Abstract
Shifts in activity patterns during the COVID-19 pandemic might have impacted the benefits of outdoor activities for mental health. By leveraging an existing mobile application, we collected self-reported data on daily outdoor activities, emotional well-being, and the influence of COVID-19 on participant’s outdoor activity levels during April–July 2020. Individuals reporting outdoor activities, in greenspaces or in their residence, had higher well-being scores and this effect increased with age. Self-reported impacts of COVID-19 on emotional well-being were associated with lower well-being scores. This work suggests that outdoor activities may have improved mental health during the COVID-19 pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10393-022-01598-4.
Keyword: Mental health, COVID-19, Outdoor activities, Well-being
Short Communication
Significant impacts of the COVID-19 pandemic on physical and mental health necessitate the identification of resilience strategies (Galea et al. 2020; Xiong et al. 2020; Panchal et al. 2021). Strong evidence supports a relationship between time spent in natural environments and an improved sense of well-being, including recovery from stress and mental fatigue (Park et al. 2010; Pearson and Craig 2014; White et al. 2016, 2019; Frumkin et al. 2017). Thus, evaluating the potential links between outdoor activities and emotional well-being during the COVID-19 pandemic can shed light on the role of outdoor recreation on improving well-being during crises (Jackson et al. 2021; Pouso et al. 2021; Larson et al. 2022).
In this study, we examine the association between emotional well-being and outdoor activity levels from April through July 2020, by leveraging an existing mobile application designed to study human outdoor activity patterns and the association with tick exposure (The Tick App) (Fernandez et al. 2019). We collected information on self-reported emotional well-being and the impact of COVID-19 among users from the Northeast and Midwest USA, through daily surveys (Fernandez et al. 2021). Questions included how participants felt, using a 10-point well-being score (WBS), how much COVID-19 influenced their responses (five-point Likert scale “A lot” to “Not at all”), and if they did any outdoor activities. The WBS was derived from a survey question “how did you feel today?” with a slider that went from 1 = “not feeling well at all (depressed or anxious)” to 10 = “I’m feeling great (calm, happy, and relaxed).” Emotional well-being refers to “the emotional quality of an individual's everyday experience—the frequency and intensity of experiences of joy, fascination, anxiety, sadness, anger, and affection that make one's life pleasant or unpleasant” (Kahneman and Deaton 2010). Since participants were asked to complete daily surveys for at least a week during the study period, emotional well-being was assessed with a single item to avoid participant fatigue. Single-item measures of psychological health have been found to be correlated with multi-item measures (Ahmad et al. 2014).
A binomial regression GLMM model with logit link function and user identity as a random variable was used to examine the association between the WBS and outdoor activities, self-reported COVID-19 impact on their emotional well-being (Fernandez et al. 2021), and demographic variables. We included Shelter in Place Index as a proxy for mobility restrictions (SafeGraph 2020), the number of COVID-19 cases per 100,000 population in the county of residence and nationwide (Center for Disease Control 2020), and urbanicity levels (National Center for Health Statistics 2019) as confounders.
The well-being score is a discrete numeric variable bounded between 0 and 10; thus, the distribution is not appropriately fitted by a Gaussian distribution (which can include values beyond both the lower and upper limits) nor a Poisson distribution (which is bounded at 0 but has no upper limit). Instead, we used a binomial model to account for the upper and lower bounds of the WBS (Liang et al. 2014). The response variable is not a binary variable, but instead consisted of a vector of “successes” and “failures,” such that each observation was coded as a two-dimensional vector ([WBS], [upper boundary for WBS]–[WBS]), where 10 is the upper boundary for WBS. This way, we account for the bounded distribution of the variable between 0 and 1. The estimated coefficients refer to a one-point increase in WBS. Age was rescaled to estimate the coefficients per 5 years. We compared two models including the number of COVID-19 cases per 100 k at the national and at the county level using the Akaike information criterion (AIC). The adjusted odds ratios were calculated for all independent factors. The final model evaluated was:
Y (WBS, 10-WBS) ~ β0 + β1*COVID impact on emotional well-being + β2*Doing an outdoor activity on the same day + β3* Shelter in Place Index + β4* Number of COVID-19 cases per 100k (nationwide OR local) + β5* Urbanicity + β6*gender + β7*age (5 year bins) + (1|participant ID) + ε.
