Abstract
This Review, in addressing the unacceptably high mortality of patients with liver disease admitted to acute hospitals, reinforces the need for integrated clinical services. The masterplan described is based on regional, geographically sited liver centres, each linked to four to six surrounding district general hospitals—a pattern of care similar to that successfully introduced for stroke services. The plan includes the establishment of a lead and deputy lead clinician in each acute hospital, preferably a hepatologist or gastroenterologist with a special interest in liver disease, who will have prime responsibility for organising the care of admitted patients with liver disease on a 24/7 basis. Essential for the plan is greater access to intensive care units and high-dependency units, in line with the reconfiguration of emergency care due to the COVID-19 pandemic. This Review strongly recommends full implementation of alcohol care teams in hospitals and improved working links with acute medical services. We also endorse recommendations from paediatric liver services to improve overall survival figures by diagnosing biliary atresia earlier based on stool colour charts and better caring for patients with impaired cognitive ability and developmental mental health problems. Pilot studies of earlier diagnosis have shown encouraging progress, with 5–6% of previously undiagnosed cases of severe fibrosis or cirrhosis identified through use of a portable FibroScan in primary care. Similar approaches to the detection of early asymptomatic disease are described in accounts from the devolved nations, and the potential of digital technology in improving the value of clinical consultation and screening programmes in primary care is highlighted. The striking contribution of comorbidities, particularly obesity and diabetes (with excess alcohol consumption known to be a major factor in obesity), to mortality in COVID-19 reinforces the need for fiscal and other long delayed regulatory measures to reduce the prevalence of obesity. These measures include the food sugar levy and the introduction of the minimum unit price policy to reduce alcohol consumption. Improving public health, this Review emphasises, will not only mitigate the severity of further waves of COVID-19, but is crucial to reducing the unacceptable burden from liver disease in the UK.
Introduction
The remit of The Lancet, following its report in 2019,1 was to address the high mortality figures for ill patients with liver disease admitted to acute hospitals, figures 7–8 times higher than those for stroke and myocardial infarction. The Commission was also asked to examine the earlier detection of liver disease through screening of individuals in primary and community care at high risk. The importance of comorbidities, particularly obesity and diabetes, in fatal cases of COVID-19 demonstrates the need to improve public health before further waves of infection and to reduce the current burden of liver disease. The UK Government's new enthusiasm to actively tackle obesity gives us encouragement that effective measures endorsed by the Commission might be finally adopted.
Any plan for hospital services must consider the large number of unfilled hepatology consultant posts and the probable reconfigurations of acute hospital services following the COVID-19 pandemic, including the increased intensive care capacity left in place for potential COVID-19 outbreaks. We must build on the success of hospital alcohol care teams, supported in the UK Government's long-term plan for the National Health Service (NHS), to improve the care of patients with alcohol-related liver disease and integrate these teams with community care to reduce readmissions.
Earlier detection of liver disease must include an effective alcohol risk assessment in primary care—a legal duty of local authorities since 2013.2 However, an analysis of patients attending NHS Health Check appointments showed that a lower proportion of people recalled advice about safe alcohol consumption compared with other elements of the Health Check (eg, diet, physical activity, blood pressure, cholesterol, smoking, and weight management).3 Earlier detection plans must embrace the non-invasive technique of transient elastography (FibroScan) and start to use new digital technology in consultations and data handling. Experience and progress with liver plans must be shared between UK nations.
Comorbidity and COVID-19 and the improvement of population health
Most deaths due to COVID-19 in patients younger than 65 years occur in those with underlying diseases such as obesity and diabetes.4 People with obesity are 40% more likely to die or deteriorate rapidly when admitted to hospital with COVID-19.5, 6 The results of a nationwide analysis in England showed that type 1 and type 2 diabetes were both independently associated with a significant increase in odds of in-hospital death with COVID-19.7 A report from the Intensive Care National Audit and Research Centre that used data from March 1 to June 11, 2020, showed that 7·8% of critically ill patients with confirmed COVID-19 in intensive care units (ICUs) were severely obese (ie, body-mass index [BMI] ≥40 kg/m2) compared with 2·9% of the general population (after adjusting for age and sex).8 This disparity was also seen when looking at different ethnicities separately.8 An early study from Beijing, China, reported that progression to severe disease was more probable in those with underlying non-alcoholic fatty liver disease than in those without.9 Viral shedding was also prolonged in these individuals, making them infectious for longer.9 More data from China indicate that the severity of COVID-19 increases with a BMI of more than 23 kg/m2.10 The metabolic consequences of weight gain affect ethnic minorities at a lower BMI.11
UK data are emerging of the hazards of liver disease in COVID-19. Liver disease was identified as an independent risk factor for COVID-19 mortality in a study of more than 17 million adult NHS patients (hazard ratio 1·75 [95% CI 1·51–2·03], including adjustments for age, gender, and ethnicity).12 Moreover, moderate and severe liver disease has emerged as a comorbidity, along with cardiorespiratory disease and diabetes, for ICU admission and increased risk of mortality.8, 13 Systematic reviews have also shown that patients with severe COVID-19 have higher rates of liver injury (odds ratio 2·20 [95% CI 1·60–3·02]; p<0·00001) than do those with non-severe COVID-19.14 Together, these findings strongly reinforce the need to tackle the prevalence of lifestyle risk factors.1, 15 Obesity and alcohol consumption are substantial risk factors for many common cancers, including breast and colon, and age-related complications, including strokes, cardiac events, and dementia. Enhancing population health should increase societal resilience against future waves of COVID-19.
To tackle obesity, changes to urban infrastructure are needed to encourage both walking and cycling, the benefits of physical activity adding to those of healthier diets and calorie restriction. Proposals in the Government's child obesity plan,16 most of which have been stalled at the consultation stage, need implementation, and restrictions on the promotion and advertising of unhealthy foods in children's media need to be extended to adult media. A tax on dietary sugar and saturated fat is needed to encourage reformulation of products by industry. Rates of bariatric surgery are lower in the UK than in other countries like France and Italy, where the prevalence of obesity is lower.17 Once elective surgeries resume, catching up with the backlog of procedures is essential and will benefit those with severe obesity the most.18 Facilities in the UK to help patients with weight problems are inadequate and the uptake of effective calorie-restricted diets is low.19
To combat excess alcohol consumption, a minimum unit price policy needs to be implemented in England. In Scotland, per adult off-sales of alcohol have decreased by 4–5% since the introduction of a minimum unit price, and Australian data provide further support to this tactic.20, 21 A study of 16 interventions to tackle obesity in Australia showed that increasing the price of alcohol through tax changes was the most cost-effective approach and produced the largest health gains.22 In the Northern Territory of Australia, a minimum unit price of AU$1·30 per standard drink (10 g) was introduced in October, 2018, as part of measures, which also included a register of those banned from purchasing takeaway alcohol, to reduce alcohol-related harm to heavy drinkers while minimising the impact on moderate drinkers. After 1 year, preliminary findings were of a sharp decline in harms associated with alcohol-related violence and considerable reductions in hospital admissions and ambulance attendances related to alcohol.20 In the Northwest Territories of Canada, large, coloured, pictorial labels with cancer warnings were introduced in 2017 and reduced sales of alcohol by around 7%, suggestive of behavioural changes and improved risk awareness.23
The Independent Commission on Alcohol Harm set up by the Alcohol Health Alliance have produced a report24 on the extensive damage alcohol can cause, not just to dependent people but also to their partners, families, and communities. A supporting editorial in the BMJ detailed the risks of heavy drinking during lockdown and in the aftermath of financial stress and redundancies.25 The UK Government must commit to a strategy to mitigate the damage caused by alcohol and protect public health.
