Abstract
Background
COVID-19 restrictive measures have had a considerable impact on daily life routines, which may be especially challenging for families of children with autism. In pre-schoolers with autism, it is likely that the disruption of routines mainly impacts the presence of restrictive and repetitive behaviours (RRBs). Furthermore, influence of comorbid conditions, secondary behavioural difficulties and home environment characteristics on RRBs was explored.
Method
A cross-sectional online survey design was used to collect parent-report data on 254 children with autism (2.5–6 years) during lockdown in the early months of the pandemic. RRBs were assessed using the Repetitive Behaviour Scale-Revised (RBS-R).
Results
Parents reported a significant increase in stereotypic, self-injurious, compulsive and ritualistic behaviour, and restricted interests after implementation of COVID-19 restrictions. The presence of a co-occurring condition, such as language impairments or intellectual disability, was associated with more self-injurious and stereotypic behaviour. However, there was no effect of home environment on RRBs. Further, most children showed increases in internalising and/or externalising behaviour. Increased inattentive behaviour was associated with more ritualistic and stereotypic behaviour, and restricted interests. Decreases in hyperactivity were related to more restricted interests. Importantly, in a subset of children, parents reported less behavioural difficulties during the lockdown.
Conclusions
Findings highlight the importance of flexible implementation and continuity of care for pre-schoolers with autism and support for parents. Further follow-up of children with autism and RRBs, and co-occurring behavioural difficulties is needed and could enhance our understanding of the long-term effects associated with sudden restrictive measures to daily routines.
Keywords: COVID-19 pandemic, Autism, Pre-school children, Restricted and repetitive behaviours (RRBs)
COVID-19 pandemic; Autism; Pre-school children; Restricted and repetitive behaviours (RRBs).
1. Introduction
The coronavirus disease 2019 (COVID-19) was officially declared a global pandemic by the World Health Organization (WHO) on March 11, 2020 (WHO, 2020). Since then, many governments have rapidly imposed physical distancing restrictions including stay-at-home directives to contain the spread of the disease. For a lot of families, these restrictions have led to considerable disturbance to personal, educational and work routines, as well as disruptions in social connection. In particular, families with young children with autism are likely to find these sudden changes in daily routine challenging and stressful – especially in the context of school routine and therapy (Bentenuto et al., 2021; Kong, 2021). Autism is a common heterogeneous neurodevelopmental condition, characterised by difficulties in social communication and interaction and restricted and repetitive patterns of behaviour (Diagnostic and Statistical Manual of Mental Disorders 5th ed [DSM-5]; American Psychiatric Association [APA], 2013). - with a global prevalence under 1% (e.g., Elsabbagh et al., 2012), but estimates are higher in high-resource countries (for an overview see Lord et al., 2020). The sudden closure of schools, rehabilitation and therapy centres causing suspension of therapeutic activities along with other changes in daily life, may result in deteriorating autism characteristics and increasing behavioural difficulties. While little is known regarding the impact of COVID-19 restrictions on children with autism, the presence of behavioural manifestations – in particular, restricted and repetitive patterns of behaviour and interests - are likely to generate new challenges and increased levels of stress as a result of the restrictions.
Restricted and repetitive behaviours (RRBs) as described by DSM-5 can be subdivided into four subtypes: (a) stereotypic or repetitive motor movements, use of objects, or speech; (b) insistence on sameness, inflexible adherence to routines, or ritualized patterns of verbal or nonverbal behaviour; (c) highly restricted, fixated interests that are abnormal in intensity or focus; and (d) hyper- or hyporeactivity to sensory input or unusual interests in sensory aspects of the environment (APA, 2013). Next to the classification of RRBs outlined by DSM-5, a more empirically-driven framework classifies RRBs as “lower order” (including repetitive motor actions and movements such as hand-flapping or body rocking, and physical and/or sensory manipulation of objects) and “higher order” (characterised by rigid routines, resistance to change, insistence on sameness, and intense circumscribed interests) (Melo et al., 2020; Turner, 1999). Lower order behaviour is usually more common in younger children, especially those with co-occurring intellectual disability (ID) and/or language impairments, while higher order behaviour involves more advanced cognitive and language capacities and is more common in older children (Esbensen et al., 2009; Richler et al., 2010; Shuster et al., 2014; Szatmari et al., 2006). The expression of RRBs in autism is extremely heterogeneous and although some children with autism show certain RRBs at some point during their development, not all children will display them ubiquitously (Turner, 1999; Walker et al., 2004). In addition, RRBs are not unique to autism and may also be observed in other developmental and psychiatric conditions (de Vaan et al., 2020; Moss et al., 2013; Zandt et al., 2007) or in typical development when infants and toddlers are in the early process of developing coordinated voluntary movements (Honey et al., 2007; Leekam et al., 2007; MacDonald et al., 2007). However, in young children with autism these early repetitive motor movements may be more frequent, intense and persistent through childhood (Bodfish et al., 2000; Harrop et al., 2014; Leekam et al., 2011).
Although certain RRBs can be considered as unique features of autism and may have advantages in life (Bury et al., 2020; Russell et al., 2019), they are among the most stressful behaviours for parents of young children (Bishop et al., 2007) and are linked to less frequent and lower qualitative active participation in daily and family activities (Dickie et al., 2009; Hochhauser and Engel-Yeger, 2010), as well as to less adaptive behaviour (Goldman et al., 2009; Lane et al., 2010). Nonetheless, in comparison to the social communication and interaction-domain of autism, RRBs are under-studied and behavioural mechanisms underpinning their onset, manifestation, and development over time are less clear (Melo et al., 2020). Evidence from clinical studies indicates that key proximal triggers for RRBs are arousal and unstructured environments (Leekam et al., 2011) – two factors which can potentially be provoked by the sudden changes caused by the COVID-pandemic.
Furthermore, given the high prevalence rate (up to 90%) of co-occurring conditions (e.g., ID, language condition, Attention Deficit Hyperactivity Disorder (ADHD) and Developmental Coordination Disorder (DCD)) and co-occurring behavioural difficulties (e.g., eating or sleeping difficulties, high levels of anxiety or presence of aggressive and oppositional behaviour) in pre-schoolers with autism (APA, 2013; Salazar et al., 2015), it is likely that the manifestation of RRBs may, in part, be associated with the presence of such co-occurring difficulties. For instance, existing research frequently reports an association between increased levels of anxiety and higher frequency of RRBs in autistic children (Gotham et al., 2013; Sukhodolsky et al., 2008). Disruptions to daily routine could be a specific trigger for increased levels of anxiety and stress (Ozsivadjian et al., 2012), which over time, may increase frequency of RRBs (Lidstone et al., 2014; Rodgers et al., 2012). Similarly, increased levels of parent-reported infant sleep difficulties are linked to higher levels of RRBs, including ritualistic behaviour and insistence on sameness (Gabriels et al., 2005; Hundley et al., 2016; MacDuffie et al., 2020), as well as self-injurious and compulsive behaviour (Goldman et al., 2011). Other results showed correlations between increases in RRBs and hyperactivity, inattention and externalizing behaviours (Gabriels et al., 2005; Tsai et al., 2020). Therefore, given the associations between RRBs and co-occurring conditions and behavioural difficulties, it is likely that sudden changes to daily routines and habits as a consequence of the COVID-19-related restrictions may lead to an increase in these co-occurring behavioural difficulties.
Finally, given the stay-at-home directives, children spend an extensive amount of time at home. Hence, it is important to understand how aspects of the home environment may influence the manifestation of RRBs. In contrast to holiday periods in which school closures are expected and planned, the COVID-restrictions were applied suddenly; thereby limiting families in activities they could engage in outside their home, as well as organising care for their children. Previous studies examined the association between housing type and mental and emotional well-being in children with atypical development through parent-report. The results suggest that residents of a single-family detached house typically have better mental health compared to those living in multiple dwelling units (Evans et al., 2003; Nagib and Williams, 2017). Likewise, other housing characteristics such as larger unit size and more outdoor space, have been linked to higher quality of life outcomes in children with autism (Nagib and Williams, 2017).
Currently, the impact of the COVID-19 restrictions in pre-schoolers with autism is still poorly understood. Thus, given the existing reports documenting the impact RRBs and behavioural difficulties have on daily routines in pre-schoolers with autism and their parents, the main goal of this study was to investigate how parents report the impact of the sudden COVID-19 restrictions on RRBs and co-occurring behavioural difficulties during the early months of the pandemic.
First, we aimed to assess if parents reported more RRBs after the onset of the COVID-19 restrictions. As a result of sudden changes in routines leading to an unstructured environment, autistic children might engage in more ritualistic or insistence on sameness behaviour. Further, physical distancing restrictions may lead to a lack of environmental stimulation, and thus, to lower levels of arousal potentially triggering an increase in stereotypic and sensory stimulating behaviour (Leekam et al., 2011). In addition, given the link between COVID-19 restrictions and psychological stress in the general population (Cooke et al., 2020; Gonçalves et al., 2020; Smith et al., 2020), children with autism may similarly experience more distress, which could be related to an increase in co-occurring internalizing and/or externalizing behavioural difficulties (Gotham et al., 2013; Leekam et al., 2011).