From April 23 through July 31, 2020, we received 5155 reports of WBS by 1134 participants. The median age of participants was 51 years (IQR = 26, range = 18–86) (Supp. Figure 1); 58.9% were women, 40.2% were men, and 0.9% identified as other gender identity or chose not to identify themselves. Participants were equally distributed along an urbanization gradient: 32.5% lived in rural counties, 37.2% lived in small and medium metropolitan areas, and 30.3% lived in large metropolitan areas. The WBS had a median score of 8 (IQR = 7–9), but the broad range of responses indicated heterogeneities in the responses (Fig. 1). Higher well-being scores were reported by males and increased with age (Table 1). At least one-third of the responses to the daily surveys indicated that COVID-19 affected emotional well-being “Somewhat” or “A lot” which was associated with a lower WBS (Table 1). By contrast, doing any type of outdoor activity was significantly and positively associated with a higher WBS and this relationship was modified by age (Table 1, Fig. 2). The magnitude of association between outdoor activities and well-being was greater in older respondents (ORinteraction[Age*Outdoor activity] = 1.03 CI = 1.01–1.06, P = 0.03). No other interactions were significant.
Figure 1.
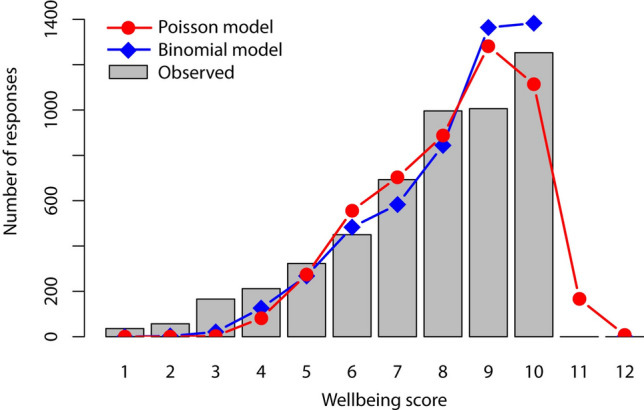
Distribution of the emotional well-being scores and predicted values for the GLMM binomial model and GLMM Poisson model.
Table 1.
GLMM for COVID-19 impact on emotional well-being score. A binomial regression GLMM with logit link function and user identity as a random variable was used to estimate the odds ratios for all independent variables.
| Variables | Odds ratio | 95% CI | P-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Intercept | 2.03 | 1.50 | 2.52 | < .001* |
| COVID-19 impact on emotional well-being | ||||
| Neutral | 1 | |||
| Not at all | 1.45 | 1.29 | 1.62 | < .001* |
| A little | 0.89 | 0.80 | 0.99 | 0.04* |
| Somewhat | 0.61 | 0.55 | 0.67 | < .001* |
| A lot | 0.34 | 0.30 | 0.38 | < .001* |
| Shelter in place index | 0.94 | 0.86 | 1.02 | .12 |
| Number of COVID-19 cases per 100 k nationwide | 99.34E-1 | 98.74E-1 | 99.95E-2 | .03* |
| Did any outdoor activities that day? | ||||
| No | 1 | |||
| Yes | 1.24 | 1.15 | 1.34 | < .001* |
| Urbanicity | ||||
| Lives in a rural county | 1 | |||
| Lives in a small or medium metro area | 0.99 | 0.84 | 1.18 | .93 |
| Lives in a large metro area | 1.10 | 0.92 | 1.18 | .29 |
| Gender | ||||
| Female | 1 | |||
| Male | 1.39 | 1.20 | 1.61 | < .001* |
| Other/prefer not to say | 2.64 | 1.17 | 5.91 | .02* |
| Age | 1.08 | 1.06 | 1.12 | < .001* |
*P-value < 0.05. R2 (marginal) = 0.21 and R2 (conditional) = 0.80 were estimated using the r.squaredGLMM function from MuMIn package
Figure 2.