Masterplan for improving survival in acute hospitals
The chair of the 2013 National Confidential Enquiry into Patient Outcome and Death report, looking at those who died from alcohol-related liver disease, commented, “The first thing I found surprising was how many of these extremely ill people were admitted under doctors who claimed no specialist knowledge of their disease, and how many of them were not then seen by an appropriate specialist within a reasonable period”.26 The situation has not changed. In 2018–19, 3352 (24·2%) of 13 865 patients admitted to acute hospitals in England with severe liver disease died within 60 days, a rate largely unchanged from that in 2004–12.27 Longer survival continues to be associated with treatment in London, treatment in a transplant centre, and specialist gastroenterological, rather than generalist, care in other hospitals. Life expectancy for patients with severe liver disease is much reduced;26 in England and Wales in 2018, the mean ages at death from liver disease were 61 years for men and 63 years for women, whereas the mean ages at death for all causes were 80 years for men and 83 years for women.28, 29 Since 1970, population mortality for liver disease in people younger than 65 years has risen by almost 500% and, in 2018, liver disease was the leading cause of death for those aged 35–49 years, accounting for more than 10% of deaths.30
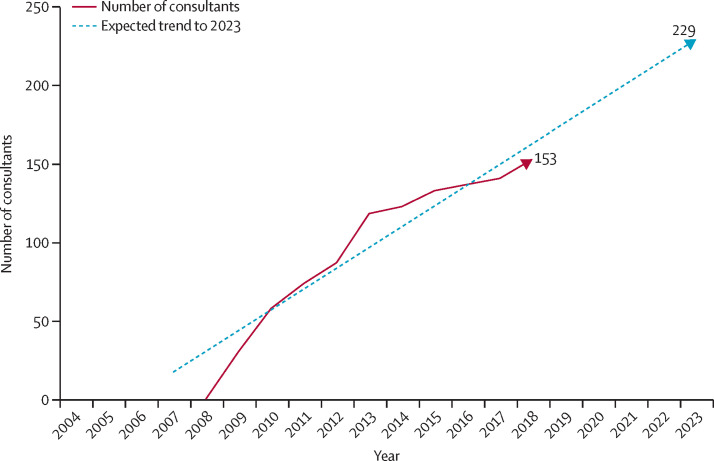
In 2018–19, only 8473 (61·1%) of 13 865 patients with liver disease admitted to an acute hospital in England were seen by a specialist in gastroenterology or hepatology. Although the numbers of consultants are increasing, the annual Royal College of Physicians census31 showed that in 2018 there were only 153 hepatologists, compared with 1417 gastroenterologists (Figure 1, Figure 2 ). Of the hepatologists, 64 (42%) were working in the seven transplant centres, 71 (46%) in 46 teaching hospitals, and 18 (12%) in the remaining 99 hospitals.
Figure 1.
Royal College of Physicians census of gastroenterology consultants
Data were provided by the Medical Workforce Unit of the Royal College of Physicians.32
Figure 2.
Royal College of Physicians census of hepatology consultants
Hepatology only became an option as a primary speciality in 2008. Data were provided by the Medical Workforce Unit of the Royal College of Physicians.32
The longer survival for patients managed by gastroenterologists or hepatologists exemplifies the need for more specialist care, which cannot be achieved by creating a specialist hepatology service in every hospital or by transferring every unwell patient to a specialist referral centre. Instead, the number of gastroenterologists with a special interest in liver disease, hepatologists, or both, especially in hospitals that currently have no input, has to be increased. However, during the past 5 years, 50% of advertised gastroenterology and hepatology consultant posts, particularly in district general hospitals, have been unfilled because of a paucity of trainees, and this shortfall needs to be considered in the changes to specialist medical training currently underway.31 The UK Government must prioritise the expansion of medical student numbers, but even then it will take around 15 years to see an increase in hepatologists. Currently, shortfalls are filled, where possible, with locums, who often command higher salaries, and so expanding training posts could result in savings. Including a commitment to acute medicine in job descriptions probably also hampers recruitment.
Until the numbers of liver-trained physicians are increased, the Commission recommends developing 30 specialist regional centres providing more complex assessment and treatment, each linked to and supporting four to six district hospitals. This process should be done according to geographical and local needs instead of the current haphazard distribution of services. Many specialist liver centres are appropriately located but some areas remain ill served and additional centres will be required. The minimum standard of care for every UK hospital that admits patients with liver conditions is a designated liver lead clinician to oversee the service and ensure that all admitted patients are seen by an appropriately trained specialist within 24 h of admission. The local liver lead should be provided with support, as set out in the Improving Quality in Liver Services accreditation scheme of the Royal College of Physicians,33 and would be responsible for creating appropriate care pathways and audits to reduce avoidable deaths. The lead would have a central role in developing community services for patients with liver disorders, including alcohol rehabilitation, community hepatitis C therapy, primary care diagnostics, and lifestyle support for those with non-alcoholic fatty liver disease. Establishing local liver leads could be done largely through the existing workforce. Survey data from the British Society of Gastroenterology and the British Association for the Study of the Liver identified a potential liver lead, defined as a gastroenterologist with an interest in hepatology, in 78% of NHS trusts (unpublished). Currently, 52 hospitals have registered for accreditation (including 28 district general hospitals) with the Improving Quality in Liver Services accreditation programme and this number needs to be substantially increased. This framework supports patient-centred reorganisation of services and workforce.
Regionally, standardised care bundles, as advocated for in previous Lancet Commission Reviews, have been shown to reduce variation between hospitals in mortality rates for patients admitted with alcohol-related liver disease.34 Medical directors should work alongside specialist commissioners to identify appropriate locations. Public Health England's Atlas of Variation in liver outcomes provides a framework to identify areas with the highest need.35 A regional liver centre might expect between eight and 12 referrals per week, a manageable number. Funding should be provided through the specialist commissioning service, which should also take responsibility for monitoring outcomes.
Until now, the challenge in implementing a district general hospital and regional centre masterplan has been the scarcity of bed capacity in high-dependency units and ICUs, but the increase mandated by the COVID-19 pandemic provides new opportunities. Additional ICU capacity is likely to be maintained to deal with future surges in COVID-19 cases and could be used for patients with severe liver disease in the periods in which the number of COVID-19 cases decline. Whether a referral originates from the emergency department, primary care, or another hospital department, a standardised protocol needs to be agreed for ill patients with liver disease requiring ICU admission. Those patients fulfilling the criteria will need to be promptly transferred to a regional centre (usually within 24 h). So-called smart ambulance technology, where patients are directed to the most appropriate hospital rather than the nearest one, has been effectively deployed for the management of strokes and myocardial ischaemia, for which outcomes have been greatly improved by specialist centres.36 Smart ambulance technology needs to be developed for liver disease to ensure that, wherever possible, patients are admitted immediately to regional units where specialist care can be delivered. Weekly multidisciplinary team meetings (eg, by video platform) should be part of establishing better communication and dialogue between district general hospitals and regional centres.