Second, we aimed to explore the impact of co-occurring conditions and characteristics of the home environment on changes in RRBs due to COVID-19 restrictions. We hypothesized that, parents of children with co-occurring conditions, would report higher levels of RRBs (Bishop et al., 2006; Melo et al., 2020), compared to children without co-occurring conditions. Regarding the home environment, we explored if children who live in multiple dwelling units and do not have a private bedroom would exhibit increased levels of RRBs after onset of COVID-19 restrictions (Nagib and Williams, 2017).
Third, we also aimed to explore links between changes in RRBs and changes in co-occurring behavioural difficulties as a result of COVID-19 restrictions. More specifically, whether children who display increased levels of co-occurring behavioural difficulties also exhibit increased levels of RRBs after onset of COVID-19 restrictions (Gabriels et al., 2005; Lidstone et al., 2014).
2. Methods
2.1. Participants
A cross-sectional online survey design was adopted to assess the potential impact of the restrictions imposed by the government due to the COVID-19 pandemic on RRBs in children with autism. In total, 254 primary caregivers of pre-schoolers with a parent-reported diagnosis of autism, who were already attending pre-primary education (M age = 4.5 years, SD = 0.98, range = 2.5–6 years), completed the online survey around the time of the first lockdown phase in Flanders, Belgium. During this period, the government issued stay-at-home directives and working from home was compulsory for non-essential businesses. Schools and intervention/rehabilitation centres were closed.
The primary caregiver was defined as the person who was, at the time when the questionnaire was filled out (after onset of COVID-19 restrictions), taking most care of the child (or at least as much as the partner if present). On the question “How is your child's care divided after March 16th?”, 108 (42.5%) of the respondents indicated that they are responsible for the majority of care, 57 (22.4%) indicated that they are more responsible for the care of their children as compared to their partner and 89 (35%) indicated that they are equally responsible for the care. On the question “How is your child's care divided before March 16th?”, 95 (37.4%) of the respondents indicated that they were responsible for the majority of care, 77 (30.3%) indicated that they were more responsible, 75 (29.5%) indicated that they were equally responsible. Only 7 (2.8%) respondents indicated that they were less responsible for their children's care before COVID-19 restrictions than their partner.
Respondents could only start the survey after giving consent and data were collected anonymously. If respondents had more than one child who met inclusion criteria, they were asked to only report on the oldest pre-schooler with autism. Initially, 393 respondents filled out the survey of which 139 were excluded (72 did not meet inclusion criteria since they were not the primary caregiver - these parents indicated that they were less responsible for the care of the children than their partner after onset of COVID-19 restrictions - and 67 filled out the questionnaire only partially). See Tables 1 and 2 for demographics of included respondents and children (N = 254). The respondents consisted primarily of mothers (93%, n = 237), with a smaller participation of fathers (5%, n = 13) and relatives (2%, n = 4). The mean age of caregivers was 35.26 years (SD = 6.16). Half of the caregivers reported having a college degree or education beyond college (54%, n = 138). The majority of the children were attending regular pre-primary education before the lockdown (66%, n = 169) and many of them were also receiving therapeutic support (79%, n = 200). Half of the children were reported to have (or to be suspected of, in the case of ADHD features) a comorbid diagnosis.
Table 1.
Respondent demographic characteristics for the total sample (N = 254).
| Age (years): mean (±SD) | 35.26 (6.16) |
| Relation to the child: n (%) | |
| Mother | 237 (93.31) |
| Father | 13 (5.12) |
| Other | 4 (1.57) |
| Occupation: n (%) | |
| Student | 3 (1.18) |
| (Self-)Employed | 204 (80.31) |
| In receipt of benefits/disability | 17 (6.69) |
| Unsalaried absence of leave | 12 (4.72) |
| Other | 8 (3.15) |
| Unemployed | 10 (3.94) |
| Educational level: n (%) | |
| High school∗ or lower | 116 (45.67) |
| Higher education (non-university) | 94 (37.01) |
| Higher education (university) | 44 (17.32) |
| Work situation (BR/AR): n (%) | |
| Travel to work | 149 (58.66)/ 51 (20.08) |
| Sometimes working from home | 31 (12.20)/ 28 (11.02) |
| Always working from home | 16 (6.30)/ 70 (27.56) |
| Not currently working/sick leave/parent leave | 58 (22.83)/ 105 (41.34) |
Note. BR = Before COVID-19 Restrictions; AR = After COVID-19 Restrictions; ∗ High school in Belgium is commonly considered as 12 years of education starting at the age of 6.
Table 2.
Child demographic and home environment characteristics for total sample (N = 254).
| Age (years): mean (±SD) | 4.5 (0.98) |
| Co-occurring conditions: n (%)a | |
| Language condition | 46 (18.11) |
| DCD | 19 (7.48) |
| ID | 33 (12.99) |
| ADHD (condition/features) | 17 (6.69) |
| Genetic condition | 7 (2.76) |
| Education type: n (%) | |
| Regular pre-school | 169 (66.54) |
| Special pre-school | 84 (33.07) |
| Special boarding pre-school | 1 (0.39) |
| Therapeutic support BR: n (%)b | |
| Receiving support (yes) | 200 (78.74) |
| Type of support | |
| Rehabilitation centre | 88 (34.65) |
| Home guidance therapy | 94 (37.00) |
| Private therapy | 60 (23.62) |
| Other (school support/tutoring) | 42 (16.53) |
| Type of residence: n (%) | |
| Detached house | 75 (29.53) |
| Semi-detached house | 162 (63.78) |
| Flat <10 units building | 15 (5.91) |
| Flat >10 units building | 2 (0.79) |
| Home characteristics: n (%) | |
| Private space to play outside | 244 (96.06) |
| Private bedroom | 199 (78.35) |
| House with ≤2 bedroom(s) | 39 (15.35) |
| House with >2 bedrooms | 215 (84.65) |
| Number other children <18 years: n (%) | |
| ≤2 children <18 | 190 (74.80) |
| >2 children <18 | 64 (25.20) |
Note.a 122 parents reported that the child had more than one co-occurring condition; b 74 parents reported that the child received more than one type of therapeutic support; BR = Before COVID-19 Restrictions.
2.2. Procedure
The survey was distributed through the online platform Limesurvey (Limesurvey GmbH, 2017) during the early months of the pandemic between the 8th of April and 11th of May 2020. In total, the survey consisted of 110 questions of which 72 were considered for the present study. Most parents completed the survey in 20–30 min. As the government recommended people to isolate themselves at home as much as possible from the 16th of March onwards, the survey was advertised via digital platforms, such as Facebook, Instagram and organisational websites of several clinical services, home guidance services, parent associations and special education schools. There was no compensation provided. Ethical approval was received prior to data collection by the ethics committee of the Faculty of Psychology and Educational Sciences, Ghent University (Belgium) on the 7th of April 2020 (file number 2020/48).
2.3. Materials
2.3.1. Demographic and home environmental data
See Tables 1 and 2 for an overview of the variables included in the online survey.
2.3.2. Restricted and repetitive behaviours
RRBs were measured by an adapted version of the “Repetitive Behavior Scale-Revised” (RBS-R; Bodfish et al., 2000). The RBS-R is a 43-item informant-based questionnaire for measuring presence and severity of a variety of RRBs in individuals with autism. In line with previous psychometric findings (Lam and Aman, 2007; Mirenda et al., 2010), five subscales were retained in the present study: (a) Rituals/Sameness (17 items), (b) Self-injurious Behaviour (8 items), (c) Stereotypic Behaviour (6 items), (d) Compulsive Behaviour (8 items), and (e) Restricted Interests (4 items). Higher RBS-R subscale scores indicate more severe behaviours. Only subscale scores were included in the analyses since RRBs are not unidimensional and the total score is therefore difficult to interpret (Lam and Aman, 2007; Mirenda et al., 2010). After the author's permission, the original 4-point rating scale was adapted to a 7-point rating scale (1 = behaviour does not occur and 7 = behaviour occurs and is a severe problem) to enlarge score variation and enhance detection of differences in scores. Participants were asked to read an item on a certain behaviour and then choose the score that best described how present the behaviour had been before and after March 16th. Thus, caregivers completed the survey for each behaviour before the restrictions (BR) and after the restrictions (AR) in a sequence. This particular order was not only the most time-efficient (otherwise parents would have to go through the questionnaire twice) but also allowed the parent to visually evaluate changes on a rating scale for each specific behaviour. By expanding the rating scale, parents could also indicate more subtle changes. However, to avoid ‘leading questions’ it is important to mention that no direct questions on change in behaviours were asked, only presence of the behaviour before and after March 16th. In this study, the internal consistency of most RBS-R subscales ranged from acceptable to excellent (Cronbach's alpha's ranging from .73 to .91), which is in line with the internal consistency found in a previous study using the Dutch version of the RBS-R (Duvekot et al., 2017). With regard to the subscale Restricted Interests, consistent with previous research and given that this scale only consists of 4 items (Lam and Aman, 2007), its internal consistency BR and AR was questionable (.63 for both). Thus, findings on this subscale should be interpreted with caution and considered exploratory.
