for improving implementation of complex interventions: systematic review of reviews. BMJ Open 2015;5:e009993. 10.1136/bmjopen-2015-009993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ham C, Baird B, Gregory S. The NHS under the coalition government. Part one: NHS reform. London: King’s Fund, 2015. [Google Scholar]
- 162.Hacking S, Taylor J. An evaluation of the scope and practice of Non Medical Prescribing in the North West For NHS North West. Manchester, UK: NHS North West, 2010. [Google Scholar]
- 163.i5 Health . Non-Medical prescribing; an economic evaluation. NHS Health Education North West, 2015. [Google Scholar]
- 164.Pettigrew LM, Kumpunen S, Mays N, et al. The impact of new forms of large-scale general practice provider collaborations on England's NHS: a systematic review. Br J Gen Pract 2018;68:e168. 10.3399/bjgp18X694997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sheaff R. Plural provision of primary medical care in England, 2002–2012. J Health Serv Res Policy 2013;18:20–8. 10.1177/1355819613489544 [DOI] [PubMed] [Google Scholar]
- 166.Smith J, Holder H, Edwards N. Securing the future of general practice: new models of primary care. London: Kings' Fund, Nuffield Trust, 2013. [Google Scholar]
- 167.Digital NHS. General Practice Workforce: interactive dashboard. London: NHS Digital, 2022. [Google Scholar]
- 168.Tonna A, McCaig D, Diack L, et al. Development of consensus guidance to facilitate service redesign around pharmacist prescribing in UK hospital practice. Int J Clin Pharm 2014;36:1069–76. 10.1007/s11096-014-9996-8 [DOI] [PubMed] [Google Scholar]
- 169.Abuzour AS, Lewis PJ, Tully MP. Practice makes perfect: a systematic review of the expertise development of pharmacist and nurse independent prescribers in the United Kingdom. Res Social Adm Pharm 2018;14:6–17. 10.1016/j.sapharm.2017.02.002. 10.1016/j.sapharm.2017.02.002 [DOI] [PubMed] [Google Scholar]
- 170.Bowskill D, Timmons S, James V. How do nurse prescribers integrate prescribing in practice: case studies in primary and secondary care. J Clin Nurs 2013;22:2077–86. 10.1111/j.1365-2702.2012.04338.x [DOI] [PubMed] [Google Scholar]
- 171.Courtenay M, Carey N, Stenner K. Non medical prescribing leads views on their role and the implementation of non medical prescribing from a multi-organisational perspective. BMC Health Serv Res 2011;11:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lim RHM, Courtenay M, Fleming G. Roles of the non-medical prescribing leads within organisations across a strategic health authority: perceived functions and factors supporting the role. Int J Pharm Pract 2013;21:82–91. 10.1111/j.2042-7174.2012.00224.x [DOI] [PubMed] [Google Scholar]
- 173.Ziegler L, Bennett M, Blenkinsopp A, et al. Non-medical prescribing in palliative care: a regional survey. Palliat Med 2015;29:177–81. 10.1177/0269216314557346 [DOI] [PubMed] [Google Scholar]
- 174.Spillane D, Courtenay M, Chater A, et al. Factors influencing the prescribing behaviour of independent prescriber optometrists: a qualitative study using the theoretical domains framework. Ophthalmic Physiol Opt 2021;41:301-315. 10.1111/opo.12782 [DOI] [PubMed] [Google Scholar]
- 175.Stenner K, van Even S, Collen A. Early adopters of paramedic prescribing: a qualitative study. Br Paramed J 2021;6:30–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. CoP. Improving patients' access to medicines: a guide to implementing Paramedic prescribing within the NHS in the UK. Bridgewater, UK: College of Paramedics, 2018. [Google Scholar]
- 177.Eaton G, Wong G, Williams V, et al. Contribution of paramedics in primary and urgent care: a systematic review. Br J Gen Pract 2020;70:e421. 10.3399/bjgp20X709877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wagstaff B, Mistry V. The integration of paramedics into primary care. Br J Gen Pract 2020;70:123. 10.3399/bjgp20X708545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Dixon M. The developing role of the paramedic prescriber. J Prescr Pract 2020;2:98–101. 10.12968/jprp.2020.2.2.98 [DOI] [Google Scholar]
- 180.Regmi K, Mudyarabikwa O. A systematic review of the factors - barriers and enablers - affecting the implementation of clinical commissioning policy to reduce health inequalities in the National Health Service (NHS), UK. Public Health 2020;186:271–82. 10.1016/j.puhe.2020.07.027 [DOI] [PubMed] [Google Scholar]
- 181.Marshall M, Holti R, Hartley J, et al. GP leadership in clinical commissioning groups: a qualitative multi-case study approach across England. Br J Gen Pract 2018;68:e427. 10.3399/bjgp18X696197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Peckham S, Falconer J, Gillam S. The organisation and delivery of health improvement in general practice and primary care: a scoping study. health services and delivery research Southampton (UK). NIHR Journals Library, 2015. [PubMed] [Google Scholar]
- 183.Smith JA, Parkinson S, Harshfield A. Early evidence of the development of primary care networks in England: a rapid evaluation study. NIHR Health Services and Delivery Research Topic Report: Southampton, 2020. [PubMed] [Google Scholar]
- 184.Bunce AE, Gruß I, Davis JV, et al. Lessons learned about the effective operationalization of champions as an implementation strategy: results from a qualitative process evaluation of a pragmatic trial. Implement Sci 2020;15:87. 10.1186/s13012-020-01048-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Miech EJ, Rattray NA, Flanagan ME, et al. Inside help: an integrative review of champions in healthcare-related implementation. SAGE Open Med 2018;6:2050312118773261. 10.1177/2050312118773261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the expert recommendations for implementing change (ERIC) project. Implement Sci 2015;10:21. 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bryce C, Russell R, Dale J. Learning from the transfer of a fellowship programme to support primary care workforce needs in the UK: a qualitative study. BMJ Open 2019;9:e023384. 10.1136/bmjopen-2018-023384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.O'Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open 2019;9:e029954. 10.1136/bmjopen-2019-029954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.. NVivo qualitative data analysis software. Version 12. [program]. 2018.
- 190.Evans C, Tweheyo R, McGarry J, et al. Seeking culturally safe care: a qualitative systematic review of the healthcare experiences of women and girls who have undergone female genital mutilation/cutting. BMJ Open 2019;9:e027452. 10.1136/bmjopen-2018-027452 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-052227supp001.pdf (33.7KB, pdf)
bmjopen-2021-052227supp002.pdf (41.4KB, pdf)
bmjopen-2021-052227supp003.pdf (151.6KB, pdf)
Data Availability Statement
No data are available. No additional data are available.