Improving hospital outcomes for patients with severe liver disease also requires new measures to circumvent early, unplanned readmissions of those with decompensated cirrhosis, which are commonly caused by recurrent ascites, hepatic encephalopathy, and alcohol dependency.37 A scheduled outpatient visit at day 7 post-discharge to optimise further outpatient care was shown to reduce hospital readmissions and emergency department attendances.38 The visit could also ensure that patients with cirrhosis or severe fibrosis are entered into a surveillance programme for the early detection of hepatocellular carcinoma, a complication with steadily rising mortality rates.
Improving outcomes of childhood liver disease
Late diagnosis of neonatal liver disease remains the main cause of chronic liver disease, necessitating paediatric liver transplantation.39 In Taiwan and Canada, the use of stool colour charts has effectively abolished late presentation of biliary atresia. This strategy has led to a considerable decrease in mortality and a reduction in the numbers and costs of early transplants by ensuring Kasai portoenterostomy takes place within 90 days of birth.40, 41, 42 The inclusion of a stool colour chart in the personal child health record (the red book that is given to parents) would alert health visitors to refer infants to have the concentration of conjugated bilirubin in their blood measured to confirm the diagnosis. The impact of liver disease on the developing brain in infants and children also needs to be addressed. Deficits in all areas of neurodevelopment, including cognitive, behavioural, and motor development, are described, and up to 42% of children after liver transplantation have additional educational needs.41, 42 Similar to guidance from the National Institute for Health and Care Excellence for children born preterm, those with liver disease require enhanced developmental surveillance, including formal assessments by a multidisciplinary team of health professionals at set times during infancy and in the long term.43 Collaboration with educational psychologists will be important in achieving the goal of meaningful survival: a state of physical, mental, and social wellbeing (not merely the absence of disease).1
The high prevalence of non-adherence to treatment—particularly following transplantation—has also highlighted the need for dedicated specialist care during the period of transition from paediatric to adult services; hence, each centre should appoint a dedicated young person's champion to oversee this care. One national, online survey found that only nine (50%) of 18 secondary and tertiary adult liver centres in the UK had a liver transition service.44 In these centres, young adults were more likely to have adequate knowledge about their condition, better adherence to treatment, and were less dependent on the paediatric provider than were young adults in centres without a transition service.
Alcohol care teams in the integration of alcohol and liver care
Around 30% of wholly alcohol-attributable hospital admissions are because of alcohol-related liver disease45 and alcohol care teams must have close links with acute liver services to ensure expert care of both alcohol addiction and liver disease. An estimated one in ten patients in acute hospitals are dependent on alcohol, and a further 20% are harmful drinkers (defined in the International Classification of Diseases, Diagnostic Criteria for Research, tenth revision).46 The key components of effective alcohol care teams include a clinician-led multidisciplinary team, a 7-day alcohol specialist nurse, integrated addiction and liaison psychiatry services, and medical consultants with expertise in liver disease.47 A quality and productivity case study describes how alcohol care teams have significantly reduced avoidable bed days and readmissions.48 Modelling suggests that an alcohol care team in a non-specialist acute hospital will save 254 000 bed days and 78 000 admissions annually by the third year of full optimisation, with a cost saving by the first year of £3·85 for each £1·00 invested.48 Despite this compelling evidence, full implementation of alcohol care teams has not been achieved. Since local authorities took over the commissioning of alcohol treatment services following the Health and Social Care Act of 2012 and because of the widespread cuts to public health grants to local authorities, funding responsibility remains unclear.
In 2019, the NHS' Long Term Plan for England49 aimed to expand the capacity of alcohol care teams and identified the health inequalities funding supplement of clinical commissioning groups as a legitimate source of funding.49 The following year, NHS England and NHS Improvement and Public Health England published a core service descriptor for alcohol care teams, with national funding planned for additional or improved services in areas with a high prevalence of alcohol dependence.50 Implementation of this programme remains a priority, particularly with the increase in high-risk drinking during the COVID-19 pandemic.51 There also needs to be a greater focus on improving the clinical competencies of staff working in alcohol care teams and hepatology, with appropriate training programmes.52
Alcohol assertive outreach treatment
People who frequently (on three or more occasions per year) attend hospitals for alcohol-related reasons place a disproportionate burden on the NHS, accounting for 59% of all alcohol-attributable admissions.53 Individuals who frequently attend hospitals for alcohol-related issues tend to be clustered in areas of high deprivation,54 often do not engage with community addiction services, and commonly have alcohol-related liver disease and untreated mental health comorbidities. Alcohol assertive outreach treatment (AAOT), involving assertive engagement and intensive case management, has been shown to reduce rehospitalisation by up to 50%.54 A 2017 national survey in England identified 37 (26%) of 141 acute NHS trusts providing one or more AAOT service elements.55 However, only six (16%) of these 37 services provided five or more components of effective AAOT. Having a multidisciplinary team was the least observed AAOT component across all trusts and the majority of services were not sufficiently resourced to provide comprehensive AAOT, which requires a high staff to patient ratio compared with conventional community alcohol treatment services. Implementation of AAOT has been hampered by the same policy and funding barriers identified for alcohol care teams.
A service evaluation of AAOT in south London, UK, in 2018 showed that, compared with standard care, AAOT saved £13 548 per patient in the first year of implementation in reduced inpatient bed days alone. Considering the cost of intervention (£2979 per patient), there was a net short-term cost saving of £10 569 per patient.54 If AAOT was rolled out nationally in England to the estimated 54 369 alcohol-related frequent hospital attendees, savings of about £575 million could be achieved within 1 year for an implementation cost of £161 million, a return of investment of £3·42 for each £1·00 spent.54
Specialist community alcohol treatment
The success of hospital-based alcohol care is crucially dependent on a continuing care pathway in the community. The 18% (£162 million) cut to funding for community addiction services run by local authorities in England has led to a 22% reduction in the number of people entering specialist alcohol treatment.1 Public Health England estimates that, in 2018–19, 82% of people with alcohol dependence in England did not access specialist alcohol treatment.56 The number of specialist NHS addiction consultants reduced by 39% between 2007 and 2017,57 with a 60% reduction in the number of specialist addiction trainees in the past 10 years.1 The table shows, for the four nations of the UK, the specialist alcohol treatment access ratios—the number of patients admitted to NHS hospitals for alcohol use disorder (F10 in the International Classification of Diseases, tenth revision) relative to the number of people accessing alcohol treatment in a given year. Between 2016–17 and 2018–19, the ratios remained relatively stable in Scotland and Wales, but increased in England and Northern Ireland (table). In 2018–19, England had approximately a third of the level of access in Scotland and Northern Ireland had roughly a fifth (table). This low access means that specialist alcohol treatment services based in the community in England and Northern Ireland are increasingly ill equipped to respond to the prevailing level of need in the community, including the aftercare needs of patients discharged from hospital with alcohol-related liver disease.