2.3.3. Co-occurring behavioural difficulties
Eight broad questions were included on (1) emotional symptoms (anxious or down e.g., easily upset, nervous or tense, easily offended), (2) inattention (difficulties with focussing e.g., can't concentrate, switches quickly from one activity to another), (3) hyperactivity (restless or hyperactive e.g., can't sit still, runs around a lot), (4) conduct behaviour (aggressive behaviour e.g., damages own property or property of others, angry tempers, beats a lot), (5) oppositional behaviour (e.g., is sometimes provocative, has angry temper, is stubborn, steering or irritable, does not cooperate), (6) physical complaints without clear medical cause (e.g., constipation, diarrhoea, headaches, nausea, abdominal pain, vomiting), (7) sleep difficulties (e.g., troubles to fall asleep, wakes up very often, nightmares, talks during sleep), and (8) eating difficulties (e.g., doesn't want to eat anymore, eats less, eats too much). These eight areas of behavioural difficulties were clearly defined to the parents and included the abovementioned examples to enhance differentiation between items. Participants had to indicate whether difficulties were “more”, “less” or “similar/equally” present after implementation of the COVID-19 restrictions. Children with no reported co-occurring difficulty, were excluded for analyses of the second research question. The questions were based on questions from the Child Behavior Checklist (CBCL; Dutch translation by Verhulst & van der Ende, Erasmus MC Rotterdam (1990)) for the ages 1.5–5 years (Achenbach and Rescorla, 2001) and the Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997; Dutch translation by Treffers and van Widenfelt (2005)) and adapted to the purpose of the present research.
2.4. Analysis
Statistical analyses were conducted with IBM SPSS version 25.0 (IBM Corp., 2017) and the statistical computing environment R (version 4.0.3; R Core Team, 2020).
First, since difference scores between the subscales BR and AR followed a non-normal distribution (based on both visual inspection of the histograms and Shapiro-Wilk tests), a Wilcoxon two-sample paired signed-rank test was conducted to examine if parents reported more RRBs AR. As an indication of the size of the effects, raw mean difference scores, standardized mean difference scores and standardized median differences scores in combination with the proportions of lower scores AR, proportions of equal scores and proportions of higher scores AR are provided. In order to test the robustness of the results, both paired sample t-tests and Wilcoxon paired signed-rank tests were additionally conducted on log-transformed data and added in Appendix 1. Given that for this first research question we had clear expectations about the direction of the expected effect and the fact that we conducted different comparisons, strict Bonferroni adjustments were applied to control for inflation of Type I error rate due to multiple comparisons (Bonferroni, 1936).
Second, Chi-square tests were conducted to investigate significant differences in percentages of children who exhibited less, similar or more co-occurring behavioural difficulties AR. Again, Bonferroni adjustments were applied to control for inflation of Type I error rate due to multiple comparisons (Bonferroni, 1936).
Third, for each RBS-R subscale a linear mixed-effects models was fitted. Each model included main effects of time (i.e., BR and AR), co-occurring condition, home environment, and co-occurring behavioural difficulties, as well as two-way interaction terms of time with the other variables. Given our aim to explore (1) the impact of co-occurring conditions and home environment on changes in RRBs, and (2) the association between changes in RRBs and changes in co-occurring behavioural difficulties due to COVID-19 restrictions, only the parameter estimates and corresponding tests of the two-way interaction terms were interpreted. Based on visual inspection of the histograms and the RR-plot and residual analyses it was clear that distributions of the subscales were positively skewed and (mainly for the subscale Self-injurious behaviour) error terms were not normally distributed – an assumption underlying linear regression models. In addition, given that these research questions were exploratory, the analyses were not interpreted as confirmatory hypothesis tests. In line with the exploratory nature of the research questions, we did not apply dichotomous null-hypothesis testing. Therefore, and because we aimed to form new hypotheses, we did not use any corrections with respect to type-I error inflation (like the conservative Bonferroni corrections). Thus, these results and especially the results with regard to the Self-injurious scale, need to be interpreted with caution. As a test for the robustness of the effects, analyses were also performed on log-transformed data and included in Appendix 2. Similar results were obtained with both approaches.
3. Results
3.1. Parent-reported RRBs before and after COVID-19 restrictions
Wilcoxon paired signed-rank tests indicated that parents reported significantly more RRBs on all RBS-R subscales AR. The largest raw mean difference score (i.e., 2.99), standardized mean difference score (i.e., 0.26) and standardized median difference score (i.e., 0.17) were found for Stereotypic Behaviour. The highest proportions of higher scores AR were found for both Stereotypic Behaviour (56.7%) and Rituals/Sameness (58.7%). The smallest raw difference score (i.e., 0.90), standardized mean difference score (i.e., 0.16) and standardized median difference score (i.e., 0.00) were found for Restricted Interests. See also Table 3. As a test for robustness of the effects, Wilcoxon paired signed-rank tests were also conducted on log-transformed data (see Appendix 1).
Table 3.
Mean differences in the RBS-R subscales BR and AR (N = 254).
| RBS-R subscale | BR Mean (SD) |
AR Mean (SD) |
Raw Mean Diff |
Stdz Mean Diff | Stdz Median Diff | V∗ | df (n) | p | Prop lower AR | Prop equal | Prop higher AR |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rituals/Sameness | 29.29 (10.78) | 32.06 (12.92) | 2.77 | 0.16 | 0.12 | 3588.5 | 254 | <.001 | 15.4 | 26.0 | 58.7 |
| Self-injurious | 11.03 (4.21) | 12.73 (6.83) | 1.70 | 0.21 | 0.12 | 775.5 | 254 | <.001 | 7.9 | 58.3 | 33.9 |
| Stereotypic | 19.21 (6.59) | 22.20 (9.34) | 2.99 | 0.26 | 0.17 | 1824.5 | 254 | <.001 | 9.4 | 33.9 | 56.7 |
| Compulsive | 11.98 (4.53) | 13.26 (5.69) | 1.28 | 0.18 | 0.14 | 939 | 254 | <.001 | 7.1 | 54.3 | 38.6 |
| Restricted Interests | 9.15 (3.65) | 10.05 (4.22) | 0.90 | 0.16 | 0.00 | 1242 | 254 | <.001 | 8.3 | 52.0 | 39.8 |
Note. RBS-R = Repetitive Behavior Scale-Revised; BR = Before COVID-19 Restrictions; AR = After COVID-19 Restrictions; Diff = Difference scores; Stdz = Standardized; Prop lower AR = proportions of lower scores after COVID-19 Restrictions; Prop equal = proportions of equal scores; Prop higher AR = proportions of higher scores after COVID-19 Restrictions; ∗ = Test Statistic of Wilcoxon paired signed-rank test; df = degrees of freedom; p-values significant after Bonferroni-correction (α = 0.05/4 =0.0125) are depicted in bold.
3.2. Parent-reported co-occurring behavioural difficulties before and after COVID-19 restrictions
Chi-square tests revealed that reported co-occurring difficulties increased significantly AR in 47–65% of the autistic children. Most children mainly showed more hyperactive, oppositional, emotional and aggressive behaviour. However, both physical complaints and eating difficulties remained similar in most of the children (52 and 48%, respectively). Importantly, in a smaller amount of children (ranging from 10 to 22%), co-occurring difficulties were reported to decrease AR. See also Table 4.
Table 4.
Differences in proportions of parents reporting less, similar or more co-occurring behavioural difficulties BR and AR.
| Co-occurring difficulties | N | Less (%) | Similar (%) | More (%) | χ2 | df | p-value | q-value (BH) |
|---|---|---|---|---|---|---|---|---|
| Emotional | 244 | 21 | 18 | 61 | 82.36 | 2 | <.001 | <.001 |
| Inattention | 245 | 10 | 40 | 50 | 63.12 | 2 | <.001 | <.001 |
| Hyperactivity | 241 | 12 | 23 | 65 | 114.63 | 2 | <.001 | <.001 |
| Conduct/Aggressive | 204 | 14 | 26 | 60 | 69.29 | 2 | <.001 | <.001 |
| Oppositional | 247 | 15 | 20 | 65 | 110.92 | 2 | <.001 | <.001 |
| Sleep | 204 | 15 | 38 | 47 | 32.85 | 2 | <.001 | <.001 |
| Physical | 143 | 22 | 52 | 26 | 23.89 | 2 | <.001 | <.001 |
| Eating | 218 | 12 | 48 | 40 | 45.53 | 2 | <.001 | <.001 |
Note. df = degrees of freedom; Q-value = adjusted p-value for the False Discovery Rate (FDR) or the proportion of false positives according to Benjamin Hochberg method; p-values significant after Bonferroni-correction (α = 0.05/8 = 0.00625) are depicted in bold.