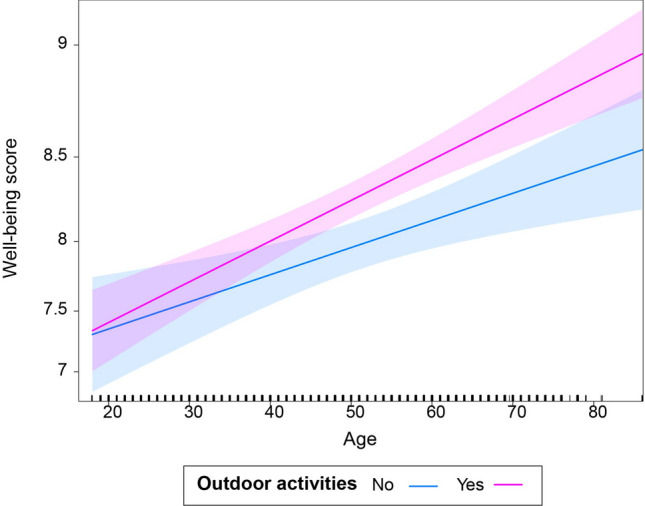
Effect of outdoor activities and age on participant’s daily emotional well-being. The mean well-being score predicted by the model is shown by age and stratified by reporting doing an outdoor activity on the same day for all participants.
The final GLMM model (Table 1) was significantly different from the null model (log-likelihood ratio test (12), P < 0.001; AICnull = 16,755), and model diagnosis did not detect significant issues with model assumptions and multicollinearity (Supp. Figure 2). We also evaluated a Poisson GLMM (right-truncated Conway–Maxwell–Poisson for underdispersed data) the Poisson model underperformed compared with a binomial model because it failed to limit the results to 10 (Fig. 1). The GLMM, including the rate of COVID-19 cases nationwide, had a better fit (AIC = 16,055) than the GLMM model including the number of cases per county the respondent resided in (AIC = 16,059). Thus, the final model retained the nationwide COVID-19 cases as a confounder.
Our work contributes to a growing body of literature that supports the benefit of engagement with the outdoors to cope with stress and anxiety. Herein, we examined repeated measures of emotional well-being and the association with outdoor activities during the pandemic in the general population in the USA, while previous studies have focused on university students (Jackson et al. 2021; Larson et al. 2022) or were global (Pouso et al. 2021). We found that both the self-reported impact of COVID-19 and the nationwide COVID-19 incidence were negatively associated with the WBS, confirming that the COVID-19 pandemic was a major stressor on the emotional well-being of participants. The hypothesized role of outdoor activities as a coping strategy was supported by its positive association with WBS. The underlying mechanisms linking outdoor activities to increased well-being can be related to increased contact with nature but can also have synergistic effects by reducing sedentary behaviors and increasing physical well-being (Browning et al. 2021; Larson et al. 2022).
The emotional disproportionate burden of COVID-19 on women compared with men has been widely reported, and it is also represented here (Guadagni et al. 2020; Connor et al. 2020; Zamarro and Prados 2021). Although COVID-19 disproportionately impacts the physical health of older adults, in our study, the WBS increased with age. This finding is in agreement with relative low reporting rates of anxiety and depression among older adults amid the pandemic (Koma et al. 2020). By contrast, studies focusing on university students found widespread emotional distress in this population (Huckins et al. 2020; Browning et al. 2021). Lower emotional well-being in younger adults and women, in particular, could be associated with job and childcare loss, remote learning, and social isolation, which affected this age group disproportionally (Koma et al. 2020; Browning et al. 2021). The main challenges faced by older adults during the pandemic consisted of mitigating risk by physical distancing while avoiding social isolation (Koma et al. 2020). In this context, it is not surprising that while our results indicate the importance of outdoor activity on the emotional well-being for all ages and genders, outdoor activities had a higher impact on the emotional well-being of older individuals.