Table.
Specialist alcohol treatment access ratios across the UK, 2016–19
| Number accessing treatment for alcohol only*in 2018–19 | Number of F10 hospital admissions due to alcohol†in 2018–19 | Treatment access ratio in 2018–19 | Treatment access ratio in 2017–18 | Treatment access ratio in 2016–17 | |
|---|---|---|---|---|---|
| Scotland | 26 536 | 27 474 | 1·0 | 1·0 | 1·1 |
| Wales | 8344 | 12 266 | 1·5 | 1·5 | 1·5 |
| England | 75 555 | 220 731 | 2·9 | 2·6 | 2·4 |
| Northern Ireland | 2560 | 12 548 | 4·9 | 3·9 | 3·9 |
| UK | 112 995 | 273 019 | 2·4 | 2·2 | 2·1 |
The treatment access ratio is the number of F10 admissions to National Health Service hospitals divided by the number of people accessing specialist alcohol treatment. The lower the ratio the more favourable the level of access to treatment.
Excludes concurrent drug misuse as a reason for treatment.
Primary or secondary diagnosis of F10 in the International Classification of Diseases, tenth revision: mental and behavioural disorders due to use of alcohol. This measure is a proxy of the prevalence of alcohol dependence in the general population.58
Early detection of liver disease in primary care and groups at high risk
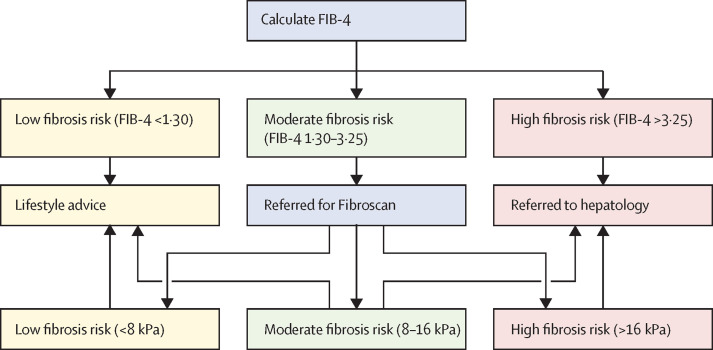
Early identification and management of liver disease is an essential prerequisite to improve outcomes and avoid complications in non-alcoholic fatty liver disease and alcohol-related liver disease. Primary care must have a central role in identifying patients at risk and in providing initial interventions, although mobilising primary care at the appropriate scale remains challenging given other perceived priorities. Nevertheless, the COVID-19 pandemic has had the unexpected effect of accelerating the use of digital solutions and pathways in primary care and the interface with hospital care. This digitisation has the potential to transform care by allowing consistent, early identification of people at risk and better management and follow-up of those with established disease. Examples of excellent practice already exist in pockets and need to be replicated widely. Evidence suggests that introducing a two-tier system to screen patients in primary care for liver fibrosis is the most cost-effective strategy.59 This approach comprises an initial simple screening test with a high negative predictive value (eg, the Fibrosis-4 Index for Liver Fibrosis [FIB-4] or the Non-Alcoholic Fatty Liver Disease Fibrosis Score) and then a second test reserved for detecting advanced fibrosis in those with a high or indeterminate score on the first test. Second-stage tests with suitable accuracy include the Enhanced Liver Fibrosis blood test, the acoustic radiation force impulse technique, and transient elastography (FibroScan).60
In 2014, an integrated primary–secondary care pathway was established in Portsmouth to assess and manage patients with non-alcoholic fatty liver disease across three clinical commissioning groups with a combined adult population of more than 650 000 people. If the Non-Alcoholic Fatty Liver Disease Fibrosis Score indicates a low risk, patients are issued with standardised advice regarding cardiovascular risk and weight management in primary care. Patients at high risk are referred to a consultant-led hepatology clinic for further management. Those with an indeterminate risk are seen in a nurse-led non-alcoholic fatty liver disease clinic and receive a FibroScan. Patients with a FibroScan reading less than 7·9 kPa are discharged to primary care and those with a FibroScan reading 7·9 kPa or more are referred for an assessment by a consultant. An evaluation of the first 904 patients seen in the nurse-led clinic showed that 790 patients met non-alcoholic fatty liver disease criteria, 519 of whom could be discharged to primary care on the first visit.61 Similarly, in a north London population, improvements in fibrosis detection and the quality of referrals were seen when a two-step algorithm (FIB-4 followed by the Enhanced Liver Fibrosis blood test) was used.59 The pathway led to an improvement in advanced fibrosis detection by four times and an 88% reduction in unnecessary referrals.59
A more portable, miniature FibroScan machine has improved access for general practitioner (GP) surgeries and community centres. An unpublished pilot study initiated in early 2019 in the Mid-Hampshire clinical commissioning group (figure 3 ), the first to make the FibroScan available for GPs to use in primary care, has allowed better detection of the high-risk category referred to hospital, and costs are £24 per community scan. The authors of this pilot study estimated that prevention of progression to cirrhosis and ultimately transplantation represents a saving of at least £12 000 per patient, with an ICU bed priced at £1328 per day and a general hospital bed at £195 per day at least. The Mid-Hampshire pilot of 1115 scans in 2019 cost £26 760, equivalent to 20 ICU days (Gordon H, unpublished).
Figure 3.
The Mid-Hampshire FibroScan 1-year pilot project
This pilot project was done at 18 participating general practitioner surgeries and assessed patients in high-risk groups (ie, those with diabetes, a high body-mass index, and high-risk alcohol drinking). FIB-4=Fibrosis-4 Index for Liver Fibrosis.
Most approaches to early diagnosis have used abnormal liver enzyme concentrations as the entry point to a diagnostic pathway, whereas the Scarred Liver Project in Nottinghamshire uses risk identification (eg, the presence of obesity, diabetes, or alcohol excess) as the primary trigger for investigation, which includes a FibroScan.62 In four Nottinghamshire clinical commissioning groups (with a total population of 700 000 people) during 12 months, 222 (23%) of 968 patients assessed had an elevated liver stiffness (≥8 kPa) and liver stiffness was indicative of advanced chronic liver disease in 60 (27%) of these 222 patients.62 If a traditional approach based on raised liver enzyme concentrations had been followed, approximately 39% of those with advanced liver disease (≥8 kPa) would have gone undetected.62
The use of electronic medical records in most NHS primary care contexts offers untapped opportunities for the identification of patients at risk. Algorithms in development could identify such cohorts directly from their electronic records. Once identified, these individuals can be directed for referral by automated digital referral processes. Clinical decision support can also be deployed within the electronic medical record to assist practitioners in their management of patients along appropriate pathways, further accelerating the referral process and improving outcomes. These opportunities to deploy a national coordinated response to prevention and intervention for those with risk factors for liver disease, integrated within the current mandated Health Check, should be a national priority.