3.3. Impact of co-occurring conditions and home environment on changes in RRBs due to COVID-19 restrictions
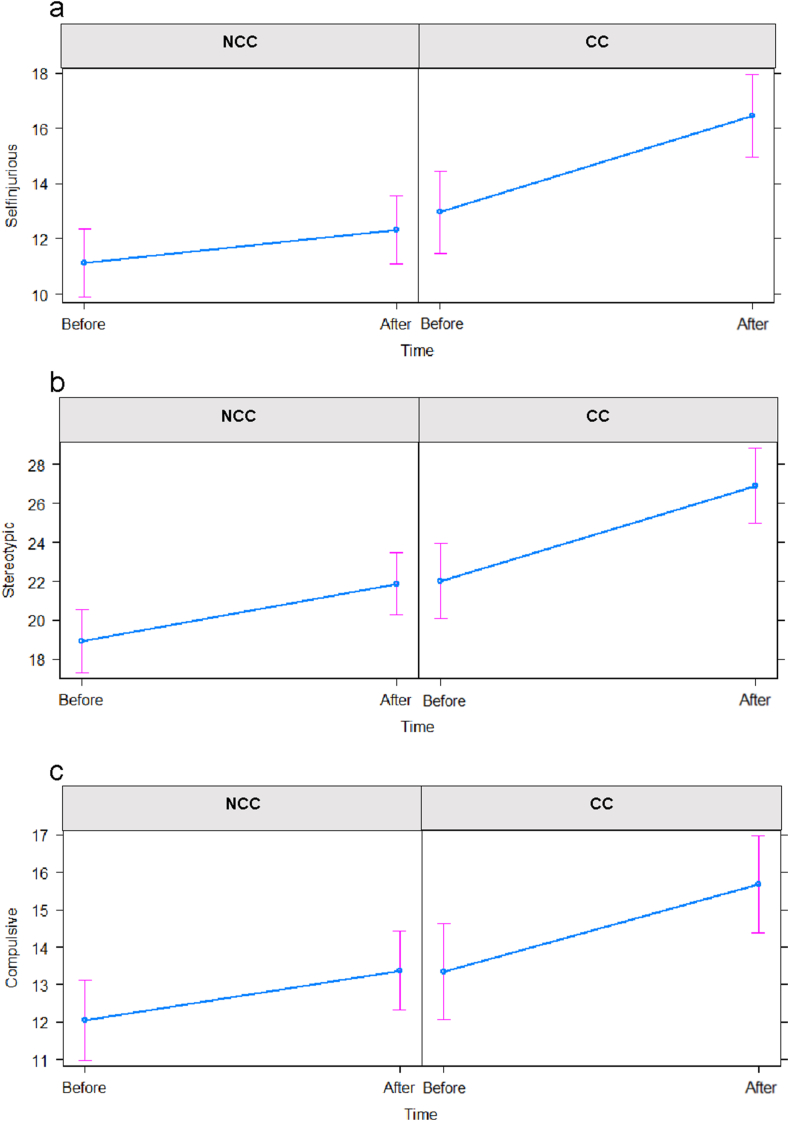
Two groups of autistic children with Co-occurring Conditions (CC; n = 100) and No Co-occurring Condition (NCC; n = 154) were distinguished. Linear mixed-effect models suggest that in all groups more self-injurious behaviours were reported. However, specific results suggest (χ2(1) = 7.97, p = .00) that the difference was smaller in NCC (BR: M = 11.13, 95%CI [9.90–12.37]; AR: M = 12.33, 95%CI [11.10–13.56]) compared to CC (BR: M = 12.95, 95%CI [11.46–14.44]; AR: M = 16.45, 95%CI [14.96–17.94]) (see also Figure 1a). In addition, both groups showed more stereotypic behaviours. However, the results suggest (χ2(1) = 4.53, p = .03) that the difference was smaller in NCC (BR: M = 18.91, 95%CI [17.31–20.51]; AR: M = 21.87, 95%CI [20.27–23.47]) compared to CC (BR: M = 22.02, 95%CI [20.09–23.95]; AR: M = 26.89, 95%CI [24.96–28.82]) (see also Figure 1b). Lastly, parents also reported more compulsive behaviours in both groups. However, the results suggest (χ2(1) = 3.99, p = .05) that the difference was smaller in NCC (BR: M = 12.04, 95%CI [10.98–13.11]; AR: M = 13.38, 95%CI [12.31–14.44]) compared to CC (BR: M = 13.35, 95%CI [12.06–14.63]; AR: M = 15.68, 95%CI [14.39–16.97]) (see also Figure 1c). Importantly, these results with regard to stereotypic and compulsive behaviours need to be cautiously interpreted since p-values of log-transformed data indicated low effects (see also Appendix 2).
Figure 1.
Interaction effects between Time and groups of children with Co-occurring Conditions (CC) and No Co-occurring Condition (NCC) for raw scores on RBS-R subscales Self-injurious (a), Stereotypic (b) and Compulsive Behaviour (c).
With regard to the impact of home environment, three groups were distinguished based on type of residence (detached = 75 children; semi/terrace = 162 children; flat = 17 children) and two groups based on children having a private room (n = 199) or not (n = 55). However, linear mixed-effect models suggest no interaction effects between characteristics of home environment and change in RRBs. See Table 5 for an overview of exploratory interaction effects and Appendix 2 for log-transformed analyses.
Table 5.
Linear mixed-effects models for each RBS-R subscale with main and interaction effects.
| Rituals/Sameness |
Self-injurious |
Stereotypic |
Compulsive |
Restricted |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | p | χ2 | df | p | χ2 | df | p | χ2 | df | p | χ2 | df | p | |
| Time | 3.83 | 1 | 0.05 | 0.93 | 1 | 0.34 | 4.40 | 1 | 0.03 | 3.33 | 1 | 0.07 | 5.14 | 1 | 0.02 |
| Co-occurring condition | 0.09 | 1 | 0.76 | 10.27 | 1 | 0.00 | 10.85 | 1 | 0.00 | 4.63 | 1 | 0.03 | 2.55 | 1 | 0.11 |
| Type Residence | 0.35 | 2 | 0.84 | 0.93 | 2 | 0.63 | 1.87 | 2 | 0.39 | 2.84 | 2 | 0.24 | 0.22 | 2 | 0.90 |
| Private Room | 2.27 | 1 | 0.13 | 0.09 | 1 | 0.76 | 0.73 | 1 | 0.39 | 0.40 | 1 | 0.53 | 0.00 | 1 | 0.97 |
| Emotional | 0.69 | 2 | 0.71 | 7.43 | 2 | 0.02 | 7.50 | 2 | 0.02 | 0.10 | 2 | 0.95 | 0.85 | 2 | 0.65 |
| Inattention | 2.92 | 2 | 0.23 | 0.78 | 2 | 0.68 | 3.32 | 2 | 0.19 | 7.57 | 2 | 0.02 | 4.28 | 2 | 0.12 |
| Hyperactivity | 0.42 | 2 | 0.81 | 0.47 | 2 | 0.79 | 1.18 | 2 | 0.55 | 4.56 | 2 | 0.10 | 3.46 | 2 | 0.18 |
| Aggressive | 0.11 | 2 | 0.94 | 0.02 | 2 | 0.99 | 1.92 | 2 | 0.38 | 0.32 | 2 | 0.85 | 0.35 | 2 | 0.84 |
| Oppositional | 0.45 | 2 | 0.80 | 0.64 | 2 | 0.72 | 6.24 | 2 | 0.04 | 2.34 | 2 | 0.31 | 0.85 | 2 | 0.65 |
| Sleep | 2.54 | 2 | 0.28 | 0.35 | 2 | 0.84 | 0.97 | 2 | 0.61 | 0.43 | 2 | 0.81 | 3.66 | 2 | 0.16 |
| Time x co-occurring cond. | 0.00 | 1 | 0.94 | 7.97 | 1 | 0.00 | 4.53 | 1 | 0.03 | 3.99 | 1 | 0.05 | 0.15 | 1 | 0.70 |
| Time x type residence | 3.30 | 2 | 0.19 | 0.96 | 2 | 0.62 | 0.35 | 2 | 0.84 | 1.08 | 2 | 0.58 | 1.38 | 2 | 0.50 |
| Time x private room | 0.70 | 1 | 0.40 | 0.16 | 1 | 0.69 | 1.16 | 1 | 0.20 | 0.04 | 1 | 0.84 | 0.15 | 1 | 0.70 |
| Time x emotional | 2.75 | 2 | 0.25 | 2.18 | 2 | 0.34 | 2.40 | 2 | 0.30 | 2.46 | 2 | 0.29 | 0.41 | 2 | 0.82 |
| Time x inattention | 7.96 | 2 | 0.02 | 3.60 | 2 | 0.17 | 5.99 | 2 | 0.05 | 4.66 | 2 | 0.10 | 6.10 | 2 | 0.05 |
| Time x hyperactivity | 8.86 | 2 | 0.05 | 0.10 | 2 | 0.95 | 2.06 | 2 | 0.36 | 2.00 | 2 | 0.37 | 6.74 | 2 | 0.03 |
| Time x aggressive | 2.07 | 2 | 0.36 | 4.95 | 2 | 0.84 | 2.08 | 2 | 0.35 | 2.90 | 2 | 0.23 | 1.43 | 2 | 0.49 |
| Time x oppositional | 1.17 | 2 | 0.56 | 0.91 | 2 | 0.63 | 1.73 | 2 | 0.42 | 1.86 | 2 | 0.39 | 0.74 | 2 | 0.69 |
| Time x sleep | 1.62 | 2 | 0.44 | 0.55 | 2 | 0.76 | 1.30 | 2 | 0.52 | 0.05 | 2 | 0.97 | 3.83 | 2 | 0.15 |
Note. χ2 = value of the type III Wald chi square; df = degree of freedom; p = p-value of the type III Wald chi square; Interpreted exploratory interaction effects are depicted in bold.