Finally, since these data were collected opportunistically in the context of a tick-borne disease study, it is critical to examine outdoor activity through a multi-hazard lens. Outdoor activity could lead to increased exposure to other hazards, including ticks and tick-borne pathogens, potentially offsetting some of the benefits of accessing parks and natural areas (Fernandez et al. 2021). However, when we added the variable “finding a tick” to the final model (post hoc analysis), we found no association with the WBS. Lastly, it is important to note that individuals who use The Tick App are more likely to be “outdoorsy” (Fernandez et al. 2019); therefore, the impact on their mental well-being may be higher than other individuals who do not already have a propensity for outdoor activities. Further studies that examine a broader cross section of the population would better define the potential impact of outdoor activity as a resilience strategy during events like the COVID-19 pandemic.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This publication was supported by the Cooperative Agreements Number U01CK000509-01 and U01CK000505, funded by the Centers for Disease Control and Prevention, and the National Science Foundation's Dynamics of Integrated Socio-Environmental Systems (CNH2) program (Award #1924061). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention, the Department of Health and Human Services, or the National Science Foundation.
We thank all participants for taking time to share their experiences, and we thank those who promoted The Tick App. We thank the University of Wisconsin Center for Health Enhancement System Services for continued support of The Tick App and the students, Midwest Center of Excellence for Vector-borne Disease summer fellows, and colleagues, Megan Porter and Sandra Zapata for Tick App communications.
References
- Ahmad F, Jhajj AK, Stewart DE, Burghardt M, Bierman AS. Single item measures of self-rated mental health: a scoping review. BMC Health Serv Res. 2014;14:398. doi: 10.1186/1472-6963-14-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning MHEM, Larson LR, Sharaievska I, Rigolon A, McAnirlin O, Mullenbach L, Cloutier S, Vu TM, Thomsen J, Reigner N, Metcalf EC, D’Antonio A, Helbich M, Bratman GN, Alvarez HO. Psychological impacts from COVID-19 among university students: risk factors across seven states in the United States. PLOS ONE. 2021;16:e0245327. doi: 10.1371/journal.pone.0245327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control (2020) national environmental public health tracking network query tool. https://ephtracking.cdc.gov/DataExplorer/. Accessed 28 Dec 2020
- Connor J, Madhavan S, Mokashi M, Amanuel H, Johnson NR, Pace LE, Bartz D. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: a review. Social Science & Medicine. 2020;266:113364. doi: 10.1016/j.socscimed.2020.113364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez MP, Bron GM, Kache PA, Larson SR, Maus A, Gustafson D, Jr, Tsao JI, Bartholomay LC, Paskewitz SM, Diuk-Wasser MA. Usability and feasibility of a smartphone app to assess human behavioral factors associated with tick exposure (The Tick App): quantitative and qualitative study. J Med Internet Res. 2019;7:e14769. doi: 10.2196/14769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez MP, Bron GM, Kache PA, Tsao JI, Bartholomay LC, Ernst KC, Hayden MH, Berry K, Diuk-Wasser MA (2021) Shifts in outdoor activity patterns in the time of COVID-19 and its implications for exposure to vector-borne diseases in the United States. Research Square 10.21203/rs.3.rs-502309/v1.