Alcohol-related liver disease generates challenges around early detection because there is considerable under-reporting of alcohol use within medical records. This under-reporting might lessen the potential of algorithmic digital approaches in case finding, which is further compounded by the greater proportion of heavy drinkers who do not complete investigation or treatment pathways. However, there are other routes to detect individuals who drink more than the recommended upper limit of 14 units per week, such as through drink driving or domestic violence records. A more consistent, coordinated, multidisciplinary approach in the community and in hospitals is needed to increase the likelihood that patients and their families get the treatment they require and improve outcomes in this major cause of preventable death.
Hospital plans in Scotland, Wales, and Northern Ireland
Scotland
In the year following the introduction of a minimum unit price on May 1, 2018, the consumption of cider, previously the cheapest form of off-sales alcohol, fell by 18·6% in Scotland, but rose by 8·2% in England and Wales.63 In the financial year 2018–19, which included 10 months of the minimum unit price policy, the European age–sex standardised rates for hospital stays due to alcohol-related liver disease in Scotland fell from 139·9 in 2017–18 to 129·3, having risen or remained static for each of the previous 5 years.64 However, the longstanding and recurring staff shortages facing district general hospitals is of concern, and few have formal alcohol care teams.
As in other parts of the UK, there is increasing interest in the presymptomatic detection of liver disease, such as the opportunistic detection of abnormal liver function tests. So-called intelligent liver function tests, the automated analysis and interpretation of abnormal liver function tests in primary care, have been developed and piloted in Tayside,65 improve diagnosis, and are being extended to other parts of Scotland. Also, as many patients with even advanced liver disease have normal liver function tests,62 additional approaches to presymptomatic diagnosis based on the use of liver fibrosis markers (including the FIB-4 score) are being piloted. The potential target population in Scotland is the 40 000 drinkers in primary care at risk of liver disease that are identified annually by the national alcohol brief intervention programme.66 A pilot project in Edinburgh has shown that FibroScan use in an alcohol treatment setting is feasible and worthwhile.67
Wales
The Gwent Liver Unit (Newport) was commissioned to undertake a pilot study in which patients routinely had their liver enzyme concentrations measured and were referred for a FibroScan if their aspartate aminotransferase:alanine aminotransferase ratio was more than 1. In 2016–18, 18 000 people were risk-assessed and advanced fibrosis was identified in 192 individuals. This testing resulted in an 81% increase in the diagnosis of cirrhosis (Yeoman A, unpublished). This pilot has formed the backbone of a new Welsh liver blood test pathway that incorporates assertive fibrosis testing, the launch of which has been delayed due to the COVID-19 pandemic. A free, comprehensive, online education resource has been produced for all primary care clinicians in Wales to improve their understanding of liver blood tests, the rationale for fibrosis testing, and the management of risk factors. The Wales liver plan is also funding a liver disease support worker in each health board for 2 years to increase FibroScan capacity, take testing into the community, and, in future, extend testing to those with non-alcoholic fatty liver disease and alcohol misuse.
A national alcohol care team working group has been convened to engage with value-based health care in producing a benefits realisation report for the Chief Medical Officer of Wales. This report will complement the introduction of the minimum unit price policy in Wales, which came into force on March 2, 2020. Additionally, a Welsh Parliament cross-party working group has been convened to help to engage politicians in driving progress in the three key Lancet Commission priorities: hospital care, alcohol care teams, and early detection.
Northern Ireland
Consultant-led alcohol care teams are in place in three of the five trusts in Northern Ireland. The remaining two trusts have lost their alcohol specialist nurses because the Department of Health has implemented the Rapid Assessment, Interface and Discharge (RAID) model of liaison psychiatry services—many alcohol specialist nurses were not considered sufficiently trained in mental health for redeployment as RAID practitioners. However, the services are complementary and the aim to create alcohol care teams in all trusts remains.
Data from 2016–17 to 2018–19 show marked health inequalities in alcohol harm in Northern Ireland. In the 20% most deprived areas, the standardised alcohol-related admission rate was four times that in the 20% least deprived areas (1410 admissions per 100 000 population vs 353 admissions per 100 000 population).68 In addition, the alcohol-specific standardised mortality rate was four times higher in the 20% most deprived areas than in the 20% least deprived areas (31·7 deaths per 100 000 population vs 7·6 deaths per 100 000 population).68 These data strengthen the call for the introduction of a minimum unit price policy, which was delayed by the suspension of the devolved Northern Ireland Government until recently. Such a policy is now being considered again as part of a new substance misuse strategy.
Conclusions
Implementation of the main recommendations of this Review (panel ) would result in improved outcomes and survival rates for patients with both acute and chronic liver disease requiring hospital admission. Our recommended approach would provide greater expertise in all acute hospitals, with lead and deputy lead positions optimising 24/7 emergency cover, and will provide acute hospitals with active links to 30 specialist regional centres in England. As well as ensuring better cover for deprived areas, our recommendations represent an integrated, high-quality service that can work alongside the probable reconfiguration of hospitals, particularly high-dependency units and ICUs, as a consequence of the COVID-19 pandemic. Fully staffed alcohol care teams in every hospital that manage patients with liver disease will also help to care for the most common group of alcohol-attributable hospital admissions, namely individuals with alcohol-related liver disease. Close links with hospital liver services will be essential and there also needs to be joint follow-up arrangements between alcohol care teams and hepatologists for patients after they are discharged from hospital to reduce high readmission rates. The Commission strongly recommends that cuts in funding for addiction services should be reversed and AAOTs should be established to maintain long-term care outside of the hospital, resulting in substantial financial savings to the NHS and reducing pressure created by repeat attenders. The implementation of AAOTs on a national level would cost £161 million but save the NHS £575 million.52 These savings would complement those produced by fully establishing alcohol care teams in all hospitals, which would save an average of £448 000 for an implementation cost of £157 000 per hospital in the first year.48
Panel. Summary of main recommendations.
-
1
Establish a lead and deputy liver lead in each acute hospital who will be responsible for 24/7 care of acute admissions. Acute hospitals should be linked to one of 30 regional centres, which should have capacity in their high-dependency units and intensive care units and the facilities for specialist treatment.
-
2
Increase the number of training posts in hepatology. There is also an urgent need to reverse the fall in training posts in addiction psychiatry.
-
3
Extend 7-day alcohol care teams to all acute hospitals, with appropriate links to liver services.
-
4
Use assertive outreach services in the community to support frequent hospital attenders with alcohol use disorders. Reverse the decline of alcohol treatment services.
-
5
Expand primary care access to FibroScan to detect severe fibrosis or cirrhosis in asymptomatic individuals within high-risk groups. Assess liver health as part of the adult Health Check.
-
6
Prioritise public health by extending the levy on sugar content in soft drinks to foods, introduce meaningful alcohol labelling, and intensify government recommendations on physical activity to reduce levels of obesity and diabetes.
-
7
Facilitate translation of best practice across and between the health systems of the four nations.