3.4. Association between changes in RRBs and changes in co-occurring difficulties due to COVID-19 restrictions
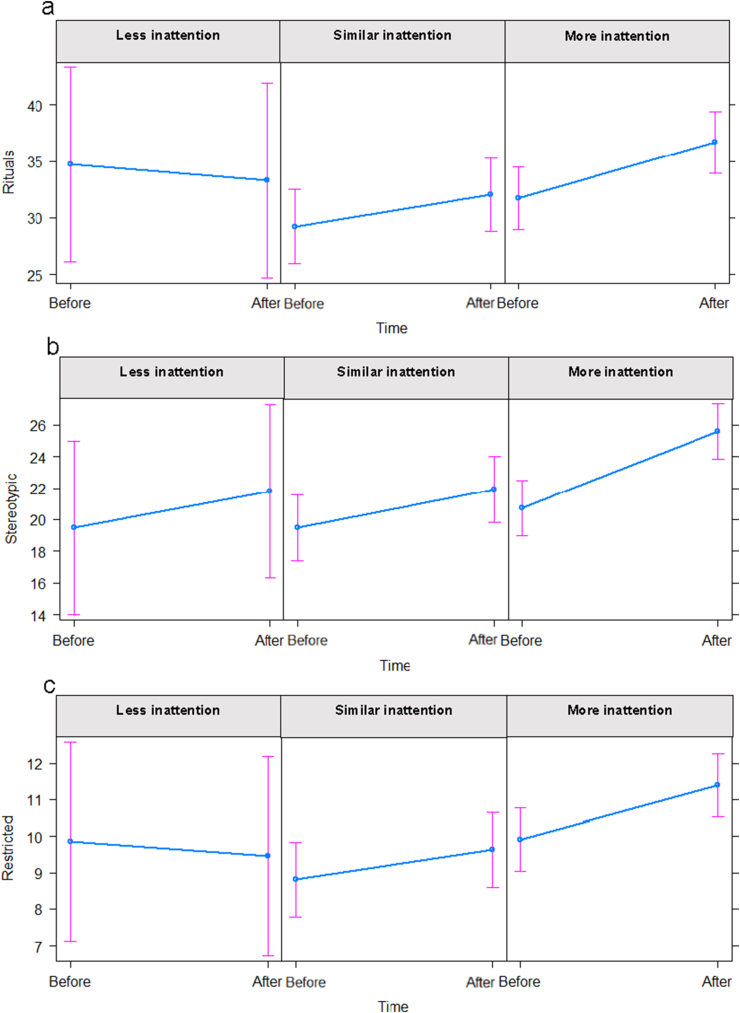
The results of the linear mixed-effects model suggest an interaction effect (χ2(2) = 7.96, p = .02) between inattention and Rituals/Sameness. More specifically, children who showed less inattention AR showed less ritualistic behaviours (M = 33.30; 95%CI [24.69–41.90]) than BR (M = 34.72; 95%CI [26.11–43.32]). In contrast, children who showed more inattention AR also showed more ritualistic behaviours (M = 36.67; 95%CI [33.91–39.42]) compared to BR (M = 31.72; 95%CI [28.97–34.48]). Children who showed similar inattention AR also showed more ritualistic behaviours (M = 32.05; 95%CI [28.78–35.31]) than BR (M = 29.22; 95%CI [25.95–32.49]), however, this difference is smaller compared to children who showed more inattention (see also Figure 2a).
Figure 2.
Interaction effects between Time and Inattention groups for raw scores on RBS-R subscales Rituals/Sameness (a), Stereotypic Behaviour (b) and Restricted Behaviour (c).
Further, the results suggest an interaction effect (χ2(2) = 5.99, p = .05) between inattention and Stereotypic Behaviour. Children who showed less inattention AR showed more stereotypic behaviours (M = 21.80; 95%CI [16.31–27.29]) than BR (M = 19.50; 95%CI [14.01–24.99]). Similarly, children who showed similar inattention AR showed more stereotypic behaviours (M = 21.90; 95%CI [19.81–23.98]) than BR (M = 19.49; 95%CI [17.41–21.58]). However, children who showed more inattention showed the largest difference in stereotypic behaviours (BR: M = 20.75; 95%CI [18.99–22.51]; AR: M = 25.57; 95%CI [23.81–27.33]) (see also Figure 2b).
Furthermore, the results also suggest an effect (χ2(2) = 6.10, p = .05) between inattention and Restricted Interests. Children who showed less inattention AR also showed less restricted interests (M = 9.40; 95%CI [6.73–12.18]) compared to BR (M = 9.85; 95%CI [7.13–12.58]). In contrast, children who showed more inattention AR also showed more restricted interests (M = 11.40; 95%CI [10.52–12.27]) than BR (M = 9.91; 95%CI [9.04–10.78]). Similarly, children who showed similar inattention AR also showed more restricted interests (M = 9.63; 95%CI [8.59–10.66]) than BR (M = 8.81; 95%CI [7.77–9.84]), however, this difference is smaller in comparison with children who showed more inattention AR (see also Figure 2c).
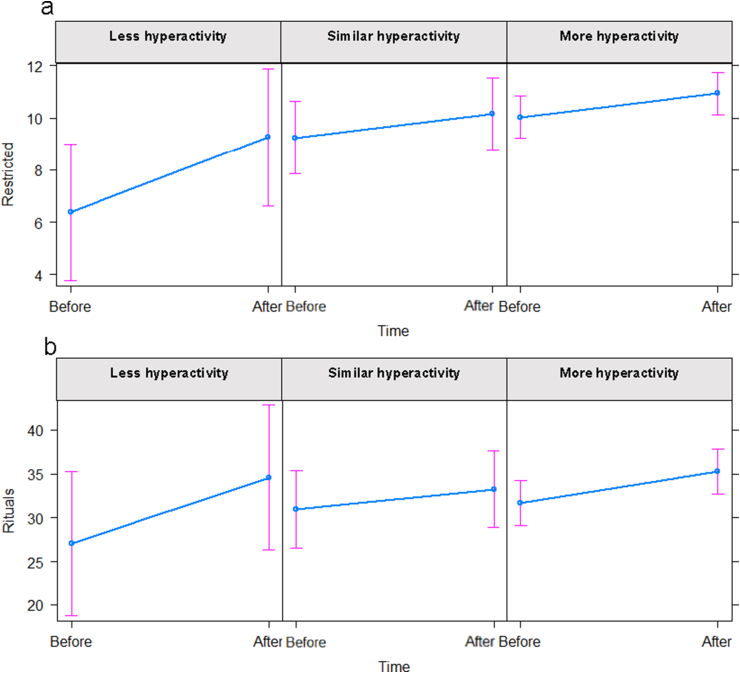
Further, the results suggest an effect (χ2(2) = 6.74, p = .03) between hyperactivity and restricted interests. Children who showed less hyperactivity AR showed more restricted behaviours (M = 9.25; 95%CI [6.64–11.87]) than BR (M = 6.39; 95%CI [3.78–9.01]). This difference was larger compared to children who showed similar hyperactivity (BR: M = 9.24, 95%CI [7.86–10.63]; AR: M = 10.16, 95%CI [8.78–11.55]) or more hyperactivity (BR: M = 10.03, 95%CI [9.22–10.85]; AR: M = 10.94, 95%CI [10.12–11.75]) (see also Figure 3a).
Figure 3.
Interaction effects between Time and Hyperactivity groups for raw scores on RBS-R subscales Restricted Behaviour (a) and Rituals/Sameness (b).
Lastly, the results also suggest an effect (χ2(2) = 8.86, p = .05) between hyperactivity and Ritualistic/Sameness. Children who showed less hyperactivity AR were reported to show more ritualistic behaviours (M = 34.57; 95%CI [26.32–42.83]) than BR (M = 27.01; 95%CI [18.76–35.27]). This difference was larger compared to differences in children who showed similar hyperactivity (BR: M = 30.97, 95%CI [26.60–35.34]; AR: M = 33.24, 95%CI [28.87–37.61]) or more hyperactivity (BR: M = 31.65, 95%CI [29.08–34.22]; AR: M = 35.23, 95%CI [32.66–37.80]) (see also Figure 3b). Importantly, these results regarding hyperactivity need to be interpreted with caution since p-values of log-transformed data indicated low effects. See Table 5 for an overview of exploratory interaction effects and Appendix 2 for log-transformed analyses.
4. Discussion
In the present study, we conducted a cross-sectional online survey to assess the parent-reported impact of the COVID-19 restrictions on the manifestation of restricted and repetitive behaviours (RRBs) in children with autism between 2.5 and 6 years old during the early months of the pandemic. Our results showed that the introduction of COVID-19 restrictions may have been associated with less optimal behavioural outcomes in young children with autism – specifically, parents reported that they noticed higher levels of stereotypic, self-injurious, compulsive and ritualistic behaviour, and more restricted interests. Evidence from previous clinical studies suggests that arousal is a key proximal trigger for RRBs (Leekam et al., 2011); thus, ritualistic behaviour could function as a self-regulating coping strategy in children with autism. This may help to regulate hyperarousal caused by changes in daily life routines. Further, stereotypic and self-injurious behaviour may compensate for a lack of stimulation or hypo-arousal linked to reduction in social connection, linked to COVID-19 restrictions.
In addition, our results demonstrate that primarily children with autism and a co-occurring condition display more self-injurious and stereotypic behaviour, after the introduction of the COVID-19 restrictions. This finding could be associated with the large proportion of children with a reported concurrent language impairment (i.e., 18%) and/or ID (i.e., 13%). In prior research, these co-occurring conditions seemed to be linked to repetitive motor actions and movements, and physical and/or sensory manipulation of objects (Esbensen et al., 2009; Leekam et al., 2011; Melo et al., 2020).