- Frumkin H, Bratman GN, Breslow SJ, Cochran B, Kahn PH, Lawler JJ, Levin PS, Tandon PS, Varanasi U, Wolf KL, Wood SA. Nature contact and human health: a research agenda. Environ Health Perspect. 2017;125:075001. doi: 10.1289/EHP1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Merchant RM, Lurie N. The Mental Health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Guadagni V, Umilta A, Iaria G. Sleep quality, empathy, and mood during the isolation period of the COVID-19 pandemic in the canadian population: females and women suffered the most. Front Glob Womens Health. 2020 doi: 10.3389/fgwh.2020.585938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huckins JF, daSilva AW, Wang W, Hedlund E, Rogers C, Nepal SK, Wu J, Obuchi M, Murphy EI, Meyer ML, Wagner DD, Holtzheimer PE, Campbell AT. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. Journal of Medical Internet Research. 2020;22:e20185. doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SB, Stevenson KT, Larson LR, Peterson MN, Seekamp E. Outdoor activity participation improves adolescents’ mental health and well-being during the COVID-19 pandemic. International Journal of Environmental Research and Public Health. 2021;18:2506. doi: 10.3390/ijerph18052506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D, Deaton A. High income improves evaluation of life but not emotional well-being. Proceedings of the National Academy of Sciences. 2010;107:16489–16493. doi: 10.1073/pnas.1011492107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koma W, True S, Fuglesten Biniek J, Cubanski J, Orgera K, Garfield R (2020) One in four older adults report anxiety or depression amid the COVID-19 Pandemic. In: KFF. https://www.kff.org/medicare/issue-brief/one-in-four-older-adults-report-anxiety-or-depression-amid-the-covid-19-pandemic/. Accessed 6 May 2021
- Larson LR, Mullenbach LE, Browning MHEM, Rigolon A, Thomsen J, Metcalf EC, Reigner NP, Sharaievska I, McAnirlin O, D’Antonio A, Cloutier S, Helbich M, Labib SM. Greenspace and park use associated with less emotional distress among college students in the United States during the COVID-19 pandemic. Environ Res. 2022;204:112367. doi: 10.1016/j.envres.2021.112367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Y, Sun D, He C, Schootman M. Modeling bounded outcome scores using the binomial-logit-normal distribution. Chilean Journal of Statistics. 2014;5:3–14. [Google Scholar]
- National center for health statistics (2019) Urban rural classification scheme for counties. https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed 28 Dec 2020
- Panchal N, Kamal R, 2021 (2021) The Implications of COVID-19 for mental health and substance Use. In: KFF. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/. Accessed 6 May 2021
- Park BJ, Tsunetsugu Y, Kasetani T, Kagawa T, Miyazaki Y. The physiological effects of Shinrin-yoku (taking in the forest atmosphere or forest bathing): evidence from field experiments in 24 forests across Japan. Environ Health Prev Med. 2010;15:18–26. doi: 10.1007/s12199-009-0086-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson DG, Craig T. The great outdoors? Exploring the mental health benefits of natural environments. Front Psychol. 2014 doi: 10.3389/fpsyg.2014.01178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouso S, Borja Á, Fleming LE, Gómez-Baggethun E, White MP, Uyarra MC. Contact with blue-green spaces during the COVID-19 pandemic lockdown beneficial for mental health. Science of the Total Environment. 2021;756:143984. doi: 10.1016/j.scitotenv.2020.143984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SafeGraph (2020) Shelter in place index: the impact of coronavirus on human movement. In: SafeGraph. https://safegraph.com/data-examples/covid19-shelter-in-place/. Accessed 28 Dec 2020
- White MP, Elliott LR, Taylor T, Wheeler BW, Spencer A, Bone A, Depledge MH, Fleming LE. Recreational physical activity in natural environments and implications for health: A population based cross-sectional study in England. Prev Med. 2016;91:383–388. doi: 10.1016/j.ypmed.2016.08.023. [DOI] [PubMed] [Google Scholar]
- White MP, Alcock I, Grellier J, Wheeler BW, Hartig T, Warber SL, Bone A, Depledge MH, Fleming LE. Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Scientific Reports. 2019;9:7730. doi: 10.1038/s41598-019-44097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamarro G, Prados MJ. Gender differences in couples’ division of childcare, work and mental health during COVID-19. Rev Econ Household. 2021;19:11–40. doi: 10.1007/s11150-020-09534-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