-
8
Increase survival and improve outcomes for young people through the earlier diagnosis of biliary atresia by adopting stool colour charts as part of neonatal screening and enhancing neurocognitive developmental surveillance.
Technologies for the presymptomatic diagnosis of liver disease, such as transient elastography (FibroScan) and serum fibrosis markers, are now ready for wide implementation in primary and community care throughout the UK as part of clear and locally owned care pathways. These technologies should accompany an assessment of alcohol consumption, required by the adult Health Check in primary care, and other tools of proven benefit such as brief interventions, which are short, evidence-based, structured conversations about alcohol consumption. The potential value of digital technology in improving consultations in general practice, which has come to the fore during the COVID-19 pandemic and has increased the involvement of patients in their own care pathways, has also been detailed in this Review.
The importance of tackling alcohol, obesity, and diabetes in the UK is further highlighted by the striking effects of these comorbidities on mortality in COVID-19, especially given the possibility of further waves of infection. It is only by a comprehensive public health approach, including the long overlooked alcohol strategy, that the UK Government can turn the tide on deaths from liver disease, especially in younger people of working age (35–55 years). An extension of the levy on sugar content in drinks to foodstuffs should be part of the more active measures now being considered by the Government. The evidence, both from Scotland and outside the UK, of the effectiveness of a minimum unit price policy unassailably supports its urgent implementation, as well as the implementation of proper labelling for alcohol products that includes calorie content and health warnings. The need to address similar deficiencies to England in the plans for liver and addiction services in the devolved nations has been highlighted and our main recommendations (panel) include measures to improve long-term outcomes in children with liver disease.
Acknowledgments
Acknowledgments
We thank all those who attended meetings of the working groups of the Commission, including Mark Hudson (Freeman Hospital, Newcastle, UK); Camille Manceau and Mark Tyrell (Echosens, Paris, France); Jonny Greenberg, Riddhi Thakrar, and Thomas Stephens (Incisive Health, London, UK); John Wass (Department of Endocrinology, Churchill Hospital, Oxford, UK); Pamela Healy and Vanessa Hebditch (British Liver Trust, Bournemouth, UK); Jyotsna Vohra (Cancer Research UK, London, UK); Alison Taylor (Children's Liver Disease Foundation, Birmingham, UK); Ian Gee (Worcestershire Acute Hospital, Worcester, UK); Matthew Cramp (Plymouth University Peninsula Schools of Medicine and Dentistry, Plymouth, UK); Mead Mathews (St Mary's Surgery, Southampton, UK); Helen Jarvis (Newcastle University, Newcastle, UK, and The Royal College of General Practitioners, London, UK); Annie McCloud (Kent and Medway NHS and Social Care Partnership, Gillingham, UK); Martin McKee (London School of Hygiene & Tropical Medicine, London, UK); Joanne Morling (Nottingham University Hospitals NHS Trust and the University of Nottingham, Nottingham, UK); Michael Goldacre (Unit of Health-Care Epidemiology, Nuffield Department of Population Health, University of Oxford, Oxford, UK); Peter Rice (Scottish Health Action on Alcohol Problems, Edinburgh, UK); Robyn Burton (Public Health England, Leeds, UK); Guruprasad Aithal (Nottingham Digestive Diseases Centre and the National Institute for Health Research [NIHR] Nottingham Biomedical Research Centre at the Nottingham University Hospitals NHS Trust and the University of Nottingham, Nottingham, UK); and Tamara Pinedo (Royal College of Emergency Medicine, London, UK). We thank Norgine for their unrestricted grant to the Foundation for Liver Research (London, UK), which has enabled the Commission to work with Incisive Health (London, UK) in bringing the work of the Commission to the attention of the UK Government. CD was partly funded by the NIHR Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King's College London, London, UK, and by the NIHR Collaboration for Leadership in Applied Health Research and Care South London, now recommissioned as the NIHR Applied Research Collaboration South London, and receives funding from an NIHR senior investigator award. The views expressed in this Review are those of the authors and not necessarily those of the Medical Research Council, the NHS, the NIHR, or the UK Government's Department of Health and Social Care.
Contributors
RW was responsible for planning and providing content for the Summary, Introduction, and Conclusions, and the writing, editing, and overall direction of the initial paper submitted. ND was responsible for coordinating content and editing. HR, NB, RW, RP, RLB, and MA contributed to the section on COVID-19. GF, HG, RA, DT, MA, JF, RG, ZM, JW, SR, and JV contributed to the section on the hospital services masterplan. AD, DK, and MS contributed to the section on paediatric liver disease. CD, KM, NS, IG, KS, and CH contributed to the sections on alcohol services. CA, HG, SR, and RA contributed to the section on primary care. AY, NM, AM, and RM contributed to the sections on the devolved nations. GA was involved in planning and discussions, particuarly those on reconfiguring liver services, and editing the manuscript. PN contributed to writing and editing the overall manuscript. IG took over the role of corresponding author in August, 2020, following the untimely death of Roger Williams.
Declaration of interests
RLB declares personal fees from NovoNordisk, Pfizer, ViiV, International Medical Press, and Boehringer Ingelheim, and consultancy and grant support from NovoNordisk, outside the submitted work. MA declares grants from GSK/Takeda and personal fees from Intercept, outside the submitted work. GF declares consulting and speaker fees from AbbVie, Bristol Myers Squibb, Gilead, GSK, and MSD, outside the submitted work. RA declares personal fees from Norgine UK, Intercept Pharmaceuticals, and Novartis UK, outside the submitted work. All other authors declare no competing interests.