However, there was no association between characteristics of the home environment (i.e., type of residence and children having a private room) and the change in RRBs after COVID-19 restrictions. To the best of our knowledge, there is no existing empirical evidence reporting a link between characteristics of the home environment and RRBs.
Our results indicated that 47–65% of the parents noticed that their child displayed more co-occurring behavioural difficulties, after the introduction of COVID-19 restrictions, including emotional difficulties, inattention, hyperactivity, conduct or aggressive behaviour and oppositional behaviour, and sleep difficulties. The highest parent-reported increases were related to externalising behaviour. This is in line with previous evidence indicating that children and adolescents showed increased externalising behaviour during the lockdown, independent of diagnostic status (i.e., neurodevelopmental disorder or typical development; Bentenuto et al., 2021). Moreover, more than 50% of the pre-schoolers with autism in the present study showed higher levels of parent-reported anxiety symptoms and low mood. This is in line with prior research in older children and adolescents with autism (Amorim et al., 2020; Asbury et al., 2020). Our findings also support existing reports documenting the impact of COVID-19 restrictions on behavioural functioning in individuals with autism (3–29 years) more broadly (Colizzi et al., 2020; Levante et al., 2021; Mutluer et al., 2020).
With regard to the impact of co-occurring behavioural difficulties, our findings suggest that mainly children who experience increased inattentive behaviour after the onset of COVID-19 restrictions may show both more higher (i.e., more rituals and restricted interests) and lower order (i.e., stereotypies) RRBs. Furthermore, parents noticed more restricted interests in children who displayed less hyperactivity after the restrictions. Thus staying at home for a considerable amount of time may provide these children with more opportunities to be engaged with their preoccupations, leading to a potential decrease in hyperactivity. However, it is important to note that since the restrictive interests subscale of the RBS-R consists of only four items with relatively low internal consistency, these findings should be considered exploratory (Lam and Aman, 2007). Likewise, caution is needed when interpreting interaction effects since we did not have a baseline measure of the level of co-occurring behavioural difficulties prior to the start of the COVID-19 restrictions.
Finally, in a smaller proportion of children (ranging from 10 to 22%), parents noticed a decrease in co-occurring behavioural difficulties. Hence, in some children, a significant reduction in day-to-day obligations which provoke high levels of arousal might reduce the level of experienced behavioural difficulties. Similarly, a study by Asbury et al. (2020) indicated that a minority of parents of children with disabilities reported that the COVID-19 pandemic had a minimal impact on their child's mental health – with parents even reporting improvements in overall well-being for those who experienced difficulties in the school environment. It is important to note that in our sample, there was considerable variation in change in RRBs scores within this small group of children who displayed less co-occurring difficulties after the introduction of the restrictions. Thus, these interaction effects must be interpreted with caution (see also Figures 2 and 3).
4.1. Strengths and limitations
This study has several strengths, including: (i) the inclusion of very young children with autism, (ii) the focus on RRBs, which are currently understudied in the autism literature and are considered among the most challenging characteristics associated with autism as reported by parents (South et al., 2005), and (iii) the fact that the study was conducted during the very first weeks of lockdown which allowed us to immediately measure its direct impact. Furthermore, although the survey was distributed online, the current study represented parents with various degrees of education since almost half of them indicated 12 years of education or lower (“high school or lower”) as their highest educational level.
The main limitation of this study is that parents had to retrospectively report on the behaviour of their child before the introduction of the restrictions. In this respect, it is important to note that there may be several factors that impact the reliability of the baseline RRBs and therefore influence the internal validity of the results. First, there may be recall bias given that parents may not reliably recall their child's day-to-day behaviour with sufficient detail and accuracy from earlier in the year. Second, the reported behaviour could be influenced by parent exposure. With regard to changes in parenting habits, 64% of the caregivers indicated that the amount of care for their child remained the same after implementation of the COVID-19 restrictions. A subset of parents indicated an increase of care (i.e., 20%) or a decrease in care (i.e., 16%). In most families (i.e., 92%) there was no change in the parent who provided the most care to the child. Concerning work routines two out of five parents had to start working from home (increase of 22%) or had to stop working (increase of 18%) after implementation of the COVID-19 restrictions (see also Table 1). Therefore, in some of the parents, it could have been the case that they spent more time with their children leading to an increased awareness of RRBs and other behavioural difficulties almost certainly impacting their perception and thus ratings. Although we want to mention these general data on changes in parenting and work routines, we are aware that these provide only very limited information on the degree of disturbance in the areas of parenting, education, personal (mental and physical) and work routines which influence parent's perceptions. Finally, given the potentially adverse impact of the COVID-19 pandemic on caregivers' mental health, it is possible that parents reported their child's behaviour more negatively. With regard to the mixed-effect models that were used in the present study, it is important to note that the data did not meet all of the assumptions underlying linear regression models. Although there could be multiple strategies to analyse the data, for interpretability reasons, we chose to present the analysis using the raw data in the present study. Yet, similar results were obtained with log-transformed data. Given that the research questions related to the mixed-effect models were exploratory, the analyses were not interpreted as confirmatory hypothesis tests. In addition, no corrections for multiple testing were used to reduce the probability of missing possible explanations. Therefore, these results and especially the results with regard to the Self-injurious scale, need to be interpreted with caution and are only used to generate new research questions that should be tested confirmatory with independent data.
4.2. Implications
Several authors have already pointed to the potential negative impact of changes in daily-life routines and disruptions of regular services on children with autism linked to COVID-19 restrictions (Ameis et al., 2020; Kong, 2021). In our study, 33% of the children attended special education and 79% received different forms of therapeutic support before COVID-19 restrictions which have been abruptly interrupted during the first months of the pandemic. Similarly, White et al. (2021) found that particularly children under the age of five had the most severely disrupted services and lowest benefit of adaptations of regular interventions. Ensuring the continuity of care during the restrictions could be particularly relevant for pre-schoolers with autism, since previous studies demonstrated that intervening early is related to more progress in the current treatment process and more optimal long-term outcomes (Fuller and Kaiser, 2020). Moreover, at this young age, discontinuity of care may also increase risk of developmental stagnation or even regression (Boterberg et al., 2019). Furthermore, since RRBs are among the most stressful manifestations of autism (Bishop et al., 2007) and the COVID-19 pandemic itself evokes additional psychological distress (Asbury et al., 2020; Bentenuto et al., 2021; Kong, 2021), there is an increased need for psychological services for parents. Availability of such services through accessible means (e.g., telehealth programs or online platforms) may prevent these families from feeling further isolated during the ongoing pandemic.
In sum, the present results highlight the importance of having strategies ready for flexible implementation of accessible support services for potential future pandemic-related lockdowns, as well as the need to consider interventions for immediate post-pandemic applications (e.g., with solutions for in-person contact for critical therapies such as interventions including wearing a mouth-mask) focused on improving the well-being of families (Ameis et al., 2020; degli Espinosa et al., 2020; Narzisi, 2020a, 2020b; Sivaraman et al., 2021; White et al., 2021). Information concerning the possible impact of the restrictions on specific symptomatic manifestations of autism (i.e., RRBs) and other co-occurrent difficulties (e.g., inattention and hyperactivity) may be relevant to clinicians working with young children with autism. It may be useful to assess whether worsening in these areas has actually occurred and thus, provide further support and strategies to the parents or include these aspects in the current treatment of the child. Clinicians need to be alert to the impact of the restrictions, both during and immediately after periods of lockdowns and also later on when daily life routines are back to normal.
5. Conclusion
It is clear that RRBs persist pre and post COVID-19 restrictions in young children with autism as reported by parents. However, our findings demonstrate that the COVID-19 restrictions may increase restricted and repetitive behaviours (RRBs), as well as both internalising and externalising behaviours in children with autism, even at a very young age. These findings highlight the importance of flexible implementation and continuity of care for pre-schoolers with autism and support for their parents. Given the potentially negative impact of the COVID-19 restrictions at the very beginning of the pandemic, further clinical follow-up of the severity of RRBs and co-occurring behavioural difficulties is required to investigate if these behaviours returned to previous levels after the initial transition period of the lockdown was finished and how additional lockdown phases influenced these behaviours. This could further enhance our understanding of the long-term effects of sudden changes related to increased amount of time spent at home during the COVID-19 pandemic.
Declarations
Author contribution statement
Sofie Boterberg: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Arianna Zanatta: Conceived and designed the experiments; Performed the experiments; Wrote the paper.
Floor Moerman; Sarah Schaubroeck & Jasmine Siew: Conceived and designed the experiments; Performed the experiments.
Maarten Deschryver: Analyzed and interpreted the data.
Herbert Roeyers: Conceived and designed the experiments.
Funding statement
Sofie Boterberg and Floor Moerman are supported by the Research Foundation - Flanders, Belgium (SB: FWO-12Z8821N; FM: FWO-SBO-S001517N); Arianna Zanatta and Jasmine Siew are supported by the European Union's Horizon 2020 Research and Innovation Program - Marie Skłodowska Curie action (Call: H2020-MSCA-ITN-2018; Grant ID: 814302); Sarah Schaubroeck is supported by the relief fund Marguerite-Marie Delacroix Belgium. Funding sources had no involvement in study design, the collection, analysis or interpretation of data, the writing of the report and the decision to submit the article for publication.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
We are very grateful to the parents who participated in this study and to the community stakeholders and agency leaders who helped spreading the survey during this challenging period. Finally, we would also like to thank dr. Dries De Beer and dr. Jamie Cummins for their advice and help regarding the adaptations of the analyses during the revision of the manuscript.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Achenbach T.M., Rescorla L.A. University of Vermont, Research Center for Children; Youth, and Families: 2001. Manual for the ASEBA School-Age Forms & Profiles. [Google Scholar]
- Ameis S.H., Lai M.C., Mulsant B.H., Szatmari P. Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Mol. Autism. 2020;11(1):61. doi: 10.1186/s13229-020-00365-y. BioMed Central. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . fifth ed. American Psychiatric Publishing; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Amorim R., Catarino S., Miragaia P., Ferreras C., Viana V., Guardiano M. The impact of COVID-19 on children with autism spectrum disorder. Rev. Neurol. 2020;71(8):285–291. doi: 10.33588/rn.7108.2020381. [DOI] [PubMed] [Google Scholar]
- Asbury K., Fox L., Deniz E., Code A., Toseeb U. How is COVID-19 affecting the mental health of children with special educational needs and disabilities and their families? J. Autism Dev. Disord. 2020 doi: 10.1007/s10803-020-04577-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentenuto A., Mazzoni N., Giannotti M., Venuti P., de Falco S. Psychological impact of Covid-19 pandemic in Italian families of children with neurodevelopmental disorders. Res. Dev. Disabil. 2021;109(103840) doi: 10.1016/j.ridd.2020.103840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop S.L., Richler J., Cain A.C., Lord C. Predictors of perceived negative impact in mothers of children with autism spectrum disorder. Am. J. Ment. Retard. 2007;112(6):450–461. doi: 10.1352/0895-8017(2007)112[450:POPNII]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Bishop S.L., Richler J., Lord C. Association between restricted and repetitive behaviors and nonverbal IQ in children with Autism Spectrum Disorders. Child Neuropsychol. 2006;12(4–5):247–267. doi: 10.1080/09297040600630288. [DOI] [PubMed] [Google Scholar]
- Bodfish J.W., Symons F.J., Parker D.E., Lewis M.H. Varieties of repetitive behavior in autism: comparisons to mental retardation. J. Autism Dev. Disord. 2000;30(3):237–243. doi: 10.1023/a:1005596502855. [DOI] [PubMed] [Google Scholar]
- Bonferroni C.E. Pubblicazioni Del R Istituto Superiore Di Scienze Economiche e Commerciali Di Firenze. Vol. 8. 1936. Teoria statistica delle classi e calcolo delle probabilità; pp. 3–62. [Google Scholar]
- Boterberg S., Charman T., Marschik P.B., Bölte S., Roeyers H. Regression in autism spectrum disorder: a critical overview of retrospective findings and recommendations for future research. Neurosci. Biobehav. Rev. 2019;102:24–55. doi: 10.1016/j.neubiorev.2019.03.013. [DOI] [PubMed] [Google Scholar]
- Bury S.M., Hedley D., Uljarević M., Gal E. The autism advantage at work: a critical and systematic review of current evidence. Res. Dev. Disabil. 2020;105 doi: 10.1016/j.ridd.2020.103750. [DOI] [PubMed] [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci. 2020;10(6) doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke J.E., Eirich R., Racine N., Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatr. Res. 2020;292(113347) doi: 10.1016/j.psychres.2020.113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vaan G., Vervloed M.P.J., Knoors H., Verhoeven L. Profiles of stereotyped behaviour in people with combined sensory impairments and intellectual disabilities. Br. J. Vis. Impair. 2020;38(2):168–183. [Google Scholar]
- degli Espinosa F., Metko A., Raimondi M., Impenna M., Scognamiglio E. A model of support for families of children with autism living in the COVID-19 lockdown: lessons from Italy. Behav. Anal. Prac. 2020;13(3):550–558. doi: 10.1007/s40617-020-00438-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickie V.A., Baranek G.T., Schultz B., Watson L.R., McComish C.S. Parent reports of sensory experiences of preschool children with and without autism: a qualitative study. Am. J. Occup. Ther. 2009;63(2):172–181. doi: 10.5014/ajot.63.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duvekot J., van der Ende J., Verhulst F.C., Slappendel G., van Daalen E., Maras A., Greaves-Lord K. Factors influencing the probability of a diagnosis of autism spectrum disorder in girls versus boys. Autism. 2017;21(6):646–658. doi: 10.1177/1362361316672178. [DOI] [PubMed] [Google Scholar]
- Elsabbagh M., Divan G., Koh Y.J., Kim Y.S., Kauchali S., Marcin C., Montiel-Nava C., Patel V., Paula C.S., Wang C.Y., Yasamy M.T., Fombonne E. Global prevalence of autism and other pervasive developmental disorders. Autism Res. 2012;5(3):160–179. doi: 10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esbensen A.J., Seltzer M.M., Lam K.S.L., Bodfish J.W. Age-related differences in restricted repetitive behaviors in autism spectrum disorders. J. Autism Dev. Disord. 2009;39(1):57–66. doi: 10.1007/s10803-008-0599-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans G.W., Wells N.M., Moch A. Housing and mental health: a review of the evidence and a methodological and conceptual critique. J. Soc. Issues. 2003;59(3):475–500. [Google Scholar]
- Fuller E.A., Kaiser A.P. The effects of early intervention on social communication outcomes for children with autism spectrum disorder: a meta-analysis. J. Autism Dev. Disord. 2020;50(5):1683–1700. doi: 10.1007/s10803-019-03927-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriels R.L., Cuccaro M.L., Hill D.E., Ivers B.J., Goldson E. Repetitive behaviors in autism: relationships with associated clinical features. Res. Dev. Disabil. 2005;26(2):169–181. doi: 10.1016/j.ridd.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Goldman S.E., McGrew S., Johnson K.P., Richdale A.L., Clemons T., Malow B.A. Sleep is associated with problem behaviors in children and adolescents with Autism Spectrum Disorders. Res. Autism Spect. Disord. 2011;5(3):1223–1229. [Google Scholar]
- Goldman S., Wang C., Salgado M.W., Greene P.E., Kim M., Rapin I. Motor stereotypies in children with autism and other developmental disorders. Dev. Med. Child Neurol. 2009;51(1):30–38. doi: 10.1111/j.1469-8749.2008.03178.x. [DOI] [PubMed] [Google Scholar]
- Gonçalves A., Zuanazzi A.C., Salvador A.P., Jaloto A., Pianowski G., Carvalho L. Preliminary findings on the associations between mental health indicators and social isolation during the COVID-19 pandemic. Arch. Psychiatr. Psychother. 2020;22(2):10–19. [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: a research note. JCPP (J. Child Psychol. Psychiatry) 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Gotham K., Bishop S.L., Hus V., Huerta M., Lund S., Buja A., Krieger A., Lord C. Exploring the relationship between anxiety and insistence on sameness in autism spectrum disorders. Autism Res. 2013;6(1):33–41. doi: 10.1002/aur.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrop C., McConachie H., Emsley R., Leadbitter K., Green J., PACT Consortium. Restricted and repetitive behaviors in autism spectrum disorders and typical development: cross-sectional and longitudinal comparisons. J. Autism Dev. Disord. 2014;44(5):1207–1219. doi: 10.1007/s10803-013-1986-5. [DOI] [PubMed] [Google Scholar]
- Hochhauser M., Engel-Yeger B. Sensory processing abilities and their relation to participation in leisure activities among children with high-functioning autism spectrum disorder (HFASD) Res. Autism Spect. Disord. 2010;4(4):746–754. [Google Scholar]
- Honey E., Leekam S., Turner M., McConachie H. Repetitive behaviour and play in typically developing children and children with autism spectrum disorders. J. Autism Dev. Disord. 2007;37(6):1107–1115. doi: 10.1007/s10803-006-0253-4. [DOI] [PubMed] [Google Scholar]
- Hundley R.J., Shui A., Malow B.A. Relationship between subtypes of restricted and repetitive behaviors and sleep disturbance in autism spectrum disorder. J. Autism Dev. Disord. 2016;46(11):3448–3457. doi: 10.1007/s10803-016-2884-4. [DOI] [PubMed] [Google Scholar]
- IBM Corp . IBM Corp; 2017. IBM SPSS Statistics for Windows. Version 25.0. [Google Scholar]
- Kong M. What COVID-19 means for non-neurotypical children and their families. Pediatr. Res. 2021;89(3):396–397. doi: 10.1038/s41390-020-0913-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam K.S.L., Aman M.G. The repetitive behavior scale-revised: independent validation in individuals with autism spectrum disorders. J. Autism Dev. Disord. 2007;37(5):855–866. doi: 10.1007/s10803-006-0213-z. [DOI] [PubMed] [Google Scholar]