References
- 1.Williams R, Aithal G, Alexander GJ, et al. Unacceptable failures: the final report of the Lancet Commission into liver disease in the UK. Lancet. 2020;395:226–239. doi: 10.1016/S0140-6736(19)32908-3. [DOI] [PubMed] [Google Scholar]
- 2.UK Government The local authorities (public health functions and entry to premises by local Healthwatch representatives) regulations. 2013. http://www.legislation.gov.uk/uksi/2013/351/contents/made
- 3.Baker C, Loughren EA, Crone D, Kallfa' N. Patients' perceptions of a NHS Health Check in the primary care setting. Qual Prim Care. 2014;22:232–237. [PubMed] [Google Scholar]
- 4.Ioannidis JPA, Axfors C, Contonpoulos-Ioannides DG. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. 2020;188 doi: 10.1016/j.envres.2020.109890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barron E, Bakhai C, Kar P, et al. Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol. 2020;8:813–822. doi: 10.1016/S2213-8587(20)30272-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Intensive Care National Audit & Research Centre ICNARC report on COVID-19 in critical care. June 12, 2020. https://www.icnarc.org/DataServices/Attachments/Download/7e1a720c-dcac-ea11-9126-00505601089b
- 9.Ji D, Qin E, Xu J, et al. Non-alcoholic fatty liver diseases in patients with COVID-19: a retrospective study. J Hepatol. 2020;73:451–453. doi: 10.1016/j.jhep.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yan H, Valdes AM, Vijay A, et al. Role of drugs affecting the renin-angiotensin-aldosterone system on susceptibility and severity of COVID-19: a large case-control study from Zheijang province, China. Clin Pharmacol Ther. 2020;108:1185–1194. doi: 10.1002/cpt.2047. [DOI] [PubMed] [Google Scholar]
- 11.WHO expert consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 12.Williamson EJ, Walker AJ, Bhaskaran K. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Intensive Care National Audit & Research Centre COVID-19 report. June 12, 2020. https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports
- 14.Mao R, Qiu Y, He J-S, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667–678. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams R, Alexander G, Aspinall R, et al. Gathering momentum for the way ahead: fifth report of the Lancet Standing Commission on Liver Disease in the UK. Lancet. 2018;392:2398–2412. doi: 10.1016/S0140-6736(18)32561-3. [DOI] [PubMed] [Google Scholar]
- 16.UK Government Childhood obesity: a plan for action. Chapter 2. June 25, 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/718903/childhood-obesity-a-plan-for-action-chapter-2.pdf
- 17.Angrisani L, Santonicola A, Iovino P, Ramos A, Shikora S, Kow L. Bariatric surgery survey 2018: similarities and disparities among the 5 IFSO chapters. Obes Surg. 2021 doi: 10.1007/s11695-020-05207-7. published online Jan 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rubino F, Cohen RV, Mingrone G, et al. Bariatric and metabolic surgery during and after the COVID-19 pandemic: DSS recommendations for management of surgical candidates and postoperative patients and prioritisation of access to surgery. Lancet Diabetes Endocrinol. 2020;8:640–648. doi: 10.1016/S2213-8587(20)30157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hazlehurst JM, Logue J, Parretti HM, et al. Developing integrated clinical pathways for the management of clinically severe adult obesity: a critique of NHS England policy. Curr Obes Rep. 2020;9:530–543. doi: 10.1007/s13679-020-00416-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coomber K, Miller P, Taylor N, et al. Investigating the introduction of the alcohol minimum unit price in the Northern Territory. February, 2020. https://alcoholreform.nt.gov.au/__data/assets/pdf_file/0009/818280/investigating-introduction-of-alcohol-minimum-unit-price-nt-summary-report.pdf
- 21.Robinson M, Mackay D, Giles L, Lewsey J, Beeston C. Evaluating the impact of minimum unit pricing (MUP) on sales-based alcohol consumption in Scotland: controlled interrupted time series analyses. June, 2020. http://www.healthscotland.scot/media/3097/evaluating-the-impact-of-mup-on-sales-based-alcohol-consumption-in-scotland-controlled-interrupted-time-series-analyses.pdf
- 22.Ananthapavan J, Sacks G, Brown V, et al. Assessing cost-effectiveness of obesity prevention policies in Australia. 2018. https://secureservercdn.net/192.169.221.188/y97.516.myftpupload.com/wp-content/uploads/2018/12/ACE-Obesity-Report_Final.pdf [DOI] [PMC free article] [PubMed]
- 23.Zhao J, Stockwell T, Vallance K, Hobin E. The effects of alcohol warning labels on population alcohol consumption: an interrupted time series analysis of alcohol sales in Yukon, Canada. J Stud Alcohol Drugs. 2020;81:225–237. [PubMed] [Google Scholar]
- 24.Alcohol Health Alliance “It's everywhere”—alcohol's public face and privte harm. The report of the Commission on Alcohol Harm. https://ahauk.org/wp-content/uploads/2020/09/Its-Everywhere-Commission-on-Alcohol-Harm-final-report.pdf
- 25.Finlay I, Gilmore I. Covid-19 and alcohol—a dangerous cocktail. BMJ. 2020;369 doi: 10.1136/bmj.m1987. [DOI] [PubMed] [Google Scholar]
- 26.National Confidential Enquiry into Patient Outcome and Death Alcohol related liver disease: measuring the units. June 14, 2013. https://www.ncepod.org.uk/2013arld.html
- 27.Roberts SE, John A, Brown J, Napier DJ, Lyons RA, Williams JG. Early and late mortality following unscheduled admissions for severe liver disease across England and Wales. Aliment Pharmacol Ther. 2019;49:1334–1345. doi: 10.1111/apt.15232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Office for National Statistics National population projections, mortality assumptions: 2018-based. Oct 21, 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/methodologies/nationalpopulationprojectionsmortalityassumptions2018based
- 29.Office for National Statistics Deaths registered in England and Wales. July 1, 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathsregisteredinenglandandwalesseriesdrreferencetables
- 30.Public Health England Liver disease: applying all our health. https://www.gov.uk/government/publications/liver-disease-applying-all-our-health/liver-disease-applying-all-our-health
- 31.Royal College of Physicians Focus on physicians: 2018–19 census (UK consultants and higher specialty trainees) Oct 3, 2019. https://www.rcplondon.ac.uk/projects/outputs/focus-physicians-2018-19-census-uk-consultants-and-higher-specialty-trainees
- 32.Royal College of Physicians Census of consultant physicians and higher speciality trainees in the UK. https://www.rcplondon.ac.uk/projects/census-consultant-physicians-and-higher-specialty-trainees-uk
- 33.Royal College of Physicians RCP launches IQILS accreditation scheme. Oct 10, 2017. https://www.rcplondon.ac.uk/news/rcp-launches-iqils-accreditation-scheme
- 34.Kallis C, Dixon P, Silberberg B, et al. Reducing variation in hospital mortality for alcohol-related liver disease in North West England. Aliment Pharmacol Ther. 2020;52:182–195. doi: 10.1111/apt.15781. [DOI] [PubMed] [Google Scholar]
- 35.Public Health England Atlas of Variation. https://fingertips.phe.org.uk/profile/atlas-of-variation
- 36.NHS England Transforming urgent and emergency care services in England. Clinical models for ambulance services. November, 2015. https://www.nhs.uk/nhsengland/keogh-review/documents/uecr-ambulance-guidance-fv.pdf