- Lane A.E., Young R.L., Baker A.E.Z., Angley M.T. Sensory processing subtypes in autism: association with adaptive behavior. J. Autism Dev. Disord. 2010;40(1):112–122. doi: 10.1007/s10803-009-0840-2. [DOI] [PubMed] [Google Scholar]
- Leekam S., Prior M.R., Uljarevic M. Restricted and repetitive behaviors in autism spectrum disorders: a review of research in the last decade. Psychol. Bull. 2011;137(4):562–593. doi: 10.1037/a0023341. [DOI] [PubMed] [Google Scholar]
- Leekam S., Tandos J., McConachie H., Meins E., Parkinson K., Wright C., Turner M., Arnott B., Vittorini L., Couteur A. Le. Repetitive behaviours in typically developing 2-year-olds. J. Child Psychol. Psychiatry Allied Discip. 2007;48(11):1131–1138. doi: 10.1111/j.1469-7610.2007.01778.x. [DOI] [PubMed] [Google Scholar]
- Levante A., Petrocchi S., Bianco F., Castelli I., Colombi C., Keller R., Narzisi A., Masi G., Lecciso F. Psychological impact of COVID-19 outbreak on families of children with autism spectrum disorder and typically developing peers: an online survey. Brain Sci. 2021;11(6):808. doi: 10.3390/brainsci11060808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidstone J., Uljarević M., Sullivan J., Rodgers J., McConachie H., Freeston M., Le Couteur A., Prior M., Leekam S. Relations among restricted and repetitive behaviors, anxiety and sensory features in children with autism spectrum disorders. Res. Autism Spect. Disord. 2014;8(2):82–92. [Google Scholar]
- Limesurvey GmbH . 2017. LimeSurvey: an Open Source Survey Tool. LimeSurvey GmbH.http://www.limesurvey.org [Google Scholar]
- Lord C., Brugha T.S., Charman T., Cusack J., Dumas G., Frazier T., Jones E.J.H., Jones R.M., Pickles A., State M.W., Taylor J.L., Veenstra-VanderWeele J. Autism spectrum disorder. Nat. Rev. Dis. Prim. 2020;6(1):5. doi: 10.1038/s41572-019-0138-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald R., Green G., Mansfield R., Geckeler A., Gardenier N., Anderson J., Holcomb W., Sanchez J. Stereotypy in young children with autism and typically developing children. Res. Dev. Disabil. 2007;28(3):266–277. doi: 10.1016/j.ridd.2006.01.004. [DOI] [PubMed] [Google Scholar]
- MacDuffie K.E., Munson J., Greenson J., Ward T.M., Rogers S.J., Dawson G., Estes A. Sleep problems and trajectories of restricted and repetitive behaviors in children with neurodevelopmental disabilities. J. Autism Dev. Disord. 2020;50(11):3844–3856. doi: 10.1007/s10803-020-04438-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melo C., Ruano L., Jorge J., Pinto Ribeiro T., Oliveira G., Azevedo L., Temudo T. Prevalence and determinants of motor stereotypies in autism spectrum disorder: a systematic review and meta-analysis. Autism. 2020;24(3):569–590. doi: 10.1177/1362361319869118. [DOI] [PubMed] [Google Scholar]
- Mirenda P., Smith I.M., Vaillancourt T., Georgiades S., Duku E., Szatmari P., Bryson S., Fombonne E., Roberts W., Volden J., Waddell C., Zwaigenbaum L. Validating the repetitive behavior scale-revised in young children with autism spectrum disorder. J. Autism Dev. Disord. 2010;40(12):1521–1530. doi: 10.1007/s10803-010-1012-0. [DOI] [PubMed] [Google Scholar]
- Moss J., Richards C., Nelson L., Oliver C. Prevalence of autism spectrum disorder symptomatology and related behavioural characteristics in individuals with Down syndrome. Autism. 2013;17(4):390–404. doi: 10.1177/1362361312442790. [DOI] [PubMed] [Google Scholar]
- Mutluer T., Doenyas C., Aslan Genc H. Behavioral implications of the covid-19 process for autism spectrum disorder, and individuals’ comprehension of and reactions to the pandemic conditions. Front. Psychiatr. 2020;11(561882) doi: 10.3389/fpsyt.2020.561882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagib W., Williams A. Toward an autism-friendly home environment. Hous. Stud. 2017;32(2):140–167. [Google Scholar]
- Narzisi A. Handle the autism spectrum condition during coronavirus (Covid-19) stay at home period: ten tips for helping parents and caregivers of young children. Brain Sci. 2020;10(4):207. doi: 10.3390/brainsci10040207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi A. Phase 2 and later of COVID-19 lockdown: is it possible to perform remote diagnosis and intervention for autism spectrum disorder? An online-mediated approach. J. Clin. Med. 2020;9(6):1850. doi: 10.3390/jcm9061850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozsivadjian A., Knott F., Magiati I. Parent and child perspectives on the nature of anxiety in children and young people with autism spectrum disorders: a focus group study. Autism. 2012;16(2):107–121. doi: 10.1177/1362361311431703. [DOI] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; 2020. R: A Language and Environment for Statistical Computing.https://www.r-project.org/ [Google Scholar]
- Richler J., Huerta M., Bishop S.L., Lord C. Developmental trajectories of restricted and repetitive behaviors and interests in children with autism spectrum disorders. Dev. Psychopathol. 2010;22(1):55–69. doi: 10.1017/S0954579409990265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers J., Glod M., Connolly B., McConachie H. The relationship between anxiety and repetitive behaviours in autism spectrum disorder. J. Autism Dev. Disord. 2012;42(11):2404–2409. doi: 10.1007/s10803-012-1531-y. [DOI] [PubMed] [Google Scholar]
- Russell G., Kapp S.K., Elliott D., Elphick C., Gwernan-Jones R., Owens C. Mapping the autistic advantage from the accounts of adults diagnosed with autism: a qualitative study. Autism Adulthood. 2019;1(2):124–133. doi: 10.1089/aut.2018.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar F., Baird G., Chandler S., Tseng E., O’sullivan T., Howlin P., Pickles A., Simonoff E. Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. J. Autism Dev. Disord. 2015;45(8):2283–2294. doi: 10.1007/s10803-015-2361-5. [DOI] [PubMed] [Google Scholar]
- Shuster J., Perry A., Bebko J., Toplak M.E. Review of factor analytic studies examining symptoms of autism spectrum disorders. J. Autism Dev. Disord. 2014;44(1):90–110. doi: 10.1007/s10803-013-1854-3. [DOI] [PubMed] [Google Scholar]
- Sivaraman M., Virues-Ortega J., Roeyers H. Telehealth mask wearing training for children with autism during the COVID-19 pandemic. J. Appl. Behav. Anal. 2021;54(1):70–86. doi: 10.1002/jaba.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L., Jacob L., Yakkundi A., McDermott D., Armstrong N.C., Barnett Y., López-Sánchez G.F., Martin S., Butler L., Tully M.A. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: a cross-sectional study of UK-based respondents. Psychiatr. Res. 2020;291(113138) doi: 10.1016/j.psychres.2020.113138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South M., Ozonoff S., McMahon W.M. Repetitive behavior profiles in asperger syndrome and high-functioning autism. J. Autism Dev. Disord. 2005;35(2):145–158. doi: 10.1007/s10803-004-1992-8. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky D.G., Scahill L., Gadow K.D., Arnold L.E., Aman M.G., McDougle C.J., McCracken J.T., Tierney E., Williams White S., Lecavalier L., Vitiello B. Parent-rated anxiety symptoms in children with pervasive developmental disorders: frequency and association with core autism symptoms and cognitive functioning. J. Abnorm. Child Psychol. 2008;36(1):117–128. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- Szatmari P., Georgiades S., Bryson S., Zwaigenbaum L., Roberts W., Mahoney W., Goldberg J., Tuff L. Investigating the structure of the restricted, repetitive behaviours and interests domain of autism. JCPP (J. Child Psychol. Psychiatry) 2006;47(6):582–590. doi: 10.1111/j.1469-7610.2005.01537.x. [DOI] [PubMed] [Google Scholar]
- Tsai C.H., Chen K.L., Li H.J., Chen K.H., Hsu C.W., Lu C.H., Hsieh K.Y., Huang C.Y. The symptoms of autism including social communication deficits and repetitive and restricted behaviors are associated with different emotional and behavioral problems. Sci. Rep. 2020;10(1):1–8. doi: 10.1038/s41598-020-76292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner M. Annotation: repetitive behaviour in autism: a review of psychological research. JCPP (J. Child Psychol. Psychiatry) 1999;40(6):839–849. [PubMed] [Google Scholar]
- Walker D.R., Thompson A., Zwaigenbaum L., Goldberg J., Bryson S.E., Mahoney W.J., Strawbridge C.P., Szatmari P. Specifying PDD-NOS: a comparison of PDD-NOS, asperger syndrome, and autism. J. Am. Acad. Child Adolesc. Psychiatr. 2004;43(2):172–180. doi: 10.1097/00004583-200402000-00012. [DOI] [PubMed] [Google Scholar]
- White L.C., Law J.K., Daniels A.M., Toroney J., Vernoia B., Xiao S., Feliciano P., Chung W.K., Abbeduto L., Aberbach G., Aberle S., Acampado J., Ace A., Ahlers K., Albright C., Alessandri M., Alvarez N., Amaral D., Amatya A.…White-Lehman L.C. Brief report: impact of COVID-19 on individuals with ASD and their caregivers: a perspective from the SPARK cohort. J. Autism Dev. Disord. 2021:1–8. doi: 10.1007/s10803-020-04816-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. WHO Director-General’s Opening Remarks at the media Briefing on COVID-19 - 11 March 2020. 11 March.https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- Zandt F., Prior M., Kyrios M. Repetitive behaviour in children with high functioning autism and obsessive compulsive disorder. J. Autism Dev. Disord. 2007;37(2):251–259. doi: 10.1007/s10803-006-0158-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.