- 37.Gaspar R, Rodrigues S, Silva M, et al. Predictive models of mortality and hospital readmission of patients with decompensated liver cirrhosis. Dig Liver Dis. 2019;51:1423–1429. doi: 10.1016/j.dld.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 38.Morales BP, Planas R, Bartoli R, et al. HEPACONTROL. A program that reduces early readmissions, mortality at 60 days, and healthcare costs in decompensated cirrhosis. Dig Liver Dis. 2018;50:76–83. doi: 10.1016/j.dld.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 39.Davenport M, Ong E, Sharif K, et al. Biliary atresia in England and Wales: results of centralization and new benchmark. J Pediatr Surg. 2011;46:1689–1694. doi: 10.1016/j.jpedsurg.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 40.Chen SM, Chang MH, Du JC, et al. Screening for biliary atresia by infant stool color card in Taiwan. Pediatrics. 2006;117:1147–1154. doi: 10.1542/peds.2005-1267. [DOI] [PubMed] [Google Scholar]
- 41.Rodijk LH, den Heijer AE, Hulscher JBF, Verkade HJ, de Kleine RHJ, Bruggink JLM. Neurodevelopmental outcomes in children with liver diseases: a systematic review. J Pediatr Gastroenterol Nutr. 2018;67:157–168. doi: 10.1097/MPG.0000000000001981. [DOI] [PubMed] [Google Scholar]
- 42.Talcott JB, Beath SV, Patel T, Griffiths G, Kelly DA. Long-term effects of cholestatic liver disease in childhood on neuropsychological outcomes and neurochemistry. J Pediatr Gastroenterol Nutr. 2019;69:145–151. doi: 10.1097/MPG.0000000000002380. [DOI] [PubMed] [Google Scholar]
- 43.Rennie J, Burman-Roy S, Murphy MS. Neonatal jaundice: summary of NICE guidance. BMJ. 2010;340 doi: 10.1136/bmj.c2409. [DOI] [PubMed] [Google Scholar]
- 44.Joshi D, Dyson J, Hudson M, Levitsky J, Heldman M, Samyn M. Paediatric to adult liver transition services: the state of play in the UK. Clin Med (Lond) 2019;19:425–426. doi: 10.7861/clinmed.2019-0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.National Health Service Digital Statistics on alcohol. 2020. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-alcohol
- 46.Roberts E, Morse R, Epstein S, Hotopf M, Leon D, Drummond C. The prevalence of wholly attributable alcohol conditions in the United Kingdom hospital system: a systematic review, meta-analysis and meta-regression. Addiction. 2019;114:1726–1737. doi: 10.1111/add.14642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moriarty KJ. Alcohol care teams: where are we now? Frontline Gastroenterol. 2020;11:293–302. doi: 10.1136/flgastro-2019-101241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.The British Society of Gastroenterology and the Royal Bolton Hospital NHS Foundation Trust Quality and productivity case study. March 2, 2016. https://www.nice.org.uk/savingsandproductivityandlocalpracticeresource?id=2603
- 49.National Health Service England Online version of the NHS Long Term Plan. Alcohol. 2019. https://www.longtermplan.nhs.uk/online-version/chapter-2-more-nhs-action-on-prevention-and-health-inequalities/alcohol/
- 50.Public Health England Alcohol care teams: core service descriptor. November, 2019. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/11/ACT-core-service-descriptor-051119.pdf
- 51.Jackson SE, Garnett C, Shahab L, Oldham M, Brown J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: an analysis of 2019–20 data. Addiction. 2020 doi: 10.1111/add.15295. published online October 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Phillips T, Porter A, Sinclair J. Clinical competencies for the care of hospitalized patients with alcohol use disorders. Alcohol Alcohol. 2020;55:395–400. doi: 10.1093/alcalc/agaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blackwood R, Lynskey M, Drummond C. Prevalence and patterns of hospital use for people with frequent alcohol-related hospital admissions, compared to non-alcohol and non-frequent admissions: a cohort study using routine administrative hospital data. Addiction. 2020 doi: 10.1111/add.15354. published online Nov 27. [DOI] [PubMed] [Google Scholar]
- 54.Drummond C, Wolstenholme A, Blackwood R, Kimergård A. Assertive outreach for high-need, high-cost alcohol-related frequent NHS hospital attenders: the value-based case for investment. 2018. http://www.clahrc-southlondon.nihr.ac.uk/files/Assertive%20outreach_May_2019.pdf
- 55.Fincham-Campbell S, Kimergård A, Wolstenholme A, et al. A national survey of assertive outreach treatment services for people who frequently attend hospital due to alcohol-related reasons in England. Alcohol Alcohol. 2018;53:277–281. doi: 10.1093/alcalc/agx095. [DOI] [PubMed] [Google Scholar]
- 56.Public Health England Adult substance misuse treatment statistics 2018 to 2019: report. Nov 7, 2019. https://www.gov.uk/government/publications/substance-misuse-treatment-for-adults-statistics-2018-to-2019/adult-substance-misuse-treatment-statistics-2018-to-2019-report
- 57.Royal College of Psychiatrists Training in addiction psychiatry: current status and future prospects. 2020. https://www.rcpsych.ac.uk/members/your-faculties/addictions-psychiatry/training-in-addiction-psychiatry-current-status-and-future-prospects
- 58.Roberts E, Clark G, Hotopf M, Drummond C. Estimating the prevalence of alcohol dependence in Europe using routine hospital discharge data: an ecological study. Alcohol Alcohol. 2020;55:96–103. doi: 10.1093/alcalc/agz079. [DOI] [PubMed] [Google Scholar]
- 59.Srivastava A, Jong S, Gola A, et al. Cost-comparison analysis of FIB-4, ELF and fibroscan in community pathways for non-alcoholic fatty liver disease. BMC Gastroenterol. 2019;19:122. doi: 10.1186/s12876-019-1039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.National Institute for Health and Care Excellence FibroScan for assessing liver fibrosis and cirrhosis in primary care. June 16, 2020. https://www.nice.org.uk/advice/mib216/chapter/Summary
- 61.Fowell AJ, Fancey K, Gamble K, et al. Evaluation of a primary to secondary care referral pathway and novel nurse-led one-stop clinic for patients with suspected non-alcoholic fatty liver disease. Frontline Gastroenterol. 2020 doi: 10.1136/flgastro-2019-101304. published online April 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chalmers J, Wilkes E, Harris R, et al. The development and implementation of a commissioned pathway for the identification and stratification of liver disease in the community. Frontline Gastroenterol. 2020;11:86–92. doi: 10.1136/flgastro-2019-101177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Giles L, Robinson M, Beeston C. Minimum unit pricing (MUP) for alcohol evaluation. Sales-based consumption: a descriptive analysis of one year post-MUP off-trade alcohol sales data. November, 2019. http://www.healthscotland.scot/media/2954/c-users-kims-desktop-sales-based-consumption-descriptive-analysis-of-one-year-post-mup-off-trade-alcohol-sales-data.pdf
- 64.Information Services Division Scotland Alcohol-related hospital statistics Scotland 2018/19. Nov 19, 2019. https://www.isdscotland.org/Health-Topics/Drugs-and-Alcohol-Misuse/Publications/2019-11-19/2019-11-19-ARHS-Report.pdf
- 65.Dillon JF, Miller MH, Robinson EM, et al. Intelligent liver function testing (iLFT): a trial of automated diagnosis and staging of liver disease in primary care. J Hepatol. 2019;71:699–706. doi: 10.1016/j.jhep.2019.05.033. [DOI] [PubMed] [Google Scholar]
- 66.Public Health Scotland Drugs and alcohol misuse. Alcohol-related hospital statistics. 2019. https://www.isdscotland.org/Health-Topics/Drugs-and-Alcohol-Misuse/Publications/2019-06-25/visualisation.asp
- 67.Matthews K, MacGilchrist A, Coulter-Smith M, Jones J, Cetnarskyj R. A nurse-led FibroScan outreach clinic encourages socially deprived heavy drinkers to engage with liver services. J Clin Nurs. 2019;28:650–662. doi: 10.1111/jocn.14660. [DOI] [PubMed] [Google Scholar]
- 68.Department of Health Northern Ireland Health inequalities annual report 2020. March 25, 2020. https://www.health-ni.gov.uk/publications/health-inequalities-annual-report-2020